Abstract
Introduction Population aging is a growing reality worldwide, characterized by a rapidly developing event that is not always associated with quality of life. Elderly health stands out, pointing to the need for public health policies that ensure effective and resolutive approaches for this population, and should be applied especially by primary health care, through actions that encourage active aging. The present review aimed to identify whether sleep disorders impact the quality of life in frail elderly.
Methods We proceeded with the selection of keywords that led to the search of articles. The search was defined in the Lilacs, PubMed, and Embase databases, conducted from July to November, 2020.We have found a total of 455 articles, of which 9 were included in the present review.
Results The studies obtained subjective (self-report and questionnaires) and objective (devices and exams) data that characterized frailty, disorders, and sleep quality in the elderly. Some studies have found a relationship between frailty and sleep disorders in women, others in men, and some have identified the existence of a relationship between these factors and the age of the participants who composed the samples.
Conclusion Based in our results, we conclude that disorders and poor sleep quality interfere in the quality of life of frail elderly.
Keywords: aging, frailty, sleep disorders, quality of life, quality of sleep
Introduction
Population aging is an evident and growing reality around the world that has impacts on the economy, politics, and health. It is characterized by stages, starting with a reduction in birth rates and an increase in life expectancy, with a consequent reduction in mortality rates over the years. In Brazil, this phenomenon is justified by an economic change that ceases to be agricultural and becomes industrial, causing a migration from rural to urban centers, and by the change in the behavior of diseases and health problems. 1 2
Between the 1950s and 1960s, there was a predominance of infectious and parasitic diseases which were difficult to control, given the poor living conditions and underdevelopment, nonexistence of vaccines and precariousness in basic sanitation, causing a lower life expectancy for the population at the time. With the modernization of the country and migration to urban centers, lifestyle also changed, and the disease processes changed from infectious and contagious diseases to chronic noncommunicable diseases and external causes, such as work and car accidents. 2
All these changes generated an alteration in the age pyramid, whose base, which was previously comprehensive, representing young people at working age, now shows an inversion trend, with its top expanded, showing a predominance of elderly people who in general are no longer inserted in the job market, generating an impact on the social, economic, health, and labor spheres. 3
According to the Brazilian Institute of Geography and Statistics (IBGE, in the Portuguese acronym), the life expectancy of the population is 76.6 years. Hence, the process of aging is considered as an event of rapid development, but not always associated to quality of life, causing diverse burdens on the health system. In this sense, elderly health is highlighted, generating demands that point to the need for public health policies that guarantee effective and resolute approaches. 3
Strategies for working with elderly population seek to encourage active aging, defined by the World health Organization (WHO) as the process in which opportunities for health, participation, and safety are optimized, with the aim to improve the quality of life in both individuals and groups as people age. 4 Active aging therefore comprises the encouragement of independence and autonomy as a way of maintaining functional capacity, which is manifested through the performance of activities of daily living (ADLs) relating to self-care behaviors (eating, dressing, bathing) and instrumental activities of daily living (IADL), which are behaviors of autonomy and social participation such as shopping, managing finances, and taking transportation. 5 6
Every effort to maintain the independence and autonomy of the individual in their activities is aimed at promoting quality of life. This is a term with notoriety in the health field and, according to the WHO, concerns the aspects of well-being that permeate all life circumstances (physical, mental, spiritual, psychological, emotional, social), that lead the individual to establish perceptions of the context in which they are inserted, and the expectations and goals they have in relation to their daily life. 7
In order to have quality of life, it is necessary to understand the factors that negatively affect its existence and outline strategies that mitigate them. Of the countless aspects that we must consider in the health of the elderly, frailty and sleep disorders require attention.
Frailty in the elderly is a comprehensive and multidimensional concept. The National Health Policy for the Elderly (2006) considered as frail people > 75 years old, those residing in long-stay institutions, hospitalized, patients with incapacitating diseases, and victims of domestic violence. 8 Science papers present comprehensiveness in relation to the definition and concepts of frailty, with no consensus yet. The best-known concept is the one proposed by Fried et al. 9
Fried et al. 9 proposed that frailty could not be considered only as a synonym for deficiencies, comorbidities, or aging, but identified it as a syndrome that is related to a reduction in organic reserves and resistance to stress mechanisms, generating successive and cumulative declines in the organism, promoting vulnerability. The authors proposed a phenotype to identify frailty, which consists of evaluating the individual, considering: low-fat identified by unintentional weight loss in the last year, proven through direct weight measurement; weakness, recognized by a 20% reduction in grip strength, adjusting the result for gender, and body mass index (BMI); energy reduction, measured by self-report of exhaustion using the Center of Epidemiologic Studies Depression Scale (CES-D); slowness, identified by walking speed, adjusted for gender and height; and low level of physical activity, measured by the kilocalories burned over a week. Thus, individuals who did not present any of these characteristics were considered strong, those with one or two were in the intermediate stage (prefrail) and those with three or more components, in the frail stage.
In addition, aging is a process that triggers physiological and functional changes, affecting mobility and consequently decreasing autonomy. Based on this, elderly's frailty is prevalent in this population, leading to negative consequences and outcomes. It is a consensus that the deterioration of these various systems impacts the risk of falls, affecting health condition, increasing inability, hospitalization, and consequently the risk of mortality. 9 10 11
Hu et al. 12 have explored a new geriatric syndrome associated with decreases in skeletal muscle mass, strength, and function, defined as sarcopenia. However, there are controversies in the prevalence of sarcopenia among studies due to the differences of diagnosis criteria. On the other hand, its prevalence increases significantly with advancing age, which negatively affects elderly's health, generating functional disability, increased risk of falls, contributing to low quality of life and possible increased mortality in this age group. Sarcopenia is more prevalent in the elderlies with short sleep duration compared with those with normal sleep durations. Therefore, a potential association may exist between sleep disorders and sarcopenia.
Sleep is a physiological aspect, and it is closely related to the circadian rhythm, that is, the light-dark cycle, and is a result of the mechanisms that determine its characteristics (need, duration, and deepness, as well as its behavior throughout the day). Because it is biological, sleep is related to neural and hormonal mechanisms, and its alternation with periods of wakefulness promotes the reorganization of cell metabolic activities and acts on memory and learning mechanisms. 13 14
Sleep can have its quality compromised and can be characterized by disorders. The main disorders are insomnia (difficulty to initiate and maintain sleep or waking up before the necessary sleep time), restless legs syndrome (involuntary movement of lower limbs during rest, with relief during activities), obstructive sleep apnea (obstruction of airway in the oropharyngeal region for ∼ 20 seconds during sleep), excessive daytime sleepiness (exaggerated need for sleep during the day, with no improvement in sleepiness) and sleep fragmentation (frequent brief or long awakenings). 14 15
Thus, the present narrative review aims to identify whether sleep disorders can impact the quality of life in frail elderly, and aggravate reflections on the relevance of the development of future research directed to aspects of frailty and sleep quality in the process of aging, awakening in health professionals, especially those in primary care, the importance of early identification and treatment of changes in elderly individuals, to promote health and quality of life.
Material and Methods
The present study is a narrative review that tried to find an answer to the following question: What changes do sleep disorders produce on the quality of life of the frail elderly?
The question was structured on the PECO strategy, with population (P) being the frail elderly, the exposure (E) to sleep disorders, the comparison (C) does not apply to the study and as the primary outcome (O), the quality of life and quality of sleep as a secondary outcome.
For this purpose, a search for articles that addressed the topic was carried out. The search started by defining keywords that would guide the study. We have used Health Science Descriptors (DeCS) and Medical Subject Headings (MeSH) to identify controlled vocabulary. We also used PubReMiner and Yale Mesh Analyzer to survey and identify descriptors mostly used by authors who have addressed the topic of interest. The words were then defined by the authors of the present study ( Table 1 ) and, later, the combinations between them were performed for each database chosen for the study ( Table 2 ). Among all available databases, the search was defined in Lilacs, PubMed, and Embase, and the study was carried out from July to November, 2020.
Table 1. Words defined by the authors to search for articles in databases.
| REPRESENTATION OF PECO QUESTION | WORDS USED IN THE SEARCH |
|---|---|
| P (POPULATION) | Aged OR Aging OR Elderly OR Frailty OR Elderly, Frail OR Sarcopenia OR Postural Balance OR Ageing OR Mobility Limitation |
| E (EXPOSURE) | Sleep Wake Cycle Disorder OR Sleep Wake Disorder OR Sleep Initiation and Maintenance disorders OR Sleep Stages OR Circadian Rhythm OR Circadian Rhythm Sleep Disorder OR Circadian Rhythm Sleep Disorders OR Insomnia OR Sleep Disorders |
| C (COMPARISON) | Does not apply |
| O (OUTCOME) | Quality of Life OR Sleep Quality |
Table 2. Word combinations in each database.
| DATABASE | WORD COMBINATIONS |
|---|---|
| PUBMED | ((((((((((((((((((aged[MeSH Terms]) OR (aging[MeSH Terms])) OR (elderly[MeSH Terms])) AND (frailty[MeSH Terms])) OR (elderly, frail[MeSH Terms])) OR (sarcopenia[MeSH Terms])) OR (mobility limitation[MeSH Terms])) OR (postural balance[MeSH Terms])) OR (aged)) OR (aging)) OR (elderly)) OR (ageing)) AND (frailty)) OR (elderly, frail)) OR (sarcopenia)) OR (mobility limitation)) OR (postural balance)) AND ((((((((((((((((sleep wake cycle disorder[MeSH Terms]) OR (sleep wake disorder[MeSH Terms])) OR (sleep initiation and maintenance disorders[MeSH Terms])) OR (sleep stages[MeSH Terms])) OR (circadian rhythm[MeSH Terms])) OR (circadian rhythm disorder[MeSH Terms])) OR (circadian rhythm sleep disorders[MeSH Terms])) OR (sleep wake cycle disorder)) OR (sleep wake disorder)) OR (sleep initiation and maintenance disorders)) OR (sleep stages)) OR (circadian rhythm)) OR (circadian rhythm disorder)) OR (circadian rhythm sleep disorders)) OR (insomnia)) OR (sleep disorders))) AND ((((quality of life[MeSH Terms]) OR (sleep quality[MeSH Terms])) OR (quality of life)) OR (sleep quality)) |
| EMBASE | (((((((((((((((((('aged'/exp) OR ('aging'/exp)) OR ('elderly'/exp)) AND ('frailty'/exp)) OR ('elderly, frail'/exp)) OR ('sarcopenia'/exp)) OR ('mobility limitation'/exp)) OR ('postural balance'/exp)) OR (aged)) OR (aging)) OR (elderly)) OR (ageing)) AND (frailty)) OR (“elderly, frail”)) OR (sarcopenia)) OR (“mobility limitation”)) OR (“postural balance”)) AND (((((((((((((((('sleep wake cycle disorder'/exp) OR ('sleep wake disorder'/exp)) OR (“sleep initiation” AND 'maintenance disorders'/exp)) OR ('sleep stages'/exp)) OR ('circadian rhythm'/exp)) OR ('circadian rhythm disorder'/exp)) OR ('circadian rhythm sleep disorders'/exp)) OR (“sleep wake cycle disorder”)) OR (“sleep wake disorder”)) OR (“sleep initiation” AND “maintenance disorders”)) OR (“sleep stages”)) OR (“circadian rhythm”)) OR (“circadian rhythm disorder”)) OR (“circadian rhythm sleep disorders”)) OR (insomnia)) OR (“sleep disorders”))) AND (((('quality of life'/exp) OR ('sleep quality'/exp)) OR (“quality of life”)) OR (“sleep quality”)) |
| LILACS | (tw:(envelhecimento)) OR (tw:(idoso)) AND (tw:(distúrbios do sono)) AND (tw:(qualidade de vida)) OR (tw:(qualidade do sono)) |
In the present review, we have used as inclusion criteria studies with elderly (> 60 years old), classified as frail or sarcopenic, and with sleep disorders; studies in which sleep was an outcome; and articles with full texts available and published in English or Portuguese. We defined for exclusion all studies with participants < 60 years old; whose samples were composed of individuals who are hospitalized; and studies published in other languages than English and Portuguese.
Having defined all criteria, we carried out the search in the databases. We found a total of 455 articles, 115 in PubMed, 153 in Embase, and 187 in Lilacs. We used Rayyan as a work reducer, and in it we inserted some inclusion and exclusion words to carry out the first phase of article selection. With this software, we identified 49 duplicate articles which were excluded, then a total of 406 articles was used for analysis. Still with the help of Rayyan, we visualized titles and abstracts of all articles, noting the words which could include or exclude an article from the search. An attentive reading was done through the filters obtained with the software, and after excluding 385 studies that did not address the topic of interest in this review, we settled on a total of 21 articles included in the first phase of selection.
We then proceeded with the search of full texts and download of these 21 articles. One was excluded because it was not possible to find the full text. With the remaining 20 articles, we carried out the second phase of selection, which involved reading all the articles to obtain the 9 articles included in the present narrative review ( Figure 1 ).
Fig. 1.
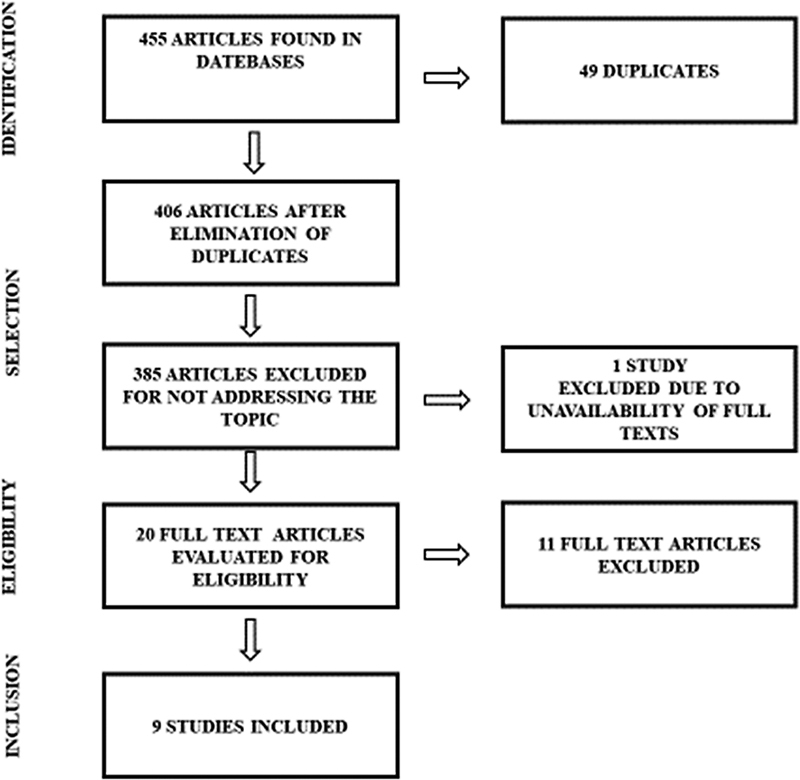
Selection and inclusion of articles in the present narrative review. Source: The authors.
Results
From the 455 articles found in the search, only 9 were included in the present narrative review. The exclusions were made for various reasons, such as articles not addressing the theme of the present study, review studies, and full texts not available for consultation. The main information of the articles included are described in Table 3 .
Table 3. List of selected articles according to authors, aim, assessment made, major findings, and conclusion.
| Author | Year | Aim | Assessment | Major findings | Conclusion |
|---|---|---|---|---|---|
| Pereira et al. 16 | 2013 | To analyze the association between symptoms of insomnia, daytime naps and the occurrence of falls in elderly persons living in the community in Brazil. |
Sample
689 elderly persons between the 65 and 90 years old Sleep Assessment Nottingham Health profile Self-report on medication use Self-report on daytime naps, frequency, and duration Physical Assessment Self-report of ADL and IADL Minnesota Leisure Activity Questionnaire validated for Brazil Self-report of falls in the last 12 months Walking speed for covering a distance of 4.6 m (Average of 3 attempts) Depression Geriatric Depression Scale (GDS) |
The authors found that falls were predominant in females, elderly > 80 years old, individuals who had the habit of taking daytime naps for 90 minutes or more, in use of sleeping medication, who had depression or insomnia symptoms, and who had functional limitations with IADLs. | Sleep disorders and falls are complex and multidetermined phenomena that interact with health and contextual variables. The most effective strategy for reducing the prevalence of falls in elderly individuals in the community is to intervene in alterable risk factors including night sleep and daytime napping. |
| Hu et al. 12 | 2017 | To investigate the possible association between sleep duration and sarcopenia of an elderly population in a Chinese community. |
Sample
607 elderly individuals between the 60 and 90 years old Sleep assessment Self-report of bedtime and time of waking up Self-report on sleep quality perception Sarcopenia Assessment Asia Working Group for Sarcopenia (AWGS) – participants with low muscle mass associated with low grip strength and/ or slow walking speed were considered to have sarcopenia. Cognitive Function Assessment Mini Mental State Examination (MMSE) Depression Assessment Geriatric Depression Scale (Chinese version) |
Participants with short sleep duration were 4 times more likely to have sarcopenia and those with long sleep duration were 3 times more likely. Women with short or long sleep were more likely to have sarcopenia. Participants with sarcopenia were older than those without sarcopenia. Sarcopenic women were more likely to have short or long sleep duration and poor sleep quality. Sarcopenic participants may have worse nutritional status and cognitive function and a higher prevalence of depression. Those who had short or long sleep duration also had worse sleep quality. |
A U-shaped relationship between self-reported sleep duration and sarcopenia was identified in a population of older adults who live in the Chinese community, especially in women, implying the possibility of a potential relationship between sleep disorders and sarcopenia. |
| Sun et al. 17 | 2020 | To investigate the associations of different sleep disorder symptoms (poor sleep quality, various aspects of sleep quality, prolonged and insufficient sleep duration) with frailty in a Chinese community. |
Sample
1,726 elderlies between 70 and 87 years old. Sleep Assessment Pittsburgh Sleep Quality Index (PSQI) Frailty Assessment Self-repot of unintentional weight loss, exhaustion, and low level of physical activity. Gait speed by TUG test (Timed Up and Go), considering the time taken by participants to get up, walk a distance of 3m and sit down again. Grip strength assessed through highest score obtained in 3 attempts (measured bilaterally). Cognitive Function Assessment Hasegawa Dementia Scale-Revised (HDS-R) |
43.6% of older adults had poor sleep quality (PSQI > 5) and 8.2% had short sleep duration, 27.8% had long sleep duration. The prevalence of frailty was 9.2% and that of prefrailty was 52.8%. Participants who had long sleep duration had a significant result for the risk of pre-frailty. Poor sleep quality increased significantly with frailty rate. |
Subjective poor sleep quality, some sleep disorder symptoms measured using the PSQI and prolonged sleep duration were associated with greater chances of frailty and even with prefrailty in an elderly population. |
| Moreno-Tamayo et al. 18 |
2020 | To analyze the influence that gender has on the associations between insomnia, sleep quality, sleep duration and frailty in elderly individuals, using validated instruments. |
Sample
493 elderly individuals (299 women and 194 men) between 64 and 95 years old Sleep Assessment Pittsburgh Sleep Quality Index (PSQI) Athens Insomnia Scale Frailty Assessment Fried Frailty Phenotype: Self-report of unintentional weight loss in the last year; Self-report of burnout assessed by 35 item revised version of the Center for Epidemiologic Studies Depression Scale-Revised (CESD-R), Low grip strength in dominant hand, corrected for gender and Body Mass Index, Slow gait speed (assessed by a distance of 4.5m and adjusted for gender and height) Low level of physical activity - Physical Activity Scale for the Elderly (PASE) |
Among women, the association between insomnia and frailty was highly significant and insomnia was associated with a higher risk of frailty. Frail women were more prone to insomnia, poor sleep quality and short sleep duration; 13.4% of participants were considered as frail elderly, 62.5% as prefrail, and 24.1% as robust. Women had a higher percentage of frailty (16.7%) than men (8.3%). The study showed that among men, the frail group experienced poor sleep quality. |
The results of this study show that insomnia, poor sleep quality, and sleeping for < 5 hours are associated with frailty in women but not in men. |
| Nóbrega et al. 19 | 2013 | To assess the influence of sleep on frailty syndrome in institutionalized elderly persons in Brazil. |
Sample
69 elderly individuals (43 women and 26 men) between 61 and 95 years old Sleep Assessment Pittsburgh Sleep Quality Index (PSQI) Actimetry (assessment of circadian rhythm during rest period) – in only 30 participants Frailty Assessment Self-report of unintentional weight loss in the last year; Self-report of fatigue assessed by questions 7 and 20 of the Center for Epidemiologic Studies Depression Scale (CES-D), Low grip strength in dominant hand, corrected for gender and Body Mass Index, Slow gait speed (assessed by a distance of 4.6m and adjusted for gender and height) Low level of physical activity - International Physical Activity Questionnaire (IPAQ) |
49.3% of participants made up the frail group. For sleep, the general classification showed poor quality with a greater presence in the frail group and the most highlighted component being sleep latency. There is a resting rhythm pattern for each frailty phenotype. Prefrail elderly individuals had an irregular, polyphasic and fragmented rhythm while nonfrail individuals presented a constant rhythm. |
Sleep alterations including poor sleep quality and prolonged latency were related to frailty in institutionalized elderly individuals. A higher prevalence of frailty syndrome was found, a result that was expected since institutionalized older adults usually present high levels of physical, mental and functional impairments, showing a close relation with the clinical manifestation of frailty and sleep-wake disorders. The factor most associated with frailty was the prolonged time between going to bed and falling asleep. This result suggests the possibility of deficient mechanisms that induce sleep and could contribute to frailty. |
| Moreno-Tamayo et al. 10 |
2017 | To assess whether sleep disorders were associated with frailty phenotype in a cohort study with rural elderly aged ≥ 70 years old in Mexico. |
Sample
591 elderly individuals ≥ 70 years old. Sleep assessment Self-report through the question “Have you had any trouble sleeping recently?”. Frailty Assessment Fried Frailty Phenotype: Slow gait speed: assessed by the time taken to walk a distance of 4m. Low grip strength, highest score of 3 bilateral measurements. Low level of physical activity- International Physical Activity Questionnaire (IPAQ) Exhaustion: Geriatric Depression Scale “Do you feel full of energy?” and “Do you have enough energy for your everyday life?” – those with at least one negative answer were considered Self-reported unintentional weight loss of ≥ 5 kg in the 6 months prior to the interview Katz Scale for difficulty in ADL Lawnton Scale for difficulty in IADL Short Physical Performance Battery (SPPB) for assessment of physical performance of lower limbs – walking, balance and the ability to get up from a chair. |
Most of the participants were women (52.8%). 10.7% (63) were frail, 51.9% (307) were prefrail and 37.4% (221) were nonfrail. 20% of the participants had complaints, with complaints being more prevalent among women (21.8%) compared with men (16.8%). Among women, the probability of being frail tripled when there were complaints related to sleep quality. Considering the entire sample (men and women), there were similarities in subjective sleep complaints of frail and prefail groups. Sleep apnea was associated with slow walking and decreased grip strength in women. For difficulty with memory, the frail group was more affected and showed a higher level of dependence in ADL and IADL, also presented a low physical performance and a higher use of medications. |
The plausibility of differential association between men and women is based on the fact that women experience more physiological disorders and greater vulnerability to stress than men. Elderly Mexicans in rural settings are more likely to engage in agricultural activities that demand high metabolic expenditure, which combined with a history of poor diet (proteins and micronutrients) may explain poor physical performance. The relation between sleep disorders and frailty may be bidirectional; individuals with sleep disorders are more likely to have medical problems and vice versa. These findings have implications on clinical interventions, where understanding the causes of sleep complaints can prevent or delay frailty. Future frailty prevention interventions must take sleep disorders into account. |
| Ensrud et al. 20 | 2009 | To test the hypothesis that sleep disorders are independently associated with frail state in older men. |
Sample
3,133 men > 67 years old Sleep Assessment Pittsburgh Sleep Quality Index (PSQI) Epworth Sleepiness Scale (ESS) Actimetry Sleep diary Polysomnography Frailty Assessment Similar to Fried Frailty Phenotype: Unintentional weight loss – self-report Low grip strength - Lack of energy for activities – Geriatric Depression Scale “Do you feel full of energy?” Slowness of 6m walk Low level of physical activity - Physical Activity Scale for the Elderly (PASE) Cognitive function - Mini Mental State Examination (MMSE) modified by Teng. Functional capacity – self-report on difficulty performing IADL, grip strength, walking speed and body mass index (BMI). |
1,007 participants (32%) were robust, 1,689 (54%) were in the o intermediate group, and 437 (14%) were frail. All sleep disorders assessed (poor sleep quality, excessive daytime sleepiness, short sleep duration, low sleep efficiency, prolonged sleep latency, sleep fragmentation, sleep disordered breathing, nocturnal hypoxemia and periodic limb movements were present in the frail elderly classification. After adjusting for covariates, poor sleep quality and excessive daytime sleepiness were the components greatly associated with frailty. Participants with sleep-disordered breathing and nocturnal hypoxemia were 1.3 to 1.4 times more likely to develop frailty stage. |
The results of this study indicate that the prevalence of sleep disorders (poor sleep quality, excessive daytime sleepiness, short sleep duration, low sleep efficiency, prolonged sleep latency, sleep fragmentation, disordered breathing, nocturnal hypoxemia, and frequent periodic limb movements) increased gradually with greater evidence of frailty stage. Greater sleep fragmentation and short sleep duration (actigraphy) and severe sleep-disordered breathing and nocturnal hypoxemia (polysomnography) were associated with poor physical performance scores. Sleep-disordered breathing was associated with lower levels of physical activity. |
| Ensrud et al. 21 | 2012 | Test the hypothesis that older nonfrail men with poorer sleep at the beginning of the study had a higher risk of frailty and death along the study (United States). |
Sample
2,505 men Sleep Assessment Pittsburgh Sleep Quality Index (PSQI) Actimetry Sleep diary Polysomnography Frailty Assessment Fried Frailty Phenotype: Unintentional weight loss Grip strength Exhaustion (assessed using the Geriatric Depression Scale) Walking speed (walking a distance of 6m at usual pace) Low level of physical activity - Physical Activity Scale for the Elderly (PASE). Depression symptoms - 15 item Geriatric Depression Scale Cognitive function - Mini Mental State Examination modified by Teng |
37.6% (
n =
941) were robust and 62.4% (
n =
1564) were prefrail.
In the follow-up assessment, the robust group decreased to 28% ( n = 701) and the prefrail to 14.4% ( n = 360). 49.8% ( n = 468) of all participants who started the study in the robust stage evolved to the prefrail stage and 41% ( n = 386) to the frail stage. Sleep disorders were common, with 8.9% being Severe Obstructive Sleep Apnea (IAH ≥ 30) and 40.7% being self-reported poor sleep quality (PSQI > 5). Self-reported poor sleep quality and excessive daytime sleepiness were associated with greater chances of being classified as prefrail or frail and higher nighttime wakefulness was associated with greater chances of frailty. Nocturnal hypoxemia was related with frailty. Severe Obstructive Sleep Apnea was more related to mortality. |
Sleep disorders may be indicators of conditions including health problems, prefrailty stage and comorbidities which, by themselves, impair sleep and increase the likelihood of frailty or death. Among nonfrail elderly men, poor sleep quality, increased nighttime wakefulness, and increased nocturnal hypoxemia were associated with an increased risk of frailty or death upon the follow-up. Excessive daytime sleepiness, increased nighttime wakefulness, severe sleep apnea and increased nocturnal hypoxemia were associated with an increased risk of mortality. Additional studies are needed to assess the prognostic use of sleep disorders in predicting the risk of frailty and death in older adults. |
| Del Brutto et al. 11 | 2016 | To assess the magnitude of the effect of age on the relationship between frailty and sleep quality in older adults in Ecuador. |
Sample
311 older adults with an average age of 71 years old Sleep Assessment Pittsburgh Sleep Quality Index ( PSQI) – validated Spanish version Frailty Assessment Edmonton Frail Scale (EFS) |
46% of the individuasl were classified as robust, 23% as prefrail, and 31% as frail. Prefrail and frail individuals were older, and had poor sleep quality as well, being mostly women, with lower level of education and more cardiovascular diseases and depression symptoms. Older participants therefore had higher scores on the frailty scale and for sleep quality assessment as well. |
This study shows the strong effect of age on the relationship between poor sleep quality and frailty. |
In a study by Pereira et al., 16 the authors analyzed the relationship between insomnia, daytime napping, and falls in elderly people in Brazil through a multicenter cross-sectional cohort study, with a sample of 689 elderly between 65 and 90 years old. Regarding sleep in the last 12 months, they assessed insomnia through self-report using the Nottingham Health Profile (regarding difficulty to initiate or to maintain sleep, early awakening and nonrestorative sleep), verified the use of medications and identified the habit of daytime napping, questioning the weekly frequency and naps duration.
In the advanced activities of daily living (AADL) component, they obtained self-reports related to recreation, socialization, work, and the participation in elderly groups, trying to understand how many and which activities the elderly continued to perform, and those already discontinued. In the context of IADL, the authors aimed to understand the independence of participants through self-report on shopping, household activities, and medication use, classifying participants as totally independent, with partial or total need for help. To consider physical activity, the Minnesota Leisure Activity Questionnaire validated for Brazil was used, containing questions about weekly frequency and daily duration of physical activity, with elderly individuals who performed 150 minutes of moderate physical activity or 120 minutes of vigorous physical activities being considered active. 16
To assess depression, the geriatric depression scale (GDS) was used, considering the response of the previous week. Elderlies with ≥ 6 points were considered to have depressive symptoms. Fall was assessed through questions identifying its occurrence or not in the last 12 months and frequency. Finally, they assessed gait or walking speed through the average time used for walking 4.6m in 3 attempts. 16
As result of the study, the authors found that 49.9% of the participants complained of one or more insomnia symptoms, with a high prevalence of early awakening. The use of sleeping medication was reported by 19.7% of the elderlies, and a majority of participants reported daytime napping (62.8%). On average, the weekly time of daytime naps in the last year was 166 minutes, with an average of 5.5 days a week, and 19.6% were classified as having depression symptoms (GDS ≥ 6). Most participants (56%) were sedentary, 74.1% were functionally independent in IADLs, and maintained social involvement or AADLs (53.5%). The most elderly (84%) scored below the value of slow walking speed. The occurrence of falls in the last year had a prevalence of 26.2%, with 11.9% of recurrent falls. The authors found that falls prevailed in females, > 80 years old, who had the habit of taking daytime naps for 90 minutes or more, in use of sleeping medications, those who had depressive symptoms or insomnia, and had functional limitations in IADLs. 16
Another cross-sectional study carried out by Hu et al. 12 aimed to identify a relationship between sleep duration and presence of sarcopenia in elderly Chinese. The sample was composed by 607 elderlies, between 60 and 90 years old, and data were obtained through interviews containing self-reports of the participants. Regarding sleep duration, the participants were asked about sleeping and waking time in the previous week and were classified as short-term (< 6 hours), normal (6 to 8 hours) and long-term sleep (> 8 hours). Concerning sleep quality, they were asked about their perception of their own sleep, whether it was good, regular, or poor.
Sarcopenia was evaluated by the recommendation of the Asia Working Group for Sarcopenia (AWGS), considering sarcopenic individuals as those with low muscle mass, associated with low grip strength and/or low gait speed. Skeletal muscle mass was obtained through an equation, considering weight, height, and age, adapted for men and women. Grip strength was obtained by the highest value in three measurements by a dynamometer. According to the AWGS recommendation, low grip strength was referred to as < 26kg for men and < 18kg for women. For gait assessment, a 20m walk was used, with < 0.8m/s considered the low value. 12
Demographic and chronic disease-related variables were also obtained through self-reports. Cognitive function was assessed by the Mini Mental State Examination (MMSE), and depression was assessed using the Chinese version of the GDS. 12
The study found that participants with short sleep had 4 times more chance to have sarcopenia, and those with long sleep were 3 times more likely to have sarcopenia, when compared with individuals with normal sleep. Authors also identified that women with < 6 hours of sleep, and women with > 8 hours of sleep, had greater chance of sarcopenia when compared with women with normal sleep time. 12
Their results indicated that the prevalence of sarcopenia in all participants was 18.5%, and that women (19.9%) seemed to be more susceptible to sarcopenia than men (16.3%), without statistical difference, possibly explained by the difference in the number of participants, men ( n = 251) and women ( n = 356). Participants with sarcopenia were older than those who were not sarcopenic. Sarcopenic women were more likely to have short or long sleep duration, and poor sleep quality, when compared with nonsarcopenic women. The prevalence of sarcopenia was significantly higher in the short-term sleep group (27.5%) and in the long-term sleep group (22.2%), when compared with those with normal sleep duration (13.9%). 12
The study showed that sarcopenic participants may have worse nutritional status and cognitive function, with higher prevalence of depression. For both men and women, those who had short or long sleep duration also had worse sleep quality when compared with participants with normal sleep duration. 12
On the other hand, a study by Sun et al. 17 has used data from a larger study and investigated different association symptoms of sleep disorders (poor sleep quality, various components of sleep quality, prolonged duration and insufficient sleep), with frailty in a sample of 1,726 elderlies between 70 and 87 years old living in Rugao (China).
Regarding sleep information, the authors used the Pittsburgh Sleep Quality Index (PSQI), considering scores > 5 as poor sleep quality. However, for frailty, they considered the self-report according to the criteria of unintentional weight loss, exhaustion, and low activity. Gait speed was assessed using the Timed Up and Go (TUG) test, considering the time spent by participants to get up, walk 3 meters and sit down. Grip strength was recorded using the highest value obtained from 3 attempts, measured bilaterally using a dynamometer. Cognitive function assessment was carried out by the Hasegawa Dementia Scale-Revised (HDS-R), considering participants with a score ≤ 21.5 as showing impairment. For demographic variables and other information on chronic diseases, self-reports of elderly participants were used. 17
As a result, the authors found that the average PSQI score of the elderly population studied (77.6 ± 3.9 years) was 5.4 (standard deviation [SD]: 3.1), and the average nighttime sleep was 7.6 hours (SD: 1.7 hours). Overall, 43.6% of the elderlies had poor sleep quality (PSQI > 5), 8.2% had short sleep duration, and 27.8% had long sleep duration. The prevalence of frailty was 9.2% and of prefrailty was 52.8%.
Poor sleep quality increased significantly with frailty, with 34.5% of elderlies in the healthy group having poor sleep quality, 48% of the prefrail group, and 56.1% of the elderlies were classified as frail. Components such as sleep latency, sleep disorders, and components of daytime dysfunction were significantly associated with greater chances of prefrailty and frailty. However, after adjustments, short sleep duration did not show an influence on the frailty component. Long sleep duration, on the other hand, had a statistically significant result for prefrailty risk in the study participants. 17
The authors also identified that part of their sample (374 elderlies), were residents at long-stay institutions, and that the association between poor sleep quality and frailty also extends to institutionalized settings. The same study identified the need to consider the clinical importance of the prefrailty stage, so that health professionals can interfere in this stage aiming to avoid progression to the frailty stage. 17
A study by Moreno-Tamayo et al. 18 was carried out from the fifth wave of a larger cross-sectional cohort study in Mexico, aiming to identify the association between gender and insomnia, sleep quality, sleep duration, and frailty in the elderly. The sample consisted of 493 elderlies, 299 women and 194 men. Regarding sleep, insomnia was assessed by the Athens Insomnia Scale (AIS) (score ≥ 6 points were used to indicate presence of insomnia), sleep quality was assessed by the Pittsburgh Sleep Quality Index (PSQI) (> 5 was used to define poor sleep quality), and sleep duration was measured by the PSQI component that calculates the average sleep over the last 30 days. The participants were divided into four groups according to the recommendations of the National Sleep Foundation: short sleep duration (subdivided into < 5 hours and 5 to 6 hours), recommended sleep duration (7 to 8 hours), and long sleep duration (> 9 hours).
Moreno-Tamayo et al. 18 assessed frailty using the Fried frailty phenotype criteria, considering self-report of unintentional weight loss in the last year, self-report of burnout assessed by the revised version of item 35 from the Center of Epidemiologic Studies Depression Scale-Revised (CESD-R). Low grip strength was assessed by a dynamometer in the dominant hand, corrected for gender and BMI, low gait speed (assessed by a distance of 4.5m and adjusted for gender and height), and low physical activity identified using the Physical Activity Scale for the Elderly (PASE), which assesses household and leisure activities over 7 days.
The mean age was 70.1 ± 5.6 years old (ranging from 64 to 95 years old), and 89% of them ( n= 439) had ≥ 6 years of education. Among women, the association between insomnia and frailty was highly significant, and the authors identified that insomnia was associated with a higher frailty risk. Among men, there was no statistical significance. For women, poor quality of sleep was associated with frailty in the adjusted and unadjusted models for covariates. For men, the association was only in the unadjusted model. 18
The study also identified that 13.4% ( n = 36) of the participants were considered frail elderlies, 62.5% ( n = 308) were prefrail, and 24.1% ( n = 119) were healthy. Overall, 46.7% ( n = 230) had low grip strength, 44.6% ( n = 220) presented low physical activity, 21.5 ( n = 106) presented exhaustion, 14.2% ( n = 70) presented low walking speed, and 6.9% ( n = 34) presented weight loss. Once gender was compared, women had a higher percentage of frailty (16.7%; n = 50) than men (8.3%; n = 16). It is noteworthy that frail women were more predisposed to insomnia, poor sleep quality, and short sleep duration. Among men, the study showed that the frail group experienced a poorer quality of sleep than prefrail and nonfrail men. In both men and women, the frail group had higher scores for depression and difficulties in activities of daily living, when compared with the prefrail and nonfrail groups. Frail women had greater cognitive decline and abdominal obesity than women who were prefrail or nonfrail. 18
Short sleep duration was associated with frailty in the unadjusted model, and in the adjusted model for elderly women, it was related to frailty. For men, on the other hand, sleep duration did not explain frailty. The study results showed that insomnia, poor quality sleep, and sleeping for < 5 hours were associated with frailty in women but not in men. 18
The study by Nóbrega et al., 19 carried out in Brazil, aimed to assess the influence of sleep on frailty syndrome in institutionalized elderlies. The research consisted of an analytical cross-sectional study, carried out with elderly residents of the long-stay institution in João Pessoa, state of Paraiba, Brazil. The sample was composed by 69 elderlies, (43 women and 26 men) between 61 and 95 years old (77.52 ± 7.82). As in previous studies, frailty was assessed by the Fried phenotype criteria, considering self-report of unintentional weight loss in the last year, exhaustion criteria through self-reported fatigue according to two questions (items 7 and 20) from the Center for Epidemiologic Studies Depression Scale (CES-D). Strength was measured using a dynamometer by grip strength in the dominant hand, adjusted for gender and BMI. Slowness criteria was assessed by gait speed in a 4.6m course and the level of physical activity was measured by the abridged version of the International Physical Activity Questionnaire (IPAQ). For frailty classification, in a total of five phenotype measurement items, elderlies with three or more positive criteria were considered as frail, while those with one or two criteria were classified as prefrail.
Regarding sleep, the Pittsburgh Sleep Quality Index (PSQI) was used to provide an easily interpretable measure of standardized sleep quality. Scores greater than five indicated poor quality sleep, and those below five suggested good quality. Authors also assessed the circadian rhythm during the rest period using Actimetry. The actimeter was ACT10, (Consultoria Eletrônica-CE), firmware version v1.11 Revision C, Brazil; however, due to difficulties related to visual system and device handling, this measurement could only be obtained from 30 participants, using the device for 7 days (day and night), and they were instructed to record their sleep time, wakefulness, nap times, and time and reason for removing the device in a sleep diary. Also, a questionnaire for sociodemographic and health variables was applied in addition to the Mini Mental State Examination (MMSE) for cognitive assessment. 19
As results, Nóbrega et al. 19 found that most elderlies were in the frail group (49.3%), 45% were classified as being in the prefrail stage, and only 5.7% were considered nonfrail. Regarding sleep, the general classification showed poor quality with PQSI score of 8.87 ± 4.53. The most prominent component was sleep latency, with an average of 1.74 ± 1.13, and the least was the component related to the use of sleep medication, with an average of 0.78 ± 1.28. Poor quality sleep was present in all frailty classification groups; however, the frail group had a significantly higher score when compared with the nonfrail and healthy groups, presenting a longer delay initiating the sleep period, greater daytime sleepiness, and lack of enthusiasm for daily activities. Sleep latency was the stage with greatest influence on frailty.
For circadian rhythm assessment, Nóbrega et al. 19 found that among 30 elderly (19 women and 11 men) who used the actimetry device, 16 were frail, 11 were prefrail, and 3 were nonfrail. However, the authors did not find a significant relation between frail state and resting activity rhythm variables. In spite of this, analysis of the actogram showed that there was a pattern of resting rhythm for each frailty phenotype, with pre-frail individuals having an irregular, polyphasic, and fragmented rhythm and nonfrail individuals presenting a constant rhythm.
In another study by Moreno-Tamayo et al., 10 authors aimed to clarify whether sleep disorders were related to frailty phenotype in an elderly cohort living in rural Mexico. The sample was composed by 591 elderlies aged ≥ 70 years old. For frailty measures, the authors used the phenotype proposed by Fried, considering gait speed, grip strength, level of physical activity, exhaustion, and unintentional weight loss in the last year. For sleep quality, however, they used the answers of the participants to the question “Have you had any trouble sleeping recently?”.
For sociodemographic and health variables, they applied a questionnaire. They also used the Katz Scale to identify difficulties in ADL, and the Lawnton Scale for difficulties in IADL, considering that participants who needed help with an activity, or who were not able to perform at least one activity, had difficulty. For cognitive function and memory, the authors asked the following question: “Have you had any difficulty with your memory?”, and the assessment was performed through self-report. Finally, they assessed the physical performance of lower limbs by the Short Physical Performance Battery standard measure for walking, balance, and ability to get up from a chair. Scores ranged from 0 to 12, with lower scores affecting lower limb function levels. 10
In this study, the average age was 76.3 ± 3.3 years old, and most of them were women (52.8%). In frailty classification, they found that 10.7% ( n = 63) were frail, 51.9% ( n = 307) were prefrail, and 37.4% ( n = 221) were nonfrail. Regarding sleep, 20% of participants had complaints, which was more prevalent in women (21.8%) when compared with men (16.8%). Among women, the probability of being frail tripled when there were complaints regarding sleep quality. Considering all participants (men and women), there were similarities in subjective sleep complaints for the frail and prefrail groups. For difficulty with memory, the frail group was more affected, and showed higher dependence level on ADL and IADL, having low physical performance and higher usage of medications. 10
Ensrud et al. 20 have hypothesized that sleep disorders were associated with frailty in elderly men. The authors performed a cross-sectional cohort study with 3,133 men > 67 years old in the United States. For sleep assessment, the authors used self-reports and applied the Pittsburgh Sleep Quality Index (PSQI) as well as the Epworth Sleepiness Scale (ESS) to classify daytime sleepiness. They also performed measurements using an actimeter, a device that assesses the sleep-wake pattern through movement. Participants used the device for 5 nights and 6 days, removing it only at bath time. Associated with its use, they were instructed to record a sleep diary, noting bedtime, waking time, and times when the device was removed. They also applied polysomnography to identify sleep-related breathing disorders, nocturnal hypoxemia, and periodic limb movements associated with nocturnal awakenings.
These same authors obtained information about chronic diseases and medication use through self-reports of the participants. They assessed physical activity using the Physical Activity Scale for the Elderly (PASE). Cognitive function was assessed through the Mini Mental State Examination modified by Teng et al. 7 Functional capacity was assessed by self-report on difficulty in performing IADL, grip strength, walking speed, and BMI. Frailty was measured by the presence of three or more Fried phenotype components, considering unintentional weight loss, low grip strength, lack of energy for activities, slow walking, and low level of physical activity. 20
Ensrud et al. 20 evaluated 3,133 men; 1,007 (32%) were healthy, 1,689 (54%) were in the intermediate group, and 437 (14%) were frail. All sleep disorders assessed (poor sleep quality (PQSI > 5), excessive daytime sleepiness (ESS > 10), short sleep duration (< 5 hours), low sleep efficiency (< 70%), prolonged sleep latency (> 60 minutes), sleep fragmentation (night wakefulness > 90 minutes or 8 episodes of long wakefulness), sleep-disordered breathing (RDI >15), nocturnal hypoxemia (> 10% of sleep time with SaO 2 < 90%) and periodic limb movement (> 5/hour), were common in frail elderlies. After adjustments for covariates were performed, poor sleep quality (PQSI > 5) and excessive daytime sleepiness (ESS < 10), were the components more associated to the frailty stage. Another finding was that sleep-disordered breathing (RDI >15) and nocturnal hypoxemia were associated with an increase in 1.3 to 1.4 times for frail stage development in the elderly.
In another study, Ensrud et al. 21 aimed to assess the predisposition of elderly men with poor sleep quality to develop frailty or die in a study carried out from 2003 to 2005. The study was based on data from a prospective cohort study. A total of 2,505 male elderly, with an average age of 77.5 years old, were included. Sleep was assessed using self-report obtained by the PSQI, and the Epworth Sleepiness Scale (ESS). For objective assessment, the participants used actigraphs for 5 nights and 6 days, recording the sleep pattern they had during the time they were using the device in a sleep diary. To assess sleep disorders, they used a portable polysomnograph and identified apneas, hypopneas, and nocturnal hypoxemia. Frailty was measured by the Fried phenotype to identify unintentional weight loss, grip strength, exhaustion (measured using the Geriatric depression Scale), walking speed (walking 6m at usual pace), and low physical activity by Physical Activity Scale for the Elderly (PASE).
They also conducted interviews to obtain information on health problems and medication use. Depression symptoms were assessed by the Geriatric Depression Scale, and cognitive function was assessed by the Mini Mental State Examination modified by Teng et al. 7 Frailty classification was based in healthy participants, those who did not present any component, and prefrail participants who presented one or two components. Those classified as frail, who presented three or more components, were excluded. 21
As results, the authors identified that out of 2,505 elderlies enrolled, 37.6% ( n = 941) were healthy and 62.4% ( n = 1564) were prefrail. In the follow-up assessment, the healthy group reduced to 28% ( n = 701), the prefrail group reduced to 14.4% ( n = 360), and 7.2% ( n = 180) died during the study. Of all participants classified as healthy in the beginning of the study, 49.8% ( n = 468) evolved to the prefrail stage, and 41% ( n = 386) evolved to the frail stage; 14.9% ( n = 233) of the participants from the beginning of the study in prefrail stage became healthy, 56.1% ( n = 878) remained in this stage, and 19.8% ( n = 310) evolved to the frail stage. At the beginning, sleep disorders were common, with severe obstructive sleep apnea present in 8% (AHI ≥ 30), and poor sleep quality (PSQI > 5) in 40.7%. Self-reported poor sleep quality and excessive daytime sleepiness were associated with greater chances of being classified as prefrail and frail, and increased nighttime wakefulness was associated with greater chances of frailty. 21
Regarding respiratory disorders, the authors found that nocturnal hypoxemia was related to frailty, but they did not find sufficient evidence to relate severe obstructive sleep apnea to prefrailty or frailty stages, not even with the finding of a previous history of chronic obstructive pulmonary disease (COPD). However, it was associated with a higher mortality rate. 21
A study conducted by Del Brutto et al., 11 a cross-sectional population-based study in Ecuador, aimed to assess age influence among frailty and sleep quality. A total of 311 elderly were enrolled in the study, with an average age of 71 years old and a majority (52%) of participants being women. Frailty was assessed by the Edmonton Frail Scale (EFS), which assesses cognition, general health state (hospitalizations and self-reported health state), functional independence (ADL), social support, medication use, weight loss, depression, incontinence and balance, and mobility. To assess sleep quality, the PSQI validated for the Spanish language was applied. For demographic and health data, interviews were conducted together with data collection by self-reports.
The authors found that 46% of the individuals were classified as healthy, 23% as prefrail, and 31% as frail. The prefrail and frail participants were older, and also presented poor sleep quality. Most of them were women, with lower education level, presented more cardiovascular infection, and depression symptoms compared with healthy individuals. Therefore, older participants had higher scores for frailty and sleep quality assessment. 11
Discussion
We know that aging is a process and includes a series of factors that can interfere in the independence and autonomy of individuals. It is necessary to identify these factors and to adopt strategies and approaches aiming to control these factors in order to stimulate and promote active aging. Based on this, the aim of the present study was to recognize how sleep disorders and frailty can negatively interfere in the aging process.
The articles presented in the present review addressed important information regarding the relationship between sleep disorders and frailty, which should be considered for all health professionals, regarding the quality of life of the elderly.
Although the study conducted by Pereira et al. 16 did not directly verify characteristics related to frailty phenotype, the authors showed the importance of considering an event (fall from standing height), which can be a consequence of sleep disorders and frailty and has a negative impact on quality of life. Data from this study showed the prevalence and reoccurrence of falls in individuals who complained of insomnia, need for sleep medications, and frequent daytime naps. In addition, most participants were sedentary and admitted having functional limitations. The authors attributed the fact that sleepiness worsened functional performance, especially addressing the fact that sleep fragmentation seems to be harmful to the relationship between sleep disorders and falling. However, they highlighted the importance of looking at both sleep and falls in a complex and multifactorial way, and not just reducing them to a simplistic association.
The study results may also be related to physical aspects, such as lack of stimuli regarding proprioception, reflexes and balance, and muscle weakness, which are very common factors in the elderly. Regarding sleep aspects, once disorders from self-reports are identified, falls can easily be related to sensorimotor changes caused by medications commonly used, and to a decrease in attention and reflex pattern caused by sleepiness, indicating that quality of sleep is not adequate, and does not produce the necessary rest for reestablishment of biological functions.
It is also very important to consider that falls can be the cause of frailty. Since they are usually associated with fractures, occasionally, correction surgeries can cause immobility syndrome, leading to inactivity and, consequently, causing dependency, weight reduction, and loss of strength, generating frailty.
Hu et al. 12 used the term sarcopenia as a synonym for frailty to assess the relationship with sleep, and then raise some hypotheses for results found in their study, also pointed out by Sun et al., 17 Moreno-Tamayo et al., 10 Ensrud et al., 20 and Ensrud et al. 21
The point made is, regarding how sleep can exert influence on metabolism and body's hormones, as well as how these are compromised by alteration in sleep (short duration or deprivation). Association among sarcopenia and frailty would then be related to reduction in the secretion of growth hormone and testosterone, and an increase in cortisol (responsible for regulating stress, inflammation, helping the immune system), which would contribute to muscle degeneration, causing sarcopenia. Short sleep duration was described as a factor that can cause resistance to insulin, also causing muscle degeneration and consequently sarcopenia. It can also be associated to oxidative stress, generating metabolic alterations and promoting catabolism, which would be a risk for frailty. 10 17 20 21 This possibility supports the argument proposed by Pereira et al., 16 that the frailty syndrome and its relationship with aspects of sleep should be looked at in a complex, systemic, and multidirectional manner.
Regarding the findings by Hu et al., 12 Moreno-Tamayo et al, 18 Moreno-Tamayo et al. 10 and Del Brutto et al., 11 who proved that women are more likely to have sleep disorders associated with frailty, these authors identified some factors that may have generated this result. First is the fact that women were more represented in the population of these studies. 10 12 18 They also point that this may be related to hormonal changes caused by menopause, in addition to the greater predisposition of women to have an increase in inflammatory markers that cause a state of frailty. This data was confirmed by one of the studies whose sample was composed by women who had a high percentage of abdominal obesity, causing a higher level of inflammation and consequent classification into frailty stages. 10 18
Nóbrega et al. 19 were the only authors in the present review to assess the relationship between alterations in sleep and frailty in institutionalized elderly. Although they identified that frail elderly presented an irregular and fragmented rhythm of sleep phases, they understood the result as something to be expected. This is justified by the fact that institutionalization on its own reveals aspects of vulnerability, arising from previous impairments or being caused, given (often) the conditions of physical and mental incapacities, as well as bring related to depression and loneliness aspects.
On the other hand, Moreno-Tamayo et al. 10 introduced another perspective of frailty when they carried out their research with rural elderly. They understood frailty as a possible consequence of the agricultural activity performed by these elderlies, which demands high metabolic spending, and could be associated with low nutrients intake necessary for a good nutritional status. The results associated with poor sleep quality could then be an aggravating factor for this state of frailty, due to metabolic problems, suggested by the other authors included in the review.
Another point to be considered is highlighted in the study by Ensrud et al. 21 and Del Brutto et al., 11 that sleep disorders and frailty may be related to comorbidities previously presented by participants, and may be causative factors for comorbidities, thus presenting a bidirectional aspect. This must be considered, especially because the most commonly accepted definition of health is not dissociated from presence of disease, neither is quality of life; it requires the absence of underlying diseases. On the other hand, it should be considered that aging is permeated by a diversity of health alterations, and there are mechanisms of interactions among these alterations, requiring a comprehensive understanding of the associations they may present. Than approaches for controlling these alterations are as effective as possible.
An interesting aspect highlighted in most of the studies we reviewed is the fact that most individuals who participated in this research were categorized in the prefrail stage, suggesting an intermediate stage for frailty syndrome. This must be considered, due to the possibility of intervening in this stage to prevent elderly from evolving into frail stage, by carrying out a good assessment and outlining assertive and well-defined strategies and actions. Based on this, professionals involved with the elderly population will have another instrument to promote the quality of life of the elderly, and then preventing them from reaching the frailty stage.
Another important aspect raised in the studies is that the higher score related to sleep disorders and poor sleep quality, and the higher frailty stage, suggests that these conditions are in fact related to each other. A similar data was identified by Pereira et al. 16 and Del Brutto et al. 11 , who showed that older participants were more predictable for the frailty stage. This information becomes even more relevant with the constant increase in life expectancy around the world, reinforcing the need to encourage the elderly to live an active aging process.
We identified that understanding the relationship between sleep disorders and frailty is very important to health professionals who work with the elderly, especially to those who work in primary health care (PHC), in order to establish better links with this population, to promote actions that will prevent diseases, promote health and quality of life by strategies that aim to encourage active aging, as proposed by the WHO.
We know that our study has some limitations, such as the limited number of articles included in the present review, the lack of a process to assess the quality and risk of bias of articles selected, as well as the impossibility of establishing criteria recommendation based in our results. However, we understand that the association between sleep disorders and frailty is probably bidirectional, since poor sleep quality gradually increases the frailty status and, consequently, frailty can lead to decreased daily activities, low performance level and physical activities, increasing risk of falls and negatively impacting sleep quality. Furthermore, the decreases in sleep quality in frail elderly are related to a low quality of life. Therefore, promoting potentially effective actions to increase physical activity level improving sleep quality is a strategy that can increase the quality of life and reduce the number of falls and risk of death in the elderly. Therefore, we understand the need and encourage further studies that associate sleep disorders, frailty, and quality of life in the elderly.
Conclusion
Based on our results, it is possible to conclude that sleep disorders and decreased sleep quality interfere negatively in the quality of life of frail elderlies, thus becoming a predisposing risk factor for falls which increases with aging. Hence, different elderly populations can develop frailty associated with sleep disorders, which can be aggravated as age advances with a direct impact on life quality.
Footnotes
Conflict of Interests The authors have no conflict of interests to declare.
References
- 1.Miranda G MD, Mendes A CG, Silva A LA. O envelhecimento populacional brasileiro: desafios e consequências sociais atuais e futuras. Rev Bras de Geriatria e Gerontologia. 2016;19(03):507–519. doi: 10.1590/1809-98232016019.150140.. [DOI] [Google Scholar]
- 2.Júnior J PB. São Paulo: Hucitec; 2013. Trajetória da Fisioterapia no Brasil: um olhar a partir da Saúde Coletiva. Fisioterapia e Saúde Coletiva: reflexões, fundamentos e desafios/organizador José Patrício Bispo Júnior; pp. 17–49. [Google Scholar]
- 3.Júnior W MR, Fernandes M H, Ferreira L N. São Paulo: Hucitec; 2013. Fisioterapia e envelhecimento populacional. Fisioterapia e Saúde Coletiva: reflexões, fundamentos e desafios/organizador José Patrício Bispo Júnior; pp. 198–216. [Google Scholar]
- 4.Gontijo S.Envelhecimento ativo: uma política de saúdeIn: Envelhecimento ativo: uma política de saúde.200560–60.
- 5.Formiga L MF. Envelhecimento ativo: revisão integrativa. Revista Interdisciplinar Ciências e Saúde. 2017;4(02):9–18. [Google Scholar]
- 6.Farías-Antúnez S, Lima N P, Bierhals I O, Gomes A P, Vieira L S, Tomasi E. Incapacidade funcional para atividades básicas e instrumentais da vida diária: um estudo de base populacional com idosos de Pelotas, Rio Grande do Sul, 2014. Epidemiol Serv Saude. 2018;27(02):e2017290. doi: 10.5123/S1679-49742018000200005.. [DOI] [PubMed] [Google Scholar]
- 7.Teng E L, Chui H C. The Modified Mini-Mental State (3MS) examination. J Clin Psychiatry. 1987;48(08):314–318. [PubMed] [Google Scholar]
- 8.BRASIL Portaria n° 2.528, de 19 de outubro de 2006Aprova a Política Nacional de Saúde da Pessoa Idosa. Diário oficial da União, v. 1, 2006.
- 9.Cardiovascular Health Study Collaborative Research Group . Fried L P, Tangen C M, Walston J. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(03):M146–M156. doi: 10.1093/gerona/56.3.m146.. [DOI] [PubMed] [Google Scholar]
- 10.Moreno-Tamayo K, Manrique-Espinoza B, Rosas-Carrasco O, Pérez-Moreno A, Salinas-Rodríguez A. Sleep complaints are associated with frailty in Mexican older adults in a rural setting. Geriatr Gerontol Int. 2017;17(12):2573–2578. doi: 10.1111/ggi.13111.. [DOI] [PubMed] [Google Scholar]
- 11.Del Brutto O H, Mera R M, Sedler M J. The effect of age in the association between frailty and poor sleep quality: a population-based study in community-dwellers (The Atahualpa Project) J Am Med Dir Assoc. 2016;17(03):269–271. doi: 10.1016/j.jamda.2015.12.009.. [DOI] [PubMed] [Google Scholar]
- 12.Hu X, Jiang J, Wang H, Zhang L, Dong B, Yang M. Association between sleep duration and sarcopenia among community-dwelling older adults: A cross-sectional study. Medicine (Baltimore) 2017;96(10):e6268. doi: 10.1097/MD.0000000000006268.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ropke L M. Efeito da atividade física na qualidade do sono e qualidade de vida: revisão sistematizada. Archives of Health Investigation. 2017;6(12) doi: 10.21270/archi.v6i12.2258.. [DOI] [Google Scholar]
- 14.Gomes M M, Quinhones M S, Engelhardt E. Neurofisiologia do sono e aspectos farmacoterapêuticos dos seus transtornos. Rev Bras Neurol. 2010;46(01):5–15. [Google Scholar]
- 15.Guimarães G M.Diagnóstico polissonográfico Pulmão RJ. 201019(3–4):88–92. [Google Scholar]
- 16.Pereira A A, Ceolim M F, Neri A L. Associação entre sintomas de insônia, cochilo diurno e quedas em idosos da comunidade. Cad Saude Publica. 2013;29(03):535–546. doi: 10.1590/S0102-311X2013000300011.. [DOI] [PubMed] [Google Scholar]
- 17.Sun X H, Ma T, Yao S. Associations of sleep quality and sleep duration with frailty and pre-frailty in an elderly population Rugao longevity and ageing study. BMC Geriatr. 2020;20(01):9. doi: 10.1186/s12877-019-1407-5.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Moreno-Tamayo K, Manrique-Espinoza B, Ortiz-Barrios L B, Cárdenas-Bahena Á, Ramírez-García E, Sánchez-García S. Insomnia, low sleep quality, and sleeping little are associated with frailty in Mexican women. Maturitas. 2020;136:7–12. doi: 10.1016/j.maturitas.2020.03.005.. [DOI] [PubMed] [Google Scholar]
- 19.Nóbrega P VN, Maciel A C, de Almeida Holanda C M, Oliveira Guerra R, Araújo J F. Sleep and frailty syndrome in elderly residents of long-stay institutions: a cross-sectional study. Geriatr Gerontol Int. 2014;14(03):605–612. doi: 10.1111/ggi.12144.. [DOI] [PubMed] [Google Scholar]
- 20.Osteoporotic Fractures in Men Study Group . Ensrud K E, Blackwell T L, Redline S. Sleep disturbances and frailty status in older community-dwelling men. J Am Geriatr Soc. 2009;57(11):2085–2093. doi: 10.1111/j.1532-5415.2009.02490.x.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ensrud K E, Blackwell T L, Ancoli-Israel S. Sleep disturbances and risk of frailty and mortality in older men. Sleep Med. 2012;13(10):1217–1225. doi: 10.1016/j.sleep.2012.04.010.. [DOI] [PMC free article] [PubMed] [Google Scholar]


