Abstract
This study provides an overview of research findings on long-term effects on healthcare workers mental health and factors associated with positive or negative changes. Medline and PubMed databases were searched for observational longitudinal studies and 18 papers were included in the review (PROSPERO: CRD42021260307). 12 articles indicated negative changes over time and six studies revealed a positive trend in a variety of mental health outcomes (anxiety, depression, insomnia, and others). Female sex, younger age, nursing occupation, frontline work, longer working hours and concerns about contracting COVID-19 were identified to be associated with negative changes. Conversely, a supportive environment, access to psychological resources, provision of sufficient personal protective equipment and availability of COVID-19 tests were linked to positive changes. Therefore, our findings can assist governmental and institutional authorities with effective interventions to improve psychological care for healthcare workers.
Keywords: medical staff, COVID-19, SARS-CoV-2, mental health, systematic review
Introduction
In December, 2019 the world was first informed of pneumonia cases in Wuhan, China, which were of unknown etiology (Ali et al., 2020). Soon after, the World Health Organization (WHO) classified the viral disease as COVID-19 and subsequently declared the outbreak of global pandemic on March 11, 2020 (Ali et al., 2020; Pappa et al., 2021).
This unprecedented situation challenged the healthcare resources in many countries. While hospitals and other healthcare services were unable to cope with the rapid growth of patients (Lima et al., 2020), healthcare professionals experienced immeasurable pressure, which included an acute shortage of personal protection equipment (PPE), insurmountable workloads, frequent sleep deprivation, insufficient support, continuous fear of infection and transmission of the virus, prolonged social isolation, insufficient information on the novel virus, inadequate media coverage and tenuous treatment protocols (Cai, Cui, et al., 2020; Lai et al., 2020; Lázaro-Pérez et al., 2020). In addition to these challenges, healthcare workers (HCWs) encountered an unprecedented number of deaths (Lázaro-Pérez et al., 2020).
All of these factors may have contributed to the HCWs’ experience of various mental health issues, especially in frontline workers who were at higher risk for psychological distress and other mental health problems (Elkholy et al., 2020; Lai et al., 2020). For example, studies conducted in various countries showed that frontline workers, especially women and nurses, experienced higher rates of anxiety, insomnia, depression, stress, burnout and exhaustion (Aebischer et al., 2020; Q. Cai, Cui, et al., 2020; Elkholy et al., 2020; Haravuori et al., 2020; Lai et al., 2020; Lázaro-Pérez et al., 2020). Another study which investigated suicidal ideation and harmful behaviors in these hospital workers determined the prevalence of both to be high, with a reported six suicide attempts in a 30-day timespan (Mortier et al., 2021). Moreover, the global pandemic revealed the lack of mental health services during emergencies (Lima et al., 2020).
Furthermore, studies conducted during past outbreaks confirm the tendency for HCWs to experience psychological issues. For instance, a study by Chua et al. (2004) showed that 89% of HCWs reported tiredness, health concerns, and social contact fears during the SARS epidemic. Furthermore, some studies indicate that acute mental health issues experienced by healthcare professionals may have long-term psychological effects (Maunder et al., 2006). For example, Lee et al., (2007) determined that significantly higher stress levels as well as increased rates of depression, anxiety and posttraumatic symptoms persisted among HCWs even 1 year after the SARS outbreak when compared with non-health care work.
A number of systematic reviews have already explored the mental health of HCWs in the context of COVID-19 and many of these include cross-sectional studies on the prevalence of mental health issues (Allan et al., 2020; Muller et al., 2020; Pappa et al., 2021; Vizheh et al., 2020). However, only one of these studies includes early longitudinal studies (Muller et al., 2020). An updated systematic review is warranted due to the sufficient amount of published studies on the long-term impact of the COVID-19 pandemic on mental health.
The COVID-19 pandemic affected healthcare systems and HCWs in various ways. Because it was not the first pandemic and most probably not the last one, there is a need to synthesize existing knowledge and evidence so that administrators could better prepare needed resources for future events. A better understanding of the long-term effects of pandemics on HCWs’ mental health and of the contributing risk factors will aid in the development of effective psychological and emotional care provisions for healthcare workers. Therefore, with this study we aim to synthesize the available evidence of long-term mental health effects, changes in mental health over time, and factors which contributed to these changes in medical care providers during the COVID-19 pandemic.
Methods
The systematic review was performed in accordance with PRISMA statement guidelines. The study protocol has been registered in PROSPERO-CRD42021260307 and is available online.
Search Strategy
Medline Complete and PubMed databases were searched to identify relevant publications. A comprehensive search strategy was applied to find relevant literature from these databases using the following medical subject headings (MeSH) and keywords: “Health Personnel”[Mesh] OR “Medical Staff”[Mesh] OR “healthcare workers” OR “healthcare professionals” OR “frontline workers” OR “medical staff” AND “COVID-19”[Mesh] OR “Pandemics”[Mesh] OR “SARS-CoV-2”[Mesh] OR “Coronavirus”[Mesh] OR coronavirus OR COVID-19 OR SARS-COV-2 OR pandemic AND “Mental Health”[Mesh] OR “Depression”[Mesh] OR “Anxiety”[Mesh] OR “mental health” OR depression OR anxiety OR insomnia. All database-specific technical variations were considered during the search. The results were limited to articles in the English language and time-framed from January 2020 up to November 8th, 2021. In addition, the reference lists of the selected articles were manually searched to identify further potentially eligible studies.
Selection Criteria
The selection process was carried out by two independent researchers. After search results from two databases were checked for duplicates, the repeating findings were removed. The title and abstract of the processed results were screened. In the following stage, full-text articles of potentially suitable articles were obtained and assessed for eligibility according to the following criteria: (1) studies on healthcare professionals (including doctors, nursing staff, and other hospital staff) engaged in providing care to patients with COVID-19 infection; (2) reports on any type of mental health-related outcome; (3) longitudinal observational studies. Inclusion and exclusion criteria were agreed on by all authors of the current study. Publications which did not meet the eligibility criteria were excluded. Discrepancies arising during abstract and full text review were discussed and agreement was reached by a third researcher adjudication. To minimize selection bias, reviewers could not see the author, journal, or publication date during the title and abstract review phases.
Data Extraction
The information from the included articles was gathered by two researchers using a previously designed data collection form. The following data were extracted from each study: the first author, country, size, characteristics of involved HCWs, follow-up period, type of mental health issues, and measurement tools. An independent reviewer examined all the collected data in the data collection form. In case of disagreements, the agreement was reached either by consensus or by the involvement of the same independent reviewer.
Quality Assessment
The quality of the eligible longitudinal studies was assessed with a Joanna Briggs Institute (JBI) tool (Santos et al., 2018). Two reviewers independently assessed the methodological quality of the studies based on the JBI Cohort checklist. This checklist consists of 11 questions which assess study design, exposure conditions, validity and reliability of outcomes, confounding factors, strategies to deal with confounders and follow-up losses, statistical analysis appropriateness, and others. Any disagreement between the reviewers was resolved through discussion.
Data Synthesis
A narrative synthesis approach was used to summarize findings from the included studies. We described changes in mental health outcomes and determined factors that were associated with these changes based on the information presented in the studies. We decided not to perform a quantitative summary of the associations between the various covariates and mental health factors, due to the high variation in reported mental health outcomes (e.g., anxiety, depression, insomnia, stress, and burnout) and the inconsistency of assessment measures.
Results
Search Results
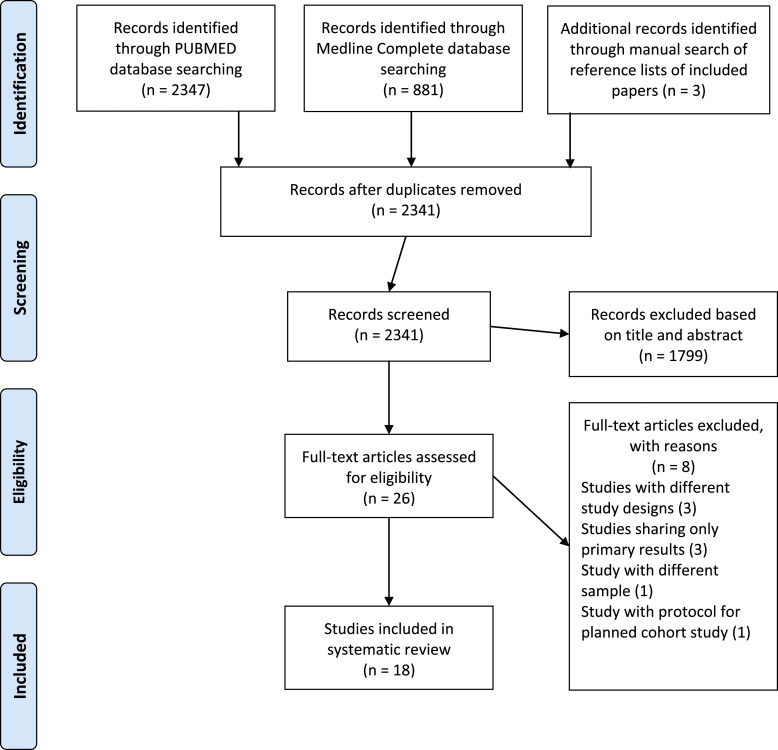
The literature search identified 3228 publications from two databases. After eliminating duplicate studies, screening titles and abstracts, and reviewing the references of the included studies, 26 articles were selected and assessed in full text. Out of the 26 articles, eight were found not to be eligible due to the following reasons: three articles were not from longitudinal studies; three articles contained only baseline results; one article focused on the general population; and one article presented protocol for a potential cohort study project. As a result, 18 papers were included in this systematic review. Figure 1 illustrates the selection process.
Figure 1.
Prisma flow diagram.
Description of Studies
The total sample size of included studies ranged from 96 to 1570. Female HCWs composed the majority of study subjects. All studies focused primarily on healthcare staff including doctors and nurses, except two studies which assessed the mental health of non-healthcare workers as well. The 18 studies were undertaken in eight countries - six in China, four in the USA, two in Argentina, two in Singapore, one in Japan, one in Mexico, one in the Netherlands, and one in Portugal. The majority of studies included two or three follow-up surveys. The interval between follow-up measurements varied from 1 week to 1 year. Table 1 provides detailed characteristics of the included studies.
Table 1.
Characteristics of included studies.
| № | Author and Country | Population Characteristics | Gender | Age | Follow-up Assessments and Sample Size | Mental Health Outcomes | Measurement Tools |
|---|---|---|---|---|---|---|---|
| No (%) | mean ± SD/median (IQR) or No (%) | ||||||
| 1 | Abdalla et al. USA | Healthcare workers | Female-183 (79.6%) | 36(31–48) | 1st assessment - 230 | Insomnia | ISI |
| Male-46 (20.0%) | 2nd - 155 | ||||||
| 3rd - 130 | |||||||
| 4th - 118 | |||||||
| 5th - 95 | |||||||
| 6th - 89 | |||||||
| 2 | Baumann et al. USA | Physicians | Female-129 (49.8%) | 35 (30–44) | 1st assessment - 426 2nd - 262 | Anxiety behavioral changes | PC-PTSD-5 |
| Male-130 (50.2%) | Burout concerns | ||||||
| PTSD stress mitigators | |||||||
| Stressors | |||||||
| 3 | Cai et al. China | Nurses | Female-605 (97.4%) | 85% less than 40 | 1st assessment - 7092nd - 621 | Anxiety | GAD-7 PHQ-9 |
| Male-16 (2.6%) | Depression | ISI | |||||
| Insomnia status | IES-R | ||||||
| PTSD | |||||||
| 4 | Chew et al. Singapore | Residents in training | Female-110 (49.8%) | 30.8±2.87 | 1st assessment - 274 2nd - 221 | Perceived stress traumatic stress stigma | PSS IES-R HWSS COPE |
| Male-111 (50.2%) | Coping strategy | ||||||
| 5 | Elliott et al. USA | Healthcare workers | Female-471 (70.7%) | 51.49±12.62 | 1st assessment - 1419 | Personality prototypes | TIPI |
| Male-195 (29.3%) | 2nd - 666 | Coping | B-COPE | ||||
| Self-reported resilience | CDRISC | ||||||
| Depression | PHQ-9 | ||||||
| Anxiety | GAD-7 | ||||||
| 6 | Hines et al. USA | Physicians and professional staff members | Female-49 (51.0%) | 40.6±10.4 | 1st assessment - 219; 2nd - NG 3rd - 96 | Moral injury distress resilience factors | IES-R |
| Male-47 (49.0%) | MIES | ||||||
| 7 | Kok et al. Netherlands | ICU professionals (physicians, nurses) | Female-168 (72.1%) | 41.8±10.7 | 1st assessment - 252 | Burnout | MBI |
| Male-65 (27.9%) | 2nd - 233 | Moral distress | MDS | ||||
| 8 | Li et al. China | Physicians | Female-247(64%) | 25 (23–28) | 1st assessment - 385 2nd - 385 | Anxiety depression workplace violence mood valence | GAD-7 PHQ-9 workplace violence mood valence |
| 9 | Liu et al. China | Healthcare workers | Female-1260 Male-310 | 35.68±8.54 | 1st assessment - 50182nd - 1570 | Psychological symptoms | SCL-90 |
| 10 | López Steinmetz et al. Argentina | Healthcare workers | Female-242 (79.34%) | 41.26±9.37 | 1st assessment - 339 | General discomfort | GHQ-12 |
| Male-63 (20.66%) | 2nd - 305 | Psychological distress | K-10 | ||||
| Mental disorder history | |||||||
| Self-perceived job performance | |||||||
| 11 | López Steinmetz et al. Argentina | Healthcare workers | Female-242 (79.34%) | Younger 40–150 (49.18%) | 1st assessment - 339 | Anxiety | STAI |
| Male-63 (20.66%) | Older 40–155 (50.82%) | 2nd - 305 | |||||
| 12 | Miguel-Puga et al. Mexico | Healthcare workers | Female-112 Male-92 | 19–58 | 1st assessment - 2042nd - 2043rd - 204 | Pre-existing anxiety | HADS DES resilience scale PSQI DD SASQ |
| Depression Dissociative symptoms | STAIsv burnout measure PTSD | ||||||
| Resilience PTSD | |||||||
| Quality of sleep | |||||||
| Depersonalization/Derealization symptoms | |||||||
| Acute stress | |||||||
| Anxiety | |||||||
| Burnout | |||||||
| 13 | Sampaio et al. Portugal | Nurses | Female-675 (81.4%) | 39±9.4 | 1st assessment - 8292nd - 3643rd - 296 | Depression | DASS-21 |
| Male −154 (18.6%) | Anxiety stress | ||||||
| Sleep quality | |||||||
| 14 | Sasaki et al. Japan | Healthcare and non-healthcare workers | Female-72 (64.9%) | 41.31±10.6 | 1st assessment - 1112nd - 108 | Psychological distress | Brief job stress Questionnaire |
| Male-39 (35.1%) | 3rd - 95 | ||||||
| 4th - 83 | |||||||
| 15 | Th’ng et al. Singapore | Healthcare workers | Female-173 (71.8%) | Categorical variable | 1st assessment - 327 | Depression | DASS-21 |
| Male-68 (28.2%) | 2nd - 279 | Anxiety | |||||
| 16 | Yuan et al. China | 939 individuals from endemic and non-endemic provinces: 249 of them are medical staff | Female-582 (61.98%) | Categorical variable | 1st assessment - 9392nd - 939 | Emotional state Somatic responses behavior sleep quality | SRQ PSQI |
| Male-357 (38.02%) | |||||||
| 17 | Zhao et al. China | Healthcare workers | Female doctors-69±59.5 | Doctors 37.39±0.724 nurses 34.44±0.669 | 1st assessment - 215 | Sleep quality | PSQI |
| Female nurses-95±96 | 2nd - 215 | Psychological distress | |||||
| Concerns | |||||||
| 18 | Zhou et alChina | Healthcare workers | 1st assessment - 494 | Psychiatric status | SCL-90 | ||
| 2nd - 462 | Fatigue | NRS | |||||
| Sleep quality | PSQI |
B-COPE, Brief COPE; CDRISC, Connor-Davidson Resilience Scale; COPE, Brief Coping Orientation to Problems Experienced; DASS-21, Depression Anxiety Stress Scales – short version; DD, Depersonalization/derealization inventory; DES, Dissociative Experiences Scale; GAD-7, Generalized Anxiety Disorder; GHQ-12, General Health Questionnaire; HADS, Hospital Anxiety and Depression Scale; HWSS, Healthcare Workers Stigma Scale; IES-R, Impact of Events Scale-Revised; ISI, Insomnia Severity Index; K-10, Kessler Psychological Distress Scale; MBI, Maslach Burnout Inventory; MDS, Moral Distress Scale; MIES, Moral Injury Events Scale; NRS, Numeric rating scale; PC-PTSD-5, Posttraumatic stress disorder screen; PHQ-9, Patient Healthy Questionnaire; PSQI, Pittsburg Sleep Quality Index; PSS, Perceived Stress Scale; PTSD, Posttraumatic Stress Disorder Symptom Severity Scale-Revised; SASQ, Stanford Acute Stress Questionnaire; SCL-90, Symptom Check List-90; SRQ, Stress Response Questionnaire; STAI, State-Trait Anxiety Inventory; STAIsv, short-form of the State-Trait Anxiety Inventory; TIPI, Ten-Item Personality Inventory.
The results of the quality assessment with the JBI critical appraisal tool are presented in the Appendix in the standard risk of bias format. The most common weaknesses among studies were failure to describe reasons for follow-up loss and strategies to address incomplete follow-up. Overall, all 18 studies were judged as having high methodological quality and were included for the systematic review.
Patterns of Mental Health Impact
Deterioration of Mental Health Symptoms Over Time
Among the articles included in the current systematic review, 12 studies predominantly reported mental health decline among HCWs over time. These mental health issues included psychological distress, anxiety, depression, insomnia, burnout symptoms and others. The majority of studies identified significant worsening of psychological distress during the follow-up period (Elliott et al., 2021; López Steinmetz et al., 2021a; Sasaki et al., 2020; 2021; Zhao et al., 2020). The same trend was observed in anxiety and depression among HCWs (Li et al., 2020; López Steinmetz et al., 2021a; 2021b; Th et al., 2021; Yuan et al., 2020). The deterioration of sleep quality was reported in three follow-up studies (Miguel-Puga et al., 2021; Zhao et al., 2020; Zhou et al., 2021). Yuan et al. (2020) also highlighted that the greatest sleep deprivation was seen among people in the 18–24 age group in the 2-week follow-up assessment. Unfortunately, the occupation of this age group was not specified in the study (Yuan et al., 2020). The results of a study by Zhao et al. (2020) revealed continued sleep disruption in the 1-month follow-up assessment. Additionally, Miguel-Puga et al. (2021) indicated that sleep quality was unsatisfactory during the peak of hospital admissions and was related to the development of PTSD symptoms. Other mental health problems among HCWs that worsened over time included burnout symptoms (Kok et al., 2021), self-perceived job performance (López Steinmetz et al., 2021a), daily mood scores (Li et al., 2020), workplace violence among beginning physicians (Elliott et al., 2021), mental health symptoms (Zhou et al., 2021), and anxiety over COVID-19 (Sasaki et al., 2021). One exception to the trend of deterioration during the follow up period was that HCWs were found to have stable moral injury scores (Hines et al., 2021).
Improvement in Mental Health Symptoms Over Time
Nonetheless, positive trends were observed in six studies examining the following mental health issues: anxiety, depression, and stress among HCWs (Cai et al., 2020, 2020b; Chew et al., 2020; Liu et al., 2020; Baumann et al., 2021; Hines et al., 2021; Sampaio et al., 2021). For instance, Chew et al. (2020) identified a significant positive change over time in perceived stress and perceived stigma (HCWs’ disclosure concerns and concerns about public attitudes). Similarly, a downward tendency was noticed in PTSD scores during the follow-up period (Baumann et al., 2021; Z. Cai, Cui, et al., 2020). In addition, three studies identified significant improvement of sleep quality among medical staff as time passed (Abdalla et al., 2021; Z. Cai, Cui, et al., 2020; Sampaio et al., 2021). These changes were observed mostly among nurses (Z. Cai, Cui, et al., 2020; Sampaio et al., 2021) and one study identified improvement in insomnia symptoms in HCWs in general (Abdalla et al., 2021). However, one contrary exception was found in Liu et al.’s (2020) positive study when the authors assessed the psychological status of medical personnel using the SCL-90 instrument which assesses nine mental health symptoms including anger-hostility, anxiety, depression, paranoid ideation, phobic anxiety, psychoticism, obsessive-compulsive, interpersonal sensitivity, and somatization. While the study results identified a significant reduction in almost all SCL-90 scores during the follow-up assessment, the only exception was the somatization score (Liu et al., 2020) which is inconsistent with the aforementioned studies.
Risk and Resilience Factors for Mental Health in HCWs
Some of the studies examined factors associated with positive or negative mental health trends among HCWs. Of these, four studies revealed that female HCWs tended to have higher levels of mental health problems compared to their male counterparts (Baumann et al., 2021; Z. Cai, Cui, et al., 2020; Liu et al., 2020; Miguel-Puga et al., 2021). Nursing staff were also more prone to various mental health issues compared to physicians. (Liu et al., 2020; Kok et al., 2021). Moreover, frontline work (Abdalla et al., 2021; Z. Cai, Cui, et al., 2020; Kok et al., 2021; Liu et al., 2020; Zhao et al., 2020) and increased workload (Z. Cai, Cui, et al., 2020; Kok et al., 2021; Yuan et al., 2020; Zhao et al., 2020) are significantly associated with the development of various psychological problems. HCWs with deeper concerns about potential COVID-19 infection were more likely to experience mental health symptoms (Z. Cai, Cui, et al., 2020; López Steinmetz et al., 2021b; Th et al., 2021; Zhao et al., 2020). Likewise, increased fear of infection or transmission corresponded to increased depression, anxiety and stress symptoms among HCWs (Sampaio et al., 2021). Finally, younger age correlated to less resilience (Miguel-Puga et al., 2021).
In contrast, workplace support was related to the reduction of psychological symptoms among HCWs (Hines et al., 2021; Th et al., 2021). Access to PPE and COVID-19 tests correlated to stress reduction and anxiety levels (Baumann et al., 2021). Furthermore, extensive experience and access to online psychological information were associated with significant mental health improvement over time (Z. Cai, Cui, et al., 2020; Zhao et al., 2020).
It was also found that pre-existing anxiety/depression and dissociation, acute stress and acute anxiety may have contributed to the development of PTSD in frontline workers during the peak of hospital admissions (Miguel-Puga et al., 2021). Whereas pre-existent resilience had a protective influence, persistent burnout appeared to contribute to depersonalization and acute stress (Miguel-Puga et al., 2021). In addition, avoidance coping strategy was positively associated with all three psychological responses (perceived stress, traumatic stress and stigma) across the follow-up period (Chew et al., 2020) and the negative trend of perceived stress was predicted by the use of positive thinking for responses across the two time points (Chew et al., 2020). In contrast, respondents deployed to high-risk areas also reported less perceived stress (Chew et al., 2020) while during the follow-up, specific factors such as living alone, less problem-solving skills and seeking social support positively predicted perceived stress and traumatic stress. Thus, researchers suggested that higher traumatic stress could lead to more social support seeking (Chew et al., 2020).
Discussion
This study provides an up-to-date systematic review of research into the mental health dynamics of HCWs during the COVID-19 pandemic. This current review brought together 18 longitudinal studies to explore long-term effects of providing medical care during the pandemic on HCWs’ mental health status. We identified 12 studies reporting deterioration of mental health issues and six studies showing improvement of mental health issues over time.
While there are ambiguous patterns of changes in HCWs’ mental health symptoms over the time identified in our systematic review, these could be attributed to the use of different assessment instruments, timing, sampling, and place. For instance, depression was assessed in six included studies and among these two studies revealed positive changes over time (Z. Cai, Cui, et al., 2020; Sampaio et al., 2021); two studies identified depression worsening(Li et al., 2020; Th et al., 2021); one study reported stability of the condition (Elliott et al., 2021); and one study assessed depression as a baseline and reported its contribution to the development of PTSD in frontline HCWs (Miguel-Puga et al., 2021). Regarding differences, whereas studies showing improvement in mental health included only nurses, negative changes were identified among physicians. Moreover, another study revealed significant association between non-doctoral level and depression. This remarkable variation does not allow us to draw a single conclusion. Therefore, more follow-up studies with similar measurement tools, compatible time frames and similar samples could minimize inconsistency in the findings and should improve our understanding of the long-term impacts of working with infected patients.
Our findings on the improvement of mental health issues in HCWs over time are in line with the results of longitudinal studies on previous outbreaks (Lung et al., 2009; SU et al., 2007). The significant reduction in depression, anxiety, PTSD, and sleep disturbances over time after the SARS outbreak is possibly due to psychological adaptation, increase in knowledge and experience with managing SARS patients, a decrease in perceived negative feelings, and continuous positive coping behavior (SU et al., 2007).
As mentioned previously, a systematic review conducted by Muller et al. (2020), two longitudinal studies were included and showed only positive changes in mental health of healthcare workers over time. Having reviewed additional longitudinal studies, our findings indicate not only positive, but also negative patterns.
Risk factors identified in the current study are consistent with existing research. These factors include: being a female HCW, working as a nurse or other frontline worker, being younger in age, working overtime, and experiencing fear of COVID-infection (Q. Cai, Cui, et al., 2020; Mo et al., 2020; Muller et al., 2020; Sahebi et al., 2021; Spoorthy et al., 2020). It is possible that being a nurse may raise concern primarily due to the fact that nurses work longer hours with patients in comparison with other staff, which involves more challenges and negative emotional state (Lai et al., 2020; Liu et al., 2020). Likewise, frontline HCWs find it particularly stressful to take responsibility for COVID-19 patients and to witness the high contagion, morbidity and fatality rates (Liang et al., 2020; Santabárbara et al., 2021). In addition, a global pandemic is an exigent concern; therefore, HCWs are especially vulnerable to mental health issues not only because of their duties with patients, but also due to fear of infection and transmission to vulnerable family members (Shah et al., 2020; Vizheh et al., 2020).
In addition to harmful risk factors, we revealed resilience factors that can help to fight against mental health problems among HCWs. These factors include a supportive environment, sufficient PPE, access to COVID-19 diagnostics, and access to online psychological interventions (Baumann et al., 2021; Z. Cai, Cui, et al., 2020; Hines et al., 2021; Miguel-Puga et al., 2021; Th et al., 2021; Zhao et al., 2020). Identical protective factors were revealed in previous studies (Kang et al., 2020; Kisely et al., 2020; Muller et al., 2020; Sahebi et al., 2021; Vizheh et al., 2020). For instance, Pappa et al. (2021) highlighted the importance of timely psychological support provisions, workload reductions and PPE management to decrease anxiety among HCWs.
The current study has several limitations. Firstly, we searched only two databases - Medline Complete and PubMed and therefore, some studies may have been missed. However, these two are the largest available medical databases. In addition to the main search, a thorough effort was made to cross-check the references of the included articles. Secondly, mental health issues that were investigated in the included studies varied widely and were not always comparable; so, it was impossible to conduct a meta-analysis. Considering the high heterogeneity among reporting measures, findings from our study should therefore be interpreted with some caution.
Conflicting evidence on changes in HCW’s mental health symptoms over time, which were identified in our systematic review, create a broad space for future research on long-term mental health impacts during pandemics, while the evidence also reveals various associations of risk and resilience factors with shifts in psychological well-being. Extensive follow-up prospective longitudinal research studies could create a sufficient evidence base for relevant parties to accurately determine the future demand and necessity of developing and implementing proper mental health services for HCWs and could allow for adequate support to be offered to those who need it not only during but also after a pandemic.
Meanwhile, intervention studies during previous outbreaks show that some measures can lead to positive changes in the mental health of HCWs. For instance, significant improvements in confidence in support and training, in pandemic self-efficacy, and in interpersonal problems among HCWs were observed by implementing computer-assisted resilience training (Maunder et al., 2010). Likewise, group training sessions on themes such as identifying stressors associated with pandemic influenza, dealing with fear, responding to extraordinary stress, using organizational and individual approaches to build resilience and reducing stress, demonstrate that a significantly higher proportion of HCWs (76%) felt better able to cope after attending one of these sessions (Aiello et al., 2011). Thus, these studies confirm the effectiveness of interventions to minimize the mental health impact of providing frontline care and these measures could be adapted to develop future interventions.
Conclusion
This systematic review has synthesized existing knowledge about long-term psychological influences of the pandemic on HCWs. Among the 18 longitudinal studies examining the mental health of healthcare workers during COVID-19, both positive and negative patterns across a variety of mental health outcomes were identified. The female gender, a younger age, a nursing profession, a frontline position, overwork, and concerns over COVID-19 infection were associated with a deterioration of mental health. Conversely, a supportive environment, access to psychological information, sufficiency of personal protective equipment and access to COVID-19 tests were identified as protective measures against mental health problems. Future research in this area should consider conducting a meta-analysis to provide a more accurate view on HCWs’ mental health affected by the impact of the pandemic.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: This study was supported by the Nazarbayev University Faculty-development competitive research grants program for 2021–2022 (Covid-19 project). Grant Number: 280720FD1906.
ORCID iDs
Saltanat Umbetkulova https://orcid.org/0000-0002-9250-4956
Akbota Kanderzhanova1 https://orcid.org/0000-0002-8153-9774
References
- Abdalla M., Chiuzan C., Shang Y., Ko G., Diaz F., Shaw K., et al. (2021). Factors associated with insomnia symptoms in a longitudinal study among New York city healthcare workers during the COVID-19 pandemic. International Journal of Environmental Research and Public Health, 18(17), 8970. 10.3390/ijerph18178970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aebischer O., Weilenmann S., Gachoud D., Méan M., Spiller T. R. (2020). Physical and psychological health of medical students involved in the coronavirus disease 2019 response in Switzerland. Swiss Medical Weekly, 150, w20418. 10.4414/smw.2020.20418 [DOI] [PubMed] [Google Scholar]
- Aiello A., Khayeri M. Y.-E., Raja S., Peladeau N., Romano D., Leszcz M., et al. (2011). Resilience training for hospital workers in anticipation of an influenza pandemic. The Journal of Continuing Education in the Health Professions, 31(1), 15–20. 10.1002/chp.20096 [DOI] [PubMed] [Google Scholar]
- Ali S., Maguire S., Marks E., Doyle M., Sheehy C. (2020). Psychological impact of the COVID-19 pandemic on healthcare workers at acute hospital settings in the south-east of Ireland: An observational cohort multicentre study. BMJ Open, 10(12), e042930. 10.1136/bmjopen-2020-042930 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allan S. M., Bealey R., Birch J., Cushing T., Parke S., Sergi G., et al. (2020). The prevalence of common and stress-related mental health disorders in healthcare workers based in pandemic-affected hospitals: A rapid systematic review and meta-analysis. European Journal of Psychotraumatology, 11(1), 1810903. 10.1080/20008198.2020.1810903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumann B. M., Cooper R. J., Medak A. J., Lim S., Chinnock B., Frazier R., et al. (2021). Emergency physician stressors, concerns, and behavioral changes during COVID-19: A longitudinal study. Academic Emergency Medicine: Official Journal of the Society for Academic Emergency Medicine, 28(3), 314–324. 10.1111/acem.14219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai Z., Cui Q., Liu Z., Li J., Gong X., Liu J., et al. (2020). Nurses endured high risks of psychological problems under the epidemic of COVID-19 in a longitudinal study in Wuhan China. Journal of Psychiatric Research, 131(January), 132–137. 10.1016/j.jpsychires.2020.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai Q., Feng H., Huang J., Wang M., Wang Q., Lu X., et al. (2020). The mental health of frontline and non-frontline medical workers during the coronavirus disease 2019 (COVID-19) outbreak in China: A case-control study. Journal of Affective Disorders, 275(January), 210–215. 10.1016/j.jad.2020.06.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chew Q. H., Chia F. L. A., Ng W. K., Lee W. C. I., Tan P. L. L., Wong C. S., et al. (2020). Perceived stress, stigma, traumatic stress levels and coping responses amongst residents in training across multiple specialties during covid-19 pandemic—a longitudinal study. International Journal of Environmental Research and Public Health, 17(18), 6572–6613. 10.3390/ijerph17186572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chua S. E., Cheung V., Cheung C., McAlonan G. M., Wong J. W. S., Cheung E. P. T., et al. (2004). Psychological effects of the SARS outbreak in Hong Kong on high-risk health care workers. Canadian journal of psychiatry. Revue canadienne de psychiatrie, 49(6), 391–393. 10.1177/070674370404900609 [DOI] [PubMed] [Google Scholar]
- Elkholy H., Tawfik F., Ibrahim I., Salah El-din W., Sabry M., Mohammed S., et al. (2021). Mental health of frontline healthcare workers exposed to COVID-19 in Egypt: A call for action. The International Journal of Social Psychiatry, 67(5), 522–531. 10.1177/0020764020960192 [DOI] [PubMed] [Google Scholar]
- Elliott T. R., Perrin P. B., Bell A.-S., Powers M. B., Warren A. M. (2021). Resilience, coping, and distress among healthcare service personnel during the COVID-19 pandemic. BMC Psychiatry, 21(1), 489. 10.1186/s12888-021-03506-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haravuori H., Junttila K., Haapa T., Tuisku K., Kujala A., Rosenström T., et al. (2020). Personnel well-being in the helsinki university hospital during the COVID-19 pandemic—a prospective cohort study. International Journal of Environmental Research and Public Health, 17(21), 7905–7909. 10.3390/ijerph17217905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hines S. E., Chin K. H., Glick D. R., Wickwire E. M. (2021). Trends in moral injury, distress, and resilience factors among healthcare workers at the beginning of the covid-19 pandemic. International Journal of Environmental Research and Public Health, 18(2), 488–511. 10.3390/ijerph18020488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kang L., Ma S., Chen M., Yang J., Wang Y., Li R., et al. (2020). Impact on mental health and perceptions of psychological care among medical and nursing staff in wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain, Behavior, and Immunity, 87(January), 11–17. 10.1016/j.bbi.2020.03.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kisely S., Warren N., McMahon L., Dalais C., Henry I., Siskind D. (2020). Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: Rapid review and meta-analysis. BMJ (Clinical Research Ed.), 369, m1642. 10.1136/bmj.m1642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kok N., van Gurp J., Teerenstra S., van der Hoeven H., Fuchs M., Hoedemaekers C., et al. (2021). Coronavirus disease 2019 immediately increases burnout symptoms in ICU professionals: A longitudinal cohort study. Critical Care Medicine, 49(3), 419–427. 10.1097/CCM.0000000000004865 [DOI] [PubMed] [Google Scholar]
- Lai J., Ma S., Wang Y., Cai Z., Hu J., Wei N., et al. (2020). Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open, 3(3), e204012. 10.1001/jamanetworkopen.2020.3976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lázaro-Pérez C., Martínez-López J. Á., Gómez-Galán J., López-Meneses E. (2020). Anxiety about the risk of death of their patients in health professionals in Spain: Analysis at the peak of the covid-19 pandemic. International Journal of Environmental Research and Public Health, 17(16), 5938–6016. 10.3390/ijerph17165938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- doi: 10.1177/070674370705200405. Lee, A. M., Wong, J. G. W. S., McAlonan, G. M., Cheung, V., Cheung, C., Sham, P. C., Chu, N. M., Wong, P. C., Tsang, K. W. T., & Chua, S. E. (2007). Stress and psychological distress among SARS survivors 1 year after the outbreak. Canadian Journal of Psychiatry, 52(4), 233–240. [DOI] [PubMed] [Google Scholar]
- Liang Y., Wu K., Zhou Y., Huang X., Zhou Y., Liu Z. (2020). Mental health in frontline medical workers during the 2019 novel coronavirus disease epidemic in China: A comparison with the general population. International Journal of Environmental Research and Public Health, 17(18), 6550–6612. 10.3390/ijerph17186550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W., Frank E., Zhao Z., Chen L., Wang Z., Burmeister M., et al. (2020). Mental health of young physicians in China during the novel coronavirus disease 2019 outbreak. JAMA Network Open, 3(6), e2010705. 10.1001/jamanetworkopen.2020.10705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lima C. K. T., Carvalho P. M. d. M., Lima I. d. A. A. S., Nunes J. V. A. d. O., Saraiva J. S., de Souza R. I., et al. (2020). The emotional impact of Coronavirus 2019-nCoV (new Coronavirus disease). Psychiatry Research, 287, 112915. 10.1016/j.psychres.2020.112915 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Z., Wu J., Shi X., Ma Y., Ma X., Teng Z., et al. (2020). Mental health status of healthcare workers in China for COVID-19 epidemic. Annals of Global Health, 86(1), 128. 10.5334/aogh.3005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- López Steinmetz L. C., Herrera C. R., Fong S. B., Godoy J. C. (2021. b). Changes in healthcare workers’ anxiety during two time points of the COVID-19 pandemic: Evidence from a longitudinal study. International Journal of Mental Health and Addiction, 6: 1–15. 10.1007/s11469-021-00667-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- López Steinmetz L. C., Herrera C. R., Fong S. B., Godoy J. C. (2022). A longitudinal study on the changes in mental health of healthcare workers during the COVID-19 pandemic. Psychiatry, 85(1), 56–71. 10.1080/00332747.2021.1940469 [DOI] [PubMed] [Google Scholar]
- Lung F.-W., Lu Y.-C., Chang Y.-Y., Shu B.-C. (2009). Mental symptoms in different health professionals during the SARS attack: A follow-up study. The Psychiatric Quarterly, 80(2), 107–116. 10.1007/s11126-009-9095-5 [DOI] [PubMed] [Google Scholar]
- Maunder R. G., Lancee W. J., Balderson K. E., Bennett J. P., Borgundvaag B., Evans S., et al. (2006). Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerging Infectious Diseases, 12(12), 1924–1932. 10.3201/eid1212.060584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maunder R. G., Lancee W. J., Mae R., Vincent L., Peladeau N., Beduz M. A., et al. (2010). Computer-assisted resilience training to prepare healthcare workers for pandemic influenza: A randomized trial of the optimal dose of training. BMC Health Services Research, 10(1), 72. 10.1186/1472-6963-10-72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miguel-Puga J. A., Cooper-Bribiesca D., Avelar-Garnica F. J., Sanchez-Hurtado L. A., Colin-Martínez T., Espinosa-Poblano E., et al. (2021). Burnout, depersonalization, and anxiety contribute to post-traumatic stress in frontline health workers at COVID-19 patient care, a follow-up study. Brain and Behavior, 11(3), e02007-e02009. 10.1002/brb3.2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mo Y., Deng L., Zhang L., Lang Q., Liao C., Wang N., et al. (2020). Work stress among Chinese nurses to support Wuhan in fighting against COVID-19 epidemic. Journal of Nursing Management, 28(5), 1002–1009. 10.1111/jonm.13014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mortier P., Vilagut G., Ferrer M., Serra C., Molina J. D., López‐Fresneña N., et al. (2021). Thirty‐day suicidal thoughts and behaviors among hospital workers during the first wave of the Spain COVID‐19 outbreak. Depression and Anxiety, 38(5), 528–544. 10.1002/da.23129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muller A. E., Hafstad E. V., Himmels J. P. W., Smedslund G., Flottorp S., Stensland S. Ø., et al. (2020). The mental health impact of the covid-19 pandemic on healthcare workers, and interventions to help them: A rapid systematic review. Psychiatry Research, 293(July), 113441. 10.1016/j.psychres.2020.113441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pappa S., Ntella V., Giannakas T., Giannakoulis V. G., Papoutsi E., Katsaounou P. (2021). Corrigendum to "prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis" [Brain Behav. Immun. 88 (2020) 901-907]. ImmunBrain, Behavior, and Immunity, 8892(xxxx), 247245–247907. 10.1016/j.bbi.2020.11.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahebi A., Nejati-Zarnaqi B., Moayedi S., Yousefi K., Torres M., Golitaleb M. (2021). The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: An umbrella review of meta-analyses. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 107(November 2020), 110247. 10.1016/j.pnpbp.2021.110247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sampaio F., Sequeira C., Teixeira L. (2021). Impact of COVID-19 outbreak on nurses’ mental health: A prospective cohort study. Environmental Research, 194(January), 110620. 10.1016/j.envres.2020.110620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santabárbara J., Bueno-Notivol J., Lipnicki D. M., Olaya B., Pérez-Moreno M., Gracia-García P., et al. (2021). Prevalence of anxiety in health care professionals during the COVID-19 pandemic: A rapid systematic review (on published articles in Medline) with meta-analysis. Progress in Neuro-Psychopharmacology & Biological Psychiatry, 107, 110244. 10.1016/j.pnpbp.2021.110244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santos W. M. d., Secoli S. R., Püschel V. A. d. A. (2018). The Joanna Briggs Institute approach for systematic reviews. Revista Latino-Americana de Enfermagem, 26, e3074. 10.1590/1518-8345.2885.3074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sasaki N., Asaoka H., Kuroda R., Tsuno K., Imamura K., Kawakami N. (2021). Sustained poor mental health among healthcare workers in COVID‐19 pandemic: A longitudinal analysis of the four‐wave panel survey over 8 months in Japan. Journal of Occupational Health, 63(1), e12227. 10.1002/1348-9585.12227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sasaki N., Kuroda R., Tsuno K., Kawakami N. (2020). The deterioration of mental health among healthcare workers during the COVID-19 outbreak: A population-based cohort study of workers in Japan. Scandinavian Journal of Work, Environment & Health, 46(6), 639–644. 10.5271/sjweh.3922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah K., Kamrai D., Mekala H., Mann B., Desai K., Patel R. S. (2020). Focus on mental health during the coronavirus (COVID-19) pandemic: Applying learnings from the past outbreaks. Cureus, 12(3), e7405. 10.7759/cureus.7405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spoorthy M. S., Pratapa S. K., Mahant S. (2020). Mental health problems faced by healthcare workers due to the COVID-19 pandemic–A review. Asian Journal of Psychiatry, 51(January), 102119. 10.1016/j.ajp.2020.102119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su T. P., Lien T. C., Yang C. Y., Su Y. L., Wang J. H., Tsai S. L., et al. (2007). Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: A prospective and periodic assessment study in Taiwan. Journal of Psychiatric Research, 41(1–2), 119–130. 10.1016/j.jpsychires.2005.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Th F., Rao K. A., Ge L., Mao D., Neo H. N., Molina J. A.De., et al. (2021). A one-year longitudinal study : Changes in depression and anxiety in frontline emergency department healthcare workers in the COVID-19 pandemic. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vizheh M., Qorbani M., Arzaghi S. M., Muhidin S., Javanmard Z., Esmaeili M. (2020). The mental health of healthcare workers in the COVID-19 pandemic: A systematic review. Journal of Diabetes and Metabolic Disorders, 19(2), 1967–1978. 10.1007/s40200-020-00643-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan S., Liao Z., Huang H., Jiang B., Zhang X., Wang Y., et al. (2020). Comparison of the indicators of psychological stress in the population of Hubei Province and non-endemic Provinces in China during two weeks during the coronavirus disease 2019 (COVID-19) outbreak in February 2020. Medical Science Monitor: International Medical Journal of Experimental and Clinical Research, 26, e923810. 10.12659/MSM.923767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao X., Zhang T., Li B., Yu X., Ma Z., Cao L., et al. (2020). Job-related factors associated with changes in sleep quality among healthcare workers screening for 2019 novel coronavirus infection: A longitudinal study. Sleep Medicine, 75(January), 21–26. 10.1016/j.sleep.2020.07.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou Y., Ding H., Zhang Y., Zhang B., Guo Y., Cheung T., et al. (2021). Prevalence of poor psychiatric status and sleep quality among frontline healthcare workers during and after the COVID-19 outbreak: A longitudinal study. Translational Psychiatry, 11(1), 223. 10.1038/s41398-020-01190-w [DOI] [PMC free article] [PubMed] [Google Scholar]