Abstract
The detailed anatomy of the rectus femoris and corresponding injury appearances were first described in 1995. Since then, there has been little published to change our understanding of this complex anatomical area. More recent anatomical dissection work in 2004 and 2006 alluded to the presence of an altered configuration of the proximal tendon anatomy. Whilst widely accepted that the proximal rectus femoris muscle has two distinct tendon slips, the authors in 2006 described a third separate tendon slip arising from the anterior femoral capsule and this has been widely termed the ‘capsular head’. We provide evidence that imaging features corroborate this revised anatomical concept. Whilst the clinical relevance of these findings is yet to be established, it remains important that our understanding of the radiological anatomy in this area advances with the forward growth of imaging clarity. In this review, we revisit anatomical concepts and present atypical injury cases that may be explained by the presence of a separate capsular head.
Introduction
The proximal rectus femoris muscle is one of the most frequently injured muscles in professional and amateur athletes occurring mostly with kicking sports such as soccer. 1 As musculoskeletal radiologists, particularly those working in sports radiology centres will attest, the grading of muscle and tendon injuries, and attempt to prognosticate approximate return-to-play times, can be challenging. A clear understanding of tendon and myotendinous anatomy is the key to reliable injury grading particularly in multihead muscles for grading of tendon involvement, which can carry worse prognosis and delayed return-to-play (RTP) times. 2,3
In both 2004 and 2006, dissection work on the proximal rectus femoris tendon anatomy was undertaken by Tubbs et al which demonstrated the presence of a third proximal rectus femoris tendon which arose from the anterior hip capsule and had a separate origin and insertion to the indirect head arising from the acetabular roof. 4 This revised the conventional two-tendon anatomy. Surprisingly, since this study little work has since been published regarding this, and to our knowledge no work has been published assessing the imaging characteristics of this area. No description of the myotendinous junction anatomy or muscle fibres associated with the capsular head have been described. Specifically, there appears to be a subdivision of proximal rectus femoris tears occurring within the indirect head central septum myotendinous junction (MTJ) that we believe relates to injury of the aforementioned capsular head.
In this review, we describe the MR imaging evidence of the capsular head in the context of acute injury where the presence of muscle oedema and tissue fluid allows delineation of the relevant structures. These variations in appearance should be appreciated by the musculoskeletal radiologist to aide more precise grading of tendon and myotendinous injury and help reduce misgrading. As described below, we believe some of these injuries may represent a subclassification of the pathognomonic “bulls-eye” lesion 5 of the indirect head MTJ which, when combined with longitudinal studies could improve imaging prognostication. 6
Case source
The cases presented in this review are of skeletally mature professional athletes imaged at our institution (Department of Musculoskeletal Radiology, Chapel Allerton Hospital, Leeds Teaching Hospitals NHS Trust, Leeds, UK) between September 2017 and November 2020, presenting with acute proximal rectus femoris injuries associated with professional sporting activity. Institutional guidance deemed ethics committee approval was not required for this retrospective review article.
All athletes were scanned on a 3-Tesla Siemens Magnetom Skyra (Erlangen, Germany). Standard sequences included a large field of view coronal short tau inversion-recovery (STIR) of both proximal thighs. Small field of view imaging of the symptomatic side included axial T2 fat-saturated sequence, sagittal STIR sequence and both axial and coronal T1 sequences (Table 1).
Table 1.
MRI parameters
| Sequence | Plane | TR (ms) | TE (ms) | FONT (mm) | Slice thickness (mm) |
|---|---|---|---|---|---|
| STIR | Coronal | 3080 | 54 | 430 | 3 |
| STIR | Sagittal | 3000 | 39 | 380 | 3 |
| T2 fat saturated | Axial | 5070 | 84 | 320 | 4 |
| T1 | Coronal | 517 | 9 | 380 | 4 |
| T1 | Axial | 648 | 10 | 320 | 4 |
STIR, short tau inversion-recovery; TE, echo time; TR, repetition time.
The cases were reviewed by two experienced musculoskeletal sports radiologists (BP, POC) of 11 and 25 years’ experience respectively and were assigned injury grades based on the BAMIC classification (British Athletics Muscle Injury Classification) which is common to professional sports practice in the United Kingdom at present. 7
Conventional proximal rectus femoris anatomy
The rectus femoris is a biarticular fusiform muscle that makes up the most superficial component of the quadriceps muscle complex. It plays an important role in the fast dynamic movements and contains a high volume of Type II muscle fibres. Biomechanically, the rectus femoris muscle acts over two joints producing flexion at the hip and extension at the knee. This muscle fibre structure makes it particularly prone to stretch injury. 8 It acts as an antagonist to the hamstring muscles and is innervated by the posterior division of the femoral nerve. For the professional sports radiologist, detailed anatomical knowledge of the tendons and MTJ anatomy is essential in the assessment of injury to propose an accurate grade to predict recovery and RTP times. 9
Detailed musculotendinous anatomy of the proximal rectus femoris muscle and corresponding injury patterns were first described in 1995 by Hasselman et al. 10 Most publications since this time describe two main proximal tendons of the rectus femoris. The first is a direct head, also known as the straight head, which arises from the anterior inferior iliac spine (AIIS). The second, the indirect or reflected head is a broader tendon said to arise from the superior acetabular ridge with contributions from the joint capsule. A few centimetres below these origins both tendons converge to form a conjoined tendon (Figure 1). The direct head lies within the superficial fibres of the conjoined tendon with the indirect fibres lying deep. After approximately 1 cm, the conjoined tendon then separates into the respective tendons which form the proximal MTJ. The direct head MTJ fibres blends with the superficial aponeurosis of the muscle. The indirect tendon fibres extend deep into the muscle belly and lie as an intramuscular MTJ, sometimes referred to as the central septum, lying medially to the superficial direct head. 6 The distal rectus femoris tendon arises from the posterior aspect of the distal muscle and merges with the vastus tendons to form the quadriceps tendon above the knee.
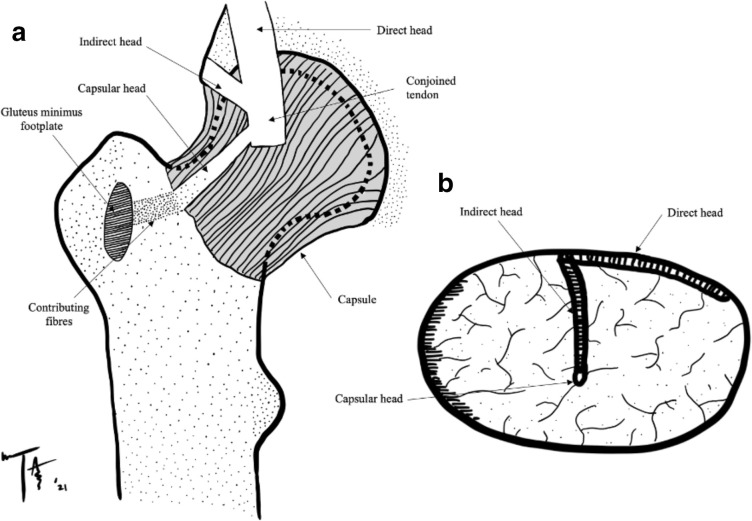
Figure 1.
Artistic anatomical representation of the approximate orientation of the capsular head. (A) Demonstrates the proximal tendon anatomy with contribution from the anterior hip capsule (iliofemoral ligament) and gluteus minimus tendon at the insertion onto the anterior facet of the greater trochanter. (B) Demonstrates the proposed proximal MTJ anatomy (axial plane) with the capsular head fibres lying within the posterior-most fibres of the central septum. MTJ, myotendinous junction
The osseous footplate of the direct head tendon arising from the AIIS has an average surface area of 1.3 × 2.6 cm. The indirect tendon footplate is larger with average measurement described of 1.7 × 4.7 cm. 11 Gyftopoulos et al in 2008, attempted to define the anatomy of the proximal rectus femoris on imaging and had previously alluded to the indirect tendon footplate anatomy as being more complex with a broad component that arises from both the superior acetabular ridge and anterior joint capsule; 6 however, the authors did not suggest any evidence of a separate tendon slip arising from the anterior hip capsule at this time or identify the myotendinous junction or muscle fibres associated with a capsular head. The more recent work undertaken by Tubbs et al would support the notion that the true anatomy here may comprise a capsular head component that arises separately from the anterior hip capsule to blend with the conjoined tendon.
Imaging anatomy of the capsular head
Following an initial case report in 2004 believed to be the first description of a ‘femoral’ tendon slip of rectus femoris, 12 in 2006, Tubbs et al dissected 96 proximal rectus femoris origins in 48 cadavers. The capsular head was found to be either bilaterally present or bilaterally absent with only a small number of cases where this was unilaterally present (4.2% on the left; 5.2% on the right). Interestingly, this tendon was bilaterally present in 83% of dissected specimens. The capsular head tendon was found to attach deeply to the iliofemoral ligament and in some cases had a bilaminar morphology in which the superficial component of this attached to the gluteus minimus tendon. When present, the tendon formed a 60 degree angle with the indirect head and was orientated in an inferolateral direction relative to the direct head. The mean tendon length and width was 2 cm and 4 cm respectively with a thickness of 3 mm. The authors stated whilst the functional ramification of such an attachment is speculative, clinicians should consider this anatomical revision when performing surgery or imaging of the area. 4
Since the publication of this anatomical paper, no articles have been published regarding this anatomy on imaging. In 2010, Pasta et al described the sonographic assessment of the proximal rectus femoris tendons, stating the presence of the capsular head in their anatomical drawings, however, the authors failed to address this anatomy on sonographic assessment, instead focusing on the conventional direct and indirect head morphology. 13
In the following cases of proximal rectus femoris injury, we describe imaging findings that support the capsular head being visible on MRI imaging particularly in the context of acute injury of the proximal rectus femoris tendons. Figures 1 and 2 demonstrate an artistic representation of the updated anatomy of this area and the proximal myotendinous junction.
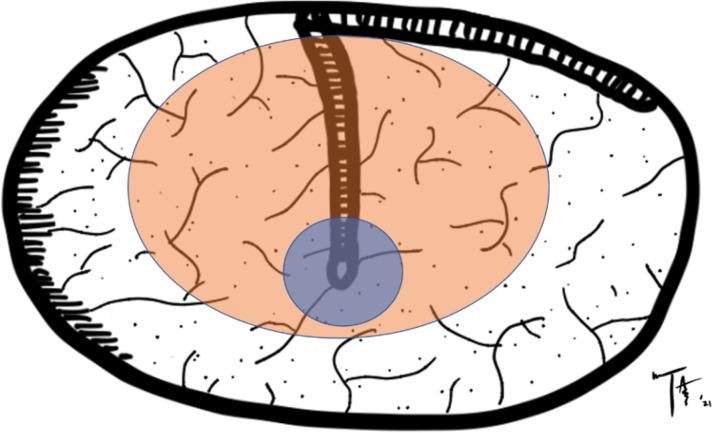
Figure 2.
Artistic anatomical representation demonstrating the hypothesised orientation of fibres of the central septum of the proximal rectus femoris. The bipennate fibres associated with the indirect head (orange) may contain further separate bipennate fibres around the capsular head (blue) which may explain the atypical focal patterns seen in several injury cases in elite athletes as described.
Injury to the proximal direct and indirect heads
Injury to the proximal indirect (posterior, reflected) head myotendon has been described as up to 16 times more common that the direct head. 14 Injury to the proximal tendons proper or bony avulsion fracture is rare in skeletally mature individuals. 15 As known from previous anatomical descriptions, the indirect head fibres are positioned posteriorly to the direct head fibres within the conjoined tendon and lie deep within the proximal muscle belly as the proximal MTJ (known as the central septum). Injury to these deep fibres can be seen on MRI as loss of clarity of the hypointense linear fibres, and replacement with fluid, haematoma and surrounding muscular oedema. Occasionally, a degloving type of injury occurs due to separation of the bipennate proximal muscle belly of the indirect head within the surrounding unipennate muscle of the direct head. This has been described as a ‘bulls-eye’ type pattern. 16
Proximal rectus femoris injury cases in professional footballers
Direct head injury
This is characterised by oedema within the superficial anterior fibres of rectus femoris and loss of normal tendon configuration. Haematoma/fluid tracks along the superficial aponeurosis adjacent to the direct head tendon and there is sparing of the central septum. Figure 3 demonstrates such an injury in a 19-year-old male professional footballer. In chronic injury, fat replacement within the muscle can occur as well as tendon/myotendinous scarring. Figure 3b demonstrates the corresponding T1 sequences of the same athlete as shown in Figure 3a with evidence of loss of the normal hypointense structure of the superficial direct component of the myotendinous junction. This injury is classified as a BAMIC Grade 2b (see below).
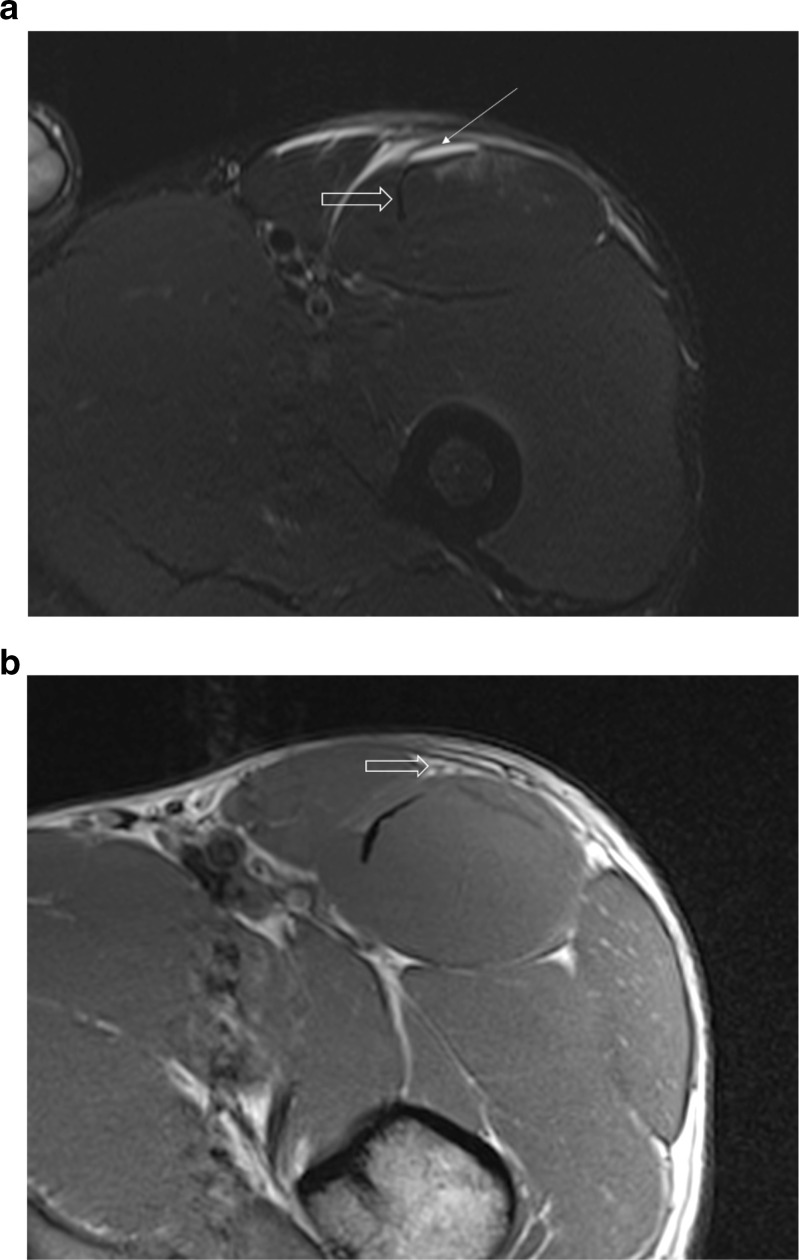
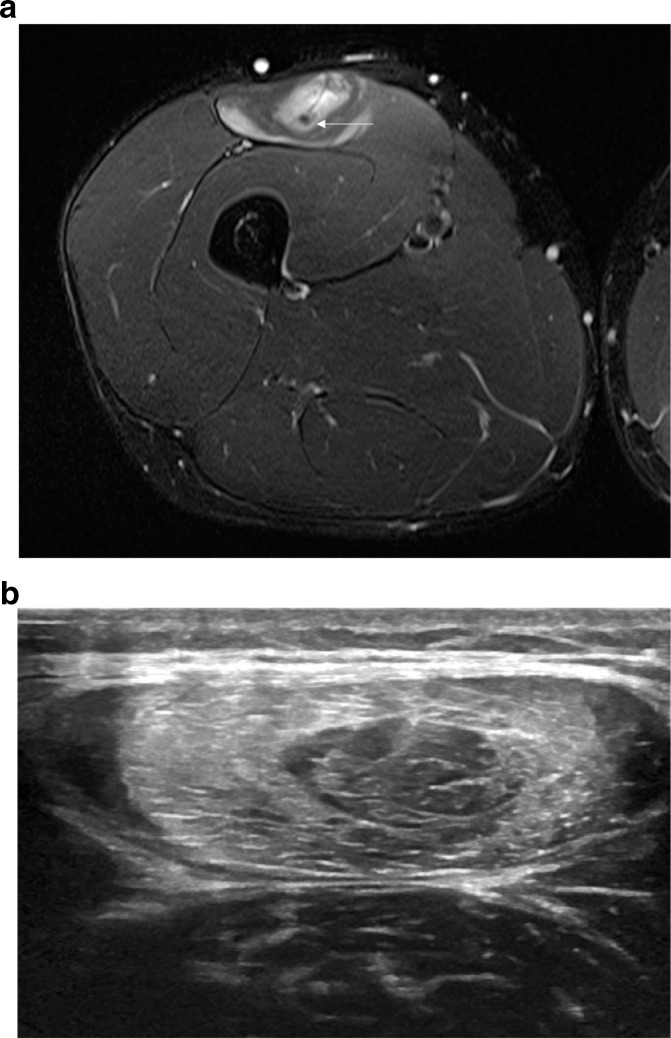
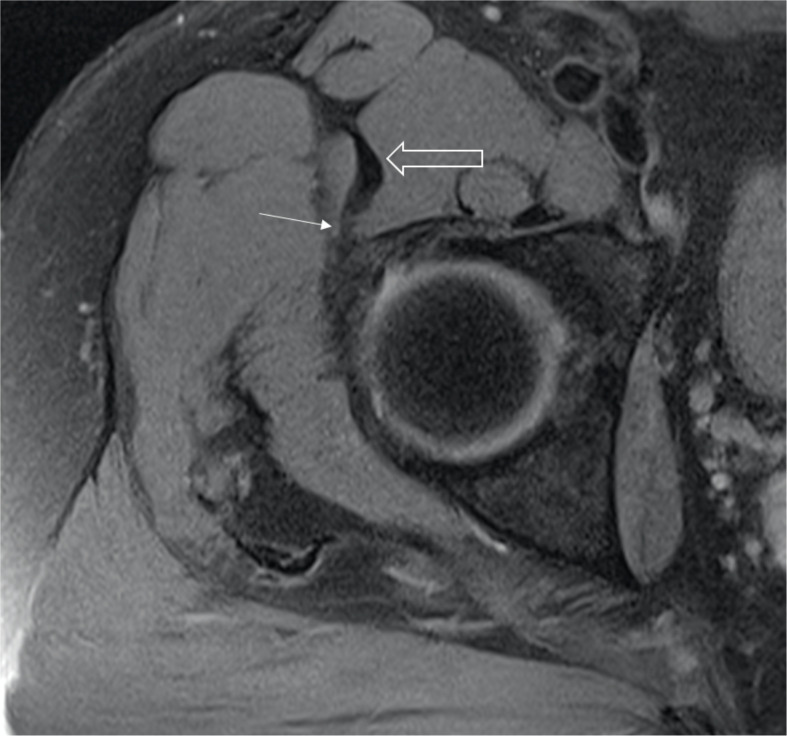
Figure 3.
A 19-year-old male professional football player with a BAMIC Grade 2b injury to the proximal direct head of the left rectus femoris. (a) Axial T2 fat saturated image of a classical direct head myotendinous injury of the proximal rectus femoris. Note the loss of clarity of the superficial fibres (white arrow), oedema tracking along the aponeurosis and sparing of the central septum fibres (open arrow). (b) Axial T1 sequences showing the direct head myotendinous injury with loss of clarity of the superficial fibres and loss of the hypointense tendon structure (open arrow).
Indirect head injury
When the indirect head myotendinous junction is injured, there is loss of clarity of the thin hypointense intramuscular tendon (central septum) which is replaced with fluid and haematoma. There is either partial or complete loss of tendon structure. Figure 4 demonstrates a BAMIC Grade 3c injury to the proximal rectus femoris, which is the commonly used classification system in the UK when grading injury in professional sport. Briefly, the BAMIC classification of injuries are graded from 0 to 4, which includes normal imaging, and myotendinous/muscular injury severity of <10% or <5 cm Grade 1, 10–50% or 5–15 cm Grade 2, > 50% or >15 cm Grade 3 and finally, a complete tear which is Grade 4. A suffix is added as either a, b or c which subclassifies the injury as myofascial, myotendinous or tendinous in origin respectively (Table 2). In the case of this athlete, there is greater than 50% involvement of the central tendon itself over greater than 15 cm length with some tendon laxity seen. 7
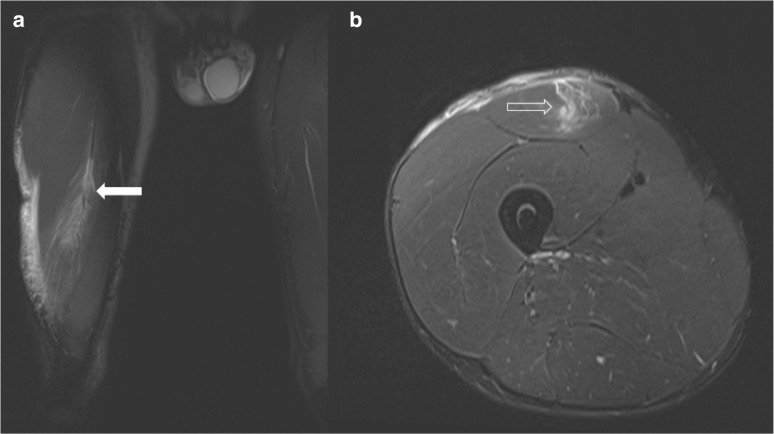
Figure 4.
A 22-year-old professional male footballer with a proximal right rectus femoris indirect head Grade 3c injury. Coronal (A) and axial (B) T2 fat-saturated sequences of an indirect head injury of the proximal rectus femoris myotendon demonstrate loss of tendon fibre clarity and replacement with haematoma and oedema (open white arrow). Coronal sequences demonstrate tendon laxity (thick white arrow).
Table 2.
BAMIC grading system
| GRADE | Description | MRI features |
|---|---|---|
| Oa | Focal neuromuscular injury | Normal |
| Ob | Generalised muscular soreness (DOMS) | Normal or patchy hyperintensity within the muscles. If suspicion of a neural component, then “+N” can be added to either injury |
| 1a | Focal myofascial tear | High STIR signal in periphery of the muscle. Less than 10% of width of muscle involved. Longitudinal length of less than 5 cm |
| 1b | Focal myotendinous tear | Sited within the muscle, or more commonly at the MTJ. Less than 10% muscle cross-section and less than 5 cm in length. |
| 2a | Moderate myofascial tear | Between 10–50% of muscle cross-section involved over 515 cm. Architectural fibre disruption of less than 5 cm. |
| 2b | Moderate myotendon tear | As above but sited at the MTJ. |
| 2c | Moderate intratendinous tear | Extension into the tendon is evident over a length of less than 5 cm and less than 50% of maximal tendon diameter on axial images. If the injury lies near the free end of the tendon there may be some laxity. |
| 3a | Extensive myofascial tear | Greater than 50% muscle cross-section involved over a length greater than 15 cm. Architectural fibre disruption likely greater than 5 cm. |
| 3b | Extensive myotendon tear | As above but sited at the MTJ as opposed to periphery of the muscleim-uscle belly. |
| 3c | Extensive intratendinous tear | Involves greater than 50% of the tendon width or over a length of greater than 5 cm. No evidence of complete defect but may be some loss of tendon tension. |
| 4 | Complete muscle tear | Visible complete gap in muscle |
| 4c | Complete tendon tear | Complete gap in the tendon filled with interposed haematoma or oedema on STIR imaging. |
MTJ, myotendinous junction; STIR, short tau inversion-recovery.
Injury to the capsular head myotendon
To our knowledge, injury to the capsular head and the proximal myotendon has not been described on imaging. In the following case discussion, we outline cases demonstrating unusual oedema patterns around the proximal myotendinous junction that allude to the presence of a distinct capsular head MRI imaging. In a case of a 19-year-old male professional footballer who presented with proximal rectus femoris injury (BAMIC Grade 2b), the MRI shows evidence of a “de-gloving” type proximal MTJ injury of the central septum (Figure 5). Unusually, both MRI and sonographic assessment reveal sparing of a small central bipennate component within the larger de-gloving injury of the indirect muscle belly which suggests more complex underlying anatomy and may reflect an indirect MTJ injury with sparing of the capsular head component. This case suggests that the capsular head fibres likely run in the posterior-most fibres of the central septum and may in fact have their own smaller MTJ within this. Figures 1 and 2 demonstrate an artistic line diagram of the proposed revised myotendinous anatomy.
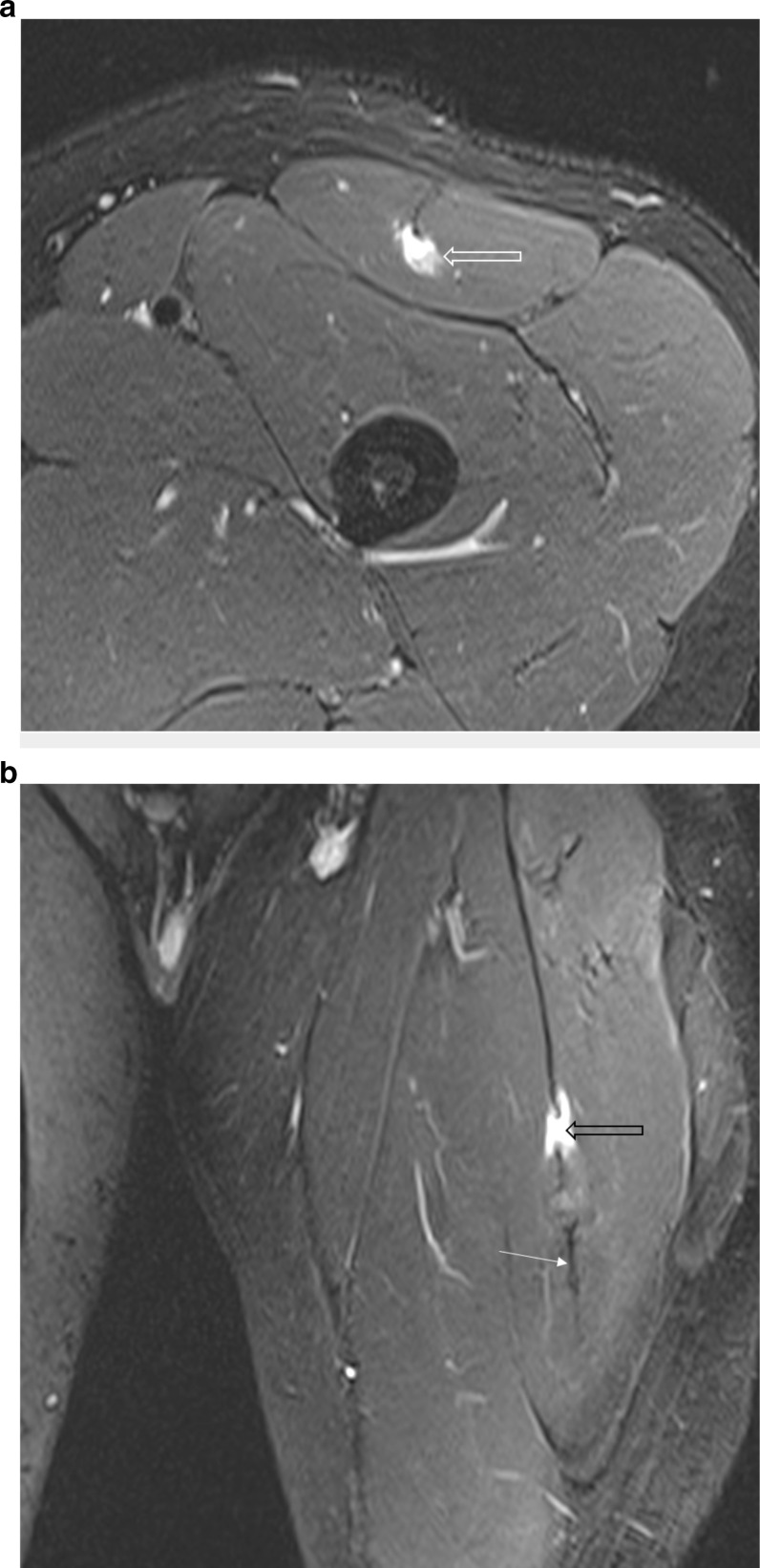
Figure 5.
A 19-year-old male professional football player with a BAMIC Grade 2b injury to the indirect head musculotendinous junction. (a) Axial T2 fat-saturated image of the proximal rectus femoris with injury to the indirect head MTJ with a degloving type injury. Note there is also deep injury to the unipennate muscle adjacent to the posterior myofascia. The posterior-most fibres of the central septum appear intact and enlarged (white arrow). This likely reflects the intact capsular head which has been described in this location on dissection. This appearance may suggest chronic scarring from previous injury (we liken this to a tadpole sign). (b) Transverse ultrasound image demonstrating bizarre sparing of the central muscle surrounding the deeper myotendon with echogenic bullseye haemorrhagic oedema surrounding this and muscular sparing of the direct unipennate fibres in the periphery of the transverse section. This may partially be explained by the revised anatomical depiction in Figure 2. MTJ, myotendinous junction.
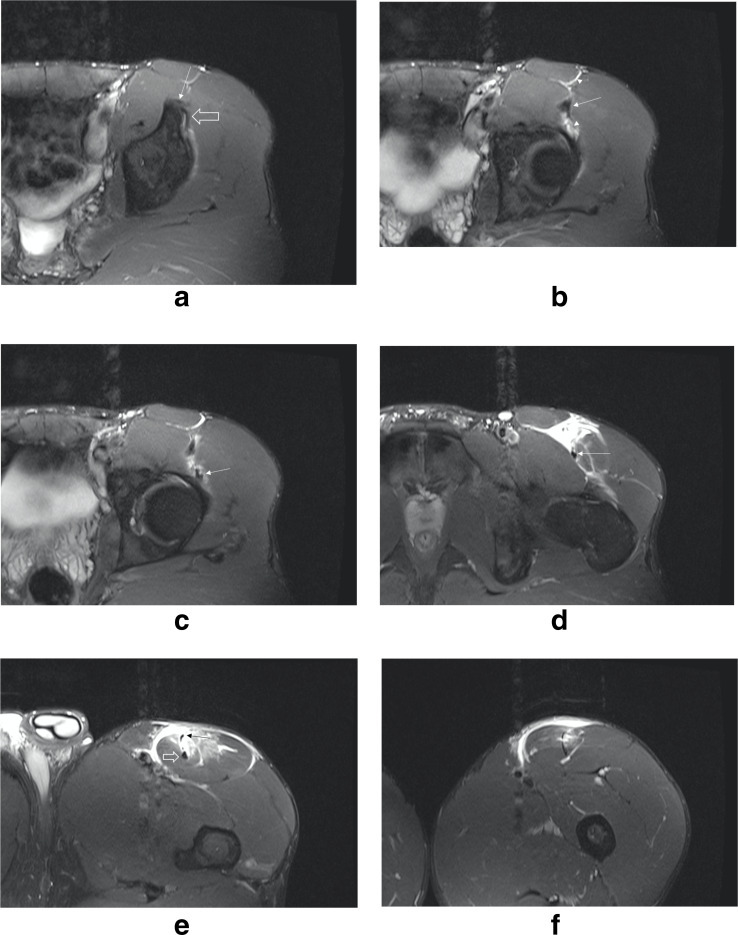
Sequential axial T2 FS slices through a proximal rectus femoris MTJ injury of a 31-year-old male professional footballer (Figure 6) demonstrates full-thickness tendon injury to the indirect head tendon (BAMIC Grade 3c) just distal to the conjoined tendon which is easily visualised (Figure 6b). Just inferior to this, arising from the anterior aspect of the iliofemoral ligament, and separate from the superior acetabular ridge indirect tendon origin, is a distinct tendon slip (Figure 6c) which is made more conspicuous by surrounding oedema. This blends with the conjoined tendon and is seen intact within the posterior-most aspect of the central septum before reconstitution distally of the indirect head fibres which then blend with these.
Figure 6.
A 31-year-old male professional football player with a BAMIC Grade 3c injury to the indirect head of the rectus femoris. (a) Axial T2FS sequence demonstrating the origin of the direct head (arrow) and indirect head (open arrow) arising from the AIIS and superior acetabulum respectively. (b) Axial T2FS just inferior to Figure 6a, the direct and indirect tendons have now merged to form the conjoined tendon (long arrow). Note the oedema superficial and deep to this tendon (arrowheads) alluding to the presence of injury distally. (c) Axial T2FS one slice inferior to Figure 6b. Note a separate structure is now visible (white arrow) arising from the anterior femoral capsule (iliofemoral ligament) heading towards the conjoined tendon. This likely reflects the commonly present capsular head which can be distinguished more easily in the presence of surrounding oedema. (d) Axial T2FS inferior to Figure 6c demonstrating full thickness rupture of the indirect head which is replaced by fluid. Note the posterior-most fibres of the deep myotendinous junction are intact which represents the capsular head component (white arrow). (e) Axial T2FS further inferior to Figure 6d of the upper rectus femoris muscle belly of the same athlete demonstrating the indirect head (black arrow) re-emerging and lying superficial to the capsular head (open arrow) which has a rounded thickened morphology which may reflect chronic scarring (tadpole sign). (f) Axial T2FS. Distal to Figure 6e, the deep myotendon now appears as a single intramuscular deep tendon in which the two components are now inseparable. AIIS, anterior inferior iliac spine
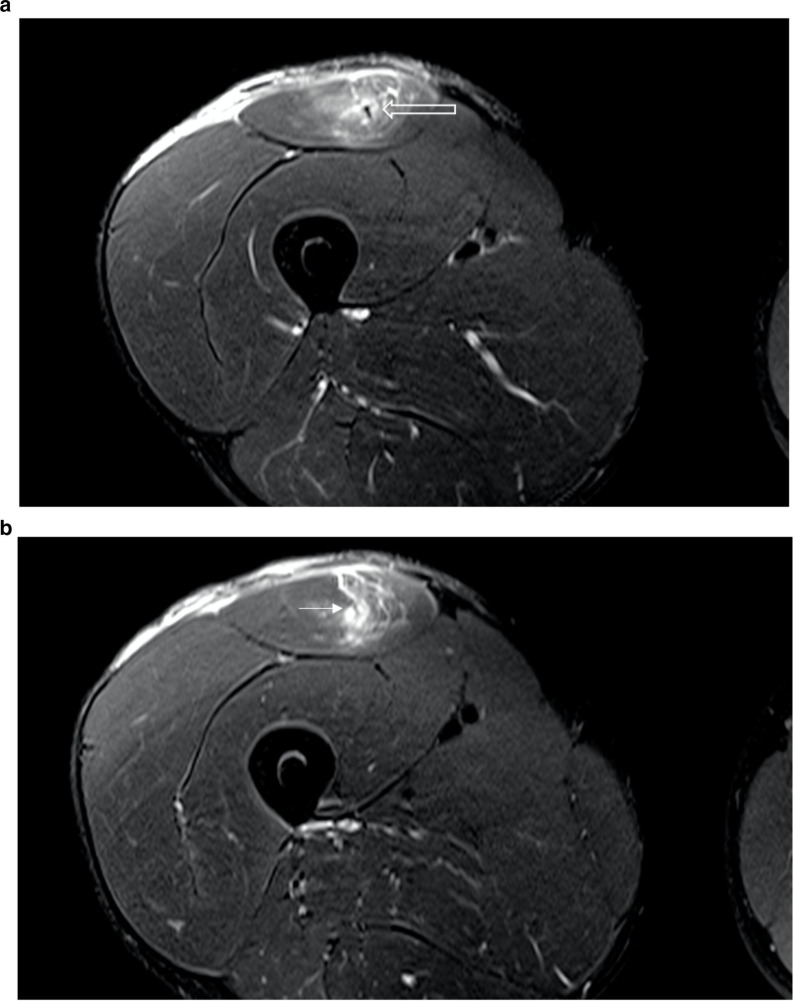
These findings are once again corroborated in a different 22-year-old male professional footballer who also has extensive injury to both the direct and indirect proximal myotendons which have been replaced with fluid and haematoma (Figure 7a–c). Note again, the atypical findings of sparing of intact deep posterior fibres within the central septum which have a tubular morphology. Figure 7b demonstrates the total absence of myotendinous fibres suggesting full thickness injury to all components but sequential slices do show that these myotendons reconstitute. The deep myotendinous junction appears to have a consistent morphology in these athletes with the scarred most posterior fibres having a rounded appearance on axial MR sequences which we liken to a tadpole (we have termed this the ‘tadpole sign’). Many normal imaging cases do not show this clear separation in morphology of the deep myotendon, and therefore we postulate that this may reflect remodelling or scarring changes within the deep myotendon from previous injury or microtrauma as demonstrated in this case and below. This is again demonstrated in a separate case of a different professional footballer with no acute injury but a history of previous injury suggestive of scar tissue formation (Figure 8).
Figure 7.
A 22-year-old professional male footballer with a BAMIC Grade 3c injury of the proximal right rectus femoris. (a) Axial T2FS. Note the full-thickness tear of the direct and indirect heads. Again, the presence of the likely capsular head component of the deep myotendon is noted (open arrow). (b) Axial T2FS. Distal to Figure 7a the capsular head now demonstrates full-thickness rupture with fluid replacing the entirety of the deep myotendinous junction of the proximal rectus femoris (arrow). (c) Axial T2FS. Distal to Figure 7b the intramuscular tendon re-emerges with the linear-appearing indirect head (arrow) and the slightly thickened rounded capsular head (open arrow) lying within the deeper aspect of the fibres (tadpole sign).
Figure 8.
Axial T2FS. A different athlete to those in the previous Figures 4–7. Again, note the tadpole-like morphology in this athlete with no acute tear but a history of previous injury. We believe this may reflect previous injury with chronic scarring of the deep myotendon, mostly affecting the capsular component.
The athlete shown in Figure 9 did not have an acute proximal rectus femoris injury but this case did demonstrate evidence of a visible separate capsular head tendon slip. In this case, a faint hypointense band of tissue is seen arising from the anterior capsule and joining the posterior aspect of the conjoined tendon fibres at the level of the acetabular roof. This corroborates the notion that the capsular head fibres run in the posterior-most aspect of the conjoined, and subsequently central septum (deep myotendon).
Figure 9.
Axial T2FS In healthy athlete, with no known injury. The capsular head (arrow) is likely seen arising from the anterior right hip capsule and merging with the posterior fibres of the conjoined tendon (open arrow).
A further case of likely capsular head injury shown in Figure 10(a–b), in which a 27-year-old male professional footballer has a BAMIC Grade 2c injury. In this case, there appears to be a unusual focal injury of the most posterior fibres of the central septum. Coronal STIR sequences seen in Figure 10b confirm a full-thickness tear of the central myotendon with a surrounding small haematoma that may conform to a subtype of the de-gloving type injury which we suggest is analogous to a ‘mini’ bulls-eye type appearance.
Figure 10.
A 27-year-old professional male footballer with a BAMIC Grade 2c injury of the left rectus femoris which appears to involve the capsular head in isolation. (a) Axial T2FS. Note the focal oedema around the deep portion of the intramuscular myotendon with absence of the normal tendon fibres. Also note the relative sparing of the remaining indirect head tendon which has a normal morphology. As suggested by Tubbs et al, this is the region of the capsular head fibres suggesting isolated capsular head tear. (b) Coronal STIR sequence of same athlete as Figure 10a demonstrating complete disruption of tendon fibres within the deep-most fibres of the intramuscular tendon (black open arrow). Note scarring of the more distal tendon fibres in keeping with recurrent injury (arrow). STIR, short tau inversion-recovery
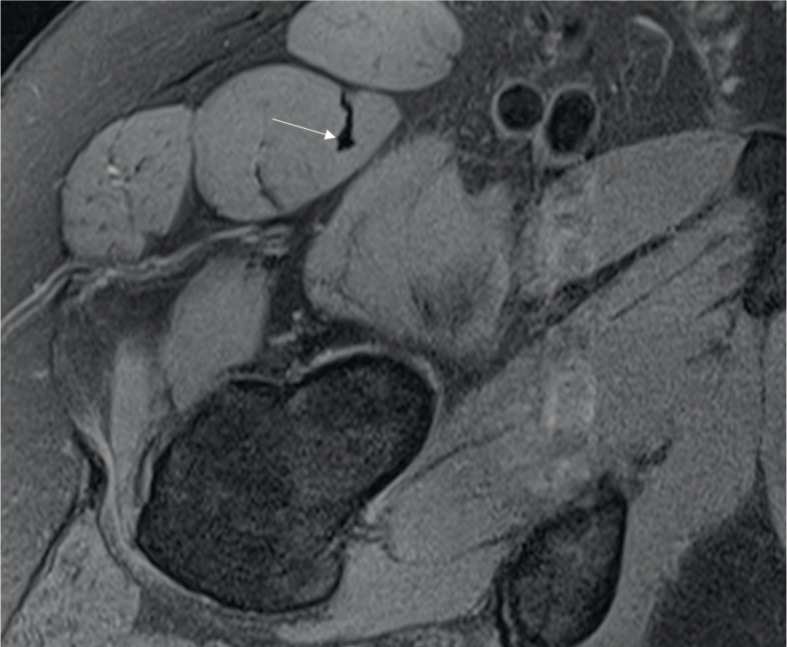
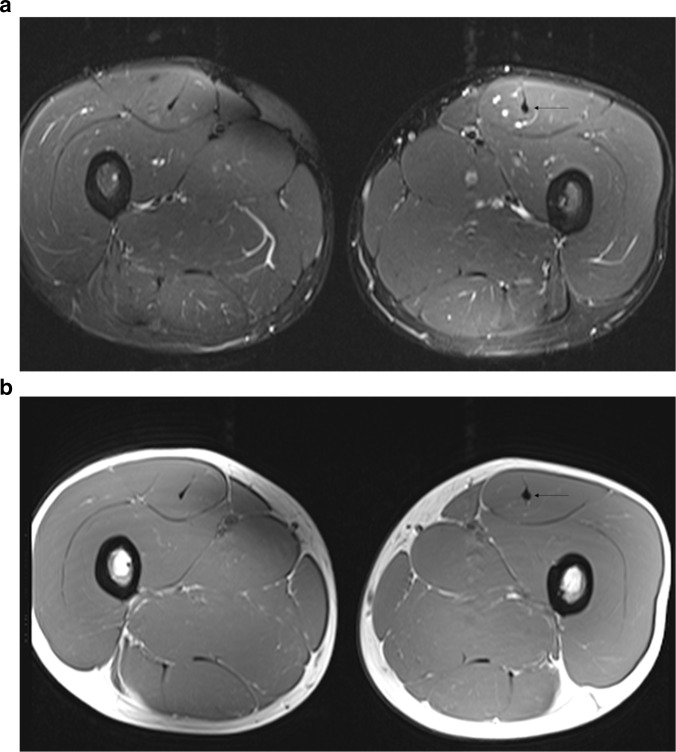
Finally, we present a case of a professional footballer with imaging features of chronic rectus femoris capsular head injury (Figure 11a–b). The MRI comprises of large field of view axial T1 and T2 fat-saturated sequences and demonstrates the clear discrepancy between the normal right side and chronically injured left side. Again, a “tadpole sign” is demonstrated with focal thickening and scarring within the most posterior fibres of the central septum suggestive of an isolated chronic capsular head myotendon injury.
Figure 11.
A healthy athlete with no acute injury but evidence of likely chronic left-sided capsular head injury with scar formation/remodelling. (a) Axial large FOV T2FS of both thighs in an athlete with a history of previous injuries to the left rectus femoris. Note the asymmetrical appearance of posterior fibres of the central septum when compared to the normal right side. (b( Axial large FOV T1 sequences in the same athlete in Figure 11a. Note the “tadpole” appearance of the deep fibres of the central septum which appears to correlate location of the posterior capsular head fibres and likely reflects chronic isolated injury with scarring.
Discussion
To date, the presence, or at least clinical relevance of a separate third capsular head remains unknown with little published data on the topic. The unusual patterns of proximal rectus femoris MTJ injury presented in this review are difficult to explain using the binary anatomical description of direct and indirect tendon anatomy only. Whilst the clinical implications of capsular head isolated injury or sparing are unknown it remains important for the radiologist reviewing these cases to be aware of this anatomical concept to avoid misinterpretation.
We have expanded on earlier dissection work carried out by Tubbs et al by demonstrating atypical cases that raise the awareness of this anatomy on imaging. In our routine clinical practice, we do not typically observe evidence of a separate tendon head in cases where no injury is apparent. On standard imaging sequences, perception of the capsular head in normal individuals would likely depend on slice thickness, sequence parameter and slice orientation, somewhat analogous to the popliteofibular ligament or anterolateral ligament of the knee which can be variable and challenging to see in normal individuals due to technical scanning factors alone. Given the capsular head size parameters on dissection, it is entirely plausible this should be seen on MRI in normal individuals. Further longitudinal studies are required in this field, but our current work serves as a benchmark for this area of musculoskeletal anatomy.
We are not yet aware of any prognostic impact of isolated injury or sparing of the capsular head myotendon in the context of professional sport and why isolated capsular head injury or sparing occurs. We postulate the separate attachment to the hip abductor gluteus minimus or the orientation angle with the straight head may play a structural role. Isolated injury or sparing of the capsular head may be clinically irrelevant from a functional or prognostic point of view. It is however important that we are able to explain these atypical imaging findings, even if only to dismiss them and prevent misclassifying a full thickness indirect head myotendon tear as partial thickness.
When grading injury, it is important to differentiate between partial and full thickness tears, which are graded 2 and 3 respectively by historical clinical and radiological grading systems. 17 This grading system has been accepted widely in many studies assessing injury of the proximal rectus femoris although is probably overly simplistic. 18 In the setting of professional sports practice in the UK, the BAMIC classification system which was originally described for the assessment of hamstring injury is widely used. It can be extrapolated to other areas of the body and aims to more accurately subclassify injuries based on the degree of tendon involvement amongst other parameters to aid more accurate prognostication and RTP times. 2 It is known that high-grade injuries involving the central tendon lead to slower recover times for athletes and delay in returning to competitive play. 19 A lack of awareness of this newly defined anatomy of the proximal rectus femoris could lead to greater interobserver discrepancy of grading.
Aside from our findings that support Tubbs et al in the presence of a capsular head tendon of rectus femoris and our ability to resolve this on imaging, our review has also shed light on the possibility of a separate myotendinous anatomy of the central septum. As suggested by Kassarjian in 2013, injury to the deep intramuscular tendon causes a ‘de-gloving’ type injury in which the inner bipennate component of the indirect head is dissociated from the more superficial unipennate direct head. 16 As shown in the in Figures 5 and 10, the cases shown demonstrate uncommon oedema patterns with sparing of the deep fibres of the central septum in a case of indirect tendon injury (Figure 5) and conversely with focal absence of the deep fibres of the central septum (the authors term ‘mini-bullseye’) in Figure 7 suggestive of isolated capsular head injury. These cases are discussed further below.
In our institution, we evaluate all proximal rectus femoris injuries in professional athletes with MRI. Ultrasound has been suggested by some authors as a first-line investigation for rectus femoris injury 20 and whilst we demonstrated an atypical appearance of a proximal myotendinous tear on ultrasound in Figure 5b, the ability of ultrasound to resolve the capsular head fibres as a separate entity remain unknown. It is clear from this review that the anatomy of the proximal rectus femoris is unique and highly complex even prior to the concept of the capsular head. The revised human anatomy of this interesting area as initially suggested in 2004 warrants further critical evaluation both clinically and on imaging to further determine its significance and further our understanding.
Footnotes
Acknowledgements: This article/paper/report presents independent research funded/supported by the National Institute for Health Research (NIHR) Leeds Biomedical Research Centre (BRC). The views expressed are those of the author(s) and not necessarily those of the NIHR or the Department of Health and Social Care.
Contributor Information
Thomas Armstrong, Email: thomas.armstrong1@nhs.net.
Bill Pass, Email: bill.pass@nhs.net.
Philip O'Connor, Email: philip.oconnor@nhs.net.
REFERENCES
- 1. Mendiguchia J, Alentorn-Geli E, Idoate F, Myer GD. Rectus femoris muscle injuries in football: a clinically relevant review of mechanisms of injury, risk factors and preventive strategies. Br J Sports Med 2013; 47: 359–66. doi: 10.1136/bjsports-2012-091250 [DOI] [PubMed] [Google Scholar]
- 2. Pollock N, Kelly S, Lee J, Stone B, Giakoumis M, Polglass G, et al. A 4-year study of hamstring injury outcomes in elite track and field using the british athletics rehabilitation approach. Br J Sports Med 2022; 56: 257–63. doi: 10.1136/bjsports-2020-103791 [DOI] [PubMed] [Google Scholar]
- 3. Shamji R, James SLJ, Botchu R, Khurniawan KA, Bhogal G, Rushton A. Association of the british athletic muscle injury classification and anatomic location with return to full training and reinjury following hamstring injury in elite football. BMJ Open Sport Exerc Med 2021; 7: e001010. doi: 10.1136/bmjsem-2020-001010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.. Tubbs RS, Stetler W, Savage AJ, Shoja MM, Shakeri AB, Loukas M, et al. Does a third head of the rectus femoris muscle exist? Folia Morphol. 2006;65(4):377–80. [PubMed] [Google Scholar]
- 5. Brukner P, Connell D. “Serious thigh muscle strains”: beware the intramuscular tendon which plays an important role in difficult hamstring and quadriceps muscle strains. Br J Sports Med 2016; 50: 205–8. doi: 10.1136/bjsports-2015-095136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gyftopoulos S, Rosenberg ZS, Schweitzer ME, Bordalo-Rodrigues M. Normal anatomy and strains of the deep musculotendinous junction of the proximal rectus femoris: MRI features. AJR Am J Roentgenol 2008; 190: W182-6. doi: 10.2214/AJR.07.2947 [DOI] [PubMed] [Google Scholar]
- 7. Pollock N, James SLJ, Lee JC, Chakraverty R. British athletics muscle injury classification: a new grading system. Br J Sports Med 2014; 48: 1347–51. doi: 10.1136/bjsports-2013-093302 [DOI] [PubMed] [Google Scholar]
- 8. Johnson MA, Polgar J, Weightman D, Appleton D. Data on the distribution of fibre types in thirty-six human muscles. an autopsy study. J Neurol Sci 1973; 18: 111–29. doi: 10.1016/0022-510x(73)90023-3 [DOI] [PubMed] [Google Scholar]
- 9. Moraux A, Balbi V, Cockenpot E, Vandenbussche L, Miletic B, Letartre R, et al. Sonographic overview of usual and unusual disorders of the rectus femoris tendon origins. J Ultrasound Med 2018; 37: 1543–53. doi: 10.1002/jum.14352 [DOI] [PubMed] [Google Scholar]
- 10. Hasselman CT, Best TM, Hughes C, Martinez S, Garrett WE. An explanation for various rectus femoris strain injuries using previously undescribed muscle architecture. Am J Sports Med 1995; 23: 493–99. doi: 10.1177/036354659502300421 [DOI] [PubMed] [Google Scholar]
- 11. Ryan JM, Harris JD, Graham WC, Virk SS, Ellis TJ. Origin of the direct and reflected head of the rectus femoris: an anatomic study. Arthroscopy 2014; 30: 796–802: S0749-8063(14)00227-8. doi: 10.1016/j.arthro.2014.03.003 [DOI] [PubMed] [Google Scholar]
- 12. Tubbs RS, Salter G, Oakes WJ. Femoral head of the rectus femoris muscle. Clin Anat 2004; 17: 276–78. doi: 10.1002/ca.10186 [DOI] [PubMed] [Google Scholar]
- 13. Pasta G, Nanni G, Molini L, Bianchi S. Sonography of the quadriceps muscle: examination technique, normal anatomy, and traumatic lesions. J Ultrasound 2010; 13: 76–84. doi: 10.1016/j.jus.2010.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Ouellette H, Thomas BJ, Nelson E, Torriani M. MR imaging of rectus femoris origin injuries. Skeletal Radiol 2006; 35: 665–72. doi: 10.1007/s00256-006-0162-9 [DOI] [PubMed] [Google Scholar]
- 15. Lempainen L, Kosola J, Pruna R, Puigdellivol J, Ranne J, Orava S. Operative treatment of proximal rectus femoris injuries in professional soccer players: A series of 19 cases. Orthop J Sports Med 2018; 6: 2325967118798827. doi: 10.1177/2325967118798827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kassarjian A, Rodrigo RM, Santisteban JM. Intramuscular degloving injuries to the rectus femoris: findings at MRI. AJR Am J Roentgenol 2014; 202: W475-80. doi: 10.2214/AJR.13.10931 [DOI] [PubMed] [Google Scholar]
- 17. Zarins B, Ciullo JV. ACute muscle and tendon injuries in athletes. Clin Sports Med 1983; 2: 167–82. [PubMed] [Google Scholar]
- 18. Boutin RD, Fritz RC, Steinbach LS. Imaging of sports-related muscle injuries. Radiol Clin North Am 2002; 40: 333–62. doi: 10.1016/s0033-8389(02)00008-8 [DOI] [PubMed] [Google Scholar]
- 19. Balius R, Maestro A, Pedret C, Estruch A, Mota J, Rodríguez L, et al. Central aponeurosis tears of the rectus femoris: practical sonographic prognosis. Br J Sports Med 2009; 43: 818–24. doi: 10.1136/bjsm.2008.052332 [DOI] [PubMed] [Google Scholar]
- 20. Bianchi S, Martinoli C, Waser NP, Bianchi-Zamorani MP, Federici E, Fasel J. Central aponeurosis tears of the rectus femoris: sonographic findings. Skeletal Radiol 2002; 31: 581–86. doi: 10.1007/s00256-002-0559-z [DOI] [PubMed] [Google Scholar]