Abstract
Background:
Smoking cannabis using a tobacco-derived cigar shell or wrap, called blunt smoking, exposes individuals to non-trivial amounts of nicotine. The extent smoking blunts impact the risk of initiating other tobacco products is not well understood. We investigated if past-year blunt smoking is related to the risk of initiating cigarettes, e-cigarettes, and cigars.
Methods:
We obtained data on a nationally representative, non-institutionalized, civilian cohort of US residents aged 12 years and older who had never used cigarettes, e-cigarettes, or any cigar at baseline and surveyed annually for three years from the Population Assessment of Tobacco and Health Study. We estimated the proportional hazard (odds) of initiating these tobacco products associated with past-year blunt smoking, non-blunt cannabis use, or neither using discrete-time survival analyses.
Results:
Smoking blunts increased the risk of starting cigarettes (OR = 4.5), e-cigarettes (OR = 3.7), and cigars (OR = 6.7) compared to using neither blunts nor cannabis. Non-blunt cannabis use also increased the risk of starting cigarettes (OR = 4.0) but moderately for e-cigarettes (OR = 2.8) and any cigar (OR = 2.2). Blunt use was strongly related to starting combustible tobacco (cigarettes or cigars; OR = 9.0) and any three tobacco products (OR = 10.9). Exploratory findings showed that cigarillos drove cigar results and effect modification by age, race/ethnicity, and sex.
Conclusions:
People who smoke blunts risk starting cigarettes, e-cigarettes, and cigars more than those who abstain from cannabis. Blunts may contribute to tobacco initiation above cannabis alone.
Keywords: Blunts, cannabis, cigarette, e-cigarette, cigar, cigarillo
Introduction
Blunt smoking involves removing some or all loose tobacco from a cigar and replacing it with cannabis. Blunt smoking originated in and has been the most studied in the United States (US), where 12% of young adults and 4% of youth smoked blunts in the past month as of 2014 (Montgomery & Mantey, 2017a, 2017b). Among people using cannabis in the past year surveyed in 2009–2012, 40% smoked a blunt in the past month, and 8% smoked blunts daily or near-daily (Fairman, 2015). People who smoke blunts are disproportionately young adults, male, and Black (Corey et al., 2018; Montgomery & Mantey, 2017b). Outside the US, national prevalence estimates of blunt smoking are lacking. Nonetheless, one study found that around 35% of Ontario, Canada youth who used cannabis in the past 12 months smoked blunts (Kolar et al., 2020). In another study, 6.1% of adults who used cannabis in the past year in Mexico smoked blunts, 2.8% in Brazil, and 2.0% in France compared to 3.4% in the US (Hindocha et al., 2016). These findings suggest blunt smoking is not strictly a US phenomenon.
Cannabis use poses health risks, but a significant concern is whether blunt smoking contributes to tobacco-related harms (U.S. Department of Health and Human Services, 2012; Volkow et al., 2014) for youth and young adults. Although cigarette initiation has declined among youth, it has increased among young adults (Cantrell et al., 2018). Studies also suggest little change in cigar use trends among youth and young adults and increased use in specific populations, like Black women (East et al., 2021; Weinberger et al., 2019). Blunts are a concern for further tobacco use because they contain non-trivial amounts of nicotine (1.2 to 6.0 mg), exposing individuals who smoke them to significant levels, but are perceived as less harmful than cigarettes or cigars (Nardone et al., 2019; Peters et al., 2016; Sterling et al., 2016). Since cannabis use alone increases tobacco use (Cornacchione Ross et al., 2020; Patton et al., 2005; Weinberger et al., 2021), it is unclear whether blunt smoking might contribute further to this risk.
Significant gaps remain in our understanding of whether blunt smoking contributes to the risk of using other tobacco products. For example, Hu and colleagues (2008) observed that youth who initiated smoking blunts before cigarette use increased their likelihood of early and sustained nicotine dependence. Audrain-McGovern and others (2019) found that youth who had ever smoked blunts were likelier to progress to current cigar use. Unfortunately, neither of these studies assessed the risk of initiating cigarettes or cigars. More recently, Mayer and colleagues (2019) reported that Connecticut and California youth who smoked blunts were twice as likely to initiate combustible tobacco (cigarettes or cigars) compared to youth who never used cannabis but not compared to non-blunt cannabis use.
We sought to build upon this prior literature by investigating whether past-year blunt smoking is associated with initiating different tobacco products in a cohort of youth and adults followed prospectively over three years. We examined the independent risk of initiating cigarettes and cigars but also explored the initiation of either combustible product, as in Mayer et al. (2019). Further, given the epidemic of nicotine vaping among youth and the links between cannabis and e-cigarette use, we additionally examined e-cigarette initiation (Chen et al., 2018; Seo et al., 2020). We hypothesized that people who smoked blunts in the past year would be at an increased risk of starting to use cigarettes, e-cigarettes, and cigars for the first time. The increased risk would be relative to those who used cannabis but not blunts (non-blunt cannabis) and those who used neither. We further expected that the risk would be greater for cigar initiation, given their use in blunt construction, followed by cigarettes and e-cigarettes. Lastly, we explored initiation by cigar type (traditional, cigarillo, and filtered cigars), any of the three tobacco products studied (cigarettes, e-cigarettes, or cigars), and interactions with age, race, and sex.
Methods
Study Design
The National Institutes of Health (NIH), through the National Institute on Drug Abuse (NIDA), has partnered with the Food and Drug Administration’s (FDA) Center for Tobacco Products (CTP) to conduct the Population Assessment of Tobacco and Health (PATH) Study. The PATH Study is an ongoing, nationally representative, longitudinal cohort study of non-institutionalized adults and youth in the US. It uses audio computer-assisted self-interviews (ACASI) available in English and Spanish to collect self-reported information on tobacco-use patterns and associated health behaviors. Recruitment for the Wave 1 cohort employed a stratified address-based, area-probability sampling design at Wave 1 that oversampled adults who use tobacco, young adults (18 to 24 years), and Black adults. An in-person screener was used at Wave 1 to randomly select youths and adults from households for participation in the study (Hyland et al., 2017). We excluded youth interviewed for the first time in Waves 2 and 3 because the PATH Study did not ask them about non-blunt cannabis use in the past year.
The PATH Study surveyed a total of 13,651 youth (12–17) and 32,320 adults (18+) at Wave 1 (September 2013-December 2014). Weighted response rates for youth and adults were 78.4% and 74.0%, respectively. Interviewers surveyed participants for Waves 2–4 close to their 1-year anniversary of participation in the previous wave. The unweighted attrition rate among the Wave 1 cohort was 16.4% at Wave 2, 21.8% at Wave 3, and 27.4% at Wave 4. We analyzed the publicly available data from the PATH Study Waves 1–4 Public Use Files (PUF) (United States Department of Health and Human Services et al., 2012). We excluded a small number of participants (n=6) who requested their data removed. Further details regarding the PATH Study design and methodology are published elsewhere (Hyland et al., 2017). Information about interviewing procedures, questionnaires, sampling, weighting, response rates, and data access are described in the PATH Study PUF User Guide found at https://doi.org/10.3886/Series606. Westat administered the PATH Study, and the Westat Institutional Review Board approved the protocols. All adult respondents gave informed consent. Youth respondents gave assent while their parent/legal guardian provided consent.
Measures
Outcomes: Initiation of Cigarettes, E-Cigarettes, and Cigars
We had three primary outcomes: time to the first use of cigarettes, e-cigarettes, and any cigar (traditional, cigarillo, or filtered cigars) among those at risk for those outcomes at baseline (Wave 1). We defined time in terms of years, with each follow-up wave occurring, on average, one year after the last interview. Respondents were at-risk if they had never used the tobacco product at baseline. We coded respondents as missing if they had ever used the tobacco product at baseline since they could not be at risk for initiation in subsequent waves (they would be considered left-censored). Respondents were asked if they had used each tobacco product in the preceding 12 months at each annual follow-up wave. The first wave that participants used the tobacco product defined the time-to-event for those who experienced the event—the last wave of continuous observation defined the time-to-event for those who did not experience the event (censored). Therefore, the first wave that at-risk respondents could initiate tobacco product use would be Wave 2. Our exploratory outcomes included the time to the first use of a specific cigar type (traditional, cigarillo, and filtered), any combustible tobacco (cigarettes or cigars), and any three product types (cigarettes, e-cigarettes, or any cigar).
At Wave 1 (2013–2014), respondents were asked about e-cigarettes and provided examples of popular brands, including NJOY®, Blu®, or Smoke Everywhere®. Respondents were asked more broadly about e-cigarettes and other electronic nicotine devices (ENDS) starting in Wave 2 (2014–2016). Descriptions included e-cigarettes, e-cigars, e-pipes, e-hookahs, personal vaporizers, vape pens, and hookah pens, with brand examples updated to reflect market popularity and new brands (e.g., Juul®).
Exposure of Interest: Past-Year Blunt Use
The PATH Study defined blunts as, “Sometimes people take tobacco out of a cigar, cigarillo or filtered cigar and replace it with marijuana. This is sometimes called a ‘blunt’‖. Respondents reported whether they had smoked blunts in the past 12 months at each wave. Separately, respondents said if they last used “marijuana, hash, THC, grass, pot or weed” in the past 12 months. We defined past-year blunt use as using blunts, cannabis but not blunts (non-blunt cannabis), or neither in the past 12 months.
Covariates
Our conceptual models considered time-invariant and time-varying covariates. Time-invariant covariates included the respondents’ sex, race or ethnicity, and Census region of residence in Wave 1. Time-varying covariates included age, income, other substance use, household tobacco use, and mental health assessed in Waves 1–4. Adults and parents/guardians of youth reported total annual family income. All respondents reported past-month use (yes/no) of cigarettes, e-cigarettes, any cigars, other tobacco products (pipes, hookah, and smokeless), alcohol, and other drug use (Ritalin®, Adderall®, painkillers, sedatives, tranquilizers, cocaine or crack, stimulants like methamphetamine or speed, and any other drugs like heroin, inhalants, solvents, or hallucinogens). Both adults and youth reported their recent mental health and whether they lived with a tobacco user. The PATH Study assessed mental health problems using a modified Global Appraisal of Individual Needs − Short Screener (GAIN-SS) (Dennis et al., 2006). Following Conway et al. (2018), we summed four items for the internalizing problem subscale (range: 0–4) and seven items for the externalizing problem subscale (range: 0–7); scale reliability (Cronbach’s alpha) was 0.82 and 0.72, respectively.
Statistical Analysis
Missing Data and Bias
The PATH Study imputed missing data on sex, race/ethnicity, and age at Waves 1 and 4 using responses from the household screener and statistical imputation; there was no missing data on the Census region. We logically imputed missing values on age for a small number (n=6) of participants using information from other waves. Annual family income had the most missing data, ranging from 6.2% (Wave 4) to 9.8% (Wave 1, adults only). The PATH Study did not assess income for youth via parental report until Wave 2. We imputed missing data on income based on the respondent’s median value of responses across all waves rounded down to the nearest integer. Pairwise correlations between respondents’ median and observed values were high (>0.88). Imputation reduced missing data on income for adults to less than 3.4% and less than 10.7% for youth. Otherwise, we based analyses on complete cases.
Lifetables and Discrete-Time Survival Analysis
We initially examined time to tobacco initiation using a lifetable approach and stratifying by past-year blunt use status. We then conducted a series of discrete-time survival analyses (DTSA) to estimate the hazard of initiating cigarettes, e-cigarettes, and any cigar associated with past-year blunt and non-blunt cannabis use, controlling for time-invariant and time-varying covariates. Standard logistic regression models can estimate the proportional hazards (as odds ratios) after the data are expanded to person-years, such that respondents contribute a row of data for each year observed (Ziegel & Allison, 1997). In addition to providing relative risk measures, we estimated absolute numbers of tobacco initiates in the population by past-year blunt use and non-blunt cannabis use status based on our models. In exploratory analyses, we examined differences in initiation by cigar type (traditional, cigarillo, and filtered cigars), combustible tobacco use (cigarettes or any cigar), and any tobacco use (cigarettes, e-cigarettes, or cigars). Finally, we explored effect modification by age, race/ethnicity, and sex by including model interaction terms, and then estimated the predicted probability of initiating each tobacco product. All of our analyses except the lifetables accounted for the PATH Study’s complex survey design and respondent non-response across waves using balanced repeated replication (BRR) weights (Wave 1 Cohort) with Fay’s adjustment (p = 0.3). We conducted all analyses using Stata version 17 (StataCorp, 2021).
Results
Characteristics of Participants At Risk for Tobacco Initiation at Baseline
Most people at baseline (Wave 1) had never used e-cigarettes (82.9%) or any cigar (62.6%), while a minority had never smoked cigarettes (38.1%; Table 1). Those who had never vaped e-cigarettes used blunts in the past year at higher rates (2.7%) than those who had never smoked any cigar (0.9%) or cigarettes (1.4%). Most at-risk respondents were female, especially those who had never used any cigar (63.3%). People who never smoked cigarettes were younger (51.3% under age 35), while those who had not initiated e-cigarettes or any cigar were older (33.8% and 38.4% under age 35, respectively). Most at-risk respondents were non-Hispanic White, but non-Whites were more likely to report never smoking cigarettes (44.7%) than e-cigarettes (36.0%) or any cigar (38.4%). Most people lived in households earning below the US median in 2014 (approximately $50,000), and a plurality lived in the South. We present distributions for all covariates measured at Wave 1 in Supplemental Table S1.
Table 1.
Characteristics of the PATH Study Wave 1 Cohort Who Never Used Cigarettes, E-Cigarettes, or Any Cigar
| Cigarettes | E-Cigarettes | Any Cigar | ||||
|---|---|---|---|---|---|---|
| Covariates1 | n | Wgt% | n | Wgt% | n | Wgt% |
|
| ||||||
| Never Used @ Wave 1 | ||||||
| Total | 18,907 | 38.1% | 32,888 | 82.9% | 26,414 | 62.6% |
| Past-Year Blunt Use | ||||||
| Neither | 17,705 | 96.4% | 29,007 | 92.9% | 24,334 | 95.8% |
| Non-Blunt Cannabis | 607 | 2.2% | 1,890 | 4.5% | 1,330 | 3.3% |
| Blunts | 472 | 1.4% | 1,679 | 2.7% | 527 | 0.9% |
| Sex | ||||||
| Male | 8,962 | 42.5% | 16,420 | 47.1% | 10,986 | 36.7% |
| Female | 9,945 | 57.5% | 16,468 | 52.9% | 15,428 | 63.3% |
| Age | ||||||
| 12–14 | 6,557 | 11.8% | 6,618 | 5.5% | 6,602 | 7.5% |
| 15–17 | 5,235 | 9.8% | 5,538 | 4.7% | 5,671 | 6.7% |
| 18–24 | 3,144 | 14.4% | 5,209 | 9.6% | 3,902 | 10.6% |
| 25–34 | 1,168 | 15.3% | 3,503 | 13.9% | 2,277 | 13.6% |
| 35 or older | 2,801 | 48.7% | 12,015 | 66.2% | 7,956 | 61.6% |
| Race/Ethnicity | ||||||
| White | 9,127 | 55.3% | 17,858 | 64.0% | 13,750 | 60.1% |
| Black | 3,071 | 14.1% | 5,162 | 12.0% | 3,905 | 12.3% |
| Other2 | 1,734 | 10.8% | 2,637 | 8.0% | 2,253 | 9.1% |
| Hispanic | 4,975 | 19.7% | 7,231 | 16.0% | 6,506 | 18.5% |
| Total Family Income3 | ||||||
| Less than $10K | 2,531 | 14.0% | 4,873 | 12.2% | 4,041 | 13.8% |
| $10K to $24,999 | 3,463 | 19.8% | 6,450 | 19.6% | 5,489 | 21.6% |
| $25K to $49,999 | 3,966 | 22.4% | 7,028 | 22.6% | 5,741 | 23.0% |
| $50K to $99,999 | 4,110 | 25.5% | 7,053 | 25.7% | 5,375 | 24.4% |
| $100K or more | 3,247 | 18.4% | 5,390 | 19.9% | 3,848 | 17.2% |
| Census Region | ||||||
| Northeast | 2,964 | 18.2% | 5,229 | 18.4% | 4,163 | 18.6% |
| Midwest | 3,965 | 19.4% | 7,393 | 21.1% | 5,836 | 20.6% |
| South | 7,210 | 38.1% | 12,463 | 37.1% | 10,049 | 37.4% |
| West | 4,768 | 24.2% | 7,803 | 23.4% | 6,366 | 23.4% |
Data: Population Assessment of Tobacco and Health Study, Wave 1 Cohort (n=45,971)
The table excluded respondents with missing data on each variable
This category included non-Hispanic Asian, American Indian, Alaska Native, Native Hawaiian, other Pacific Islander, and those indicating more than one race.
Total family income for youth was not assessed until Wave 2. Youth total family income for Wave 1 was imputed based on their median values assessed across Waves 2–4.
Cigarette, E-Cigarette, and Any Cigar Initiation and Associations with Past-Year Blunt Use
Over the study period (3 years), we observed a greater proportion of people starting e-cigarettes (19.6%) than cigarettes (13.3%) or any cigar (12.2%; see Supplemental Figure S1). Around half of the people using blunts in the past year initiated cigarettes (46.1%), e-cigarettes (55.9%), or any cigar (50.4%; Figure 1). Meanwhile, people using non-blunt cannabis started these tobacco products at moderate rates (27.1%, 35.4%, and 17.7%, respectively). By contrast, those who used neither blunts nor cannabis at baseline initiated these tobacco products at the lowest rates (7.5%, 13.9%, and 6.8%, respectively). Thus, this evidence shows higher tobacco initiation related to past-year blunt use and, to a lesser extent, non-blunt cannabis use.
Figure 1.
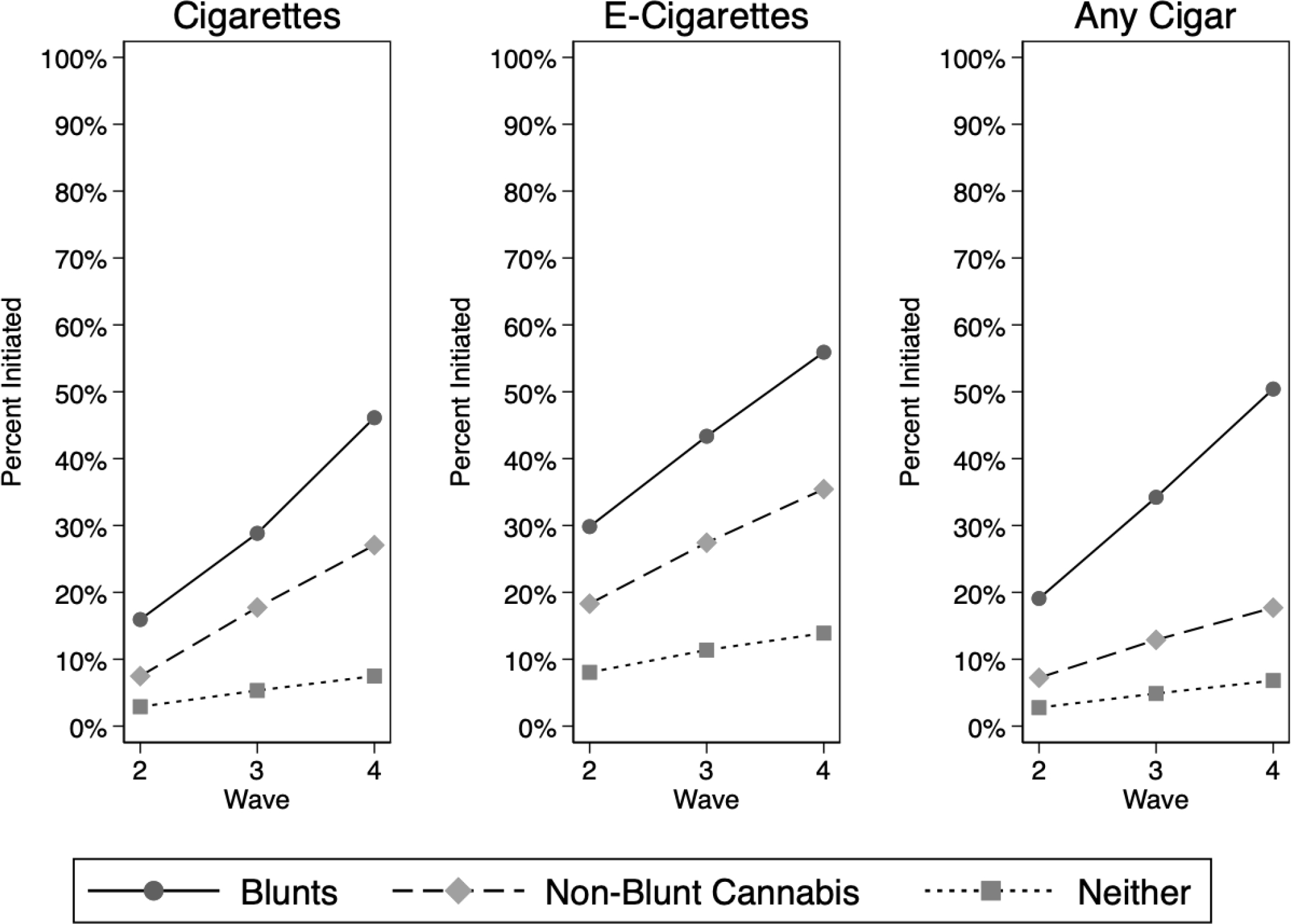
Cumulative percentage of the PATH Study Wave 1 Cohort initiating cigarettes, e-cigarettes, and any cigar by past-year blunt use.
Our regression analyses confirmed a positive association between past-year blunt use and tobacco initiation, even after accounting for multiple possible confounders (Table 2). People who used blunts elevated their odds of starting cigarettes (OR = 4.5, 95% CI [3.6, 5.6]), as did those who used non-blunt cannabis (OR = 4.0, 95% CI [3.0, 5.3]) relative to those who used neither, and we did not observe differences in the odds of cigarette initiation between those who used blunts versus non-blunt cannabis. By contrast, the odds of initiating e-cigarettes and any cigar differed between blunts versus non-blunt cannabis. Those who smoked blunts were likelier to initiate e-cigarettes (OR = 3.7, 95% CI [3.2, 4.3]) than those who used non-blunt cannabis (OR = 2.8, 95% CI [2.4, 3.3]; adjusted Wald test: F[1,99] = 7.91; p = 0.006). People smoking blunts were also likelier to start smoking any cigar (OR = 6.7, 95% CI [5.6, 7.9]) than those who used non-blunt cannabis (OR = 2.2, 95% CI [1.7, 2.8]; adjusted Wald test: F[1,99] = 115.49; p < 0.001). We present unadjusted and complete adjusted model estimates in Supplemental Tables S2 and S3, respectively. Our data suggest that past-year blunt use is more strongly associated with starting to smoke any cigar than cigarettes or e-cigarettes.
Table 2.
Association Between Past-Year Blunt Use and Initiating Cigarettes, E-Cigarettes, and Any Cigar
| Cigarettes1,3,4 | E-Cigarettes1,2,4 | Any Cigar1,2,3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | |
|
| |||||||||
| Past-Year Blunt Use | |||||||||
| Neither (ref.) | 1.0 | 1.0 | 1.0 | ||||||
| Non-Blunt Cannabis | 4.0 | (3.0, 5.3) | <0.001 | 2.8 | (2.4, 3.3) | <0.001 | 2.2 | (1.7, 2.8) | <0.001 |
| Blunts | 4.5 | (3.6, 5.6) | <0.001 | 3.7 | (3.2, 4.3) | <0.001 | 6.7 | (5.6, 7.9) | <0.001 |
Data: Population Assessment of Tobacco and Health (PATH) Study Public Use Files (PUF), Waves 1–4
Model controlled for sex, age, race/ethnicity, annual family income, Census region, past-month other tobacco use, past-month alcohol use, past-month drug use, living with a tobacco user, and recent internalizing and externalizing problems
Model controlled for past-month cigarette use
Model controlled for past-month e-cigarette use
Model controlled for past-month traditional cigar, cigarillo, and filtered cigar use
To place these results in absolute terms, our models estimated that 2.6 million people in the US aged 12 years and older started smoking cigarettes over the study period (see Supplemental Table S4). About 13% (335,946) of these new initiates might be explained by past-year blunt smoking and 9.4% (242,878) by non-blunt cannabis. For 7.6 million e-cigarette initiates, 9.8% (741,993) and 10.8% (815,455) might be due to blunts and non-blunt cannabis, respectively. Lastly, there were about 3.6 million initiates of any cigars, with 15.4% (551,047) due to blunts and another 6.6% (235,948) from non-blunt cannabis. Our evidence indicates that blunt and non-blunt cannabis use may significantly contribute to the number of people who start tobacco.
Differences By Cigar Type: Traditional Cigars, Cigarillos, and Filtered Cigars
Considering the strong association between past-year blunt smoking and any cigar initiation, we explored differences by cigar type. We found most respondents had never used traditional cigars (75.8%), cigarillos (87.5%), or filtered cigars (87.5%) at baseline (data not shown in tables). Over the study period, more people had started smoking traditional cigars (11.0%) than cigarillos (9.1%) or filtered cigars (6.3%; Supplemental Figure S1). Those who used blunts in the past year initiated traditional cigars (35.0%), cigarillos (44.1%), and filtered cigars (23.5%) at higher rates than those using non-blunt cannabis (12.7%, 10.7%, and 6.5%, respectively) or neither (6.3%, 4.5%, and 3.3%, respectively; Figure 2). These findings indicate that past-year blunt smoking may be significantly related to starting to smoke cigarillos.
Figure 2.
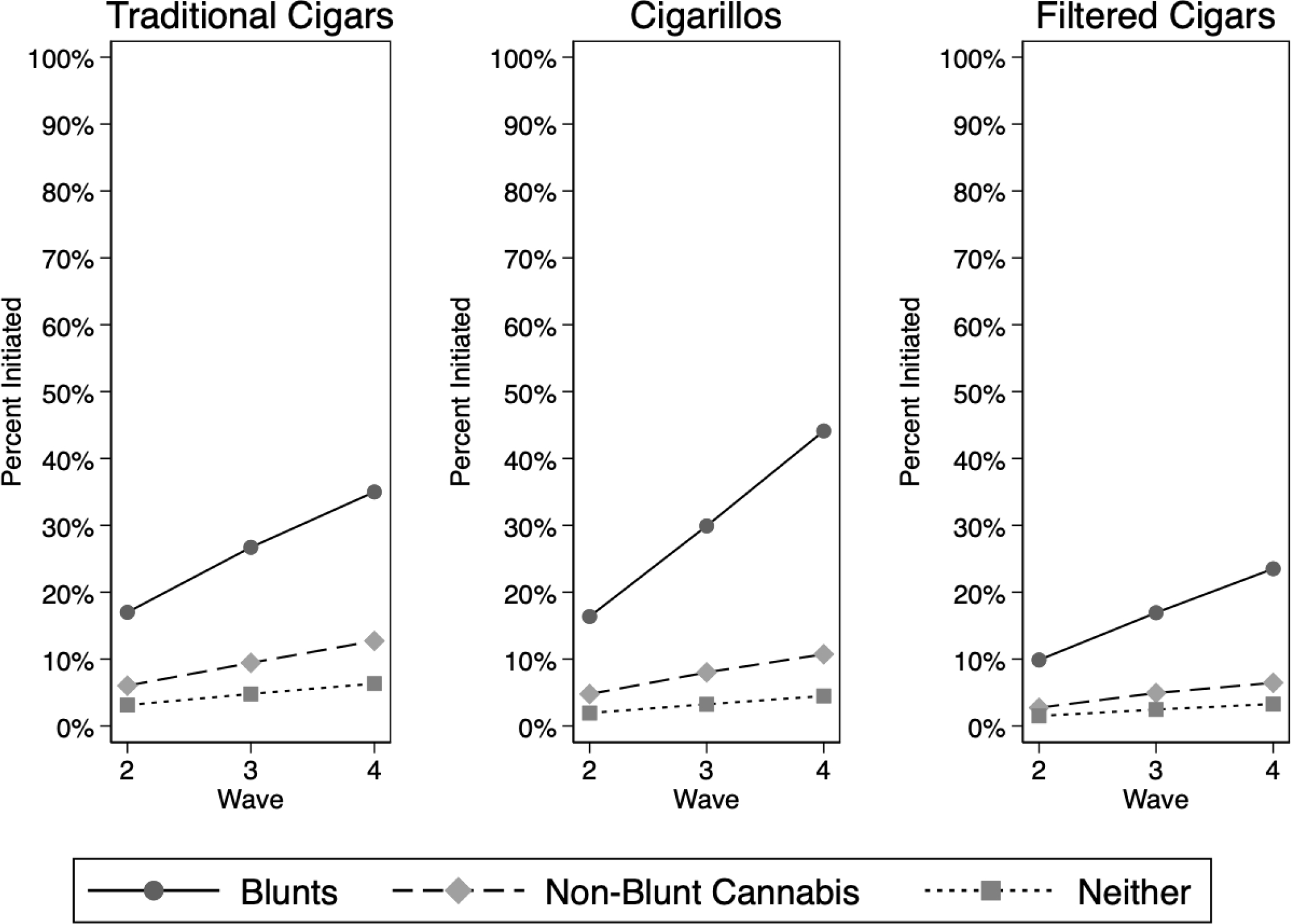
Cumulative percentage of the PATH Study Wave 1 Cohort initiating traditional cigars, cigarillos, and filtered cigars by past-year blunt use.
Our regression results confirmed a strong association between past-year blunt smoking and cigarillo initiation (Table 3). People smoking blunts were much likelier to begin smoking cigarillos (OR = 6.5, 95% CI [5.5,7.8]) than non-blunt cannabis (OR = 1.8, 95% CI [1.4, 2.3]) or neither. By contrast, blunt and non-blunt cannabis use modestly increased the odds of starting traditional (ORs = 2.2 and 1.6, respectively) or filtered cigars (OR = 1.3 and 1.2, respectively). We present unadjusted estimates in Supplemental Table S5. These results suggest that the association between blunt use and initiating any cigars may be primarily due to cigarillos.
Table 3.
Association Between Past-Year Blunt Use and Initiating Traditional, Cigarillo, and Filtered Cigars
| Traditional Cigars1,3,4 | Cigarillos1,2,4 | Filtered Cigars1,2,3 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | OR | 95% CI | p-value | |
|
| |||||||||
| Past-Year Blunt Use | |||||||||
| Neither (ref.) | 1.0 | 1.0 | 1.0 | ||||||
| Non-Blunt Cannabis | 1.6 | (1.2, 2.1) | <0.001 | 1.8 | (1.4, 2.3) | <0.001 | 1.2 | (0.9, 1.5) | 0.284 |
| Blunts | 2.2 | (1.9, 2.7) | <0.001 | 6.5 | (5.5, 7.8) | <0.001 | 1.3 | (1.1, 1.6) | 0.016 |
Data: Population Assessment of Tobacco and Health (PATH) Study Public Use Files (PUF), Waves 1–4
Model controlled for sex, age, race/ethnicity, annual family income, Census region, past-month cigarette use, past-month e-cigarette use, past-month other tobacco use, past-month alcohol use, past-month drug use, living with a tobacco user, and recent internalizing and externalizing problems
Model controlled for past-month traditional cigar use
Model controlled for past-month cigarillo use
Model controlled for past-month filtered cigar use
Initiation of Combustible Tobacco or Any Three Tobacco Products Only
We next estimated the association between past-year blunt use and starting to use combustible tobacco (cigarettes or cigars), similar to Mayer et al. (2019), and starting any three of the tobacco products studied (cigarettes, e-cigarettes, or cigars). About one-third of respondents had never used a combustible product (34.2%) or any of the three tobacco products (33.6%; data not shown in tables). About 1-in-6 (17.6%) started using a combustible product, and almost a quarter (24.6%) started using any of the three products (Supplemental Figure S1). Almost two-thirds (63.0%) of people using blunts in the past year initiated a combustible product, while more than 3-in-4 (77.7%) initiated any tobacco (Figure 3). Comparatively, we observed lower rates for non-blunt cannabis use (34.8% and 54.3%, respectively) and neither (10.4% and 17.0%, respectively).
Figure 3.
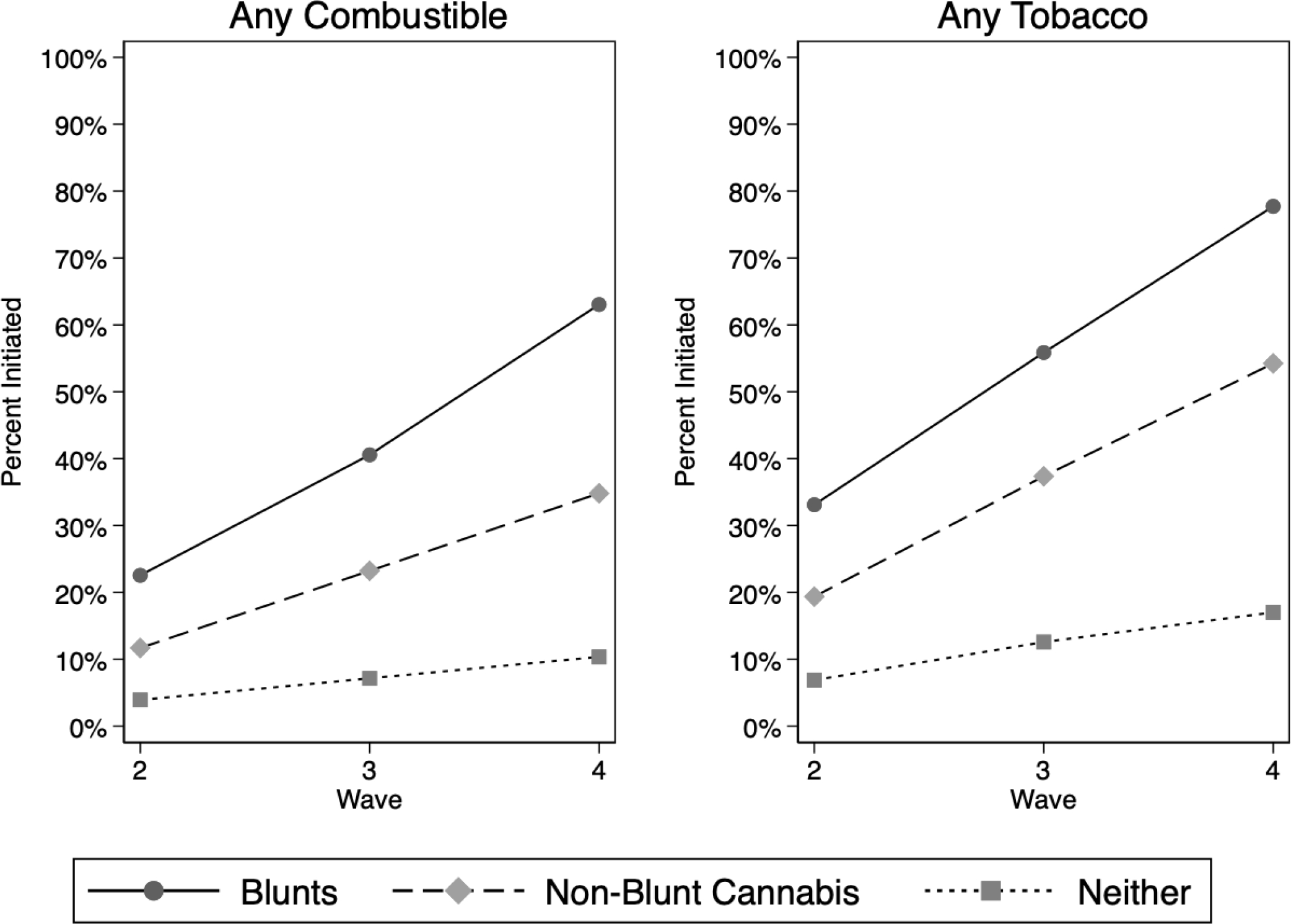
Cumulative percentage of the PATH Study Wave 1 Cohort initiating any combustible tobacco (cigarettes or cigars) and any tobacco (cigarettes, e-cigarettes, or cigars) by past-year blunt use.
Our regression analyses corroborated these findings (Table 4). Past-year blunt smoking significantly elevated the odds of starting combustible products (OR = 9.0, 95% CI [7.6, 10.8]) or any of the three products (OR = 10.9, 95% CI [9.0, 13.1]) relative to modest associations with non-blunt cannabis use or our reference group of neither. We present unadjusted estimates in Supplemental Table S6. These findings demonstrate a stronger association between past-year blunt use and tobacco initiation.
Table 4.
Association Between Past-Year Blunt Use and Initiating Combustible Tobacco and Any Tobacco
| Combustible Tobacco1,2,3 | Any Tobacco1,2 | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | |
|
| ||||||
| Past-Year Blunt Use | ||||||
| Neither (ref.) | 1.0 | 1.0 | ||||
| Non-Blunt Cannabis | 3.8 | (3.0, 4.8) | <0.001 | 4.5 | (3.6, 5.5) | <0.001 |
| Blunts | 9.0 | (7.6,10.8) | <0.001 | 10.9 | (9.0,13.1) | <0.001 |
Data: Population Assessment of Tobacco and Health (PATH) Study Public Use Files (PUF), Waves 1–4
Any tobacco included cigarettes, e-cigarettes, or cigars; Combustible tobacco included cigarettes or cigars
Model controlled for sex, age, race/ethnicity, annual family income, Census region, past-month other tobacco use, past-month alcohol use, past-month drug use, living with a tobacco user, and recent internalizing and externalizing problems
Model controlled for past-month e-cigarette use
Differences by Age, Race/Ethnicity, and Sex
Lastly, we explored effect modification by age, race/ethnicity, and sex by estimating the predicted probabilities of tobacco initiation (see Supplemental Figures S2–S10). For example, 15–17-year-olds who smoked blunts had a higher predicted probability of initiating cigarettes and e-cigarettes than 18–24-year-olds who smoked blunts, but these groups looked similar for starting any cigar (Figures S2–S4). Whites and Hispanics who smoked blunts had a higher probability of initiating cigarettes and e-cigarettes than Blacks. Still, Blacks who smoked blunts had the highest probability of starting any cigar (Figures S5–S7). Finally, males who smoked blunts had a higher probability of initiating e-cigarettes and any cigar than females who smoked blunts (Figures S9–S10).
Discussion
We had expected people who smoked blunts, which combine tobacco and cannabis, would elevate their risk of starting to use cigarettes, e-cigarettes, and cigars. Our data confirm this hypothesis. We find that people who smoked blunts in the past year are about four times likelier to start using cigarettes, three times likelier to start e-cigarettes, and six times likelier to start any cigar than people who did not smoke blunts or cannabis. These findings remained robust after accounting for possible confounders, such as sociodemographics, current use of other tobacco, alcohol, and drugs, living with a tobacco user, and internalizing and externalizing problems. Further, we observed stronger associations for initiating a combustible product (cigarettes or cigars) or any three of the tobacco products studied. This finding suggests residual confounding by past tobacco use may be insufficient to explain our results. Mayer and colleagues (2019) previously reported a two-fold association between lifetime blunt use and combustible tobacco product initiation one year later among youth in California and Connecticut. However, they did not find differences between blunt and non-blunt cannabis use. By contrast, we assessed more recent exposures, observed participants longer, and benefited from a larger, more nationally representative sample of youth and adults.
Our findings are consistent with a growing literature showing cannabis use as a risk factor for tobacco use, typically cigarettes – sometimes referred to as the “reverse gateway” theory (Agrawal et al., 2008; Badiani et al., 2015; Kristman-Valente et al., 2017; Patton et al., 2005). One explanation for the co-use of tobacco and cannabis is that people commonly inhale both, and such familiarity with one supports the use of the other (Agrawal & Lynskey, 2009). Co-use might also result from overlapping genetic and environmental factors, such as a predisposition for externalizing and drug use behaviors, peer influences, and availability (Agrawal et al., 2012). Additionally, exposure to blunts might have reduced people’s tobacco harm perception, produced nicotine cravings or withdrawal, or habituated individuals to the taste and effects of inhaling tobacco smoke. Qualitative studies also report the practice of blunt “chasing,” where a peer group passes around a blunt followed by a cigar or cigarette (Antognoli et al., 2018; Sifaneck et al., 2005). Therefore, social pressure and peer aspects could also play a unique role.
We observed differences in the risk of tobacco product initiation associated with blunt use. Blunt use was strongly associated with any cigar use, especially cigarillos. Cigarillos are a common choice for making blunts (Giovenco et al., 2016). People who smoke blunts might smoke cigars as a substitute when cannabis is unavailable or due to other legal or social restrictions (Antognoli et al., 2018). People also perceive blunts as less harmful than cigars and cigars as less harmful than cigarettes (Sinclair et al., 2013; Sterling et al., 2016); therefore, smoking blunts might serve as a gateway to other tobacco use, especially cigars.
Our finding that people who smoked blunts were likelier to start vaping e-cigarettes may be novel. Prior studies have reported the co-occurrence of e-cigarettes and cannabis (Simon et al., 2017; Wills et al., 2021) or that e-cigarette use increases the risk of using cannabis (Dai et al., 2018; Sun et al., 2022). People may perceive blunts and e-cigarettes as less harmful than cigarettes and cigars (Berg et al., 2014; Sterling et al., 2016). Therefore, health concerns might prompt those who smoke blunts to be more receptive to trying e-cigarettes when initiating another tobacco product. Additionally, studies find that e-cigarettes are an attractive choice for consuming tobacco in places where cigarettes are prohibited (Sapru et al., 2020). Devices that can vape nicotine and THC may be an attractive alternative to those who smoke blunts for similar reasons, but studies have not confirmed this.
Despite these findings, we acknowledge limitations when interpreting these results. First, the PATH Study does not ask people about other forms of mixing tobacco and cannabis in a single preparation, such as in joints (spliffs), pipes, or bongs, which could confound our estimates. However, consuming cannabis without tobacco in these forms appears to be the preferred method in the US (Hindocha et al., 2016). Second, we do not know whether these findings will generalize to populations outside the US or to other forms of tobacco and cannabis co-administration. Mixing tobacco and cannabis inside a joint is common in Europe and Australia and may contribute to cigarette smoking (Belanger et al., 2011; Patton et al., 2005). Third, the PATH Study at Wave 1 asked participants questions about their lifetime cigar use before questions about blunts. Some participants might interpret blunt smoking as cigar use even if they never smoked a cigar except as a blunt. Misclassification would have led to incorrectly excluding such participants. Finally, the past-year use of blunts and non-blunt cannabis is a relatively crude measure of exposure to cannabis and tobacco via blunts. We lacked data on recent use (e.g., past month) or frequency of use which might better inform tobacco initiation risk and may be an avenue for future studies.
Our findings have implications for the co-marketing of tobacco products and cannabis within an environment of liberalized cannabis laws, such as in the US. First, we should reconsider the co-marketing of tobacco and cannabis. For example, tobacco companies market flavored cigars and wraps that share the exact name as a strain of cannabis (e.g., Kush, Pineapple Express, and Purple Haze) and are sold cheaper than cigars without a cannabis-related flavor (Delnevo et al., 2019). Co-marketing is also more prevalent in school neighborhoods with a higher proportion of younger residents (Henriksen et al., 2018). In April 2022, the US Food and Drug Administration (FDA) proposed new rules prohibiting flavored cigar products (Food and Drug Administration, 2022). Should this rule be implemented and withstand legal challenges, it will be essential to determine whether cigar-using behaviors will change among those who primarily use them for smoking blunts. Second, the co-use of blunts and e-cigarettes warrants further attention. For example, an earlier studying using PATH Study data found that a quarter of cannabis-using young adults had used an ENDS device for cannabis consumption (Seaman et al., 2020). Another recent study using PATH Study data reported a strong association between adolescent e-cigarette use and prevalent cannabis use 1-year later (Sun et al., 2022). Therefore, using ENDS to co-use nicotine and cannabis could appeal to those who use co-use tobacco and cannabis via blunts or vice versa. Finally, most patients who developed e-cigarette or vaping use-associated lung injury (EVALI) in July 2019 used ENDS products containing cannabis e-liquid (Ghinai et al., 2019). Nearly all (96%) used prefilled cartridges or pods in either a universal vape pen or a proprietary nicotine-containing product (e.g., Juul). Therefore, safeguards may be needed to limit the modification of ENDS to vape cannabis e-liquid and restrict the sale of universal vape pens capable of vaping both substances to reduce their appeal to youth.
To conclude, people who smoke blunts are at a greater risk of starting cigarettes, e-cigarettes, and cigars. Blunts may contribute to an increased risk of initiating cigars and e-cigarettes above the risk due to cannabis alone. However, further study is needed to determine if the added risk is due to the co-administration of tobacco and cannabis from blunts or other social factors. Future studies should investigate the extent blunt smoking contributes to other tobacco endpoints, such as escalation to daily or regular use, dependence, and difficulty quitting.
Supplementary Material
Highlights.
Smoking blunts increased the risk of starting cigarettes, e-cigarettes, and cigars.
E-cigarette and cigar initiation greater for blunt vs. non-blunt cannabis use.
Associations stronger for initiating any tobacco and combustible use.
Association between blunts and cigar initiation strongest for cigarillos.
Youth smoking blunts had higher odds of starting cigarettes and e-cigarettes.
Acknowledgments
We thank the following colleagues for their feedback and support: Dr. Daniela Marshall, Dr. Marushka L. Silveria, Dr. Colm Everard, Dr. Melisa R. Creamer, and Ms. Kellie Washington.
Funding:
Dr. Fairman is supported in part by a seed grant from the Vice Chancellor for Research and Innovation at UAMS. The PATH Study was supported with Federal funds from the National Institute on Drug Abuse (NIDA), National Institutes of Health (NIH), and the Center for Tobacco Products (CTP), Food and Drug Administration (FDA), Department of Health and Human Services, under contract to Westat (contract nos. HHSN271201100027C and HHSN271201600001C), and through an interagency agreement between NIH NIDA and FDA CTP. Heather L. Kimmel, Carlos Blanco, and Wilson M. Compton were substantially involved in the scientific management of and providing scientific expertise for contract nos. HHSN271201100027C and HHSN271201600001C.
Footnotes
Author Disclosures
Conflict of Interest
Compton reports long-term stock holdings in Pfizer Incorporate, General Electric Company, and 3M Companies unrelated to this manuscript. Other authors have no conflicts of interest to declare.
Disclosures: Compton reports long-term stock holdings in Pfizer Incorporate, General Electric Company, and 3M Companies unrelated to this manuscript. Other authors have no conflicts of interest to declare.
Disclaimers: The views and opinions expressed in this manuscript are those of the authors only and do not necessarily represent the views, official policy, or position of the US Department of Health and Human Services or any affiliated institutions or agencies.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Agrawal A, Budney AJ, & Lynskey MT (2012). The co-occurring use and misuse of cannabis and tobacco: a review. Addiction (Abingdon, England), 107(7), 1221–1233. 10.1111/j.1360-0443.2012.03837.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agrawal A, & Lynskey MT (2009). Tobacco and cannabis co-occurrence: does route of administration matter? Drug and Alcohol Dependence, 99(1–3), 240–247. 10.1016/j.drugalcdep.2008.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agrawal A, Madden PAF, Bucholz KK, Heath AC, & Lynskey MT (2008). Transitions to regular smoking and to nicotine dependence in women using cannabis. Drug and Alcohol Dependence, 95(1–2), 107–114. 10.1016/j.drugalcdep.2007.12.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antognoli E, Koopman Gonzalez S, Trapl E, Cavallo D, Lim R, Lavanty B, & Flocke S (2018). The Social Context of Adoles0063ent Co-Use of Cigarillos and Marijuana Blunts. Substance Use and Misuse, 53(4), 654–661. 10.1080/10826084.2017.1355388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Audrain-McGovern J, Rodriguez D, Alexander E, Pianin S, & Sterling KL (2019). Association Between Adolescent Blunt Use and the Uptake of Cigars. JAMA Network Open, 2(12), e1917001. 10.1001/jamanetworkopen.2019.17001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Badiani A, Boden JM, de Pirro S, Fergusson DM, Horwood LJ, & Harold GT (2015). Tobacco smoking and cannabis use in a longitudinal birth cohort: Evidence of reciprocal causal relationships. Drug and Alcohol Dependence, 150, 69–76. 10.1016/j.drugalcdep.2015.02.015 [DOI] [PubMed] [Google Scholar]
- Belanger RE, Akre C, Kuntsche E, Gmel G, Suris J-C, Bélanger RE, Akre C, Kuntsche E, Gmel G, Suris J-C, Belanger RE, Akre C, Kuntsche E, Gmel G, Suris J-C, Bélanger RE, Akre C, Kuntsche E, Gmel G, … Suris J-C (2011). Adding tobacco to cannabis--its frequency and likely implications. Nicotine & Tobacco Research : Official Journal of the Society for Research on Nicotine and Tobacco, 13(8), 746–750. 10.1093/ntr/ntr043 [DOI] [PubMed] [Google Scholar]
- Berg CJ, Stratton E, Schauer GL, Lewis M, Wang Y, Windle M, & Kegler M (2014). Perceived Harm, Addictiveness, and Social Acceptability of Tobacco Products and Marijuana Among Young Adults: Marijuana, Hookah, and Electronic Cigarettes Win. 10.3109/10826084.2014.958857, 50(1), 79–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantrell J, Bennett M, Mowery P, Xiao H, Rath J, Hair E, & Vallone D (2018). Patterns in first and daily cigarette initiation among youth and young adults from 2002 to 2015. 1–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen JC, Green KM, Arria AM, & Borzekowski DLGG (2018). Prospective predictors of flavored e-cigarette use: A one-year longitudinal study of young adults in the U.S. Drug and Alcohol Dependence, 191(July), 279–285. 10.1016/j.drugalcdep.2018.07.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conway KP, Green VR, Kasza KA, Silveira ML, Borek N, Kimmel HL, Sargent JD, Stanton CA, Lambert E, Hilmi N, Reissig CJ, Jackson KJ, Tanski SE, Maklan D, Hyland AJ, & Compton WM (2018). Co-occurrence of tobacco product use, substance use, and mental health problems among youth: Findings from wave 1 (2013–2014) of the population assessment of tobacco and health (PATH) study. Addictive Behaviors, 76(January), 208–217. 10.1016/j.addbeh.2017.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corey CG, Holder-Hayes E, Nguyen AB, Delnevo CD, Rostron BL, Bansal-Travers M, Kimmel HL, Koblitz A, Lambert E, Pearson JL, Sharma E, Tworek C, Hyland AJ, Conway KP, Ambrose BK, & Borek N (2018). US adult cigar smoking patterns, purchasing behaviors, and reasons for use according to cigar type: Findings from the Population Assessment of Tobacco and Health (PATH) study, 2013–2014. Nicotine and Tobacco Research, 20(12), 1457–1466. 10.1093/ntr/ntx209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornacchione Ross J, Sutfin EL, Suerken C, Walker S, Wolfson M, & Reboussin BA (2020). Longitudinal associations between marijuana and cigar use in young adults. Drug and Alcohol Dependence, 211, 107964. 10.1016/J.DRUGALCDEP.2020.107964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dai H, Catley D, Richter KP, Goggin K, & Ellerbeck EF (2018). Electronic cigarettes and future marijuana use: A longitudinal study. Pediatrics, 141(5), 2014–2015. 10.1542/peds.2017-3787 [DOI] [PubMed] [Google Scholar]
- Delnevo C, Giovenco DP, Kurti MK, & Al-Shujairi A (2019). Co-marketing of marijuana and cigars in US convenience stores. Tobacco Control, 29(2). 10.1136/tobaccocontrol-2018-054651 [DOI] [PubMed] [Google Scholar]
- Dennis ML, Chan YF, & Funk RR (2006). Development and Validation of the GAIN Short Screener (GSS) for Internalizing, Externalizing and Substance Use Disorders and Crime/Violence Problems Among Adolescents and Adults. The American Journal on Addictions, 15(SUPPL. 1), s80–s91. 10.1080/10550490601006055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- East KA, Reid JL, Rynard VL, & Hammond D (2021). Trends and Patterns of Tobacco and Nicotine Product Use Among Youth in Canada, England, and the United States From 2017 to 2019. Journal of Adolescent Health, 69(3), 447–456. 10.1016/J.JADOHEALTH.2021.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairman BJ (2015). Cannabis problem experiences among users of the tobacco–cannabis combination known as blunts. Drug and Alcohol Dependence, 150, 77–84. 10.1016/j.drugalcdep.2015.02.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Food and Drug Administration. (2022). FDA Proposes Rules Prohibiting Menthol Cigarettes and Flavored Cigars to Prevent Youth Initiation, Significantly Reduce Tobacco-Related Disease and Death. https://www.fda.gov/news-events/press-announcements/fda-proposes-rules-prohibiting-menthol-cigarettes-and-flavored-cigars-prevent-youth-initiation
- Ghinai I, Pray IW, Navon L, O’Laughlin K, Saathoff-Huber L, Hoots B, Kimball A, Tenforde MW, Chevinsky JR, Layer M, Ezike N, Meiman J, & Layden JE (2019). E-cigarette Product Use, or Vaping, Among Persons with Associated Lung Injury - Illinois and Wisconsin, April-September 2019. MMWR. Morbidity and Mortality Weekly Report, 68(39), 865–869. 10.15585/mmwr.mm6839e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giovenco DP, Miller Lo EJ, Lewis MJ, & Delnevo CD (2016). “They’re Pretty Much Made for Blunts”: Product Features That Facilitate Marijuana Use Among Young Adult Cigarillo Users in the United States. Nicotine & Tobacco Research, ntw182. 10.1093/ntr/ntw182 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henriksen L, Schleicher NC, Ababseh K, Johnson TO, & Fortmann SP (2018). Marijuana as a “concept” flavour for cigar products: Availability and price near California schools. Tobacco Control, 27(5), 585–588. 10.1136/tobaccocontrol-2017-053961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hindocha C, Freeman TP, Ferris JA, Lynskey MT, & Winstock AR (2016). No smoke without tobacco: A global overview of cannabis and tobacco routes of administration and their association with intention to quit. Frontiers in Psychiatry, 7(JUL), 1–9. 10.3389/fpsyt.2016.00104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu MC, Muthén B, Schaffran C, Griesler PC, & Kandel DB (2008). Developmental trajectories of criteria of nicotine dependence in adolescence. Drug and Alcohol Dependence, 98(1–2), 94–104. 10.1016/j.drugalcdep.2008.04.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyland A, Ambrose BK, Conway KP, Borek N, Lambert E, Carusi C, Taylor K, Crosse S, Fong GT, Cummings KM, Abrams D, Pierce JP, Sargent J, Messer K, Bansal-Travers M, Niaura R, Vallone D, Hammond D, Hilmi N, … Compton WM (2017). Design and methods of the Population Assessment of Tobacco and Health (PATH) Study. Tobacco Control, 26(4), 371–378. 10.1136/tobaccocontrol-2016-052934 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kolar K, Elton-Marshall T, Mann RE, & Hamilton HA (2020). Routes of cannabis administration among adolescents during criminal prohibition of cannabis in Canada. Drugs: Education, Prevention and Policy, 27(5), 421–426. 10.1080/09687637.2020.1715920 [DOI] [Google Scholar]
- Kristman-Valente AN, Hill KG, Epstein M, Kosterman R, Bailey JA, Steeger CM, Jones TM, Abbott RD, Johnson RM, Walker D, & David Hawkins J (2017). The Relationship Between Marijuana and Conventional Cigarette Smoking Behavior from Early Adolescence to Adulthood. Prevention Science, 18(4), 428–438. 10.1007/S11121-017-0774-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayer ME, Kong G, Barrington-Trimis JL, McConnell R, Leventhal AM, & Krishnan-Sarin S (2019). Blunt and Non-Blunt Cannabis Use and Risk of Subsequent Combustible Tobacco Product Use Among Adolescents. Nicotine & Tobacco Research, 26(6), 1–15. 10.1093/ntr/ntz225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Montgomery L, & Mantey D (2017a). Racial/Ethnic Differences in Prevalence and Correlates of Blunt Smoking among Adolescents. Journal of Psychoactive Drugs, 00(00), 1–11. 10.1080/02791072.2017.1401186 [DOI] [PubMed] [Google Scholar]
- Montgomery L, & Mantey DS (2017b). Correlates of Blunt Smoking Among African American, Hispanic/Latino, and White Adults: Results From the 2014 National Survey on Drug Use and Health. Substance Use & Misuse, 52(11), 1449–1459. 10.1080/10826084.2017.1284238 [DOI] [PubMed] [Google Scholar]
- Nardone N, Jain S, & Benowitz NL (2019). Biomarkers of Exposure to Nicotine and Tobacco-specific Nitrosamines in Adolescent Blunt Users. Nicotine & Tobacco Research, 1–19. 10.1093/ntr/ntz144 [DOI] [PubMed] [Google Scholar]
- Patton GC, Coffey C, Carlin JB, Sawyer SM, & Lynskey M (2005). Reverse gateways? Frequent cannabis use as a predictor of tobacco initiation and nicotine dependence. Addiction (Abingdon, England), 100(10), 1518–1525. 10.1111/j.1360-0443.2005.01220.x [DOI] [PubMed] [Google Scholar]
- Peters EN, Schauer GL, Rosenberry ZR, & Pickworth WB (2016). Does marijuana “blunt” smoking contribute to nicotine exposure?: Preliminary product testing of nicotine content in wrappers of cigars commonly used for blunt smoking. Drug and Alcohol Dependence, 168, 119–122. 10.1016/j.drugalcdep.2016.09.007 [DOI] [PubMed] [Google Scholar]
- Seaman EL, Stanton CA, Edwards KC, & Halenar MJ (2020). Use of tobacco products/devices for marijuana consumption and association with substance use problems among U.S. young adults (2015–2016). Addictive Behaviors, 102(October 2019), 106133. 10.1016/j.addbeh.2019.106133 [DOI] [PubMed] [Google Scholar]
- Seo DC, Kwon E, Lee S, & Seo JD (2020). Using susceptibility measures to prospectively predict ever use of electronic cigarettes among adolescents. Preventive Medicine, 130(June 2019), 105896. 10.1016/j.ypmed.2019.105896 [DOI] [PubMed] [Google Scholar]
- Sifaneck S, Johnson B, & Dunlap E (2005). Cigars-for-Blunts: Choice of Tobacco Products by Blunt Smokers. Journal of Ethnicity in …, 23–42. 10.1300/J233v04n03 [DOI] [PubMed] [Google Scholar]
- Simon P, Camenga DR, Kong G, Connell CM, Morean ME, Cavallo DA, & Krishnan-Sarin S (2017). Youth E-cigarette, Blunt, and Other Tobacco Use Profiles: Does SES Matter? Tobacco Regulatory Science, 3(1), 115–127. 10.18001/TRS.3.1.12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinclair CF, Foushee HR, Scarinci I, & Carroll WR (2013). Perceptions of harm to health from cigarettes, blunts, and marijuana among young adult African American men. Journal of Health Care for the Poor and Underserved, 24(3), 1266–1275. 10.1353/hpu.2013.0126 [DOI] [PubMed] [Google Scholar]
- StataCorp. (2021). Stata Statistical Software: Release 17. StataCorp, LLC. [Google Scholar]
- Sterling KL, Fryer CS, & Fagan P (2016). The Most Natural Tobacco Used: A Qualitative Investigation of Young Adult Smokers’ Risk Perceptions of Flavored Little Cigars and Cigarillos. Nicotine and Tobacco Research, 18(5), 827–833. 10.1093/ntr/ntv151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun R, Mendez D, & Warner KE (2022). Use of Electronic Cigarettes Among Cannabis-Naive Adolescents and Its Association With Future Cannabis Use. JAMA Network Open, 5(7), e2223277–e2223277. 10.1001/JAMANETWORKOPEN.2022.23277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Health and Human Services, National Institutes of Health National Institute on Drug Abuse, & Department of Health and Human Services Food and Drug Administration. (2012). Population Assessment of Tobacco and Health (PATH) Study [United States] Public-Use Files. In Population Assessment of Tobacco and Health (PATH) Study Public-Use Files. Inter-university Consortium for Political and Social Research [distributor]. 10.3886/ICPSR36498.v16 [DOI]
- U.S. Department of Health and Human Services. (2012). Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. [Google Scholar]
- Volkow ND, Baler RD, Compton WM, & Weiss SRB (2014). Adverse health effects of marijuana use. The New England Journal of Medicine, 370(23), 2219–2227. 10.1056/NEJMra1402309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberger AH, Delnevo CD, Zhu J, Gbedemah M, Lee J, Cruz LN, Kashan RS, & Goodwin RD (2019). Trends in Cigar Use in the United States, 2002–2016: Diverging Trends by Race/Ethnicity. Nicotine & Tobacco Research, 1–5. 10.1093/ntr/ntz060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinberger AH, Zhu J, Lee J, Xu S, & Goodwin RD (2021). Cannabis Use and the Onset of Cigarette and E-cigarette Use: A Prospective, Longitudinal Study among Youth in the United States. Nicotine and Tobacco Research, 23(3), 609–613. 10.1093/ntr/ntaa158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wills TA, Leventhal AM, Sargent JD, & Pagano I (2021). Concurrent Use of E-cigarettes, Combustible Cigarettes, and Marijuana. Pediatrics, 148(4). 10.1542/peds.2021-050749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ziegel ER, & Allison PD (1997). Survival Analysis Using the SAS System. Technometrics, 39(3), 344. 10.2307/1271161 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


