Abstract
Background
Simultaneous cannabis/alcohol use, using both substances within a short time interval so that their effects overlap, has a greater risk of potential negative consequences than single-substance use and is more common in younger age. Relationships between recreational cannabis laws (RCLs) and changes in simultaneous cannabis/alcohol use prevalence remain untested.
Objective
To examine trends in simultaneous cannabis/alcohol use from 2008 to 2019, and investigate associations between implementation of RCLs (i.e., presence of active legal dispensaries or legal home cultivation) and simultaneous cannabis/alcohol use in the United States (U.S.).
Design
Repeated cross-sectional samples from the 2008–2019 U.S. National Survey on Drug Use and Health (NSDUH).
Participants
Respondents (51% female) aged 12 and older.
Interventions
Changes in simultaneous cannabis/alcohol use before and after RCL implementation (controlling for medical cannabis law implementation) were compared in different age groups (12–20, 21–30, 31–40, 41–50, 51+), using adjusted multi-level logistic regression with state random intercepts and an RCL/age group interaction.
Measurements
Self-reported simultaneous cannabis/alcohol use.
Results
From 2008 to 2019, the overall prevalence of simultaneous cannabis/alcohol use declined among those aged 12–20 but increased in adults aged 21+. Model-based simultaneous cannabis/alcohol use prevalence increased after RCL implementation among respondents aged 21–30 years (+1.2%; aOR= 1.15 [95%CI = 1.04–1.27]), 31–40 years (+1.0; 1.15 [1.04–1.27]), and 41–50 years (+1.75; 1.63 [1.34–1.98]), but not in individuals aged <21 or 51+ years.
Conclusions
Implementation of recreational cannabis policies resulted in increased simultaneous use of cannabis and alcohol, supporting the complementarity hypothesis, but only among adults aged 21+. Efforts to minimize harms related to simultaneous cannabis/alcohol use are critical, especially in states with RCLs. Future studies should investigate cultural norms, perceived harm, and motives related to simultaneous use.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-022-07948-w.
KEY WORDS: recreational cannabis laws, simultaneous cannabis/alcohol use, cannabis use, alcohol use
INTRODUCTION
Individuals using cannabis and alcohol represent several different patterns of consumption, including cannabis/alcohol co-use (using both substances in a given period, for example, the same month, but not necessarily simultaneously) and simultaneous cannabis/alcohol use (using both substances within a short time interval so that their effects overlap).1 Both co-use and simultaneous use are associated with severe consequences in all age groups.1–16 However, specific age groups seem to be more vulnerable to particular consequences. In adolescents, cannabis/alcohol co-use is associated with disruptions in brain structure and function, cognitive development, poor cognition, limited educational achievement, and increased risk for psychiatric disorders.3–6 In adults, cannabis/alcohol co-use is related to risky behaviors,6, 7 heavy patterns of cannabis/alcohol use,2, 9, 10 and alcohol use disorder.2,11 Simultaneous cannabis/alcohol use is even more concerning than co-use as the combined effects of both substances can interfere with absorption, bioavailability, and subjective intoxication effects.17–20 However, little is known about the trends of simultaneous use in adults in the United States (U.S.), where adult cannabis use21, 22 and alcohol use23–25 are increasing in a changing cannabis policy environment.
Cannabis legislation is an important environmental factor influencing cannabis supply, availability, risk perception, cannabis use, and simultaneous cannabis/alcohol use.26–31 Cannabis legalization is complex, involving multiple policy decisions, including regulations of supply chain and operation (e.g., government monopoly, profit retail sales, legal home cultivation, advertisement), types of products distributed, prices, and taxes.32, 33 Permissive cannabis laws can increase cannabis use by two mechanisms: (1) increased availability and (2) decreased perceived risk.26, 28, 30, 34 However, these mechanisms show different impacts across age groups.26, 28–31, 35–37
Shifts in cannabis legislation have raised questions about unintended effects on alcohol use patterns, with evidence supporting both the substitution hypothesis and the complementarity hypothesis.38–42 The substitution hypothesis proposes that policy changes would lead people to replace the use of one intoxicating substance for another, which would result in individuals opting to use cannabis instead of alcohol due to reductions in the price and legal/societal consequences of cannabis use. The complementarity hypothesis proposes that more flexible cannabis policies would result in individuals increasing the use of multiple substances, including simultaneous cannabis/alcohol use38–42.
There is a gap in the literature regarding shifts in simultaneous cannabis/alcohol use after implementation of recreational cannabis laws (RCLs). Existing studies of the effects of RCL on cannabis/alcohol use focus either on each substance separately36, 37 or only on cannabis/alcohol co-use in specific states27, 43 or nationally.29 The only study specifically examining simultaneous cannabis/alcohol use was performed over a short period (2014–2016) which may not be sufficient time to observe changes in substance use patterns related to RCLs.44 Therefore, little is known about how implementation of RCLs may affect the prevalence of simultaneous cannabis/alcohol use in the US.
Our study examined trends and changes in simultaneous cannabis/alcohol use prevalence before and after RCL implementation by age groups, which both builds on previous research demonstrating age differences and incorporates age restrictions inherent in RCLs. We focused on implementation of legal supply mechanisms (e.g., presence of recreational dispensaries in a state) due to RCLs, which more directly reflects access to legal cannabis for those aged 21+. We hypothesized that following RCL implementation, simultaneous cannabis/alcohol use would (1) increase among adults aged 21+ years, because legal recreational use is limited to adults 21+ and previous work suggests that RCLs are associated with increased cannabis use in adults26, 28; (2) result in more pronounced increases among adults aged 51+ years, considering documented increases in cannabis and alcohol use separately45, 46 and findings from state-level research44; and (3) not be associated with changes in simultaneous cannabis/alcohol use among adolescents and young adults below the legal age (12–20 years old) based on prior work which indicates no difference in cannabis use alone and cannabis/alcohol co-use related to cannabis laws in this age group.29, 30, 35, 47
METHODS
We used restricted-access data from individuals aged 12+ who participated in the 2008–2019 National Survey on Drug Use and Health (NSDUH) (n = 817,359). Data included respondents’ state of residence which enabled us to determine state RCL exposure status. The 2019 survey was the most recently available at the time of analysis (June 2021 to April 2022). The NSDUH uses a multistage probability design for annual cross-sectional household surveys of the U.S. non-institutionalized population aged 12 and older. The NSDUH includes survey weights to adjust for the probability of selection at each sampling stage, nonresponse and coverage. Interview response rates over the study period varied from 64 to 76%.48
Our outcome was self-report of simultaneous cannabis/alcohol use. In the NSDUH, survey participants were asked “what other drug or drugs did you use while you were drinking or within a couple of hours of drinking?” Participants who reported using marijuana or hashish were classified as “using marijuana or hashish at the same time or within a couple of hours of the respondent's last alcohol use”,49 as a dichotomous variable (e.g., yes, no).
Our primary exposure was living in a state that implemented RCL and had an operational legal channel for obtaining cannabis for recreational purposes (i.e., legal cannabis supply). This definition includes the adoption of laws allowing home cannabis cultivation or the presence of a legal recreational dispensary in the state, whichever came first. Individual interview dates were compared with RCL and MCL operationalization dates, which were obtained from multiple sources, to determine exposure status.50–53 Where discrepancies in RCL/MCL dates between sources were noted, we referred to the specific text of the statute for clarification. These dates have been used in previous work.54, 55 Individuals interviewed in a state that did not implement any form of cannabis legalization by 2019 were classified as “Never MCL/RCL” exposure; those in states that eventually implemented MCL only were classified as “Before MCL.” Those interviewed after MCL implementation in a state that did not implement RCL by 2019 were categorized as “After MCL/Never RCL” while those interviewed prior to RCL implementation were categorized as “After MCL/Before RCL.” Individuals interviewed after RCL implementation were classified as “After MCL/After RCL.” State classifications over time are presented in Appendix Table 1.
Because a state’s MCL/RCL exposure status could change over the study period, for descriptive analyses, we also created a time-invariant three-level exposure variable reflecting state’s MCL/RCL status by the end of the analysis period in 2019. This included states that never implemented any form of cannabis legalization (Never MCL/RCL), states that legalized medical cannabis but not recreational cannabis (MCL only/No RCL), and states that legalized recreational cannabis (Ever RCL) by the end of the analysis period. In regression models, we used the time-varying indicator of state cannabis law status based on the date of the respondent interview as described above. Because our primary interest was in examining changes in simultaneous cannabis/marijuana in response to RCL only, we focused on contrasts during the period after MCL operationalization (After MCL/Before RCL vs. After MCL/After RCL.)
Age at interview was categorized as follows: 12–20, 21–30, 31–40, 41–50, and 51+ years old. The rationale for this categorization was to classify individuals at each life decade and to separate participants under the age of 21, the legal age for purchasing alcohol and cannabis. Other individual-level covariates included gender, racial/ethnic group, education, family income, and urbanicity. State-level covariates were based on 2010 U.S. Census data on the proportion of each state’s population that was white, male, aged 10–24 years, aged 25+ with at least a high school education, state unemployment rates, and median household income.
Statistical Analysis
We first described the cumulative prevalence of simultaneous cannabis/alcohol use and examined differences by sociodemographic characteristics, grouping respondents by state RCL exposure status at the end of the observation period, 2019 (Never MCL/RCL, MCL only/No RCL, Ever RCL). Next, to test associations between RCLs and simultaneous cannabis/alcohol use, we utilized a two-stage process. First, we generated adjusted predicted prevalences of simultaneous cannabis/alcohol use by RCL exposure status group by age. Next, to examine changes in prevalence of simultaneous use after versus before RCL enactment (i.e., after MCL/after RCL vs. after MCL/before RCL), we contrasted the model-based marginal predictions, computing adjusted odds ratios (aOR) and 95% confidence intervals (95%CI). In the first step, we used the lme4 R package to fit a multi-level logistic regression, including an interaction between the RCL exposure group variable and age group. Models included state random intercepts to account for the clustering of individuals within states. Categorical year fixed effects were also included to account for secular trends in simultaneous use across all states over the observation period. We further controlled for individual-level and state-level covariates, as listed above. Following prior research,54–56 we did not apply survey weights, and rather included the individual-level indicators listed above that are related to the NSDUH sampling design.57 In the second step of the process, we used the emmeans R package to generate adjusted odds ratios for the contrast of interest, after versus before RCL, from the model-based prevalences.
Our models controlled for several individual- and state-level factors that might confound the relationships between RCL and simultaneous cannabis/alcohol use, but other sources of potential unobserved confounding remain possible. Therefore, we conducted a sensitivity analysis using e-values to evaluate the potential impact of time-varying unmeasured confounding56, 58, 59 on our results. Small e-values closer to 1.0 suggest that little unmeasured confounding may account for observed associations; larger e-values indicate that results are increasingly robust to unmeasured confounding. E-values were obtained for the estimated aOR and lower level of the 95%CI (LL95%CI) using the EValue package in R software.56, 58, 59
This manuscript was prepared according to STROBE guidelines for cross-sectional studies60 and approved by the Columbia University Institutional Review Board (approval number AAAS4624).
RESULTS
Demographic characteristics were similar when comparing people in states by cannabis legalization status as of 2019 (Table 1).
Table 1.
Demographic Characteristics, Self-reported Simultaneous Cannabis/Alcohol Use, and State-Level Covariates by States Cannabis Law Status in 2019. National Survey on Drug Use and Health (NSDUH), 2008–2019
| Never MCL/RCL | MCL only/No RCL | Ever RCL | ||||
|---|---|---|---|---|---|---|
| Weighted n’s | % Weighted | Weighted n’s | % Weighted | Weighted n’s | % Weighted | |
| Characteristics | ||||||
| Gender | ||||||
| Male | 42154400 | 48.40 | 54353500 | 48.29 | 31136700 | 48.98 |
| Female | 44947500 | 51.60 | 58197600 | 51.71 | 32428800 | 51.02 |
| Age | ||||||
| 12–20 | 13075500 | 15.01 | 15694800 | 13.95 | 9265600 | 14.58 |
| 21–30 | 14284500 | 16.40 | 17594900 | 15.63 | 10594200 | 16.67 |
| 31–40 | 13666400 | 15.69 | 16753300 | 14.89 | 10167700 | 15.99 |
| 41–50 | 13782100 | 15.82 | 17618400 | 15.65 | 10124000 | 15.93 |
| 51+ | 32293500 | 37.08 | 44889800 | 39.88 | 23414100 | 36.83 |
| Race/ethnicity | ||||||
| Non-Hispanic white | 58044500 | 66.64 | 75550200 | 67.12 | 36538800 | 57.48 |
| Non-Hispanic Black | 13098600 | 15.04 | 14119800 | 12.55 | 4207800 | 6.62 |
| Hispanic | 11806700 | 13.55 | 14989900 | 13.32 | 14781500 | 23.25 |
| Non-Hispanic other | 4152100 | 4.77 | 7891200 | 7.01 | 8037400 | 12.64 |
| Education | ||||||
| Less than HS | 12100900 | 15.42 | 13077200 | 12.78 | 7750200 | 13.45 |
| HS graduate | 22654300 | 28.87 | 29339200 | 28.68 | 14002200 | 24.31 |
| Some college | 22405200 | 28.56 | 28288500 | 27.65 | 16673400 | 28.94 |
| College graduate | 21298000 | 27.15 | 31609400 | 30.89 | 19182000 | 33.30 |
| Family income | ||||||
| <$20,000 | 16244500 | 18.65 | 19159700 | 17.02 | 10233900 | 16.10 |
| $20,000–$49,999 | 28511900 | 32.73 | 34186800 | 30.37 | 18745100 | 29.49 |
| $50,000–$74,999 | 14935800 | 17.15 | 18576000 | 16.51 | 10114100 | 15.91 |
| $75,000+ | 27409700 | 31.47 | 40628600 | 36.10 | 24472400 | 38.50 |
| Urbanicity | ||||||
| Large metro | 36841000 | 42.30 | 67020800 | 59.55 | 41904300 | 65.92 |
| Small metro | 31497100 | 36.16 | 31250300 | 27.76 | 16836400 | 26.49 |
| Nonmetro | 18763900 | 21.54 | 14279900 | 12.69 | 4824800 | 7.59 |
| Simultaneous cannabis/alcohol use | 2192300 | 2.52 | 3607300 | 3.22 | 2842900 | 4.49 |
State-level cannabis laws were categorized as a time-invariant three-level variable (Never MCL/RCL, MCL only/No RCL, and Ever RCL) as of RCL status in 2019
All results are weighted and rounded to conform to SAMSHA disclosure requirements to ensure confidentiality
Overall Trends in Simultaneous Cannabis/Alcohol Use by Age
From 2008 to 2019, the overall prevalence of simultaneous cannabis/alcohol use increased in adults. The largest increases were observed among those aged 51+ years old (from 0.63% [95%CI, 0.35–0.92] to 1.91% [1.59–2.23]), followed by participants aged 41–50 years (from 1.54% [1.18–1.90] to 3.61% [3.12–4.11]), those aged 31–40 years (from 2.82% [2.28–3.35] to 6.10% [5.49–6.70]), and those aged 21–30 years old (from 6.07% [5.46–6.68] to 10.00% [9.34–10.66]) (results not shown in figures). However, for respondents aged 12–20 years old, prevalence declined about 12% (from 4.31% [3.99–4.64] in 2008 to 3.84% [3.44–4.18] in 2019).
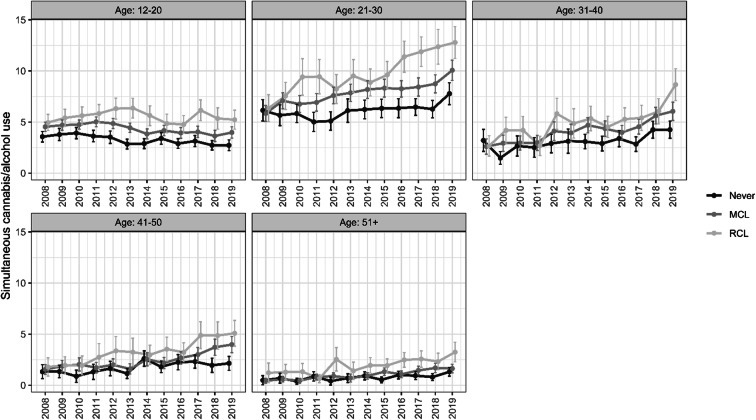
Figure 1 displays the prevalence of simultaneous cannabis/alcohol use in states by age group, according to state RCL status at the end of the observation period in 2019 (i.e., Never MCL/RCL, MCL only/No RCL, and RCL). Overall, simultaneous use prevalence was lower in never MCL/RCL relative to MCL or RCL.
Figure 1.
Trends of prevalences of simultaneous cannabis/alcohol use and implementation of recreational cannabis laws (RCL) during 2008–2019. Note: State-level cannabis law status was classified by 2019 and categorized as a time-invariant the following three-level variable: (1) Never — refers to states that have never implemented medical cannabis laws or recreational cannabis laws, (2) MCL — refers to states that only implemented medical cannabis laws, and (3) RCL — refers to states implemented recreational cannabis laws.
Changes in Simultaneous Cannabis/Alcohol Use by Age After RCL Enactment (Table 2)
Table 2.
Simultaneous Cannabis/Alcohol Use After Versus Before Legalization of Recreational Cannabis by Age Groups Among U.S. Individuals. NSDUH 2008–2019
| Age groups | % who reported simultaneous cannabis/alcohol use | AOR (95%CI) | |
|---|---|---|---|
| After MCL/ Before RCL |
After MCL/ After RCL |
||
| 12–20 | 9.31 | 8.44 | 0.90 (0.78, 1.04) |
| 21–30 | 9.20 | 10.40 | 1.15 (1.04, 1.27) |
| 31–40 | 5.12 | 6.12 | 1.21 (1.04, 1.41) |
| 41–50 | 2.93 | 4.68 | 1.63 (1.34, 1.98) |
| 51+ | 1.72 | 2.13 | 1.25 (0.99, 1.58) |
NSDUH National Survey on Drug Use and Health, RCL recreational cannabis laws, AOR adjusted odds ratio
All states that legalized recreational cannabis previously legalized medical cannabis. The before versus after RCL contrast therefore compared simultaneous cannabis/alcohol prevalence in states after MCL but before RCL relative to simultaneous cannabis/alcohol prevalence in states after MCL and after RCL
Individual- and state-level predictors: state random effects, year fixed effects, gender, race/ethnicity, family income, and urbanicity, % white, % male, % ages 10–24, % of adults (<25) with at least a high school education, unemployment, and state’s median household income
For point estimates with corresponding lower limit 95% confidence interval (LL95%CI) greater than 1, we estimated e-values to quantify the minimum strength of the relationship between an unmeasured/uncontrolled confounder and both our exposure (RCL) and outcome (simultaneous cannabis/alcohol use) needed to reduce the aOR and the lower limit of the 95% confidence interval (LL95%CI) to the null. For age group 21–30 years, these were as follows: ae-value for aOR = 1.55 and LL95%CI = 1.23; for age group 31–40 years, these were as follows: ae-value for aOR = 1.71 and LL95%CI = 1.22; and for age group 41–50 years, these were as follows: ae-value for aOR = 2.63 and LL95%CI = 2.01
Simultaneous cannabis/alcohol use increased in the After MCL/After RCL period among respondents aged 21–30 years, 31–40, and 41–50 but not among respondents aged 12–20 or 51+ (Table 2). For example, comparing the period after RCL to before RCL, the prevalence of simultaneous use among respondents aged 21–30 increased from 9.20 to 10.40% (aOR=1.15 [95%CI=1.04–1.27]). Similarly, among participants aged 31–40 years and 41–50 years, prevalence increased from 5.12 to 6.12% (aOR=1.21 [1.04–1.41]) and from 2.93 to 4.68% (aOR=1.63 [1.34–1.98]) respectively. Small but nonsignificant increases were observed among respondents aged 51 or older (aOR=1.25 [0.99, 1.58]). In contrast, there was a decrease in prevalence following RCL among respondents aged 12–21 (from 9.31 to 8.44%); however, the adjusted odds ratio overlapped the null (aOR=0.90 [0.78, 1.04]).
In sensitivity analyses, e-value results suggested that a moderate degree of unmeasured confounding would be required to explain the observed results if no relationship existed between RCLs and simultaneous use. For example, the observed adjusted odds ratio for the 21–30-year-old group could be explained by an unmeasured confounder that was associated with both the exposure (RCL) and the outcome (simultaneous use) by a risk ratio of 1.23 above the measured confounders, but weaker confounding could not do so. E-value results among those aged 41–50 were the most robust to potential unmeasured confounding (e-value 95%CI lower limit=2.01).
DISCUSSION
This study aimed to investigate changes in simultaneous cannabis/alcohol use before and after RCL implementation by different age groups, and found increases in simultaneous use after RCLs in adults aged 21–50 years. Our results showed no changes in simultaneous cannabis/alcohol use among individuals aged 12–20 and older adults (51+ years) associated with RCLs. These findings confirm our hypotheses of increases in adults aged 21+ and no changes in youth aged 12–20, which are in line with prior research focused on RCL in youth reporting no shifts in cannabis and alcohol use in adolescents aged 14–18 years old,37 no shifts in cannabis/alcohol co-use in those aged 18–25, and declines in adolescents aged 12–17 years.29
The availability and opportunity to access cannabis through legal supply chains such as dispensaries, present in most RCL states, may explain why we observed increases in simultaneous cannabis/alcohol use in those aged 21–50 but not 12–20 years after RCLs in this sample. These findings build upon prior MCL research showing that states allowing dispensaries had a greater likelihood of alcohol-related outcomes in adults aged 21+. Also, prior RCL studies reported increases in the prevalence of cannabis/alcohol co-use and simultaneous use,29, 43, 44 consistent with the complementarity hypothesis.38–42 Some of the possible explanations for the complementary hypothesis and simultaneous cannabis/alcohol use include an individual’s search for enhancement of intoxicating effects17–20 and declines in inhibitory control and decision-making caused by the use of one substance making an individual more prone to use the other available substance.61–64 Our work confirms these findings and extends them by reporting increased simultaneous use after RCL with cannabis supply implementation using a nationally representative sample across age groups over a long period (2008–2019).29, 65
RCLs were not associated with simultaneous cannabis/alcohol use in individuals aged < 21 which aligns with previous findings from research examining effects of MCL and cannabis use alone and cannabis/alcohol co-use,29, 30, 35, 47 and data showing shifts in cannabis risk perception did not co-occur with an increase in cannabis use in this age group.35 This finding could be explained by the effective restrictions in access to legal supply chains, enforcement of minimum age requirements for cannabis purchase, marketing restrictions on commercial ads targeting this age group (e.g., no advertisements in places where more than 30% of viewers are < 21 years), and prevention strategies (e.g., community- and school-based campaigns) in some RCL states.32, 33, 65 However, RCL states have different legislation regarding supply chains, regulatory mechanisms for types of products allowed, and prevention strategies. Therefore, further research should examine the impact of various sources of cannabis legal supply and types of prevention strategies in place in different RCL states.
Finally, there was a large increase in the prevalence of simultaneous cannabis/alcohol in older adults (51+ years) across all U.S. states. The overall increase in simultaneous use is in line with prior literature reporting that adults 50+ years experienced the largest increases in cannabis use of any age group.12, 66, 67 Thus, discussions about cannabis/alcohol co-use may be warranted in this population, including medical providers who ask about alcohol/cannabis use patterns in older adults.68
Our study has some limitations. First, this study was conducted using self-reported data on simultaneous alcohol/cannabis use and individuals’ perceptions of their own alcohol and cannabis use patterns which may be related to state RCL status. However, the NSDUH collects this sensitive information using computer-assisted self-interviewing which should reduce differential measurement error. Second, our analyses examined all RCL states as a single category and did not examine cannabis policy provisions (e.g., products permitted, cultivation restrictions, pricing control, the tax imposed, and consumption restrictions) or the density of recreational cannabis and alcohol retail outlets, which may lead to varied outcomes within RCL states. However, our exposure definition followed prior recommendations on conducting cannabis legislation research, such as using supply dates instead of effective dates of recreational cannabis legislation. Using supply dates is important because states may pass a law and take longer to authorize cannabis dispensaries and/or home cultivation.32,33 Third, we did not report overall findings, just age-stratified results as our focus was to investigate changes in simultaneous use by age groups. Fourth, we did not assess differences in alcohol policies across states (e.g., prices, alcohol sale hours). Some of the potential confounding effects of alcohol policies would be controlled through the use of state random effects. However, alcohol policies changing over this time period may contribute to uncontrolled confounding. Nevertheless, this study has significant strengths, including the use of nationally representative samples across multiple years (2008–2019), and a survey design that provided for accurate national- and state-level estimates. We used RCL variables based on supply dates instead of effective date, which allowed specific investigation of the effects of increased legal access to cannabis either by purchasing at a dispensary or through home cultivation; however, we were not able to make comparisons between implementation (i.e., supply dates) and enactment (i.e., effective dates) of the RCLs which could have provided valuable information on different policies components, future studies should address this issue.
Implementation of RCLs was associated with increases in simultaneous cannabis/alcohol use in individuals aged 21–50 years; however, no changes in simultaneous cannabis/alcohol use were observed in individuals younger than 21 years or those older than 51+ years old. This study contributes to our understanding of age group changes in simultaneous cannabis/alcohol use after the legalization of adult cannabis use in the U.S. beyond medical laws. It also extends research on changes in the prevalence of simultaneous use after changes in the legal cannabis supply. Our findings coupled with previous research suggest that there may be a need to develop strategies to reduce harms related to simultaneous cannabis/alcohol use in adults aged 21–50, especially in states with RCLs. Future studies should investigate changes in cultural norms, perceived harm and motives related to simultaneous cannabis/alcohol use, and the effects of specific cannabis policy provisions as more U.S. states legalize cannabis for adult recreational use.
Supplementary Information
(DOCX 46 kb)
Funding
This study was funded by grants from the U.S. National Institutes of Health, National Institute on Drug Abuse R01DA037866 (Martins), T32DA031099 (Hasin), R01DA048860 (Hasin), K01DA045224 (Mauro). This research was supported in part by a Grant 1 R49 CE002096-01 from the National Center for Injury Prevention and Control, Centers for Disease Control and Prevention to the Center for Injury Epidemiology and Prevention at Columbia University (New York, NY).
All analyses were conducted at the New York Federal Statistical Research Data Center, a Census Bureau administered facility providing secure access to restricted-access NSDUH microdata. Statistical output was reviewed by Substance Abuse and Mental Health Services Administration (SAMSHA) staff and conformed to SAMSHA disclosure requirements to ensure confidentiality, including sample size rounding (to the nearest hundred) and suppression of values less than 100 or with large standard errors.
The sponsors had no role in the design and conduct of the study, collection, management, analysis, and interpretation of the data, and preparation, review, or approval of this manuscript.
Declarations
Conflict of Interest
All authors have no conflict of interest related to this present work.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Subbaraman MS, Kerr WC. Simultaneous Versus Concurrent Use of Alcohol and Cannabis in the National Alcohol Survey. Alcohol Clin Exp Res. 2015;39(5):872–9. doi: 10.1111/acer.12698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Yurasek AM, Aston ER, Metrik J. Co-use of Alcohol and Cannabis: A Review. Curr Addict Rep. 2017;4(2):184–93. doi: 10.1007/s40429-017-0149-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Karoly HC, Ross JM, Ellingson JM, Feldstein Ewing SW. Exploring Cannabis and Alcohol Co-Use in Adolescents: A Narrative Review of the Evidence. J Dual Diagn. 2020;16(1):58–74. doi: 10.1080/15504263.2019.1660020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Morin JFG, Afzali MH, Bourque J, Stewart SH, Séguin JR, O’Leary-Barrett M, et al. A Population-Based Analysis of the Relationship Between Substance Use and Adolescent Cognitive Development. Am J Psychiatry. 2019;176(2):98–106. doi: 10.1176/appi.ajp.2018.18020202. [DOI] [PubMed] [Google Scholar]
- 5.Bucholz KK, McCutcheon VV, Agrawal A, Dick DM, Hesselbrock VM, Kramer JR, et al. Comparison of Parent, Peer, Psychiatric, and Cannabis Use Influences Across Stages of Offspring Alcohol Involvement: Evidence from the COGA Prospective Study. Alcohol Clin Exp Res. 2017;41(2):359–68. doi: 10.1111/acer.13293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lees B, Debenham J, Squeglia LM. Alcohol and Cannabis Use and the Developing Brain. Alcohol Res Curr Rev. 2021;41(1):11. doi: 10.35946/arcr.v41.1.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schuckit MA, Smith TL, Goncalves PD, Anthenelli R. Alcohol-related blackouts across 55 weeks of college: Effects of European-American ethnicity, female sex, and low level of response to alcohol. Drug Alcohol Depend. 2016;169:163–70. doi: 10.1016/j.drugalcdep.2016.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gonçalves PD, Smith TL, Anthenelli RM, Danko G, Schuckit MA. Alcohol-related blackouts among college students: impact of low level of response to alcohol, ethnicity, sex, and environmental characteristics. Rev Bras Psiquiatr. 2017;40(2):128–37. doi: 10.1590/1516-4446-2016-2165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Linden-Carmichael AN, Stamates AL, Lau-Barraco C. Simultaneous Use of Alcohol and Marijuana: Patterns and Individual Differences. Subst Use Misuse. 2019;54(13):2156–66. doi: 10.1080/10826084.2019.1638407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Metrik J, Gunn RL, Jackson KM, Sokolovsky AW, Borsari B. Daily Patterns of Marijuana and Alcohol Co-Use Among Individuals with Alcohol and Cannabis Use Disorders. Alcohol Clin Exp Res. 2018;42(6):1096–104. doi: 10.1111/acer.13639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Waddell JT. Between- and within-group effects of alcohol and cannabis co-use on AUD/CUD in the NSDUH 2002–2019. Drug Alcohol Depend. 2021;225:108768. doi: 10.1016/j.drugalcdep.2021.108768. [DOI] [PubMed] [Google Scholar]
- 12.Han BH, Palamar JJ. Marijuana use by middle-aged and older adults in the United States, 2015–2016. Drug Alcohol Depend. 2018;191:374–81. doi: 10.1016/j.drugalcdep.2018.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Terry-McElrath YM, Patrick ME. Simultaneous Alcohol and Marijuana Use Among Young Adult Drinkers: Age-Specific Changes in Prevalence from 1977 to 2016. Alcohol Clin Exp Res. 2018;42(11):2224–33. doi: 10.1111/acer.13879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sokolovsky AW, Gunn RL, Micalizzi L, White HR, Jackson KM. Alcohol and marijuana co-use: Consequences, subjective intoxication, and the operationalization of simultaneous use. Drug Alcohol Depend. 2020;212:107986. doi: 10.1016/j.drugalcdep.2020.107986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee C. Simultaneous Alcohol and Marijuana Use Among Young Adults: A Scoping Review of Prevalence, Patterns, Psychosocial Correlates, and Consequences. Alcohol Res Curr Rev. 2022;42(1):08. doi: 10.35946/arcr.v42.1.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Gonçalves PD, Gutkind S, Segura LE, Castaldelli-Maia JM, Martins SS, Mauro PM. Simultaneous Alcohol/Cannabis Use and Driving Under the Influence in the U.S. Am J Prev Med. 2022;62(5):661–9. doi: 10.1016/j.amepre.2021.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bramness JG, Khiabani HZ, Mørland J. Impairment due to cannabis and ethanol: clinical signs and additive effects. Addict Abingdon Engl. 2010;105(6):1080–7. doi: 10.1111/j.1360-0443.2010.02911.x. [DOI] [PubMed] [Google Scholar]
- 18.Lukas SE, Orozco S. Ethanol increases plasma Δ9-tetrahydrocannabinol (THC) levels and subjective effects after marihuana smoking in human volunteers. Drug Alcohol Depend. 2001;64(2):143–9. doi: 10.1016/S0376-8716(01)00118-1. [DOI] [PubMed] [Google Scholar]
- 19.Hartman RL, Brown TL, Milavetz G, Spurgin A, Gorelick DA, Gaffney G, et al. Controlled Cannabis Vaporizer Administration: Blood and Plasma Cannabinoids with and without Alcohol. Clin Chem. 2015;61(6):850–69. doi: 10.1373/clinchem.2015.238287. [DOI] [PubMed] [Google Scholar]
- 20.Pava MJ, Woodward JJ. A review of the interactions between alcohol and the endocannabinoid system: Implications for alcohol dependence and future directions for research. Alcohol. 2012;46(3):185–204. doi: 10.1016/j.alcohol.2012.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hasin DS. US Epidemiology of Cannabis Use and Associated Problems. Neuropsychopharmacology. 2018;43(1):195–212. doi: 10.1038/npp.2017.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hasin DS, Shmulewitz D, Sarvet AL. Time trends in US cannabis use and cannabis use disorders overall and by sociodemographic subgroups: a narrative review and new findings. Am J Drug Alcohol Abuse. 2019;45(6):623–43. doi: 10.1080/00952990.2019.1569668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Grant BF, Chou SP, Saha TD, Pickering RP, Kerridge BT, Ruan WJ, et al. Prevalence of 12-Month Alcohol Use, High-Risk Drinking, and DSM-IV Alcohol Use Disorder in the United States, 2001-2002 to 2012-2013: Results From the National Epidemiologic Survey on Alcohol and Related Conditions. JAMA Psychiatry. 2017;74(9):911. doi: 10.1001/jamapsychiatry.2017.2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hasin DS, Shmulewitz D, Keyes K. Alcohol use and binge drinking among U.S. men, pregnant and non-pregnant women ages 18-44: 2002-2017. Drug Alcohol Depend. 2019;205:107590. doi: 10.1016/j.drugalcdep.2019.107590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Keyes KM, Jager J, Mal-Sarkar T, Patrick ME, Rutherford C, Hasin D. Is There a Recent Epidemic of Women’s Drinking? A Critical Review of National Studies. Alcohol Clin Exp Res. 2019;43(7):1344–59. doi: 10.1111/acer.14082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martins SS, Mauro CM, Santaella-Tenorio J, Kim JH, Cerda M, Keyes KM, et al. State-level medical marijuana laws, marijuana use and perceived availability of marijuana among the general U.S. population. Drug Alcohol Depend. 2016;169:26–32. doi: 10.1016/j.drugalcdep.2016.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.García-Ramírez G, Paschall MJ, Grube JW. Retail Availability of Recreational Marijuana and Alcohol in Oregon Counties and Co-Use of Alcohol and Marijuana and Related Beliefs among Adolescents. Subst Use Misuse. 2021;56(3):345–52. doi: 10.1080/10826084.2020.1858104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Levy NS, Mauro PM, Mauro CM, Segura LE, Martins SS. Joint perceptions of the risk and availability of Cannabis in the United States, 2002-2018. Drug Alcohol Depend. 2021 Jul;108873. [DOI] [PMC free article] [PubMed]
- 29.Kim JH, Weinberger AH, Zhu J, Barrington-Trimis J, Wyka K, Goodwin RD. Impact of state-level cannabis legalization on poly use of alcohol and cannabis in the United States, 2004–2017. Drug Alcohol Depend. 2021;218:108364. doi: 10.1016/j.drugalcdep.2020.108364. [DOI] [PubMed] [Google Scholar]
- 30.Compton WM, Han B, Jones CM, Blanco C, Hughes A. Marijuana use and use disorders in adults in the USA, 2002–14: analysis of annual cross-sectional surveys. Lancet Psychiatry. 2016;3(10):954–64. doi: 10.1016/S2215-0366(16)30208-5. [DOI] [PubMed] [Google Scholar]
- 31.Compton WM, Han B, Jones CM, Blanco C. Cannabis use disorders among adults in the United States during a time of increasing use of cannabis. Drug Alcohol Depend. 2019;204:107468. doi: 10.1016/j.drugalcdep.2019.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kilmer B. How will cannabis legalization affect health, safety, and social equity outcomes? It largely depends on the 14 Ps. Am J Drug Alcohol Abuse. 2019;45(6):664–72. doi: 10.1080/00952990.2019.1611841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kilmer B, Pacula RL. Understanding and learning from the diversification of cannabis supply laws. Addict Abingdon Engl. 2017;112(7):1128–35. doi: 10.1111/add.13623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hasin DS, Sarvet AL, Cerdá M, Keyes KM, Stohl M, Galea S, et al. US Adult Illicit Cannabis Use, Cannabis Use Disorder, and Medical Marijuana Laws: 1991-1992 to 2012-2013. JAMA Psychiatry. 2017;74(6):579. doi: 10.1001/jamapsychiatry.2017.0724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sarvet AL, Wall MM, Keyes KM, Cerdá M, Schulenberg JE, O’Malley PM, et al. Recent rapid decrease in adolescents’ perception that marijuana is harmful, but no concurrent increase in use. Drug Alcohol Depend. 2018;186:68–74. doi: 10.1016/j.drugalcdep.2017.12.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Alley ZM, Kerr DCR, Bae H. Trends in college students’ alcohol, nicotine, prescription opioid and other drug use after recreational marijuana legalization: 2008–2018. Addict Behav. 2020;102:106212. doi: 10.1016/j.addbeh.2019.106212. [DOI] [PubMed] [Google Scholar]
- 37.Coley RL, Kruzik C, Ghiani M, Carey N, Hawkins SS, Baum CF. Recreational Marijuana Legalization and Adolescent Use of Marijuana, Tobacco, and Alcohol. J Adolesc Health. 2021;69(1):41–9. doi: 10.1016/j.jadohealth.2020.10.019. [DOI] [PubMed] [Google Scholar]
- 38.Risso C, Boniface S, Subbaraman MS, Englund A. Does cannabis complement or substitute alcohol consumption? A systematic review of human and animal studies. J Psychopharmacol (Oxf). 2020;34(9):938–54. doi: 10.1177/0269881120919970. [DOI] [PubMed] [Google Scholar]
- 39.Guttmannova K, Lee CM, Kilmer JR, Fleming CB, Rhew IC, Kosterman R, et al. Impacts of Changing Marijuana Policies on Alcohol Use in the United States. Alcohol Clin Exp Res. 2016;40(1):33–46. doi: 10.1111/acer.12942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Subbaraman MS. Substitution and Complementarity of Alcohol and Cannabis: A Review of the Literature. Subst Use Misuse. 2016;51(11):1399–414. doi: 10.3109/10826084.2016.1170145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Weinberger AH, Zhu J, Levin J, Moeller SJ, McKee SA, Goodwin RD. Changes in alcohol use by cannabis use status among adolescents and young adults in the United States: Emerging evidence for both substitution and complementarity. Alcohol Clin Exp Res. 2021;45(12):2536–45. doi: 10.1111/acer.14737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gunn R. Patterns of Cannabis and Alcohol Co-Use: Substitution Versus Complementary Effects. Alcohol Res Curr Rev. 2022;40(2):04. doi: 10.35946/arcr.v42.1.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Paschall MJ, García-Ramírez G, Grube JW. Recreational Marijuana Legalization and Co-use With Alcohol Among Adolescents. Am J Prev Med. 2022;62(1):57–64. doi: 10.1016/j.amepre.2021.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Subbaraman MS, Kerr WC. Subgroup trends in alcohol and cannabis co-use and related harms during the rollout of recreational cannabis legalization in Washington state. Int J Drug Policy. 2020;75:102508. doi: 10.1016/j.drugpo.2019.07.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Grucza RA, Sher KJ, Kerr WC, Krauss MJ, Lui CK, McDowell YE, et al. Trends in Adult Alcohol Use and Binge Drinking in the Early 21st-Century United States: A Meta-Analysis of 6 National Survey Series. Alcohol Clin Exp Res. 2018;42(10):1939–50. doi: 10.1111/acer.13859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mauro PM, Carliner H, Brown QL, Hasin DS, Shmulewitz D, Rahim-Juwel R, et al. Age Differences in Daily and Nondaily Cannabis Use in the United States, 2002–2014. J Stud Alcohol Drugs. 2018;79(3):423–31. doi: 10.15288/jsad.2018.79.423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Wen H, Hockenberry JM, Cummings JR. The effect of medical marijuana laws on adolescent and adult use of marijuana, alcohol, and other substances. J Health Econ. 2015;42:64–80. doi: 10.1016/j.jhealeco.2015.03.007. [DOI] [PubMed] [Google Scholar]
- 48.Substance Abuse and Mental Health Services Administration. 2019 National Survey on Drug Use and Health: Methodological summary and definitions. [Internet]. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2020 [cited 2022 Apr 23]. Available from: https://www.samhsa.gov/data/. Accessed 23 Apr 2022
- 49.Substance Abuse and Mental Health Services Administration. Key substance use and mental health indicators in the United States: Results from the 2019 National Survey on Drug Use and Health [Internet]. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration; 2020 [cited 2021 Mar 10]. (NSDUH Series H-55). Report No.: PEP20-07-01–001. Available from: https://www.samhsa.gov/data/. Accessed 21 Mar 2022
- 50.Procon. Legal Medical & Recreational Marijuana States and DC. [Internet]. 2022 Mar. Available from: https://marijuana.procon.org/legal-recreational-marijuana-states-and-dc/. Accessed 8 Mar 2022
- 51.RAND Corporation. OPTIC-Vetted Policy Data Sets: Medical Marijuana Policy Data [Internet]. [cited 2022 Apr 26]. Available from: https://www.rand.org/health-care/centers/optic/resources/datasets.html. Accessed 26 Apr 2022
- 52.Alcohol Policy Information System. Cannabis Policy Topics. Recreational Use of Cannabis: Volume 1 [Internet]. National Institute on Alcohol Abuse and Alcoholism; [cited 2022 Apr 25]. Available from: https://alcoholpolicy.niaaa.nih.gov/cannabis-policy-topics/recreational-use-of-cannabis-volume-1/104/about-this-policy. Accessed 20 Apr 2022
- 53.Marijuana Policy Project [Internet]. Washington; 2020. Available from: https://www.mpp.org/issues/medical-marijuana/state-by-state-medical-marijuana-laws. Accessed 26 Apr 2022
- 54.Martins SS, Segura LE, Levy NS, Mauro PM, Mauro CM, Philbin MM, et al. Racial and Ethnic Differences in Cannabis Use Following Legalization in US States With Medical Cannabis Laws. JAMA Netw Open. 2021;4(9):e2127002. doi: 10.1001/jamanetworkopen.2021.27002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Cerdá M, Mauro C, Hamilton A, Levy NS, Santaella-Tenorio J, Hasin D, et al. Association Between Recreational Marijuana Legalization in the United States and Changes in Marijuana Use and Cannabis Use Disorder From 2008 to 2016. JAMA Psychiatry. 2020;77(2):165. doi: 10.1001/jamapsychiatry.2019.3254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Segura LE, Mauro CM, Levy NS, Khauli N, Philbin MM, Mauro PM, et al. Association of US Medical Marijuana Laws With Nonmedical Prescription Opioid Use and Prescription Opioid Use Disorder. JAMA Netw Open. 2019;2(7):e197216. doi: 10.1001/jamanetworkopen.2019.7216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Little RJ. To Model or Not To Model? Competing Modes of Inference for Finite Population Sampling. J Am Stat Assoc. 2004;99(466):546–56. doi: 10.1198/016214504000000467. [DOI] [Google Scholar]
- 58.VanderWeele TJ, Ding P. Sensitivity Analysis in Observational Research: Introducing the E-Value. Ann Intern Med. 2017;167(4):268. doi: 10.7326/M16-2607. [DOI] [PubMed] [Google Scholar]
- 59.Haneuse S, VanderWeele TJ, Arterburn D. Using the E-Value to Assess the Potential Effect of Unmeasured Confounding in Observational Studies. JAMA. 2019;321(6):602. doi: 10.1001/jama.2018.21554. [DOI] [PubMed] [Google Scholar]
- 60.Elm E von, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007 Oct 20;335(7624):806–8. [DOI] [PMC free article] [PubMed]
- 61.Field M, Wiers RW, Christiansen P, Fillmore MT, Verster JC. Acute alcohol effects on inhibitory control and implicit cognition: implications for loss of control over drinking. Alcohol Clin Exp Res. 2010 Aug;34(8):1346–52. [DOI] [PMC free article] [PubMed]
- 62.Claus ED, Feldstein Ewing SW, Magnan RE, Montanaro E, Hutchison KE, Bryan AD. Neural mechanisms of risky decision making in adolescents reporting frequent alcohol and/or marijuana use. Brain Imaging Behav. 2018;12(2):564–76. doi: 10.1007/s11682-017-9723-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Kroon E, Kuhns L, Cousijn J. The short-term and long-term effects of cannabis on cognition: recent advances in the field. Curr Opin Psychol. 2021;38:49–55. doi: 10.1016/j.copsyc.2020.07.005. [DOI] [PubMed] [Google Scholar]
- 64.Nigg JT, Wong MM, Martel MM, Jester JM, Puttler LI, Glass JM, et al. Poor Response Inhibition as a Predictor of Problem Drinking and Illicit Drug Use in Adolescents at Risk for Alcoholism and Other Substance Use Disorders. J Am Acad Child Adolesc Psychiatry. 2006;45(4):468–75. doi: 10.1097/01.chi.0000199028.76452.a9. [DOI] [PubMed] [Google Scholar]
- 65.Klieger SB, Gutman A, Allen L, Pacula RL, Ibrahim JK, Burris S. Mapping medical marijuana: state laws regulating patients, product safety, supply chains and dispensaries, 2017: State medical marijuana laws. Addiction. 2017;112(12):2206–16. doi: 10.1111/add.13910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lloyd SL, Striley CW. Marijuana Use Among Adults 50 Years or Older in the 21st Century. Gerontol Geriatr Med. 2018;4:233372141878166. doi: 10.1177/2333721418781668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Salas-Wright CP, Vaughn MG, Cummings-Vaughn LA, Holzer KJ, Nelson EJ, AbiNader M, et al. Trends and correlates of marijuana use among late middle-aged and older adults in the United States, 2002-2014. Drug Alcohol Depend. 2017;171:97–106. doi: 10.1016/j.drugalcdep.2016.11.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Mauro PM, Askari MS, Han BH. Gender differences in any alcohol screening and discussions with providers among older adults in the United States, 2015 to 2019. Alcohol Clin Exp Res. 2021;45(9):1812–20. doi: 10.1111/acer.14668. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 46 kb)