Abstract
Cardiovascular diseases are among important causes of death. Atherosclerosis is an important etiology for coronary artery diseases in which coronary artery calcification plays a principal role. Recently novel cardiovascular risk factors in coronary calcification are under attention. In this study, we investigated possible association between novel cardiovascular risk factors and coronary calcification. This is a prospectively registered systematic review and meta-analysis in PROSPERO and was performed in accordance with PRISMA guidelines. Medical databases were searched. Primary papers were screened and studies reporting our outcomes of interest were selected for data extraction. Quantitative data syntheses were performed using Comprehensive Meta-analysis Ver.3. In this study, 5252 papers were screened and finally 28 papers including 31241 patients underwent data extraction. Based on our findings, neutrophil/lymphocyte ratio (8 out of 10), red cell distribution width (r = 0.250, p < 0.0001), and interleukin 6 (odds ratio [OR]: 1.101 [95% confidence interval (CI): 1.001-1.210], p = 0.047) were associated with severity of coronary calcification while C-reactive protein (one out of eight) was not associated with coronary calcification. Results of lymphocyte/monocyte ratio (r = –0.120, p < 0.001), platelet/lymphocyte ratio (OR: 1.47 [95% CI: 0.89-2.41, p = 0.124]), and MPV (r = 0.017, p = 0.814 vs. OR: 1.91 [95% CI: 1.28-2.85, p = 0.002]) remained controversial due to few number of included studies or contrary results. We can conclude that neutrophil/lymphocyte ratio, red cell distribution width, and interleukin-6 are significantly associated with coronary calcification and C-reactive protein is not significantly associated with severity of coronary calcification. Our results about mean platelet volume, platelet/lymphocyte ratio, and lymphocyte/monocyte ratio are not reliable and require further investigations.
Keywords: Systematic review, Metaanalysis, Inflammation, Risk factors, Atherosclerosis, Coronary artery disease
Resumen
Las enfermedades cardiovasculares se encuentran entre las primeras causas de mortalidad. La aterosclerosis es una etiología importante de las enfermedades de las arterias coronarias en la que la calcificación de las arterias coronarias juega un papel principal. Recientemente, se están prestando atención a factores novedosos de riesgo cardiovascular en la calcificación coronaria. En este estudio investigamos la asociación posible entre los factores novedosos de riesgo cardiovascular y la calcificación coronaria. Esta es una revisión sistemática y metaanálisis registrados de forma prospectiva en PROSPERO y se realizó de acuerdo con las pautas de PRISMA. Se realizaron búsquedas en bases de datos médicas. Se examinaron los artículos primarios y se seleccionaron para la extracción de datos los estudios cuyos resultados fueron de nuestro interés. Las síntesis de datos cuantitativos se realizaron utilizando Comprehensive Meta-analysis Ver.3. En este estudio se seleccionaron 5252 artículos y finalmente se extrajeron los datos de 28 artículos que incluían 31241 pacientes. Según nuestros hallazgos, la proporción de neutrófilos/linfocitos (8 de 10), el ancho de distribución de glóbulos rojos (r = 0,250, valor de p < 0.0001) y la interleucina 6 (OR: 1.101 [IC del 95%: 1.001-1.210], valor p = 0.047) se asociaron con la gravedad de la calcificación coronaria, mientras que la proteína C reactiva (1 de 8) no se asoció con la calcificación coronaria. Resultados de la proporción linfocitos/monocitos (r = –0,120, valor p < 0,001), la proporción plaquetas/linfocitos (OR: 1,47 [IC 95%: 0.89-2.41, valor p = 0.124]) y el volumen plaquetario medio (r = 0.017, valor p = 0.814 C. OR: 1.91 [IC 95%: 1.28-2.85, valor p = 0.002]) siguieron siendo polémicos debido al escaso número de estudios incluidos o resultados contrarios. Podemos concluir que la proporción de neutrófilos/linfocitos, el ancho de distribución de los glóbulos rojos y la interleucina 6 se asocian significativamente con la calcificación coronaria y la proteína C reactiva no se asocia significativamente con la gravedad de la calcificación coronaria. Nuestros resultados sobre el volumen plaquetario medio, la proporción de plaquetas/linfocitos y la proporción de linfocitos/monocitos no son confiables y requieren más investigaciones.
Palabras clave: Revisión sistemática, Metaanálisis, Inflamación, Factores de riesgo, Aterosclerosis, Arteriopatía coronaria
Introduction
Coronary artery diseases (CAD) are a subgroup of wide spectrum of cardiovascular diseases and are one of the most common causes of death around the world and lead to a high mortality and morbidity rate annually1. In recent literature, different etiologies are defined for CADs and atherosclerosis is pointed out to be among the most important ones2.
Estimating burden and severity of atherosclerosis-mediated coronary artery diseases can be achieved by different modalities and depends on different parameters such as plaque morphology, plaque composition, and intensity of calcification in atherosclerotic plaque3,4.
Coronary computed tomography angiography (CCTA) is one of the most precise modalities in measuring severity of coronary artery calcification (CAC) in susceptible and high-risk patients for CADs. Extent of CAD is assessed through different markers and indices in CCTA such as morphology of plaque or coronary calcium score (CCS)5.
Considering low accessibility of CCTA and high expenses of CCTA especially in low-income countries along with technical and radiation limitations of CCTA, it is important to separate high-risk and low-risk patients for CAD; thus, different factors are being under attention for risk assessment of CAD in susceptible patients6.
In the past decades, some inflammatory and routine hematological markers have attracted attention of researchers around the world and are being studied under “novel cardiovascular risk factors” title. Several studies in different designs are performed in this field and controversial results are reported from different regions7-10.
Considering high number of primary papers and long period of time spent on investigating so called novel cardiovascular risk factors along with importance of coronary artery calcification during atherosclerotic processes, in this study, we aimed to sum up any possible association between novel cardiovascular risk factors and coronary artery calcification.
Methods
Study design and search strategy
This is a systematic review which was performed to investigate any possible association between recently discussed inflammatory markers and coronary artery calcification detected through coronary computed tomography (CT) angiography. This study covers all published literature in this area before September 2020 without any limitation. This systematic review was designed and performed based on latest PRISMA guidelines and was prospectively registered in PROSPERO (international prospective register of systematic reviews of university of York, UK) with CRD42020177566 registration ID11.
Our search protocol was based on a PICO as P: patients at risk of coronary artery disease, I: computed tomography angiography, C: coronary artery calcification, and O: different novel cardiovascular risk factors including red cell distribution width (RDW), platelet distribution width (PDW), red cell distribution width to platelet ratio (RPR), neutrophil to lymphocyte ratio (NLR), platelet to lymphocyte ratio (PLR), C-reactive protein (CRP), interleukin 6 (IL-6), mean platelet volume (MPV), and lymphocyte to monocyte ratio (LMR). To achieve an acceptable search sensitivity, we only searched keywords associated with I, C, and O sections.
To obtain comprehensive and reliable search results, all prominent medical databases including PubMed, Web of Science, Scopus, and Embase were accurately searched in a systematic manner. Our PubMed search query was as (red cell distribution width[MeSH Terms]) OR (C-reactive protein[MeSH Terms]) OR (interleukin-6[MeSH Terms]) OR (mean platelet volume[MeSH Terms]) OR (inflammation[MeSH Terms]) OR (risk factors[MeSH Terms]) OR (blood cell count[MeSH Terms]) OR (red cell distribution width[Title/Abstract]) OR (platelet distribution width[Title/Abstract]) OR (red cell distribution width to platelet ratio[Title/Abstract]) OR (neutrophil to lymphocyte ratio[Title/Abstract]) OR (platelet to lymphocyte ratio[Title/Abstract]) OR (c reactive protein[Title/Abstract]) OR (interleukin 6[Title/Abstract]) OR (mean platelet volume[Title/Abstract]) OR (lymphocyte to monocyte ratio[Title/Abstract]) OR (inflammation[Title/Abstract]) OR (risk factor[Title/Abstract]) OR (inflammatory marker[Title/Abstract]) OR (inflammatory index[Title/Abstract]) OR (blood cell count[Title/Abstract]) OR (complete blood count[Title/Abstract]) AND (arteriosclerosis[MeSH Terms]) OR (atherosclerosis[MeSH Terms])) OR (arteriosclerosis[Title/Abstract]) OR (atherosclerosis[Title/Abstract]) OR (coronary calcification[Title/Abstract]) OR (coronary artery calcification[Title/Abstract]) OR (coronary calcium score[Title/Abstract]) AND (computed tomography angiography[Title/Abstract]) OR (CT angiography[Title/Abstract]) OR (computed tomography angiography[MeSH Terms]). All other databases were similarly searched with the same keywords but carefully adjusted based on requirements of each database. No limitations such as language, publication time, location, or study type were applied in any of searched databases.
Inclusion and exclusion criteria
Two authors (AN and HV) started the screening process separately and all decisions about disagreements were made by a third author (HH). All studies that may report any association between severity of coronary calcification were eligible regardless of study type. Since we aimed to reach clinically applicable results, only studies performed on human were enrolled.
Hereby, we even enrolled conference abstracts that reported our outcomes of interest and bibliography of all relevant review articles were also carefully checked.
Data extraction and quality assessment
All studies about association between CAC and circulating levels of inflammatory markers might have possibly reported our outcomes of interest including severity of CAC, CCS, NLR, RDW, PLR, RPR, LMR, CRP, and IL-6 entered data extraction and quality assessment.
Information associated with first author’s name, publication year, studied population, sample size, gender distribution, studied categories and number of patients in each category, measured levels of inflammatory markers in each category, and results of statistical tests was extracted. For this goal, Microsoft Office Package 2020 and EndNote X9 softwares were used.
Since there were different types of studies included in this systematic review, a four level GRADE scoring system was used for quality assessment and evaluating certainty of evidences for each paper. Articles were categorized based on GRADE scoring system in four categories of very low, low, moderate, and high certainty rate12.
All articles that entered data extraction step were also assessed for quality by two different authors (AN and HV) separately and disagreements were solved by consensus.
Statistical analysis
Comprehensive Meta-analysis Ver.3 Software (latest version) was used for all statistical analyses during quantitative data synthesis.
For all analyses, random effects model was used Fishers’ Z (standard error) and log odds ratio (standard error) were computed effect sizes for RDW and IL-6 meta-analyses, respectively.
Heterogeneity tests were performed in both analyses and subgroup analysis was performed if applicable. Results of heterogeneity tests are reported as Cochrane’s Q statistic, I², and associated P.
For both meta-analyses, Begg’s funnel plot with both observed and imputed studies was used to visualize the results. Begg’s, Egger’s, and Rosenthal’s fail-safe N tests were used for quantitative evaluation of publication bias.
For sensitivity analysis, “one study removed” method was used.
Results are reported in the form of forest plots (for main analysis and sensitivity analysis) and funnel plots (for publication bias). In all tests, p < 0.05 was considered to be statistically significant except for Begg’s and Egger’s tests in which p < 0.1 was considered as statistically significant.
Results
Search results
After primary search up to September 9, 2020, a number of 5252 articles were found in all databases which were separately as PubMed: 1152 articles, Web of Science: 1653 articles, Scopus: 1178 articles, Embase: 1269 articles, and 22 more articles were also found while checking bibliography of included articles.
All references were imported into EndNote X9 software and a number of 2686 duplicate records were removed meaning that 2588 primary papers entered title and abstract screening phase.
Considering our obsession for not missing any single paper, in title and abstract screening step, a very large number of papers were carefully screened and all papers that could have possibly reported any association between considered inflammatory markers and severity of coronary artery calcification were selected. In this step, a number of 2547 papers were excluded from the study, so 41 papers entered full-text screening step.
In full-text screening step, 13 articles were removed and 28 final articles entered quality assessment and data extraction step. Among excluded papers, one was written in Chinese13, one was a review article14, three were removed15-17 because of reporting the same research material of two included articles18,19, and eight of them seemed to report our outcomes of interest during title and abstract screening but were finally excluded after full-text screening20-27.
In this research, we aimed to assess any possible relationship between coronary calcification with RDW, PDW, RPR, NLR, PLR, CRP, IL-6, MPV, and LMR but detected papers only included RDW, IL-6, LMR, NLR, PLR, CRP, and MPV meaning that we were unable to find any article reporting results associated with RPR and PDW markers.
In included papers, some of them reported more than one inflammatory marker, thus in data extraction tables, 37 rows of data extracted from 28 articles are reported which some of them are the same study but reporting different variables.
At the end, ten papers were eligible for quantitative data synthesis; 5 in IL-6 meta-analysis and 5 in RDW meta-analysis. Performing meta-analysis for other inflammatory markers was impossible due to different result reporting formats.
The search diagram is summed up in PRISMA search flowchart as shown in figure 1.
Figure 1.
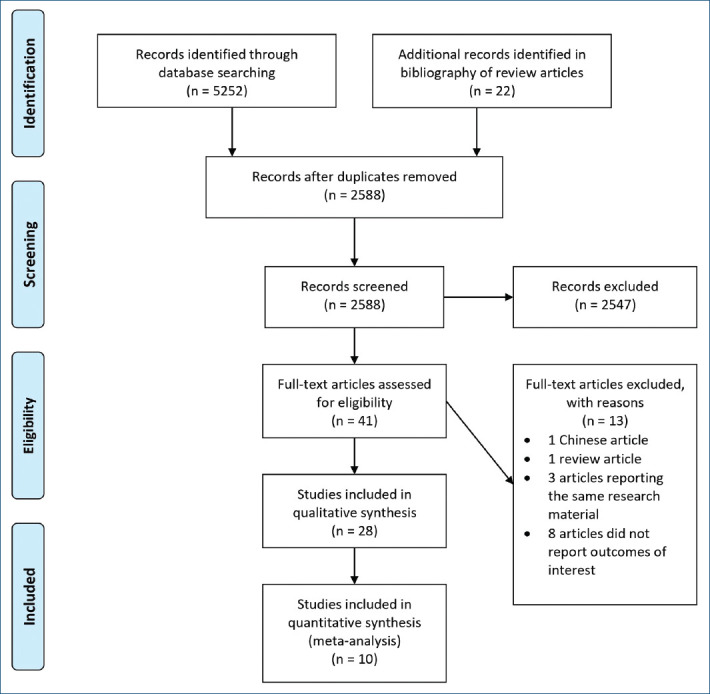
Diagram of our search protocol.
Studies and patients’ characteristics
In this study, a total number of 28 scientific papers covering 31241 patients were enrolled. Based on what we found in our primary search, this topic was studied since 2005 and is still being under attention up to 2020.
The researches were all performed on patients that are somehow at risk of coronary artery calcification and coronary artery disease and most of them were performed on patients with susceptible coronary artery disease or patients with diabetes, chronic kidney disease, non-alcoholic fatty liver disease, rheumatoid arthritis, or apparently healthy population.
All information associated with coronary artery calcification were obtained through non-contrast CT angiography of 8-slice multidetector computed tomography (MDCT) up to 320-slice MDCT device. All studies were performed on adult population and none of them were performed on patients below 18 years.
NLR
Among enrolled papers, 10 of them28-37 included information about NLR and coronary artery calcification. Results of all of them indicate a very significant association between NLR and intensity of CAC but considering different types of data reporting formats, we were not able to perform a meta-analysis on NLR.
Only two articles (out of 10) did not detect any significant association between NLR and CAC which one was performed on healthy adults (Nam et al.)35 and one (Chaikriangkrai et al.)37 was performed on patients with acute chest pain; this is while other studies were performed on patients with a more chronic condition or moderate-to-high risk for CAD. This is also notable that Park et al. also worked on healthy population and achieved p = 0.045 while other statistically significant studies were not performed on healthy population and reported a much more significant P.
Results associated with all above mentioned 10 studies along with quality assessment of studies are reported in Supplementary Table 128-37.
RDW
Among 28 enrolled studies, eight of them28,37-43 reported information about RDW. All eight articles reported a statistically significant association between RDW levels and coronary artery calcification except one which was performed by K Chaikriangirai et al. on patients with acute chest pain.
There was no study performed on patients with acute symptoms among those with statistically significant results. Data extracted from studies about RDW are summarized in Supplementary Table 228,37-43.
We were able to enter five studies28,38,41-43 (out of eight) in a meta-analysis of correlational type since they were reporting a correlational r and P. As seen in the forest plot (Fig. 2), there is a statistically significant correlation between RDW and coronary calcification (r = 0.250, p < 0.0001).
Figure 2.
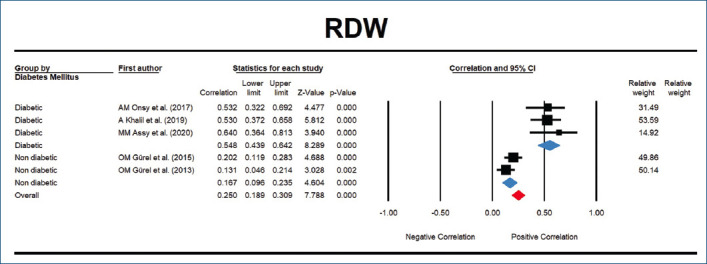
There is a statistically significant correlation between red cell distribution width and severity of coronary artery calcification (r = 0.250, p < 0.0001, I² = 87.890) in both diabetic (r = 0.548, p < 0.0001, I² = 0.000) and non-diabetic (r = 0.167, p < 0.0001, I² = 28.765) patients.
Considering very high heterogeneity among five included studies (Q = 33.031, I² = 87.890, p < 0.0001), we performed a subgroup analysis based on diabetes mellitus. Among five papers, three were performed on diabetic patients41-43 and two were performed on non-diabetic patients28. After grouping studies and performing the analysis once more, heterogeneity reduced in both diabetic (Q = 0.641, I² = 0.000, p = 0.726) and non-diabetic (Q = 1.404, I² = 28.765, p = 0.236) groups. We found that the correlation between RDW and coronary calcification is higher in diabetic patients (r = 0.548, p < 0.0001) compared to non-diabetic patients (r = 0.167, p < 0.0001).
Associated funnel plot (Fig. 3) is suggestive for existence of a possible publication bias among included papers which is confirmed by Egger’s test (p = 0.016); this is while the hypothesis of existence of publication bias is rejected by Begg’s test (p = 0.462) or Rosenthal’s fail-safe N (121 more studies in opposite direction are required to bring the p > 0.05) and this conflict can be due to few number of analyzed studies.
Figure 3.
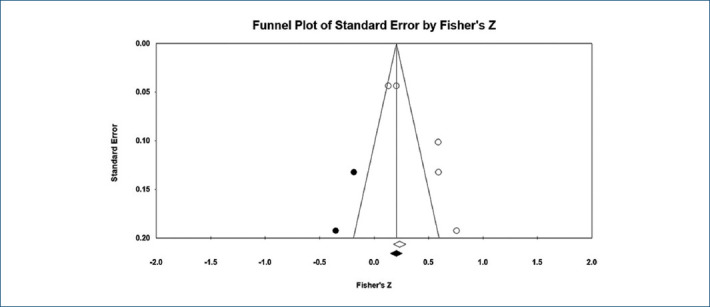
Begg’s funnel plot is suggestive for a slight publication bias (Egger’s p = 0.016, Begg’s p = 0.462).
As seen in supplementary figure 1, results of “one study removed” sensitivity analysis indicate that our overall results are not significantly dependent to any of primary studies.
CRP
Eight studies29,35,44-49 reported information about CRP levels and its association with coronary calcification and only one of them reported a really weak statistically significant correlation between CRP and coronary calcification with r = 0.06. This study was performed by Arad et al. in 2005 on apparently healthy population which is also the oldest included study in this systematic review.
There also exist two controversial studies on CRP. In the study performed by Ramadan MM, et al., the authors declare that CRP is higher in CAC positive group but the correlational analysis denies any significant correlation between CRP and CAC.
The other controversial study is done by Jenny, et al. in which the authors claim a relationship between CRP and CAC based on their first statistical model with less adjustments; this is while in their second model with more adjustments, this relationship is insignificant.
Results extracted from studies performed on CRP are summed in Supplementary Table 329,35,44-49.
Considering different formats in reporting the results of CRP along with lack of any significant association in almost all studies, we ignored to perform a meta-analysis on association between CRP levels and coronary artery calcification.
IL-6
In this systematic review, seven primary researches19,44,47-51 reported results about correlation between IL-6 levels and severity of coronary artery calcification which six of them reported a significant association between IL-6 and intensity of coronary calcification.
Results of data extraction from all seven articles of IL-6 are presented in Supplementary Table 419,44,47-51.
In terms of association between IL-6 and coronary calcification, we were able to do a meta-analysis on five articles19,44,47-49, including the only non-significant study performed on patients with rheumatoid arthritis19. As seen in the forest plot (Fig. 4), there is a significant association between IL-6 and coronary artery calcification (OR: 1.101 [95% CI: 1.001–1.210], p = 0.047).
Figure 4.

There is a statistically significant association between interleukin-6 and severity of coronary artery calcification (OR: 1.101 [95% CI: 1.001–1.210], p = 0.047, I² = 88.645).
We could also record a very high between study heterogeneity with a Q = 35.227, I² = 88.645, p < 0.001 which could not be resolved by different logical subgroup or regression analyses.
As seen in funnel plot (Fig. 5), there is a slight asymmetry in the plot which means imputed studies can slightly change the results of this meta-analysis. The hypothesis of existence of publication bias is rejected by Begg’s test (p = 0.462) and is confirmed by Egger’s test (p = 0.041). These are while Rosenthal’ss fail-safe N test indicates that a number of 43 papers of opposite direction can bring the p > 0.05.
Figure 5.

Begg’s funnel plot is suggestive for a slight publication bias (Egger’s p = 0.041, Begg’s p = 0.462).
Results of “one study removed” sensitivity analysis indicate a very sensitive and fragile result since removing almost any of the included studies can change direction of the results (Supplementary Fig. 2).
LMR
Among all 28 primary articles only in Si et al.’s article51, the authors investigated possible associated between LMR and coronary calcification in which they found a slight negative correlation r = –0.120 between LMR and coronary calcification; meaning lower LMR levels are associated with elevated CCS and thus higher risk for coronary artery diseases.
Detailed information about above mentioned paper is shown in Supplementary Table 552.
PLR
PLR was also reported only in one primary paper36 in which the authors found a significant difference in PLR levels across different groups of coronary artery calcium score but they were unable to find any significant association between PLR and severity of coronary artery calcification in their odds ratio model.
Information related to this paper is reported in Supplementary Table 636.
MPV
Two papers53,54 included information about relationship between MPV and coronary calcification. M Bulunmaz et al. investigated patients with diagnosed chronic ischemic heart disease and could not find any association between MPV and coronary calcification; this is while DH Jung et al. performed their study on general population and reported that people with positive coronary calcification with have a higher MPV level compared to people with CCS = 0.
Results of both papers are extracted and demonstrated in Supplementary Table 753,54.
Discussion
We performed this study aiming to achieve a final conclusion about any association between “novel cardiovascular risk factors” and extent of coronary artery calcification and thus coronary artery disease.
This systematic review started with a sensitive search and included an intense screening of a vast number of 5252 primary papers. Based on our knowledge, there is not any similar systematic review published in this field up to this date.
The idea of performing this systematic review was triggered by achieving controversial results after publishing several primary papers about importance of novel cardiovascular risk factors in different CVDs including CADs. We decided to cover all inflammatory markers from all regions without any limitation and for this goal, a careful evaluation was done on different up to date review articles in this field and some novel risk factors were defined to include our main search query.
After performing the systematic search over almost all important databases, unfortunately, we had to ignore RPR and PDW markers since no paper was published on association between these two and severity of coronary artery calcification.
We can sum up that RDW, NLR, and IL-6 are associated with severity of coronary artery calcification while CRP is not associated with severity of coronary calcification. In case of MPV, our results cannot be helpful since two study with almost the same quality showed opposite results. It must be noted that our results about LMR and PLR are not clinically applicable or reliable at all since only one study was found for each of them.
Another point that should be in mind while reading our results is that we only focused on association between mentioned markers and severity of coronary artery calcification, which under specific circumstances, does not necessarily mean severity of coronary artery disease and the relationship between coronary artery calcification and severity of coronary artery disease can also be questionable.
Qualitative results of NLR show that we can at least rely on this marker on susceptible patients for coronary artery disease with a more chronic condition and this marker was not helpful on healthy population or acute chest pain. Our findings about NLR are in accordance with a systematic review and meta-analysis performed by Angkananard et al.55 in 2018. In mentioned paper, the authors reported that higher NLR ratio is associated with coronary artery disease, acute coronary syndrome, and composite cardiovascular events.
The same point of chronicity can be also true about RDW since the only insignificant study was performed on patients with acute symptoms while all other studies reported a significant association. In this study, we found that RDW has a stronger correlation with severity of coronary artery calcification in diabetic patients compared to non-diabetic patients but the overall correlation in both groups is closer to those non-diabetic patients. Based on C Su et al.’s findings in 2015, it is notable that RDW is also associated with increased risk of mortality in patients with stablished CAD56.
Based on our observations, IL-6 is associated with severity of coronary calcification. The positive point about meta-analysis on this marker is that we were able to include the only non-significant study among other significant studies and this reduces possible bias in quantitative results.
Focusing more on high between study heterogeneity and fragile results of sensitivity analysis, it is expected that the final conclusion on IL-6 marker can be easily changed after a quality study is published in this field and it makes us uncertain about clinical applicability of the results.
Our uncertainty even increased while reading a paper by Danesh et al. in 2008. In this really valuable paper, the authors performed two more prospective studies plus a systematic review in which authors declared that long-term IL-6 levels are associated with risk of coronary heart disease57.
In this study, we could evaluate eight papers in association between CRP concentration and severity of coronary artery calcification and only in one of them CRP was reported to be associated with severity of CAC with a very low correlation strength. These findings about CRP are well supported by previously published reviews.
In a valuable systematic review performed by Shah et al. in 2009, the authors concluded that superiority of CRP against Framingham risk equation is not proved and they also stated that clinical use of CRP in prediction of coronary events requires further researches58.
In another large systematic review and meta-analysis of 83 cohort studies performed by Hemingway et al., the authors stated that no clinical practice recommendation can be made due to uncertainty of evidences about association between CRP and prognosis of patients with stable coronary disease which is totally confirmed by our results59.
Another valuable critical review done by Casas et al. found the same results as others. They concluded that animal studies indicate that CRP can be definitely pathogenic after ischemic infarction by the relevance with process of atherogenesis is unproved60. Since coronary artery calcification is a part of atherogenesis process, we believe that our results are confirming their findings.
Although we were unable to achieve a reliable and strong evidence about association between MPV and severity of coronary artery calcification, other similar studies with a focus on MPV have concluded that MPV is associated with coronary artery disease and can be helpful in risk prediction especially in combination with other risk factors61,62
We could only find one primary paper in association between LMR and severity of CAC which showed a negative correlation between LMR and CAC. We were unable to find any review article of high quality in association between LMR and severity of coronary artery disease. Only two primary papers with acceptable quality were found on this topic which both of them concluded that LMR is independently correlated with severity of coronary atherosclerosis or presence of CAD and high SYNTAX scores63,64.
In this systematic review, we could only find one paper that points out to the role of PLR in predicting CAC in which the authors reported a very significant difference in mean PLR in different groups of patients based on CAC while in their model, the odds ratio was not significant.
In a recent systematic review published by Z Qiu et al. in 2020 about relationship between PLR and stable CAD, the authors have reported that PLR is associated with stable CAD, severe stenosis in CAD, collateral circulation, and coronary slow flow phenomenon. They also suggested that future studies are required to better clarify this association and this is totally supported by our results65.
We feel like that it must be remarked again at the end that in all qualitative and quantitative analyses in this paper, we aimed to assess the association between novel cardiovascular risk factors and coronary artery calcification; not mortality rate, necessarily severity of coronary artery stenosis or even incidence or prevalence of newly stablished coronary artery disease and this is what makes our paper novel and such data were not presented priorly.
Like any other systematic review, one of our main challenges was to be able to unify data formats of primary papers to do a meta-analysis for better results. Unfortunately, we could only achieve this task in case of RDW and IL-6. We are lucky to report that our qualitative results about other markers except MPV, PLR, and LMR are reliable since we did not find any serious controversial results in qualitative analyses.
What we found after reviewing 5252 articles and performing data extraction on results of more than 31,000 patients indicate that most of these so called novel cardiovascular risk factors are not yet investigated enough and are not clinically reliable at all and there is still a long way ahead of researchers to achieve a unique conclusion about them. This reliability may vary between markers but what seems to be clear is that NLR, RDW, and IL-6 are significantly associated with severity of coronary artery calcification while CRP is not associated with CAC because of the fact that mentioned markers were studied more and the results are less controversial.
Conclusion
This systematic review and meta-analysis is a totally novel paper with a scientific and sensitive search strategy covering more than 5000 published papers and included seven different markers.
Based on our results, we can conclude that severity of coronary artery calcification is correlated with at least NLR, RDW, and IL-6 and is not correlated with CRP.
Our results about other novel risk factors including MPV, LMR, and PLR are not reliable and a lot of more primary papers and further meta-analyses are required to achieve a trustable result.
Supplementary data
Supplementary data are available at (Archivos de Cardiología de México) online (DOI: 10.24875/ACM.210004061). These data are provided by the corresponding author and published online for the benefit of the reader. The contents of supplementary data are the sole responsibility of the authors.
Acknowledgments
The authors thank to Maria João Pisco Almeida and Cecilia Ariza Gómez for their excellent medical writing and translation services, title and abstract of this paper are also available and presentable in Portuguese and Spanish, respectively.
Funding
This research has not received any specific grant from public, commercial, or non-profit sector agencies.
Conflicts of interest
The authors have no conflicts of interest to declare.
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that no patient data appear in this article.
Right to privacy and informed consent. The authors declare that no patient data appear in this article.
References
- 1.Bauersachs R, Zeymer U, Brière JB, Marre C, Bowrin K, Huelsebeck M. Burden of coronary artery disease and peripheral artery disease:a literature review. Cardiovasc Ther. 2019;2019:8295054. doi: 10.1155/2019/8295054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Libby P, Theroux P. Pathophysiology of coronary artery disease. Circulation. 2005;111:3481–8. doi: 10.1161/CIRCULATIONAHA.105.537878. [DOI] [PubMed] [Google Scholar]
- 3.Lee JM, Choi KH, Koo BK, Park J, Kim J, Hwang D, et al. Prognostic implications of plaque characteristics and stenosis severity in patients with coronary artery disease. J Am Coll Cardiol. 2019;73:2413–24. doi: 10.1016/j.jacc.2019.02.060. [DOI] [PubMed] [Google Scholar]
- 4.Mori H, Torii S, Kutyna M, Sakamoto A, Finn AV, Virmani R. Coronary artery calcification and its progression:what does it really mean? JACC Cardiovasc Imaging. 2018;11:127–42. doi: 10.1016/j.jcmg.2017.10.012. [DOI] [PubMed] [Google Scholar]
- 5.Eckert J, Schmidt M, Magedanz A, Voigtländer T, Schmermund A. Coronary CT angiography in managing atherosclerosis. Int J Mol Sci. 2015;16:3740–56. doi: 10.3390/ijms16023740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005;352:1685–95. doi: 10.1056/NEJMra043430. [DOI] [PubMed] [Google Scholar]
- 7.Tousoulis D. Novel risk factors in coronary artery disease:are they clinically relevant? Hellenic J Cardiol. 2019;60:149–51. doi: 10.1016/j.hjc.2019.06.003. [DOI] [PubMed] [Google Scholar]
- 8.Rusnak J, Fastner C, Behnes M, Mashayekhi K, Borggrefe M, Akin I. Biomarkers in stable coronary artery disease. Curr Pharm Biotechnol. 2017;18:456–71. doi: 10.2174/1389201018666170630120805. [DOI] [PubMed] [Google Scholar]
- 9.Ikonomidis I, Michalakeas CA, Parissis J, Paraskevaidis I, Ntai K, Papadakis I, et al. Inflammatory markers in coronary artery disease. Biofactors. 2012;38:320–8. doi: 10.1002/biof.1024. [DOI] [PubMed] [Google Scholar]
- 10.Lubrano V, Zym L, Balzan S. Neutrophyl to lymphocyte ratio and c reactive protein are indipendent predictors of severe coronary artery disease:comparison with hydroperoxides and consolidated inflammatory markers. Theor Biol Forum. 2018;111:49–56. doi: 10.19272/201811402004. [DOI] [PubMed] [Google Scholar]
- 11.Bernardo WM. PRISMA statement and PROSPERO. Int Braz J Urol. 2017;43:383–4. doi: 10.1590/S1677-5538.IBJU.2017.03.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ryan R, Hill S. How to GRADE the Quality of the Evidence. Cochrane Consumers and Communication Group. 2016 [Google Scholar]
- 13.Nah EH, Cho S, Kim S, Cho HI. Association of mean platelet volume with subclinical coronary atherosclerosis in diabetes and prediabetes. Int J Lab Hematol. 2018;40:103. [Google Scholar]
- 14.Balta S, Celik T, Mikhailidis DP, Ozturk C, Demirkol S, Aparci M, et al. The relation between atherosclerosis and the neutrophil-lymphocyte ratio. Clin Appl Thromb Hemost. 2016;22:405–11. doi: 10.1177/1076029615569568. [DOI] [PubMed] [Google Scholar]
- 15.De Graaf MA, Caselli C, Lorenzoni V, Rovai D, Marinelli M, Del Ry S, et al. HDL cholesterol, leptin and interleukin-6 are predictors of overall coronary atherosclerotic burden as assessed by CT angiography in patients with stable angina:results from the EVINCI study. Eur Heart J Cardiovascu Imaging. 2015;16:i1–2. [Google Scholar]
- 16.Karpouzas GA, Rezaeian P, Estis J, Todd J, Budoff MJ. Cardiac-specific troponin-I and interleukin-6 predict coronary atherosclerosis burden in rheumatoid arthritis. Ann Rheum Dis. 2014;73:467. [Google Scholar]
- 17.Rezaeian P, Estis J, Todd J, Budoff M, Karpouzas G. Correlation of ultra-sensitive cardiac troponin-I and inflammatory biomarker interleukin-6 with heart-scores in rheumatoid arthritis:using multi-slice computed tomography angiography. Clin Cardiol. 2017;40:11. [Google Scholar]
- 18.Caselli C, De Graaf M, Lorenzoni V, Rovai D, Marinelli M, Del Ry S, et al. HDL cholesterol, leptin and interleukin-6 are independent predictors of coronary atherosclerotic burden and plaque composition assessed by coronary CT angiography in patient with stable angina. Circulation. 2014;130:A13678. [Google Scholar]
- 19.Karpouzas GA, Estis J, Todd J, Budoff M. Biomarkers of cardiac dysfunction and inflammation in plasma predict occult coronary plaque burden and composition in rheumatoid arthritis. Arthritis Rheumatol. 2014;66:S158. [Google Scholar]
- 20.Nana-Goar Pogosova N, Koltunov IE, Kachanova NP, Yufereva YM, Vygodin VA. Associations of blood chemistry parameters with subclinical coronary atherosclerosis. Eur J Prev Cardiol. 2018;25:S85–6. [Google Scholar]
- 21.Bahrami H, Budoff M, Palella F, Witt M, Kingsley L, Jocobson L, et al. Inflammatory markers associated with subclinical coronary artery disease in HIV infected patients. J Am Coll Cardiol. 2015;65:A1158. [Google Scholar]
- 22.Gurses KM, Yalcin MU, Kocyigit D, Dural M, Canpolat U, Yorgun H, et al. MPV levels predict the severity of coronary atherosclerosis detected by multidetector computed tomography. Am J Cardiol. 2014;113:S116–7. [Google Scholar]
- 23.Nilsson L, Wieringa WG, Pundziute G, Gjerde M, Engvall J, Swahn E, et al. Neutrophil/lymphocyte ratio is associated with non-calcified plaque burden in patients with coronary artery disease. PLoS One. 2014;9:e108183. doi: 10.1371/journal.pone.0108183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shreibati JB, Baker LC, McConnell MV, Hlatky MA. Outcomes after coronary artery calcium and other cardiovascular biomarker testing among asymptomatic medicare beneficiaries. Circ Cardiovasc Imaging. 2014;7:655–62. doi: 10.1161/CIRCIMAGING.113.001869. [DOI] [PubMed] [Google Scholar]
- 25.Yalcin MU, Gurses KM, Kocyigit D, Dural M, Canpolat U, Yorgun H, et al. RDW levels predict the severity and morphology of coronary atherosclerosis detected by multidetector computed tomography. Am J Cardiol. 2014;113:S113–4. [Google Scholar]
- 26.Ates AH, Canpolat U, Yorgun H, Kaya EB, Sunman H, Demiri E, et al. Total white blood cell count is associated with the presence, severity and extent of coronary atherosclerosis detected by dual-source multislice computed tomographic coronary angiography. Cardiol J. 2011;18:371–7. [PubMed] [Google Scholar]
- 27.Çetin M, Kocaman SA, Bostan M, Çanga A, Çiçek Y, Erdoǧan T, et al. Red blood cell distribution width (RDW) and its association with coronary atherosclerotic burden in patients with stable angina pectoris. Eur J Gen Med. 2012;9:7–13. [Google Scholar]
- 28.Gürel OM, Demircelik MB, Bilgic MA, Yilmaz H, Yilmaz OC, Cakmak M, et al. Association between red blood cell distribution width and coronary artery calcification in patients undergoing 64-multidetector computed tomography. Korean Circ J. 2015;45:372–7. doi: 10.4070/kcj.2015.45.5.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Li T, Gu C, Wang F, Lv B, Zhang C, Peng R, et al. Association of neutrophil-lymphocyte ratio and the presence of noncalcified or mixed coronary atherosclerotic plaques. Angiology. 2018;69:256–63. doi: 10.1177/0003319717718330. [DOI] [PubMed] [Google Scholar]
- 30.Ateş AH, Aytemir K, Koçyiğit D, Yalcin MU, Gürses KM, Yorgun H, et al. Association of neutrophil-to-lymphocyte ratio with the severity and morphology of coronary atherosclerotic plaques detected by multidetector computerized tomography. Acta Cardiol Sin. 2016;32:676–83. doi: 10.6515/ACS20160225A. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Aygün F, Efe D. Association of neutrophil/lymphocyte ratio with obstructive coronary artery disease and coronary artery calcium score detected by multislice computed tomography in type 2 diabetes mellitus patients. Patient Prefer Adherence. 2015;9:1023–31. doi: 10.2147/PPA.S85577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Varastehravan H, Naghedi A, Naghedi A, Razavi-Ratki SK, Namiranian N, Moghadam RN, et al. Correlation between neutrophil to lymphocyte ratio and coronary calcium score in CT angiography. NLR and coronary calcification. Med Balear. 2020;35:41–46. [Google Scholar]
- 33.Açar G, Fidan S, Uslu ZA, Turkday S, Avci A, Alizade E, et al. Relationship of neutrophil-lymphocyte ratio with the presence, severity, and extent of coronary atherosclerosis detected by coronary computed tomography angiography. Angiology. 2015;66:174–9. doi: 10.1177/0003319714520954. [DOI] [PubMed] [Google Scholar]
- 34.Park BJ, Shim JY, Lee HR, Lee JH, Jung DH, Kim HB, et al. Relationship of neutrophil-lymphocyte ratio with arterial stiffness and coronary calcium score. Clin Chim Acta. 2011;412:925–9. doi: 10.1016/j.cca.2011.01.021. [DOI] [PubMed] [Google Scholar]
- 35.Nam SH, Kang SG, Song SW. The neutrophil-lymphocyte ratio is associated with coronary artery calcification in asymptomatic Korean males:a cross-sectional study. Biomed Res Int. 2017;2017:1989417. doi: 10.1155/2017/1989417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Serrano CV, Jr, de Mattos FR, Pitta FG, Nomura CH, de Lemos J, Ramires JA, et al. Association between neutrophil-lymphocyte and platelet-lymphocyte ratios and coronary artery calcification score among asymptomatic patients:data from a cross-sectional study. Mediators Inflamm. 2019;2019:6513847. doi: 10.1155/2019/6513847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chaikriangkrai K, Kassi M, Alchalabi S, Bala SK, Adigun R, Botero S, et al. Association between hematological indices and coronary calcification in symptomatic patients without history of coronary artery disease. N Am J Med Sci. 2014;6:433–9. doi: 10.4103/1947-2714.141625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gürel ÖM, Bilgic A, Demircelik B, Güneş M, Yilmaz ÖÇ, Bozduman F, et al. Association of red blood cell distribution width with coronary artery calcification. J Am Coll Cardiol. 2013;62:C86. [Google Scholar]
- 39.den Harder AM, de Jong PA, de Groot MC, Wolterink JM, Budde RP, Iŝgum I, et al. Commonly available hematological biomarkers are associated with the extent of coronary calcifications. Atherosclerosis. 2018;275:166–73. doi: 10.1016/j.atherosclerosis.2018.06.017. [DOI] [PubMed] [Google Scholar]
- 40.Ates AH, Hazirolan T, Kocyigit D, Yalcin MU, Gurses KM, Canpolat U, et al. Association of red cell distribution width with characteristics of coronary atherosclerotic plaques as detected by computed tomography angiography. Eur J Ther. 2019;25:58–63. [Google Scholar]
- 41.Onsy AM, Shehata MA, El Tawab AA, Khalil AE. The relation between red cell distribution width (RDW) and coronary artery calcium score (CACS) in the diabetic patients undergoing coronary CT angiography. Egypt J Hosp Med. 2017;69:1838–48. [Google Scholar]
- 42.Khalil A, Shehata M, Abdeltawab A, Onsy A. Red blood cell distribution width and coronary artery disease severity in diabetic patients. Future Cardiol. 2019;15:355–66. doi: 10.2217/fca-2018-0066. [DOI] [PubMed] [Google Scholar]
- 43.Assy MM, Khalil MF, Alaa Eldin A. The relation between the red cell distribution width and coronary artery calcium scoring in diabetic patients undergoing coronary CT angiography. Zagazig Univ Med J. 2020;26:28–37. [Google Scholar]
- 44.Lai S, Fishman EK, Lai H, Pannu H, Detrick B. Serum IL-6 levels are associated with significant coronary stenosis in cardiovascularly asymptomatic inner-city black adults in the US. Inflamm Res. 2009;58:15–21. doi: 10.1007/s00011-008-8150-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Arad Y, Goodman KJ, Roth M, Newstein D, Guerci AD. Coronary calcification, coronary disease risk factors, C-reactive protein, and atherosclerotic cardiovascular disease events:the St. Francis heart study. J Am Coll Cardiol. 2005;46:158–65. doi: 10.1016/j.jacc.2005.02.088. [DOI] [PubMed] [Google Scholar]
- 46.Hosseinsabet A, Mohebbi A, Almasi A. C-reactive protein and coronary calcium score association in coronary artery disease. Cardiol J. 2008;15:431–6. [PubMed] [Google Scholar]
- 47.Jenny NS, Brown ER, Detrano R, Folsom AR, Saad MF, Shea S, et al. Associations of inflammatory markers with coronary artery calcification:results from the multi-ethnic study of atherosclerosis. Atherosclerosis. 2010;209:226–9. doi: 10.1016/j.atherosclerosis.2009.08.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Simon TG, Trejo ME, McClelland R, Bradley R, Blaha MJ, Zeb I, et al. Circulating Interleukin-6 is a biomarker for coronary atherosclerosis in nonalcoholic fatty liver disease:results from the multi-ethnic study of atherosclerosis. Int J Cardiol. 2018;259:198–204. doi: 10.1016/j.ijcard.2018.01.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ramadan MM, Mahfouz EM, Gomaa GF, El-Diasty TA, Alldawi L, Ikrar T, et al. Evaluation of coronary calcium score by multidetector computed tomography in relation to endothelial function and inflammatory markers in asymptomatic individuals. Circ J. 2008;72:778–85. doi: 10.1253/circj.72.778. [DOI] [PubMed] [Google Scholar]
- 50.Saremi A, Anderson RJ, Luo P, Moritz TE, Schwenke DC, Allison M, et al. Association between IL-6 and the extent of coronary atherosclerosis in the veterans affairs diabetes trial (VADT) Atherosclerosis. 2009;203:610–4. doi: 10.1016/j.atherosclerosis.2008.07.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kamińska J, Stopiński M, Mucha K, Jędrzejczak A, Gołębiowski M, Niewczas MA, et al. IL 6 but not TNF is linked to coronary artery calcification in patients with chronic kidney disease. Cytokine. 2019;120:9–14. doi: 10.1016/j.cyto.2019.04.002. [DOI] [PubMed] [Google Scholar]
- 52.Si Y, Liu J, Shan W, Zhang Y, Han C, Wang R, et al. Association of lymphocyte-to-monocyte ratio with total coronary plaque burden in patients with coronary artery disease. Coron Artery Dis. 2020;31:650–5. doi: 10.1097/MCA.0000000000000857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bulunmaz M, Demir M, Uysal BB, Erdem S, Polat H, Erguney MH. Comparison of coronary artery calcium scores with platelet volume and uric acid levels in patients who underwent coronary artery imaging with computed tomography. Istanbul Med J. 2015;16:5–9. [Google Scholar]
- 54.Jung DH, Lee HR, Lee YJ, Kim JK, Park BJ, Shim JY. The association between coronary artery calcification and mean platelet volume in the general population. Platelets. 2011;22:567–71. doi: 10.3109/09537104.2011.580397. [DOI] [PubMed] [Google Scholar]
- 55.Angkananard T, Anothaisintawee T, McEvoy M, Attia J, Thakkinstian A. Neutrophil lymphocyte ratio and cardiovascular disease risk:a systematic review and meta-analysis. Biomed Res Int. 2018;2018:2703518. doi: 10.1155/2018/2703518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Su C, Liao LZ, Song Y, Xu ZW, Mei WY. The role of red blood cell distribution width in mortality and cardiovascular risk among patients with coronary artery diseases:a systematic review and meta-analysis. J Thorac Dis. 2014;6:1429–40. doi: 10.3978/j.issn.2072-1439.2014.09.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Danesh J, Kaptoge S, Mann AG, Sarwar N, Wood A, Angleman SB, et al. Long-term interleukin-6 levels and subsequent risk of coronary heart disease:two new prospective studies and a systematic review. PLoS Med. 2008;5:e78. doi: 10.1371/journal.pmed.0050078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Shah T, Casas JP, Cooper JA, Tzoulaki I, Sofat R, McCormack V, et al. Critical appraisal of CRP measurement for the prediction of coronary heart disease events:new data and systematic review of 31 prospective cohorts. Int J Epidemiol. 2009;38:217–31. doi: 10.1093/ije/dyn217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Hemingway H, Philipson P, Chen R, Fitzpatrick NK, Damant J, Shipley M, et al. Evaluating the quality of research into a single prognostic biomarker:a systematic review and meta-analysis of 83 studies of C-reactive protein in stable coronary artery disease. PLoS Med. 2010;7:e1000286. doi: 10.1371/journal.pmed.1000286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Casas JP, Shah T, Hingorani AD, Danesh J, Pepys MB. C-reactive protein and coronary heart disease:a critical review. J Intern Med. 2008;264:295–314. doi: 10.1111/j.1365-2796.2008.02015.x. [DOI] [PubMed] [Google Scholar]
- 61.Sansanayudh N, Anothaisintawee T, Muntham D, McEvoy M, Attia J, Thakkinstian A. Mean platelet volume and coronary artery disease:a systematic review and meta-analysis. Int J Cardiol. 2014;175:433–40. doi: 10.1016/j.ijcard.2014.06.028. [DOI] [PubMed] [Google Scholar]
- 62.Pafili K, Penlioglou T, Mikhailidis DP, Papanas N. Mean platelet volume and coronary artery disease. Curr Opin Cardiol. 2019;34:390–8. doi: 10.1097/HCO.0000000000000624. [DOI] [PubMed] [Google Scholar]
- 63.Gong S, Gao X, Xu F, Shang Z, Li S, Chen W, et al. Association of lymphocyte to monocyte ratio with severity of coronary artery disease. Medicine (Baltimore) 2018;97:e12813. doi: 10.1097/MD.0000000000012813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Kose N, Akin F, Yildirim T, Ergun G, Altun I. The association between the lymphocyte-to-monocyte ratio and coronary artery disease severity in patients with stable coronary artery disease. Eur Rev Med Pharmacol Sci. 2019;23:2570–5. doi: 10.26355/eurrev_201903_17406. [DOI] [PubMed] [Google Scholar]
- 65.Qiu Z, Jiang Y, Jiang X, Yang R, Wu Y, Xu Y, et al. Relationship between platelet to lymphocyte ratio and stable coronary artery disease:meta-analysis of observational studies. Angiology. 2020;71:909–15. doi: 10.1177/0003319720943810. [DOI] [PubMed] [Google Scholar]


