Abstract
Background
Enhanced recovery after surgery (ERAS) is a pathway designed to improve the care of surgical patients and achieve early recovery. The clinical outcomes and usage of key elements of ERAS pathways in total joint arthroplasty (TJA) need further reanalysis. This article aims to provide an overview of the latest clinical outcomes and current usage of key elements of ERAS pathways in TJA.
Methods
We undertook a systematic review of the PubMed, OVID, and EMBASE databases in February 2022. Studies investigating the clinical outcomes and usage of key elements of ERAS in TJA were included. The components of successful ERAS programs and their usage were further determined and discussed.
Results
Twenty‐four studies involving 216,708 patients assessed ERAS pathways for TJA. A total of 95.8% (23/24) of studies reported a reduced length of stay (LOS), followed by reduce overall opioid consumption or pain (87.5% [7/8]), save costs (85.7% [6/7]), improvements in patient‐reported outcomes or functional recovery (60% [6/10]), and reduced incidence of complications (50% [5/10]). In addition, preoperative patient education (79.2% [19/24]), anesthetic protocol (54.2% [13/24]), use of local anesthetics for infiltration analgesia or nerve blocks (79.2% [19/24]), perioperative oral analgesia (66.7% [16/24]), perioperative surgical factors including reduced use of tourniquets and drains (41.7% [10/24]), use of tranexamic acid (41.7% [10/24]) and early mobilization (100% [24/24]) were contemporary comparatively “active” components of ERAS.
Conclusions
ERAS for TJA has favorable clinical outcomes in terms of reducing LOS and overall pain, saving costs, accelerating functional recovery, and reducing complications, although the evidence is still low in quality. In the current clinical scenario, only some “active” components of the ERAS program are widely used.
Keywords: Enhanced Recovery After Surgery, Perioperative Care, Postoperative Care, Systematic Review, Total Joint Arthroplasty
A total of 2761 relevant articles were retrieved, and 24 studies were ultimately included.
Introduction
Total joint arthroplasty (TJA) is one of the most commonly performed elective surgical procedures in the world, and its volume has risen in recent decades. 1 The rapid increase in TJA volume along with huge medical costs poses a great challenge to our healthcare system, of which excess length of hospital stay (LOS) accounts for most of the total costs. 2 Enhanced recovery after surgery (ERAS) pathways are multidisciplinary care pathways that integrate multiple evidence‐based interventions to improve perioperative management, hasten recovery, and improve clinical outcomes as well as save costs. 3 Studies have shown that ERAS adoption optimizes patient care and experience during the perioperative pathway, resulting in reduced LOS and risk of complications with significant hospital cost savings. 4 , 5
Several components have been proposed for the ERAS pathway, including preoperative information education and counseling, preoperative optimization, and preoperative fasting. These protocols are being improved constantly. A recent consensus recommended by the ERAS® Society proposed 17 key recommendations for perioperative care in total hip replacement and total knee replacement surgery. 6 The consensus does provide guidance for perioperative care for TJA patients; however, the recommended key elements may not be widely accepted in clinical practice. In addition, due to the complexity of executing completely recommended ERAS protocols, studies are still needed to simplify the protocols or determine the most important components of care. To achieve the above goals, the contemporary use of the key elements of ERAS pathways in TJA as well as its clinical outcomes should be reviewed.
Regarding the clinical outcomes of the ERAS pathway, most of the studies have reported confusing overall results. Some studies have reported that ERAS usage results in a reduced LOS and a decreased incidence of complications for hip and knee arthroplasty. 7 , 8 Others found that the ERAS pathway reduced LOS after primary TJA but had minimal to no impact on perioperative complications. 9 In addition, the performance and importance of individual components in TJA remain controversial, and the available evidence in the literature has not been systematically reviewed until now. 10 Therefore, the aims of this study are (1) to reanalyze the contemporary performance and clinical outcomes of ERAS in TJA and (2) to evaluate the current usage of ERAS components in TJA and determine the “active” components.
Methods
Search Strategy and Study Selection
The systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta‐Analyses statement. For the principal literature search, we searched the PubMed, OVID, and EMBASE databases to identify relevant articles published prior to February 2022. Medical subject heading terms as well as accompanying entry terms were used. The search parameters were “enhanced postsurgical recovery”, “enhanced postoperative recovery”, “enhanced recovery after surgery”, “enhanced recovery”, “accelerated recovery”, “fast track recovery”, “fast track surgery”, “recovery program” or “recovery pathway,” and “total hip arthroplasty” or “total knee arthroplasty.”
Exclusion and Inclusion Criteria
The criteria of ERAS pathways were defined as follows: (1) included a bundle of multiple perioperative interventions, (2) had labeled differences from traditional care or controlled pathways, and (3) had a formal way of measuring outcomes. Outcome measures included LOS, incidence of complications, readmission rates, patient‐reported outcomes or functional recovery, overall opioid consumption or pain, costs, and/or patients' anxiety and depression or patient satisfaction.
For the full‐text screening, two reviewers independently screened each article based on the following inclusion criteria: (1) the intervention met our study's definition of an ERAS pathway and (2) the article specifically addressed clinical outcomes of ERAS pathway implementation and described the usage of the elements of the ERAS pathway. As the protocols of the ERAS pathway are constantly being improved, it is important to identify studies that have been more recent in the past 5 years. Therefore, we included original studies if they met the above inclusion criteria from any randomized controlled trials (RCTs), retrospective, or prospective studies within the past 5 years.
We excluded studies published before 2017, studies concerning unicompartmental knee replacement, studies without extractable data, studies without addressed clinical outcomes, comments, case reports, posters or letters, editorials, conference abstracts, irrelevant or narrative reviews, guidelines, study protocols, and non‐English studies. Disagreements about study selection were resolved through discussion.
Data Extraction and Quality Assessment
The data of eligible studies were extracted after study selection. The following characteristics were extracted from each study: first author, year of publication, number of patients, study design, mean age, controlled pathway, ERAS program, findings, and outcomes. For statistical description, categorical variables are presented as frequencies and percentages, while continuous variables are presented as the means.
RCTs 11 were appraised using the Jadad score, which ranges from 0 to 5, with 5 being optimal. Nonrandomized studies (prospective or retrospective) were appraised using the Methodological Index for Nonrandomized Studies (MI‐NORS) criteria, which range from 0 to 16, with a higher score reflecting higher quality. 12 Disagreements about study quality were resolved by discussion with a review author until consensus was reached. All studies were appraised by two authors.
Results
Study Selection and Demographic Characteristics
Our original search identified 2761 publications on total joint arthroplasty. After excluding duplicates, we screened 2291 titles and abstracts; 2229 papers were excluded based on their titles and abstracts. We therefore reviewed the full texts of 62 articles. We excluded 38 studies after reviewing the full texts (the reasons for exclusion are given in Figure 1). Finally, 24 studies (n = 216,708) published after 2017 were included; these studies compared the traditional care or controlled pathway (n = 209,330) to ERAS (n = 7378) strategies (Table 1). Of these studies, 14 studies 13 , 14 , 15 , 16 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 retrospectively compared the ERAS pathway with historical or standard controls, and eight 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 prospectively described ERAS pathways with associated controls. The remaining two 35 , 36 studies were conducted as RCTs. Details are shown in Table 1.
FIGURE 1.
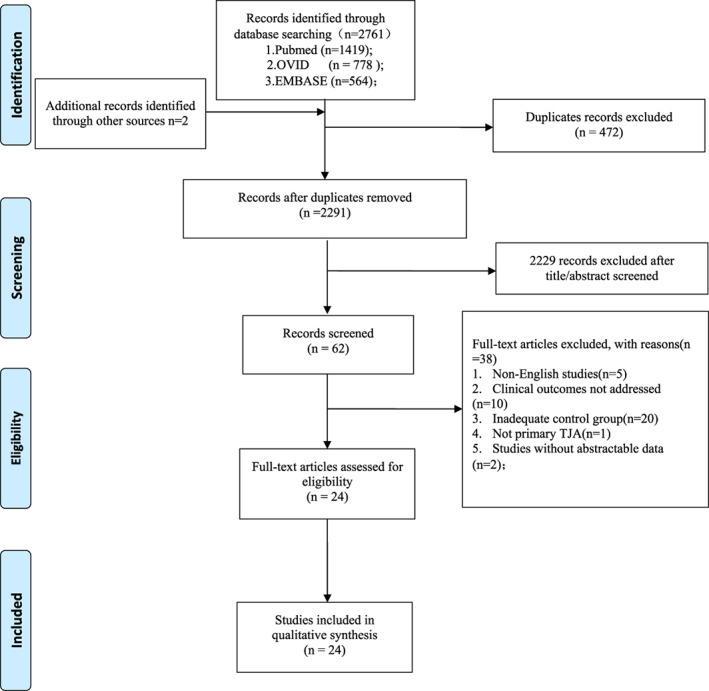
Selection process according to the preferred reporting items for systematic reviews and meta‐analyses statement
TABLE 1.
Study characteristics and patient demographics
| Authors | Study Design | Included number of patients(ERAS pathway) | Surgery | Female (n, %) | Age (Range) | Level of evidence | Quality assessment |
|---|---|---|---|---|---|---|---|
| Javier Ripollés‐Melchor 2020 27 | Prospective cohort study | 6146 (1592) | THA/TKA | 3580 (58.2%) | interquartilerange 71 (63–76, IQR) | III | 12 (MI‐NORS) |
| Sergio Castorina 2018 13 | Retrospective observational study | 132 (95) | TKA | NA | 72.1 | IV | 11 (MI‐NORS) |
| Angela Elizabeth Marchisio 2020 35 | Randomized double blinded clinical trial | 48 (23) | THA | 22 (45.8%) | 64.46 ± 10.37 | II | 3 (Jadad) |
| Joris A Jansen 2020 14 | Retrospective cohort | 686 (403) | TKA | 206 (30%) | 68 years (range 46–88) | III | 10 (MI‐NORS) |
| Robert H Thiele 2021 15 | Retrospective cohort | 1681 (833) | THA/TKA | 426 (53.1%) | 64.5 (55–72) | III | 11 (MI‐NORS) |
| Nicole Lay Tin Tan 2018 28 | Prospective cohort study | 230 (121) | THA | 153 (66.5%) | 64.05 | III | 12 (MI‐NORS) |
| Hong‐Hui Jiang 2019 29 | Prospective controlled study | 247 (106) | TKA | 141 (49.8%) | 74.9 | III | 12 (MI‐NORS) |
| M M T Chung 2021 16 | Retrospective cohort | 228 (111) | THA/TKA | 145 (63.6%) | 50–89 | III | 9 (MI‐NORS) |
| Anouk G M Didden 2019 17 | Retrospective cohort | 170 (85) | TKA | 194 (71.9%) | 69 | III | 9 (MI‐NORS) |
| Pascal‐André Vendittoli 2019 30 | Prospective cohort | 264 (114) | THA/TKA | 137 (51.9%) | 55.9 | III | 11 (MI‐NORS) |
| Aymard De Ladoucette 2020 31 | Prospective observational study | 105,864 (1110) | THA | 611 (55%) | 67.5 ± 11.9 | III | 10 (MI‐NORS) |
| Jean‐Yves Jenny 2021 32 | Observational prospective study | 97,168 (839) | TKA | 525 (62.6%) | 70.3 ± 9.3 | III | 10 (MI‐NORS) |
| Chiara Arienti 2020 33 | Prospective, case–control study | 43 (20) | TKA | 33 (76.7%) | 69 (50–82) | III | 11 (MI‐NORS) |
| Bas L Fransen 2018 36 | Non‐blinded RCT | 49 (25) | TKA | 20 (40.8%) | 62.5 | II | 2 (Jadad) |
| Raul Frankllim de Carvalho Almeida 2021 18 | Retrospective cohort | 98 (47) | THA | 48 (49%) | N/A | III | 10 (MI‐NORS) |
| David J Milligan 2021 19 | Retrospective cohort | 200 (100) | THA/TKA | 126 (63%) | 65.75 | III | 9 (MI‐NORS) |
| Meiyan Zhong 2021 34 | Prospective cohort study | 348 (180) | THA | 197 (56.6%) | 64.5 | III | 11 (MI‐NORS) |
| Baptiste Picart 2021 20 | Retrospective case‐control study | 551 (216) | TKA | N/A | 69.06 ± 9.29 (37–92) | III | 10 (MI‐NORS) |
| Daniel Plessl 2020 21 | Retrospective observational study | 323 (194) | TKA | 217 (67.2%) | 67.1 | III | 9 (MI‐NORS) |
| Yehoshua Gleicher 2021 22 | Retrospective observational study | 615 (383) | TKA | 376 (61.1%) | 66.3 | III | 9 (MI‐NORS) |
| Georgios I Drosos 2020 23 | Retrospective study | 114 (67) | THA/TKA | 89 (78.1%) | 70.4 | III | 9 (MI‐NORS) |
| Blake J Schultz 2019 24 | Retrospective study | 216 (108) | THA/TKA | N/A | 63.15 | III | 9 (MI‐NORS) |
| David P Gwynne‐Jones 2017 25 | Retrospective study | 1035 (528) | THA/TKA | N/A | 68.6 | III | 8 (MI‐NORS) |
| John M Yanik 2018 26 | Retrospective cohort | 252 (78) | THA/TKA | 25 (9.9%) | 66.1 | III | 9 (MI‐NORS) |
Quality Assessment
The quality of the included studies was variable, with an average MI‐NORS score of 9.5 points (range 8–12) and average Jadad scores of 2.5 points (range 2–3), which demonstrates a relatively low study quality. Considerable heterogeneity between individual pathways limits comparisons. Thus, we conducted a systematic review due to the generally poor quality of the studies. The MI‐NORS and Jadad scores of each study are shown in Table 1.
Latest Clinical Outcomes
LOS
The results of LOS varied considerably (Table 2). Among them, 95.8% (23/24) of the studies reported a significantly reduced LOS of the ERAS pathway to different degrees compared with the standard/traditional pathway, but one study reported a reduced LOS without statistical significance.
TABLE 2.
Summary of clinical outcomes after Implementation of ERAS programs
| Reduced LOS | Reduced incidence of complications | Reduced readmission rates | Improvements in patient‐reported outcomes or functional recovery | Reduce overall opioid consumption or pain | Save costs | Decreased anxiety and depression or improved patient satisfaction | Others | |
|---|---|---|---|---|---|---|---|---|
| Javier Ripollés‐Melchor 2020 27 | √ | √ | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | |
| Sergio Castorina 2018 13 | √ | Not mentioned | Not mentioned | √ | √ | Not mentioned | Not mentioned | |
| Angela Elizabeth Marchisio 2020 35 | √ | Not mentioned | Not mentioned | No difference | Not mentioned | Not mentioned | Not mentioned | Higher muscle strength |
| Joris A Jansen 2020 14 | √ | No difference | Not mentioned | No difference | Not mentioned | √ | Not mentioned | |
| Robert H Thiele 2021 15 | √ | Not mentioned | Not mentioned | Not mentioned | √ | √ | Not mentioned | Aggregate increase in profit |
| Nicole Lay Tin Tan 2018 28 | √(Not statistically significant) | Not mentioned | 8 in ERAS and 5 in traditional pathway | No difference | No difference | Not mentioned | Not mentioned | |
| Hong‐Hui Jiang 2019 29 | √ | √ | Not mentioned | √(Short term) | Not mentioned | No difference | Not mentioned | Decreased intraoperative blood loss, total blood loss, transfusion rate |
| M M T Chung 2021 16 | √ | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | |
| Anouk G M Didden 2019 17 | √ | Not mentioned | √ | Improved functional recovery time | Not mentioned | Not mentioned | Not mentioned | |
| Pascal‐André Vendittoli 2019 30 | √ | √ | Not mentioned | Not mentioned | Not mentioned | √ | Not mentioned | |
| Aymard De Ladoucette 2020 31 | √ | Not mentioned | √ | Not mentioned | Not mentioned | Not mentioned | Not mentioned | |
| Jean‐Yves Jenny 2021 32 | √ | Not mentioned | √ | Not mentioned | Not mentioned | Not mentioned | Not mentioned | |
| Chiara Arienti 2020 33 | √ | Not mentioned | Not mentioned | √ | √ | Not mentioned | Not mentioned | |
| Bas L Fransen 2018 36 | √ | No difference | Not mentioned | √(First week) | √(First 7 days) | Not mentioned | Not mentioned | |
| Raul Frankllim de Carvalho Almeida 2021 18 | √ | No difference | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Decreased blood transfusion and usage of the critical care unit |
| David J Milligan 2021 19 | √ | Not mentioned | No difference | Not mentioned | Not mentioned | √ | Not mentioned | ERAS patients had a small increases in postoperative resource usage |
| Meiyan Zhong 2021 34 | √ | √ | Not mentioned | Not mentioned | √ | Not mentioned | √ | |
| Baptiste Picart 2021 20 | √ | Not mentioned | No difference | Not mentioned | √ | Not mentioned | Not mentioned | |
| Daniel Plessl 2020 21 | √ | Not mentioned | Not mentioned | √ | Not mentioned | Not mentioned | Not mentioned | |
| Yehoshua Gleicher 2021 22 | √ | Not mentioned | √ | Not mentioned | √ | Not mentioned | Not mentioned | |
| Georgios I Drosos 2020 23 | √ | No difference | No difference | Not mentioned | Not mentioned | Not mentioned | Not mentioned | |
| Blake J Schultz 2019 24 | √ | √ | No difference | Not mentioned | Not mentioned | √ | Not mentioned | |
| David P Gwynne‐Jones 2017 25 | √ | Not mentioned | No difference | √ | Not mentioned | Not mentioned | √ | 30‐day readmission rate increased from 3.2% to 5.5% (p = 0.065) |
| John M Yanik 2018 26 | √ | No difference | No difference | Not mentioned | Not mentioned | √ | Not mentioned | Lower unplanned readmissions and overall complications without statistically significance |
| Total | 95.8% (23/24) | 50% 5/10) | 36.4% (4/11) | 60% (6/10) | 87.5% (7/8) | 85.7% (6/7) | 2 |
Complications
The results of complications were also varied, and nine studies reported outcomes (Table 2). A total of 55.6% (5/9) of the studies found that the ERAS pathway had a reduced incidence of complications compared with the traditional pathway. Ripollés‐Melchor et al. 27 found that patients with the highest adherence to ERAS components had fewer overall postoperative complications. Jiang et al. 29 reported that the ERAS pathway had significantly fewer total complications without a significant difference in short‐term mortality. Vendittoli et al. 30 found that the ERAS pathway had a significantly lower rate of grade 1 and 2 complications according to the Clavien–Dindo classification; however, the difference in complications of grades 3, 4, or 5 was not significant. Schultz et al. 24 also found that the ERAS protocol had significantly fewer overall complications than traditional protocols (7% vs. 21%), specifically fewer acute medical complications (4% vs. 12%). Zhong et al. 34 reported that the ERAS pathway had lower incidences of deep vein thrombosis in the lower limbs, urinary tract infection, and pulmonary infection than the standard pathway. However, the rest of the studies found no notable difference in the overall postoperative complication rate between ERAS and the standard/traditional pathway (Table 3).
TABLE 3.
Summary of current usage of the key elements recommended by EARS society
| Preoperative information, education, and counseling | Preoperative optimization | Preoperative fasting | Standard anesthetic protocol | Perioperative surgical factors | Use of local anesthetics for infiltration analgesia(1) and nerve blocks(2) | Maintaining normothermia | Perioperative fluid management | Postoperative nausea and vomiting | Prevention of perioperative blood loss | Perioperative oral analgesia | Antimicrobial prophylaxis | Antithrombotic prophylaxis treatment | Postoperative nutritional care | Early mobilization | Criteria‐based discharge | Continuous improvement and audit | Others | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Javier Ripollés‐Melchor 2020 27 | √ | √ | √ | Not mentioned | Not mentioned | √(1) | √ | √ | √ | Not mentioned | Not mentioned | √ | √ | √ | √ | Not mentioned | Not mentioned | Postoperative glycemic control |
| Sergio Castorina 2018 13 | √ | Not mentioned | Not mentioned | Not mentioned | √ | Not mentioned | Not mentioned | Not mentioned | √ | √ | Not mentioned | Not mentioned | Not mentioned | Not mentioned | √ | Not mentioned | Not mentioned | Parapatellar medial incision; no tourniquet fascia and articular drainage; continuous elastomeric pumps infusion for pain control |
| Angela Elizabeth Marchisio 2020 35 | Not mentioned | Not mentioned | Not mentioned | √ | √ | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | √ | Not mentioned | Not mentioned | Not mentioned | √ | Not mentioned | Not mentioned | Spinal anesthesia; posterior approach |
| Joris A Jansen 2020 14 | √ | Not mentioned | Not mentioned | √ | √ | √(1) | Not mentioned | Not mentioned | √ | Not mentioned | √ | Not mentioned | Not mentioned | Not mentioned | √ | √ | Not mentioned | Spinal anesthesia; No wound drains, urinary catheters or patient‐controlled analgesia pumps |
| Robert H Thiele 2021 15 | √ | Not mentioned | √ | Not mentioned | Not mentioned | √(1 + 2) | Not mentioned | √ | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | √ | Not mentioned | Not mentioned | |
| Nicole Lay Tin Tan 2018 28 | √ | Not mentioned | √ | √ | Not mentioned | Not mentioned | √ | √ | √ | √ | √ | Not mentioned | Not mentioned | Not mentioned | √ | √ | Not mentioned | Increase in spinal anesthesia and decrease in general anesthesia |
| Hong‐Hui Jiang 2019 29 | √ | √ | √ | √ | Not mentioned | √(1) | √ | √ | √ | √ | √ | Not mentioned | Not mentioned | √ | √ | Not mentioned | Not mentioned | Spinal (preferred) or general anesthetic; Joint function and Lung function exercise |
| M M T Chung 2021 16 | √ | Not mentioned | Not mentioned | √ | √ | √(1 + 2) | Not mentioned | Not mentioned | √ | √ | √ | Not mentioned | Not mentioned | Not mentioned | √ | Not mentioned | Not mentioned | Spinal anesthesia(preferred); medial parapatellar approach; higher dose of intravenous steroid; hypnotics |
| Anouk G M Didden 2019 17 | √ | Not mentioned | Not mentioned | √ | Not mentioned | √(1) | Not mentioned | Not mentioned | Not mentioned | Not mentioned | √ | Not mentioned | Not mentioned | Not mentioned | √ | √ | Not mentioned | spinal analgesia or general anesthesia |
| Pascal‐André Vendittoli 2019 30 | √ | √ | √ | √ | √ | √(1) | Not mentioned | √ | Not mentioned | √ | √ | √ | √ | √ | √ | Not mentioned | Not mentioned | Spinal (preferred) or general anesthetic; no tourniquet |
| Aymard De Ladoucette 2020 31 | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | √(1) | Not mentioned | Not mentioned | Not mentioned | Not mentioned | √ | Not mentioned | √ | Not mentioned | √ | √ | Not mentioned | |
| Jean‐Yves Jenny 2021 32 | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | √(1 + 2) | Not mentioned | Not mentioned | Not mentioned | Not mentioned | √ | Not mentioned | Not mentioned | Not mentioned | √ | √ | Not mentioned | One dose of peri‐operative glucocorticoids |
| Chiara Arienti 2020 33 | Not mentioned | Not mentioned | Not mentioned | Not mentioned | √ | √(1) | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | √ | Not mentioned | Not mentioned | Sub‐vastus approach vs. midline approach |
| Bas L Fransen 2018 36 | √ | Not mentioned | Not mentioned | Not mentioned | √ | √(1) | Not mentioned | Not mentioned | Not mentioned | Not mentioned | √ | Not mentioned | Not mentioned | Not mentioned | √ | Not mentioned | Not mentioned | No tourniquet; sub‐vastus approach vs. midline approach; no pain pumps, wound drains or bladder catheters |
| Raul Frankllim de Carvalho Almeida 2021 18 | √ | Not mentioned | Not mentioned | √ | √ | √(1) | Not mentioned | Not mentioned | Not mentioned | √ | Not mentioned | Not mentioned | Not mentioned | Not mentioned | √ | √ | Not mentioned | Spinal or general Anesthetic; no delayed bladder catheterization |
| David J Milligan 2021 19 | √ | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | √ | Not mentioned | √ | Post‐ discharge phone call one day after discharge |
| Meiyan Zhong 2021 34 | √ | Not mentioned | √ | Not mentioned | Not mentioned | Not mentioned | √ | √ | Not mentioned | Not mentioned | √ | Not mentioned | Not mentioned | Not mentioned | √ | Not mentioned | Not mentioned | Nutrition assessment before and after the operation |
| Baptiste Picart 2021 20 | √ | √ | √ | Not mentioned | √ | √(1) | Not mentioned | Not mentioned | Not mentioned | √ | √ | Not mentioned | Not mentioned | √ | √ | √ | Not mentioned | No perineural block, tourniquet or drainage. An intra‐articular catheter was fitted for less than 24 h |
| Daniel Plessl 2020 21 | Not mentioned | Not mentioned | Not mentioned | √ | Not mentioned | √(2) | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | Not mentioned | √ | Not mentioned | Not mentioned | Planned discharge to home on the day of surgery; spinal anesthesia with a single adductor block |
| Yehoshua Gleicher 2021 22 | √ | Not mentioned | Not mentioned | √ | √ | √(1 + 2) | Not mentioned | Not mentioned | √ | Not mentioned | √ | Not mentioned | Not mentioned | Not mentioned | √ | Not mentioned | Not mentioned | No preoperative catheterization and intermittent catheterization; shorter duration spinal anesthetics |
| Georgios I Drosos 2020 23 | √ | Not mentioned | Not mentioned | Not mentioned | Not mentioned | √(1) | Not mentioned | Not mentioned | Not mentioned | √ | √ | √ | √ | Not mentioned | √ | Not mentioned | √ | |
| Blake J Schultz 2019 24 | √ | √ | Not mentioned | √ | Not mentioned | √(1) | Not mentioned | Not mentioned | Not mentioned | √ | √ | Not mentioned | Not mentioned | Not mentioned | √ | Not mentioned | Not mentioned | Perioperative spinal anesthesia; Peripheral nerve blocks were not routinely used |
| David P Gwynne‐Jones 2017 25 | √ | √ | Not mentioned | √ | Not mentioned | √(1 + 2) | √ | √ | Not mentioned | √ | √ | Not mentioned | Not mentioned | Not mentioned | √ | √ | Not mentioned | Day of surgery admission; Spinal anesthesia + intrathecal morphine |
| John M Yanik 2018 26 | √ | Not mentioned | Not mentioned | √ | Not mentioned | √(1) | Not mentioned | Not mentioned | Not mentioned | Not mentioned | √ | Not mentioned | Not mentioned | Not mentioned | √ | Not mentioned | Not mentioned | Implementation of spinal anesthesia and elimination of femoral nerve blocks |
| Total | 79.2% (19/24) | 16.7% (4/24) | 29.2% (7/24) | 54.2% (13/24) | 41.7% (10/24) | 79.2% (19/24) | 20.8% (5/24) | 29.2%(7/24) | 29.2%(7/24) | 41.7%(10/24) | 66.7%(16/24) | 12.5%(3/24) | 16.7% (4/24) | 16.7% (4/24) | 100%(24/24) | 33.3%(8/24) | 8.3%(2/24) |
Readmission Data
Eleven studies reported appropriate readmission data, and three were prospective studies. A total of 36.4% (4/11) of studies found that the ERAS pathway decreased readmission rates. However, Tan et al. 28 reported mildly increased readmission rates. They found that eight of 115 patients had an unplanned readmission in the ERAS pathway for reasons including hip fractures, urinary retention, and allergies. Five of 115 patients in the traditional/standard pathway had an unplanned readmission to the hospital for reasons including hip fractures, surgical infection, pneumonia and pain management.
Functional Outcome
Ten studies reported functional outcomes, of which three were prospective studies and two were RCTs. Sixty percent (6/10) of studies found that the ERAS pathway improved patient‐reported outcomes or functional recovery. Fransen et al. 36 found that patients in the ERAS pathway had significantly lower knee pain scores and improved functional outcomes in the first 7 days after TKA compared to a regular protocol. Similarly, Jiang et al. 29 also found that ERAS patients had higher KSS scores of the knee than traditional patients at POD 1 and POD 5; they also found that ERAS patients had a significantly increased ROM degree at POD 1; however, the ROM of the knee tended to be comparable at POD 5.
Pain Management
Eight studies assessed the impact of the ERAS pathway on pain management in patients undergoing TJA. A total of 87.5% (7/8) of patients in the ERAS pathway had reduced pain parameters. Fransen et al. 36 found that ERAS patients have lower mean VAS scores for knee pain than their controls during movement with weight bearing of the affected knee in the first 7 days, which is significant on POD4 and POD6, and the pain tended to decrease during the following time up to 12 weeks and remained at comparatively lower levels than that in the standard/traditional patients.
Hospitalization Cost and Patients' Experience
Seven studies reported the effect of the ERAS pathway on hospitalization costs. A total of 85.7% (6/7) of studies favored the usage of the EARS pathway in TJA to achieve cost‐effectiveness. However, few studies have reported changes in anxiety, depression, or satisfaction in patients after undergoing ERAS. Only two studies 25 , 34 found that ERAS implementation decreased anxiety and depression or improved patient satisfaction compared with the traditional/standard pathway.
Current Usage of the Key Elements
The guidelines recommended by the ERAS Society 6 described and proposed 17 key ERAS components for total hip replacement and total knee replacement surgery. As seen from our results, the usage of the ERAS pathway has been widely accepted in TJA to achieve an accelerated recovery of patients. However, the components of the ERAS pathway were used differently, although there are some coordinated “active” components.
Preadmission Phases
Preoperative Education
Preoperative education can provide information about perioperative exercise, rehabilitation, and expectations of LOS, which is useful to reduce the anxiety of patients but improve their understanding of the surgery. A total of 79.2% (19/24) of studies recorded the usage or partial usage of preoperative information, education, and expectation counseling. The largest study was conducted by Ripolles‐Melchor et al. 27 which was a prospective cohort study that included 1592 patients who adopted the ERAS pathway. They conducted preoperative education on the ERAS pathway via verbal and written consent; however, the details of education were not mentioned.
Preoperative Phases
Preoperative Optimization
The aim of optimization is to optimize preoperative risk factors, such as smoking, alcohol consumption, anemia, nutritional and metabolic status, and low physical activity, to reduce the occurrence of potential complications or a prolonged length of stay. However, only 16.7% (4/24) of studies highlighted the usage of preoperative optimization in their ERAS protocols.
Preoperative Fasting
The traditional purpose of fasting is to reduce the risk of aspiration at the induction of anesthesia.
The ERAS society recommended the intake of clear fluids until 2 h before the induction of anesthesia and a 6‐h fast for solid food. 6 However, only 29.2% (7/24) of studies highlighted this strategy as a part of their EARS protocols.
Perioperative Oral Analgesia
Pain can heavily limit the recovery of patients, while appropriate analgesia can facilitate early postoperative mobility and recovery. Perioperative oral analgesia in the ERAS pathways may yield additional pain relief for patients undergoing TJA, especially using nonopioid oral analgesia, including paracetamol and NSAIDs. A total of 66.7% (16/24) of studies highlighted the usage of perioperative oral analgesia in their EARS pathway.
During Surgery Phases
Anesthetic Protocol: Systemic and Regional Anesthesia
A consensus of the standard anesthetic protocol in the ERAS setting is still lacking. A total of 54.2% (13/24) of studies highlighted the importance of the anesthetic protocol in their ERAS pathway. Among them, 84.6% (11/13) chose a spinal‐preferred anesthetic protocol. Only two studies 17 , 18 reported that both spinal analgesia and general anesthesia were acceptable. However, Palanne et al. 37 found through a randomized controlled trial that for TKA patients, spinal anesthesia shared a similar condition with general anesthesia in terms of 24‐h postoperative opioid consumption, pain management, blood transfusions, in‐hospital complications, and length of hospital stay; however, vomiting incidence in the spinal anesthesia group was higher than that in the general anesthesia group.
Regional or local anesthesia plays a vital role in controlling postoperative pain and enhancing mobilization. Among them, local infiltration analgesia (LIA) has an advantage over nerve blocks because it produces no motor blockade and has little interference effect on muscle strength. In addition, 79.2% (19/24) of studies reported the use of local anesthetics for nerve blocks or infiltration analgesia as an important part of their EARS protocols. In addition, 63.2% (12/19) of studies adopted the intraoperative use of local infiltration analgesia. A prospective study compared LIA, peripheral nerve blocks, general and spinal anesthesia on early functional recovery, and pain control in primary TKA, and they found that pain relief was comparable within the four groups and that LIA showed significant advantages in mobilization and muscle strength in the early postoperative period. 38
Prevention of Perioperative Blood Loss
Pronounced blood loss was indicated in TJA, and tranexamic acid (TXA) has been favored to decrease blood loss and reduce the risk for transfusion. 39 Studies have demonstrated that the use of TXA is both efficient and safe and has little effect on the risks of venous thromboembolic events 39 ; even 3 g of TXA has no significant effect on the level of D‐dimer, an important diagnostic parameter of thrombosis. 40 , 41 Furthermore, a systematic review and meta‐analysis also revealed that TXA plus drain clamping is more efficient than its control (including TXA alone and drain clamping alone) to control blood loss after TKA, which can significantly reduce the need for transfusion, total blood loss, blood loss in drainage, and the decrease in hemoglobin. 42 In this review, we found that only 41.7% (10/24) of the studies reported the use of TXA to prevent perioperative blood loss.
Maintaining Normothermia
Failing to maintain perioperative normothermia can result in devastating physiologic consequences, including increased catabolism and wound infections as well as increased surgical bleeding. 43 Therefore, maintaining normothermia in TJA patients should be targeted as an important part of anesthetic care. However, only 20.8% (5/24) of the studies highlighted this strategy in their ERAS protocols.
Antimicrobial Prophylaxis
Infection after TJA is a serious consequence that is difficult to treat, and evidence has demonstrated that TJA patients benefit from surgical antibiotic prophylaxis. 44 Antimicrobial prophylaxis is now the standard of care for patients receiving hip or knee arthroplasty. 45 A systematic review and meta‐analysis conducted by Siddiqi et al. 44 found that surgical antibiotic prophylaxis continued beyond 24 h in TJA and added no benefit to the prevention of surgical site infection. However, for patients at high risk for infection, extended postoperative antibiotic prophylaxis may lead to a statistically significant reduction in the 90‐day infection rate after primary TJA. 46 However, only 12.5% (3/24) of the studies highlighted antimicrobial prophylaxis in their EARS pathways.
Perioperative Surgical Factors
Perioperative surgical factors may influence outcomes, complications, and recovery rates. Among them, the use of a tourniquet may aggravate muscle injury and cause swelling, increase postoperative pain, and impair early functional recovery, while drainage may increase blood loss and the transfusion rate. 47 , 48 A total of 41.7% (10/24) of the studies highlighted the importance of perioperative surgical factors in their ERAS protocols. Sixty percent (6/10) of studies 13 , 14 , 16 , 33 , 35 , 36 reported the use of specific surgical approaches; 50% (4/8) of studies 13 , 20 , 30 , 36 with knee replacement highlighted the reduced or abandoned use of tourniquets; and 60% (6/10) of studies 13 , 14 , 18 , 20 , 22 , 36 did not support the routine use of drains. Furthermore, only two studies 13 , 36 supported the use of specific surgical approaches and reduced or abandoned the use of tourniquets and drains. Though surgical approach is hotly discussed in TJA, the preferred surgical approach was not highlighted or recommended in the guidelines as well as recent publications 6 , 10 ; of which, subvastus approach for TKA was reported to have increased ROM at 6 months post‐surgery and short‐term recovery favors limited incision over standard incision for THA. 49 , 50 Thus, the surgical approach that could support ERAS still remains controversial.
Perioperative Fluid Management
Maintaining fluid balance should be regarded as an important part of ERAS pathways because either too little or too much fluid in the perioperative period may be associated with an increased risk of complications and prolongation of hospital stay. 51 Surgical stress may result in renal vasoconstriction and salt and water retention. 52 Therefore, balanced crystalloids should be preferred to avoid salt overload. 51 Optimized fluid management in the ERAS pathway, such as a minimized period of preoperative fasting, limited intraoperative blood and fluid loss, and the early intake of postoperative oral fluids, should be judiciously used. Within ERAS, both restricted and balanced fluid management protocols as well as goal‐directed therapy (GDT) have been advocated. 6 In this review, only 29.2% (7/24) of the studies highlighted perioperative fluid management protocols in their ERAS pathways.
After Surgery Phases
Antithrombotic Prophylaxis Treatment
Thromboembolism is a major preventable cause of mortality, morbidity, and delayed discharge, and its methods of prophylaxis include mechanical (such as graduated compression stockings and intermittent calf compression) and pharmacological (such as low‐molecular‐weight heparins) methods. 53 Only 16.7% (4/24) of studies highlighted antithrombotic prophylaxis in their EARS pathways.
Postoperative Nausea and Vomiting
Postoperative nausea and vomiting (PONV) remain common and distressing complications following surgery, which can negatively affect nutritional postoperative recovery, prolong the hospital stay, and increase medical costs. 54 Key PONV risk factors include female sex, increasing duration of surgical procedures, and intraoperative and postoperative opioids. 55 PONV can be reduced or minimized by prophylactically administering antiemetic agents such as ondansetron. 56 In addition, dexamethasone is also safe and efficacious for the prophylaxis of PONV, which can decrease the incidence and severity of PONV and is associated with less frequent administration of antiemetic agents. 57 Only 29.2% (7/24) of studies highlighted PONV prophylaxis in their ERAS protocols.
Postoperative Early Feeding
Return to normal food intake as soon as possible following surgery is recommended. The benefits of early postoperative feeding include decreased postoperative ileus, improved wound healing, reduced wound complications, and a faster recovery. 58 , 59 A randomized controlled trial demonstrated that early postoperative feeding can safely begin approximately 4 hr after elective THA, which showed no difference in nausea, return of bowel function, or LOS compared with late postoperative feeding (⩾8 h postoperatively). 60 Only 16.7% (4/24) of studies highlighted early postoperative feeding in their EARS protocols.
Early Mobilization
Early mobilization may hasten functional recovery after surgery, which has been shown to reduce LOS approximately 1.8 days after TJA. 61 Early mobilization has been widely adopted to facilitate early discharge in the last 5 year. of ERAS protocols. A total of 100% (24/24) of studies encouraged patients to mobilize as early as possible.
Criteria‐Based Discharge and Continuous Improvement and Audit
A total of 33.3% (8/24) of studies defined the requirements of discharge for EARS patients; however, only 8.3% (2/24) of studies supported continuous improvement and auditing as an element of their ERAS protocols. Milligan et al. 19 introduced a postdischarge phone call 1 day after discharge and patient access to a 24/7 dedicated helpline to reduce LOS, while Drosos et al. 23 chose to encourage patients to have regular follow‐ups in the outpatient clinic from where they were discharged to their homes.
Discussion
After the introduction of the ERAS concept, an increasing number of studies have been conducted and have demonstrated the superiority of the ERAS pathway over traditional/standard treatment. ERAS programs have been demonstrated to be safe, efficacious, acceptable, and widely applicable in the perioperative period and share a number of similarities across a range of specialties. Our review is an attempt to appraise the overall results of contemporary ERAS pathways and the current usage of the recommended components by the ERAS® Society in TJA. We showed that ERAS for TJA has favorable clinical outcomes in terms of reducing LOS and overall pain, saving costs, accelerating functional recovery, and reducing complications, although the evidence is still low in quality. In addition, the content of currently used ERAS protocols is varied and significantly heterogeneous. These dramatic variations in clinical programs demonstrate the lack of consensus in practice. However, the ERAS pathway in contemporary studies had some coordinative “active” components.
In this systematic review, we sought to review the direct evidence for each recommended component of ERAS within TJA that has been demonstrated to be clearly effective. However, due to the great variation in ERAS programs, direct evidence for individual components of EARS is still lacking. Nevertheless, we still identified some “active” components of ERAS in TJA. These components include preoperative patient education, anesthetic protocol, use of local anesthetics for infiltration analgesia or nerve blocks, perioperative oral analgesia, perioperative surgical factors including reduced use of tourniquets and drains, use of tranexamic acid, and early mobilization. We believe these “active” components of recommendations are clinically effective key components in TJA, which may be the strongest contributing factors of the recommendations of the ERAS® Society. However, further studies are still needed to verify our hypothesis.
There is no denying that the pros of enhanced recovery after total joint arthroplasty are evident; however, the cons should not be neglected. The results in this review showed that reduced readmission rates, decreased anxiety and depression, and improved patient satisfaction were less reported outcomes in the current ERAS project. This may in turn indicate that the consensus of these outcomes was not widely reached. For example, some patients may feel unready or reluctant to be discharged to their home for safety concerns, although they are physically capable. 62 In addition, some aged patients may have problems in the perception of discharge teaching. 63 These reasons may have a negative influence on readmission, anxiety and depression, or patient satisfaction. Therefore, a whole course of auditing the rehabilitation process after TJA is necessary. Various measures of promoting the quality of discharge teaching or providing postdischarge support, such as postdischarge phone calls and guidance, to achieve successful rehabilitation of TJA should be advocated.
Our study has a number of limitations. First, although a comprehensive literature search was conducted, we may omit some relevant non‐English studies or studies not referenced in the included databases. Second, low‐quality assessment of the included studies indicated a high risk of bias. Third, the heterogeneity of ERAS protocols may heavily influence the validity of this systematic review. Although challenges exist, the implementation of full ERAS protocols does have many benefits. Thus, studies with higher quality data, such as high‐quality RCTs, are needed to determine the effect of fully recommended ERAS protocols or the effect of “active” components of recommendations to provide optimal recommendations for clinical practice.
Conclusion
ERAS for TJA has favorable clinical outcomes in terms of reducing LOS and overall pain, saving costs, accelerating functional recovery, and reducing complications, although the evidence is still low in quality. In the current clinical scenario, only some “active” components of the ERAS program are widely used.
Authors' Contributions
CJ C participated in the drafting, writing, and revising of the manuscript. L JK, Y Y, W YG, R YJ and Z DB participated in the data selection and analysis. PD K participated in the conception and design of the study and contributed to analysis and interpretation of the data and they approved the final version of the manuscript to be submitted, and agreed to be accountable for all aspects of the work.
Conflict of Interest
The authors declare that they have no conflict of interest.
Availability of Data and Material
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Consent for Publication
The authors have seen and approved the manuscript.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (grant numbers 81974333, 82172414); 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (ZYJC18040).
References
- 1. Sloan M, Premkumar A, Sheth NP. Projected volume of primary total joint arthroplasty in the U.S., 2014 to 2030. J Bone Jt Surg Am. 2018;100(17):1455–60. [DOI] [PubMed] [Google Scholar]
- 2. Giraldi G, Montesano M, Sandorfi F, Iachini M, Orsi GB. Excess length of hospital stay due to healthcare acquired infections: methodologies evaluation. Annali di Igiene. 2019;31(5):507–16. [DOI] [PubMed] [Google Scholar]
- 3. Ljungqvist O, Scott M, Fearon KC. Enhanced recovery after surgery: a review. JAMA Surg. 2017;152(3):292–8. [DOI] [PubMed] [Google Scholar]
- 4. Findlay JM, Gillies RS, Millo J, Sgromo B, Marshall REK, Maynard ND. Enhanced recovery for esophagectomy: a systematic review and evidence‐based guidelines. Ann Surg. 2014;259(3):413–31. [DOI] [PubMed] [Google Scholar]
- 5. Zhou X, Zhou X, Cao J, Hu J, Topatana W, Li S, et al. Enhanced recovery care vs. traditional care in laparoscopic hepatectomy: a systematic review and meta‐analysis. Front Surg. 2022;9:850844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wainwright TW, Gill M, McDonald DA, et al. Consensus statement for perioperative care in total hip replacement and total knee replacement surgery: enhanced recovery after surgery (ERAS(®)) society recommendations. Acta Orthop. 2020;91(1):3–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Zhu S, Qian W, Jiang C, Ye C, Chen X. Enhanced recovery after surgery for hip and knee arthroplasty: a systematic review and meta‐analysis. Postgrad Med J. 2017;93(1106):736–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Khan SK, Malviya A, Muller SD, Carluke I, Partington PF, Emmerson KP, et al. Reduced short‐term complications and mortality following enhanced recovery primary hip and knee arthroplasty: results from 6,000 consecutive procedures. Acta Orthop. 2014;85(1):26–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Morrell AT, Layon DR, Scott MJ, Kates SL, Golladay GJ, Patel NK. Enhanced recovery after primary total hip and knee arthroplasty: a systematic review. J Bone Jt Surg Am. 2021;103(20):1938–47. [DOI] [PubMed] [Google Scholar]
- 10. Changjun C, Xin Z, Yue L, Liyile C, Pengde K. Key elements of enhanced recovery after total joint arthroplasty: a reanalysis of the enhanced recovery after surgery guidelines. Orthop Surg. 2023;15(3):671–678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chen C, Alqwbani M, Zhao J, Yang R, Wang S, Pan X. Effects of Teriparatide versus Salmon calcitonin therapy for the treatment of osteoporosis in Asia: a meta‐analysis of randomized controlled trials. Endocr Metab Immune Disord Drug Targets. 2021;21(5):932–42. [DOI] [PubMed] [Google Scholar]
- 12. Changjun C, Xin Z, Mohammed A, Liyile C, Yue L, Pengde K. Survivorship and clinical outcomes of 'cup‐cage' reconstruction in revision of hip arthroplasty for chronic pelvic discontinuity: a systematic review. Surgeon. 2021;19(6):e475–84. [DOI] [PubMed] [Google Scholar]
- 13. Castorina S, Guglielmino C, Castrogiovanni P, et al. Clinical evidence of traditional vs fast track recovery methodologies after total arthroplasty for osteoarthritic knee treatment. A retrospective observational study. Muscles, Ligaments Tendons J. 2017;7(3):504–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jansen JA, Kruidenier J, Spek B, Snoeker BAM. A cost‐effectiveness analysis after implementation of a fast‐track protocol for total knee arthroplasty. Knee. 2020;27(2):451–8. [DOI] [PubMed] [Google Scholar]
- 15. Thiele RH, Sarosiek BM, Modesitt SC, et al. Development and impact of an institutional enhanced recovery program on opioid use, length of stay, and hospital costs within an Academic Medical Center: a cohort analysis of 7774 patients. Anesth Analg. 2021;132(2):442–55. [DOI] [PubMed] [Google Scholar]
- 16. Chung MMT, Ng JKF, Ng FY, Chan PK, Chiu KY. Effects of enhanced recovery after surgery practices on postoperative recovery and length of stay after unilateral primary total hip or knee arthroplasty in a private hospital. Hong Kong Med J. 2021;27(6):437–43. [DOI] [PubMed] [Google Scholar]
- 17. Didden AGM, Punt IM, Feczko PZ, Lenssen AF. Enhanced recovery in usual health care improves functional recovery after total knee arthroplasty. Int J Orthop Trauma Nurs. 2019;34:9–15. [DOI] [PubMed] [Google Scholar]
- 18. de Carvalho Almeida RF, Serra HO, de Oliveira LP. Fast‐track versus conventional surgery in relation to time of hospital discharge following total hip arthroplasty: a single‐center prospective study. J Orthop Surg Res. 2021;16(1):488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Milligan DJ, Hill JC, Agus A, Bryce L, Gallagher N, Beverland D. The impact of an enhanced recovery programme on length of stay and post‐discharge resource usage following hip and knee arthroplasty: a service evaluation and cost analysis. Bone Jt Open. 2021;2(11):966–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Picart B, Lecoeur B, Rochcongar G, Dunet J, Pégoix M, Hulet C. Implementation and results of an enhanced recovery (fast‐track) program in total knee replacement patients at a French university hospital. Orthop Traumatol: Surg Res. 2021;107(3):102851. [DOI] [PubMed] [Google Scholar]
- 21. Plessl DMD, Salomon BBS, Haydel ABS, Leonardi C, Bronstone A, Dasa V. Rapid versus standard recovery protocol is associated with improved recovery of range of motion 12 weeks after total knee arthroplasty. J Am Acad Orthop Surg. 2020;28(21):e962–8. [DOI] [PubMed] [Google Scholar]
- 22. Gleicher Y, Siddiqui N, Mazda Y, Matelski J, Backstein DJ, Wolfstadt JI. Reducing acute hospitalization length of stay after Total knee arthroplasty: a quality improvement study. J Arthroplasty. 2021;36(3):837–44. [DOI] [PubMed] [Google Scholar]
- 23. Drosos GI, Kougioumtzis IE, Tottas S, Ververidis A, Chatzipapas C, Tripsianis G, et al. The results of a stepwise implementation of a fast‐track program in total hip and knee replacement patients. J Orthop. 2020;21:100–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Schultz BJMD, Segovia NBS, Castillo TNMD. Successful implementation of an accelerated recovery and outpatient total joint arthroplasty program at a county hospital. JAAOS Glob Res Rev. 2019;3(9):e110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Gwynne‐Jones DP, Martin G, Crane C. Enhanced recovery after surgery for hip and knee replacements. Orthop Nurs. 2017;36(3):203–10. [DOI] [PubMed] [Google Scholar]
- 26. Yanik JM, Bedard NA, Hanley JM, Otero JE, Callaghan JJ, Marsh JL. Rapid recovery total joint arthroplasty is safe, efficient, and cost‐effective in the veterans administration setting. J Arthroplasty. 2018;33(10):3138–42. [DOI] [PubMed] [Google Scholar]
- 27. Ripolles‐Melchor J, Abad‐Motos A, Diez‐Remesal Y, et al. Association between use of enhanced recovery after surgery protocol and postoperative complications in Total hip and knee arthroplasty in the postoperative outcomes within enhanced recovery after surgery protocol in elective total hip and knee arthroplasty study (POWER2). JAMA Surg. 2020;155(4):e196024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Tan NLT, Hunt JL, Gwini SM. Does implementation of an enhanced recovery after surgery program for hip replacement improve quality of recovery in an Australian private hospital: a quality improvement study. BMC Anesthesiol. 2018;18(1):64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Jiang HH, Jian XF, Shangguan YF, Qing J, Chen LB. Effects of enhanced recovery after surgery in total knee arthroplasty for patients older than 65 years. Orthop Surg. 2019;11(2):229–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Vendittoli PA, Pellei K, Desmeules F, Massé V, Loubert C, Lavigne M, et al. Enhanced recovery short‐stay hip and knee joint replacement program improves patients outcomes while reducing hospital costs. Orthop Traumatol: Surg Res. 2019. November;105(7):1237–43. [DOI] [PubMed] [Google Scholar]
- 31. De Ladoucette A, Mertl P, Henry MP, et al. Fast track protocol for primary total hip arthroplasty in non‐trauma cases reduces the length of hospital stay: prospective French multicenter study. Orthop Traumatol, Surg Res. 2020;106(8):1527–31. [DOI] [PubMed] [Google Scholar]
- 32. Jenny JY, Courtin C, Boisrenoult P, Chouteau J, Henky P, Schwartz C, et al. Fast‐track procedures after primary total knee arthroplasty reduce hospital stay by unselected patients: a prospective national multi‐centre study. Int Orthop. 2021;45(1):133–8. [DOI] [PubMed] [Google Scholar]
- 33. Arienti C, Pollet J, Buraschi R, Piovanelli B, Villafañe JH, Galeri S, et al. Fast‐track rehabilitation after total knee arthroplasty reduces length of hospital stay: a prospective, case‐control clinical trial. Turk J Phys Med Rehabil. 2020;66(4):398–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Zhong M, Liu D, Tang H, Zheng Y, Bai Y, Liang Q, et al. Impacts of the perioperative fast track surgery concept on the physical and psychological rehabilitation of total hip arthroplasty: a prospective cohort study of 348 patients. Medicine. 2021;100(32):e26869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Marchisio AE, Ribeiro TA, Umpierres CSA, et al. Accelerated rehabilitation versus conventional rehabilitation in total hip arthroplasty (ARTHA): a randomized double blinded clinical trial. Rev Col Bras Cir. 2020;47:e20202548. [DOI] [PubMed] [Google Scholar]
- 36. Fransen BL, Hoozemans MJM, Argelo KDS, Keijser LCM, Burger BJ. Fast‐track total knee arthroplasty improved clinical and functional outcome in the first 7 days after surgery: a randomized controlled pilot study with 5‐year follow‐up. Arch Orthop Trauma Surg. 2018;138(9):1305–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Palanne R, Rantasalo M, Vakkuri A, Madanat R, Olkkola KT, Lahtinen K, et al. Effects of anaesthesia method and tourniquet use on recovery following total knee arthroplasty: a randomised controlled study. Br J Anaesth. 2020;125(5):762–72. [DOI] [PubMed] [Google Scholar]
- 38. Berninger MT, Friederichs J, Leidinger W, Augat P, Bühren V, Fulghum C, et al. Effect of local infiltration analgesia, peripheral nerve blocks, general and spinal anesthesia on early functional recovery and pain control in total knee arthroplasty. BMC Musculoskeletal Disord. 2018;19(1):232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Fillingham YA, Ramkumar DB, Jevsevar DS, Yates AJ, Shores P, Mullen K, et al. The efficacy of tranexamic acid in Total knee arthroplasty: a network meta‐analysis. J Arthroplasty. 2018;33(10):3090–3098.e1. [DOI] [PubMed] [Google Scholar]
- 40. Wells PS, Anderson DR, Rodger M, Forgie M, Kearon C, Dreyer J, et al. Evaluation of D‐dimer in the diagnosis of suspected deep‐vein thrombosis. N Engl J Med. 2003;349(13):1227–35. [DOI] [PubMed] [Google Scholar]
- 41. Changjun C, Xin Z, Yue L, Chengcheng Z, Qiuru W, Qianhao L, et al. Tranexamic acid attenuates early post‐operative systemic inflammatory response and nutritional loss and avoids reduction of fibrinogen in total hip arthroplasty within an enhanced recovery after surgery pathway. Int Orthop. 2021;45(11):2811–8. [DOI] [PubMed] [Google Scholar]
- 42. Liao L, Chen Y, Tang Q, Chen YY, Wang WC. Tranexamic acid plus drain‐clamping can reduce blood loss in total knee arthroplasty: a systematic review and meta‐analysis. Int J Surg. 2018;52:334–41. [DOI] [PubMed] [Google Scholar]
- 43. Allen MW, Jacofsky DJ. Normothermia in arthroplasty. J Arthroplasty. 2017;32(7):2307–14. [DOI] [PubMed] [Google Scholar]
- 44. Siddiqi A, Forte SA, Docter S, Bryant D, Sheth NP, Chen AF. Perioperative antibiotic prophylaxis in total joint arthroplasty: a systematic review and meta‐analysis. J Bone Jt Surg Am. 2019;101(9):828–42. [DOI] [PubMed] [Google Scholar]
- 45. Morris AM, Gollish J. Arthroplasty and postoperative antimicrobial prophylaxis. Can Med Assoc J. 2016;188(4):243–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Inabathula A, Dilley JE, Ziemba‐Davis M, Warth LC, Azzam KA, Ireland PH, et al. Extended oral antibiotic prophylaxis in high‐risk patients substantially reduces primary total hip and knee arthroplasty 90‐day infection rate. J Bone Joint Surg Am. 2018;100(24):2103–9. [DOI] [PubMed] [Google Scholar]
- 47. Lai YH, Xu H, Su Q, Wan XF, Yuan MC, Zhou ZK. Effect of tourniquet use on blood loss, pain, functional recovery, and complications in robot‐assisted total knee arthroplasty: a prospective, double‐blinded, randomized controlled trial. J Orthop Surg Res. 2022;17(1):118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Kelly EG, Cashman JP, Imran FH, Conroy R, O'Byrne J. Systematic review and meta‐analysis of closed suction drainage versus non‐drainage in primary hip arthroplasty. Surg Technol Int. 2014;24:295–301. [PubMed] [Google Scholar]
- 49. Bouché PA, Corsia S, Nizard R, Resche‐Rigon M. Comparative efficacy of the different surgical approaches in total knee arthroplasty: a systematic‐review and network meta‐analysis. J Arthroplasty. 2021;36(3):1187–1194.e1. [DOI] [PubMed] [Google Scholar]
- 50. Moskal JT, Capps SG. Is limited incision better than standard total hip arthroplasty? A meta‐analysis. Clin Orthop Relat Res. 2013;471(4):1283–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Varadhan KK, Lobo DN. A meta‐analysis of randomised controlled trials of intravenous fluid therapy in major elective open abdominal surgery: getting the balance right. Proc Nutr Soc. 2010;69(4):488–98. [DOI] [PubMed] [Google Scholar]
- 52. Sladen RN. Effect of anesthesia and surgery on renal function. Crit Care Clin. 1987;3(2):373–93. [PubMed] [Google Scholar]
- 53. Bartlett MA, Mauck KF, Stephenson CR, Ganesh R, Daniels PR. Perioperative venous thromboembolism prophylaxis. Mayo Clin Proc. 2020;95(12):2775–98. [DOI] [PubMed] [Google Scholar]
- 54. Mc Loughlin S, Terrasa SA, Ljungqvist O, Sanchez G, Garcia Fornari G, Alvarez AO. Nausea and vomiting in a colorectal ERAS program: impact on nutritional recovery and the length of hospital stay. Clin Nutr ESPEN. 2019;34:73–80. [DOI] [PubMed] [Google Scholar]
- 55. Gan TJ. Risk factors for postoperative nausea and vomiting. Anesth Analg. 2006;102(6):1884–98. [DOI] [PubMed] [Google Scholar]
- 56. Schlesinger T, Weibel S, Kranke P. Postoperative/postdischarge nausea and vomiting: evidence‐based prevention and treatment. Curr Opin Anaesthesiol. 2022;36:109–16. [DOI] [PubMed] [Google Scholar]
- 57. Corcoran TB, Martin C, O'Loughlin E, Ho KM, Coutts P, Chan MT, et al. Dexamethasone and clinically significant postoperative nausea and vomiting: a prespecified substudy of the randomised perioperative administration of dexamethasone and infection (PADDI) trial. Br J Anaesth. 2022;129(3):327–35. [DOI] [PubMed] [Google Scholar]
- 58. Hellstrom EA, Ziegler AL, Blikslager AT. Postoperative ileus: comparative pathophysiology and future therapies. Front Vet Sci. 2021;8:714800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Abela G. The potential benefits and harms of early feeding post‐surgery: a literature review. Int Wound J. 2017;14(5):870–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Kim JW, Park YG, Kim JH, Jang EC, Ha YC. The optimal time of postoperative feeding after Total hip arthroplasty: a prospective, randomized, controlled trial. Clin Nurs Res. 2020;29(1):31–6. [DOI] [PubMed] [Google Scholar]
- 61. Guerra ML, Singh PJ, Taylor NF. Early mobilization of patients who have had a hip or knee joint replacement reduces length of stay in hospital: a systematic review. Clin Rehabil. 2015;29(9):844–54. [DOI] [PubMed] [Google Scholar]
- 62. Heine J, Koch S, Goldie P. Patients' experiences of readiness for discharge following a total hip replacement. Aust J Physiother. 2004;50(4):227–33. [DOI] [PubMed] [Google Scholar]
- 63. Bobay KL, Jerofke TA, Weiss ME, Yakusheva O. Age‐related differences in perception of quality of discharge teaching and readiness for hospital discharge. Geriatr Nurs. 2010;31(3):178–87. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.


