Abstract
Cite this article: Bone Joint Res 2023;12(5):309–310.
Keywords: Total hip arthroplasty, Early osteoarthritis, Subchondral cysts, early osteoarthritis, total hip arthroplasty (THA), MRI scans, Oxford Hip Scores (OHS), patient-acceptable symptom state’, Anesthesiologists, EQ-5D scores, visual analogue scale, EuroQol five-dimension questionnaire (EQ-5D), Kellgren and Lawrence (KL) grades
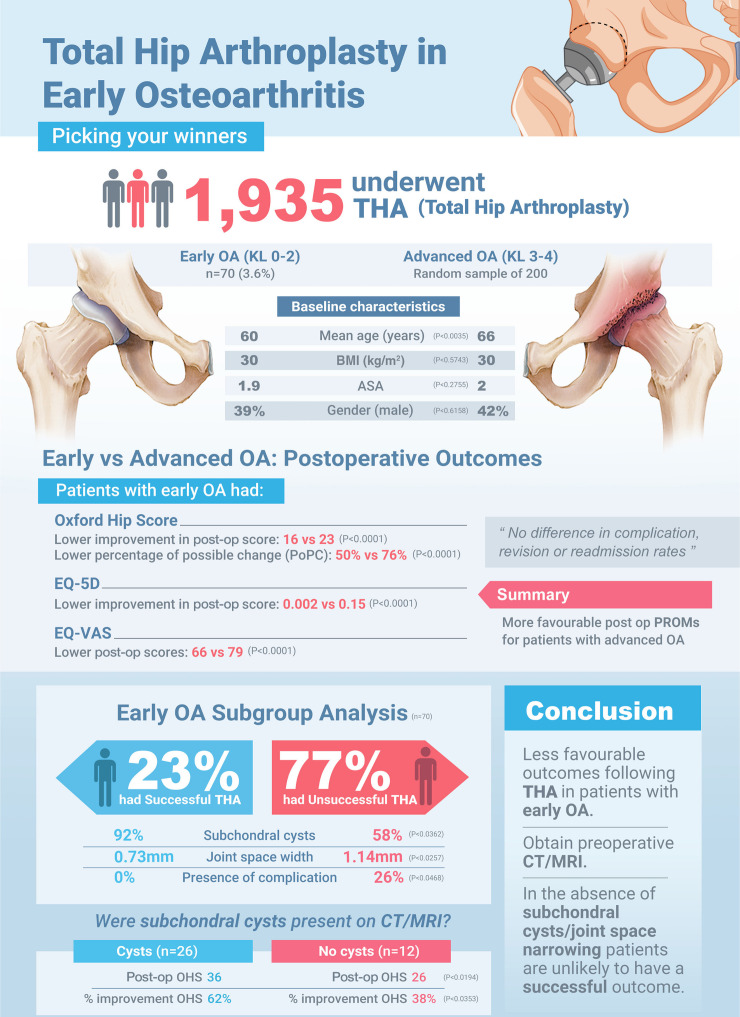
The outcomes following total hip arthroplasty (THA) in patients with early osteoarthritis (OA) are less predictable than in severe disease.1-4 We wanted to assess the factors that are associated with successful outcome.
We compared 70 patients with early OA (Kellgren and Lawrence (KL) grades 0 to 2) with 200 patients with advanced OA (KL grades 3 and 4). Oxford Hip Scores (OHS),5,6 EuroQol five-dimension questionnaire (EQ-5D), and EuroQol-visual analogue scale (EQ-VAS) scores were analyzed preoperatively and one year postoperatively. A subgroup analysis was performed for those with early OA to identify factors (clinical and radiological) associated with a successful THA – defined as a postoperative OHS ≥ 42; the so-called ‘patient-acceptable symptom state’.7
Patients undergoing THA with early OA were significantly younger (61 vs 66 years; p = 0.004), however no differences in BMI, American Society of Anesthesiologists (ASA),8 or sex were noted. After confounders were adjusted for, there were no differences in preoperative OHS or EQ-5D scores between the two groups, however postoperative function scores were significantly lower in the early OA group. In the early OA group, EQ-VAS was significantly lower preoperatively and also postoperatively. No differences in complication, revision, or readmission rates were observed.
Only 16/70 (23%) patients with early OA had a successful THA (OHS ≥ 42). In the radiological analysis (n = 38 with preoperative CT or MRI scans), subchondral cysts were seen more commonly in the successful THA group compared with the unsuccessful group (92% vs 58%; p = 0.036). A narrower joint space width on CT or MRI was associated with a successful THA, as was the absence of a postoperative complication.
We recommend obtaining a preoperative CT or MRI scan in patients with early radiological OA, and if this fails to demonstrate subchondral cysts then a THA is unlikely to provide a satisfactory outcome.
Author contributions
M. Sharrock: Data curation, Formal analysis, Methodology, Writing – original draft.
T. Board: Conceptualization, Methodology, Supervision, Writing – review & editing.
Funding statement
The authors did not receive any financial or material support for the research, authorship, and/or publication of this article.
© 2023 Author(s) et al. This is an open-access article distributed under the terms of the Creative Commons Attribution Non-Commercial No Derivatives (CC BY-NC-ND 4.0) licence, which permits the copying and redistribution of the work only, and provided the original author and source are credited. See https://creativecommons.org/licenses/by-nc-nd/4.0/
Contributor Information
Martin Sharrock, Email: martin.sharrock@doctors.org.uk.
Tim Board, Email: boardtim@gmail.com.
References
- 1. Huynh C, Puyraimond-Zemmour D, Maillefert JF, et al. Factors associated with the orthopaedic surgeon’s decision to recommend total joint replacement in hip and knee osteoarthritis: an international cross-sectional study of 1905 patients. Osteoarthritis Cartilage. 2018;26(10):1311–1318. doi: 10.1016/j.joca.2018.06.013. [DOI] [PubMed] [Google Scholar]
- 2. Tilbury C, Holtslag MJ, Tordoir RL, et al. Outcome of total hip arthroplasty, but not of total knee arthroplasty, is related to the preoperative radiographic severity of osteoarthritis. A prospective cohort study of 573 patients. Acta Orthop. 2016;87(1):67–71. doi: 10.3109/17453674.2015.1092369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Keurentjes JC, Fiocco M, So-Osman C, et al. Patients with severe radiographic osteoarthritis have a better prognosis in physical functioning after hip and knee replacement: a cohort-study. PLoS One. 2013;8(4):e59500. doi: 10.1371/journal.pone.0059500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nilsdotter AK, Aurell Y, Siösteen AK, Lohmander LS, Roos HP. Radiographic stage of osteoarthritis or sex of the patient does not predict one year outcome after total hip arthroplasty. Ann Rheum Dis. 2001;60(3):228–232. doi: 10.1136/ard.60.3.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Dawson J, Fitzpatrick R, Carr A, Murray D. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br. 1996;78(2):185–190. [PubMed] [Google Scholar]
- 6. Murray DW, Fitzpatrick R, Rogers K, et al. The use of the Oxford hip and knee scores. J Bone Joint Surg Br. 2007;89(8):1010–1014. doi: 10.1302/0301-620X.89B8.19424. [DOI] [PubMed] [Google Scholar]
- 7. Rabin R, de Charro F. EQ-5D: a measure of health status from the EuroQol Group. Ann Med. 2001;33(5):337–343. doi: 10.3109/07853890109002087. [DOI] [PubMed] [Google Scholar]
- 8. Feng Y, Parkin D, Devlin NJ. Assessing the performance of the EQ-VAS in the NHS PROMs programme. Qual Life Res. 2014;23(3):977–989. doi: 10.1007/s11136-013-0537-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Keurentjes JC, Van Tol FR, Fiocco M, et al. Patient acceptable symptom states after totalhip or knee replacement at mid-term follow-up: Thresholds of the Oxford hip and knee scores. Bone Joint Res. 2014;3(1):7–13. doi: 10.1302/2046-3758.31.2000141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Saklad M. Grading of patients for surgical procedures. Anesthesiology. 1941;2(3):281–284. doi: 10.1097/00000542-194105000-00004. [DOI] [Google Scholar]


