Abstract
Background:
Subdural hematoma (SDH) is considered spontaneous in the absence of trauma history. It is a common presentation in the geriatric age group due to the many influential factors. Most cases have a known underlying etiology that explains the incidence, otherwise, they are considered idiopathic. We present a rare case report of idiopathic nontraumatic bilateral SDH with a literature review of similar cases.
Case Description:
A 28-year-old fit individual presented to the Emergency Department with a chronic history of severe headache and neck pain, associated with behavioral changes in the last 2 days. He reported that his symptoms started after lifting a heavy object 2 months ago; however, they became worse after a neck chiropractor therapy session. He is not on any chronic medications, and there was a negative history of trauma, seizure, hematological diseases, family history of neurological conditions, smoking, alcohol, or drug abuse with an unremarkable systemic review. A brain computerized tomography (CT) showed bilateral SDHs, for which he underwent bilateral mini craniotomies and drainage. The symptoms improved after surgery and the follow-up brain CT showed no recurrence.
Conclusion:
Idiopathic spontaneous bilateral SDH in the adult age group is an extremely rare pathology and the literature review only revealed three similar cases. With the absence of any pathology that would explain the presentation after extensive investigations, we hypothesized that a sudden rise in vascular pressure was the underlying etiology, especially with the fact that the symptoms became unbearable after the neck chiropractor therapy session.
Keywords: Bilateral subdural hematoma, Headache, Idiopathic, Nontraumatic

INTRODUCTION
Subdural hematoma (SDH) is one of the common pathologies in the field of neurosurgery, especially in the geriatric age group. Brain atrophy increases the space between the brain cortex and the skull, which causes the bridging veins to be stretched; therefore, it increases the probability of veins rupturing. Thus, the incidence of SDH is directly proportional to the space between the brain and the skull.[7,12] A literature review found the incidence rate of chronic SDH ranged between 8.2/100,000/year and 48/100,000/year with a 200–600% increase in the incidence rate over the past 50 years. In the absence of trauma history, SDH is considered spontaneous.[13] It has been suggested that spontaneous chronic SDH occurs due to trivial head injury in the presence of other cofactors such as brain atrophy, systemic hypertension, coagulopathy, alcohol consumption, anticoagulant medications, and intracranial hypotension.[1,5,7,12] Nontraumatic bilateral SDH in the middle-aged group is rare, and the literature is limited to sporadic case reports.[2,8,10] We report a rare case of an idiopathic spontaneous bilateral SDH in a 28-year-old male and present a literature review of similar cases of idiopathic spontaneous bilateral SDH in adult patients.
CASE DESCRIPTION
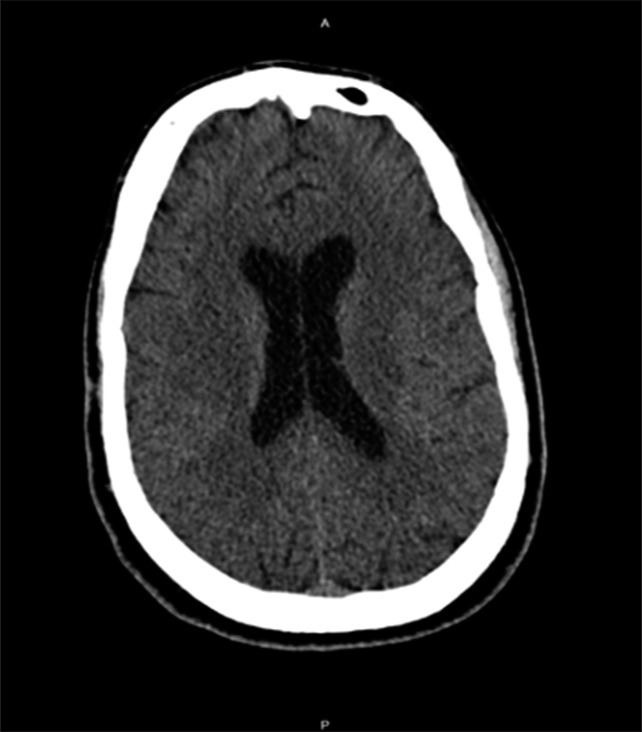
A 28-year-old fit male soldier was brought by his family to Emergency Department (ED) with a history of severe headache, neck pain, nausea, and vomiting, which were associated with behavioral changes in the past 2 days. His symptoms started 2 months ago after lifting a heavy object when he developed neck pain associated with a severe headache that increased in severity over time. He has visited the ED twice before this time, and he was only investigated by a cervical spine X-ray with no brain images; then, he was discharged on analgesia and an outpatient department clinic appointment. As his symptoms did not improve with time, he went to an uncertified chiropractor for neck pain, asking for a neck therapy session, after which his symptoms increased in severity. As the headache became unbearable after the therapy session, he went to a hospital and did a brain computerized tomography (CT) which showed bilateral SDH [Figures 1 and 2]. There was no history of trauma, loss of consciousness, or seizure. He was not on any chronic medications, anticoagulants, or antiplatelets. The patient had a negative history of bleeding tendency, no constitutional symptoms, and an unremarkable systemic review. He was a nonsmoker with no history of alcohol or drug abuse. He had a negative family history of a brain aneurysm and bleeding disorders. On assessment, he was vitally stable, afebrile, conscious, alert, and oriented; however, he looked depressed and agitated. He had an abnormal involuntary repetitive extension movement involving his little fingers bilaterally that started 2 days ago. The rest of the neurological examination was unremarkable. All laboratory investigations were normal. CT angiography, magnetic resonance angiography, and whole spine magnetic resonance imaging did not reveal any identifiable cause that would explain the SDH [Figures 3a, b and 4]. The patient underwent bilateral mini craniotomies with bilateral subdural drains [Figure 5]. A specimen of the SDH external membrane was sent for a histopathology examination, which revealed typical histological findings of the external membrane of the hematoma. The surgery went successfully with no complications or abnormal bleeding. His symptoms improved immediately after the surgery. During his hospital stay, further blood investigations (Blood smear,
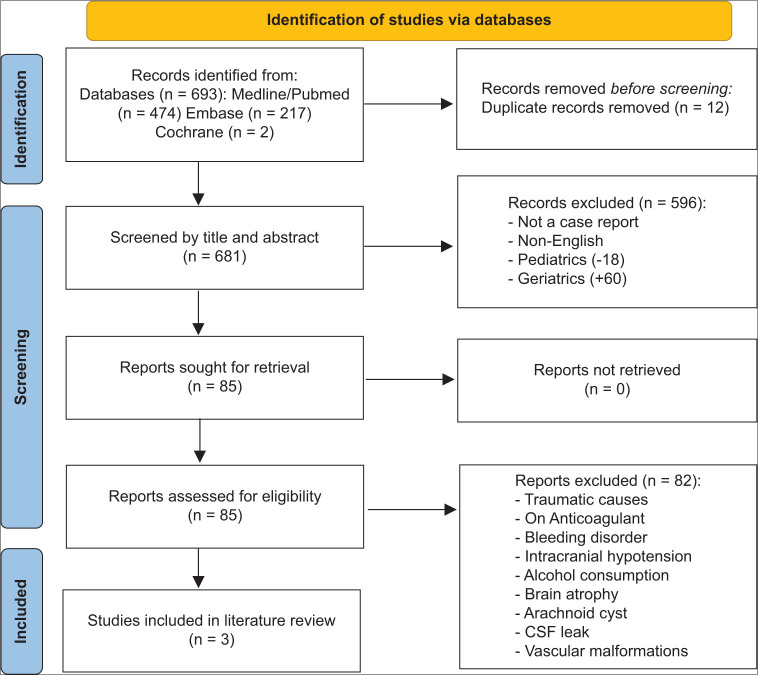
Figure 1:
(A) Preoperative coronal cut brain computerized tomography scan.
Figure 2:

Preoperative axial cut brain computerized tomography scan.
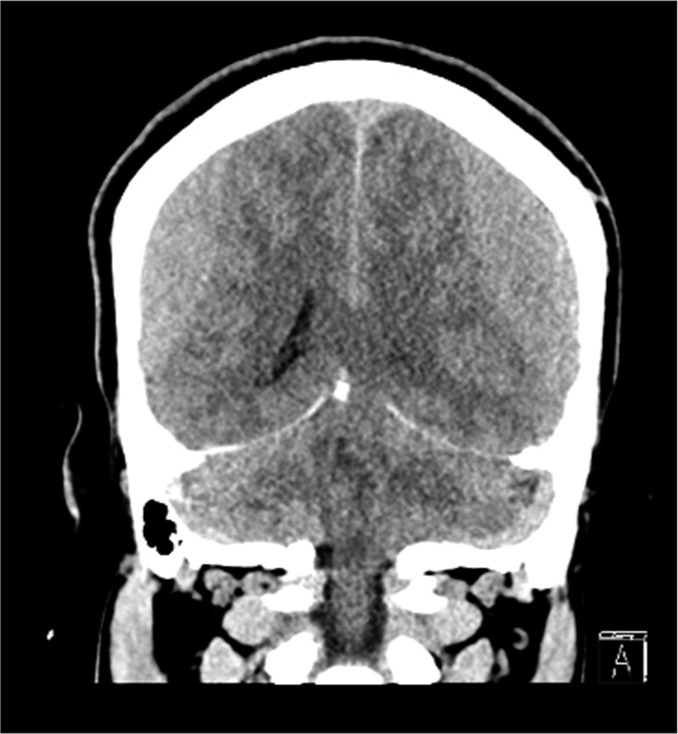
Figure 3:
(a) Preoperative axial cut brain magnetic resonance angiography. (b) Preoperative axial cut brain computerized tomography angiography.
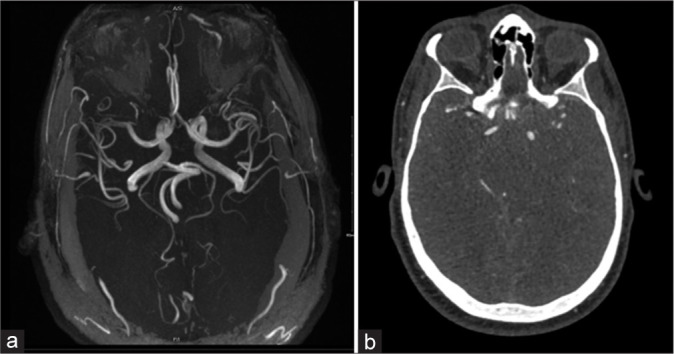
Figure 4:
Preoperative spine magnetic resonance imaging.
Figure 5:

Posoperative axial cut brain computerized tomography scan.
Factor VIII and XIII, and vWF cofactor and Antigen) were done and came within normal ranges. The psychiatry team was consulted, and he was diagnosed with major depressive disorder. Eventually, the patient was discharged home in stable condition and completely resolved symptoms on the 6th-day post-surgery. After 8 months, a follow-up brain CT scan was done, and it showed an interval resolution of the bilateral SDH with no signs of recurrence [Figure 6]. The patient had no recurrence of the clinical symptoms and was discharged from the clinic.
Figure 6:
Postoperative axial cut brain computerized tomography scan.
METHODS
We performed a literature review of idiopathic spontaneous SDH case reports in the databases: PubMed/Medline, Embase, and Cochrane utilizing the keywords: (Bilateral SDH) and (case report) in July 2022. The following keywords: Traumatic and spinal have been used to exclude further the unwanted articles and the language of the included articles was restricted to only articles written in English. A thorough literature review of the enrolled articles by two independent reviewers in duplicate was conducted in two steps, the first step involved screening the titles and abstracts, and the second step involved screening the full texts, and conflicts, if any, were handled by a third independent reviewer. Only case reports of idiopathic spontaneous bilateral SDH in patients aged between 18 and 60 who underwent full investigations to rule out any identifiable causes were included in the study. The case reports of bilateral SDH with identifiable causes such as trauma, anticoagulant therapy, vascular malformation, bleeding disorders, cerebrospinal fluid leak, intracranial hypotension, alcohol consumption, or brain atrophy were excluded from the study. After the full-text screening was completed, two independent authors in duplicate further conducted the data extraction. The extracted data involved the following variables: Author name, year of publication, age, gender, chronic conditions, presenting symptoms, medications, neurological examination findings, intervention, recurrence, and outcome. The descriptive statistics such as frequencies and percentages were then analyzed using John’s Macintosh project software version 15.0.
RESULTS
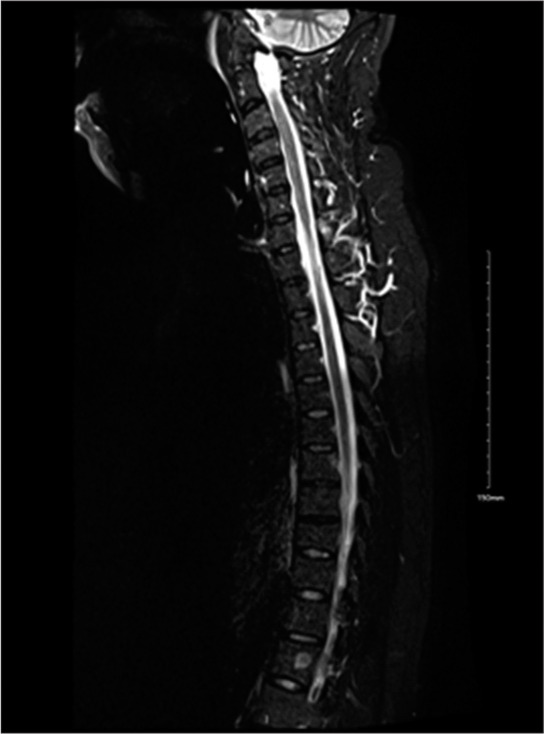
Initially, 693 articles were identified from the previously mentioned databases. After the full-text screening, only three case reports fit our criteria and they were included in this literature review [Table 1 and Figure 7]. The case reports had three male patients (100.00%), and their ages ranged from 28 to 55 years old. All the patients presented with headaches and other different symptoms (100.00%). For example, in Tasneem et al.,[9] case report, the patient presented also with oculomotor disorders (33.33%). In the neurological examinations on the presentation, only one case (33.33%) had a normal examination. The other two cases (66.66%) had some abnormalities in their neurological examinations such as diplopia, bilateral papilledema, and/or Babinski sign. Two patients (66.66%) were treated by bilateral burr hole evacuation, and 1 (33.33%) patient was treated by unilateral burr hole on one side, while the other side was treated conservatively. All the surgeries went uneventfully. There was no bleeding recurrence, and all three cases showed good outcomes with an improvement in symptoms (100.00%) [Table 1].
Table 1:
Synopsis of three cases of idiopathic spontaneous bilateral subdural hematoma in adults aged between 18 and 60 years old reported in the literature.
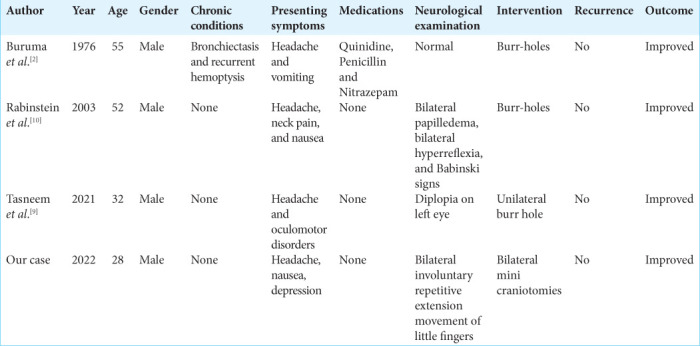
Figure 7:
Prisma chart of articles screening and selection
DISCUSSION
Spontaneous SDH is a common pathology in the geriatric age group, unlike in other age groups, where it is considered uncommon. There is enough data in the literature that suggests a relationship between some factors and the incidence of chronic SDH such as advanced age, high blood pressure, alcohol intake, use of blood thinners, and coagulopathies.[5,12] An analysis of 176 cases with chronic SDH in 2015 by Neto et al. showed that 37.7% of the patients had systemic hypertension, 19% were alcoholic, 9.6% were using antiplatelet agents, 7.5% had cerebrovascular diseases, and 6.2% had malignant neoplasms.[5] Another study done in 2012 by Sim et al. included 290 chronic SDH patients with an average of 63.94 ± 11.75 years old and a male-female ratio of 196:94. Out of the 290 cases, 21.0% were suffering from chronic alcoholism, 14.8% had hypertension, 10.3% were using either anticoagulants or antiplatelets, and 7.9% had coagulopathy.[12] There are other possible factors that could be related to spontaneous SDH and have been reported in multiple case reports such as intracranial hypotension, steroid intake, and arachnoid cyst.[1,4,6]
Spontaneous SDH in the middle age group usually occurs unilaterally with one or more of the predisposing factors mentioned above.[7,12] In the nongeriatric age group, extensive investigations should be conducted before labeling the case as a spontaneous idiopathic SDH. A study that performed a literature review on spontaneous SDH case reports found only 22 cases of patients <40-years-old, and all the cases had unilateral SDH. Out of the 22 cases, 6 (27.3%) had arterial causes, 5 (22.7%) were idiopathic, 4 (18.2%) were coagulopathic, and 4 (18.2%) had spontaneous intracranial hypotension.[3] Hence, spontaneous idiopathic bilateral SDH in the middle age group is an extremely rare pathology, the literature lacks data about its incidence and its associated risk factors. The symptoms of spontaneous idiopathic SDH are usually vague and not specific; in most cases, the diagnosis of the condition comes late after the severity of the symptoms worsened. The most common symptom is a persistent headache that worsens over time and is associated with nausea.[2,9,10] Several studies found a relationship between spontaneous SDH and the appearance of new or deterioration of pre-existing psychiatric illness, these studies were not included in the literature review, because the patients were either addicted to alcohol or had brain atrophy.[4,6] Furthermore, the same thing happened with our patient, who was diagnosed with major depressive disorder. Thus, screening such neurological conditions with neuroimaging is recommended in such cases.
The underlying pathophysiology is still not clearly understood; however, the anatomical nature of the bridging veins makes them more susceptible to rupture, as they lack the presence of any supporting reinforcement from the arachnoid in addition to their structural lack of elastic or muscular layers.[11] Furthermore, Yamashima and Friede’s study showed that subarachnoid veins share a uniform wall diameter of 50–200 um in addition to the fact that they obtain a dense reinforcement from the arachnoid trabecular cells; in contrast to the bridging veins, as they have different wall diameters and lack the volume of support from the arachnoid trabecular cells, and this makes them more prone to tearing and rupture.[14] In the light of these anatomic characteristics of the bridging veins with no apparent reason to explain their rupture and bleeding, such as brain atrophy, intracranial hypotension, or other previously mentioned reasons, we believe that the underlying cause of such presentation was a sudden rise in the pressure of the venous system, which led to veins rupture.
Some studies have proven that a sudden rise in vascular pressure leads to a defect in the blood-brain barrier, especially in the venules. An experimental study that was done by Mayhan and Heistad demonstrated a marked venules dilatation and blood–brain barrier disruption after acute arterial hypertension and superior vena cava occlusion.[8] This is a rational explanation for the incidence in our case as the symptoms appeared after the patient underwent a chiropractic session by a noncertified person for the neck area, which led to a sudden rise in the venous system pressure which, in turn, was responsible for the presented sequelae. The validity of this belief is reinforced by the fact that the bleeding occurred on both sides, with the absence of any pathology that would explain the event after the extensive conducted investigations.
Limitations
This study has some limitations as the included literature evidence is only provided by case reports; therefore, it affects the quality of the study. However, considering how rare idiopathic spontaneous bilateral SDH in adults is, this study provides the best and latest evidence in the literature. Further studies to help understand the underlying causes and mechanisms of idiopathic spontaneous bilateral SDH in adults are recommended.
CONCLUSION
Spontaneous idiopathic bilateral SDH is an extremely rare pathology in the young age group. It is a diagnosis of exclusion with a favorable outcome. It must be included in the differential diagnosis for unexplained persistent neurological or psychiatric deterioration.
Footnotes
How to cite this article: Algahtani AY, Alghamdi AM, Ashqar A, Basurrah AA, Alzahrani M. Idiopathic spontaneous bilateral subdural hematoma in a 28-year-old male: A comprehensive literature review and case report. Surg Neurol Int 2023;14:130.
Contributor Information
Abdulhadi Y. Algahtani, Email: gahtaniay@gmail.com.
Abdulaziz M. Alghamdi, Email: abdulazizmahdigh@gmail.com.
Alaa Ashqar, Email: ashqaradelalaa@gmail.com.
Abdulaziz Abdullah Basurrah, Email: abdulazizBasurrah@hotmail.com.
Moajeb Alzahrani, Email: Dr_alzahrani@hotmail.com.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
REFERENCES
- 1.Alaraj AM, Chamoun RB, Dahdaleh NS, Haddad GF, Comair YG. Spontaneous subdural haematoma in anabolic steroids dependent weight lifters: Reports of two cases and review of literature. Acta Neurochir (Wien) 2005;147:85–7. doi: 10.1007/s00701-004-0415-0. discussion 87-8. [DOI] [PubMed] [Google Scholar]
- 2.Buruma OJ, Sande JJ. Bilateral acute spontaneous subdural hematoma. A case report. Clin Neurol Neurosurg. 1976;79:211–4. doi: 10.1016/s0303-8467(76)80052-2. [DOI] [PubMed] [Google Scholar]
- 3.Coombs JB, Coombs BL, Chin EJ. Acute spontaneous subdural hematoma in a middle-aged adult: Case report and review of the literature. J Emerg Med. 2014;47:e63–8. doi: 10.1016/j.jemermed.2014.04.026. [DOI] [PubMed] [Google Scholar]
- 4.Erkulvrawatr S, Srinivasan G. Complete spontaneous resolution of bilateral subdural hematoma. South Med J. 1978;71:456–8. doi: 10.1097/00007611-197804000-00030. [DOI] [PubMed] [Google Scholar]
- 5.Farhat Neto J, Araujo JL, Ferraz VR, Haddad L, Veiga JC. Chronic subdural hematoma: Epidemiological and prognostic analysis of 176 cases. Rev Col Bras Cir. 2015;42:283–7. doi: 10.1590/0100-69912015005003. [DOI] [PubMed] [Google Scholar]
- 6.Kar SK, Kumar D, Singh P, Upadhyay PK. Psychiatric manifestation of chronic subdural hematoma: The unfolding of mystery in a homeless patient. Indian J Psychol Med. 2015;37:239–42. doi: 10.4103/0253-7176.155656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kostić A, Kehayov I, Stojanović N, Nikolov V, Kitov B, Milošević P, et al. Spontaneous chronic subdural hematoma in elderly people-Arterial hypertension and other risk factors. J Chin Med Assoc. 2018;81:781–6. doi: 10.1016/j.jcma.2018.03.010. [DOI] [PubMed] [Google Scholar]
- 8.Mayhan WG, Heistad DD. Role of veins and cerebral venous pressure in disruption of the blood-brain barrier. Circ Res. 1986;59:216–20. doi: 10.1161/01.res.59.2.216. [DOI] [PubMed] [Google Scholar]
- 9.Mohamed T, Swed S, Al-Mouakeh A, Sawaf B. Nontraumatic bilateral subdural hematoma: Case report. Ann Med Surg (Lond) 2021;71:102907. doi: 10.1016/j.amsu.2021.102907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rabinstein AA, Pittock SJ, Miller GM, Schindler JJ, Wijdicks EF. Pseudosubarachnoid haemorrhage in subdural haematoma. J Neurol Neurosurg Psychiatry. 2003;74:1131–2. doi: 10.1136/jnnp.74.8.1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Scranton RA, Evans RW, Baskin DS. A motion simulator ride associated with headache and subdural hematoma: First case report. Headache. 2016;56:372–8. doi: 10.1111/head.12717. [DOI] [PubMed] [Google Scholar]
- 12.Sim YW, Min KS, Lee MS, Kim YG, Kim DH. Recent changes in risk factors of chronic subdural hematoma. J Korean Neurosurg Soc. 2012;52:234–9. doi: 10.3340/jkns.2012.52.3.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stubbs DJ, Vivian ME, Davies BM, Ercole A, Burnstein R, Joannides AJ. Incidence of chronic subdural haematoma: A single-centre exploration of the effects of an ageing population with a review of the literature. Acta Neurochir (Wien) 2021;163:2629–37. doi: 10.1007/s00701-021-04879-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Yamashima T, Friede RL. Why do bridging veins rupture into the virtual subdural space? J Neurol Neurosurg Psychiatry. 1984;47:121–7. doi: 10.1136/jnnp.47.2.121. [DOI] [PMC free article] [PubMed] [Google Scholar]