Abstract
Background
The relationship between elevated body mass index (BMI) and adverse outcomes in joint arthroplasty is well established in the literature. This paper aims to challenge the conventional thought of excluding patients from a total knee or hip replacement based on BMI alone. Instead, we propose using the metabolic syndrome (MetS) and its defining components to better identify patients at high risk for intraoperative and postoperative complications.
Methods
Patients who underwent primary, elective total knee and total hip arthroplasty were identified in the 2015-2020 American College of Surgeons National Surgical Quality Improvement Program database. Several defining components of MetS, such as hypertension, diabetes, and obesity, were compared to a metabolically healthy cohort. Postoperative outcomes assessed included mortality, length of hospital stay, 30-day surgical and medical complications, and discharge.
Results
The outcomes of 529,737 patients from the American College of Surgeons National Surgical Quality Improvement Program who underwent total knee and total hip arthroplasty were assessed. MetS is associated with increased complications and increased mortality. Both hypertension and diabetes are associated with increased complications but have no impact on mortality. Interestingly, while obesity was associated with increased complications, there was a significant decrease in mortality.
Conclusions
Our results show that the impact of MetS is more than the sum of its constitutive parts. Additionally, obese patients experience a protective effect, with lower mortality than their nonobese counterparts. This study supports moving away from strict BMI cutoffs alone for someone to be eligible for an arthroplasty surgery and offers more granular data for risk stratification and patient selection.
Keywords: Metabolic syndrome, Obesity, Total joint replacement, 30-Day outcomes, Complications
Introduction
Over the past several decades, arthroplasty utilization has increased per capita and overall volume [[1], [2], [3], [4], [5]]. This increase in arthroplasty has been linked to the concurrent rise in obesity, as higher adiposity is strongly associated with a higher incidence and earlier onset of degenerative joint disease with the subsequent need for arthroplasty [6,7]. Orthopedic surgeons are increasingly faced with the challenge of stratifying a patient’s intraoperative and postoperative risk level and often resort to body mass index (BMI) values. A BMI of 40 kg/m2 is often used as a cut-off value above which many surgeons will not perform total knee arthroplasty (TKA) or total hip arthroplasty (THA) [8,9].
This paper assesses an increasingly prevalent medical condition known as metabolic syndrome (MetS) and its defining components to gauge better the risks associated with undergoing a total joint replacement. Although there are various definitions, generally, the MetS includes at least a combination of 3 of the following: obesity (waist circumference), high fasting glucose (or diabetes mellitus), dyslipidemia, and hypertension [10]. MetS is associated with increased complications, poor outcomes across multiple surgical specialties, and an increased risk of serious cardiovascular events such as myocardial infarction [11]. As patients become more obese, more medically complex, and increasingly comorbid, a better understanding of their risk profiles is warranted [[12], [13], [14], [15]]. This study aims to assess the impact of MetS and its components (hypertension, diabetes, and obesity) on total joint arthroplasty outcomes. We hypothesize that patients who are obese but metabolically healthy (eg, do not have the triad of comorbidities for MetS) will have similar outcomes compared to nonobese metabolically healthy patients, while patients with MetS will have increased complications associated with their arthroplasty.
Material and methods
Data source
This retrospective study utilized the American College of Surgeons National Surgical Quality Improvement Program (ACS-NSQIP). The ACS-NSQIP is a national dataset that has been well validated and contains demographics, preoperative, perioperative, and postoperative data on patients undergoing surgical procedures [16,17]. Quality of data is ensured through stringent audits by NSQIP at participating sites.
Study population and outcomes
For this study, patients undergoing elective TKA or THA older than 18 years of age were included. Patients with other concurrent procedures were excluded to focus on the procedures of interest and minimize confounding factors. Patients with missing or incorrect data were also excluded. Data were drawn from the ACS-NSQIP by querying for current procedural terminology codes 27130 (THA) and 27447 (TKA). As the ACS-NSQIP does not include all of the criteria for defining MetS, a modified definition was needed for this study. Similar to other studies, we used validated criteria for defining modified MetS: BMI >30 kg/m2, a diagnosis of diabetes mellitus, and hypertension requiring medication [18,19].
Variable selection
Preoperative variables from the NSQIP included patient demographics such as age, sex, race, ethnicity, height, and weight, medical comorbidities; smoking within the past year; currently undergoing dialysis; and American Society of Anesthesiology classification. BMI was calculated using height and weight. Intraoperative data collected were the procedure and type of anesthesia.
Postoperative outcomes extracted were 30-day complications, Clavien-Dindo IV life-threatening complications, hospital length of stay, readmission, and adverse discharge disposition [20]. Complications were grouped by organ system and are defined as the following occurrences within 30 days of surgery; cardiac complication is defined as any occurrence of cardiac arrest requiring cardiopulmonary resuscitation or myocardial infarction; pulmonary complication is defined as any occurrence of pneumonia, pulmonary embolism, unplanned intubation, or being on a ventilator for more than 48 hours; renal complication is defined as occurrence of acute renal failure or progressive renal insufficiency; hematological complication is defined as occurrence of deep vein thrombosis or bleeding requiring a transfusion; and wound complication is defined as the occurrence of a superficial or deep surgical site infection or wound dehiscence. Clavien Dindo IV life-threatening complication was defined as having any of the following occurrences: cardiac arrest requiring cardiopulmonary resuscitation, myocardial infarction, septic shock, pulmonary embolism, acute renal failure, or cerebrovascular accidentstrok with a neurological defect within 30 days of surgery.
Statistical analysis
To assess each component of MetS individually, patients with a single component (eg, obesity) were compared to a metabolically healthy cohort without the characteristic of interest (eg, nonobese patients who, by definition, do not meet the 3 comorbidities for MetS). For patients with MetS, the comparison group consisted of patients who did not meet all 3 criteria for MetS. The obese cohort, patients with a BMI>30 kg/m2, but without MetS, was compared to a metabolically healthy nonobese cohort. In a similar fashion, the remaining 2 cohorts, one comprised of patients with hypertension and one with diabetes, were compared to a group without hypertension or diabetes, respectively. This design allowed us to isolate and compare MetS and its individual components to a metabolically healthy control group.
Categorical results are reported as counts with group percentages. Continuous data are reported as means and standard deviations. Pearson’s chi-square or Fisher's exact test was performed for demographics, comorbidities, preoperative, and intraoperative data to compare baseline differences between MetS patients, metabolically healthy patients, and patients with a single comorbidity. All covariates with a P-value < .1 were controlled for in multivariate regression as an independent variable. Outcomes required a preadjusted P-value of P < .05 to be considered for multivariate logistic regression. Variables with a P-value < .05 after multivariate regression were considered significant, and results were reported as adjusted odds ratio (OR) and 95% confidence intervals (95% CI). All statistical analysis was done using the R Foundation for Statistical Computing software version 4.20.
Results
For inclusion, 529,737 patients who underwent THA or TKA between 2015-2020 were identified. Patient characteristics such as demographics, medical comorbidities, and preoperative and intraoperative data were collected from the ACS-NSQIP. A total of 54,709 patients met our modified definition of MetS, while 475,028 did not have it. The preoperative baseline characteristics of the patients are shown in Table 1.
Table 1.
Preoperative demographics, preoperative, intraoperative, and operative data for patients undergoing total joint arthroplasty.
| Variable | Mets | No mets | P-value |
|---|---|---|---|
| Demographics | |||
| Age (y) | 66.6 ± 8.3 | 66.4 ± 10.3 | <.001 |
| Body mass index | 36.8 ± 5.4 | 30.9 ± 6.4 | <.001 |
| BMI category | <.001 | ||
| <30 | 0 (0.0) | 223,101 (47.0) | |
| 30-34.99 | 21,638 (39.6) | 128,749 (27.1) | |
| 35-39.99 | 18,516 (33.8) | 76,206 (16.1) | |
| ≥40 | 14,555 (26.6) | 46,608 (9.8) | |
| Hispanic | 3838 (7.0) | 20,812 (4.4) | <.001 |
| Race | <.001 | ||
| American Indian or Alaska Native | 360 (0.7) | 2148 (0.5) | |
| Asian | 899 (1.6) | 8895 (1.9) | |
| Black or African American | 6924 (12.7) | 36,026 (7.6) | |
| Native Hawaiian or Pacific Islander | 237 (0.4) | 1412 (0.3) | |
| Unknown/not reported | 8770 (16.0) | 86,294 (18.2) | |
| White | 37,502 (68.5) | 339,817 (71.6) | |
| Other | 17 (0.0) | 72 (0.0) | |
| Gender | <.001 | ||
| Female | 30,249 (55.3) | 280,024 (59.0) | |
| Male | 24,460 (44.7) | 194,627 (41.0) | |
| Comorbidity | |||
| Ascites | 6 (0.0) | 59 (0.0) | .929 |
| Bleeding disorders | 1480 (2.7) | 8312 (1.8) | <.001 |
| Preoperative dialysis | 134 (0.2) | 801 (0.2) | <.001 |
| Diabetes | <.001 | ||
| IDDM | 13,750 (25.1) | 6085 (1.3) | |
| NIDDM | 40,959 (74.9) | 23,792 (5.0) | |
| Disseminated cancer | 74 (0.1) | 924 (0.2) | .003 |
| Dyspnea | <.001 | ||
| At rest | 197 (0.4) | 658 (0.1) | |
| At moderate exertion | 4601 (8.4) | 21,211 (4.5) | |
| Functional status prior to surgery | <.001 | ||
| Independent | 53,521 (97.8) | 467,290 (98.4) | |
| Partially dependent | 856 (1.6) | 5151 (1.1) | |
| Totally dependent | 21 (0.0) | 204 (0.0) | |
| Congestive heart failure in 30 d | 424 (0.8) | 1438 (0.3) | <.001 |
| Prior to surgery | |||
| History of severe COPD | 2856 (5.2) | 15,789 (3.3) | <.001 |
| Hypertension requiring medication | 54,709 (100.0) | 266,427 (56.1) | <.001 |
| History of systemic sepsis | .002 | ||
| Sepsis | 7 (0.0) | 24 (0.0) | |
| Septic shock | 1 (0.0) | 8 (0.0) | |
| SIRS | 164 (0.3) | 1099 (0.2) | |
| Acute renal failure | 37 (0.1) | 123 (0.0.) | <.001 |
| Smoker within past year | 4529 (8.3) | 45,740 (9.6) | <.001 |
| Chronic steroid use | 1754 (3.2) | 17,076 (3.6) | <.001 |
| Transfusion within 72 h of surgery | 15 (0.0) | 202 (0.0) | .122 |
| Ventilator dependent | |||
| Wound infection | 132 (0.2) | 659 (0.1) | <.001 |
| >10% Weight loss in the last 6 mo | 47 (0.1) | 594 (0.1) | .015 |
| Preoperative | |||
| ASAa class | <.001 | ||
| I | 56 (0.1) | 12,583 (2.7) | |
| II | 11,816 (21.6) | 249,259 (52.5) | |
| III | 40,770 (74.5) | 205,964 (43.4) | |
| IV | 2062 (3.8) | 6836 (1.4) | |
| V | 5 (0.0) | 22 (0.0) | |
| Time to operation | .743 | ||
| >2 d | 122 (0.2) | 1097 (0.2) | |
| 0-2 d | 54,587 (99.8) | 473,567 (99.8) | |
| Transferred from | .106 | ||
| Acute care hospital inpatient | 38 (0.1) | 459 (0.1) | |
| Home | 54,440 (99.5) | 472,283 (99.5) | |
| Nursing home/chronic care | 108 (0.2) | 820 (0.2) | |
| Other/unknown | 114 (0.2) | 975 (0.2) | |
| Outside emergency department | 9 (0.0) | 127 (0.0) | |
| Operative | |||
| Anesthesia type | |||
| General | 25,705 (47.0) | 195,478 (41.2) | <.001 |
| Other | 28,998 (53.0) | 279,134 (58.8) | |
| Procedure | <.001 | ||
| THA | 14,714 (26.9) | 189,418 (39.9) | |
| TKA | 39,995 (73.1) | 285,246 (60.1) | |
Boldface values indicate statistical significance (P < .05).
American Society of Anesthesiologists Physical Status Classification System.
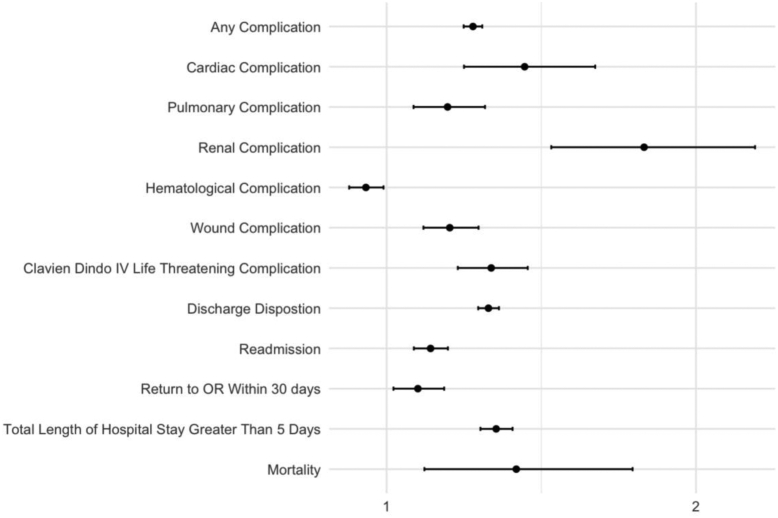
Postoperative data were collected from the ACS-NSQIP and analyzed for significant baseline differences between the cohorts (Table 2). Following baseline differences, significant outcomes were analyzed further through multivariate regression. Multivariate analysis found that patients with MetS had increased odds of having any complication (OR 1.279 [95% CI 1.249-1.309]; P < .001), cardiac complications (OR 1.446 [95% CI 1.25-1.674]; P < .001), renal complications (OR 1.832 [95% CI 1.532-2.191]; P < .001), wound complications (OR 1.204 [95% CI 1.119-1.297]; P < .001), life-threatening complications (OR 1.338 [95% CI 1.23-1.456]; P < .001), an adverse discharge (OR 1.329 [95% CI 1.296-1.363]; P < .001), an extended hospital stay (OR 1.354 [95% CI 1.303-1.407]; P < .001) and 30-day mortality (OR 1.419 [95% CI 1.22-1.795]; P = .004) when compared to patients without MetS. Patients with MetS were also 1.142 times more likely to return to the hospital within 30 days ([95% CI 1.088-1.198; P < .001) and 1.101 times more likely to return to the OR within 30 days ([95% CI 1.022-1.186]; P = .011, Table 3, Figure 1) than patients without MetS.
Table 2.
Postoperative outcomes for patients undergoing total joint arthroplasty.
| Variable | Mets | No mets | P-value |
|---|---|---|---|
| Postoperative | |||
| Any complication | 12,583 (23.0) | 75,403 (15.9) | <.001 |
| Cardiac complication | 248 (0.5) | 1084 (0.2) | <.001 |
| Cardiac arrest requiring cardiopulmonary resuscitation | 67 (0.1) | 303 (0.1) | <.001 |
| Myocardial infarction | 198 (0.4) | 831 (0.2) | <.001 |
| Pulmonary complication | 553 (1.0) | 3087 (0.7) | <.001 |
| Pneumonia | 227 (0.4) | 1194 (0.3) | <.001 |
| Pulmonary embolism | 246 (0.4) | 1631 (0.3) | <.001 |
| On ventilator greater than 48h | 51 (0.1) | 183 (0.0) | <.001 |
| Unplanned intubation | 123 (0.2) | 477 (0.1) | <.001 |
| Hematological complication | 1403 (2.6) | 11,777 (2.5) | .242 |
| Bleeding requiring transfusion | 1103 (2.0) | 9288 (2.0) | .352 |
| Deep vein thrombosis | 311 (0.6) | 2588 (0.5) | .505 |
| Renal complication | 186 (0.3) | 492 (0.1) | <.001 |
| Progressive renal insufficiency | 114 (0.2) | 338 (0.1) | <.001 |
| Acute renal failure | 75 (0.1) | 155 (0.0) | <.001 |
| Wound complication | 953 (1.7) | 5443 (1.1) | <.001 |
| Wound disruption | 159 (0.3) | 800 (0.2) | <.001 |
| Superficial incisional SSI | 550 (1.0) | 3249 (0.7) | <.001 |
| Deep incisional SSI | 113 (0.2) | 582 (0.1) | <.001 |
| Organ/space SSI | 195 (0.4) | 1103 (0.2) | <.001 |
| Clavien-Dindo IV complicationa | 744 (1.4) | 3767 (0.8) | <.001 |
| Stroke/cerebrovascular accident | 70 (0.1) | 340 (0.1) | <.001 |
| Septic shock | 47 (0.1) | 192 (0.0) | <.001 |
| Sepsis | 159 (0.3) | 782 (0.2) | <.001 |
| Urinary tract infection | 534 (1.0) | 3155 (0.7) | <.001 |
| Discharge destination | <.001 | ||
| Home | 44,381 (81.1) | 416,052 (87.7) | |
| Nonhome | 10,328 (19.9) | 58,612 (12.3) | |
| Mortality | 96 (0.2) | 430 (0.1) | <.001 |
| 30 d readmission | 2282 (4.2) | 13,870 (2.9) | <.001 |
| 30 d unplanned reoperation | 905 (1.7) | 6181 (1.3) | <.001 |
| Length of stay | <.001 | ||
| >5 d | 3791 (6.9) | 20,392 (4.3) | |
| 0-5 d | 50,918 (93.1) | 454,272 (95.7) | |
Boldface values indicate statistical significance (P < .05).
Clavien-Dindo IV complications also include cardiac arrest, myocardial infarction, acute renal failure, stroke, sepsis, and pulmonary embolism.
Table 3.
Multivariate logistic regression for postoperative complications of patients with metabolic syndrome metabolic syndrome odds ratio.
| Complication | Odds ratio | 95% CI | P value |
|---|---|---|---|
| Any complication | 1.279 | 1.249-1.309 | <.001 |
| Cardiac complication | 1.446 | 1.25-1.674 | <.001 |
| Pulmonary complication | 1.197 | 1.087-1.318 | <.001 |
| Renal complication | 1.832 | 1.532-2.191 | <.001 |
| Hematological complication | 0.933 | 0.879-0.99 | .022 |
| Wound complication | 1.204 | 1.119-1.297 | <.001 |
| Clavien-Dindo IV life threatening complication | 1.338 | 1.23-1.456 | <.001 |
| Discharge disposition | 1.329 | 1.296-1.363 | <.001 |
| Readmission | 1.142 | 1.088-1.198 | <.001 |
| Return to OR within 30 d | 1.101 | 1.022-1.186 | .011 |
| Total length of hospital stay greater than 5 d | 1.354 | 1.303-1.407 | <.001 |
| Mortality | 1.419 | 1.122-1.795 | .004 |
Boldface values indicate statistical significance (P < .05).
Figure 1.
Forest plot of odds ratios for multivariate regression of postoperative complications for patients with metabolic syndrome.
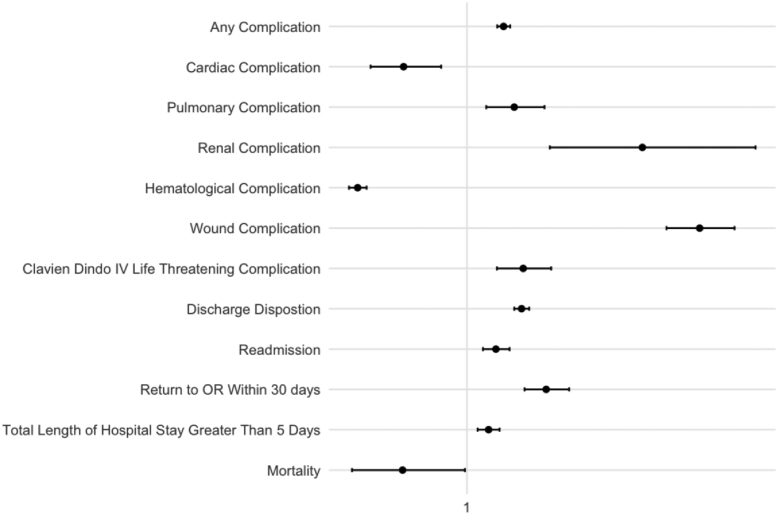
Obese patients (BMI > 30) and nonobese metabolically healthy patients' 30-day outcomes were compared after controlling for covariates (Table 4, Fig. 2). Obese patients who did not meet our criteria for MetS were more likely to have pulmonary complications (OR 1.142 [95% CI 1.058-1.233]; P = .001), renal complications (OR 1.527 [95% CI 1.249-1.867]; P < .001), wound complications(OR 1.699 [95% CI 1.599-1.804; P < .001), an adverse discharge (OR 1.164 [95% CI 1.142-1.187; P < .001), readmission to the hospital (OR 1.087 [95% CI 1.048-1.128; P < .001), a return to the OR within 30 days (OR 1.238 [95% CI 1.173-1.307]; P < .001), and an extended hospital stay (OR 1.065 [95% CI 1.032-1.098]; P < .001) than nonobese metabolically healthy patients. Non-MetS obese patients were 0.810 times less likely ([95% CI 0.711-0.923]; P = .002) to have cardiac complications, 0.672 times less likely ([95% CI 0.646-0.699; P < .001) to have hematological complications, and had reduced (0.807 times less) mortality ([95% CI 0.655-0.994]; P = .044). Significant full comparisons controlled for covariates for metabolically healthy patients with obese type 1 (30 kg/m2<BMI<35 kg/m2), obese type 2 (35 kg/m2<BMI<40 kg/m2), obese type 3 (BMI>40 kg/m2), diabetes, and hypertension compared to metabolically healthy patients without the corresponding component were also reported (Tables 5 and 6).
Table 4.
Multivariate logistic regression for postoperative complications of obese but metabolically healthy patients BMI split odds ratio.
| Complication | Odds ratio | 95% CI | P value |
|---|---|---|---|
| Any complication | 1.11 | 1.091-1.13 | <.001 |
| Cardiac complication | 0.81 | 0.711-0.923 | .002 |
| Pulmonary complication | 1.142 | 1.058-1.233 | .001 |
| Renal complication | 1.527 | 1.249-1.867 | <.001 |
| Hematological complication | 0.672 | 0.646-0.699 | <.001 |
| Wound complication | 1.699 | 1.599-1.804 | <.001 |
| Clavien-Dindo IV life threatening complication | 1.169 | 1.09-1.253 | <.001 |
| Discharge disposition | 1.164 | 1.142-1.187 | <.001 |
| Readmission | 1.087 | 1.048-1.128 | <.001 |
| Return to OR within 30 d | 1.238 | 1.173-1.307 | <.001 |
| Total length of hospital stay greater than 5 d | 1.065 | 1.032-1.098 | <.001 |
| Mortality | 0.807 | 0.655-0.994 | .044 |
Boldface values indicate statistical significance (P < .05).
Figure 2.
Forest plot of odds ratios for multivariate regression of postoperative complications for obese but metabolically healthy patients.
Table 5.
Multivariate logistic regression for postoperative complications for type I, type II, and type III obese but metabolically healthy.
| Complication | Odds ratio | 95% CI | P value |
|---|---|---|---|
| Type I obesity odds ratio | |||
| Any complication | 1.018 | 0.997-1.039 | .091 |
| Cardiac complication | 0.823 | 0.706-0.96 | .013 |
| Pulmonary complication | 1.115 | 1.019-1.22 | .018 |
| Renal complication | 1.406 | 1.108-1.784 | .005 |
| Hematological complication | 0.72 | 0.686-0.754 | <.001 |
| Wound complication | 1.377 | 1.282-1.48 | <.001 |
| Clavien-Dindo IV life threatening complication | 1.116 | 1.029-1.211 | .008 |
| Discharge disposition | 1.054 | 1.029-1.078 | <.001 |
| Readmission | 1.016 | 0.973-1.061 | .477 |
| Return to OR within 30 d | 1.084 | 1.016-1.156 | .015 |
| Total length of hospital stay greater than 5 d | 0.999 | 0.962-1.036 | .943 |
| Mortality | 0.822 | 0.641-1.055 | .123 |
| Type II obesity odds ratio | |||
| Any complication | 1.123 | 1.095-1.151 | <.001 |
| Cardiac complication | 0.723 | 0.588-0.888 | .002 |
| Pulmonary complication | 1.188 | 1.067-1.323 | .002 |
| Renal complication | 1.245 | 0.923-1.679 | .152 |
| Hematological complication | 0.627 | 0.59-0.667 | <.001 |
| Wound complication | 1.701 | 1.568-1.846 | <.001 |
| Clavien-Dindo IV life threatening complication | 1.188 | 1.076-1.313 | .001 |
| Discharge disposition | 1.189 | 1.156-1.223 | <.001 |
| Readmission | 1.076 | 1.02-1.133 | .007 |
| Return to OR within 30 d | 1.268 | 1.175-1.37 | <.001 |
| Total length of hospital stay greater than 5 d | 1.01 | 0.965-1.058 | .655 |
| Mortality | 0.771 | 0.562-1.059 | .108 |
| Type III obesity odds ratio | |||
| Any complication | 1.419 | 1.377-1.463 | <.001 |
| Cardiac complication | 0.972 | 0.765-1.235 | .817 |
| Pulmonary complication | 1.133 | 0.99-1.296 | .07 |
| Renal complication | 2.782 | 2.083-3.716 | <.001 |
| Hematological complication | 0.568 | 0.525-0.614 | <.001 |
| Wound complication | 2.538 | 2.316-2.781 | <.001 |
| Clavien-Dindo IV life threatening complication | 1.364 | 1.209-1.54 | <.001 |
| Discharge disposition | 1.562 | 1.511-1.615 | <.001 |
| Readmission | 1.289 | 1.211-1.373 | <.001 |
| Return to OR within 30 d | 1.703 | 1.558-1.862 | <.001 |
| Total length of hospital stay greater than 5 d | 1.381 | 1.311-1.455 | <.001 |
| Mortality | 0.792 | 0.533-1.176 | .248 |
Boldface values indicate statistical significance (P < .05).
Table 6.
Multivariate logistic regression for postoperative complications for hypertension and diabetes but metabolically healthy.
| Complication | Odds ratio | 95% CI | P value |
|---|---|---|---|
| Diabetes odds ratio | |||
| Any complication | 1.257 | 1.219-1.297 | <.001 |
| Cardiac complication | 1.405 | 1.159-1.703 | .001 |
| Pulmonary complication | 1.103 | 0.695-1.26 | .151 |
| Renal complication | 1.871 | 1.408-2.485 | <.001 |
| Hematological complication | 1.153 | 1.078-1.233 | <.001 |
| Wound complication | 0.988 | 0.881-1.107 | .831 |
| Clavien-Dindo IV life threatening complication | 1.27 | 1.132-1.425 | <.001 |
| Discharge disposition | 1.287 | 1.244-1.332 | <.001 |
| Readmission | 1.161 | 1.089-1.237 | <.001 |
| Return to OR within 30 d | 0.988 | 0.889-1.097 | .818 |
| Total length of hospital stay greater than 5 d | 1.367 | 1.3-1.436 | <.001 |
| Mortality | 1.309 | 0.973-1.76 | .075 |
| Hypertension odds ratio | |||
| Any complication | 1.147 | 1.127-1.168 | <.001 |
| Cardiac complication | 1.635 | 1.415-1.89 | <.001 |
| Pulmonary complication | 1.111 | 1.027-1.201 | .008 |
| Renal complication | 2.332 | 1.84-2.955 | <.001 |
| Hematological complication | 1.07 | 1.028-1.114 | .001 |
| Wound complication | 1.066 | 1.006-1.129 | .031 |
| Clavien-Dindo IV life threatening complication | 1.202 | 1.119-1.291 | <.001 |
| Discharge disposition | 1.177 | 1.154-1.2 | <.001 |
| Readmission | 1.202 | 1.158-1.248 | <.001 |
| Return to OR within 30 d | 1.167 | 1.105-1.232 | <.001 |
| Total length of hospital stay greater than 5 d | 0.996 | 0.966-1.028 | .823 |
| Mortality | 1.176 | 0.945-1.465 | .147 |
Boldface values indicate statistical significance (P < .05).
Discussion
Our analysis of the impact of MetS on arthroplasty produced mixed but intriguing results. MetS was associated with a significant increase in complications, including Clavien-Dindo grade IV (life-threatening) complications and an increase in mortality. For both the hypertension and diabetes alone groups, patients experienced a significant increase in complications; however, they had no change in mortality. Interestingly, when obesity was examined independently, we found that mortality decreased significantly, despite an increase in complications (albeit a smaller increase than in MetS patients). While the odds of complication increased as the obesity class increased, the reduction in mortality remained significant in both class I and II obesity. For class III obesity, there was no significant change; however, it is quite notable that there is no increase in mortality for these patients.
In general, these findings are consistent with the literature. Della Valle et al. found that MetS was associated with increased major complications, nonroutine discharge, and higher hospital costs [21]. In a meta-analysis, Guofeng et al. confirmed this increase in complications; however, contrary to our results, they found no difference in mortality [22]. Despite this difference, we have confidence in our findings due to our exceptionally large sample size and statistical power. Furthermore, this particular outcome is still debated in the literature. For example, Cichos et al. found that MetS was associated with decreased mortality in hip fracture patients [23]. While this result seems suspect at first glance, there is ample evidence of a reduction in mortality in obese patients (a core component of MetS) in orthopedic surgery [[24], [25], [26], [27]].
Our component-based analysis provides further support for this obesity paradox—the reduced mortality in obese patients—and offers an explanation for the mixed findings surrounding MetS and mortality. While we did find a significant increase in mortality, it was relatively modest compared to the large increase in complications that MetS patients experienced. We isolated obesity as the only individual component to significantly impact mortality, but it was also associated with decreased mortality. This result explains the mixed findings surrounding MetS patients, who are at higher risk due to their multiple comorbidities but benefit from the protective effect of obesity. Obese patients appear more robust than their nonobese counterparts in the general population. Further exploration of this phenomenon could yield results that aid in extending this protective effect to nonobese patients.
Of note, our results suggest that MetS patients' outcomes are not solely attributable to the comorbidities composing it, indicating an underlying or superimposed disease process impacting outcomes. Gandhi et al. had similar findings: MetS patients' increased risk was greater than the expected sum of the constitutive parts [28]. Put simply, the 3 comorbidities assessed—obesity, diabetes, and hypertension—did not adequately explain the risk of MetS patients. Similarly, Gage et al. found that MetS was associated with increased complications unattributable to obesity alone [29]. Edelstein et al. found that a higher BMI did not significantly increase complications in MetS patients, contending that MetS was a more valuable risk assessment data point than BMI in arthroplasty [30]. This indicates that obese but metabolically healthy patients are not as risky as conventional wisdom would assume. MetS, rather than obesity, is the more concerning risk factor in arthroplasty patients.
Still, there are negative impacts of excess adiposity on total joint arthroplasty, and weight loss for obese patients is encouraged. However, weight loss interventions with arthroplasty have produced mixed results and minimal efficacy, so guidance remains unclear [31,32]. Only 7% of morbidly obese patients attain a BMI under 40 kg/m2 through lifestyle changes, suggesting weight loss is unrealistic for most. Further, Seward and Chen found that bariatric surgery was associated with increased complications. In conjunction with the rise of obesity and increased arthroplasty utilization (attributable to both obesity and a secular trend), these studies point to a need for improved data in orthopedic surgery on obese patients [33].
Together, these findings question the joint arthroplasty BMI cutoff of 40 kg/m2 [34]. Patients with a BMI >40 kg/m2 can experience significant benefits from arthroplasty, reporting reduced pain and improved joint function, so withholding care ought to have ample evidence [35]. However, Roth et al. did not find any BMI cutoff had a substantial positive predictive value, suggesting it is an inappropriate metric for patient selection if used in isolation [36]. Similarly, Foreman et al. found that, in isolation, a BMI of 40 or higher did not dramatically increase complications [37]. Adhikary et al. found that patients with a BMI between 40 kg/m2 and 45 kg/m2 have a significantly lower risk profile than those with a BMI>45 kg/m2 [38]. Giori et al. concluded that a BMI cutoff of 40 kg/m2 had little impact on preventing poor outcomes, denying 14 times as many patients a complication-free procedure per complication avoided [34]. Furthermore, Nowak et al. found that complications in obese patients with BMIs of 40 kg/m2-45 kg/m2 have decreased in recent years, suggesting improvements in the care of this demographic [39]. These studies find little benefit to a BMI >40 cutoff, but the cost of denying patients care remains [40].
The risk of complication is inherent in any surgery, including arthroplasty. A discussion of acceptable risk ought to occur between the surgeon and patient, considering the potential benefits and the consequences of complications. This study provides more granular data, facilitating better risk assessment of patients with a set of common comorbidities. For example, a patient with a BMI of 42 kg/m2 but no other comorbidities—typically ineligible—may be a suitable arthroplasty candidate. In contrast, a patient with a more moderate BMI but MetS may have a risk profile substantially greater than conventional tools predict. Current practice would exclude the former but not the latter, a problematic outcome given the evidence on the subject.
Kerbel et al. found that appropriate risk stratification in morbidly obese patients brought complication rates in line with nonobese patients following TKA, indicating that the increased complication rates in obese patients can be avoided, further supporting the abolition of strict BMI cutoffs [41]. Instead, efforts should move toward optimizing care for these patients. Targeted interventions can accomplish this; Sayed-Noor et al. found that reoperation rates were higher in obese patients [42]. They found this was primarily from increased rates of postoperative infection and proposed customized preoperative prophylaxis. These studies support moving away from strict BMI criteria, as improved management and interventions can improve outcomes in these traditionally labeled higher-risk groups.
Limitations
As with any study, ours is not without limitations. This was a retrospective study. While the NSQIP gives us access to an extraordinarily large sample of 529,737 patients, it lacks several key variables, such as patient-reported outcomes, surgical approaches, and outcomes and complications, such as revision surgery, beyond 30 days. Analysis of these metrics at 1 year, 5 years, and beyond would provide valuable data. Additionally, we could not control for patient socioeconomic status, insurance status, and rehabilitation protocol, all of which may influence outcomes in arthroplasty. Future work would include designing a prospective study to more closely examine the components of MetS and their impact on arthroplasty patients.
Conclusions
A component-based analysis of MetS shows that neither hypertension nor diabetes is associated with changes in mortality. Furthermore, our results indicate that the total increase of complications in MetS is more than a cumulative effect of all 3 traits; no single comorbidity adequately predicted the observed complication rates. Most importantly, we found that obesity offers a protective effect, reducing mortality despite relatively higher rates of complications. Our study can aid surgeons in selecting patients for arthroplasty despite having traditionally disqualifying characteristics.
Conflicts of interest
The authors declare there are no conflicts of interest.
For full disclosure statements refer to https://doi.org/10.1016/j.artd.2023.101139.
Appendix A. Supplementary data
References
- 1.Wolford M.L., Palso K., Bercovitz A. Hospitalization for total hip replacement among inpatients aged 45 and over: United States, 2000-2010. NCHS Data Brief. 2015:1–8. [PubMed] [Google Scholar]
- 2.Cram P., Lu X., Kates S.L., Singh J.A., Li Y., Wolf B.R. Total knee arthroplasty volume, utilization, and outcomes among Medicare beneficiaries, 1991-2010. JAMA. 2012;308:1227–1236. doi: 10.1001/2012.jama.11153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Maradit Kremers H., Larson D.R., Crowson C.S., et al. Prevalence of total hip and knee replacement in the United States. J Bone Joint Surg Am. 2015;97:1386–1397. doi: 10.2106/JBJS.N.01141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singh J.A., Yu S., Chen L., Cleveland J.D. Rates of total joint replacement in the United States: future projections to 2020–2040 using the national inpatient sample. The J Rheumatol. 2019;46:1134–1140. doi: 10.3899/jrheum.170990. [DOI] [PubMed] [Google Scholar]
- 5.Kurtz S., Ong K., Lau E., Mowat F., Halpern M. Projections of primary and revision hip and knee arthroplasty in the United States from 2005 to 2030. J Bone Joint Surg Am. 2007;89:780–785. doi: 10.2106/JBJS.F.00222. [DOI] [PubMed] [Google Scholar]
- 6.Johnson C.A., White C.C., Kunkle B.F., Eichinger J.K., Friedman R.J. Effects of the obesity epidemic on total hip and knee arthroplasty demographics. J Arthroplasty. 2021;36:3097–3100. doi: 10.1016/j.arth.2021.04.017. [DOI] [PubMed] [Google Scholar]
- 7.Changulani M., Kalairajah Y., Peel T., Field R.E. The relationship between obesity and the age at which hip and knee replacement is undertaken. J Bone Joint Surg Br. 2008;90:360–363. doi: 10.1302/0301-620X.90B3.19782. [DOI] [PubMed] [Google Scholar]
- 8.Sherman W.F., Patel A.H., Kale N.N., Freiberger C.M., Barnes C.L., Lee O.C. Surgeon decision-making for individuals with obesity when indicating total joint arthroplasty. J Arthroplasty. 2021;36:2708–2715.e1. doi: 10.1016/j.arth.2021.02.078. [DOI] [PubMed] [Google Scholar]
- 9.Abdel M.P., Berry D.J. Current practice trends in primary hip and knee arthroplasties among members of the American Association of hip and knee surgeons: a long-term update. J Arthroplasty. 2019;34:S24–S27. doi: 10.1016/j.arth.2019.02.006. [DOI] [PubMed] [Google Scholar]
- 10.Samson S.L., Garber A.J. Metabolic syndrome. Endocrinol Metab Clin North Am. 2014;43:1–23. doi: 10.1016/j.ecl.2013.09.009. [DOI] [PubMed] [Google Scholar]
- 11.Bhupathiraju S.N., Hu F.B. Epidemiology of obesity and diabetes and their cardiovascular complications. Circ Res. 2016;118:1723–1735. doi: 10.1161/CIRCRESAHA.115.306825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Halawi M.J., Gronbeck C., Metersky M.L., et al. Time trends in patient characteristics and in-hospital adverse events for primary total knee arthroplasty in the United States: 2010-2017. Arthroplast Today. 2021;11:157–162. doi: 10.1016/j.artd.2021.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wolf B.R., Lu X., Li Y., Callaghan J.J., Cram P. Adverse outcomes in hip arthroplasty: long-term trends. J Bone Joint Surg Am. 2012;94:e103. doi: 10.2106/JBJS.K.00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cram P., Lu X., Kaboli P.J., et al. Clinical characteristics and outcomes of Medicare patients undergoing total hip arthroplasty, 1991-2008. JAMA. 2011;305:1560–1567. doi: 10.1001/jama.2011.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Odum S.M., Springer B.D., Dennos A.C., Fehring T.K. National obesity trends in total knee arthroplasty. J Arthroplasty. 2013;28:148–151. doi: 10.1016/j.arth.2013.02.036. [DOI] [PubMed] [Google Scholar]
- 16.Huang C.-S., Cheu Y.-D., Ying J., Wei M.-H. Association between provider volume and comorbidity on hospital utilization and outcomes of total hip arthroplasty among National Health Insurance enrollees. J Formos Med Assoc. 2011;110:401–409. doi: 10.1016/S0929-6646(11)60059-4. [DOI] [PubMed] [Google Scholar]
- 17.American College of Surgeons . ACS NSQIP: user guide for the 2020 ACS NSQIP procedure targeted participant use data file (PUF) American College of Surgeons; Chicago, IL: 2020. [Google Scholar]
- 18.Garcia G.H., Fu M.C., Webb M.L., Dines D.M., Craig E.V., Gulotta L.V. Effect of metabolic syndrome and obesity on complications after shoulder arthroplasty. Orthopedics. 2016;39:309–316. doi: 10.3928/01477447-20160517-03. [DOI] [PubMed] [Google Scholar]
- 19.Bhayani N.H., Hyder O., Frederick W., et al. Effect of metabolic syndrome on perioperative outcomes after liver surgery: a National Surgical Quality Improvement Program (NSQIP) analysis. Surgery. 2012;152:218–226. doi: 10.1016/j.surg.2012.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Clavien P.A., Barkun J., de Oliveira M.L., et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250:187–196. doi: 10.1097/SLA.0b013e3181b13ca2. [DOI] [PubMed] [Google Scholar]
- 21.Gonzalez Della Valle A., Chiu Y.L., Ma Y., Mazumdar M., Memtsoudis S.G. The metabolic syndrome in patients undergoing knee and hip arthroplasty: trends and in-hospital outcomes in the United States. J Arthroplasty. 2012;27:1743–1749.e1. doi: 10.1016/j.arth.2012.04.011. [DOI] [PubMed] [Google Scholar]
- 22.Guofeng C., Chen Y., Rong W., Ruiyu L., Kunzheng W. Patients with metabolic syndrome have a greater rate of complications after arthroplasty. Bone Joint Res. 2020;9:120–129. doi: 10.1302/2046-3758.93.BJR-2019-0138.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cichos K.H., Churchill J.L., Phillips S.G., et al. Metabolic syndrome and hip fracture: epidemiology and perioperative outcomes. Injury. 2018;49:2036–2041. doi: 10.1016/j.injury.2018.09.012. [DOI] [PubMed] [Google Scholar]
- 24.Modig K., Erdefelt A., Mellner C., Cederholm T., Talbäck M., Hedström M. “Obesity paradox” holds true for patients with hip fracture: a registry-based cohort study. J Bone Joint Surg Am. 2019;101:888–895. doi: 10.2106/JBJS.18.01249. [DOI] [PubMed] [Google Scholar]
- 25.Tahir M., Ahmed N., Samejo M.Q.A., Jamali A.R. The phenomenon of “obesity paradox” in neck of femur fractures. Pak J Med Sci. 2020;36:1079–1083. doi: 10.12669/pjms.36.5.1952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hennrikus M., Hennrikus W.P., Lehman E., Skolka M., Hennrikus E. The obesity paradox and orthopedic surgery. Medicine (Baltimore) 2021;100:e26936. doi: 10.1097/MD.0000000000026936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ehne J., Tsagozis P., Lind A., Wedin R., Hedström M. The obesity paradox and mortality after pathological hip fractures: a Swedish registry study. Acta Orthop. 2022;93:185–189. doi: 10.2340/17453674.2021.1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gandhi K., Viscusi E.R., Schwenk E.S., Pulido L., Parvizi J. Quantifying cardiovascular risks in patients with metabolic syndrome undergoing total joint arthroplasty. J Arthroplasty. 2012;27:514–519. doi: 10.1016/j.arth.2011.06.027. [DOI] [PubMed] [Google Scholar]
- 29.Gage M.J., Schwarzkopf R., Abrouk M., Slover J.D. Impact of metabolic syndrome on perioperative complication rates after total joint arthroplasty surgery. J Arthroplasty. 2014;29:1842–1845. doi: 10.1016/j.arth.2014.04.009. [DOI] [PubMed] [Google Scholar]
- 30.Edelstein A.I., Suleiman L.I., Alvarez A.P., et al. The interaction of obesity and metabolic syndrome in determining risk of complication following total joint arthroplasty. J Arthroplasty. 2016;31:192–196. doi: 10.1016/j.arth.2016.05.016. [DOI] [PubMed] [Google Scholar]
- 31.Fournier M.N., Hallock J., Mihalko W.M. Preoperative optimization of total joint arthroplasty surgical risk: obesity. J Arthroplasty. 2016;31:1620–1624. doi: 10.1016/j.arth.2016.02.085. [DOI] [PubMed] [Google Scholar]
- 32.Martin J.R., Jennings J.M., Dennis D.A. Morbid obesity and total knee arthroplasty: a growing problem. J Am Acad Orthop Surg. 2017;25:188–194. doi: 10.5435/JAAOS-D-15-00684. [DOI] [PubMed] [Google Scholar]
- 33.Seward M.W., Chen A.F. Obesity, preoperative weight loss, and telemedicine before total joint arthroplasty: a review. Arthroplasty. 2022;4:2. doi: 10.1186/s42836-021-00102-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Giori N.J., Amanatullah D.F., Gupta S., Bowe T., Harris A.H.S. Risk reduction compared with access to care: Quantifying the trade-off of enforcing a body mass index eligibility criterion for joint replacement. J Bone Joint Surg Am. 2018;100:539–545. doi: 10.2106/JBJS.17.00120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cleveland Clinic OME Arthroplasty Group. Arnold N., Anis H., Barsoum W.K., Bloomfield M.R., Brooks P.J., Higuera C.A., et al. Preoperative cut-off values for body mass index deny patients clinically significant improvements in patient-reported outcomes after total hip arthroplasty. Bone Joint J. 2020;102-B:683–692. doi: 10.1302/0301-620X.102B6.BJJ-2019-1644.R1. [DOI] [PubMed] [Google Scholar]
- 36.Roth A., Anis H.K., Emara A.K., et al. The potential effects of imposing a body mass index threshold on patient-reported outcomes after total knee arthroplasty. J Arthroplasty. 2021;36:S198–S208. doi: 10.1016/j.arth.2020.08.060. [DOI] [PubMed] [Google Scholar]
- 37.Foreman C.W., Callaghan J.J., Brown T.S., Elkins J.M., Otero J.E. Total joint arthroplasty in the morbidly obese: how body mass index ≥40 influences patient retention, treatment decisions, and treatment outcomes. J Arthroplasty. 2020;35:39–44. doi: 10.1016/j.arth.2019.08.019. [DOI] [PubMed] [Google Scholar]
- 38.Adhikary S.D., Liu W.-M., Memtsoudis S.G., Davis C.M., Liu J. Body mass index more than 45 kg/m(2) as a cutoff point is associated with dramatically increased postoperative complications in total knee arthroplasty and total hip arthroplasty. J Arthroplasty. 2016;31:749–753. doi: 10.1016/j.arth.2015.10.042. [DOI] [PubMed] [Google Scholar]
- 39.Nowak L.L., Campbell D.H., McKee M.D., Schemitsch E.H. Decreasing trend in complications for patients with obesity and metabolic syndrome undergoing total knee arthroplasty from 2006 to 2017. J Arthroplasty. 2022;37:S159–S164. doi: 10.1016/j.arth.2022.02.036. [DOI] [PubMed] [Google Scholar]
- 40.DeMik D.E., Muffly S.A., Carender C.N., Glass N.A., Brown T.S., Bedard N.A. What is the impact of body mass index cutoffs on total knee arthroplasty complications? J Arthroplasty. 2022;37:683–687.e1. doi: 10.1016/j.arth.2021.12.024. [DOI] [PubMed] [Google Scholar]
- 41.Kerbel Y.E., Johnson M.A., Barchick S.R., et al. Preoperative risk stratification minimizes 90-day complications in morbidly obese patients undergoing primary total knee arthroplasty. Bone Joint J. 2021;103-B:45–50. doi: 10.1302/0301-620X.103B6.BJJ-2020-2409.R1. [DOI] [PubMed] [Google Scholar]
- 42.Sayed-Noor A.S., Mukka S., Mohaddes M., Kärrholm J., Rolfson O. Body mass index is associated with risk of reoperation and revision after primary total hip arthroplasty: a study of the Swedish Hip Arthroplasty Register including 83,146 patients. Acta Orthop. 2019;90:220–225. doi: 10.1080/17453674.2019.1594015. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.