Abstract
Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder characterized by executive dysfunction. Physical activity (PA) may improve executive dysfunction; however, specific barriers and facilitators to PA participation for adults with ADHD have not been formally documented, which was the aim of the present study. Thirty adults with ADHD completed virtual semi-structured interviews, which were analyzed thematically and guided by the Theoretical Domains Framework. Expressions of both barriers and facilitators to PA were identified. Themes such as executive dysfunction (described as forgetfulness, difficulty with sustained focus, and time management), poor self-esteem, and lack of motivation were seen as barriers to PA. Key facilitators were tied to the benefits of being physically active including improvements in executive functioning, mood, and mental health during and after activity, as well as the enjoyment of being active with others. To better support adults with ADHD in initiating physical activity, it is crucial to develop unique resources that are tailored to their specific needs. These resources should be designed to minimize barriers and maximize facilitators, while also supporting the awareness and acceptance of neurodiverse experiences.
Keywords: ADHD, Physical activity, Qualitive, Barrier, Facilitator
Introduction
Attention deficit hyperactivity disorder (ADHD) is a neurodevelopmental disorder characterized by persistent patterns of inattention and/or hyperactivity-impulsivity that is rooted in deficiencies of executive functioning including inhibition, working memory, and task switching (Felt et al., 2014). Because executive functions are needed for effective decision making (Cristofori et al., 2019), individuals with ADHD often struggle to complete routine tasks, resulting in a sense of underachievement that negatively impacts their daily life (Matheson et al., 2013). While ADHD is commonly diagnosed during childhood, estimates suggest that 65% of childhood ADHD cases persist into adulthood (Wesemann & Van Cleve, 2018) affecting approximately 5% of adults globally (Song et al., 2021). Yet, research on adults with ADHD is lacking (Schneider et al., 2019). In fact, there is a misconception that ADHD is restricted to childhood and, therefore, adults with ADHD are left under-supported by social services and insurance coverage (Singh & Tuomainen, 2015). Furthermore, the first line of treatment for managing symptoms of ADHD is psychostimulant medication (Meppelink et al., 2016); however, research on children suggests that 30% of users do not respond to medication (Geladé et al., 2017). For those who do respond, they can experience an array of unpleasant side effects coupled with the uncertainty concerning the long-term efficacy of using the medication into adulthood.
Physical activity (PA) interventions may be a viable supplementary approach for both children and adults with ADHD. When children with ADHD engage in acute (< 30 min/short-term) and chronic (over the span of several weeks) PA, they can experience notable improvements in their executive functions, including inattention, impulsivity, response inhibition, vigilance, set switching, cognitive control, organization, and planning (Den Heijer et al., 2017; Ng et al., 2017; Pontifex et al., 2014; Quesada et al., 2018; Suarez-Manzano et al., 2018). In turn, PA can improve their academic performance, reading skills, and arithmetic ability (Den Heijer et al., 2017; Ng et al., 2017; Pontifex et al., 2014). It can also reduce certain behavioural symptoms associated with ADHD by boosting self-esteem, wellbeing, and social functioning, while also diminishing interruptive behaviours and comorbid conditions of anxiety and depression (Den Heijer et al., 2017; Pontifex et al., 2014). The sparse evidence available suggests that adults with ADHD experience similar benefits from PA as children with respect to executive functions of inattention, impulsivity, and response inhibition (Den Gapin et al., 2015; Heijer et al., 2017; Mehren et al., 2019). Additionally, physically active adults with ADHD tend to be more motivated, and less worried, tired, and depressed (Den Heijer et al., 2017).
Despite these documented benefits, PA engagement by people with ADHD tends to be lower than their neurotypical peers (i.e., those with typical neurodevelopment; Cook et al., 2015; Fritz & O’Connor, 2018; Quesada et al., 2018) and, in turn, they experience elevated risk of metabolic conditions (e.g., metabolic syndrome and Type 2 diabetes; Landau & Pinhas-Hamiel, 2019). It is conceivable that specific symptoms of ADHD may create unique barriers to engaging in regular PA (Pontifex et al., 2014). For example, given the deficits in the dopamine reward system in the brains of those with ADHD, if a task does not immediately elicit a sense of reward there may be poorer motivation to complete it (Addicott et al., 2019; Barkley et al., 2019). However, to date, there is limited qualitative data directly investigating the lived experiences of adults with ADHD, and their personal accounts of barriers to and facilitators of PA (Bussing et al., 2011; Harvey et al., 2014; Singh & Tuomainen, 2015; Taylor & Foreman, 2019). Identifying barriers and facilitators are important for informing the future development of interventions, and supporting behaviour change in this population (Hussein et al., 2021). The aim of the present study was to fill that gap using semi-structured interviews to capture the lived experiences of adults with ADHD. Questions queried participants’ perceived impact of PA on ADHD symptoms, barriers and facilitators to being physically active, and opinions concerning needed supports and directions for future research.
Methods
Participants
Participants were 30 Canadians between the ages of 18–65 years old, who could communicate in spoken English and had a clinical diagnosis of ADHD. In addition to their self-reported clinical diagnosis, the Conner’s Adult ADHD Rating Scale (CAARS) was used to confirm the presence of ADHD symptoms (Conners et al., 1998). Given COVID-19 restrictions, participants were recruited primarily using social media—specifically via a Canadian adult ADHD Facebook group and through Twitter. Previous participants from ADHD studies in McMaster’s NeuroFit lab were also contacted. The sample size was determined using existing recommendations of 25–30 participants minimum to reach saturation for interview studies (Dworkin, 2012). All procedures were approved by the McMaster Research Ethics Board (#2557), which participants received information about in advance of scheduling their interview. Prior to starting the interview, participants were reminded of the research protocol, that their participation was completely voluntary, that they were able to withdraw their consent at any time, and that their data would be anonymized. Participants provided informed verbal consent to be interviewed and were compensated with a $15 gift card.
Interview Design and Delivery
Semi-structured, one-on-one interviews were conducted via Zoom in an open-ended manner. All interviews were conducted by M.O., a PhD candidate in the NeuroFit lab with training in conducting qualitative work. MO is a woman in her late twenties who studies ADHD and has experience both personally and professionally in connecting with neurodiverse people. Aligning with other qualitative work, the interview consisted of 11 primary questions (see Appendix; Abdelghaffar et al., 2019; Gilbert et al., 2019; Martínez-Andres et al., 2020; Yungblut et al., 2012). We operationally defined PA to participants as any incidental, occupational, and structured movement at all intensities. Given that the interviews took place during the COVID-19 pandemic (March to April 2022), which may have impacted PA behaviour and wellness (Marashi et al., 2021), specific questions were included to contextualize participant experiences before the pandemic, during lockdowns, and at the time of their interview. The interviews were between 20 to 65 min in length, with an average interview time of 40 min ± 12 SD. Interviews concluded with an open-ended question where participants were given the opportunity to discuss anything else that they thought would be relevant to the subject matter, which introduced variability to interview length. After the interview had concluded, participants were debriefed on the purpose of the study and the current evidence supporting benefits of PA for those with ADHD.
Analysis
A total of 30 interviews were completed, with no participant drop out. All interviews were recorded and automatically transcribed via Zoom. Prior to data analysis, transcripts were reviewed against audio recordings by two members of the team (S.K. and B.M.) to ensure accuracy. The transcripts were then loaded into MAXQDA 2022 (1.1) (Kuckartz & Rädiker, 2019) to be analyzed thematically first using an open-coding approach (Walker & Myrick, 2006). Three coders (B.M., S.K., M.O.) conducted the analysis using a stepwise approach, leveraging suggestions outlined by Maguire and Dalahunt (2017) and Connor and Joffe (2020) to improve rigour. While recognizing that a researcher’s personal lens is part of the process when reviewing qualitative data, including multiple coders helped to limit individual bias.
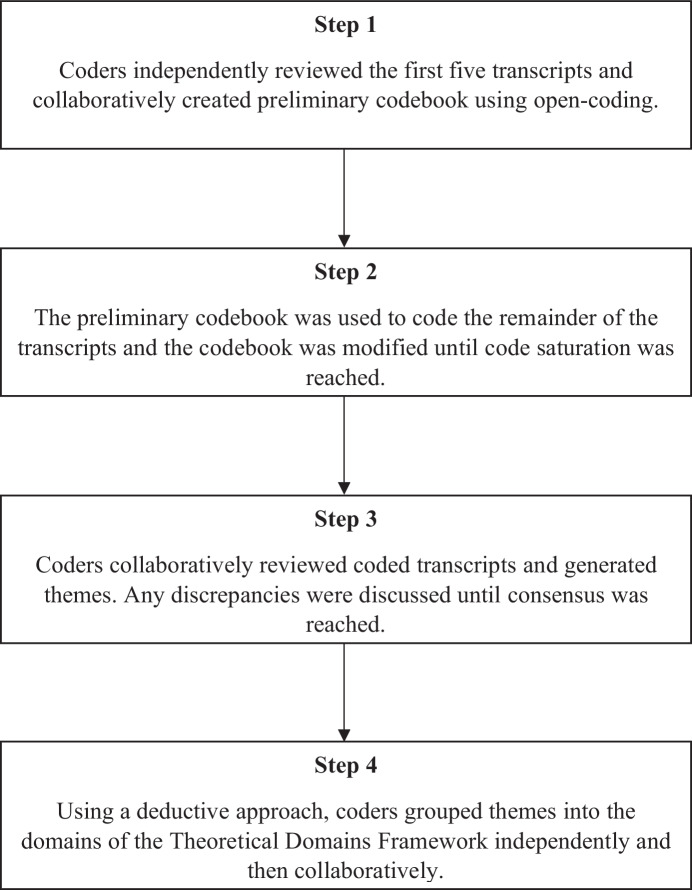
A flow diagram of the analysis process can be seen in Fig. 1. During step one, coders independently reviewed the first five transcripts to familiarize themselves with the data, noting down codes using open coding. Coders then met to create the preliminary codebook. Using the codebook, the coders independently coded the first five interviews. Their codes were compared using the Intercoder Agreement in MAXQDA and resulted in inter-coder reliability (ICR) comparisons > 0.8. ICR is a measure of agreement between different coders reviewing the same data and a score of 0.8 or greater has been noted as an excellent threshold for reliability (Connor & Joffe, 2020). During step two, coders independently reviewed five more interviews (ICR > 0.8) and met to discuss any new codes. After this meeting, all remaining interviews were coded. Anytime a new code was added, previous interviews were recoded (ICR > 0.8). Code saturation was reached when no additional codes were identified and the codebook stabilized (Hennink et al., 2017). In step three, each coded interview was reviewed as a group and themes were generated. Any discrepancies were discussed until a consensus was reached. In step four, the final themes were reviewed and, using a deductive approach, each coder grouped the themes into the domains of the Theoretical Domains Framework (TDF); Atkins et al., 2017). Organization of themes into this behaviour change framework was then reviewed collaboratively and finalized for reporting. Representative excerpts from participants were identified to authentically capture the participants’ perspectives.
Fig. 1.
Overview of steps of thematic analysis
The TDF consists of twelve tenets to explain how behaviour change occurs, including: knowledge; identity; memory, attention, and decision processes; emotions; beliefs about consequences; social influences; beliefs about capabilities; motivation and goals; behavioural regulation; nature of the behaviours; skills, and; environmental context and resources (Atkins et al., 2017).
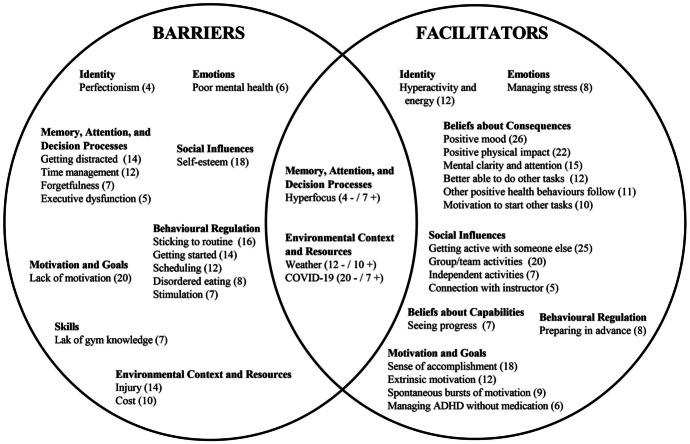
This framework has been previously applied when analyzing and reporting qualitative data assessing PA barriers and facilitators in stroke survivors, pregnant women, school-based programs, and adults (Flannery et al., 2018; Nicholson et al., 2014; Spiteri et al., 2019; Weatherson et al., 2017). Results of the analysis are organized below using participant quotes within the context of the 12 domains from the TDF. See Fig. 2 for an overview and frequency count of themes within each domain.
Fig. 2.
Barriers and facilitators to physical activity for adults with ADHD, categorized within the Theoretical Domains Framework. Bolded headings represent domains from the TDF. Written words below represent identified themes. Numbers represent frequency of theme out of 30 total interviews [when theme overlapped, barrier (-) and facilitator (+)]
Results
Demographics
Participants were 18 to 56 years old (Mean = 29.6, SD = 9.9) and consisted of 25 women and five men, all cis gender. Age of ADHD diagnosis ranged from seven to 56 years old. Twenty-seven participants had a CAARS score > 65; three participants scored below (two participants scored 64, one scored 52). While a score of 65 has been listed as a suggested cut-off, individuals with scores below 65 have been noted to experience similar symptomology (Harrison et al., 2019). As such, all participants were included in the analysis.
Seventy-seven percent reported using ADHD medication at some point since their diagnosis, and 70% were currently using medication. Sixty-seven percent had another diagnosed disorder—most commonly anxiety (40%) and/or depressive (40%) disorder. See Table 1 for a description of participant demographics and Fig. 2 for an overview of identified barriers and facilitators.
Table 1.
Participant Demographic Characteristics
| Characteristic | Variables | N |
|---|---|---|
| Total | 30 | |
| Age | ||
| 18–24 | 10 | |
| 25–34 | 13 | |
| 35–44 | 5 | |
| 45–54 | 0 | |
| 55–64 | 2 | |
| Mean Age (SD) | 29.63 (9.85) | |
| Gender | ||
| Man | 5 | |
| Woman | 25 | |
| Non-Binary | 0 | |
| Highest Level of Education | ||
| Less Than High School | 2 | |
| High School Diploma | 10 | |
| College Degree/Certificate | 5 | |
| Bachelor's Degree | 11 | |
| Master’s/Professional Degree | 2 | |
| Age of ADHD Diagnosis | ||
| Under 12 Years Old | 5 | |
| 12–17 | 6 | |
| 18–24 | 9 | |
| 25–34 | 5 | |
| 35–44 | 3 | |
| 45–54 | 1 | |
| 55–64 | 1 | |
| ADHD Subtype | ||
| Hyperactive | 0 | |
| Inattentive | 6 | |
| Combined | 4 | |
| Unsure/Not Identified | 20 | |
| Comorbid Diagnoses | ||
| Anxiety Disorders | 12 | |
| Mood Disorders | 12 | |
| Autism Spectrum Disorder | 0 | |
| Other Disorder Not Specified Above | 10 |
Knowledge – Knowledge About PA and the Effects of PA for ADHD
Almost a third of participants reported having no formal knowledge about the relationship between PA and ADHD symptoms. Half reported knowing “a little bit”, but very few were confident in this knowledge. Yet, when asked to reflect on their own experiences with PA, more than half believed that exercise likely benefited people with ADHD more than neurotypical people.
“I think it’s one of those things where if I don’t exercise, I’m a terrible person like for myself and others around me where I feel like if somebody who is neurotypical doesn’t exercise they’re still able to function in the world.”
Identity – Personal Factors that Influence PA Engagement
Hyperactivity and high energy levels were noted as a PA facilitator for over a third of participants. However, not all people with ADHD experience hyperactivity (Mowlem et al., 2019; Roberts et al., 2017), and therefore, its role as a PA facilitator may be limited to a subset of individuals with ADHD. “If you’re hyperactive, one way to quench that is to be active.”
Perfectionism was identified as a PA barrier by participants, who likened their need to be ‘perfect’ to their ADHD. "[Those with ADHD] get too nuanced in having the right stuff I find. A lot want to be perfect about it from the outset. Because you feel imperfect."
Memory, Attention, and Decision Process – Influence of Memory, Attention, and Decision on Engagement in PA
“Executive dysfunction”, a hallmark symptom of ADHD, was explicitly identified by participants as a PA barrier. Executive dysfunction made goal-oriented, planned behaviour challenging, such that participants wanted to be physically active but felt that they could not follow through.
"...there are times where you know I really want to go to the gym but that executive dysfunction kicks in and I just don't want to go, or my brain is telling me like go to the gym you have to do it, but my body is like no you're just going to stay here in bed."
Getting distracted, whether it be following instructions or during active participation, was a significant PA barrier, reported by almost half of participants. “When I’m working out, if I’m lifting weights by myself like I just get so distracted and then it takes me so long to get through my workout because I just get distracted.”
Forgetfulness (i.e., forgetting to be physically active or forgetting equipment) was identified as a PA barrier. "I would say it's mostly the working memory and the forgetting to exercise because some days I’ll be like oh yeah I really I intended to work out today, but now I'm in bed and it's 10 o'clock."
Time-management difficulties, including experiences with time-blindness (i.e., being unaware of how much time is passing) and taking longer to do other tasks, was a PA barrier for over a third of participants. "In between sets, I go on my phone and then sometimes…a lot of the time I don't realize how long I've been on my phone. And then I never remember that I'm at the gym."
Hyper-fixation (i.e., being particularly concentrated on one thing; Hupfeld et al., 2019), was identified as both a barrier and facilitator. While fixating on another task (that was not PA) was a barrier for participants, hyper-fixating on PA was a facilitator.
"Like if it's work, for example, I’ll get hyper-focused on that, and then I forget oh it's 10 o'clock at night and I wanted to do something like a yoga practice."
"When I decide that I want to go to the gym, I can't stop thinking about it until I go."
Emotions – Affective States that Influence PA Engagement or Result from PA Engagement
Poor mental health was a barrier for participants who found that feeling depressed or anxious made it difficult to engage in PA. “And especially since comorbidities [alongside having ADHD] with anxiety and depression can come by which can just make it a lot harder to like just get the basic exercise.”
Using PA to manage stress and feeling well-rested was identified as a facilitator.
"Exercise helps to process stress and I think it's even more important because I went up into a manager role, which is increasing executive functioning requirements, which is more difficult for ADHD-ers. Access to lunch hour and that exercise at lunch was removed, and it was really, really challenging."
Beliefs About Consequences – Expectations About Being Physically Active
The positive impact of PA on mood was a facilitator for almost all participants. Being physically active increased mental clarity and attention on subsequent tasks for half of the participants. Two thirds of participants reported that being less physically active decreased their mood and mental health and led to poorer focus.
"Some of the noise quiets down [after being active], and I’m able to focus more on what's happening immediately in front of me."
“But I do find that when my activity is down, my depression does increase, and I do get more anxiety and more scattered brain and less focused."
Positive physical health outcomes (i.e., fitness, weight management, relaxation) and feeling physically better were described as PA facilitators by the majority of participants. Additionally, a third of participants noted how once they engaged in PA, other positive health behaviours followed (i.e., routine, sleeping habits, eating habits). "[Exercising] start[s] cascading effects for every other kind of health benefit in my life. So yeah, kind of started that first domino for me."
A third of participants identified that being physically active resulted in the motivation to start other tasks. Participants also noted that they were not only more motivated to start other tasks, but better able to do them after being physically active. "That's a really productive way for my ADHD to be and it gives me so much energy to keep going and doing stuff."
When discussing the benefits of being physically active, most participants acknowledged that the benefits were most prominent following activity and that those benefits lasted anywhere from a few hours to the full day, with a few identifying benefits beyond the day.
Social Influences – Social Aspects that Influenced PA Engagement
Social pressures and feelings of self-consciousness relating to body image and self-esteem were PA barriers for over half of participants.
"People that struggle with having a lack of exercise with ADHD oftentimes it's something else too, it's not just an ADHD symptom, you know its body dysphoria which could be a symptom from ADHD or something comorbid that maybe isn't diagnosed."
Almost all participants highlighted that the social support from getting active with someone, or “body-doubling”, was a facilitator to being physically active. "Since finding out about my ADHD, I found that body doubling is a very strong motivator. It makes things easier."
Group or team activities were PA facilitators for the majority of participants, who reported feeling a sense of community that led to less loneliness and more fun. However, seven participants felt deterred by group activities and preferred to be physically active alone because it meant they could avoid the fear of letting someone else down.
"I also play soccer in the men's league just to get a bit more group activity, because the gym is typically a lonely thing."
"But things like running, yoga, I'm like okay, no one’s depending on me, I could do this myself."
A meaningful connection with the instructor (i.e., they were friendly, provided well-paced instructions that avoided cognitive overload) was identified as a PA facilitator by a few participants. “It’s a little different when you have someone that is like a drill sergeant and you’re like okay you’re a little scary, and this is too fast, and this is too much stuff for my brain.”
Beliefs About Capabilities – Self-perceptions of Abilities to Engage in PA
A third of participants reported that “seeing progress” with perceived increases in competence, confidence, and self-esteem was an important PA facilitator. "A lot with going to the gym you're going to see progress, and the progress is what really keeps me going."
Motivation and Goals – Reasons Participants Did or Did Not Want to Engage in PA
Not being motivated (in general) was a PA barrier for many participants, and was particularly true during the COVID-19 lockdowns. "I really wish [getting physically active] was easier. I like being active. I like feeling active it's just… it feels like such a Herculean task."
When discussing specific facilitators for PA, examples could be categorized into extrinsic and intrinsic motivators. Extrinsic motivators (i.e., looking good, training for a competition, or being a good role model) and being goal-oriented were PA facilitators. “So a couple weeks ago I was at a wedding it motivated me to work out a little bit wanted to fit into my suit nicely.”
Intrinsic motivators (i.e., feeling a sense of accomplishment, capitalizing on bursts of motivation, and managing ADHD symptoms) were PA facilitators. More than half of participants described that the sense of accomplishment felt from being physically active motivated them.
“I feel in control like hey look, I was able to do something I wasn't motivated to do, I was able to put a plan into action that I wanted to do, and with ADHD, that's a really big success."
Experiencing spontaneous bursts of motivation, attributed to their ADHD, was a PA facilitator for participants. As one participant shared, predicting “when the spirit will move [them]” is difficult, but when a burst in motivation occurs, they are compelled to be active and follow through. “Let’s say like for three weeks, you haven’t been doing a lot of physical activity and then one day ADHD is just like we have to do this right now.”
Participants were motivated to be physically active to manage their ADHD without medication, as they felt similar benefits without negative side effects.
"I didn't want to jump right into medication, and it's still something that I'm on the fence about but I'm willing to try, but I wanted to see if there were ways to manage my ADHD without relying on medication per se."
Behavioural Regulation – Planning Processes for Engaging in PA
Both in relation to their ADHD and more broadly, scheduling (i.e., not enough time, inconvenient timing) PA was a barrier. Over half of participants felt that even after scheduling in PA, it was difficult to stick to their plan and noted a disconnect between their intentions and ability to follow through. "I feel like it’s never a good time [to be active] because I make myself believe that it's not a good time."
Participants commented that the ability to “get going” or start being physically active was “a big hurdle”. Once PA was initiated, participants highlighted a lack of structure and boredom as significant barriers to regulating their behaviour and completing PA. "Sometimes it's harder, again executive functioning, we're not on the same level as like people who probably don't have ADHD so it's like when you don't have that motivation its harder to get it and to start."
Disordered eating (i.e., lack of hunger cues as a side effect from ADHD medication, concurrent diagnoses of eating disorders) was a PA barrier for participants, as having limited energy input made engaging in and following through with PA difficult.
"When I was on Adderall, I ended up losing almost 40 pounds in the span of a year... yes, I can work out every morning, but then I'm not putting back in the energy in my body, so the rest of the day I would be mentally like, “great I did a workout” but physically I'd be exhausted, I'd be starving, I’d feel groggy. I think that also could be the reason why I stopped working out. Instead of feeding myself, I'm just going to end the thing that's making me hungry."
Some participants mentioned that “stimulation” impacted PA levels. As a barrier, feeling overstimulated by other tasks outside of being physically active could lead to feeling “couch locked”. As a facilitator, the PA needed to be mentally and physically stimulating to make engagement worthwhile. "I prefer to do things with friends or like physically stimulating and mentally stimulating things so if there's nothing to encourage me it's just not going to happen. I feel like that's the ADHD version."
Preparing in advance or taking pre-planned actions was a PA facilitator for a few participants. "The night before I'll usually have my gym bag packed, I'll usually have breakfast half meal prepped in the fridge. All those things add up to just getting going in the morning."
Nature of the Behaviours – Developed Routines and Past Experiences with PA
Over half of the participants believed that their previous experiences and past PA behaviours impacted their current decisions to be active. Habitual PA early in life was a PA facilitator for most participants because it established a framework for how to build a routine and use PA to manage ADHD symptoms.
"I never realized the impact [of exercise] on my ADHD until definitely later in life... I feel like I've always had an urge to be physically active. I don't know if that's innate or if that’s because I started early."
Skills – Abilities and Strategies for Engaging in PA
A lack of gym knowledge was a PA barrier for a few participants. They discussed skills in the context of having (or not having) the competency or ability necessary to do their PA of interest. “Or not knowing how to like... not knowing gym equipment very well, but wanting to learn, but being too scared to try learning on my own, where there could be other people watching me or judging me.”
Environmental Context and Resources – Circumstances and Conditions Impacting PA Engagement
Physical injuries, weather, and cost were acknowledged as PA barriers by many participants. The COVID-19 pandemic was an environmental stressor for most participants who noted that pandemic-related changes (i.e., self-isolation, gym closures, and fear of contracting COVID) created PA barriers and led them to be more sedentary.
"These places want to charge you an arm and a leg and the government doesn't support you, because they don't think ADHD is a disability. Then it's like, if you don't have the financial means, you can't do the physical."
“Once the pandemic hit there was a good period of time where I didn’t leave the house at all. I barely left my room so there was no physical activity.”
Convenience and accessibility (i.e., access to transportation, proximity to activity space, and having time) were identified by two thirds of participants as PA facilitators. While most participants reported negative impacts pertaining to COVID, seven participants described being more active during the pandemic because they had more free time.
“Pandemic was nice because I was able to put in that time to start building that sort of dopamine reward system in an environment that was very low on barriers. I didn’t have to worry about, you know, showering right after for a meeting.”
Beyond TDF Domains – Future Considerations
After reflecting on their relationship with PA, participants were asked to share their thoughts on the next steps for future ADHD supports and research. While opinions varied, examples brought up included increasing knowledge about ADHD in adulthood and in women. Over half of participants mentioned wanting tailored, credible, and accessible information about being physically active with ADHD. Participants felt that general guidelines did not always work for them and wanted specific information about how PA impacts symptoms of ADHD, as well as specific strategies for navigating executive dysfunction during exercise. For example, a participant explained how coaches and instructors should be aware that people with ADHD may have different cognitive needs and should be mindful of factors such as instruction pace and detail to ensure everyone can comfortably participate. Finally, a few participants spoke of wanting a sense of community in the form of community classes, events, or support groups specific to those with ADHD.
“ADHD is still one of those invisible illnesses that’s not so understood. You're really trying to advocate for yourself against people who don't have resources themselves.”
“…where it's like well that could work for them, but I don't see how that could work for me.”
Discussion
This is the first study to identify the perceived barriers and facilitators of PA by adults with ADHD. Thirty semi-structured interviews were conducted, analyzed into prominent themes and categorized using the Theoretical Domains Framework (TDF), which has been previously used to organize and conceptualize barriers and facilitators to PA in qualitative work (Flannery et al., 2018; Nicholson et al., 2014; Spiteri et al., 2019; Weatherson et al., 2017). Given the documented benefits of PA for ADHD (Den Heijer et al., 2017; Gapin et al., 2015; Mehren et al., 2019), recognizing what factors prevent and encourage adults with ADHD to engage in PA is important for behaviour change and making decisions about future research. In fact, methods for behaviour change underscore that the first step is to identify barriers and facilitators, from the population's perspective, that need to be overcome or leveraged (Atkins et al., 2017). Figure 2 provides an overview of the key barriers and facilitators noted by participants.
Based on individual accounts, one major barrier identified was a knowledge gap between adults with ADHD and the benefits of PA. When facilitators were identified, almost all were tied to anecdotal experiences of the positive outcomes from PA including the expected benefits to executive functioning, mood, and mental health during or after being physically active. However, most participants reported having no formal education about the benefits of PA to help manage their ADHD symptoms. Additionally, participants who were not previously active—and therefore had not experienced the benefits of PA through past behaviours—were less likely to be active, a finding that is consistent with prior research (Telama, 2009). Ensuring that people are both knowledgeable about the benefits of PA and can get firsthand opportunities to experience the expected outcomes, may help create a positive cycle to increase PA engagement. Providing formal and credible education that is communicated by doctors, psychologists, teachers, and other care providers about the benefits of PA for individuals with ADHD is needed. Creating resources that educate about the connection between PA and ADHD and making them more accessible through avenues such as social media can also help bridge the knowledge gap. In behaviour change settings, communication from credible sources via social media has been beneficial for supporting health and weight management in the general population (Jane et al., 2018; Laverack, 2017) and may be valuable in promoting PA engagement for adults with ADHD.
Additionally, supports on how to navigate symptoms of ADHD when being physically active should be developed and, as revealed by the current findings, are critical for the initiation of PA. Almost all participants commented on feeling less inclined to engage in PA due to their executive dysfunction, a cognitive symptom of ADHD. Executive dysfunction caused problems with forgetfulness, sustained focus, and time management, and made it difficult for participants to initiate PA, despite their best intentions. Like executive dysfunction, hyper-focus, a symptom of ADHD, was a barrier when the focus was directed toward other non-PA tasks. Coping strategies like action planning and advanced preparation were noted by participants as effective for helping to overcome their ADHD-symptom barriers and increasing PA participation. When reflecting on being physically active, participants noted benefits to their executive functioning, which aligns with previous research (Mehren et al., 2019). Having participants engage in more PA may, in turn, improve executive function and the self-regulatory skills needed to be physically active in the future (Daly et al., 2015). Another facilitator connecting to self-regulatory skills was “body doubling”, a common term to describe completing a task with someone else, which can encourage accountability (Burke et al., 2006) and may be particularly useful for adults with ADHD who struggle to self-regulate behaviour. Strategies on how to overcome executive dysfunction and break up periods of hyper-focus such as using overt prompts (e.g., setting an alarm or having someone to check-in or be active with) may help promote PA engagement among adults with ADHD.
Poor self-esteem also prevented adults with ADHD from initiating PA. Compared to their neurotypical peers, children with ADHD tend to have lower self-esteem and more difficulty building relationships, which can carry on into adulthood (Gardner & Gerdes, 2015; Mikami & Normand, 2015), causing anti-social and avoidance behaviours that make it harder to engage in PA (Carter, 2018; Donnellan et al., 2005). As such, inclusive communities (e.g., ADHD groups) and social supports focused on building self-esteem and developing healthy relationships could also bolster PA participation among adults with ADHD. This may simultaneously benefit self-regulation through “body doubling” as mentioned above. Previous research has demonstrated that a sense of belonging or identity with a group is related to increased PA engagement and adherence in local neighborhood communities (Ross & Searle, 2019; Wood et al., 2010). Fostering a sense of community, beyond geographical location, may be valuable for increasing PA engagement in adults with ADHD.
Finally, level of “stimulation” was an ADHD-specific barrier that interfered with both the initiation and maintenance of activity. Being “overstimulated” prior to PA fostered a sense of overwhelm and posed as a barrier to initiating activity. However, the actual PA itself needed to be mentally and physically stimulating enough to maintain the activity, hold engagement, and avoid boredom. To help keep individuals with ADHD interested but not overwhelmed, simple adaptations can be made, such as keeping distractions out of sight and following a logical sequence of engaging activities (Taylor et al., 2019). Additionally, within the context of being physically active, creating more structure may not only reduce overstimulation but also symptoms of impulsivity, hyperactivity, and inattention that tend to worsen when the environment is too unstructured (Higgins et al., 2018; Taylor et al., 2019).
It is important to contextualize the data within our sample. Specifically, participants were mostly women (25/30) who were diagnosed later in life (17/25 diagnosed after 18 years of age) and who had struggled without treatment. Girls and women are more likely to be “missed” in childhood, and go undiagnosed (Quinn & Madhoo, 2014), because their symptoms differ from boys and men (i.e., suppressing hyperactivity symptoms, masking inattentive nature etc.; Holthe & Langvik, 2017). Many participants with late diagnoses voiced that it was “life changing” when they received their diagnosis. This underscores the value of this project in bringing to light the voices of those who often are underrepresented. There were also participants diagnosed with comorbid mental illnesses; 12 noted having an anxiety disorder and 12 noted having a mood disorder. While it is common for those with ADHD to suffer from comorbid mental illnesses (Gnanavel et al., 2019), participants’ accounts of the benefits of PA on their ADHD symptoms may not be independent of the benefits to mental health (Kandola et al., 2019).
Strengths and Limitations
Strengths of the current work include the qualitative approach—as semi-structured interviews allow for more open-ended discussion that captures authentic experiences—and the large sample size of 30 participants. Although using a virtual platform allowed researchers to capture the experiences of adults with ADHD from across Canada, it limited participation to those who have access to some form of technology and social media. Additionally, participants self-reported their formal clinical diagnosis, and many were unsure of whether they were diagnosed with a particular ADHD subtype; no participants explicitly noted having a hyperactive subtype. While most participants were women, it is unclear why. Perhaps women who received later diagnoses are more likely to turn to social media for information and a sense of community. It has been previously documented that women with ADHD have higher rates of social media use (Young et al., 2020), which was our primary recruitment strategy.
While this work captures the lived experiences of 30 adults with ADHD, it does not capture everyone’s experience. For example, no participants in our sample expressed their gender beyond the binary. Also, gender is only one component of social identity; other pieces including race, ethnicity, class, and sexual orientation influence access, power, and privilege, which can impact PA participation (Black et al., 2019; Choi et al., 2017). We did not collect complete information about social location, including race and ethnicity. Given these limitations, it is important to acknowledge that not all perspectives of those with ADHD may be captured by our work. Future research on the barriers and facilitators of PA for those with ADHD should examine different lived experiences from an intersectional lens (Cho et al., 2013). It is possible that if there was a different sample, there may be different barriers and facilitators noted.
Finally, it is important to acknowledge that part of the analysis process incorporated a deductive approach, where themes were organized into domains of the TDF. Though previous work exploring barriers and facilitators has used the TDF to guide their analysis, deductive analysis runs the risk of influencing researcher perspective and that unexpected or unplanned phenomena may be missed. While using an open coding process to generate themes prior to categorizing by the TDF domains helped minimize the risk of missing unexpected phenomena, the limitations of employing a deductive analysis process should be acknowledged.
Conclusion
This is the first study to examine the perceived barriers and facilitators to being physically active as expressed by adults with ADHD. Participants identified unique barriers to being physically active that were often tied to their symptomology including executive dysfunction, hyperfocus, and overstimulation, which made it more difficult for them to initiate PA. Identified facilitators were tied to their beliefs that PA reduced their cognitive symptoms of ADHD and improved their mental health. Many participants expressed never receiving any formal education about the benefits of PA for their ADHD symptoms; however, for those who had been previously active, their prior experience being active was valuable in that it allowed them to recognize the benefits through their experience. Therefore, ensuring those with ADHD are exposed to the benefits of PA (i.e., improved executive functioning, mood, and mental health) early on and receive formal education about the benefits of PA may motivate participation across the lifespan and improve symptoms. Although some strategies have been identified to improve PA engagement for those with ADHD (i.e., removing distractions, action planning, scheduling), our research highlights the need for more individualized supports alongside societal shifts that are inclusive of neurodiverse perspectives. It is essential to not frame ADHD as a problem to solve, but rather to recognize that neurodiverse ways of thinking are not always supported in society (Oliver, 2013). These findings serve as an important foundation for researchers and clinicians who aim to help adults with ADHD become more physically active.
Appendix: Semi-Structured Interview Questions
What sort of physical activity do you currently participate in?
What sort of physical activity have you participated in, in the past?
How, if at all, has your physical activity levels changed since the onset of the COVID-19 pandemic?
How, if at all, do your previous physical activity levels influence your current decisions to participate in physical activity?
When you are being physically active, how do you feel like it impacts you?
What do you believe are the greatest barriers to you being physically active?
What do you believe are the greatest facilitators to you being physically active?
How, if at all, do you feel your ADHD symptoms impact your ability to participate in physical activity?
What, if at all, do you know about the relationship between physical activity and ADHD symptoms?
What information, if any, informed your knowledge about the relationship between physical activity and ADHD symptoms?
How, if at all, would you want to learn about future research related to physical activity and ADHD?
Funding
This work was supported by the Canada Research Chair Program (950–232967).
Compliance with Ethical Standards
Conflict of Interest
The authors have no conflicts of interest to declare.
Ethical Approval
This study was performed in accordance with the ethical standards outlined in the 1964 Declaration of Helsinki and its later amendment.
Informed Consent
The current research involved human participants who gave informed consent before participating in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Abdelghaffar EA, Hicham EK, Siham B, Samira EF, Youness EA. Perspectives of adolescents, parents, and teachers on barriers and facilitators of physical activity among school-age adolescents: A qualitative analysis. Environmental Health and Preventive Medicine. 2019;24(1):21. doi: 10.1186/s12199-019-0775-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Addicott MA, Schechter JC, Sapyta JJ, Selig JP, Kollins SH, Weiss MD. Methylphenidate increases willingness to perform effort in adults with ADHD. Pharmacology, Biochemistry, and Behavior. 2019;183:14–21. doi: 10.1016/j.pbb.2019.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkins L, Francis J, Islam R, O’Connor D, Patey A, Ivers N, Michie S. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implementation Science. 2017;12(1):1–18. doi: 10.1186/s13012-017-0605-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barkley, R. A., Smith, K. M., & Fischer, M. (2019). ADHD risk genes involved in dopamine signaling and metabolism are associated with reduced estimated life expectancy at young adult follow-up in hyperactive and control children. American Journal of Medical Genetics. Part B, Neuropsychiatric Genetics : The Official Publication of the International Society of Psychiatric Genetics, 180(3), 175–185. 10.1002/ajmg.b.32711 [DOI] [PubMed]
- Black N, Johnston DW, Propper C, Shields MA. The effect of school sports facilities on physical activity, health and socioeconomic status in adulthood. Social Science & Medicine. 2019;1982(220):120–128. doi: 10.1016/j.socscimed.2018.10.025. [DOI] [PubMed] [Google Scholar]
- Burke, S. M., Carron, A. V., Eys, M. A., Ntoumanis, N., & Estabrooks, P. A. (2006). Group versus individual approach? A meta-analysis of the effectiveness of interventions to promote physical activity. Sport and Exercise Psychology Review, 2(1), 19–35. http://spex.bps.org.uk/spex/publications/sepr.cfm
- Bussing R, Zima BT, Mason DM, Porter PC, Garvan CW. Receiving treatment for attention-deficit hyperactivity disorder: Do the perspectives of adolescents matter? The Journal of Adolescent Health : Official Publication of the Society for Adolescent Medicine. 2011;49(1):7–14. doi: 10.1016/j.jadohealth.2010.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter JS. Stress and self-esteem in adolescence predict physical activity and sedentary behavior in adulthood. Mental Health and Physical Activity. 2018;14:90–97. doi: 10.1016/j.mhpa.2018.02.005. [DOI] [Google Scholar]
- Cho, S., Crenshaw, K. W., & McCall, L. (2013). Toward a field of intersectionality studies: Theory, applications, and praxis. Signs: Journal of Women in Culture and Society, 38(4), 785–810. 10.1086/669608
- Choi J, Lee M, Lee JK, Kang D, Choi JY. Correlates associated with participation in physical activity among adults: A systematic review of reviews and update. BMC Public Health. 2017;17(1):356. doi: 10.1186/s12889-017-4255-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook BG, Li D, Heinrich KM. Obesity, physical activity, and sedentary behavior of youth with learning disabilities and ADHD. Journal of Learning Disabilities. 2015;48(6):563–576. doi: 10.1177/0022219413518582. [DOI] [PubMed] [Google Scholar]
- Conners, C. K. P., Erhardt, D. P., & Sparrow, E. P. P. (1998). CAARS – Self-Report : Screening Version (CAARS – S: SV ). 800, 2–4.
- Connor CO, Joffe H. Intercoder Reliability in Qualitative Research: Debates and Practical Guidelines. 2020;19:1–13. doi: 10.1177/1609406919899220. [DOI] [Google Scholar]
- Cristofori I, Cohen-Zimerman S, Grafman J. Executive functions. Handbook of Clinical Neurology. 2019;163:197–219. doi: 10.1016/B978-0-12-804281-6.00011-2. [DOI] [PubMed] [Google Scholar]
- Daly M, McMinn D, Allan JL. A bidirectional relationship between physical activity and executive function in older adults. Frontiers in Human Neuroscience. 2015;8:1044. doi: 10.3389/fnhum.2014.01044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Den Heijer, A. E., Groen, Y., Tucha, L., Fuermaier, A. B. M., Koerts, J., Lange, K. W., … Tucha, O. (2017). Sweat it out? The effects of physical exercise on cognition and behavior in children and adults with ADHD: A systematic literature review. Journal of Neural Transmission, 124(S1), 3–26. 10.1007/s00702-016-1593-7 [DOI] [PMC free article] [PubMed]
- Donnellan MB, Trzesniewski KH, Robins RW, Moffitt TE, Caspi A. Low self-esteem is related to aggression, antisocial behavior, and delinquency. Psychological Science. 2005;16(4):328–335. doi: 10.1111/j.0956-7976.2005.01535.x. [DOI] [PubMed] [Google Scholar]
- Dworkin SL. Sample size policy for qualitative studies using in-depth interviews. Archives of Sexual Behavior. 2012;41(6):1319–1320. doi: 10.1007/s10508-012-0016-6. [DOI] [PubMed] [Google Scholar]
- Felt, B. T., Biermann, B., Christner, J. G., Kochhar, P., & Van Harrison, R. (2014). Diagnosis and management of ADHD in children. American Family Physician, 90(7), 456–464. https://www.aafp.org/pubs/afp/issues/2014/1001/p456.html [PubMed]
- Flannery C, McHugh S, Anaba AE, Clifford E, O’Riordan M, Kenny LC, Byrne M. Enablers and barriers to physical activity in overweight and obese pregnant women: An analysis informed by the theoretical domains framework and COM-B model. BMC Pregnancy and Childbirth. 2018;18(1):1–13. doi: 10.1186/s12884-018-1816-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fritz, K., & O’Connor, P. J. (2018). Cardiorespiratory fitness and leisure time physical activity are low in young men with elevated symptoms of attention deficit hyperactivity disorder. Exercise Medicine, 2, 1. 10.26644/em.2018.001
- Gapin JI, Labban JD, Bohall SC, Wooten JS, Chang Y-K. Acute exercise is associated with specific executive functions in college students with ADHD: A preliminary study. Journal of Sport and Health Science. 2015;4(1):89–96. doi: 10.1016/J.JSHS.2014.11.003. [DOI] [Google Scholar]
- Gardner DM, Gerdes AC. A review of peer relationships and friendships in youth with ADHD. Journal of Attention Disorders. 2015;19(10):844–855. doi: 10.1177/1087054713501552. [DOI] [PubMed] [Google Scholar]
- Geladé K, Bink M, Janssen TWP, van Mourik R, Maras A, Oosterlaan J. An RCT into the effects of neurofeedback on neurocognitive functioning compared to stimulant medication and physical activity in children with ADHD. European Child and Adolescent Psychiatry. 2017;26(4):457–468. doi: 10.1007/s00787-016-0902-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilbert, A. S., Duncan, D. D., Beck, A. M., Eyler, A. A., & Brownson, R. C. (2019). A qualitative study identifying barriers and facilitators of physical activity in rural communities. Journal of Environmental and Public Health, 2019. 10.1155/2019/7298692 [DOI] [PMC free article] [PubMed]
- Gnanavel, S., Sharma, P., Kaushal, P., & Hussain, S. (2019). Attention deficit hyperactivity disorder and comorbidity: A review of literature. World Journal of Clinical Cases, 7(17), 2420–2426. 10.12998/wjcc.v7.i17.2420 [DOI] [PMC free article] [PubMed]
- Harrison AG, Nay S, Armstrong IT. Diagnostic accuracy of the Conners' Adult ADHD Rating Scale in a postsecondary population. Journal of Attention Disorders. 2019;23(14):1829–1837. doi: 10.1177/1087054715625299. [DOI] [PubMed] [Google Scholar]
- Harvey W, Wilkinson S, Pressé C, Joober R, Grizenko N. Children say the darndest things: Physical activity and children with attention-deficit hyperactivity disorder. Physical Education and Sport Pedagogy. 2014;19(2):205–220. doi: 10.1080/17408989.2012.754000. [DOI] [Google Scholar]
- Hennink MM, Kaiser BN, Marconi VC. Code Saturation Versus Meaning Saturation: How Many Interviews Are Enough? Qualitative Health Research. 2017;27(4):591–608. doi: 10.1177/1049732316665344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Higgins, A. K., Sluder, J. B., Richards, J. M., & Buchanan, A. M. (2018). A new and improved physical education setting for children with ADHD. Strategies, 31(4), 26–32. 10.1080/08924562.2018.1465869
- Holthe, M. E. G., & Langvik, E. (2017). The strives, struggles, and successes of women diagnosed with ADHD as adults. Sage Open, 7(1), 2158244017701799. 10.1177/2158244017701799
- Hupfeld KE, Abagis TR, Shah P. Living “in the zone”: Hyperfocus in adult ADHD. ADHD Attention Deficit and Hyperactivity Disorders. 2019;11(2):191–208. doi: 10.1007/s12402-018-0272-y. [DOI] [PubMed] [Google Scholar]
- Hussein R, Whaley CR, Lin EC, Grindrod K. Identifying barriers, facilitators and behaviour change techniques to the adoption of the full scope of pharmacy practice among pharmacy professionals: Using the Theoretical Domains Framework. Research in Social and Administrative Pharmacy. 2021;17(8):1396–1406. doi: 10.1016/j.sapharm.2020.10.003. [DOI] [PubMed] [Google Scholar]
- Jane M, Hagger M, Foster J, Ho S, Pal S. Social media for health promotion and weight management: A critical debate. BMC Public Health. 2018;18(1):1–7. doi: 10.1186/s12889-018-5837-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kandola A, Ashdown-Franks G, Hendrikse J, Sabiston CM, Stubbs B. Physical activity and depression: Towards understanding the antidepressant mechanisms of physical activity. Neuroscience and Biobehavioral Reviews. 2019;107:525–539. doi: 10.1016/j.neubiorev.2019.09.040. [DOI] [PubMed] [Google Scholar]
- Kuckartz U, Rädiker S. Analyzing qualitative data with MAXQDA. Springer International Publishing; 2019. pp. 1–290. [Google Scholar]
- Landau Z, Pinhas-Hamiel O. Attention Deficit/Hyperactivity, the Metabolic Syndrome, and Type 2 Diabetes. Current Diabetes Reports. 2019;19(8):46. doi: 10.1007/s11892-019-1174-x. [DOI] [PubMed] [Google Scholar]
- Laverack, G. (2017). The challenge of behaviour change and health promotion. International Journal of Innovative Research and Development, 7(9), 25.10.24940/ijird/2018/v7/i9/SEP18027
- Maguire, M., & Delahunt, B. (2017). Doing a thematic analysis: A practical, step-by-step guide for learning and teaching scholars. All Ireland Journal of Higher Education, 9(3).
- Marashi, M. Y., Nicholson, E., Ogrodnik, M., Fenesi, B., & Heisz, J. J. (2021). A mental health paradox: Mental health was both a motivator and barrier to physical activity during the COVID-19 pandemic. PloS One, 16(4), e0239244. 10.1371/journal.pone.0239244 [DOI] [PMC free article] [PubMed]
- Martínez-Andrés M, Bartolomé-Gutiérrez R, Rodríguez-Martín B, Pardo-Guijarro MJ, Garrido-Miguel M, Martínez-Vizcaíno V. Barriers and facilitators to leisure physical activity in children: A qualitative approach using the socio-ecological model. International Journal of Environmental Research and Public Health. 2020;17(9):3033. doi: 10.3390/ijerph17093033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matheson L, Asherson P, Wong ICK, Hodgkins P, Setyawan J, Sasane R, Clifford S. Adult ADHD patient experiences of impairment, service provision and clinical management in England: A qualitative study. BMC Health Services Research. 2013;13(1):184. doi: 10.1186/1472-6963-13-184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehren A, Özyurt J, Lam AP, Brandes M, Müller HHO, Thiel CM, Philipsen A. Acute Effects of Aerobic Exercise on Executive Function and Attention in Adult Patients With ADHD. Frontiers in Psychiatry. 2019;10:132. doi: 10.3389/fpsyt.2019.00132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meppelink R, de Bruin EI, Bögels SM. Meditation or Medication? Mindfulness training versus medication in the treatment of childhood ADHD: A randomized controlled trial. BMC Psychiatry. 2016;16(1):1–16. doi: 10.1186/s12888-016-0978-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikami AY, Normand S. The importance of social contextual factors in peer relationships of children with ADHD. Current Developmental Disorders Reports. 2015;2(1):30–37. doi: 10.1007/s40474-014-0036-0. [DOI] [Google Scholar]
- Mowlem F, Agnew-Blais J, Taylor E, Asherson P. Do different factors influence whether girls versus boys meet ADHD diagnostic criteria? Sex differences among children with high ADHD symptoms. Psychiatry Research. 2019;272:765–773. doi: 10.1016/j.psychres.2018.12.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng QX, Ho CYX, Chan HW, Yong BZJ, Yeo W-S. Managing childhood and adolescent attention-deficit/hyperactivity disorder (ADHD) with exercise: A systematic review. Complementary Therapies in Medicine. 2017;34:123–128. doi: 10.1016/j.ctim.2017.08.018. [DOI] [PubMed] [Google Scholar]
- Nicholson SL, Donaghy M, Johnston M, Sniehotta FF, van Wijck F, Johnston D, Greig C, McMurdo ME, Mead G. A qualitative theory guided analysis of stroke survivors' perceived barriers and facilitators to physical activity. Disability and Rehabilitation. 2014;36(22):1857–1868. doi: 10.3109/09638288.2013.874506. [DOI] [PubMed] [Google Scholar]
- Oliver, M. (2013). The social model of disability: Thirty years on. Disability & Society, 28(7), 1024–1026. 10.1080/09687599.2013.818773
- Pontifex, M. B., Fine, J. G., Da Cruz, K., Parks, A. C., & Smith, A. L. (2014). VI. The role of physical activity in reducing barriers to learning in children with developmental disorders. Monographs of the Society for Research in Child Development, 79(4), 93–118. 10.1111/mono.12132 [DOI] [PubMed]
- Quesada D, Ahmed NU, Fennie KP, Gollub EL, Ibrahimou B. A Review: Associations Between Attention-deficit/hyperactivity Disorder, Physical Activity, Medication Use, Eating Behaviors and Obesity in Children and Adolescents. Archives of Psychiatric Nursing. 2018;32(3):495–504. doi: 10.1016/j.apnu.2018.01.006. [DOI] [PubMed] [Google Scholar]
- Quinn PO, Madhoo M. A review of attention-deficit/hyperactivity disorder in women and girls: Uncovering this hidden diagnosis. The Primary Care Companion for CNS Disorders. 2014;16(3):27250. doi: 10.4088/PCC.13r01596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts BA, Martel MM, Nigg JT. Are there executive dysfunction subtypes within ADHD? Journal of Attention Disorders. 2017;21(4):284–293. doi: 10.1177/1087054713510349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross A, Searle M. A conceptual model of leisure time physical activity, neighborhood environment, and sense of community. Environment and Behavior. 2019;51(6):749–781. doi: 10.1177/0013916517751582. [DOI] [Google Scholar]
- Schneider, B. C., Schöttle, D., Hottenrott, B., Gallinat, J., & Moritz, S. (2019). Assessment of Adult ADHD in Clinical Practice: Four Letters-40 Opinions. Journal of Attention Disorders, 1087054719879498. Advance online publication. 10.1177/1087054719879498 [DOI] [PubMed]
- Singh SP, Tuomainen H. Transition from child to adult mental health services: Needs, barriers, experiences and new models of care. World Psychiatry. 2015;14(3):358–361. doi: 10.1002/wps.20266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song P, Zha M, Yang Q, Zhang Y, Li X, Rudan I. The prevalence of adult attention-deficit hyperactivity disorder: A global systematic review and meta-analysis. Journal of Global Health. 2021;11:04009. doi: 10.7189/jogh.11.04009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiteri K, Broom D, Bekhet AH, de Caro JX, Laventure B, Grafton K. Barriers and motivators of physical activity participation in middle-aged and older adults—a systematic review. Journal of Aging and Physical Activity. 2019;27(6):929–944. doi: 10.1123/japa.2018-0343. [DOI] [PubMed] [Google Scholar]
- Suarez-Manzano S, Ruiz-Ariza A, De La Torre-Cruz M, Martínez-López EJ. Acute and chronic effect of physical activity on cognition and behaviour in young people with ADHD: A systematic review of intervention studies. Research in Developmental Disabilities. 2018;77:12–23. doi: 10.1016/j.ridd.2018.03.015. [DOI] [PubMed] [Google Scholar]
- Taylor A, Novo D, Foreman D. An Exercise Program Designed for Children with Attention Deficit/Hyperactivity Disorder for Use in School Physical Education: Feasibility and Utility. Healthcare (basel, Switzerland) 2019;7(3):102. doi: 10.3390/healthcare7030102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor A, Foreman D. Exercise to increase engagement of children with attention-deficit/hyperactivity disorder in physical education: Method development. Movement and Nutrition in Health and Disease. 2019;3:33–37. doi: 10.5283/mnhd.18. [DOI] [Google Scholar]
- Telama R. Tracking of physical activity from childhood to adulthood: A review. Obesity Facts. 2009;2(3):187–195. doi: 10.1159/000222244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker D, Myrick F. Grounded theory: An exploration of process and procedure. Qualitative Health Research. 2006;16(4):547–559. doi: 10.1177/1049732305285972. [DOI] [PubMed] [Google Scholar]
- Weatherson KA, McKay R, Gainforth HL, Jung ME. Barriers and facilitators to the implementation of a school-based physical activity policy in Canada: Application of the theoretical domains framework. BMC Public Health. 2017;17(1):1–16. doi: 10.1186/s12889-017-4846-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wesemann D, Van Cleve SN. ADHD: From childhood to young adulthood. Nurse Practitioner. 2018;43(3):8–15. doi: 10.1097/01.NPR.0000530307.76316.cf. [DOI] [PubMed] [Google Scholar]
- Wood, L., Frank, L. D., & Giles-Corti, B. (2010). Sense of community and its relationship with walking and neighborhood design. Social Science & Medicine (1982), 70(9), 1381–1390. 10.1016/j.socscimed.2010.01.021 [DOI] [PubMed]
- Young, S., Adamo, N., Ásgeirsdóttir, B. B., Branney, P., Beckett, M., Colley, W., Cubbin, S., Deeley, Q., Farrag, E., Gudjonsson, G., Hill, P., Hollingdale, J., Kilic, O., Lloyd, T., Mason, P., Paliokosta, E., Perecherla, S., Sedgwick, J., Skirrow, C., Tierney, K., … Woodhouse, E. (2020). Females with ADHD: An expert consensus statement taking a lifespan approach providing guidance for the identification and treatment of attention-deficit/ hyperactivity disorder in girls and women. BMC Psychiatry, 20(1), 404. 10.1186/s12888-020-02707-9 [DOI] [PMC free article] [PubMed]
- Yungblut, H. E., Schinke, R. J., & McGannon, K. R. (2012). Views of adolescent female youth on physical activity during early adolescence. Journal of Sports Science & Medicine, 11(1), 39–50. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3737842/ [PMC free article] [PubMed]