Abstract
Objective.
Multi-level treatment barriers prevent up to 80% of individuals experiencing eating disorders (EDs) from accessing care. This treatment gap creates a critical need to identify interventions that are accessible, easily completable, and optimized for effectiveness by targeting core mechanisms linked to ED onset and maintenance. We propose single-session interventions (SSIs) as a promising path toward catalyzing innovation in the development of accessible, effective ED interventions. SSIs are structured programs that intentionally involve one encounter with a program or provider; they may serve as stand-alone or adjunctive clinical supports. All SSIs are built to acknowledge that any session might be someone’s last—and that any single session can nonetheless yield meaningful clinical benefit.
Method.
We define SSIs, summarize research supporting their utility for ED symptoms and other mental health problems, and recommend future directions for work in this domain.
Results.
SSIs may hold promise to reduce some ED symptoms and risk factors, including restrictive eating and negative body image. Steps toward realizing this promise include (1) testing whether existing evidence-based SSIs (e.g., for depression) can also reduce EDs, risk factors, and symptoms; (2) developing novel SSIs that target modifiable ED risk factors and symptoms largely unaddressed by SSIs, such as purging and binge eating; (3) studying diverse implementation pathways; (4) capitalizing on SSIs’ transdiagnostic utility to broaden funding opportunities; and (5) educating ED researchers and clinicians about SSIs.
Discussion.
Understanding the strengths and limits of mechanism-targeted SSIs for ED-related problems could be a low-risk, high-reward avenue towards reducing EDs at scale.
The gap between need for mental health support and access to effective care is costly, persistent, and profound. In the United States alone, up to 50% of adults and 80% of children with treatment needs go without care each year (Kazdin & Rabbitt, 2013; Konrad et al., 2009). Although this gap exists across virtually all mental health conditions, it is dire among individuals with eating disorders (EDs). Despite considerable progress in the identification of effective treatments for eating disorders, most EDs go undetected or un(der)treated, with just 10–30% of individuals with EDs in the United States accessing any form of treatment whatsoever (Eisenberg et al., 2011; Hudson et al., 2007). Even for the few who do receive care, few access evidence-based treatments (EBTs), and EBTs only lead to symptom remission for 30–40% of patients (Fairburn et al., 2015; McIntosh et al., 2016; Wonderlich et al., 2014), leading a growing chorus of prominent ED researchers to call for new approaches to intervention science within the field, including innovative strategies for prevention and treatment alike (Kass et al., 2017; Kazdin et al., 2017; Taylor et al., 2020; Stice et al., 2021).
These treatment access gaps reflect personal, structural, and logistical access barriers to existing ED interventions. First, societal and self-stigma around EDs often precludes people from seeking support, and this same stigma can increase odds of treatment dropout for those who do access care (Foran et al., 2020). Second, most health service providers lack any formal training in treating individuals with EDs, contributing to national and international ED provider shortages. Third, and perhaps most centrally, many EBTs that do exist for EDs are structurally incompatible with real-world implementation and access. Some EDs, such as anorexia nervosa, may require inpatient treatment many months of intensive, one-to-one sessions, are designed for delivery by interdisciplinary teams of highly trained providers (including psychiatrists, psychologists, and dieticians), which can be incredibly costly for patients and families and require acceess to brick-and-mortar clinics. EBTs for other types of eating disorders may be briefer—for instance, involving 8 to 10 sessions of cognitive-behavioral therapy (Davey et al., 2022)—but these approaches are seldom used in practice, with clinicians tending toward longer-than recommended interventions that lack evidence-based components (e.g., exposure, tracking weight; Mulkens et al., 2018). Indeed, even the mean amount of patient time, resources, and commitment required to engage in shorter-term EBTs for EDs stands in contrast with real-world treatment utilization patterns. Among those who begin mental health treatment, the most common number of psychotherapy sessions people actually receive is just one—a statistic consistent across studies from Australia, the US, Canada, Mexico, Japan, and Spain (Weir et al., 2008; Abel et al., 2022; Barrett et al., 2008; Ono et al., 2011; Bados et al., 2007). Given the wide treatment gap and the low treatment utilization patterns among those who are successful in starting treatment, preventing EDs is a top priority (Kazdin et al., 2017). Multiple approaches to evidence-based prevention have been shown to significantly reduce ED onset, but these promising findings are dampened by the fact that, as with ED treatment, attendance and completion of ED prevention programs is low (Stice et al., 2021), which may result in poorer outcomes (Linardon et al., 2020). There is an urgent need to identify ED supports that overcome structural limitations of traditional interventions and prevention programs; that may be sustainably, reliably offered in real-world settings; and that are built to reach the many individuals with and at-risk for EDs who are unlikely or unable to access support at all.
Recent innovations in intervention science have spurred the development, evaluation, and dissemination of interventions that may help meet this need, including work evaluating relatively brief, digital and self-guided, and lay-provider delivered programs to treat and prevent a variety of mental health problems (O’Mara et al., 2023). However, only a small portion of these interventions explicitly target ED symptoms or risk factors, which reflects a history of siloing of ED-focused treatment research from intervention research on depression, anxiety, and other common mental health problems (Haynos et al., under review). In addition to hampering integration of knowledge across ED- and non-ED-focused intervention research, this siloing may worsen rifts between ED research and practice, on the one hand, and patient needs and demands, on the other. Whereas some ED practitioners and researchers have veered toward longer-term, higher-intensity interventions (e.g., treatments for “severe and enduring” or so-called “terminal” eating disorders, e.g., Kotilahti et al., 2020), experts by experience have called for a focus on scalable, accessible ED supports (Downs et al., 2023). Although leading professional organizations already recommend brief, low-intensity ED interventions as first-line supports (such as guided self-help as a first-line support; National Guideline Alliance UK, 2017), these guidelines are inconsistently followed, and evidence-based, low-intensity interventions are not easily accessible to those without access to a trained provider (Mulkens et al., 2018). Further, existing brief and digital interventions for EDs have only modest effects on symptoms relative to treatments for other symptom types (e.g., depression, anxiety; see Davey et al., 2022, and Weisz et al., 2017), and premature dropout remains high even in relatively brief ED interventions (Fassino et al., 2009), suggesting continued needs for scalable ED interventions that are both easily completable and optimized for effectiveness by targeting core mechanisms linked to ED onset and maintenance.
We therefore propose single-session interventions as a highly promising but virtually untapped opportunity to catalyze innovation in the design and implementation of accessible, effective ED supports. Our team at the Lab for Scalable Mental Health has written extensively about the promise of single-session interventions, or SSIs, for a diversity of mental health problems (Schleider et al., 2020a); indeed, more than 60 clinical trials with tens of thousands of participants now support their clinical utility for diverse mental health problems—including certain ED symptoms and risk factors, such as restrictive eating (Schleider et al., 2022) and negative body image (Smith et al., under review). However, there have been no efforts to formally introduce SSI research to the ED field, nor to outline how ED treatment and prevention research may capitalize on the SSI approach to increase access to targeted, evidence-based interventions. In the present paper, we aim to accomplish just that. First, we define SSIs and their potential roles within ecosystems of ED treatment and prevention. We then summarize literature supporting the utility of both digital (self-guided) and provider-delivered SSIs for (1) a variety of common mental health problems (e.g., depression, anxiety, behavior problems), and (2) ED-related symptoms and risk factors, in particular. Finally, we will overview recommendations and opportunities for developing, testing, and implementing SSIs for people at-risk for and experiencing ED symptoms and disorders, with the goal of complementing and extending existing systems of care. We are hopeful this viewpoint will offer a valuable roadmap for ED scientists and clinicians, supporting field-wide and cross-disciplinary efforts to increase access to treatment at scale.
A crucial caveat to the ideas presented below is that EDs are far from a monolithic condition. As such, best-fit applications of SSIs will necessarily vary by diagnosis, severity, and risk—and there is considerable work to be done toward uncovering which types of SSIs (and to what degree, and under what conditions) can yield sustainable benefits. We are not proposing that SSIs are equally capable of ameliorating EDs across diagnoses, severity levels, and contexts. Rather, we aim to provide a framework for field-wide discussions of how SSIs might be harnessed to (1) spur meaningful change for people experiencing diverse ED-related challenges; (2) forward accessible, evidence-based ED supports; (3) supplement existing ED treatment models; and (4) mitigate the individual, familial, and societal burdens of EDs at scale.
What are Single-Session Interventions (SSIs)?
SSIs are defined as “structured programs that intentionally involve only one visit or encounter with a clinic, provider, or program; they may serve as stand-alone or adjunctive clinical services” (Schleider et al., 2020a). Importantly, SSIs are designed for a “one-at-a-time” approach to intervention: Although they may be completed on multiple occasions or as adjuncts to intentionally longer-term care, they are designed such that any individual session holds potential to yield some degree of positive, meaningful change (Dryden, 2022; Schleider et al., 2020a). That is, SSIs acknowledge the dual realities that any given session might be someone’s last (whether or not they want or might benefit from additional support), and that any single-session can nonetheless yield meaningful benefit.
Often, SSIs target core mechanisms of longer-term mental health interventions, such as a program teaching a single evidence-based treatment strategy for depression (behavioral activation; self-compassion). However, their flexibility and brevity renders them inherently more scalable and lower-cost than their multi-session counterparts. SSIs may be delivered by trained providers or via digital, self-guided programs, and within diverse settings, from clinics to schools to smartphones.
Can SSIs improve mental health?
SSIs have helped improve diverse patient-level outcomes, from social connectedness to crisis resource uptake to substance use and depression. SSIs have increased motivation to empathize with others, empathic accuracy, and the number of friendships in college students (Weisz et al., 2021); decreased alcohol consumption among individuals with alcohol use disorder (Miller, 2000); increased distress tolerance and endorsement of positive parenting practices among high-anxiety parents of young children (Sung et al., 2021); decreased self-hatred and increased intentions to stop self-harming in youth with histories of non-suicidal self-injury (Schleider et al., 2020b; Dobias et al., 2021; Dobias et al., 2022); doubled uptake rates of mental health crisis resources among young people identified as at-risk within social media platforms (Cohen et al., in press); and produced clinically significant improvements in pain catastrophizing, pain intensity, and pain interference in adults with chronic lower back pain, with non-inferior effects to 8-session cognitive behavioral therapy (Darnell et al., 2021). In a randomized trial including 2,452 U.S. adolescents with elevated depressive symptoms, two digital, self-guided SSIs (one teaching behavioral activation; another teaching that personal characteristics are malleable) significantly reduced three-month depressive symptoms and hopelessness versus a control program designed to mimic supportive therapy (Schleider et al., 2022). In other randomized trials of the same SSIs, reductions in depression and anxiety symptoms have extended across 4–9 month follow-ups in clinical and community samples alike (Schleider et al., 2020c; Schleider & Weisz, 2018a). In a meta-analysis of 50 randomized-controlled trials (Schleider & Weisz, 2017), SSIs for youth mental health problems demonstrated a significant beneficial effect compared to control conditions, g = .32; reflecting a “small-to-medium” overall effect (Cohen, 2013), with follow-up periods ranging from two weeks to 24 months. SSI effects were consistent across prevention and treatment trials and regardless of participants’ diagnostic status, suggesting SSIs’ ability to benefit youth regardless of symptom severity. Further, significant SSI effects emerged even for SSIs that were self-guided (e.g., digital interventions) that involved no therapist (g = .32). Numerically, SSIs’ effects are slightly smaller than those for multi-session, evidence-based youth treatments (Weisz et al., 2017; mean g = .46 for treatments lasting a mean of 16 sessions)—but their relative accessibility may allow for broader, faster public health impact.
How can such brief interventions produce any positive change in complex mental health problems, let alone benefits lasting months post-intervention? Broadly, SSIs target theory-driven factors, or change mechanisms, that underlie sustained change in beliefs, emotions, and behaviors. Schleider and colleagues (2020a) describe a four-element process to designing SSIs that can spur meaningful clinical change, based on social psychology, learning science, and marketing research. These components are: (1) including scientific evidence and social-norming data to normalize patients’ experiences, increase buy-in, and boost the credibility of an SSI’s core message; (2) empowering patients to serve as “experts” (based on their lived experience with mental health problems), rather than passive recipients of treatment or information; (3) allowing users to share back what they learn through the SSI, in order to help others in similar circumstances navigate shared challenges; and (4) embedding testimonials and personal narratives from other people who have faced (and overcome) similar problems in their lives. Many SSIs also support patients in crafting an “action plan” for using the key skill taught in the SSI; the action plan is meant to build motivation, capacity, and self-efficacy in future skill use (Schleider et al., 2020a; Schleider et al., 2022). These four design components echo insights from participatory action research, which suggest the benefits of empowering traditionally-disempowered individuals (here, young people and/or patients in mental health care contexts) to ‘expert’ positions (Baum et al., 2006); self-determination theory, which suggests that boosting feelings of competence, agency, and relatedness motivate adaptive behavior change (Berg et al., 2009); and meta-analyses suggesting that narratives increase persuasiveness of health-related messaging (van Laer et al., 2019). Indeed, self-guided SSIs adhering to this four-part framework have significantly decreased hopelessness and strengthened perceived agency (Schleider et al., 2022; Schleider et al., 2020b) and have increased expectancies that changes in emotions and behaviors are possible (Schleider & Weisz, 2018a; Schleider & Weisz, 2018b), all of which are known to support clinical and behavior change. Moreover, evidence from SSI trials suggests that short-term changes in these outcomes (e.g., perceived control and agency) predict larger improvements in long-term clinical outcomes (e.g., depression, anxiety), suggesting these short-term targets as likely mechanisms of change in SSIs (Schleider et al., 2019). Notably, all four of these design principles may be integrated into even the briefest of SSIs, including those that have required just 5–8 minutes of users’ time (e.g., via inclusion of a single peer quotation, a single free-response item, or a two-sentence description of a psychoeducational concept). The SSI design components are recommendations for framing the content in a given SSI, which may then be constructed as a shorter (5 minutes) or longer (1 hour) program based on context- and problem-specific needs.
Can SSIs reduce eating disorders and risk factors?
While many treatments for EDs are designed to be long-term and high-intensity, research suggests that lower-intensity interventions can be effective as well. In fact, one recent meta-analysis found that, when compared to very high-intensity ED interventions, relatively low-intensity interventions—lasting 8 to 10 sessions—were superior at reducing eating disorder pathology at follow-up (g = 0.20, 95% CI: 0.01, 0.40; Davey et al., 2022). Further, NICE guidelines for the treatment of eating disorders indicates that self-help interventions—generally multi-session, but relatively low-intensity—should be a first line treatment for EDs in some cases (National Guideline Alliance, 2017). Research on single-session ED interventions is sparse, but also promising; a meta-analysis found that single-session interventions targeting ED symptoms and disorders had a large, albeit not statistically significant (as there were only three SSIs included in this sub-category), average effect (g = 1.05; 95% CI: −0.33, 2.93; Schleider & Weisz, 2017).
To date, most SSIs in this area have targeted known ED risk factors such as negative body image. On the whole, these interventions have shown small-to-medium effects at post-intervention and short-term follow-up. Single-session imagery rescripting has been shown to significantly impact body acceptance (ds 0.49 – 0.65), self-compassion (d = 0.59 – 0.61), disordered eating (ds 0.42 – 0.59), and global eating psychopathology (d = 0.60) at one-week follow-up among college-age women at risk of developing an ED (Pennesi & Wade, 2018; Zhou et al., 2020). Likewise, a single-session body image intervention delivered by teachers demonstrated small-to-medium effects at post-intervention (ds 0.19 – 0.76) that were not maintained at a follow-up 4 – 9.5 weeks later (Diedrichs et al., 2015). In another trial, a single-session video intervention showed a similar pattern of effects in school-age girls (Withers et al., 2002). Lastly, a pair of SSIs targeting depression symptoms (but not ED risk factors or symptoms explicitly) have demonstrated small, but long-term, effects on restrictive eating (ds 0.10 – 0.15; Schleider et al., 2022). There are promising SSIs that target ED risk factors in development, as well, as we discuss more thoroughly in the following sections.
There are fewer SSIs that aim to treat existing eating disorders in clinical populations. One such intervention (Fursland et al., 2018) provided assessment plus psychoeducation to individuals on the waitlist of a public outpatient eating disorder clinic. Not only did this intervention increase the likelihood of patients entering treatment (from 58% to 70%), but it led to reductions in eating disorder symptoms (d = 0.27) and impairment (d = 0.29).
How might SSIs effectively treat or prevent EDs? As stated above, SSIs target theory-driven factors, or change mechanisms, that can lead to sustained change in beliefs, emotions, and behaviors. Existing SSIs for depression produce long-term impacts by targeting perceived control and agency (Schleider et al., 2019), which are also implicated in eating disorder pathology (Sassaroli et al., 2008). New SSIs developed for eating disorders specifically may target these constructs as well as others implicated in EDs (e.g., body dissatisfaction).
Moreover, SSIs developed for eating disorders may seek to deliver one or more core components of longer-term effective interventions for EDs in a single session, using the best practices described above. Best practices for SSIs for youth mental health include compelling psychoeducation, empowering youths to a “helper” or “expert” role, saying-is-believing exercises to solidify learning, and testimonials from valued others (Schleider et al., 2020a). Notably, many of these components are shared by the effective Body Project intervention (Stice et al., 2012). In this intervention, participants are encouraged to assume an expert role and convince others not to pursue unrealistic body standards (the “thin ideal”). These saying-is-believing activities are designed to produce cognitive dissonance, as participants’ anti-thin ideal behavior conflicts with their pro-thin ideal attitudes; in order to reduce cognitive dissonance, participants bring their attitudes into line with their behavior, effectively reducing their internalization of the thin ideal (Stice et al., 2019), which reduces future risk of EDs as explained in the dual-pathway model (Stice & Van Ryzin, 2019). As SSIs have shown the potential to produce changes in attitudes via just one saying-is-believing exercise, future SSIs for EDs may seek to leverage saying-is-believing exercises to target thin-ideal internalization.
Paths forward for SSIs in ED research and practice
Embracing SSIs within treatment ecosystems for EDs would represent a fundamental, but necessary, expansion beyond supports available to patients today—most of which involve months of intensive, individual care. Because this prevailing, high-intensity treatment approach is unlikely to reach the majority of people struggling with EDs (Kazdin et al., 2017), SSIs open paths to diversifying how ED interventions are delivered, where and when they may be accessed, and who can deliver them, both within and beyond existing systems of care. SSIs can also be employed to efficiently and impactfully reach people during the critical risk period that precedes clinical ED onset, which for some individuals, could prevent the need for inaccessible, high-intensity treatment in the first place.
Harnessing existing SSIs to reduce ED symptoms and risk factors
Tapping into existing structures outside of formal treatment systems (namely, capitalizing on social media as a means of direct-to-youth intervention dissemination), our research team has already developed and tested two depression-focused SSIs that significantly reduced past-month restrictive eating, compared to an active control program designed to mimic support therapy in a self-guided format (Schleider et al., 2022). Neither of these depression-focused SSIs targeted ED symptoms directly; Project Personality teaches how and why personal traits and depression symptoms are malleable, and the ABC Project teaches how values-based actions can improve mood (Schleider et al., 2020b). Nevertheless, both SSIs led to small, but significant and long-term (3-month), reductions in restrictive eating, along with expected reductions in depressive symptom severity and other markers of internalizing distress (Schleider et al., 2022). These findings align with research highlighting the tight link, and potentially shared risk factors, across negative affect and eating pathology (Stice & Van Ryzin, 2019). Further, longitudinal and cross-sectional analyses have shown significant links between depressive symptoms and the initiation of restrictive eating during adolescence, further suggesting that addressing depressive symptoms may help prevent restrictive eating from escalating (Haynos et al., 2016). With so many adolescents lacking support for depression or EDs, let alone symptoms of both, simply disseminating these existing, evidence-based SSIs may help mitigate restrictive eating—in addition to depressive symptoms (their primary target)—at the population level.
To optimize the relevance of SSI research to treating and preventing EDs, future trials must include validated assessments of diverse ED symptoms—even in trials of SSIs not explicitly targeting EDs. Although EDs have long been misrepresented within psychology and psychiatry training as “niche” disorders, they are highly comorbid with many common mental health concerns (Haynos, et al., under review). As researchers continue to evaluate existing SSIs for common mental health problems, including depression and anxiety, we strongly recommend assessing their potential secondary impacts on ED-relevant outcomes, including body image and eating concerns. Some examples of validated assessments used in recent SSI trials include the Dietary Restriction Screener (Haynos & Fruzetti, 2015), the Body Shape Satisfaction Scale (Kelly et al., 2005), the Functionality Appreciation Scale (Alleva et al., 2017), the Sociocultural Attitudes Towards Appearance Questionnaire (Heinberg et al., 1995), the Body Esteem Scale for Adolescents & Adults (Mendelson et al., 2001), and the Eating Disorder Examination-Questionnaire (Fairburn & Beglin, 1994).
The more existing SSIs with transdiagnostic benefits we can identify, the better, as this may allow users to independently choose which SSIs best-fit their current needs. Personal choice has been proposed as a factor that may improve the use of digital mental health interventions (Linardon et al., 2022). In the context of EDs specifically, when given the choice between two binge eating interventions—a focused program targeting restrictive eating practices and a broad program targeting dietary restraint, body image concerns, and mood problems—the majority of participants selected the broad program (Linardon et al., 2022). This finding suggests that some individuals struggling with EDs prefer multifaceted interventions that explicitly target mood. We should harness existing SSIs within this category to provide more acceptable and scalable options to individuals struggling with EDs.
Creating new SSIs to reduce ED symptoms
In addition to exploring the utility of existing SSIs, there are great opportunities for developing new SSIs designed to reduce ED symptoms and to prevent their onset. As one example, our research team piloted a transdiagnostic SSI intended to mitigate proximal risk factors for both EDs and depression in adolescents: Body dissatisfaction (Becker et al., 2014; Jacobi & Fittig, 2010). Our resulting program, “Project Body Neutrality,” is a digital, self-guided SSI designed to alleviate body dissatisfaction through encouraging users to adopt a “body neutrality” mindset, whereby youth are encouraged to value their body based on the functions it performs, even if they are not always satisfied with its physical appearance (Smith et al., under review). The hypothesized theory of change for this SSI, reproduced from a manuscript describing results from a recent pilot of Project Body Neutrality (Smith et al., under review), is presented here as Figure 1. Body neutrality diverges from the popular “body positivity” movement, which advocates and scientists have criticized for excluding marginalized communities (Cwynar-Horta, 2016; Darwin & Miller, 2021; Miller, 2016) and for its appearance-centered message, which may not resonate with those who feel unable to love the way their body looks (e.g., gender-diverse young adults experiencing gender dysphoria linked to their physicality; Hartman-Munick et al., 2021; Legault & Sago, 2022; Rodgers et al., 2022; Lazuka et al., 2020; McGuire et al., 2016). The body neutrality concept draws from the academic literature on functionality appreciation research (Alleva & Tylka, 2021), and holds a culturally relevant, inclusive framing that explicitly rejects using appearance satisfaction to inform self-worth. There is preliminary evidence for the effectiveness of Project Body Neutrality among adolescents reporting co-occurring depressive symptoms and body dissatisfaction (i.e., significant post-intervention decreases in body dissatisfaction, increases in functionality appreciation, and decreases in hopelessness) (Smith et al., under review), and the SSI may provide a source of support for individuals with limited access to or negative experiences with other ED treatments. By addressing a modifiable, transdiagnostic risk factor, Project Body Neutrality is a potentially effective, easily-disseminable SSI that, like other ED-focused SSIs, could diversify ED treatment and prevention options.
Figure 1.
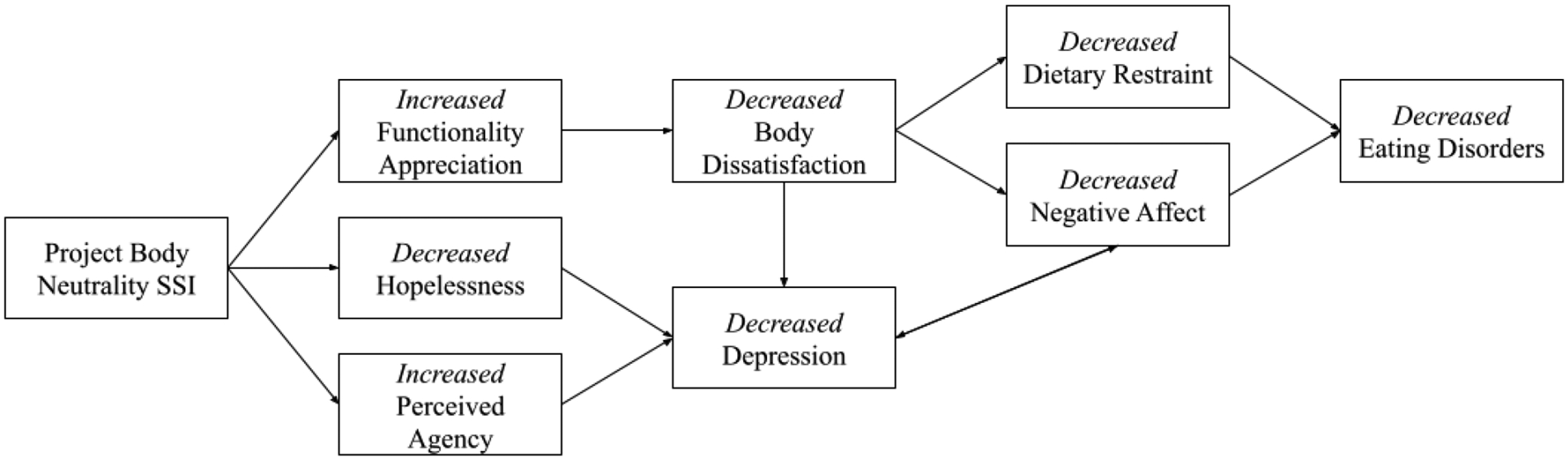
Hypothesized Theory of Change for “Project Body Neutrality,” a single-session digital intervention designed to target both an ED risk factor (body dissatisfaction) and depressive symptoms simultaneously
In designing novel SSIs to target facets of EDs, where might ED researchers begin? A key first-step is to identify the proximal target of the to-be-developed SSI. There are numerous potential targets, or modifiable risk factors, maintenance factors, and treatment mediators, that ED-focused SSIs might target in order to spur downstream improvements in EDs. A systematic review identified the pursuit of the thin body ideal, weight/shape overvaluation, body dissatisfaction, fear of weight gain, strict dieting, weight suppression, feeling fat, overeating, binge eating, negative affect, and impaired psychosocial functioning as robust risk factors for ED onset (Stice et al., 2021). When selecting a specific target risk factor for an SSI, we suggest that researchers consider if there is evidence to support that the target could be altered—even to a small but meaningful degree—via a brief psychosocial intervention. Regarding treatment-focused SSIs designed for individuals already struggling with subclinical or clinical EDs, potentially-valuable targets include predictors and mediators of response to longer-term treatments. A meta-analysis of 126 studies found that the rate and extent of early ED symptom improvement, early motivation to recover, and early self-efficacy predicted more favorable clinical outcomes (Vall & Wade, 2015). Early reductions in shame and early increases in self-compassion have also been associated with greater improvement in ED symptoms, in the context of multi-session treatment (Kelly et al., 2014). Moreover, in a randomized trial of an online, self-guided SSI, an eight-minute program teaching that emotions and anxiety are malleable significantly increased parents’ receptivity to psychotherapy—both for themselves and for their children—by increasing their confidence that mental health treatment could be effective (Schleider & Weisz, 2018). Although this program did not target attitudes toward ED treatment specifically, it does suggest SSIs’ potential to help mitigate common barriers to ED treatment-seeking, including denial and perceived inability of others to help (Radunz, Ali, & Wade, 2022).Whether developing a novel SSI for individuals who are at-risk for or already experiencing ED symptoms, identifying a single, potentially-modifiable, and evidence-informed target is a key first-step towards building a cohesive, digestible SSI with promise for effectiveness. From there, researchers may proceed with SSI development by drawing on previously-established design principles in SSI content creation (Schleider et al., 2020a), partnering with patients to ensure program acceptability and usability (Weinheimer et al., 2020), drawing on “key components” of multi-session evidence-based ED interventions, and constructing novel SSIs to maximize scalability (e.g., by designing the program for online, self-guided administration; by creating SSIs deliverable by lay health workers; by publicly sharing program content and implementation guides).
Points of implementation for ED-focused SSIs
Given their brevity, accessibility, and diverse potential uses (e.g., as a means of reducing symptoms directly, mitigating risk for clinically-significant EDs, or encouraging motivation for and uptake of other forms of ED treatment), ED-focused SSIs may be useful to implement at myriad points within and outside of ED treatment ecosystems (Schleider et al., 2020a). One possibility is SSI delivery immediately following administration of an online or primary care-based ED symptom screen. Online ED screeners are used by millions of people each year, and many primary care providers implement screeners during annual well-visits for patients. These screeners create opportunities to offer in-the-moment referrals or links to brief interventions, potentially helping to narrow the ED treatment gap and maximizing the benefits of ED prevention and early intervention (Kazdin et al., 2017; Fitzsimmons-Craft et al., 2019). By linking ED-focused SSIs with screener administration (e.g., automatically offering digital SSIs to people who screen positive for EDs), SSIs might help promote uptake and pursuit of additional treatment resources. Indeed, very brief (1–8 minute) online SSIs have significantly increased uptake of online crisis resources among adolescents (Cohen et al., in press) and increased parents’ expectancies that psychotherapy could be helpful both for themselves and for their children (Schleider & Weisz, 2018). As such, linking ED screeners with brief, evidence-based SSIs could serve as a powerful “just-in-time” approach to boosting openness to treatment and connecting people with support.
Beyond traditional screening, individuals struggling with EDs may be identified and offer in-the-moment support within social media platforms (Kasson et al., 2021). Given that a high proportion of youth who engage with pro-ED content on social media suffer from EDs and support harnessing technology for treatment (Fitzsimmons-Craft et al., 2020), it may be beneficial to embed ED-focused SSIs as resources that vulnerable individuals can access when “flagged” within social media platforms (e.g., due to searches for triggering ED-relevant content). Recently, our team partnered with the mental health nonprofit Koko to embed 5-to-8 minute versions of our evidence-based SSIs within Tumblr, to gauge whether this “just-in-time” approach to offering SSIs might have merit. Indeed, results of this open trial—which included N = 6,179 adolescents flagged within Tumblr as “at-risk” for mental health difficulties—showed that our depression- and self-harm-focused SSIs significantly reduced users’ hopelessness, self-hate, and desire to stop self-injury (ps < .0001) (Dobias et al., 2022). An SSI focusing on body image concerns has also been embedded within Tumblr in collaboration with Koko. From pre-intervention to post-intervention, this SSI resulted in improvements in body image and increased motivation to continue positive changes in body image (Nemesure et al, 2023). Brief, self-guided, ED-specific SSIs hold promise for offering immediate support for social media users with eating or body image concerns.
Another well-tested application for SSIs involves offering support to people facing long waiting-times for treatment. Many treatment-seeking individuals face months-long waiting lists after reaching out for help, and longer waits can adversely impact treatment motivation and response (Carter et al., 2012). SSIs may therefore be a useful tool to support individuals waiting for treatment. In fact, a solution-focused SSI for individuals on psychotherapy waitlists has increased motivation for change, reduced hopelessness, and mitigated psychological distress in individuals on waiting lists for outpatient psychotherapy—and these trials included a number of individuals endorsing ED symptoms (Schleider et al., 2021; Sung et al., 2023). Additionally, a single-session psychoeducational intervention delivered to patients on a waitlist at a public ED clinic led to reductions in ED symptoms and clinical impairment, and increased the likelihood that patients attended their first scheduled appointment (Fursland et al., 2018).
SSIs may also be implemented as adjunctive supports during longer-term ED treatments. For example, digital technologies can be used to deliver ED treatment components and to support clients between sessions (Sadeh-Sharvit, 2019). Furthermore, internet-based maintenance programs have been used to continue helping patients following discharge from higher levels of care (Aardoom et al., 2016; Bauer et al., 2012). Future research may consider the potential of SSIs to augment effects of traditional ED treatment, between sessions and post-intensive care.
Although aforementioned suggestions cover ED SSI implementation from screening through prevention or treatment, they are by no means exhaustive. Other possibilities include, but are not limited to, implementation within schools, community centers, and emergency rooms, as detailed elsewhere (Schleider & Weisz, 2017; Schleider et al., 2020a).
Seeking out Funding for ED Single-Session Interventions
In addition to the support that SSIs may provide to individuals living with EDs, SSIs may also open doors to additional ED research funding pathways. Despite the severity and societal cost of EDs, funding for ED research is low compared to other psychiatric disorders (Murray et al., 2017). Although a broader recognition that EDs are “not niche” disorders will be needed to address the root causes of inadequate investment in ED treatment (Haynos et al., under review), a more immediate path to expanding funding opportunities might involve capitalizing on the transdiagnostic utility of SSIs (e.g., for EDs and depression, per Schleider et al., 2022; Smith et al., under review). Transdiagnostic interventions have been considered a “best buy” due to their broad clinical scope and relative cost-effectiveness (Kazdin et al., 2017); likewise, SSIs’ potential for scalability is well-suited to addressing large-scale public health needs. Thus, ED- and non-ED-researchers might partner on joint grants to investigate the promise of transdiagnostic SSIs, across multiple settings, for co-occurring EDs and other forms of psychopathology.
Equipping ED Therapists with SSI Expertise
For ED clinicians and researchers to capitalize on the promise of SSIs, a key first-step is to institute education around SSIs into graduate training programs. At the time of our writing this paper, SSIs are seldom—if ever—mentioned in training programs for psychologists or psychiatrists. Some social work and counseling programs offer clinical placements on brief intervention techniques (such as solution-focused brief therapy), but an explicit focus on SSIs is rare. A likely explanation for this omission reflects long-standing biases in psychotherapy research, including the ED field. For instance, the authors (in their professional experience) have observed implicit assumptions that people with more severe problems (including, but not limited to EDs) can only experience progress over extended periods of time, and that more treatment for people with EDs is necessarily better. In fact, research suggests that clinical change often occurs over brief time-spans (Schleider et al., 2019)—and treatment length has no consistent link with effectiveness, although some meta-analyses (Ost & Ollendick, 2017; Weisz et al., 2017) and individual studies (Bell et al., 2017) have observed that more sessions are associated with worse response. Trainees specializing in EDs should have access to this information, and they should have opportunities to learn how and why single-session approaches may carry value.
Ultimately, achieving this goal will require a fundamental shift in clinical thinking and training, toward one that acknowledges the value of a “single-session mindset” in reducing and preventing EDs. That is, ED researchers and therapists might be trained to maximize the therapeutic potential of every moment; to communicate and internalize that change can occur even in brief periods of time; to appreciate that all clients can bring about meaningful improvements in their lives; and to celebrate steps forward in ED treatment, however seemingly small, as important. Ultimately, these are the core tenets of embracing a single-session approach, within ED clinical research and beyond.
Conclusion
Our goal in this article was to introduce SSI research to ED researchers; to describe their potential utility within ED research and practice; and to spark ideas for harnessing SSIs to help treat and prevent EDs at scale. Although SSIs cannot and should not replace any forms of ED treatment that are already in place, the gaps in existing treatment systems are overwhelming—and SSIs are well-equipped to fill them. Given the astronomical and rising costs of EDs for individuals, families, and populations, learning the strengths and limits of a single-session approach of EDs could be a low-risk, potentially high-reward avenue towards reducing and preventing EDs in the long-term.
Public Health Significance Statement:
Most individuals experiencing eating disorders (EDs) never access any form of treatment, creating an urgent need to identify ED interventions built to overcome barriers to engaging with care. This Forum article introduces Single-Session Interventions (SSIs) as a promising path to rapidly developing and testing accessible, evidence-based ED supports; supplementing existing ED treatment models; and reducing the individual, familial, and societal burdens of EDs at scale.
Acknowledgements.
JLS has received funding from the National Institute of Health Office of the Director (DP5OD028123), National Institute of Mental Health (R43MH128075), the Upswing Fund for Adolescent Mental Health, the National Science Foundation (2141710), Health Research and Services Association (U3NHP45406-01-00), the Society for Clinical Child and Adolescent Psychology, HopeLab, and the Klingenstein Third Generation Foundation. Preparation of this article was supported in part by the Implementation Research Institute (IRI), at the George Warren Brown School of Social Work, Washington University in St. Louis; through an award from the National Institute of Mental Health (R25MH080916; JLS is an IRI Fellow).
Footnotes
Conflicts of Interest. JLS serves on the Scientific Advisory Board for Walden Wise and the Clinical Advisory Board for Koko; receives consulting fees from Kooth, LLC; is Co-Founder and Co-Director of Single Session Support Solutions; and receives book royalties from New Harbinger, Oxford University Press, and Little Brown Book Group.
References
- Aardoom JJ, Dingemans AE, & Van Furth EF (2016). E-health interventions for eating disorders: Emerging findings, issues, and opportunities. Current Psychiatry Reports, 18(4), 42. 10.1007/s11920-016-0673-6 [DOI] [PubMed] [Google Scholar]
- Abel MR, Gilbert R, Bianco A, & Schleider JL (2022). When is psychotherapy brief? Considering sociodemographic factors, problem complexity, and problem type in us adolescents. Journal of Clinical Child & Adolescent Psychology, 51, 740–749. 10.1080/15374416.2020.1759076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alleva JM, & Tylka TL (2021). Body functionality: A review of the literature. Body Image, 36, 149–171. 10.1016/j.bodyim.2020.11.006 [DOI] [PubMed] [Google Scholar]
- Alleva JM, Tylka TL, & Van Diest AMK (2017). The Functionality Appreciation Scale (FAS): Development and psychometric evaluation in US community women and men. Body Image, 23, 28–44. [DOI] [PubMed] [Google Scholar]
- Bados A, Balaguer G, & Saldaña C (2007). The efficacy of cognitive–behavioral therapy and the problem of drop-out. Journal of Clinical Psychology, 63(6), 585–592. 10.1002/jclp.20368 [DOI] [PubMed] [Google Scholar]
- Barrett MS, Chua WJ, Crits-Christoph P, Gibbons MB, & Thompson D (2008). Early withdrawal from mental health treatment: Implications for psychotherapy practice. Psychotherapy, 45(2), 247–267. 10.1037/a0016184 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer S, Okon E, Meermann R, & Kordy H (2012). Technology-enhanced maintenance of treatment gains in eating disorders: efficacy of an intervention delivered via text messaging. Journal of Consulting and Clinical Psychology, 80(4), 700–706. 10.1037/a0028030 [DOI] [PubMed] [Google Scholar]
- Baum F, MacDougall C, & Smith D (2006). Participatory action research. Journal of Epidemiology and Community Health, 60(10), 854–857. 10.1136/jech.2004.028662 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becker CB, Plasencia M, Kilpela LS, Briggs M, & Stewart T (2014). Changing the course of comorbid eating disorders and depression: what is the role of public health interventions in targeting shared risk factors? Journal of Eating Disorders, 2, 15. 10.1186/2050-2974-2-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell C, Waller G, Shafran R, & Delgadillo J (2017). Is there an optimal length of psychological treatment for eating disorder pathology? International Journal of Eating Disorders, 50(6), 687–692. 10.1002/eat.22660 [DOI] [PubMed] [Google Scholar]
- Berg M, Coman E, & Schensul JJ (2009). Youth action research for prevention: A multi-level intervention designed to increase efficacy and empowerment among urban youth. American Journal of Community Psychology, 43(3–4), 345–359. 10.1007/s10464-009-9231-2 [DOI] [PubMed] [Google Scholar]
- Carter O, Pannekoek L, Fursland A, Allen KL, Lampard AM, & Byrne SM (2012). Increased wait-list time predicts dropout from outpatient enhanced cognitive behaviour therapy (CBT-E) for eating disorders. Behaviour Research and Therapy, 50(7–8), 487–492. 10.1016/j.brat.2012.03.003 [DOI] [PubMed] [Google Scholar]
- Cohen J (2013). Statistical power analysis for the behavioral sciences. Routledge. [Google Scholar]
- Cohen K, Dobias ML, Morris R, & Schleider JL (in press). Improving uptake of mental health crisis resources: Randomized test of a single-session intervention embedded in social media. 10.31234/osf.io/afvws [DOI] [Google Scholar]
- Cwynar-Horta J (2016). The commodification of the body positive movement on Instagram. STREAM Journal, 8(2), 36–56. 10.21810/strm.v8i2.203 [DOI] [Google Scholar]
- Darnall BD, Roy A, Chen AL, Ziadni MS, Keane RT, You DS, Slater K, Poupore-King H, Mackey I, Kao MC, Cook KF, Lorig K, Zhang D, Hong J, Tian L, & Mackey SC (2021). Comparison of a single-session pain management skills intervention with a single-session health education intervention and 8 sessions of cognitive behavioral therapy in adults with chronic low back pain: A randomized clinical trial. JAMA Network Open, 4(8), e2113401. 10.1001/jamanetworkopen.2021.13401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darwin H, & Miller A (2021). Factions, frames, and postfeminism(s) in the Body Positive Movement. Feminist Media Studies, 21(6), 873–890. 10.1080/14680777.2020.1736118 [DOI] [Google Scholar]
- Davey E, Bennett S, Bryant-Waugh R, Micali N, Takeda A, Alexandrou A, & Shafran R (2022). Low intensity psychological interventions for the treatment of feeding and eating disorders: A systematic review and meta-analysis. 10.31234/osf.io/uryq7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diedrichs PC, Atkinson MJ, Steer RJ, Garbett KM, Rumsey N, & Halliwell E (2015). Effectiveness of a brief school-based body image intervention “Dove Confident Me: Single Session” when delivered by teachers and researchers: Results from a cluster randomised controlled trial. Behaviour Research and Therapy, 74, 94–104. 10.1016/j.brat.2015.09.004 [DOI] [PubMed] [Google Scholar]
- Dobias ML, Morris RR, & Schleider JL (2022). Single-session interventions embedded within tumblr: Acceptability, feasibility, and utility study. JMIR Formative Research. 6(7), e39004. 10.2196/39004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobias ML, Schleider JL, Jans L, & Fox KR (2021). An online, single-session intervention for adolescent self-injurious thoughts and behaviors: Results from a randomized trial. Behaviour Research and Therapy, 147, 103983. 10.1016/j.brat.2021.103983 [DOI] [PubMed] [Google Scholar]
- Downs J, Ayton A, Collins L, Baker S, Missen H, & Ibrahim A (2023). Untreatable or unable to treat? Creating more effective and accessible treatment for long-standing and severe eating disorders. Lancet Psychiatry, 10, 146–154. [DOI] [PubMed] [Google Scholar]
- Dryden W (2022). New ideas: one-at-a-time therapy. Oxford Guide to Brief and Low Intensity Interventions for Children and Young People, 280–285. [Google Scholar]
- Fairburn CG, & Beglin SJ (1994). Assessment of eating disorders: Interview or self‐report questionnaire?. International journal of eating disorders, 16(4), 363–370. [PubMed] [Google Scholar]
- Fairburn C, Bailey-Straebler S, Basden S, Doll H, Jones R, Murphy R, et al. (2015). Atransdiagnostic comparison of enhanced cognitive behaviour therapy (CBT-E) and interpersonal psychotherapy in the treatment of eating disorders. Behaviour Research and Therapy, 70, 64–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fassino S, Pierò A, Tomba E, & Abatte-Daga (2009). Factors associated with dropout from treatment for eating disorders: a comprehensive literature review. BMC Psychiatry, 9, 67. 10.1186/1471-244X-9-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzsimmons-Craft EE, Balantekin KN, Graham AK, Smolar L, Park D, Mysko C, Funk B, Taylor CB, & Wilfley DE (2019). Results of disseminating an online screen for eating disorders across the U.S.: Reach, respondent characteristics, and unmet treatment need. International Journal of Eating Disorders, 52(6), 721–729. 10.1002/eat.23043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzsimmons-Craft EE, Krauss MJ, Costello SJ, Floyd GM, Wilfley DE, & Cavazos-Rehg PA (2020). Adolescents and young adults engaged with pro-eating disorder social media: Eating disorder and comorbid psychopathology, health care utilization, treatment barriers, and opinions on harnessing technology for treatment. Eating and Weight Disorders. 25(6), 1681–1692. 10.1007/s40519-019-00808-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foran AM, O’Donnell AT, & Muldoon OT (2020). Stigma of eating disorders and recovery-related outcomes: A systematic review. European Eating Disorders Review, 28(4), 385–397. 10.1002/erv.2735 [DOI] [PubMed] [Google Scholar]
- Fursland A, Erceg-Hurn DM, Byrne SM, & McEvoy PM (2018). A single session assessment and psychoeducational intervention for eating disorders: Impact on treatment waitlists and eating disorder symptoms. International Journal of Eating Disorders, 51(12), 1373–1377. 10.1002/eat.22983 [DOI] [PubMed] [Google Scholar]
- Hartman-Munick SM, Silverstein S, Guss CE, Lopez E, Calzo JP, & Gordon AR (2021). Eating disorder screening and treatment experiences in transgender and gender diverse young adults. Eating Behaviors, 41, 101517. 10.1016/j.eatbeh.2021.101517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haynos AF, Watts AW, Loth KA, Pearson CM, & Neumark-Stzainer D (2016). Factors predicting an escalation of restrictive eating during adolescence. Journal of Adolescent Health, 59(4), 391–396. 10.1016/j.jadohealth.2016.03.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haynos AF, Egbert AH, Fitzsimmons-Craft EE, Levinson CA, & Schleider JL (under review). Not niche: Eating disorders and the dangers of over-specialization [DOI] [PMC free article] [PubMed]
- Haynos AF, & Fruzzetti AE (2015). Initial evaluation of a single-item screener to assess problematic dietary restriction. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity, 20, 405–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinberg LJ, Thompson JK, & Stormer S (1995). Development and validation of the sociocultural attitudes towards appearance questionnaire. International Journal of Eating Disorders, 17(1), 81–89. [DOI] [PubMed] [Google Scholar]
- Jacobi C, & Fittig E (2010). Psychosocial risk factors for eating disorders. In Agras WS (Ed.), The Oxford Handbook of Eating Disorders, 123–136. [Google Scholar]
- Kass AE, Balantekin KN, Fitzsimmons-Craft EE, Jacobi C, Wilfley DE, & Taylor CB (2017). The economic case for digital interventions for eating disorders among United States college students. International Journal of Eating Disorders, 50(3), 250–258. 10.1002/eat.22680 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasson E, Vázquez MM, Doroshenko C, Fitzsimmons-Craft EE, Wilfley DE, Taylor CB, & Cavazos-Rehg PA (2021). Exploring social media recruitment strategies and preliminary acceptability of an mHealth tool for teens with eating disorders. International Journal of Environmental Research and Public Health, 18(15), 7979. 10.3390/ijerph18157979 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin AE, Fitzsimmons-Craft EE, & Wilfley DE (2017). Addressing critical gaps in the treatment of eating disorders. International Journal of Eating Disorders, 50(3), 170–189. 10.1002/eat.22670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazdin AE, & Rabbitt SM (2013). Novel models for delivering mental health services and reducing the burdens of mental illness. Clinical Psychological Science, 1(2), 170–191. 10.1177/2167702612463566 [DOI] [Google Scholar]
- Kelly AC, Carter JC, & Borairi S (2014). Are improvements in shame and self-compassion early in eating disorders treatment associated with better patient outcomes? International Journal of Eating Disorders, 47(1), 54–64. 10.1002/eat.22196 [DOI] [PubMed] [Google Scholar]
- Kelly AM, Wall M, Eisenberg ME, Story M, & Neumark-Sztainer D (2005). Adolescent girls with high body satisfaction: who are they and what can they teach us?. Journal of Adolescent Health, 37(5), 391–396. [DOI] [PubMed] [Google Scholar]
- Konrad TR, Ellis AR, Thomas KC, Holzer CE, & Morrissey JP (2009). County-level estimates of need for mental health professionals in the United States. Psychiatric Services, 60(10), 1307–1314. 10.1176/ps.2009.60.10.1307 [DOI] [PubMed] [Google Scholar]
- van Laer T, Feiereisen S, & Visconti LM (2019). Storytelling in the digital era: A meta-analysis of relevant moderators of the narrative transportation effect. Journal of Business Research, 96, 135–146. 10.1016/j.jbusres.2018.10.053 [DOI] [Google Scholar]
- Kotilahti E, West M, Isomaa R, Karhunen L, Rocks T, & Ruusunen A (2020). Treatment interventions for severe and enduring eating disorders: systematic review. International Journal of Eating Disorders, 53(8), 1280–1302. [DOI] [PubMed] [Google Scholar]
- Lazuka RF, Wick MR, Keel PK, & Harriger JA (2020). Are we there yet? Progress in depicting diverse images of beauty in instagram’s body positivity movement. Body Image, 34, 85–93. 10.1016/j.bodyim.2020.05.001 [DOI] [PubMed] [Google Scholar]
- Legault L, & Sago A (2022). When body positivity falls flat: Divergent effects of body acceptance messages that support vs. undermine basic psychological needs. Body Image, 41, 225–238. 10.1016/j.bodyim.2022.02.013 [DOI] [PubMed] [Google Scholar]
- Linardon J, Shatte A, Messer M, Firth J, & Fuller-Tyszkiewicz M (2020). E-mental health interventions for the treatment and prevention of eating disorders: An updated systematic review and meta-analysis. Journal of Consulting and Clinical Psychology, 88(11), 994. [DOI] [PubMed] [Google Scholar]
- Linardon J, Shatte A, Messer M, McClure Z, & Fuller-Tyszkiewicz M (2022). Effects of participant’s choice of different digital interventions on outcomes for binge-spectrum eating disorders: A pilot doubly randomized preference trial. Behavior Therapy. 10.1016/j.beth.2022.09.007 [DOI] [PubMed] [Google Scholar]
- Pennesi JL, & Wade TD (2018). Imagery rescripting and cognitive dissonance: A randomized controlled trial of two brief online interventions for women at risk of developing an eating disorder. International Journal of Eating Disorders, 51(5), 439–448. [DOI] [PubMed] [Google Scholar]
- Mendelson BK, Mendelson MJ, & White DR (2001). Body-esteem scale for adolescents and adults. Journal of personality assessment, 76(1), 90–106. [DOI] [PubMed] [Google Scholar]
- McIntosh V, Jordan J, Carter J, Luty S, McKenzie J, Bulik C, et al. (2016). Psychotherapy for transdiagnostic binge eating: A randomized controlled trial of cognitive-behavioural therapy, appetite-focused cognitive-behavioural therapy, and scheme therapy. Psychiatric Research, 240, 412–420. [DOI] [PubMed] [Google Scholar]
- McGuire JK, Doty JL, Catalpa JM, & Ola C (2016). Body image in transgender young people: Findings from a qualitative, community based study. Body Image, 18, 96–107. 10.1016/j.bodyim.2016.06.004 [DOI] [PubMed] [Google Scholar]
- Miller AL (2016). Eating the other yogi: Kathryn Budig, the yoga industrial complex, and the appropriation of body positivity. Race and Yoga, 1(1). 10.5070/R311028507 [DOI] [Google Scholar]
- Miller WR (2000). Rediscovering fire: Small interventions, large effects. Psychology of Addictive Behaviors, 14(1), 6–18. [PubMed] [Google Scholar]
- Murray SB, Pila E, Griffiths S, & Le Grange D (2017). When illness severity and research dollars do not align: are we overlooking eating disorders? World Psychiatry, 16(3), 321. 10.1002/wps.20465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulkens S, de Vos C, de Graaff A, & Waller G (2018). To deliver or not to deliver cognitive behavioral therapy for eating disorders: Replication and extension of our understanding of why therapists fail to do what they should do. Behaviour Research and Therapy, 106, 57–63. [DOI] [PubMed] [Google Scholar]
- National Guideline Alliance (UK). (2017). Eating Disorders: Recognition and Treatment. National Institute for Health and Care Excellence (NICE). [PubMed] [Google Scholar]
- Nemesure MD, Park C, Morris RR, Chan WW, Fitzsimmons-Craft EE, Rackoff GN, Fowler LA, Taylor CB, & Jacobson NC (2023). Evaluating change in body image concerns following a single session digital intervention. Body Image, 44, 64–68. 10.1016/j.bodyim.2022.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Mara M, Greene D, Watson H, Shafran R, Kenworthy I, Cresswell C, & Egan SJ (2023). The efficacy of randomised controlled trials of guided and unguided self-help interventions for the prevention and treatment of eating disorders in young people: A systematic review and preliminary meta-analysis. Journal of Behavior Therapy and Experimental Psychiatry, 78(101777), 101777. 10.1016/j.jbtep.2022.101777 [DOI] [PubMed] [Google Scholar]
- Ono Y, Furukawa TA, Shimizu E, Okamoto Y, Nakagawa A, Fujisawa D, Nakagawa A, Ishii T, & Nakajima S (2011). Current status of research on cognitive therapy/cognitive behavior therapy in Japan. Psychiatry and Clinical Neurosciences, 65(2), 121–129. 10.1111/j.1440-1819.2010.02182.x [DOI] [PubMed] [Google Scholar]
- Öst LG, & Ollendick TH (2017). Brief, intensive and concentrated cognitive behavioral treatments for anxiety disorders in children: A systematic review and meta-analysis. Behaviour Research and Therapy, 97, 134–145. 10.1016/j.brat.2017.07.008 [DOI] [PubMed] [Google Scholar]
- Radunz M, Ali K, & Wade TD (2022). Pathways to improve early intervention for eating disorders: Findings from a systematic review and meta-analysis. International Journal of Eating Disorders. [DOI] [PubMed] [Google Scholar]
- Rodgers RF, Wertheim EH, Paxton SJ, Tylka TL, & Harriger JA (2022). #Bopo: Enhancing body image through body positive social media-evidence to date and research directions. Body Image, 41, 367–374. 10.1016/j.bodyim.2022.03.008 [DOI] [PubMed] [Google Scholar]
- Sadeh-Sharvit S (2019). Use of technology in the assessment and treatment of eating disorders in youth. Child and Adolescent Psychiatric Clinics of North America, 28(4), 653–661. 10.1016/j.chc.2019.05.011 [DOI] [PubMed] [Google Scholar]
- Sassaroli S, Gallucci M, & Ruggiero GM (2008). Low perception of control as a cognitive factor of eating disorders. Its independent effects on measures of eating disorders and its interactive effects with perfectionism and self-esteem. Journal of Behavior Therapy and Experimental Psychiatry, 39(4), 467–488. 10.1016/j.jbtep.2007.11.005 [DOI] [PubMed] [Google Scholar]
- Schleider JL, Abel MR, & Weisz JR (2019). Do immediate gains predict long-term symptom change? Findings from a randomized trial of a single-session intervention for youth anxiety and depression. Child Psychiatry and Human Development, 50(5), 868–881. 10.1007/s10578-019-00889-2 [DOI] [PubMed] [Google Scholar]
- Schleider JL, Dobias ML, Sung JY, & Mullarkey MC (2020a). Future directions in single-session youth mental health interventions. Journal of Clinical Child and Adolescent Psychology, 49(2), 264–278. 10.1080/15374416.2019.1683852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schleider JL, Dobias M, Sung J, Mumper E, & Mullarkey MC (2020b). Acceptability and utility of an open-access, online single-session intervention platform for adolescent mental health. JMIR Mental Health, 7(6), e20513. 10.2196/20513 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schleider JL, Burnette JL, Widman L, Hoyt C, & Prinstein MJ (2020c). Randomized trial of a single-session growth mind-set intervention for rural adolescents’ internalizing and externalizing problems. Journal of Clinical Child & Adolescent Psychology, 49(5), 660–672. 10.1080/15374416.2019.1622123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schleider JL, Mullarkey MC, Fox KR, Dobias ML, Shroff A, Hart EA, & Roulston CA (2022). A randomized trial of online single-session interventions for adolescent depression during COVID-19. Nature Human Behaviour, 6(2), 258–268. 10.1038/s41562-021-01235-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schleider JL, Sung JY, Bianco A, Gonzalez A, Vivian D, & Mullarkey MC (2021). Open pilot trial of a single-session consultation service for clients on psychotherapy waitlists. The Behavior Therapist, 44, 8–15. [Google Scholar]
- Schleider JL, & Weisz JR (2017). Little treatments, promising effects? Meta-analysis of single-session interventions for youth psychiatric problems. Journal of the American Academy of Child and Adolescent Psychiatry, 56(2), 107–115. 10.1016/j.jaac.2016.11.007 [DOI] [PubMed] [Google Scholar]
- Schleider J, & Weisz J (2018a). A single-session growth mindset intervention for adolescent anxiety and depression: 9-month outcomes of a randomized trial. Journal of Child Psychology and Psychiatry, 59(2), 160–170. 10.1111/jcpp.12811 [DOI] [PubMed] [Google Scholar]
- Schleider JL, & Weisz JR (2018b). Parent expectancies and preferences for mental health treatment: the roles of emotion mind-sets and views of failure. Journal of Clinical Child & Adolescent Psychology, 47(sup1), S480–S496. 10.1080/15374416.2017.1405353 [DOI] [PubMed] [Google Scholar]
- Smith AC, Ahuvia I, Ito S, & Schleider JL (under review). Project Body Neutrality: Piloting a digital single session intervention for body image and depression. [DOI] [PMC free article] [PubMed]
- Stice E, Marti CN, Shaw H, & Rohde P (2019). Meta-analytic review of dissonance-based eating disorder prevention programs: Intervention, participant, and facilitator features that predict larger effects. Clinical Psychology Review, 70, 91–107. 10.1016/j.cpr.2019.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Onipede ZA, & Marti CN (2021). A meta-analytic review of trials that tested whether eating disorder prevention programs prevent eating disorder onset. Clinical Psychology Review, 87, 102046. 10.1016/j.cpr.2021.102046 [DOI] [PubMed] [Google Scholar]
- Stice E, Rohde P, & Shaw H (2012). The Body Project: A Dissonance-Based Eating Disorder Prevention Intervention. Oxford University Press. [Google Scholar]
- Stice E, & Van Ryzin MJ (2019). A prospective test of the temporal sequencing of risk factor emergence in the dual pathway model of eating disorders. Journal of Abnormal Psychology, 128(2), 119–128. 10.1037/abn0000400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sung J, Bugatti M, Vivian D, & Schleider JL (2023, in press). Evaluating a telehealth single-session consultation service for clients on psychotherapy wait-lists. Practice Innovations. [Google Scholar]
- Sung JY, Mumper E, & Schleider JL (2021). Empowering anxious parents to manage child avoidance behaviors: Randomized control trial of a single-session intervention for parental accommodation. JMIR Mental Health, 8(7), e29538. 10.2196/29538 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor CB, Ruzek JI, Fitzsimmons-Craft EE, Sadeh-Sharvit S, Topooco N, Weissman RS, Eisenberg D, Mohr D, Graham A, Jacobi C, & Oldenburg B (2020). Using digital technology to reduce the prevalence of mental health disorders in populations: Time for a new approach. Journal of Medical Internet Research, 22(7), e17493. 10.2196/17493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vall E, & Wade TD (2015). Predictors of treatment outcome in individuals with eating disorders: A systematic review and meta-analysis. International Journal of Eating Disorders, 48(7), 946–971. 10.1002/eat.22411 [DOI] [PubMed] [Google Scholar]
- Weinheimer EA, Chang A, Neubert SW, Wildes JE, & Graham AK (2020). Past, current, and future willingness to engage with treatment targets: Applying user-centered design to inform the design of a mobile behavioral intervention. International Journal of Eating Disorders, 53(4), 611–617. 10.1002/eat.23252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weir S, Wills M, Young J, & Perlesz A (2008). The implementation of single session work in community health. The Bouverie Centre, La Trobe University, Brunswick, Australia. [Google Scholar]
- Weisz JR, Kuppens S, Ng MY, Eckshtain D, Ugueto AM, Vaughn-Coaxum R, Jensen-Doss A, Hawley KM, Krumholz Marchette LS, Chu BC, Weersing VR, & Fordwood SR (2017). What five decades of research tells us about the effects of youth psychological therapy: A multilevel meta-analysis and implications for science and practice. American Psychologist, 72(2), 79–117. 10.1037/a0040360 [DOI] [PubMed] [Google Scholar]
- Weisz E, Ong DC, Carlson RW, & Zaki J (2021). Building empathy through motivation-based interventions. Emotion, 21(5), 990–999. 10.1037/emo0000929 [DOI] [PubMed] [Google Scholar]
- Withers GF, Twigg K, Wertheim EH, & Paxton SJ (2002). A controlled evaluation of an eating disorders primary prevention videotape using the Elaboration Likelihood Model of Persuasion. Journal of Psychosomatic Research, 53(5), 1021–1027. 10.1016/s0022-3999(02)00493-2 [DOI] [PubMed] [Google Scholar]
- Wonderlich S, Peterson C, Crosby R, Smith T, Klein M, Mitchell J, et al. (2014). A randomized controlled comparison of integrative cognitive-affective therapy (ICAT) and enhanced cognitive-behavioral therapy (CBT-E) for bulimia nervosa. Psychological Medicine, 44, 543–553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Y, Pennesi JL, & Wade TD (2020). Online imagery rescripting among young women at risk of developing an eating disorder: A randomized controlled trial. International Journal of Eating Disorders, 53(12), 1906–1917. [DOI] [PubMed] [Google Scholar]


