Abstract
Background:
Post traumatic seizures (PTS) are a known sequel of traumatic brain injury (TBI). Incidence of PTS is dependent on many factors including study design and characteristics of the study population. As incidence of TBI increases and death due to TBI decreases, more individuals will be at risk of developing and living with chronic complications. The objective of the present study was to determine the frequency and risk factors for PTS following TBI.
Methods:
A prospective study was conducted on patients admitted with TBI from April 1, 2019, to May 31, 2020, to determine the frequency, time to event, and risk factors for PTS following TBI. We classified the severity of head injury using a standard criterion, into mild, moderate and severe injury. Follow-up of 3 months was undertaken for all patients. Variables include age, sex, trauma severity, Glasgow coma scale, onset of PTS, and neuroradiological finding.
Results:
We enrolled 450 post traumatic subjects, out of which 36 (8%) developed seizures. Of the total of 36 patients detected to have hemorrhagic contusion on computerized tomography scan, 12 patients developed seizures. We found that the independent risk factors associated with occurrence of PTS were frontal— temporal lobar contusion and severity of head injury. All these findings were statistically significant.
Conclusion:
We found that the independent risk factors associated with occurrence of PTS were frontal-temporal lobar contusion and severity of head injury. Type of management (Operative vs. Non operative) does not affect the outcome of PTS.
Keywords: Antiepileptic, Head injury, Post traumatic seizures, Traumatic brain injury

INTRODUCTION
Traumatic brain injury (TBI) is a significant public health concern and is a major cause of morbidity and mortality, especially in patients <45 years.[7,13] Patients may experience many different complications and comorbidities associated with TBI that may continue chronically, persisting for many years or even throughout the lifetime following injury.[2,6,19,21]
Individuals with more severe injury are particularly affected by chronic conditions associated with TBI. Among individuals who survive a severe TBI, disability rates are estimated as high as 77%.[3] Chronic complications include poor functional outcome, decreased cognitive function, psychosocial and/or behavioral problems, decreased general health, and other neurological sequelae. These complications contribute significantly to the cost of care associated with TBI, which is estimated at more than $60 billion annually.[20] In addition to medical cost, TBI may significantly increase years of potential life lost and decrease the quality of life.
Despite decades of research, there are no effective pharmacological interventions to prevent post-traumatic seizures (PTS) that develop after 7 days post injury and, it does not appear that rates of PTS are decreasing.[16] Increasingly, novel risk factors for PTS and mechanisms of epileptogenesis following TBI are being investigated to identify potential new targets for therapeutic treatment.
MATERIALS AND METHODS
A prospective study was conducted on patients admitted with TBI in a Tertiary care Centre in North India from April 1, 2019, to May 31, 2020. Prior ethics committee permission was obtained and written informed consent was taken from each participant before including them in the study.
Inclusion criterion
All patients who presented with acute TBI in the hospital were included in the study.
Exclusion criterion
(1) A preceding history of brain injury or major mental disorder, (2) Pregnancy, (3) Predisposition to seizures (such as a history of brain tumor or stroke), (4) Family history of seizures.
In this study, we used the classification of head injury severity as defined by Annegers et al.[5] Mild injuries were those in which no skull fracture was found and the period of post traumatic amnesia or loss of consciousness was ≤30 min. The moderately injured group of patients included those with skull fractures or other injuries with >30 min of post traumatic amnesia or loss of consciousness, who did not otherwise meet the criteria for a severe injury. Severe injuries were those with a documented brain contusion, an intracerebral hematoma or >24 h of post traumatic amnesia or loss of consciousness.[9] Follow-up of 3 months was done. Variables such as age, sex, trauma severity, Glasgow coma scale (GCS), onset of PTS, and neuroradiological findings were studied.
Statistical analysis
All statistical calculations were done using 17 Statistical Package for the Social Science 21 version statistical program for Microsoft Windows.
RESULTS
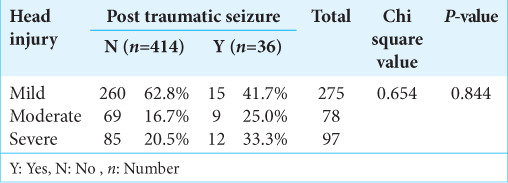
In our study, 450 post traumatic patients were included in the study. Thirty-six (8%) patients developed seizures. Patients with seizures were classified into three categories based on the GCS score. The group with GCS score of 3–6 had 15 patients developing seizures out of 275 patients. The group with GCS score of 7–12 had nine patients developing seizures out of 78 patients. The group with GCS score of 13–15 had 12 numbers of patients developing seizures out of 97 patients. Mean GCS of patients developing seizure is 12.28 ± 3.551 [Table 1].
Table 1:
Post traumatic seizures in various head injuries.
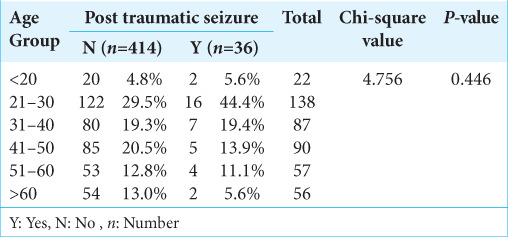
In our study, total number of patients were 450, 22 patients below the age group of 20 out of which two developed seizures (5.6%). One hundred and thirty-eight patients in the age group of 21–30 years, out of which 16 developed seizures (44.4%). Eighty-seven patients were in the age group of 31–40, out of which seven developed seizures (19.4%). Ninety patients were in the age group of 41–50, out of which five developed seizures (13.9). Fifty-seven patients were in the age group of 51–60, out of which four developed seizures (11.1%). Fifty-six patients had age more than 60 year, out of which two developed seizures (5.6%). Mean age of patients developing seizure is 36.14 ± 13.7 [Table 2].
Table 2:
Post traumatic seizures in various age groups.
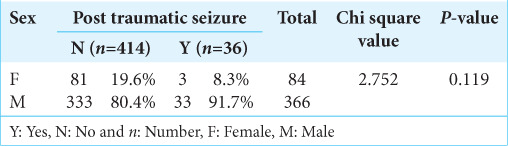
In our study, out of 450 patients, 366 were males and 84 were females. Thirty-three males and three females developed seizures [Table 3]. Mean duration of stay, in patients developing seizures was 17.04 days and in patients not developing seizure was 17.03 days.
Table 3:
Post traumatic seizures in different genders.
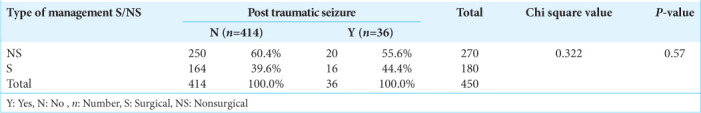
Patients were also classified on the basis of computerized tomography (CT) findings. Of the total of 36 patients detected to have hemorrhagic contusion on CT scan, 12 patients developed seizures (33%). Of the total of eight patients diagnosed diffuse axonal injury, one patient developed seizures (12.5%). Of the total of 70 patients detected to have depressed fracture on CT scan, seven developed seizures (10%). Forty-seven patients who were diagnosed as a case of extradural hemorrhage on CT scan, one patient developed seizures (2%). Of the total of 61 patients diagnosed subarachnoid hemorrhage on CT scan, six patients developed seizures (9.8%), of the total of 131 patients detected to have subdural hemorrhage on CT scan, nine patients developed seizures (6.8%). Of the two patients diagnosed with intraparenchymal hemorrhage, none developed seizures. Of the total 450 patients, 270 were managed conservatively and 180 patients were operated. Twenty patients out of 270 patients had seizures.
One hundred and eighty patients were operated, 16 had seizures [Table 4].
Table 4:
Incidence of post traumatic seizures in operative versus non operative group.
DISCUSSION
In our study, 450 patients with diagnosis of TBI were evaluated. The patients underwent detailed clinical evaluation and radiological investigation as and when indicated. In a study conducted by Lee et al., total of 4232 consecutively treated adult patients with mild closed head injury were examined. They ranged in age from 16 to 88 years mean (32.82 years); the male: Female ratio was 3.8:1. The most common causes of trauma are motorcycle accidents (53.78%) and pedestrian injury (28.89%). In 100 patients (2.36) who developed seizures within the1st week after head injury, the male: female was 7:1, the mean age was 29.74 years.[17]
In this study, subjects that were 21–30 years at age were more likely to develop PTS than subjects >30 years of age, but no significant difference between subjects 21–50 and those >50 years. Immaturity of the brain, which has been offered as the explanation for the greater susceptibility of children to early PTS, may explain the greater susceptibility of the younger age groups for seizures.
In our study, the overall incidence of PTS was found to be 8%. The incidence in normal civilian is 1.8–5%.[11,14] In our study, we found that the independent risk factors associated with occurrence of PTS were frontal—temporal lobar contusion and severity of head injury measured using GCS.
Several reports (Annegers et al.; Angeleri et al.; Englander et al.) have shown cerebral contusion was indeed a risk factor.[4,5,9] Englander et al.[9] reported the highest cumulative probability for late post traumatic seizures included biparietal contusions (66%) and multiple or bilateral cortical contusions (25%).[8,12,18] Former studies have reported that TBI has a predilection for frontal and temporal lobes. However, the mechanisms of PTS caused by contusion are still not clear.
A possible explanation for this may be the following; Cortical neurons are injured following contusions and this would lead the iron from the blood deposited in the cortex; the deposited iron would lead to iron induced membrane peroxidation and would make the seizure spread to the subcortical areas (hippocampus mainly); the occurrence and evolution of the epileptiform activity in the subcortical structures would in parallel with that in the cortical focus.[1,8,15,23,25]
TBI severity measured by GCS score is also a risk factor in this study. The patients with lower GCS scores (more severe injury) have more risk to develop PTS.[24] Haltiner et al.;[12] Schütze et al.;[22] and Ferguson et al.[10] have reported that severity of the TBI patients was a risk factor for PTS and the risk was increased with the severity of TBI. In these studies, GCS score was used to measure the brain injury severity. All of those reported the risk of PTS increased with increased TBI severity.
In our study, we used GCS score to measure the TBI severity and the results were consistent with the former studies. We found that the patients with GCS scores from 3 to 8 had the highest seizure frequency (19.9%) and the highest risk to develop PTS (4.103 times risk rate). However, some studies showed that the GCS score is not a risk factor. Englander et al.[9] showed that GCS score alone could not predict late post traumatic seizure risk. The authors found the patients whose GCS scores from 9 to 12 had the highest seizure frequency compared to those whose GCS scores from 3 to 8. The difference may be caused by different study methods, different entry criteria and different population the studies based and the characteristic of the patients.
CONCLUSION
In this study of TBI patients, frontal-temporal lobar contusion and severity of TBI measured by initial GCS were significant in the multivariate model analysis. The reason PTS happens still needs to be investigated. Thorough follow-up of patients with PTS and antiepileptic therapy may attain rehabilitation goals.
Footnotes
How to cite this article: Garg T, Sood R, Chaudhary A, Sobti S, Sharma S, Chaudhary AK, et al. A prospective study to determine the risk factors associated with post traumatic seizures: A single institution experience. Surg Neurol Int 2023;14:143.
Contributor Information
Tarun Garg, Email: tarungarg187@gmail.com.
Raghav Sood, Email: dr.raghavsood@gmail.com.
Akshay Chaudhary, Email: 01akshayc@gmail.com.
Shivender Sobti, Email: sobtish@gmail.com.
Saurabh Sharma, Email: saurabh11803551@gmail.com.
Ashwani K. Chaudhary, Email: ashwanidmc@yahoo.co.in.
Hanish Bansal, Email: y2khanish@gmail.com.
Jagminder Singh, Email: jagmindersinghdr@yahoo.com.
Manish Sharma, Email: drmanishsharma03@gmail.com.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
REFERENCES
- 1.Agrawal A, Timothy J, Pandit L, Manju M. Posttraumatic epilepsy: An overview. Clin Neurol Neurosurg. 2006;108:433–9. doi: 10.1016/j.clineuro.2005.09.001. [DOI] [PubMed] [Google Scholar]
- 2.Andriessen TM, Horn J, Franschman G, van der Naalt J, Haitsma I, Jacobs B, et al. Epidemiology, severity classification, and outcome of moderate and severe traumatic brain injury: A prospective multicenter study. J Neurotrauma. 2011;28:2019–31. doi: 10.1089/neu.2011.2034. [DOI] [PubMed] [Google Scholar]
- 3.Andriessen TM, Jacobs B, Vos PE. Clinical characteristics and pathophysiological mechanisms of focal and diffuse traumatic brain injury. J Cell Mol Med. 2010;14:2381–92. doi: 10.1111/j.1582-4934.2010.01164.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Angeleri F, Majkowski J, Cacchio G. Posttraumatic epilepsy risk factors: One-year prospective study after head injury. Epilepsia. 1999;40:1222–30. doi: 10.1111/j.1528-1157.1999.tb00850.x. [DOI] [PubMed] [Google Scholar]
- 5.Annegers JF, Hauser WA, Coan SP, Rocca WA. A population based study of seizures after traumatic brain injuries. N Engl J Med. 1998;338:20–4. doi: 10.1056/NEJM199801013380104. [DOI] [PubMed] [Google Scholar]
- 6.Brooks JC, Strauss DJ, Shavelle RM, Paculdo DR, Hammond FM, Harrison-Felix CL. Long-term disability and survival in traumatic brain injury: Results from the National Institute on Disability and Rehabilitation Research Model Systems. Arch Phys Med Rehabil. 2013;94:2203–9. doi: 10.1016/j.apmr.2013.07.005. [DOI] [PubMed] [Google Scholar]
- 7.Bruns J, Jr, Hauser WA. The epidemiology of traumatic brain injury: A review. Epilepsia. 2003;44:2–10. doi: 10.1046/j.1528-1157.44.s10.3.x. [DOI] [PubMed] [Google Scholar]
- 8.Dakin KA, Weaver DF. Mechanisms of post-traumatic seizures: A quantum pharmacological analysis of the molecular properties of an epileptogenic focus following iron-induced membrane peroxidation. Seizure. 1993;2:21–33. doi: 10.1016/s1059-1311(05)80098-6. [DOI] [PubMed] [Google Scholar]
- 9.Englander J, Bushnik T, Duong TT, Cifu DX, Zafonte R, Wright J, et al. Analyzing risk factors for late posttraumatic seizures: A prospective, multicenter investigation. Arch Phys Med Rehabil. 2003;84:365–73. doi: 10.1053/apmr.2003.50022. [DOI] [PubMed] [Google Scholar]
- 10.Ferguson PL, Smith GM, Wannamaker BB. A population-based study of risk of epilepsy after hospitalization for traumatic brain injury. Epilepsia. 2010;51:891–8. doi: 10.1111/j.1528-1167.2009.02384.x. [DOI] [PubMed] [Google Scholar]
- 11.Frey LC. Epidemiology of posttraumatic epilepsy: A critical review. Epilepsia. 2003;44:11–7. doi: 10.1046/j.1528-1157.44.s10.4.x. [DOI] [PubMed] [Google Scholar]
- 12.Haltiner AM, Temkin NR, Dikmen SS. Risk of seizure recurrence after the first late posttraumatic seizure. Arch Phys Med Rehabil. 1997;78:835–40. doi: 10.1016/s0003-9993(97)90196-9. [DOI] [PubMed] [Google Scholar]
- 13.Harrison-Felix C, Pretz C, Hammond FM, Cuthbert JP, Bell J, Corrigan J, et al. Life expectancy after inpatient rehabilitation for traumatic brain injury in the United States. J Neurotrauma. 2015;32:1893–901. doi: 10.1089/neu.2014.3353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jennett B. Early traumatic epilepsy. Incidence and significance after non-missile injuries. Arch Neurol. 1974;30:394–8. doi: 10.1001/archneur.1974.00490350052008. [DOI] [PubMed] [Google Scholar]
- 15.Kharatishvili I, Nissinen JP, McIntosh TK, Pitkänen A. A model of posttraumatic epilepsy induced by lateral fluid-percussion brain injury in rats. Neuroscience. 2006;140:685–97. doi: 10.1016/j.neuroscience.2006.03.012. [DOI] [PubMed] [Google Scholar]
- 16.Kirmani BF, Robinson DM, Fonkem E, Graf K, Huang JH. Role of anticonvulsants in the management of posttraumatic epilepsy. Front Neurol. 2016;7:32. doi: 10.3389/fneur.2016.00032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee ST, Lui TN, Wong CW, Yeh YS, Tzuan WC, Chen TY, et al. Early seizures after severe closed head injury. Can J Neurol Sci. 1997;24:40–3. doi: 10.1017/s0317167100021077. [DOI] [PubMed] [Google Scholar]
- 18.Lowenstein DH. Epilepsy after head injury: An overview. Epilepsia. 2009;50:4–9. doi: 10.1111/j.1528-1167.2008.02004.x. [DOI] [PubMed] [Google Scholar]
- 19.Atlanta, GA: Centers for Disease Control and Prevention; 2014. Report to Congress on Traumatic Brain Injury in the United States: Epidemiology and Rehabilitation. [DOI] [PubMed] [Google Scholar]
- 20.Rockhill CM, Jaffe K, Zhou C, Fan MY, Katon W, Fann JR. Health care costs associated with traumatic brain injury and psychiatric illness in adults. J Neurotrauma. 2012;29:1038–46. doi: 10.1089/neu.2010.1562. [DOI] [PubMed] [Google Scholar]
- 21.Salazar AM, Jabbari B, Vance SC, Grafman J, Amin D, Dillon JD. Epilepsy after penetrating head injury. I. Clinical correlates: A report of the Vietnam Head Injury Study. Neurology. 1985;35:1406–14. doi: 10.1212/wnl.35.10.1406. [DOI] [PubMed] [Google Scholar]
- 22.Schütze M, Dauch WA, Güttinger M, Hämpel-Christiansen M, Firsching R. Risk factors for posttraumatic fits and epilepsy. Zentralbl Neurochir. 1999;60:163–7. [PubMed] [Google Scholar]
- 23.Sharma V, Babu PP, Singh A, Singh S, Singh R. Iron-induced experimental cortical seizures: Electroencephalographic mapping of seizure spread in the subcortical brain areas. Seizure. 2007;16:680–90. doi: 10.1016/j.seizure.2007.05.012. [DOI] [PubMed] [Google Scholar]
- 24.Temkin NR, Dikmen SS, Anderson GD, Wilensky AJ, Holmes MD, Cohen W, et al. Valproate therapy for prevention of posttraumatic seizures: A randomized trial. J Neurosurg. 1999;91:593–600. doi: 10.3171/jns.1999.91.4.0593. [DOI] [PubMed] [Google Scholar]
- 25.Willmore LJ, Triggs WJ. Effect of phenytoin and corticosteroids on seizures and lipid peroxidation in experimental posttraumatic epilepsy. J Neurosurg. 1984;60:467–72. doi: 10.3171/jns.1984.60.3.0467. [DOI] [PubMed] [Google Scholar]


