INTRODUCTION
High blood pressure (BP) is the single leading risk factor for cardiovascular disease worldwide,1–4 and lowering BP substantially reduces that risk.5–7 Effective BP management relies on accurate measurement. This joint statement from 13 scientific health organizations around the globe has the focused goal of emphasizing the importance of, and introducing a pragmatic approach to, standardized clinic BP measurement implemented in clinical practice.
Clinic or office BP measurement is one of the most common procedures in medical practice. In most settings worldwide, estimation of a patient’s usual level of BP is based on clinic measurements, often as the only method available. Thus, while recognizing the importance of out-of-clinic BP measurements, the focus of this report is on BP measured in clinic settings. Measuring BP following a standardized approach and using clinically validated devices are important because these methods have been employed in research to establish BP thresholds associated with cardiovascular disease risk, to determine the benefits of lowering BP on health outcomes, and to establish optimal BP treatment targets. Although not a focus here, these principles of standardization are directly applicable to the measurement of BP at home. The lack of standardization in BP measurement is a serious and frequent problem in contemporary clinical practice that impacts patient safety and health system performance.8
For several decades, clinical practice guidelines9–17 and position statements18–22 have provided detailed instructions on clinic BP measurement. Despite these efforts, standardization is not implemented in most clinical practices18 because its importance is often underappreciated, and the necessary steps are considered time-consuming and impractical.23 However, reliable, accurate BP measurements are essential to best manage hypertension. We posit that it is feasible to streamline the clinic workflow and adopt other strategies that minimize the amount of time required to perform standardized BP measurements. An important recommendation among these strategies is to discriminate between various types of clinic visits depending on whether or not BP management is an objective during the visit. In this paradigm, standardized BP would be routinely obtained during clinic visits where the screening, diagnosis, and treatment of hypertension are objectives.
This document represents a consensus statement by the authors, all of whom represent the position of one or more professional health organizations and other health partners. It is not intended to provide a comprehensive review of the literature or a summary of other detailed guidelines, nor is it intended to reconcile differences across guidelines. Instead, we aim to balance the rigor of BP measurement techniques used in all hypertension outcome trials with the pragmatism that is required in daily clinical practice. Our report is based on a careful examination of the procedures recommended in clinical practice guidelines and a compilation of the most essential elements that are supported by consensus among the authors of this document. Recommendations of individual details in this document are not graded by their strength of evidence, but standardized BP measurement itself is our strong recommendation. The readers are referred to published guidelines and scientific statements for other elements of BP measurement (Appendix 1, available online). Our presumption is that a simplified standardized BP measurement protocol will lead to its wide adoption in daily practice, with minimal compromise in measurement accuracy and reliability.
In addition to making a strong recommendation to adopt the streamlined protocol described herein, we provide the rationale for standardization, discuss barriers to its implementation, and propose strategies to overcome these barriers. The ultimate goal of this joint statement is to ensure that health care organizations, health care professionals and patients can have greater confidence that the BP measurements used to guide management will improve clinical outcomes.
WHAT IS STANDARDIZED CLINIC BP MEASUREMENT?
In this document, standardized clinic BP measurement refers to readings obtained following procedures outlined in a protocol that includes steps recommended by most practice guidelines (Figure). It necessitates preparation of the patient as well as specifications of the setting, equipment, measurement procedure, and the way in which the BP readings are recorded. Further explanations and certain details of the recommendations are provided in the text at the end of this section.
Figure.
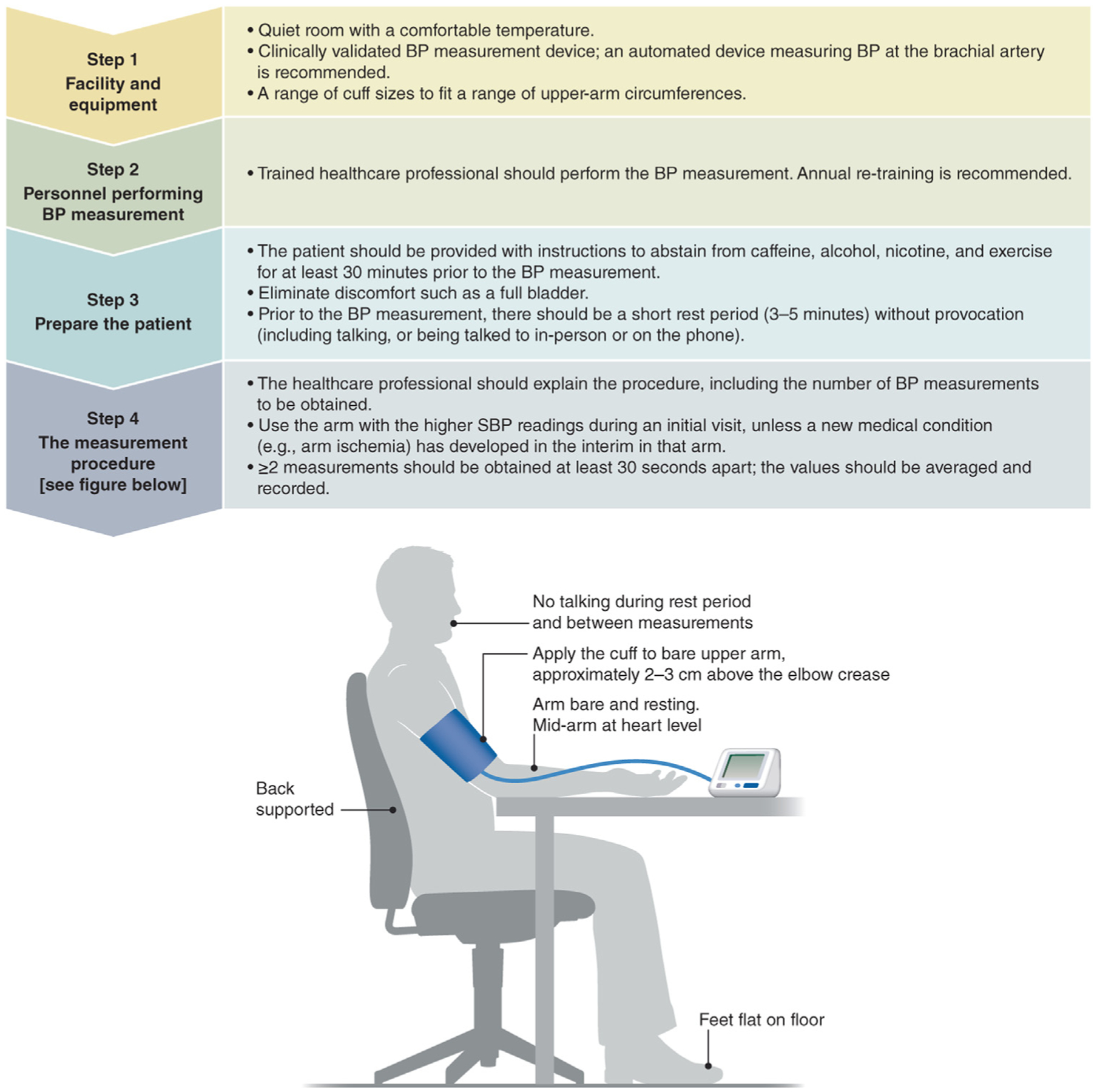
Steps for implementing standardized clinic BP measurement. BP = blood pressure; SBP = systolic blood pressure.
Additional comments on the steps of implementation in the Figure.
Facility and Equipment
- An automated upper-arm cuff monitor is strongly recommended for several reasons.
- It eliminates human error associated with manual devices (eg, those due to hearing impairment and digit preference) and requires less training.
- It minimizes interactions between the patient and health care professionals and, therefore, distractions during the preparatory and BP measurement phases.
- It allows the health care professionals to perform other tasks during the measurements.
- Upper-arm (brachial) BP measurements have been used in many large, randomized, controlled outcome hypertension trials.
Properly validated automated BP monitors with upper-arm cuff are listed in Table 1. The authors do not endorse any specific brand or model.
Details of facility and equipment requirements can be found in published practice guidelines and position statements (Appendix 1, available online).
Electronic monitors for children, pregnant women, and individuals with a large arm circumference (>42 cm) should be validated in dedicated clinical studies that address these specific populations. The reader is referred to the manufacturer’s instructions and relevant literature for detailed information for these populations.
Table 1.
Organizations Providing Online Lists of Validated BP Monitors
| Organization | Monitor lists (language) | Scientific association | Website |
|---|---|---|---|
| STRIDE BP | International (English, Chinese, Spanish) | European Society of Hypertension - International Society of Hypertension - World Hypertension League | www.stridebp.org |
| BIHS | UK, Ireland (English) | British and Irish Hypertension Society | www.bihsoc.org/bp-monitors |
| VDL | US (English) | American Medical Association | www.validatebp.org |
| Hypertension Canada | Canada (English) | Hypertension Canada | www.hypertension.ca/bpdevices |
| Deutsche Hochdruckliga | Germany (German) | German High Pressure League | www.hochdruckliga.de/betroffene/blutdruckmessgeraete-mit-pruefsiegel |
| JSH | Japan (Japanese) | Japanese Society of Hypertension | www.jpnsh.jp/com_ac_wg1.html |
BP = blood pressure; STRIDE BP = Science and Technology for Regional Innovation and Development in Europe Blood Pressure; VDL = validated device listing.
Two websites are not associated with a scientific organization (www.dableducational.org, www.medaval.ie). Modified from 2021 ESH practice guidelines for blood pressure measurement.17
Personnel Performing BP Measurement
Patient preparation and BP measurement should be performed by medical staff or health care professionals who are trained in these procedures. Retraining on a routine basis (eg, annually) is helpful to ensure proficiency.24
Systematic certification and regular recertification will promote proper training and retraining of proper BP measurement.
Details on descriptions of qualifications, training. and certifications of personnel performing BP measurements can be found in published practice guidelines and position statements (Appendix 1, available online).
Prepare the Patient
Proper preparation by and of the patient is essential regardless of the equipment used.
There should be a rest period of 3–5 minutes prior to the BP measurement to minimize stressors that may increase BP. However, clinical judgment should be exercised on the individual circumstance to determine whether this duration of rest is sufficient to achieve the goal.
If the patient has not been adequately prepared (eg, the patient has ingested caffeine immediately prior to the clinic visit), repeat BP measurements at a later time during the visit should be considered.
Measurement Procedure
There is unanimous agreement among the work group members that BP should be measured at least 2 times and the readings should be averaged, without specifying whether any reading should be discarded. Automated averaging is performed by several BP monitors.
There is no consensus on the importance of whether BP measurements should be conducted in the absence of a health care professional in the room, a condition referred to as unattended office BP. Some automated monitors allow repeat measurements to be made unattended, which has the advantage of minimizing distraction prior to and during the measurements. The presence of medical staff or a health care professional is, of course, necessary for manual measurements.
BP measurement on the bare arm is recommended. Although some of the authors feel that thin clothing may be acceptable, it is not ideal because the thickness of clothing on individual patients may be difficult to quantify.
Details on the BP measurement procedure can be found in published guidelines and position statements (Appendix 1, available online).
RATIONALE FOR STANDARDIZED CLINIC BP MEASUREMENT
Almost all of the cohort studies that estimated BP-related cardiovascular disease risks and the randomized controlled trials that underpin the recommendations for antihypertensive treatment and BP treatment goals for adults with high BP have employed standardized BP measurements in the clinic. Hence, guideline committees and professional societies have repeatedly emphasized the importance of standardized clinic BP measurements that aim to minimize systematic and random errors in estimation. The practice of evidence-based medicine and the likelihood of achieving outcome results similar to those shown in randomized controlled trials require adherence to these recommendations.
Standardization is essential because there are many aspects of BP measurement, including the patient’s physical condition, clinic environment, and equipment that can readily result in inaccurate and unreliable values.23,25,26 A systematic review of 328 articles found 29 components of the BP measurement procedure that can affect systolic BP (SBP) and diastolic BP (DBP) levels.27 Clinic BP measurements that do not follow a standardized protocol are likely to result in inaccurate and highly variable readings from one clinic visit to the next, making targeting a specified BP goal very challenging.
Usually, BP readings obtained in nonstandardized practice in the clinic are higher than those obtained by standardized measurements.15,26,28–30 Therefore, the use of nonstandardized clinic BP measurements tend to result in overtreatment. In contrast, for some people, routine clinic BP readings are lower than those obtained following a standardized protocol,29,30 resulting in a missed opportunity to detect high BP or the need to intensify antihypertensive treatment. Further, the variability of nonstandardized BP at the individual patient level is very large. Hence, there is no algorithm that can reliably convert BP values measured in a nonstandardized fashion to standardized measurement equivalents for patient management.
The lack of standardized BP measurement also makes it difficult to accurately determine the prevalence of under-treatment or overtreatment of BP from a population-health standpoint. It has been estimated that approximately 1 in 5 US adults could have their hypertension diagnosis or control status misclassified if BP were measured in a nonstandardized manner.27
ROLE OF HOME BP MONITORING AND AMBULATORY BP MONITORING
Many guidelines advocate greater use of out-of-clinic BP measurement (ie, home BP monitoring [HBPM] or ambulatory BP monitoring [ABPM]) to confirm the diagnosis of hypertension and guide BP management.10,11,15,17 The advantages, limitations, and applications of ABPM and HBPM have been detailed by many guidelines and position statements,10,17,22,31 including the ability to detect white-coat and masked hypertension. However, no large randomized controlled outcome trial addressing BP targets or anti-hypertensive drugs has used ABPM or HBPM to guide management. As such, the evidence base to support BP targets using ABPM or HBPM is uncertain and their role at present should be considered complementary to standardized clinic BP measurements, unless clinic BP measurements are unavailable.23
BARRIERS TO IMPLEMENTATION OF STANDARDIZED CLINIC BP MEASUREMENTS
The barriers to standardized BP measurements are well recognized (Table 2). However, studies have also shown that addressing these barriers can dramatically improve the quality of clinic BP measurements.32–36
Table 2.
Barriers and Solutions to Implementation of Standardized Clinic BP Measurement
| Barriers | Solutions | |||
|---|---|---|---|---|
| Patient | Health care professional | Institution | Government, regulatory, reimbursement agencies | |
| Equipment | Become educated and demand proper equipment, such as a validated monitor and proper cuff size | Acquire or demand properly validated equipment and cuffs for different arm sizes | Recognize importance of standardized measurement and provide properly validated equipment, and cuffs for different arm sizes | Mandate or incentivize proper equipment |
| Workflow | Facilitate by preparing for measurement before clinic appointment | Coordinate workflow with institution and clinic staff | Optimize workflow to accommodate standardized measurement | Facilitate institutions to develop policies and procedures |
| Staff | Not applicable | Demand and facilitate training and developing standardized procedures; promote team-based approach | Facilitate and mandate training and certification; ensure adequate staffing; promote team-based approach | Mandate training and certification |
| Patients | Become educated on the importance of and demand standardized measurements | Provide education to patients; provide reminders prior to clinic visit; explain and facilitate the procedure | Empower patient by informing and inviting comments and concerns about their BP measurements36 | Conduct education campaigns |
| Cost | Understand that standardized BP measurement and proper BP management are important for favorable clinical outcome and cost-effective care | Facilitate patient preparation and optimization of workflows that do not significantly increase costs | Recognize importance of standardized BP measurement in affecting clinical outcomes and population health; facilitate patient preparation and optimize workflow that does not significantly increase costs | Incentivize standardized measurements; encourage development of low-cost monitors |
BP = blood pressure.
Appreciation of importance of standardized BP measurement by health care workers. Many health care workers are unaware of the large degree of variability of nonstandardized BP measurement and its implications for patient safety.
Patient knowledge. Patients are usually unaware of the importance and procedures of standardized BP measurements as well as the clinical consequences of poor-quality BP measurements.
Equipment. In some world regions, a stable source of electricity for automated BP monitors is not available. The limited availability of cuffs with various sizes is another common barrier.
Staff training. Many health professionals are inadequately trained, and many clinics lack training and certification schedules and procedures, including curricula.
Environment and workflow. A major challenge can be the clinic space, environment, and time constraints. During the BP measurement procedure, health care staff are often taking other vital signs or medical history or are performing other tasks in the room. Triage is often performed in busy and noisy spaces where resting prior to BP measurements is difficult. Examination rooms (eg, with wall-mounted aneroid devices) lack appropriate configuration for proper BP measurement. Often, insufficient time is built into the visit schedule for proper patient preparation and BP measurements.
Regulatory and system oversight of quality standards. Although many aspects of clinical practice are subjected to quality assessment and mandatory training, BP measurement does not fall into this category. In fact, the measurement procedure is even much less regulated than the manufacturing of BP monitors.
SOLUTIONS TO OVERCOME BARRIERS AND SUCCESS STORIES
Be Pragmatic, Not Dogmatic
Many clinics have workflow constraints, with BP measurement being only one of many tasks assigned to members of the health care team. Thus, the standardized BP measurement procedure must be pragmatic, time-efficient, patient- and staff-friendly, and focused on essential aspects of the measurement process (Figure) that contribute to large errors and avoid being dogmatic regarding elements in which both supporting evidence and theoretical basis are not rigorous.
Roles of Patients and Clinic Personnel
A concerted effort by patients, health care professionals, health care institutions, government, and other payers, and professional societies can overcome barriers to wide adoption of standardized clinic BP measurements (Table 2). Well-informed patients will expect and demand high-quality, standardized BP measurements, and automated reminder messages advise the patients to make proper preparations in advance.
Clinic personnel should be trained and preferably certified in standardized BP measurement and receive regularly scheduled refresher training and undergo annual recertification. A number of training videos are available online (https://www.whleague.org/whl-resources/awareness-and-screening/new-online-bp-certification-course; https://targetbp.org/blood-pressure-improvement-program/control-bp/measure-accurately/accurate-bp-measurement-matters/). Organizations such as the World Hypertension League and STRIDE BP (https://www.stridebp.org/training) offer brief online BP measurement training and certification geared toward health workers from all countries.37 Brief health worker trainings have been shown to be effective. For example, after receiving instructions in a brief curriculum in standardized hypertension screening and management, 33 health care professionals staffing 18 primary care clinics in Tanzania substantially improved BP measurement knowledge and BP measurement techniques.38 Countries where physicians currently execute all tasks related to BP measurement and management may be ill-equipped to support the implementation of standardized BP measurements;39 these countries may need to adopt team-based approaches that include non-physician personnel.
Roles of Institutions and Governments
Health care institutions can prioritize standardized BP measurement by providing clinically validated BP monitors, adequate space, adequate staffing, efficient clinic workflow plans, regularly scheduled training of personnel, quality-improvement practices, and incentive programs based on objective benchmarks. Governments and payers can promote standardization by requiring or incentivizing its practice, in addition to dissemination of patient education materials, providing data sharing, and using value-based instead of fee-for-service payment models. Positive and negative financial and nonfinancial incentives provided by government regulatory agencies, health care funding agencies and health care institutions are often effective in modifying medical practice, for example, by disseminating educational materials via lectures and postings on their websites.
Standardized BP Measurements in Clinics Are Feasible
Several examples support the premise that implementing standardized BP measurement is feasible in primary health care settings, admittedly mostly in high-income countries. The US Centers for Disease Control and Prevention’s Million Hearts Hypertension Control Champions and the American Medical Association/American Heart Association’s TargetBP recognition programs both promote higher national standards for BP measurement through health care institution best-practice facilitation, training, and certification.40,41 One cornerstone of the successful Kaiser Permanente Hypertension program was the unfettered availability of automated BP monitors.35 This approach has also been successfully replicated in San Francisco Health Network safety-net clinics, which provide care to predominantly minoritized and low-income patients.34 The amount of time required to perform standardized BP measurement is minimal if the clinic workflow is streamlined with an automated BP monitor.33 The “Measure accurately, Act rapidly and Partner with patients” (MAP) protocol used a practice facilitation model to transition 16 South Carolina primary care clinics and more than16,000 patients from usual care BP measurement practices to standardized BP measurement.42 Transition to higher BP measurement standards was successful and, in fact, favored by participating health care workers.42
Low- and middle-resource health care systems may struggle to implement standardized clinic BP measurements due to scarcity of BP monitors, optimal clinic environment, personnel training, and other barriers. HEARTS in the Americas, the adaptation of WHO Global HEARTS initiative, promote and implement strategic approaches to improve the BP accuracy, including a simple and standardized measurement protocol and clinically validated BP devices (https://www.paho.org/en/hearts-americas/hearts-americas-blood-pressure-measurement).43
Be Proactive and Persistent
Despite the clear rationale and necessity for standardized BP measurement, any change to clinic workflow, particularly when it involves multiple stakeholders such as patients, health care providers, institutions, and administrators, is likely to be met with resistance. Early and periodic active engagement of these parties to set common goals and execute the plans will be necessary.
CALL TO ACTION
Health care professionals. Adopt standardized clinic BP measurement; educate patients and staff on its importance; coordinate efforts with health care institutions.
Health care institutions. Recognize the importance of standardized clinic BP measurements; provide proper equipment, clinic space, time, staffing, and workflow; mandate and facilitate staff training and certification.
Health care funding agencies. Provide positive and/or negative financial incentives for standardized clinic BP measurements.
BP monitor manufacturers. Provide and maintain BP equipment and cuffs for various populations at reasonable prices. Support independent researchers to validate equipment.
Government regulatory agencies. Recognize the importance of standardized clinic BP measurement on public health; educate the public, health care providers, and institutions; and mandate training and certification of staff.
Professional societies. Promote the importance of standardized clinic BP measurement; educate the public and health care providers.
The importance of clinic BP measurement has been recognized for many decades but adherence to guidelines on proper, standardized BP measurement remains uncommon in clinical practice. The time has come that all parties must collaborate actively to make standardized clinic BP measurement a routine procedure in order to improve BP control and public health.
ACKNOWLEDGMENT
The Work Group would like to acknowledge the work of Amy Earley, Michael Cheung, Melissa Thompson, and Debbie Maizels for their support during the development this manuscript.
Conflicts of Interest:
AKC declared having received consultancy fees from Boehringer Ingelheim; he reported having served on an expert committee for Boehringer Ingelheim; and has stock/stock options in Merck. AES declared having received speaker honoraria from Omron Healthcare and Aktiia. BW declared having received research support and speaker honoraria from Omron Cooperation*. PS declared having received research support from Elpen Pharmaceuticals* and Servier*; he declared having received consultancy fees from Primeview* and ReCor Medical*; and declared having received speaker honoraria from Sanofi* and Winmedica*. TIC declared having received consultancy fees from George Clinical, Gilead*, Novo Nordisk, and Bayer*; she reported having served on an expert committee for AstraZeneca, and Bayer. SSD declared having received speaker honoraria from Servier. RK declared having received speaker honoraria from Bayer, Berlin-Chemie, Daiichi-Sankyo, Ferrer, Menarini, Merck, Sanofi, and Servier. JMF declared having received research support from GlaxoSmithKline, Indorsia, Quantum Genomics, ReCor Medical, and Vascular Dynamics; he declared having received consultancy fees from ReCor Medical and Sanofi; he reported having received payment for expert testimony from Teva; he reported having served on an expert committee for Amgen, Fibrogen, and Janssen; and has stock/stock options in Amphastar and CVS. GM declared having received speaker honoraria from Boehringer Ingelheim, Gedeon Richter, Medtronic, Menarini, Merck, Sandoz, Sanofi, and Servier. PO is staff member of the Pan American Health Organization (PAHO). The authors hold sole responsibility for the views expressed in the manuscript, which may not necessarily reflect the opinion or policy of PAHO. RP declared being the Chief Executive Officer at mmHg, Inc. AP declared having received research support from Ablative Solutions, Quantum Genomics, Recor Medical, and Servier; he reported having served on an expert committee for Ablative Solutions and Quantum Genomics. MS declared having received research support from Abbott, Idorsia, Medtronic, Metavention, ReCor; he reported having received speaker honoraria from Abbott, Medtronic, and ReCor; and support for travel from Medtronic*. GSS declared having received research support from Braun*, InBody*, and Microlife*; he declared having received consultancy fees from Huawei, InBody, and Microlife. SWT declared having received consultancy fees from AstraZeneca*; he declared having received speaker honoraria from Amgen*, AstraZeneca*, BMS*, Bayer*, Boehringer Ingelheim*, Janssen*, Eli Lily and Company*, Novartis*, Novo Nordisk*, Pfizer*, and Sanofi-Genzyme*. JFEM declared having received research support from Novo Nordisk; he declared having received consultancy fees from AstraZeneca, Boehringer Ingelheim, Bayer, and Novartis; and declared having received speaker honoraria from AstraZeneca, Bayer, Fresenius, Novartis, and Novo Nordisk. All the other authors declared no competing interests. *Monies paid to institution.
Appendix Table.
Published Practice Guidelines and Positions Statements on Blood Pressure Measurement
| Organization | Most recent guideline | URL |
|---|---|---|
| ACC/AHA | ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines | https://www.ahajournals.org/doi/full/10.1161/HYP.0000000000000066?rfr_dat=cr_pub+0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org |
| AHA | Measurement of Blood Pressure in Humans | https://www.ahajournals.org/doi/full/10.1161/HYP.0000000000000087?rfr_dat=cr_pub+0pubmed&url_ver=Z39.88-2003&rfr_id=ori%3Arid%3Acrossref.org |
| A Scientific Statement from the American Heart Association | ||
| ESC/ESH | 2018 ESC/ESH Guidelines for the management of arterial hypertension | https://journals.lww.com/jhypertension/Fulltext/2018/10000/2018_ESC_ESH_Guidelines_for_the_management_of.2.aspx |
| The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension | ||
| ESH | 2021 European Society of Hypertension practice guidelines for office and out-of-office blood pressure measurement | https://journals.lww.com/jhypertension/Fulltext/2021/07000/2021_European_Society_of_Hypertension_practice.5.aspx |
| Hypertension Canada | Hypertension Canada’s 2020 Comprehensive Guidelines for the Prevention, Diagnosis, Risk Assessment, and Treatment of Hypertension in Adults and Children | https://www.onlinecjc.ca/action/showPdf?pii=S0828-282X%2820%2930191-4 |
| ISH | 2020 International Society of Hypertension Global Hypertension Practice Guidelines | https://www.ahajournals.org/doi/epdf/10.1161/HYPERTENSIONAHA.120.15026 |
| KDIGO | KDIGO 2021 Clinical Practice Guideline for the Management of Blood Pressure in Chronic Kidney Disease | https://kdigo.org/wp-content/uploads/2016/10/KDIGO-2021-BP-GL.pdf |
| Lancet Commission for Hypertension | Optimizing observer performance of clinic blood pressure measurement | https://journals.lww.com/jhypertension/Fulltext/2019/09000/Optimizing_observer_performance_of_clinic_blood.2.aspx |
| A position statement from the Lancet Commission on Hypertension Group | ||
| Lancet Commission for Hypertension | Lancet Commission on Hypertension group position statement on the global improvement of accuracy standards for devices that measure blood pressure | https://journals.lww.com/jhypertension/pages/articleviewer.aspx?year=2020&issue=01000&article=00004&type=Fulltext |
| National Heart Foundation Australia | Guideline for the diagnosis and management of hypertension in adults (2016) | https://www.heartfoundation.org.au/getmedia/c83511ab-835a-4fcf-96f5-88d770582ddc/PRO-167_Hypertension-guideline-2016_WEB.pdf |
| National Heart, Lung, and Blood | Blood Pressure Assessment in Adults in Clinical Practice and Clinic-Based Research | https://www.sciencedirect.com/sdfe/reader/pii/S0735109718392738/pdf |
| JACC Scientific Expert Panel | ||
| NICE | Hypertension in adults: diagnosis and management | https://www.nice.org.uk/guidance/ng136/resources/hypertension-in-adults-diagnosis-and-management-pdf-66141722710213 |
| PAHO | HEARTS in the Americas: Guide and Essentials for Implementation | https://iris.paho.org/bitstream/handle/10665.2/55804/9789275125281_eng.pdf?sequence=1&isAllowed=y |
| WHO | WHO technical specifications for automated non-invasive blood pressure measuring devices with cuff | https://apps.who.int/iris/handle/10665/331749 |
AAPA = American Academy of Physician Assistants; ABC = Association of Black Cardiologists; ACC = American College of Cardiology; ACPM = American College of Preventive Medicine; AGS = American Geriatrics Society; AHA = American Heart Association; APhA = American Pharmacists Association; ASH = American Society of Hypertension; ASPC = American Society for Preventive Cardiology; ESH = European Society of Hypertension; ESC = European Society of Cardiology; ISH = International Society of Hypertension; KDIGO = Kidney Disease: Improving Global Outcomes; NICE = National Institute for Health and Care Excellence; NMA = National Medical Association; PAHO = Pan American Health Organization; PCNA = Preventive Cardiovascular Nurses Association; WHO = World Health Organization.
Footnotes
SUPPLEMENTARY MATERIALS
Supplementary data to this article can be found online at https://doi.org/10.1016/j.amjmed.2022.12.015.
References
- 1.Flint AC, Conell C, Ren X, et al. Effect of systolic and diastolic blood pressure on cardiovascular outcomes. N Engl J Med 2019;381(3):243–51. [DOI] [PubMed] [Google Scholar]
- 2.Fuchs FD, Whelton PK. High blood pressure and cardiovascular disease. Hypertension 2020;75(2):285–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.He J, Whelton PK. Elevated systolic blood pressure and risk of cardiovascular and renal disease: overview of evidence from observational epidemiologic studies and randomized controlled trials. Am Heart J 1999;138(3 Pt 2):211–9. [DOI] [PubMed] [Google Scholar]
- 4.Rapsomaniki E, Timmis A, George J, et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet 2014;383(9932):1899–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blood Pressure Lowering Treatment Trialists Collaboration. Pharmacological blood pressure lowering for primary and secondary prevention of cardiovascular disease across different levels of blood pressure: an individual participant-level data meta-analysis. Lancet 2021;397(10285):1625–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bundy JD, Li C, Stuchlik P, et al. Systolic blood pressure reduction and risk of cardiovascular disease and mortality: a systematic review and network meta-analysis. JAMA Cardiol 2017;2(7):775–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet 2016;387(10022):957–67. [DOI] [PubMed] [Google Scholar]
- 8.Sharman JE, O’Brien E, Alpert B, et al. Lancet Commission on Hypertension group position statement on the global improvement of accuracy standards for devices that measure blood pressure. J Hyper-tens 2020;38(1):21–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gabb GM, Mangoni AA, Anderson CS, et al. Guideline for the diagnosis and management of hypertension in adults - 2016. Med J Aust 2016;205(2):85–9. [DOI] [PubMed] [Google Scholar]
- 10.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension 2018;71(6):1269–324. [DOI] [PubMed] [Google Scholar]
- 11.Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: The Task Force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens 2018;36(10):1953–2041. [DOI] [PubMed] [Google Scholar]
- 12.National Institute for Health and Care Excellence (NICE). Hypertension in adults: diagnosis and management. [NICE guideline NG136]. Available at: https://www.nice.org.uk/guidance/ng136. Accessed January 29, 2020. [PubMed] [Google Scholar]
- 13.Rabi DM, McBrien KA, Sapir-Pichhadze R, et al. Hypertension Canada’s 2020 comprehensive guidelines for the prevention, diagnosis, risk assessment, and treatment of hypertension in adults and children. Can J Cardiol 2020;36(5):596–624. [DOI] [PubMed] [Google Scholar]
- 14.Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension global hypertension practice guidelines. J Hypertens 2020;38(6):982–1004. [DOI] [PubMed] [Google Scholar]
- 15.Kidney Disease: Improving Global Outcomes Blood Pressure Work Group. KDIGO 2021 clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int 2021;99(3S): S1–S87. [DOI] [PubMed] [Google Scholar]
- 16.Pan American Health Organization. HEARTS in the Americas: Guide and Essentials for Implementation. Washington, DC: Pan American Health Organization; 2022. 10.37774/9789275125281 Accessed April 25, 2022. [DOI] [Google Scholar]
- 17.Stergiou GS, Palatini P, Parati G, et al. 2021 European Society of Hypertension practice guidelines for office and out-of-office blood pressure measurement. J Hypertens 2021;39(7):1293–302. [DOI] [PubMed] [Google Scholar]
- 18.Stergiou G, Kollias A, Parati G, O’Brien E. Office blood pressure measurement: the weak cornerstone of hypertension diagnosis. Hyper-tension 2018;71(5):813–5. [DOI] [PubMed] [Google Scholar]
- 19.Muntner P, Einhorn PT, Cushman WC, et al. Blood pressure assessment in adults in clinical practice and clinic-based research: JACC Scientific Expert Panel. J Am Coll Cardiol 2019;73(3):317–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Muntner P, Shimbo D, Carey RM, et al. Measurement of blood pressure in humans: a scientific statement from the American Heart Association. Hypertension 2019;73(5):e35–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Padwal R, Campbell NRC, Schutte AE, et al. Optimizing observer performance of clinic blood pressure measurement: a position statement from the Lancet Commission on Hypertension Group. J Hyper-tens 2019;37(9):1737–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.O’Brien E, Parati G, Stergiou G, et al. European Society of Hypertension position paper on ambulatory blood pressure monitoring. J Hypertens 2013;31(9):1731–68. [DOI] [PubMed] [Google Scholar]
- 23.Hwang KO, Aigbe A, Ju HH, Jackson VC, Sedlock EW. Barriers to accurate blood pressure measurement in the medical office. J Prim Care Community Health 2018;9(1–7):2150132718816929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bruce NG, Shaper AG, Walker M, Wannamethee G. Observer bias in blood pressure studies. J Hypertens 1988;6(5):375–80. [PubMed] [Google Scholar]
- 25.Kallioinen N, Hill A, Horswill MS, Ward HE, Watson MO. Sources of inaccuracy in the measurement of adult patients’ resting blood pressure in clinical settings: a systematic review. J Hypertens 2017;35(3):421–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Picone DS, Padwal R, Campbell NRC, et al. How to check whether a blood pressure monitor has been properly validated for accuracy. J Clin Hypertens (Greenwich) 2020;22(12):2167–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sakhuja S, Jaeger BJ, Akinyelure OP, et al. Potential impact of systematic and random errors in blood pressure measurement on the prevalence of high office blood pressure in the United States. J Clin Hypertens (Greenwich) 2022;24(3):263–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.STRIDE BP. An international scientific organization founded by hypertension experts with the mission of improving the diagnosis and management of hypertension. Available at: https://www.stridebp.org/. Accessed January 26, 2022.
- 29.Agarwal R Implications of blood pressure measurement technique for implementation of systolic blood pressure intervention trial (SPRINT). J Am Heart Assoc 2017;6(2):e004536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Drawz PE, Agarwal A, Dwyer JP, et al. Concordance between blood pressure in the systolic blood pressure intervention trial and in routine clinical practice. JAMA Intern Med 2020;180(12):1655–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Parati G, Stergiou GS, Bilo G, et al. Home blood pressure monitoring: methodology, clinical relevance and practical application: a 2021 position paper by the Working Group on Blood Pressure Monitoring and Cardiovascular Variability of the European Society of Hypertension. J Hypertens 2021;39(9):1742–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Boonyasai RT, Carson KA, Marsteller JA, et al. A bundled quality improvement program to standardize clinical blood pressure measurement in primary care. J Clin Hypertens (Greenwich) 2018;20(2):324–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Doane J, Buu J, Penrod MJ, Bischoff M, Conroy MB, Stults B. Measuring and managing blood pressure in a primary care setting: a pragmatic implementation study. J Am Board Fam Med 2018;31(3):375–88. [DOI] [PubMed] [Google Scholar]
- 34.Fontil V, Gupta R, Moise N, et al. Adapting and evaluating a health system intervention from Kaiser Permanente to improve hypertension management and control in a large network of safety-net clinics. Circ Cardiovasc Qual Outcomes 2018;11(7):e004386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jaffe MG, Young JD. The Kaiser Permanente Northern California story: improving hypertension control from 44% to 90% in 13 years (2000 to 2013). J Clin Hypertens (Greenwich) 2016;18(4):260–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Elias MF, Goodell AL. Human errors in automated office blood pressure measurement: still room for improvement. Hypertension 2021;77(1):6–15. [DOI] [PubMed] [Google Scholar]
- 37.Campbell NRC, Khalsa T, Ordunez P, et al. Brief online certification course for measuring blood pressure with an automated blood pressure device. A free new resource to support World Hypertension Day Oct 17, 2020. J Clin Hypertens (Greenwich) 2020;22(10):1754–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Edward A, Kagaruki GB, Manase F, Appel LJ, Matsushita K. Effectiveness of instructional videos for enhancing healthcare provider competencies for hypertension management - a pre-post study in primary healthcare settings, Tanzania. BMC Health Serv Res 2022;22(1):721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Giraldo GP, Joseph KT, Angell SY, et al. Mapping stages, barriers and facilitators to the implementation of HEARTS in the Americas initiative in 12 countries: a qualitative study. J Clin Hypertens (Greenwich) 2021;23(4):755–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Million Hearts Champions program. Hypertension Control Champions. Available at: https://millionhearts.hhs.gov/partners-progress/champions/index.html. Accessed January 26, 2022.
- 41.AHA/AMA. Target BP Recognition Program. Available at: https://targetbp.org/recognition-program/. Accessed January 26, 2022.
- 42.Egan BM, Sutherland SE, Rakotz M, et al. Improving hypertension control in primary care with the measure accurately, act rapidly, and partner with patients protocol. Hypertension 2018;72(6):1320–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ordunez P, Lombardi C, Picone DS, et al. HEARTS in the Americas: a global example of using clinically validated automated blood pressure devices in cardiovascular disease prevention and management in primary health care settings [e-pub ahead of print]. J Hum Hypertens. 10.1038/s41371-022-00659-z. Accessed March 15, 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]


