Abstract
Objective:
To evaluate the effectiveness and safety of transcatheter arterial embolization (TAE) of the branches of the subclavian and axillary arteries for hemorrhage control.
Methods:
Between January 2015 and June 2022, 35 TAE procedures were performed for hemorrhage from the branches of the subclavian and axillary arteries in 34 patients (22 men, 12 women; 1 male underwent TAE twice; mean age = 76 years). Pre-TAE CT showed hematomas in the chest (n = 25) and abdominal walls (n = 3), shoulder (n = 2), and lower neck (n = 2). CT showed hemothorax in eight cases. Angiographic findings, embolization technique, and technical and clinical success of TAE were retrospectively assessed in all cases.
Results:
TAE was performed by transfemoral (n = 16), transradial (n = 12), and transbrachial (n = 7) approaches. Angiography revealed contrast media extravasation or pseudoaneurysms in 32 cases (91.4%). The most commonly embolized arteries were the internal thoracic (n = 12), lateral thoracic (n = 6), and thoracoacromial (n = 6) arteries. Technical and clinical success rates were 100 and 85.7%, respectively. A complication (skin necrosis after injection of the liquid embolic agent) developed in only one patient (2.9%) and was conservatively managed.
Conclusion:
TAE is an effective and safe treatment for hemorrhage from the branches of the subclavian and axillary arteries.
Advances in knowledge:
Transfemoral approach has been used for TAE of the branches of the subclavian and axillary artery. Transradial and transbrachial approaches can also be considered.
Introduction
Branches of the subclavian and axillary arteries supply blood to the chest wall, neck, shoulder, and upper limb. Hemorrhage from these branches is an uncommon event, but may occur due to trauma, central venous catheter insertion, percutaneous biopsy, post-operative complication, infection, or systemic diseases that cause vascular fragility. 1,2 Many case reports have described the effectiveness of transcatheter arterial embolization (TAE) for the management of hemorrhage in this area. 3–9 However, no case series has focused on the effectiveness and safety of TAE of these branches. In contrast, several studies reported the usefulness of TAE of the intercostal arteries. 10–13 Additionally, the subclavian and axillary artery branches areeasily accessed with transradial and transbrachial approaches, which are different from endovascular intervention in the abdominal and pelvic arteries. We believe that TAE of the subclavian and axillary artery branches is an important procedure in our clinical practice and that our experience is worth sharing. The objective of this study was to evaluate the effectiveness and safety of TAE of the branches of the subclavian and axillary arteries for hemorrhage control.
Methods and materials
Patients
This retrospective study was approved by our institutional review board. The requirement for informed consent was waived. Between January 2015 and June 2022, 55 embolization procedures of the branches of the subclavian and axillary arteries for hemorrhage were performed by interventional radiologists in three institutions; 18 procedures for hemoptysis were excluded because many studies have already reported the effectiveness of embolization of systemic arteries from the subclavian and axillary arteries for this indication. 14,15 Two more cases were excluded: one was of a patient with multiple trauma in which the abdominopelvic involvement was more severe than that of the chest, and the other case was of a patient who underwent stent graft placement to the subclavian artery in addition to the embolization procedure. Thus, the study population included 34 patients (22 men and 12 women) on whom 35 embolization procedures were performed. One male underwent TAE twice; a second TAE was performed for bleeding at a different site 3 months after the first TAE. The mean age at TAE was 76 years (range, 46–98 years). Emergency TAE was performed for hemostasis in all cases. The causes of hemorrhage were diverse; the most common were iatrogenic complications (n = 17). Comorbidities were found in 28 cases. The patient characteristics are summarized in Table 1.
Table 1.
Patient characteristics in 35 embolization procedures
| Patient characteristics | N |
|---|---|
| Cause of bleeding | |
| Iatrogenic complication | 17 |
| Percutaneous drainage tube placement | 5 (4 for pleural effusion, 1 for abdominal abscess) |
| Post-operative bleeding (1–7 days after surgery) | 3 |
| Arterial injury during endovascular intervention | 2 |
| Cardiopulmonary resuscitation | 2 |
| Percutaneous aspiration | 2 (1 for pericardial fluid, 1 for hepatic cyst) |
| Percutaneous biopsy | 2 (1 for supraclavicular LN, 1 for breast tumor) |
| Reduction for shoulder dislocation | 1 |
| Antithrombotic drug | 7 |
| Trauma | 4 |
| Hematologic disease⁎ | 3 |
| Spontaneous bleeding | 2 |
| Skin invasion of a breast cancer | 1 |
| Thoracic aortic aneurysm rupture | 1 |
| Comorbidities | |
| Renal impairment | 9 |
| Diabetes mellitus | 8 |
| Cerebrovascular disease | 5 |
| Hematologic disease | 5 |
| Aortic disease | 4 |
| Heart failure | 4 |
| Malignancy | 4 |
| Angina pectoris | 3 |
| Hepatic impairment | 2 |
| Pancreatitis | 1 |
| None | 7 |
| Administration of antithrombotic drug | 15 |
LN: lymph node, NBCA: N-butyl cyanoacrylate.,
⁎Abnormal coagulation status was caused by a hematologic disease.
CT findings
Contrast-enhanced CT was performed before TAE in all but one case. In this exceptional case, the hemorrhage was caused by a vessel injury during embolization for a Type 2 endoleak after thoracic endovascular aortic repair; TAE was performed during the procedure. Pre-TAE CT showed hematomas located in chest (n = 25) and abdominal (n = 3) walls, shoulder (n = 2), lower neck (n = 2), and/or hemothorax (n = 8) in 34 cases. Extravasation of contrast media (n = 28) and/or pseudoaneurysm (n = 6) was observed in 33 cases; 1 patient had both extravasation and pseudoaneurysm. In one patient, neither extravasation nor pseudoaneurysm was observed. This patient had breast cancer, and TAE was performed to stop continuous bleeding from the tumor.
Evaluation
Angiographic findings and embolization technique were assessed in all cases. When contrast media extravasation or pseudoaneurysm was observed on angiography, technical success was defined as no visualization of these findings on post-TAE angiography. When neither pseudoaneurysm nor active bleeding was observed, technical success was defined as stasis of blood flow at the target artery on post-TAE angiography. Clinical success was defined as hemorrhage-free survival for 1 month after TAE. When additional treatment, such as repeated TAE or surgery, was performed for bleeding, it was regarded as a clinical failure. Complications of TAE were evaluated using the Cardiovascular and Interventional Radiological Society of Europe Classification System. 16
Results
Embolization procedure
Ten interventional radiologists with more than 3 years of experience in abdominal vascular intervention performed all TAE. TAE was performed under local anesthesia and moderate sedation in 29 cases, and under general anesthesia in 6 cases. A 4- or 5 F vascular sheath was placed in the femoral, radial, and brachial arteries in 16, 12, and 7 cases, respectively. A 4- or 5 F diagnostic catheter with various shapes was used for the procedure: Headhunter, JB2, Judkins right, Judkins left, internal mammary, shepherd hook, and Simmons for transfemoral approach; Rosch inferior mesenteric, Judkins right, Judkins left, cobra, and Berenstein for transradial and transbrachial approaches. In one case, transfemoral approach was used for TAE for bleeding from the internal thoracic artery; however, its selection was difficult. Subsequently, the approach was changed to transradial during the procedure. Conversely, in one case, transradial approach was used for TAE for bleeding from the deep cervical artery; however, its selection was difficult. The approach was subsequently changed to transfemoral. A microcatheter with a distal tip of 1.5–2.7 F was used for embolization. A tri-axial system using high-flow- and selective-type microcatheters was also used in 12 cases. Angiography showed extravasation (n = 26) of the contrast media or pseudoaneurysm (n = 6) in 32 cases; TAE was performed for these indications. Among the three cases without extravasation or pseudoaneurysm on angiography, active bleeding in the chest wall was observed on CT in two patients; the bleeding originated from the internal thoracic artery or intercostal arteries and TAE of the appropriate artery was performed accordingly. The remaining one case had continuous bleeding from a cancer in the left breast. Angiography of the left internal thoracic artery revealed tumor stain of the breast cancer, and embolization of this artery was subsequently performed. The number of embolized arteries in each patient was as follows: 1 in 24 cases, 2 in 9 cases, and 7 and 8 in 1 patient each. Embolized arteries are shown in Table 2. Embolic agents were gelatin sponge (n = 11), N-butyl cyanoacrylate (NBCA) (n = 9), coils (n = 4), gelatin sponge and coils (n = 9), gelatin sponge and NBCA (n = 1), and coils and NBCA (n = 1). When used, NBCA was mixed with lipiodol at a ratio of 1: 1–1: 7.
Table 2.
Embolized arteries
| Artery | N |
|---|---|
| Internal thoracic artery | 12 |
| Lateral thoracic artery | 6 |
| Thoracoacromial artery | 6 |
| Posterior humeral circumflex artery | 4 |
| Thoracodorsal artery | 4 |
| Intercostal arteries originating from the aorta | 3 |
| Subscapular artery | 3 |
| Dorsal scapular artery | 2 |
| Scapular circumflex artery | 2 |
| Superior thoracic artery | 2 |
| Inferior epigastric artery | 2 |
| Costocervical trunk | 1 |
| Deep cervical artery | 1 |
| Superficial thoracic artery | 1 |
| Superficial and deep circumflex iliac arteries | 1 |
| Suprascapular artery | 1 |
| Supreme intercostal artery | 1 |
| Thyrocervical trunk | 1 |
| Transverse cervical artery | 1 |
Technical and clinical success of TAE and complications
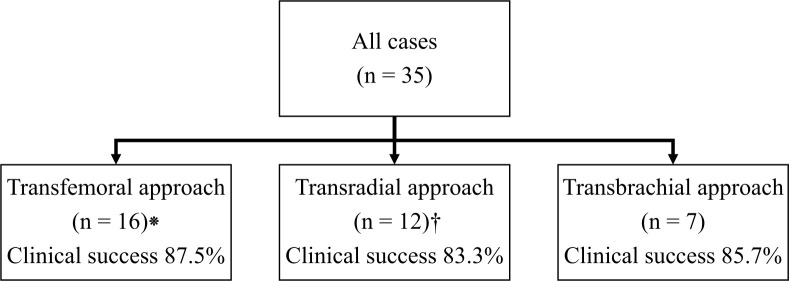
Technical success was achieved in all the cases (Figures 1 and 2). Clinical success was achieved in 30 cases (85.7%). The clinical success rate for each approach is shown in a flowchart (Figure 3). Clinical success was not achieved in five cases (Table 3). One patient became hemodynamically unstable during TAE, and emergency thoracotomy for the evacuation of hematoma and hemostasis was performed immediately after TAE (Patient 2 in Table 3). Additional treatments were performed for two other patients (a second TAE and thoracotomy for patients 3 and 4, respectively) 1 or 2 days after TAE. Among the five patients without clinical success, three died within 1 month after TAE, whereas two patients improved and were discharged.
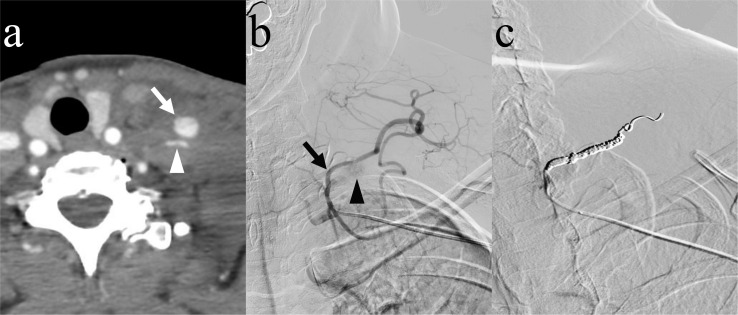
Figure 1.
A 62-year-old female underwent transcatheter arterial embolization of the transverse cervical artery for hemorrhage caused by percutaneous biopsy of left supraclavicular lymph node. (a) Contrast-enhanced CT showing a pseudoaneurysm (arrow) of the left transverse cervical artery (arrowhead). (b) Angiography of the left thyrocervical trunk showing a faint enhancement of the pseudoaneurysm (arrowhead) of the transverse cervical artery (arrow). Note that the diagnostic catheter is advanced from the left upper limb. (c) After coil embolization of the transverse cervical artery, angiography shows no enhancement of the pseudoaneurysm.
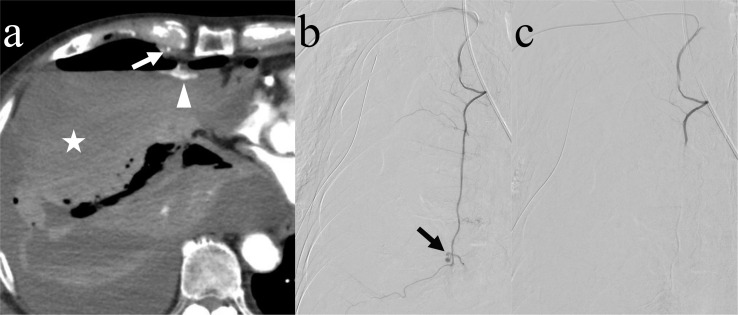
Figure 2.
An 88-year-old male underwent transcatheter arterial embolization of the internal thoracic artery for hemorrhage caused by cardiopulmonary resuscitation. (a) Contrast-enhanced CT showing extravasation of the contrast media (arrowhead) from the right internal thoracic artery (arrow). Hemothorax (star) is also observed. (b) Angiography of the right internal thoracic artery showing contrast media extravasation (arrow). Note that the diagnostic catheter is advanced from the right upper limb. (c) After embolization of the internal thoracic artery using gelatin sponge, angiography shows no extravasation of the contrast media.
Figure 3.
Flowchart showing the number of cases and clinical success rates for each approach method. ⁕In one case, the transfemoral approach was changed to a transradial approach during the procedure. †In one case, the transradial approach was changed to a transfemoral approach during the procedure.
Table 3.
Patients in whom clinical success was not achieved
| Pt. no. /Age/Sex | Cause of bleeding | Comorbidities | Embolized arteries | Additional treatment | Clinical course |
|---|---|---|---|---|---|
| 1/64 /M | Percutaneous drainage tube placement for abdominal abscess | Gastric cancer, pancreatitis | Seven arteriesa | No | Died due toliver failure 10 days later. |
| 2/69 /F | Percutaneous aspiration for pericardial fluid | Myelodysplastic syndrome | Internal thoracic artery | Thoracotomy for removal of hematoma and hemostasis on the same day | Transferred to a rehabilitation hospital 45 days later. |
| 3/78 /M | Arterial injury during endovascular intervention | Post-TEVAR due to aortic pseudoaneurysm | Costocervical trunk, internal thoracic artery | Second TAE, 1 day later because of decrease of blood pressure and progression of anemia. | Discharged home 20 days after embolization. |
| 4/81 /M | Antithrombotic drug | Angina pectoris, chronic kidney disease | Lateral thoracic artery | Thoracotomy for hematoma removal because of respiratory deterioration and hematoma enlargement 2 days later | Died due to acute respiratory distress syndrome 25 days after embolization. |
| 5/89 /M | Thoracic aortic aneurysm ruptureb | Chronic kidney disease | Eight arteriesc | No | Died due to disseminated intravascular coagulation 20 days later. |
F: female, M: male, TAE: transcatheter arterial embolization, TEVAR: thoracic endovascular aortic repair
Inferior epigastric, internal thoracic, 10–12th intercostal, and superficial and deep circumflex iliac arteries.
This patient presented with a ruptured thoracic aortic aneurysm. Contrast media extravasation into the pleural cavity around the right pulmonary apex was observed. The association between the hemorrhage and aortic aneurysm rupture remains uncertain. After emergency endovascular aneurysm repair, embolization was performed.
Dorsal scapular, superior cervical, thoracoacromial, lateral thoracic, thoracodorsal, and scapular circumflex arteries and thyrocervical and costocervical trunks.
A 73-year-old male who underwent TAE for post-operative bleeding developed skin necrosis as a complication. In the embolization procedure, a mixture of NBCA and lipiodol was injected from a branch of the right internal thoracic artery. Skin necrosis of the chest wall, restricted to the embolized area, developed a few days later, was managed conservatively, and resolved subsequently. This complication was Grade 2 based on CIRSE classification.
Discussion
This study evaluated the effectiveness and safety of TAE of the branches of the subclavian and axillary arteries for hemorrhage control. In previous studies that reported the usefulness of TAE for chest trauma and internal thoracic artery injury, all procedures were performed via transfemoral approach. 13,17,18 In this study, however, transradial or transbrachial approach was used in 19 of the 35 cases (54.2%). Stroke is a serious complication associated with TAE of the branches of the subclavian and axillary arteries. Transradial and transbrachial approaches do not require manipulation of a catheter in the aortic arch and brachiocephalic trunk, possibly resulting in a lower risk of stroke than a transfemoral approach. Additionally, the study population was characterized by old age (mean age, 76 years) and high rates of renal impairment (26.5%) and cerebrovascular disease (14.7%), which are known risk factors of stroke during percutaneous coronary intervention. 19 Thus, transradial and transbrachial approaches can be used as primary techniques in TAE of the branches of the subclavian and axillary arteries. One disadvantage of transradial and transbrachial approaches is that an additional approach might be needed when angiography and embolization of the contralateral subclavian or axillary artery branches or other branches supplying the chest wall or abdominal wall, such as the intercostal and inferior epigastric arteries, are performed.
This study showed a high technical and clinical success rate of TAE for bleeding from the branches of the subclavian and axillary arteries. Although no previous studies have focused on TAE for bleeding from the subclavian or axillary artery branches, several have reported its effectiveness in these arteries. One study evaluated the effectiveness of TAE for chest trauma in 68 patients. 13 In this study, 88 arteries were embolized, of which 40 were branches of the subclavian or axillary arteries. This study reported a clinical success rate of 92.6%. Others have evaluated the effectiveness of TAE for internal thoracic artery injury, and have reported high clinical success rates of 83.3 and 100%. 17,18
Complication was observed only in one case, and we believe that TAE of the subclavian and axillary artery branches is a safe procedure. However, in addition to the aforementioned risk of stroke, the risk of spinal cord infarction should be considered. Spinal cord infarction may develop because of the communications between the ascending and deep cervical arteries and vertebral artery. 20 Additionally, spinal cord infarction after embolization of the thyrocervical trunk has been reported. 21 We recommend careful evaluation of the angiographic image before TAE, and that the embolization method should be determined based on the image; e.g. coils would be preferable to particles if angiography shows a branch to the spinal cord. 22
In this study, the most common cause of bleeding wasiatrogenic complications, which accounted for nearly half of the cases. Iatrogenic complications occur in various procedures, e.g. surgery, transcatheter arterial intervention, percutaneous drainage, aspiration, biopsy, cardiopulmonary resuscitation, and reduction of shoulder dislocation. Although not found in this study, central venous catheter insertion has also been reported as a cause of bleeding from the subclavian and axillary artery branches. 17,23 Clinicians ought to understand that various procedures can cause injury to the subclavian and axillary artery branches and that TAE is an effective treatment.
This study revealed that the internal thoracic artery was most commonly embolized, followed by the lateral thoracic and thoracoacromial arteries. This result is in line with that of a previous study that reported the effectiveness of TAE for chest trauma. 13 In a previous study, the most commonly injured arterial branch of the subclavian and axillary arteries was the internal thoracic artery, followed by the lateral thoracic artery. This study also revealed that various arteries were associated with bleeding: 16 different branches of the subclavian and axillary arteries were embolized. The vascular anatomy of the branches of the subclavian and axillary arteries is complex; variable patterns of origin and bifurcation are well known. 24,25 Interventionists should understand the vascular anatomy of this area to correctly identify the bleeding artery and promptly perform a TAE.
This study has some limitations. First, the study was retrospective in design and the study population was relatively small. Second, we could not assess factors influencing the technical and clinical success rates because failure rates were low.
In conclusion, TAE is an effective and safe treatment for hemorrhage from the branches of the subclavian and axillary arteries.
Contributor Information
Yasuyuki Onishi, Email: goforawalktoday@yahoo.co.jp.
Hironori Shimizu, Email: hshimizu@kuhp.kyoto-u.ac.jp.
Saya Ando, Email: kaw_saya@me.com.
Hitomi Kawamura, Email: khitomi673@gmail.com.
Motofumi Onishi, Email: moto_radiology@yahoo.com.
Takanori Taniguchi, Email: tan9523929@yahoo.co.jp.
Hiroyoshi Isoda, Email: sayuki@kuhp.kyoto-u.ac.jp.
Yuji Nakamoto, Email: ynakamo1@kuhp.kyoto-u.ac.jp.
REFERENCES
- 1. Lee W-K, Mossop PJ, Little AF, Fitt GJ, Vrazas JI, Hoang JK, et al. Infected (mycotic) aneurysms: spectrum of imaging appearances and management. Radiographics 2008; 28: 1853–68. doi: 10.1148/rg.287085054 [DOI] [PubMed] [Google Scholar]
- 2. Darwazah AK, Eida M, Batrawy M, Isleem I, Hanbali N. Surgical treatment of circumflex coronary aneurysm with fistulous connection to coronary sinus associated with persistent left superior vena cava. J Card Surg 2011; 26: 608–12. doi: 10.1111/j.1540-8191.2011.01283.x [DOI] [PubMed] [Google Scholar]
- 3. Antevil JL, Holmes JF, Lewis D, Battistella F. Successful angiographic embolization of bleeding into the chest wall after blunt thoracic trauma. J Trauma 2006; 60: 1117–18. doi: 10.1097/01.ta.0000196326.38754.da [DOI] [PubMed] [Google Scholar]
- 4. Khalil MW, Cleveland TJ, Sarkar PK, Rao J. Successful angiographic embolisation of bleeding into the chest wall after chest drain insertion. Interact Cardiovasc Thorac Surg 2009; 8: 166–67. doi: 10.1510/icvts.2008.178582 [DOI] [PubMed] [Google Scholar]
- 5. Patel K, Kimbrell BJ, Marx MV, Petrone P, Asensio JA. Angiographic embolization of an expanding breast hematoma after blunt trauma: a novel approach to a rare injury. J Trauma 2009; 67: E14–6. doi: 10.1097/TA.0b013e3180485cc4 [DOI] [PubMed] [Google Scholar]
- 6. Fischman AM, Epelboym Y, Siegelbaum RH, Weintraub JL, Kim E, Nowakowski FS, et al. Emergent embolization of arterial bleeding after vacuum-assisted breast biopsy. Cardiovasc Intervent Radiol 2012; 35: 194–97. doi: 10.1007/s00270-011-0174-2 [DOI] [PubMed] [Google Scholar]
- 7. Wright AE, Wall M, Slaney P, Downing R. An unusual presentation of thoracoacromial artery pseudoaneurysm following shoulder arthroplasty. BMJ Case Rep 2014; 2014: bcr2014204625. doi: 10.1136/bcr-2014-204625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hoonjan B, Thayur N, Abu-Own A. Aneurysmal rupture of the costo-cervical trunk in a patient with neurofibromatosis type 1: a case report. Int J Surg Case Rep 2014; 5: 100–103: S2210-2612(13)00368-4. doi: 10.1016/j.ijscr.2013.12.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Miwa Y, Matsumura N, Suzuki T, Iwamoto T, Nakamura M, Matsumoto M. Pseudoaneurysm of the posterior humeral circumflex artery after reverse shoulder arthroplasty: a case report. JBJS Case Connect 2020; 10: e2000245. doi: 10.2106/JBJS.CC.20.00245 [DOI] [PubMed] [Google Scholar]
- 10. Chemelli AP, Thauerer M, Wiedermann F, Strasak A, Klocker J, Chemelli-Steingruber IE. Transcatheter arterial embolization for the management of iatrogenic and blunt traumatic intercostal artery injuries. J Vasc Surg 2009; 49: 1505–13. doi: 10.1016/j.jvs.2009.02.001 [DOI] [PubMed] [Google Scholar]
- 11. Stampfl U, Sommer C-M, Bellemann N, Kortes N, Gnutzmann D, Mokry T, et al. Emergency embolization for the treatment of acute hemorrhage from intercostal arteries. Emerg Radiol 2014; 21: 565–70. doi: 10.1007/s10140-014-1231-3 [DOI] [PubMed] [Google Scholar]
- 12. Tamburini N, Carriel N, Cavallesco G, Molins L, Galeotti R, Guzmán R, et al. Technical results, clinical efficacy and predictors of outcome of intercostal arteries embolization for hemothorax: a two-institutions’ experience. J Thorac Dis 2019; 11: 4693–99. doi: 10.21037/jtd.2019.10.27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lee CM, Jeon CH, Lee R, Kwon H, Kim CW, Kim JH, et al. Traumatic hemothorax caused by thoracic wall and intrathoracic injuries: clinical outcomes of transcatheter systemic artery embolization. Taehan Yongsang Uihakhoe Chi 2021; 82: 923–35. doi: 10.3348/jksr.2020.0116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Yoon W, Kim JK, Kim YH, Chung TW, Kang HK. Bronchial and nonbronchial systemic artery embolization for life-threatening hemoptysis: a comprehensive review. Radiographics 2002; 22: 1395–1409. doi: 10.1148/rg.226015180 [DOI] [PubMed] [Google Scholar]
- 15. Chun JY, Morgan R, Belli AM. Radiological management of hemoptysis: a comprehensive review of diagnostic imaging and bronchial arterial embolization. Cardiovasc Intervent Radiol 2010; 33: 240–50. doi: 10.1007/s00270-009-9788-z [DOI] [PubMed] [Google Scholar]
- 16. Filippiadis DK, Binkert C, Pellerin O, Hoffmann RT, Krajina A, Pereira PL. Cirse quality assurance document and standards for classification of complications: the cirse classification system. Cardiovasc Intervent Radiol 2017; 40: 1141–46. doi: 10.1007/s00270-017-1703-4 [DOI] [PubMed] [Google Scholar]
- 17. Chemelli AP, Chemelli-Steingruber IE, Bonaros N, Luckner G, Millonig G, Seppi K, et al. Coil embolization of internal mammary artery injured during central vein catheter and cardiac pacemaker lead insertion. Eur J Radiol 2009; 71: 269–74. doi: 10.1016/j.ejrad.2008.04.024 [DOI] [PubMed] [Google Scholar]
- 18. Corvino F, Giurazza F, Cangiano G, Cavaglià E, Amodio F, De Magistris G, et al. Safety and effectiveness of transcatheter embolization in the treatment of internal mammary artery injuries. Radiol Med 2018; 123: 369–77. doi: 10.1007/s11547-017-0844-5 [DOI] [PubMed] [Google Scholar]
- 19. Werner N, Bauer T, Hochadel M, Zahn R, Weidinger F, Marco J, et al. Incidence and clinical impact of stroke complicating percutaneous coronary intervention: results of the Euro heart survey percutaneous coronary interventions registry. Circ Cardiovasc Interv 2013; 6: 362–69. doi: 10.1161/CIRCINTERVENTIONS.112.000170 [DOI] [PubMed] [Google Scholar]
- 20. Geibprasert S, Pongpech S, Armstrong D, Krings T. Dangerous extracranial-intracranial anastomoses and supply to the cranial nerves: vessels the neurointerventionalist needs to know. AJNR Am J Neuroradiol 2009; 30: 1459–68. doi: 10.3174/ajnr.A1500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. An JY, Song IU, Kim WJ, Kim JS, Kim YI, Lee KS. Posterior cervical spinal cord infarction following thyrocervical trunk embolization. Eur Neurol 2008; 59: 200–201. doi: 10.1159/000114046 [DOI] [PubMed] [Google Scholar]
- 22. Perrucci L, Graziano M, Ferrante Z, Salviato E, Carnevale A, Galeotti R. Pitfalls in the embolisation of a thyrocervical trunk bleeding: a case report. Patient Saf Surg 2020; 14: 19: 19. doi: 10.1186/s13037-020-00244-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wicky S, Meuwly J-Y, Doenz F, Uské A, Schnyder P, Denys A. Life-threatening vascular complications after central venous catheter placement. Eur Radiol 2002; 12: 901–7. doi: 10.1007/s003300101018 [DOI] [PubMed] [Google Scholar]
- 24. HUELKE DF. A study of the transverse cervical and dorsal scapular arteries. Anat Rec 1958; 132: 233–45. doi: 10.1002/ar.1091320302 [DOI] [PubMed] [Google Scholar]
- 25. Takafuji T, Sato Y. Study on the subclavian artery and its branches in Japanese adults. Okajimas Folia Anat Jpn 1991; 68: 171–85. doi: 10.2535/ofaj1936.68.2-3_171 [DOI] [PubMed] [Google Scholar]