Abstract
Purpose:
Hepatitis B (HBV), the leading cause of hepatocellular carcinoma (HCC), disproportionately affects minorities. Compared to other races, Blacks more often present with advanced HCC and have decreased survival. We observed higher HBV-associated HCC rates among Blacks than reported nationally. In our center, Haitian Blacks had the highest rates of HBV-associated HCC and shorter survival compared to other Blacks. We investigated knowledge and perceptions regarding HBV and HCC among Blacks born in the United States or Haiti.
Methods:
Using community partnerships, participants were recruited via word of mouth, email, social media or from Hepatology clinic. Focus groups were conducted in Haitian Creole or English and stratified by birthplace, gender and infection status. Discussions were audio-recorded and transcribed verbatim. A constant comparative method was used for data analysis; themes are based on conversational details.
Results:
There were 55 participants; 49% were male and 27% had chronic HBV. Only 42% of Haitian Blacks knew about HBV prior to participation vs. 78% of African-Americans, p 0.03. Both groups expressed that fear, mistrust of the medical establishment, denial and stigma might compel persons to avoid seeking care. Both groups attributed higher rates of late stage HCC diagnosis in Blacks to inadequate financial resources and education. Those with HBV reported confusion regarding their infection and suboptimal communication with healthcare providers.
Conclusions:
In two communities disproportionately affected by HBV, misconceptions about disease transmission, stigma, low health literacy and decreased access to care may limit detection for HBV. Culturally-relevant community-based interventions are needed to increase HBV detection.
Keywords: Disparities, focus groups, chronic liver disease, patient knowledge, community-based participatory research
INTRODUCTION:
The incidence of hepatocellular carcinoma (HCC) has increased significantly over the past three decades[1] and is projected to surpass breast, colorectal and prostate cancer to become the third leading cause of cancer-related death by 2030.[2] Globally, hepatitis B (HBV) contributes to over 50% of HCC cases;[3] HBV increases the odds of developing HCC by 21.6-fold.[4] Most who are chronically infected with HBV are unaware of their infection and there are significant racial/ethnic disparities in awareness of HBV infection,[5] which has implications for HBV treatment and cancer screening. Worldwide, vertical transmission is the most common mechanism for HBV infection; 90% of those infected as infants develop chronic infection.[6] The United States (US) is considered to have low prevalence of chronic HBV, 0.27%.[7] However, prevalence increases with age and is higher in persons over age 40 compared to younger adults and children,[5] as the former were born before childhood HBV vaccination became universally recommended in 1991.[8] In certain states like New York, California and Florida, the burden of disease is higher, reflecting immigration patterns. Of persons with chronic HBV living in the US, 64% were born outside the US.[9] Rates of acute HBV are higher in Florida than nationally and rose 6% between 2012–2016.[10] Nationally, non-Hispanic Blacks are disproportionately affected by both acute[10] and chronic HBV.[11–13]
South Florida is home to the largest enclave of Haitian immigrants in the US. Haiti has high HBV endemicity; the prevalence of chronic infection is approximately 14%[14] and nearly 1/3 of adults have evidence of prior infection.[15] In a retrospective analysis of HCC patients in our system, we found that Blacks were more affected by HBV than other races. Compared to 8% of Whites, 21% of African-American (AA) Blacks and 30% of Haitians with HCC were chronically infected with HBV. Blacks were least likely to have received antivirals prior to HCC diagnosis. Often, HBV and HCC diagnoses were concurrent.[16] Although the Centers for Disease Control and Prevention (CDC) recommend screening for persons born in countries where hepatitis B surface antigen (HbsAg) prevalence exceeds 2%, adherence to these recommendations is variable,[17] even in settings where both patients and providers are from high-risk countries,[18] with dire consequences. Delayed HBV diagnosis contributes to advanced HCC stage at presentation and decreased survival.
Factors contributing to delayed HBV and HCC diagnoses include suboptimal patient, provider, and community knowledge and barriers to obtaining care.[19] Despite widespread availability of vaccines and antiviral therapy, chronic HBV remains a major public health problem globally and in pockets of the US. There is low knowledge in many populations that are disproportionately affected.[20–22] Also, concerns about stigma might influence the decision to seek treatment. Programs such as San Francisco’s Hep B Free,[23, 24] Hep Free NYC, [25] and BFreeNYC[26] have incorporated community engagement, media campaigns and provider education in an effort to increase community awareness and destigmatize HBV. Although these programs cannot be implicated directly in the declining HCC incidence in Asians, Asian immigrants were the primary targets and HCC incidence has declined among Asians in the US, while rising in all other races.[1]
These successful programs could be replicated in other cities and populations. However, little formative research has been conducted in other minority groups at increased risk for HBV.[27] Despite successful screening studies conducted among African immigrants,[28, 29] it is unknown which screening and education strategies would be most effective from the perspective of Blacks born in the US or Haiti, two populations which are disproportionately affected by HBV and extremely relevant for our catchment area. In this study, we used mixed methods to ascertain knowledge about HBV infection and to assess cultural differences in perceptions about HBV, HCC and access to care between African-Americans and Haitians.
EXPERIMENTAL PROCEDURES:
Research Paradigm:
Our previous study found that although Blacks with HCC were disproportionately affected by HBV, they were least likely to be aware of their HBV infection until HCC diagnosis.[16] Recognizing that data regarding community knowledge of HBV risk and screening is essential to successfully design and implement community-based HBV screening programs, we decided to conduct focus groups to elicit general knowledge and perceptions about HBV, HCC and access to screening. We opted for focus groups to elicit individual perceptions and to also observe how perceptions were shaped by interaction with other community members. In 2016, we shared our research findings with the Sylvester Comprehensive Cancer Center (SCCC) Community Advisory Board (CAB). We presented our tentative plan to recruit community members with and without HBV as well as recruit established patients with known HBV to participate in focus groups. We discussed recruitment methods and the planned incentive for participation. The CAB did not recommend any modifications to planned study procedures and we received CAB approval. In order to contextualize the focus group findings, we assessed the health literacy of participants using the Short Assessment of Health Literacy (SAHL).[30, 31] We also collected detailed demographic data including information on medical comorbidities and data regarding prior knowledge of HBV. This mixed-methods approach allowed us to fully characterize the study population and understand the degree to which our participants represent the larger target community. Results from this study were shared with the community at one of Sylvester’s biannual CAB meetings in 2019. The CAB includes key stakeholders who represent the communities from which we recruited. The results of this study were also presented to the academic community via various forums, including seminars at Sylvester, local and national research meetings
Participant Recruitment:
Using the tenets of community-engaged research, we leveraged partnerships between stakeholders, community advisory boards and SCCC’s Behavioral and Community-Based Research Shared Resource Core (BCSR) to recruit participants. Community members participated in recruitment as the primary mode of advertising the study was by word of mouth. Other methods included local radio, email and social media. We recruited participants with chronic HBV using the above methods and purposive sampling, e.g. direct referral from treating physicians and posted fliers at the University of Miami and Jackson Memorial Hospital Hepatology clinics. We targeted Black men and women born in the US or Haiti and excluded participants with known hepatitis C (HCV) infection, cirrhosis, or HCC. We stratified groups by HBV infection; we anticipated that HBV-infected participants would be more knowledgeable and have different perspectives. Additionally, we wanted to minimize any discomfort that HBV-infected participants might experience by participating in a mixed group. Participants were grouped further by birthplace: HBV-negative Haitian women, HBV-negative AA women, HBV-negative Haitian men, HBV-negative AA men, HBV-positive Haitian women, HBV-positive AA women, HBV-positive Haitian men, and HBV-positive AA men. We aimed to enroll ten participants per group. [32]
Focus Groups:
The initial focus group was conducted on February 17, 2017 and the final focus group was conducted on February 22, 2018. A moderator guide was developed to facilitate discussion regarding general health and risk factors for HBV, cirrhosis and HCC. The moderator subsequently informed participants about local HCC prevalence patterns and survival outcomes by race. Finally, the moderator asked about barriers and facilitators to community education and healthcare access. The guide was developed by the principal investigator (PDJ) and reviewed with collaborators (JS, EK, and PM). The PI conducted cognitive debriefing on the moderator guide and demographic questionnaire with BCSR staff who were representative of the intended study population. Informed consent was obtained from all individual participants included in the study. Although we planned to conduct eight focus groups with ten participants each, we conducted more focus groups with fewer participants for ease of scheduling and to facilitate participation. Additionally, some Haitian participants preferred to participate in English while others preferred Haitian Creole. Focus groups were conducted in English or Haitian Creole according to participant preference. Thus, those focus groups could not be combined. Eleven focus groups were held at partnering community-based organizations. Participants received refreshments during the discussion and a $50 gift card for a local grocery store. After the discussion, all participants completed a demographic questionnaire and the Short Assessment of Health Literacy (SAHL),[30, 31] which was translated to Haitian Creole by American Translators Association-certified translators employed by the BCSR. All data collection took place in private.
Recruitment Challenges with Hepatitis B Infected Participants:
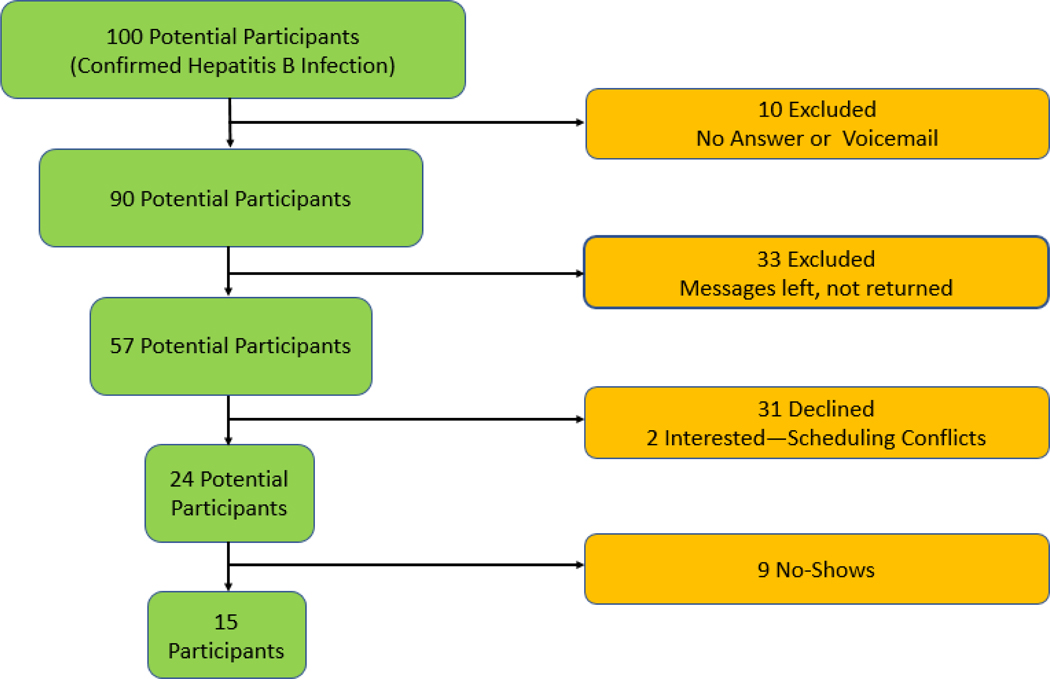
As noted previously, we planned to recruit 40 participants with chronic HBV infection. Based on our robust clinical practice, we did not anticipate challenges meeting this goal. We maintain lists of patients with chronic liver diseases, including HBV, for quality and research purposes. Potential participants were identified by reviewing these lists and many were recruited from clinic after the study was introduced by treating physicians. Although research staff made three attempts to contact 100 potential participants, only fifteen participants with chronic HBV participated. The study was terminated before forty HBV-positive participants were enrolled due to funding and time constraints. Based on yield, recruitment efforts appeared to have reached the point of diminishing returns. Figure 1.
Fig. 1.
Flow chart of potential participants with chronic hepatitis B infection
Statistical Analysis:
Discussions were audio-recorded, transcribed verbatim and translated to English, when applicable. Qualitative data was analyzed using a constant comparative method, in which the research team compared the focus group transcripts to emerging categories. The transcripts were reviewed line by line to identify common themes. Data were broken down into discrete incidents and coded into categories. Each category was compared to previously coded categories to establish relationships and elicit overall themes.
Categorical variables are expressed using proportions and continuous variables using median and interquartile range. We identified associations between baseline characteristics and birthplace using Wilcoxon rank-sum and Kruskal-Wallis tests for continuous and Pearson’s chi-square for categorical variables. For quantitative analyses, p-values ≤ 0.05 were considered statistically significant. Statistical analyses were performed using Stata/SE 14.2 (College Station, TX) and NVivo12 Plus. This study was approved by the SCCC Community Advisory Board and Institutional Review Board at the University of Miami Miller School of Medicine.
RESULTS:
Characteristics of the sample, stratified by birthplace:
There were 55 participants; 27 were Haitian-born and 27 were US-born, e.g African-American (AA). One participant was born in Jamaica, but had lived in the US for 30 years and self-identified as AA. Thus, he participated and was analyzed with AA males. One Haitian participant was US-born but self-identified as Haitian. She was grouped and analyzed with Haitian women. The sample was 52.7% male; there were no significant gender differences by birthplace. Median age of Haitian participants was 51, compared to 55 for AA participants. There were differences in education level and health literacy, as measured by median SAHL score. There were no significant ethnic differences in the percentage of participants reporting hypertension, obesity, diabetes, hyperlipidemia, cancer, or other medical comorbidities. We found variable levels of HBV awareness; 38% of those surveyed had never heard of HBV before the focus group. Over 50% of Haitian participants reported they had never heard of HBV, compared to fewer than 25% of AA Blacks. See Table 1 for additional details. Supplementary Table 1 details characteristics, stratified by gender, birthplace and disease status.
Table 1.
Baseline characteristics of the sample, overall and stratified by birthplace.
| Overall | US-born (n = 27) | Haitian (n = 28) | p-value | |
|---|---|---|---|---|
|
| ||||
| Median age, years (IQR) | 53 (47–59) | 55 (51–59) | 51 (42.5–56) | 0.03 |
|
| ||||
| US-born, n (%) | 27 (49.1)) | 26 (96.3) | 1 (3.7) | <0.001 |
|
| ||||
| Male, n (%) | 29 (52.7) | 15 (55.6) | 14 (50) | 0.68 |
|
| ||||
| Chronic HBV Infection, n (%) | 15 (27.3) | 7 (25.9) | 8 (28.6) | 0.83 |
|
| ||||
| Marital Status, n (%) | ||||
| Married | 20 (36.4) | 2 (7.4) | 18 (64.3) | < 0.001 |
| Divorced | 8 (14.6) | 8 (29.6) | 0 | |
| Widowed | 2 (3.6) | 1 (3.7) | 1 (3.6) | |
| Separated | 12 (21.8) | 6 (22.2) | 6 (21.4) | |
| Never Married | 12 (21.8) | 9 (33.3) | 3 (10.7) | |
| Unmarried Partner | 1 (1.8) | 1 (3.7) | 0 | |
|
| ||||
| Employment Status, n(%) | ||||
| Employment for wages | 18 (33.3) | 5 (18.5) | 13 (48.2) | 0.48 |
| Self-employed | 8 (14.8) | 5 (18.5) | 3 (11.1) | |
| Out of work for > 1 year | 8 (14.8) | 5 (18.5) | 3 (11.1) | |
| Out of work for <1 year | 2 (3.7) | 1 (3.7) | 1 (3.7) | |
| A homemaker | 0 | 0 | 0 | |
| A student | 5 (9.3) | 3 (11.1) | 2 (7.4) | |
| Retired | 3 (5.6) | 2 (7.4) | 1 (3.7) | |
| Unable to work | 10 (18.5) | 6 (22.2) | 4 (14.8) | |
|
| ||||
| Highest Education Level | ||||
| Never attended school | 2 (3.7) | 0 | 2 (7.4) | 0.02 |
| Grades 1–8 | 6 (11.1) | 0 | 6 (22.2) | |
| Grades 9–11 | 10 (18.5) | 7 (25.9) | 3 (11.1) | |
| Grade 12/GED | 18 (33.3) | 13 (48.2) | 5 (18.5) | |
| College (1–3 Years) | 10 (18.5) | 3 (11.1) | 7 (25.9) | |
| College Graduate | 5 (9.3) | 2 (7.4) | 3 (11.1) | |
| Grad/Adv Degree | 3 (5.6) | 2 (7.4) | 1 (3.7) | |
|
| ||||
| Median SAHL Score, (IQR) | 14 (12–16) | 15 (14–17) | 13 (11–14.5) | 0.01 |
|
| ||||
| Hypertensive, n (%) | 26 (47.3) | 12 (44.4) | 14 (50) | 0.68 |
|
| ||||
| Obese/Overweight, n (%) | 7 (12.7) | 4 (14.8) | 3 (10.7) | 0.65 |
|
| ||||
| Diabetes, n (%) | 12 (21.8) | 7 (25.9) | 5 (17.9) | 0.47 |
|
| ||||
| High cholesterol, n (%) | 17 (30.9) | 7 (25.) | 10 (35.7) | 0.43 |
|
| ||||
| Previous non-liver cancer, n (%) | 4 (7.3) | 3 (11.1) | 1 (3.6) | 0.28 |
|
| ||||
| Smoking Status, n (%) | 0.001 | |||
| Current | 8 (14.8) | 7 (26.9) | 1 (3.6) | |
| Former | 17 (31.5) | 12 (46.2) | 5 (17.9) | |
| Never | 29 (53.7) | 7 (26.9) | 21 (78.6) | |
|
| ||||
| Drug Use, n (%) | <0.001 | |||
| None | 37 (69.8) | 12 (44.4) | 25 (96.2) | |
| Current | 4 (7.6) | 4 (14.8) | 0 | |
| Past | 12 (22.6) | 11 (40.7)) | 1 (3.9) | |
|
| ||||
| Alcoholic Drinks/Day, n (%) | 0.39 | |||
| Non-drinker | 23 (44.2) | 9 (33.3) | 14 (56) | |
| Less than 1 | 16 (30.8) | 9 (33.3) | 7 (28) | |
| One | 4 (7.7) | 2 (7.4) | 2 (8) | |
| Two | 4 (7.7) | 4 (14.8) | 0 | |
| Three to five | 1 (1.9) | 1 (3.7) | 0 | |
| More than five | 2 (3.9) | 1 (3.7) | 1 (4) | |
| Prefer not to comment | 2 (3.9) | 1 (3.7) | 1 (4) | |
|
| ||||
| Seen by a liver specialist, n (%) | 13 (24.1) | 4 (15.4) | 9 (32.1) | 0.11 |
|
| ||||
| Heard of HBV, n (%) | ||||
| Yes | 32 (60.4) | 20 (76.9) | 12 (44.4) | 0.05 |
| No | 20 (37.7) | 6 (23.1) | 14 (51.9) | |
| Don’t know | 1 (1.9) | 0 | 1 (3.7) | |
|
| ||||
| Know a person with HBV, n (%) | ||||
| Yes | 9 (17) | 5 (19.2) | 4 (14.8) | 0.29 |
| No | 42 (79.3) | 19 (73.1) | 23 (85.2) | |
| Don’t know | 2 (3.8) | 2 (7.7) | 0 | |
|
| ||||
| Know a person with cirrhosis, n (%) | ||||
| Yes | 10 (19.2) | 5 (19.2) | 5 (19.2) | 1 |
| No | 40 (76.9) | 20 (76.9) | 20 (76.9) | |
| Don’t know | 2 (3.9) | 1 (3.8) | 1 (3.9) | |
|
| ||||
| Know a person with liver cancer, n (%) | ||||
| Yes | 12 (23.1) | 8 (30.8) | 4 (15.4) | 0.41 |
| No | 36 (69.2) | 16 (61.5) | 20 (76.9) | |
| Don’t know | 4 (7.7) | 2 (7.7) | 2 (2.2) | |
|
| ||||
| Help needed with questionnaire, n (%) | 15 (34.9) | 1 (6.3) | 14 (51.9) | 0.002 |
Abbreviations: GED = General Education Diploma, HBV = hepatitis B, IQR = interquartile range, SAHL = Short Assessment of Health Literacy, US = United States
Characteristics of the sample, stratified by HBV infection:
There were fifteen participants with chronic HBV infection, 27.3% of the sample. Stratified by HBV status, there were no significant differences in age, birthplace or marital status. A higher percentage of participants with HBV reported being unable to work, 40%, compared to 10.3% of those without HBV, p 0.003. There was no significant difference in the highest educational level attained. However, participants with chronic HBV had higher health literacy than participants without HBV, p 0.02. Participants with HBV were more likely to report personal history of diabetes, p 0.05, and hyperlipidemia, p 0.03. There were no significant differences in reported smoking, drug or alcohol use. See Table 2.
Table 2.
Baseline characteristics of the sample, stratified by infection status.
| No HBV Infection (n = 40) | Chronic HBV Infection (n = 15) | p-value | |
|---|---|---|---|
|
| |||
| Median Age, years (IQR) | 53.5 (45.5–58.5) | 53 (47–59) | 0.99 |
|
| |||
| Male gender, n (%) | 20 (50) | 9 (60) | 0.51 |
|
| |||
| US-born, n (%) | 21 (52.5) | 6 (40) | 0.41 |
|
| |||
| Marital Status, n (%) | |||
| Married | 14 (35) | 6 (40) | 0.92 |
| Divorced | 6 (15) | 2 (13.3) | |
| Widowed | 2 (5) | 0 | |
| Separated | 9 (22.5) | 3 (20) | |
| Never Married | 8 (20) | 4 (26.7) | |
| Unmarried Partner | 1 (2.5) | 0 | |
|
| |||
| Employment Status, n (%) | |||
| Employment for wages | 13 (33.3) | 5 (33.3) | 0.003 |
| Self-employed | 8 (20.5) | 0 | |
| Out of work for > 1 year | 7 (18) | 1 (6.7) | |
| Out of work for <1 year | 2 (5.1) | 0 | |
| A homemaker | 0 | 0 | |
| A student | 5 (12.8) | 0 | |
| Retired | 0 | 3 (20) | |
| Unable to work | 4 (10.3) | 6 (40) | |
|
| |||
| Smoking Status, n (%) | |||
| Current | 6 (15.4) | 2 (13.3) | 0.70 |
| Former | 11 (28.2) | 6 (40) | |
| Never | 22 (56.4) | 7 (46.7) | |
|
| |||
| Drug Use, n (%) | |||
| None | 28 (71.8) | 9 (64.3) | 0.23 |
| Current | 4 (10.3) | 0 | |
| Past | 7 (18) | 5 (35.7) | |
|
| |||
| Alcoholic Drinks/Day, n (%) | |||
| Non-drinker | 17 (44.7) | 6 (42.9) | 0.47 |
| Less than 1 | 11 (29) | 5 (35.7) | |
| One | 3 (7.9) | 1 (7.1) | |
| Two | 4 (10.5) | 0 | |
| Three to five | 0 | 1 (7.1) | |
| More than five | 1 (2.6) | 1 (7.1) | |
| Prefer not to comment | 2 (5.3) | 0 | |
|
| |||
| Highest Education Level, n (%) | |||
| Never attended school | 0 | 2 (13.3) | 0.16 |
| Grades 1–8 | 5 (12.8) | 1 (6.7) | |
| Grades 9–11 | 6 (15.4) | 4 (26.7) | |
| Grade 12/GED | 16 (41) | 2 (13.3) | |
| College (1–3 Years) | 7 (18) | 3 (20) | |
| College Graduate | 3 (7.7) | 2 (13.3) | |
| Grad/Adv Degree | 2 (5.1) | 1 (6.7) | |
|
| |||
| Median SAHL Score (IQR) | 13 (12–15) | 16 (14–18) | 0.02 |
|
| |||
| Hypertensive, n (%) | 17 (42.5) | 9 (60) | 0.25 |
|
| |||
| Obese/Overweight, n (%) | 3 (7.5) | 4 (26.7) | 0.06 |
|
| |||
| Diabetes, n (%) | 6 (15) | 6 (40) | 0.05 |
|
| |||
| High Cholesterol, n (%) | 9 (22.5) | 8 (53.3) | 0.03 |
|
| |||
| Previous non-liver cancer, n (%) | 2 (5) | 2 (13.3) | 0.29 |
|
| |||
| Other Medical Problem, n (%) | 6 (15) | 5 (35.7) | 0.1 |
|
| |||
| Seen Liver Specialist, n(%) | 2 (5.1) | 11 (73.3) | <0.001 |
|
| |||
| Heard of HBV, n (%) | |||
| Yes | 20 (52.6) | 12 (80) | 0.18 |
| No | 17 (44.7) | 3 (20) | |
| Don’t Know | 1 (2.6) | 0 | |
|
| |||
| Know a person with HBV, n (%) | |||
| Yes | 2 (5.3) | 7 (46.7) | 0.001 |
| No | 34 (89.5) | 8 (53.3) | |
| Don’t Know | 2 (5.3) | 0 | |
|
| |||
| Know a person with cirrhosis, n (%) | |||
| Yes | 5 (13.5) | 5 (33.3) | 0.19 |
| No | 30 (81.1) | 10 (66.7) | |
| Don’t Know | 2 (5.4) | 0 | |
|
| |||
| Know a person with HCC, n (%) | |||
| Yes | 9 (24.3) | 3 (20) | 0.92 |
| No | 25 (67.6) | 11 (73.3) | |
| Don’t Know | 3 (8.1) | 1 (6.7) | |
|
| |||
| Help needed with Questionnaire, n (%) | 13 (41.9) | 2 (16.7) | 0.12 |
Abbreviations: GED = General Education Diploma, HBV = hepatitis B, IQR = interquartile range, SAHL = Short Assessment of Health Literacy, US = United States
Emerging Themes:
The purpose of this study was to compare the perceptions, beliefs and experiences related to HBV and liver cancer risk among ethnically diverse communities. Participants with HBV were asked additional questions related to their diagnosis, health status and treatment options. The key themes or areas of concern for both groups included: 1) the community’s perception of disease; 2) health knowledge; 3) barriers to care; and 4) health promotion. Below we compare the themes of interest between the two ethnically diverse communities.
(1). Community Perceptions of Disease Burden:
Participants were asked to describe what was known about hepatitis and liver disease in their community and more importantly, how people in their community reacted to those who were infected. Although there were members of each community who had previously heard of the disease, the perceptions of disease burden were very different.
African-American Community:
In the AA community, hepatitis and liver cancer were thought to be uncommon. Most participants reported not hearing much regarding either disease in relation to their friends, family and others living in their community. Although some participants had heard of HBV and liver cancer, most did not believe it impacted their community. One woman stated,
“You rarely hear that black people suffer with cancer. It was the other way around. White people used to always die with cancer. That’s why I don’t understand how you said Black people now is with cancer.”
However, this may be due to lack of transparency pertaining to illness. When asked if they knew anyone with liver cancer, the consensus was that people do not speak openly about illness in their community.
“No. We don’t know about it until that person disappear most of the time.”
Adding to this idea that African-Americans do not share their health status and when they do, the prognosis is already very poor, one male stated:
“It’s a hidden disease in our community because like you said we wouldn’t find out until that person is actually bedridden or he or she has passed…No one talks about it.”
Haitian Community:
In contrast to African-Americans, Haitian participants more often reported hearing about liver disease both in the US and Haiti. When asked if people in their community are affected by liver disease, one woman commented,
“Yes, I have heard that there are a lot of people with liver problem. Sometimes, I meet people and as they talk they mention they have liver problem (disease)…they are sick.”
Another woman initially learned of liver disease in Haiti,
“I could say the same thing because when I was a young girl in Haiti, I knew of someone who died and that’s how they died, cirrhosis of the liver.”
Although, Haitians report liver disease is an issue in their communities, they too believe that those who are diagnosed are unlikely to share their diagnosis or experience with others.
“Even if it happens, they don’t really focus on it, they don’t talk much about it, but there are people with liver disease. There are people that die from cirrhosis of the liver.”
(2). Knowledge of Disease
After discussing their communities’ perceptions of disease burden, we investigated knowledge in our sample regarding HBV, cirrhosis and HCC. Moderators asked questions related to disease knowledge including routes of HBV transmission and the symptoms, diagnosis and treatments available for HBV, cirrhosis and HCC.
African-American Community:
Overall, AA participants knew some causes and symptoms of cirrhosis. In contrast to the low perceived burden of HBV and HCC, many described cirrhosis as common in their communities. Each participant knew at least one person who had suffered from cirrhosis. Most participants linked cirrhosis to heavy drinking and drug use. When asked about the causes of cirrhosis, responses included:
“that’s (be)cause they drink” and “they started drinking young and it messed up their lives…”
Moreover, many participants were aware of the signs and symptoms.
“Then they just swell up, like the swelling never go away. Their stomach and their face. I know their face and their stomach be swollen because I know a couple of people. But they still drink. They drink every day.”
“They say your eyes get like blood yellowish red and jaundice color…Yes, they look like they be turning real dark.”
Although many participants were aware of the symptoms of cirrhosis and one leading cause of cirrhosis, they were less knowledgeable about HBV and HCC. Most AA participants were unaware or misinformed regarding HBV transmission; some thought HBV could be transmitted through cough.
“Yeah being around people coughing around you, stuff like that…mm-hmm. Airborne.”
“I heard it was contagious… I heard it too. They can’t do too much coughing around peoples and none of that.”
Additionally, there was confusion regarding the relationship between HBV and human immunodeficiency virus (HIV). Many participants believed that the two diseases were interrelated. As one participant asked,
“Ok. Can you have HIV and not have this virus or can you have this virus but not have HIV?”
Haitian Community:
Members of the Haitian community were better informed about cirrhosis and HBV compared to the AA group. In addition to knowing the symptoms of liver disease, some were aware of preventative strategies, e.g vaccines.
“Your color. You get a yellow color, that jaundiced color. Okay, your abdomen becomes inflammation (inflamed).”
“I remember once I was traveling to Haiti, going back to Haiti, I took a vaccine for it. Because it can be easily contracted in the country.”
Although some Haitian participants were aware of signs/symptoms of HBV and cirrhosis, many did not know how the disease was contracted and its relationship to HCC. Many asked questions during this time, rather than giving responses. Several participants asked,
“But what is the cause of this disease?”
“Is it contagious?”
“Can you give it to somebody else?”
Additionally, members of the Haitian groups discussed the widespread cultural belief that “supernatural” causes may lead to illness. Although most recognized that supernatural forces do not cause illness, they explained how deeply these beliefs are entrenched into their culture, making it hard to bring new knowledge into their community. When asked what causes the disease, some responses included:
“Also, up till now, some people back home still believe in supernatural diseases and deal in mysticism that is not something scientific.”
“In Haiti, whenever someone dies, they say that it is because someone killed them (supernatural). That is not true. What happened is that the person is not able to go to the doctor to get a checkup, to know the state of their health; they don’t know what’s going on... then when they die you hear that it is because someone killed them (supernaturally).”
Members of the Haitian community stated that they knew there was a difference between HBV and HIV, but the stigma was very similar. One woman stated,
“They consider it... though it isn’t worse than HIV, they consider it the same way. If a parent knew that someone’s child had the disease, they would not allow their child to talk to them, even less date them. Very bad.”
(3). Barriers to Care
Both groups emphasized the overarching theme of “If you’re rich, you’re going to live longer,” in describing barriers to care. Participants believed that opportunities and access to care were significantly affected by the lack of economic resources in their communities. When asked why they thought Blacks were more likely to die from liver cancer compared to other races, participants explained:
“When you look at the environment that people are living in, you can understand how their environment can affect them. Whether it be their financial situation or the way they have to function.”
“We cannot afford to go to the doctor. By the time, it gets to where it is a problem; in our body, it is too late or then people are saying you are giving up.”
Specifically related to HBV and liver cancer, both communities agreed that due to their minority status, they are less likely to have the same resources or receive the same care as their white counterparts.
“Yes, as I said before, it depends on the state of the person. Whites sometimes have the chance to get liver transplant but for Blacks it is more difficult. So, if the person does not have insurance, and ways to get to the doctor... that is the only way they can get better. If they cannot do this, that is why Black people die more from the disease.”
“What can they do to help Black people not to die so quickly? For Whites, they have easier access to care not to die too quick, but is there a way to ameliorate?”
(4). Health Promotion
The group discussions concluded with questions related to next steps and what could be done to promote health in their communities. Both groups agreed that the top priority is raising awareness about HBV, cirrhosis and HCC and how to prevent them. They remarked that educating the community should be the first step.
“They’re gonna wanna know what you what you mean by the liver. You’re gonna have to have someone there who’s educated about it because they’re gonna ask a lot of questions…”
In addition to increasing awareness, both communities suggested that testing and health promotion should happen in the community, rather than a medical office.
“If we could get tested in our community or center in our community that would be great, because a lot of people can’t afford to go to the doctor.”
Participants provided useful suggestions regarding care delivery and community engagement. They mentioned using public service announcements, social media and utilizing schools and universities to educate their communities. They suggested enlistment of community leaders to promote awareness as community members would be more inclined to listen. Many participants suggested a confidential mobile testing unit. Others suggested town-hall educational sessions with medical personnel who were able to explain the disease process clearly.
Unique Perspectives of Hepatitis B Infected Participants:
As expected, the perspectives of HBV-infected participants differed from uninfected participants due to their life experiences and history with diagnosis. Interestingly, three participants indicated via questionnaire that they had not heard of HBV until participating in the focus groups. Review of the medical record revealed that these participants had confirmed HBV infection; two had been prescribed antiviral treatment. In fact, for one participant the treating provider was concerned about medication non-adherence and referred the patient for participation in hopes that the focus group would improve understanding and adherence.
During the focus groups, it became clear that there is significant misunderstanding about their diagnosis and how HBV was transmitted. Similar to HBV-negative participants, one person indicated they were informed that HBV could be contracted by cough. Furthermore, there was confusion regarding the fluctuating course of the infection (e.g. immune tolerant, inactive carrier, immune active) and what the status means for transmission risk.
“How is it that when they send results to the doctor, 6 months ago it was negative… then in a year it is positive? Well, in that case I guess the doctor will call me in to go over with me what’s been going on, if I have been with anybody new, etc. But since I was told I do not have it anymore, they don’t see it, I don’t worry. The only thing is that I protect myself.”
Participants with HBV discussed the emotional burden they carry as a result of the stigma. Many discussed feeling unwanted and ostracized from their community, saying,
“You say you got Hepatitis B, they look at you like you’re crazy. Just like HIV or AIDS. They talk about it.”
“They don’t want to touch you, don’t want to have sex with you. They’re scared. They don’t want to rub against you or touch your skin. They think it’s going to jump on you like that. But that’s not true.”
DISCUSSION:
This study aimed to assess knowledge and explore perceptions of HBV, cirrhosis and liver cancer in two South Florida Black communities disproportionately affected by HBV. There were significant differences in baseline knowledge about HBV by birthplace. Although highly prevalent in Haiti, fewer than 50% of Haitian participants were previously aware of HBV. Analysis of the group discussions revealed differences in the perception of HBV burden and knowledge regarding signs/symptoms of cirrhosis when comparing AA and Haitian Blacks. Haitian Blacks suggested that community members may ascribe HBV and liver disease to supernatural causes, a concept which has been previously well-described.[33, 34] Both groups had similar misconceptions about modes of disease transmission. Additionally, both AA and Haitian Blacks felt that financial and other socioeconomic barriers adversely affected access to care and were the most plausible explanation for increased likelihood of late cancer diagnosis in Blacks with HBV. Participants were aware of the increased focus on HCV in the past five years and provided thoughtful suggestions to improve HBV-specific health promotion efforts. These findings will inform future public-health interventions.
Hepatitis B remains a significant public health problem in the US and worldwide. Of the estimated 1.4 million people in the US with chronic HBV, only 26.2% of those with chronic HBV infection were aware of their infection.[5] The Institute of Medicine determined that lack of knowledge/awareness among healthcare providers, at-risk populations, the public and policymakers and inadequate public resources are hindering efforts to prevent and control viral hepatitis.[19] For HBV, screening recommendations are risk-based, e.g. country of origin, drug use, and household contacts.[35] Despite recommendations, uptake of hepatitis screening is suboptimal.[18, 36, 37] There is a paucity of data describing systematic strategies to improve HBV screening. Most interventions are population-based and focus on specific immigrant communities rather than the healthcare system.[28, 38]
As evidenced by the success of the Hep B Free,[23, 24] Hep Free NYC, [25]and BFreeNYC[26] programs, targeted screening programs can successfully identify HBV-infected persons and effectively link these persons to appropriate follow-up care in some cases.[29] Additionally, screening programs can identify persons who are vulnerable to infection and link them to vaccination, which is a key intervention for cancer prevention. However, it is unclear how these programs perform in other cities with unique cultural mores, like Miami, a city where most residents, 53%, are foreign-born.[39] It was unknown whether minority communities in our catchment area would find such programs acceptable. Study participants believed that community-based educational programs could be highly effective to increase knowledge and awareness regarding hepatitis and its sequelae. They recommended educational town halls, but also suggested utilization of social media platforms and community-specific radio programs, e.g. Haitian radio. They suggested that financial barriers to participation could be overcome by appropriate incentives, including food.
The groups with HBV-infected participants provided rich data regarding patient perceptions of physician-patient communication. Of the 31 potential participants with confirmed HBV who declined participation, eight believed they could not participate because they did not have HBV. While one could speculate that this observation was due to denial and/or stigma, it is equally possible that communication was so ineffective that these potential participants did not understand their infection status. An additional four persons who declined participation reported they had HCV rather than HBV, which amplifies concern about the effectiveness of physician-patient communication. Despite being screened and enrolling in the study, three HBV-infected participants indicated they had not previously heard of HBV. Many participants with HBV did not understand modes of transmission or that HBV is more prevalent in certain regions of the world.
Many HBV patients expressed confusion regarding the status of their infection. This is not unique to these participants[40] and may be explained by current treatment and management practices. Since not all patients with HBV require treatment, they may not fully understand the potential for disease progression and development of complications, like HCC.[41] Furthermore, the nomenclature of some stages of HBV, e.g. inactive carriers, may provide false reassurance. As mentioned by focus group participants and echoed daily during consultations in our Hepatology clinics, “My doctor told me it’s not active, but I’ll always have it. I still don’t really got an understanding about it.” For some participants who had been prescribed treatment, the cost was prohibitive, and the prescriptions went unfilled. Participants perceived that they had to educate themselves about HBV because the information they received from their healthcare providers or the Health Department was inadequate in some cases and frightening in others. Some stated that this uncertainty motivated them to participate in the focus groups to increase their HBV knowledge. These findings highlight the need for improved education of healthcare providers regarding effective communication, patient perceptions and barriers to treatment. Assessment of health literacy is crucial because physicians likely assume patients operate from a higher literacy level than found in our participants. In addition, community-based approaches are essential. Participants indicated that mistrust of the medical establishment, denial/fear and financial barriers prevent many in their communities from accessing health care.
We explored the barriers to adequate screening for HBV and HCC, which contribute to late stage presentation of HCC. Participants indicated that there is disparate access to healthcare in their communities, when compared to non-Blacks. This sentiment is supported by Census data, which reports that non-Hispanic Whites are more likely to be insured compared to Hispanics and non-Hispanic Blacks.[42] In Miami, 19.4% of the population are uninsured.[43] Although there has been marginal improvement,[42] Florida still ranks in the top five states with the highest percentage of uninsured persons. Due to financial constraints, participants may skip appointments. Others stated that it is pointless to seek medical care if unable to afford the recommended treatments.
Participants suggested that future interventions be culturally-relevant and consider the needs and challenges of the community, especially financial challenges. They suggested leveraging existing health fairs, but highlighted the importance of maintaining confidentiality to avoid stigma. They recommended community outreach using mobile screening units/teams and home-based screening. Participants felt that educational sessions targeted to various age groups, as young as middle school, could improve overall community knowledge. Participants highlighted the importance of a community spokesperson, e.g. pastors, coaches, athletes, or local politicians, to bring visibility and lend credibility to the need for HBV screening.[24, 44]
Through this formative work, we have identified several opportunities for intervention. However, there are some limitations. We recruited a smaller sample of HBV-infected participants than intended. Despite this, our groups were large enough to achieve thematic saturation; similarly-sized studies have yielded informative data.[41] Although considerable efforts were made to ensure privacy, some potential HBV-positive participants may have declined due to discomfort with the group setting. This is not unique to our study and is an inherent limitation of focus group studies. Through discussions among our HBV participants, we identified significant challenges with physician-patient communication. It is possible that our HBV-infected participants are more knowledgeable and engaged than those HBV patients who declined participation, which could impact generalizability. However, we expect that the knowledge of the participants reflects the best-case scenario, which exposed significant knowledge gaps.
CONCLUSIONS:
The Department of Health and Human Services (HHS) published the National Viral Hepatitis Action Plan, which sets goals of reducing viral hepatitis health disparities, reducing deaths and improving health for people living with viral hepatitis.[45] To achieve these goals on a local level, we must understand the needs of the affected communities. Participants identified several barriers to timely HBV diagnosis. These include lack of health insurance, financial impediments, inadequate access to healthcare, stigma, inadequate informational material and cultural norms which drive Blacks to delay seeking care until symptomatic. This study is the first to use community-engaged research methods to assess knowledge and perceptions regarding HBV and HCC in the Haitian community compared to AA Blacks. Future research should investigate the needs and perspectives of healthcare providers, develop and implement novel methods to improve communication and patient understanding. The rich qualitative data obtained through this study will inform community-based educational and screening efforts for HBV and will hopefully improve current local epidemiological trends for HCC.
Supplementary Material
Acknowledgements:
The authors acknowledge members of the Behavioral and Community-Based Research Shared Resource for assisting with study recruitment and moderation of focus groups.
Financial Support:
The salary of the corresponding author is partially supported by a Diversity Supplement awarded by the National Institutes of Health (NIH) National Institute on Minority Health and Health Disparities (U01MD010614–01S1). The NIH was not involved in study design or in the collection, analysis or interpretation of data. Further, the NIH did not contribute to the writing of this manuscript or decision to submit for publication. Study procedures and patient incentives were made possible by the Sylvester Catchment Center Grant awarded to the corresponding author in 2016.
Abbreviations:
- AA
African American
- AIDS
acquired immunodeficiency syndrome
- BCSR
Behavioral Community Shared Resource Core
- CDC
Centers for Disease Control and Prevention
- HBV
hepatitis B virus
- HCV
hepatitis C virus
- HHS
Department of Health and Human Services
- HIV
human immunodeficiency virus
- HCC
hepatocellular carcinoma
- SAHL
Short Assessment of Health Literacy
- US
United States
REFERENCES:
- 1.White DL, Thrift AP, Kanwal F, Davila J, El-Serag HB. Incidence of Hepatocellular Carcinoma in All 50 United States, From 2000 Through 2012. Gastroenterology. 2017; 152(4):812–20 e5. doi: 10.1053/j.gastro.2016.11.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rahib L, Smith BD, Aizenberg R, Rosenzweig AB, Fleshman JM, Matrisian LM. Projecting cancer incidence and deaths to 2030: the unexpected burden of thyroid, liver, and pancreas cancers in the United States. Cancer Res. 2014; 74(11):2913–21. doi: 10.1158/0008-5472.CAN-14-0155 [DOI] [PubMed] [Google Scholar]
- 3.Kulik L, El-Serag HB. Epidemiology and Management of Hepatocellular Carcinoma. Gastroenterology. 2018. doi: 10.1053/j.gastro.2018.08.065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Makarova-Rusher OV, Altekruse SF, McNeel TS, et al. Population attributable fractions of risk factors for hepatocellular carcinoma in the United States. Cancer. 2016; 122(11):1757–65. doi: 10.1002/cncr.29971 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim HS, Rotundo L, Yang JD, et al. Racial/ethnic disparities in the prevalence and awareness of Hepatitis B virus infection and immunity in the United States. J Viral Hepat. 2017; 24(11):1052–66. doi: 10.1111/jvh.12735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hyun Kim B, Ray Kim W. Epidemiology of Hepatitis B Virus Infection in the United States. Clin Liver Dis (Hoboken). 2018; 12(1):1–4. doi: 10.1002/cld.732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schweitzer A, Horn J, Mikolajczyk RT, Krause G, Ott JJ. Estimations of worldwide prevalence of chronic hepatitis B virus infection: a systematic review of data published between 1965 and 2013. Lancet. 2015. doi: 10.1016/S0140-6736(15)61412-X [DOI] [PubMed] [Google Scholar]
- 8.https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5125a3.htm. Date accessed 8/10/2020.
- 9.https://www.cdc.gov/hepatitis/statistics/2013surveillance/pdfs/2013hepsurveillancerpt.pdf. Date accessed 8/10/2020.
- 10.https://www.cdc.gov/hepatitis/statistics/2016surveillance/index.htm#tabs-5-1. Date accessed 8/10/2020.
- 11.Ioannou GN. Hepatitis B virus in the United States: infection, exposure, and immunity rates in a nationally representative survey. Ann Intern Med. 2011; 154(5):319–28. doi: 10.7326/0003-4819-154-5-201103010-00006 [DOI] [PubMed] [Google Scholar]
- 12.Roberts H, Kruszon-Moran D, Ly KN, et al. Prevalence of chronic hepatitis B virus (HBV) infection in U.S. households: National Health and Nutrition Examination Survey (NHANES), 1988–2012. Hepatology. 2016; 63(2):388–97. doi: 10.1002/hep.28109 [DOI] [PubMed] [Google Scholar]
- 13.Forde KA. Ethnic Disparities in Chronic Hepatitis B Infection: African Americans and Hispanic Americans. Curr Hepatol Rep. 2017; 16(2):105–12. doi: 10.1007/s11901-017-0348-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schweitzer A, Horn J, Mikolajczyk RT, Krause G, Ott JJ. Estimations of worldwide prevalence of chronic hepatitis B virus infection: a systematic review of data published between 1965 and 2013. Lancet. 2015; 386(10003):1546–55. doi: 10.1016/S0140-6736(15)61412-X [DOI] [PubMed] [Google Scholar]
- 15.Tohme RA, Andre-Alboth J, Tejada-Strop A, et al. Hepatitis B virus infection among pregnant women in Haiti: A cross-sectional serosurvey. J Clin Virol. 2016; 76:66–71. doi: 10.1016/j.jcv.2016.01.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jones PD, Diaz C, Wang D, Gonzalez-Diaz J, Martin P, Kobetz E. The Impact of Race on Survival After Hepatocellular Carcinoma in a Diverse American Population. Dig Dis Sci. 2018; 63(2):515–28. doi: 10.1007/s10620-017-4869-3 [DOI] [PubMed] [Google Scholar]
- 17.Hu DJ, Xing J, Tohme RA, et al. Hepatitis B testing and access to care among racial and ethnic minorities in selected communities across the United States, 2009–2010. Hepatology. 2013; 58(3):856–62. doi: 10.1002/hep.26286 [DOI] [PubMed] [Google Scholar]
- 18.Chu D, Yang JD, Lok AS, et al. Hepatitis B screening and vaccination practices in asian american primary care. Gut Liver. 2013; 7(4):450–7. doi: 10.5009/gnl.2013.7.4.450 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mitchell AE, Colvin HM, Palmer Beasley R. Institute of Medicine recommendations for the prevention and control of hepatitis B and C. Hepatology. 2010; 51(3):729–33. doi: 10.1002/hep.23561 [DOI] [PubMed] [Google Scholar]
- 20.Ma GX, Shive SE, Fang CY, et al. Knowledge, attitudes, and behaviors of hepatitis B screening and vaccination and liver cancer risks among Vietnamese Americans. J Health Care Poor Underserved. 2007; 18(1):62–73. doi: 10.1353/hpu.2007.0013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nishimura A, Shiono P, Stier D, Shallow S, Sanchez M, Huang S. Knowledge of hepatitis B risk factors and prevention practices among individuals chronically infected with hepatitis B in San Francisco, California. J Community Health. 2012; 37(1):153–8. doi: 10.1007/s10900-011-9430-2 [DOI] [PubMed] [Google Scholar]
- 22.Shah SA, Chen K, Marneni S, et al. Hepatitis B awareness and knowledge in hepatitis B surface antigen-positive parturient immigrant women from West Africa in the Bronx, New York. J Immigr Minor Health. 2015; 17(1):302–5. doi: 10.1007/s10903-013-9914-5 [DOI] [PubMed] [Google Scholar]
- 23.Shiau R, Bove F, Henne J, Zola J, Fang T, Fernyak S. Using survey results regarding hepatitis B knowledge, community awareness and testing behavior among Asians to improve the San Francisco Hep B Free campaign. J Community Health. 2012; 37(2):350–64. doi: 10.1007/s10900-011-9452-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bailey MB, Shiau R, Zola J, et al. San Francisco hep B free: a grassroots community coalition to prevent hepatitis B and liver cancer. J Community Health. 2011; 36(4):538–51. doi: 10.1007/s10900-0109339-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.https://hepfree.nyc/. Date accessed 8/10/2020. [Google Scholar]
- 26.Pollack H, Wang S, Wyatt L, et al. A comprehensive screening and treatment model for reducing disparities in hepatitis B. Health Aff (Millwood). 2011; 30(10):1974–83. doi: 10.1377/hlthaff.2011.0700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Robotin MC, George J. Community-based hepatitis B screening: what works? Hepatol Int. 2014; 8(4):478–92. doi: 10.1007/s12072-014-9562-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chandrasekar E, Song S, Johnson M, et al. A Novel Strategy to Increase Identification of African-Born People With Chronic Hepatitis B Virus Infection in the Chicago Metropolitan Area, 2012–2014. Prev Chronic Dis. 2016; 13:E118. doi: 10.5888/pcd13.160162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shankar H, Blanas D, Bichoupan K, et al. A Novel Collaborative Community-Based Hepatitis B Screening and Linkage to Care Program for African Immigrants. Clin Infect Dis. 2016; 62 Suppl 4:S289–97. doi: 10.1093/cid/ciw090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.SAHL-E Keys for Health Literacy Measurement Tools. Content last reviewed October 2014. Agency for Healthcare Research and Quality R, MD. http://www.ahrq.gov/professionals/quality-patientsafety/quality-resources/tools/literacy/sahl-e-keys.html. Date accessed 8/10/2020. [Google Scholar]
- 31.Lee SY, Stucky BD, Lee JY, Rozier RG, Bender DE. Short Assessment of Health Literacy-Spanish and English: a comparable test of health literacy for Spanish and English speakers. Health Serv Res. 2010; 45(4):1105–20. doi: 10.1111/j.1475-6773.2010.01119.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guest GN E; McKenna K How Many Focus Groups are Enough? Building and Evidence Base for Nonprobability Sample Sizes. Field Methods. 2017; 29(1):3–22. doi: 10.1177/1525822X16639015. Date accessed 8/10/2020 [DOI] [Google Scholar]
- 33.Desrosiers A, St Fleurose S. Treating Haitian patients: key cultural aspects. Am J Psychother. 2002; 56(4):508–21. doi: 10.1176/appi.psychotherapy.2002.56.4.508 [DOI] [PubMed] [Google Scholar]
- 34.Miller NL. Haitian ethnomedical systems and biomedical practitioners: directions for clinicians. J Transcult Nurs. 2000; 11(3):204–11. doi: 10.1177/104365960001100307 [DOI] [PubMed] [Google Scholar]
- 35.https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/hepatitis-b-virus-infection-screening-2014#consider. Date accessed 8/10/2020
- 36.Jemal A, Fedewa SA. Prevalence of hepatitis C virus testing in cohorts born between 1945 and 1965 in the U.S. Am J Prev Med. 2015; 48(5):e7–9. doi: 10.1016/j.amepre.2014.12.002 [DOI] [PubMed] [Google Scholar]
- 37.Thompson MJ, Taylor VM, Jackson JC, et al. Hepatitis B knowledge and practices among Chinese American women in Seattle, Washington. J Cancer Educ. 2002; 17(4):222–6. doi: 10.1080/08858190209528842 [DOI] [PubMed] [Google Scholar]
- 38.Walters J, Sullivan A. Early Identification and Linkage to Care of Foreign-Born People with Chronic Hepatitis B Virus Infection, Multnomah County, Oregon, 2012–2014. Public Health Rep. 2016; 131 Suppl 2:105–11. doi: 10.1177/00333549161310S216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.https://www.census.gov/quickfacts/fact/table/miamidadecountyflorida/PST045218. Date accessed 8/10/2020.
- 40.Davies J, Bukulatjpi S, Sharma S, Davis J, Johnston V. “Only your blood can tell the story”--a qualitative research study using semi-structured interviews to explore the hepatitis B related knowledge, perceptions and experiences of remote dwelling Indigenous Australians and their health care providers in northern Australia. BMC Public Health. 2014; 14:1233. doi: 10.1186/1471-2458-14-1233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Blanas DA, Nichols K, Bekele M, et al. Adapting the Andersen model to a francophone West African immigrant population: hepatitis B screening and linkage to care in New York City. J Community Health. 2015; 40(1):175–84. doi: 10.1007/s10900-014-9916-9 [DOI] [PubMed] [Google Scholar]
- 42.https://www.census.gov/content/dam/Census/library/publications/2018/demo/p60-264.pdf. Date accessed 8/10/2020.
- 43.https://www.census.gov/quickfacts/fact/table/miamidadecountyflorida/POP060210. Date accessed 8/10/2020.
- 44.https://www.nbcnews.com/news/asian-america/documentary-be-about-it-pushes-asian-americancommunity-talk-about-n576546. Date accessed 8/10/2020
- 45.https://www.hhs.gov/sites/default/files/National%20Viral%20Hepatitis%20Action%20Plan%202017-2020.pdf. Date accessed 8/10/2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.