Abstract
This case report presents a 70-year-old-male, brought in by ambulance for assessment of chest pain and presyncope, with a paced ECG showing possible non-capture following ventricular pacing spikes. This was demonstrated to be pseudo non-capture with a 12-lead electrocardiogram performed in emergency and a device interrogation demonstrating ventricular capture.
1. Case presentation
A 70-year-old male was brought to the emergency department via ambulance for further assessment of chest pain and presyncope. He had a history of ischaemic cardiomyopathy and a biventricular implantable defibrillator (BiV ICD) in situ in the setting of an underlying left bundle branch block pattern electrocardiogram (ECG).
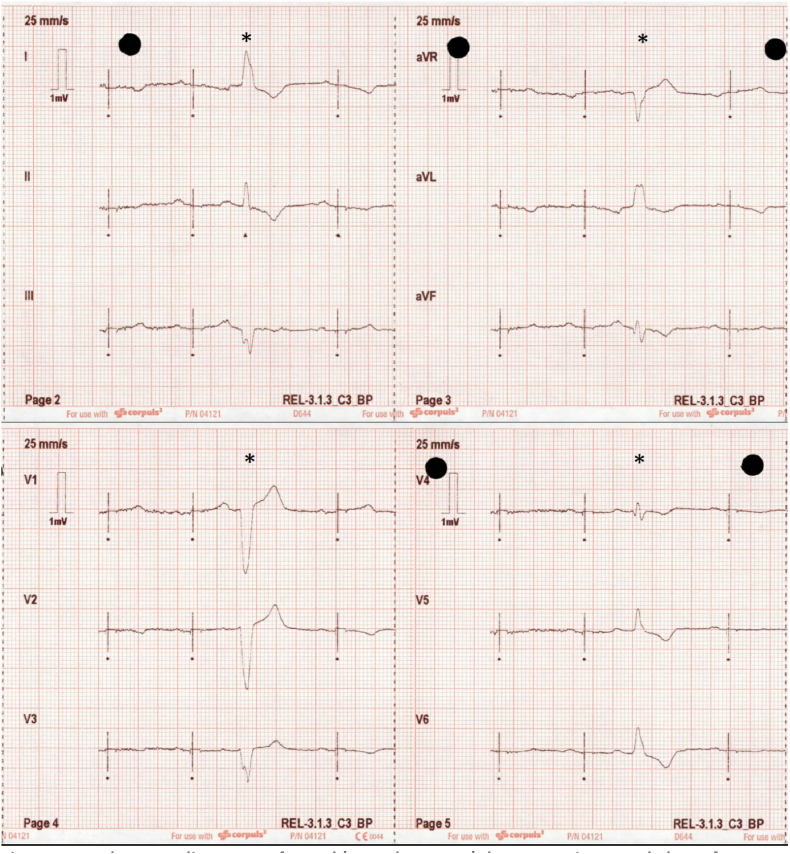
The patient's initial ECG completed enroute to hospital demonstrated sinus rhythm with atrioventricular synchronous ventricular pacing artifacts but no evoked QRS complex (Fig. 1). This initial ECG was thought to be suggestive of loss of capture. The patient's palpated pulse rate was 75 beats per minute and his conscious state was preserved.
Fig. 1.
An electrocardiogram performed (Corpuls3 D-ECG) demonstrating pseudo loss of capture following ventricular pacing spikes of a biventricular implantable defibrillator (BiV ICD). Note the premature atrial contractions with intrinsic left bundle branch block pattern (∗) do not have preceding pacing spikes and therefore are not blanked.
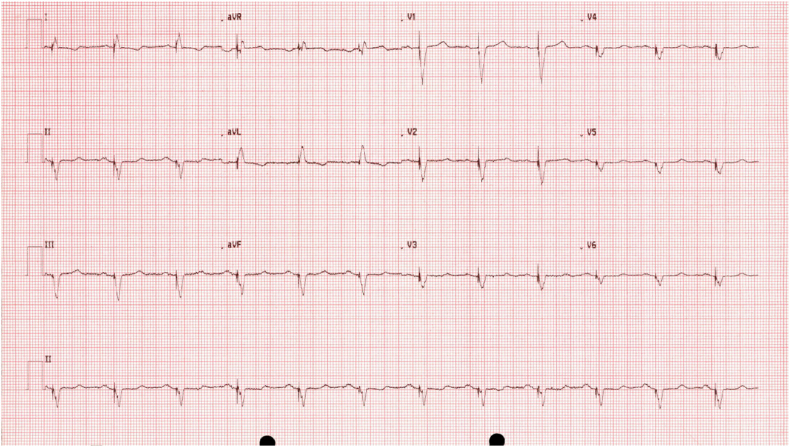
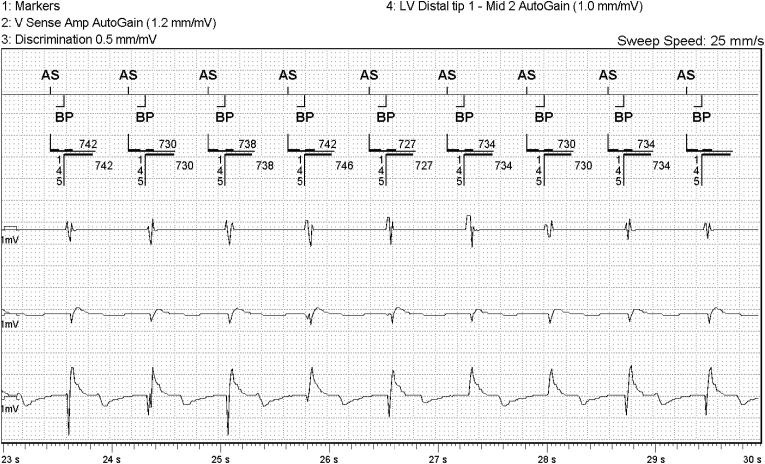
Upon arrival to the emergency department a standard 12-lead ECG was repeated (Fig. 2) and the BiV ICD was interrogated. The repeat ECG demonstrated sinus rhythm with atrioventricular synchronous biventricular pacing. Assessment of the BiV ICD function via standard technical and clinical assessment, including review of the intracardiac electrograms (Fig. 3) and provocative manoeuvres, confirmed that the device was fully functional, and the underlying rhythm was sinus rhythm with biventricular pacing. This correlates with the palpated pulse rate of 75 beats per minute and preserved conscious state.
Fig. 2.
A standard 12-lead electrocardiogram performed (Welch Allyn Mortara ELI 280) demonstrating ventricular capture following ventricular pacing spikes of a biventricular implantable defibrillator (BiV ICD).
Fig. 3.
Intracardiac EGMs of biventricular implantable defibrillator (BiV ICD; Abbott 3371-40Qc Quadra Assura MP) demonstrating AV synchronous pacing, with evidence of myocardial capture on ventricular channels (2–4).
In response to the conflicting ECGs of similar rhythms: ECG recording devices, settings and operation manuals were reviewed and the manufacturers contacted. The first ECG recording device (Corpuls, Kaufering, Germany) was found to be unable to differentiate between intracardiac pacing and transcutaneous pacing. Therefore, after a pacing artifact was detected, a 100 ms blanking period was triggered. Closer inspection of the initial ECG (Fig. 1) demonstrates a non-physiological 100 ms isoelectric segment obscuring the biventricular paced QRS that is apparent in the next ECG (Fig. 2) performed with an alternative machine (Welch Allyn Mortara ELI 280).
Recent advances in pacemaker technologies have resulted in briefer and lower voltage electrical impulses, resulting in pacing stimulus artifact becoming more difficult for automated algorithms to identify and increasing reports of inappropriate pacing stimulus responses [1]. The ability of an ECG recording device to appropriately detect pacing spikes, either internal or external, is vital for heart rate detection; otherwise, impulses may be detected as QRS complexes, leading to inappropriately detected high heart rates and inhibition of demand pacing [2]. Although there is limited literature on the phenomenon of pseudo loss of capture via blanking, in this scenario it is likely occurring to ensure that the ECG recording device does not detect both the pacing stimulus and paced QRS complexes, as this would lead to inhibition of pacing when transcutaneous pacing is occurring.
2. Commentary
This case illustrates an example of pseudo non capture due to inadvertent blanking of a QRS complex due to an embedded default feature in an ambulance ECG recording device. Misdiagnosis of non-capture and bradyarrhythmia in this setting can potentially lead to unnecessary pharmacological treatment or external pacing. In this case, the patient's preserved conscious state and palpable pulse prevented the administration of any unnecessary treatment until normal device function was confirmed via device interrogation and repeat ECG.
Footnotes
Peer review under responsibility of Indian Heart Rhythm Society.
References
- 1.Smulyan H. The computerized ECG: friend and foe. Am J Med. 2019 Feb 1;132(2):153–160. doi: 10.1016/j.amjmed.2018.08.025. [DOI] [PubMed] [Google Scholar]
- 2.Lall C., Zhang Z., Chen Y. Performance challenges in ECG pacemaker pulse detection systems. Comput Cardiol. 2012 Sep 9:765–768. https://cinc.org/archives/2012/pdf/0765.pdf Available from: [Google Scholar]