Abstract
Introduction
Prostate cancer is the most common cancer in men. It was initially a disease of older men above the age of 55 years. Of recent, there has been reports of increase in the number of young men <55 years with prostate cancer (PCa). The disease in this age group has been reported to be more lethal because of aggressive characteristics and metastatic potential. Different populations have different proportions of young-onset PCa. The aim of this study was to determine the proportion of young men aged <55 years with PCa in Nigeria.
Methods
Data on the prevalence of young men <55 years with PCa was extracted from the 2022 report of the prevalence of cancer in Nigeria from 2009 to 2016 based on the records of 15 major Cancer Registries in Nigeria. This was a publication of the Nigerian Ministry of Health and represents the most up to date data.
Results
In 4864 men diagnosed with malignancies before age 55, PCa was the second common, following liver cancer. Out of a total of 4091 cases of PCa in all age groups, 355 were diagnosed in men <55 years representing 8.86%. Furthermore, the proportion of young men with the disease in the Northern part of the country was 11.72%, whereas in the South, it was 7.77%.
Conclusions
PCa is the second most common cancer in young Nigerian men aged< 55 years preceded by liver cancer. The proportion of young men with PCa was 8.86%. It is therefore important to consider PCa in young men as a different entity and develop appropriate ways to control this disease to ensure survival and good quality of life.
Keywords: prostate, cancer, proportion, young men, Nigeria
Introduction
Prostate cancer (PCa) is the most common cancer among men older than 55 years of age. Globally, more than 1.4 4 million cases were diagnosed in 2020 with age-standardised incidence rate (ASIR) of 30.7 per 100,000 males. Although continents of the developed economies with ASIR of 59 per 100,000 have age-standardised mortality rate (ASMR) of 8.3 per 100,000, countries of Africa with low ASIR of 30 per 100,000 have high ASMR of 16.3 per 100,000. 1 Close to 60% of PCa are diagnosed in men 65 years or older. Although it can be seen from the age of 50 years and above, the rate of occurrences rapidly increases from the age of 55 years. 2 Previous autopsy reports revealed latent PCa in 3% of African-American men aged 20 to 29 years, 26% of men aged 30 to 39 years and in 50% of men aged 30 to 44 years. 3 The incidence of PCa has been increasing in patients less than 55 years of recent. In the USA, PCa in young men increased by 5.7-fold (95% CI 5.0, 6.7) between 1986 and 2008 from 5.6 to 32 cases per 100,000 person years. 4 This was however attributed to the wide use of PSA screening. Although ethnicity and other factors such as genetics (BRCA2 and HOXB13 mutations) often significantly increase the chances in younger men, the reason for overall extent of occurrence is not clear. 2 It has been postulated that BRCA2 carriers had about 23-fold increased risk of early PCa; nevertheless, BRCA2 mutation was described in only 2% of PCa cases diagnosed at the age of ≤55 years in a study report. 2 This implies that other factors including yet-to-be-identified genetic, epidemiologic and environmental factors can also be contributory factors. Young-age PCa has been defined as any PCa, regardless of tumour extent or clinical manifestations in men aged <55 years. 2
Although the selection of the age of 55 years as the upper age limit to study PCa in young men is arbitrary, it was initially proposed by Hussein and colleagues (2015). 2 This was based on an extensive review of the literature on the epidemiology of PCa in the United States of America and the United Kingdom as well as other data cited from other publications. More so, the American urological association recommended routine PSA testing for men aged 55 years and above. 2 Therefore, PCa diagnosed in unscreened men less than 55 years is likely to be symptomatic and may result in poor outcome. It is important to highlight the problem of PCa outside the recommended age for screening to draw attention to this group of patients. This report considered PCa among young adults because PCa is observed to be a disease of older men. This is to draw attention to PCa at this age range which may require different approach to prevention, diagnosis and management.
In 2014, the U.S. recorded that over 10% of new diagnoses of PCa occurred in men ≤55 years. This differs from older men because those with early-onset PCa are more likely to die of their cancer and have higher cause-specific mortality than all others except those diagnosed at age 80 years and above. Higher prevalence of high Gleason scores of PCas has been identified through autopsy in men under 55 years compared with older men although there was inadequate documentation on the mortality rate of PCa at this young age. 2 This indicates that important biological differences may exist in early-onset disease. 5
Recent studies have reported that globally, there have been an increase in PCa in all age groups between 15 and 40 years and that the increase was at a steady rate averaging 2% per year since 1990. Furthermore, distant disease at diagnosis was more than six times more likely in this age group than older men in the U.S. 4 The variation in the incidence rates worldwide reflects differences in the use of diagnostic testing especially between high-income and low-income countries. 6 Men of African Ancestry in the United States and the Caribbean have the highest incidence rates globally, supporting the role of Western African ancestry in modulating PCa. 7
Overview of Prostate Cancer in Nigeria
Nigeria is in the West African subregion. Currently, the western region of Africa has the fourth highest risk for PCa mortality in the world. 8 The estimated population of Nigeria in 2020 by the World Bank is 206,139,587 million people occupying a total surface area of approximately 923,768 square kilometres. 9 Close to 31% of the population in 2012 were youths aged 15–35 years. 10 In Nigeria, high mortality from PCa persists with approximately 80% of Nigerian patients being incurable at diagnosis 11 . Contributory factors to this include inadequate population awareness, poor health-seeking behaviour, low levels of literacy and empowerment in addition to a poor health system leading to low uptake of screening services, and poor access to treatment.
Access to health services which includes patient navigation and individualised assistance, genetic testing, and screening that are available in high-income countries creates an environment to help access optimal care. Awareness of risk factors, need for early detection and better adherence to medical recommendations enable them overcome system barriers to quality cancer. 12 Nonetheless, the situation is different in low-income countries such as Nigeria. 8 The first step of screening for the diagnosis of Nigerian men with PCa is not common and genetic testing is not currently available. 13 The situation is worse in young men whose diagnosis may be missed because of low suspicion of the disease at presentation.
Different countries have described different figures ranging between 3 and 50% of young adults with PCa. 4 There is need to evaluate the problem in Nigeria possibly starting with prevalence, to document the extent of the disease in our population towards understanding the epidemiology and biology that will guide population-based management approach. Data on the proportion of young patients with PCa are scarce in Nigeria.
The objective of this study was to determine the proportion of young adults less than 55 years with PCa in Nigeria by examining current Nigerian data on PCa to document the prevalence of PCa among young men (<55 years). A literature review on the peculiar problems faced by PCa patients in this age group which is distinct from disease in older ones (55 years and above) was also done.
Methods
We performed secondary analysis using data from the February 2021 version of the Nigerian National System of Cancer Registries data on Cancer in Nigeria. 14 This is currently the most comprehensive data on cancer incidence in Nigeria and was curated using available data from population and hospital-based cancer registries in Nigeria. The publication was from the Nigerian Federal Ministry of Health. The publication contains information on cancer cases diagnosed from 2009 to 2016 based on reports from available cancer registries in Nigeria. Cancer incidence data were extracted from fourteen hospital-based cancer registries in Nigeria. We also reported data from the Ibadan Cancer Registry Report for 2009 to 2012 published in 2016. 15 The data were analysed using proportions and percentages. Entries with missing data on age were excluded from further analysis. This research was not on human tissue/samples, so an Ethics/Review board approval was not required as we only reviewed existing data from cancer registries.
Results
Data from a total of 15 cancer registries in Nigeria covering from 2009 to 2016 who had sufficient entries of interest were extracted and analysed. Eight out of the selected 15 registries were population-based while 7 were hospital-based. The proportion of cancers in young men aged <55 years in descending order is presented in Table 1.
Table 1.
Proportion of Cancer Sites in Males Below 55 Years From 2009–2016 in Descending Order (N = 4864).
| S/No | Site | Total | Proportion, % |
|---|---|---|---|
| 1 | Liver | 519 | 10.67 |
| 2 | Prostate | 355 | 7.30 |
| 3 | Connective and soft tissue | 337 | 6.93 |
| 4 | Other skin | 337 | 6.93 |
| 5 | Non-Hodgkin lymphoma | 318 | 6.54 |
| 6 | Colon | 256 | 5.26 |
| 7 | Bone | 214 | 4.40 |
| 8 | Nasopharynx | 208 | 4.28 |
| 9 | Rectum | 193 | 3.97 |
| 10 | Eye | 180 | 3.70 |
| 11 | Hodgkin disease | 158 | 3.25 |
| 12 | Kaposi sarcoma | 151 | 3.10 |
| 13 | Kidney | 137 | 2.82 |
| 14 | Myeloid leukaemia | 137 | 2.82 |
| 15 | Stomach | 122 | 2.51 |
| 16 | Breast | 116 | 2.38 |
| 17 | Bladder | 115 | 2.36 |
| 18 | Nose, sinuses, etc. | 98 | 2.01 |
| 19 | Anus | 97 | 1.99 |
| 20 | Brain, nervous system | 68 | 1.40 |
| 21 | Lymphoid leukaemia | 61 | 1.25 |
| 22 | Mouth | 58 | 1.19 |
| 23 | Salivary glands | 58 | 1.19 |
| 24 | Trachea, bronchus and lung | 57 | 1.17 |
| 25 | Testis | 55 | 1.13 |
| 26 | Pancreas | 50 | 1.03 |
| 27 | Larynx | 37 | .76 |
| 28 | Myeloproliferative disorders | 34 | .70 |
| 29 | Leukaemia unspecified | 33 | .68 |
| 30 | Thyroid | 30 | .62 |
| 31 | Oesophagus | 30 | .62 |
| 32 | Melanoma of skin | 29 | .60 |
| 33 | Hypopharynx | 29 | .60 |
| 34 | Multiple myeloma | 22 | .45 |
| 35 | Other endocrine | 16 | .33 |
| 36 | Tonsil | 20 | .41 |
| 37 | Other oropharynx | 19 | .39 |
| 38 | Tongue | 18 | .37 |
| 39 | Pharynx unspecified | 15 | .31 |
| 40 | Lip | 13 | .27 |
| 41 | Small intestine | 12 | .25 |
| 42 | Other thoracic organs | 11 | .23 |
| 43 | Adrenal gland | 9 | .19 |
| 44 | Gallbladder etc. | 9 | .19 |
| 45 | Other male genital organs | 8 | .16 |
| 46 | Other urinary organs | 5 | .10 |
| 47 | Mesothelioma | 3 | .06 |
| 48 | Penis | 3 | .06 |
| 49 | Renal pelvis | 3 | .06 |
| 50 | Immunoproliferative diseases | 1 | .02 |
| Total | 4864 | 100 |
The total number of cancer cases recorded was 4864 among males below 55 years from 2009–2016. Overall, cancer of the liver was the most common in the age group followed by cancer of the prostate. However, all registries had PCa as the most common cancer among men across all ages except for registry in Sokoto (Northern part of Nigeria) where cancer of the bladder was the most common.
Across the cancer registries in Nigeria, there were 4104 cases of PCa recorded between 2009 and 2016. A total of 13 entries were of unknown age and were excluded from further analysis leaving 4091. There was varying number of PCa values up to the age of 39 years with 9 cases being the highest number of PCa between ages 30 and 34. However, the incidence of PCa increased more than 5 times between ages 35 and 39 and from 6 cases to 35 cases between the age of 40 and 44 years. This figure also doubled between ages 45 and 49 years to 77 cases and approximately tripled between 50 and 54 years to 214 cases (Table 2).
Table 2.
Prostate Cancer Across the Various Age Groups in 15 Cancer Registries in Nigeria.
| Name of registry | All ages (Years) | Age UNK | 0- | 5- | 10- | 15- | 20- | 25- | 30- | 35- | 40- | 45- | 50- | 55- | 60- | 65- | 70- | 75- | 80- | 85- | % of Total |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Abuja 2009–2016 (FCT) | 686 | 11 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 3 | 6 | 14 | 67 | 106 | 126 | 136 | 105 | 56 | 28 | 27 | 16.77 |
| NAUTH 2009–2016 | 743 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 9 | 9 | 21 | 42 | 86 | 134 | 152 | 138 | 103 | 47 | 18.16 |
| Yenagoa 2009–2016 | 56 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 5 | 1 | 8 | 8 | 16 | 11 | 5 | 1 | 1.37 |
| Maiduguri 2016 | 39 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 0 | 0 | 4 | 11 | 4 | 8 | 4 | 3 | 3 | .95 | ||
| Calabar 2009–2016 | 188 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 2 | 9 | 12 | 15 | 47 | 35 | 27 | 20 | 10 | 10 | 4.60 | |
| Benin 2014–2016 | 304 | 0 | 0 | 0 | 0 | 0 | 3 | 2 | 1 | 5 | 11 | 11 | 19 | 44 | 62 | 65 | 38 | 27 | 16 | 7.43 | |
| Ekiti 2014–2016 | 248 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 1 | 2 | 2 | 9 | 23 | 34 | 34 | 51 | 38 | 29 | 22 | 6.06 |
| Enugu 2012–2016 | 352 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 4 | 15 | 33 | 45 | 68 | 71 | 56 | 42 | 14 | 8.60 | |
| Gombe 2009–2016 | 149 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 3 | 4 | 14 | 19 | 33 | 29 | 25 | 17 | 4 | 3.64 | |
| LASUTH 2009–2016 | 192 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 4 | 4 | 11 | 32 | 43 | 47 | 28 | 15 | 6 | 4.69 |
| LUTH 2009–2016 | 260 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 2 | 7 | 24 | 55 | 64 | 53 | 33 | 17 | 3 | 6.36 | |
| Keffi 2009–2016 | 50 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 3 | 2 | 9 | 7 | 11 | 9 | 4 | 1 | 1.22 |
| UPTH 2009–2016 | 490 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 1 | 6 | 10 | 36 | 53 | 77 | 94 | 105 | 56 | 40 | 9 | 11.98 |
| UDUTH 2014–2015 | 15 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 4 | 2 | 2 | 3 | 0 | 1 | .37 | |
| Ibadan 2009–2012 | 319 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 5 | 19 | 26 | 46 | 53 | 69 | 51 | 29 | 19 | 7.80 |
| TOTAL | 4091 | 13 | 0 | 0 | 0 | 0 | 0 | 14 | 9 | 6 | 35 | 77 | 214 | 374 | 643 | 777 | 811 | 566 | 369 | 183 | 100 |
Abbreviations: LASUTH, Lagos State University Teaching Hospital, Lagos State; LUTH, Lagos University Teaching Hospital, Lagos State; NAUTH, Nnamdi Azikiwe University Teaching Hospital, Anambra State; UPTH, University of Port-Harcourt Teaching Hospital, Rivers State; UDUTH, Usman Dan Fodio University Teaching Hospital, Sokoto State; UNK, unknown.
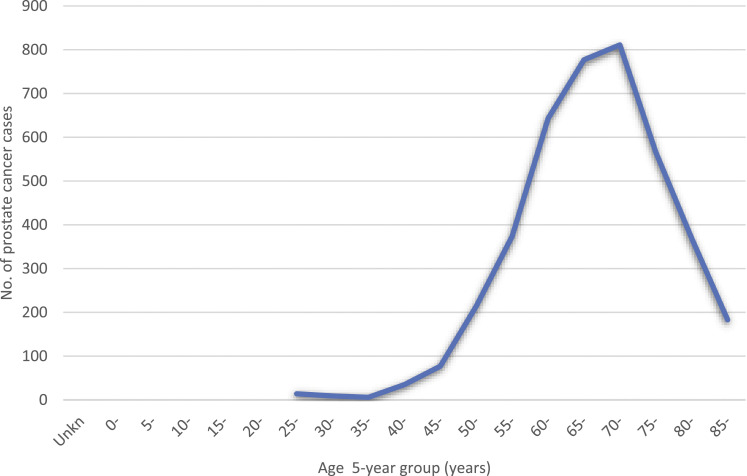
PCa cases show a rise from 35 years reaching a peak at the seventh decade. Although the cases of PCa from 55 years upward continued to increase more rapidly, it reached a peak of 811 cases between ages 70 and 74 (range 25 to >85 years) (Figure 1).
Figure 1.
Age distribution of PCa cases in Nigeria.
A total of 355 (8.7%) patients were below the age of 55 years (Table 3).
Table 3.
Proportion of Prostate Cancer Cases Among Males Below 55 Years in 15 Cancer Centres in Nigeria From 2009–2016.
| Total | Prostate Cancer in Men Below 55 | Proportion, % | |
|---|---|---|---|
| Northern states | |||
| Abuja 2009–2016 (FCT) | 686 | 91 | 13.27 |
| Maiduguri 2016 | 39 | 2 | 5.13 |
| Gombe 2009–2016 | 149 | 8 | 5.37 |
| Keffi 2009–2016 | 50 | 7 | 14.00 |
| UDUTH 2014–2015 | 15 | 2 | 13.33 |
| Sub-total | 939 | 110 | 11.72 |
| Southern states | |||
| NAUTH 2009–2016 | 743 | 41 | 5.52 |
| Yenagoa 2009–2016 | 56 | 6 | 10.71 |
| Calabar 2009–2016 | 188 | 24 | 12.77 |
| Benin 2014–2016 | 304 | 33 | 10.86 |
| Ekiti 2014–2016 | 248 | 17 | 6.85 |
| Enugu 2012–2016 | 352 | 22 | 6.25 |
| LASUTH 2009–2016 | 192 | 10 | 5.21 |
| LUTH 2009–2016 | 260 | 11 | 4.23 |
| UPTH 2009–2016 | 490 | 56 | 11.43 |
| Ibadan 2009–2012 | 319 | 25 | 7.84 |
| Sub total | 3152 | 245 | 7.77 |
| Grand total | 4091 | 355 | 8.68 |
In Table 3, registries are also grouped under those located in the Southern part of Nigeria and those in the North.
There are more cancer registries in the southern parts of Nigeria than in the North (10 vs 5) and this translated to more data with 3152 cases recorded in the South compared with 939 in the North. Although there were fewer PCa cases among men below 55 years in the North − 110 cases against 245 cases in the South (Table 3), however, the proportion of young men with PCa was higher in the North.
Discussion
PCa is becoming a common diagnosis in young adult men aged <55 years globally. In Nigeria, this report shows that PCa is the second most common cancer in this age group following liver cancer (Table 1). Although PCa is commonly seen as a disease of older men, a sizable proportion occurred in young men. Diagnosis was made at ages as low as 25 years and the incidence were increasing from age 35 years till age <55 years. However, a sharp rise occurred from age 55 years upwards (Figure 1; Table 2). This pattern follows the global trend of PCa as rapidly increasing in incidence from age 55 upwards. 2 The proportion of young people <55 years with PCa from this report is 8.7%. (Table 3). This falls within reported range between 2 and 30% although not all studies used same cut-off ages. Other studies also contained autopsy findings which included latent diseases with no clinical manifestations. Such will raise the percentages of the disease in this age group in various countries. The peak age of diagnosis on all men in this report was 70 years age group (Range 25 to >85 years). This is similar to a previous report by Oluwole and colleagues (2015) who reported a peak age as seventh decade (Range 30–79 years) from a ten-year review of an institutional data from Northern Nigeria. 16
The proportion of cancer of the prostate among young age group was slightly higher in the Northern part of the country than the south (8.68% vs 11.72%). Aside from the difference in the total number of cases among the two regions, which might be responsible, it may indicate possible influence of other factors that are yet to be identified. These include genetics, environmental and other epidemiological factors which might be different between the two regions. Varying genetic mutations, environmental as well as lifestyle factors have been postulated to be responsible for the onset of PCa in young adults though the precise connections are yet to be elucidated. 6
Most hospital registries in Nigeria do not include genetic variations through genetic testing, but based on genetic variations arising from ethnicity coupled with epidemiologic factors, it may be necessary to have a thorough genetic evaluation of men below 55 years. 2 PCa below year 55 in Nigeria is compounded by poor screening including genetic screening especially as genetic mutations have already been established to exist in men of African descent in the US where more advanced disease and more frequent biochemical recurrence among young African-American compared with Caucasian men have been reported.7,17 The low rate of screening in Nigeria is due to low health infrastructure which is also common in countries of sub-Sahara Africa.
In a 2014 US Surveillance Epidemiology and End Result Analysis, higher Gleason score and mortality (2.8–3.2 times) and metastatic disease were demonstrated among African-American men compared with American men of European descent within the age of 40–49 years. 18 Owing to this higher incidence of aggressive and rapidly growing early-onset PCa in American-African men, Hussein and colleagues (2015) speculated that this may be due to increased expression of genes associated with lethal PCa like fatty acid synthase gene and higher expression of inflammatory cytokines, such as interleukin 6 (IL6), IL8 and IL 1B. 2
The two genetic mutations BRCA 1 and 2 increase the risk of not just breast carcinomas but PCa as well. Carriers of BRCA1 may have an increased risk of PCa although studies are still underway to report this. All studies consistently reported that BRCA2 carriers have increased risk of more aggressive PCa at younger age.19,20 The strongest predictors for the presence of a germline mutation of BRCA2 genes in patients with PCa are a young age at onset and a family history of breast and/or ovarian cancer and PCa occurrence.21,22 The diversity in early-onset PCa and young age is yet to be clearly studied especially among indigenous Africans to understand fully the factors fuelling PCa among this group.
The implications of PCa at a young age are manifold. This is a very active age group; hence, diagnosis of PCa has both economic and social implications that should be understood and considered in their care. The longer life expectancy of this group of patients compared with their elderly counterpart means that they are likely to suffer for longer periods from late side effects of treatment and possible disease progression which may lead to death. 5 In addition, this group of patients are physiologically stronger and less likely to have co-morbidities and hence can withstand more aggressive therapy than their elderly counterparts. This should be considered in planning their therapy especially as they are likely to have more aggressive disease.
To address these issues, more work needs to be done towards having a detailed analysis of the epidemiologic and other risk factors that can assist in understanding the link between genetic mutations and environmental risk factors in causing these mutations that lead to tumour initiation and progression. It is important that the differences in pathological types between young and elderly PCa patients are assessed. These will enable the identification of at-risk persons towards the development of effective screening and preventive methods. 6 Towards this end, adjustment in screening schedules might be necessary to enable early diagnosis and treatment.
Limitations
The study was based on existing data that are often incomplete. The records used (hospital-based registries and population-based registries) do not reflect the incidence of PCa in the populations represented. There are more registries (10) in the southern parts of the country than in the north (5). Some data may therefore not have been captured in the registries. Some entries were discarded due to missing information on age. There was no consistency on the cut-off age for young men with PCa in the reports consulted. In spite of these limitations, this report gives information on the extent of the problem of PCa among young men in Nigeria. Further prospective studies are needed to capture further epidemiological, biological and clinical information on this group of PCa patients.
Conclusion
There were rising cases of PCa among young persons in Nigeria. The proportion of PCa among young persons in Nigeria aged less than 55 years was 8.7%. The peak age of PCa in Nigeria was in the seventh decade. The proportion of young men with PCa was higher in the Northern part of Nigeria than in the South. PCa among young people has been found to have different characteristics; hence, a different approach towards prevention, diagnosis and treatment is highly needed. The research and health care system would need to dedicate more interest into this domain to ensure early diagnosis, commencement and adherence to therapy.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval: This article uses secondary data that has already been published. It does not contain any data with human or animal participants. Ethics approval is not required.
ORCID iD
Atara Ntekim https://orcid.org/0000-0003-4830-8365
References
- 1.Wang L, Lu B, He M, Wang Y, Wang Z, Du L. Prostate cancer incidence and mortality: Global status and temporal trends in 89 countries from 2000 to 2019. Front Public Health. 2022;10:811044. doi: 10.3389/fpubh.2022.811044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hussein S, Satturwar S, Van der Kwast T. Young-age prostate cancer. J Clin Pathol. 2015;68(7):511-515. doi: 10.1136/jclinpath-2015-202993 [DOI] [PubMed] [Google Scholar]
- 3.Sakr WA, Grignon DJ, Crissman JD, et al. High grade prostatic intraepithelial neoplasia (HGPIN) and prostatic adenocarcinoma between the ages of 20-69: An autopsy study of 249 cases. Vivo. 1994;8(3):439-443. http://www.ncbi.nlm.nih.gov/pubmed/7803731 [PubMed] [Google Scholar]
- 4.Bleyer A, Spreafico F, Barr R. Causation of increased prostate cancer in young men. Oncoscience. 2021;8:37-39. doi: 10.18632/oncoscience.527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Salinas CA, Tsodikov A, Ishak-Howard M, Cooney KA. Prostate cancer in young men: An important clinical entity. Nat Rev Urol. 2014;11(6):317-323. doi: 10.1038/nrurol.2014.91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rawla P. Epidemiology of prostate cancer. World J Oncol. 2019;10(2):63-89. doi: 10.14740/wjon1191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rebbeck TR, Devesa SS, Chang B-L, et al. Global patterns of prostate cancer incidence, aggressiveness, and mortality in men of African descent. Prostate Cancer. 2013;2013:560857-560912. doi: 10.1155/2013/560857 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209-249. doi: 10.3322/caac.21660 [DOI] [PubMed] [Google Scholar]
- 9.World Bank . Population - Total Nigeria. Washington, DC: Data - World Bank; Published 2020. https://data.worldbank.org/indicator/SP.POP.TOTL?locations=NG. Accessed February 5, 2022. [Google Scholar]
- 10.Nigerian National Bureau of Statistics . Distribution of youth (15-35) by age group and sex. 2012 National Baseline Youth Survey. National Baseline Youth Survey Report_1.pdf. Published 2012. https://www.nigerianstat.gov.ng/pdfuploads/2102. Accessed February 5, 2022. [Google Scholar]
- 11.Chidebe Runcie C W, Orjiakor Charles T, Pereira Ian, Ipiankama Sampson C, Lounsbury David W, Moraes Fabio Y. Navigating prostate cancer control in Nigeria. Lancet Oncol 2019;20(11):1489-1491. doi: 10.1016/S1470-2045(19)30625-4 [DOI] [PubMed] [Google Scholar]
- 12.Chidebe RCW, Orjiakor CT, Pereira I, Ipiankama SC, Lounsbury DW, Moraes FY. Navigating prostate cancer control in Nigeria. Lancet Oncol. 2019;20(11):1489-1491. doi: 10.1016/S1470-2045(19)30625-4 [DOI] [PubMed] [Google Scholar]
- 13.Ikuerowo SO, Omisanjo OA, Bioku MJ, Ajala MO, Mordi VPN, Esho JO. Prevalence and characteristics of prostate cancer among participants of a communitybased screening in Nigeria using serum prostate specific antigen and digital rectal examination. Pan Afr Med J. 2013;15(129):129-137. doi: 10.11604/pamj.2013.15.129.2489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Akintola A, Odutola M, Olayinka T, Akinjiola A, Nwokwu O, Adebamowo C, et al. In: Akintola A, et al, eds. Cancer in Nigeria 2009-2016. Abuja, Nigeria: Nigerian National System of Cancer Registries; 2021. [PubMed] [Google Scholar]
- 15.Ogunbiyi O, Ladipo AA, Ogun GO, Adeyemi AO, Fabowale AO, Bodunwa AM. In: Ogunbiyi O, eds. Cancer Incidence and Top Ten Cancers in Ibadan. Ibadan, Nigeria: Ibadan Cancer Registry; 2016. [Google Scholar]
- 16.Oluwole OP, Rafindadi AH, Shehu MS, Samaila MOA. A ten-year study of prostate cancer specimens at Ahmadu Bello University Teaching Hospital (ABUTH), Zaria, Nigeria. Afr J Urol. 2015;21(1):15-18. doi: 10.1016/j.afju.2014.09.004 [DOI] [Google Scholar]
- 17.Powell IJ, Banerjee M, Sakr W, et al. Should African-American men be tested for prostate carcinoma at an earlier age than white men? Cancer. 1999;85(2):472-477. http://www.ncbi.nlm.nih.gov/pubmed/10023717 [PubMed] [Google Scholar]
- 18.Powell IJ, Vigneau FD, Bock CH, Ruterbusch J, Heilbrun LK. Reducing prostate cancer racial disparity: Evidence for aggressive early prostate cancer PSA testing of African-American men. Cancer Epidemiol Biomarkers Prev. 2014;23(8):1505-1511. doi: 10.1158/1055-9965.EPI-13-1328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mersch J, Jackson MA, Park M, et al. Cancers associated with BRCA1 and BRCA2 mutations other than breast and ovarian. Cancer. 2015;121(2):269-275. doi: 10.1002/cncr.29041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Risbridger GP, Taylor RA, Clouston D, et al. Patient-derived xenografts reveal that intraductal carcinoma of the prostate is a prominent pathology in brca2 mutation carriers with prostate cancer and correlates with poor prognosis. Eur Urol. 2015;67(3):496-503. doi: 10.1016/j.eururo.2014.08.007 [DOI] [PubMed] [Google Scholar]
- 21.Kote-Jarai Z, Leongamornlert D, Saunders E, et al. BRCA2 is a moderate penetrance gene contributing to young-onset prostate cancer: Implications for genetic testing in prostate cancer patients. Br J Cancer. 2011;105(8):1230-1234. doi: 10.1038/bjc.2011.383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Edwards SM, Kote-Jarai Z, Meitz J, et al. Two percent of men with early-onset prostate cancer harbor germline mutations in the brca2 gene. Am J Hum Genet. 2003;72(1):1-12. doi: 10.1086/345310 [DOI] [PMC free article] [PubMed] [Google Scholar]