Abstract
Background:
Compared with symptomatic bone marrow edema (BME) associated with stress fractures, asymptomatic BME seen on magnetic resonance imaging (MRI) is a phenomenon that has been described in high-level athletes and is thought to be related to bone adaptation to biomechanical loading unique to each sport. However, the prevalence, natural history, and management of these lesions remain poorly understood, particularly in dance, which places tremendous stress on the feet and ankles.
Purposes/Hypothesis:
The purposes of this study were to (1) determine the prevalence of asymptomatic BME in the talus before the start of the performance season, (2) identify contributing demographic and training factors, and (3) compare the radiological evidence of talar BME with validated functional foot and ankle scores. We hypothesized that talar BME would be highly prevalent among asymptomatic professional dancers.
Study Design:
Case series; Level of evidence, 4.
Methods:
A total of 14 professional ballet dancers (6 female and 8 male; mean age, 24 years) were included in this 2-year prospective study. For each participant, we recorded complete medical and surgical history along with scores on the Foot and Ankle Ability Measure (FAAM) and the Foot and Ankle Disability Index. Bilateral foot and ankle 3.0-T MRI scans without contrast were completed before the start of the performance season and were evaluated for BME of the talus using the Fredericson criteria.
Results:
Evidence of talar BME was seen in 15 of the 28 (54%) ankles examined and in 9 of 14 (64%) dancers. We found that 6 dancers demonstrated bilateral talar BME, 3 dancers demonstrated unilateral BME, and 5 dancers demonstrated no evidence of BME. The most common location of BME was the posterior talus, seen in 8 of 15 (53%) ankles. No statistically significant differences were noted in dancers with versus those without talar BME with regard to functional scores, demographic characteristics, or weekly training hours.
Conclusion:
Asymptomatic talar BME was highly prevalent (64%) in professional ballet dancers and tended to occur posteriorly. Long-term clinical and radiographic follow-up is necessary to determine the natural history of these lesions.
Keywords: foot, ankle, dancer, ballet, bone edema, talus, stress fractures
Edema-like marrow signal intensity, also known as bone marrow edema (BME), is a phenomenon of increased interstitial fluid accumulation within the bone marrow. 9 BME is a finding on magnetic resonance imaging (MRI), is most frequently seen in athletes, and is associated with pain and lower extremity joint swelling. BME is most commonly diagnosed in middle-aged men (aged 30-60 years) and younger women (aged 20-40 years)16,20 and is often symptomatic, is associated with pain-producing pathology, and may be accompanied by stress fractures. 7 In athletes, symptomatic BME can prevent participation in sports practices or competition; a number of treatments are available, ranging from nonoperative regimens with weightbearing restrictions, analgesics, physical therapy, and pharmacologic management to surgical interventions.
Foot and ankle injuries in professional dancers reportedly account for 14% to 57% of all bodily injuries and are predominantly overuse in nature with a high rate of stress fracture.6,27 The talus, with its tenuous blood supply, is identified as high risk with respect to stress fracture complications such as fracture completion, subchondral degeneration, and avascular necrosis. 27 One study in the literature evaluated MRI findings in 11 ballet dancers without performance-limiting foot and ankle injury and found that 9 dancers experienced activity-related ankle pain, with 5 of those dancers also reporting ankle pain at rest. 6 BME in these symptomatic dancers was observed mainly in the neck and body portion of the talus and corresponded with clinical localizable tenderness, with no other bony involvement seen.
In contrast, asymptomatic BME in the foot and ankle represents a different entity and has been described in the literature as an imaging finding associated with long-distance running and altered gait biomechanics in the absence of other confounding pathologies.13,14,25 Unfortunately, the relationship between BME and the predisposition for future injury remains unclear. In comparison with other athletes, professional ballet dancers experience significant and unique loading patterns and mechanical stresses on their feet and ankles, particularly through repetitive activities that entail maximum forced dorsiflexion and plantarflexion. 23 However, a paucity of information exists regarding the expected foot and ankle MRI findings in a population of asymptomatic dancers. An improved understanding of the expected bone reaction to the biomechanical stresses of ballet would aid the clinician in managing these high-level athletes, identifying incidental MRI findings, and avoiding prescribed training or performance restrictions due to concern for stress injury.
Our study purposes were (1) to determine the prevalence of asymptomatic BME in the talus before the start of the performance season, (2) to identify demographic and training factors that may contribute to these findings, and (3) to compare the radiological evidence of talar BME with validated and widely used functional foot and ankle scores. We hypothesized that BME would have a high prevalence among asymptomatic professional dancers. Additionally, we hypothesized that increased age and training hours would be positively associated with the presence of BME on MRI scans.
Methods
After informed consent was obtained, 14 professional ballet dancers were enrolled in this 2-year prospective, institutional review board–approved study. Participation in this study did not affect the dancer’s training or performance regimen unless a performance-limiting injury was found on examination or MRI. Exclusion criteria included dancers reporting foot and ankle pain on initial history and physical examination at the beginning of the season, foot and ankle surgery or injury within the past year, and any contraindications for MRI.
A complete medical and surgical history was obtained for all enrolled participants. Participants underwent physical examination by a fellowship-trained orthopaedic foot and ankle surgeon (S.M.) . Dancer training hours were logged over the performance season, with preseason hours averaged over the previous 3 months before start of the season. All dancers were asymptomatic at the pre-enrollment physical evaluation, and physical examination findings were unremarkable for performance-limiting foot and ankle pathology. None of the enrolled dancers had experienced a time-loss foot and ankle injury within 3 years of study enrollment.
The Foot and Ankle Ability Measure, including its Activities of Daily Living and Sports Function subscales, and the Foot and Ankle Disability Index were completed by all enrolled participants. The reliability and sensitivity of these outcome measures have been described in both normal populations and elite athletes, with evidence showing that these patient-reported outcome measures are sensitive to changes in functional and symptomatic foot and ankle status in athletes.10,12,18 Therefore, these outcome measures are suitable quantitative indicators of asymptomatic status in our patient population and were used during the study.
Imaging Data
Bilateral foot and ankle MRI without contrast using a 3.0-T magnet was completed before the start of the performance season; the sequences used included axial and coronal T1-weighted and T2-weighted fat saturation (T2FS) fast spin-echo sequences and sagittal T1-weighted fast spin-echo and short-tau inversion recovery (STIR) sequences. All MRI scans were interpreted by a blinded, fellowship-trained musculoskeletal radiologist (N.F.) using the Fredericson criteria.1,8,11
The presence of BME was determined by hyperintense marrow signal abnormality on the T2FS and STIR sequences and was described radiologically as edema-like marrow signal intensity, which describes abnormal signal intensity with the absence of clear margins and may exceed anatomic borders. 17 Images from STIR sequences were used to reliably identify and localize cases of BME. This practice is supported by current literature, which suggests that superior fat suppression and, therefore, identification of BME are achieved with STIR relative to T2FS sequencing.3,20 Although STIR sequencing is superior for BME identification, it has inferior signal-to-noise ratio relative to T2FS sequencing and thus does not produce as high-resolution images as are expected from a 3.0-T MRI image.3,20 BME represents a histopathological diagnosis; however, to be consistent with prior clinical studies, the term BME was used throughout this article instead of edema-like marrow signal intensity.
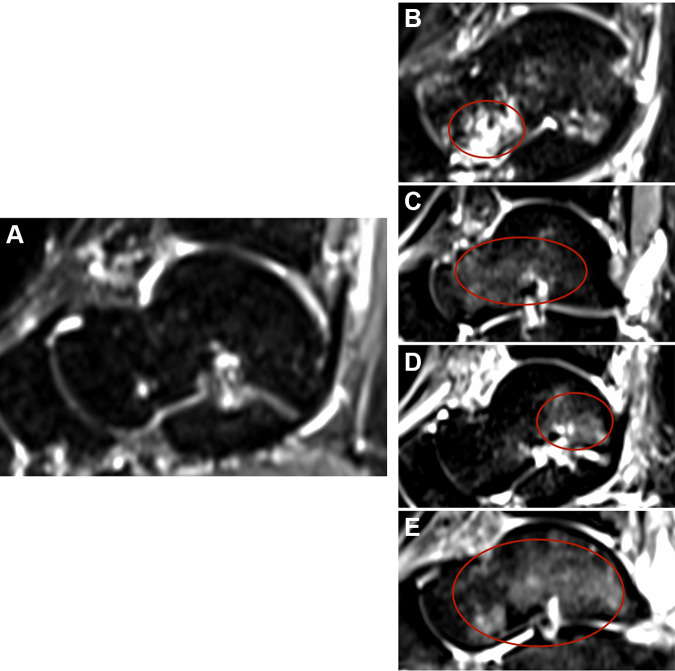
The location of BME was characterized into the following regions: talar head and neck, talar body, posterior talus, and pan-talar (Figure 1). When BME extended to multiple regions of the talus, the area with highest signal intensity was recorded. If hyperintense marrow signal was visualized on the T2FS sequence but no corresponding marrow signal abnormality was visualized on STIR, this was determined to represent inhomogeneous fat saturation rather than true BME. There were no instances where hyperintense marrow signal was visualized on STIR but not T2FS.
Figure 1.
Sagittal magnetic resonance images of the ankle, obtained by T2-weighted fat saturation sequences, with representative images of various types of talar bone marrow edema (BME) identified (circles): (A) no BME; (B) head and neck BME; (C) body BME; (D) posterior BME; (E) pan-talar BME.
If BME was visualized, any corresponding T1-weighted signal abnormality was recorded. Furthermore, the presence or absence of any intracortical signal abnormality was noted in conjunction with BME. To exclude confounding pathologies that could have caused BME, images were reviewed for the presence of osteoarthrosis (focal areas of subchondral signal abnormality at opposing articular surfaces) and osteochondral lesions (subchondral crescentic signal abnormality). Marrow edema subjacent to a tendinous or ligamentous insertion or attachment was attributed to represent enthesopathy or reactive rather than stress-related marrow signal abnormality. Evaluation for the presence or absence of signs of posterior ankle impingement was also recorded as suggested by combinations of the presence of an os trigonum, the Stieda process, focally prominent fluid in the posterior joint recess, posterior talofibular ligament abnormality, or flexor hallucis longus tenosynovitis. Focal tubular, well-delineated, T2-weighted, hyperintense marrow signal abnormality was determined to be a vascular channel rather than true BME. Finally, osteonecrosis was considered if there was serpiginous, intraosseous, marrow signal abnormality with the presence of a T2-weighted hyperintense linear signal with adjacent T2-weighted hypointense linear signal.
Statistical Analysis
The Welch 2-sample t test was used to compare demographic characteristics between participants with versus without radiological evidence of talar BME. We used the Kruskal-Wallis H test to compare distributions of demographic criteria between dancers with bilateral BME, unilateral BME, and normal ankles. Categorical variables such as sex were not suitable for inclusion in the t test and H test, and sample size was not appropriate for analysis with the chi-square test. Statistical significance was determined at P ≤ .05. All statistical analysis was performed in R studio (Posit, Joseph J Allaire). 22
Results
Of the 14 professional ballet dancers enrolled in the study, 6 were female and the mean age was 24.4 years (age range, 19-34 years). Dancers reported an average of 36.9 hours of ballet training per week during preseason training, averaged over the previous 3 months of off-season training.
In total, 15 of the 28 (54%) ankles examined with MRI demonstrated evidence of talar BME. Evidence of talar BME was seen in 9 of 14 (64%) dancers, with 6 dancers demonstrating bilateral talar BME and 3 demonstrating unilateral findings. Of the ankles with positive findings of BME, 8 (53%) had BME localized to the posterior talus, 3 (20%) had pan-talar BME, 2 (13%) had BME localized to the talar body, and 2 (13%) had BME localized to the talar head and neck (Table 1).
Table 1.
Distribution of Talar Bone Marrow Edema by Regions
| Talar Region | No. (%) of Participants |
|---|---|
| Pan-talar | 3 (20) |
| Talar head and neck | 2 (13) |
| Talar body | 2 (13) |
| Posterior talus | 8 (53) |
We found no statistically significant differences between the radiological presence of talar BME and functional outcome scores, demographic characteristics (age, body mass index), or self-reported weekly training hours (Table 2). Comparison of groups (BME present vs absent) using the Kruskal-Wallis test revealed no statistically significant difference in the distributions of functional outcome scores or demographic characteristics.
Table 2.
Functional Scores and Participant Characteristics According to the Presence of Talar BME a
| Talar BME Absent (n = 13) |
Talar BME Present (n = 15) |
P (Welch t test) | |
|---|---|---|---|
| Functional scores | |||
| FAAM-ADL, % | 98.9 ± 3.6 | 97.9 ± 3.4 | .47 |
| FAAM–Sports Function, % | 95.9 ± 6.3 | 94.8 ± 6.5 | .65 |
| FADI | 2.8 ± 3.3 | 3.9 ± 4.2 | .11 |
| Age, y | 26.3 ± 5.9 | 22.8 ± 2.7 | .06 |
| Body mass index | 21.5 ± 3.0 | 21.3 ± 1.9 | .86 |
| Weekly training, h | 35.4 ± 4.7 | 34.9 ± 7.9 | .29 |
a Data are reported as mean ± SD. ADL, activities of daily living; BME, bone marrow edema; FAAM, Foot and Ankle Ability Measure; FADI, Foot and Ankle Disability Index.
Discussion
Results from our study suggest that asymptomatic BME of the talus is highly prevalent (seen in 64% of professional ballet dancers), thus confirming our hypothesis. Comparing dancers without talar BME with those with talar BME bilaterally or unilaterally, we found no statistically significant differences between demographic characteristics, functional outcome scores, or number of training hours. The distribution of BME most commonly involved the posterior talus (53%), followed by pan-talar (20%). Considering the qualitative features of MRI findings, we expect that chronic loading leads to altered bone metabolism with resultant remodeling and neovascularization. As to why the posterior talar BME was observed, we suspect that with ankle hyperplantarflexion during en pointe and demi-pointe, the posterior aspect of the talus encounters increased weightbearing forces due to decreased contact area between the posterior aspect of the talus and the posterior tibia, given that the posterior portion of the talus is narrower because it sits in the mortise. 4 This also appears to be confirmed in light of a previous study of 9 female ballet dancers undergoing a new MRI scanning technique while maintaining the en pointe position. 24 In that study, a significant anatomic contact point was noted to occur between 3 structures: posterior tibial plafond, posterior talus (including the nonarticular portion), and superior calcaneus at its posterior-most portion of the posterior facet. 24
In the literature for specific sports, the presence of asymptomatic BME on MRI may represent incidental radiographic findings secondary to repetitive stress-induced physiologic processes throughout the body. Lazzarini et al 13 found BME in the ankles of 16 of 20 asymptomatic runners versus only 4 of 12 nonrunners. Additionally, Major and Helms 15 found BME on MRI scans in 14 of 34 knees in asymptomatic collegiate basketball players. Last, Brunner et al 5 examined 40 knees in 20 professional basketball or collegiate football players and found significant baseline MRI abnormalities, including asymptomatic BME in 10 of the 20 athletes examined. However, the current literature provides a paucity of evidence regarding the progression of asymptomatic BME in high-level athletes. At present, no clear guidelines are available for the management of these purely radiographic findings in the setting where athletes undergo MRI due to pain in the extremity but pain location does not exactly correspond to the areas of BME observed. 2
Interestingly, in reports of painful talar BME and talar stress fractures, a different predominant pattern of talar involvement appears. In a study that used 2.0-T MRI, dancers with ankle pain localized over the talus had BME mainly in the talar body and neck. 6 Two studies revealed that talar stress fractures are rare, tend to occur with repetitive axial loading activities, and predominantly involve the superior portion of the talar head.19,26 In a large military study of 56 talar stress fractures, only 8% occurred in the posterior talus. 26 These findings suggest that patterns of BME in symptomatic dancers may differ from patterns of BME in asymptomatic dancers and that certain distributions of talar BME may have worse prognoses than others.
Consequently, in ballet dancers and other athletic populations at high risk of osseous stress injury, we are cautious when these findings are incidentally found in bones at high risk for secondary stress fracture complications (ie, avascular necrosis, fracture completion, articular collapse, and posttraumatic osteoarthritis). 21 However, using our study’s results combined with a careful history and physical examination demonstrating no localizable pain or effusion over the talus, a clinician can reasonably consider monitoring a dancer with talar BME over the performance season, allowing continued participation without the need for immediate immobilization or restricted weightbearing.
Limitations
We must consider the findings of the present investigation in the context of its limitations. Our study was limited by the availability of asymptomatic dancer volunteers available for MRI examination and so may be underpowered. However, due to the rarity of the asymptomatic state and the consequently limited information available in the literature, we believe that our sample size is adequate to describe a baseline prevalence for asymptomatic BME in professional ballet dancers. Another potential shortcoming of our study is that the participants were dedicated professional dancers, and some dancers may be reluctant to report pain on examination due to fear of missing out on the performance season. This is an inherent limitation in any study involving pain in high-level athletes. However, the impact of “masking” pain must be considered, because it directly affects our assessment of the prevalence of asymptomatic BME. We attempted to minimize this impact by using additional screening measures such as the Foot and Ankle Disability Index, which includes 4 pain items, and the Foot and Ankle Ability Measure Sports Function subscale. Ceiling effects likely were demonstrated, as the professional dancers were very high-functioning athletes, and perhaps a more dancer-specific, validated screening system could be developed to aid future investigations. A third limitation to our study is the lack of long-term follow-up to better understand sex-related differences and the prognosis of asymptomatic BME. Nonetheless, the purpose of our study was solely to determine the prevalence of asymptomatic BME in asymptomatic dancers at the start of the season. Our ongoing investigation will address this limitation by conducting long-term follow-up in order to determine the natural history of BME in professional dancers.
Conclusion
Asymptomatic BME of the posterior talus can be highly prevalent in professional ballet dancers. In our limited cohort of dancers without foot and ankle ailments, we did not find an association between the presence of talar BME and body mass index, functional foot and ankle scores, or weekly training hours. Long-term clinical and radiographic follow-up is necessary to better understand the clinical significance and appropriate management recommendations for asymptomatic BME of the talus in professional ballet dancers.
Footnotes
Final revision submitted October 2, 2022; accepted November 15, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: S.M.has received education payments from Arthrex. E.R.H. has received education payments from Rock Medical Orthopedics. J.I. has received education payments from Rock Medical Orthopedics. J.V. has received education payments from Arthrex, consulting fees from DePuy Synthes, and speaking fees from Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from University Hospitals Cleveland Medical Center (ref No. STUDY20200651).
References
- 1.Arendt EA, Griffiths HJ. The use of MR imaging in the assessment and clinical management of stress reactions of bone in high-performance athletes. Clin Sports Med. 1997;16(2):291–306. [DOI] [PubMed] [Google Scholar]
- 2.Baumbach SF, Pfahler V, Bechtold-Dalla Pozza S, et al. How we manage bone marrow edema—an interdisciplinary approach. J Clin Med. 2020;9(2):551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brandão S, Seixas D, Ayres-Basto M, et al. Comparing T1-weighted and T2-weighted three-point Dixon technique with conventional T1-weighted fat-saturation and short-tau inversion recovery (STIR) techniques for the study of the lumbar spine in a short-bore MRI machine. Clin Radiol. 2013;68(11):e617–e623. [DOI] [PubMed] [Google Scholar]
- 4.Brockett CL, Chapman GJ. Biomechanics of the ankle. Orthop Trauma. 2016;30(3):232–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brunner MC, Flower SP, Evancho AM, Allman FL, Apple DF, Fajman WA. MRI of the athletic knee: findings in asymptomatic professional basketball and collegiate football players. Invest Radiol. 1989;24(1):72–75. [DOI] [PubMed] [Google Scholar]
- 6.Elias I, Zoga AC, Raikin SM, et al. Bone stress injury of the ankle in professional ballet dancers seen on MRI. BMC Musculoskelet Disord. 2008;9:39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fernandez-Canton G. From bone marrow edema to osteonecrosis: new concepts. Article in Spanish. Reumatol Clin. 2009;5(5):223–227. [DOI] [PubMed] [Google Scholar]
- 8.Fredericson M, Bergman AG, Hoffman KL, Dillingham MS. Tibial stress reaction in runners: correlation of clinical symptoms and scintigraphy with a new magnetic resonance imaging grading system. Am J Sports Med. 1995;23(4):472–481. [DOI] [PubMed] [Google Scholar]
- 9.Ghasemi RA, Sadeghi S, Rahimee N, Tahmasebi M. Technologies in the treatment of bone marrow edema syndrome. Orthop Clin North Am. 2019;50(1):131–138. [DOI] [PubMed] [Google Scholar]
- 10.Hale SA, Hertel J. Reliability and sensitivity of the Foot and Ankle Disability Index in subjects with chronic ankle instability. J Athl Train. 2005;40(1):35–40. [PMC free article] [PubMed] [Google Scholar]
- 11.Hwang B, Fredericson M, Chung CB, Beaulieu CF, Gold GE. MRI findings of femoral diaphyseal stress injuries in athletes. AJR Am J Roentgenol. 2005;185(1):166–173. [DOI] [PubMed] [Google Scholar]
- 12.Kim H, Chung E, Lee BH. A comparison of the foot and ankle condition between elite athletes and non-athletes. J Phys Ther Sci. 2013;25(10):1269–1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lazzarini KM, Troiano RN, Smith RC. Can running cause the appearance of marrow edema on MR images of the foot and ankle? Radiology. 1997;202(2):540–542. [DOI] [PubMed] [Google Scholar]
- 14.Lohman M, Kivisaari A, Vehmas T, Kallio P, Malmivaara A, Kivisaari L. MRI abnormalities of foot and ankle in asymptomatic, physically active individuals. Skeletal Radiol. 2001;30(2):61–66. [DOI] [PubMed] [Google Scholar]
- 15.Major NM, Helms CA. MR imaging of the knee: findings in asymptomatic collegiate basketball players. Am J Roentgenol. 2002;179(3):641–644. [DOI] [PubMed] [Google Scholar]
- 16.Manara M, Varenna M. A clinical overview of bone marrow edema. Reumatismo. 2014;66(2):184–196. [DOI] [PubMed] [Google Scholar]
- 17.Maraghelli D, Brandi ML, Matucci Cerinic M, Peired AJ, Colagrande S. Edema-like marrow signal intensity: a narrative review with a pictorial essay. Skeletal Radiol. 2021;50(4):645–663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Martin RL, Irrgang JJ, Burdett RG, Conti SF, Van Swearingen JM. Evidence of validity for the Foot and Ankle Ability Measure (FAAM). Foot Ankle Int. 2005;26(11):968–983. [DOI] [PubMed] [Google Scholar]
- 19.McGlone JJ. Stress fracture of the talus. J Am Podiatry Assoc. 1965;55(12):814–817. [DOI] [PubMed] [Google Scholar]
- 20.Mirghasemi SA, Trepman E, Sadeghi MS, Rahimi N, Rashidinia S. Bone marrow edema syndrome in the foot and ankle. Foot Ankle Int. 2016;37(12):1364–1373. [DOI] [PubMed] [Google Scholar]
- 21.Pearce DH, Mongiardi CN, Fornasier VL, Daniels TR. Avascular necrosis of the talus: a pictorial essay. Radiogr Rev Publ Radiol Soc N Am Inc. 2005;25(2):399–410. [DOI] [PubMed] [Google Scholar]
- 22.R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing; 2020. https://www.R-project.org/ [Google Scholar]
- 23.Russell JA, McEwan IM, Koutedakis Y, Wyon MA. Clinical anatomy and biomechanics of the ankle in dance. J Dance Med Sci. 2008;12(3):75–82. [PubMed] [Google Scholar]
- 24.Russell JA, Shave RM, Yoshioka H, Kruse DW, Koutedakis Y, Wyon MA. Magnetic resonance imaging of the ankle in female ballet dancers en pointe. Acta Radiol. 2010;51(6):655–661. [DOI] [PubMed] [Google Scholar]
- 25.Schweitzer ME, White LM. Does altered biomechanics cause marrow edema? Radiology. 1996;198(3):851–853. [DOI] [PubMed] [Google Scholar]
- 26.Sormaala MJ, Niva MH, Kiuru MJ, Mattila VM, Pihlajamäki HK. Bone stress injuries of the talus in military recruits. Bone. 2006;39(1):199–204. [DOI] [PubMed] [Google Scholar]
- 27.Sormaala MJ, Niva MH, Kiuru MJ, Mattila VM, Pihlajamäki HK. Outcomes of stress fractures of the talus. Am J Sports Med. 2006;34(11):1809–1814. [DOI] [PubMed] [Google Scholar]