Introduction
Epipericardial fat necrosis (EFN), first described in 1957,1 is an inflammatory process that affects the epipericardial fat. It is a benign and self-limited cause of acute chest pain.2 Chest computed tomography (CT) is the preferred imaging method to diagnose this condition.2 Its noninvasive treatment with nonsteroidal anti-inflammatory drugs (NSAIDs) leads to the resolution of the symptoms.2 This case report illustrates the clinical presentation of this disease.
Case report
We report the case of a 39-year-old woman, previously healthy, presenting to the emergency department (ED) of a tertiary care hospital with a 2-week history of pleuritic chest pain. Other symptoms, such as fever, cough, or dyspnea, were denied. Physical examination was unremarkable. Routine laboratory testing showed a slight elevation of C-reactive protein (46 mg/L [<3.0 mg/L]), with normal high-sensitivity troponin-I and D-dimer titers. The electrocardiogram was unrevealing (Fig. 1). Chest x-ray showed an opacity overlapping the cardiac shadow (Fig. 2). The chest CT performed in the ED described a nodular mass with heterogeneous density measuring 41 × 25 mm, without contrast enhancement. Because no specific imaging findings were described, the hypothesis of a suspicious pulmonary mass was raised, and the patient was admitted in the ward for further investigation.
Figure 1.
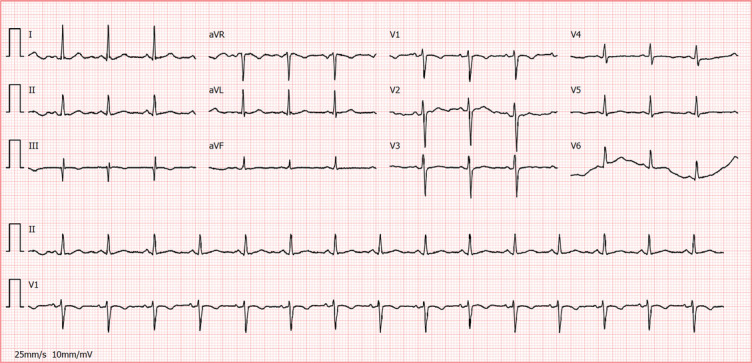
Electrocardiogram at emergency department presentation.
Figure 2.
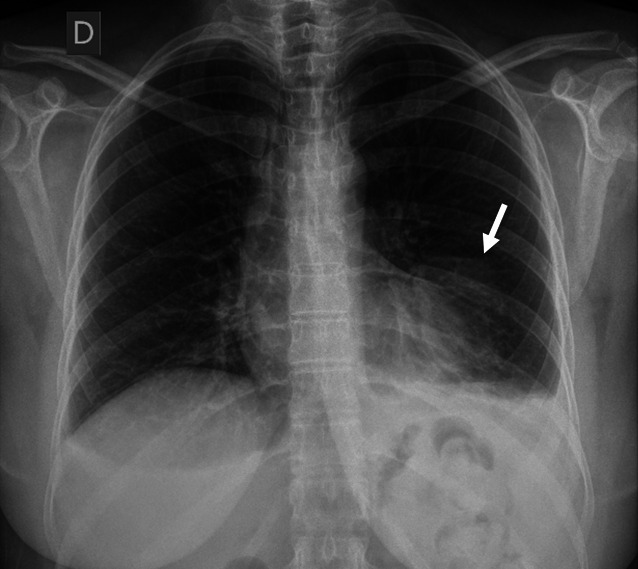
Chest radiograph with an opacity overlapping the cardiac shadow (arrow).
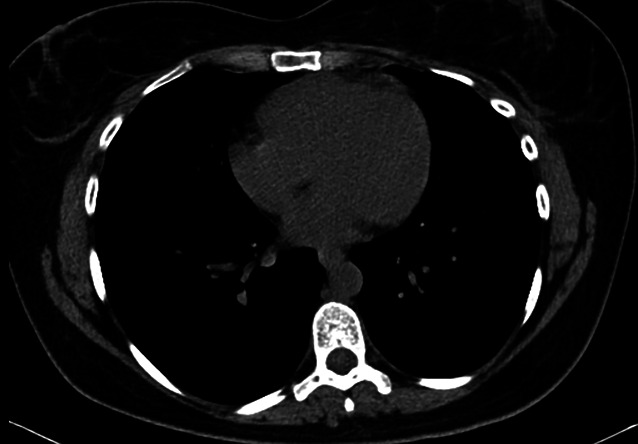
To rule out neoplasia, the patient underwent a chest-abdomen-pelvis CT, which showed an area of fat densification adjacent to the anterior wall of the heart, measuring 42 × 18 mm, consistent with EFN, associated with a slight left pleural effusion (Fig. 3). Anti-inflammatory therapy with NSAIDs (ibuprofen 600 mg three times a day) was started, after which the symptoms improved. No biopsy was necessary because of the favorable evolution.
Figure 3.

Chest computed tomography with an area of fat densification/necrosis adjacent to the anterior wall of the heart (arrow).
The patient was seen in the outpatient clinic two months after discharge, in which she reported being asymptomatic. A chest CT was performed for re-evaluation, and it showed a regression of the area of fat densification/necrosis (Fig. 4).
Figure 4.
Reassessment chest computed tomography with regression of the area of fat densification/necrosis.
Discussion
EFN, affecting mainly previously healthy individuals, presents as acute pleuritic chest pain.3 Its exact prevalence is not well known.3 Giassi et al retrospectively reviewed CT scans of patients referred from the ED with acute chest pain. The authors found that 11 of 426 patients (2.58%) with acute chest pain who underwent chest CT had EFN.4 However, the reporting of EFN is increasing in the past few years because of the widespread use of imaging modalities.5
The pathophysiology of the condition is not well established.4 However, two possible mechanisms may explain the underlying process. One of the proposed mechanisms is that an acute torsion of the fatty tissue attached to the heart by a vascular pedicle causes necrosis.1,4 The alternative mechanism is related to the intrathoracic pressure and shearing forces during the cardiac cycle. No risk factor has yet been identified for EFN.5
The classical clinical presentation is acute pleuritic chest pain, not associated with other symptoms (fever, myalgia).5 Owing to its presentation, EFN is often mistaken with other causes of chest pain, namely pulmonary embolism, myocardial infarction, pericarditis, and musculoskeletal symptoms.5
Laboratory findings including troponin, D-dimer, and creatine kinase titers are commonly within the normal range.6 Electrocardiography and echocardiography usually show no abnormal findings. Increased C-reactive protein has been reported with no other abnormal laboratory findings.3 Diagnostic imaging is essential because of the low specificity of symptoms, clinical findings, and blood tests.7
Chest X-ray findings are usually nonspecific and may include juxta-phrenic opacity and a small pleural effusion.6 Chest CT is the standard for the diagnosis of EFN,2 with typical findings that support the diagnosis.6 The main feature is an ovoid-shaped soft-tissue mass of adipose tissue density and surrounding soft-tissue stranding, measuring approximately 30 × 20 mm.3 Inflammatory changes of the adjacent pericardium may be seen, although deeper cardiac structures or chest wall are usually not involved.3 A small pleural effusion, usually at the left side, is commonly seen.3 Some entities mimic EFN on CT scans, such as primary fatty masses, pericardial mesotheliomas, thymolipomas, and teratomas. However, the presence of stranding, a capsule surrounding the fatty tissue, the lack of solid components, and diaphragmatic integrity are hallmark signs of EFN.8
Owing to the decreased availability of magnetic resonance imaging (MRI), there are few reports of EFN on MRI scans. Contrast-enhanced MRI also helps distinguish benign and malignant fatty tumors in cases where chest CT cannot.7 EFN appears as an oval-shaped fat content mass showing low sign focus on T1-weighted images and high signal on T2-weighted images, with mild enhancement after gadolinium.6 In cases were Ga-97 scintigraphy is performed, a mildly increased gallium uptake has been reported, reflecting an inflammatory process.6
In 2010, Fred et al reviewed 23 cases of EFN.9 Regarding histologic findings, in the early course of the disease, a central focus of necrotic fat cells surrounded by macrophages with intense neutrophilic infiltration is seen. Later in the clinical course fibrosis is seen as well.9
Although, to the best of our knowledge, there are no evidence-based guidelines specifically designed for this condition, conservative treatment, usually with a short course of NSAIDs, leads to symptomatic improvement and resolution of the CT findings.2 A follow-up chest CT, weeks or months after the initial presentation, usually shows a decrease in the size of the lesion and adjacent pericardial thickening in most of the individuals.4 Relapses may be seen; however, the recurrence is rare and the prognosis is prosperous.7
Conclusion
It is important to improve the understanding of EFN, its clinical presentation, and imaging findings. Therefore, more invasive techniques to confirm this diagnosis may be avoided. Owing to the benign course of EFN, conservative symptomatic treatment is usually indicated.
Assistance with the study
This case was presented in 27º Congresso Nacional de Medicina Interna, in October 2021, in Portugal.
Conflicts of interest
None.
Contributor Information
Paula C. F. Matias, Email: paulacfmatiass@gmail.com.
Carlos M. S. P. M. Grijó, Email: carlos.macedo.grijo@gmail.com.
Rita B. Gouveia, Email: ritaborgesgouveia@gmail.com.
Marta F. S. Patacho, Email: marta.patacho@gmail.com.
References
- [1].Jackson RC, Clagett OT, Mcdonald JR. Pericardial fat necrosis; report of three cases. J Thorac Surg. 1957;33:723–729. [PubMed] [Google Scholar]
- [2].Baig A, Campbell B, Russell M, Singh J, Borra S. Epicardial fat necrosis: an uncommon etiology of chest pain. Cardiol J. 2012;19:424–428. [DOI] [PubMed] [Google Scholar]
- [3].Gayer G. Mediastinal (epipericardial) fat necrosis: an overlooked and little known cause of acute chest pain mimicking acute coronary syndrome. Semin Ultrasound CT MRI. 2017;38:629–633. [DOI] [PubMed] [Google Scholar]
- [4].Giassi K de S, Costa AN, Bachion GH, et al. Epipericardial fat necrosis: an underdiagnosed condition. Br J Radiol. 2014;87:20140118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Zafar MR, Mustafa SF, Shahbaz A, Warraich S, Altaf A. Epipericardial fat necrosis: a concise review of literature. Cureus. 2021;13:e13106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Gayer G, Shroff GS, Truong MT. Two unusual fat-containing mediastinal entities: pearls and pitfalls in imaging of Morgagni hernia and fat necrosis. Semin Ultrasound CT MRI. 2022;43(3):267–278. [DOI] [PubMed] [Google Scholar]
- [7].Mortensen SG, Buchmann P, Lappegård KT. Epipericardial fat necrosis: a case report and a review of the literature. Clin Med Insights Case Rep. 2020;13:117954762094076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Hernandez D, Galimany J, Pernas JC, Llauger J. Case 170: pericardial fat necrosis. Radiology. 2011;259:919–922. [DOI] [PubMed] [Google Scholar]
- [9].Fred HL. Pericardial fat necrosis: a review and update. Tex Heart Inst J. 2010;37:82–84. [PMC free article] [PubMed] [Google Scholar]


