Abstract
Objective. The purpose of this study was to extend our understanding of escape room pedagogical design by investigating the impact of escape room puzzle content on changes in students’ immediate recall knowledge and demonstration of interprofessional skills during a subsequent simulation.
Methods. Students from nursing, pharmacy, and physical therapy programs were randomized to complete an escape room themed around acute management of sepsis (intervention group; n=133) or general acute care (control group; n=129) prior to participating in a simulated patient discharge case conference. Students completed a knowledge assessment before the escape room, immediately after the escape room, and immediately after the simulation. Additionally, students completed the Interprofessional Socialization and Valuing Scale (ISVS-21) before and after the experience along with a post-program evaluation. Faculty rated student achievement of interprofessional learning objectives during the simulation using a standardized rubric.
Results. Students in the intervention group had higher scores on the knowledge test administered immediately after the escape room. All participants’ ISVS-21 scores increased from before to after the activity. Interprofessional learning objectives, as evaluated by faculty, were met by 248 (94.7%) students.
Conclusion. Participating in an interprofessional escape room activity with specific puzzle content improved students’ immediate recall knowledge. In both groups, self-assessed interprofessional socialization improved, and a high percentage of students achieved the interprofessional learning objectives in a subsequent simulation. Escape rooms can be an innovative pedagogical tool that can positively impact immediate recall knowledge and interprofessional collaborative skills of health professions students.
Keywords: interprofessional education, educational game, escape room, students
INTRODUCTION
Health professions programs continue to develop novel approaches to interprofessional education to ensure students graduate proficient in the Interprofessional Education Collaborative’s core competencies for interprofessional collaborative practice.1,2 Learning experiences commonly used to develop these competencies include interprofessional small group case discussions, simulation-based learning experiences, and clinical collaborative practice experiences.3-5 However, interprofessional learning experiences with the goal of developing knowledge, in addition to communication and teamwork skills, continue to evolve.
Recently, escape rooms have become popular in health professions education as an active-learning strategy and are associated with improved knowledge and skill acquisition as compared to traditional educational strategies.6,7 Despite the growing popularity of escape rooms, many reports rely on student satisfaction and single-group preactivity-postactivity knowledge assessments.8-14 These data are limited by small sample sizes and a lack of randomization. Furthermore, escape rooms are often standalone experiences that do not objectively evaluate student performance of interprofessional skills relevant to the clinical setting.
Given the lack of quality and pedagogical standards for health professions escape room design and assessment, the purpose of this study was to extend our understanding of escape room pedagogical design by investigating the impact of an escape room on students’ immediate recall knowledge and ability to demonstrate interprofessional collaboration during a subsequent, clinically relevant, simulated interprofessional patient discharge conference. We hypothesized that an escape room with specific puzzle content focused on a theme would improve students’ immediate recall knowledge of that theme. Additionally, we hypothesized that irrespective of the puzzle content, students would demonstrate interprofessional collaborative skills during the simulation.
METHODS
This activity, conducted in fall 2019, was required for senior nursing, third-year pharmacy, and second-year physical therapy students. These cohorts were chosen as they were at similar stages of professional and clinical experience. Students earned credit for this activity in a required course. The activity included asynchronous online learning (one hour) about sepsis management and postoperative hip precautions prior to the in-person activity, which consisted of the escape room and simulation. These topics were selected because students from each respective program had exposure to them. The online learning was curated by program faculty, and students accessed it independently approximately one week prior to the activity. The in-person activity took place in the School of Nursing Simulation Center at a mutually convenient time. Students were divided into teams of two pharmacy, two nursing, and one physical therapy student. Student teams were randomly assigned to either the intervention or control group and had 30 minutes to complete the escape room.
To assess the impact of the escape room puzzles (ie, the independent variable) on immediate recall knowledge, two separate escape rooms were designed. The intervention escape room included puzzles focused on the theme of sepsis management and postoperative precautions for patients following total hip arthroplasty. For example, a puzzle in the intervention escape room challenged students to interpret a contact precautions policy for a patient with a positive blood culture (methicillin-resistant Staphylococcus aureus), which directly related to the theme of sepsis management. The control escape room included puzzles focused on general knowledge of acute care practice but did not relate to the theme of sepsis management and postoperative precautions.
After participating in the escape room, students completed the simulated patient discharge conference. They were tasked with creating and discussing an interprofessional discharge plan for an individual leaving an acute care facility following total hip arthroplasty complicated by sepsis. Students were given a patient chart and had 15 minutes to develop the plan and 15 minutes to educate the patient. A standardized actor, trained by faculty, played the role of the patient. Then the standardized actor and a faculty member moderated a reflection-based debriefing using the plus-delta debriefing framework, consistent with best practices for interprofessional simulation.15,16
This study collected and analyzed three student self-reported data sources (a knowledge test, the Interprofessional Socialization and Valuing Scale [ISVS-21], and a post-program evaluation), and one faculty-reported data source (the Modified McMaster-Ottawa Scale). The knowledge test was an investigator-developed, 10-item multiple choice test on sepsis management and postoperative hip precautions. The knowledge test was administered to all students on paper at three different time points: the first was administered immediately prior to the escape room (baseline knowledge), the second was administered immediately after the escape room, and the third immediately after the simulation.
The ISVS-21 self-assesses interprofessional socialization among students and health practitioners and their readiness to function in interprofessional teams.17 The reliability and validity of the instrument has been examined with a variety of health professionals with evidence supporting using the instrument before and after interprofessional education interventions.17 The ISVS-21 consists of 21 items using a seven-point Likert-type scale. Item scores are added together and divided by 21 to obtain an overall score.
The anonymous post-program evaluation consisted of six items. Four items asked students to rate their level of agreement that the activity met the learning objectives using a five-point Likert-type scale (1=strongly disagree, 2=disagree, 3=neutral, 4=agree, and 5=strongly agree). Data for these four items were reported as the frequency of respondents that selected agree or strongly agree. The remaining two evaluation items were optional, open-ended questions that asked students what about this learning experience they enjoyed most and what would improve this learning experience. Responses were analyzed by two individuals using a thematic analysis, a method commonly used in qualitative research studies.18 The number and percentage of responses coded for each theme were computed, and examples were collected.
Faculty rating of individual students occurred during the simulated patient discharge conference using a four-item rubric. The rubric, adapted from the Modified McMaster-Ottawa Scale, which assesses individual student performance in interprofessional teams,19 consisted of four items assessed on a met-not met scale that mirrored the Interprofessional Education Collaborative’s core competency domains of values and ethics, roles and responsibilities, communication, and teamwork.1,2
All statistical tests were conducted using Statistical Package for Social Science (SPSS) version 26 software (IBM Corp). For all statistical tests, p<.05 was considered statistically significant. The University at Buffalo Institutional Review Board reviewed and approved this study.
RESULTS
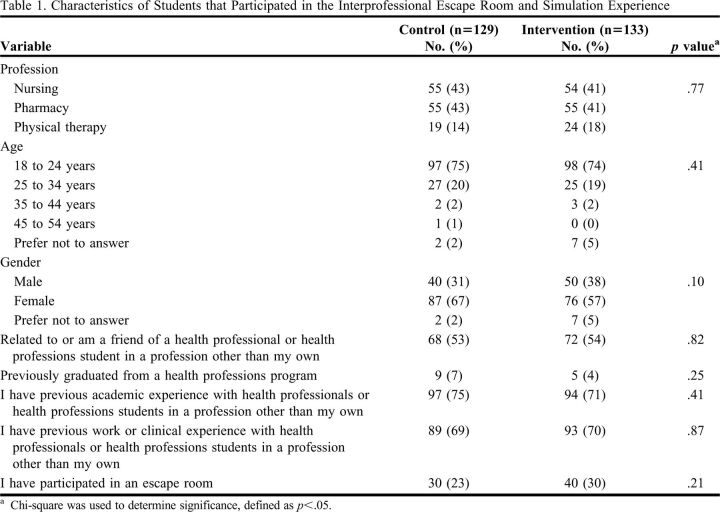
Of the 262 students who participated in the activity, 129 were in the control group and 133 were in the intervention group. Characteristics were similar between groups (Table 1). Forty-two (33%) students (eight groups) in the control group and 67 (50%) students (14 groups) in the intervention group successfully escaped the room (p=.003).
Table 1.
Characteristics of Students that Participated in the Interprofessional Escape Room and Simulation Experience
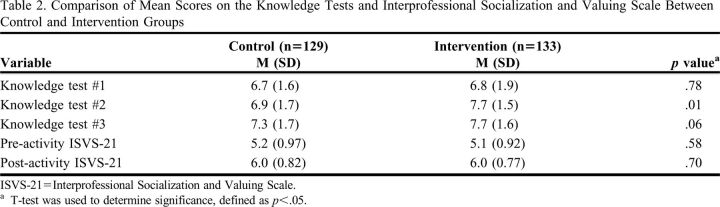
Prior to the escape room activity, students in both groups correctly answered a mean (SD) of 6.7 (1.8) questions correctly (Table 2). For participants in the intervention group, a significant increase in mean score occurred between knowledge test 1 and 2 (p<.01) and between knowledge test 1 and 3 (p<.01) but not between knowledge test 2 and 3 (p>.99). For participants in the control group, a significant increase in mean score occurred between knowledge test 1 and 3 (p<.01) and knowledge test 2 and 3 (p=.003) but not between knowledge test 1 and 2 (p=.09).
Table 2.
Comparison of Mean Scores on the Knowledge Tests and Interprofessional Socialization and Valuing Scale Between Control and Intervention Groups
Prior to the activity, participants in both groups responded that they displayed, on average, the interprofessional beliefs, behaviors, and attitudes on the ISVS-21 to a “fairly great extent” (mean [SD]: 5.1 [0.9]; Table 2). Following the activity, ISVS-21 scores increased similarly in both groups (control: 0.85 [1.3]; intervention: 0.96 [1.2]; p=.51) to a mean response of “to a great extent” (6.0 [0.8]).
A total of 248 (94.7%) students met the interprofessional collaboration criteria as evaluated by faculty. There was no difference in the frequency of students that met the learning criteria between the control (95%) and intervention (94%) groups (p=.38).
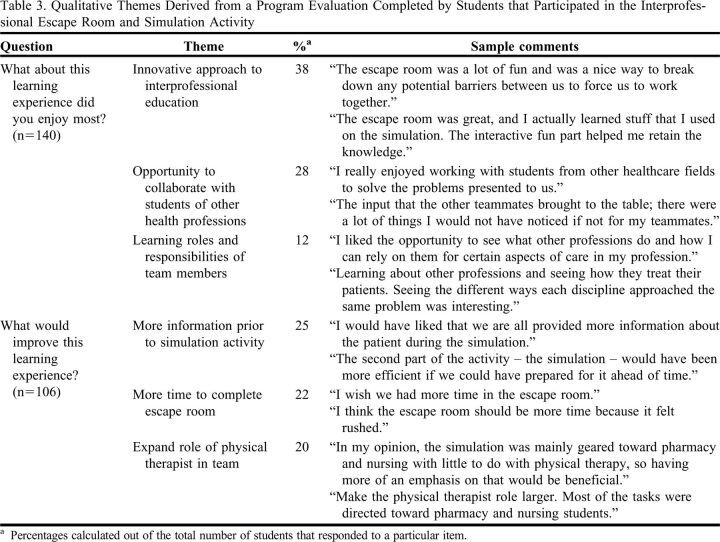
Overall, this learning activity was rated highly by participants (n=156; response rate: 60%). The frequency of students that responded “agree” or “strongly agree” with each evaluation rating item were as follows: Overall, 90% indicated that the escape room was an effective way to develop interprofessional teamwork skills; 79% indicated that the simulation (case conference) was an effective way to develop interprofessional collaboration skills; 85% indicated that learning experiences like this are important to their professional development; and 79% indicated that learning experiences like this should be a required part of their interprofessional education. The qualitative analysis (Table 3) revealed three major themes for each question.
Table 3.
Qualitative Themes Derived from a Program Evaluation Completed by Students that Participated in the Interprofessional Escape Room and Simulation Activity
DISCUSSION
Participating in an interprofessional escape room with puzzles focused on a theme improved students’ immediate recall knowledge of that theme, and this recall was sustained during simulation. Conversely, participation in an interprofessional escape room with general knowledge puzzles (ie, not related to a theme) resulted in no improvement in immediate recall knowledge of that theme. However, participation in the simulation resulted in an increase in these (control group) students’ knowledge to a point that was not different from the intervention group. Students demonstrated significant increases in interprofessional socialization, and a high percentage of all students successfully met the interprofessional collaboration criteria as evaluated by faculty during the simulation. Based on these findings, an escape room paired with a contextually relevant simulation may be an effective pedagogical tool to enhance students’ immediate recall knowledge while positively impacting their socialization with other students and health practitioners and their readiness to function in interprofessional teams.
In a prior study, pharmacy student participation in diabetes-themed escape rooms was found to increase immediate but not delayed post-activity knowledge, suggesting that knowledge gained through the escape experience may not be retained.12 Our study did not include a delayed post-activity assessment, but our findings of an increase in immediate recall knowledge are consistent with these data. Our data add to the existing literature by including students from multiple health professions programs, where data are lacking.
Qualitative feedback identified that students learned from each other during the experiences. A comment reflective of this was, “I think it was well planned. In terms of the three pre, mid and post quizzes we did, depending on what I heard my group member say during the escape room or even the simulation activity, some of my answers changed. So, I like how the activities were connected.” This comment supports the premise that they were learning about, from, and with each other.20
All students, regardless of which escape room they were randomized to, experienced an increase in self-assessed interprofessional socialization. Previous studies examining interprofessional escape rooms on student attitudes found that students reported that their teams understood their roles and responsibilities, listened to each other, and that their individual opinions were valued.21,22 Our study is similar, but it enhances these existing data by adding the assessment of knowledge gained during the experience while also analyzing two other important sources of data: namely student self-assessed interprofessional socialization through a validated instrument17 and faculty assessment of individual student performance within a team using the Modified McMaster-Ottawa Scale.19 These data complement the findings of knowledge gained by students by also revealing that students’ self-assessed ability to engage in interprofessional teamwork improved and that a high percentage of students achieved the interprofessional learning objectives as rated by observing faculty.
Our data support the use of an escape room to increase students’ knowledge related to a specific theme. Our study strengthens existing escape room pedagogy literature by using a large sample size, including students from different health professions programs, providing a comparison between participation in an intervention or control (sham) escape room, and employing random group assignment. The observed group differences in mean knowledge test scores directly after the escape room likely reflect the knowledge gained through the themed escape room experience.
There were several limitations to this study. The program evaluation data revealed there were opportunities for improvement with the activities. Specifically, the physical therapy students commented that the physical therapist role was not as robust compared to the pharmacist and nurse roles. A high percentage of students achieved the interprofessional collaboration criteria evaluated by faculty. However, we did not objectively assess interprofessional competencies prior to the simulation experience. The experience included pharmacy, nursing, and physical therapy students only and, thus, could be enhanced by expanding the number of professions involved, including student prescribers. Lastly, the outcomes were evaluated immediately after the activity. The long-term impact of experiences such as this should be further studied.
CONCLUSION
An interprofessional escape room with specific puzzle content improved students’ immediate recall knowledge. Self-assessed interprofessional socialization improved, and faculty assessments showed that most students had attained interprofessional collaboration criteria during the simulation, irrespective of the puzzle content of the escape room. Escape rooms can be an innovative pedagogical tool that can positively impact immediate recall knowledge and interprofessional skills of students from multiple health professions programs.
REFERENCES
- 1.Interprofessional Education Collaborative Expert Panel. Core competencies for interprofessional collaborative practice: Report of an expert panel. https://ipec.memberclicks.net/assets/2011-Original.pdf. Accessed November 10, 2022.
- 2.Interprofessional Education Collaborative Expert Panel. Core competencies for interprofessional collaborative practice: 2016 update. https://ipec.memberclicks.net/assets/2016-Update.pdf. Accessed November 10, 2022.
- 3.Charrette AL, Sullivan KM, Kucharski-Howard J, Seed S, Lorenz L. Physical therapy and pharmacy interprofessional education in the context of a university pro bono physical therapy setting. J Interprof Care. 2020;34(3):315-323. doi: 10.1080/13561820.2019.1663160. Accessed November 10, 2022. [DOI] [PubMed] [Google Scholar]
- 4.Fusco NM, Maerten-Rivera J, Doloresco F, Ohtake PJ. Improving Pharmacy Students’ Attitudes Toward Collaborative Practice Through a Large-scale Interprofessional Forum Targeting Opioid Dependence. Am J Pharm Educ . 2019;83(6):Article 7034. doi: 10.5688/ajpe7034. Accessed November 10, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stockert B, Ohtake PJ. A National Survey on the Use of Immersive Simulation for Interprofessional Education in Physical Therapist Education Programs. Simul Healthc . Oct 2017;12(5):298-303. doi: 10.1097/SIH.0000000000000231. Accessed November 10, 2022. [DOI] [PubMed] [Google Scholar]
- 6.Brown N, Darby W, Coronel H. An Escape Room as a Simulation Teaching Strategy. Clin Simul Nurs . 2019;30:1-6. doi: 10.1016/j.ecns.2019.02.002. Accessed November 10, 2022. [DOI] [Google Scholar]
- 7.Gentry SV, Gauthier A, L’Estrade Ehrstrom B, et al. Serious Gaming and Gamification Education in Health Professions: Systematic Review. J Med Internet Res . 2019;21(3):e12994. doi: 10.2196/12994. Accessed November 10, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aubeux D, Blanchflower N, Bray E, et al. Educational gaming for dental students: Design and assessment of a pilot endodontic-themed escape game. Eur J Dent Educ . 2020;24(3):449-457. doi: 10.1111/eje.12521. Accessed November 10, 2022. [DOI] [PubMed] [Google Scholar]
- 9.Caldas LM, Eukel HN, Matulewicz AT, Fernandez EV, Donohoe KL. Applying educational gaming success to a nonsterile compounding escape room. Curr Pharm Teach Learn . 2019;11(10):1049-1054. doi: 10.1016/j.cptl.2019.06.012. Accessed November 10, 2022. [DOI] [PubMed] [Google Scholar]
- 10.Foltz-Ramos K, Fusco NM, Paige JB. Saving patient x: A quasi-experimental study of teamwork and performance in simulation following an interprofessional escape room. [published online head of print, 2021 Feb 15]. J Interprof Care. 2021:1-8. doi: 10.1080/13561820.2021.1874316. Accessed November 10, 2022. [DOI] [PubMed] [Google Scholar]
- 11.Guckian J, Eveson L, May H. The great escape? The rise of the escape room in medical education. Future Healthc J . 2020;7(2):112-115. doi: 10.7861/fhj.2020-0032. Accessed November 10, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kavanaugh R, George S, Lamberton N, Frenzel JE, Cernusca D, Eukel HN. Transferability of a diabetes escape room into an accelerated pharmacy program. Curr Pharm Teach Learn . 2020;12(6):709-715. doi: 10.1016/j.cptl.2020.01.022. Accessed November 10, 2022. [DOI] [PubMed] [Google Scholar]
- 13.Morrell BLM, Eukel HN. Escape the Generational Gap: A Cardiovascular Escape Room for Nursing Education. J Nurs Educ . 2020;59(2):111-115. doi: 10.3928/01484834-20200122-11. Accessed November 10, 2022. [DOI] [PubMed] [Google Scholar]
- 14.Podlog M, Husain A, Greenstein J, Sanghvi S. Escape the Trauma Room. AEM Educ Train . 2020;4(2):158-160. doi: 10.1002/aet2.10410. Accessed November 10, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cheng A, Eppich W, Epps C, Kolbe M, Meguerdichian M, Grant V. Embracing informed student self-assessment during debriefing: the art of plus-delta. Adv Simul (Lond) . 2021;6(1):22. doi: 10.1186/s41077-021-00173-1. Accessed November 10, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.INACSL Standards Committee. INACSL Standards of Best Practice: Simulation-Enhanced Interprofessional Education (Sim-IPE). Clin Sim Nurs. 2016;12:S34-S38. doi: 10.1016/j.ecns.2016.09.011. Accessed November 10, 2022. [DOI] [Google Scholar]
- 17.King G, Orchard C, Khalili H, Avery L. Refinement of the Interprofessional Socialization and Valuing Scale (ISVS-21) and Development of 9-Item Equivalent Versions. J Contin Educ Health Prof . 2016;36(3):171-177. doi: 10.1097/CEH.0000000000000082. Accessed November 10, 2022. [DOI] [PubMed] [Google Scholar]
- 18.Castleberry A, Nolen A. Thematic analysis of qualitative research data: Is it as easy as it sounds? Curr Pharm Teach Learn . 2018;10(6):807-815. doi: 10.1016/j.cptl.2018.03.019. Accessed November 10, 2022. [DOI] [PubMed] [Google Scholar]
- 19.Lie DA, Richter-Lagha R, Forest CP, Walsh A, Lohenry K. When less is more: validating a brief scale to rate interprofessional team competencies. Med Educ Online . 2017;22(1):1314751. doi: 10.1080/10872981.2017.1314751. Accessed November 10, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.World Health Organization. Framework for action on interprofessional educaiton & collaborative practice. https://www.who.int/publications/i/item/framework-for-action-on-interprofessional-education-collaborative-practice. Accessed November 10, 2022.
- 21.Friedrich C, Teaford H, Taubenheim A, Boland P, Sick B. Escaping the professional silo: an escape room implemented in an interprofessional education curriculum. J Interprof Care . 2019;33(5):573-575. doi: 10.1080/13561820.2018.1538941. Accessed November 10, 2022. [DOI] [PubMed] [Google Scholar]
- 22.Friedrich C, Teaford H, Taubenheim A, Sick B. Interprofessional Health Care Escape Room for Advanced Students. J Nurs Educ . 2020;59(1):46-50. doi: 10.3928/01484834-20191223-11. Accessed November 10, 2022. [DOI] [PubMed] [Google Scholar]