Abstract
Background
Several measurements have been used to predict the success of weaning from mechanical ventilation; however, their efficacy varies in different studies. In recent years, diaphragmatic ultrasound has been used for this purpose. We conducted a systematic review and meta-analysis to evaluate the effectiveness of diaphragmatic ultrasound in predicting the success of weaning from mechanical ventilation.
Methods
Two investigators independently searched PUBMED, TRIP, EMBASE, COCHRANE, SCIENCE DIRECT, and LILACS for articles published between January 2016 and July 2022. The methodological quality of the studies was assessed using the Quality Assessment of Diagnostic Accuracy Studies-2 tool; additionally, the certainty of the evidence is evaluated using the GRADE (Grading of Recommendations Assessment, Development, and Evaluation) methodology. Sensitivity and specificity analysis was performed for diaphragmatic excursion and diaphragmatic thickening fraction; positive and negative likelihood ratios and diagnostic odds ratios (DOR) with their confidence intervals (95% CI) were calculated by random effects analysis, summary receiver operating characteristic curve was estimated. Sources of heterogeneity were explored by subgroup analysis and bivariate meta-regression.
Results
Twenty-six studies were included, of which 19 were included in the meta-analysis (1204 patients). For diaphragmatic excursion, sensitivity was 0.80 (95% CI 0.77–0.83), specificity 0.80 (95% CI 0.75–0.84), area under the summary receiver operating characteristic curve 0.87 and DOR 17.1 (95% CI 10.2–28.6). For the thickening fraction, sensitivity was 0.85 (95% CI 0.82–0.87), specificity 0.75 (95% CI 0.69–0.80), area under the summary receiver operating characteristic curve 0.87 and DOR 17.2 (95% CI 9.16–32.3). There was heterogeneity among the included studies. When performing a subgroup analysis and excluding studies with atypical cutoff values, sensitivity and specificity increased for diaphragmatic thickening fraction; sensitivity increased and specificity decreased for diaphragmatic excursion; when comparing studies using pressure support (PS) versus T-tube, there was no significant difference in sensitivity and specificity; bivariate meta-regression analysis shows that patient position at the time of testing was a factor of heterogeneity in the included studies.
Conclusions
Measurement of diaphragmatic excursion and diaphragmatic thickening fraction predict the probability of successful weaning from mechanical ventilation with satisfactory diagnostic accuracy; however, significant heterogeneity was evident in the different included studies. Studies of high methodological quality in specific subgroups of patients in intensive care units are needed to evaluate the role of diaphragmatic ultrasound as a predictor of weaning from mechanical ventilation.
Supplementary Information
The online version contains supplementary material available at 10.1186/s13054-023-04430-9.
Keywords: Diaphragm, Ultrasonography, Diagnostic imaging, Weaning, Mechanical ventilation, Airway extubation
Background
The process of weaning from mechanical ventilation remains one of the most critical challenges in patients undergoing mechanical ventilation in the intensive care unit (ICU) [1]; the multidisciplinary team must study the optimal time for weaning from the mechanical ventilator as premature weaning may lead to weaning failure and thus increase the risk of hospital acquired infections, costs in care, ICU length of stay, hospital length of stay and diaphragmatic dysfunction [2, 3].
Current guidelines recommend several indices applied at the bedside to predict successful weaning from mechanical ventilation. However, they have yet to prove ideal [4], probably due to the heterogeneity of critically ill patients, which limits the predictive ability of these indices in different patient subgroups [5]. A spontaneous breathing trial (SBT) is an appropriate way to prepare the patient for extubation [6]; however, even after successful SBT, failure rates and subsequent reintubation can exceed 20% in the highest-risk patients [7].
Patients on mechanical ventilation may have a multifactorial deterioration of diaphragmatic function that can lead to weaning failure and prolongation of invasive mechanical ventilation [8, 9]; therefore, assessing diaphragmatic function could help predict the patient's ability to maintain spontaneous breathing over time [10].
The use of diaphragmatic ultrasound in the intensive care unit is a technique of growing interest due to its portability, speed, and safety. Its use allows reporting on the structural and functional status of the diaphragm and can predict the probability of successful mechanical ventilator weaning [11]. Although some studies have demonstrated the usefulness of ultrasound in predicting the success of mechanical ventilator weaning, others have shown controversial results that continue to motivate continued research of this technique. This systematic review and meta-analysis aim to compile the best available evidence to elucidate the effectiveness of diaphragmatic ultrasound as a predictor of successful weaning from the mechanical ventilation.
Materials and methods
Search for studies
A systematic review and meta-analysis of observational studies involving intubated patients connected to mechanical ventilation who underwent uni- or bilateral diaphragmatic ultrasound to assess diaphragm function prior to extubation was performed to identify whether there is an association between diaphragm function and extubation success. The systematic review protocol was registered in the Prospective International Register of Systematic Reviews (PROSPERO) CRD42022316349 database, and the systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Two investigators conducted independent systematic literature searches of PUBMED, TRIP, EMBASE, COCHRANE, SCIENCE DIRECT, and LILACS databases published between January 2016 through July 2022, discrepancies between the two investigators were resolved with the intervention of a third investigator. The terms diaphragm, diagnostic imaging, ultrasound, weaning, mechanical ventilation, extubation, ultrasonography, and articles in all languages were included.
Methodological quality assessment was performed independently by two investigators using the Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2) instrument, followed by the kappa coefficient to assess inter-investigator agreement; additionally, the certainty of the evidence is evaluated using the GRADE (Grading of Recommendations Assessment, Development, and Evaluation) methodology.
Selection criteria and outcome measures
The meta-analysis included studies published between 2016 and 2022, and weaning success was defined as maintaining spontaneous breathing for the next 48 h after extubation.
Inclusion criteria
Prospective or retrospective observational studies involving adult patients with more than 24 h of invasive mechanical ventilation in whom uni- or bilateral diaphragmatic ultrasound was performed during spontaneous breathing trial.
Exclusion criteria
Non-primary studies, studies with less than 20 participants, patients with neuromuscular disease, studies in pregnant patients, case reports, animal studies, and editorials.
Statistical analysis
Rev Man 5.4 the Cochrane Collaboration (2014) software was used for bias assessment, and Metadisc software (Hospital Ramón Y Cajal, Madrid, Spain) for meta-analysis [12]. Independent analyses were performed for diaphragm excursion (DE) and diaphragm thickening fraction (DTF); likewise, an independent analysis of the results according to hemi-diaphragm was assessed; weaning success was defined as the absence of disease in the 2 × 2 table. Sensitivity and specificity analysis was performed for the studies that evaluated DE and DTF, positive and negative likelihood ratios, and diagnostic odds ratios with their respective 95% confidence intervals (CI). A statistically significant value of P < 0.05 was considered.
Summary receiver operator characteristic curves (SROC) and area under the summary curve (AUSROC) were created to assess the accuracy of DE and DTF for predicting extubation success [13]. Publication bias was assessed using the funnel plot and Egger's statistic [14].
The Cochrane Q and I2 tests assessed heterogeneity, and the source of heterogeneity was assessed by meta-regression analysis and a subgroup analysis on both sensitivity and specificity. Study characteristics that could cause uncertainty related to the diagnostic accuracy of diaphragm ultrasound were examined; for example, the cutoff values used as a reference, the risk of bias assessed concerning index test and flow and times, the type of spontaneous breathing trial (pressure support (PS) or T-piece), the homogeneity versus heterogeneity of age, the prevalence of success, and the position of the patient. In addition, an analysis was performed to identify whether the cause of the requirement for mechanical ventilation could influence the diagnostic performance of ultrasound.
Results
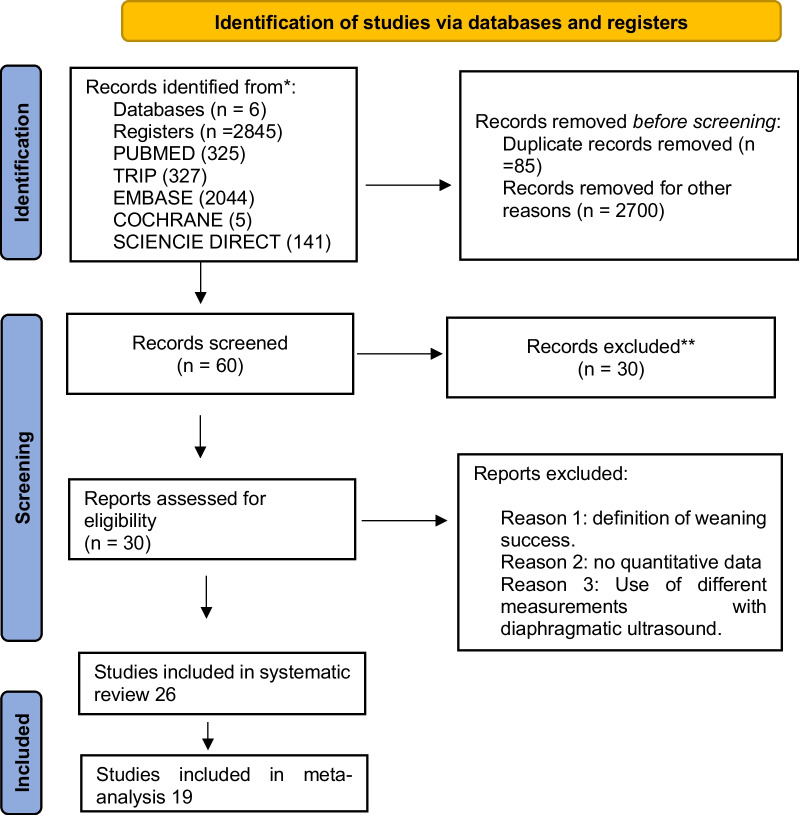
In the initial search, 2845 articles were obtained in six databases, 85 duplicates and 2700 articles were eliminated by titles and abstracts, leaving 60 articles; subsequently, the full-text reading proceeded, eliminating 34 articles. (The detailed flow diagram is shown in Fig. 1.)
Fig. 1.
Study selection flowchart
Twenty-six studies were included in the qualitative analysis of which 19 were included in the quantitative analysis. The meta-analysis included 1204 subjects, of whom 908 had DE assessment, and 945 had DTF assessment; in several studies, both DE and DTF were measured.
Characteristics of the included studies
The different characteristics of the studies in the systematic review are listed in Table 1. Most of the studies were of the prospective cohort type, with the exception of [15], a retrospective observational study, and [16], a prospective randomized clinical trial.
Table 1.
Studies included in the systematic review and meta-analysis
| Autors | Country | Year | Design | n | Age | Reason for mechanical ventilation | Prevalence of success | Patient position during US | Cut-off success weaning | MV duration at inclusion (hours) | Evaluated Diaphragm | Mode/ sound | Tipe SBT | Weaning success definition |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Jung B, et al | France | 2016 | Prospective cohort | 40 | 58 (51–67) | ARF 65% | 50% | 20 a 30° | DTF ≥ 30% | > 48 h | Left and right | Not described | PS /T-tube | No reintubation or tracheostomy > 48 h after extubation |
| Blumhof et al | USA | 2016 | Prospective cohort | 56 | 62 ± 17 | ARF 73% | 86.5% | Semi-recumbent 20–40° | DTF > 20% | > 24 h | Right | Mode B 7,5–10 MHz | PS | Spontaneous respiration > 48 h after extubation |
| Mariani Lf et al | France | 2016 | Prospective cohort | 34 | 646 ± 14.8 | Multicausal COPD 26% | 100% | Semi-recumbent 30° | DE left _ > 11 mm ED right ≥ 10 mm | MV > 7 days | Left and right | 3–5 MHz/ Mode M | T-tube | Spontaneous respiration > 72 h after extubation |
| Flevari et al | Greece | 2016 | Prospective cohort | 27 | 65 | Multicausal | Not described | Supine | DE right > 10 mm > 7 mm left | Not described | Left and right | 5 MHz Mode B/ M | T-tube | SBT success, no reintubation or NIV > 48 h after extubation |
| Hayat et al | Pakistan | 2017 | Prospective observational | 100 | 40.5 | Respiratory disease 73% | 76% | Supine | DE > 1.2 cm | Not described | Left and right | 3.5 MHz/not described | Not described | Success in the next 48 h without the need for NIV or reintubation |
| Huang et al | China | 2017 | Prospective observational | 40 | 84.25 ± 7.07 | Multicausal COPD 52.5% | 30% | Semi-incorporated | DE > 10 mm | > 48 h | Left and right | 1.5 MHZ/ Mode M | T-tube | Unassisted respiration > 48 h |
| Farghaly et al | Egypt | 2017 | Prospective observational | 54 | Success group 65 (55–67.8) Failure group 62.5 (55–70.7) | Respiratory disease unspecified | 74% | Semi-recumbent | DE ≥ 10.5 mm, Tdi ≥ 21 mm end inspiration, ≥ 10.5 mm Tdi end expiration, DTF ≥ 34.2% | Not described | Right | 3.5 MHZ/Mode B | PS | Spontaneous respiration > 48 h after extubation |
| Osman et al | Egypt | 2017 | Prospective observational | 68 | 56 (45–65) | Major surgery | 73.5% | Semi-recumbent | DE > 10 mm DTF > 28% | Not described | Left and right | 3.5 y 9–11 MHZ Mode M | T-tube | Spontaneous respiration > 48 h after extubation |
| Dres et al | France | 2018 | Prospective cohort | 76 | 58 (48–68) | Multicausal ARF 40% | 43.5% | Semi-incorporated | Contraction pressure > 7.2 cmH2O, DTF 25.8% | > 24 h | Left and right | 4–12/Mode M | PS | Spontaneous respiration > 48 h after extubation |
| Yoo et al | Corea | 2018 | Prospective observational | 60 | 69.5 (57.5–76) | Multicausal COPD 23.3% | 78.3% | Not described | DE ≥ 1 cm and Δtdi ≥ 20% | > 48 h | Right | 2–5; 6–13 /Mode M/ B | PS /T-tube | Success > 48 h without requiring NIV |
| Pirompanich et al | Thailand | 2018 | Prospective cohort | 34 | 66.5 (± 13.5) | Multicausal COPD/ asthma 5.9% | 73.5% | Semi-incorporated | DTF right ≥ 26% | > 24 h | Left and right | Lineal 10 MHZ/mode B/ M | T-tube | Spontaneous respiration > 48 h after extubation |
| Palkar et al | Norway | 2018 | Prospective cohort | 73 | 71 | Multicausal COPD/ asthma 21.9% | 72.6% | Semi-recumbent 20–40° | Excursion-time index > 3.8% | > 24 h | Right | 3.5 MHZ/Mode M | PS | Spontaneous respiration > 48 h after extubation |
| Tenza Lozano | Spain | 2018 | Prospective cohort | 69 | 66 (53–78) | Multicausal respiratory disease 34.8% | 63.7% | Semi-recumbent 20 a 40° | DTF > 24% | > 24 h | Right | Lineal 7 a 10 MHZ/ mode B/ M | PS/T-tube | Spontaneous respiration > 48 h after extubation |
| Theerawit et al | Thailand | 2018 | Prospective cross-sectional | 62 | 66.48 (± 16,7) | Multicausal respiratory disease 19.3% | 82.2% | Supine | DE > 12.85 mm | > 48 h | Left and right | 1–5 MHZ/Mode B/ M | PS/T-tube | Spontaneous respiration > 48 h after extubation |
| Mowafy et al | Egypt | 2019 | Prospective randomized clinical trial | 106 | Group I 35.83(± 9.46) Group II 35.77(± 9.56) | Polytrauma | 68.9% | Semi-recumbent 30 a 40° | DRSBI > 1.6 | > 48 h | Right | 2–5 MHZ Mode B/ M | PS | Spontaneous respiration > 48 h after extubation |
| Vivier et al | France | 2019 | Prospective multicenter | 191 | 68 (±) | Respiratory disease 40% | 83% | Not described | DE > 10 mm and DTF > 30% | vm > 7 days | Left and right | Lineal 4 y 10 MHZ Mode M | T-tube | Reintubation failure or death within 7 days after extubation |
| Varon et al | Colombia | 2019 | Prospective observational | 84 | 58(35–51) | HRF 25% | 79.8% | Semi-incorporated 45° | DC velocity > 2.9 cm/s in the SG; > 2.02 cm/s in the FG | > 48 h | Right | 1–5 y 6–13 MHZ Mode M | PS/T-tube | Spontaneous respiration > 48 h after extubation |
| Soliman et al | Egypt | 2019 | Prospective observational | 100 | 57.1 (± 14.5) | ARF unspecified 62% | 80% | Not described | DTF > 29.5% | > 24 h | Left and right | Lineal 10 MHZ/Mode B/ M | PS | Success of SBT, no reintubation or death > 48 h |
| Eltrabili et al | Egypt | 2019 | Prospective observational | 30 | Success 52.7 (± 13.4) Failure 51.4 (± 13.1) | Abdominal sepsis | 56.6% | Semi-recumbent | DTF > 30.7% and DE > 10.4 mm | > 48 h | Left and right | 7.5-10MHZ Mode B/ M | PS | Successful spontaneous breathing and no use of NIV > 48 h after extubation |
| Abdelwahed et al | Egypt | 2019 | Prospective observational | 65 | Success 43.49 ± 12.88 Failure 40.85 ± 14.28 | Multicausal respiratory disease 16.98% | 78.4% | Semi-incorporated 30–45° | DTF > 30% | Not described | Left and right | 10–15 MHZ Mode B/ M | T-tube | Spontaneous respiration > 48 h after extubation |
| Elshazly et al | Egypt | 2020 | Prospective observational | 62 | Success 65 (55–70) Failure 60.5 (52.2–70) | Respiratory disease COPD 24% | 54.8% | Semi-incorporated | DE > 1.25 cm and DTF > 21.5% | > 24 h | Left and right | 3.5 y 7–12 MHZ Mode B/ M | Not described | Spontaneous respiration > 48 h after extubation |
| Fossat et al | France | 2021 | Single-center prospective observational | 100 | 66(± 15) | Multicausal COPD 14% | 91% | Not described | RSBI and RSBI/DE had a value of 0.50 either at minute 5 and 0.55 at minute 25 of SBT to predict success | > 24 h | Right | 5MHZ/Mode M | PS | Spontaneous respiration > 72 h after extubation |
| Shigang Li et al | China | 2021 | Prospective observational | 101 | > 65 | Multicausal COPD 10% | 68.3% | Not described | DTF ≥ 30%, DE ≥ 1.3 cm | > 24 h | Left and right | 2–5, 5–13 MHZ/Mode B/ M | T-tube | No reintubation, NIV or tracheostomy > 48 h after extubation |
| Funda Gok et al | Turkey | 2021 | Prospective observational | 62 | 57.6 (± 14.1) | Polytrauma 77% | 64% | Not described | DTF > 27.5% DE > 1.3 cm | > 48 h | Right | 2–4 MHZ/Mode M | T-tube | SBT success, no reintubation, no NIV > 48 h post-extubation |
| Alam M et al | Bangladesh | 2022 | Prospective observational | 31 | 42 (± 16) | Multicausal COPD 32% | 58% | Semi-recumbent 20–40° | DE ≥ 11.43 mm DTF 19.77% | > 11 days | Right | 2–4-13 MHZ/Mode B/ M | T-tube | Spontaneous respiration > 48 h after extubation |
| Mawla et al | Egypt | 2022 | Prospective cohort | 90 | 18–97 | Respiratory disease COPD 36.7% | 56.6% | Semi-recumbent | DE 1.3 cm DTF 13.5%, contraction velocity > 0.95 cm/s and relaxation rate 0.7 cm/sg | > 48 h | Right | Mode B 9 MHZ/M 4MHZ | PS | Spontaneous respiration > 48 h after extubation |
From: Effectiveness of diaphragmatic ultrasound as a predictor of successful weaning from mechanical ventilation: a systematic review and meta-analysis
DRSBI rapid and shallow diaphragmatic breathing rate, DE diaphragmatic excursion, DTF diaphragm thickening fraction, VM mechanical ventilation, PS pressure support, SBT spontaneous breathing trial, NIV noninvasive ventilation, US ultrasound, SG success group, FG failure group, MHZ megahertz, TDi diaphragmatic thickness, DC Diaphragmatic contraction, ARF Acute respiratory failure, COPD chronic obstructive pulmonary disease, HRF hypoxemic respiratory failure
Those studies published between 2016 and 2022 were conducted in different countries such as eight from Egypt [1, 2, 16–21]; one from the USA [22]; five from France [10, 23–26]; one from Greece [27]; one from Pakistan [28]; two from China [29, 30]; one from Korea [15]; two from Thailand [31, 32]; one from Spain [33]; one from Norway [34]; one from Colombia [35]; one from Turkey [36]; one from Bangladesh [37].
Twelve studies evaluated DTF and DE [1, 2, 10, 15, 17, 20, 21, 26, 30, 35-37]; five studies evaluated only DE [24, 27–29, 32]; six studies evaluated only DTF [18, 19, 22, 23, 31, 33]; one study measured index excursion time [34]; two studies measured diaphragmatic rapid shallow breathing index (DRSBI) [10, 16]; and two studies measured contraction velocity [21, 35]. Most studies evaluated both diaphragms (57.7%), and 11 studies evaluated only the right diaphragm (42%).
Ultrasound measurements were performed in different positions, the most prevalent being semi-sitting from 20 to 45° reported in 16 studies [1, 2, 16, 17, 19–24, 24, 25, 31, 33, 35, 37]; three studies performed the measurement in a supine position [27, 28, 32], and six studies did not report the patient position [10, 15, 18, 26, 30, 36].
There was a variation of 24 to 48 h in the minimum duration of mechanical ventilation prior to inclusion in the studies; five studies did not describe the time on mechanical ventilation prior to the start of weaning; in one study, the duration of mechanical ventilation prior to inclusion was 11 days [37]; in two studies, it was seven days [24, 26]. Exclusion criteria for most studies were conditions affecting diaphragm function, predominantly phrenic nerve injury.
Different definitions of weaning were identified. Successful weaning was defined as the patient's ability to maintain spontaneous breathing within 48 h after extubation without requiring invasive or noninvasive ventilatory support or performance of tracheostomy. Failure of extubation was defined in most studies as the inability to maintain spontaneous breathing within 48 h after extubation with a requirement of noninvasive ventilation, high-flow nasal cannula, reintubation, or tracheostomy.
Regarding the weaning protocol, in all studies, patients were prepared by a spontaneous breathing trial, which was performed with pressure support (PS inspiratory pressure = 5–8 cmH2O and PEEP = 0–5 cmH2O) [1, 2, 10, 16, 18, 22, 25, 34], or using the T-tube [17, 19, 20, 24, 26, 30, 36, 37], some studies combined PS and T-tube [15, 23, 27, 29, 32, 33, 35], and two studies did not record the spontaneous breathing trial method [20, 28].
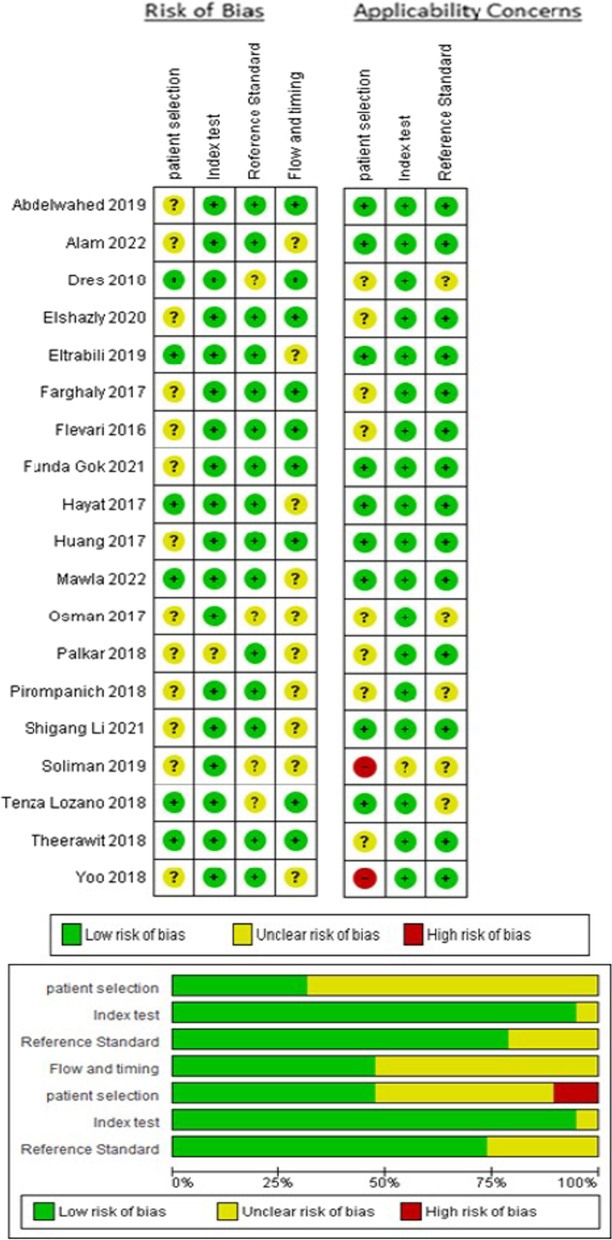
Evaluation of methodological quality
The results of the risk of bias assessment for the studies included in the meta-analysis are shown in Fig. 2. There was agreement among the authors Cohen's Kappa 0.67 (95% CI 0.54–0.73); in 68% of the studies, there was the unclear risk of bias regarding patient selection, in 5.2% of the studies, there is an unclear risk of bias regarding the index test, in 21% of the studies, there is an unclear risk of bias regarding the standard reference, and 53% in flow and timing; regarding applicability concerns in two studies (10.5%), there was severe concern regarding patient selection [15, 18] unclear concern in one (5.2%) study regarding the index test [18] and in five (26.3%) studies regarding the standard reference [17, 18, 25, 31, 33]. The evaluation of the certainty of the articles included in the meta-analysis shows a moderate accuracy of the test (diaphragmatic ultrasound) (see Additional file 1: Table S1).
Fig. 2.
Risk of bias and applicability issues with Quality Assessment of Diagnostic Accuracy Studies (QUADAS)
In most studies, diaphragmatic ultrasonography was performed during the spontaneous breathing trial with a variation of the exact timing of the test, and in other studies, diaphragmatic ultrasonography was performed before and after extubation. Most studies did not clearly report the elapsed time between diaphragmatic ultrasound and extubation [2, 17–21, 25, 27, 28, 33, 34].
The method of patient selection was not reported in most studies. Several studies did not present the flowchart explaining in detail the patient selection and follow-up [1, 15, 17, 18, 21, 28, 30, 31, 35, 37].
The outcome of weaning varied according to the definition of extubation success or failure and, in some studies, needed to be clearly defined. In most of the included studies, the index test (ultrasound of the diaphragm) was interpreted without knowing the outcome of weaning.
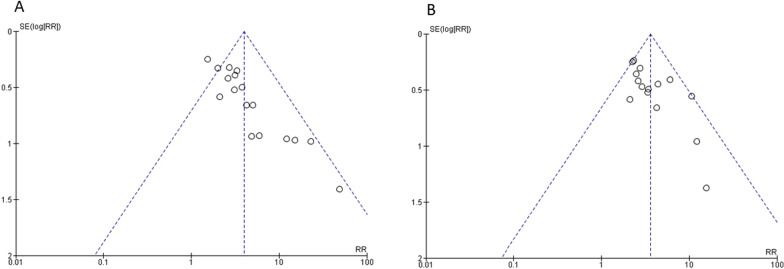
No publication bias is evident for the studies that analyzed DE, funnel plot (see Fig. 3), and Egger's test 0.75, nor for those that analyzed the DTF Egger's test 0.73. (Additional file 1: Fig. S1).
Fig. 3.
Funnel plot for diaphragmatic excursion (A) and diaphragm thickening fraction (B)
Heterogeneity of studies
Nineteen studies were included in the meta-analysis [1, 2, 15, 17–21, 25, 27-34, 36, 37], and seven studies were excluded from the meta-analysis. After all, their definition of success did not include the ability to maintain spontaneous breathing for 48 h after extubation, because they used other ultrasound measurements and because they did not present accurate data for quantitative analysis.
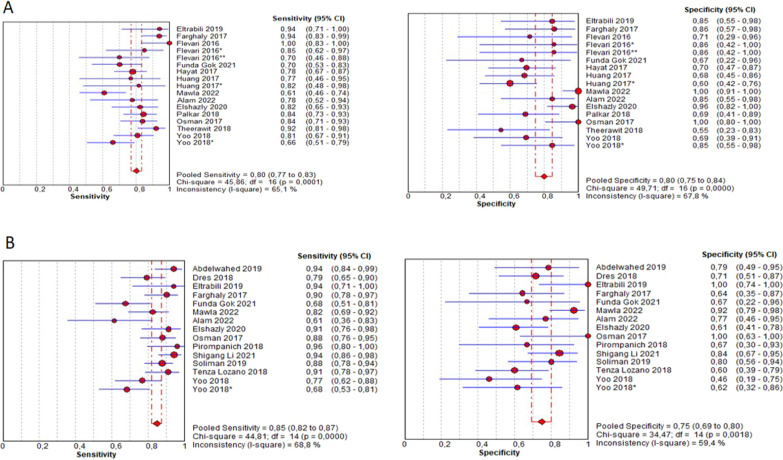
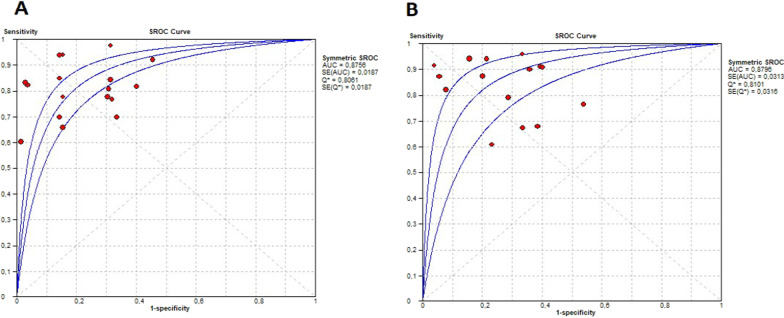
Figure 4 presents the forest plot of sensitivity 0.80 (95% CI 0.77–0.83) and specificity 0.80 (95% CI 0.75–0.84) for DE and sensitivity 0.85 (95% CI 0.82–0.87) and specificity 0.75 (95% CI 0.69–0.80) for the DTF; Fig. 5 shows the SROC curve illustrating the summary point and the estimation of the sensitivity and specificity of each of the studies; also, the prediction contours with 95% CI and for DE AUSROC 0.87 and DTF AUSROC 0.87. The likelihood ratios obtained in the bivariate analysis for DE were L.R. (+) 4.64 (95% CI 4.19–5.0) L.R. (-) 0.21 (95% CI − 0.08–0.5) and for DTF L.R. (+) 3.5 (95% CI 3.19–3.84) LR (−) 0.18 (95% CI − 0.17–0.54) (see Additional file 1: Table S2).
Fig. 4.
Forest plot of sensitivity and specificity (A) Diaphragmatic excursion. B Diaphragmatic thickening fraction. Flevari DE left > 10 mm*, **DE right < 10 mm; Huang*DE right; Yoo*DE ≥ 1.4 cm, DTF > 30%
Fig. 5.
SROC curves of sensitivity and specificity (A) diaphragmatic excursion (B) diaphragmatic thickening fraction
Additional file 1: Fig. S2 shows the forest plot for the diagnostic odds ratio (DOR) for DE 17.1 (95% CI 10.2–28.6) and for DTF 17.2 (95% CI 9.16–32.3). Heterogeneity was evidenced in the sensitivity and specificity for DE (I2 65.1% Chi-square 45.86 P 0.001; I2 67.8% Chi-square 49.7 P 0.001, respectively) and for DTF (I2 68.8% Chi-square 44.8 P 0.001; I2 59.4% Chi-square 34.4 P 0.001); the threshold effect measure was evaluated by Spearman correlation, obtaining a value of 0.125 (P 0.63) for DE and − 0.198 (P 0.47) for DTF.
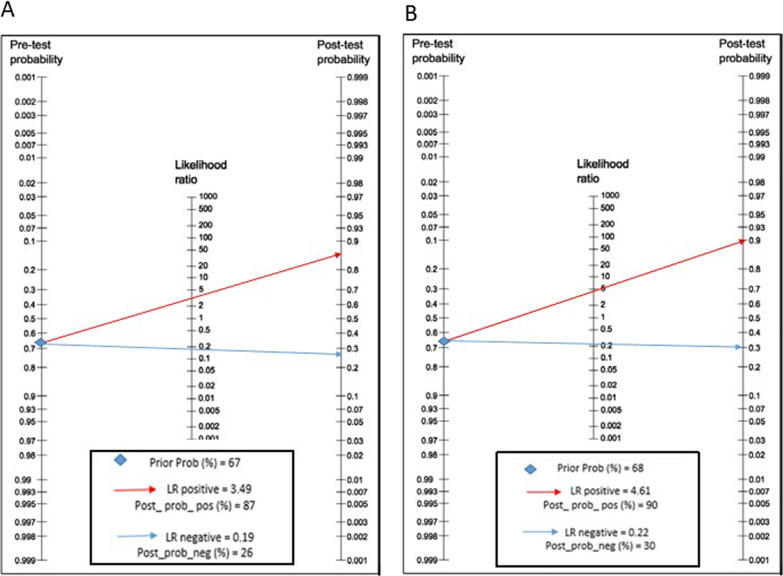
A Fagan nomogram was constructed to illustrate diaphragm ultrasonography's pre- and post-test probability of predicting extubation success (Fig. 6). The pretest probability of ultrasonography predicting successful extubation was 67% for DE and 68% for positive DTF (above the cutoff point); the post-test probability for DE and DTF was 87% and 90%, respectively. The post-test probability of successful extubation for negative DE (below the cutoff point) was reduced to 26%, and for thickening, the DTF was reduced to 30%, respectively.
Fig. 6.
Fagan's nomogram for diaphragmatic excursion (A) and diaphragmatic thickening fraction (B)
Subgroup analysis and meta-regression
After eliminating studies with outlier DTF cutoff values [15, 20, 37], sensitivity increased to 0.86 (CI 0.83–0.89 I2 68.5% Chi2 34.9 P 0.002) with no changes in heterogeneity; specificity increased to 0.78 (0.72–0.83 I2 56.9% Chi2 25.5 P 0.01), with decreasing heterogeneity, and AUSROC increased to 0.90; continuing with the manual analysis by subgroups, studies with atypical values of sensitivity [15, 21] and specificity [32] for the DE were eliminated, showing an increase in sensitivity to 0.83 (95% CI 0.79–0.86) with a decrease in heterogeneity (I2 43.9%, Chi2 23.1 P 0.03); and decreased specificity to 0.77 (95% CI 0.71–0.83); likewise, decreased heterogeneity (I2 52.9%, chi2 27.5 P 0.01); the AUSROC increased to 0.88 (see Additional file 1: Fig. S3).
The exclusion of studies that presented a high risk of applicability according to the QUADAS 2 evaluation [15, 18] was performed, showing an increase in sensitivity to 0.87 (I2 66% Chi2 32.4 P 0.006) and specificity to 0.77 (I2 60% Chi2 27.7 P 0.003) without significant changes in the heterogeneity for DTF; concerning DE, there is an increase in sensitivity to 0.82 (I2 60% chi2 40 P 0.003) with no change in heterogeneity, no change in specificity for diaphragmatic excursion; the AUSROC was modified to 0.88 for a diaphragmatic excursion and 0.89 for DTF (see Additional file 1: Fig. S4).
A subgroup analysis was performed to evaluate whether the cause for which mechanical ventilation was required affects the diagnostic performance of ultrasound, eliminating studies where the main cause was not respiratory; there was no increase in sensitivity and specificity for DE 0.80 and 0.79, respectively, and AUSROC 0.86; similarly, there was no increase in sensitivity and specificity for thickening fraction 0.85 and 0.73, respectively, and AUSROC 0.86 (see Additional file 1: Fig. S5).
Finally, a subgroup analysis was performed for studies using PS and T-tube during the spontaneous breathing trial, with no evidence of statistically significant changes in sensitivity and specificity for DE and DTF (see Additional file 1: Fig. S6).
The meta regression analysis was performed, exploring possible sources of heterogeneity such as age, the prevalence of success, and patient position during the index test (diaphragmatic ultrasound); it was evidenced that patient position was a cause of heterogeneity for the diagnostic accuracy of the diaphragmatic thickening fraction in the studies included in the meta-analysis (coefficient of − 1,99 P = 0.012 DOR 0.14 CI 95% 0.03–0.6) (see Additional file 1: Table S3); no statistically significant differences were found between the age of patients who successfully weaned from mechanical ventilation and those who failed; likewise, there was no evidence that the prevalence of success was a source of heterogeneity.
Discussion
The results of this study suggest adequate accuracy of diaphragmatic ultrasound in predicting weaning success; the combined sensitivity and specificity of DE and the AUSROC were 0.85, 0.75, 0.87, respectively, and for DTF 0.80, 0.80, 0.87. Our data show a satisfactory diagnostic accuracy for predicting extubation success. It is relevant to report that there was heterogeneity in the sensitivity and specificity of the studies included in the meta-analysis; likewise, several studies presented significant methodological weaknesses, two studies with a high risk of applicability in patient selection, and several studies with unclear risk of bias in patient selection, flow and timing.
During the last few years, some systematic reviews and meta-analyses have been published on the usefulness of diaphragmatic ultrasound in predicting the success or failure of weaning in patients undergoing mechanical ventilation [38–41]. The results of our study are consistent with most of the previously mentioned published studies. Li et al. evidenced in their study a satisfactory diagnostic accuracy in predicting the outcome of extubation; Llamas Alvarez concluded that DTF is by itself a modest predictor of weaning outcome; Garcia Sanchez et al. concluded that ultrasound dysfunction of the diaphragm is associated with an increased risk of extubation failure; Le Neindre et al. demonstrate that low values of diaphragmatic excursion and diaphragmatic thickening fraction predict the risk of extubation failure with moderate to high specificity.
This research included five new studies compared to the previous meta-analysis [41] that mainly analyzed DE and DTF, which allowed the number of subjects studied to be increased to 1204; likewise, an exhaustive subgroup analysis was performed to find sources of heterogeneity in the sensitivity and specificity of diaphragmatic excursion and diaphragmatic thickening fraction that could affect the ability of diaphragmatic ultrasound to predict extubation success, finding mainly factors such as cutoff values or atypical thresholds for each of the measurements and the risk of applicability found in the quality assessment of the studies; likewise, a bivariate meta-regression analysis was performed, finding the patient's position at the time of the test as the primary source of heterogeneity.
The high sensitivity values reported in the present study indicate that patients with values above approximately 29% for DTF and > 1 cm for DE have a high probability of successful extubation; however, it is essential to mention that weaning success may be influenced by additional factors such as nutritional status, respiratory and cardiovascular integrity and psychological conditions to mention a few [42].
We can evidence in the limitations of this study; the possible biases that may contain each of the studies included in the meta-analysis as randomized trials were not included; the absence of a common reference value for diaphragmatic thickening and excursion fraction may introduce biases that cause measurement imprecision; sex was not considered in the analysis by subgroups, nor the time on mechanical ventilation before the spontaneous breathing trial and ultrasound measurement; and these could influence the ultrasound result.
In contrast to the findings of this meta-analysis, the two studies mentioned here found no association between values below the cutoff point of diaphragmatic excursion and thickening fraction measured with ultrasound and the outcome of weaning from mechanical ventilation [24, 26]. Mariani et al. defined extubation failure as the need for intubation within 72 h after extubation, and Vivier et al. defined extubation failure as the need for intubation or death seven days after extubation, which differs from our investigation since the studies included in this meta-analysis evaluated extubation success 48 h after mechanical ventilator weaning.
Slight variations in the measurement between observers may affect the measurement result and cause heterogeneity; it is undoubtedly an observer-dependent technique; despite this, several studies have concluded that diaphragmatic ultrasound measurements are reproducible.
The results of this study have implications for clinical practice, showing that diaphragmatic ultrasound is a technique that can be used in the intensive care unit during the spontaneous breathing trial to contribute to objectively predict the success of weaning from mechanical ventilation; it is a portable, fast, noninvasive, simple and safe technique that does not emit any ionizing radiation that affects health-care personnel; However, given the high heterogeneity found, which is frequent in meta-analyses of diagnostic tests, the results of the pooled measurements should be interpreted with caution, especially in the different subgroups of critically ill patients, in order to achieve a personalized determination of the optimal result.
Therefore, access to diaphragmatic ultrasound in the intensive care unit should be generalized, and priority should be given to achieving its universal use, especially in routine respiratory monitoring, to guide the management of patients undergoing mechanical ventilation.
Conclusions
The results of this systematic review and meta-analysis show that measurement of diaphragmatic excursion and diaphragmatic thickening fraction predict the probability of successful weaning from mechanical ventilation with satisfactory diagnostic accuracy; however, significant heterogeneity was evident in the different included studies. Studies of high methodological quality in specific subgroups in intensive care unit patients are needed to evaluate the role of diaphragmatic ultrasound as a predictor of weaning from mechanical ventilation.
Supplementary Information
Additional file 1. Search strategy, supplemental Tables, and supplemental Figures.
Acknowledgements
None
Abbreviations
- ICU
Intensive care unit
- SBT
Spontaneous breathing trial
- QUADAS-2
Quality Assessment of Diagnostic Accuracy Studies-2
- SROC
Summary receiver operator characteristic curve
- AUSROC
Area under the summary receiver operator characteristic curve
- DE
Diaphragmatic excursion
- DTF
Diaphragmatic thickening fraction
- PS
Pressure support
- DRSBI
Diaphragmatic rapid shallow breathing index
- PEEP
Positive end-expiratory pressure
Author contributions
HMP, DMF and JRM were the main contributors regarding conceptualization, methodology, analysis and interpretation of the data, as well as writing, editing and visualizing the manuscript. VHN and WAA critically revised the statistical methods. ARM was the supervisor and administrator of the project. ALT and PPT made substantial contributions to the editing and revision of the manuscript. All authors read and approved the final manuscript.
Funding
None.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Eltrabili H, Husain A, Silliman M, Lofty A, Hammy W, Mukhtar A. Evaluation of diaphragmatic ultrasound indices as predictors of successful liberation from mechanical ventilation in subjects with abdominal sepsis. Respir Care. 2019;64(5):564–569. doi: 10.4187/respcare.06391. [DOI] [PubMed] [Google Scholar]
- 2.Farghaly S, Hasan A. Diaphragm ultrasound as a new method to predict extubation outcome in mechanically ventilated patients. Aust Crit Care. 2017;30(1):37–43. doi: 10.1016/j.aucc.2016.03.004. [DOI] [PubMed] [Google Scholar]
- 3.Jaber S, Quintard H, Cinotti R, Asehnoune K, Arnal J, Guitton C, et al. Risk factors and outcomes for airway failure versus non-airway failure in the intensive care unit: a multicenter observational study of 1514 extubation procedures. Crit Care. 2018;22(1):468. doi: 10.1186/s13054-018-2150-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Girard T, Alhazzani W, Kress J, Ouellette D, Schmidt G, Truwit J, et al. An Official American Thoracic Society/American College of Chest Physicians Clinical Practice Guideline: Liberation from Mechanical Ventilation in Critically Ill Adults. Rehabilitation protocols, ventilator liberation protocols, and cuff leak tests. Am J Respir Crit Care Med. 2017;195(1):120–133. doi: 10.1164/rccm.201610-2075ST. [DOI] [PubMed] [Google Scholar]
- 5.Amoateng-Adjepong Y, Jacob B, Ahmad M, Manthous C. The effect of sepsis on breathing pattern and weaning outcomes in patients recovering from respiratory failure. Chest. 1997;112(2):472–477. doi: 10.1378/chest.112.2.472. [DOI] [PubMed] [Google Scholar]
- 6.Thille A, Boissier F, Ben Ghezala H, Razazi K, Mekontso-Dessap A, Brun-Buisson C. Risk factors for and prediction by caregivers of extubation failure in ICU patients. Crit Care Med. 2015;43(3):613–620. doi: 10.1097/CCM.0000000000000748. [DOI] [PubMed] [Google Scholar]
- 7.Boles J, Bion J, Connors A, Herridge M, Marsh B, Melot C, et al. Weaning from mechanical ventilation. Eur Respir J. 2007;29(5):1033–1056. doi: 10.1183/09031936.00010206. [DOI] [PubMed] [Google Scholar]
- 8.Dres M, Goligher E, Hunks L, Brochard L. Critical illness-associated diaphragm weakness. Intensive Care Med. 2017;43(10):1441–1452. doi: 10.1007/s00134-017-4928-4. [DOI] [PubMed] [Google Scholar]
- 9.Hermans G, Agent A, Testelmans D, Decramer M, Gayan-Ramirez G. Increased duration of mechanical ventilation is associated with decreased diaphragmatic force: a prospective observational study. Crit Care. 2010;14(4):R127. doi: 10.1186/cc9094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fossat G, Daillet B, Desmalles E, Boulain T. Does diaphragm ultrasound improve the rapid shallow breathing index accuracy for predicting the success of weaning from mechanical ventilation? Aust Crit Care. 2022;35(3):233–240. doi: 10.1016/j.aucc.2021.05.008. [DOI] [PubMed] [Google Scholar]
- 11.Summerhill E, El-Sameed Y, Glidden T, McCool F. Monitoring recovery from diaphragm paralysis with ultrasound. Chest. 2008;133(3):737–743. doi: 10.1378/chest.07-2200. [DOI] [PubMed] [Google Scholar]
- 12.Zamora J, Abraira V, Muriel A, Khan K, Coomarasamy A. Meta-DiSc: a software for meta-analysis of test accuracy data. BMC Med Res Method. 2006;6(1):498. doi: 10.1186/1471-2288-6-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Harbord R, Deeks J, Egger M, Whiting P, Sterne J. A unification of models for meta-analysis of diagnostic accuracy studies. Biostatistics. 2006;8(2):239–251. doi: 10.1093/biostatistics/kxl004. [DOI] [PubMed] [Google Scholar]
- 14.Sterne J, Egger M. Funnel plots for detecting bias in meta-analysis. J Clin Epidemiol. 2001;54(10):1046–1055. doi: 10.1016/s0895-4356(01)00377-8. [DOI] [PubMed] [Google Scholar]
- 15.Yoo J, Lee S, Lee J, Kim H. Comparison of clinical utility between diaphragm excursion and thickening change using Ultrasonography to predict extubation success. Korean J Intern Med. 2019;34(3):686–686. doi: 10.3904/kjim.2016.152.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mowafy S, Abdelgalel E. Diaphragmatic rapid shallow breathing index for predicting weaning outcome from mechanical ventilation: comparison with traditional rapid shallow breathing index. Egyptian J Anaesthesia. 2019;35(1):9–17. [Google Scholar]
- 17.Osman A, Hashim R. Diaphragmatic and lung ultrasound application as new predictive indices for the weaning process in ICU patients. Egyptian J Radiol Nucl Med. 2017;48(1):61–66. [Google Scholar]
- 18.Soliman S, Ragab F, Soliman R, Gaber A, Kamal A. Chest ultrasound in prediction of weaning failure. Open Access Macedonian J Med Sci. 2019;7(7):1143–1147. doi: 10.3889/oamjms.2019.277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abdelwahed W, Abd Elghafar M, Amr Y, Alsherif S, Eltomey M. Prospective study: diaphragmatic thickness as a predictor index for weaning from mechanical ventilation. J Crit Care. 2019;52:10–15. doi: 10.1016/j.jcrc.2019.03.006. [DOI] [PubMed] [Google Scholar]
- 20.Elshazly M, Kamel K, Elkorashy R, Ismail M, Ismail J, Assal H. Role of bedside ultrasonography in assessment of diaphragm function as a predictor of success of weaning in mechanically ventilated patients. Tuberculosis Respiratory Dis. 2020;83(4):295–302. doi: 10.4046/trd.2020.0045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mawla T, Fattah S, Halim A, Elhefeny R. Diaphragmatic function assessment using chest ultrasonography as a predictor for weaning from mechanical ventilation. Egyptian J Crit Care Med. 2022;9(1):1–9. [Google Scholar]
- 22.Blumhof S, Wheeler D, Thomas K, McCool F, Mora J. Change in diaphragmatic thickness during the respiratory cycle predicts extubation success at various levels of pressure support ventilation. Lung. 2016;194(4):519–525. doi: 10.1007/s00408-016-9911-2. [DOI] [PubMed] [Google Scholar]
- 23.Jung B, Moury P, Mahul M, de Jong A, Galia F, Prades A, et al. Diaphragmatic dysfunction in ICU-acquired weakness and its impact on extubation failure. Intensive Care Med. 2015;42(5):853–861. doi: 10.1007/s00134-015-4125-2. [DOI] [PubMed] [Google Scholar]
- 24.Mariani L, Bedel J, Gros A, Lerolle N, Milojevic K, Laurent V, et al. Ultrasonography for screening and follow-up of diaphragmatic dysfunction in the ICU. J Intensive Care Med. 2015;31(5):338–343. doi: 10.1177/0885066615583639. [DOI] [PubMed] [Google Scholar]
- 25.Dres M, Dubé B, Mayaux J, Delemazure J, Reuter D, Brochard L, et al. Coexistence and impact of limb muscle and diaphragm weakness at time of liberation from mechanical ventilation in medical intensive care unit patients. Am J Respir Crit Care Med. 2017;195(1):57–66. doi: 10.1164/rccm.201602-0367OC. [DOI] [PubMed] [Google Scholar]
- 26.Vivier E, Muller M, Putegnat J, Steyer J, Barrau S, Boissier F, et al. Inability of diaphragm ultrasound to predict extubation failure. Chest. 2019;155(6):1131–1139. doi: 10.1016/j.chest.2019.03.004. [DOI] [PubMed] [Google Scholar]
- 27.Flevari A, Lignos M, Konstantonis D, Armaganidis A. Diaphragmatic ultrasonography as an adjunct predictor tool of weaning success in patients with difficult and prolonged weaning. Minerva Anesthesiol. 2016;82(11):1149–1157. [PubMed] [Google Scholar]
- 28.Hayat A, Khan A, Khalil A, Asghar A. Diaphragmatic excursion: does it predict successful weaning from mechanical ventilation? J Coll Physicians Surg Pak. 2017;27(12):743–746. [PubMed] [Google Scholar]
- 29.Huang D, Ma H, Zhong W, Wang X, Wu Y, Qin T, et al. Using M-mode Ultrasonography to assess diaphragm dysfunction and predict the success of mechanical ventilation weaning in elderly patients. J Thorac Dis. 2017;9(9):3177–3186. doi: 10.21037/jtd.2017.08.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Li S, Chen Z, Yan W. Application of bedside ultrasound in predicting the outcome of weaning from mechanical ventilation in elderly patients. BMC Pulmonary Med. 2021;21(1):985. doi: 10.1186/s12890-021-01605-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pirompanich P, Romsaiyut S. Use of diaphragm thickening fraction combined with rapid shallow breathing index for predicting success of weaning from mechanical ventilator in medical patients. J Intensive Care. 2018;6(1):498. doi: 10.1186/s40560-018-0277-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Theerawit P, Eksombatchai D, Sutherasan Y, Suwatanapongched T, Kiatboonsri C, Kiatboonsri S. Diaphragmatic parameters by Ultrasonography for predicting weaning outcomes. BMC Pulmonary Med. 2018;18(1):5478. doi: 10.1186/s12890-018-0739-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Tenza-Lozano E, Llamas-Alvarez A, Jaimez-Navarro E, Fernández-Sánchez J. Lung and diaphragm ultrasound as predictors of success in weaning from mechanical ventilation. Crit Ultrasound J. 2018;10(1):1789. doi: 10.1186/s13089-018-0094-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Palkar A, Narasimhan M, Greenberg H, Singh K, Koenig S, Mayo P, et al. Diaphragm excursion-time index. Chest. 2018;153(5):1213–1220. doi: 10.1016/j.chest.2018.01.007. [DOI] [PubMed] [Google Scholar]
- 35.Varón-Vega F, Hernández Á, López M, Cáceres E, Giraldo-Cadavid L, Uribe-Hernandez A, et al. usefulness of diaphragmatic ultrasound in predicting extubation success. Med Intensiva. 2021;45(4):226–233. doi: 10.1016/j.medin.2019.10.007. [DOI] [PubMed] [Google Scholar]
- 36.Gok F, Mercan A, Kilicaslan A, Sarkar G, Yosunkaya A. Diaphragm and lung ultrasonography during weaning from mechanical ventilation in critically Ill patients. Cureus. 2021;5:497. doi: 10.7759/cureus.15057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alam M, Roy S, Ikeda M, Padma F, Nipun K, Chowdhury S, et al. Diaphragm ultrasound as a better predictor of successful extubation from mechanical ventilation than rapid shallow breathing index. Acute Crit Care. 2022;37(1):94–100. doi: 10.4266/acc.2021.01354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Li C, Li X, Han H, Cui H, Wang G, Wang Z. Diaphragmatic ultrasonography for predicting ventilator weaning. Medicine. 2018;97(22):e10968. doi: 10.1097/MD.0000000000010968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Llamas-Alvarez A, Tenza-Lozano E, Latour-Pérez J. Diaphragm and lung ultrasound to predict weaning outcome. Chest. 2017;152(6):1140–1150. doi: 10.1016/j.chest.2017.08.028. [DOI] [PubMed] [Google Scholar]
- 40.García-Sánchez A, Barbero E, Pintado B, Pérez A, Velasco D, Rodríguez C, et al. Ultrasound-assessed diaphragmatic dysfunction as a predictor of extubation failure: systematic review and meta-analysis. Open Respiratory Arch. 2020;2(4):267–277. [Google Scholar]
- 41.Le Neindre A, Philippart F, Luperto M, Wormser J, Morel-Sapene J, Aho S, et al. Diagnostic accuracy of diaphragm ultrasound to predict weaning outcome: a systematic review and meta-analysis. Int J Nurs Stud. 2021;117:103890. doi: 10.1016/j.ijnurstu.2021.103890. [DOI] [PubMed] [Google Scholar]
- 42.Boles J, Bion J, Connors A, Herridge M, Marsh B, Melot C, et al. Weaning from mechanical ventilation. Eur Respir J. 2007;29(5):1033–1056. doi: 10.1183/09031936.00010206. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Search strategy, supplemental Tables, and supplemental Figures.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.