Abstract
Introduction Surgical techniques for soft palate repair aiming for zero velopharyngeal insufficiency (VPI) are still not achieved. Straight line closure of the soft palate by various techniques of intravelar veloplasty (IVVP) leads to higher incidence of VPI due to scar contracture. Furlow's Z plasty has long, narrow, thin mucosal flaps and mucomuscular flaps with malaligned muscle closure. We present a technique of “hybrid palatoplasty” which borrows from and adds to the existing methods, is robust, is easy to replicate, and results in normal speech consistently.
Aim (1) To design a technique of “hybrid palatoplasty”—combining double opposing Z (DOZ) plasty and IVVP, which is applicable to all types of cleft palate. (2) To evaluate the results of cleft palate children operated using the technique of “hybrid palatoplasty” from 2014 to 2015 in terms of surgical complications (fistulae and dehiscence) and incidence of VPI.
Methods Our procedure combines aspects of both DOZ and IVVP. It is simplified with design of smaller Z plasties. On one side, from the oral Z plasty muscle is dissected off and sutured to the nasal mucomuscular flap of the opposite side to complete the palatal sling. Oral Z plasty is purely mucosal and reverse of the nasal side. A total of 123 cases, operated below 5 years of age were followed up. Speech was assessed by direct evaluation and tele-evaluation.
Results A total of 123 cases, below 5 years of age, were operated between 2014 and 2016 with at least 5 years of follow-up. Note that 120 had normal speech, and 3 had VPI of which 2 were subsequently corrected and went on to develop normal speech.
Conclusion This novel “hybrid palatoplasty” is a simple technique with good speech outcome as it combines the principles of Z plasty and direct muscle repair with palatal sling formation.
Keywords: palatoplasty, Furlow's Z plasty, intravelar veloplasty
Introduction
Surgical techniques of soft palate repair with zero velopharyngeal insufficiency (VPI) are still being aimed at. Historically, straight line closure with direct muscle repair, techniques described as intravelar veloplasty (IVVP), has demonstrated good palatal muscular sling recreation. But straight line closure of the soft palate has inevitable contracture which leads to higher incidence of VPI. Furlow's double opposing Z plasty (DOZ) involves creation of long, narrow thin mucosal flaps with malaligned muscle approximation and is generally held to be difficult to master. We present a technique of “hybrid palatoplasty” which borrows from and adds to the existing methods, is robust, is easy to replicate, and results in normal speech consistently.
Aim
To design a technique of “hybrid palatoplasty”—combining DOZ plasty and IVVP, which is applicable to all types of cleft palate.
To evaluate the results of cleft palate children operated using the technique of hybrid palatoplasty from 2014 to 2015 in terms of surgical complications (fistulae and dehiscence) and incidence of VPI.
Materials and Methods
Retrospective longitudinal clinical study was conducted at our comprehensive cleft care clinic in a private trust hospital after the institute's ethical committee approval. Children less than 5 years of age with isolated cleft palate, unilateral or bilateral cleft lip, and palate who attended the comprehensive cleft care clinic were evaluated and operated using the “hybrid palatoplasty” technique. One hundred and twenty-three primary cleft palate cases (group II and III according to Nagpur cleft classification), 1 operated between 2014 and 2016, with minimum of 5 years of follow-up were included in the study, after taking informed consent from parents/guardian. They were followed up at regular interval and physical examination of palate for evidence of partial dehiscence or fistula was done. Subjective speech evaluation was done after 3 years of age by two speech therapists at our institute and reported as per universal parameters for reporting speech outcomes. 2 It was evaluated by direct evaluation, and tele-evaluation using audio and video recordings. Video-fluoroscopic evaluation was done when there was clinical suspicion of VPI.
Surgical Procedure
Supplementary Video S1 Intraoperative video demonstrating the marking, dissection, and suturing of “hybrid palatoplasty.”
Procedure is started by splitting the cleft margin a few millimeters lateral to the edge on either side ( Fig. 1 ). Proximal nasal repair is performed up to the level of posterior nasal spine. In complete clefts, nasal repair is done up to the junction of posterior and inferior border of the vomerine bone which can be called as “high vomerine suspension.” The proximal part of soft palate is consciously moved toward the roof to reduce the resting gap.
Fig. 1.
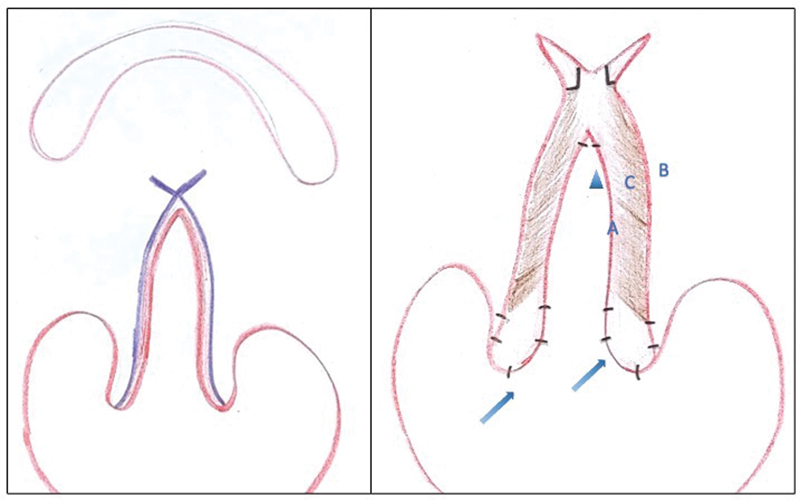
Schematic diagram showing (left) markings for incision (purple line) and (right) nasal layer ( A ), oral layer ( B ), abnormally inserted palatal muscle ( C ) and markings for anterior (arrowhead) and posterior stabilization (uvuloplasty - arrow mark) before nasal Z plasty.
Uvula is then split. Nasal and oral layers of uvula are repaired using interrupted suture (4-0 monocryl) ( Fig. 1 ). Same procedure is performed even when the palates are of unequal length. This stabilizes the central limb of Z plasty between two stable points before designing the nasal Z plasty ( Fig. 2 ). First the right side incision is given to develop a posteriorly based mucomuscular triangular flap dividing all the muscle fibers, aponeurosis, and mucosa for a few millimeters with the lateral end directed slightly posterior. Muscle is further pushed posteriorly by developing a plane oral to the aponeurosis for about a millimeter. This incision to develop the flap is usually less than 5 mm and can be further extended depending on the size of the mucosal flap on the left side.
Fig. 2.
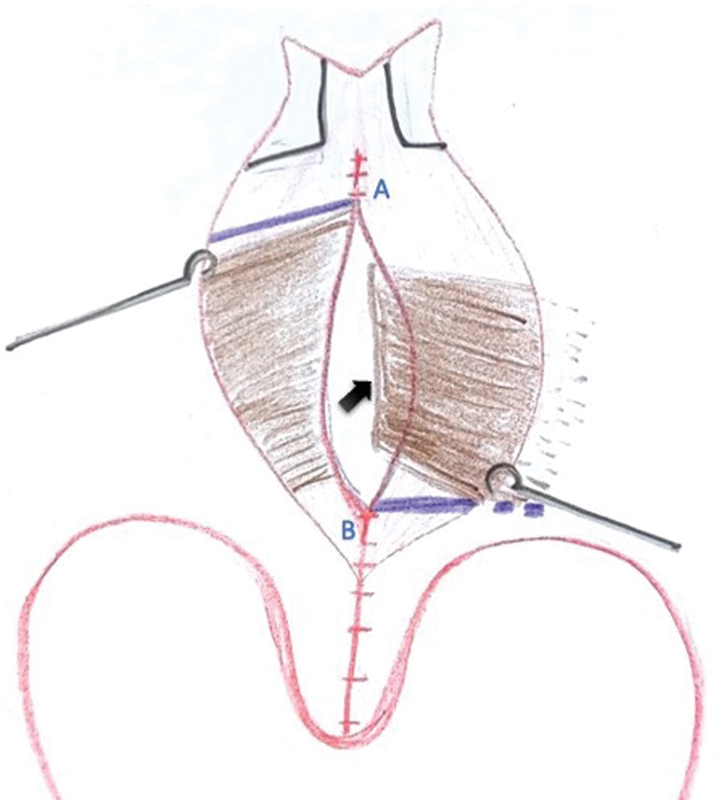
Schematic diagram showing dissected left palatal muscle bundle (arrow mark); stabilized anterior ( A ) and posterior end ( B ) before nasal Z plasty (purple line).
On the left side, palatal muscle bundle (confluence of levator, palatoglossus, and palatopharyngeus) is separated from the aponeurosis which is white in color. The separation is done using knife to create this plane between the muscle and submucosal glandular tissue nearer the nasal edge and by blunt dissection more laterally by pushing with the knife. The mucosal flap so developed contains apart from the mucosa, palatal aponeurosis laterally and considerable amount of mucosal glands and few muscle fibers medially. The incision is at right angles to the nasal edge (central limb) and is also close to the nasal uvular stitch as possible ( Fig. 2 ). The flap so developed is thick and vascular and one is able to suture without tension to complete the Z plasty ( Fig. 3 ).
Fig. 3.
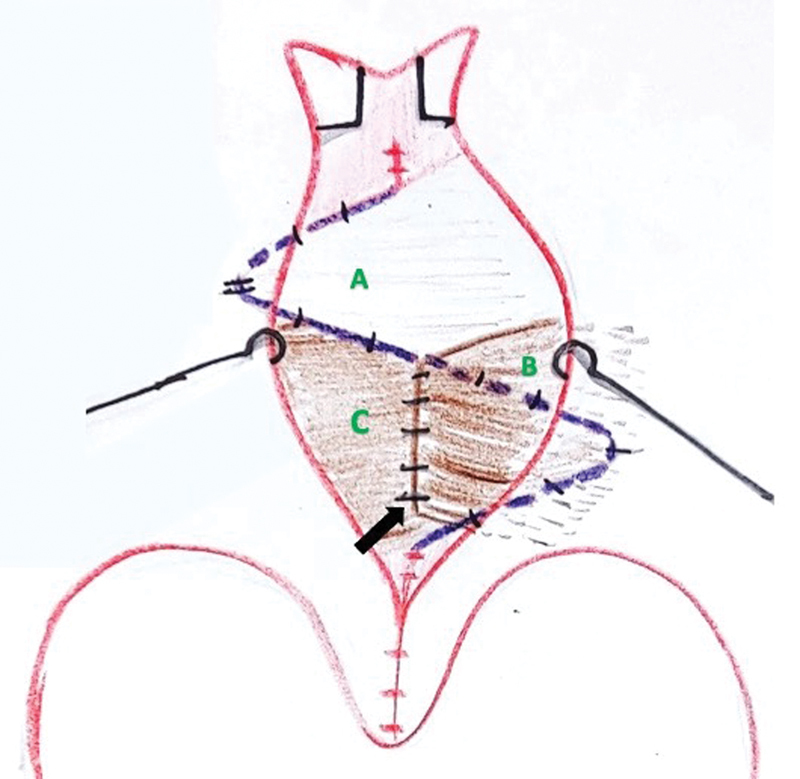
Schematic diagram showing transposed anteriorly based nasal Z plasty mucosal flap with few muscle fiber ( A ) and left dissected palatal muscle bundle ( B ) sutured to the transposed posteriorly based mucomuscular nasal Z plasty flap ( C ) for palatal sling reconstruction.
Muscle which is in the posterior half of the soft palate is then approximated together as a sling using one or two sutures under vision ( Fig. 3 ). This takes away the slack of the muscle dissected on the left side and creates a well-formed palatal sling.
Before oral closure it is usually necessary to give relaxing incisions in the retromolar area extending onto the molar area ( Fig. 4 ). The incision is in the grove close to the molar area up to the bone underneath and is dissected medially by blunt dissection. The greater palatine pedicle need not be visualized though it is possible to see it at this stage. The attachment of tensor veli palatini muscle may need to be released by cutting with knife so that the soft palate can move medially. The junction of hard and soft palate is sutured with a mattress suture. This is usually the thickest part of the soft palate because of the submucosal glandular tissue. On the mucosa this is identified by looking for a small dimple.
Fig. 4.
Schematic diagram showing markings for small unequal oral Z plasty (green line) with retromolar relaxing incision extending on the molar region (arrow marks).
Once this is secured, the oral “Z” plasty is planned with about a 60-degree proximal cut on the left side. This goes through the mucosal gland and a thick flap is elevated and underneath this the earlier repaired muscle bundle becomes visible. The distal cut on right side is at right angles, close to the base of uvula and is dissected off the underlying muscle till it is free to move across. The oral “Z” plasty is then completed. Design of the flaps is done in such a way that the incisions do not extend into the relaxing incisions given laterally and leave a small bridge of tissue in-between as shown in the diagram ( Figs. 4 and 5 ).
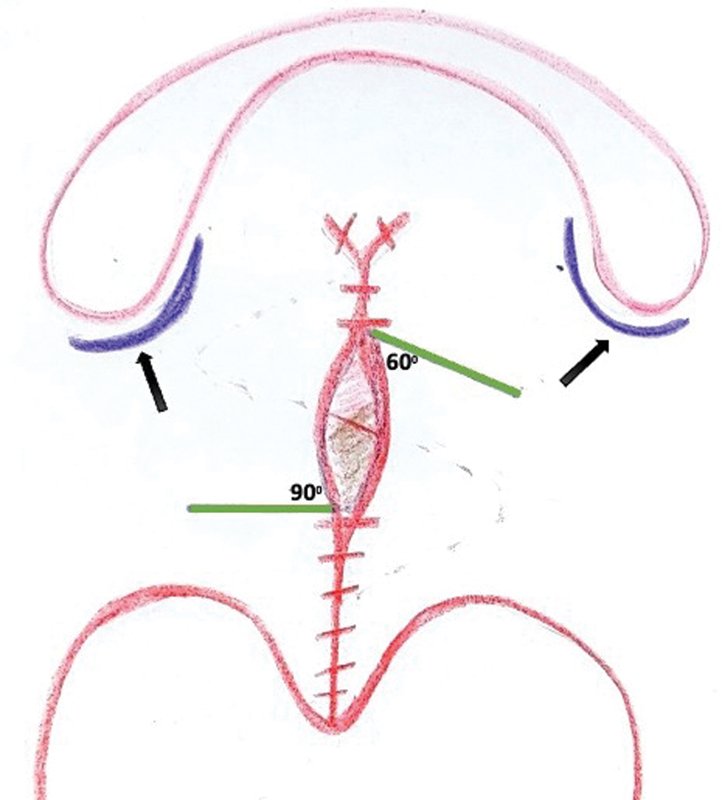
Fig. 5.
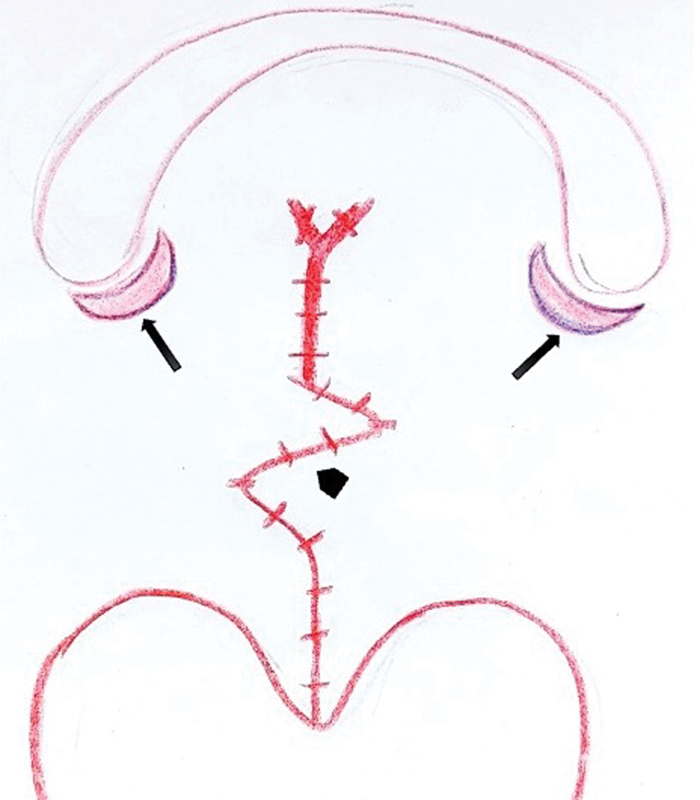
Schematic diagram showing final suture line of the lengthened palate with the transposed small oral Z plasty (arrow head) and raw area of retromolar incisions (arrow marks).
At completion, any bleeding in lateral relaxing incision is controlled with bipolar cautery and dead space filled with pieces of Surgicel to ensure that there is no postoperative ooze. For illustration, preoperative and immediate postoperative image of a case is presented in Figs. 6 and 7 . Intraoperative video of this technique is presented ( Supplementary Video S1 ).
Fig. 6.
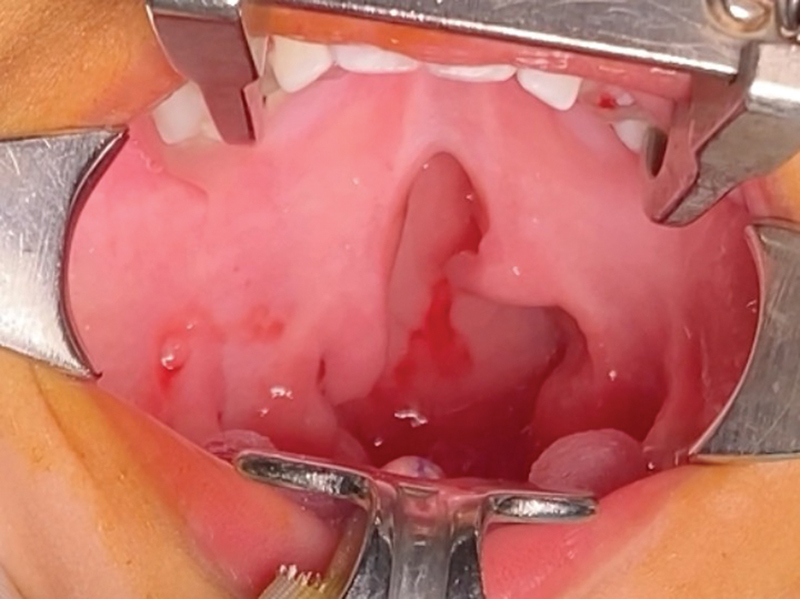
Preoperative image showing group II cleft.
Fig. 7.

Intraoperative image showing final suture line with “hybrid palatoplasty.”
Results
Supplementary Audio S1 Postoperative audio recording following “hybrid palatoplasty” at 1 year of age.
Supplementary Audio S2 Postoperative audio recording following “hybrid palatoplasty” at 4 years of age.
A total of 123 cleft palate patients were studied, which included 39 isolated cleft palate, 66 complete unilateral cleft, and 18 complete bilateral cleft cases. Age group at operation was below 1 year (83), up to 2 years (21), and 2 to 5 years (19).
There were 5 fistulae (4%) at the perialveolar area and no bifid uvulae. There was no dehiscence. Speech was normal in 97.6% of children ( Supplementary Audio S1 and S2 ) and 2.4% (3 cases) had VPI. Two cases were subsequently operated for VPI and went on to develop normal speech. Surprisingly, speech was normal even when operated above 1 year of age ( Supplementary Audio S2 ). Among the VPI cases, one child was operated at 3 years for group II cleft and two cases were operated at 1 year of age for group III cleft palate ( Table 1 ).
Table 1. Details of VPI cases post-“hybrid palatoplasty”.
| Serial no. | Type of cleft | Age at which operated for CP (years) | Age at which VPI correction done (years) | Final speech outcome |
|---|---|---|---|---|
| Case 1 | Group II | 3 | Yet to be operated | |
| Case 2 | Unilateral group III | 1 | 4 | Normal |
| Case 3 | Bilateral group III | 1 | 5 | Normal |
Abbreviations: CP, cleft palate; VPI, velopharyngeal insufficiency.
Discussion
Surgical techniques for cleft palate repair with good speech outcome consistently are still not obtained. Initially described techniques borrowed tissues from hard palate and pushed toward the soft palate. This leads to alveolar arch collapse which requires further intervention. Furlow described DOZ plasty that lengthens soft palate without borrowing hard palate tissue. 3 Several theoretical advantages have been described by this Z plasty like lengthening of soft palate and avoiding scar contracture. 4 5 6 Techniques that result in a good palatal length will help achieve good speech outcomes. Randall et al measured soft palates length and established that length is an important factor for outcomes of palatoplasty. 7 Cephalometric analysis allows us to measure soft palate length at rest. 8 Guneren and Uysal analyzed intraoperative and postoperative lengthening of soft palate in 17 cases operated by Furlow's palatoplasty with a mean follow-up of 4.5 years and demonstrated mean intraoperative and postoperative soft palatal elongation of 16.11 and 12.47 mm, respectively. 6 Chang et al studied 180 primary and secondary cases operated by Furlow's method and documented immediate postoperative soft palate lengthening of 30.6%. 5
Fistula rates were also analyzed when operated by Furlow's technique in various studies. Chang et al's study showed 4% oronasal fistula among 108 patients. 5 Chen and Noordhoff had 4 oronasal fistulae among 35 operated cases at Chang Gung Memorial Hospital. 9 Losken et al noticed higher fistula rate (35.8%) when majority were operated using Furlow's, especially among wider clefts and later restricted Furlow's technique only for clefts with width less than 8 mm and performed Bardach's two-flap palatoplasty in wider clefts and the fistula rate reduced to 1.6%. 10
Another major component of Furlow's repair was the transverse repositioning of abnormally attached soft palate musculature. 3 But the repositioned muscle is likely to be malaligned and is not directly approximated to form a proper muscular sling. Good speech being the main aim, good muscle repair and function is also equally important apart from length of soft palate.
Direct muscle repair with straight line closure has also been scrupulously described and widely followed. 11 Palatine muscle was dissected to various extent by different surgeons and repaired in IVVP. It was initially described by Braithwaite. The term IVVP was coined by Kriens 12 who suggested division of tensor tendon, dissection of velar muscle from hard palate margin and oral layer but not from nasal lining as it would lead to its sloughing. Cutting et al described radical IVVP in which he described separating the levator muscle from both nasal and oral layer after careful dissection of descending palatine artery. 13 Sommerlad modified it further by dissecting soft palate muscles under microscope. 14
Various studies have described the advantages and disadvantages of IVVP.
Bosi et al evaluated immediate and late complications after palatoplasty with IVVP which showed 16.67% incidence of fistulae and 18.6% incidence of hypernasality incidence. 15
A systematic review was conducted by Timbang et al to compare the speech outcomes and fistula rates following repair of the cleft palate with Furlow double- opposing Z-plasty and IVVP techniques. On analyzing 12 studies, the mean failure rates were higher with IVVP than Furlow's DOZ. The overall oronasal fistula rate was 7.87% in the Furlow repair group compared with 9.81% in the IVVP group. This difference was not statistically significant but the difference in the odds of requiring secondary surgery for VPI in the IVVP group was statistically significant than the Furlow group ( p = 0.03) in unilateral cleft lip–cleft palate. 16
In another comparative study between Furlow's and IVVP by Zietsman et al in 108 patients, 1 out of 34 (2.9%) in the Furlow group and 8 out of 74 (10.8%) in the IVVP group had fistulas, though the difference was not significant. 17
Various modifications of Furlow's have been described in the literature. 18 Nagy and Swennen followed Sommerlad's IVVP with straight line closure on nasal side and Z plasty on oral side. Two-year follow-up of 25 cases showed good early speech outcome but lacked long-term follow-up. 19
To combine the advantages of both Furlow's and IVVP technique, “hybrid palatoplasty” has been designed at our institute. The “hybrid palatoplasty” technique is robust, easy to replicate, and produces consistent normal speech by borrowing from and adding to the existing methods:
Z plasties are designed smaller.
Nasal Z plasty contains mucomuscular flap posteriorly; anteriorly based flap is mucosal with few fibers of muscle to have a robust flap.
On the left side palatal muscle is released from both nasal and oral mucosa and sutured with opposite palatal muscle to form palatal sling which restores velopharyngeal competence along with lengthening of soft palate.
Oral Z plasty is purely mucosal on both sides and reverse of nasal Z plasty.
Andrades et al classified IVVP based on various extent of muscle dissection 20 :
Type 0: No muscle dissection or suturing of muscle.
Type 1: No dissection, parallel suturing of muscle.
Type IIa: Partial dissection (release from posterior palatal shelf but minimal dissection from nasal and oral mucosa) creating inverted-U muscle sling.
Type IIb: Partial dissection (dissection from nasal mucosa but not oral mucosa) creating inverted-V muscle sling.
Type III: Complete dissection creating a transverse muscle sling (radical IVV).
According to this classification, our dissection would be type III on the left side and type IIb on the right side but it is dissected from oral mucosa and left attached to nasal mucosa as mucomuscular flap.
Mucosal tear and scaring is less if it is retained as mucomuscular flap rather than mucosal flap. But good approximation of muscle and palatal sling is also targeted by dissecting the muscle free at least on one side. Author's “hybrid palatoplasty” was designed this way taking both the pros and cons of muscle dissection into consideration.
In our study, out of 123 speech recordings available, only 3 had VPI. Among the VPI cases, one child was operated at 3 years for group II cleft and two cases were operated at 1 year of age for group III cleft palate (unilateral 1, bilateral 1). As the numbers are low, further analysis was not possible. Studies in cleft cases have shown that levator muscle is hypoplastic with more connective tissue and less contractile elements. 21 This may be the reason for VPI in spite of good reconstruction of palatine muscular sling.
Surprisingly, even when operated after 1 year of age, speech was normal for almost all cases (39/40). We believe creation of good palatal sling and lengthening of soft palate together helped achieve normal speech even in older children. This observation has encouraged the author to recommend this surgical technique for children with cleft palate up to the age of 5 years.
In this study, five patients had fistula. All fistulas occurred in the perialveolar region not affecting velopharyngeal closure. No fistulas were found in the soft palate or the junctional area. The cases of fistula and VPI were exclusive of each other.
Conclusion
“Hybrid palatoplasty” yields excellent speech results with minimal surgical complications. It is simple to replicate when approached in a stepwise manner.
Footnotes
Conflict of Interest None declared.
References
- 1.Agrawal K. Classification of cleft lip and palate: an Indian perspective. J Cleft Lip Palate Craniofacial Anomalies. 2014;1:78–84. [Google Scholar]
- 2.Speech Parameters Group . Henningsson G, Kuehn D P, Sell D, Sweeney T, Trost-Cardamone J E, Whitehill T L. Universal parameters for reporting speech outcomes in individuals with cleft palate. Cleft Palate Craniofac J. 2008;45(01):1–17. doi: 10.1597/06-086.1. [DOI] [PubMed] [Google Scholar]
- 3.Furlow L T., Jr Cleft palate repair by double opposing Z-plasty. Plast Reconstr Surg. 1986;78(06):724–738. doi: 10.1097/00006534-198678060-00002. [DOI] [PubMed] [Google Scholar]
- 4.Huang M H, Riski J E, Cohen S R, Simms C A, Burstein F D. An anatomic evaluation of the Furlow double opposing Z-plasty technique of cleft palate repair. Ann Acad Med Singap. 1999;28(05):672–676. [PubMed] [Google Scholar]
- 5.Chang B L, Yu J W, Nikonova E, Low D W, Taylor J A, Jackson O. Palatal measurements pre- and post-Furlow cleft palate repair: analysis of palatal lengthening and comparison within cleft types. Cleft Palate Craniofac J. 2019;56(05):601–609. doi: 10.1177/1055665618802150. [DOI] [PubMed] [Google Scholar]
- 6.Guneren E, Uysal O A. The quantitative evaluation of palatal elongation after Furlow palatoplasty. J Oral Maxillofac Surg. 2004;62(04):446–450. doi: 10.1016/j.joms.2003.05.015. [DOI] [PubMed] [Google Scholar]
- 7.Randall P, LaRossa D, McWilliams B J, Cohen M, Solot C, Jawad A F.Palatal length in cleft palate as a predictor of speech outcome Plast Reconstr Surg 2000106061254–1259., discussion 1260–1261 [DOI] [PubMed] [Google Scholar]
- 8.Subtelny J D. A cephalometric study of the growth of the soft palate. Plast Reconstr Surg. 1957;19(01):49–62. doi: 10.1097/00006534-195701000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Chen K T, Noordhoff S M. Experience with Furlow palatoplasty. Changge-ng Yi-xue Zazhi. 1994;17(03):211–219. [PubMed] [Google Scholar]
- 10.Losken H W, van Aalst J A, Teotia S S, Dean S B, Hultman S, Uhrich K S. Achieving low cleft palate fistula rates: surgical results and techniques. Cleft Palate Craniofac J. 2011;48(03):312–320. doi: 10.1597/08-288. [DOI] [PubMed] [Google Scholar]
- 11.Jayarajan R, Natarajan A, Nagamuttu R. Intravelar veloplasty: a review. J Cleft Lip Palate Craniofacial Anomalies. 2018;5(02):68–73. [Google Scholar]
- 12.Kriens O B. An anatomical approach to veloplasty. Plast Reconstr Surg. 1969;43(01):29–41. doi: 10.1097/00006534-196901000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Cutting C B, Rosenbaum J, Rovati L. The technique of muscle repair in the cleft soft palate. Oper Tech Plast Reconstr Surg. 1995;2(04):215–222. [Google Scholar]
- 14.Sommerlad B C. A technique for cleft palate repair. Plast Reconstr Surg. 2003;112(06):1542–1548. doi: 10.1097/01.PRS.0000085599.84458.D2. [DOI] [PubMed] [Google Scholar]
- 15.Bosi V, Brandão G, Yamashita R. Speech resonance and surgical complications after primary palatoplasty with intravelar veloplasty in patients with cleft lip and palate. Rev Bras Cir Plást. 2016;31(01):43–52. [Google Scholar]
- 16.Timbang M R, Gharb B B, Rampazzo A, Papay F, Zins J, Doumit G. A systematic review comparing Furlow double-opposing Z-plasty and straight-line intravelar veloplasty methods of cleft palate repair. Plast Reconstr Surg. 2014;134(05):1014–1022. doi: 10.1097/PRS.0000000000000637. [DOI] [PubMed] [Google Scholar]
- 17.Zietsman M S, Dibbs R P, Davis M J, Volk A S, Buchanan E P, Monson L A. Furlow versus straight line repair with intravelar veloplasty: a 7-year single institution experience with fistula formation. FACE. 2021;2(04):364–370. doi: 10.1097/01.JAA.0000800696.39721.ae. [DOI] [PubMed] [Google Scholar]
- 18.Gupta R, Kumar S, Murarka A K, Mowar A. Some modifications of the Furlow palatoplasty in wide clefts–a preliminary report. Cleft Palate Craniofac J. 2011;48(01):9–19. doi: 10.1597/09-051. [DOI] [PubMed] [Google Scholar]
- 19.Nagy K, Swennen G. Oral mucosal Z-plasty in combination with intravelar veloplasty. Plast Reconstr Surg Glob Open. 2015;3(07):e456. doi: 10.1097/GOX.0000000000000424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Andrades P, Espinosa-de-Los-Monteros A, Shell D H., IV The importance of radical intravelar veloplasty during two-flap palatoplasty. Plast Reconstr Surg. 2008;122(04):1121–1130. doi: 10.1097/PRS.0b013e3181845a21. [DOI] [PubMed] [Google Scholar]
- 21.Lindman R, Paulin G, Stål P S. Morphological characterization of the levator veli palatini muscle in children born with cleft palates. Cleft Palate Craniofac J. 2001;38(05):438–448. doi: 10.1597/1545-1569_2001_038_0438_mcotlv_2.0.co_2. [DOI] [PubMed] [Google Scholar]


