Abstract
Objective:
Despite evidence supporting the link between dietary restraint (i.e., attempts at dietary restriction) and loss of control (LOC) eating among individuals with binge-spectrum eating disorders, some research suggests that dietary restraint may not be linked to LOC eating in all contexts. It is currently unknown how often dietary restraint results in successful dietary restriction, or which types of restraint/restriction confer highest risk for LOC eating. Further, little research has evaluated momentary, temporal associations between dietary restraint and LOC eating. Thus, the present study aimed to, 1) characterize dietary restraint and restriction, among individuals with LOC eating, and 2) examine temporal relationships between restraint/restriction and LOC eating within- and between-subjects.
Method:
The current study recruited adults with binge spectrum eating disorders (N=96, 80.4% Female) to complete a 7 to 14-day ecological momentary assessment protocol assessing ED symptoms. Multilevel models and linear regression evaluated within- and between-subjects associations between momentary restraint/restriction and LOC eating, respectively.
Results:
Attempted avoidance of enjoyable foods, limiting the amount eaten, and any restraint predicted greater likelihood of LOC eating at the next survey. Attempts to delay eating predicted reduced likelihood of LOC eating at the next survey, though this effect was no longer statistically significant after correcting for multiple comparisons. Diagnostic presentation moderated the association between attempted avoidance of enjoyable foods and LOC eating such that this association was significantly stronger for those on the BN-spectrum.
Discussion:
Dietary restraint seems to be more predictive of LOC eating than dietary restriction both within- and between-subjects. Future treatments should target dietary restraint to reduce LOC eating.
Keywords: dietary restriction, dietary restraint, binge eating, bulimia nervosa, binge eating disorder, ecological momentary assessment
Introduction
Engagement in loss-of-control (LOC) eating (i.e., an episode of eating accompanied by a subjective sense of loss of control) is a key feature of binge-spectrum eating disorders (EDs) and is associated with a range of adverse health outcomes, including increased risk of anxiety, depression, substance use, and functional impairment (Byrne, LeMay-Russell, & Tanofsky-Kraff, 2019). Dietary restraint (i.e., purposeful cognitive attempts at decreasing food intake, regardless of behavioral outcome) is theorized to maintain LOC eating episodes (Fairburn, Cooper, & Shafran, 2003; Polivy & Herman, 1985; Stice, Nemeroff, & Shaw, 1996). Specifically, dietary restraint is posited to lead to physiological or hedonic hunger/deprivation and results in increased risk for LOC eating episodes. Importantly, there are several different types of dietary restraint, including avoidance of specific enjoyed foods (i.e., hedonic restraint), delaying eating (i.e., fasting), and limiting intake (e.g., reducing calories, limiting portion sizes), all of which are theorized to increase risk for and maintain LOC eating (Linardon et al., 2018).
There is strong theoretical and empirical evidence linking dietary restraint and LOC eating (Fairburn, 2008; Fairburn et al., 2003; Stice et al., 1996). Specifically, dieting has been shown to prospectively predict LOC eating (Goldschmidt, Wall, Loth, Le Grange, & Neumark-Sztainer, 2012; Kukk & Akkermann, 2020; Liechty & Lee, 2013; Neumark-Sztainer et al., 2006; Stice, 2001). Furthermore, experimental research has shown that individuals with higher dietary restraint tended to eat more food in a laboratory setting after a preload to induce a sense of having already overeaten, but ate less food than those with lower dietary restraint in the absence of the preload (Herman & Mack, 1975). These findings suggest that for individuals with high dietary restraint, consuming food inconsistent with the goal of dietary restraint may lead to a state of disinhibition, which may result in LOC eating.
Despite evidence supporting the link between dietary restraint and LOC eating, there is some opposing research that suggests that dietary restraint may not produce LOC eating in all contexts. For example, a 6-week weight loss diet in women at a normal BMI led to decreased LOC eating (Presnell & Stice, 2003). Similarly, a weight maintenance intervention for adolescent girls that included caloric restriction (i.e., actual reduced caloric intake) also resulted in decreased LOC eating (Stice, Presnell, Groesz, & Shaw, 2005). Additionally, in individuals with overweight or obesity, dietary restraint as part of a behavioral weight loss program reduces LOC eating (Da Luz et al., 2015; Goodrick, Poston II, Kimball, Reeves, & Foreyt, 1998; House et al., 2021). Even within clinical ED samples, there is some variation in the types of dietary restraint associated with LOC eating. For example, individuals with bulimia nervosa (BN) who reported eating fewer meals per day, but not those who reported eating smaller or lower-calorie meals, tended to have more frequent LOC eating episodes (Elran-Barak et al., 2015). Another study found that elevated dietary restraint in a BN sample was associated with increased urges to engage in LOC eating, but not actual LOC eating episodes (Engelberg, Gauvin, & Steiger, 2005).
The mixed evidence suggests there are gaps in our understanding of the relationship between dietary restraint and LOC eating. First, while there is significant evidence in support of the dietary restraint model of LOC eating, theories are less clear on whether successful dietary restraint (i.e., dietary restriction) matters. For example, it is unknown successful (i.e., restriction) versus unsuccessful attempts at delayed eating are more likely to trigger an LOC episode. Relatedly, it is unknown 1) how often dietary restraint results in successful restriction, 2) which types of restraint (i.e., avoiding specific foods, delaying eating, limiting intake) are the most common and the most influential for LOC eating risk, and 3) the time of day at which certain types of restraint are most likely to occur. Furthermore, little research has evaluated momentary, temporal associations between dietary restraint/restriction and LOC eating. While several studies have examined the temporal relationship between dietary restraint and LOC eating in individuals with binge-spectrum EDs (De Young et al., 2014; Engelberg et al., 2005; Holmes, Fuller‐Tyszkiewicz, Skouteris, & Broadbent, 2014; Zunker et al., 2011), their protocols either confounded dietary restraint and restriction or do not measure “successful” restraint attempts (i.e., restriction). A better understanding of which types of restraint (and resulting restriction) contribute to LOC eating and their temporal relationship would help treatments more efficiently target the most problematic aspects of restraint. Moreover, it is unknown how the frequency and type of dietary restraint might differ across diagnostic categories (e.g., BN-spectrum vs. BED-spectrum).
Thus, the present study used an ecological momentary assessment (EMA) design to: 1) characterize dietary restraint (and resulting successful restriction), including types of restraint, frequency of consecutive attempts, and times of day restraint/restriction were endorsed and 2) examine temporal relationships between restraint/restriction and LOC eating within- and between-subjects in a transdiagnostic, treatment-seeking sample with clinically-significant LOC eating. An exploratory aim of the study was to evaluate whether these relationships differed based on diagnostic presentation (BN-spectrum vs. BED-spectrum).
Methods
Participants
We recruited adults with binge-spectrum EDs (i.e., LOC eating defined as objective or subjective binge eating episodes ≥ 1x/week over the past 3 months; N=96) who were enrolling in a treatment study at Drexel University. Participants were included in the study if they were: 1) currently residing in the United States, 2) had access to a smartphone, and 3) were willing to complete ecological momentary assessment (EMA) surveys for at least 7 days before starting treatment. Participants were excluded from the study if they: 1) lacked fluency in English, 2) had a BMI < 18.5, 3) were currently and/or intended to enroll in eating or weight related treatment outside of Drexel in the next 16 months, 4) had severe psychopathology (i.e., psychosis), or 5) had an intellectual disability.
Procedures
Recruitment.
Participants who were eligible for treatment studies were invited to participate in the current study prior to start of their treatment. Informed consent was obtained and the EMA protocol was reviewed with participants prior to the start of the EMA surveys. The Drexel University Institutional Review Board approved all study procedures.
EMA Surveys.
Participants received 6 daily EMA surveys over 7–14 days. The duration of surveys completed by each participant was determined by the number of days available between the completion of baseline assessment and the first day of treatment. Once treatment started, participants were no longer eligible to continue EMA assessments. Surveys were delivered semi-randomly throughout participants’ waking hours every day during the recording period such that each participant received six surveys total, ~3 surveys in the morning and ~3 surveys in the afternoon/evening. Participants had forty-five minutes to complete each survey following receival of the prompts. Participants were asked to complete additional EMA surveys after engagement in LOC eating or compensatory behaviors (e.g., vomiting, laxative misuse).
Measures
Diagnostic Presentation.
A well-validated semi-structured interview, the Eating Disorders Examination 17.0, evaluated study eligibility and ED diagnosis (Fairburn, Cooper, & O’Connor, 1993).
Momentary LOC Eating.
As in previous ED studies (Schaefer et al., 2020), ED behavior engagement (i.e., LOC eating, vomiting, and laxative and diuretic misuse) was assessed via checklist. LOC eating was described to participants as, “eating episodes characterized by a sense that you can’t stop eating once you start eating and/or that you can’t control what or how much you’re eating.”
Momentary Dietary Restraint/Restriction.
At each survey, dietary restraint was assessed by asking, “Since the last survey, to what extent did you attempt the following behaviors (even if you were unsuccessful) in order to influence your weight or your shape?” Answer choices included 1) “Tried to limit the amount you ate,” 2) “Tried to avoid eating certain foods that you like,” and 3) “Tried to delay eating.” Participants responded to each prompt using a checkbox. Any engagement in dietary restraint was defined as responding “yes” to any type of attempted restriction. Dietary restraint also included any attempts in which participants reported successful dietary restriction. If participants endorsed any attempts at restraint, dietary restriction was assessed by asking, “Since the last survey, were you successful in ACTUALLY [limiting/delaying/avoiding] eating in order to influence your shape or weight?”. These questions were answered using a “Yes/No” format. Dietary restriction was defined as any answer of “Yes” to any type of restriction.
Statistical Analyses
Analyses used SPSS 28.0 and used an alpha < .05 as the threshold for statistical significance.
Characterization.
Central tendency and variability statistics were calculated for frequency of each type of restraint/restriction episode. To examine differences in restraint/restriction by diagnostic presentation and time of day, observed frequencies were calculated by diagnostic category (grouped into BN-spectrum vs. BED-spectrum, to maximize cell counts) for each restriction/restraint type. Chi-square tests for independence were used to evaluate whether there was a relationship between each type of restraint/restriction and diagnosis or time of day in the current sample. A post-hoc Phi statistic (ϕ) was calculated as a measure of effect size.
Within-Subjects.
because of the nested nature of EMA data (observations within person over time), we used individual multilevel models using a binomial distribution with a logit link function to examine whether engagement in restraint/restriction (i.e., any restriction, avoidance of enjoyable foods, limiting the amount eaten, and delaying eating) at time1 predicted LOC eating at the next survey. We controlled for presence of LOC eating and restraint/restriction at the previous survey. A cross-level interaction term for diagnostic presentation and restraint/restriction at time1 was included in additional models. In all analyses, we included fixed predictor variables and both random intercepts and slopes for person as well as estimates of between-person variance in order to better observe within-person variance in dietary restraint/restriction. Post-hoc power analyses revealed that we were fully powered to detect a medium effect (d=0.5) in the current sample with 4,032 potential observations of dietary restraint/restriction (6 surveys per day * 7 days * 96 participants; Kleiman) assuming a conservative 75% compliance rate. False discovery rate (FDR) correction was used to correct for multiple comparisons.
Between-subjects.
Linear regression models were used to examine the association between restraint/restriction across the recording period and overall engagement in LOC eating. An interaction term for diagnostic presentation and restraint or restriction was included in additional models. FDR correction was used to correct for multiple comparisons.
Results
Participant Characteristics
The current sample (80.4% female) included 96 treatment-seeking adults (Mage=41.36, SD=13.52) with transdiagnostic LOC eating and mean BMI=34.83 (SD=9.06). Participants primarily identified as Caucasian (n=71; 75.2%) with others identifying as: African American (n=11; 10.5%), Asian (n=3; 2.9%), American Indian/Alaska Native (n=1; 1.0%), more than one race (n=6; 6.7%), or unknown or prefer not to say (n=4; 3.8%); 10 participants (10.4%) identified as Hispanic or Latino. At baseline, participants endorsed an average of 25.26 (SD=21.42; range=4.00–109.00) LOC episodes and 13.88 (SD=11.38, range=1.00–52.00) compensatory behaviors in those with BN and 0.27 (SD=0.96, range=0.00–5.00) compensatory behaviors over the past month in those with BED, per the EDE interview. Fifteen participants were diagnosed with BED of low frequency (14.3%), 29 with full-threshold BED (31.0%), 15 with BN of low frequency (14.3%), and 37 with full-threshold BN (40.5%). Low frequency diagnoses were assigned when participants experienced < 12 LOC eating episodes (i.e., any combination of subjective or objective binge episodes) in the past three months and/or (in the case of subthreshold BN) < 12 compensatory behavior episodes. On average, participants completed 87.2% of EMA signaled surveys.
Characterization of dietary restraint & restriction
Overall, the majority (70.9%) of restraint attempts were also reported as successful restriction. There was no difference in the “conversion rate” for those with BN vs. those with BED (table 1). We also observed that individuals with BED were more likely than those with BN to endorse attempted avoidance of foods they enjoy, limiting of eating, and any restriction (table 2). In contrast, individuals with BN were more likely than those with BED to endorse attempted delaying of eating, attempted limiting of eating, any restraint, and actual delaying of eating (table 2). Attempted delaying of eating was significantly more likely to be reported in the morning compared to the afternoon and evening. Attempted limiting the amount eaten was significantly less likely to be reported in the morning and actual limiting the amount eaten was significantly more likely to be reported in the afternoon. Finally, actual delaying of eating and any restriction were significantly more likely to be reported in the evening (table 3).
Table 1.
Percent conversion from dietary restraint (reported attempts at restriction) to dietary restriction by diagnostic presentation.
| Type | % BED | % BN | % Total |
|---|---|---|---|
|
| |||
| Avoidance | 63.9 | 54.7 | 59.5 |
| Delaying | 90.6 | 82.7 | 86.4 |
| Limiting | 71.4 | 63.6 | 67.3 |
| Any | 72.5 | 69.5 | 70.9 |
BED = binge eating disorder spectrum
BN = bulimia nervosa spectrum
Table 2.
Number (N) and percent (%) of surveys at which each type of restraint/restriction was reported by diagnostic presentation. Reported percentages represent the percent of all EMA surveys on which the behavior was reported for each group (e.g., avoidance of eating was reported on 9.5 percent of all surveys completed by participants with BN and 9.8 percent of surveys completed by those with BED).
| Type | BED | BN | χ2 | p | ϕ | |||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | |||||
|
| ||||||||
| Restraint | Avoidance | 477 | 17.4 | 444 | 15.3 | 4.51 | .03* | 0.07 |
| Delaying | 490 | 15.8 | 561 | 22.0 | 36.39 | <.001* | 0.19 | |
| Limiting | 679 | 21.8 | 739 | 29.0 | 38.45 | <.001* | 0.16 | |
|
| ||||||||
| Any | 1151 | 37.0 | 1196 | 47.0 | 57.10 | <.001* | 0.16 | |
|
| ||||||||
| Restriction | Avoidance | 305 | 9.8 | 243 | 9.5 | 0.11 | .74 | 0.01 |
| Delaying | 444 | 14.3 | 464 | 18.2 | 16.14 | <.001* | 0.13 | |
| Limiting | 485 | 18.5 | 470 | 15.6 | 8.15 | .004* | 0.09 | |
|
| ||||||||
| Any | 834 | 32.6 | 831 | 26.8 | 22.76 | <.001* | 0.12 | |
BED = binge eating disorder spectrum
BN = bulimia nervosa spectrum
Table 3.
Number (N) and percent (%) of surveys at which restraint/restriction was endorsed by time of day. Reported percentages represent the percent of all EMA surveys on which the behavior was reported for each time of day.
| Type | Morning | Afternoon | Evening | Late-night | χ2 | p | ϕ | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | |||||
|
| ||||||||||||
| Restraint | Avoidance | 207 | 14.7 | 378 | 16.9 | 365 | 16.7 | 4 | 2.2 | 3.56 | .17 | 0.06 |
| Delaying | 325 | 23.0 | 460 | 20.5 | 327 | 15.0 | 7 | 3.9 | 41.19 | <.001* | 0.19 | |
| Limiting | 316 | 22.4 | 580 | 25.9 | 576 | 26.4 | 24 | 13.4 | 8.05 | .02* | 0.07 | |
|
| ||||||||||||
| Any | 578 | 40.9 | 985 | 43.9 | 884 | 40.5 | 31 | 17.3 | 6.22 | .05 | 0.05 | |
|
| ||||||||||||
| Restriction | Avoidance | 143 | 10.1 | 227 | 10.1 | 199 | 9.1 | 1 | 0.6 | 1.61 | .45 | 0.05 |
| Delaying | 292 | 20.7 | 410 | 18.3 | 261 | 11.9 | 3 | 1.7 | 56.03 | <.001* | 0.24 | |
| Limiting | 228 | 16.1 | 424 | 18.9 | 350 | 16.0 | 10 | 5.6 | 7.86 | .02* | 0.09 | |
|
| ||||||||||||
| Any | 450 | 31.9 | 738 | 32.9 | 570 | 26.1 | 13 | 7.3 | 27.28 | <.001* | 0.12 | |
Note. Morning=5–11:59am, Afternoon=12–4:59pm, Evening=5–11:59pm, Late-night= 12–4:59am. Late-night was excluded from chi-square tests as we expected this to differ.
Within-subjects associations between dietary restraint/restriction and LOC eating
After FDR correction, attempted avoidance of enjoyable foods, limiting the amount eaten, and any restraint all predicted greater likelihood of LOC eating at the next survey. Conversely, attempts to delay eating predicted reduced likelihood of LOC eating at the next survey, however, this effect was not statistically significant after FDR correction. Successful dietary restriction was not predictive of LOC eating at the next survey. Additionally, diagnosis did not moderate any within-subjects associations between dietary restraint/restriction and subsequent LOC eating. See table 4 for all within-subjects associations and cross-level interactions.
Table 4.
Within-subjects associations and cross-level interactions between restraint/restriction and LOC eating moderated by diagnostic presentation.
| Predictor | Interaction term | β | S.E. | p | O.R. | FDR crit | |
|---|---|---|---|---|---|---|---|
| Restraint | Avoidance | -- | .464 | .161 | .004* | 1.59 | .009† |
| Diagnosis | .246 | .292 | .40 | 1.28 | .041 | ||
| Delaying | -- | −.306 | .143 | .03* | 0.74 | .013 | |
| Diagnosis | .358 | .257 | .16 | 1.43 | .019 | ||
| Limiting | -- | .642 | .179 | <.001* | 1.87 | .006† | |
| Diagnosis | .248 | .275 | .37 | 1.28 | .034 | ||
| Any | -- | 1.057 | .179 | <.001* | 2.88 | .003† | |
| Diagnosis | .256 | .251 | .31 | 1.29 | .031 | ||
| Restriction | Avoidance | -- | −.300 | .292 | .30 | 0.74 | .028 |
| Diagnosis | .034 | .646 | .96 | 1.04 | .050 | ||
| Delaying | -- | −.435 | .264 | .10 | 0.65 | .016 | |
| Diagnosis | .085 | .363 | .81 | 1.09 | .047 | ||
| Limiting | -- | −.260 | .234 | .27 | 0.77 | .025 | |
| Diagnosis | .299 | .460 | .52 | 1.35 | .044 | ||
| Any | -- | .640 | .494 | .20 | 1.90 | .022 | |
| Diagnosis | .297 | .353 | .40 | 1.35 | .038 | ||
Note. Diagnosis was coded as 0=BED, 1=BN;
p < .05,
remained statistically significant after FDR correction; FDR = False discovery rate; p < FDR critical value indicates that there is a < 5% chance this result is a false positive; BED = binge eating disorder spectrum; BN = bulimia nervosa spectrum.
Between-subjects associations between dietary restraint/restriction and LOC eating
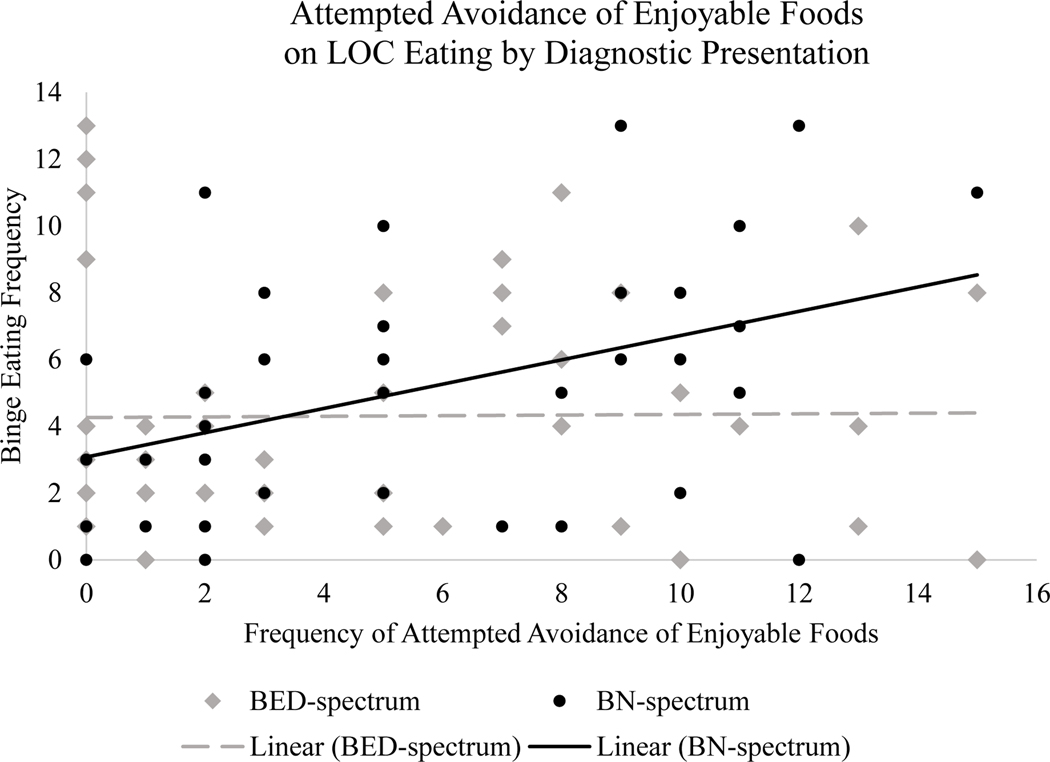
After FDR correction, any restraint was associated with increased frequency of LOC eating across the recording period. Greater frequency of attempted avoidance of enjoyable foods and attempted limiting the amount eaten were associated with increased frequency of LOC eating across the recording period, however, this effect was not statistically significant after FDR correction. We did not find significant associations between frequency of attempts to delay eating, or any type of restriction (including avoidance of enjoyable foods, limiting the amount eaten, and delaying eating) and frequency of LOC eating across the recording period. Diagnostic presentation moderated the association between attempted avoidance of enjoyable foods and LOC eating such that the association between attempted avoidance and LOC eating was significantly stronger for those with BN (figure 1), however, this effect was not statistically significant after FDR correction. See table 5 for all between-subjects associations.
Figure 1.
Diagnostic presentation moderates the association between attempted avoidance of enjoyable foods and LOC eating.
Table 5.
Between-subjects associations between restraint/restriction and loss-of-control eating moderated by diagnostic presentation.
| Predictor | Interaction term | β | S.E. | p | R2 | FDR crit | |
|---|---|---|---|---|---|---|---|
| Restraint | Avoidance | -- | .181 | .079 | .02* | .053 | .006 |
| Diagnosis | .221 | .107 | .04* | .097 | .013 | ||
| Delaying | -- | .149 | .084 | .08 | .032 | .022 | |
| Diagnosis | .003 | .099 | .98 | .031 | .050 | ||
| Limiting | -- | .190 | .078 | .02* | .058 | .009 | |
| Diagnosis | .147 | .084 | .09 | .092 | .025 | ||
| Any | -- | .274 | .080 | <.001* | .109 | .003† | |
| Diagnosis | .072 | .067 | .29 | .119 | .031 | ||
| Restriction | Avoidance | -- | .043 | .094 | .64 | .002 | .044 |
| Diagnosis | .281 | .144 | .06 | .042 | .016 | ||
| Delaying | -- | .066 | .086 | .44 | .006 | .038 | |
| Diagnosis | .067 | .107 | .53 | .012 | .041 | ||
| Limiting | -- | .027 | .089 | .76 | .001 | .047 | |
| Diagnosis | .196 | .106 | .07 | .038 | .019 | ||
| Any | -- | .129 | .086 | .14 | .023 | .028 | |
| Diagnosis | .079 | .080 | .33 | .039 | .034 | ||
Note. Diagnosis was coded as 0=BED, 1=BN;
p < .05,
remained statistically significant after FDR correction; FDR = False discovery rate; p < FDR critical value indicates that there is a < 5% chance this result is a false positive; BED = binge eating disorder spectrum; BN = bulimia nervosa spectrum.
Discussion
This study aimed to characterize dietary restraint, including types of dietary restraint, frequency of endorsed restraint, and the time-of-day dietary restraint was endorsed. Additionally, this study was the first to examine temporal relationships between different types of dietary restraint and LOC eating within- and between-subjects in a sample of adults with binge-spectrum eating disorders.
Overall, results of the present study showed that the majority (~70%) of dietary restraint attempts were successful (i.e., resulted in dietary restriction), that engagement in dietary restraint varied throughout the day, and that attempts were comparable by diagnosis. Additionally, attempted and actual delaying of eating were more likely to be reported in the morning while attempted and actual limiting the amount eaten and any restriction were more likely to be reported in the afternoon/evening. The fact that restriction was more likely in the afternoon than the morning was surprising in that the “conventional wisdom” is that individuals with BN/BED restrict earlier in the day and experience subsequent loss of control later in the day. However, it is possible that there are fewer food temptations in the mornings and thus restraint may feel less necessary. Restraint then may occur in the afternoon, with LOC episodes occurring in the evening.
No significant difference by diagnostic presentation in the “conversion rate” of attempted to successful dietary restraint was identified, indicating that individuals with BN and BED share a common pattern of restraint and restriction. Notably, and somewhat surprisingly, individuals with BED-spectrum EDs were more likely than those with BN-spectrum EDs to endorse successful restriction. This finding is somewhat in contrast to other research suggesting individuals with BN have higher levels of dietary restriction (Elran-Barak et al., 2015). There are a few possible reasons for this finding. First, it is possible that one’s report of “successful” dietary restraint may be influenced by (1) one’s definition of “success” and relatedly, (2) whether or not an LOC or overeating episode occurred since the restriction attempt. Those with BN may have more rigid rules regarding their eating, and thus different standards for what constitutes a “successful” restriction attempt. To better personalize intervention, future research should further investigate differing definitions of restriction by diagnostic presentation.
We found that attempted avoidance, limiting, and any restraint (but not delaying eating) predicted a greater likelihood of LOC eating at the following survey; however, somewhat surprisingly, no type of successful dietary restriction was predictive of subsequent LOC eating. Diagnosis did not moderate these within-subjects associations. Additionally, frequency of any restraint was associated with frequency of LOC eating episodes across the EMA period, suggesting that those with greater restraint had more LOC eating episodes overall. These findings are somewhat consistent with existing literature suggesting that restraint, not restriction, is the key maintaining variable for LOC eating (Lowe et al., 1996). It is possible that LOC eating originally occurs in response to acute dietary restriction, but that over time, the psychological/cognitive deprivation from restraint attempts, even if not successful, maintains LOC eating episodes. Surprisingly, results suggested that attempts to delay eating was associated with 35% reduced likelihood of LOC eating at the following survey, although these results became statistically non-significant after FDR correction. Perhaps delaying eating can be adaptive in some cases for individuals with binge-spectrum EDs, who often show high rates of grazing behavior, which may convert into LOC episodes (Heriseanu, Hay, Corbit, & Touyz, 2017). As such, future research should further explore whether delaying eating can be adaptive for patients who have the tendency to graze. Another explanation is that the time frame for the analyses was incorrect, and that delaying eating could lead to LOC episodes over a longer time frame, e.g., if one delays eating on one day or endorses delayed eating at several consecutive surveys, they would be more likely to have an LOC eating episode on the following day or later that day, respectively. Such analyses were outside the scope of this study. These findings are consistent with other research suggesting that delaying eating is a unique facet of restraint that is only weakly related to other facets of restraint (Linardon et al., 2018). Currently, restraint is treated as uniformly maladaptive in CBT for EDs. It is possible that for some individuals, not all restraint is equally maladaptive and future research should investigate this possibility. Future research should also examine relations between unsuccessful restraint attempts and subsequent LOC (and restraint/restriction) to further elucidate whether disinhibition may lead to LOC eating.
The present study has several notable strengths. First, to our knowledge, this is the first study to examine within-day momentary associations between different types of dietary restraint and LOC eating. Second, the present study has strong ecological validity, attributable to momentary assessments of dietary restraint and LOC eating. Third, by collecting momentary data, we were able to infer temporal relationships between attempted dietary restraint versus dietary restriction and LOC eating. Fourth, this study recruited a transdiagnostic sample of individuals with clinically significant loss of control eating, increasing the generalizability of our findings, and allowed us to examine the moderation of diagnosis between BN-spectrum and BED-spectrum. However, several study limitations should be considered when contextualizing our results. Although including individuals with subthreshold EDs improves the generalizability of our sample, the severity and frequency of ED symptoms (e.g., LOC eating, restraint, restriction) may be underrepresented relative to a sample comprising only individuals with full-threshold EDs. Additionally, though momentary assessments allow us to establish temporal associations and we are unable to determine any causal relationship between the variables observed. Third, participants may not have logged all instances of dietary restraint and LOC eating which may have impacted our ability to fully picture the nuanced relationship between types of dietary restraint and LOC eating. Fourth, assessments of dietary restriction were subjective, and participants may have over or under-reported instances of restraint or restriction; as described above, participants may have had differing definitions of what constituted a “successful” restriction attempt. Finally, assessment of both restraint and dietary restriction used binary responses. It is possible that restraint is experienced on a continuum. Future studies should aim to capture a more detailed account of behaviors which individuals associate with types of dietary restraint as well as eating patterns throughout the day. Additionally, future studies may aim to identify other, more fine-grained types of dietary restraint. For example, it may be useful to differentiate between restraint intended to avoid LOC eating in particular versus restraint intended to avoid eating altogether.
Conclusions
The current study sought to characterize dietary restraint and restriction in a transdiagnostic, treatment-seeking sample with clinically-significant LOC eating in naturalistic settings. This study is also among the few to naturalistically investigate the prospective associations between dietary restraint and LOC and between dietary restriction and LOC in individuals with clinically-significant LOC eating. Finally, the study also examined whether the prospective relationships between dietary restraint and restriction and LOC eating were moderated by diagnoses (BN vs BED). Overall results suggest that a nuanced relationship exists between restraint, restriction, and LOC eating. Dietary restraint appears to be more predictive of LOC eating both within and between-subjects. Furthermore, this study’s findings provide further evidence that treatments targeting specific subtypes of dietary restraint may be warranted.
Public Significance Statement.
Some research suggests that dietary restriction (i.e., reduced calorie intake) and restraint (i.e., attempted restriction) may not be linked to loss of control (LOC) eating in all contexts. We found that dietary restraint is more predictive of LOC eating than dietary restriction both within and between individuals. Future treatments should target dietary restraint to reduce LOC eating.
Funding:
Dr. Manasse is supported by an award from the National Institute of Health (K23DK124514).
Footnotes
Conflicts of Interest: The authors have no conflict to declare.
Data Availability:
Data is available upon reasonable request to the corresponding author.
References
- Byrne ME, LeMay-Russell S, & Tanofsky-Kraff M.(2019). Loss-of-control eating and obesity among children and adolescents. Current obesity reports, 8(1), 33–42. [DOI] [PubMed] [Google Scholar]
- Da Luz F, Hay P, Gibson AA, Touyz SW, Swinbourne JM, Roekenes JA, & Sainsbury A.(2015). Does severe dietary energy restriction increase binge eating in overweight or obese individuals? A systematic review. obesity reviews, 16(8), 652–665. [DOI] [PubMed] [Google Scholar]
- De Young KP, Lavender JM, Crosby RD, Wonderlich SA, Engel SG, Mitchell JE, . . . Le Grange D.(2014). Bidirectional associations between binge eating and restriction in anorexia nervosa. An ecological momentary assessment study. Appetite, 83, 69–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elran-Barak R, Sztainer M, Goldschmidt AB, Crow SJ, Peterson CB, Hill LL, . . . Le Grange D.(2015). Dietary restriction behaviors and binge eating in anorexia nervosa, bulimia nervosa and binge eating disorder: Trans-diagnostic examination of the restraint model. Eating behaviors, 18, 192–196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engelberg MJ, Gauvin L, & Steiger H.(2005). A naturalistic evaluation of the relation between dietary restraint, the urge to binge, and actual binge eating: a clarification. International Journal of Eating Disorders, 38(4), 355–360. [DOI] [PubMed] [Google Scholar]
- Fairburn CG (2008). Cognitive behavior therapy and eating disorders: Guilford Press. [Google Scholar]
- Fairburn CG, Cooper Z, & O’Connor M.(1993). The eating disorder examination. International Journal of Eating Disorders, 6, 1–8. [Google Scholar]
- Fairburn CG, Cooper Z, & Shafran R.(2003). Cognitive behaviour therapy for eating disorders: A “transdiagnostic” theory and treatment. Behaviour research and therapy, 41(5), 509–528. [DOI] [PubMed] [Google Scholar]
- Goldschmidt AB, Wall M, Loth KA, Le Grange D, & Neumark-Sztainer D.(2012). Which dieters are at risk for the onset of binge eating? A prospective study of adolescents and young adults. Journal of Adolescent Health, 51(1), 86–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodrick GK, Poston II WSC, Kimball KT, Reeves RS, & Foreyt JP (1998). Nondieting versus dieting treatment for overweight binge-eating women. Journal of consulting and clinical psychology, 66(2), 363. [DOI] [PubMed] [Google Scholar]
- Heriseanu AI, Hay P, Corbit L, & Touyz S.(2017). Grazing in adults with obesity and eating disorders: A systematic review of associated clinical features and meta-analysis of prevalence. Clinical Psychology Review, 58, 16–32. [DOI] [PubMed] [Google Scholar]
- Herman CP, & Mack D.(1975). Restrained and unrestrained eating. Journal of personality. [DOI] [PubMed] [Google Scholar]
- Holmes M, Fuller‐Tyszkiewicz M, Skouteris H, & Broadbent J.(2014). Improving prediction of binge episodes by modelling chronicity of dietary restriction. European Eating Disorders Review, 22(6), 405–411. [DOI] [PubMed] [Google Scholar]
- House ET, Gow ML, Lister NB, Baur LA, Garnett SP, Paxton SJ, & Jebeile H.(2021). Pediatric weight management, dietary restraint, dieting, and eating disorder risk: a systematic review. Nutrition Reviews. [DOI] [PubMed] [Google Scholar]
- Kleiman E.Power Curves for Multilevel Studies. Retrieved from 10.1007/s40519-022-01371-0 [DOI] [Google Scholar]
- Kukk K, & Akkermann K.(2020). Emotion regulation difficulties and dietary restraint independently predict binge eating among men. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity, 25(6), 1553–1560. [DOI] [PubMed] [Google Scholar]
- Liechty JM, & Lee MJ (2013). Longitudinal predictors of dieting and disordered eating among young adults in the US. International Journal of Eating Disorders, 46(8), 790–800. [DOI] [PubMed] [Google Scholar]
- Linardon J, Phillipou A, Newton R, Fuller-Tyszkiewicz M, Jenkins Z, Cistullo LL, & Castle D.(2018). Testing the relative associations of different components of dietary restraint on psychological functioning in anorexia nervosa and bulimia nervosa. Appetite, 128, 1–6. [DOI] [PubMed] [Google Scholar]
- Lowe MR, Gleaves DH, DiSimone-Weiss RT, Furgueson C, Gayda CA, Kolsky PA, . . . McKinney S.(1996). Restraint, dieting, and the continuum model of bulimia nervosa. Journal of Abnormal Psychology, 105(4), 508. [DOI] [PubMed] [Google Scholar]
- Neumark-Sztainer D, Wall M, Guo J, Story M, Haines J, & Eisenberg M.(2006). Obesity, disordered eating, and eating disorders in a longitudinal study of adolescents: how do dieters fare 5 years later? Journal of the American Dietetic Association, 106(4), 559–568. [DOI] [PubMed] [Google Scholar]
- Polivy J, & Herman CP (1985). Dieting and binging: A causal analysis. American psychologist, 40(2), 193. [DOI] [PubMed] [Google Scholar]
- Presnell K, & Stice E.(2003). An experimental test of the effect of weight-loss dieting on bulimic pathology: tipping the scales in a different direction. Journal of abnormal psychology, 112(1), 166. [PubMed] [Google Scholar]
- Schaefer LM, Smith KE, Anderson LM, Cao L, Crosby RD, Engel SG, . . . Wonderlich SA (2020). The role of affect in the maintenance of binge-eating disorder: Evidence from an ecological momentary assessment study. Journal of Abnormal Psychology, 129(4), 387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E.(2001). A prospective test of the dual-pathway model of bulimic pathology: mediating effects of dieting and negative affect. Journal of abnormal psychology, 110(1), 124. [DOI] [PubMed] [Google Scholar]
- Stice E, Nemeroff C, & Shaw HE (1996). Test of the dual pathway model of bulimia nervosa: Evidence for dietary restraint and affect regulation mechanisms. Journal of Social and Clinical Psychology, 15(3), 340–363. [Google Scholar]
- Stice E, Presnell K, Groesz L, & Shaw H.(2005). Effects of a weight maintenance diet on bulimic symptoms in adolescent girls: an experimental test of the dietary restraint theory. Health Psychology, 24(4), 402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zunker C, Peterson CB, Crosby RD, Cao L, Engel SG, Mitchell JE, & Wonderlich SA (2011). Ecological momentary assessment of bulimia nervosa: Does dietary restriction predict binge eating? Behaviour Research and Therapy, 49(10), 714–717. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is available upon reasonable request to the corresponding author.