Abstract
Background
According to International Convention on the Right of Person with Disabilities (CRPD), all nations should discern Sexual and Reproductive Health (SRH) as human rights and needs of all people living with disabilities. Women and girls with disabilities are highly vulnerable to SRH disparities including unintended pregnancy, acquiring sexual transmitted infections and unsafe abortion. Little has known about SRH service uptake and influencing factors among reproductive aged women living with disabilities.
Methods
A community-based cross-sectional study was conducted from January 1–30, 2021, the central Gondar zone selected districts. A total of 535 reproductive-age (18–49 years) women with disabilities had been interviewed through face-to-face using structured questionnaire. Multistage cluster sampling method was applied. A binary logistic regression model was computed to look the relationship between independent variables and uptake of SRH, and p-value < 0.05 was a cut-off point to declare statistical significance.
Results
A total of 33.27% (178/535) women with disabilities used at least one SRH service in the last twelve months preceding the survey. Those who had three or more children [AOR = 4.85; 95% CI (1.24–9.71)], autonomy to visit health care facilities [AOR = 3.30; 95% CI (1.45–6.92)], lived with sexual partner [AOR = 9.2; 95% CI (2.84–13.60)], subjected to radio/television in daily bases [AOR = 5.9; 95% CI (1.26–13.04)], autonomy to visit friends and relatives [AOR = 3.95; 95% CI (1.28–12.17)], had a discussion with family members about sexual and reproductive health [AOR = 9.36; 95% CI (3.44–17.47)], and engaged in sexual activity after the age of 18 years [AOR = 7.2; 95% CI (2.51–14.45)] were important predictors for service uptake.
Conclusions
Only one in three reproductive age women with disabilities used at least one SRH service. These findings suggest that accessing information through mainstream media exposure, having full autonomous to visit friends and families, open discussion with family members, live with sexual partner, having optimal family size and starting sexual act at the recommended age improve the uptake of SRH services. Therefore, the stakeholders (both governmental and non-governmental) need to make efforts to increase the uptake of SRH services.
Keywords: Disabilities, Reproductive-aged, SRH, Uptake, Women
Background
The World Health Organization (WHO) defined disability in many ways but generally refers to any casualty that prevents an individual from living their normal life. It includes people who are blind, deaf, physically disabled, intellectually impaired, or disabilities related to mental health. Disability is also explained as difficulties in any or all three areas of functioning: impairment, activity limitation and participation restriction [1, 2]. Around 15% of the world’s population or estimated more than a billion people live with disabilities, of whom 200 million experience considerable difficulties in functioning in daily life, and approximately 80% are living in developing countries [3]. Globally, there is a significant difference in the prevalence of disability between men and women: the male disability prevalence rate is 12% while the female is 19.2% [3, 4]. The World Bank and WHO estimated that there are about 15 million people living with disabilities in Ethiopia, standing for 17.6% of the population, and 14.0% in the Amhara region. However, this figure is agreed to be extremely low by different actors working in the area [5].
Disability is a human right issue; because people with disability experience inequalities in access to health care and education and subjected to violation of dignities like violence and abuse [6, 7]. Visually impaired teenagers are not well informed about prevention mechanism of unplanned pregnancy and sexually transmitted infections when they engage in pre-marital sexual acts [8]. Since Sexual and Reproductive Health (SRH) is being a significant part of health for sustainable development [9], many resource-limited countries have focused and set prevention strategies on the practice of unsafe sex, abortions, sexual transmitted infections including Human Immunodeficiency Virus (HIV), gender-based violence and other risk factors for adverse pregnancy outcomes [10, 11]. A population-based study conducted in Canada, Ontario revealed that, when women with disabilities have low accessibility and utilization of SRH programs and information may have poor preconception health [12]. The evidence from Northern Ireland has shown that family planning services do not adequately meet the needs of disabled clients because clinics are inaccessible in terms of physical access, informational exposure/access, and service provision. Social perspective on disabled people thought like they are asexual and not need to avail of reproductive health services including family planning [13]. In addition, SRH services are often inaccessible because of many reasons including stigma and discrimination, physical barriers, lack of accessible information and communication materials, health care providers’ negative attitudes and lack of disability related clinical services [14]. Qualitative study among women with hearing impairment (deaf) showed that inconsistent communication access and difficult in accessing health information were the barriers to get best pregnancy related care services [15]. Health providers who often assume disabled women are not sexually active, do not screen them for sexually transmitted infections (STIs), and do not provide contraceptives services and information about STIs including HIV. This exclusion has been found to be especially prevalent in many developing countries [14, 16]. United Nations General Assembly Convention article 25 stated that persons with disabilities have equal rights to SRH with nondisabled. This is important to achieve a Sustainable Development Goal (SDG) and create a truly inclusive society. However, the full number of SRH issues for women with disabilities is not yet clearly written, and highly unmet [17].
The SDG has striven to ensure ‘no one is left behind’ by promoting a stronger focus on disability. Accessing sexual and reproductive health services and reproductive rights for all persons with disabilities (targets 3.7 and 5.6) have been among the agendas of United Nation (UN) as SDG which could be achieved by 2030. Women with disabilities have the same SRH needs as women without disabilities. People with disabilities are among the most marginalized and disadvantaged by the community, and even by their family. They face physical, social, and attitudinal barriers in taking part as equal members of society and accessing community resources like health facilities in every part of their life, predominantly SRH services. However, few studies have been done on the real problems/gaps on SRH related issues. Thus, this study aimed to determine the prevalence of SRH service use and identify associated factors among reproductive age women with disabilities in Northwest Ethiopia.
Methods
Study setting, design and period
Community based cross-sectional study design was employed in Central Gondar zone of Amhara regional state which is found 748 Km to the Northwest of Addis Ababa, the capital city of Ethiopia. This zone has 15 woredas (districts) and one administrative town. According to Central Gondar zone reports related to risk exposure community of the year 2019/20 has shown that 5624 people lived with disabilities, and of these 2661 were females. Mi’irab Belesa, Gondar Zuria and Tach Armachiho were the three leading woredas reported high number of females living with disabilities [18]. The data was collected from January 1, 2021, to January 30, 2021.
Source and study population
All visual and hearing impaired, and physical disabled women in the age range of 18 to 49 years in Central Gondar Zone were source population and those who lived in selected districts were study populations.
Inclusion and exclusion criteria/s
Those reproductive age women (18–49 years) who had hearing and visual impairment, and physically disabled were included while seriously ill at the time of data collection were excluded. Interviewing intellectually/developmentally disabled people is challenging due to their limited communication abilities and difficulty in sustaining attention and concentration. Thus, the process requires excessive cost, time and experts.
Sample size determination, sampling technique and procedure
To estimate the sample size of this study, single population proportion formula has used, where P = proportion of family planning utilization among reproductive aged disabled women in Arbaminch, Ethiopia was 33.7% [19], 95% confidence interval, 5% marginal error, considering 10% non-response rate and 1.5 design effect. Then, the final sample size with this assumption was 567. A multi-stage cluster sampling technique was applied. Clusters were chosen at random and every disabled woman in selected cluster was sampled.
Seven (7) woredas had been selected by lottery method and the total sampled participants were allocated proportionally based on the previous year’s number of disabilities reported by Central Gondar zone, social and labor office. Alefa, Aykel, Gondar Zuria, Misirak Dembiya, Chilga Kutir 1, Mi’irab Belesa, and Wegera woreda were selected. Again, the distributed sample size was distributed proportionally for each Kebele (smallest administrative unit in Ethiopia) and Gotts (governmental structure below kebele level in rural administrative structure which is similar with “Ketena” in urban administrative structure). All vision, hearing and physically disabled individuals aged 18–49 years in the households from selected areas had been included to this study.
Study variables
Utilization of SRH service was the outcome variable, whereas, background characteristics; age, marital status, religion, occupation, educational level, partner occupation, educational level of spouse, residence, currently where she lives, family size, with whom she lives, forms of disability, membership, and decision- making characteristics; membership to disability association, availability of support, living situation, exposure to medias, forms of disability and autonomy to visit health facilities, families, and other relatives, and reproductive health history, service information and access related variables like; age of menarche, ever have sex, age when have first sexual intercourse, sources of information about where to use and access SRH services source of information, and materials accessible in appropriate format were the explanatory variables.
Operational definition
Utilization of SRH services
Appropriate package of one or more of SRH services (modern family planning, maternal care, cervical cancer screening, HIV/AIDS testing and other STIs screening, abortion/post abortion care) can be obtained by the women from pharmacy, health institutions (private or governmental), community-based distribution (rarely practiced in this study setting) or some other sources. Women who used at least one SRH service from the list five components considers as used the service. The question was forwarding like “Have you used at least one SRH services from the five components in the last 12 months preceding to the study?”, which was self-reported, and the list of the services had been validated by reminding the components [20, 21].
Data collection tools and procedures
The women with disability had been screened from general population using rapid assessment disability (RAD) tool which was adapted from Washington Group for disability statistics to identify disabled women [22]. This tool includes a small number of questions and is recommended for use in community surveys because of its simplicity to overcome the practical and conceptual difficulties in measuring disability. Then, those identified vision, hearing or physically disabled women were further interviewed about SRH service utilization and associated factors. Some steps were involved in developing data collection tool (questionnaire). These were; setting the research aim, defining the target participants, deciding the research method to reach out the participants, content the questionnaire need to be included, and develop the questions in meaningful order and format. The tool was adapted from previous literatures [23–30]. These interviewers administer paper questionnaire used to gather/collect the primary data from the study participants. Since some questions were sensitive to ask in the study setting culture, interviewers were matched for gender. Interview was taking place in locations with privacy, such as closed rooms or quiet places in the house/institution. Fourteen (14) data collectors and 7 supervisors were recruited. Data collection was facilitated by experts in special need education and who had adequate prior experience of data collection in similar surveys. Additionally, professional sign language interpreters were involved. Both data collectors and supervisors had been trained for one day in interviewing techniques, purpose of the study, importance of privacy, and how to use questionnaires with practical demonstration.
Data analysis and presentation
The collected data checked for completeness, coded, and then entered into Epi Data version 3.1 software and exported to SPSS (Statistical Package for Social Sciences) version 21 Software for analysis. Data organized and presented using tables, graphs, charts. Bivariable and multivariable logistic regression were performed to find statistically significant variables using a cut-off p < 0.2 in the bivariable analysis to identify candidate variables for multivariable logistic regression [31–33]. Adjusted odds ratio with 95% confidence interval used to declare statistically significant variables based on p < 0.05 in the multivariable logistic regression model. The Hosmer-Lemeshow test was performed to check the goodness of fit test and the decision was made at p > 0.05.
Data quality management
The questionnaire was adapted from previous literatures conducted in various parts of the world. There was detailed communication with senior researchers, and experts in reproductive health and special need about the entire paper and check its theoretical validity, and their comments were considered. The questionnaire was translated from English to local language (Amharic) via forward and backward translation by experts in both languages. Besides, intensive training was provided to all interviewers and supervisors. Sign language experts took part in data collection during the interview of deaf participants. The questionnaire was pre-tested before the start of actual data collection on 5% (29 study subjects) of the total required sample size in Gondar city which was not selected as study area. Filled out questionnaires have been checked for completeness and its consistency every night at the time of data collection and incomplete questionnaires were sent back to the data collector for check-up under supervision. Based on the pretest results; clarity, wording, logical sequence, and skip patterns of the questions were amended.
Results
Background related characteristics
A total of 535 disabled reproductive age women were participated in this study with a response rate of 94.35%. More than two-fifths (42.1%) of the study participants were found in the age range of 35–49 years, and the mean age of them was 31.46 years (SD ± 8.93). More than half (54.6%) of the study participants were unable to read and write, and more than three-fourths.
(87.7%) of the study participants were orthodox religion followers. Most of the study participants (362/535) lived in the rural part of the study area. Regarding the employment and marital status; only 19 (3.6%) disabled participants were governmental employee and 129 (24.1) were married. Of those who were married, more than one-third (34.05%) of their sexual partners were unable to read and write, and half (49.72%) of their partner were farmers. Three-hundred nineteen (59.6%) study participants had three or more household members, and 45% (241/535) of the participants had no live child (Table 1).
Table 1.
Background characteristics of reproductive-age women with disabilities in Northwest Ethiopia, 2021 (N = 535)
| Variables | Category | Frequency | Percent (%) |
|---|---|---|---|
| Age in years | 18–24 | 176 | 32.9 |
| 25–34 | 134 | 25.0 | |
| 35–49 | 225 | 42.1 | |
| Educational level | Unable to read and write | 292 | 54.6 |
| Able to read and/or write | 49 | 9.2 | |
| Elementary (1–8 grades) | 107 | 20.0 | |
| High school (9–12 grades) | 50 | 9.3 | |
| College and above | 37 | 6.9 | |
| Religion | Orthodox | 469 | 87.7 |
| Muslim | 66 | 12.3 | |
| Resident | Urban | 173 | 32.3 |
| Rural | 362 | 67.7 | |
| Current employment | Housewife | 177 | 33.1 |
| Governmental Employee | 19 | 3.6 | |
| Merchant/Private business | 77 | 14.4 | |
| Regularly beg from others | 87 | 16.3 | |
| Student | 105 | 19.6 | |
| Get supported from family members | 48 | 9 | |
| Daily laborer | 22 | 4.1 | |
| Current sexual relationship status | Married | 129 | 24.1 |
| Cohabitant or boyfriend | 56 | 10.5 | |
| Widowed | 116 | 21.7 | |
| Single | 32 | 6.0 | |
| Divorced | 202 | 37.8 | |
| Sexual partner educational level (N = 185) | Unable to read and write | 63 | 34.05 |
| Able to read and/or write | 43 | 23.24 | |
| Elementary (1–8 grades) | 26 | 14.05 | |
| High school (9–12 grades) | 20 | 10.81 | |
| College and above | 33 | 17.85 | |
| Sexual partner occupation (N = 185) | Farmer | 92 | 49.72 |
| Merchant/private business | 29 | 15.68 | |
| Governmental employee | 23 | 12.44 | |
| Student | 24 | 13 | |
| Daily laborer | 17 | 9.16 | |
| Household size | Fewer than three | 216 | 40.4 |
| Greater or equal to three | 319 | 59.6 | |
| Number of alive children (birthed, adopted and stepchildren) | No child | 241 | 45.0 |
| one child | 93 | 17.4 | |
| two children | 75 | 14.0 | |
| Three and above | 126 | 23.6 |
Forms of disability, membership, and decision-making related characteristics
From the total 535 disabled participants, 237(44.3%) of them were physically impaired followed by visual impairment (35%).
Only one-fifth of the study participants knew organizations deal with disabilities around where they live, and one-fourth (26.7%) of the participants were membership in any community group/s. More than half (57.6%) of the study participants were visiting health facilities for any care services without seeking others’ permission. Beside to this, nearly two-third (64.9%) of disabled women had no autonomy to visit their friends and relatives (decision making and freedom to move out of the house), and 198 (37.0%) were live alone. More than half (54.2%) of the study participants lived in their own home. Only 72 (13.5%) of the study participants were exposed to radio/television every day, and 234 (43.7%) participants decided alone when they wanted to do something (Table 2).
Table 2.
Frequency distribution of participants by their forms of disabilities, membership and decision-making related variables in Northwest Ethiopia, 2021(N = 535)
| Variables | Category | Frequency | Percent (%) |
|---|---|---|---|
| Time when disability occurred | Since birth | 105 | 19.6 |
| Childhood (birth to 18 years) | 259 | 48.4 | |
| Later (after 18 years of age) | 98 | 18.3 | |
| I do not remember | 73 | 13.6 | |
| Organization/s present around that work/s on people with disabilities empowerment | Yes | 115 | 21.5 |
| No | 420 | 78.5 | |
| Membership any community group/s | Yes | 143 | 26.7 |
| No | 392 | 73.3 | |
| Membership to any disability association/federation | Yes | 73 | 13.6 |
| No | 462 | 86.4 | |
| Autonomy to visits health facilities (decision making and freedom to move out of the house) | Yes | 308 | 57.6 |
| No | 227 | 42.4 | |
| Autonomy to visit friends and relatives (decision making and freedom to move out of the house) | Yes | 188 | 35.1 |
| No | 347 | 64.9 | |
| Living situation (with whom they live) | With parents | 139 | 26.0 |
| With partner | 131 | 24.5 | |
| Alone in my home | 198 | 37.0 | |
| Live with children | 28 | 5.3 | |
| Live with other else | 39 | 7.2 | |
| Currently live at | My own home | 290 | 54.2 |
| Rented house | 214 | 40.0 | |
| Institution based | 12 | 2.2 | |
| Street based | 19 | 3.6 | |
| Exposure to Radio/Television | Never | 249 | 46.5 |
| Rarely | 158 | 29.5 | |
| Sometimes (2–3 days/week) | 56 | 10.5 | |
| Almost every day | 72 | 13.5 | |
| Decision maker to do something (on all issues) | Me (herself) | 234 | 43.7 |
| Husband/boyfriend | 37 | 6.9 | |
| Joint | 103 | 19.3 | |
| Other family members (caregivers) | 161 | 30.1 |
Reproductive health history, service information and access related variables
Almost half (49.9%) of the study participants experienced the first menstruation when they were in the age range of 15–18 years. One-hundred fifty-three (28.6%) of the participants never had sexual contact history, and 15.3% (82/535) were pregnant before the age of 18 years. The majority (96.8%) of respondents visited governmental health facilities when they needed medical assistance, and 29.2% (156/535) participants said that getting reproductive care service is exceedingly difficult. Half (49.9%) of study participants also mentioned, there was problem in accessing information related to SRH services, and two-thirds (67.5%) of the participant were not being recommended to be tested for HIV/AIDS or/and pregnancy and screened for cervical cancer. Almost four-fifths (78.3%) of the study participants replied that materials are accessible in proper format for people living with disabilities at health facilities (Table 3).
Table 3.
Reproductive/sexual health history, service information and access related variables of participants in central Gondar, Northwest Ethiopia, 2021 (N = 535)
| Variable | Category | Frequency | Percent (%) |
|---|---|---|---|
| Age of menarche | Before 15 years of age | 140 | 26.2 |
| 15–18 years of age | 267 | 49.9 | |
| Do not know | 126 | 23.6 | |
| Never seen | 2 | 0.4 | |
| First sexual intercourse | Before 15 years of age | 34 | 6.4 |
| 15–18 years of age | 143 | 26.7 | |
| After 18 years of age | 137 | 25.6 | |
| Had never | 153 | 28.6 | |
| Do not remember | 68 | 12.7 | |
| Age of first pregnancy | Below 15 years of age | 6 | 1.1 |
| 15–17 years of age | 76 | 14.2 | |
| Above or equal to 18 years | 160 | 29.9 | |
| Do not remember | 116 | 21.7 | |
| Never pregnant | 177 | 33.1 | |
| Place where she seeks care when she sick | Private | 13 | 2.4 |
| Governmental | 518 | 96.8 | |
| Other | 4 | 0.7 | |
| Place where SRH care service most frequently accessed | Private | 6 | 1.1 |
| Governmental | 354 | 66.2 | |
| Pharmacy | 1 | 0.2 | |
| Never used | 174 | 32.5 | |
| Ease of getting reproductive care services | Very difficult | 156 | 29.2 |
| Somewhat difficult | 152 | 28.4 | |
| Not difficult | 185 | 34.6 | |
| I do not know | 42 | 7.9 | |
| Problem to get information related to SRH services | Problem | 267 | 49.9 |
| No problem | 259 | 48.4 | |
| I do not know | 9 | 1.7 | |
| Know where HIV/AIDS or/and pregnancy testing, and cervical cancer screening are provided | Yes | 182 | 34.0 |
| No | 353 | 66.0 | |
| Materials/equipment are available in proper format for people with disabilities in health facilities | Yes | 4 | 0.7 |
| No | 112 | 20.9 | |
| I do not know | 419 | 78.3 |
Abbreviations: HIV/AIDS, Human immunodeficiency virus/acquired immune deficiency syndrome; and SRH, sexual and reproductive health
SRH service utilization and awareness about the services
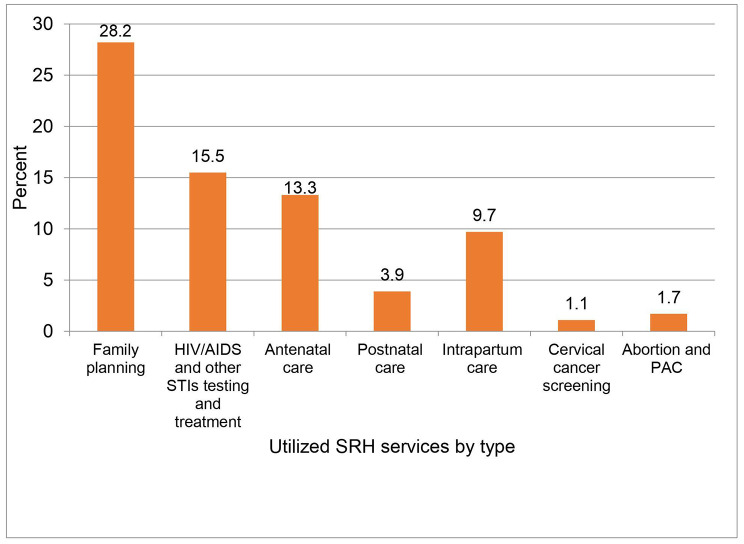
Of the total study participants, 33.3% (178/535) utilized at least one sexual and reproductive health service in the last 12 months, and 151(28.2%) of them used family planning which is one of the components of SRH service (Fig. 1).
Fig. 1.
Types of SRH services used by reproductive-age women with disabilities in the last 12 months in Northwest Ethiopia, 2021
Abbreviations: HIV/AIDS, Human immunodeficiency virus/acquired immune deficiency syndrome; PAC, post-abortion care; and SRH, sexual and reproductive health.
From those who utilized family planning, 108 (20.2%) of them used injectable (Depo-Provera) contraceptive method, and 108 (20.2%) participants preferred females as service provider (Table 4).
Table 4.
SRH service utilization and awareness related factors among disabled reproductive aged women, Northwest Ethiopia, 2021(N = 535)
| Variable | Category | Frequency | Percent (%) |
|---|---|---|---|
| Have ever heard about at least one SRH service? | Yes | 424 | 79.3 |
| No | 111 | 20.7 | |
|
If “yes”, about what she heard? # Multiple answer was possible |
Family planning | 395 | 73.8 |
| HIV/AIDS and other STIs testing and treatment | 286 | 53.5 | |
| Cervical cancer screening | 43 | 8.0 | |
|
Maternal care (ANC, IP & PNC) |
245 | 45.8 | |
| Abortion and PAC | 31 | 5.8 | |
| The most common source of information | Mainstream media (TV or radio) | 99 | 18.5 |
| Health professionals | 270 | 50.5 | |
| Associations | 33 | 6.2 | |
| Training | 4 | 0.7 | |
| Other | 18 | 3.4 | |
| Discussed about SRH services within a family member | Yes | 145 | 27.1 |
| No | 390 | 72.9 | |
| Types of family planning used by the participants (n = 151) | Oral contraceptive pills | 14 | 2.6 |
| Injectable | 108 | 20.2 | |
| Implanon | 29 | 5.4 | |
| Preference of service provider’s sex for those who used the service (N = 178) | Male | 17 | 3.2 |
| Female | 108 | 20.2 | |
| Anybody | 53 | 9.9 |
Note: Other; neighbors, family members
Abbreviations: ANC, antenatal care; IP, intrapartum care; PAC, post-abortion care; PNC, postnatal care; and TV, television
Factors associated with SRH service utilization
A total of thirteen (13) independent variables were identified as factors in bivariate regression at p-value less than 0.2, and after controlling cofounders, seven (7) factors were found to have significant association with SRH service utilization in multivariate logistic regression at p-value less than 0.05. These were; age of first sexual activity, those who discussed about SRH services with family, exposure to radio/television, living with partner, number of live children, autonomy to visit health facilities, and able to visit friends and relatives without keeping any permission (Table 5).
Table 5.
Regression table that shows the factors associated with SRH service/s uptake of reproductive age disabled women in Northwest Ethiopia, 2021
| Variables | Uptake of SRH service/s | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|
| No (%) | Yes (%) | |||
| Age in years | ||||
| 18–24 | 138(78.4) | 38(21.6) | 1.00 | 1.00 |
| 25–34 | 85(63.40 | 49(36.6) | 2.09 (1.267–3.46) | 2.64 (0.82–17.40) |
| 35–49 | 134(59.6) | 91(40.4) | 2.46 (1.58–3.86) | 1.09 (0.14–8.73) |
| Educational level | ||||
| Unable to read and write | 208(71.2) | 84(28.8) | 1.00 | 1.00 |
| Able to read and/or write | 29 (52.9) | 20(40.8) | 1.71(0.92–3.19) | 1.41(0.47–9.83) |
| Elementary (1–8 grades) | 77 (72.0) | 30(28.0) | 0.96(0.60–1.58) | 0.44 (0.16–3.23) |
| Highschool (9–12 grades) | 22(44.0) | 28(56.0) | 3.15(1.71–5.82) | 2.01(0.22–18.69) |
| College and above | 21(56.8) | 16(43.2) | 1.89(0.94–3.80) | 0.38 (0.16–2.33) |
| Employment/occupation | ||||
| Housewife | 62(35.0) | 115(65.0) | 1.00 | 1.00 |
| Governmental Employee | 12(63.2) | 7(36.8) | 0.31 (0.12–0.84) | 0.02 (0.008–1.13) |
| Merchant/Personalbusiness | 60(77.9) | 17(22.1) | 0.15 (0.10–0.28) | 0.01 (0.006–1.06) |
| Regularly beg from others | 70(80.5) | 17(15.5) | 0.13 (0.12–0.24) | 0.33 (0.07–1.71) |
| Student | 83(79.0) | 22(11.0) | 0.14 (0.10–0.25) | 0.29 (0.08–1.10) |
| Others | 64 (91.4) | 6(8.6) | 0.05 (0.02–0.84) | 0.001(0.002–1.01) |
| Sexual relationship status | ||||
| Married | 28(21.7) | 101(78.3) | 1.00 | 1.00 |
| Cohabitant or boyfriend | 24(42.9) | 32(57.1) | 0.37(0.19–0.73) | 0.42 (0.10–1.75) |
| Widowed | 106(91.4) | 10(8.6) | 0.03(0.01–0.06) | 0.04 (0.02–1.25) |
| Single | 17(53.1) | 15(46.9) | 0.24(0.11–0.55) | 0.21 (0.03–1.34) |
| Divorced | 182(90.1) | 20(9.9) | 0.03(0.02–0.06) | 0.23 (0.12–1.36) |
| Household size | ||||
| < 3 | 168(77.8) | 48(22.2) | 1.00 | 1.00 |
| > or = 3 | 189(59.2) | 130(40.8) | 2.41(1.63–3.56) | 3.16 (0.55–18.05) |
| Number of a live children | ||||
| No children | 195(80.9) | 46(19.1) | 1.00 | 1.00 |
| One child | 61(65.6) | 32(34.4) | 2.22(1.30–3.80) | 6.05 (0.18–12.97) |
| Two children | 50(66.7) | 25(33.3) | 2.12(1.19–3.78) | 0.54 (0.11–2.53) |
| Three and above | 51(40.5) | 75(59.5) | 6.23(3.86–10.1) | 4.85 (1.24–9.71) * |
| Autonomy to visit health facilities | ||||
| Yes | 154(50.0) | 154(50.0) | 8.46(5.24–13.7) | 3.30 (1.45–6.92) * |
| No | 203(89.4) | 24(10.6) | 1.00 | 1.00 |
| Autonomy to visit friends and relatives | ||||
| Yes | 83(44.1) | 105(55.9) | 4.75(3.23–6.99) | 3.95(1.28–12.17) * |
| No | 274(79.0) | 73(21.0) | 1.00 | 1.00 |
| With whom she lives | ||||
| With parents | 126(90.6) | 13(9.4) | 1.00 | 1.00 |
| With partner | 31(23.7) | 100(76.3) | 31.3 (15.55–62.8) | 9.2 (2.84–13.60) * |
| Alone | 159(80.3) | 39(19.7) | 2.38 (1.22–4.65) | 5.28 (0.89–10.14) |
| Other | 41(61.2) | 26(38.8) | 6.15 (2.89–13.05) | 4.74 (0.42–5.29) |
| Exposure to mainstream media (Radio and/Television) | ||||
| Never | 183(73.5) | 66(26.5) | 1.00 | 1.00 |
| Rarely | 103(65.2) | 55(34.8) | 1.48(0.96–2.28) | 0.84 (0.25–2.79) |
| Sometimes (2–3 days/week) | 44(78.6) | 12(21.4) | 0.76(0.376–1.52) | 0.07 (0.01–1.32) |
| Almost every day | 27(37.5) | 45(62.5) | 4.62(2.66–8.04) | 5.9 (1.26–13.04) * |
| Discussed about SRH and services with their families | ||||
| Yes | 53(36.6) | 92(63.4) | 6.14 (4.10–9.29) | 9.36(3.44–17.46) * |
| No | 304(77.9) | 86(22.1) | 1.00 | 1.00 |
| Age of first sexual intercourse | ||||
| Before 15 years of age | 30(88.2) | 4(11.8) | 1.00 | 1.00 |
| 15–18 years of age | 62(43.4) | 81(56.6) | 9.8 (3.28–29.27) | 5.63 (0.79–19.75) |
| After 18 years of age | 65(47.4) | 72(52.6) | 8.31(2.78–24.85) | 7.2 (1.51–13.40) * |
| Never had sexual intercourse | 143(93.5) | 10(6.5) | 0.52 (0.15–1.79) | 0.042 (0.012–1.86) |
| Do not remember | 57(83.8) | 11(16.2) | 1.45 (0.42–4.94) | 1.3 (0.13–4.93) |
| Materials available in proper format for disabled people at health facilities | ||||
| Yes | 1(25.0) | 3(75.0) | 7.84 (0.81–76.23) | 3.62 (0.21–19.30) |
| No | 53(47.3) | 59(53.7) | 2.91(1.89–4.42) | 2.41 (0.10–4.59) |
| I do not know | 303(72.3) | 116(27.7) | 1.00 | 1.00 |
Note: *p-value less than 0.05 and significantly associated, and 1.00: reference
Abbreviations: COR, Crude Odds Ratio; AOR, Adjusted Odds Ratio; CI, Confidence Interval.
Discussion
This study was community based and 535 reproductive age (18–49 years) women with disabilities were participated. Of these, 44.3% of the women had physical/mobility disabilities followed by 35% (visual impairment) and 20.7%, hearing impairment. Since, this study aimed to assess the uptake of sexual and reproductive health services and associated factors, 33.27% (95%CI; 29.29–37.44) disabled women were using at least one SRH services in the last 12 months preceding to the survey. This study was in line with the study conducted in Arbaminch (33.7%) and Addis Ababa (31.1%), Ethiopia which were conducted to assess the use of family planning method alone [19, 34].
On the other side, the utilization of SRH service/s in the last 12 months in this study was lower than the study conducted in Ghana (70%) [35]. The study conducted in Ghana was among school age disabled students and assessed ever used of SRH services that might be the reason made high use. However, this study was higher than the study conducted in Gondar, Ethiopia (13.1%) [36]. The plausible reason for the disparities could be due to the difference of study participants, time gap and only one type of SHR service uptake that is family planning method was assessed in Gondar.
After controlling confounders, seven independent variables were significantly associated with SRH service utilization. Mothers who had three and above alive children were 4.85 times more likely to use at least one SRH service in the last 12 months preceding to the survey compared to those who had no child. Even if, no studies revealed that this factor as predictor to use SRH services among women with disabilities. However, it was consistent with the study conducted in Nepal, Ghana, and Malawi [37–39] among non-disabled women. The possible explanation could be mothers who had more children were married and reach the desire family size or want to limit the number of children compared to those who had no children, because most participants in this study used family planning methods from the five SRH services.
Living conditions were another factor affecting the use of SRH services. Mothers who lived with their sexual partner were 9.2 times more likely to use SRH services compared to those who lived with their parents. No studies clearly stated that living with partner is a predictor to use SRH services so far. Those who lived with their partners are more transparent and feel free to discuss reproductive health issues compared to those who lived with their parents. Social norms are the possible barriers that might be restricted to not make transparent communication with their parents, and result that consider themselves asexual. The study conducted in United States highlighted that people do not decide in women with disabilities health and they are regularly engaging in smoking and drinking alcohol because of discrimination [40].
The study done in Ghana showed that discussion about sexual actions with their daughters mentioned as protective strategy against irresponsible sexual behaviors [41], while those who live with partners have sexual intercourse experience and no hesitation to discuss sexual and reproductive health with their partner and neighbors. The study conducted in Northwest Ethiopia proved that those who experienced parental discussion on SRH issues had ever sexual intercourse and use some SRH services [42].
On the other side, those who had open discussion with their families about SRH services were 9.36 times more likely to uptake the service when compared with their counterparts. This finding is consistent with the study conducted in Kenya and Ethiopia among non-disabled adolescents [43, 44]. A systematic review in qualitative study revealed that communicative problem is a barrier to use health care services for women with disabilities [45]. Moreover, the study conducted in Nairobi, Kenya showed that parent-child communication is strongly associated with child’s safer sex practice, including using condom and delayed sexual debut [46]. The reason could be those who openly discussed with their family members would have sufficient awareness about the service benefits, where to be accessed, and comfort to use without any restriction. Lack of family support and low self-esteem may contribute to low utilization of the service.
Women who had full autonomy to visit health facilities, friends and relatives were the positive factors influenced SRH service utilization compared to those who had none. This result agrees with the studies conducted in Nepal and Nigeria [37, 47]. It has proved by the study conducts in Nigeria (here cited above) that autonomy plays a significant role in women’s use of SRH services which is independent of education and several other factors related to women’s status. In fact, that women who have great decision-making power can do what they want to do.
Reproductive-age disabled women who were exposed for Radio/Television every day were 5.9 times more likely to use at least one SRH service compared to those who never listened/watched. This finding is supported with the study done in Nepal [37]. The plausible explanation might be due to mainstream medias’ potential of disseminating health related information for the community who has limited educational attainment like these disabled women. The media plays a key role in amplifying awareness and encouraging the use of different health care services including SRH.
Those who started sexual intercourse after the age of 18 were 7.2 times more likely to use at least one SRH service in the last twelve months compared to those who started before 15. Previous studies have said nothing about this factor the probable reason for the association could be that those who are 18 and above years of age may use SRH service because they are married and not fears social discrimination (feel free) when they visit of health facilities.
Limitations of the study
The data were self-reported and liable to recall bias and did not show the causal relationship due to the nature of cross-sectional study design. Our study also did not incorporate health care providers, family members and organizations working related to disabilities’ perspective were other limitations of this study.
Implications
These findings focus on the needs for increased attention to sexual and reproductive health of reproductive age women with disabilities. The utilization of SRH health services in this study and along with the previous [19, 34, 36] suggest more could be done to improve SRH of women with disabilities. The exclusion of reproductive aged women with disabilities from SRH service interventions may increase the risk of adverse health outcomes, particularly has main impact on unplanned and unintended pregnancy, unsafe abortion, STIs infection including HIV/AIDS and infertility [10, 11]. Attending ANC, institutional delivery and postnatal care follow up are the components of SRH care services. Maternal disability is associated with increased the risk of pregnancy, delivery and postpartum complications [48]. Population based study conducted in United States highlighted that the odds of untended pregnancy had higher among women with disabilities compared to non-disabled women [49]. Low accessibility and utilization of SRH programs and information may result in poor preconception health as well [12].
Based on our findings, potential areas for action to improve the uptake of SRH care services among reproductive aged women with disabilities should include; women’s autonomy to decide and realize when they need to visit health facility, regular media exposure, open discussion with family about SRH and live with partner than parents.
Disabled women live with their partners were more likely by far to use SRH services compare to those who live with parents. Evidence revealed that women with disabilities often face stigma and discrimination from family in their reproductive health. Myths, misinformation and social norms are mentioned as reasons for individual belief and attitude [50].
Therefore, multifaceted understanding of reasons for low utilization of SRH services by involving other key-informants’ perspectives (health care providers and other stake holders) and consider in transforming social norms and beliefs about women with disabilities are the future research and intervention areas. Furthermore, all health facilities need to have sign language interpreter, decision support tool to decide and use SRH health care services.
Conclusions
Reproductive age women with disabilities uptake of SRH services were the issue that needs action. Low uptake of SRH services has increased the risk of short-and long-term health outcomes. The concerned governmental and non-governmental organizations should make efforts to increase the uptake of SRH services and address factors associated with the outcome of interest variable. Additionally, the scientific community needs to investigate the barriers and facilitators to use SRH services from families, health care providers and other key informants’ perspective.
Acknowledgements
We are grateful to the Central Gondar zone of labour and social affairs for allowing us to conduct the study and providing the necessary preliminary information and support letter while conducting this study. We would also like to thank the University of Gondar for its financial support for materials, data collectors and supervisors. Finally, our special thanks should extend to data collectors, supervisors, and study participants.
Abbreviations
- AOR
adjusted odds ratio
- COR
crude odds ratio
- HIV
human immunodeficiency virus
- OR
odds ratio
- PAC
post abortion care
- SRH
sexual and reproductive health
- STIs
Sexual transmitted infections
- WHO
world health organizations
Authors’ contributions
BKR, GLA and ATT have made substantial contributions to research conception, analysis, interpretation data and wrote the mauscript; EBT, MMA, EAC, MM and AA have been involved in conception and data interpretation. All authors have approved the submitted version of the manuscript and are accountable for their contributions and accuracy of the work.
Funding
This study was funded by the University of Gondar with award Ref no: VP/RCS/598/03/2013 EC. However, the funder had no role in the study design, analysis, interpretation, writing, or decision to publish this manuscript.
Data Availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethical approval and consent to participate
Ethical clearance was obtained from University of Gondar research ethics committee, Institutional Review Board (IRB) (R. No.: V/P/RCS/05/530/2020). A letter of support was also obtained from the Central Gondar zone labour and social affairs office for each selected district. Again, support letters were also obtained from each respective selected district higher officials. Written informed consent was obtained from study participants who can read and write, while verbal informed consent was obtained from those who can’t able to read and write participants. The University of Gondar ethics committee approved the verbal informed consent. Study participants’ privacy and confidentiality were ensured before data collection. The right to not participate or refuse to answer any or all questions and to withdraw from interview at any time was respected. Additionally, all methods were carried out in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kostanjsek N. Use of The International Classification of Functioning, Disability and Health (ICF) as a conceptual framework and common language for disability statistics and health information systems. Paper presented at: BMC public health; 2011. [DOI] [PMC free article] [PubMed]
- 2.WHO . International classifi cation of functioning, disability, and health. Switzerland: Geneva: World Health Organization; 2006. [Google Scholar]
- 3.World Report on Disability.,WHO and World Bank Geneva, Switzerland, 2011.
- 4.Marella M, Devine A, Armecin GF, Zayas J, Marco MJ, Vaughan C. Rapid assessment of disability in the Philippines: understanding prevalence, well-being, and access to the community for people with disabilities to inform the W-DARE project. Popul Health Metrics. 2016;14:26. doi: 10.1186/s12963-016-0096-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.ECDD. General Overview of Disability in Ethiopia, Addis Ababa, Ethiopia, 2010.
- 6.Physical disability. Children with special educational needs. Hampshire County Council; 2005.
- 7.Shakespeare T. Disabled sexuality: toward Rights and Recognition. Sex Disabil. 2000;18(3):159–66. doi: 10.1023/A:1026409613684. [DOI] [Google Scholar]
- 8.Abdul Karimu A. Exploring the sexual and reproductive health issues of visually impaired women in Ghana. Reprod Health Matters. 2017;25(50):128–33. doi: 10.1080/09688080.2017.1333893. [DOI] [PubMed] [Google Scholar]
- 9.Starrs AM, Ezeh AC, Barker G, Basu A, Bertrand JT, Blum R, Coll-Seck AM, Grover A, Laski L, Roa M, et al. Accelerate progress—sexual and reproductive health and rights for all: report of the Guttmacher–Lancet Commission. Lancet. 2018;391:2642–92. doi: 10.1016/S0140-6736(18)30293-9. [DOI] [PubMed] [Google Scholar]
- 10.Glasier A, Gulmezoglu AM, Schmid GP, Moreno CG, Van Look PF. Sexual and reproductive health: A matter of life and death. Lancet. 2006;368:1595–607. doi: 10.1016/S0140-6736(06)69478-6. [DOI] [PubMed] [Google Scholar]
- 11.Ezzati M, Lopez AD, Rodgers A, Vander Hoorn S. Murray C.J. selected major risk factors and global and regional burden of disease. Lancet. 2002;360:1347–60. doi: 10.1016/S0140-6736(02)11403-6. [DOI] [PubMed] [Google Scholar]
- 12.Tarasoff LA, Lunsky Y, Chen S, Guttmann A, Havercamp SM, Parish SL, Vigod SN, Carty A, Brown HK. Preconception Health characteristics of women with disabilities in Ontario: a Population-Based, cross-sectional study. J Womens Health (Larchmt) 2020;29(12):1564–75. doi: 10.1089/jwh.2019.8273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Andersona P, Kitchin R. Disability, space and sexuality: access to family planning services. Social Science & Medicine. 2000;51(2000):1163-73. [DOI] [PubMed]
- 14.Factsheet. Disability & Sexual and Reproductive Health and Rights Dutch Coalition on Disability and Development, 2013.
- 15.Tiffany L, Panko JC, Albert S, Smith LD, Margarita M, Cooley M, Herschel M, Mitra, McKee M. Experiences of pregnancy and perinatal healthcare access of women who are deaf: a qualitative study. BJOG: An International Journal of Obstetrics & Gynaecology. 2022;130(5):514–21. doi: 10.1111/1471-0528.17300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.UNFPA. Global study on Youth and Disability. www.theisg.com; 2016.
- 17.Groce N, Izutsu T, Reier S, Rinehart W, Temple B. Promoting sexual and Reproductive Health for Persons with Disabilities: WHO/UNFPA Guidance note. World Health Organization; 2009.
- 18.Central Gondar Labour . And Social Affairs Office report (unpublished) Ethiopia: Gondar; 2021. [Google Scholar]
- 19.Yibeltal Mesfin, Yesgat FG. Wubshet Estifanous,Yordanos Gizachew, Seid Jemal, Natnael Atnafu and Keyredin Nuriye. Utilization of Family Planning Methods and Associated Factors Among Reproductive-Age Women with Disability in Arba Minch Town, Southern Ethiopia. Open Access Journal of Contraception, vo. 11, 2020. [DOI] [PMC free article] [PubMed]
- 20.Jane T, Bertrand KH, Robert J, Magnani, Marcia A. Angle Access, Quality of Care and Medical Barriers in Family Planning Programs. Int Fam Plan Perspect. 1995;21:64–9. doi: 10.2307/2133525. [DOI] [Google Scholar]
- 21.Levesque, et al. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013;12:18. doi: 10.1186/1475-9276-12-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Altman B. The Washington Group: origin and purpose. In: Barnartt B, editor. International views on disability measures: moving toward comparative measurement (research in Social Science and disability); Altman. Bradford, UK: Emerald Group Publishing Limited; 2006. pp. 9–16. [Google Scholar]
- 23.UN. Disability and Development Report, Realizing the Sustainable Development Goals by, for and with persons with disabilities, No. 19.IV.4, 2018.
- 24.Pierre DeBeaudrap CM, Pasquier E, Mac-Seing M. Mukangwije and Gervais Beninguisse. Disability and Access to sexual and Reproductive Health Services in Cameroon: a mediation analysis of the role of socioeconomic factors. Int J Environ Res Public Health. 2019;16:417. doi: 10.3390/ijerph16030417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bersamin, et al. Reproductive Health Services: barriers to Use among College Students. J Community Health. 2017 February;42(1):155–9. 10.1007/s10900-016-0242-2. [DOI] [PMC free article] [PubMed]
- 26.Redshaw, et al. Women with disability: the experience of maternity care during pregnancy, labour and birth and the postnatal period. BMC Pregnancy Childbirth. 2013;13:174. doi: 10.1186/1471-2393-13-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Eva Burke F, Kébé I, Flink, Miranda, van Reeuwijk. & Alex le May. A qualitative study to explore the barriers and enablers for young people with disabilities to access sexual and reproductive health services in Senegal, Reproductive Health Matters, 2017, 25:50, 43–54. 10.1080/09688080.2017.1329607. [DOI] [PubMed]
- 28.Ahumuza, et al. Challenges in accessing sexual and reproductive health services by people with physical disabilities in Kampala, Uganda. Reproductive Health. 2014;11:59. doi: 10.1186/1742-4755-11-59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.David Paul Ngilangwa et al. Accessibility to sexual and reproductive health and rights education among marginalized youth in selected districts of Tanzania. Pan Afr Med J. 2016;25 (Supp 2):2. [DOI] [PMC free article] [PubMed]
- 30.Modiba ASYaLM. Modern contraceptive methods knowledge and practice among blind and deaf women in Ethiopia. A cross-sectional survey. BMC Womens Health. 2019 19(151). [DOI] [PMC free article] [PubMed]
- 31.Mickey RM, Greenland S. The impact of confounder selection criteria on effect estimation. Am J Epidemiol. 1989 Jan;129(1):125 – 37. 10.1093/oxfordjournals.aje.a115101. Erratum in: Am J Epidemiol 1989 Nov;130(5):1066. PMID: 2910056. [DOI] [PubMed]
- 32.Bendel RB, Afifi AA. “Comparison of Stopping Rules in Forward ‘Stepwise’ Regression.” Journal of the American Statistical Association, vol. 72, no. 357, 1977, pp. 46–53. JSTOR, 10.2307/2286904. Accessed 27 Jun. 2022.
- 33.Hosmer DW, Lemeshow S, Sturdivant RX. Applied logistic regression. New York: John Wiley & Sons, Incorporated; 2013. [Google Scholar]
- 34.Modiba AS. Modern contraceptive methods knowledge and practice among blind and deaf women in Ethiopia. A cross-sectional survey. BMC Womens Health, 2019 19(151). [DOI] [PMC free article] [PubMed]
- 35.Kumi-Kyereme A. Sexual and reproductive health services utilisation amongst in-school young people with disabilities in Ghana. Afr J Disabil. 2021;10(0):a671. doi: 10.4102/ajod.v10i0.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Getalem A, Beyene AMM, Fekadu GA. Modern Contraceptive Use and Associated Factors among Women with Disabilities in Gondar City, Amhara Region, North West Ethiopia: A Cross Sectional Study. Afr J Reprod Health 2019. 23(2). [DOI] [PubMed]
- 37.Thapa NR. Factors influencing the use of reproductive health services among young women in Nepal: analysis of the 2016 Nepal demographic and health survey. Reproductive Health 2020. 17(102). [DOI] [PMC free article] [PubMed]
- 38.Aviisah PA, Dery S, Atsu BK, et al. Modern contraceptive use among women of reproductive age in Ghana: analysis of the 2003–2014 Ghana demographic and health surveys. BMC Womens Health. 2018;18:1–10. doi: 10.1186/s12905-018-0634-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Palamuleni ME. Socio-economic and demographic factors affecting contraceptive use in Malawi. Afr J Reprod Health. 2013;17:91–104. [PubMed] [Google Scholar]
- 40.Horner-Johnson W, Akobirshoev I, Amutah-Onukagha NN, Slaughter-Acey JC, Mitra M. Preconception Health Risks among U.S. women: disparities at the intersection of disability and race or ethnicity. Womens Health Issues. 2021;31(1):65–74. doi: 10.1016/j.whi.2020.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Elizabeth AKu Baku IA, AgnesMillicent, Kotoh, Adanu RichardMK. Parents’ Experiences and Sexual Topics Discussed with Adolescents in the Accra Metropolis, Ghana: A Qualitative Study. Advances in Public Health, 2018. 2018: p. 12.
- 42.Ayehu A, Kassaw T, Hailu G. Level of young people sexual and Reproductive Health Service utilization and its Associated factors among Young People in Awabel District, Northwest Ethiopia. PLoS ONE. 2016;11(3):e0151613. doi: 10.1371/journal.pone.0151613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Beatrice W, Maina. B.A.U.a.C.W.K., Parent-child sexual and reproductive health communication among very young adolescents in Korogocho informal settlement in Nairobi, Kenya. Reproductive Health, 2020. 17(79). [DOI] [PMC free article] [PubMed]
- 44.Gelila Abraham KY, Morankar SN. Determinants of adolescents reproductive health service utilization in Ethiopia: a systematic review of quantitative evidence. Adolesc Health Med Ther, 2019. 10 p. 49–58. [DOI] [PMC free article] [PubMed]
- 45.Matin BK, Karyani HJWAKazemi, Rezaei S. Moslem Soofi and Shahin Soltani, Barriers in access to healthcare for women with disabilities: a systematic review in qualitative studies. BMC Women’s Health 2021. 21(44). [DOI] [PMC free article] [PubMed]
- 46.Sidze EM, Elungata’a P, Maina BW, Mutua MM. Does the quality of parent child connectedness matter for adolescents’ sexual behaviors in Nairobi informal settlements? Arch Sex Behav. 2015;44:631–8. doi: 10.1007/s10508-014-0402-3. [DOI] [PubMed] [Google Scholar]
- 47.Saritha P, Viswan TKSR, Ngianga-Bakwin Kandala, Max G, Petzold, Fonn S. Sexual autonomy and contraceptive use among women in Nigeria: findings from the demographic and Health Survey data. Int J Women’s Health. 2017;9:581–90. doi: 10.2147/IJWH.S133760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tarasoff LA, Ravindran S, Malik H, Salaeva D, Brown HK. Maternal disability and risk for pregnancy, delivery, and postpartum complications: a systematic review and meta-analysis. Am J Obstet Gynecol. 2020; 222(1):27.e1-27.e32. [DOI] [PMC free article] [PubMed]
- 49.Horner-Johnson W, Dissanayake M, Wu JP, Caughey AB, Darney BG. Pregnancy intendedness by maternal disability status and type in the United States. Perspect Sex Reprod Health. 2020;52(1):31–8. doi: 10.1363/psrh.12130. [DOI] [PubMed] [Google Scholar]
- 50.Devkota HR, Kett M, Groce N. Societal attitude and behaviours towards women with disabilities in rural Nepal: pregnancy, childbirth and motherhood. BMC Pregnancy Childbirth 2019 Jan 9;19 (1):20. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.