Key Points
Question
What are the odds of high obesity-related cancer mortality rates in US counties with low-income food desert or food swamp environments?
Findings
In this ecologic cross-sectional study that included 3038 counties or county equivalents, those with the highest food swamp score had a 77% increased odds of high obesity-related cancer mortality.
Meaning
Findings suggest that the increase in the creation and use of food swamps may be of national significance, warranting holistic methods of combating obesity and cancer through providing healthier food options.
Abstract
Importance
Obesity-related cancers account for 40% of all cancers in the US. Healthy food consumption is a modifiable factor shown to reduce obesity-related cancer mortality, but residing in areas with less access to grocery stores (food deserts) or higher access to fast food (food swamps) reduces healthy food access and has been understudied.
Objective
To analyze the association of food deserts and food swamps with obesity-related cancer mortality in the US.
Design, Setting, and Participants
This cross-sectional ecologic study used US Department of Agriculture Food Environment Atlas data from 2012, 2014, 2015, 2017, and 2020 and Centers for Disease Control and Prevention mortality data from 2010 to 2020. A total of 3038 US counties or county equivalents with complete information on food environment scores and obesity-related cancer mortality data were included. An age-adjusted, generalized, mixed-effects regression model was performed for the association of food desert and food swamp scores with obesity-related cancer mortality rates. Data were analyzed from September 9, 2022, to September 30, 2022.
Exposures
Food swamp score was calculated as the ratio of fast-food and convenience stores to grocery stores and farmers markets. Higher food swamp and food desert scores (20.0 to ≥58.0) indicated counties with fewer healthy food resources.
Main Outcomes and Measures
Obesity-related cancer (based on the International Agency for Research on Cancer evidence between obesity and 13 types of cancer) mortality rates were categorized as high (≥71.8 per 100 000 population) vs low (<71.8 per 100 000 population) per county.
Results
A total of 3038 counties or county equivalents with high obesity-related cancer mortality rates had a higher percentage of non-Hispanic Black residents (3.26% [IQR, 0.47%-26.35%] vs 1.77% [IQR, 0.43%-8.48%]), higher percentage of persons older than 65 years (15.71% [IQR, 13.73%-18.00%] vs 15.40% [IQR, 12.82%-18.09%]), higher poverty rates (19.00% [IQR, 14.20%-23.70%] vs 14.40% [IQR, 11.00%-18.50%]), higher adult obesity rates (33.00% [IQR, 32.00%-35.00%] vs 32.10% [IQR, 29.30%-33.20%]), and higher adult diabetes rates (12.50% [IQR, 11.00%-14.20%] vs 10.70% [IQR, 9.30%-12.40%]) compared with counties or county equivalents with low obesity-related cancer mortality. There was a 77% increased odds of having high obesity-related cancer mortality rates among US counties or county equivalents with high food swamp scores (adjusted odds ratio, 1.77; 95% CI, 1.43-2.19). A positive dose-response relationship among 3 levels of food desert and food swamp scores and obesity-related cancer mortality was also observed.
Conclusions and Relevance
The findings of this cross-sectional ecologic study suggest that policy makers, funding agencies, and community stakeholders should implement sustainable approaches to combating obesity and cancer and establishing access to healthier food, such as creating more walkable neighborhoods and community gardens.
This cross-sectional study investigates food deserts and food swamps in US counties and their association with obesity-related cancer mortality.
Introduction
Cancer continues to be a formidable public health concern both in the US and internationally. In 2022 alone, it was projected that more than 1.9 million people in the US would receive a diagnosis of cancer, and among current survivors, an estimated 609 000 individuals will die from it.1 Major risk factors associated with carcinogenesis are either nonmodifiable (eg, age, sex, and genetics) or modifiable through healthy lifestyle changes (eg, reduced consumption of alcohol, tobacco abstinence, exercise, and dietary patterns).2,3,4 Of these modifiable risk factors, obesity and overweight status due to lack of exercise and healthy diet have been associated with 13 types of cancer according to the International Agency for Research on Cancer (endometrial, esophageal adenocarcinoma, gastric cardia, liver, kidney, multiple myeloma, meningioma, pancreatic, colorectal, gallbladder, breast, ovarian, and thyroid), which accounts for 40% of all cancers diagnosed in the US each year.5 Pathologic mechanisms associated with obesity continue to be explored but have been largely associated with increased chronic inflammation, hormonal disruption, and changes to the microbiome of the gut.6 The elevated chronic inflammatory environment due to obesity may lead to an increased risk of cancer mortality.7,8,9
Increased heathy eating has been associated with reduced risk of obesity and cancer incidence and mortality.10,11,12,13,14,15 One key barrier to healthy lifestyle access is residing in a food desert or food swamp.16 Food deserts are geographic regions where persons live more than 1.6 km (1 mile) from a supermarket and lack healthy food options. However, food swamps are unique in that these communities are more than 1.6 m (1 mile) from supermarkets and healthy food options and have more proinflammatory food options (eg, corner stores and fast-food restaurants) compared with fresh food options or no options.17,18 Although some studies have shown a larger promotion of unhealthy food options in African American communities compared with predominantly White communities,19,20,21,22,23,24,25 other studies have found that underserved populations are more willing to consume healthy foods when given equitable access to them.26,27
Food deserts and food swamps mainly exist in the South or Southeastern region, where chronic disease rates are the highest among US adults,28,29 including clusters for breast, lung, colorectal, and prostate cancers.30,31 Only 1 US study, to our knowledge, examined the association of food deserts with breast and colorectal cancers,32 finding that patients residing in food deserts had 16% increased 5-year breast cancer mortality risk and 12% increased 5-year colorectal cancer mortality risk compared with patients not residing in food deserts.32 A different US study found that food swamps were strongly correlated with obesity compared with food deserts alone.17 Finally, another US study found that patients with esophageal cancer who resided in food deserts had a more than 6-fold increased risk of hospital readmission after esophagectomy.33 There is a paucity of research on the association of food deserts and food swamps with obesity-related cancer morbidity and mortality, which calls for additional research to comprehensively characterize this association. The purpose of this study was to examine the association of food deserts and food swamps with obesity-related cancer mortality among all US counties in the past decade.
Methods
Ethical Review of the Study
This analysis was considered exempt by Augusta University from undergoing institutional review board review and receiving informed consent, given that the data were deidentified and publicly available. All analyses were performed according to relevant regulations and the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline.
Study Design
We conducted a cross-sectional study at the ecologic level among US counties (n = 3142), using 2010 to 2020 county-level cancer mortality data from the Centers for Disease Control and Prevention (CDC)34 and 2012, 2014, 2015, 2017, and 2020 county-level food environment data from the Economic Research Service of the US Department of Agriculture.35 We elected these respective time periods to provide robust estimation of county-level food environment measures at multiple levels. The county-level CDC cancer mortality data include multiple causes of cancer death (esophagus adenocarcinoma, gastric cardia, colon and rectum, liver, gallbladder, pancreas, postmenopausal breast, corpus uteri, ovary, kidney, meningioma, thyroid, and multiple myeloma) for noninstitutionalized adults aged 18 years or older and residing in the US.34 We linked the county-level mortality data to the county-level food environment data via the Food Environment Atlas (FEA) by the available Federal Information Processing System Codes.
Study Sample
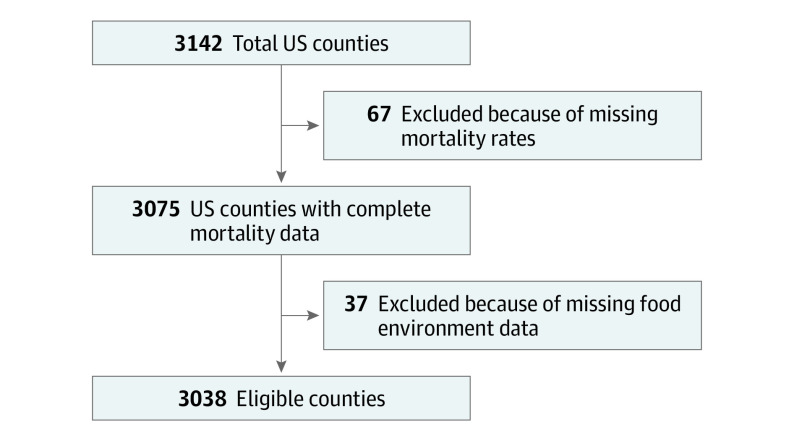
The FEA and CDC mortality data had 3142 US counties or county equivalents36 (henceforth counties), respectively. To obtain an eligible sample for our study, we excluded counties with missing data for mortality rates (n = 67) and missing food environment factors, including incomplete data on fast-food restaurants or grocery stores (n = 37). The final sample size for this analysis included 3038 US counties with complete FEA and CDC mortality data (Figure 1).
Figure 1. Flowchart of US Counties or County Equivalents Reporting Food Environment Measures.
Obesity-Related Cancer Mortality: Outcome of Interest
The outcome of interest (obesity-related cancer mortality) between 2010 and 2020 was based on International Statistical Classification of Diseases and Related Health Problems, Tenth Revision codes for underlying cause of death (eTable 1 in Supplement 1) and findings from the International Agency for Research on Cancer Handbook Working Group.5 Death certificates, which include a record for every death of a US resident, provided the underlying data for cause of death. Overweight status was defined as having a body mass index (calculated as weight in kilograms divided by height in meters squared) of 25 to 29.9, and obesity status was defined as having a body mass index of 30 or higher.37 Given that overweight status, obesity status, or both are a major risk factor for multiple cancer types, we used the age-adjusted mortality rates (per 100 000 population) from the CDC that consisted of all 13 obesity-related cancer types. Furthermore, we categorized the continuous cancer mortality rates as high (≥71.8 per 100 000 population) vs low (<71.8 per 100 000 population) according to the median of county-level mortality rates.
Food Deserts and Food Swamps: Primary Exposures of Interest
Food desert and food swamp scores (also considered food environment measures) were the key exposures of interest. County-level data (2012, 2014, 2015, 2017, and 2020) from the FEA were used to examine the association between food choices and causes of cancer death in the US. The FEA data include updated county-level food environment factors (eg, store count based on the North American Industry Classification System, store or restaurant proximity, and food and nutrition assistance programs) and demographic and clinical characteristics, such as county obesity and diabetes prevalence rates.35 Food deserts were calculated through the FEA as the proportion of each county’s total population identified as having both low income and low access to grocery stores. Low income was defined as having a household income less than or equal to 200% of the federal poverty threshold, and low access to grocery stores was defined as living more than 1.6 km (1 mile) from a supermarket or grocery store in an urban area or more than 16 km (10 miles) in a rural area.38,39 The food swamp score was calculated as the ratio of fast-food restaurants and convenience stores (eg, corner stores) to grocery stores and farmers markets. This score was modified from the traditional Retail Food Environment Index score.17 Each county had its respective scores calculated for 2012, 2014, 2015, 2017, and 2020; then the scores were aggregated over the 10-year period of the cancer mortality data to estimate continuous food swamp and food desert scores from 2010 to 2020. After the continuous measures were calculated, we categorized food desert and food swamp scores into low, moderate, and high scores based on the distribution (tertiles) of the total scores per county. Higher food swamp and food desert scores (20.0 to ≥58.0) indicate counties with fewer healthy food resources.
Covariates
Other covariates of interest reported and considered for analysis were obtained from the FEA according to their latest year of availability. The covariates included race and ethnicity (percentage of each racial group per county in 2010: non-Hispanic American Indian or Alaska Native, non-Hispanic Asian, non-Hispanic Black, non-Hispanic Hawaiian or Pacific Islander, Hispanic, and non-Hispanic White), age (percentage of the population ≥65 years in 2010), median household income in 2015, poverty rate in 2015 (per 100 000 population), adult obesity rates per county in 2017 (per 100 000 population), and adult diabetes rates per county in 2013 (per 100 000 population).
Statistical Analysis
Analysis of variance was used to assess differences in demographic and clinical characteristics among counties with high or low obesity-related cancer mortality rates. Pearson correlation coefficients were used to evaluate the association between the measured food environments and cancer mortality rates. We performed a generalized linear mixed model accounting for an unstructured covariance-variance matrix to examine the association between county-level food swamps (and deserts) and obesity-related cancer mortality to account for possible between-county correlation using a binomial distribution and logit function. The exponentiated effects from this model may be interpreted as the odds ratios and associated 95% CIs of the association between the food environment measures and obesity-related cancer mortality. Additionally, a multilevel generalized linear mixed-effects model was used to analyze the association among 3 levels of food desert scores, 3 levels of food swamp scores, and 3 levels of obesity-related cancer mortality rates (low, moderate, and high). Results from this polytomous model can be interpreted as the log odds of counties with either high or moderate obesity-related cancer mortality rates compared with the log odds of counties with low mortality rates (referent category). All models were reported as adjusted odds ratios (AORs) and associated 95% CIs, with statistical significance set at .05 and the P values based on 2-sided t tests. All analyses were conducted with SAS, version 9.4 (SAS Institute). Data were analyzed from September 9, 2022, to September 30, 2022.
Results
Of the 3142 counties in the US, a total of 3038 (96.7%) were included in this analysis, of which 758 (25.0%) had high (within the fourth [highest] quartile) obesity-related cancer mortality. These specific counties had a higher percentage of non-Hispanic Black residents (3.26% [IQR, 0.47%-26.35%] vs 1.77% [IQR, 0.43%-8.48%]), higher percentage of persons older than 65 years (15.71% [IQR, 13.73%-18.00%] vs 15.40% [IQR, 12.82%-18.09%]), higher poverty rates (19.00% [IQR, 14.20%-23.70%] vs 14.40% [IQR, 11.00%-18.50%]), higher adult obesity rates (33.00% [IQR, 32.00%-35.00%] vs 32.10% [IQR, 29.30%-33.20%]), and higher adult diabetes rates (12.50% [IQR, 11.00%-14.20%] vs 10.70% [IQR, 9.30%-12.40%]) compared with counties with low obesity-related cancer mortality (Table 1). Furthermore, these counties had higher percentages of persons residing in food deserts (7.39% [IQR, 4.09%-11.65%] vs 5.99% [IQR, 3.47%-9.50%]) and food swamps (19.86% [IQR, 13.91%-26.40%] vs 18.20% [IQR, 13.14%-24.00%]) compared with counties with low cancer mortality. The correlation analysis (Figure 2) observed that both food desert and food swamp scores were positively correlated with obesity-related cancer mortality, with the correlation being slightly higher between food deserts and obesity-related cancer mortality (food deserts, ρ = 0.12; food swamps, ρ = 0.08). Nevertheless, food desert and food swamp index scores were determined to be unique, given the low coefficients.
Table 1. Descriptive and Clinical Characteristics Among 3038 US Counties or County Equivalents.
| Study characteristics | Age-adjusted obesity-related cancer mortality rates, median (IQR) | P valuec | |
|---|---|---|---|
| Low (n = 2289)a | High (n = 758)b | ||
| Demographic characteristics | |||
| Race and ethnicity, % | |||
| Non-Hispanic American Indian or Alaska Native | 0.31 (0.20-0.63) | 0.27 (0.18-0.51) | <.001 |
| Non-Hispanic Asian | 0.52 (0.30-1.19) | 0.35 (0.23-0.57) | <.001 |
| Non-Hispanic Black | 1.77 (0.43-8.48) | 3.26 (0.47-26.35) | <.001 |
| Non-Hispanic Hawaiian or Pacific Islander | 0.03 (0.01-0.05) | 0.02 (0.01-0.03) | .03 |
| Hispanic | 3.69 (1.77-9.35) | 2.34 (1.30-5.21) | <.001 |
| Non-Hispanic White | 86.11 (70.30-94.07) | 82.85 (58.71-94.29) | <.001 |
| Population aged ≥65 y, % | 15.40 (12.82-18.09) | 15.71 (13.73-18.00) | .02 |
| Income | |||
| Household income, No. (SD), $ | 48 598 (12 692) | 41 783 (8915) | <.001 |
| Poverty rate, % | 14.40 (11.00-18.50) | 19.00 (14.20-23.70) | <.001 |
| Clinical characteristics, % | |||
| Adult obesity rate | 32.10 (29.30-33.20) | 33.00 (32.00-35.00) | <.001 |
| Adult diabetes rate | 10.70 (9.30-12.40) | 12.50 (11.00-14.20) | <.001 |
| Food environment, % | |||
| Fast-food restaurantsd | 18.20 (6.20-60.00) | 11.20 (4.40-25.00) | <.001 |
| Convenience storesd | 17.40 (8.00-42.60) | 13.30 (6.80-25.20) | <.001 |
| Grocery storesd | 6.00 (3.00-14.80) | 4.40 (2.40-8.00) | <.001 |
| Supercentersd | 1.00 (0.00-2.00) | 0.60 (0.00-1.00) | <.001 |
| Specialized food storesd | 1.60 (0.20-5.40) | 0.60 (0.00-2.00) | <.001 |
| Farmers marketd | 1.20 (0.40-3.00) | 0.80 (0.00-1.40) | <.001 |
| Food deserte | 5.99 (3.47-9.50) | 7.39 (4.09-11.65) | <.001 |
| Food swamp (comprehensive RFEI) | 18.20 (13.14-24.00) | 19.86 (13.91-26.40) | <.001 |
Abbreviation: RFEI, Retail Food Environment Index.
Low categorized as counties with obesity-related cancer mortality rates from 31.0 to 71.7 per 100 000 population.
High categorized as counties with obesity-related cancer mortality rates from 71.8 to 185.7 per 100 000 population.
Determined from 1-way analysis of variance.
Denotes the count of respective variable within each county.
Denotes the counties with percentage of residents with low income and low access to grocery stores.
Figure 2. Correlations Between Food Deserts and Obesity-Related Cancer Mortality and Between Food Swamps and Obesity-Related Cancer Mortality.
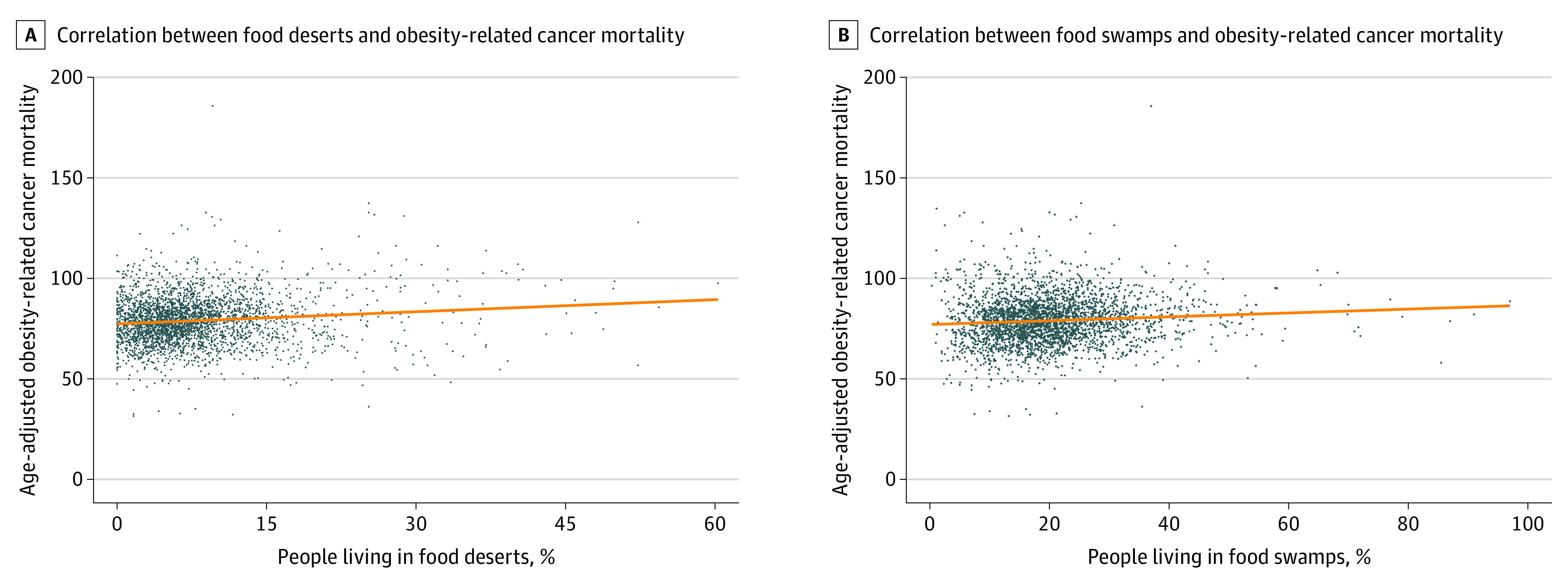
A, Correlation between total percentage of people living in food deserts and age-adjusted obesity-related cancer mortality (ρ = 0.12). B, Correlation between food swamp scores and age-adjusted obesity-related cancer mortality (ρ = 0.08).
The age-adjusted odds of counties having high obesity-related cancer mortality were elevated (77%) among counties with high food desert scores (AOR, 1.59; 95% CI, 1.29-1.94) and high food swamp scores (AOR, 1.77; 95% CI, 1.43-2.19) compared with low food environment measures (Table 2). Additionally, we observed a positive dose-response relationship (Table 3) between tertiles of the food environment measures and obesity-related cancer mortality, including greater than 2-fold increased odds of high obesity-related cancer mortality among counties with high food swamp scores (AOR, 2.10; 95% CI, 1.67-2.63) compared with counties with low food swamp scores. After adjusting for age, race, and poverty rate (eTable 2 in Supplement 1), we observed an almost 30% increased odds of high obesity-related cancer mortality among counties with high food swamp scores (AOR, 1.29; 95% CI, 1.03-1.63). However, additional adjustment by adult obesity rates showed no significance. Also, we observed nonsignificant associations in fully adjusted models between tertiles of the food environment measures and obesity-related cancer mortality (eTable 3 in Supplement 1).
Table 2. Association of Food Environment Measures With Obesity-Related Cancer Mortality Among 3038 US Counties or County Equivalents.
| Variable | Odds of high obesity-related cancer mortality | ||
|---|---|---|---|
| Counties with low obesity-related cancer mortality, No. (%) (n = 2283)a,b | Counties with high obesity-related cancer mortality, No. (%) (n = 758)a,b | AOR (95% CI) | |
| Food desert | |||
| Low | 800 (35.0) | 215 (28.4) | 1 [Reference] |
| Moderate | 781 (34.2) | 235 (31.0) | 1.12 (0.91-1.38) |
| High | 708 (31.0) | 307 (40.5) | 1.59 (1.29-1.94) |
| Food swamp (comprehensive RFEI) | |||
| Low | 794 (34.8) | 219 (28.9) | 1 [Reference] |
| Moderate | 785 (34.4) | 229 (30.2) | 1.15 (0.93-1.43) |
| High | 708 (31.0) | 306 (40.4) | 1.77 (1.43-2.19) |
Abbreviations: AOR, adjusted odds ratio; RFEI, Retail Food Environment Index.
Adjusted for the percentage of county population aged 65 years or older. Results from the adjusted generalized mixed-effects models can be interpreted as the odds of counties with high obesity-related cancer mortality rates compared with that of those with low mortality rates (referent category).
Group percentage presented as the proportion of counties within variable strata with food environment category.
Table 3. Multivariable Polytomous Association of Food Environment Measures With Obesity-Related Cancer Mortality Among 3038 US Counties or County Equivalentsa.
| Variable | Low, %b,c | Moderated | Highe | ||
|---|---|---|---|---|---|
| %c | AOR (95% CI) | %c | AOR (95% CI) | ||
| Food desert | |||||
| Low | 38.4 | 32.7 | 1 [Reference] | 28.9 | 1 [Reference] |
| Moderate | 29.7 | 38.4 | 1.52 (1.23-1.87) | 31.9 | 1.43 (1.15-1.78) |
| High | 31.8 | 29.4 | 1.06 (0.86-1.32) | 38.8 | 1.59 (1.28-1.96) |
| Food swamp (comprehensive RFEI) | |||||
| Low | 38.1 | 32.3 | 1 [Reference] | 29.6 | 1 [Reference] |
| Moderate | 33.8 | 35.7 | 1.33 (1.07-1.64) | 30.5 | 1.29 (1.03-1.61) |
| High | 28.1 | 32.5 | 1.50 (1.20-1.88) | 39.4 | 2.10 (1.67-2.63) |
Abbreviations: AOR, adjusted odds ratio; RFEI, Retail Food Environment Index.
Adjusted for the percentage of county population aged 65 years or older. Results from this polytomous generalized mixed-effects models can be interpreted as the log odds of counties with either high or moderate obesity-related cancer mortality rates compared with the log odds of counties with low mortality rates (reference category).
Low categorized as counties with obesity-related cancer mortality rates from 31.0 to 74.0 per 100 000 population.
Group percentage presented as the proportion of counties within variable strata with food environment category.
Moderate categorized as counties with obesity-related cancer mortality rates from 75.0 to 82.0 per 100 000 population.
High categorized as counties with obesity-related cancer mortality rates from 83.0 to 185.7 per 100 000 population.
Discussion
Medical advancements have been associated with reduced cancer mortality rates in the US. However, prior studies showed an association of socioeconomic factors and social determinants of health with worse cancer outcomes.32,40,41,42,43 Among most US counties, we observed a 77% elevated odds of obesity-related cancer death among counties with higher food swamp scores. This was a higher magnitude of association vs the association between food deserts and obesity-related cancer mortality. Additionally, counties with the highest food swamp scores had a more than 2-fold increased risk of cancer mortality compared with counties with moderate or the lowest scores. Our results indicate that food swamps may be a more comprehensive and novel indicator of the typical US food environment compared with food deserts because the counties with the fewest healthy food resources had the highest odds of obesity-related cancer mortality. This is the first study, to our knowledge, to assess whether food desert and food swamp areas across the nation were associated with obesity-related cancer mortality among multiple cancer types in the past 10 years.
To date, only 3 studies have observed that different food environments are associated with obesity or obesity-related cancers. Specifically, these studies showed that food swamps are correlated with obesity alone,17 that persons residing in food deserts in California had higher mortality risk of 2 obesity-related cancer types (breast and colorectal),32 and that patients with esophageal cancer who resided in food deserts in New Hampshire had a higher risk of 30-day readmission after esophagectomy.33 Our findings mirror results from the only previous study analyzing food deserts and cancer mortality. Fong and colleagues32 found that patients with breast cancer who resided in food deserts had a 16% mortality risk and that patients with colorectal cancer who resided in food deserts had a 12% greater mortality risk. The observed elevated association in our study could be due to the difference in data sources (county level vs patient level) despite the fact that both respective studies used multiple years of cancer mortality data. Also, the observed association in our study could be due to an increase in obesity-related cancer deaths, likely explained by treatment complications (eg, surgery or chemotherapy) among patients with obesity vs patients without obesity.44
Stark increases in obesity rates occurred in the US between the late 1990s and 2017,45 threatening population health at epidemic proportions.46 Contemporaneous obesity research and growing policy-making concerns continue to focus on preventive interventions aimed at exploring and bringing awareness to the mechanisms of known associated factors, such as physical inactivity, improper diet or malnutrition, and specific environmental characteristics. As a result, researchers have begun to assess the role of the neighborhood environment and its potential association with obesity and overall health,47 including the consideration of food accessibility, acquisition, and consumption, and to what degree healthy food options are promoted.
The established existence of food deserts and the emergence of food swamps can be explained by a few theories. One proposed theory is that chain grocery stores (eg, Kroger, Sprouts, and Publix) lack a vested interest in remaining in urban neighborhoods with lower socioeconomic status (where most of the population is often composed of racial and ethnic minority groups) for longer periods, thus creating a food desert.43 Coupled with the increasing growth rate of fast-food restaurants in recent years48,49 and the intentional advertisement of unhealthy foods in urban neighborhoods with lower socioeconomic status,19,20,23,24,50 the food desert may transform into a food swamp. Another theory proposes competition issues between chain grocery stores and smaller grocery stores (ie, mom-and-pop shops). Finally, disparities regarding food-barren environments (including the excess promotion of unhealthy foods in communities with racial and ethnic minority groups) can be traced to the historic and resurging discriminatory practices of gentrification and redlining.51
Redlining is commonly known as the denial of services (eg, insurance, banking, supermarkets) to residents with lower socioeconomic status or to racial and ethnic minority groups either by not building resources in underserved neighborhoods or through the selective price gouging of goods.51,52,53,54 The results of these racially charged practices arguably resonate throughout the country and affect successive generations of racial and ethnic minority groups, particularly in the Southeast. Therefore, one could infer that disparities in access to healthy food options through the disenfranchisement of communities with lower socioeconomic status or of racial and ethnic minority groups are a probable augmenting factor regarding obesity and obesity-related cancer types. Future prospective studies should expound on the racial differences between residing in a food desert or food swamp and obesity-related cancer outcomes.
A distinct resource that can improve healthy food access in the US is community gardens.55 Although gardens span the country, garden building and maintenance surged during the 1970s and 1980s in the New England and West Coast regions of the US despite the strong agrarian culture in the South and Southeast and a longer growing season. Community gardening has been an essential aspect for healthy lifestyle movements, with various benefits such as increased physical activity, food intake, and communal engagement.56 Also, studies incorporating individual or community garden–based components for healthy lifestyle changes have primarily been conducted with children.57,58,59 Future clinical trials should implement an innovative healthy lifestyle intervention using neighborhood- and patient-level data along with the maintenance and use of community gardens among adults residing in food deserts or food swamps to better understand the growing concern of unhealthy food environments in the US.
Strengths and Limitations
Findings from our analysis were the first of their kind, to our knowledge, and comprehensively delineated how the increase in of food swamps adversely affects obesity and obesity-related cancer outcomes. We had complete data on 3038 of the 3142 US counties (96.7%) and used a comprehensive scoring system to classify the difference between food deserts and food swamps. Our study has limitations, however. The ecologic design of the analysis did not account for temporal sequence; thus, no causal association of food deserts and food swamps with obesity-related cancer mortality exists. Results are based on groups instead of individuals, so interpretation should be made at the county level to avoid individual inferences of aggregate data (ie, committing the ecologic fallacy). The food environment measures were based on county reporting of the healthy and unhealthy food options available; misclassification of various food stores (and subsequent validity concerns) could have occurred because they were categorized by North American Industry Classification System codes.60 Last, information on race, ethnicity, and income was based on county-level data, which may limit the ability to further examine racial, ethnic, or socioeconomic differences at the individual level in the association of food deserts and food swamps with obesity-related cancer mortality.
Conclusions
This cross-sectional study found that counties with food desert or food swamp environments had significantly greater odds of obesity-related cancer mortality. Food swamps appear to be a growing epidemic across the US, likely because of systemic issues, and should draw concern and conversation from local and state officials. Future studies should analyze the potential mediating association of obesity and specific social determinants of health with unhealthy food environments and cancer outcomes via group-level (Census tract or neighborhood-level areas) and individual-level data to provide a thorough illustration regarding specific social determinants of health and cancer. Also, researchers should consider clinical and mixed-methods studies to determine whether racial, sex, or socioeconomic status differences exist in the association between food desert or food swamp environments and cancer. Community-based participatory research efforts can include partnerships with local policy makers, community stakeholders (eg, farmers and gardeners), and funding agencies to create and maintain sustainable approaches to combating obesity and establishing healthier accessible foods, including community garden development in underserved communities nationwide.
eTable 1. ICD-10 Codes for Identification of Obesity-Related Cancers
eTable 2. Additional Generalized Mixed Effects Models for the Association of Food Environment Measures and Obesity-Related Cancer Mortality Among U.S. Counties (N = 3038)
eTable 3. Fully Adjusted Multilevel Generalized Mixed Effects Models for the Association of Food Environment Measures and Obesity-Related Cancer Mortality among U.S. Counties (N = 3038)
eReferences.
Data Sharing Statement
References
- 1.Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72(1):7-33. doi: 10.3322/caac.21708 [DOI] [PubMed] [Google Scholar]
- 2.Lewandowska AM, Rudzki M, Rudzki S, Lewandowski T, Laskowska B. Environmental risk factors for cancer—review paper. Ann Agric Environ Med. 2019;26(1):1-7. doi: 10.26444/aaem/94299 [DOI] [PubMed] [Google Scholar]
- 3.Goding Sauer A, Siegel RL, Jemal A, Fedewa SA. Current prevalence of major cancer risk factors and screening test use in the United States: disparities by education and race/ethnicity. Cancer Epidemiol Biomarkers Prev. 2019;28(4):629-642. doi: 10.1158/1055-9965.EPI-18-1169 [DOI] [PubMed] [Google Scholar]
- 4.Akinyemiju T, Moore JX, Pisu M, et al. A prospective study of dietary patterns and cancer mortality among Blacks and Whites in the REGARDS cohort. Int J Cancer. 2016;139(10):2221-2231. doi: 10.1002/ijc.30287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lauby-Secretan B, Scoccianti C, Loomis D, Grosse Y, Bianchini F, Straif K; International Agency for Research on Cancer Handbook Working Group . Body fatness and cancer—viewpoint of the IARC Working Group. N Engl J Med. 2016;375(8):794-798. doi: 10.1056/NEJMsr1606602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kinlen D, Cody D, O’Shea D. Complications of obesity. QJM. 2018;111(7):437-443. doi: 10.1093/qjmed/hcx152 [DOI] [PubMed] [Google Scholar]
- 7.Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003;348(17):1625-1638. doi: 10.1056/NEJMoa021423 [DOI] [PubMed] [Google Scholar]
- 8.Harvey AE, Lashinger LM, Hursting SD. The growing challenge of obesity and cancer: an inflammatory issue. Ann N Y Acad Sci. 2011;1229:45-52. doi: 10.1111/j.1749-6632.2011.06096.x [DOI] [PubMed] [Google Scholar]
- 9.Akinyemiju T, Moore JX, Pisu M, et al. A prospective study of obesity, metabolic health, and cancer mortality. Obesity (Silver Spring). 2018;26(1):193-201. doi: 10.1002/oby.22067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Villarini A, Pasanisi P, Raimondi M, et al. Preventing weight gain during adjuvant chemotherapy for breast cancer: a dietary intervention study. Breast Cancer Res Treat. 2012;135(2):581-589. doi: 10.1007/s10549-012-2184-4 [DOI] [PubMed] [Google Scholar]
- 11.Thomson CA, Stopeck AT, Bea JW, et al. Changes in body weight and metabolic indexes in overweight breast cancer survivors enrolled in a randomized trial of low-fat vs. reduced carbohydrate diets. Nutr Cancer. 2010;62(8):1142-1152. doi: 10.1080/01635581.2010.513803 [DOI] [PubMed] [Google Scholar]
- 12.Scott E, Daley AJ, Doll H, et al. Effects of an exercise and hypocaloric healthy eating program on biomarkers associated with long-term prognosis after early-stage breast cancer: a randomized controlled trial. Cancer Causes Control. 2013;24(1):181-191. doi: 10.1007/s10552-012-0104-x [DOI] [PubMed] [Google Scholar]
- 13.Kohler LN, Garcia DO, Harris RB, Oren E, Roe DJ, Jacobs ET. Adherence to diet and physical activity cancer prevention guidelines and cancer outcomes: a systematic review. Cancer Epidemiol Biomarkers Prev. 2016;25(7):1018-1028. doi: 10.1158/1055-9965.EPI-16-0121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kenfield SA, DuPre N, Richman EL, Stampfer MJ, Chan JM, Giovannucci EL. Mediterranean diet and prostate cancer risk and mortality in the Health Professionals Follow-up Study. Eur Urol. 2014;65(5):887-894. doi: 10.1016/j.eururo.2013.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yang M, Kenfield SA, Van Blarigan EL, et al. Dietary patterns after prostate cancer diagnosis in relation to disease-specific and total mortality. Cancer Prev Res (Phila). 2015;8(6):545-551. doi: 10.1158/1940-6207.CAPR-14-0442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.White M, Addison C, Jenkins BWC, et al. Factors affecting dietary practices in a Mississippi African American community. Int J Environ Res Public Health. 2017;14(7):718. doi: 10.3390/ijerph14070718 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cooksey-Stowers K, Schwartz MB, Brownell KD. Food swamps predict obesity rates better than food deserts in the United States. Int J Environ Res Public Health. 2017;14(11):1366. doi: 10.3390/ijerph14111366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Camp NL. Food insecurity and food deserts. Nurse Pract. 2015;40(8):32-36. doi: 10.1097/01.NPR.0000453644.36533.3a [DOI] [PubMed] [Google Scholar]
- 19.Gordon C, Purciel-Hill M, Ghai NR, Kaufman L, Graham R, Van Wye G. Measuring food deserts in New York City’s low-income neighborhoods. Health Place. 2011;17(2):696-700. doi: 10.1016/j.healthplace.2010.12.012 [DOI] [PubMed] [Google Scholar]
- 20.Hurvitz PM, Moudon AV, Rehm CD, Streichert LC, Drewnowski A. Arterial roads and area socioeconomic status are predictors of fast food restaurant density in King County, WA. Int J Behav Nutr Phys Act. 2009;6:46. doi: 10.1186/1479-5868-6-46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Galvez MP, Morland K, Raines C, et al. Race and food store availability in an inner-city neighbourhood. Public Health Nutr. 2008;11(6):624-631. doi: 10.1017/S1368980007001097 [DOI] [PubMed] [Google Scholar]
- 22.Kwate NO, Yau CY, Loh JM, Williams D. Inequality in obesigenic environments: fast food density in New York City. Health Place. 2009;15(1):364-373. doi: 10.1016/j.healthplace.2008.07.003 [DOI] [PubMed] [Google Scholar]
- 23.Powell LM, Chaloupka FJ, Bao Y. The availability of fast-food and full-service restaurants in the United States: associations with neighborhood characteristics. Am J Prev Med. 2007;33(4)(suppl):S240-S245. doi: 10.1016/j.amepre.2007.07.005 [DOI] [PubMed] [Google Scholar]
- 24.Block JP, Christakis NA, O’Malley AJ, Subramanian SV. Proximity to food establishments and body mass index in the Framingham Heart Study offspring cohort over 30 years. Am J Epidemiol. 2011;174(10):1108-1114. doi: 10.1093/aje/kwr244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Morland K, Diez Roux AV, Wing S. Supermarkets, other food stores, and obesity: the atherosclerosis risk in communities study. Am J Prev Med. 2006;30(4):333-339. doi: 10.1016/j.amepre.2005.11.003 [DOI] [PubMed] [Google Scholar]
- 26.Fisher BD, Strogatz DS. Community measures of low-fat milk consumption: comparing store shelves with households. Am J Public Health. 1999;89(2):235-237. doi: 10.2105/AJPH.89.2.235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ayala GX, Baquero B, Laraia BA, Ji M, Linnan L. Efficacy of a store-based environmental change intervention compared with a delayed treatment control condition on store customers’ intake of fruits and vegetables. Public Health Nutr. 2013;16(11):1953-1960. doi: 10.1017/S1368980013000955 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Oates GR, Jackson BE, Partridge EE, Singh KP, Fouad MN, Bae S. Sociodemographic patterns of chronic disease: how the mid-South region compares to the rest of the country. Am J Prev Med. 2017;52(1s1):S31-S39. doi: 10.1016/j.amepre.2016.09.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nowakowski ACH, Shin J, Carretta HJ. Regional risk: mapping single and multiple chronic conditions in the United States. SAGE Open. 2019;9(1):2158244018822385. doi: 10.1177/2158244018822385 [DOI] [Google Scholar]
- 30.Moore JX, Royston KJ, Langston ME, et al. Mapping hot spots of breast cancer mortality in the United States: place matters for Blacks and Hispanics. Cancer Causes Control. 2018;29(8):737-750. doi: 10.1007/s10552-018-1051-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Moore JX, Tingen MS, Coughlin SS, et al. Understanding geographic and racial/ethnic disparities in mortality from four major cancers in the state of Georgia: a spatial epidemiologic analysis, 1999–2019. Sci Rep. 2022;12(1):14143. doi: 10.1038/s41598-022-18374-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fong AJ, Lafaro K, Ituarte PHG, Fong Y. Association of living in urban food deserts with mortality from breast and colorectal cancer. Ann Surg Oncol. 2021;28(3):1311-1319. doi: 10.1245/s10434-020-09049-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fay KA, Maeder ME, Emond JA, et al. Residing in a food desert is associated with an increased risk of readmission following esophagectomy for cancer. J Thorac Dis. 2022;14(6):1854-1868. doi: 10.21037/jtd-21-1637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Centers for Disease Control and Prevention. About multiple cause of death, 1999-2020. CDC WONDER. Accessed July 13, 2022. https://wonder.cdc.gov/mcd-icd10.html
- 35.Economic Research Service. Food Environment Atlas. US Department of Agriculture. Accessed July 13, 2022. https://www.ers.usda.gov/data-products/food-environment-atlas/data-access-and-documentation-downloads/
- 36.Census county divisions (CCDs) and equivalent entities for the 2020 Census—final criteria: a notice by the Census Bureau on 11/13/2018. Federal Register: the daily journal of the United States government. Accessed March 24, 2023. https://www.federalregister.gov/documents/2018/11/13/2018-24566/census-county-divisions-ccds-and-equivalent-entities-for-the-2020-census-final-criteria#citation-2-p56285
- 37.Jensen MD, Ryan DH, Apovian CM, et al. ; American College of Cardiology/American Heart Association Task Force on Practice Guidelines; Obesity Society . 2013 AHA/ACC/TOS guideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. Circulation. 2014;129(25)(suppl 2):S102-S138. doi: 10.1161/01.cir.0000437739.71477.ee [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Walker RE, Keane CR, Burke JG. Disparities and access to healthy food in the United States: a review of food deserts literature. Health Place. 2010;16(5):876-884. doi: 10.1016/j.healthplace.2010.04.013 [DOI] [PubMed] [Google Scholar]
- 39.ver Ploeg M, Breneman V, Farrigan T, et al. Access to affordable and nutritious food: measuring and understanding food deserts and their consequences: report to Congress. Published June 2009. Accessed June 1, 2022. https://ageconsearch.umn.edu/record/292130/files/12716_ap036_1_.pdf
- 40.Warner ET, Gomez SL. Impact of neighborhood racial composition and metropolitan residential segregation on disparities in breast cancer stage at diagnosis and survival between black and white women in California. J Community Health. 2010;35(4):398-408. doi: 10.1007/s10900-010-9265-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Landrine H, Corral I, Lee JGL, Efird JT, Hall MB, Bess JJ. Residential segregation and racial cancer disparities: a systematic review. J Racial Ethn Health Disparities. 2017;4(6):1195-1205. doi: 10.1007/s40615-016-0326-9 [DOI] [PubMed] [Google Scholar]
- 42.Russell EF, Kramer MR, Cooper HL, Gabram-Mendola S, Senior-Crosby D, Jacob Arriola KR. Metropolitan area racial residential segregation, neighborhood racial composition, and breast cancer mortality. Cancer Causes Control. 2012;23(9):1519-1527. doi: 10.1007/s10552-012-0029-4 [DOI] [PubMed] [Google Scholar]
- 43.Cummins S, Macintyre S. Food environments and obesity—neighbourhood or nation? Int J Epidemiol. 2006;35(1):100-104. doi: 10.1093/ije/dyi276 [DOI] [PubMed] [Google Scholar]
- 44.Horowitz NS, Wright AA. Impact of obesity on chemotherapy management and outcomes in women with gynecologic malignancies. Gynecol Oncol. 2015;138(1):201-206. doi: 10.1016/j.ygyno.2015.04.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Centers for Disease Control and Prevention. Adult obesity facts. Updated May 17, 2022. Accessed May 17, 2022. https://www.cdc.gov/obesity/data/adult.html
- 46.World Health Organization. Obesity and overweight. Published June 9, 2021. Accessed May 17, 2022. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
- 47.Bodor JN, Rice JC, Farley TA, Swalm CM, Rose D. The association between obesity and urban food environments. J Urban Health. 2010;87(5):771-781. doi: 10.1007/s11524-010-9460-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zhou H, Kim G, Wang J, Wilson K. Investigating the association between the socioeconomic environment of the service area and fast food visitation: a context-based crystal growth approach. Health Place. 2022;76:102855. doi: 10.1016/j.healthplace.2022.102855 [DOI] [PubMed] [Google Scholar]
- 49.Jeffery RW, Baxter J, McGuire M, Linde J. Are fast food restaurants an environmental risk factor for obesity? Int J Behav Nutr Phys Act. 2006;3:2. doi: 10.1186/1479-5868-3-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Hilmers A, Hilmers DC, Dave J. Neighborhood disparities in access to healthy foods and their effects on environmental justice. Am J Public Health. 2012;102(9):1644-1654. doi: 10.2105/AJPH.2012.300865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Li M, Yuan F. Historical redlining and food environments: a study of 102 urban areas in the United States. Health Place. 2022;75:102775. doi: 10.1016/j.healthplace.2022.102775 [DOI] [PubMed] [Google Scholar]
- 52.Gross TA. A “forgotten history” of how the US government segregated America. Transcript. National Public Radio. Published May 3, 2017. Accessed November 1, 2019. https://www.npr.org/2017/05/03/526655831/a-forgotten-history-of-how-the-u-s-government-segregated-america
- 53.Zenou Y, Boccard N. Racial discrimination and redlining in cities. J Urban Econ. 2000;48(2):260-285. doi: 10.1006/juec.1999.2166 [DOI] [Google Scholar]
- 54.Eisenhauer E. In poor health: supermarket redlining and urban nutrition. GeoJournal. 2001;53(2):125-133. doi: 10.1023/A:1015772503007 [DOI] [Google Scholar]
- 55.Malberg Dyg P, Christensen S, Peterson CJ. Community gardens and wellbeing amongst vulnerable populations: a thematic review. Health Promot Int. 2020;35(4):790-803. doi: 10.1093/heapro/daz067 [DOI] [PubMed] [Google Scholar]
- 56.Al-Delaimy WK, Webb M. Community gardens as environmental health interventions: benefits versus potential risks. Curr Environ Health Rep. 2017;4(2):252-265. doi: 10.1007/s40572-017-0133-4 [DOI] [PubMed] [Google Scholar]
- 57.Gatto NM, Ventura EE, Cook LT, Gyllenhammer LE, Davis JN. LA Sprouts: a garden-based nutrition intervention pilot program influences motivation and preferences for fruits and vegetables in Latino youth. J Acad Nutr Diet. 2012;112(6):913-920. doi: 10.1016/j.jand.2012.01.014 [DOI] [PubMed] [Google Scholar]
- 58.Heim S, Bauer KW, Stang J, Ireland M. Can a community-based intervention improve the home food environment? parental perspectives of the influence of the delicious and nutritious garden. J Nutr Educ Behav. 2011;43(2):130-134. doi: 10.1016/j.jneb.2010.01.003 [DOI] [PubMed] [Google Scholar]
- 59.Khan M, Bell R. Effects of a school based intervention on children’s physical activity and healthy eating: a mixed-methods study. Int J Environ Res Public Health. 2019;16(22):4320. doi: 10.3390/ijerph16224320 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fleischhacker SE, Evenson KR, Sharkey J, Pitts SB, Rodriguez DA. Validity of secondary retail food outlet data: a systematic review. Am J Prev Med. 2013;45(4):462-473. doi: 10.1016/j.amepre.2013.06.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. ICD-10 Codes for Identification of Obesity-Related Cancers
eTable 2. Additional Generalized Mixed Effects Models for the Association of Food Environment Measures and Obesity-Related Cancer Mortality Among U.S. Counties (N = 3038)
eTable 3. Fully Adjusted Multilevel Generalized Mixed Effects Models for the Association of Food Environment Measures and Obesity-Related Cancer Mortality among U.S. Counties (N = 3038)
eReferences.
Data Sharing Statement