Abstract
Background:
Lumbar drain (LD) placement can be a difficult procedure leading to postprocedure complications, particularly in patients with persistent cerebrospinal fluid leaks or a large body habitus. The objective of this technical case report is to describe the use of Medtronic’s SureTrak Navigation system for navigated LD placement.
Case Description:
The patient was an 18-year-old morbidly obese male who initially underwent a suboccipital craniectomy with duraplasty and a C1 laminectomy for Chiari Malformation. Postoperatively, he developed a pseudomeningocele and was taken to the operating room for wound revision, duraplasty repair, and LD placement. Medtronic’s SureTrak Navigation system was used for LD placement before wound revision. Successful LD placement was achieved in a single pass using the SureTrak Navigation. The patient did well postoperatively, and LD removal occurred on postoperative day 6. The patient was discharged in good condition without evidence of a cerebral spinal fluid leak.
Conclusion:
Navigation using the SureTrak system is a reasonable option to use in patients with a high body mass index and a persistent cerebrospinal fluid leak. When the patient is already undergoing an operative procedure, it can aid in an efficient low-risk intervention completed in a single prone positioning.
Keywords: Cerebrospinal fluid leak, Cerebrospinal fluid, Lumbar drain, Medtronic SureTrak, Navigation, Neurosurgery

INTRODUCTION
Lumbar cerebrospinal fluid (CSF) access is critical for the management and treatment of neurosurgical conditions. Lumbar access including both punctures and drains is often indicated for diagnostic workup to evaluate CSF, to treat diseases complicated by hydrocephalus, and to aid in cranial procedures to prevent the development of CSF fistulas and the need for brain retraction.[2] Lumbar drains (LDs) are second-line therapy for iatrogenic CSF leaks.[5,7,10] Understandably, accessing the lumbar space comes with its own set of risks that should be weighed against the benefits of performing the procedure. One of the most common and major risks is CNS infection.[1,2] Meningitis occurs about 5–20% of the time in patients with LDs. Furthermore, the duration of catheter placement and frequency of CSF sampling are known independent risk factors for developing meningitis.[2,8] Other LD complications consist of low-pressure headaches and pneumocephalus from dynamic changes in CSF flow rates, blockage and misplacement of the catheter, nerve root injury, post removal CSF leak, subdural hematoma formation, and brain herniation.[1,2] To mitigate these complications, standardized practices for LD placement have been established; however, these practices are often hospital dependent and not universally followed.
LDs are typically placed at bedside or intraoperatively. In each situation, sterile technique is used with a designated LD toolkit. Yet, placement of the needle and catheter is performed blindly by the proceduralist. This blind approach introduces additional risks for the patient when multiple attempts are required. Multiple attempts at insertion can damage the dura and adjacent structures leading to unnecessary pain and distress for the patient, increased infection rate, extended length of the procedure, and potentially lasting neurological deficits.[2] Therefore, techniques to ensure limited attempts at LD placement should be investigated. In this report, we describe the utilization of Medtronic’s SureTrak system for navigated LD placement. No patient consent was obtained for this case report considering no identifiable patient information is provided. However, the patient did consent to the operation and navigated LD placement procedure. The Institutional Review Board approval was not obtained based on similar aforementioned reasons.
CASE DESCRIPTION
Navigation systems provide a reasonable adjunct for LD placement, particularly in cases, in which the patient is already going to the operating room for a concurrent CSF leak repair and in cases, where factors make LD placement a high-risk procedure, such as body habitus.
We utilize the Medtronic SureTrak system in patients undergoing CSF leak repair in the operating room. Patients are placed in the prone position and the reference frame is either secured with Ioban over the bony prominences of the thoracic spine, with care taken not to move the frame or patient during the procedure, or secured to the Mayfield headframe, if it is being used in the procedure. The optical array is placed at the head of the patient’s bed, facing the procedure field. An O-arm spin is completed and the SureTrak frame is then registered to the top portion of the spinal needle, ensuring the bevel and the frame are facing the head of the bed and optical array. The needle is tested on several anatomical points to ensure accuracy and LD placement is completed in typical fashion.[8]
CASE EXAMPLE
The patient was an 18-year-old male who was morbidly obese with a body mass index (BMI) of 46. He initially underwent a suboccipital craniectomy with duraplasty and a C1 laminectomy for Chiari Malformation and associated cervicothoracic syrinx. Postoperatively, he developed a pseudomeningocele with incisional drainage and was subsequently taken to the operating room for wound revision, duraplasty repair, and concurrent LD placement. The patient was placed in the prone position and the navigation reference frame was secured with Ioban over the thoracic spine [Figure 1]. Medtronic’s SureTrak was, then, registered to the spinal needle and used for LD placement before wound revision [Figure 2]. Successful LD placement was achieved in a single pass using SureTrak navigation [Figure 3]. The patient did well postoperatively, and the LD was removed on post-operative day 6. The patient was discharged in good condition without evidence of cerebral spinal fluid leak.
Figure 1:
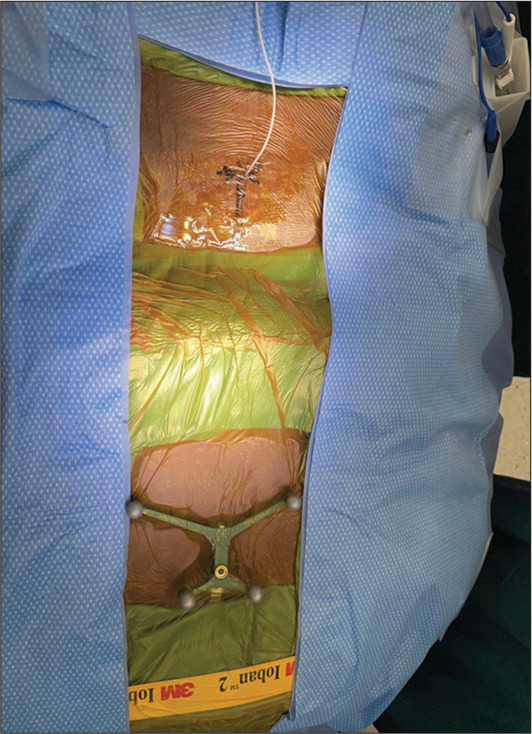
Patient and navigation setup. The patient was placed in the prone position and Ioban was used to secure the navigation reference frame over the thoracic spine.
Figure 2:
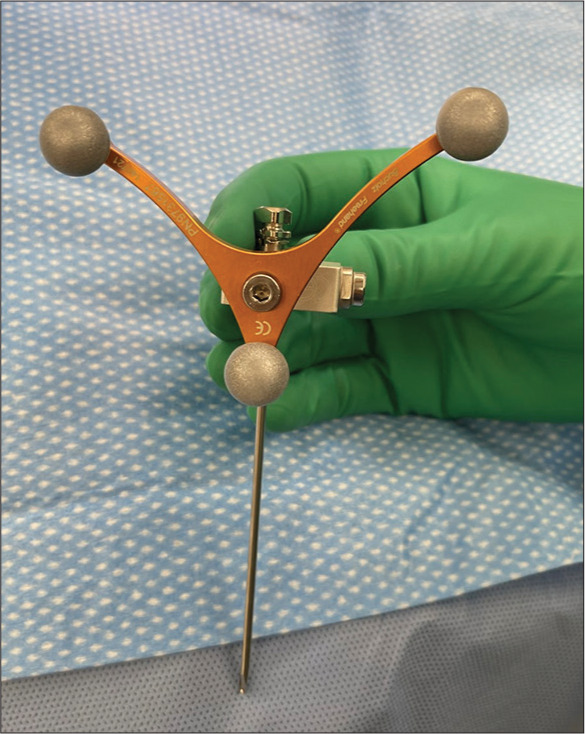
Navigation probe registration. Medtronic SureTrak Navigation system was registered to the Tuohy spinal needle using the navigation probe as depicted for lumbar drain placement.
Figure 3:
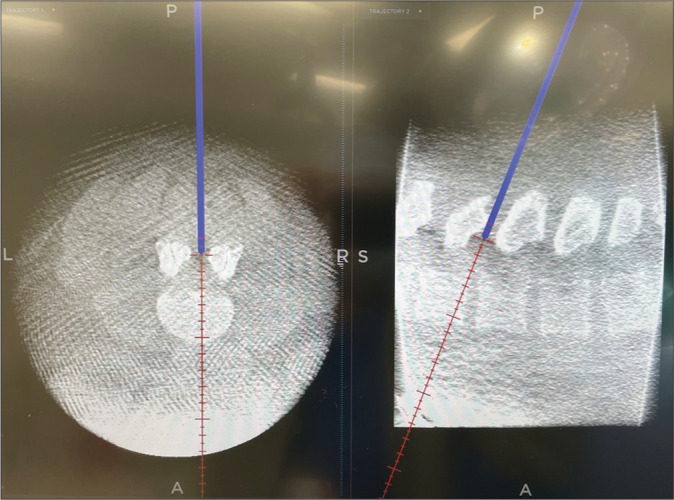
Navigation-guided computerized topography (CT) images. Lumbar CT images illustrate the use of the Medtronic SureTrak Navigation system allowing for successful lumbar drain placement. The left image shows an axial view. The right image shows a sagittal view.
DISCUSSION
An approach that may reduce the complications of LD insertion associated with multiple attempts is navigation. Especially in cases, where additional factors make LD placement a high-risk procedure like patient body habitus, utilizing a navigation-guided technique would be preferred. However, these navigation-guided approaches have not been reported for LD placement to our knowledge. In this report, we describe a case where we utilized Medtronic’s SureTrak system for navigated LD placement in an 18-year-old morbidly obese patient who developed a post-operative pseudomeningocele following a suboccipital craniectomy and a C1 laminectomy.
Postoperative pseudomeningoceles in the setting of CSF leaks and dural tears are the most common complication of posterior fossa decompression for Chiari malformation given the risk profile for CSF leaks is greater than other intradural spine procedures.[6,9] If dural tears and CSF leaks go unnoticed or re-open after closure, secondary management consists of reparative operations such as epidural blood patches (EBP) and less invasive procedures like LD placement. These procedures are used as a standalone or in conjunction with direct dural repair. Unlike LD placement, a guided approach for lumbar spine access for EBP placement has been described in the literature. Studies describing ultrasound-guided and O-arm navigation EBP treatment have shown good success rates with limited associated risk of radiation compared to other fluoroscopic techniques.[11,12] However, radiation exposure is still a concern for both patient and operator even with O-arm use during a computerized tomography (CT)-guided approach for LD placement. Costa et al. reported a mean dose of 0.005 µSv for O-arm operators in spinal surgeries and a mean dose of 5.15 mSv for patients.[4] Moreover, when comparing a CT guided and fluoroscopic guided approach, a study found that the CT approach had a lower average effective radiation dose; yet, this was not a statistically significant difference.[3] While the levels of radiation are below the recommendation for occupational radiation exposure, optimization of CT and fluoroscopic guided techniques or use of alternatives can further reduce radiation exposure.[4] Radiation considerations are particularly important for radiologists who frequently perform LD placement under fluoroscopy. Ultimately in describing our experience using the SureTrak navigation technique for LD placement, we hope to highlight an effective method that may reduce complication rates of LD and avoid radiation exposure of other navigation techniques.
Limitations
There are a few limitations to our technical case report. First, we only describe a single case example using the navigation SureTrak system for LD placement. Additional case series and comparative effectiveness studies evaluating SureTrak LD navigation to other LD placement techniques are needed to determine superiority. Second, the SureTrak system has its own drawbacks. There is potential for inaccuracy since the SureTrak reference frame is attached to the patient’s thoracic spine, a non-ridge object. Care should be taken to ensure the frame is not moved after the use of the O-arm. However, this is of little concern since the procedure is short and does not involve manipulation. In addition, procedural time and cost can increase with use of the O-arm spin especially if the patient was not originally scheduled for an operating room procedure. Still, we believe that the SureTrak navigation LD placement technique is a viable and likely time saving option for cases with known or perceived challenges.
CONCLUSION
Navigation using the SureTrak system is a reasonable option to use in patients with high BMI and persistent CSF leak. When the patient is already undergoing an operative procedure, it can aid in an efficient intervention completed in a single prone positioning.
Footnotes
How to cite this article: Montgomery CT, Blue R, Spadola M, Ajmera S, Jabarkheel R, Schuster J. Navigated lumbar drain placement: A description of technique and case example. Surg Neurol Int 2023;14:116.
Contributor Information
Canada T. Montgomery, Email: canada.montgomery@pennmedicine.upenn.edu.
Rachel Blue, Email: rachel.blue@pennmedicine.upenn.edu.
Michael Spadola, Email: michael.spadola@pennmedicine.upenn.edu.
Sonia Ajmera, Email: sonia.ajmera@pennmedicine.upenn.edu.
Rashad Jabarkheel, Email: rashad.jabarkheel@pennmedicine.upenn.edu.
James Schuster, Email: james.schuster@pennmedicine.upenn.edu.
Declaration of patient consent
Patient’s consent not required as patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Disclaimer
The views and opinions expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Journal or its management. The information contained in this article should not be considered to be medical advice; patients should consult their own physicians for advice as to their specific medical needs.
REFERENCES
- 1.Açikbaş SC, Akyüz M, Kazan S, Tuncer R. Complications of closed continuous lumbar drainage of cerebrospinal fluid. Acta Neurochir (Wien) 2002;144:475–80. doi: 10.1007/s007010200068. [DOI] [PubMed] [Google Scholar]
- 2.Bakhshi SK, Suhail N, Mitha R, Moazzam M, Zahid N, Shamim MS. Lumbar drain for temporary cerebrospinal fluid diversion: Factors related to the risks of complications at a university hospital. World Neurosurg. 2020;143:e193–8. doi: 10.1016/j.wneu.2020.07.120. [DOI] [PubMed] [Google Scholar]
- 3.Brook AD, Burns J, Dauer E, Schoendfeld AH, Miller TS. Comparison of CT and fluoroscopic guidance for lumbar puncture in an obese population with prior failed unguided attempt. J Neurointerv Surg. 2014;6:324–8. doi: 10.1136/neurintsurg-2013-010745. [DOI] [PubMed] [Google Scholar]
- 4.Costa F, Tosi G, Attuati L, Cardia A, Ortolina A, Grimaldi M, et al. Radiation exposure in spine surgery using an image-guided system based on intraoperative cone-beam computed tomography: Analysis of 107 consecutive cases [published correction appears in J Neurosurg Spine 2017;26:542] J Neurosurg Spine. 2016;25:654–9. doi: 10.3171/2016.3.SPINE151139. [DOI] [PubMed] [Google Scholar]
- 5.Deen HG, Pettit PD, Sevin BU, Wharen RE, Reimer R. Lumbar peritoneal shunting with video-laparoscopic assistance: A useful technique for the management of refractory postoperative lumbar CSF leaks. Surg Neurol. 2003;59:473–8. doi: 10.1016/s0090-3019(03)00165-4. discussion 477-8. [DOI] [PubMed] [Google Scholar]
- 6.De Tommasi C, Bond AE. Complicated pseudomeningocele repair after chiari decompression: Case report and review of the literature. World Neurosurg. 2016;88:688.e1–7. doi: 10.1016/j.wneu.2015.11.056. [DOI] [PubMed] [Google Scholar]
- 7.Lee YM, Ordaz A, Durcanova B, Viner JA, Theodosopoulos PV, Aghi MK, et al. Cerebrospinal fluid leaks and pseudomeningocele after posterior fossa surgery: Effect of an autospray dural sealant. Cureus. 2020;12:e8379. doi: 10.7759/cureus.8379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Moza K, McMenomey SO, Delashaw JB., Jr Indications for cerebrospinal fluid drainage and avoidance of complications. Otolaryngol Clin North Am. 2005;38:577–82. doi: 10.1016/j.otc.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 9.Sellin JN, Kolcun JP, Levi AD. Cerebrospinal fluid leak and symptomatic pseudomeningocele after intradural spine surgery. World Neurosurg. 2018;120:e497–502. doi: 10.1016/j.wneu.2018.08.112. [DOI] [PubMed] [Google Scholar]
- 10.Slavnic D, Mccabe R, Tong D, Soo TM. Repair of postoperative cervical pseudomeningocele with the use of bone morphogenetic protein. Cureus. 2019;11:e5200. doi: 10.7759/cureus.5200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Takai K, Taniguchi M. Targeted epidural blood patch under o-arm-guided stereotactic navigation in patients with intracranial hypotension associated with a spinal cerebrospinal fluid leak and ventral dural defect. World Neurosurg. 2017;107:351–7. doi: 10.1016/j.wneu.2017.07.168. [DOI] [PubMed] [Google Scholar]
- 12.West JL, De Biase G, Abode-Iyamah K, Nottmeier EW, Deen HG, Chen SG, et al. Initial results of precision treatment of postoperative cerebrospinal fluid leak with ultrasound-guided epidural blood patch. World Neurosurg. 2021;153:e204–12. doi: 10.1016/j.wneu.2021.06.090. [DOI] [PubMed] [Google Scholar]


