Abstract
Background
The skin is a protective barrier of the body against external factors, and its damage leads to a loss of integrity. Normal wound healing results in a correct, flat, bright, and flexible scar. Initial skin damage and patient specific factors in wound healing contribute that many of these scars may progress into widespread or pathologic hypertrophic and keloid scars. The changes in cosmetic appearance, continuing pain, and loss of movement due to contracture or adhesion and persistent pruritis can significantly affect an individual's quality of life and psychological recovery post injury. Many different treatment methods can reduce the trauma and surgical scars. Manual scar treatment includes various techniques of therapy. The most effectiveness is a combined therapy, which has a multidirectional impact. Clinical observations show an effectiveness of manual scar therapy.
Material and methods
The aim of this work was to evaluate effectiveness of the scar manual therapy combined with complementary methods on the postoperative scars. Treatment protocol included two therapies during 30 min per week for 8 weeks. Therapy included manual scar manipulation, massage, cupping, dry needling, and taping.
Results
Treatment had a significant positive effect to influence pain, pigmentation, pliability, pruritus, surface area, and scar stiffness. Improvement of skin parameters (scar elasticity, thickness, regularity, color) was also noticed.
Conclusion
To investigate the most effective manual therapy strategy, further studies are needed, evaluating comparisons of different individual and combined scar therapy modalities.
Keywords: cesarean section, dry needling, manual therapy, scar taping, scars
1. INTRODUCTION
The skin is a protective barrier of the body against external factors, and its damage leads to a loss of integrity. Scars are formed as an effect of damaging the skin. They affect most people on earth. Scars arise as a result of mechanical damages, burns, surgical procedures, chemical or biological agents, and long‐lasting skin diseases. 1 The optimal result of wound healing is a mature, well healed scar. Normal wound healing results in a correct, flat, bright, and flexible scar. Normal scars do not go beyond the original area of damage and are aesthetically satisfactory. Among the factors increasing the risk of pathological scarring, we can distinguish: age, anatomic location, race, and type of trauma. An important problem in the wound healing process is the formation of pathological scars, such as hypertrophic scars, keloids, and atrophic scars. The keloids and hypertrophic scars incidence is determined at the level of 4.5%–16%. 1 , 2 Pathologic scar formation manifests itself by low tensile strength, pigment alterations, increased tension texture, and sensation irregularities. Abnormal scars arising as a result of disorders in the process of fibrosis raised above the surface of the skin, beyond the original area of damage. Often abnormal scars are accompanied by pain, itching, and contractures. 1 , 2
Initial skin damage and patient specific factors in wound healing cause that many of these scars may progress into widespread or pathologic hypertrophic and keloid scars. Any dysfunction in the wound healing process may result in excessive scar tissue formation. Despite the continual advancement or surgical care, patients who have undergone surgical interventions are often left with scars, persistent functional impairments, and symptomology. 3
In addition, scar esthetics can also have a negative influence on psychosocial factors. Inevitable problems associated with postoperative scars are adhesions. Adhesions occur after every abdominal operation but the majority of them are clinically silent. Parts of postoperative adhesions (i.e., after cesarean section [CS]) contribute significantly to chronic abdominal pain, recurrent intestinal obstruction, chronic back pain, and infertility. Intraabdominal adhesions occur at a 7% rate after one CS up to 68% with repeated cesareans. Despite recent advances in surgical techniques and scar therapies, there is no dependable strategy to manage postoperative adhesions. In many cases as consequences of deep dermal defects appear hypoesthesia, hyperalgesia around the injured area, and functional limitations. 4 , 5
The normal wound healing process is a strictly controlled state of balance between the process of disintegration of the structure of the damaged tissue and the repair consisting in the synthesis and formation of a new, correct one. Mediators, blood cells, extracellular matrix cells, and parenchymal cells are involved in the process. Increased activation and migration of fibroblasts to the wound bed regulated deposition of the extracellular matrix and its shrinkage are responsible for the proper healing of the skin. 3 , 6 , 7 , 8
During the wound healing, four phases overlapping each other in time and closely related to each other are distinguished. The first phase occurring immediately after the damage is the hemostasis phase; the second phase is the inflammatory phase lasting from 24 to 72 h, which can extend from 5 to 7 days. From 1 to 3 weeks after the damage, there is a phase of proliferation and repair of the damaged tissue lasting about 3–4 weeks. In the fourth stage of the healing process, remodeling takes place, and this phase can be extended from 3 weeks to several years, during which the wound will mature and reach the final strength. 8
Scars can greatly affect the quality of life. Many different treatment methods can reduce the trauma and surgical scars. These include physical methods: manual therapy, appropriate pressure, taping, cryotherapy, dermabrasion, radiation, laser therapy, pharmacological methods, and surgical techniques. The most effective is a combined therapy. Cosmetologists focus on esthetic problems with scars, whereas physiotherapists work with pain and functional limitations caused by tissue damage and scars. The purpose of physical scar management focuses primarily on the prevention of an abnormal healing process of the skin. 9 , 10 , 11
External mechanical impacts in daily activities can lead to in the formation of marked scar strands and adhesions. Overloading leads to renewed inflammatory reaction and thus in further restriction. An effective method used in anti‐adhesions prevention is postoperative scar physiotherapy, including lymphatic drainage, scar mobilization, kinesiotaping, or myofascial relaxation. Manual scar therapy to be effective requires applying physiological stimuli adequately to the phase of wound healing. Scar tissue therapy is a treatment for reducing pain and functional limitations, improving pliability, reducing hyperpigmentation, pruritus, fascial adhesions, to reduce scar thickness and smooth surface area. Scar tissue massage is a form of rehabilitation that uses pulling and stretching to remodel scar tissue. 7 , 8 , 11 Scar massage helps regain mobility and strength in damaged tissue. After a few minutes of mechanical stimuli directly in the scar, a release in the tissue can be observed. The second way of influence of mechanical stimuli from outside to the body is a mechanotransduction. It describes the ability of a cell to actively sense, integrates, and converts mechanical stimuli into biochemical signals. Every stimulus has result in intracellular changes, such as ion concentrations, activation of signaling pathways, and transcriptional regulation. The aim of the therapeutically applied manual techniques is therefore not only to mechanically lengthen collagen fibers but also to directly influence the cell biological processes by means of adequate stimulation. The protocol of effective manual scar therapy should include correct dosage of stimulation. The adequate dosage should be determined according to the wound healing phase and needs adjustment of amplitude, duration, and frequency of stimulation. Overloading the scar tissue can lead to cellular damage and triggers a new inflammatory reaction. However, underloading leads to reduced elasticity, resilience, and disorganized form of cross‐links. 7 , 8 , 11 Koller11 suggested dosage recommendations depend on the wound healing phase. In the proliferation phase (until day 21), stimulation should be lower, in the area of the first remarkable increase in connective tissue resistance. In the last remodulation phase of wound healing, stimulation can be higher, until the second remarkable increase in connective tissue resistance, but not exceeding the anatomical barrier. The recommended duration of application is 1 min per localization, three to five times per a therapy unit and supplemented by an oscillating frequency of 0.2 Hz at the end of the respective amplitude. 11
To increase the effectiveness of the scar therapy, it is advisable to use combined treatment. Manual work often proceeds alternately or together with cupping, dry needling, kinesiotaping, instrument therapy, electrodermal therapy, exercises, compression, pharmacotherapy, and other. Adjusting of the therapy requires considering various factors and an individual approach to the patient. 12
Cupping is a supporting method used in scar treatment. Subatmospheric pressure suction affected by cup, promote peripheral blood circulation, and improve tissue elasticity. Cupping therapy can be used with caution only in the remodeling phase of the wound healing and in old scars treatment. The reported effect of cupping therapy includes modification of the skin's biomechanical properties and improving local anaerobic metabolism. However, too high pressure can induce microtraumatic injures and triggers new inflammatory phases. Especially in the early phase, it can quickly lead to an overdose. 12 , 13 , 14
Kinesiotaping takes advantage of the physical properties of elastic therapeutic tapes and specific methods of its applications. Mechanism of this treatment is based on lifting skin microscopically and improving blood and lymph circulation. It causes fascia relaxation, improves tissue nourishment, and reduces edema. Previous studies have shown that the tape application directly over a wound or scar can reduce skin tension and prevent tissue overgrowth. Tape application, through pulling fresh wound closure, can reduce the mechanical forces affecting the wound. 15 , 16 , 17 , 18
Dry needling is a method applied to decrease pain and improve scar mobility. The classic technique is named “surrounding the dragon” that involves encircling the problem area with needles. The mechanism of action remains unclear. The current literature suggests that dry needling may be an effective method for treating scar tissue by suppressing local inflammation, stimulating reepithelization, and reducing scar hyperproliferation. In older scars, dry needling triggers regenerative mechanisms and induces collagen formation, neoangiogenesis, and skin cell proliferation. 19 , 20
Scar treatment includes various techniques of therapy. Clinical observations show an effectiveness of manual scar therapy. However, the question of which dosage should be applied in which wound healing phase at which intervention time is not easy to answer. Further studies are needed to verify and quantify the efficacy of combined methods, to understand the underlying mechanism, and to establish a protocol of effective intervention.
The aim of the research was to evaluate effectiveness of the scar manual therapy combined with complementary methods on the postoperative scars.
2. MATERIALS AND METHODS
Eleven volunteers (women) of average age 32.9 ± 5.2 with postoperative scar were classified in this study. Patients had scars after elbow operation (1), abdominal operation (3), and CS (7). The average age of the scar was 5 months (±2.9). All respondents notice ailments and discomfort correlated with the scar. One person was excluded from the study due to initiation of the other treatment.
The inclusion criteria for the study were as follows:
presence of at least one linear, surgical scar;
age of the scar under 12 months;
the current lack of any scar therapy;
nonuse topical treatment.
The exclusion criteria for the study were as follows:
use of any topical treatment on the scar;
current other scar therapy;
unhealed wounds or age scar under 6 weeks.
The research was conducted after receiving a positive opinion of the Bioethics Committee of the SUM, no. KNW/0022/KB1/27/I/16 on 06.06.2016. All volunteers received information about conditions of participation in the study.
Before and after the end of the scar therapy, the patients had a series of measurement. To evaluate objective results of therapy were used: clinical photography, measurement of skin parameters, and high‐frequency ultrasounds (HFUS). Photographies were taken using a dermatoscope Heine DELTA 30 (×10 optical magnifications). Examinations of skin parameters were carried out using Multi Probe Adapter MPA 10 (Courage + Khazaka Electronic GmbH, Germany). Hydration (Corneometer CM 825), transepidermal water loss (TEWL; Tewameter TM Hex), melanin and hemoglobin levels (Mexameter MX 18), and viscoelasticity (Cutometer 580) were measured before and after the therapy on the scar and on the healthy skin. Scar tissue was also imaged using DUB SkinScanner high‐frequency ultrasound equipped with a 33 MHz transducer. The DUB SkinScanner 75 5.21 software was used to evaluate the scar height and their structure and density. Scars were also subjective evaluated by patients and an observer with Patient and Observer Scar Assessment Scale (POSAS) scale (Figure 1).
FIGURE 1.
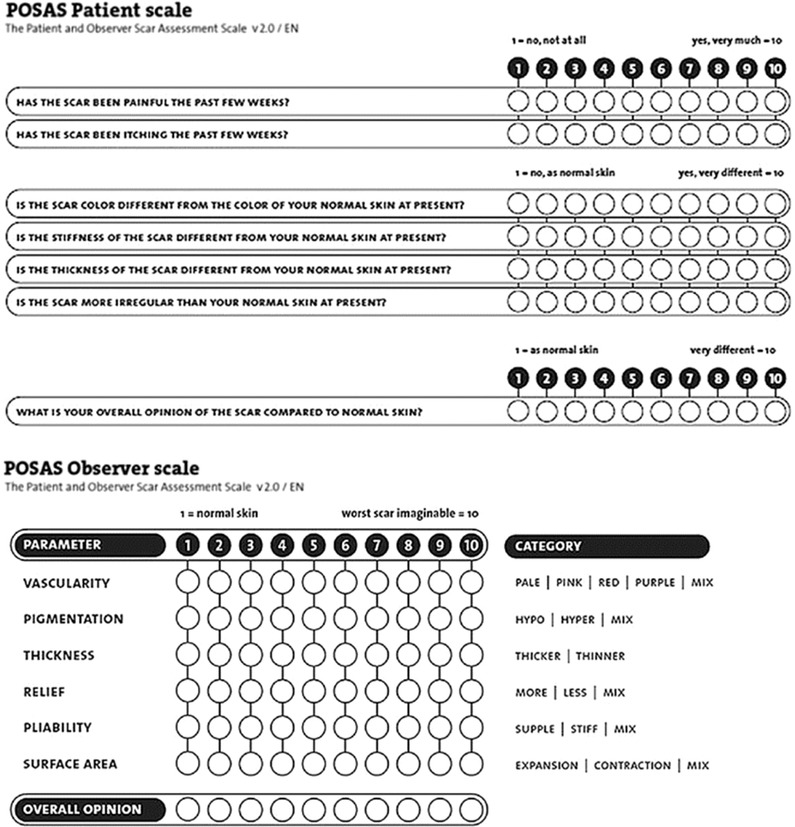
The Patient and Observer Scar Assessment Scale
Statistical data analysis was conducted with the use of Statistica 13.3 (TIBCO Software, Palo Alto, CA, USA) and MS Excel 2016 (Microsoft, Redmond, WA, USA). All results are presented as mean ± standard deviation and were examined for normality of distribution by the Shapiro–Wilk test. Parametric data were analyzed using Student's t‐test. For nonparametric data, Mann–Whitney U test was applied to indicate statistical significance. A p < 0.05 was considered statistically significant.
The treatment protocol included two therapies during 30 min per week for 8 weeks. The treatment protocols were the same for all patients but required an individual approach. Therapy included manual scar manipulation (every session), massage (every session), cupping (every second session; four times per whole treatment), dry needling (two times per the entire protocol; at 9th and 13th session), and taping (every second session, eight times per whole treatment). Cupping and dry needling were used from 5th week of the therapy. The classical technique of dry needling was used (“surrounding the dragon”; Figure 2). Tapes were applied once a week with “zig‐zag” or “star technique” (Figures 3 and 4).
FIGURE 2.

Scar dry needling
FIGURE 3.

“Star” technique of scar taping
FIGURE 4.

“Zig‐zag” technique of scar taping
3. RESULTS
Visually comparison based on photography confirms noticeable influence of the manual scar therapy. Scars after 8 weeks therapy are paler, flatter, and more regular, which can be observed on Figures 5, 6, 7, 8.
FIGURE 5.
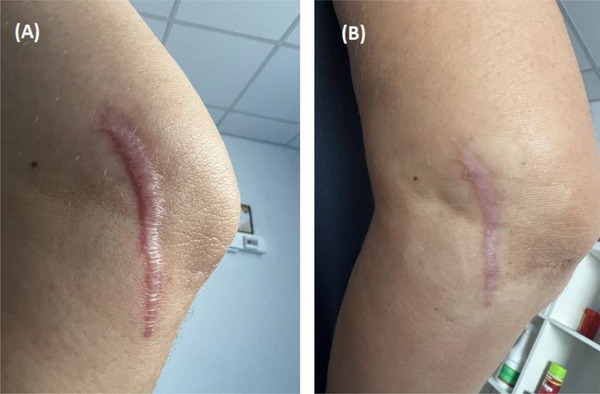
Photographs of scar after elbow operation before (A) and after (B) manual scar therapy
FIGURE 6.
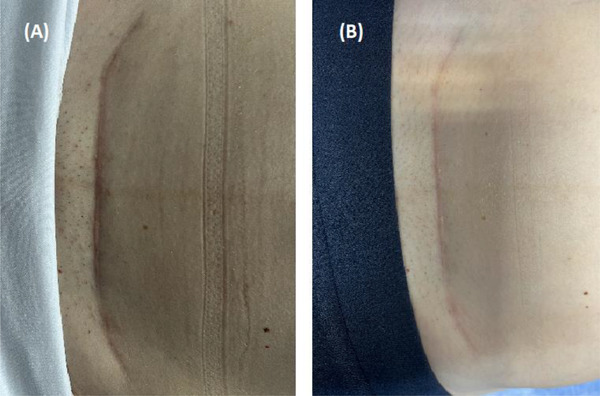
Photographs of scar after cesarean section (CS) before (A) and after (B) manual scar therapy
FIGURE 7.
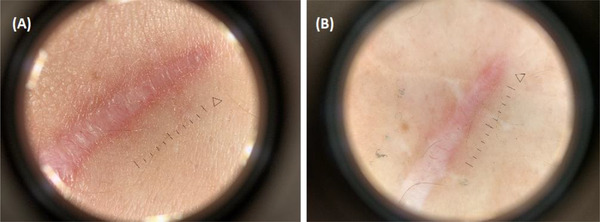
Dermatoscopic view of scar after elbow operation before (A) and after (B) manual scar therapy
FIGURE 8.
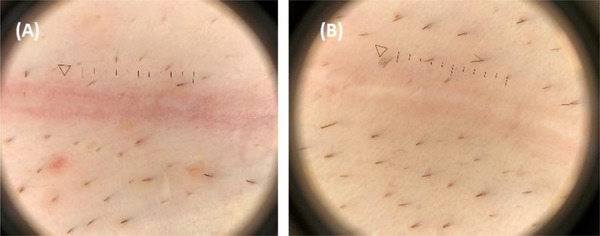
Dermatoscopic view of scar after cesarean section (CS) before (A) and after (B) manual scar therapy
HFUS show real‐time images of the skin layers, appendages, and skin lesions in vivo and allow us to evaluate effects of different skin treatments. Pathological conditions (e.g., scars) related to the accumulation of fibers within increase the echogenicity of the skin. In this study, HFUS were used to assess the influence of scar manual therapy on scar height and their structure (Figure 9). Differences in scar structure regarding the arrangement of collagen fibers, after the therapy, were observed with statistical significance (Avg = 3.1 ± 1.3 vs. Avg = 5.7 ± 1.3; p < 0.005). Manual scar work caused its relaxation and reduced the density of collagen fibers cross‐linking within it. The effect on the scar height was not observed (Figure 10).
FIGURE 9.
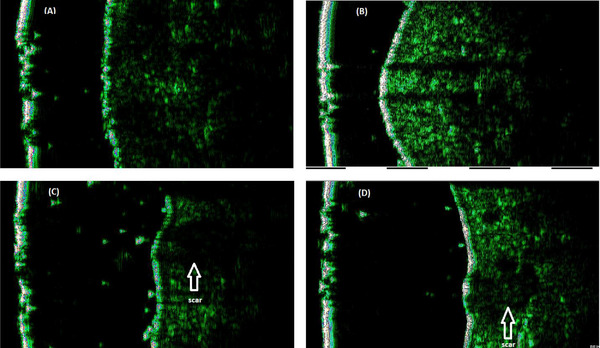
High‐frequency ultrasounds (HFUS) of the skin with scar longitudinal section (A and B) and transverse section (C and D) before (A and C) and after (B and D) manual scar therapy
FIGURE 10.
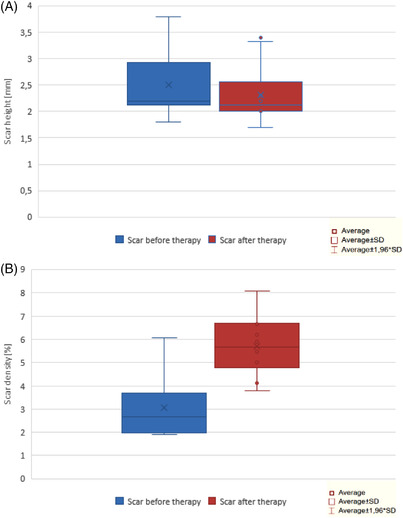
The results of the measurements the scar height (A) and structure (B) before and after manual therapy; average, average ± SD, and average ± 1.96*SD
Differences in skin parameters, including hydration (Avg = 37.8 ± 7.7 vs. Avg = 48.6 ± 1.2; Figure 11), TEWL (g/m2/h) (Avg = 13 ± 4 vs. Avg = 9.7 ± 2.4; Figure 12), stretchability (mm) (Avg = 0.003 ± 0.0003 vs. Avg = 0.05 ± 0.01; Figure 13), and erythema level (Avg = 352.1 ± 103.1 vs. Avg = 249.9 ± 89.8; Figure 14), were found. Level changes of melanin in the scar tissue after treatment were not statistically significant (Avg = 104.9 ± 44 vs. Avg = 83.7 ± 27.7; Figure 14).
FIGURE 11.
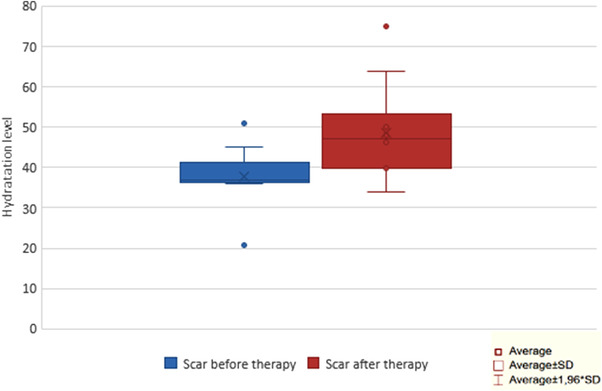
Hydration level of the scar before and after 8 weeks therapy; average, average ± SD, and average ± 1.96*SD
FIGURE 12.
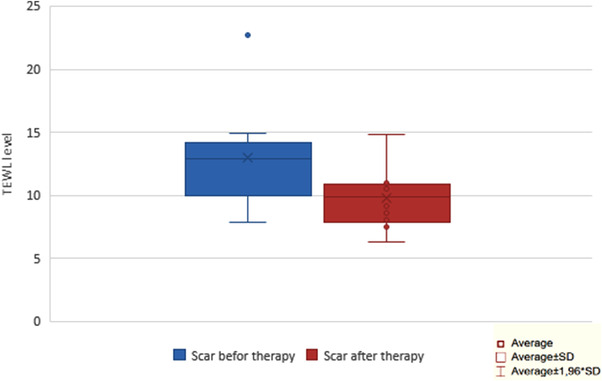
Transepidermal water loss (TEWL) level of scar before and after 8 weeks therapy; average, average ± SD, and average ± 1.96*SD
FIGURE 13.
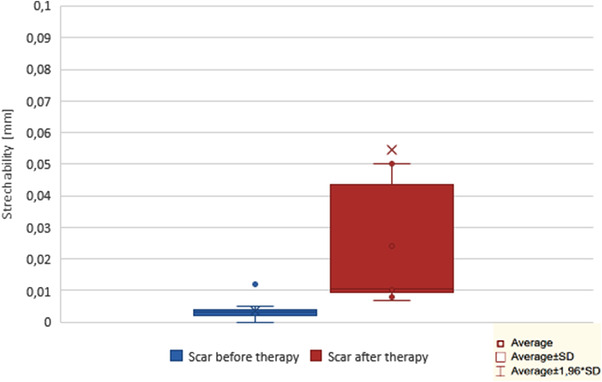
Stretchability level of scar before and after 8 weeks therapy; average, average ± SD, and average ± 1.96*SD
FIGURE 14.
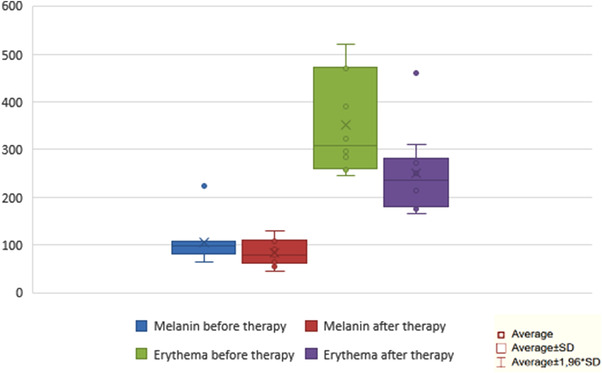
Melanin and erythema level of scar before and after 8 weeks therapy; average, average ± SD, and average ± 1.96*SD
The POSAS was used in the last part of scar evaluation. Patient self‐assessment was performed using the patient component of the POSAS. Volunteers have to rate using scale from 1 to 10, where 1—means lack of indicated feeling and 10—means high intensity feeling. Patient components, which were assessed, were pain, pruritus, color, stiffness, regularity and additionally vascularization, and elasticity. Differences in all groups were statistically significant (Figures 15 and 16). After the therapy, patients were most satisfied with the scar color and elasticity. All respondents observed an improvement in the appearance of the scar and reduction of discomfort associated with this lesion.
FIGURE 15.
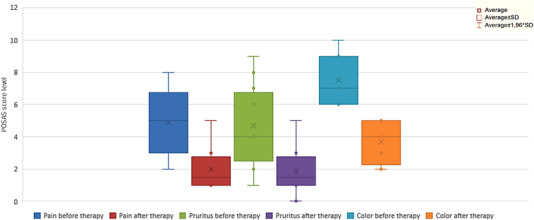
Subjective assessment of scar pain, pruritus, color level before and after therapy; average, average ± SD, and average ± 1.96*SD
FIGURE 16.
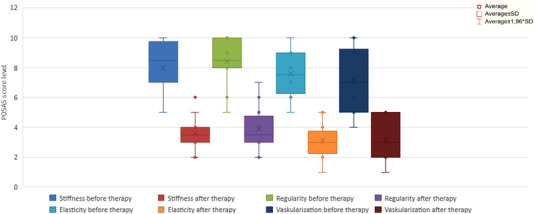
Subjective assessment of scar stiffness, regularity, elasticity, and vascularization level before and after therapy; average, average ± SD, and average ± 1.96*SD
4. DISCUSSION
Scars are a natural result of the healing process. If during this process any disruptions or elongation time of healing appear, it may result in excessive scar tissue formation. The changes in cosmetic appearance, continuing pain, and loss of movement due to contracture or adhesion and persistent pruritis can significantly affect an individual's quality of life and psychological recovery after the injury. The formation of adhesions can bind the visceral organs to other tissues of the abdominal and pelvic wall, causing low back pain, bowel obstruction, infertility, painful bladder syndrome, severe pain with menstruation/ovulation, and decreased mobility. Hypertrophic scarring has a genetic compound but can sometimes also result from repeated or excessive stresses on the wound site during the proliferative phase of healing. Hypertrophic scars often appear thick, wide, and raised from the skin. 1 , 2
The scar therapy is often a neglected element of postoperative physiotherapy. Patients often do not correlate their pain and mobility restrictions with scar tissue. Early treatment can prevent hypertrophy of the scar reduce discomfort and ailments and learn proper skin care. 10 Many different methods may be used to reduce or prevent pathological scarring. Gianatasio et al.3 proposed combination scars treatment customized to scar type, depth, texture, and dyschromia. Early intervention is not essential to scar mitigation. Careful and appropriate treatment algorithms may restore significant scar function. 3
The research team under the direction Kantor et al. 21 utilized a rigorous psychometric approach to develop a new scar rating scale, the Scar Cosmesis Assessment and Rating (SCAR) scale. The SCAR scale consists of six items scored by the observer and two simple yes/no questions answered by the patient. In practice the most popular scales to evaluate the scars are the Observer Scar Assessment Scale and the Vancouver Scar Scale (VSS). VSS enables analysis of scars according to four parameters: the vascularity, pigmentation, pliability, and height of scars. In POSAS, there have also been attempts to include subjective symptoms, such as pain, discomfort, and itching, which had not been considered in previous scar assessment scales. 21 , 22
The manual scar tissue therapy uses techniques such as massage, skin rolling, cupping, myofascial release, dry needling, and instrument‐assisted soft tissue mobilization to help the fiber in scar tissue and fascia to become more aligned. These techniques also reduce tension within the scar and improve blood flow to the area which supports the healing process. The aim of the therapy is to introduce motion and nutrition to the affected tissue which will affect the alignment of the collagen fibers. Taping is used as a supporting method between therapeutic sessions. Tapes promote drainage‐treated area, prevent overloading, and exert a slight, constant pressure on the scar tissue. Although taping is a recommended method for scar therapy, there is not any confirmed treatment procedure. 23 , 24 , 25
The scar massage and manual manipulations are commonly used in the management of linear surgical scarring. They are easy, noninvasive, and low‐cost methods. The scar massage may improve some scar characteristics with evidence supporting its use to reduce pain and increase movement. Deflorin et al., 10 in their systematic review and meta‐analysis concerning on the effect of physical treatment methods on scar tissue, suggested that massage had a positive influence on scar pruritus and pliability. The evidence of improvements in scar thickness was inconclusive. Shin et al., 26 in their earlier literature review, noted that scar massage can be effective, but the lack of a consistent procedure for implementation, complicate an objective evaluation. The similar conclusion is highlighted by Scott et al. in their review. The scar tissue massage may be beneficial in reducing pain, increasing movement, and improving scar characteristics but needs consistent scheme of intervention. Cited protocols used for randomized control trials in the burn scar massage literature include 5 min, three times per week, for 12 weeks with no evidence of long‐term benefit and 30 min, three times per week, for up to 8 weeks with improvements to pain, pruritis, and scar characteristics. Application of scar massage for linear, surgical scar can be different and in clinical practice may be altered to fit the patient. In this study, the treatment protocol includes the scar massage in combination with other manual technique, 30 min, two times per week for 8 weeks. Patients using POSAS evaluate effectiveness therapy in all criteria positively assessed: pain, pruritis, color, stiffness, thickness, regularity, vascularity, and elasticity of scar, after treatment. The scar assessment using high‐frequency ultrasound showed a significant change in tissue structure and also benefits in skin parameters were observed. 10 , 25 , 26 , 27 , 28 , 29
Taping and dry needling are supporting methods. They are more effective combined with other techniques. Dry needling of scars can be an effective method in reduction of pain and other scar‐related symptoms. Existing evidences are limited and require verification. Tapes application in managing scar and keloids has good results as a maintained therapy but also as an independent method. Taping therapy is supposed to weaken subcutaneous adhesions and thus improves the appearance and softness of the scar. In previous studies, Daya and Karwacińska et al. reported statistically significant reduction in itch, pain, thickness, scar elevation, and positive effect on scar color and height. Tape application made scars become brighter, softer, and less elevated. Changes involving scar mobility were also observed, the pulling sensation was reduced, and the range of motion of the involved joint was improved. There are also reports of effectiveness of keloid taping in size and pain intensity reduction. Tapes were mostly applied on 3–5 days with 2–3 days breaks for 12 weeks. The stretch of the tape ranged from 25% to 100%. The final tension depended on an individual evaluation by the therapist. Kinesiotaping is highly effective and recommended especially to hypertrophic, contracture scars, and keloids. 15 , 16 , 17 , 18
Rozenfeld et al.20 suggested a protocol of effective application of needles. Needles (0.25 mm × 30 mm) should be placed along the entire scar in 0.5–1.0 cm increments. Needles should be inserted at a distance of 0.5–1.0 cm from the scar angled 30°–45° toward the scar. Needle twisting should be depended on the patient's sensitivity. The treatment duration is about 20 min once or twice a week until resolution, or a symptom plateau is achieved. 20
The integrated therapy in this study allowed obtaining an effectiveness protocol of manual therapy in linear, surgical scar. Patients’ satisfaction evaluated by POSAS shows significant positive effect in scar characteristic. After 8 weeks of therapy, improvement in scar elasticity, thickness, regularity, and color was observed. Measurements confirm observations. Objective methods of assessment included HFSU, and examination of skin parameters indicates improvement scar hydration, elasticity, and fiber structure. The decrease in the hemoglobin value was also observed. Differences in height of scar and level of melanin were not noticed.
The limitations of the study include a small number of patients, lack of comparison to completely normal skin, and lack of a control group. In future, the research group should be extended, and the comparison with the control group is necessary and single methods with the same conditions.
5. CONCLUSIONS
The manual scar tissue therapy includes a variety of methods and techniques and requires management protocols with details about the type, frequency, time, and duration of the treatment. However, it should be taken into consideration that each therapy requires adaptation to the patient and has to be treated individually.
The therapy, including scar massage, soft tissue manipulation, cupping, dry needling, and taping, was applied in this study. The treatment has a significant positive effect on pain, pigmentation, pliability, pruritus, surface area, and scar thickness. Improvement of skin parameters was also noticed.
To investigate the most effective manual therapy strategy, further studies are needed, evaluating comparisons of different individual and combined scar therapy modalities.
Clinical observations show effectiveness of manual scar therapy. However, the question of which dosage should be applied in which wound healing phase at which intervention time is not easy to answer. Further studies are needed to verify and quantify the efficacy of combined methods, to understand the underlying mechanism, and to establish a protocol of effective intervention.
CONFLICTS OF INTEREST
The authors declare no conflict of interest.
ACKNOWLEDGMENT
This study was supported by the Medical University of Silesia (PCN‐2‐092/N/1/I).
Lubczyńska A, Garncarczyk A, Wcisło‐Dziadecka D. Effectiveness of various methods of manual scar therapy. Skin Res Technol. 2023;29:e13272. 10.1111/srt.13272
DATA AVAILABILITY STATEMENT
Data sharing not applicable.
REFERENCES
- 1. Nouri K, Vidulich K, Rivas MP. Lasers for scars: a review. J Cosmet Dermatol. 2006;5:14‐22. [DOI] [PubMed] [Google Scholar]
- 2. Guo S, DiPietro LA. Critical review in oral biology & medicine: factors affecting wound healing. J Dent Res. 2010;89(3):219‐229. 10.1177/0022034509359125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Gianatasio C, Abrouk M, Waibel JS. Treatment approaches for treating hypertrophic scars and keloids. Dermatol Rev. 2021;2(1):11‐22. 10.1002/der2.64 [DOI] [Google Scholar]
- 4. Elprince M, Taha OT, Ibrahim ZM, et al. Prediction of intraperitoneal adhesions using striae gravidarum and scar characteristics in women undergoing repeated cesarean sections. BMC Pregnancy Childbirth. 2021;21(1):286. 10.1186/s12884-021-03763-z [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 5. Moris D, Chakedis J, Rahnemai‐Azar AA, et al. Postoperative abdominal adhesions: clinical significance and advances in prevention and management. J Gastrointest Surg. 2017;21(10):1713‐1722. 10.1007/s11605-017-3488-9 [DOI] [PubMed] [Google Scholar]
- 6. Chouhan D, Dey N, Bhardwaj N, Mandal BB. Emerging and innovative approaches for wound healing and skin regeneration: current status and advances. Biomaterials. 2019;216:119267. 10.1016/j.biomaterials.2019.119267 [DOI] [PubMed] [Google Scholar]
- 7. Korzekwa K, Sobolewski K, Sobolewski B. Burn wound—the processes of its development and selected etiological factors of infection. Rana Oparzeniowa â Procesy Jej Rozwoju Oraz Wybrane Czynniki Etiologiczne Zakażenia. Postępy Mikrobiologii – Adv Microbiol. 2021;60(4):281‐298. doi: 10.21307/pm-2021.60.4.22 [DOI] [Google Scholar]
- 8. Strodtbeck F. Physiology of wound healing. Newborn Infant Nurs Rev. 2001;1(1):43‐52. 10.1053/nbin.2001.23176 [DOI] [Google Scholar]
- 9. Kauvar ANB, Kubicki SL, Suggs AK, Friedman PM. Laser therapy of traumatic and surgical scars and an algorithm for their treatment. Lasers Surg Med. 2020;52(2):125‐136. 10.1002/lsm.23171 [DOI] [PubMed] [Google Scholar]
- 10. Deflorin C, Hohenauer E, Stoop R, van Daele U, Clijsen R, Taeymans J. Physical management of scar tissue: a systematic review and meta‐analysis. J Altern Complement Med. 2020;26(10):854‐865. 10.1089/acm.2020.0109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Koller T. Mechanosensitive aspects of cell biology in manual scar therapy for deep dermal defects. Int J Mol Sci. 2020;21(6):2055. 10.3390/ijms21062055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zanier E, Bordoni B. A multidisciplinary approach to scars: a narrative review. J Multidiscip Healthc. 2015;8:359‐363. 10.2147/JMDH.S87845 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Murray D, Clarkson C. Effects of moving cupping therapy on hip and knee range of movement and knee flexion power: a preliminary investigation. J Man Manip Ther. 2019;27(5):287‐294. 10.1080/10669817.2019.1600892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Aboushanab TS, AlSanad S. Cupping therapy: an overview from a modern medicine perspective. J Acupunct Meridian Stud. 2018;11(3):83‐87. 10.1016/j.jams.2018.02.001 [DOI] [PubMed] [Google Scholar]
- 15. Klingenstein A, Garip‐Kuebler A, Muth DR, Hintschich C. A prospective randomized pilot study evaluating the scar outcome after gluteal dermis fat graft with and without kinesiotaping. Int Ophthalmol. 2022;42(8):2563‐2571. Published online August 1. 10.1007/s10792-022-02304-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Karabıçak G, Hazar Z, Karabicak GO. A novel aspect in keloid treatment: short term effects of kinesio® taping. J Orthop. 2016;1:6. Case Report Mathews. www.mathewsopenaccess.com [Google Scholar]
- 17. Karwacińska J, Kiebzak W, Stepanek‐Finda B, et al. Effectiveness of kinesio taping on hypertrophic scars, keloids and scar contractures. Polish Ann Med. 2012;19(1):50‐57. 10.1016/j.poamed.2012.04.010 [DOI] [Google Scholar]
- 18. O'Reilly S, Crofton E, Brown J, Strong J, Ziviani J. Use of tape for the management of hypertrophic scar development: a comprehensive review. Scars Burn Heal. 2021;7:205951312110292. 10.1177/20595131211029206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Das G, Khan KJ. Dry needling a novel treatment option for post‐scar neuralgia: a case report. J Recent Adv Pain. 2019;5(1):29‐31. 10.5005/jp-journals-10046-0127 [DOI] [Google Scholar]
- 20. Rozenfeld E, Sapoznikov Sebakhutu E, Krieger Y, Kalichman L. Dry needling for scar treatment. Acupunct Med. 2020;38(6):435‐439. 10.1177/0964528420912255 [DOI] [PubMed] [Google Scholar]
- 21. Kantor J. The SCAR (scar cosmesis assessment and rating) scale: development and validation of a new outcome measure for postoperative scar assessment. Br J Dermatol. 2016;175(6):1394‐1396. 10.1111/bjd.14812 [DOI] [PubMed] [Google Scholar]
- 22. Bae SH, Bae YC. Analysis of frequency of use of different scar assessment scales based on the scar condition and treatment method. Arch Plast Surg. 2014;41(2):111‐115. 10.5999/aps.2014.41.2.111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Nedelec B, Couture MA, Calva V, et al. Randomized controlled trial of the immediate and long‐term effect of massage on adult postburn scar. Burns. 2019;45(1):128‐139. 10.1016/j.burns.2018.08.018 [DOI] [PubMed] [Google Scholar]
- 24. Kelly RC, Armstrong M, Bensky A, Foti A, Wasserman JB. Soft tissue mobilization techniques in treating chronic abdominal scar tissue: a quasi‐experimental single subject design. J Bodyw Mov Ther. 2019;23(4):805‐814. 10.1016/j.jbmt.2019.04.010 [DOI] [PubMed] [Google Scholar]
- 25. Wasserman JB, Copeland M, Upp M, Abraham K. Effect of soft tissue mobilization techniques on adhesion‐related pain and function in the abdomen: a systematic review. J Bodyw Mov Ther. 2019;23(2):262‐269. 10.1016/j.jbmt.2018.06.004 [DOI] [PubMed] [Google Scholar]
- 26. Shin TM, Bordeaux JS. The role of massage in scar management: a literature review. Dermatol Surg. 2012;38(3):414‐423. 10.1111/j.1524-4725.2011.02201.x [DOI] [PubMed] [Google Scholar]
- 27. Scott HC, Stockdale C, Robinson A, Robinson LS, Brown T. Is massage an effective intervention in the management of post‐operative scarring? A scoping review. J Hand Ther. 2022;35:186‐199. Published online April 1. 10.1016/j.jht.2022.01.004 [DOI] [PubMed] [Google Scholar]
- 28. Chae JK, Kim JH, Kim EJ, Park K. Values of a patient and observer scar assessment scale to evaluate the facial skin graft scar. Ann Dermatol. 2016;28(5):615‐623. 10.5021/ad.2016.28.5.615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ault P, Plaza A, Paratz J. Scar massage for hypertrophic burns scarring—a systematic review. Burns. 2018;44(1):24‐38. 10.1016/j.burns.2017.05.006 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing not applicable.


