Abstract
Background
Acceptable, effective and feasible support strategies (interventions) for parents experiencing complex post‐traumatic stress disorder (CPTSD) symptoms or with a history of childhood maltreatment may offer an opportunity to support parental recovery, reduce the risk of intergenerational transmission of trauma and improve life‐course trajectories for children and future generations. However, evidence relating to the effect of interventions has not been synthesised to provide a comprehensive review of available support strategies. This evidence synthesis is critical to inform further research, practice and policy approaches in this emerging area.
Objectives
To assess the effects of interventions provided to support parents who were experiencing CPTSD symptoms or who had experienced childhood maltreatment (or both), on parenting capacity and parental psychological or socio‐emotional wellbeing.
Search methods
In October 2021 we searched CENTRAL, MEDLINE, Embase, six other databases and two trials registers, together with checking references and contacting experts to identify additional studies.
Selection criteria
All variants of randomised controlled trials (RCTs) comparing any intervention delivered in the perinatal period designed to support parents experiencing CPTSD symptoms or with a history of childhood maltreatment (or both), to any active or inactive control. Primary outcomes were parental psychological or socio‐emotional wellbeing and parenting capacity between pregnancy and up to two years postpartum.
Data collection and analysis
Two review authors independently assessed the eligibility of trials for inclusion, extracted data using a pre‐designed data extraction form, and assessed risk of bias and certainty of evidence. We contacted study authors for additional information as required. We analysed continuous data using mean difference (MD) for outcomes using a single measure, and standardised mean difference (SMD) for outcomes using multiple measures, and risk ratios (RR) for dichotomous data. All data are presented with 95% confidence intervals (CIs). We undertook meta‐analyses using random‐effects models.
Main results
We included evidence from 1925 participants in 15 RCTs that investigated the effect of 17 interventions. All included studies were published after 2005. Interventions included seven parenting interventions, eight psychological interventions and two service system approaches. The studies were funded by major research councils, government departments and philanthropic/charitable organisations. All evidence was of low or very low certainty.
Parenting interventions
Evidence was very uncertain from a study (33 participants) assessing the effects of a parenting intervention compared to attention control on trauma‐related symptoms, and psychological wellbeing symptoms (postpartum depression), in mothers who had experienced childhood maltreatment and were experiencing current parenting risk factors. Evidence suggested that parenting interventions may improve parent‐child relationships slightly compared to usual service provision (SMD 0.45, 95% CI ‐0.06 to 0.96; I2 = 60%; 2 studies, 153 participants; low‐certainty evidence). There may be little or no difference between parenting interventions and usual perinatal service in parenting skills including nurturance, supportive presence and reciprocity (SMD 0.25, 95% CI ‐0.07 to 0.58; I2 = 0%; 4 studies, 149 participants; low‐certainty evidence). No studies assessed the effects of parenting interventions on parents' substance use, relationship quality or self‐harm.
Psychological interventions
Psychological interventions may result in little or no difference in trauma‐related symptoms compared to usual care (SMD ‐0.05, 95% CI ‐0.40 to 0.31; I2 = 39%; 4 studies, 247 participants; low‐certainty evidence). Psychological interventions may make little or no difference compared to usual care to depression symptom severity (8 studies, 507 participants, low‐certainty evidence, SMD ‐0.34, 95% CI ‐0.66 to ‐0.03; I2 = 63%). An interpersonally focused cognitive behavioural analysis system of psychotherapy may slightly increase the number of pregnant women who quit smoking compared to usual smoking cessation therapy and prenatal care (189 participants, low‐certainty evidence). A psychological intervention may slightly improve parents' relationship quality compared to usual care (1 study, 67 participants, low‐certainty evidence). Benefits for parent‐child relationships were very uncertain (26 participants, very low‐certainty evidence), while there may be a slight improvement in parenting skills compared to usual care (66 participants, low‐certainty evidence). No studies assessed the effects of psychological interventions on parents' self‐harm.
Service system approaches
One service system approach assessed the effect of a financial empowerment education programme, with and without trauma‐informed peer support, compared to usual care for parents with low incomes. The interventions increased depression slightly (52 participants, low‐certainty evidence). No studies assessed the effects of service system interventions on parents' trauma‐related symptoms, substance use, relationship quality, self‐harm, parent‐child relationships or parenting skills.
Authors' conclusions
There is currently a lack of high‐quality evidence regarding the effectiveness of interventions to improve parenting capacity or parental psychological or socio‐emotional wellbeing in parents experiencing CPTSD symptoms or who have experienced childhood maltreatment (or both). This lack of methodological rigour and high risk of bias made it difficult to interpret the findings of this review. Overall, results suggest that parenting interventions may slightly improve parent‐child relationships but have a small, unimportant effect on parenting skills. Psychological interventions may help some women stop smoking in pregnancy, and may have small benefits on parents' relationships and parenting skills. A financial empowerment programme may slightly worsen depression symptoms. While potential beneficial effects were small, the importance of a positive effect in a small number of parents must be considered when making treatment and care decisions. There is a need for further high‐quality research into effective strategies for this population.
Keywords: Female; Humans; Pregnancy; Mothers; Mothers/education; Parents; Parents/education; Pregnant Women; Psychotherapy; Psychotherapy/methods; Stress Disorders, Post-Traumatic; Stress Disorders, Post-Traumatic/therapy
Plain language summary
Do supports during pregnancy or in the two years after birth improve parenting capacity or wellbeing for parents experiencing trauma‐related symptoms, or who experienced maltreatment in their childhood?
Key messages
Most evidence either suggested that parenting and psychological interventions made little or no difference in parental psychological wellbeing and parenting capacity, or it was of low quality so that confidence in the results was very uncertain.
Parenting interventions may slightly improve relationships between mothers and their child compared to usual care.
One psychological intervention could possibly help a slightly greater number of mothers quit smoking when pregnant compared to enhanced usual treatment. Another psychological intervention potentially benefits parents' relationships slightly and another may slightly improve parenting skills.
Interventions for parents with complex PTSD (post‐traumatic stress disorder) or who experienced childhood maltreatment
Childhood maltreatment can lead to complex post‐traumatic stress disorder (CPTSD) in adulthood and problems with relationships. People who experienced childhood maltreatment are also more likely to experience other life adversities and health inequity. These problems can affect parenting and lead to ‘intergenerational cycles’ of trauma.
Types of support for parents who experience childhood maltreatment include psychological therapies, parenting interventions, mind‐body and biomedical approaches, pharmacological therapies and service system approaches.
What did we want to find out?
We wanted to find out which of these supports helped improve parenting capacity and wellbeing in parents who had experienced childhood maltreatment or CPTSD.
What did we do?
We searched for studies that looked at how well these interventions worked compared to usual perinatal supports, for improving parents' parenting skills and their wellbeing. We compared and summarised the results of the studies and rated our confidence in the evidence, based on factors such as study methods and sample sizes.
What did we find?
We found 15 studies that involved 1925 parents who had experienced childhood maltreatment and/or who had CPTSD or PTSD symptoms. About half of the studies included people who had experienced moderate‐severe childhood maltreatment, while the others experienced lower levels of childhood maltreatment.
Most studies looked at how well parenting or psychological interventions worked, and these were mostly compared to usual prenatal or postnatal care. We found no studies that looked at mind‐body, biomedical or pharmacological approaches to improving parenting capacity or parent wellbeing. Most studies reported changes in wellbeing or parenting outcomes immediately after finishing the intervention. The interventions ranged from a single session to 12 months of weekly sessions. All but one study took place in the USA, and almost all people who took part were mothers. Most studies were funded by major research councils, government departments and philanthropic/charitable organisations.
Main results
We found that most of the studies did not use rigorous methods (to account for dropout) and therefore the results were uncertain.
Parenting interventions
Evidence was very uncertain from a study of a parenting intervention compared to a control on trauma‐related symptoms, and psychological wellbeing symptoms (postnatal depression), in mothers who had experienced childhood maltreatment and were experiencing current parenting risk factors. Two studies found that parenting interventions may slightly improve the relationship between mothers and their child compared to usual care. Four studies found little to no difference between a parenting intervention and usual care in parenting skills. No studies assessed the effects of parenting interventions on parent's substance use, relationship quality or self‐harm.
Psychological interventions
Four studies found little or no difference in trauma‐related symptoms from a psychological intervention compared to usual care. Eight studies found little or no difference between a psychological intervention and usual care in parents psychological wellbeing (depression). Another study showed that the addition of a psychological intervention may help slightly more women quit smoking in pregnancy than usual prenatal care and smoking cessation counselling. Another found that a psychological intervention may help parents' relationship quality slightly. The evidence from one study was very uncertain about whether a psychological intervention made any difference to parent‐child relationships compared to usual care. Another study found that there may be small improvements in parenting skills when parents received a psychological intervention compared to usual care. No studies assessed the effects of psychological interventions on parents' self‐harm.
Service system approaches
One financial education programme for parents with low incomes and childhood maltreatment histories increased depression symptoms slightly compared to usual care. No studies assessed the effects of service system interventions on parents' trauma‐related symptoms, substance use, relationship quality, self‐harm, parent‐child relationships or parenting skills.
What are the limitations of the evidence?
We are not confident in the results from a lot of the studies because many people dropped out during the study, so there was a lot of missing data and there were not enough large, well‐designed studies to be certain about the results. There is limited evidence of important benefits available so far in this emerging field.
How up‐to‐date is this evidence?
The evidence is up‐to‐date to October 2021.
Summary of findings
Summary of findings 1. Summary of findings table ‐ Parenting interventions compared to inactive control (usual care care, attention control, waitlist) for parents who are experiencing CPTSD symptoms or have experienced maltreatment in childhood.
| Parenting interventions compared to inactive control (usual care care, attention control, waitlist) for parents who are experiencing CPTSD symptoms or have experienced maltreatment in childhood | ||||||
| Patient or population: parents who are experiencing CPTSD symptoms or have experienced maltreatment in childhood Setting: community‐based programmes, hospitals, out‐patient clinics, public community health centres Intervention: parenting interventions Comparison: inactive control (usual care care, attention control, waitlist) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with inactive control (usual care care, attention control, waitlist) | Risk with parenting interventions | |||||
| Trauma‐related symptoms ‐ post‐interventionb | ‐ | SMD 0.16 SD lower (0.85 lower to 0.53 higher) | ‐ | 33 (1 RCT) | ⊕⊝⊝⊝ Very lowc,d | The evidence is very uncertain about the effects of parenting interventions on CPTSD/PTSD symptoms |
| Psychological wellbeing ‐ post‐interventione | ‐ | SMD 0 SD (0.69 lower to 0.69 higher) | ‐ | 33 (1 RCT) | ⊕⊝⊝⊝ Very lowc,d | The evidence is very uncertain about the effects of parenting interventions on psychological wellbeing (postpartum depression) |
| Substance use ‐ post‐intervention ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported data |
| Parent relationship quality ‐ post‐intervention ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported data |
| Parental self‐harm ‐ post‐intervention ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported data |
| Parent–child relationship (continuous data) ‐ post‐interventionf | ‐ | SMD 0.45 SD higher (0.06 lower to 0.96 higher) | ‐ | 153 (2 RCTs) | ⊕⊕⊝⊝ Lowg,h,i | Parenting interventions may improve parent–child relationship slightly |
| Parenting skills ‐ post‐interventionj | ‐ | SMD 0.25 SD higher (0.07 lower to 0.58 higher) | ‐ | 149 (4 RCTs) | ⊕⊕⊝⊝ Lowk,l | Parenting interventions may result in little to no difference in parenting skills |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; SMD: standardised mean difference | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| See interactive version of this table: https://gdt.gradepro.org/presentations/#/isof/isof_question_revman_web_432966949919695522. | ||||||
a Interpretation of importance of SMD effect sizes: < 0.40 = small (trivial) effect (little or no difference), 0.40 to 0.7 = small but important effect (‘slight’ reduction/increase in outcome), > 0.7 = large effect (large reduction/increase in outcome). b Outcome: PTSD assessed with The National Women's Study PTSD Module (PNWS‐PTSD), lower scores = less harm. c Evidence downgraded 1 level for risk of bias; single study with some concerns about risk of bias. d Evidence downgraded 2 levels for imprecision; the 95% CI includes appreciable benefit and appreciable harm (i.e. crosses the threshold for both important benefit (SMD ≥ 0.4) and important harm (SMD ≤ ‐0.4)). e Outcome: postpartum depression symptoms assessed with Postpartum Depression Screening Scale (PDSS), lower scores = less harm. f Outcomes: parental sensitivity, assessed with Nursing Child Assessment Teaching Scale (NCATS); dyadic reciprocity assessed with Coding Interactive Behaviour System (CIB), higher score = greater benefit. g Evidence downgraded 1 level for risk of bias; high risk of bias for one study (49.8% of weight in the meta ‐analysis) and some concerns about risk of bias for the other study. h Evidence not downgraded for inconsistency: point estimates differ but confidence intervals overlap and, in both studies, the confidence interval is consistent with both little or no difference and important harm/benefit. (P value Chi2 = 0.11; I2 = 60%). i Evidence downgraded 1 level for imprecision; the 95% CI includes ‘little or no’ difference and appreciable benefit (i.e. crosses the threshold for important benefit: SMD ≥ 0.4). j Outcomes: Maternal supportive presence (2 studies) assessed with Coding Interactive Behaviour System (CIB) and direct observation; Parental self‐efficacy in nurturance, valuing the child and empathetic responsiveness assessed with Self‐Efficacy for Parenting Tasks Index ‐ Toddler Scale (SEPTI‐TS) (1 study); child caregiving behaviours assessed with Caregiving Helplessness Questionnaire (CHQ) (reverse scored, 1 study), higher score = greater benefit. k Evidence downgraded 1 level for risk of bias; high risk of bias for one study (51.8% of weight in the meta‐analysis) and some concerns about risk of bias for all other studies. l Evidence downgraded 1 level for imprecision; the 95% CI includes ‘little or no’ difference and appreciable benefit (i.e. crosses the threshold for important benefit: SMD ≥ 0.4).
Summary of findings 2. Summary of findings table ‐ Psychological interventions compared to inactive control (usual care care, attention control, waitlist) for parents who are experiencing CPTSD symptoms or have experienced maltreatment in their childhood.
| Psychological interventions compared to inactive control (usual care care, attention control, waitlist) for parents who are experiencing CPTSD symptoms or have experienced maltreatment in their childhood | ||||||
| Patient or population: parents who are experiencing CPTSD symptoms or have experienced maltreatment in their childhood Setting: community‐based programs, hospitals, out‐patient clinics, public community health centres Intervention: psychological interventions Comparison: inactive control (usual care care, attention control, waitlist) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with inactive control (usual care care, attention control, waitlist) | Risk with psychological interventions | |||||
| Trauma‐related symptoms ‐ post‐interventionb | ‐ | SMD 0.05 SD lower (0.4 lower to 0.31 higher) | ‐ | 247 (4 RCTs) | ⊕⊕⊝⊝ Lowc | Psychological interventions may not reduce CPTSD/PTSD symptoms |
| Psychological wellbeing ‐ post‐interventiond | ‐ | SMD 0.34 SD lower (0.66 lower to 0.03 lower) | ‐ | 507 (8 RCTs) | ⊕⊕⊝⊝ Lowe,f | Psychological interventions may result in little to no difference in psychological wellbeing (depression) |
| Substance use ‐ post‐interventiong | 95 per 1000 | 149 per 1000 (68 to 327) | RR 1.57 (0.72 to 3.45) | 189 (1 RCT) | ⊕⊕⊝⊝ Lowh,i | Psychological interventions may increase the proportion of participants who abstain from smoking slightly. |
| Parent relationship quality ‐ post‐interventionj | ‐ | SMD 0.49 SD higher (0 to 0.98 higher) | ‐ | 67 (1 RCT) | ⊕⊕⊝⊝ Lowk,l | Psychological interventions may increase parent relationship quality slightly |
| Parental self‐harm ‐ post‐intervention ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported data |
| Parent–child relationship ‐ post‐interventionm | 71 per 1000 | 334 per 1000 (43 to 1000) | RR 4.67 (0.60 to 36.29) | 26 (1 RCT) | ⊕⊝⊝⊝ Very lown,o | The evidence is very uncertain about the effects of psychological interventions on the proportion of participants with worse parent‐child relationships (disorganised infant attachment) |
| Parenting skills ‐ post‐interventionp | ‐ | SMD 0.51 SD higher (0.01 higher to 1 higher) | ‐ | 66 (1 RCT) | ⊕⊕⊝⊝ Lowk,l | Psychological interventions may improve parenting skills slightly |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; RR: risk ratio; SMD: standardised mean difference | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| See interactive version of this table: https://gdt.gradepro.org/presentations/#/isof/isof_question_revman_web_432973066814822713. | ||||||
a Interpretation of importance of SMD effect sizes: < 0.40 = small (trivial) effect ‐ (little or no difference), 0.40 to 0.7 = small but important effect (‘slight’ reduction/increase in outcome), > 0.7 = large effect (large reduction/increase in outcome). b Outcomes: PTSD symptom severity assessed with PTSD CheckList ‐ Civilian Version (PCL‐C) and Post‐traumatic Stress Scale (PSS) (2 studies); Interpersonal problems assessed with Inventory of Interpersonal Problems (IIP); Dissociation symptoms assessed with Adolescent Dissociative Experiences Scale (A‐DES), lower scores = less harm. c Evidence downgraded 2 levels for risk of bias; high risk of bias for three studies (88.2% of weight in the meta‐analysis) and some concerns about risk of bias for one other study. d Outcome: Depression symptom severity assessed with Hamilton Rating Scale for Depression (HRSD); Center for Epidemiologic Studies Depression Scale (CES‐D); Beck Depression Inventory (BDI); Beck Depression Inventory II (BDI‐II); Hopkins Symptom Checklist (SCL‐20); Quick Inventory of Depressive Symptoms (QIDS); Edinburgh Postnatal Depression Scale (EPDS), lower scores = less harm. e Evidence downgraded 1 level for risk of bias; high risk of bias for two studies (26.2% of weight in the meta‐analysis) and some concerns about risk of bias for all other studies. f Evidence downgraded 1 level for imprecision; the 95% CI includes ‘little or no’ difference and appreciable benefit (i.e. crosses the threshold for important benefit: SMD ≥ 0.4). g Outcome: smoking cessation assessed with timeline follow‐back (TLFB) interview, higher scores = greater benefit. h Evidence downgraded 1 level for risk of bias; single study with some concerns about risk of bias. i Evidence downgraded 1 level for imprecision; the 95% CI includes ‘little or no’ difference and appreciable benefit (in absolute terms from 2 fewer per 100 to 24 more). j Outcome: Social support assessed with the Interpersonal Support Evaluation List (ISEL). Higher scores = less harm. k Evidence downgraded 1 level for risk of bias; one study with some concerns. l Evidence downgraded 1 level for imprecision; the 95% CI includes 'little or no' difference and large appreciable benefit (i.e. crosses the threshold for important benefit: SMD ≥ 0.4). m Outcome: disorganised infant attachment assessed with Ainsworth Strange Situation Paradigm (SSP), lower scores = less harm. n Evidence downgraded 2 levels for risk of bias; single study at high risk of bias. o Evidence downgraded 2 levels for imprecision; the 95% CI includes ‘little or no’ difference and appreciable harm (in absolute terms from 3 fewer per 100 to 100 more); the event rate is very low (4 in intervention group; 1 in control). p Outcome: providing a stimulating, nurturing and safe environment assessed with Home Observation for Measurement of the Environment Inventory (HOME), higher score = greater benefit.
Summary of findings 3. Summary of findings table ‐ Service system approaches compared to inactive control (usual care care, attention control, waitlist) for for parents who are experiencing CPTSD symptoms or have experienced maltreatment in their childhood.
| Service system approaches compared to inactive control (usual care care, attention control, waitlist) for for parents who are experiencing CPTSD symptoms or have experienced maltreatment in their childhood | ||||||
| Patient or population: for parents who are experiencing CPTSD symptoms or have experienced maltreatment in their childhood Setting: Community‐based programs, hospitals, out‐patient clinics, public community health centres Intervention: Service system approaches Comparison: inactive control (usual care care, attention control, waitlist) | ||||||
| Outcomes | Anticipated absolute effects* (95% CI) | Relative effect (95% CI) | № of participants (studies) | Certainty of the evidence (GRADE) | Comments | |
| Risk with inactive control (usual care care, attention control, waitlist) | Risk with Service system approaches | |||||
| Trauma‐related symptoms ‐ post‐intervention ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported data |
| Psychological well‐being ‐ post‐interventiona | ‐ | SMD 0.42 SD higher (0.15 lower to 0.99 higher) | ‐ | 52 (1 RCT) | ⊕⊕⊝⊝ Lowb,c | Service system approaches may worsen psychological wellbeing (depression) slightly.d |
| Substance use ‐ post‐intervention ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported data |
| Parent relationship quality ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported data |
| Parental self‐harm ‐ post‐intervention ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported data |
| Parent–child relationship ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported data |
| Parenting skills ‐ post‐intervention ‐ not reported | ‐ | ‐ | ‐ | ‐ | ‐ | No studies reported data |
| *The risk in the intervention group (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI). CI: confidence interval; MD: mean difference; SMD: standardised mean difference | ||||||
| GRADE Working Group grades of evidence High certainty: we are very confident that the true effect lies close to that of the estimate of the effect. Moderate certainty: we are moderately confident in the effect estimate: the true effect is likely to be close to the estimate of the effect, but there is a possibility that it is substantially different. Low certainty: our confidence in the effect estimate is limited: the true effect may be substantially different from the estimate of the effect. Very low certainty: we have very little confidence in the effect estimate: the true effect is likely to be substantially different from the estimate of effect. | ||||||
| See interactive version of this table: https://gdt.gradepro.org/presentations/#/isof/isof_question_revman_web_433493680305253470. | ||||||
a Outcome: Depression symptom severity assessed with Center for Epidemiological Studies Depression scale (CESD), lower scores = less harm. b Evidence downgraded 1 level for risk of bias; one study with high risk of bias. c Evidence downgraded 1 level for imprecision; the 95% CI includes 'little or no difference' and large appreciable benefit (i.e. crosses the threshold for important harm: SMD ≥ 0.4). d Interpretation of importance of SMD effect sizes: < 0.40 = small (trivial) effect ‐ (little or no difference), 0.40 to 0.7 = small but important effect (‘slight’ reduction/increase in outcome), > 0.7 = large effect (large reduction/increase in outcome)
Background
Description of the condition
Complex post‐traumatic stress disorder (CPTSD) has been formally recognised in the International Classification of Diseases, 11th Edition (ICD‐11; WHO 2019). Core symptom clusters include those associated with post‐traumatic stress disorder (PTSD) (avoidance of traumatic reminders, persistent sense of current threat, such as hypervigilance, and re‐experiencing of the traumatic event in the present, such as flashbacks). CPTSD includes three further symptom clusters that collectively represent disturbances in self‐organisation (DSO; affect dysregulation, negative self‐concept and disturbances in relationships) (Cloitre 2018; Cloitre 2019; Erickson 2019; Frost 2020).
CPTSD symptoms are most strongly associated with repeated exposure to severe traumatic events, often involving interpersonal violation and a sense of inescapability (Cloitre 2019). Childhood maltreatment, affecting up to 50% of all children worldwide (Black 2017; Stoltenborgh 2015; WMA 2017), is the most common antecedent to complex trauma‐related symptoms (Agazzi 2019; Frost 2020; Karatzias 2017; Seng 2013). Research has highlighted long‐lasting adverse social, emotional and physical health consequences of childhood maltreatment across the life‐course (Bellis 2014; Dong 2003; Felitti 1998; Hardcastle 2018). However, not all people who experience childhood maltreatment experience CPTSD. One of the few published prevalence studies of CPTSD found that 3.8% of adults in the USA met the criteria for CPTSD, and an additional 3.4% for PTSD, with higher rates reported among women than men (Cloitre 2019). Not all people who experience CPTSD were exposed to childhood trauma; CPTSD can also be associated with and compounded by repeated exposure to cumulative traumatic events in adulthood (Cloitre 2013; Cloitre 2019; Frost 2020; Herman 1992).
The Power Threat Meaning Framework (PTMF), developed by the British Psychological Society, outlines the role of power and threat in people's lives, and the ways humans have learned to respond to threat (Johnstone 2018), often called 'symptoms' in mental health practice. The PTMF conceptualises complex trauma responses as a way people make sense of difficult experiences, as an alternative to traditional conceptualisations of mental health pathologies and 'diagnoses', which may increase feelings of shame, self‐blame and fear (Johnstone 2018).
As CPTSD has only been recently formally recognised as a condition and is therefore unlikely to be included in many previous publications, we included interventions to support parents with a history of childhood maltreatment in this review. This inclusion is because childhood maltreatment is the most common antecedent of CPTSD, and those particular childhood experiences are likely to be most relevant during the critical transition to becoming a parent. We also included studies of parents with a history of childhood removal from their family of origin, as this most commonly occurs following 'substantiated child abuse' by child protection authorities (e.g. interventions to support young people who are becoming parents in out‐of‐home care settings).
This review adopts the broad World Health Organization (WHO) definition of childhood maltreatment: "Child abuse or maltreatment constitutes all forms of physical and/or emotional ill‐treatment, sexual abuse, neglect or negligent treatment or commercial or other exploitation, resulting in actual or potential harm to the child's health, survival, development or dignity in the context of a relationship of responsibility, trust or power" (Krug 2002, page 59). Children aged three years and under are most likely to be maltreated (Sethi 2013), with one in four adults reporting being physically abused as a child and one in eight sexually abused (Stoltenborgh 2015; WHO 2020). However, few women disclose previous abuse experiences to their care providers in pregnancy (Coles 2009).
Experiences of childhood maltreatment are not equally distributed, and the WHO uses a socio‐ecological framework to illustrate how higher levels of social adversity are associated with increased rates of violence and child maltreatment worldwide (Dahlberg 2002). Factors related to adversity and childhood maltreatment also interact leading to increased prevalence of adult risk behaviours such as smoking, obesity and violence perpetuation (Bellis 2014), which can create a 'compounding intergenerational effect' on health inequities (Chamberlain 2019a).
Complex PTSD or a history of maltreatment in childhood (or both) can impact on parenting, potentially leading to 'intergenerational cycles' of trauma (Chamberlain 2019b). Evidence from populations exposed to traumatic experiences such as genocide, colonisation, social marginalisation and subjugation, and war show that parental adversity is associated with socio‐emotional and psychological problems, and poor physical health than that of non‐trauma‐exposed individuals across several generations (Brave Heart 1998; Giladi 2013; McKenna 2022; Plant 2017; Yehuda 2008). Children of parents experiencing PTSD symptoms have been found to be adversely impacted by their parent's distress and trauma responses both directly through parents' projected emotions and, potentially, epigenetic factors, and indirectly via disturbed parent‐child attachment (Conching 2019; Howe 2006; O’Neill 2018; Yehuda 2018). Proposed mechanisms include impacts on systems of self‐organisation (e.g. affective, self‐concept and relationship domains), which in turn are associated with an increased risk of anxiety and depression in parents (Cloitre 2013; Lange 2020; Zajac 2019). Critically, the parent–child relationship may be influenced by the parent's own experiences of being parented (Fava 2016; Savage 2019; Seng 2013). This can affect parent–infant attachment and, in turn, children's developmental outcomes (Bowlby 1988; Bretherton 1992; Erickson 2019; Seng 2013). Thus, parental psychological wellbeing, and parenting capacity, are important outcomes when assessing the impact of interventions delivered in the perinatal period to address effects of CPTSD or childhood maltreatment.
Description of the intervention
This review considers any intervention provided during pregnancy or up to two years after birth that is designed to support parents who are experiencing CPTSD symptoms or have experienced childhood maltreatment (or both).
The transition to parenthood is a critical life period, particularly for parents who have experienced maltreatment in their own childhoods or are impacted by CPTSD (or both) (Belsky 1980; Chamberlain 2019c; Fava 2016; Narayan 2019). Parent stress may be increased, and consequently post‐traumatic adaptations can become exacerbated or memories of childhood maltreatment relived (Berthelot 2018; Zajac 2019). For women with a history of childhood sexual abuse, for example, the intimate nature of many experiences associated with pregnancy and childbirth may trigger CPTSD symptoms such as flashbacks, hyperarousal or avoidance (Sperlich 2017). Importantly, the transition to parenthood can be an important time of hope, healing and recovery, as new or different parenting patterns are imagined and sought (Chamberlain 2019c; Counts 2017). This period from pregnancy to two years after birth is also usually the first time since childhood that regular, frequent contact with healthcare professionals occurs. This creates a unique opportunity for those impacted by CPTSD to access acceptable and effective support (Seng 2013; Sperlich 2017).
Support for parents (with or without symptoms of CPTSD and/or an explicit history of maltreatment in childhood) often includes cognitive behavioural and psycho‐educational intervention strategies (Agazzi 2019). The rationale for such interventions stems from child development and attachment theories that highlight the important role of primary carers (Erickson 2019). The multiplicity of risk and resilience factors associated with parenting while experiencing complex trauma‐related distress, and the types of support strategies which might be needed, pose challenges for developing an overarching theory of change model for interventions (Frechtling 2007; Funnell 2011). Figure 1 broadly summarises potential associations between maltreatment in childhood, possible complex trauma consequences that can be mediated by risk and resilience factors, and impacts that might need to be considered in interventions for parents.
1.
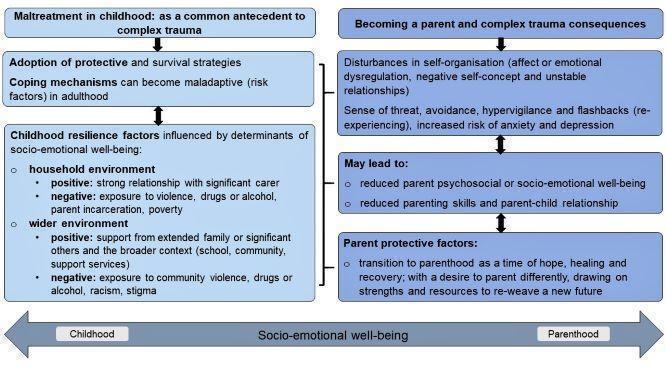
Potential associations between maltreatment in childhood, complex trauma (CPTSD) and becoming a parent.
Interventions within the scope of this review
Given the anticipated diversity of interventions and range of included support strategies for parents, and the variety of implementation contexts (e.g. antenatal and maternity clinics, general practice, community‐based public health settings or child protection departments), we proposed categories to guide the conceptual thinking for study inclusion, synthesis and identification of relevant outcomes. The rationale for the categories was grounded in the findings of our previous scoping review (Chamberlain 2019b), and qualitative systematic review of parent's experiences (Chamberlain 2019c), which point to a diverse range of preferences and needs, and the importance of choice. We also examined recommendations for support for parents in several national guidelines, including: Mental Health Care in the Perinatal Period: Australian Clinical Practice Guidelines (Austin 2017); and the Australian Department of Health (DoH) Pregnancy Care Guidelines (DOH 2020).
In addition, we consulted the evidence‐based PTMF, a multifactorial and contextual approach that incorporates social, psychological and biological factors in emotional distress (Johnstone 2018); Practice Guidelines for Treatment of Complex Trauma and Trauma Informed Care and Service Delivery (Kezelman 2012; Kezelman 2019); the Australian Guidelines for the Prevention and Treatment of Acute Stress Disorder, PTSD and Complex PTSD (Phoenix Australia 2020); and several key reviews to foster consistency of intervention categories across research reporting (Bisson 2020; Bisson 2021; Caro 2019; Erickson 2019; Law 2019; Lewis 2020; Sánchez‐Meca 2011).
Recognising that there is considerable overlap between categories and that many comprehensive interventions include elements of several categories, for the purpose of this review we grouped interventions into the categories outlined in Table 4.
1. Intervention categories, descriptions and examples.
| Category | Description/identifying features | Examples |
| Psychological interventions | These approaches address the emotions, cognitions, meanings, perceptions and behaviours associated with or arising from complex trauma, with the primary goal of improving participant mental health and social and emotional wellbeing (Lewis 2020). |
|
| Parenting‐, parent–child‐ or relationship‐focused interventions | These approaches seek to support the healthy development of early parent–child or couple's relationships, typically grounded in attachment theory. They may or may not additionally address parental emotions, cognitions and behaviours associated with or arising from complex trauma. These are relational approaches that view the parent–child or couple relationship "as the vehicle for change, insofar as mothers' representations of her child, reflexive capacity, parenting behaviours and mental well‐being are targets for intervention" (Erickson 2019, page 251‐4). Most include a range of educational and cognitive behavioural elements and techniques. Some include specific elements on peer support, and efforts to link parents to relevant services and social supports (Rosenblum 2017). |
|
| Mind–body approaches | Non‐clinical, non‐pharmacological approaches that adopt emerging or longstanding holistic strategies or theories to promoting wellbeing and recovery from trauma (Bisson 2020). |
|
| Pharmacological and biomedical therapies | Pharmacological treatments provided as an adjunct to other interventions that aim to address symptoms/comorbidities of complex trauma such as depression, anxiety and psychosis (Bisson 2021; Hoskins 2021). |
|
| Service system approaches | These approaches refer to those that are aimed at addressing issues with the care system to improve access and support for parents experiencing complex trauma or with past experiences of childhood maltreatment (or both), rather than individuals. These include targeted models of care, specific training and strategies to improve access to care (Morelen 2018; Muzik 2015; Rosenblum 2018). |
|
Categories include all modes of delivery (individual, group, Internet etc.).
CBT: cognitive behavioural therapy; Child FIRST: Child and Family Interagency Resource, Support & Training; CPP: Infant/Child Parent Psychotherapy; M‐ITG: Mother‐Infant Therapy Group.
How the intervention might work
We developed an initial logic model (see Figure 2) to outline the intervention categories from Table 4 and their characteristics, to support the reasoning underpinning our review questions (Anderson 2011). We used a staged logic modelling approach built through consensus with review authors (Rehfuess 2018). We implemented the staged approach to reduce bias and allow modification and revision of the logic model as information was revealed through the systematic review process (Rehfuess 2018). No modifications of the model were required.
2.
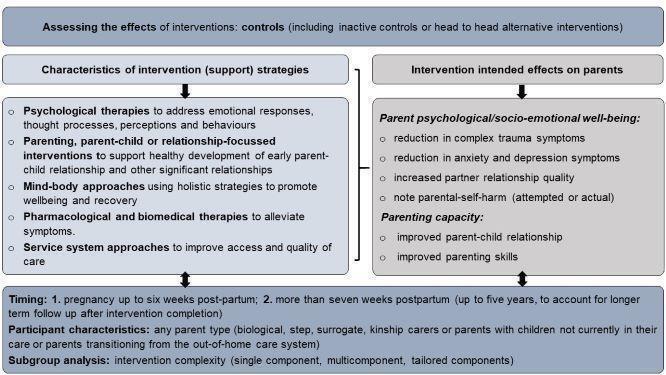
Assessing interventions: characteristics of interventions and intervention effects.
Psychological therapies
Psychological therapies broadly seek to recognise, name and process responses in relation to experiences, and many have been recommended as suitable options for parents (Arons 2005; Perlman 2011). Therapy focuses on the maladaptive mental representations of self (typically formed from experiences in childhood) (Perlman 2011) and address emotions, cognitions, meanings, perceptions and behaviours associated with or arising from complex trauma or experiences of childhood maltreatment (or both) (Lewis 2020). For example, mindfulness activities aim to reduce stress and feelings of becoming overwhelmed, or being aware of trauma response 'triggers' (in carers with childhood maltreatment histories) (Gannon 2017; Miklósi 2017; Van der Kolk 2014).
Parenting‐, parent–child‐ or relationship‐focused interventions
Parenting with CPTSD symptoms or a history of childhood maltreatment may affect the development of early parent–child and other relationships and 'parenting' beliefs, attitudes and behaviours (Morelen 2018).
The importance of parent–child attachment was highlighted several decades ago by John Bowlby and Mary Ainsworth in their seminal work on attachment theory (Ainsworth 1997; Bowlby 1988; Rajecki 1978). Attachment theory emphasises the critical need for safe, secure parent–child relationships (Bowlby 1988; Bretherton 1992; Lange 2020). Attachment theory has significantly influenced current strategies to enhance parent–child relationships. Support strategies aim to support healthy development of early parent–child relationships, and the establishment of a confident parenting identity (Fisher 2018). An example of this is the 'Mom Power' intervention (Muzik 2015).
Many parenting interventions typically incorporate attachment theory and aim to help parents respond effectively to soothe their baby, improve interpersonal relationships and foster positive parent–child interactions (Chaffin 2011; Hagan 2017; Zaccagnino 2013; Zlotnick 2011). For example, the Building Early Attachment and Resilience (BEAR) intervention study (Bant 2018).
Parenting group programmes may or may not be underpinned by theories that aim to help identify, examine and modify relevant thoughts and emotions; teach self‐care and coping skills; and employ educational approaches to increase parenting knowledge and confidence (Erickson 2019; Rouhe 2015; SmithBattle 2017; Upshur 2016). These programmes sometimes take a manualised psychosocial approach with structured, time‐limited sessions delivered by trained professionals (Upshur 2016). Group models are designed to foster social connection, improve interpersonal skills, and provide peer support and peer‐to‐peer learning. Parents often have an opportunity to share and learn from others at a similar life stage (parenthood), with similar life experiences (Hiebert‐Murphy 2000; SmithBattle 2017). Previous research has suggested that parents experiencing CPTSD symptoms or with childhood maltreatment histories (or both) may be more vulnerable to mental health difficulties due to limited personal and social resources (Berthelot 2018; Grote 2017). Hence, building and enabling a support network through group work attendance can be an important strategy in the transition to parenting.
Parenting programmes delivered from the health or community service contexts aim to help parents develop skills in parenting and influence change through a range of strategies including education, modelling and reinforcement (Paris 2013; Pickering 2015; Rosenblum 2017; Steele 2019). Home visitation models are included in this category and are aimed at prevention and early intervention. These may target a variety of outcomes including improving parent–child attachment, parenting behaviours, parenting self‐efficacy, child development, school readiness, and prevention of child abuse and neglect (Ammerman 2009; Barlow 2007; LeCroy 2011; Pickering 2015). Nurses, social workers, paraprofessionals, allied health assistants or trained peer advocates may provide this in‐home service.
Mind–body approaches
In this review, mind–body approaches refer to a broad grouping of non‐clinical, non‐pharmacological holistic modalities that aim to promote wellbeing and recovery (Bisson 2020); improve self‐esteem and confidence; assist to externalise feelings, thoughts and emotions; promote a sense of self and allow a person to tell their story (Day 2009; Van der Kolk 2014). Examples of these approaches include the healing capacity of creative expression therapies such as writing, art, music and dance, which have been used to address postpartum depression, and in children, adolescents and adults who have experienced abuse and trauma (Ayers 2018; Day 2009). Meditation has also been shown to have a positive effect on areas of the brain critical for physiological self‐regulation (Van der Kolk 2014).
Pharmacological and biomedical interventions
Pharmacological and biomedical interventions are used to reduce symptoms of distress and enhance functioning, in combination with other intervention modalities such as psychological therapies, parenting or mind–body approaches (Grote 2017; Slee 2019). Pharmacotherapies are used to treat complex trauma symptoms such as sleep difficulties, persistent hyperarousal, exaggerated startle response and irritability (angry outbursts), anxiety and depression (Berthelot 2018; Grote 2017; Hendriksen 2014; Slee 2019). Biomedical interventions such as neuromodulation strategies are sometimes proposed to modulate 'fear' or trauma responses, where pharmacological and other therapies have failed to alleviate severe symptoms of trauma‐related distress (Gouveia 2019).
Service system approaches
Parents experiencing CPTSD symptoms or with histories of maltreatment in their own childhoods, or both, may be less likely to engage in care during pregnancy and early years after birth, possibly influenced by avoidance and fear of child protection services (Chamberlain 2019c). Hence, service system approaches that aim to engage parents and foster safety and improve access to effective support strategies are important (Bunting 2019; Ko 2008; Oral 2016; Upshur 2016). These can include education to improve trauma‐informed care, described as a whole system strategy that: realises the impact of trauma; recognises the signs and symptoms; responds through integrating trauma knowledge into policies, procedures and practices; and resists re‐traumatisation through skills training and best‐practice approaches (SAMHSA 2014). Trauma‐informed care has emerged as a best‐practice approach for practitioners, based on the seminal work of Felitti and colleagues (Felitti 1998) with the Adverse Child Experiences (ACEs) studies (Bunting 2019; Oral 2016).
Trauma‐informed care also seeks to increase awareness of trauma responses and where possible reduce practices that may exacerbate or trigger trauma responses. Parents have reported a range of experiences during pregnancy and the transition to parenting that are reminiscent of the original trauma and consequently 'trigger' trauma responses, including sounds (e.g. door closing, women calling out in labour), particular smells (e.g. coffee, urine), visual cues (e.g. KY jelly) or sensory experiences (e.g. abdominal and vaginal examinations, breastfeeding) or restraint (Bunting 2019; Chamberlain 2019c). Restraint may be physical (e.g. attached to monitoring equipment and intravenous therapy lines) or pharmacological (e.g. epidural). These experiences can be intensified if the parent has limited control or choice, the carer is perceived as 'insensitive' or 'uncaring,' or a combination of these (Chamberlain 2019c). Interventions to increase trauma‐informed care aim to improve outcomes for parents through fostering safety, choice and control within pregnancy, birth and early postpartum care. Additionally, interventions to increase trauma‐informed early years services (up to child age five years) aim for continued empowerment and collaboration with parents to enhance parent experiences and increase ongoing engagement with support services (Bunting 2019; Oral 2016). Interventions to improve trauma‐informed care can include training for staff, mentoring programmes and models of care that are explicitly designed to improve care for parents experiencing trauma‐related symptoms. There are moves towards 'trauma‐integrated care' where healing trauma is a core philosophy rather than an additional overlay on existing service models or practitioner approaches (Chamberlain 2019c).
Strategies to improve access can also include 'stepped care', 'collaborative care' models and 'continuity of care' models, which enable providers to build relationships and trust with parents. Case management support strategies to assist with co‐ordination of care and service linkage (referral pathways) and access to resources (e.g. housing, clothing, nursery items) are also included within this category. For example, the Mom Power Program, within the connection to resources pillar (Rosenblum 2017).
Why it is important to do this review
There is a need to understand the effectiveness and safety of interventions employed to address CPTSD symptoms in pregnancy and the first two years after birth. Most studies assessing the effect of trauma‐focused therapies for trauma symptoms exclude pregnant women, so there is an evidence gap for this population (Arch 2012; Stevens 2021).
Acceptable, effective and feasible support strategies (interventions) for those experiencing CPTSD symptoms or with a history of childhood maltreatment may offer an opportunity to support parental recovery, reduce the risk of intergenerational transmission of trauma and improve life‐course trajectories for children and future generations (Alink 2019; Arabena 2016; Black 2017; Cusick 2019). However, the limited amount of information in this area has yet to be synthesised to allow the most comprehensive review of effectiveness possible at this time (COPE 2017). This evidence synthesised in this review will be used to help inform further research, practice and policy approaches in this emerging area.
Objectives
To assess the effects of interventions provided to support parents experiencing CPTSD symptoms or who have experienced childhood maltreatment (or both) on parenting capacity and parental psychological or socio‐emotional wellbeing.
Methods
Criteria for considering studies for this review
Types of studies
RCTs (randomised controlled trials) including parallel, cross‐over, cluster, factorial and quasi RCTs.
Types of participants
Any parent (mother or father) during pregnancy or up to two years after birth reported as experiencing trauma‐related symptoms, however defined, or with a history of childhood maltreatment (or both) (see Background for definition), including a history of being removed from their parents (e.g. history of out‐of‐home care). Where it was unclear whether all participants were experiencing CPTSD symptoms or had experienced childhood maltreatment (or both), we included studies where:
the intervention was targeted for parents experiencing CPTSD symptoms or those who had experienced childhood maltreatment (or both); and
the group allocation and outcomes were reported by CPTSD symptoms or childhood maltreatment history status, which allowed us to only include data from those participants.
Parents could be biological, step, surrogate, kinship carers or parents with children not currently in their care. We excluded studies designed for foster parents, as these studies generally have a specific and different focus from the intended interventions in this review.
Where studies included parents of children with mixed ages, we included studies where most children (greater than 50%) were aged two years or under. Where only the mean ages of children were provided, we included studies where the mean age was three years or less, to err towards inclusivity. Parents could have any number of previous children.
Where the intervention involved a service system approach aimed at supporting parents who are experiencing CPTSD symptoms or have experienced maltreatment in childhood, we included studies involving any service system and provider types.
As CPTSD has only recently been formally recognised, we recognised that it would be unlikely to be explicitly included in the published literature. Accordingly, we sought studies focused on interventions designed to support parents who are experiencing CPTSD symptoms (including PTSD and DSO symptom clusters) or who report a history of childhood maltreatment (as this exposure is the most common antecedent of CPTSD). These criteria are consistent with those used in a related scoping review (Chamberlain 2019b), and a systematic review of qualitative studies of parents' views (Chamberlain 2019c), which informed development of the review protocol.
Types of interventions
Any intervention designed to support parents experiencing CPTSD symptoms or with a history of childhood maltreatment (or both), grouped as follows:
psychological interventions;
parenting‐, parent–child‐ or relationship‐focused interventions;
mind‐body approaches;
pharmacological and biomedical therapies;
service system approaches.
See Table 4 for a description of intervention categories and examples of interventions within each category and How the intervention might work for more details.
We included multicomponent interventions from two or more of the main intervention categories and stratified interventions within these groups by 'single', 'multiple' or 'tailored' interventions (see Data collection and analysis section). We included interventions of any duration or frequency. No restrictions were placed on modes of intervention delivery, such as in groups, individual, in the home or community setting, or by postal or electronic mail or online. Interventions could be delivered by healthcare professionals (e.g. nurses, social workers, psychologists, obstetricians or general practitioners) or by lay people (such as peers or advocates) who have received specific training to support parents. Where two eligible interventions were being compared (i.e. head‐to‐head comparison), two review authors made a judgement regarding the primary intervention category grouping, erring towards grouping the more novel and 'experimental' intervention category.
Comparisons
Intervention and comparator groups were compared as follows:
each active intervention group versus any inactive comparator (controls) including usual care, no care, placebos for pharmacotherapy or wait‐list conditions; attention placebo controls of similar duration and frequency (Popp 2015); and
each intervention group versus another eligible intervention (i.e. head‐to‐head comparisons).
Types of outcome measures
Outcomes were focused on change for parents, rather than the wider family. We evaluated the effectiveness of the interventions for each outcome domain (e.g. trauma symptoms, relationship quality) listed within the following outcome categories.
Primary outcomes
Outcomes considered critical to decision makers and eligible for inclusion were as follows.
-
Parental psychological or socio‐emotional wellbeing:
trauma‐related symptoms (including PTSD and CPTSD symptom clusters);
psychological wellbeing symptoms (including anxiety symptoms, depression symptoms, other validated measures of psychological wellbeing, or a combination of these);
substance use (commenced, recommended, increased, decreased);
parents' relationship quality (with partner or significant others); and
parental self‐harm (attempted or actual).
-
Parenting capacity:
parent–child relationship (e.g. interaction, warmth, attachment, mutual responsivity); and
parenting skills (e.g. problem‐solving, coping, self‐efficacy, parent sensitivity and responsiveness).
Secondary outcomes
Other outcomes of importance to decision makers and eligible for inclusion were as follows.
-
Parental intervention acceptability:
parent satisfaction with intervention (e.g. emotional safety, cultural safety, appreciation);
medication compliance (if applicable); and
parent engagement (including dropouts; programme completion).
-
Socio‐ecological outcomes:
social functioning (increased social functioning or social networks, or both); and
changes in social capital (e.g. increased access to employment, education, support/health services) or resources (food, housing, clothing).
-
Child adverse events recorded during the intervention:
child maltreatment occurrence (including exposure to family violence);
family disruptions and child removals; and
other adverse childhood experiences.
-
Child's physical, socio‐emotional wellbeing:
child physical outcomes (e.g. preterm birth, low birth weight, small‐for‐gestational age, neonatal intensive care admission, immunisations, hospitalisations);
child developmental outcomes (e.g. cognition, speech, language, motor skills); and
child emotional and behavioural outcomes (e.g. internalising and externalising behaviour).
-
Other outcomes:
service provider knowledge, attitudes and practices; and
cost or cost‐effectiveness.
Methods of outcome assessment
Any validated measure of the outcomes was eligible. For composite outcome measures, prior to examining the results, we made a consensus judgement about whether the measure was similar enough to an outcome domain in the a priori list (Table 5) to warrant outcome inclusion.
2. Methods of outcome assessment.
| Outcome category | Outcome | Outcome domain | Example measures |
| Critical outcomes | Parental psychological or socio‐emotional well‐being |
Trauma‐related symptoms | International Trauma Questionnaire (Hyland 2017); Disturbances in Self‐Organisation (Shevlin 2018); Trauma‐Related Guilt Inventory (Kubany 1996); Post‐Traumatic Cognitions Inventory (Foa 1999); Difficulties in Emotion Regulation Scale (Gratz 2004) |
| Anxiety symptoms, depression symptoms, other validated measures of psychological wellbeing, or a combination of these | Beck Depression Inventory (Beck 1988a); Beck Anxiety Inventory (Beck 1988b); Post‐partum Depression Screening Scale (Beck 2000); Edinburgh Postnatal Depression Scale (Cox 1987) | ||
| Substance use (commenced, recommenced, increased, decreased) | Validated questionnaire such as the Leeds Dependence Questionnaire (Raistrick 1994) or self‐report or other documented programme or administrative evidence | ||
| Parent relationship quality (with partner or significant others) | Relationship Scales Questionnaire (Bartholomew 1991); Relationship Quality Questionnaire (Griffin 1994); Interpersonal Support Evaluation List (Cohen 1983) | ||
| Parental self‐harm (attempted or actual) | Validated questionnaire or self‐report or other documented programme or administrative evidence, such as the Deliberate Self‐Harm Inventory or Self‐Harm Inventory (Latimer 2013) | ||
| Parenting capacity | Parent–child relationship (e.g. interaction, warmth, attachment, mutual responsivity) | Strange Situation paradigm (Ainsworth 1978); Nursing Child Assessment Teaching Scale (Gross 1993); Toddler Attachment Sort‐45 (Bimler 2002; Kirkland 2004) | |
| Parenting skills (e.g. problem‐solving, coping, self‐efficacy, parent sensitivity and responsiveness) | Parenting Stress Index (Abidin 1990; Abidin 1995); Coping Orientation to Problems Experienced (Carver 1989); Coding Interactive Behaviour system (Feldman 2010) | ||
| Important outcomes | Parental intervention acceptability | Parent satisfaction with intervention (e.g. emotional safety, cultural safety, appreciation) | Validated questionnaires such as Client Satisfaction Questionnaire Scales and the Service Satisfaction Scale‐30 (Attkisson 1996), or self‐report measures (continuous and binary outcomes measured separately) |
| Medication compliance (if applicable) | Self‐report or other documented programme or administrative evidence such as pickup/refill rates (Anghel 2019) | ||
| Parent engagement (including dropouts; programme completion) | Self‐report measures of fidelity and engagement including self‐report, reported dropout (for any reason), retention and participation, adherence to target behaviour or attendance rates with programme or other aspects of care such as antenatal care and maternal child health visits (continuous and binary outcomes measured separately) (Walton 2017) | ||
| Socio‐ecological outcomes | Social functioning (increased social functioning or social networks, or both) | Interpersonal Support Evaluation List (Cohen 1983); Social Network Index (Cohen 1997); Work and Social Adjustment Scale (Marks 1986; Mundt 2002) | |
| Changes in social capital (e.g. increased access to employment, education, support/health services) or resources (food, housing, clothing) | Validated questionnaire or self‐report or other documented or administrative evidence, measures of access or process measures such as: Life Stressor Checklist (Rosenblum 2018); Work and Social Adjustment Scale (Marks 1986; Mundt 2002); Cornell Service Index (Sirey 2005) | ||
| Child adverse events recorded during the intervention | Child maltreatment occurrence (including exposure to family violence) | Assessed by process or administrative evidence such as reported (self‐report or medically attended injuries) and documented as part of the intervention (programme) design; process or administrative evidence such as reported and documented in the intervention outcomes; and validated questionnaires such as the Childhood Trauma Questionnaire, Escape Tool or SPUTOVAMO checklist (McTavish 2020) | |
| Family disruptions and child removals | |||
| Other adverse childhood experiences | |||
| Child's physical, socio‐emotional wellbeing | Child physical outcomes (e.g. preterm birth, low birth weight, small‐for‐gestational age, neonatal intensive care admission, immunisations, hospitalisations) | Validated measures for indicators of child development such as the Bayley Scales of Infant and Toddler Development, Third Edition (Bayley 2006) | |
| Child developmental outcomes (e.g. cognition, speech, language, motor skills) | |||
| Child emotional and behavioural outcomes (e.g. internalising and externalising behaviour) | Validated measures for child emotional and behavioural functioning or other measures of child's socio‐emotional wellbeing such as the Brief Infant‐Toddler Social and Emotional Assessment (Briggs‐Gowan 2004) | ||
| Other outcomes | Service provider knowledge, attitudes and practices | Validated questionnaires (or self‐report) directed at the intervention (programme) workforce such as a Knowledge, Attitude, and Practice survey (King 2019), or the Attitudes Related to Trauma‐Informed Care scale (Baker 2016) | |
| Cost or cost‐effectiveness | Assessed by process measures, such as reported or documented evidence of parenting intervention costs (e.g. programme material, transport, childcare, catering) relative to the costs of an alternative intervention or minimal support, or economic evaluation methods, as outlined by Elbanna 2021 |
Timing of outcome assessment
We extracted and reported data for all available time points. The first time point post‐intervention was used for inclusion in the main meta‐analyses presented in the summary of findings tables.
Selection of outcomes
Where multiple results were reported that were eligible for inclusion in the same comparison, to avoid issues with correlation between effect estimates we used methods outlined in the Cochrane Handbook of Systematic Reviews of Interventions to select the most appropriate outcome for inclusion (McKenzie 2019a).
Search methods for identification of studies
We identified relevant intervention studies by searching the electronic databases listed below up to October 2021. The relevant research literature uses diverse terminology and is not consistently indexed within bibliographic databases. Therefore, the search strategy was informed by research identified from an earlier scoping study (Chamberlain 2019b), qualitative review (Chamberlain 2019c), and further work using the 'related items' searches in PubMed. The search strategy was constructed around two key concepts: parents or the transition to parenthood and a history of childhood maltreatment or intergenerational trauma. These concepts were captured using Boolean searches comprising both index terms and free‐text searches of titles and abstracts.
Electronic searches
We searched the following databases and trials registers.
Cochrane Central Register of Controlled Trials (CENTRAL 2021, Issue 10) in the Cochrane Library and which contains the specialised register for Cochrane Developmental, Psychosocial and Learning Problems. Searched 21 October 2021.
MEDLINE Ovid (1946 to October Week 2 2021).
MEDLINE In‐process and Other Non‐Indexed Citations Ovid (October 15, 2021). Searched 19 October 2021.
MEDLINE Epub Ahead of Print via Ovid (15 October 2021). Searched 19 October 2021.
Embase Ovid (1974 to 18 October 2021).
Cumulative Index to Nursing and Allied Health Literature (CINAHL) EBSCOhost (1937 to 22 October 2021).
APA PsycINFO Ovid (1806 to October Week 3 2021).
PTSDpubs (formerly PILOTS) ProQuest (1871 to 22 October 2021).
Web of Science Core Collection (Science Citation Index, Social Sciences Citation Index, Conference Proceedings Citation Index‐Social Sciences & Humanities, Conference Proceedings Citation Index‐Science; 1970 to 20 October 2021).
Cochrane Database of Systematic Reviews (CDSR 2021, Issue 10) in the Cochrane Library. Searched 21 October 2021.
Epistemonikos (www.epistemonikos.org/en). Searched 22 October 2021.
ClinicalTrials.gov (clinicaltrials.gov). Searched 22 October 2021.
WHO International Clinical Trials Registry Platform (WHO ICTRP) (trialsearch.who.int/). Searched 22 October 2021.
The search strategy used the sensitivity‐maximising version of the Cochrane search strategy for identifying randomised trials (Lefebvre 2021). We modified the search terms and syntax for each database as appropriate (see Appendix 1).
Searching other resources
We checked the reference lists of all included studies and relevant systematic reviews to identify additional studies missed from the original electronic searches. No additional studies were identified.
We contacted relevant individuals and organisations for information about unpublished or current studies.
Prior to publication, we ran searches (2 June 2022) of included studies to identify any retractions due to error or fraud. No retractions were identified.
Data collection and analysis
Methods for this review were prespecified in the protocol (Other published versions of this review). Any unused methods specified in the protocol are outlined in Table 6, with deviations from the protocol reported in the Differences between protocol and review section.
3. Unused methods.
| Method | Details (for future updates) |
| Time‐to‐event outcomes | We will use HRs as our measure of treatment effect for any time‐to‐event outcomes and will present these with 95% CIs. |
| Individually randomised trials with clustering | Clustering may arise in individually randomised trials where each therapist treats multiple patients. For these trials, we use the same approach as described for cluster randomised trials to inflate the variance of the intervention estimates (using a design effect) when clustering has not been accounted for in the trial analysis. However, we would only apply this correction in trials where we can establish the mean number of participants per therapist, and where this number is large enough to affect the variance importantly (Higgins 2022a). |
| Cross‐over trials | If cross‐over designs had been used to evaluate any of our eligible interventions, other than pharmacotherapy, we would only use the data from the first period (if available). A cross‐over design for the interventions eligible for this review (aside from pharmacotherapy) is inappropriate because these interventions can lead to permanent change. In cross‐over trials evaluating pharmacological interventions, where an appropriate paired analysis is not available, we will attempt to approximate a paired analysis by imputing missing statistics (e.g. missing standard deviation, correlation). The values of these statistics will be informed by other trials included in the review, or trials outside the meta‐analysis (Elbourne 2002; Higgins 2022a). We would only include the first period data (if possible) in cross‐over trials in which there is less than two weeks' washout, because in this circumstance there is a serious risk of carry‐over effects arising from the effects of the first‐period antidepressant or antipsychotic persisting into subsequent period(s) (Hosenbocus 2011; Hulshof 2020). |
| Assessment of reporting biases | The risk of missing studies (termed 'unknown‐unknowns'): we will consider qualitative signals of non‐publication of studies (e.g. research area is in the early stages) and statistical signals of missing results. To examine the latter, we plan to investigate the potential for small‐study effects using contour‐enhanced funnel plots. Contour‐enhanced funnel plots aid in determining whether funnel plot asymmetry is due to publication bias or other factors (Peters 2008). |
| Data imputation | We will impute missing summary data (e.g. ICCs, standard deviations), where we are unable to obtain these data from the trial authors, and document the methods used and any assumptions made |
| Meta‐analyses | Given that random‐effects models can yield CIs that are too small, particularly in meta‐analyses with few trials, we will undertake sensitivity analyses using the restricted maximum likelihood (REML) estimator of between trial heterogeneity variance and the Hartung‐Knapp‐Sidik‐Jonkman CI methods (Hartung 2001; Sidik 2002). |
CI: confidence interval; HR: hazard ratio; ICC: intraclass correlation coefficients; REML: restricted maximum likelihood
Selection of studies
We downloaded all titles and abstracts retrieved by electronic searching and from other sources to the reference management database EndNote and removed duplicates. We used Cochrane's Screen4Me workflow to help assess the search results. Screen4Me comprises three components: known assessments – a service that matches records in the search results to records that have already been screened in Cochrane Crowd and been labelled as a randomised controlled trial (RCT) or as not a RCT; the RCT classifier – a machine learning model that distinguishes RCTs from non‐RCTs; and if appropriate, Cochrane Crowd – Cochrane's citizen science platform where the Crowd help to identify and describe health evidence. For more information about Screen4Me and the evaluations that have been done, see the Screen4Me webpage on the Cochrane Information Specialist's portal. In addition, more detailed information regarding evaluations of the Screen4Me components, can be found in the following publications: Marshall 2018; Noel‐Storr 2021; Thomas 2020.
At least two review authors (KJ, CC, TB, RF, ED, CR or IL) independently assessed the titles and abstracts identified through the literature search against the eligibility criteria using Covidence software (Covidence). All potentially eligible studies were coded as 'retrieve' (eligible, potentially eligible or unclear) or 'do not retrieve'. Where review authors disagreed on abstract inclusion, both authors assessed and discussed the full‐text article.
At least two review authors (KJ, RF, TB, IL or IF) assessed the full‐text studies against the eligibility criteria. Studies were identified for inclusion or identified for exclusion. The same two review authors discussed disagreements at either stage of screening. Where agreement could not be reached, or review authors were unsure, a third review author (CC) was consulted. Final decisions were made by consensus. We contacted study authors where eligibility was unclear.
Studies found to be ineligible at the full‐text screening were excluded with a reason. Excluded studies that initially appeared to meet eligibility criteria, but upon further inspection were found ineligible, are outlined in Characteristics of excluded studies, with reasons for exclusion reported.
Records of the search were stored in an EndNote file including folders of original search, title and abstract screening and full‐text reviews, and in a separate flowchart. The selection process was recorded in a PRISMA flow diagram (Page 2021). The flowchart includes: potential studies identified (database searching and additional records), records after duplicates removed, records screened (and excluded), full‐text articles assessed (and excluded, with reasons) and number of studies included.
We collated multiple reports of the same included study (e.g. by checking author names, trial names and trial registry numbers) so that each study, rather than the report, is the unit of interest in the review.
Data extraction and management
Four review authors (KJ, TB, CC, SB) piloted the data extraction and coding form on two purposively selected studies that represented a diversity of data types anticipated in the review. One review author extracted data relating to study characteristics and a second review author independently verified the data. We sought advice from the review topic expert and statisticians to ensure data were extracted as planned. At least two review authors independently extracted quantitative data from each study (KJ, IF, TB, LK, ED, SA). Discrepancies were resolved through discussion and consultation. When agreement could not be reached, a third review author was consulted. Final decisions were made by consensus. The data extraction form (refer to Appendix 2) was refined from the version presented in the protocol to maximise the quality and consistency of data collection. We extracted information relating to the characteristics of participants, interventions, comparators and outcomes as outlined in Appendix 2.
Two review authors (KJ, CC) categorised each intervention and made independent judgements about the 'main' strategy for each intervention type, and subcategory of single, multiple or tailored interventions. Disagreements were resolved by consensus, involving a third review author where agreement could not be reached. All interventions (including those irrelevant to this review) and coding judgements are detailed in the Characteristics of included studies tables to ensure transparency of coding and analysis.
Assessment of risk of bias in included studies
Two review authors independently assessed the risk of bias in each included study using the revised Cochrane risk of bias tool (RoB 2) for randomised trials for each of the primary (critical) outcome domains (Higgins 2022b; Sterne 2019).
RoB 2 addresses five domains:
bias arising from the randomisation process;
bias due to deviations from intended interventions;
bias due to missing outcome data;
bias in measurement of the outcome; and
bias in selection of the reported result.
Two review authors independently applied the tool to the selected results from each study following the RoB 2 guidance (RoB 2 tool 2020), and recorded supporting information and justifications for judgements for each domain (low, some concerns, high risk of bias) using the RoB 2 Excel tool as described in the Cochrane Handbook of Systematic Reviews of Interventions. Our assessment was based on the effect of assignment to the intervention. We derived an overall summary of the risk of bias from each assessment, following the algorithm in the RoB 2 guidance. For cluster trials and cross‐over trials, we used the variant of the RoB 2 tool specific for the design (Higgins 2022a).
When multiple effects of the intervention using different approaches are presented, we selected the effect based on the following hierarchy:
the effect that corresponds to a full intention‐to‐treat analysis, where missing data have been multiply imputed, or a model‐based approach has been used (e.g. likelihood‐based analysis, inverse‐probability weighting);
the effect corresponding to an analysis that adheres to intention‐to‐treat principles except that the missing outcome data are excluded;
the effect that corresponds to a full intention‐to‐treat analysis, where missing data have been imputed using methods that treat the imputed data as if they were observed (e.g. last observation carried forward, mean imputation, regression imputation, stochastic imputation); or
the effect that corresponds to an 'as‐treated' or 'per‐protocol' analysis, where missing participants are excluded (Higgins 2022b; Higgins 2022a).
We resolved discrepancies between review authors through discussion, and a third review author adjudicated where agreement could not be reached. To promote concordance, two review authors piloted the assessment on two studies.
Measures of treatment effect
We have estimated the pairwise relative treatment effects of the interventions by calculating effect sizes appropriate for the type of outcome data provided.
Dichotomous outcome data
We used risk ratios (RR) as our measure of treatment effect for dichotomous outcomes and presented these with 95% confidence intervals (CIs). Empirical evidence suggests RRs are a more consistent measure than risk differences (Deeks 2002), and are more interpretable than odds ratios (Deeks 2019). Dichotomous outcomes presented in this review index either a proportion of participants showing an improvement or the relative risk of a positive or negative state (e.g. attachment classifications). For dichotomous outcomes, when interpreting effects, we used the following thresholds for interpreting the RR: < 0.8 or > 1.25 = clinically important benefit or harm.
Continuous data
We used mean differences (MD) as our measure of treatment effect for continuous outcomes where the studies all use the same measurement instrument. For continuous outcomes where multiple instruments were used to measure the same outcome, we used the standardised mean difference (SMD). We present both with 95% CIs. When interpreting effects we used the following variation on Cohen’s guiding rules for interpreting the SMD: < 0.40 = small (trivial) effect (little or no difference), 0.40 to 0.7 = small but important effect (‘slight’ reduction/increase in outcome), > 0.7 = large effect (large reduction/increase in outcome) (Schünemann 2022).
Unit of analysis issues
We recognised that unit of analysis issues may arise from non‐standard randomised trials (cluster‐randomised trials, individually randomised trials with clustering, cross‐over trials) when the analysis in primary trials does not appropriately account for the correlation in observations these designs induce, or from trials with more than two eligible intervention groups. We outlined planned methods for making adjustments when necessary. Details of any adjustments were documented (e.g. assumed intra‐cluster correlation (ICC) and mean cluster size), and we noted where necessary adjustments were unable to be made due to missing information (e.g. the mean cluster size could not be calculated). We used methods reported in Chapter 23 of the Cochrane Handbook of Systematic Reviews of Interventions (Higgins 2022a; Waleed 2019).
Cluster‐randomised trials
We planned to extract the effect estimates from cluster‐randomised trials and include them in meta‐analyses if they were adjusted appropriately for the cluster design (Higgins 2022b; Higgins 2022a), which one cluster‐randomised trial was. We would have attempted to reanalyse cluster‐randomised trials that had not adjusted for potential clustering of participants within clusters in their analysis, however this was not required for this review. We would have done this by inflating the variance of intervention estimates by a design effect (DEFF). Calculation of a DEFF involves estimation of an ICC. We would have obtained estimates of ICCs through contact with authors, or imputed using estimates from other included studies that report ICCs, or used external estimates from empirical research (e.g. Bell 2013).
Trials with multiple treatment groups
If more than one comparison from the same trial was eligible for inclusion in the same meta‐analysis, we either combined intervention groups (if it made sense to do so), or appropriately reduced the sample size so that the same participants did not contribute more than once. Specifically, we split the sample sizes (and number of events for binary outcomes) of the shared control group by the number of comparisons the shared group contributes to. While this latter approach offers some solution to adjusting the precision of the comparison, it does not account for correlation arising from the same set of participants being in multiple comparisons.
Dealing with missing data
We contacted authors of trials to obtain missing numerical data (e.g. missing standard deviations (SDs)), request data for subgroups of participants with CPTSD symptoms or who had experienced childhood maltreatment (or both), and verify key study characteristics. We calculated summary statistics necessary for the meta‐analysis using algebraic manipulation (e.g. calculating SDs from sample sizes and exact P values). In one three‐arm trial (Booshehri 2018; for two time points) where we had calculated the SD via algebraic manipulation, we determined that the SD in one arm was unrealistically large (potentially due to a mistake in the reported P value). We therefore imputed the SD for this arm by assuming the largest of the two SDs in the other arms.
We assessed the risk of bias due to missing outcome data (see Assessment of risk of bias in included studies), and conducted sensitivity analyses to examine the impact of removing trials at a high risk of bias (see 'Summary of findings and assessment of the certainty of the evidence').
Assessment of heterogeneity
We assessed clinical (participants, interventions, outcomes) and methodological (study design, outcome measures, risk of bias) diversity, and made an assessment of whether the studies were similar enough to be pooled in a meta‐analysis (McKenzie 2019a).
We assessed statistical heterogeneity of the intervention effects by visually examining the degree of overlap of CIs on the forest plot. We undertook a formal test for heterogeneity using the Chi2 test (using a significance level of P = 0.10), and quantified heterogeneity using Tau2 and inconsistency using the I2 statistic (Higgins 2003). We interpreted the I2 statistic considering the magnitude and direction of the effects, and the number of studies. We used suggested adjectives in the Cochrane Handbook for Systematic Reviews of Interventions to describe the magnitude of the I2 statistic (Deeks 2019):
0% to 40%: might not be important;
30% to 60%: may represent moderate heterogeneity;
50% to 90%: may represent substantial heterogeneity; or
75% to 100%: considerable heterogeneity.
Assessment of reporting biases
We used the framework outlined in Chapter 13 of the Cochrane Handbook for Systematic Reviews of Interventions for assessing the risk of bias due to missing results (Page 2019). For each synthesis, we made an assessment regarding:
the risk and potential impact of missing results from studies (termed 'known‐unknowns'); and
the risk of missing studies (termed 'unknown‐unknowns').
In assessing (1), we considered selective non‐reporting of results by examining discrepancies between planned trial analyses (identified from registry entry, trial protocol, methods section of trial report where available) and those actually reported (identified from the trial report). We were unable to assess (2) due to there being insufficient studies in the meta‐analysis to yield useful contour‐enhanced funnel plots. Finally, we undertook sensitivity analyses to examine if the effect estimates in smaller trials differed from those in larger trials (see Sensitivity analysis).
Data synthesis
Meta‐analyses
For each available comparison with at least two trials, we combined the effects of all eligible studies using meta‐analysis. Since we expected clinical and methodological diversity across trials, we used a random‐effects model, which assumes that the different studies are estimating different, yet related, outcome effects (Deeks 2019). We used the methods implemented in RevMan Web to fit the random‐effects model (RevMan Web 2020), which implements the DerSimonian and Laird's method of moments estimator of between trial heterogeneity variance, and a Wald‐type CI based on the normal distribution (DerSimonian 1986). We generated forest plots to display each trial's effect estimate, CI and the combined effect.
Due to the diversity of outcomes within our outcome domains (e.g. psychological wellbeing includes depression, anxiety, etc.) the meta‐analysis results for specific outcomes that are not captured in the summary of findings table are presented in text in the Effects of interventions section.
Summary and synthesis when meta‐analysis is not possible
Additional outcomes for which only one study reported data are presented in tables.
We tabulated available effect estimates (SMD, CIs), details of scales (direction and range), risk of bias assessments and other intervention characteristics (complexity of the intervention – single component, multiple components). We ordered the tables by comparison, outcome and risk of bias assessment.
When we were unable to meta‐analyse the trial effects (e.g. due to incomplete reporting, variability in the effect measures across studies), we considered alternative synthesis methods, such as calculating summary statistics of effect estimates, combining P values or vote counting based on the direction of effect (McKenzie 2019b). We described in the text results from any cost or cost‐effectiveness analyses. Our choice of methods were determined by the available data. In describing the results from these methods, we were clear about the nature of the question addressed by the method and the studies that contribute to the synthesis (Campbell 2020).
Subgroup analysis and investigation of heterogeneity
Within each comparison we undertook subgroup analyses to explore if the magnitude of intervention effect was modified by the complexity of the intervention (single, or multiple components) for the two primary outcome domains: parental psychological or socio‐emotional wellbeing and parenting capacity.
Sensitivity analysis
We undertook and reported sensitivity analyses to examine if the meta‐analytic effect was robust to the following:
Exclusion of trials assessed with an overall high risk of bias.
Exclusion of trials with fewer than 50 participants. A value of 50 has been informed by the findings of one meta‐epidemiological study examining the impact of trial sample size on treatment effect estimates (Dechartres 2013); however, we recognise the choice of sample size to dichotomise 'small' trials is somewhat arbitrary.
Type of meta‐analytic model (i.e. comparing the combined effect from a fixed‐effect model with a random‐effects model).
Meta‐analysis method (i.e. comparing the combined effect and its CI when using the DerSimonian and Laird estimator of between trial heterogeneity (DerSimonian 1986), and the Wald‐type CI method versus the REML estimator of between trial heterogeneity variance and the Hartung‐Knapp‐Sidik‐Jonkman CI method (Hartung 2001; Sidik 2002)).
Summary of findings and assessment of the certainty of the evidence
We prepared GRADE summary of findings tables (see Table 1; Table 2; Table 3), which present a tabular overview of the primary outcomes of importance to decision makers. For the comparisons of parenting interventions compared to inactive controls, psychological interventions to inactive controls, and service system approaches to inactive controls, we have presented the findings (where data are available) for CPTSD symptoms, psychological wellbeing, substance use, parents' relationship quality, parental self‐harm, parent‐child relationship and parenting skills, at post‐intervention at the first available time point. Where outcomes were assessed using both dichotomous and continuous measures, we selected the measure with the greater number of studies contributing data. GRADEpro was used to construct the tables (GRADEpro GDT), including the number of studies, the statistical results, an interpretation of each result using informative statements to communicate the size of effect and certainty of evidence (Schünemann 2019b), and explanations for downgrading or borderline decisions.
For each result, two review authors independently assessed certainty of the evidence using GRADE methods as described in the Cochrane Handbook for Systematic Reviews of Interventions (Schünemann 2019a). An overall GRADE of high, moderate, low or very low certainty is reported for each result, based on whether we had serious, very serious or no concerns in relation to each of the following domains.
Risk of bias. We assessed the overall risk of bias across all studies contributing to each synthesised result. For GRADE, we considered the impact of studies at high risk of bias on the overall meta‐analytic result by (1) considering results of sensitivities analyses and, when these analyses were not possible/informative, we considered (2) the weight studies at high risk of bias contributed to the analysis, since studies at high risk of bias with more weight are more likely to bias the pooled estimate.
Inconsistency. We assessed whether there is important, unexplained inconsistency in results across studies, considering the overlap of CIs (non‐overlap indicating differences in direction or size of effect), statistical measures and tests for heterogeneity (I2 statistic, Chi2 test) and results of subgroup analyses (Subgroup analysis and investigation of heterogeneity).
Indirectness. We assessed whether the Participant, Intervention, Comparison or Outcome (PICO) characteristics of studies contributing to each result adequately represent the PICO target group for this review, such that the results may not be directly relevant for all population groups (e.g. parents pregnant or with a child less than two years of age, or first‐time parents) in this review.
Imprecision. We assessed whether the CI for each pooled effect estimate crossed our threshold for a small but important effect, rating imprecision as 'serious' when one threshold was crossed (i.e. the CI was compatible with both appreciable benefit and little or no difference, or vice versa) and 'very serious' when two thresholds were crossed (i.e. the CI was compatible with appreciable benefit and appreciable harm) and, for large effects, whether the sample size meets the optimal information size (based on number of events for binary outcomes; sample size for continuous outcomes) (thresholds are detailed in Measures of treatment effect).
Publication bias. We assessed reporting bias based on results of assessments in Assessment of risk of bias in included studies.
When interpreting results, we followed GRADE guidance for writing informative statements (Santesso 2020; Schünemann 2022). These statements provide a standardised phrasing for communicating the size and certainty of observed effects (i.e. for high certainty of evidence: [intervention] results in improved [outcome]; for moderate certainty of evidence: [intervention] probably improves [outcome]; for low certainty of evidence: [intervention] may improve [outcome]; and for very low certainty of evidence: the evidence is very uncertain about the effect of [intervention] on [outcome]) (Santesso 2020).
While GRADE assessments were not conducted on additional primary outcomes or secondary outcomes, we have applied GRADE principles for writing informative statements when describing the size and certainty of observed effects (i.e. we considered our thresholds for describing the size of effect, the confidence interval in relation to this threshold and risk of bias).
We conducted the review according to the published protocol and have reported any deviations from it in the Differences between protocol and review section.
Results
Description of studies
Results of the search
Electronic searches conducted on 19 October 2021 yielded 15,683 records. We identified 4145 duplicates, leaving 11,538 records. From these, we extracted 216 records of systematic reviews to be followed up for reference checking and identified 34 additional duplicates. To assess the remaining 11,288 records, we used Cochrane’s Screen4Me workflow, which helps to identify potential reports of randomised trials. The results of the Screen4Me assessment process can be seen in Figure 3. We assessed the 6572 records left in after Screen4Me, plus 17 additional records identified through other sources, using Covidence (Covidence). We identified 11 further duplicates and deemed 6417 records to be irrelevant through title and abstract screening. We retrieved the full‐text reports of the remaining 161 records for further assessment. Of these, 112 reports did not meet inclusion criteria and we excluded them (see Characteristics of excluded studies), and we identified five studies (from seven reports) as ongoing studies (see Characteristics of ongoing studies). We included 15 studies (consisting of 42 associated reports) (see Characteristics of included studies). The overall flow of studies for this review is presented in Figure 4. We contacted the authors of 10 studies to request unpublished data for the subgroup of parents who were experiencing CPTSD symptoms or who had experienced childhood maltreatment. Data for these subgroups were provided by eight author groups and used in the review (Ammerman 2016; Berry 2021; Blalock 2013; Grote 2015; Liu 2021; Pasalich 2019; Rosenblum 2017; Upshur 2016). Two author groups did not respond and we excluded these studies. We also contacted one author group to request unadjusted effect estimates (Booshehri 2018). Although the author group did not respond, we were able to calculate the required data based on the available data reported in the study (see Dealing with missing data).
3.
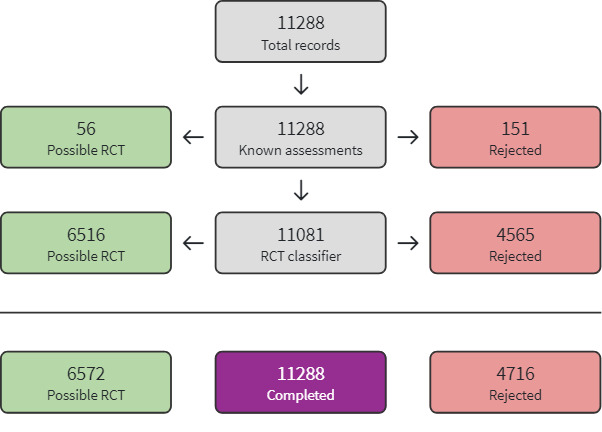
Screen4Me summary diagram
RCT = randomised controlled trial
4.

Methods
Design
Fourteen included studies were individual RCTs (parallel groups) and one was a cluster‐RCT (Upshur 2016).
Participants
A total of 1925 parents were randomised across the 15 studies, with the number of parents randomised in each study ranging from 20 (Haight 2005) to 266 (Blalock 2013). Only mothers were included in 12 studies, with three studies also including fathers (29 participants). Mothers consisted of 99% of the sample in Liu 2021, 94% in Booshehri 2018, and 91% in Pasalich 2019. Most studies included parents who self‐reported childhood maltreatment (12 studies; Ammerman 2016; Berry 2021; Blalock 2013; Booshehri 2018; Cicchetti 2006; Grote 2012; Grote 2015; Haight 2005; Liu 2021; Pasalich 2019; Rosenblum 2017; Steele 2019), one study included parents reporting PTSD symptoms (Silverstein 2011), and two studies included parents reporting both childhood maltreatment and PTSD symptoms (Madigan 2015; Upshur 2016). The mean age of parents was less than 18 years in one study (Madigan 2015), 11 studies included parents with a mean age between 18 and 29 years, two studies reported parent mean age greater than 30 years (Liu 2021; Silverstein 2011), and one study did not report mean parent age (Steele 2019). In studies conducted during the postpartum period (Ammerman 2016; Booshehri 2018; Cicchetti 2006; Haight 2005; Liu 2021; Pasalich 2019; Rosenblum 2017; Steele 2019), the mean age of children ranged from five months (Ammerman 2016) to three years (Haight 2005). Seven studies reported that more than 50% of participants had mental health comorbidity at baseline including depression/mood disorders, anxiety disorders, PTSD, substance/alcohol use disorders, eating disorders, dissociative disorders and/or psychiatric disorders (Ammerman 2016; Booshehri 2018; Grote 2012; Grote 2015; Haight 2005; Madigan 2015; Upshur 2016), and two studies reported less than 50% with mental health comorbidity (Rosenblum 2017; Silverstein 2011). The remaining six studies did not report on existing mental health comorbidity.
In all studies at least 50% of parents were experiencing at least one 'indicator of disadvantage': 13 studies with more than 50% of participants with low socio‐economic status (SES) backgrounds, 11 studies with more than 50% from ethnic minority populations, four with more than 50% of participants with less than high school education and one study with more than 50% of parents less than 18 years of age. Twelve studies included more than 50% of parents with more than one 'indicator of disadvantage' category: low SES and ethnic minority population (Berry 2021; Blalock 2013; Booshehri 2018; Grote 2012; Liu 2021; Rosenblum 2017; Silverstein 2011; Steele 2019; Upshur 2016); less than 18 years of age, from low SES background and with less than high school education (Madigan 2015); low SES, from an ethnic minority population and less than high school education (Cicchetti 2006); low SES and less than high school education (Ammerman 2016). Three studies reported just one indicator of disadvantage: less than high school education (Haight 2005), ethnic minority population (Grote 2015) and low SES (Pasalich 2019).
Recruitment setting
Included studies were published between 2005 and 2021. All studies were conducted within high‐income countries. Fourteen were set in the USA and one in Canada (Madigan 2015). Most studies were conducted in metropolitan areas (10 studies); five studies did not report the area. Four studies recruited parents from hospital or community‐based clinics (Berry 2021; Grote 2012; Grote 2015; Upshur 2016); four from government databases and records, including the Department of Human Services (Cicchetti 2006), the Public Child Welfare Office (Haight 2005), Child Protective Services (Pasalich 2019), and the Pediatrics, Child Welfare and Court Systems (Steele 2019); three from community‐based parenting programmes (Ammerman 2016; Liu 2021; Madigan 2015); one from both hospital‐based clinics and community‐based parenting programmes (Silverstein 2011); one from a government assistance office (Booshehri 2018); one reported varied recruitment settings (e.g. fliers posted in low‐income community locations/primary care clinics/community mental health clinics and referrals from primary health care providers; Rosenblum 2017); and one with a non‐specific recruitment setting (e.g. newspaper, television ads and physician referral; Blalock 2013).
Interventions
Seven studies assessed interventions coded as primarily 'parenting' interventions, eight studies assessed interventions coded as primarily 'psychological' interventions, and one study assessed interventions coded as primarily 'service system approaches'. An additional four studies included some service system approach components and were therefore coded as 'multiple‐component' interventions. We identified no studies that assessed mind‐body approaches, or pharmacological and biomedical therapies. Two studies included two eligible intervention arms (Booshehri 2018; Cicchetti 2006).
Parenting interventions included seven parent‐child interventions (Infant‐parent psychotherapy and Psychoeducational parenting intervention, Cicchetti 2006; Emotional support coaching, Haight 2005; Filming Interactions to Nurture Development (FIND), Liu 2021; Promoting First Relationships, Pasalich 2019; Group Attachment‐Based Intervention, Steele 2019) and one social support intervention (Mom Power, Rosenblum 2017). All parenting interventions utilised an attachment‐based approach except for Liu 2021, which used a strengths‐based approach (FIND). Psychological interventions consisted of six non‐trauma‐focused cognitive behavioural therapy (CBT)‐based interventions (In‐Home Cognitive Behavioural Therapy, Ammerman 2016; Cognitive Behavioral Analysis System of Psychotherapy (CBASP), Blalock 2013; Brief Interpersonal Psychotherapy, Grote 2012; MOMCare, Grote 2015; Problem‐Solving Education, Silverstein 2011; and Seeking Safety, Upshur 2016), one trauma‐focused CBT (Madigan 2015), and one psychological intervention that included both psychological and parenting components (Practical Resources for Effective Postpartum Parenting, Berry 2021). In‐home CBT, CBASP, MOMCare, Seeking Safety, Trauma‐focused CBT and FIND were augmented with treatment as usual. The service system approach included two versions of Building Wealth and Health Network, the partial version delivered financial empowerment education and the full version delivered the financial empowerment education and group, trauma‐informed peer support (Booshehri 2018).
The duration of interventions ranged from a single session (Haight 2005) to a 12‐month protocol (mean 46 weeks; Cicchetti 2006). All interventions were delivered face‐to‐face, with three studies supplementing face‐to‐face delivery with phone calls mainly when participants could not attend (Berry 2021; Grote 2012; Grote 2015). Five studies delivered interventions exclusively in participants homes (Ammerman 2016; Cicchetti 2006; Liu 2021; Pasalich 2019; Silverstein 2011), eight exclusively in clinical or community settings (Berry 2021; Blalock 2013; Grote 2012; Grote 2015; Haight 2005; Madigan 2015; Steele 2019; Upshur 2016), and one study delivered three sessions in home and 10 sessions in a clinical/community session (Rosenblum 2017). Two studies delivered the intervention in a group setting (Booshehri 2018; Steele 2019), one with a blend of three individual and 10 group sessions (Rosenblum 2017), and all other studies delivered interventions individually.
Twelve interventions were delivered across more than five sessions (Ammerman 2016; Blalock 2013; Booshehri 2018; Cicchetti 2006; Grote 2012; Grote 2015; Liu 2021; Madigan 2015; Pasalich 2019; Rosenblum 2017; Steele 2019; Upshur 2016), two interventions included two to five sessions (Berry 2021; Silverstein 2011), and one study involved a single session (Haight 2005). Eight interventions involved more than 10 hours of contact (Ammerman 2016; Booshehri 2018; Cicchetti 2006; Grote 2015; Madigan 2015; Pasalich 2019; Rosenblum 2017; Steele 2019), five involved one to 10 hours of contact (Berry 2021; Blalock 2013; Grote 2012; Liu 2021; Silverstein 2011), one involved less than one hour contact (Haight 2005), and one study did not specify the length of each session (Upshur 2016). Ten interventions were delivered weekly (Ammerman 2016; Blalock 2013; Booshehri 2018; Cicchetti 2006; Grote 2012; Grote 2015; Liu 2021; Madigan 2015; Pasalich 2019; Rosenblum 2017), one intervention was delivered three times weekly (Steele 2019), one study gave participants the option to choose weekly or bi‐weekly sessions (Silverstein 2011), one study delivered three sessions at specific times across the perinatal period (Berry 2021), one delivered the intervention at regular prenatal appointments without details of frequency (Upshur 2016), and one was a single session intervention (Haight 2005).
Most practitioners delivering the interventions received training and supervision, and delivery of the intervention was monitored. However, the training requirements of In‐Home Cognitive Behavioural Therapy practitioners was not reported (Ammerman 2016), and the training, supervision and fidelity requirements for Practical Resources for Effective Postpartum Parenting (Berry 2021), Building Wealth and Health Network (Booshehri 2018) and the emotional coaching intervention (Haight 2005) were not reported.
Details on the psychological interventions, parenting interventions and service system approaches can be found in the Characteristics of included studies and Table 7.
4. Details of interventions.
| Study | Intervention | Delivery setting and modality | Frequency of intervention delivery | Length of treatment | Description |
| Parenting interventions | |||||
| Cicchetti 2006 | Arm 1: IPP, called child‐parent psychotherapy in Stronach 2013 Arm 2: PPI |
Face‐to‐face, in‐home | Weekly | 12 months | Arm 1 (IPP) A manualised intervention focusing on the relationship between the mother and the child following a supportive, nondirective and non‐didactic approach, which includes developmental guidance based on the mother's concerns. Sessions typically occur in the families' living rooms using toys and materials already present in the home. During sessions, the therapist observes and responds empathically to the interactions between the mother and the infant, providing comment on processes in the parent‐child relationship as they occur. Arm 2 (PPI) Focus of the intervention is on the psycho‐education of the mothers (rather than on the mother‐child dyad), using a variety of cognitive and behavioural techniques to address parenting skill deficits and social‐ecological factors. This included parental education and parenting skill training to reduce maternal stress, foster social support and increase life satisfaction. The approach is didactic in nature, providing mothers with specific information and knowledge regarding child development. Training in parenting techniques, problem‐solving and relaxation were also utilised. |
| Haight 2005 | Emotional support coaching | Individual, face‐to‐face, community setting | Single session | Once | The "intervention focused on emotion support and coaching" (Haight 2005, page 466) and occurred immediately prior to the foster parent visit. The first phase of the intervention involved a discussion with the mother "about her family and any other significant relationships, and her experiences with Department of Children and Family Services" (Haight 2005, page 467). The second phase of the intervention focused on leave‐taking, including a discussion of how mothers had "tried to support their children during leave‐taking, the... interviewer sharing additional strategies" (Haight 2005, page 467) and the interviewer and mother role‐playing the implementation of strategies the child might respond to. |
| Liu 2021 | FIND, augmented with treatment as usual (standard Early Head Start services) | Individual, face‐to‐face in‐home | Weekly | 10 weeks | A manualised brief, flexible, and strength‐based video feedback intervention programme that "uses video coaching to strengthen developmentally supportive 'serve and return' interactions, a pattern characterised by attuned, reciprocal, and well‐regulated interactions." (Liu 2021, page 2) FIND is based on five core elements: (1) sharing the child's focus; (2) supporting and encouraging; (3) naming; (4) back and forth interaction; and (5) endings and beginnings. |
| Pasalich 2019 | PFR | Individual, face‐to‐face in‐home | Weekly | 10 weeks | A manualised relationship‐ and strengths‐based home visiting service that aims to help families facing adversity. "PFR seeks to increase caregivers' awareness of their children's social and emotional needs, including their need for a sense of safety and security, as well as increasing caregivers' understanding of their own needs as parents" (Oxford 2018, page 268). "Using video‐based feedback... the parent and child are recorded playing together" (Oxford 2018, page 268). The provider reviews a recorded play session with the parent, who reflects on the "recorded interactions, noting what the child is doing in relation to the caregiver's behavior and what the caregiver is doing in response to the child" (Oxford 2018, page 268). |
| Rosenblum 2017 | Mom Power | 3 x individual, in‐home, 10 x community, group sessions |
Weekly | 10 weeks | A manualised multifamily intervention "designed to strengthen protective factors for the individual and within the family system, and geared towards overcoming barriers to engagement... The fundamental aim of the intervention is to enhance mothers' wellbeing and positive parenting and to ignite motivation for further connection with care, ultimately improving children's outcomes" (Rosenblum 2017, page 3). The Mom Power curriculum rests on five core pillars: "attachment‐based parenting education, self‐care, practice, social support, and connection to resources" (Rosenblum 2017, page 4). "The Mom Power curriculum is structured but personalised, building a framework for understanding children's behaviours and paired with tailored feedback that addresses the unique experiences of each mother‐child dyad" (Rosenblum 2017, page 6). |
| Steele 2019 | GABI | Group, in‐clinic | 3 x weekly | 26 weeks | A manualised, multifamily, group‐based maltreatment prevention intervention, consisting of a distinct set of attachment‐relevant features: (1) a specified time for parents and children to interact with one another; (2) "a time for parents to interact with other parents while their children experience individual time with their age‐mates in the presence of trained clinicians who help them to engage with peers" (Steele 2019, page 205); and (3) a 'reunion' where children and parents are together again. |
| Psychological interventions | |||||
| Ammerman 2016 | IH‐CBT | Individual, face‐to‐face, in‐home | Weekly | 15 weeks | IH‐CBT follows the directives (principles and techniques) of traditional CBT, consisting of behavioural activation, identification of automatic thoughts/schemas, thought restructuring and relapse prevention, and is delivered concurrently with home visiting. Adaptions were made to maximise engagement, including (1) delivering CBT in home; (2) tailoring treatment content to issues relevant to the population (e.g. transition to adult roles, living with parents, parenting challenges); and (3) allowing communication between therapists and home visitors. |
| Berry 2021 | PREPP | Individual, 3 x face‐to‐face, clinical setting, 1 x telephone | 4 sessions | 7 to 12 weeks | A manualised coaching programme including infant behavioural interventions and targeted psychotherapy techniques. "The psychologist also contacted participants by telephone at 2 weeks postpartum and, using motivational interviewing techniques, encouraged the use of PREPP skills and answered specific participant questions" (Berry 2021, page 190). The infant behavioural interventions included: "feeding the infant between 10 PM and midnight, accentuating differences between day and night by providing higher levels of stimulation during the day, lengthening the latency to feeding time in the middle of the night by engaging in other attentive activities such as walking with the baby and diapering, thereby extinguishing the association between nighttime waking and feeding, carrying infants for a minimum of 3 hours a day, throughout the day, in addition to the carrying that occurs in response to crying and feeding, and learning to swaddle the baby" (Berry 2021, page 189). Psychotherapy techniques included supportive psychological interviewing that encourages reflection on their own childhood and how it will inform the development of their parental identity, psycho‐education about the postpartum period, and mindfulness techniques aimed at (a) helping mothers to cope better when their babies are distressed and/or unsoothable and (b) aiding mothers to return to sleep after tending to their babies during the nighttime. |
| Blalock 2013 | CBASP, augmented with standard behavioural and motivational smoking cessation counselling | Individual, face‐to‐face, clinical setting | Weekly | 10 weeks | "Each session consisted of 15 minutes of standard behavioural and motivational smoking cessation counselling (based on the Clinical Practice Guidelines)...plus 45 minutes of CBASP, a manualised, interpersonally focused psychotherapy that reduces interpersonal stress and increases the quality of one's relationships with significant others" (Blalock 2013, page 5). It includes "development of secure therapeutic relationships, improvement in interpersonal and emotion regulation skills, reduction in avoidant behaviours, examination of implicit assumptions regarding relational expectations, and activation and processing of interpersonal schema and negative emotional states associated with traumatic relational memories" (Blalock 2013, page 4). |
| Grote 2012 | IPT‐B | Individual, face‐to‐face, telephone, clinical setting | Weekly during the acute phase (8 sessions) then variable | 3 to 6 months | Culturally relevant IPT‐B is a manualised, "multicomponent model of care, consisting of a motivationally enhanced, pretreatment engagement session" (Grote 2012, page 5) (whereby the interviewer elicits participant's unique barriers to care within a culturally sensitive manner and engages in collaborative problem‐solving to overcome barriers), 8 acute sessions of IPT‐B (targeting 4 interpersonal problem areas related to the onset/maintenance of a depressive episode: role transition, role dispute, grief and interpersonal deficits), and maintenance IPT‐B (mothers encouraged to be watchful for the appearance of early somatic, affective or cognitive symptoms related to prior depressive episodes and to practice skills learned in IPT‐B to prevent relapse). A number of culturally relevant additions were integrated into IPT‐B, including free bus passes, childcare and the facilitation of access to needed social services. |
| Grote 2015 | MOMCare, augmented with treatment as usual (MSS‐Plus) | Individual, face‐to‐face, telephone, community setting or in‐home | Weekly during the acute phase (8 sessions) then variable | 3 to 6 months | MOMCare consisted of manualised IPT‐B and/or pharmacotherapy for acute treatment, as well as outreach for women missing sessions and pre‐therapy engagement session. IPT‐B consists of an engagement session followed by "eight acute sessions of IPT‐B before the birth and IPT‐B maintenance sessions up to about 1‐year postpartum and has been adapted to be relevant to the culture of race/ethnicity by incorporating the patient's cultural views of depression, treatment goals, and resources" (Grote 2015, page 823). For mothers requesting antidepressants as an initial treatment, they were encouraged to engage in a risk‐benefit decision‐making process with their OB provider to "discuss the risks of both antidepressants and untreated depression during pregnancy and lactation" (Grote 2015, page 823), which was then implemented using a stepped‐care treatment approach. Mothers with less than 50% improvement on the PHQ‐9 by 6 to 8 weeks received a revised treatment plan. Mothers receiving IPT‐B alone could be augmented with a trial of antidepressant medication. Mothers "on medication alone could receive an adjusted dosage to achieve optimal outcomes, medication change, and/or augmentation with IPT‐B" (Grote 2015, page 823). The MOMCare intervention was added onto usual care (MSS‐Plus). |
| Madigan 2015 | TF‐CBT, augmented with treatment as usual (parenting course) | Individual, face‐to‐face, clinical setting | Weekly | 12 weeks | A manualised cognitive behavioural therapy, including "psychoeducation, stress management, affective modulation, an understanding of the cognitive‐emotional‐behavioural triad, and the creation and cognitive processing of a detailed trauma narrative... In cases where a traumatic loss experience was the focus of treatment, an adapted TF‐CBT protocol designed specifically for traumatic loss was used" (Madigan 2015, page 183). |
| Silverstein 2011 | PSE | Individual, face‐to‐face, in‐home | Weekly or biweekly | 7 to 12 weeks | A "manualised, cognitive behavioral prevention intervention, adapted from Problem‐Solving Treatment...designed to impart recipients with stronger problem‐solving skills, which are theorised to reduce the negative impact of stress on personal‐social functioning, and thereby prevent the development of impairing psychological distress... In a PSE session, educators guide participants in selecting an objective, measurable problem, then proceed through a series of steps that include goal setting, brainstorming and evaluating solutions, choosing a solution, and action planning" (Silverstein 2011, page 479). |
| Upshur 2016 | SS, augmented with treatment as usual | Individual, face‐to‐face, clinical setting | Not reported | Not reported | A "manualised, psychosocial education program designed to improve coping skills among individuals with PTSD and comorbid substance abuse. It uses cognitive‐behavioral theory as its underlying change mechanism, focusing on solutions to present problems, with a major emphasis on safety, and explicitly does not focus on exploring past trauma or psychoanalytic work" (Upshur 2016, page 538). For this study, eight of the 25 topics were chosen to be delivered. |
| Service system approaches | |||||
| Booshehri 2018 | Building Wealth and Health Network | Group, face‐to‐face, clinical setting | Weekly |
6 months | Arm 1 (partial) The programme consists of helping parents open bank accounts and financial empowerment classes. Parents are encouraged to make weekly deposits over a 12‐month period, with the assistance of bank representatives. The goal of this aspect of the programme is to create a practice of asset‐building that would carry beyond their participation in the programme. The financial empowerment classes consisted of interactive exercises, worksheets and journal assignments, with the aim to foster understanding and practice of banking, building credit and debt management, making the most of one’s money, and setting financial goals for oneself and one’s family. Arm 2 (full) In addition to the assistance with opening a bank account and the financial empowerment classes, parents participate in trauma‐informed peer support groups called SEG. SEG is based on the SELF tool ‐ "creating personal, emotional, moral and physical safety (S), processing and managing emotions (E), recognising loss and letting go (L), and developing goals for a sense of future (F)" (Booshehri 2018, page 1597). |
CBASP: cognitive behavioural analysis system of psychotherapy; FIND: Filming Interactions to Nurture Development; GABI: Group Attachment‐Based Intervention; IH‐CBT: In‐Home Cognitive Behavioural Therapy; IPP: infant‐parent psychotherapy; IPT‐B: brief interpersonal psychotherapy; MSS‐Plus: Maternity Support Services‐Plus; OB: obstetrician; PFR: Promoting First Relationships; PHQ‐9: Patient Health Questionnaire‐9; PPI: psycho‐educational parenting intervention; PREPP: Practical Resources for Effective Postpartum Parenting; PSE: Problem‐Solving Education; PTSD: post‐traumatic stress disorder; SEG: Self Empowerment Groups; SELF: Safety, Emotions, Loss/letting go, Future; SS: Seeking Safety; TF‐CBT: trauma‐focused CBT.
Comparisons
Parents in 11 of the 15 comparison arms received treatment as usual or enhanced treatment as usual. Usual care in nine studies consisted of standard prenatal care services in hospital or community settings, or in the home (Berry 2021; Blalock 2013; Grote 2012; Grote 2015; Liu 2021; Madigan 2015; Silverstein 2011; Steele 2019; Upshur 2016). Other forms of usual care included standard Temporary Assistance for Needy Families (TANF) (Booshehri 2018) and standard services provided to families identified as maltreating in the community (Cicchetti 2006). These services consisted primarily of psycho‐education (e.g. psychological wellbeing, postpartum depression, parenting skills, nutrition education, childbirth education); case management; and referrals to mental health treatment, practical assistance and social services. Two studies utilised attention control comparison arms, which involved mail outs of educational material and personalised referral information (Pasalich 2019; Rosenblum 2017), and one study used an inactive control that involved standard home visiting services (Ammerman 2016). One study used a wait‐list comparison comprised of no treatment (Haight 2005).
Details on the comparators can be found in the Characteristics of included studies and Table 8.
5. Details of comparisons.
| Study | Intervention | Description |
| Comparators for parenting interventions | ||
| Cicchetti 2006 | Treatment as usual | "Families continued to receive services that were typically available to maltreating families in the community" (Cicchetti 2006, page 630), including case management from the Department of Human Services and assistance in obtaining referrals to services and resources that may have been more difficult to access outside the research trial. |
| Haight 2005 | Wait‐list | Parents received no treatment. |
| Liu 2021 | Treatment as usual (EHS programme) | EHS is a federal programme for low‐income pregnant women and families with infants and toddlers, and includes home visits, child care, case management, parenting education, health care and referrals and family support. |
| Pasalich 2019 | Attention control (R&R) | R&R was delivered over the phone in 3 sessions, which consisted of a 30‐minute needs assessment and a mailed packet of personalised information (e.g. local services). Parents also received 2 follow‐up, 10‐minute check‐in calls. |
| Rosenblum 2017 | Attention control | Mothers randomised into the control condition received 2 individual sessions and 10 weekly mailings of the Mom Power curriculum content, which "included a pre‐stamped post card for the mother to send back indicating that the week's material had been read" (Rosenblum 2017, page 679). |
| Steele 2019 | Treatment as usual (STEP) | A treatment model consisting of anger management, psycho‐education, the distinction between discipline and punishment, and role playing adaptive parenting strategies. |
| Comparators for psychological interventions | ||
| Ammerman 2016 | Inactive control (standard home visiting) | Mothers received regular services from home visitors, with an emphasis child health and development, nurturing the mother‐child relationship, maternal health and self‐sufficiency, and linkage to other community services (including community‐based treatment for depression). |
| Berry 2021 | Enhanced treatment as usual | Discussion of postpartum depression symptoms (including psycho‐educational materials) and referrals for mental health treatment (including supportive services in the community). |
| Blalock 2013 | Enhanced treatment as usual (HW) | "Each session consisted of 15 minutes of standard behavioral and motivational smoking cessation counselling" (Blalock 2013, page 5) (based on the Clinical Practice Guidelines), plus 45 minutes of HW, a time‐ and attention‐matched control that was pregnancy relevant but instructional in nature. "Participants were allowed to choose from a list of discussion topics such as stress, pregnancy symptoms, sleep, exercise, yoga, and relaxation training" (Blalock 2013, page 5). Therapists were allowed to provide reflective, supportive listening, but were prohibited from conducting solution‐focused exercises. |
| Grote 2012 | Enhanced treatment as usual | Mothers received psycho‐educational materials about depression, and were strongly encouraged to seek treatment where they were receiving prenatal services. They were provided easy access to depression treatment in the obstetrics and gynaecology clinics, familiarity with the setting, decreased stigma, childcare and free bus passes. They were also provided additional monitoring of their depression severity and diagnostic status than they typically received in the clinic. |
| Grote 2015 | Enhanced treatment as usual (MSS‐PLUS) | MSS "is the usual standard of care in the public health system of Seattle‐King County for pregnant women on Medicaid"(Grote 2015, page 823). Goals include "offering services to promote healthy pregnancies and positive birth and parenting outcomes, providing case management services to meet basic needs, and facilitating regular contact" (Grote 2015, page 823) with an obstetrician. Pregnant women scoring PHQ‐9 > 10 were eligible for intensive MSS‐Plus services, entailing more frequent, and longer visits from their multidisciplinary team. |
| Madigan 2015 | Treatment as usual | A parenting course consisting of 12 x 60‐minute sessions, covering topics such as "preparing for baby, role of fathers, supports, relationships, stress, fears, anxieties, bonding with fetus/baby, prenatal nutrition, labor/delivery, time management and budgeting" (Madigan 2015, page 182). |
| Silverstein 2011 | Treatment as usual | Mothers received usual hospital or early intervention services. |
| Upshur 2016 | Treatment as usual | "Prenatal advocates provided education and support to all women to supplement nurse/physician prenatal care visits and conducted activities such as teaching about nutrition, exercise and healthy behavior during pregnancy, providing childbirth education (e.g. phases of pregnancy, physical and mental health aspects of pregnancy, managing labor and delivery), and helping women obtain benefits and services such as health insurance, transportation, housing, legal assistance, nutrition services, and refugee support" (Upshur 2016, page 538). |
| Comparators for service system approaches | ||
| Booshehri 2018 | Treatment as usual | Standard temporary assistance for needy families programming, which consisted of 20 hours per week "of scheduled supervised job training and job search activities" (Booshehri 2018, page 1597). |
EHS: Early Head Start; HW: Health and Wellness Control; MSS(‐PLUS): Maternity Support Services(‐PLUS); PHQ‐9: Patient Health Questionnaire‐9; R&R: three‐call resource and referral; STEP: Systematic Training for Effective Parenting.
Outcomes
Timing of outcome assessment
(see also Included studies)
Ammerman 2016: baseline (children aged mean = five months), post‐intervention and at three‐month follow‐up.
Berry 2021: baseline (during pregnancy) and post‐intervention (six weeks postpartum). Daytime sleeping was only reported at post‐intervention.
Blalock 2013: baseline (during pregnancy), depression symptom severity assessed at six months postpartum and smoking abstinence at six months post‐intervention.
Booshehri 2018: baseline (children aged mean = 30 months), three‐month, six‐month and nine‐month follow‐up.
Cicchetti 2006: baseline (children aged mean = 12 months), post‐intervention (aged mean = 26 months old) and at 14‐month follow‐up (aged mean = 38 months). Behavioural outcomes were only reported at 14‐month follow‐up.
Grote 2012: baseline (during pregnancy), post‐intervention and six months postpartum.
Grote 2015: baseline (during pregnancy), post‐intervention (88% of mothers still pregnant), six‐month follow‐up (most mothers three months postpartum), 12 months post‐intervention (most mothers nine months postpartum) and 18 months post‐intervention (most mothers 15 months postpartum). Presence of PTSD and probable generalised anxiety disorder not reported at post‐intervention.
Haight 2005: post‐intervention (when children were aged mean = three years).
Liu 2021: baseline (children aged mean = 23 months old) and post‐intervention.
Madigan 2015: baseline (during pregnancy), six‐month follow‐up (children aged mean = six months) and 12‐month follow‐up (aged mean = 12 months). Behavioural problems were only assessed at baseline and 12‐month follow‐up; disorganised infant attachment was only assessed at 12‐month follow‐up.
Pasalich 2019: baseline (children aged mean = 16 months), post‐intervention, three‐month and six‐month follow‐up. Secure base behaviour was only assessed at baseline and six‐month follow‐up.
Rosenblum 2017: baseline (children aged mean = 17 months) and post‐intervention.
Silverstein 2011: three months follow‐up (child age not reported). Although additional assessments were conducted at baseline, one month post‐intervention and two‐month post‐intervention, outcomes for these time points were not reported.
Steele 2019: post‐intervention.
Upshur 2016: baseline (during pregnancy), post‐intervention (36 weeks gestation) and one month postpartum.
Primary outcomes
All included studies reported one or more primary outcomes. Details on primary outcomes can be found in the Characteristics of included studies and Table 9.
6. Details of outcomes.
| Outcome category | Outcome | Outcome domain | Specific outcome: measure(s) (study) |
| Primary (critical) outcomes | Parental psychological or socio‐emotional wellbeing |
Trauma‐related symptoms |
|
| Anxiety symptoms, depression symptoms, other validated measures of psychological wellbeing, or a combination of these |
|
||
| Substance use (commenced, recommenced, increased, decreased) |
|
||
| Parent relationship quality (with partner or significant others) |
|
||
| Parental self‐harm (attempted or actual) | No studies reported data. | ||
| Parenting capacity | Parent–child relationship (e.g. interaction, warmth, attachment, mutual responsivity) |
|
|
| Parenting skills (e.g. problem‐solving, coping, self‐efficacy, parent sensitivity and responsiveness) |
|
||
| Secondary (important) outcomes | Parental intervention acceptability | Parent satisfaction with intervention (e.g. emotional safety, cultural safety, appreciation) | No studies reported data. |
| Medication compliance (if applicable) | No studies reported data. | ||
| Parent engagement (including dropouts; programme completion) |
|
||
| Socio‐ecological outcomes | Social functioning (increased social functioning or social networks, or both) |
|
|
| Changes in social capital (e.g. increased access to employment, education, support/health services) or resources (food, housing, clothing) |
|
||
| Child adverse events recorded during the intervention | Child maltreatment occurrence (including exposure to family violence) | No studies reported data. | |
| Family disruptions and child removals | No studies reported data. | ||
| Other adverse childhood experiences | No studies reported data. | ||
| Child's physical or socio‐emotional wellbeing | Child physical outcomes (e.g. preterm birth, low birth weight, small‐for‐gestational age, neonatal intensive care admission, immunisations, hospitalisations) | No studies reported data. |
|
| Child developmental outcomes (e.g. cognition, speech, language, motor skills) |
|
||
| Child emotional and behavioural outcomes (e.g. internalising and externalising behaviour) |
|
||
| Other outcomes | Service provider knowledge, attitudes and practices | No studies reported data. | |
| Cost or cost‐effectiveness |
|
DSM‐5: Diagnostic and Statistical Manual of Mental Disorders ‐ 5th Edition; PTSD: post‐traumatic stress disorder; QALYs: quality adjusted life years
Trauma‐related symptoms were assessed in five studies. Outcomes included PTSD symptom severity assessed with the PTSD Checklist for DSM‐5 (PCL‐5; Grote 2015), National Women's Study PTSD Module (Rosenblum 2017) and Post‐traumatic Stress Scale (Upshur 2016). Other outcomes included interpersonal problems, assessed with the Inventory of Interpersonal Problems (Grote 2012), presence of PTSD, assessed with the clinician‐rated Children's PTSD Inventory (Madigan 2015) and severity of dissociation, assessed with the Adolescent Dissociative Experiences Scale (Madigan 2015).
Psychological wellbeing was assessed in 10 studies. Outcomes included depression symptom severity assessed with the Beck Depression Inventory (Ammerman 2016; Grote 2012; Madigan 2015), Hamilton Depression Rating Scale (Berry 2021), Center for Epidemiologic Studies Depression Scale (Blalock 2013; Booshehri 2018), Hopkins Symptom Checklist (Grote 2015), and Quick Inventory of Depressive Symptoms (Silverstein 2011); postpartum depression symptom severity assessed with Edinburgh Postnatal Depression Scale (Grote 2012; Upshur 2016) and Postpartum Depression Screening Scale (Rosenblum 2017); and anxiety symptom severity assessed with the Hamilton Anxiety Rating Scale (Berry 2021), Beck Anxiety Inventory (Grote 2012) and Screen for Child Anxiety Related Emotional Disorder (Madigan 2015). Depression remission was assessed as the number of individuals with Hopkins Symptom Checklist scores less than 0.5 (Grote 2015), the number of parents with a depressive episode and mean number of depressive episodes assessed on the Quick Inventory of Depressive Symptoms (Silverstein 2011) and presence of generalised anxiety disorder assessed as the number of individuals with generalised anxiety disorder on the PRIME‐MD Patient Health Questionnaire (Grote 2015). Other outcomes included self‐efficacy, assessed with the General Self‐Efficacy Scale (Booshehri 2018), behavioural problems assessed with the externalising subscale of the Youth Self‐Report (Madigan 2015), functional impairment assessed with the Work and Social Adjustment Scale (Grote 2015), severity of stress assessed on the Perceived Stress Scale (Silverstein 2011) and positive and negative coping assessed with the Brief Copes Questionnaire (Upshur 2016).
Substance use was assessed in one study. Smoking abstinence (i.e. the number of parents abstaining from smoking) was assessed with the Timeline Follow‐back Interview (Blalock 2013).
Parents' relationship quality (with partner or significant others) was assessed in one study. Social support was assessed with the Interpersonal Support Evaluation List (Ammerman 2016).
Parental self‐harm was not assessed in any studies.
Parent‐child relationship was assessed in three studies. Outcomes included the four attachment styles (secure attachment, disorganised attachment, avoidant attachment, ambivalent attachment) assessed with the Strange Situation Paradigm (Cicchetti 2006); parent sensitivity assessed with the Nursing Child Assessment Teaching Scale (Pasalich 2019); secure base behaviour assessed with the Toddler Attachment Sort‐45 (Pasalich 2019); and dyadic constriction and dyadic reciprocity assessed with the Coding Interactive Behaviour System (Steele 2019).
Parenting skills was assessed in five studies. Outcomes included maternal supportive presence and maternal hostility assessed with the Coding Interactive Behaviour System (Steele 2019) and direct observation (Haight 2005). Additional domains of maternal affect and interaction assessed via direct observation included generational boundary dissolution, detachment/disengagement, positive regard, intrusiveness, engagement/interpersonal involvement and inventiveness (Haight 2005). Other outcomes included child and parent functioning/coping assessed with the Parenting Stress Index–Short Form (Ammerman 2016), home environment (nurturing and stimulating parenting) assessed with the Home Observation for Measurement of the Environment Inventory (Ammerman 2016), leave taking behaviours assessed via direct observation (Haight 2005), parental confidence assessed with the Parental Sense of Competence Scale (Liu 2021), four domains of parental self‐efficacy (teaching, nurturance, discipline and instrumental care) assessed with the Self‐Efficacy for Parenting Tasks Index‐Toddler Scale (Liu 2021), severity of parental stress assessed with the Parenting Stress Index–Short Form (Rosenblum 2017), and care‐giving helplessness and child caregiver behaviour assessed with the Care‐giving Helplessness Questionnaire (Rosenblum 2017).
Secondary outcomes
Fourteen studies reported one or more secondary outcomes. Haight 2005 did not report any secondary outcomes. Details on secondary outcomes can be found in the Characteristics of included studies and Table 9.
Parent satisfaction with intervention was not assessed in any studies.
Medical compliance was not assessed in any studies.
Parent engagement was assessed in 15 studies. Dropout was assessed as dropout for any reason between randomisation and post‐intervention (Ammerman 2016; Berry 2021; Blalock 2013; Booshehri 2018; Cicchetti 2006; Grote 2012; Grote 2015; Haight 2005; Liu 2021; Madigan 2015; Pasalich 2019; Rosenblum 2017; Silverstein 2011; Steele 2019; Upshur 2016). This includes failure to complete the pre‐specified intervention protocol or failure to complete the post‐intervention assessment.
Social functioning was assessed in three studies. Outcomes included social networks assessed with the Social Network Index (Ammerman 2016), social functioning assessed with the Social Adjustment Scale (Silverstein 2011), and perceived social support assessed with the Medical Outcomes Study Social Support Scale (Upshur 2016).
Changes in social capital was assessed in two studies. Outcomes included economic hardship, assessed on the US Household Food Security Survey Module, an energy security survey and housing security survey (Booshehri 2018), employment status assessed on a non‐validated survey item (Booshehri 2018) and perceived connection to community professionals assessed on a non‐validated, six‐item retrospective questionnaire (Rosenblum 2017).
Child maltreatment occurrence was not assessed in any studies.
Family disruptions and child removals were not assessed in any studies.
Other adverse childhood experiences were not assessed in any studies.
Child physical health was not assessed in any studies.
Child development was assessed in one study. Child's developmental risks was assessed with the Parent’s Evaluation of Developmental Status Scale (Booshehri 2018).
Child emotional and behavioural outcomes were assessed in three studies. Outcomes included internalising and externalising behaviour assessed with the Child Behavior Checklist (Cicchetti 2006; Liu 2021), overall child behavioural problems assessed with the Child Behavior Checklist (Cicchetti 2006), and daytime sleeping assessed with the Baby's Day Diary (Berry 2021).
Service provider knowledge, attitudes and practices were not assessed in any studies.
Cost or cost‐effectiveness was assessed in two studies. Ammerman 2016 assessed quality adjusted life years (QALYs), depression‐free days and interventioncosts on a probabilistic, patient‐level Markov model/Medical Expenditure Panel Survey. Grote 2015 assessed depression‐free days (number of depression‐free days over 18 months) and intervention costs (study staff salary and fringe benefit rates plus a 30% overhead rate).
Funding sources
Funding sources included major research councils, government departments, independent research organisations and philanthropic/charitable organisations. Seven studies had a single funding body, one study had two funding bodies and six studies had three funding bodies. Eight studies sourced funding from major research councils in the US, including the National Institute of Mental Health (Ammerman 2016; Berry 2021; Cicchetti 2006; Grote 2012; Grote 2015; Pasalich 2019; Silverstein 2011) and National Institute on Drug Abuse (Blalock 2013).
Details on the funding sources can be found in Characteristics of included studies.
Excluded studies
We formally excluded 107 studies (consisting of 112 reports) from the review. Of these, 75 studies did not include parents experiencing CPTSD symptoms and/or childhood maltreatment, 20 included children older than three years of age, 10 were not RCTs, one was an ineligible intervention and one was an abstract of a symposium summarising ineligible studies. The Characteristics of excluded studies table summarises 19 studies that appeared to meet the eligibility criteria, but upon inspection with full‐text review were found to be ineligible. The reasons for exclusion for these 19 studies have been reported.
Awaiting classification
No studies were identified as awaiting classification.
Ongoing studies
Five ongoing studies were identified (Kaltenbach 2021; NCT03938350; NCT04818112; NL9179; NCT03175796), details of which can be found in Characteristics of ongoing studies.
Kaltenbach 2021 compared an adapted version of Narrative Exposure Therapy delivered via videoconferencing to wait‐list, for parents of neurodiverse children with full or partial PTSD. The primary outcome is PTSD symptom severity, with secondary outcomes of interest (e.g. depression symptom severity, parent‐child relationship and functioning). The results of the study have not been published.
NCT03938350 is comparing Dialectical Behavior Therapy Skills Training to treatment as usual for parents from an ethnic/racial minority group reporting moderate to severe childhood maltreatment (Adverse Childhood Experiences ≥ 4) and depression symptoms (PHQ‐9 ≥ 9). Primary outcomes include treatment feasibility, with secondary outcomes of interest (e.g. PTSD and depression symptom severity).
NCT04818112 is comparing a behavioural auditory, tactile, visual and vestibular intervention to an attention control for parents reporting childhood maltreatment (Adverse Childhood Experiences ≥ 2). The primary outcome is mother‐infant synchrony, gaze and affect, with secondary outcomes of interest (e.g. mother‐infant vocalisation and touch).
NL9179 is comparing an attachment‐based video‐feedback intervention to Eye Movement Desensitization and Reprocessing (EMDR) in mothers residing in women's shelters due to severe domestic violence. Primary outcomes include PTSD symptom severity (maternal) and parenting behaviours, with secondary outcomes of interest (e.g. child PTSD symptom severity).
NCT03175796 compared a home visiting programme to treatment as usual in mothers who endorsed two or more of the following: adverse childhood experiences, possible depression diagnosis, challenges with parenting and eligibility for public services (based on income). Primary outcomes included PTSD symptom severity, depression symptom severity, emotional distress/rigidity/social isolation, perception of child and relationship with child, and social‐emotional behaviour problems of child. The results of the study have not been published.
Risk of bias in included studies
The Risk of bias (tables) section outlines the risk of bias assessments for each outcome, including the judgements and supporting comments. Please contact the authors for detailed risk of bias assessment data, including consensus, for signalling questions.
We judged most outcomes overall to have 'some concerns', and we judged outcomes within six studies to be at 'high' risk of bias. Most studies did not adequately report the randomisation process (including generation of the random sequence and allocation concealment). Many studies had potential bias in the measurement of outcome (using self‐report assessment tools) and missing data (reporting moderate to large dropout).
Effects of interventions
See: Table 1; Table 2; Table 3
See Table 1; Table 2; Table 3.
Comparison 1: Parenting interventions versus inactive control
Six studies assessed parenting interventions compared to an inactive control post‐intervention (Cicchetti 2006; Haight 2005; Liu 2021; Pasalich 2019; Rosenblum 2017; Steele 2019). See Table 1. Additional outcomes reported in single studies are reported in Table 10.
7. Additional outcomes: parenting interventions.
| Outcome measure (scale) | Direction of effect | Intervention mean (SD)/events | n | Control mean (SD)/events | n | Effect estimate, 95% CI | P value | Study | Risk of bias |
| Primary outcomes | |||||||||
| Parent‐child relationship | |||||||||
| Post‐intervention | |||||||||
| Dyadic constriction (CIB) | Higher scores = worse | 2.60 (1.04) | 43 | 3.26 (1.03) | 35 | MD ‐0.66 (‐1.12 to ‐0.20) | 0.005 | Steele 2019 | High |
| 3‐month follow‐up | |||||||||
| Parent sensitivity (NCATS) | Higher scores = better | 36.17 (3.67) | 29 | 35.02 (5.03) | 41 | MD 1.15 (‐0.89 to 3.19) | 0.27 | Pasalich 2019 | Some concerns |
| 6‐month follow‐up | |||||||||
| Parent sensitivity (NCATS) | Higher scores = better | 37.14 (4.28) | 28 | 35.18 (5.96) | 38 | MD 1.96 (‐0.51 to 4.43) | 0.12 | Pasalich 2019 | Some concerns |
| Secure base behaviour (TAS‐45) | Higher scores = better | 0.16 (0.08) | 28 | 0.13 (0.08) | 38 | MD 0.03 (‐0.01 to 0.07) | 0.13 | Pasalich 2019 | Some concerns |
| Parenting skills | |||||||||
| Post‐intervention | |||||||||
| Leaving taking behaviours (direct observation) | Higher scores = better | 4.6 (1.9) | 10 | 3.3 (1.3) | 10 | MD 1.30 (‐0.13 to 2.73) | 0.07 | Haight 2005 | Some concerns |
| Generational boundary dissolution (direct observation) | Higher scores = worse | 1.9 (1.4) | 10 | 1.8 (1.3) | 10 | MD 0.10 (‐1.08 to 1.28) | 0.87 | Haight 2005 | Some concerns |
| Detachment/disengagement (direct observation) | Higher scores = worse | 1.9 (1.3) | 10 | 1.6 (1.2) | 10 | MD 0.30 (‐0.80 to 1.40) | 0.59 | Haight 2005 | Some concerns |
| Positive regard (direct observation) | Higher scores = better | 5.0 (1.7) | 10 | 5.1 (1.4) | 10 | MD ‐0.10 (‐1.46 to 1.26) | 0.89 | Haight 2005 | Some concerns |
| Intrusiveness (direct observation) | Higher scores = worse | 1.9 (1.0) | 10 | 2.2 (0.9) | 10 | MD ‐0.30 (‐1.13 to 0.53) | 0.48 | Haight 2005 | Some concerns |
| Engagement/interpersonal involvement (direct observation) | Higher scores = better | 5.6 (1.1) | 10 | 5.7 (1.0) | 10 | MD ‐0.10 (‐1.02 to 0.82) | 0.83 | Haight 2005 | Some concerns |
| Inventiveness (direct observation) | Higher scores = better | 4.3 (1.0) | 10 | 4.2 (0.7) | 10 | MD 0.10 (‐0.66 to 0.86) | 0.80 | Haight 2005 | Some concerns |
| Parental self‐efficacy in teaching (SEPTI‐TS) | Higher scores = better | 50.38 (3.07) | 15 | 43.63 (8.88) | 10 | MD 6.76 (1.04 to 12.48) | 0.02 | Liu 2021 | Some concerns |
| Parental self‐efficacy in discipline (SEPTI‐TS) | Higher scores = better | 30.69 (8.0) | 15 | 29.25 (8.84) | 10 | MD 1.44 (‐5.37 to 8.25) | 0.68 | Liu 2021 | Some concerns |
| Parental self‐efficacy in instrumental care (SEPTI‐TS) | Higher scores = better | 38.31 (5.48) | 15 | 37.88 (7.41) | 10 | MD 0.43 (‐4.94 to 5.80) | 0.88 | Liu 2021 | Some concerns |
| Parental sense of confidence (PSOC) | Higher scores = better | 41.86 (4.0) | 15 | 38.60 (5.58) | 10 | MD 3.20 (‐0.80 to 7.20) | 0.12 | Liu 2021 | Some concerns |
| Parenting Stress (PSI‐SF) | Higher scores = worse | 72.54 (22.8) | 16 | 83.01 (20.6) | 13 | MD ‐10.47 (‐26.29 to 5.35) | 0.19 | Rosenblum 2017 | Some concerns |
| Care‐giving Helplessness (CHQ) | Higher scores = worse | 11.0 (5.1) | 15 | 12.2 (5.6) | 13 | MD ‐1.16 (‐5.14 to 2.82) | 0.57 | Rosenblum 2017 | Some concerns |
CI: confidence interval; CIB: Coding Interactive Behaviour System; CHQ: Care‐giving Helplessness Questionnaire; NCATS: Nursing Child Assessment Teaching Scale; PSI‐SF: Parenting Stress Index – Short Form; PSOC: Parenting Sense of Competence Scale; SD: standard deviation; SEPTI‐TS: Self‐Efficacy for Parenting Tasks Index – Toddler Scale; TAS‐45: Toddler Attachment Sort‐45.
Primary outcomes
Parental psychological or socio‐emotional wellbeing
Trauma‐related symptoms
Post‐intervention
Very low‐certainty evidence from one RCT found no clear evidence of a difference between the Mom Power parenting intervention and attention control on PTSD symptoms (PTSD symptom severity) (SMD ‐0.16, 95% CI ‐0.85 to 0.53; 33 participants; Analysis 1.1; MD ‐0.81, 95% CI ‐4.23 to 2.61, measured with National Women's Study PTSD Module, score range 0 to 17) (Rosenblum 2017).
1.1. Analysis.

Comparison 1: Parenting interventions vs inactive control, Outcome 1: Parenting interventions vs inactive control, Outcome 1: Trauma‐related symptoms, at post‐intervention
Psychological wellbeing
Post‐intervention
Very low‐certainty evidence from one RCT found no clear evidence of a difference between the Mom Power parenting intervention relative to attention control on psychological wellbeing (postpartum depression) (SMD ‐0.00, 95% CI ‐0.69 to 0.69; 33 participants; Analysis 1.2; MD ‐0.12, 95% CI ‐24.92 to 24.68, measured with Postpartum Depression Screening Scale, score range 5 to 175) (Rosenblum 2017).
1.2. Analysis.

Comparison 1: Parenting interventions vs inactive control, Outcome 2: Parenting interventions vs inactive control, Outcome 2: Psychological wellbeing, at post‐intervention
Substance use
No studies assessed the effect of parenting interventions on substance use.
Parent relationship quality
No studies assessed the effect of parenting interventions on parent relationship quality.
Parental self‐harm
No studies assessed the effect of parenting interventions on parental self‐harm.
Parenting capacity
Parent‐child relationship
Post‐intervention
Evidence from two RCTs suggested there was a small important improvement in parent‐child relationships (parental sensitivity and dyadic reciprocity) from parenting interventions compared to inactive control (PFR: Promoting First Relationships, and GABI: Group Attachment‐Based Intervention) (SMD 0.45, 95% CI ‐0.06 to 0.96; I2 = 60%; 153 participants; Analysis 1.3) (Pasalich 2019; Steele 2019). There was low certainty in the evidence due to risk of bias and CIs that include little or no difference and important improvement. While heterogeneity was moderate it was not significant (Chi2 P = 0.11) and the CIs overlapped.
1.3. Analysis.

Comparison 1: Parenting interventions vs inactive control, Outcome 3: Parenting interventions vs inactive control, Outcome 6: Parent–child relationship (continuous data), at post‐intervention
The evidence for the effect of two parenting interventions (infant parent psychotherapy, psycho‐educational parenting intervention) on parent‐child relationships (secure attachment) compared with an inactive control was very uncertain from one RCT (Cicchetti 2006) (RR 20.11, 95% CI 4.09 to 98.89; I2 = 0%; 104 participants; very low‐certainty evidence; Analysis 1.4).
1.4. Analysis.

Comparison 1: Parenting interventions vs inactive control, Outcome 4: Parenting interventions vs inactive control, Outcome 6: Parent–child relationship (dichotomous data), at post‐intervention
Compared with an inactive control, this RCT observed reduced disorganised attachment after a parenting intervention (RR 0.50, 95% CI 0.35 to 0.73; I2 = 0%; 104 participants; Analysis 1.5) (Cicchetti 2006). They also observed reduced avoidant attachment (RR 0.29, 95% CI 0.07 to 1.13; I2 = 0%; 104 participants; Analysis 1.6), however, this effect is uncertain as the CIs included a large reduction in negative attachment and little or no difference (95% CI 0.07 to 1.13; 95% CI 0.35 to 0.73). Ambivalent attachment was also reduced (RR 0.32, 95% CI 0.01 to 7.57; 104 participants; Analysis 1.7) with a parenting intervention compared with control, however the CIs included a large reduction and a large increase (95% CI 0.01 to 7.57), indicating that differences between the intervention and control are uncertain.
1.5. Analysis.

Comparison 1: Parenting interventions vs inactive control, Outcome 5: Parenting interventions vs inactive control, Outcome 6: Parent–child relationship (disorganised attachment), at post‐intervention
1.6. Analysis.

Comparison 1: Parenting interventions vs inactive control, Outcome 6: Parenting interventions vs inactive control, Outcome 6: Parent–child relationship (avoidant attachment), at post‐intervention
1.7. Analysis.

Comparison 1: Parenting interventions vs inactive control, Outcome 7: Parenting interventions vs inactive control, Outcome 6: Parent–child relationship (ambivalent attachment), at post‐intervention
Twelve‐month follow‐up
One RCT also assessed two interventions at 12 months post‐intervention (Cicchetti 2006). Compared with usual care, they observed a large difference in favour of parenting interventions, with an increase in secure attachment (RR 3.11, 95% CI 1.33 to 7.27; I2 = 0%; 98 participants; Analysis 1.8), but little to no difference for disorganised attachment (RR 0.83, 95% CI 0.35 to 1.96; I2 = 71%; 98 participants; Analysis 1.9) and ambivalent attachment (RR 0.78, 95% CI 0.22 to 2.76; I2 = 0%; 98 participants; Analysis 1.10). They also observed a difference for avoidant attachment (RR 0.37 95% CI 0.14 to 0.95; I2 = 0%; 98 participants; Analysis 1.11) in favour of the parenting intervention compared to an inactive control; however, the CIs included appreciable improvement and little or no difference, indicating the benefits are uncertain.
1.8. Analysis.

Comparison 1: Parenting interventions vs inactive control, Outcome 8: Parenting interventions vs inactive control, Outcome 6: Parent–child relationship (secure attachment), at 12‐month follow‐up
1.9. Analysis.

Comparison 1: Parenting interventions vs inactive control, Outcome 9: Parenting interventions vs inactive control, Outcome 6: Parent–child relationship (disorganised attachment), at 12‐month follow‐up
1.10. Analysis.

Comparison 1: Parenting interventions vs inactive control, Outcome 10: Parenting interventions vs inactive control, Outcome 6: Parent–child relationship (ambivalent attachment), at 12‐month follow‐up
1.11. Analysis.

Comparison 1: Parenting interventions vs inactive control, Outcome 11: Parenting interventions vs inactive control, Outcome 6: Parent–child relationship (avoidant attachment), at 12‐month follow‐up
Parenting skills
Post‐intervention
Evidence from four RCTs suggested there was little or no difference between parenting interventions and usual care in parenting skills (maternal supportive presence, parental self‐efficacy in nurturance, child care‐giving behaviour); however, we have low certainty in these effects due to risk of bias and CIs including little or no difference and small, important improvement (SMD 0.25, 95% CI ‐0.07 to 0.58; I2 = 0%; 149 participants; Analysis 1.12) (Haight 2005; Liu 2021; Rosenblum 2017; Steele 2019).
1.12. Analysis.

Comparison 1: Parenting interventions vs inactive control, Outcome 12: Parenting interventions vs inactive control, Outcome 7: Parenting skills, at post‐intervention
Evidence from two RCTs suggested there was little or no difference between parenting interventions and usual care in parenting skills (maternal hostility) (SMD ‐0.11, 95% CI ‐0.95 to 0.73; I2 = 66%; 98 participants; Analysis 1.13) (Haight 2005; Steele 2019). There was very low certainty in the results due to high risk of bias, substantial heterogeneity between effect estimates and CIs including important benefit and important harm.
1.13. Analysis.

Comparison 1: Parenting interventions vs inactive control, Outcome 13: Parenting interventions vs inactive control, Outcome 7: Parenting skills (maternal hostility), at post‐intervention
Secondary outcomes
Parental intervention acceptability
Parent engagement
Evidence from six RCTs, including seven interventions, with moderate heterogeneity between effect estimates, suggested there was little or no difference in the number of parents who dropped out of parenting interventions compared to control (RR 1.14, 95% CI 0.89 to 1.46; I2 = 43%; 938 participants; Analysis 1.14) (Cicchetti 2006; Haight 2005; Liu 2021; Pasalich 2019; Rosenblum 2017; Steele 2019).
1.14. Analysis.

Comparison 1: Parenting interventions vs inactive control, Outcome 14: Parent engagement (dropout) ‐ earliest time point
Socio‐ecological outcomes
Changes in parental social capital
Post‐intervention
Evidence from one RCT suggested there was little or no difference between a parenting intervention with service system components (Mom Power) and usual care in changes in parental social capital (perceived connection to community professionals) (SMD 0.12, 95% CI ‐0.62 to 0.86; 29 participants; Analysis 1.15) (Rosenblum 2017).
1.15. Analysis.

Comparison 1: Parenting interventions vs inactive control, Outcome 15: Socio‐ecological outcomes (connection to community professionals) ‐ secondary outcome
Child's physical, socio‐emotional wellbeing
Child emotional and behavioural outcomes
Post‐intervention
Evidence from one RCT suggested there was little or no difference between a parenting intervention and usual care in child emotional and behavioural outcomes: externalising behaviour (SMD ‐0.19, 95% CI ‐0.99 to 0.62; 25 participants; Analysis 1.16) and internalising behaviour (SMD 0.32, 95% CI ‐0.48 to 1.13; 25 participants; Analysis 1.17) (Liu 2021).
1.16. Analysis.

Comparison 1: Parenting interventions vs inactive control, Outcome 16: Child's physical, socio‐emotional wellbeing (externalising behaviour) ‐ post‐intervention
1.17. Analysis.

Comparison 1: Parenting interventions vs inactive control, Outcome 17: Child's physical, socio‐emotional wellbeing (internalising behaviour) ‐ post‐intervention
Twelve‐month follow‐up
Evidence from one RCT assessing two interventions suggested there was little or no difference between parenting interventions and usual care in child emotional and behavioural outcomes at 12‐month follow‐up: externalising behaviour (SMD 0.03, 95% CI ‐0.37 to 0.43; I2 = 0%; 98 participants; Analysis 1.18), internalising behaviour (SMD 0.05, 95% CI ‐0.35 to 0.45; I2 = 0%; 98 participants; Analysis 1.19) or total child behaviour problems (SMD ‐0.03, 95% CI ‐0.43 to 0.37; I2 = 0%; 98 participants; Analysis 1.20) (Cicchetti 2006).
1.18. Analysis.

Comparison 1: Parenting interventions vs inactive control, Outcome 18: Child's physical, socio‐emotional wellbeing (externalising behaviour) ‐ 12‐month follow‐up
1.19. Analysis.

Comparison 1: Parenting interventions vs inactive control, Outcome 19: Child's physical, socio‐emotional wellbeing (internalising behaviour) ‐ 12‐month follow‐up
1.20. Analysis.

Comparison 1: Parenting interventions vs inactive control, Outcome 20: Child's physical, socio‐emotional wellbeing (total behaviour problems) ‐ 12‐month follow‐up
No studies assessed the effect of parenting interventions on the following secondary outcomes:
-
Parental intervention acceptability:
parent satisfaction with intervention;
medical compliance.
-
Socio‐ecological outcomes:
social functioning.
-
Child adverse events recorded during the intervention:
child maltreatment occurrence;
family disruptions and child removals;
other adverse childhood experiences.
-
Child's physical, socio‐emotional wellbeing:
child physical health;
child development.
-
Other outcomes:
service provider knowledge, attitudes and practices; or
cost or cost‐effectiveness.
Comparison 2: Psychological interventions versus inactive control
Eight studies assessed psychological intervention compared to inactive control post‐intervention (Ammerman 2016; Berry 2021; Blalock 2013; Grote 2012; Grote 2015; Madigan 2015; Silverstein 2011; Upshur 2016). See Table 2. Additional outcomes reported in single studies are reported in Table 11.
8. Additional outcomes: psychological interventions.
| Outcome measure (scale) | Direction of effect | Intervention mean (SD)/events | n | Control mean (SD)/events | n | Effect estimate, 95% CI | P value | Study | Risk of bias |
| Primary outcomes | |||||||||
| Trauma‐related symptoms | |||||||||
| Post‐intervention | |||||||||
| PTSD presence (CPI) | Higher scores = worse | 7 | 14 | 9 | 17 | RR 0.94 (0.47 to 1.88) | 0.87 | Madigan 2015 | High |
| 6‐month follow‐up | |||||||||
| Interpersonal problems (IIP) | Higher scores = worse | 2.2 (0.9) | 6 | 2.3 (0.7) | 18 | MD ‐0.10 (‐0.89 to 0.69) | 0.80 | Grote 2012 | Some concerns |
| 12‐month follow‐up | |||||||||
| PTSD presence (CPI) | Higher scores = worse | 7 | 12 | 3 | 14 | RR 2.72 (0.90 to 8.27) | 0.08 | Madigan 2015 | High |
| 18‐month follow‐up | |||||||||
| PTSD symptom severity (PCL‐C) | Higher scores = worse | 32.10 (13.48) | 39 | 37.48 (15.39) | 40 | MD ‐5.38 (‐11.76 to 1.00) | 0.10 | Grote 2015 | High |
| Psychological wellbeing | |||||||||
| Post‐intervention | |||||||||
| Functional impairment severity (WSAS) | Higher scores = worse | 13.68 (9.39) | 40 | 15.42 (10.69) | 38 | MD ‐1.74 (‐6.21 to 2.73) | 0.45 | Grote 2015 | Some concerns |
| Perceived stress (PSS) | Higher scores = worse | 9.78 (3.44) | 19 | 9.38 (3.59) | 19 | MD 0.40 (‐1.84 to 2.64) | 0.73 | Silverstein 2011 | Some concerns |
| Positive coping (BCQ) | Higher scores = better | 2.67 (0.68) | 65 | 2.7 (0.66) | 46 | MD ‐0.03 (‐0.28 to 0.22) | 0.82 | Upshur 2016 | High |
| Negative coping (BCQ) | Higher scores = worse | 1.88 (0.57) | 65 | 1.89 (0.59) | 46 | MD 0.01 (‐0.21 to 0.23) | 0.93 | Upshur 2016 | High |
| 3‐month follow‐up | |||||||||
| Depression symptoms (BDI‐II) | Higher scores = worse | 12.24 (14.4) | 29 | 23.19 (14.44) | 31 | MD ‐10.95 (‐18.25 to ‐3.65) | 0.003 | Ammerman 2016 | Some concerns |
| 6‐month follow‐up | |||||||||
| Postpartum depression (EPDS) | Higher scores = worse | 5.8 (2.8) | 6 | 13.9 (6) | 18 | MD ‐8.10 (‐11.66 to ‐4.54) | < 0.001 | Grote 2012 | Some concerns |
| Depression remission (SCL) | Higher scores = better | 17 | 40 | 13 | 41 | RR 1.34 (0.75 to 2.38) | 0.32 | Grote 2015 | Some concerns |
| Anxiety presence (PHQ) | Higher scores = worse | 5 | 40 | 10 | 41 | RR 0.51 (0.19 to 1.37) | 0.18 | Grote 2015 | High |
| Functional impairment severity (WSAS) | Higher scores = worse | 11.5 (9.55) | 40 | 13.56 (9.03) | 41 | MD ‐2.06 (‐6.11 to 1.99) | 0.32 | Grote 2015 | Some concerns |
| 12‐month follow‐up | |||||||||
| Depression remission (SCL) | Higher scores = better | 15 | 39 | 11 | 41 | RR 1.43 (0.75 to 2.73) | 0.27 | Grote 2015 | Some concerns |
| Anxiety presence (PHQ) | Higher scores = worse | 5 | 39 | 10 | 41 | RR 0.53 (0.20 to 1.50) | 0.20 | Grote 2015 | High |
| Functional impairment severity (WSAS) | Higher scores = worse | 11.21 (9.4) | 39 | 13.85 (10.96) | 41 | MD ‐2.64 (‐7.11 to 1.83) | 0.25 | Grote 2015 | Some concerns |
| Anxiety symptoms (SCARED) | Higher scores = worse | 23.18 (12.84) | 12 | 16.87 (9.5) | 14 | MD 6.31 (‐2.50 to 15.12) | 0.16 | Madigan 2015 | High |
| Behavioural problems (YSR) | Higher scores = worse | 14.92 (9.63) | 12 | 11.13 (8.5) | 14 | MD 3.79 (‐3.25 to 10.83) | 0.29 | Madigan 2015 | High |
| 18‐month follow‐up | |||||||||
| Depression symptoms (SCL) | Higher scores = worse | 0.78 (0.69) | 39 | 1.07 (0.78) | 40 | MD ‐0.29 (‐0.61 to 0.03) | 0.08 | Grote 2015 | Some concerns |
| Depression remission (SCL) | Higher scores = better | 17 | 39 | 12 | 40 | RR 1.45 (0.80 to 2.63) | 0.22 | Grote 2015 | Some concerns |
| Anxiety presence (PHQ) | Higher scores = worse | 5 | 39 | 10 | 40 | RR 0.51 (0.19 to 1.36) | 0.18 | Grote 2015 | High |
| Functional impairment severity (WSAS) | Higher scores = worse | 9.08 (8.16) | 39 | 13.33 (9.93) | 40 | MD ‐4.25 (‐8.25 to ‐0.25) | 0.04 | Grote 2015 | Some concerns |
| Parent relationship quality | |||||||||
| 3‐month follow‐up | |||||||||
| Social support (ISEL) | Higher scores = better | 83.31 (22.03) | 29 | 65.10 (23.9) | 31 | MD 18.21 (6.59 to 29.83) | 0.002 | Ammerman 2016 | Some concerns |
| Parenting skills | |||||||||
| Post‐intervention | |||||||||
| Functioning/coping (PSI‐SF) | Higher scores = worse | 73.47 (24.68) | 32 | 80.77 (17.63) | 35 | MD ‐7.30 (‐17.66 to 3.06) | 0.17 | Ammerman 2016 | Some concerns |
| 3‐month follow‐up | |||||||||
| Providing a stimulating, nurturing, safe environment (HOME) | Higher scores = better | 34.61 (6.24) | 28 | 33.13 (4.95) | 30 | MD 1.48 (‐1.43 to 4.39) | 0.32 | Ammerman 2016 | Some concerns |
| Functioning/coping (PSI‐SF) | Higher scores = worse | 67.11 (32.1) | 28 | 75.07 (26.3) | 30 | MD ‐7.96 (‐23.12 to 7.20) | 0.30 | Ammerman 2016 | Some concerns |
| Secondary outcomes | |||||||||
| Socioecological outcomes | |||||||||
| 3‐month follow‐up | |||||||||
| Social network size (SNI) | Higher scores = better | 14.15 (9.78) | 27 | 11.03 (5.83) | 29 | MD 3.12 (‐1.14 to 7.38) | 0.15 | Ammerman 2016 | Some concerns |
| 6‐month follow‐up | |||||||||
| Quality of social functioning with friends (SAS) | Higher scores = worse | 2.1 (0.7) | 6 | 3.3 (0.8) | 18 | MD ‐1.20 (‐1.87 to ‐0.53) | < 0.001 | Grote 2012 | Some concerns |
CI: confidence interval; BCQ: Brief‐COPE Questionnaire; BDI: Beck Depression Inventory; BDI‐II: Beck Depression Inventory, Second Edition; CPI: Californian Psychological Inventory – Socialization Scale; EPDS: Edinburgh Postnatal Depression Scale; HOME: Home Observation for Measurement of the Environment Inventory; IIP: Inventory of Interpersonal Problems; ISEL: Interpersonal Support Evaluation List; MD: mean difference; PCL‐C: PTSD CheckList – Civilian Version; PHQ: PRIME‐MD Patient Health Questionnaire; PSI‐SF: Parenting Stress Index Short‐Form; PSS: Perceived Stress Scale; PTSD: posttraumatic stress disorder; RR: risk ratio; SAS: Social Adjustment Scale; SCARED: Screen for Child Anxiety Related Emotional Disorders; SCL: Symptom Checklist Depression Scale; SD: standard deviation; SNI: Social Network Index; WSAS: Work and Social Adjustment Scale; YSR: Youth Self‐Report.
Primary outcomes
Parental psychological or socio‐emotional wellbeing
Trauma‐related symptoms
Post‐intervention
Low‐certainty evidence from four RCTs suggested there may be little or no difference between psychological interventions and usual care in CPTSD symptoms (interpersonal problems, PTSD symptom severity, dissociation) (SMD ‐0.05, 95% CI ‐0.40 to 0.31; I2 = 39%; 247 participants; Analysis 2.1) (Grote 2012; Grote 2015; Madigan 2015; Upshur 2016).
2.1. Analysis.

Comparison 2: Psychological interventions vs inactive control, Outcome 1: Psychological interventions vs inactive control, Outcome 1: Trauma‐related symptoms, at post‐intervention
Six‐month follow‐up
Evidence from three RCTs that assessed trauma‐related symptoms at six months post‐intervention suggested there was little or no difference between psychological interventions and usual care in CPTSD symptoms (interpersonal problems, PTSD symptom severity, dissociation) (SMD ‐0.05, 95% CI ‐0.56 to 0.46; I2 = 44%; 136 participants; Analysis 2.2) (Grote 2012; Grote 2015; Madigan 2015).
2.2. Analysis.

Comparison 2: Psychological interventions vs inactive control, Outcome 2: Psychological interventions vs inactive control, Outcome 1: Trauma‐related symptoms, at 6‐month follow‐up
Twelve‐month follow‐up
Evidence from two RCTs that reported CPTSD symptoms (PTSD symptom severity, dissociation) at 12 months post‐intervention suggested there was little or no difference between psychological interventions and usual care (SMD ‐0.14, 95% CI ‐0.62 to 0.34; I2 = 25%; 106 participants; Analysis 2.3) (Grote 2015; Madigan 2015).
2.3. Analysis.

Comparison 2: Psychological interventions vs inactive control, Outcome 3: Psychological interventions vs inactive control, Outcome 1: Trauma‐related symptoms, at 12‐month follow‐up
Psychological wellbeing
Post‐intervention
Low‐certainty evidence from eight RCTs suggested there was little or no difference between psychological interventions and usual care in psychological wellbeing (depression symptom severity) (SMD ‐0.34, 95% CI ‐0.66 to ‐0.03; I2 = 63%; 507 participants; Analysis 2.4) (Ammerman 2016; Berry 2021; Blalock 2013; Grote 2012; Grote 2015; Madigan 2015; Silverstein 2011; Upshur 2016). Heterogeneity between effect estimates was substantial in this comparison; however, we did not downgrade the certainty as there was overlap in CIs and the majority of studies showed a small improvement or little or no difference.
2.4. Analysis.

Comparison 2: Psychological interventions vs inactive control, Outcome 4: Psychological interventions vs inactive control, Outcome 2: Psychological wellbeing (continuous data), at post‐intervention
Depression remission/episodes: Evidence from two RCTs suggested that psychological interventions made little or no difference to the number of parents achieving remission from depression or experiencing moderate‐severe depressive episodes post‐intervention compared to usual care (RR 0.99, 95% CI 0.81 to 1.22; I2 = 0%; 116 participants; Analysis 2.5) (Grote 2015; Silverstein 2011).
2.5. Analysis.

Comparison 2: Psychological interventions vs inactive control, Outcome 5: Psychological interventions vs inactive control, Outcome 2: Psychological wellbeing (dichotomous data), at post‐intervention
Postpartum depression: Evidence from two RCTs suggested there was little or no difference between psychological interventions and usual care in postpartum depression symptom severity (SMD ‐0.22, 95% CI ‐0.57 to 0.13; I2 = 0%; 135 participants; Analysis 2.6) (Grote 2012; Upshur 2016).
2.6. Analysis.

Comparison 2: Psychological interventions vs inactive control, Outcome 6: Psychological interventions vs inactive control, Outcome 2: Psychological wellbeing (postpartum depression symptom severity), at post‐intervention
Anxiety: Evidence from two RCTs suggested there was little or no difference between psychological interventions and usual care in anxiety symptom severity post‐intervention (SMD ‐0.00, 95% CI ‐0.57 to 0.57; I2 = 0%; 54 participants; Analysis 2.7) (Berry 2021; Grote 2012).
2.7. Analysis.

Comparison 2: Psychological interventions vs inactive control, Outcome 7: Psychological interventions vs inactive control, Outcome 2: Psychological wellbeing (anxiety symptom severity), at post‐intervention
Six‐month follow‐up
Depression: Evidence from three RCTs that also assessed depression symptom severity at six months post‐intervention suggested there was little or no difference between psychological interventions and usual care, but there was considerable heterogeneity between effect estimates (SMD ‐0.29, 95% CI ‐1.21 to 0.63; I2 = 81%; 136 participants; Analysis 2.8) (Grote 2012; Grote 2015; Madigan 2015).
2.8. Analysis.

Comparison 2: Psychological interventions vs inactive control, Outcome 8: Psychological interventions vs inactive control, Outcome 2: Psychological wellbeing (depression symptom severity), at 6‐month follow‐up
Anxiety: Evidence from two RCTs suggested there was little or no difference between psychological interventions and usual care in anxiety symptom severity at six months post‐intervention (SMD ‐0.33, 95% CI ‐1.30 to 0.63; I2 = 62%; 55 participants; Analysis 2.9) (Grote 2012; Madigan 2015).
2.9. Analysis.

Comparison 2: Psychological interventions vs inactive control, Outcome 9: Psychological interventions vs inactive control, Outcome 2: Psychological wellbeing (anxiety symptom severity), at 6‐month follow‐up
Twelve‐month follow‐up
Depression: Evidence from two RCTs suggested there was little or no difference between psychological interventions and usual care in depression symptom severity at 12 months post‐intervention, but there was considerable heterogeneity between effect estimates (SMD 0.17, 95% CI ‐0.80 to 1.14; I2 = 78%; 106 participants; Analysis 2.10) (Grote 2015; Madigan 2015).
2.10. Analysis.

Comparison 2: Psychological interventions vs inactive control, Outcome 10: Psychological interventions vs inactive control, Outcome 2: Psychological wellbeing (depression symptom severity), at 12‐month follow‐up
Substance use
Post‐intervention
One RCT found a small, important decrease in substance use (abstinence from smoking) six months post‐intervention in mothers who received an interpersonally focused therapy ‐ cognitive behavioural analysis system of psychotherapy (CBASP) with usual behavioural and motivational smoking cessation counselling, compared to those who received usual behavioural and motivational smoking cessation counselling alone (RR 1.57, 95% CI 0.72 to 3.45; 189 participants; Analysis 2.11) (Blalock 2013). There was low certainty in this effect due to risk of bias and CIs including little or no difference and appreciable benefit (in absolute terms from 2 fewer per 100 to 24 more).
2.11. Analysis.

Comparison 2: Psychological interventions vs inactive control, Outcome 11: Psychological interventions vs inactive control, Outcome 3: Substance use, at post‐intervention
Parent relationship quality
Post‐intervention
Low‐certainty evidence from one RCT found a small appreciable benefit of a psychological intervention (in‐home CBT) compared to usual care on parent relationship quality (social support) (SMD 0.49, 95% CI 0.00 to 0.98; 67 participants; Analysis 2.12; MD 12.03, 95% CI 0.39 to 23.67, measured with Interpersonal Support Evaluation List, score range 0 to 120) (Ammerman 2016).
2.12. Analysis.

Comparison 2: Psychological interventions vs inactive control, Outcome 12: Psychological interventions vs inactive control, Outcome 4: Parent relationship quality, at post‐intervention
Parental self‐harm
No studies assessed the effect of psychological interventions on parental self‐harm.
Parenting capacity
Parent‐child relationship
Post‐intervention
Evidence from one study was very uncertain regarding whether a psychological intervention had any effect on the proportion of participants with poor parent‐child relationship outcomes (disorganised infant attachment) compared with an inactive control (RR 4.67, 95% CI 0.60 to 36.29; 26 participants; Analysis 2.13) (Madigan 2015).
2.13. Analysis.

Comparison 2: Psychological interventions vs inactive control, Outcome 13: Psychological interventions vs inactive control, Outcome 6: Parent–child relationship, at post‐intervention
Parenting skills
Post‐intervention
Low‐certainty evidence from one RCT found a small appreciable benefit of a psychological intervention (in‐home CBT) on parenting skills (providing a stimulating environment) compared with an inactive control (SMD 0.51, 95% CI 0.01 to 1.00; 66 participants; Analysis 2.14; MD 3.04, 95% CI 0.20 to 5.88, measured with Parenting Stress Index, score range 36 to 180) (Ammerman 2016).
2.14. Analysis.

Comparison 2: Psychological interventions vs inactive control, Outcome 14: Psychological interventions vs inactive control, Outcome 7: Parenting skills, at post‐intervention
Secondary outcomes
Parental intervention acceptability
Parent engagement
Evidence from seven RCTs suggested there was little to no difference in dropout numbers from the psychological intervention compared to inactive control. There was moderate heterogeneity in the effect estimates (RR 1.04, 95% CI 0.64, 1.68; I2 = 54%; 926 participants; Analysis 2.15) (Ammerman 2016; Berry 2021; Blalock 2013; Grote 2015; Madigan 2015; Silverstein 2011; Upshur 2016).
2.15. Analysis.

Comparison 2: Psychological interventions vs inactive control, Outcome 15: Parent engagement (dropout) ‐ earliest time point
Socio‐ecological outcomes
Social functioning outcomes
Post‐intervention
Evidence from four RCTs suggested there was little or no difference between psychological interventions and usual care in parental social functioning (social functioning, perceived social support, quality of functioning with friends, social network size) (SMD ‐0.13, 95% CI ‐0.39 to 0.13; I2 = 0%; 240 participants; Analysis 2.16) (Ammerman 2016; Grote 2012; Silverstein 2011; Upshur 2016).
2.16. Analysis.

Comparison 2: Psychological interventions vs inactive control, Outcome 16: Socio‐ecological outcomes (social support) ‐ secondary outcome
Child's physical, socio‐emotional wellbeing
Child emotional and behavioural outcomes
Post‐intervention
Evidence from one study found a large appreciable benefit from the Practical Resources for Effective Postpartum Parenting (PREPP) psychological and parenting intervention compared to enhanced usual care, in child emotional and behavioural outcomes (daytime sleeping minutes) (SMD 1.08, 95% CI ‐0.08 to 2.24, 14 participants; Analysis 2.17) (Berry 2021); however, the CIs crossed our threshold for appreciable increase and little or no difference indicating that any difference between intervention and control group is uncertain.
2.17. Analysis.

Comparison 2: Psychological interventions vs inactive control, Outcome 17: Child's physical, socio‐emotional wellbeing (daytime sleeping) ‐ secondary outcome
Other outcomes
Cost or cost‐effectiveness
One RCT reported health outcomes in terms of quality‐adjusted life‐years, depression‐free days and interventions costs, in a cost‐utility analysis of a psychological intervention for low‐income mothers (Ammerman 2016). The intervention (IH‐CBT) was associated with improved quality of life and reduced cost. Within three years there was an incremental health gain of 0.07 (approximately one month) and reduced costs of USD $2. Mothers receiving IH‐CBT were expected to experience 345.6 fewer days of depression compared to the control group receiving standard home visiting.
Another RCT reported health outcomes for mothers with depression alone or with comorbid PTSD in terms of depression‐free days and intervention costs in a cost‐effectiveness analysis (Grote 2015). A psychological intervention (MOMCare) was found to be cost‐effective for mothers with comorbid conditions, as a large health gain outweighed the additional costs of augmenting usual care with MOMCare. Mothers with comorbid depression and PTSD had 68 more depression‐free days than those in the control condition, with an associated cost of USD $1312 creating an overall net benefit when a depression‐free day was valued at greater than USD $20 ($20 x 68 = $1360). Mothers without comorbid PTSD reported 13 more depression‐free days compared to the control condition, with an associated cost of USD $1167 and therefore assessed as having no positive net benefit ($20 x 13 = $260).
No studies assessed the effect of psychological interventions on the following secondary outcomes:
-
Parental intervention acceptability:
parent satisfaction with intervention;
medical compliance.
-
Socio‐ecological outcomes:
changes in social capital.
-
Child adverse events recorded during the intervention:
child maltreatment occurrence;
family disruptions and child removals;
other adverse childhood experiences.
-
Child's physical, socio‐emotional wellbeing:
child physical health;
child development.
-
Other outcomes:
service provider knowledge, attitudes and practices.
Comparison 3: Service system approaches versus inactive control
One RCT compared (1) a full service system approach consisting of financial empowerment education and group, trauma‐informed peer support, with (2) a partial service system approach consisting only of financial empowerment education, and (3) usual care, post‐intervention (Booshehri 2018). See Table 3.
Primary outcomes
Parental psychological or socio‐emotional wellbeing
Trauma‐related symptoms
No studies assessed the effect of service system approaches on CPTSD/PTSD symptoms.
Psychological wellbeing
Post‐intervention
Evidence from one RCT with two intervention arms suggested that service system approaches involving financial education and group peer support resulted in slightly worse psychological wellbeing (depression symptom severity) compared to usual care (SMD 0.42, 95% CI ‐0.15 to 0.99; I2 = 0%; 52 participants; Analysis 3.1; MD 1.62 95% CI ‐1.00 to 4.25; measured with Center for Epidemiological Studies Depression Scale, score range 0 to 60) (Booshehri 2018). Our certainty in the evidence was low due to high risk of bias, and CIs consistent with little or no difference, and important harm.
3.1. Analysis.

Comparison 3: Service system approaches vs inactive control, Outcome 1: Service system approaches vs inactive control, Outcome 2: Psychological wellbeing, at post‐intervention
This RCT found that service system approaches involving financial empowerment and peer group support resulted in a possible slight increase in parental self‐efficacy (SMD 0.79, 95% CI 0.20 to 1.37; I2 = 0%; 52 participants; Analysis 3.2) (Booshehri 2018).
3.2. Analysis.

Comparison 3: Service system approaches vs inactive control, Outcome 2: Service system approaches vs inactive control, Outcome 2: Psychological wellbeing (self‐efficacy), at post‐intervention (3‐month follow‐up)
Six‐month follow‐up
This RCT with two eligible intervention arms also assessed psychological wellbeing at six months post‐intervention, and observed little or no difference in depression symptom severity between intervention and usual care (SMD ‐0.02, 95% CI ‐0.60 to 0.55; I2 = 0%; 53 participants; Analysis 3.3), and a small increase in parental self‐efficacy (SMD 0.56, 95% CI ‐0.03 to 1.15; I2 = 0%; 53 participants; Analysis 3.4) (Booshehri 2018); however, our certainty in the evidence was low as the CIs crossed our threshold for both appreciable benefit and little or no difference.
3.3. Analysis.

Comparison 3: Service system approaches vs inactive control, Outcome 3: Service system approaches vs inactive control, Outcome 2: Psychological wellbeing (depression symptom severity), at 6‐month follow‐up
3.4. Analysis.

Comparison 3: Service system approaches vs inactive control, Outcome 4: Service system approaches vs inactive control, Outcome 2: Psychological wellbeing (self‐efficacy), at 6‐month follow‐up
Nine‐month follow‐up
This RCT also assessed psychological wellbeing at nine months post‐intervention compared to control, and observed slight improvements in depression symptom severity (SMD ‐0.46, 95% CI ‐1.43 to 0.51, I² = 56%; 46 participants; Analysis 3.5), and parental self‐efficacy (SMD 0.43, 95% CI ‐0.20 to 1.07; I2 = 0%; 46 participants; Analysis 3.6) (Booshehri 2018); however, the CIs crossed our threshold for appreciable benefit and appreciable harms (depression), or little or no difference (self‐efficacy), indicating that differences between the intervention and control groups are uncertain.
3.5. Analysis.

Comparison 3: Service system approaches vs inactive control, Outcome 5: Service system approaches vs inactive control, Outcome 2: Psychological wellbeing (depression symptom severity), at 9‐month follow‐up
3.6. Analysis.

Comparison 3: Service system approaches vs inactive control, Outcome 6: Service system approaches vs inactive control, Outcome 2: Psychological wellbeing (self‐efficacy), at 9‐month follow‐up
Substance use
No studies assessed the effect of service system approaches on substance use.
Parenting capacity
Parent relationship quality
No studies assessed the effect of service system approaches on parent relationship quality.
Parental self‐harm
No studies assessed the effect of service system approaches on parental self‐harm.
Parent‐child relationship
No studies assessed the effect of service system approaches on parent‐child relationship.
Parenting skills
No studies assessed the effect of service system approaches on parenting skills.
Secondary outcomes
Parental intervention acceptability
Parent engagement
Participants in one RCT, including two intervention arms, were slightly more likely to drop out of the intervention group than the control group (RR 1.40, 95% CI 0.86 to 2.29; I2 = 0%; 103 participants; Analysis 3.7) (Booshehri 2018). The CIs were consistent with little or no difference and a large effect favouring better engagement in the control compared to the intervention group.
3.7. Analysis.

Comparison 3: Service system approaches vs inactive control, Outcome 7: Parent engagement (dropout) ‐ earliest time point
Socio‐ecological outcomes
Changes in social capital
Post‐intervention
One RCT with two intervention arms observed that service system approaches involving financial empowerment and peer group support resulted in little or no difference in changes in social capital (economic hardship) (SMD 0.03, 95% CI ‐0.53 to 0.59; I2 = 0%; 52 participants; Analysis 3.8), or employment (RR 1.16, 95% CI 0.62 to 2.18; I2 = 0%; 52 participants; Analysis 3.9) compared to usual care (Booshehri 2018).
3.8. Analysis.

Comparison 3: Service system approaches vs inactive control, Outcome 8: Socioecological outcomes (hardship) ‐ post‐intervention (3‐month follow‐up)
3.9. Analysis.

Comparison 3: Service system approaches vs inactive control, Outcome 9: Socioecological outcomes (employment status) ‐ post‐intervention (3‐month follow‐up)
Six‐month follow‐up
This RCT assessed changes in social capital at six months post‐intervention, and found a small reduction in economic hardship in the intervention compared to usual care group (SMD ‐0.49, 95% CI ‐1.07 to 0.10; I2 = 0%; 53 participants; Analysis 3.10) (Booshehri 2018); however, the CIs were consistent with a reduction and little or no effect. Little or no difference was observed between intervention participants compared to control in employment status (RR 0.85, 95% CI 0.51 to 1.41; I2 = 0%; 53 participants; Analysis 3.11).
3.10. Analysis.

Comparison 3: Service system approaches vs inactive control, Outcome 10: Socioecological outcomes (hardship) ‐ 6‐month follow‐up
3.11. Analysis.

Comparison 3: Service system approaches vs inactive control, Outcome 11: Socioecological outcomes (employment status) ‐ 6‐month follow‐up
Nine‐month follow‐up
At nine months, there was little or no difference between intervention and control in economic hardship (SMD ‐0.16, 95% CI ‐0.79 to 0.47; I2 = 0%; 46 participants; Analysis 3.12). There was a slight improvement in employment status in intervention compared to control (RR 1.37, 95% CI 0.63 to 2.96; I2 = 0%; 46 participants; Analysis 3.13) (Booshehri 2018); however, the CIs crossed our threshold for appreciable benefit and appreciable harm, indicating that differences between the intervention and control groups are uncertain.
3.12. Analysis.

Comparison 3: Service system approaches vs inactive control, Outcome 12: Socioecological outcomes (hardship) ‐ 9‐month follow‐up
3.13. Analysis.

Comparison 3: Service system approaches vs inactive control, Outcome 13: Socioecological outcomes (employment status) ‐ 9‐month follow‐up
Child's physical, socio‐emotional wellbeing
Post‐intervention
One RCT with two intervention arms found that a service system intervention involving financial counselling and group peer support may slightly decrease child developmental risk compared to usual care (RR 0.68, 95% CI 0.27 to 1.73; I2 = 0%; 52 participants; Analysis 3.14) (Booshehri 2018); however, the CIs were consistent with important benefit and important harm, so these results are uncertain.
3.14. Analysis.

Comparison 3: Service system approaches vs inactive control, Outcome 14: Child's physical, socio‐emotional wellbeing (child developmental risk) ‐ post‐intervention (3‐month follow‐up)
Six‐month follow‐up
This RCT found that the service system intervention increased child developmental risk compared to usual care at six months post‐intervention (RR 1.86, 95% CI 0.44 to 7.89; I2 = 0%; 53 participants; Analysis 3.15) (Booshehri 2018); however, the CIs crossed our threshold for both appreciable benefit and harm, indicating that differences between the intervention and control are uncertain.
3.15. Analysis.

Comparison 3: Service system approaches vs inactive control, Outcome 15: Child's physical, socio‐emotional wellbeing (child developmental risk) ‐ 6‐month follow‐up
Nine‐month follow‐up
At nine months post‐intervention, the service system intervention greatly increased child developmental risk compared to the control group (RR 2.44, 95% CI 0.49 to 12.25; I2 = 0%; 46 participants; Analysis 3.16) (Booshehri 2018); however, the CIs crossed our threshold for both appreciable benefit and appreciable harm, indicating that differences between the intervention and control are uncertain.
3.16. Analysis.

Comparison 3: Service system approaches vs inactive control, Outcome 16: Child's physical, socio‐emotional wellbeing (child developmental risk) ‐ 9‐month follow‐up
No studies assessed the effect of service system approaches on the following secondary outcomes:
-
Parental intervention acceptability:
parent satisfaction with intervention;
medical compliance.
-
Socio‐ecological outcomes:
changes in social functioning.
-
Child adverse events recorded during the intervention:
child maltreatment occurrence;
family disruptions and child removals;
other adverse childhood experiences.
-
Child's physical, socio‐emotional wellbeing:
child physical health;
child development.
-
Other outcomes:
service provider knowledge, attitudes and practices;
cost or cost‐effectiveness.
Sensitivity analyses
We conducted sensitivity analyses to examine the robustness of the meta‐analytic effects to: exclusion of trials at high risk of bias; exclusion of trials with fewer than 50 participants; and fitting a fixed‐effect model in place of our primary model (a random‐effects model); see Table 12. These analyses revealed that some of the interpretations of the size of the effect estimates were not robust to the sensitivity analyses, primarily demonstrating the fragility of the meta‐analysis results arising from few studies with small sample sizes.
9. Sensitivity analysis results.
| Outcome | Description sensitivity analysis | Measure | No. studies | Original effect estimate (95% CI) | No. studies remaining | Sensitivity analysis effect estimate (95% CI) |
| Parenting interventions | ||||||
| Parent‐child relationship | Investigation of robustness of meta‐analytic effect excluding studies of high risk of bias | Parental sensitivity (NCATS) | 2 | SMD 0.45, 95% CI ‐0.06 to 0.96 I2 = 60% Tau2 = 0.08 | 1 | SMD 0.19, 95% CI ‐0.27 to 0.65 I2 = NA Tau2 = NA |
| Investigation of robustness of meta‐analytic effect to type of meta‐analytic modela | Parental sensitivity (NCATS); Dyadic reciprocity (CIB) | 2 | SMD 0.45, 95% CI 0.12 to 0.77 I2 = 60% Chi2 = 2.49 | |||
| Parenting skills | Investigation of robustness of meta‐analytic effect excluding studies of high risk of bias | Maternal supportive presence (Direct observation, non‐validated tool); Parental self‐efficacy in nurturance (SEPTI‐TS); Child care‐giving behaviour (CHQ) | 4 | SMD 0.25, 95% CI ‐0.07 to 0.58 I2 = 0% Tau2 = 0.00 | 3 | SMD ‐0.01, 95% CI ‐0.48 to 0.46 I2 = 0% Tau2 = 0.00 |
| Investigation of robustness of meta‐analytic effect excluding studies with < 50 participants | Maternal supportive presence (CIB) | 1 | SMD 0.49, 95% CI 0.04 to 0.94 I2 = NA Tau2 = NA | |||
| Investigation of robustness of meta‐analytic effect to type of meta‐analytic modela | Maternal supportive presence (Direct observation, non‐validated tool); Parental self‐efficacy in nurturance (SEPTI‐TS); Child care‐giving behaviour (CHQ); Maternal supportive presence (CIB) | 4 | SMD 0.25, 95% CI ‐0.07 to 0.58 I2 = 0% Chi2 = 2.84 | |||
| Psychological interventions | ||||||
| Trauma‐related symptoms | Investigation of robustness of meta‐analytic effect excluding studies of high risk of bias | Interpersonal problems (IIP); PTSD (PSS) | 4 | SMD ‐0.05, 95% CI ‐0.40 to 0.31 I2 = 39% Tau2 = 0.05 | 1 | SMD 0.41, 95% CI ‐0.52 to 1.35 I2 = NA Tau2 = NA |
| Investigation of robustness of meta‐analytic effect to type of meta‐analytic modela | Interpersonal problems (IIP); PTSD (PCL‐C); Dissociation (ADES); PTSD (PSS) | 4 | SMD ‐0.11, 95% CI ‐0.36 to 0.15 I2 = 39% Chi2 = 4.90 | |||
| Psychological well‐being | Investigation of robustness of meta‐analytic effect excluding studies of high risk of bias | Depression (BDI; HRSD; CESDS; HSC; QIDS); Postpartum depression (EPDS) | 8 | SMD ‐0.34, 95% CI ‐0.66 to ‐0.03 I2 = 63% Tau2 = 0.12 | 6 | SMD ‐0.52, 95% CI ‐0.81 to ‐0.22 I2 = 41% Tau2 = 0.05 |
| Investigation of robustness of meta‐analytic effect excluding studies with < 50 participants | Depression (BDI; CESDS; HSC); Postpartum depression (EPDS) | 4 | SMD ‐0.53, 95% CI ‐0.91 to ‐0.16 I2 = 69% Tau2 = 0.10 |
|||
| Investigation of robustness of meta‐analytic effect to type of meta‐analytic modela | Depression (BDI; HRSD; HSC; QIDS); Postpartum depression (EPDS) | 8 | SMD‐0.37, 95% CI ‐0.55 to ‐0.19 I2 = 63% Chi2 = 18.8 |
|||
a i.e. comparing the combined effect from a random‐effects model (original) with a fixed‐effect model (sensitivity analysis)
ADES: Adolescent Dissociative Experiences Scale; BDI: Beck Depression Inventory; CESDS: Center for Epidemiologic Studies Depression Scale; CHQ: Care‐giving Helplessness Questionnaire; CI: confidence interval; CIB: Coding Interactive Behaviour System; EPDS: Edinburgh Postnatal Depression Scale; HRSD: Hamilton Rating Scale for Depression; HSC: Hopkins Symptom Checklist; IIP: Inventory of Interpersonal Problems; NCATS: Nursing Child Assessment Teaching Scale; PCL‐C: PTSD CheckList ‐ Civilian Version; PSS: Posttraumatic Stress Scale; PTSD: post‐traumatic stress disorder; QIDS: Quick Inventory of Depressive Symptoms; SEPTI‐TS: Self‐Efficacy for Parenting Tasks Index ‐ Toddler Scale
Specifically, parent‐child relationships shifted from a small but important difference between a parenting intervention and inactive control (SMD 0.45, 95% CI ‐0.06 to 0.96; I2 = 60%; 2 studies, 153 participants; Pasalich 2019; Steele 2019) to little or no difference (SMD 0.19, 95% CI ‐0.27 to 0.65; 1 study, 75 participants; Pasalich 2019); parenting skills shifted from little or no difference between intervention and inactive control (SMD 0.25, 95%CI ‐0.07 to 0.58; I2 = 0%; 4 studies, 149 participants; Haight 2005; Liu 2021; Rosenblum 2017; Steele 2019) to a small, important effect in favour of the intervention (SMD 0.49, 95% CI 0.04 to 0.94; 1 study, 78 participants; Steele 2019) when three studies with fewer than 50 participants were excluded.
Excluding three studies at high risk of bias from the comparison of a psychological intervention and inactive control for trauma‐related symptoms resulted in a shift from little or no difference (SMD ‐0.05, 95%CI ‐0.40 to 0.31; I2 = 39%; 4 studies, 247 participants; Grote 2012; Grote 2015; Madigan 2015; Upshur 2016) to a small, important effect in favour of the intervention group (SMD 0.41, 95% CI ‐0.52 to 1.35; 1 study, 24 participants; Grote 2012). Similarly, exclusion of two studies at high risk of bias from the comparison of a psychological intervention and inactive control for psychological wellbeing shifted the effect size from little or no difference (SMD ‐0.34, 95% CI ‐0.66 to ‐0.03; I2 = 63%; 507 participants; Ammerman 2016; Berry 2021; Blalock 2013; Grote 2012; Grote 2015; Madigan 2015; Silverstein 2011; Upshur 2016) to a small, important effect in favour of the intervention group (SMD ‐0.52, 95%CI ‐0.81 to ‐0.22; I2 = 41%; 6 studies, 365 participants; Ammerman 2016; Berry 2021; Blalock 2013; Grote 2012; Grote 2015; Silverstein 2011). Finally, exclusion of four studies with fewer than 50 participants also shifted this result for psychological wellbeing to a small, important benefit for the intervention group (SMD ‐0.53, 95% CI ‐0.91 to ‐0.16; I2 = 29%; 4 studies, 384 participants; Ammerman 2016; Blalock 2013; Grote 2015; Upshur 2016).
The fact that in all analyses (with one exception) the interpretation changed from a ‘small (trivial) effect’ in the original analysis to a ‘small but important effect’ in the sensitivity analysis provides some cautious reassurance that the original meta‐analysis effect estimates were not exaggerated towards the interventions. Furthermore, the comparison of results yielded from fixed‐ and random‐effects models provided some reassurance that small‐study effects did not importantly impact the results.
Subgroup analyses
Complexity of intervention
We conducted subgroup analyses to examine if the complexity of the intervention potentially modified the magnitude of intervention effects. The planned complexity subgroups were single‐component, multiple‐component and tailored components; however, no interventions used tailored components.
For the comparison of parenting interventions versus inactive control on parenting skills, there was no evidence that the magnitude of the effect estimates for single‐component interventions (SMD 0.31, 95% CI ‐0.06 to 0.68; I2 = 3%; 3 studies, 123 participants; Haight 2005; Steele 2019; Liu 2021) differed compared with multiple‐component interventions (SMD ‐0.06, 95% CI ‐0.83 to 0.71; 1 study, 26 participants; Rosenblum 2017) (Analysis 1.21; test for subgroup differences Chi2 = 0.74, df = 1, P = 0.39 I2 = 0%).
1.21. Analysis.

Comparison 1: Parenting interventions vs inactive control, Outcome 21: Parenting interventions vs inactive control, Outcome 7: Parenting skills, at post‐intervention, subgroup analysis (multiple component interventions)
For the comparison of psychological interventions versus inactive control on trauma‐related symptoms, there was no evidence that the magnitude of the effect estimates for single‐component interventions (SMD 0.07, 95% CI ‐0.55 to 0.69; I2 = 59%; 2 studies, 142 participants) differed compared with multi‐component interventions (SMD ‐0.08, 95% CI ‐0.79 to 0.62; I2 = 52%; 2 studies, 105 participants) (Analysis 2.18; test for subgroup differences Chi2 = 0.10, df = 1, P = 0.75, I2 = 0%; very low‐certainty evidence). The multiple‐component interventions included both psychological and service system approach components (Grote 2012; Grote 2015), while the single‐component interventions included only psychological interventions (Madigan 2015; Upshur 2016).
2.18. Analysis.

Comparison 2: Psychological interventions vs inactive control, Outcome 18: Psychological interventions vs inactive control, Outcome 1: Trauma‐related symptoms, at post‐intervention, subgroup (multiple component interventions)
For the comparison of psychological interventions versus inactive control on depression symptoms, there was no evidence that the magnitude of effect estimates for single‐component interventions (SMD ‐0.31, 95% CI ‐0.78 to 0.15; I2 = 77%; 5 studies, 375 participants) differed compared with multi‐component interventions (SMD ‐0.41, 95% CI ‐0.76 to ‐0.05; I2 = 0%; 3 studies, 132 participants) (Analysis 2.19; test for subgroup differences Chi2 = 0.10; df = 1, P = 0.76, I2 = 0%; very low‐certainty evidence). The multiple‐component interventions included both psychological and service system approach components (Berry 2021; Grote 2012; Grote 2015), while the single‐component interventions included only psychological interventions (Ammerman 2016; Blalock 2013; Madigan 2015; Silverstein 2011; Upshur 2016).
2.19. Analysis.

Comparison 2: Psychological interventions vs inactive control, Outcome 19: Psychological interventions vs inactive control, Outcome 2: Psychological wellbeing (continuous data), at post‐intervention, subgroup (multiple component interventions)
For the comparison of psychological interventions versus inactive control on number of parents achieving remission from depression, there was no evidence that the magnitude of effect estimates for single‐component interventions (RR 1.11, 95% CI 0.59 to 2.10; 1 study, 38 participants) differed compared with multi‐component interventions (RR 0.98, 95% CI 0.79 to 1.22; 1 study, 78 participants) (Analysis 2.20; test for subgroup differences Chi2 = 0.13, df = 1, P = 0.72, I2 = 0%; moderate‐certainty evidence). The types of multiple‐component intervention included both psychological and service system approach components (Grote 2015 ), while the single‐component intervention included only psychological intervention (Silverstein 2011).
2.20. Analysis.

Comparison 2: Psychological interventions vs inactive control, Outcome 20: Psychological interventions vs inactive control, Outcome 2: Psychological wellbeing (dichotomous data), at post‐intervention, subgroup (multiple component interventions)
The certainty of all the subgroup analyses was compromised because different trials contributed to the subgroups, and few trials contributed to each of the subgroups, making these analyses susceptible to confounding bias (Schandelmaier 2020; Thompson 2002).
Discussion
Summary of main results
We synthesised the reported evidence on the effects of interventions to support soon‐to‐be and new parents experiencing CPTSD symptoms or who have experienced maltreatment in their own childhoods. CPTSD has only relatively recently been formally recognised as a distinct condition in ICD‐11 (WHO 2019), and we anticipated that very few studies would have been published to date that assess interventions targeting CPTSD or assessing associated symptom‐related outcomes. We therefore also searched for studies aimed at supporting parents who have experienced childhood maltreatment as this is the most common antecedent to the development of CPTSD symptoms (Agazzi 2019; Frost 2020). As anticipated, most eligible studies were not targeting CPTSD but aimed to improve parenting capacity or parental psychological or socio‐emotional wellbeing in parents considered at higher risk of poor parenting outcomes due to a range of factors, including the experience of childhood maltreatment, or PTSD. The results should be interpreted within this context of an evolving evidence base.
Results from the 15 studies included in this review of interventions delivered during pregnancy or up to two years after birth to parents who were experiencing CPTSD symptoms or had experienced childhood maltreatment provide little or no evidence of benefit compared to usual care on most of the measured parenting and psychological outcomes. However, two parenting interventions led to small improvements in parent‐child relationships (Pasalich 2019; Steele 2019): one study that assessed a psychological intervention that comprised an interpersonally focused therapy, cognitive behavioural analysis system of psychotherapy, found a small increase in the number of mothers who quit smoking (Blalock 2013); another psychological intervention improved parent relationships and parenting skills (Ammerman 2016). Additionally, one service system approach showed that providing financial empowerment education and trauma‐informed peer support resulted in a slight increase in depression symptom severity (Booshehri 2018). Dropout rates from the included parenting and psychological intervention studies did not differ between intervention and control groups, indicating good parent acceptability of the interventions. Dropout rates were relatively high, but this is expected in studies with populations experiencing high adversity and with parenting responsibilities. In the service system intervention study parent acceptability (as indicated by dropout) was low, with more parents failing to complete the financial empowerment intervention than the control.
Heterogeneity or variation between studies combined in meta‐analyses for primary outcomes post‐intervention was mixed, ranging from I2 = 0% in parenting interventions on parenting skills in (four studies), to moderate (I2 = 39%) in psychological interventions on CPTSD symptoms (four studies), to high (I2 = 60% and I2 = 63%) in effect of parenting interventions on parent‐child relationships (two studies), and psychological interventions on depression (eight studies), respectively. Overall, we generally rated the certainty of the evidence from the included studies as low to very low, providing little certainty in most of the results.
Parenting interventions
Primary outcomes
Results of a study assessing the effect of the 'Mom Power' parenting intervention on PTSD symptoms and psychological wellbeing (33 participants) were very uncertain. Parenting interventions (PFR, GABI) were found to improve relationships between parents and their children slightly (two studies, 153 participants); however, certainty in the evidence was low, and both studies targeted mothers who were considered 'at risk' of maltreating their child. Results of another study of parents who were identified as maltreating their child (104 participants), which assessed the effect of two interventions, Infant Parent Psychotherapy, and Psychoeducational Parenting Intervention, on attachment, were very uncertain.
Results suggested that there may be no benefit from parenting interventions (Mom Power, emotional support and coaching intervention, FIND, GABI) on parenting skills, including nurturance, supportive presence and reciprocity, however there was low certainty in this evidence (four studies, 149 participants). Excluding three studies with fewer than 50 participants increased the effect to indicate a small improvement in parenting skills, however the one remaining study was at high risk of bias and there was low certainty in the result.
Subgroup analysis indicated that there was no evidence that the magnitude of effect estimates for multi‐component interventions that incorporated service system approaches into parenting interventions differed compared with single component psychological interventions.
Secondary outcomes
There was little or no difference in parent engagement, measured by dropout from treatment, between intervention and usual care groups in the parenting intervention studies (six studies, 918 participants).
Interventions including a video feedback parenting intervention (FIND), Infant Parent Psychotherapy and Psychoeducational Parenting Intervention, resulted in little or no difference in child externalising or internalising behaviours or child behaviour problems, either immediately or 12 months after the intervention compared to usual care.
There was little difference between the Mom Power parenting intervention that incorporated service system approaches, and attention control, on changes in parental social capital outcomes (perceived connection to community professionals).
Psychological interventions
Primary outcomes
There may be little or no difference between psychological interventions and usual care in CPTSD symptoms, including PTSD symptoms, dissociation or interpersonal problems (four studies, 247 participants; low‐certainty evidence). Evidence for the effect of a psychological intervention (trauma‐focused CBT (TF‐CBT)) on PTSD diagnosis was very uncertain. Evidence suggested that psychological interventions may have little benefit over usual care for: depression symptoms (eight studies, 507 participants), the number of parents achieving remission from depression, or experiencing depressive episodes three to four months post‐intervention (two studies, 116 participants), however the certainty in this evidence was low. When we excluded one study at high risk of bias, a small, important decrease in depression symptoms was found in intervention compared to control groups. Our subgroup analysis on the psychological wellbeing (depression) outcome found that there was no evidence that the magnitude of effect estimates for multi‐component interventions differed compared with single‐component psychological interventions
One study assessing an interpersonally focused depression intervention, cognitive behavioural analysis system of psychotherapy (CBASP), in a sample of pregnant women with a history of moderate‐severe levels of childhood maltreatment, found a slight increase in the number of women who stopped smoking compared to usual care, however there was low certainty in this evidence.
One study found slightly more benefit from a psychological intervention compared to control for parent's relationship and another found that a psychological intervention was slightly better that usual care for improving parenting skills, providing a stimulating, nurturing and safe environment, however there was low certainty in this evidence.
The effect of a psychological intervention (TF‐CBT) on the number of parents with disorganised infant attachment was very uncertain.
Secondary outcomes
There was little to no difference in parent engagement (dropout) between psychological intervention groups and usual care (seven studies, 926 participants). Little or no difference was found between psychological interventions and control groups on social functioning outcomes (social support) (four studies, 240 participants). One small study (14 participants) that assessed the effect of a psychological intervention with parenting skills components (PREPP) on children's physical, socio‐emotional wellbeing found a large increase in the total minutes of daytime sleeping in the babies of mothers who received the intervention compared to an enhanced usual treatment group, however due to very wide CIs and the very small sample size, the results are very uncertain and replication of these results would be desirable.
Primary outcomes
Service system approaches were found to possibly increase depression symptoms (one study, 52 participants, low‐certainty evidence) compared to usual care. This worsening of symptoms was no longer evident at six months (53 participants), and at nine‐month follow‐up there was a small decrease in depression symptoms (46 participants), however over half of the randomised participants had dropped out at these latter time points, providing little confidence in the findings.
This study also assessed parental self‐efficacy and the service system approach was found to have a small to moderately beneficial effect compared to usual care at post‐intervention, which reduced across the follow‐up time points but remained important (low‐certainty evidence).
Secondary outcomes
Parent engagement was slightly poorer in the service system approach compared to usual care (one study, 103 participants). Little or no difference was found between intervention and usual care groups in economic hardship at post‐intervention: a small beneficial effect was reported at six‐month follow‐up, which was unsustained at nine‐month follow‐up, however with over 50% participant dropout, these results should be interpreted with strong caution. Child developmental risk was slightly reduced compared to usual care in the service system approach post‐intervention (one study, 52 participants), however CIs consistent with important benefit and important harm provide low confidence in this result. At six months, child developmental risk was slightly increased in the intervention group, and it was greatly increased at nine months, however wide CIs and high rates of dropout make these results uncertain.
Overall completeness and applicability of evidence
The overall completeness and applicability of the findings are limited by a number of important factors. While there is a larger body of evidence assessing the effect of psychological interventions on mental health outcomes in women with childhood maltreatment histories, the evidence for these interventions in pregnant women or parents in the perinatal period is limited.
Study interventions
In a critical interpretive synthesis review of interventions to prevent the transmission of intergenerational trauma, Isobel et al found that the complexities of identifying intergenerational trauma as distinct from other psychological trauma limited the ability to clearly articulate relevant interventions (Isobel 2018). The rationale for the five intervention categories we sought to include in this review was grounded in the findings of our previous scoping review (Chamberlain 2019b), and qualitative systematic reviews of parent's experiences (Chamberlain 2019c). The findings of these reviews highlighted the diverse range of parent preferences and needs for prenatal care interventions, and the importance of choice. However, the range of interventions that have been studied in RCTs and included in this review are limited. In line with Isobel 2018, which concluded that resolving parental trauma and supporting parent‐infant bonding were key prevention constructs, we found that interventions categorised as psychological or parenting interventions were the most common.
Interventions identified as useful by parents in these previous reviews included those promoting connectedness and fostering positive relationships with self, children and others. A number of the reviewed interventions go some way to addressing this need. For example, all six parenting interventions included components aimed at enhancing relationships between child and parent and four of these specifically promoted positive relationships with oneself and others. Infant Parent Psychotherapy aimed to assist parents to develop positive internal representations of themselves, and themselves in relationship to others (Cicchetti 2006); a key focus of the interpersonal relationship‐focused CBASP intervention was improving the quality of mother's relationships with significant others (Blalock 2013); PFR aimed to improve parent's awareness of their own needs in addition to their child's (Pasalich 2019); and Mom Power promoted a healthy relationship with self (Rosenblum 2017).
Another strategy identified by parents in our qualitative review was "creating safety, using conscious strategies to build safe places and relationships to protect themselves and their baby" (Chamberlain 2019c, page 40). Four of the interventions reviewed here include safety as a core component: Seeking safety emphasises safety and focusses CBT elements on solving current problems and not exploring past trauma (Upshur 2016); the PFR model (Pasalich 2019) posits that improvements can only be achieved by first establishing a parent's own feelings of safety and security (Crittenden 2017; Graybeal 2007; Larrieu 2004; Oxford 2016); similarly, Mom Power seeks to establish an environment of "felt security and nurturance" in the group component, facilitating mother's provision of a "safe haven and secure base" (Bowlby 1969) for their children (Rosenblum 2017); and finally, CBASP seeks to motivate behaviour change (smoking cessation) through generating felt safety within the therapy dyad, with the aim to generalise this felt safety to the mother's other relationships (Blalock 2013).
We also examined recommendations for supports for parents in relevant national guidelines and key reviews (Austin 2017; DOH 2020; Bisson 2020; Bisson 2021; Caro 2019; Erickson 2019; Johnstone 2018; Kezelman 2012; Kezelman 2019; Law 2019; Lewis 2020; Phoenix Australia 2020; Sánchez‐Meca 2011). Through the synthesis of the interventions reviewed within these sources we developed the five intervention categories to cover the diverse range of implementation contexts: mind‐body approaches; pharmacological treatment; psychological interventions; parenting interventions and service system approaches.
However, we found no studies assessing the effect of two of our five pre‐specified intervention categories, with no eligible studies assessing the effects of mind‐body approaches, or pharmacological approaches delivered during pregnancy or up to two years after birth for parents who are experiencing CPTSD symptoms or have experienced childhood maltreatment. This dearth of studies across two core intervention categories highlights a gap in the evidence base.
Mind‐body approaches
The evidence base for the effect of mind‐body approaches such as mindfulness, art therapy and yoga, and biomedical approaches such as neurofeedback for individuals with prior trauma exposure, is growing. The Australian PTSD guidelines identify a number of mind‐body approaches and biomedical approaches with emerging evidence for interventions that warrant further research, however none have been assessed in a population of parents with complex trauma and/or childhood maltreatment history (Phoenix Australia 2020).
Pharmacological treatments
Evidence supports the use of pharmacological treatments for PTSD in the general population. Selective serotonin reuptake inhibitors (SSRIs) and venlafaxine both have conditional recommendations in the Australian PTSD guidelines (Phoenix Australia 2020), for use when an individual is unwilling or not in a position to engage in or access recommended psychological therapy (TF‐CBT, Prolonged Exposure (PE), Cognitive Therapy, Cognitive Processing Therapy (CPT) or EMDR), where they have comorbid conditions or associated symptoms where the medications are indicated, or where psychological therapies have not reduced their symptoms. No studies have assessed the effectiveness of these medications specifically in populations of parents with childhood maltreatment histories or with CPTSD symptoms.
Within the prespecified categories of interventions that we did find studies assessing, psychological interventions, parenting interventions and service system approaches, the types of interventions were limited.
Parenting interventions
The six studies we identified that assessed parenting interventions included five parent‐child interventions, and a single social‐support‐based intervention. Social support has been shown to be a critical moderating factor for enhancing parent‐child relationships (Green 2007). The positive influence of social support on parental self‐efficacy and positive parenting practices has been shown in a range of populations including low SES immigrant families (Izzo 2000) and African American single mothers with high environmental stressors and psychological distress (Kotchick 2005). No studies were found that assessed family‐ or couple‐focused interventions. These were identified our scoping review as an effective strategy for improvements in parenting and evidence suggests that couples and family based interventions may improve parental wellbeing and increase positive parenting outcomes (Bellhouse 2021; Morrill 2016). More studies of these types of parenting interventions are needed to build the evidence base for this category of interventions.
Five of the six studies assessing parenting interventions were aimed at parents who were considered at risk of or had been identified as maltreating their own children. There is an evidence gap in studies assessing the effectiveness of parenting interventions in parents with symptoms of CPTSD or childhood maltreatment histories that are targeting parental healing or recovery from trauma rather than solely prevention of child maltreatment. Growing evidence demonstrates that the perinatal period offers a unique life course opportunity for preventing intergenerational cycles of trauma, through supporting positively reinforcing cycles of nurturing and recovery, and 'earned security' (Alexander 2014; Sperlich 2017).
Additionally, all the included parenting studies were implemented in the postpartum period; studies of interventions initiated in pregnancy are missing from the literature. Conversely, seven of the eight studies assessing psychological interventions targeted parents who were pregnant, limiting generalisability of these findings to parents in postnatal parenting stages. This paradox reflects a disconnect between 'parenting' and 'psychological' interventions to support parents experiencing CPTSD symptoms, and points to the need for better integration of more holistic parenting and mental health support during the perinatal period.
Psychological interventions
Within psychological interventions we identified eight studies. Six of these studies assessed the effectiveness of non‐trauma focused CBT‐based interventions, one assessed trauma‐focused CBT (Madigan 2015), and one assessed an intervention that included parenting skills as well as psychological components such as motivational interviewing and mindfulness exercises (Berry 2021). Evidence‐based psychological approaches to treating trauma‐related symptoms include PTSD treatments such as PE, CPT, EMDR, Narrative Exposure Therapy (NET) and Dialectical Behavior Therapy (DBT). There is a large body of evidence examining the effectiveness of these therapies for other trauma‐affected populations (current and ex‐serving military members, assault and rape survivors), and so it is surprising that studies specific to assessing the effect of these interventions on parents with CPTSD symptoms or childhood maltreatment have not been conducted.
Service system approaches
Only one type of service system approach was included: a financial empowerment programme with a trauma‐informed peer support component. This highlights a gap in the types of interventions assessed in this important area. A range of service system approaches identified in our protocol, informed by our previous scoping and qualitative reviews, were not represented in the literature. These interventions were identified as desired and appropriate by parents and by what evidence from other fields suggest may be beneficial for this population.
Study setting
Another limitation to the applicability of the findings is the generalisability to other geographical contexts. All studies were conducted in one region, North America; 14 of the 15 included studies were conducted in the USA, with one conducted in Canada, and the majority (10 studies) were conducted in metropolitan settings. Two of the three identified ongoing studies are also set in the USA. Studies in different settings including low‐ and middle‐income countries and rural and remote locations are needed.
Study population
The exclusion criteria within studies included in the review present a further limitation on the generalisability of the findings, due to the common exclusion of people with conditions that frequently co‐occur with the experience of childhood maltreatment and/or CPTSD symptoms. Four of the eight studies assessing psychological interventions excluded parents experiencing substance use issues, or in receipt of other treatments or medications, while six of eight studies excluded parents with any psychiatric disorder. All but one study assessing psychological interventions excluded parents with suicidal risk (four studies) or ideation (three studies). Studies assessing parenting interventions were more inclusive with only a single study excluding parents based on experience of a psychiatric or organic mental health disorder. Exclusion of parents with mental health or psychiatric symptoms, including substance abuse, greatly limits the generalisability of the findings to those with symptoms of CPTSD and/or childhood maltreatment histories. There is a well‐established body of evidence indicating that childhood maltreatment is strongly associated with mental health and psychiatric conditions including psychological distress, mood disorder, psychosis, suicidal ideation or attempt and substance use disorders (Anda 2006; Bellis 2019; Felitti 1998; Petruccelli 2019; Sahle 2021; Varese 2012).
Five studies were specifically targeted at mothers experiencing mental health disorder (depression, three studies: Ammerman 2016; Grote 2012; Grote 2015; or PTSD, two studies: Madigan 2015; Upshur 2016). Parents in these studies would likely have started at higher baseline levels on these outcomes and may be more likely to experience treatment resistance.
Very few studies included male parents (29 participants, three studies; Booshehri 2018; Liu 2021; Pasalich 2019), limiting the generalisability of the review's findings to fathers. Twelve studies included a majority of parents with low SES, limiting generalisability to parents with moderate‐high SES.
We only included studies where experience of childhood maltreatment exposure was reported, and this was assessed with self‐report measures in most studies. Literature suggests that many individuals never disclose experiences of childhood maltreatment (Bottoms 2007; London 2005; London 2008; Finkelhor 2014; Smith 2000; Somer 2001), and those who do, disclose between 3 and 49 years after the experience/s, with an estimated average latency of 21 years (Jonzon 2004; Kogan 2004). It is probable then, that the participants in the included studies are not fully representative of broader childhood maltreatment‐exposed population as the represented individuals have selected to participate in a study addressing trauma impacts and have disclosed previous trauma.
Taken together these limitations to generalisability suggest that the results presented in this review are most applicable to mothers over 18 years, with low SES, from metropolitan settings in high‐income countries, who have disclosed experiences of childhood maltreatment.
Study outcomes
There was wide variation in the outcomes measured, limiting our ability to synthesise effects for many of the primary outcomes. Some of our primary outcomes were assessed in only one or no included studies, highlighting an evidence gap. Long‐term follow‐up was only reported in six studies, all of which reported different outcomes and thus the sustainability of any intervention effects cannot be accurately predicted. Adverse effects were not reported in any of the studies, although a possible negative effect on depression was reported in one study offering financial empowerment and peer group counselling, with concurrent possible positive effect on parenting self‐efficacy. Considering the sensitive nature of identifying and addressing issues related to a past history of childhood maltreatment, there is potential for any intervention, particularly those that are trauma‐focused, to cause some distress and potentially cause harm. This can include triggering of trauma‐related distress, inappropriate attention from child welfare agencies and 'labelling' parents as at risk (Chamberlain 2019a). This is an important outcome that should be considered in future research in addition to our other primary outcomes that were inadequately addressed: parental substance use, parental self‐harm and parent relationship quality. Qualitative (Chamberlain 2019c) and neurophysiological (Piccini 2021) studies suggest that 'hope‐inspiring' and strengths‐based approaches that focus on unique opportunities at this time and reframe the discourse of CPTSD and childhood maltreatment as described in the Power Threat Meaning Framework (Johnstone 2018) are important for parents who have experienced maltreatment in their own childhoods, and may help to reduce these risks.
The sample sizes in the included studies were small, reducing the certainty of treatment effects. Studies with larger sample sizes are needed, however the feasibility of larger sample sizes in these populations is challenging.
Only two studies reported costs or cost‐effectiveness as outcomes. This is a significant gap given the well‐documented impact of childhood maltreatment or adverse childhood experiences on adult health outcomes, including parenting and intergenerational transmission of trauma (Bellis 2019; Font 2016). There is enormous potential for any effective intervention to have significant benefits for infants at a critical period of development, parents who are predominantly young, and for other children and family members, hence having potential for significant returns on investment and cost‐effectiveness. Indeed, those studies that did present cost‐effectiveness data found psychological interventions (IH‐CBT, MOMCare) to be more cost‐effective than standard care for low‐income mothers experiencing depression (Ammerman 2016), and mothers with comorbid depression and PTSD (Grote 2015).
Our search strategy required studies to have trauma‐related terms in the title or abstract. It is possible, but unlikely, that some eligible studies were missed that assessed relevant interventions and, by nature of the study population, had high proportions of participants with childhood maltreatment or CPTSD symptoms, which subgrouped results by trauma exposure, or that examined the moderation of results by trauma exposure.
There is insufficient evidence at this stage to support the effectiveness of any interventions included in this review, due largely to small sample sizes, wide variability in study design and inconsistent findings.
Quality of the evidence
We used the GRADEpro Guideline Development tool to assess the certainty of the evidence (GRADEpro GDT). GRADE assessments were based on risk of bias, inconsistency, indirectness, imprecision and publication bias. We judged all outcomes to be low (eight outcomes) or very low (three outcomes) certainty. We downgraded the majority of outcomes due to serious or very serious risk of bias and imprecision. There were several common methodological concerns contributing to the majority of the downgrades for risk of bias. Many studies did not adequately describe allocation concealment. A large proportion of the studies experienced high study attrition, and therefore had amounts of missing outcome data that could bias effect size, which may reflect the complexities of conducting research in this field. Additionally, self‐reported outcome measures were the most frequently used tools, preventing the ability for outcome assessors to be blinded. Decisions to downgrade due to imprecision were based on the width of the CIs. We downgraded six outcomes by one level due to the fact that the CIs included both a 'little or no effect' and 'appreciable harm' or 'appreciable benefit'. We downgraded a further three outcomes two levels for imprecision due to the CIs crossing the threshold for both 'appreciable harm' and 'appreciable benefit'. We downgraded one outcome by two levels for imprecision due to very low number of events (five) and wide CIs. No outcomes were downgraded for inconsistency or indirectness.
We ran sensitivity analyses on four outcomes, excluding studies at overall high risk of bias. Two of these analyses yielded results similar to the primary results. However, the sensitivity analyses conducted on the comparison of parenting interventions versus inactive control for the outcome parent‐child relationship yielded a result that shifted the effect size from 'appreciable benefit' to 'little or no benefit', suggesting that this finding may be vulnerable to risk of bias. After excluding outcome data from three studies at high risk of bias from the comparison of psychological interventions versus inactive control for the trauma‐related symptoms outcome, the one remaining study showed a small benefit, however the certainty of evidence is very low.
We ran sensitivity analyses on three comparisons, excluding outcome data from studies with sample sizes of fewer than 50 participants. While two of these analyses resulted in no important change in effect, the comparison of parenting interventions compared to usual care for the outcome parenting skills post‐intervention showed a shift from 'little or no benefit' to 'appreciable benefit' when outcome data from three studies with fewer than 50 participants were excluded. This may be a spurious effect or could suggest that outcome data from smaller studies are at risk of biasing results towards the null.
Publication bias was not assessed with a funnel plot due to an inadequate number of studies (fewer than 10) in any single comparison to assess asymmetry. However, we searched clinical trial databases for any missing data from terminated, ongoing or unpublished eligible studies.
Potential biases in the review process
We conducted this review in accordance with the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2022). We made every effort to limit bias through the use of a rigorous comprehensive search strategy of multiple databases. We completed a handsearch of included studies and searched the references of 216 reviews to identify any additional eligible studies. We contacted study authors for any missing data and to request subgroup data of parents with CPTSD symptoms or who had experienced childhood maltreatment. Although eight of the 11 author groups provided unpublished subgroup data, we were unable to obtain the subgroup data from two studies and the unadjusted data from one study.
Levels of exposure to childhood maltreatment varied across studies; seven studies provided either published or unpublished data for a sample of parents who had experienced moderate‐severe/high trauma exposure as measured on validated scales using established cut‐off scores. Seven studies included any/at least one trauma exposure. In studies where we used a subsample of participants with moderate‐severe/high trauma exposure, we compared the effects reported in the published reports for the full sample and our effect size for the high trauma‐exposure sample. We found no important differences for any effects suggesting that studies including any trauma exposure did not dilute the effect of interventions for parents with higher levels of trauma‐exposure.
There was considerable heterogeneity in the control arms of the included studies. Fourteen studies used a 'usual care' or attention matched control comparison group. Several studies described early intervention and parenting programmes that involved multidisciplinary, in‐home supports that were considered routine in the 'high risk' study population but were more intensive than other usual care comparator arms that, for example, provided referrals and a small amount of psycho‐education. We combined the usual care control arms for use as a comparison to experimental interventions, despite this heterogeneity, as they represent an inactive control for the intervention and the small number of included studies prevented a more nuanced analysis. Heterogeneity in usual care intensity may potentially lead to biased estimates of intervention efficacy. Intensity of usual care may potentially dilute experimental intervention effects in studies where usual care involves intensive and complex support strategies compared those that used a low‐intensity usual care control group.
Agreements and disagreements with other studies or reviews
To the best of our knowledge, there has been one systematic review of psychological interventions and no reviews on parenting interventions delivered during the perinatal period for parents experiencing symptoms of CPTSD or who have experienced childhood maltreatment.
Systematic reviews of psychological interventions for parents with trauma histories
A systematic review of six studies assessed the impact of maternal childhood trauma on the effectiveness of psychological interventions for depression during pregnancy and the postpartum period (Reuveni 2021). Four of the six studies are included in our review (Ammerman 2016; Blalock 2013; Grote 2012; Grote 2015), one was excluded as it included parents without symptoms of CPTSD or childhood maltreatment, and another was ineligible for our review as it was an open trial. IPT‐based interventions were found to improve depression treatment outcomes, with the severity of childhood maltreatment corresponding to longer time to remission. There was limited evidence for CBT with only one study of high quality, which found significant improvements in depression symptoms that were not moderated or predicted by severity of childhood maltreatment. Thus, the conclusions from Reuveni 2021 are not in agreement with the findings of our review, which found no evidence for improvement in depression symptoms in a meta‐analysis of eight studies. This difference may be accounted for by the additional studies we included. The studies with positive effects on depression outcomes in Reuveni 2021 are all included in our meta‐analysis and show small, important effects on depression, however when assessed in the context of the other RCTs with comparable psychological interventions, the overall body of evidence in our review does not support the effectiveness of the interventions. Notably, we found that exclusion of the one intervention at high risk of bias in our review shifted the effect to a small, important benefit for depression symptoms, so it is possible that the difference in the review finding is due to our results being influenced by one study at high risk of bias. This study was also the only trauma‐focused study included in our review, raising questions about the effect of trauma‐focused treatments in this population, however there is too much uncertainty in the current evidence to have confidence in the results. We hope, in future updates, to have sufficient evidence from different types of psychological interventions to allow subgrouping by more specific intervention domains and a more nuanced review of the available interventions. The authors agree with our conclusion that there is an overall paucity of evidence and further research into trauma‐informed psychological interventions for postpartum depression is needed to meet the needs of this population.
No other reviews have systematically assessed the effect of psychological interventions on the other primary outcomes of this review, including other aspects of parental psychological wellbeing (e.g. CPTSD) or parenting capacity, in parents with symptoms specific to CPTSD or who have experienced childhood maltreatment, in the perinatal period. Two reviews, which assessed psychological interventions for parental psychological wellbeing during pregnancy and the postpartum period in populations that had experienced other or unspecified trauma or with PTSD symptoms (not specific to CPTSD or childhood maltreatment history) (Baas 2020; Stevens 2021), and another that reviewed studies assessing interventions for psychological wellbeing in parents with symptoms of psychological disorders (Nillni 2018), can provide some interesting comparisons, however.
Systematic reviews of psychological interventions for parents without identified trauma histories or symptoms
A systematic review of 78 studies identified a range of interventions assessed in studies of parents with diagnosable or subthreshold levels of depression, anxiety and trauma‐related disorders during the perinatal period (Nillni 2018). Evidence from 30 studies, including 21 RCTs, suggested a significant improvement in postpartum depression symptom severity for parents completing CBT or IPT interventions. For example, CBT‐based interventions reduced anxiety and depression symptoms in mothers with anxiety disorders, and PTSD and depression symptoms in parents with trauma‐related disorders. Two studies were common to our review (Grote 2012; Grote 2015). Findings from 11 studies that assessed interventions specifically targeted at mothers with mental health symptoms, who were also from low‐income and/or from ethnic minority populations, were less conclusive; two studies reported a significant improvement in depression outcomes after CBT, and the third reported a trend towards a difference between CBT and usual care. IPT reduced depression symptoms in three studies and had no benefit in two others, and studies of other 'talk' therapies (e.g. reflective listening, problem‐solving and a collaborative care model) reported significant reductions in depression symptom severity (Nillni 2018).
Systematic reviews of psychological interventions for pregnant women experiencing symptoms of PTSD
A more recent systematic review assessed the effectiveness of psychological interventions for PTSD symptoms in pregnant women exposed to trauma including previous childbirth (three studies), obstetric procedure (one study) or abuse (childhood maltreatment, physical or sexual) (nine studies) (Baas 2020). Two RCTs in populations with childhood maltreatment were common to our review (Madigan 2015; Upshur 2016). Improvements in PTSD symptom severity were found after EMDR and CBT (case studies), TF‐CBT (one cohort study), Seeking Safety (one RCT) and Survivor Moms Champion (two quasi‐experimental studies). However, most studies had low methodological quality and lacked a comparator arm.
Another recent review identified six studies of psychological interventions for mothers with prenatal PTSD (Stevens 2020), including one common to our review (Upshur 2016). Similar to Baas 2020, Stevens 2020 found preliminary evidence for the effectiveness of Seeking Safety and Survivor Moms Companion in reducing parental PTSD symptom severity. Stevens 2020 also identified one study assessing an evidenced‐based intervention for PTSD, IPT integrated within a primary care model. IPT was found to be a feasible and acceptable model of care, and although it reduced PTSD symptoms compared to usual care, it did not significantly reduce symptom severity during the postpartum period nor significantly reduce the likelihood of a PTSD diagnosis during pregnancy. No studies in perinatal populations were identified that assessed other guideline recommended interventions for PTSD, such as PE and CPT.
Systematic reviews of parenting interventions in parents with childhood maltreatment exposure or trauma symptoms
While a range of systematic reviews have assessed the evidence for the effectiveness of early parenting interventions for the general population (Jeong 2021; Mihelic 2017; Morrison 2014; Pontoppidan 2016), parents with low SES (Harris 2020), adolescent parents (Barlow 2011), parents of children with diabilities (Hohlfeld 2018; Whittingham 2011), parents of children with chronic illness (Mitchell 2020) or behavioural problems (Dretzke 2009), and parents with depression symptoms (Rayce 2020), to our knowledge no reviews have assessed the effect of parenting interventions in parents with childhood maltreatment exposure or CPTSD symptoms.
Alignment with the findings of this review
Taken together, the findings from previous systematic reviews of interventions similar to those assessed in this review for parents in the perinatal period do not fully align with our findings. The reviews detailed above generally found positive effects on psychological wellbeing outcomes such as depression and PTSD symptoms, whereas we found little or no effect. The most likely explanation for this disagreement is due to our focus on parents with trauma symptoms and/or childhood maltreatment histories. Indeed, due to this important difference, in addition to their inclusion of studies designs of low methodological rigour (open trials, case series, cohort studies), it is difficult to draw parallels between Nillni 2018, Baas 2020, Stevens 2021 and the current review. However, the lack of beneficial effects evidenced in our review of interventions in parents with trauma histories, in light of the findings from previous reviews that similar interventions were beneficial in parents with mental health symptoms, provides further support for the suggestion that parents with childhood maltreatment histories experience higher levels of distress and greater treatment resistance (Ammerman 2016; Chapman 2004; Nanni 2012). It also reinforces the need for caution with trauma‐focussed approaches and the need to consider issues raised by the British Psychological Society (Johnstone 2018), neurophysiological studies (Piccini 2021) and qualitative studies of parents' views (Chamberlain 2019c). Nillni 2018 suggests that the reduced strength of intervention effects in studies that targeted low‐income and ethnic minority women reflects specific barriers to care and that more research is needed into engaging these women in care. It also raises important concerns about the study attrition reported in the studies included in our review and provides further evidence for the problem of treatment engagement in parents facing adversity and complex issues. Evidence also suggests that complex trauma symptoms are more difficult to treat than non‐complex trauma symptoms (Karatzias 2019).
Systematic reviews of psychological interventions for PTSD in people with CPTSD symptoms or childhood maltreatment histories
Evidence for interventions to treat PTSD in people with childhood maltreatment histories or CPTSD symptoms is emerging, but remains very limited amongst populations of pregnant women. One meta‐analysis assessed the evidence from 16 RCTs of psychological interventions (TF‐CBT, non‐TF‐CBT, EMDR, group interpersonal therapy, emotion‐focused therapy) for PTSD in adults (primarily women, not pregnant) who had experienced childhood maltreatment (Ehring 2014). Results suggested improved psychological wellbeing outcomes. Trauma‐focused interventions demonstrated the greatest efficacy, and individual therapy resulted in greater symptom reduction than group therapy, however the methodological quality of the evidence was low. A more recent meta‐analysis of 51 RCTs, assessing the effects of interventions targeting PTSD in any population where participants were likely to have CPTSD symptoms, supported these findings, reporting that while trauma‐focused interventions were effective, the reduction of symptoms was less pronounced in people who had experienced childhood trauma (Karatzias 2019).
Recent RCTs of psychological interventions for PTSD in people with CPTSD symptoms or childhood maltreatment histories
Several recent RCTs have assessed trauma symptoms at longer time points to assess the effects of trauma‐focused interventions in people with childhood maltreatment histories over extended intervention protocols. PE, intensified prolonged exposure (iPE) and Skills Training in Affective and Interpersonal Regulation + PE (STAIR+PE) were all found to be effective in reducing PTSD symptoms at 12‐month follow up in an RCT of 149 participants with PTSD related to childhood maltreatment (Oprel 2021). Another recent RCT (Hoeboer 2021; 149 participants) highlighted that participants with complex PTSD experienced greater baseline PTSD symptom severity than those with (non‐complex) PTSD, but they showed a similar reduction in PTSD symptoms at 12 month post‐intervention, suggesting that people with complex PTSD require more intervention sessions rather than different interventions. And finally, two recent RCTs showed that DBT or CPT delivered over 12 months (Bohus 2020; 193 participants) and a developmentally adapted DBT (Eilers 2021; 44 participants) were effective in reducing CPTSD symptoms in women with severe childhood maltreatment experiences and CPTSD, and adolescents with probable CPTSD respectively. Thus evidence supports the use of trauma‐focused interventions following childhood maltreatment and for CPTSD, and suggests that longer protocols are required to reach adequate reduction in trauma‐related symptoms. While our review findings found little or no benefit of psychological interventions for PTSD symptoms, the evidence was of low certainty, three of the four included studies were non‐trauma‐focused, and intervention protocols were mostly eight sessions across two to three months. Studies of trauma‐focused interventions and longer intervention protocols are needed to determine whether the beneficial effects of longer TF‐CBT‐based interventions that have been found in other populations with CPTSD and childhood maltreatment are generalisable to parents with similar adverse experiences. Further research is needed in this emerging field to determine whether differential effects may be found in a population of parents in the perinatal period.
Authors' conclusions
Implications for practice.
This review has provided a summary of the existing RCTs assessing interventions for parents with childhood trauma history or CPTSD symptoms. Due to a lack of methodological rigour in the included studies, caution is advised in interpreting the results. There is a high degree of uncertainty in the findings, lending little confidence to the results and the balancing of potential benefits and harms should be considered in this context.
There is very little certainty in the evidence for the effects of parenting interventions on outcomes that are important to parents. Safe, stable, nurturing parent‐child relationships have been shown to moderate negative effects of maltreatment and protect against the intergenerational cycles of child maltreatment (Britto 2017; Schofield 2013). Our results suggest that while a small number of parents may experience improvement in aspects of their relationship with their child as a result of parenting interventions, most parents may experience no change in these outcomes. Decision makers should consider this in context with the feasibility, cost of implementation and any potential harm associated with delivery of an ineffective intervention to parents, balanced with the potential for a small number of parents to gain small to large improvements in parent relationship with their child.
The assessed interventions may have little or no benefit for CPTSD symptoms in parents with maltreatment histories. There is a need for further studies into different types of interventions to address complex trauma symptoms in this population.
While psychological interventions were found to result in little or no improvement in psychological wellbeing, a sensitivity analysis indicated that the effect may have been influenced by studies at high risk of bias, which had the effect of biasing the result towards favouring usual care. Psychological interventions may result in a slight improvement in psychological wellbeing or in no change. Decision makers should consider the risk associated with delivering ineffective interventions to parents, and the fact that alternative, potentially effective interventions may be forsaken, and balance these with the benefits for a potential small number of parents who may achieve small but important reductions in depression symptoms and the longer‐term impacts for these effects. These decisions should also take into account parent's baseline risk, comorbidity and symptom burden, and their previous treatment history when making decisions at an individual level.
An interpersonally focused CBT intervention may help some women with childhood trauma experiences to stop smoking in pregnancy. While the increase in cessation may be small, the longer‐term benefits associated with this should be considered when making treatment and care decisions.
Parents' relationships and parenting skills were both improved slightly more in participants who received a psychological intervention (In‐Home Cognitive Behavioural Therapy) compared to those who received standard home visiting in one study. These results should be considered within the context that a small number of parents may benefit from this psychological intervention, while most parents will experience no change in their relationships or parenting skills.
Overall, the results of this review provide little certainty about the effects of the reviewed interventions, and reflect an evolving evidence base. The available evidence reviewed here indicates that parenting interventions may improve relationships between some parents and children. However, the evidence must be considered in the context of the low certainty. Similarly, psychological interventions may help a small number of pregnant women with a history of maltreatment in their own childhood to stop smoking, improve some parental relationships slightly and slightly enhance a small number of parents' parenting skills, but the reviewed interventions may not improve CPTSD symptoms and may result in little or no improvement in depression outcomes in most parents. The service system approach reviewed here may increase depression symptoms. These uncertain results must be considered with other important parent and service level factors such as individual baseline risk or symptom severity, implementation costs and the availability of resources. As such, a personalised approach to supporting parents and families with CPTSD or childhood maltreatment histories is justified. Drawing on the PTMF, when services are delivered within a trauma‐informed context emphasising safety, trust, collaboration, choice and empowerment, the risk of retraumatising parents can be reduced (Bowen 2016; Johnstone 2018; Levenson 2017). Education of service providers who support families in the perinatal period, on trauma‐informed approaches and the complexity of the effects of childhood maltreatment and CPSTD, the associated systemic adversity, the impact these experiences may have on parenting, and thus the complex effects of interventions to address these outcomes, may help ensure that ineffective or even retraumatising interventions are not delivered to this priority population.
Implications for research.
There is a need for further high‐quality research into effective strategies for parents, particularly fathers, who were under‐represented in the assessed studies. This research should draw on existing qualitative evidence outlining what parents want (Chamberlain 2019c; Reid 2021), which includes strengths approaches consistent with the PTMF (Johnstone 2018) that focus on hope and the unique opportunities for recovery (Piccini 2021), as well as what has been effective in other similar populations (e.g. women with CPTSD). Acceptability of interventions in this population is of critical importance and was lacking in the studies included in this review. A recent systematic review found that acceptability of interventions for individuals with complex trauma experiences and symptoms was greater when participants were able to identify benefits and where intervention delivery accommodated personal and social needs (Melton 2020). Individualised delivery is likely to be of even greater importance in a population of parents in the perinatal period where the demands of parenting place further limitations on individuals’ availability and flexibility. Future research should include evaluation of intervention acceptability beyond using participant dropout as a proxy, to develop a greater understanding of parents' needs for effective and sustainable intervention delivery.
While recognising the complexity of conducting real‐world intervention studies in this field, there is a need for studies to be methodologically better designed and executed. Most studies did not describe adequate allocation concealment. Most studies suffered from lack of blinding of outcome assessors due to the use of self‐report measures. Trials using clinician‐rated outcome measures are required. The estimates of effect may be biased because of a lack of concealment of allocation and a lack of blinding of the assessors of the outcome. Further, all trials should be registered to ensure transparency, to assist in avoidance of duplication and to help identify gaps in the research (WHO 2018b).
Studies involving parents who have experienced childhood sexual abuse are needed to understand if the effects of interventions differ from those in parents with other childhood maltreatment exposures and whether alternative treatments or amended intervention regimes are useful. Studies should include parents with CPTSD symptoms as the existing evidence is based on studies involving parents reporting childhood maltreatment who may or may not be experiencing CPTSD symptoms. There is a need for studies conducted in regions other than North America, including low‐ and middle‐income countries, in order to assess if the results from studies to date apply to parents in regions other than North America or high‐income countries. There is also a need to consider sub‐populations within high‐income countries, including Indigenous and migrant populations. Larger sample sizes (300 parents or more) are required. There is uncertainty in the results due to the small sample sizes in many included studies, therefore the true effect may be substantially different. Studies in males will help understand whether current evidence is generalisable to fathers.
Future studies should assess extended intervention protocols in light of the current evidence for treatment of CPTSD, which suggests that people with childhood maltreatment histories and CPTSD have higher baseline symptom levels and may require more treatment to reach an adequate dose of intervention. There is also a need to consider environmental and social systems interventions such as poverty alleviation, neighbourhood support or access to urban green spaces. Consistency in outcome reporting would greatly assist our ability to confidently synthesise the evidence. There was very little overlap in outcomes in parenting intervention studies, limiting our ability to assess overall effects.
History
Protocol first published: Issue 7, 2021
Risk of bias
Risk of bias for analysis 1.1 Parenting interventions vs inactive control, Outcome 1: Trauma‐related symptoms, at post‐intervention.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Rosenblum 2017 | Some concerns | Method used to generate random sequence is adequate, however unclear how they concealed allocation, as no details provided on who called the participant informing them of their allocation, and how that individual received allocation information: "Women were randomized using a computer‐generated algorithm (urn randomization stratified by baseline trauma exposure and depression to ensure balanced groups to either the multifamily group [treatment condition] or mailing group [control condition])." No significant differences reported between groups: "Women in both conditions were balanced on demographic, mental health and trauma variables" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | Some concerns | 36‐37% dropout (from total sample) No evidence that the results was not biased by the missing data, however no analysis method or sensitivity analysis to correct for bias Reasons for dropout are not reported, however dropout is equal between groups | Some concerns | Validated outcome measure used Same measurement and assessment time points used for all participants Measurement tool is self‐report, so participants are assessors and cannot be blinded The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Some concerns | No published protocol, however outcomes in methods section align with those in the results Insufficient detail on analysis intentions, there is likely more than one way in which the outcome measurement could have been analysed | Some concerns | Overall some concerns due to no information about allocation concealment, missing outcome data (large dropout), potential bias in the measurement of outcome (self‐report), and insufficient information on the analysis intentions |
Risk of bias for analysis 1.2 Parenting interventions vs inactive control, Outcome 2: Psychological wellbeing, at post‐intervention.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Rosenblum 2017 | Some concerns | Method used to generate random sequence is adequate, however unclear how they concealed allocation, as no details provided on who called the participant informing them of their allocation, and how that individual received allocation information: "Women were randomized using a computer‐generated algorithm (urn randomization stratified by baseline trauma exposure and depression to ensure balanced groups to either the multifamily group [treatment condition] or mailing group [control condition])." No significant differences reported between groups: "Women in both conditions were balanced on demographic, mental health and trauma variables" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | Some concerns | 36‐37% dropout (from total sample) No evidence that the results was not biased by the missing data, however no analysis method or sensitivity analysis to correct for bias Reasons for dropout are not reported, however dropout is equal between groups | Some concerns | Validated outcome measure used Same measurement and assessment time points used for all participants Measurement tool is self‐report, so participants are assessors and cannot be blinded The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Some concerns | No published protocol, however outcomes in methods section align with those in the results Insufficient detail on analysis intentions, there is likely more than one way in which the outcome measurement could have been analysed | Some concerns | Overall some concerns due to no information about allocation concealment, missing outcome data (large dropout), potential bias in the measurement of outcome (self‐report), and insufficient information on the analysis intentions |
Risk of bias for analysis 1.3 Parenting interventions vs inactive control, Outcome 6: Parent–child relationship (continuous data), at post‐intervention.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Pasalich 2019 | Some concerns | Method used to generate random sequence is adequate: "Following the first research visit, families were randomized to receive PFR (n =124) or the R&R program (n = 123), using a computer randomization program that blocked families based on race and ethnicity" Methods used to conceal allocation not described No significant differences reported between groups: "There were no statistically significant (p < .05) differences by condition in baseline characteristics" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions (i.e., comparator groups only received three short phone calls) No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with incomplete outcome data. | Low risk of bias | 0% dropout at post treatment from PRF and 8% from R&R (based on unpublished subgroup data provided by authors) | Low risk of bias | Validated outcome measure used Same measurement and assessment time points used for all participants Outcome assessors were blinded to treatment condition: "Assessments were conducted by study research visitors who... were kept blind to intervention assignment, and whose offices were not near the PFR or R&R intervention staff" | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results Reported results correspond to intended outcome measures Reported results correspond to intended analyses | Some concerns | Overall some concerns due to no information about allocation concealment |
| Steele 2019 | Some concerns | Method used to generate random sequence not described: "Families were randomized in two blocks of 8, stratified by child age less than versus greater than 18 months of age, with 57% of children being under 18 months of age, and the remainder (43%) over 18 months but under 3 years of age" Methods used to conceal allocation not fully described, assignment envelopes were used without all the appropriate safeguards, no indication if they were non‐opaque or sequentially numbered: "For randomization, research staff opened sealed envelopes that allocated participants in a 1:1 ratio to treatment (GABI or STEP control) groups, stratified by child age (less than vs. greater than 18 months)" No significant differences between groups. | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions (i.e., those allocated to the intervention condition received additional care strategies and more contact time) No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | High risk of bias | 63‐68% dropout (from total sample) No evidence that the results was not biased by the missing data Some reasons for dropout reported (unstable housing), not specific to each condition, so assume missing mechanism is similar between conditions. Likely that missingness in the outcome depends on its true value as missing data from participants with unstable living conditions who may be more likely to score worse on this outcome: "Failed intakes and attrition was due mainly to housing instability with families moving and becoming un‐contactable", CONSORT states for both groups, "attended no more than a few sessions, moved, were not contactable" | Low risk of bias | Validated outcome measure used Same measurement and assessment time points used for all participants Outcome assessors were blinded to treatment condition: "Assessors (and coders) were masked to treatment group and time" | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements, however data only reported at post‐treatment, baseline data not reported. As interaction for this outcome was not significant, relevant adjusted means difference SE of difference and 95%CIs not reported: "Where an interaction of treatment group by ACE group is found to be significant, the relevant adjusted means difference for the ACE subgroups at end of treatment, standard error of difference, and 95% confidence intervals are also provided in the tables" | High risk of bias | Overall high risk of bias due to no information on the randomization process and missing outcome data (large dropout) |
Risk of bias for analysis 1.4 Parenting interventions vs inactive control, Outcome 6: Parent–child relationship (dichotomous data), at post‐intervention.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Cicchetti 2006 | Some concerns | Method used to generate random sequence and to conceal allocation are not described: "Following completion of baseline assessments, the mothers and infants recruited for the maltreatment sample were randomly assigned to one of three groups" No significant differences reported between groups: "The groups did not differ on child gender, maternal age, maternal minority race/ethnicity, current receipt of TANF, total family income, or marital status. However, the average Hollingshead level of education differed between groups, with mothers in the NC group reporting higher level education than mothers in the IPP and CS groups. However, the three maltreatment groups did not differ from each other. Finally, the groups differed on the number of children to whom the mothers had given birth, with mothers in the NC group reporting fewer children than the mothers in each of the maltreatment groups, but the IPP, PPI, and CS groups did not differ from each other" | High risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions Some deviation from intended intervention: "Mothers assigned to intervention groups who declined to participate in the intervention were added to the control group" Modified ITT excluding participants with missing outcome data | Low risk of bias | 8‐33% dropout (from total sample). Unbalanced dropout, large dropout in CS group, only moderate dropout in other conditions and control comparison group Evidence that the results was not biased by the missing data: "Treatment decliners did not differ from those who engaged in intervention on any demographic variables or baseline measures...Families who were retained versus lost to follow‐up were compared on baseline measures to determine variables that might relate to differential attrition. The groups did not differ on major family demographic variables...The retained and non‐assessed families also did not differ in terms of baseline measures of maternal representations of her own mother in childhood, the experience of maltreatment in her own childhood, parenting attitudes, stress associated with parenting, and social support" | Low risk of bias | Subscale of a validated outcome measure used Same measurement and assessment time points used for all participants Outcome assessors were blinded to treatment condition: "Children’s attachment at pre‐intervention was coded by two independent, reliably trained raters, who were unaware of children’s maltreatment statuses or intervention group assignments...[at follow‐up] Neither of the coders was aware of children’s maltreatment statuses, treatment conditions, or attachment classifications at previous assessments" | Some concerns | No published protocol, no data analysis plan reported in Cicchetti 2006 or Stronach 2013 All reported results correspond to intended outcome measurements | High risk of bias | Overall high risk of bias due to no information on the randomization process, deviations from the intended interventions, and insufficient information on the analysis intentions |
| Cicchetti 2006 | Some concerns | Method used to generate random sequence and to conceal allocation are not described: "Following completion of baseline assessments, the mothers and infants recruited for the maltreatment sample were randomly assigned to one of three groups" No significant differences reported between groups: "The groups did not differ on child gender, maternal age, maternal minority race/ethnicity, current receipt of TANF, total family income, or marital status. However, the average Hollingshead level of education differed between groups, with mothers in the NC group reporting higher level education than mothers in the IPP and CS groups. However, the three maltreatment groups did not differ from each other. Finally, the groups differed on the number of children to whom the mothers had given birth, with mothers in the NC group reporting fewer children than the mothers in each of the maltreatment groups, but the IPP, PPI, and CS groups did not differ from each other" | High risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions Some deviation from intended intervention: "Mothers assigned to intervention groups who declined to participate in the intervention were added to the control group" Modified ITT excluding participants with missing outcome data | Low risk of bias | 8‐33% dropout (from total sample). Unbalanced dropout, large dropout in CS group, only moderate dropout in other conditions and control comparison group Evidence that the results was not biased by the missing data: "Treatment decliners did not differ from those who engaged in intervention on any demographic variables or baseline measures...Families who were retained versus lost to follow‐up were compared on baseline measures to determine variables that might relate to differential attrition. The groups did not differ on major family demographic variables...The retained and non‐assessed families also did not differ in terms of baseline measures of maternal representations of her own mother in childhood, the experience of maltreatment in her own childhood, parenting attitudes, stress associated with parenting, and social support" | Low risk of bias | Subscale of a validated outcome measure used Same measurement and assessment time points used for all participants Outcome assessors were blinded to treatment condition: "Children’s attachment at pre‐intervention was coded by two independent, reliably trained raters, who were unaware of children’s maltreatment statuses or intervention group assignments...[at follow‐up] Neither of the coders was aware of children’s maltreatment statuses, treatment conditions, or attachment classifications at previous assessments" | Some concerns | No published protocol, no data analysis plan reported in Cicchetti 2006 or Stronach 2013 All reported results correspond to intended outcome measurements | High risk of bias | Overall high risk of bias due to no information on the randomization process, deviations from the intended interventions, and insufficient information on the analysis intentions |
Risk of bias for analysis 1.5 Parenting interventions vs inactive control, Outcome 6: Parent–child relationship (disorganised attachment), at post‐intervention.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Cicchetti 2006 | Some concerns | Method used to generate random sequence and to conceal allocation are not described: "Following completion of baseline assessments, the mothers and infants recruited for the maltreatment sample were randomly assigned to one of three groups" No significant differences reported between groups: "The groups did not differ on child gender, maternal age, maternal minority race/ethnicity, current receipt of TANF, total family income, or marital status. However, the average Hollingshead level of education differed between groups, with mothers in the NC group reporting higher level education than mothers in the IPP and CS groups. However, the three maltreatment groups did not differ from each other. Finally, the groups differed on the number of children to whom the mothers had given birth, with mothers in the NC group reporting fewer children than the mothers in each of the maltreatment groups, but the IPP, PPI, and CS groups did not differ from each other" | High risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions Some deviation from intended intervention: "Mothers assigned to intervention groups who declined to participate in the intervention were added to the control group" Modified ITT excluding participants with missing outcome data | Low risk of bias | 8‐33% dropout (from total sample). Unbalanced dropout, large dropout in CS group, only moderate dropout in other conditions and control comparison group Evidence that the results was not biased by the missing data: "Treatment decliners did not differ from those who engaged in intervention on any demographic variables or baseline measures...Families who were retained versus lost to follow‐up were compared on baseline measures to determine variables that might relate to differential attrition. The groups did not differ on major family demographic variables...The retained and nonassessed families also did not differ in terms of baseline measures of maternal representations of her own mother in childhood, the experience of maltreatment in her own childhood, parenting attitudes, stress associated with parenting, and social support" | Low risk of bias | Subscale of a validated outcome measure used Same measurement and assessment timepoints used for all participants Outcome assessors were blinded to treatment condition: "Children’s attachment at preintervention was coded by two independent, reliably trained raters, who were unaware of children’s maltreatment statuses or intervention group assignments...[at follow‐up] Neither of the coders was aware of children’s maltreatment statuses, treatment conditions, or attachment classifications at previous assessments" | Some concerns | No published protocol, no data analysis plan reported in Cicchetti 2006 or Stronach 2013 All reported results correspond to intended outcome measurements | High risk of bias | Overall high risk of bias due to no information on the randomization process, deviations from the intended interventions, and insufficient information on the analysis intentions |
| Cicchetti 2006 | Some concerns | Method used to generate random sequence and to conceal allocation are not described: "Following completion of baseline assessments, the mothers and infants recruited for the maltreatment sample were randomly assigned to one of three groups" No significant differences reported between groups: "The groups did not differ on child gender, maternal age, maternal minority race/ethnicity, current receipt of TANF, total family income, or marital status. However, the average Hollingshead level of education differed between groups, with mothers in the NC group reporting higher level education than mothers in the IPP and CS groups. However, the three maltreatment groups did not differ from each other. Finally, the groups differed on the number of children to whom the mothers had given birth, with mothers in the NC group reporting fewer children than the mothers in each of the maltreatment groups, but the IPP, PPI, and CS groups did not differ from each other" | High risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions Some deviation from intended intervention: "Mothers assigned to intervention groups who declined to participate in the intervention were added to the control group" Modified ITT excluding participants with missing outcome data | Low risk of bias | 8‐33% dropout (from total sample). Unbalanced dropout, large dropout in CS group, only moderate dropout in other conditions and control comparison group Evidence that the results was not biased by the missing data: "Treatment decliners did not differ from those who engaged in intervention on any demographic variables or baseline measures...Families who were retained versus lost to follow‐up were compared on baseline measures to determine variables that might relate to differential attrition. The groups did not differ on major family demographic variables...The retained and nonassessed families also did not differ in terms of baseline measures of maternal representations of her own mother in childhood, the experience of maltreatment in her own childhood, parenting attitudes, stress associated with parenting, and social support" | Low risk of bias | Subscale of a validated outcome measure used Same measurement and assessment timepoints used for all participants Outcome assessors were blinded to treatment condition: "Children’s attachment at preintervention was coded by two independent, reliably trained raters, who were unaware of children’s maltreatment statuses or intervention group assignments...[at follow‐up] Neither of the coders was aware of children’s maltreatment statuses, treatment conditions, or attachment classifications at previous assessments" | Some concerns | No published protocol, no data analysis plan reported in Cicchetti 2006 or Stronach 2013 All reported results correspond to intended outcome measurements | High risk of bias | Overall high risk of bias due to no information on the randomization process, deviations from the intended interventions, and insufficient information on the analysis intentions |
Risk of bias for analysis 1.8 Parenting interventions vs inactive control, Outcome 6: Parent–child relationship (secure attachment), at 12‐month follow‐up.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Cicchetti 2006 | Some concerns | Method used to generate random sequence and to conceal allocation are not described: "Following completion of baseline assessments, the mothers and infants recruited for the maltreatment sample were randomly assigned to one of three groups" No significant differences reported between groups: "The groups did not differ on child gender, maternal age, maternal minority race/ethnicity, current receipt of TANF, total family income, or marital status. However, the average Hollingshead level of education differed between groups, with mothers in the NC group reporting higher level education than mothers in the IPP and CS groups. However, the three maltreatment groups did not differ from each other. Finally, the groups differed on the number of children to whom the mothers had given birth, with mothers in the NC group reporting fewer children than the mothers in each of the maltreatment groups, but the IPP, PPI, and CS groups did not differ from each other" | High risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions Some deviation from intended intervention: "Mothers assigned to intervention groups who declined to participate in the intervention were added to the control group" Modified ITT excluding participants with missing outcome data | Low risk of bias | 8‐33% dropout (from total sample). Unbalanced dropout, large dropout in CS group, only moderate dropout in other conditions and control comparison group Evidence that the results was not biased by the missing data: "Treatment decliners did not differ from those who engaged in intervention on any demographic variables or baseline measures...Families who were retained versus lost to follow‐up were compared on baseline measures to determine variables that might relate to differential attrition. The groups did not differ on major family demographic variables...The retained and nonassessed families also did not differ in terms of baseline measures of maternal representations of her own mother in childhood, the experience of maltreatment in her own childhood, parenting attitudes, stress associated with parenting, and social support" | Low risk of bias | Subscale of a validated outcome measure used Same measurement and assessment timepoints used for all participants Outcome assessors were blinded to treatment condition: "Children’s attachment at preintervention was coded by two independent, reliably trained raters, who were unaware of children’s maltreatment statuses or intervention group assignments...[at follow‐up] Neither of the coders was aware of children’s maltreatment statuses, treatment conditions, or attachment classifications at previous assessments" | Some concerns | No published protocol, no data analysis plan reported in Cicchetti 2006 or Stronach 2013 All reported results correspond to intended outcome measurements | High risk of bias | Overall high risk of bias due to no information on the randomization process, deviations from the intended interventions, and insufficient information on the analysis intentions |
| Cicchetti 2006 | Some concerns | Method used to generate random sequence and to conceal allocation are not described: "Following completion of baseline assessments, the mothers and infants recruited for the maltreatment sample were randomly assigned to one of three groups" No significant differences reported between groups: "The groups did not differ on child gender, maternal age, maternal minority race/ethnicity, current receipt of TANF, total family income, or marital status. However, the average Hollingshead level of education differed between groups, with mothers in the NC group reporting higher level education than mothers in the IPP and CS groups. However, the three maltreatment groups did not differ from each other. Finally, the groups differed on the number of children to whom the mothers had given birth, with mothers in the NC group reporting fewer children than the mothers in each of the maltreatment groups, but the IPP, PPI, and CS groups did not differ from each other" | High risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions Some deviation from intended intervention: "Mothers assigned to intervention groups who declined to participate in the intervention were added to the control group" Modified ITT excluding participants with missing outcome data | Low risk of bias | 8‐33% dropout (from total sample). Unbalanced dropout, large dropout in CS group, only moderate dropout in other conditions and control comparison group Evidence that the results was not biased by the missing data: "Treatment decliners did not differ from those who engaged in intervention on any demographic variables or baseline measures...Families who were retained versus lost to follow‐up were compared on baseline measures to determine variables that might relate to differential attrition. The groups did not differ on major family demographic variables...The retained and nonassessed families also did not differ in terms of baseline measures of maternal representations of her own mother in childhood, the experience of maltreatment in her own childhood, parenting attitudes, stress associated with parenting, and social support" | Low risk of bias | Subscale of a validated outcome measure used Same measurement and assessment timepoints used for all participants Outcome assessors were blinded to treatment condition: "Children’s attachment at preintervention was coded by two independent, reliably trained raters, who were unaware of children’s maltreatment statuses or intervention group assignments...[at follow‐up] Neither of the coders was aware of children’s maltreatment statuses, treatment conditions, or attachment classifications at previous assessments" | Some concerns | No published protocol, no data analysis plan reported in Cicchetti 2006 or Stronach 2013 All reported results correspond to intended outcome measurements | High risk of bias | Overall high risk of bias due to no information on the randomization process, deviations from the intended interventions, and insufficient information on the analysis intentions |
Risk of bias for analysis 1.9 Parenting interventions vs inactive control, Outcome 6: Parent–child relationship (disorganised attachment), at 12‐month follow‐up.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Cicchetti 2006 | Some concerns | Method used to generate random sequence and to conceal allocation are not described: "Following completion of baseline assessments, the mothers and infants recruited for the maltreatment sample were randomly assigned to one of three groups" No significant differences reported between groups: "The groups did not differ on child gender, maternal age, maternal minority race/ethnicity, current receipt of TANF, total family income, or marital status. However, the average Hollingshead level of education differed between groups, with mothers in the NC group reporting higher level education than mothers in the IPP and CS groups. However, the three maltreatment groups did not differ from each other. Finally, the groups differed on the number of children to whom the mothers had given birth, with mothers in the NC group reporting fewer children than the mothers in each of the maltreatment groups, but the IPP, PPI, and CS groups did not differ from each other" | High risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions Some deviation from intended intervention: "Mothers assigned to intervention groups who declined to participate in the intervention were added to the control group" Modified ITT excluding participants with missing outcome data | Low risk of bias | 8‐33% dropout (from total sample). Unbalanced dropout, large dropout in CS group, only moderate dropout in other conditions and control comparison group Evidence that the results was not biased by the missing data: "Treatment decliners did not differ from those who engaged in intervention on any demographic variables or baseline measures...Families who were retained versus lost to follow‐up were compared on baseline measures to determine variables that might relate to differential attrition. The groups did not differ on major family demographic variables...The retained and nonassessed families also did not differ in terms of baseline measures of maternal representations of her own mother in childhood, the experience of maltreatment in her own childhood, parenting attitudes, stress associated with parenting, and social support" | Low risk of bias | Subscale of a validated outcome measure used Same measurement and assessment timepoints used for all participants Outcome assessors were blinded to treatment condition: "Children’s attachment at preintervention was coded by two independent, reliably trained raters, who were unaware of children’s maltreatment statuses or intervention group assignments...[at follow‐up] Neither of the coders was aware of children’s maltreatment statuses, treatment conditions, or attachment classifications at previous assessments" | Some concerns | No published protocol, no data analysis plan reported in Cicchetti 2006 or Stronach 2013 All reported results correspond to intended outcome measurements | High risk of bias | Overall high risk of bias due to no information on the randomization process, deviations from the intended interventions, and insufficient information on the analysis intentions |
| Cicchetti 2006 | Some concerns | Method used to generate random sequence and to conceal allocation are not described: "Following completion of baseline assessments, the mothers and infants recruited for the maltreatment sample were randomly assigned to one of three groups" No significant differences reported between groups: "The groups did not differ on child gender, maternal age, maternal minority race/ethnicity, current receipt of TANF, total family income, or marital status. However, the average Hollingshead level of education differed between groups, with mothers in the NC group reporting higher level education than mothers in the IPP and CS groups. However, the three maltreatment groups did not differ from each other. Finally, the groups differed on the number of children to whom the mothers had given birth, with mothers in the NC group reporting fewer children than the mothers in each of the maltreatment groups, but the IPP, PPI, and CS groups did not differ from each other" | High risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions Some deviation from intended intervention: "Mothers assigned to intervention groups who declined to participate in the intervention were added to the control group" Modified ITT excluding participants with missing outcome data | Low risk of bias | 8‐33% dropout (from total sample). Unbalanced dropout, large dropout in CS group, only moderate dropout in other conditions and control comparison group Evidence that the results was not biased by the missing data: "Treatment decliners did not differ from those who engaged in intervention on any demographic variables or baseline measures...Families who were retained versus lost to follow‐up were compared on baseline measures to determine variables that might relate to differential attrition. The groups did not differ on major family demographic variables...The retained and nonassessed families also did not differ in terms of baseline measures of maternal representations of her own mother in childhood, the experience of maltreatment in her own childhood, parenting attitudes, stress associated with parenting, and social support" | Low risk of bias | Subscale of a validated outcome measure used Same measurement and assessment timepoints used for all participants Outcome assessors were blinded to treatment condition: "Children’s attachment at preintervention was coded by two independent, reliably trained raters, who were unaware of children’s maltreatment statuses or intervention group assignments...[at follow‐up] Neither of the coders was aware of children’s maltreatment statuses, treatment conditions, or attachment classifications at previous assessments" | Some concerns | No published protocol, no data analysis plan reported in Cicchetti 2006 or Stronach 2013 All reported results correspond to intended outcome measurements | High risk of bias | Overall high risk of bias due to no information on the randomization process, deviations from the intended interventions, and insufficient information on the analysis intentions |
Risk of bias for analysis 1.11 Parenting interventions vs inactive control, Outcome 6: Parent–child relationship (avoidant attachment), at 12‐month follow‐up.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Cicchetti 2006 | Some concerns | Method used to generate random sequence and to conceal allocation are not described: "Following completion of baseline assessments, the mothers and infants recruited for the maltreatment sample were randomly assigned to one of three groups" No significant differences reported between groups: "The groups did not differ on child gender, maternal age, maternal minority race/ethnicity, current receipt of TANF, total family income, or marital status. However, the average Hollingshead level of education differed between groups, with mothers in the NC group reporting higher level education than mothers in the IPP and CS groups. However, the three maltreatment groups did not differ from each other. Finally, the groups differed on the number of children to whom the mothers had given birth, with mothers in the NC group reporting fewer children than the mothers in each of the maltreatment groups, but the IPP, PPI, and CS groups did not differ from each other" | High risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions Some deviation from intended intervention: "Mothers assigned to intervention groups who declined to participate in the intervention were added to the control group" Modified ITT excluding participants with missing outcome data | Low risk of bias | 8‐33% dropout (from total sample). Unbalanced dropout, large dropout in CS group, only moderate dropout in other conditions and control comparison group Evidence that the results was not biased by the missing data: "Treatment decliners did not differ from those who engaged in intervention on any demographic variables or baseline measures...Families who were retained versus lost to follow‐up were compared on baseline measures to determine variables that might relate to differential attrition. The groups did not differ on major family demographic variables...The retained and nonassessed families also did not differ in terms of baseline measures of maternal representations of her own mother in childhood, the experience of maltreatment in her own childhood, parenting attitudes, stress associated with parenting, and social support" | Low risk of bias | Subscale of a validated outcome measure used Same measurement and assessment timepoints used for all participants Outcome assessors were blinded to treatment condition: "Children’s attachment at preintervention was coded by two independent, reliably trained raters, who were unaware of children’s maltreatment statuses or intervention group assignments...[at follow‐up] Neither of the coders was aware of children’s maltreatment statuses, treatment conditions, or attachment classifications at previous assessments" | Some concerns | No published protocol, no data analysis plan reported in Cicchetti 2006 or Stronach 2013 All reported results correspond to intended outcome measurements | High risk of bias | Overall high risk of bias due to no information on the randomization process, deviations from the intended interventions, and insufficient information on the analysis intentions |
| Cicchetti 2006 | Some concerns | Method used to generate random sequence and to conceal allocation are not described: "Following completion of baseline assessments, the mothers and infants recruited for the maltreatment sample were randomly assigned to one of three groups" No significant differences reported between groups: "The groups did not differ on child gender, maternal age, maternal minority race/ethnicity, current receipt of TANF, total family income, or marital status. However, the average Hollingshead level of education differed between groups, with mothers in the NC group reporting higher level education than mothers in the IPP and CS groups. However, the three maltreatment groups did not differ from each other. Finally, the groups differed on the number of children to whom the mothers had given birth, with mothers in the NC group reporting fewer children than the mothers in each of the maltreatment groups, but the IPP, PPI, and CS groups did not differ from each other" | High risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions Some deviation from intended intervention: "Mothers assigned to intervention groups who declined to participate in the intervention were added to the control group" Modified ITT excluding participants with missing outcome data | Low risk of bias | 8‐33% dropout (from total sample). Unbalanced dropout, large dropout in CS group, only moderate dropout in other conditions and control comparison group Evidence that the results was not biased by the missing data: "Treatment decliners did not differ from those who engaged in intervention on any demographic variables or baseline measures...Families who were retained versus lost to follow‐up were compared on baseline measures to determine variables that might relate to differential attrition. The groups did not differ on major family demographic variables...The retained and nonassessed families also did not differ in terms of baseline measures of maternal representations of her own mother in childhood, the experience of maltreatment in her own childhood, parenting attitudes, stress associated with parenting, and social support" | Low risk of bias | Subscale of a validated outcome measure used Same measurement and assessment timepoints used for all participants Outcome assessors were blinded to treatment condition: "Children’s attachment at preintervention was coded by two independent, reliably trained raters, who were unaware of children’s maltreatment statuses or intervention group assignments...[at follow‐up] Neither of the coders was aware of children’s maltreatment statuses, treatment conditions, or attachment classifications at previous assessments" | Some concerns | No published protocol, no data analysis plan reported in Cicchetti 2006 or Stronach 2013 All reported results correspond to intended outcome measurements | High risk of bias | Overall high risk of bias due to no information on the randomization process, deviations from the intended interventions, and insufficient information on the analysis intentions |
Risk of bias for analysis 1.12 Parenting interventions vs inactive control, Outcome 7: Parenting skills, at post‐intervention.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Haight 2005 | Some concerns | Method used to generate random sequence and to conceal allocation are not described: "Ten mothers were randomly assigned to the treatment group, and ten to the comparison group" No significant differences reported between groups: "T‐tests and chi‐square analyses revealed that with one exception intervention and comparison groups did not differ significantly on the characteristics described above. Mothers in the intervention group were more likely to have been placed in foster care themselves as children" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Assume data available for all participants as participants did the intervention, visit and assessment (clinical interview) all on the same day in succession | Low risk of bias | Data available for all participants | Low risk of bias | Direct observation rated using an unvalidated coding strategy Same measurement and assessment time points used for all participants Outcome assessors were blinded to treatment condition: "...raters were blind as to the group assignment of mothers" | Some concerns | No published protocol Reported results correspond to intended outcome measurements No analysis plan described | Some concerns | Overall some concerns due to no information on the randomization process and insufficient information on the analysis intentions |
| Liu 2021 | Some concerns | Method used to generate random sequence and to conceal allocation not described, only reported as "conditional randomization" No significant differences reported between groups: "Except for biological sex, the control and intervention groups did not show significant differences in other demographics and study variables." Although there was a difference in sample size, "The uneven sample sizes in the active control and intervention groups were a deliberate design decision to include maximum access to active intervention in these vulnerable populations" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions, including filming, role playing and video coaching No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | Some concerns | 34% dropout (from total sample), greater dropout in FIND (38%) than control (26%) No evidence that the results was not biased by the missing data Reasons for dropout not reported | Some concerns | Validated outcome measure used, however “all measures were reported by caregivers, which might induce reporter biases.” Same measurement and assessment time points used for all participants, however “during the study procedure, contact with the families was maintained through weekly meetings with FIND coaches (for intervention group families) or weekly check‐in phone calls/texts (for control group families).” P. 4. So there appear to be some differences in the weekly contact (meeting vs check‐in / text). Also, we don’t know if there were different types of assessors (psychologists, GP’s, RA’s). Measurement tool is self‐report, so participants are assessors and cannot be blinded The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements. Note, while only the subscale that showed significant change was reported in the paper, on request, the authors supplied all subscale data Seems likely that all reported results correspond to intended analyses, even though the analysis for this outcome is not reported in the analysis plan | Some concerns | Overall some concerns due to no information on the randomization process, missing outcome data (large dropout) and potential bias in the measurement of outcome (self‐report) |
| Rosenblum 2017 | Some concerns | Method used to generate random sequence is adequate, however unclear how they concealed allocation, as no details provided on who called the participant informing them of their allocation, and how that individual received allocation information: "Women were randomized using a computer‐generated algorithm (urn randomization stratified by baseline trauma exposure and depression to ensure balanced groups to either the multifamily group [treatment condition] or mailing group [control condition])." No significant differences reported between groups: "Women in both conditions were balanced on demographic, mental health and trauma variables" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | Some concerns | 36‐37% dropout (from total sample) No evidence that the results was not biased by the missing data, however no analysis method or sensitivity analysis to correct for bias Reasons for dropout are not reported, however dropout is equal between groups | Some concerns | Validated outcome measure used Same measurement and assessment time points used for all participants Measurement tool is self‐report, so participants are assessors and cannot be blinded The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Some concerns | No published protocol, however outcomes in methods section align with those in the results Insufficient detail on analysis intentions, there is likely more than one way in which the outcome measurement could have been analysed | Some concerns | Overall some concerns due to no information about allocation concealment, missing outcome data (large dropout), potential bias in the measurement of outcome (self‐report), and insufficient information on the analysis intentions |
| Steele 2019 | Some concerns | Method used to generate random sequence not described: "Families were randomized in two blocks of 8, stratified by child age less than versus greater than 18 months of age, with 57% of children being under 18 months of age, and the remainder (43%) over 18 months but under 3 years of age" Methods used to conceal allocation not fully described, assignment envelopes were used without all the appropriate safeguards, no indication if they were non‐opaque or sequentially numbered: "For randomization, research staff opened sealed envelopes that allocated participants in a 1:1 ratio to treatment (GABI or STEP control) groups, stratified by child age (less than vs. greater than 18 months)" No significant differences between groups. | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions (i.e., those allocated to the intervention condition received additional care strategies and more contact time) No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | High risk of bias | 63‐68% dropout (from total sample) No evidence that the results was not biased by the missing data Some reasons for dropout reported (unstable housing), not specific to each condition, so assume missing mechanism is similar between conditions "Failed intakes and attrition was due mainly to housing instability with families moving and becoming un‐contactable", CONSORT states for both groups, "attended no more than a few sessions, moved, were not contactable" Likely that missingness in the outcome depends on its true value as missing data from participants with unstable living conditions who may be more likely to score worse on this outcome | Low risk of bias | Validated outcome measure used Same measurement and assessment time points used for all participants Outcome assessors were blinded to treatment condition: "Assessors (and coders) were masked to treatment group and time" | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements, however data only reported at post‐treatment, baseline data not reported. As interaction for this outcome was not significant, relevant adjusted means difference SE of difference and 95%CIs not reported: "Where an interaction of treatment group by ACE group is found to be significant, the relevant adjusted means difference for the ACE subgroups at end of treatment, standard error of difference, and 95% confidence intervals are also provided in the tables" | High risk of bias | Overall high risk of bias due to no information on the randomization process and missing outcome data (large dropout) |
Risk of bias for analysis 1.13 Parenting interventions vs inactive control, Outcome 7: Parenting skills (maternal hostility), at post‐intervention.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Haight 2005 | Some concerns | Method used to generate random sequence and to conceal allocation are not described: "Ten mothers were randomly assigned to the treatment group, and ten to the comparison group" No significant differences reported between groups: "T‐tests and chi‐square analyses revealed that with one exception intervention and comparison groups did not differ significantly on the characteristics described above. Mothers in the intervention group were more likely to have been placed in foster care themselves as children" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Assume data available for all participants as participants did the intervention, visit and assessment (clinical interview) all on the same day in succession | Low risk of bias | Data available for all participants | Low risk of bias | Direct observation rated using an unvalidated coding strategy Same measurement and assessment time points used for all participants Outcome assessors were blinded to treatment condition: "...raters were blind as to the group assignment of mothers" | Some concerns | No published protocol Reported results correspond to intended outcome measurements No analysis plan described | Some concerns | Overall some concerns due to no information on the randomization process and insufficient information on the analysis intentions |
| Steele 2019 | Some concerns | Method used to generate random sequence not described: "Families were randomized in two blocks of 8, stratified by child age less than versus greater than 18 months of age, with 57% of children being under 18 months of age, and the remainder (43%) over 18 months but under 3 years of age" Methods used to conceal allocation not fully described, assignment envelopes were used without all the appropriate safeguards, no indication if they were non‐opaque or sequentially numbered: "For randomization, research staff opened sealed envelopes that allocated participants in a 1:1 ratio to treatment (GABI or STEP control) groups, stratified by child age (less than vs. greater than 18 months)" No significant differences between groups. | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions (i.e., those allocated to the intervention condition received additional care strategies and more contact time) No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | High risk of bias | 63‐68% dropout (from total sample) No evidence that the results was not biased by the missing data Some reasons for dropout reported (unstable housing), not specific to each condition, so assume missing mechanism is similar between conditions "Failed intakes and attrition was due mainly to housing instability with families moving and becoming un‐contactable", CONSORT states for both groups, "attended no more than a few sessions, moved, were not contactable" Likely that missingness in the outcome depends on its true value as missing data from participants with unstable living conditions who may be more likely to score worse on this outcome | Low risk of bias | Validated outcome measure used Same measurement and assessment time points used for all participants Outcome assessors were blinded to treatment condition: "Assessors (and coders) were masked to treatment group and time" | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements, however data only reported at post‐treatment, baseline data not reported. As interaction for this outcome was not significant, relevant adjusted means difference SE of difference and 95%CIs not reported: "Where an interaction of treatment group by ACE group is found to be significant, the relevant adjusted means difference for the ACE subgroups at end of treatment, standard error of difference, and 95% confidence intervals are also provided in the tables" | High risk of bias | Overall high risk of bias due to no information on the randomization process and missing outcome data (large dropout) |
Risk of bias for analysis 1.15 Socio‐ecological outcomes (connection to community professionals) ‐ secondary outcome.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Rosenblum 2017 | Some concerns | Method used to generate random sequence is adequate, however unclear how they concealed allocation, as no details provided on who called the participant informing them of their allocation, and how that individual received allocation information: "Women were randomized using a computer‐generated algorithm (urn randomization stratified by baseline trauma exposure and depression to ensure balanced groups to either the multifamily group [treatment condition] or mailing group [control condition])." No significant differences reported between groups: "Women in both conditions were balanced on demographic, mental health and trauma variables" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | Some concerns | 36‐37% dropout (from total sample) No evidence that the results was not biased by the missing data, however no analysis method or sensitivity analysis to correct for bias Reasons for dropout are not reported, however dropout is equal between groups | Some concerns | Validated outcome measure used Same measurement and assessment time points used for all participants Measurement tool is self‐report, so participants are assessors and cannot be blinded The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Some concerns | No published protocol, however outcomes in methods section align with those in the results Insufficient detail on analysis intentions, there is likely more than one way in which the outcome measurement could have been analysed | Some concerns | Method used to generate random sequence is adequate, however unclear how they concealed allocation, as no details provided on who called the participant informing them of their allocation, and how that individual received allocation information: "Women were randomized using a computer‐generated algorithm (urn randomization stratified by baseline trauma exposure and depression to ensure balanced groups to either the multifamily group [treatment condition] or mailing group [control condition])."
No significant differences reported between groups: "Women in both conditions were balanced on demographic, mental health and trauma variables" Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data 36‐37% dropout (from total sample) No evidence that the results was not biased by the missing data, however no analysis method or sensitivity analysis to correct for bias Reasons for dropout are not reported, however dropout is equal between groups Validated outcome measure used Same measurement and assessment time points used for all participants Measurement tool is self‐report, so participants are assessors and cannot be blinded The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received No published protocol, however outcomes in methods section align with those in the results Insufficient detail on analysis intentions, there is likely more than one way in which the outcome measurement could have been analysde |
Risk of bias for analysis 1.21 Parenting interventions vs inactive control, Outcome 7: Parenting skills, at post‐intervention, subgroup analysis (multiple component interventions).
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Subgroup 1.21.1 Single component interventions | ||||||||||||
| Haight 2005 | Some concerns | Method used to generate random sequence and to conceal allocation are not described: "Ten mothers were randomly assigned to the treatment group, and ten to the comparison group" No significant differences reported between groups: "T‐tests and chi‐square analyses revealed that with one exception intervention and comparison groups did not differ significantly on the characteristics described above. Mothers in the intervention group were more likely to have been placed in foster care themselves as children" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Assume data available for all participants as participants did the intervention, visit and assessment (clinical interview) all on the same day in succession | Low risk of bias | Data available for all participants | Low risk of bias | Direct observation rated using an unvalidated coding strategy Same measurement and assessment time points used for all participants Outcome assessors were blinded to treatment condition: "...raters were blind as to the group assignment of mothers" | Some concerns | No published protocol Reported results correspond to intended outcome measurements No analysis plan described | Some concerns | Overall some concerns due to no information on the randomization process and insufficient information on the analysis intentions |
| Liu 2021 | Some concerns | Method used to generate random sequence and to conceal allocation not described, only reported as "conditional randomization" No significant differences reported between groups: "Except for biological sex, the control and intervention groups did not show significant differences in other demographics and study variables." Although there was a difference in sample size, "The uneven sample sizes in the active control and intervention groups were a deliberate design decision to include maximum access to active intervention in these vulnerable populations" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions, including filming, role playing and video coaching No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | Some concerns | 34% dropout (from total sample), greater dropout in FIND (38%) than control (26%) No evidence that the results was not biased by the missing data Reasons for dropout not reported | Some concerns | Validated outcome measure used, however “all measures were reported by caregivers, which might induce reporter biases.” Same measurement and assessment time points used for all participants, however “during the study procedure, contact with the families was maintained through weekly meetings with FIND coaches (for intervention group families) or weekly check‐in phone calls/texts (for control group families).” P. 4. So there appear to be some differences in the weekly contact (meeting vs check‐in / text). Also, we don’t know if there were different types of assessors (psychologists, GP’s, RA’s). Measurement tool is self‐report, so participants are assessors and cannot be blinded The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements. Note, while only the subscale that showed significant change was reported in the paper, on request, the authors supplied all subscale data Seems likely that all reported results correspond to intended analyses, even though the analysis for this outcome is not reported in the analysis plan | Some concerns | Overall some concerns due to no information on the randomization process, missing outcome data (large dropout) and potential bias in the measurement of outcome (self‐report) |
| Steele 2019 | Some concerns | Method used to generate random sequence not described: "Families were randomized in two blocks of 8, stratified by child age less than versus greater than 18 months of age, with 57% of children being under 18 months of age, and the remainder (43%) over 18 months but under 3 years of age" Methods used to conceal allocation not fully described, assignment envelopes were used without all the appropriate safeguards, no indication if they were non‐opaque or sequentially numbered: "For randomization, research staff opened sealed envelopes that allocated participants in a 1:1 ratio to treatment (GABI or STEP control) groups, stratified by child age (less than vs. greater than 18 months)" No significant differences between groups. | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions (i.e., those allocated to the intervention condition received additional care strategies and more contact time) No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | High risk of bias | 63‐68% dropout (from total sample) No evidence that the results was not biased by the missing data Some reasons for dropout reported (unstable housing), not specific to each condition, so assume missing mechanism is similar between conditions "Failed intakes and attrition was due mainly to housing instability with families moving and becoming un‐contactable", CONSORT states for both groups, "attended no more than a few sessions, moved, were not contactable" Likely that missingness in the outcome depends on its true value as missing data from participants with unstable living conditions who may be more likely to score worse on this outcome | Low risk of bias | Validated outcome measure used Same measurement and assessment time points used for all participants Outcome assessors were blinded to treatment condition: "Assessors (and coders) were masked to treatment group and time" | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements, however data only reported at post‐treatment, baseline data not reported. As interaction for this outcome was not significant, relevant adjusted means difference SE of difference and 95%CIs not reported: "Where an interaction of treatment group by ACE group is found to be significant, the relevant adjusted means difference for the ACE subgroups at end of treatment, standard error of difference, and 95% confidence intervals are also provided in the tables" | High risk of bias | Overall high risk of bias due to no information on the randomization process and missing outcome data (large dropout) |
| Subgroup 1.21.2 Multiple component interventions | ||||||||||||
| Rosenblum 2017 | Some concerns | Method used to generate random sequence is adequate, however unclear how they concealed allocation, as no details provided on who called the participant informing them of their allocation, and how that individual received allocation information: "Women were randomized using a computer‐generated algorithm (urn randomization stratified by baseline trauma exposure and depression to ensure balanced groups to either the multifamily group [treatment condition] or mailing group [control condition])." No significant differences reported between groups: "Women in both conditions were balanced on demographic, mental health and trauma variables" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | Some concerns | 36‐37% dropout (from total sample) No evidence that the results was not biased by the missing data, however no analysis method or sensitivity analysis to correct for bias Reasons for dropout are not reported, however dropout is equal between groups | Some concerns | Validated outcome measure used Same measurement and assessment time points used for all participants Measurement tool is self‐report, so participants are assessors and cannot be blinded The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Some concerns | No published protocol, however outcomes in methods section align with those in the results Insufficient detail on analysis intentions, there is likely more than one way in which the outcome measurement could have been analysed | Some concerns | Overall some concerns due to no information about allocation concealment, missing outcome data (large dropout), potential bias in the measurement of outcome (self‐report), and insufficient information on the analysis intentions |
Risk of bias for analysis 2.1 Psychological interventions vs inactive control, Outcome 1: Trauma‐related symptoms, at post‐intervention.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Grote 2012 | Some concerns | Method used to generate random sequence is adequate: "Using a permuted block design stratified by race, we randomly assigned participants to receive either enhanced IPT‐B or UC" Methods used to conceal allocation not described No significant differences reported between groups: "Analyses show that participants in the IPT‐B and UC groups did not differ significantly on any of the baseline demographic or clinical characteristics" Note group size in total sample across IPT‐B and UC is equal, however group size is unequal when looking only at 'more exposure' (i.e., n = 6 in IPT‐B, n = 18 in UC). However, it would be more problematic if larger sample size was in IPT‐B group, as could indicate that preference was given to putting pts in the intervention group | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding single participant with missing outcome data | Low risk of bias | Data available for almost all participants (data seems to be missing from one participant only) | Some concerns | Validated outcome measure used Same measurement and assessment time points used for all participants Measurement tool is self‐report, so participants are assessors and cannot be blinded. Also states in limitation section: "raters may have been able to determine intervention due to differences in ease on contact to conduct follow‐up assessment" The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | Some concerns | Overall some concerns due to no information about allocation concealment and potential bias in the measurement of outcome (self‐report) |
| Grote 2015 | Low risk of bias | Method used to generate random sequence and conceal allocation is adequate: "Randomization to the MOMCare collaborative care intervention or to MSS public health services proceeded by means of an adaptive block randomization scheme to ensure that intervention and MSS groups maintained equal sizes. Randomization was stratified on initial depression severity (SCL‐20 ≤ 40 or > 40) and gestational age (< 22 weeks or ≥ 22 weeks). Within each of the 4 strata we created random orders of block sizes of either 2 or 4 study arm assignments in order to insure balance of intervention participants within each strata. Stratified block randomization was developed by our statistician and carried out via a computerised program by the depression care specialist (DCS) responsible for screening in 3‐4 public health centres. For each eligible patient, the DCS first entered the stratification variables into her laptop computer program and then received immediate notification of the patient's group assignment" No significant differences reported between groups: "The study groups were well‐balanced on socio‐demographic and clinical variables at baseline, except that MOMCare participants were more likely to be unemployed, a difference for which we controlled in the analyses" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | Some concerns | Dropout range from 0‐19% (based on unpublished subgroup data provided by authors), with more dropout in TAU (MTT+) group (19%) vs MOMCare (0%) No evidence that the results was not biased by the missing data Reasons for dropout not reported | Low risk of bias | Validated outcome measure used Same measurement and assessment time points used for all participants Outcome assessors were blinded to treatment condition, even though conventionally the outcome is self‐report: "All assessments were conducted via phone by an interviewer blinded to intervention status" | High risk of bias | Published protocol, trial registered (NCT01045655) Reported results do not correspond to intended outcome measurements, suggesting missing outcome data for non‐significant effect: "Treatment group differences refer to a comparison of the mean of the 3‐, 6‐, 12‐, and 18‐month follow‐up assessments, controlling for baseline values. In the event of a significant main effect for group, we report the pattern of means at each time point". Results section states: "In Tables 2 and 3, we show the significant main effects for group for each variable, with the relevant P‐values at each time point". All reported results correspond to intended analyses | High risk of bias | Overall high risk of bias due to missing outcome data (unbalanced dropout) and risk that outcomes were selected after the analysis were completed |
| Madigan 2015 | Some concerns | Method used to generate random sequence and to conceal allocation not described No significant differences reported between groups: "There were no significant differences between the intervention and control group, or the participating and dropped out subjects in terms of socio‐demographic variables, the main study criteria or other mental health variables." | Low risk of bias | Unclear if participants were aware of intervention assignment as the intervention consisted of trauma focused CBT and parenting program while the control group received the parenting program. All participants informed the study was piloting two interventions. No details provided on participant blinding. Carers and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | High risk of bias | 40% dropout (from total sample) No evidence that the results was not biased by the missing data Although reasons for dropout not reported, likely that missing mechanism is related to the true value of the outcome: "Difficulty with treatment adherence is frequently reported in adolescents, and pregnant adolescents in particular, as their desire to engage in research is generally poor" | Some concerns | Validated outcome measure used Same measurement and assessment time points used for all participants Measurement tool is self‐report, so participants are assessors and cannot be blinded The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | High risk of bias | Overall high risk of bias due to no information on the randomization process, missing outcome data (large dropout) and potential bias in the measurement of outcome (self‐report) |
| Upshur 2016 | Some concerns | Method used to generate random sequence is not fully adequate (i.e., unclear how the statistician selected the intervention site), while method used to conceal allocation is adequate: "One center was chosen randomly to implement the intervention integrated with usual prenatal care, the other site continued usual prenatal care only, which included prenatal advocate visits and services, routine prenatal care visits, and referral to on‐site mental health services if a woman screened positive for depression or PTSD...by a statistician unfamiliar with the project" Significant differences reported between groups: "Intervention women tended to be younger, and were significantly more likely to speak English, more likely to be born in the USA, more likely to have had an abortion, more likely to report negative coping strategies, and more likely to report current tobacco use and drug use in the previous year" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to design of cluster RCT: "Women were not blinded to condition" No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | Some concerns | 8‐15% dropout from each cluster but outcome data available for both clusters No evidence that the result was not biased by missing outcome data. Reasons for dropout not reported. | Some concerns | Validated outcome measure used Same measurement and assessment time points used for all participants Measurement tool is self‐report, so participants are assessors and cannot be blinded The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | High risk of bias | Overall high risk of bias due to bias in the timing of identification/recruitment of participants in the cluster RCT (individuals not identified/recruited before cluster randomization, participant selection may have been affected by knowledge of the intervention assigned to each cluster, some baseline imbalances), and additional concerns due to missing outcome data (moderate dropout) and potential bias in the measurement of outcome (self‐report) |
Risk of bias for analysis 2.2 Psychological interventions vs inactive control, Outcome 1: Trauma‐related symptoms, at 6‐month follow‐up.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Grote 2012 | Some concerns | Method used to generate random sequence is adequate: "Using a permuted block design stratified by race, we randomly assigned participants to receive either enhanced IPT‐B or UC" Methods used to conceal allocation not described No significant differences reported between groups: "Analyses show that participants in the IPT‐B and UC groups did not differ significantly on any of the baseline demographic or clinical characteristics" Note group size in total sample across IPT‐B and UC is equal, however group size is unequal when looking only at 'more exposure' (i.e., n = 6 in IPT‐B, n = 18 in UC). However, it would be more problematic if larger sample size was in IPT‐B group, as could indicate that preference was given to putting pts in the intervention group | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding single participant with missing outcome data | Low risk of bias | Data available for almost all participants (data seems to be missing from one participant only) | Some concerns | Validated outcome measure used Same measurement and assessment timepoints used for all participants Measurement tool is self‐report so participants are assessors and cannot be blinded. Also states in limitation section: "raters may have been able to determine intervention due to differences in ease on contact to conduct follow up assessment" The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | Some concerns | Overall some concerns due to no information about allocation concealment and potential bias in the measurement of outcome (self‐report) |
| Grote 2015 | Low risk of bias | Method used to generate random sequence and conceal allocation is adequate: "Randomization to the MOMCare collaborative care intervention or to MSS public health services proceeded by means of an adaptive block randomization scheme to ensure that intervention and MSS groups maintained equal sizes. Randomization was stratified on initial depression severity (SCL‐20 ≤ 40 or > 40) and gestational age (< 22 weeks or ≥ 22 weeks). Within each of the 4 strata we created random orders of block sizes of either 2 or 4 study arm assignments in order to insure balance of intervention participants within each strata. Stratified block randomization was developed by our statistician and carried out via a computerised program by the depression care specialist (DCS) responsible for screening in 3‐4 public health centres. For each eligible patient, the DCS first entered the stratification variables into her laptop computer program and then received immediate notification of the patient's group assignment" No significant differences reported between groups: "The study groups were well‐balanced on socio‐demographic and clinical variables at baseline, except that MOMCare participants were more likely to be unemployed, a difference for which we controlled in the analyses" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions – add any additional sentences No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | Some concerns | Dropout range from 0‐19% (based on unpublished subgroup data provided by authors), with more dropout in TAU (MTT+) group (19%) vs MOMCare (0%) No evidence that the results was not biased by the missing data; copy and paste quote if included Reasons for dropout not reported | Low risk of bias | Validated outcome measure used Same measurement and assessment timepoints used for all participants Outcome assessors were blinded to treatment condition, even though conventionally the outcome is self‐report: "All assessments were conducted via phone by an interviewer blinded to intervention status" | High risk of bias | Published protocol, trial registered (NCT01045655) Reported results do not correspond to intended outcome measurements, suggesting missing outcome data for non‐significant effect: "Treatment group differences refer to a comparison of the mean of the 3‐, 6‐, 12‐, and 18‐month follow‐up assessments, controlling for baseline values. In the event of a significant main effect for group, we report the pattern of means at each time point" Results section states: "In Tables 2 and 3, we show the significant main effects for group for each variable, with the relevant P‐values at each time point". All reported results correspond to intended analyses | High risk of bias | Overall some concerns due to missing outcome data (unbalanced dropout) and risk that outcomes were selected after the analysis were completed |
| Madigan 2015 | Some concerns | Method used to generate random sequence and to conceal allocation not described No significant differences reported between groups: "There were no significant differences between the intervention and control group, or the participating and dropped out subjects in terms of socio‐demographic variables, the main study criteria or other mental health variables." | Low risk of bias | Unclear if participants were aware of intervention assignment as the intervention consisted of trauma focused CBT and parenting program while the control group received the parenting program. All participants informed the study was piloting two interventions. No details provided on participant blinding. Carers and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | High risk of bias | 40% dropout (from total sample) No evidence that the results was not biased by the missing data Although reasons for dropout not reported, likely that missing mechanism is related to the true value of the outcome: "Difficulty with treatment adherence is frequently reported in adolescents, and pregnant adolescents in particular, as their desire to engage in research is generally poor" | Some concerns | Validated outcome measure used Same measurement and assessment timepoints used for all participants Measurement tool is self‐report so participants are assessors and cannot be blinded The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | High risk of bias | Overall some concerns due to no information on the randomization process, missing outcome data (large dropout) and potential bias in the measurement of outcome (self‐report) |
Risk of bias for analysis 2.3 Psychological interventions vs inactive control, Outcome 1: Trauma‐related symptoms, at 12‐month follow‐up.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Grote 2015 | Low risk of bias | Method used to generate random sequence and conceal allocation is adequate: "Randomization to the MOMCare collaborative care intervention or to MSS public health services proceeded by means of an adaptive block randomization scheme to ensure that intervention and MSS groups maintained equal sizes. Randomization was stratified on initial depression severity (SCL‐20 ≤ 40 or > 40) and gestational age (< 22 weeks or ≥ 22 weeks). Within each of the 4 strata we created random orders of block sizes of either 2 or 4 study arm assignments in order to insure balance of intervention participants within each strata. Stratified block randomization was developed by our statistician and carried out via a computerised program by the depression care specialist (DCS) responsible for screening in 3‐4 public health centres. For each eligible patient, the DCS first entered the stratification variables into her laptop computer program and then received immediate notification of the patient's group assignment" No significant differences reported between groups: "The study groups were well‐balanced on socio‐demographic and clinical variables at baseline, except that MOMCare participants were more likely to be unemployed, a difference for which we controlled in the analyses" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions – add any additional sentences No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | Some concerns | Dropout range from 0‐19% (based on unpublished subgroup data provided by authors), with more dropout in TAU (MTT+) group (19%) vs MOMCare (0%) No evidence that the results was not biased by the missing data; copy and paste quote if included Reasons for dropout not reported | Low risk of bias | Validated outcome measure used Same measurement and assessment timepoints used for all participants Outcome assessors were blinded to treatment condition, even though conventionally the outcome is self‐report: "All assessments were conducted via phone by an interviewer blinded to intervention status" | High risk of bias | Published protocol, trial registered (NCT01045655) Reported results do not correspond to intended outcome measurements, suggesting missing outcome data for non‐significant effect: "Treatment group differences refer to a comparison of the mean of the 3‐, 6‐, 12‐, and 18‐month follow‐up assessments, controlling for baseline values. In the event of a significant main effect for group, we report the pattern of means at each time point" Results section states: "In Tables 2 and 3, we show the significant main effects for group for each variable, with the relevant P‐values at each time point". All reported results correspond to intended analyses | High risk of bias | Overall some concerns due to missing outcome data (unbalanced dropout) and risk that outcomes were selected after the analysis were completed |
| Madigan 2015 | Some concerns | Method used to generate random sequence and to conceal allocation not described No significant differences reported between groups: "There were no significant differences between the intervention and control group, or the participating and dropped out subjects in terms of socio‐demographic variables, the main study criteria or other mental health variables." | Low risk of bias | Unclear if participants were aware of intervention assignment as the intervention consisted of trauma focused CBT and parenting program while the control group received the parenting program. All participants informed the study was piloting two interventions. No details provided on participant blinding. Carers and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | High risk of bias | 40% dropout (from total sample) No evidence that the results was not biased by the missing data Although reasons for dropout not reported, likely that missing mechanism is related to the true value of the outcome: "Difficulty with treatment adherence is frequently reported in adolescents, and pregnant adolescents in particular, as their desire to engage in research is generally poor" | Some concerns | Validated outcome measure used Same measurement and assessment time points used for all participants Although this is a clinician rated interview, it is unclear if the interviewers were blinded, seems to be conducted by clinical project coordinator The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | High risk of bias | Overall some concerns due to no information on the randomization process, missing outcome data (large dropout) and potential bias in the measurement of outcome (blinding of assessors not clear) |
Risk of bias for analysis 2.4 Psychological interventions vs inactive control, Outcome 2: Psychological wellbeing (continuous data), at post‐intervention.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Ammerman 2016 | Some concerns | Method used to generate random sequence is adequate, authors do not specify how the list was created (i.e., computer generated by independent statistician): "Randomization schedule was stratified by race and home visiting model...the randomization schedule was prepared prior to the start of the study and assignments were placed in separate envelopes that were opened sequentially."
Methods used to conceal allocation not fully described. Although envelopes were opened sequentially, no indication that the envelopes were sealed or opaque, so assignment of envelopes without appropriate safegaurds. No significant differences reported between groups |
Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding: "because some 'home visitors' had mothers in both IH‐CBT and HV conditions, there is a risk of contamination...unlikely that this was a significant concern given the robustness of the superiority of IH‐CBT...none of the home visitors were taught CBT strategies and it is improbable that they would acquire such skills simply by having mothers in treatment" Modified ITT excluding participants with missing outcome data | Low risk of bias | 5‐16% dropout (based on unpublished subgroup data provided by authors) Data available for almost all participants | Some concerns | Validated outcome measure used Same measurement and assessment timepoints used for all participants Measurement tool is self‐report so participants are assessors and cannot be blinded The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | Some concerns | Overall some concerns due to no information about allocation concealment and the potential bias in the measurement of outcome (self‐report) |
| Berry 2021 | Some concerns | Method used to generate random sequence is adequate, however allocation is unclear as it appears to have been conducted by the psychologist who delivered the intervention.: "...the clinical psychologist who informed them of their treatment group assignment as dictated by a computer‐generated random assignment schedule". No significant differences reported between groups: "Of the overall dataset (N = 109), those randomized to PREPP did not differ from those to ETAU on CM status, baseline demographic factors, or mood measures" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | Low risk of bias | Data available for all almost participants, although 55% dropout in total sample, only < 5% dropout based on unpublished subgroup data provided by authors | Low risk of bias | Validated outcome measure used Same measurement and assessment time points used for all participants Outcome assessors were blinded to treatment condition: "Maternal depressive symptoms were measured by a trained interviewer blind to the participants’ group assignment" | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results While two depression measures were used (one self‐report, one clinician rated) authors have provided clinician‐rated data, unlikely this was selected based on results but more likely as it is a less biased measure as assessors were blinded to group allocation All reported results correspond to intended analyses | Some concerns | Overall some concerns due to no information about the allocation concealment |
| Blalock 2013 | Some concerns | Method used to generate random sequence and to conceal allocation is not described. No significant differences reported between groups: "There were no significant differences in any of the demographics between treatment groups or across levels of trauma" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions, but they may not have been aware that one intervention was expected to be superior over another as both interventions were time/attention matched, and both consisted of the same smoking cessation strategy. Control group was still pregnancy relevant and instructional in nature. No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding. ITT analysis |
Some concerns | 32‐41% dropout (from total sample)
No evidence that the results was not biased by the missing data Reasons for dropout not reported. |
Some concerns | Validated outcome measure used Same measurement and assessment time points used for all participants Measurement tool is self‐ report, so participants are assessors and cannot be blinded The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received. | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results Potentially not all reported results correspond to intended outcome measurements, as data is not reported for all time points (CES‐D is 6 months post‐ partum). Unclear why they have not reported on all 6 time points (2, 4 and 6 weeks post end of treatment, 2 weeks, 3 months and 6 months postpartum). While depression was measured using two tools and data only reported for one, the authors state "Because all results are identical for the CES‐D and Edinburgh, only the CES‐D results are reported" All reported results correspond to intended analyses. |
Some concerns | Overall some concerns due to no information on the randomization process, missing outcome data (large dropout) and potential bias in the measurement of outcome (self‐report). |
| Grote 2012 | Some concerns | Method used to generate random sequence is adequate: "Using a permuted block design stratified by race, we randomly assigned participants to receive either enhanced IPT‐B or UC" Methods used to conceal allocation not described No significant differences reported between groups: "Analyses show that participants in the IPT‐B and UC groups did not differ significantly on any of the baseline demographic or clinical characteristics" Note group size in total sample across IPT‐B and UC is equal, however group size is unequal when looking only at 'more exposure' (i.e., n = 6 in IPT‐B, n = 18 in UC). However, it would be more problematic if larger sample size was in IPT‐B group, as could indicate that preference was given to putting pts in the intervention group | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding single participant with missing outcome data | Low risk of bias | Data available for almost all participants (data seems to be missing from one participant only) | Some concerns | Validated outcome measure used Same measurement and assessment time points used for all participants Measurement tool is self‐report, so participants are assessors and cannot be blinded. Also states in limitation section: "raters may have been able to determine intervention due to differences in ease on contact to conduct follow‐up assessment" The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | Some concerns | Overall some concerns due to no information about allocation concealment and potential bias in the measurement of outcome (self‐report) |
| Grote 2015 | Low risk of bias | Method used to generate random sequence and conceal allocation is adequate: "Randomization to the MOMCare collaborative care intervention or to MSS public health services proceeded by means of an adaptive block randomization scheme to ensure that intervention and MSS groups maintained equal sizes. Randomization was stratified on initial depression severity (SCL‐20 ≤ 40 or > 40) and gestational age (< 22 weeks or ≥ 22 weeks). Within each of the 4 strata we created random orders of block sizes of either 2 or 4 study arm assignments in order to insure balance of intervention participants within each strata. Stratified block randomization was developed by our statistician and carried out via a computerised program by the depression care specialist (DCS) responsible for screening in 3‐4 public health centres. For each eligible patient, the DCS first entered the stratification variables into her laptop computer program and then received immediate notification of the patient's group assignment" No significant differences reported between groups: "The study groups were well‐balanced on socio‐demographic and clinical variables at baseline, except that MOMCare participants were more likely to be unemployed, a difference for which we controlled in the analyses" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions – add any additional sentences No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | Some concerns | Dropout range from 0‐19% (based on unpublished subgroup data provided by authors), with more dropout in TAU (MTT+) group (19%) vs MOMCare (0%) No evidence that the results was not biased by the missing data Reasons for dropout not reported | Low risk of bias | Validated outcome measure used Same measurement and assessment time points used for all participants Outcome assessors were blinded to treatment condition, even though conventionally the outcome is self‐report: "All assessments were conducted via phone by an interviewer blinded to intervention status" | Low risk of bias | Published protocol (Grote 2014), trial registered NCT01045655. All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | Some concerns | Overall some concerns due to missing outcome data (unbalanced dropout) |
| Madigan 2015 | Some concerns | Method used to generate random sequence and to conceal allocation not described No significant differences reported between groups: "There were no significant differences between the intervention and control group, or the participating and dropped out subjects in terms of socio‐demographic variables, the main study criteria or other mental health variables." | Low risk of bias | Unclear if participants were aware of intervention assignment as the intervention consisted of trauma focused CBT and parenting program while the control group received the parenting program. All participants informed the study was piloting two interventions. No details provided on participant blinding. Carers and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | High risk of bias | 40% dropout (from total sample) No evidence that the results was not biased by the missing data Although reasons for dropout not reported, likely that missing mechanism is related to the true value of the outcome: "Difficulty with treatment adherence is frequently reported in adolescents, and pregnant adolescents in particular, as their desire to engage in research is generally poor" | Some concerns | Validated outcome measure used Same measurement and assessment time points used for all participants Measurement tool is self‐report, so participants are assessors and cannot be blinded The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | High risk of bias | Overall high risk of bias due to no information on the randomization process, missing outcome data (large dropout) and potential bias in the measurement of outcome (self‐report) |
| Silverstein 2011 | Low risk of bias | Method used to generate random sequence and conceal allocation is adequate: "Eligible mothers were allocated to PSE or control according to a computer generated randomization list. We randomized in block of randomly varying sizes of two and four to ensure balance between study arms. Randomization occurred independently within each individual study and at each study site The allocation sequence was concealed from all study personnel in sequentially numbered, opaque, sealed envelopes" No significant differences reported between groups: "The PSE group had a higher proportion of women experiencing moderately severe depressive symptoms at baseline than the control group (41 vs. 28%)" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding ITT analysis used | Some concerns | 15‐19% dropout (from total sample) No evidence that the results was not biased by the missing data Reasons for dropout not reported | Low risk of bias | Validated outcome measure used Same measurement and assessment timepoints used for all participants Outcome assessors were blinded to treatment condition: "Outcome assessors, investigators, and hospital staff were blinded to study allocation." | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | Some concerns | Overall some concerns due to missing outcome data (moderate dropout) |
| Upshur 2016 | Some concerns | Method used to generate random sequence is not fully adequate (i.e., unclear how the statistician selected the intervention site), while method used to conceal allocation is adequate: "One center was chosen randomly to implement the intervention integrated with usual prenatal care, the other site continued usual prenatal care only, which included prenatal advocate visits and services, routine prenatal care visits, and referral to on‐site mental health services if a woman screened positive for depression or PTSD...by a statistician unfamiliar with the project" Significant differences reported between groups: "Intervention women tended to be younger, and were significantly more likely to speak English, more likely to be born in the USA, more likely to have had an abortion, more likely to report negative coping strategies, and more likely to report current tobacco use and drug use in the previous year" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to design of cluster RCT: "Women were not blinded to condition" No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | Some concerns | 8‐15% dropout from each cluster but outcome data available for both clusters No evidence that the result was not biased by missing outcome data. Reasons for dropout not reported. | Some concerns | Validated outcome measure used Same measurement and assessment time points used for all participants Measurement tool is self‐report, so participants are assessors and cannot be blinded The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | High risk of bias | Overall high risk of bias due to bias in the timing of identification/recruitment of participants in the cluster RCT (individuals not identified/recruited before cluster randomization, participant selection may have been affected by knowledge of the intervention assigned to each cluster, some baseline imbalances), and additional concerns due to missing outcome data (moderate dropout) and potential bias in the measurement of outcome (self‐report) |
Risk of bias for analysis 2.5 Psychological interventions vs inactive control, Outcome 2: Psychological wellbeing (dichotomous data), at post‐intervention.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Grote 2015 | Low risk of bias | Method used to generate random sequence and conceal allocation is adequate: "Randomization to the MOMCare collaborative care intervention or to MSS public health services proceeded by means of an adaptive block randomization scheme to ensure that intervention and MSS groups maintained equal sizes. Randomization was stratified on initial depression severity (SCL‐20 ≤ 40 or > 40) and gestational age (< 22 weeks or ≥ 22 weeks). Within each of the 4 strata we created random orders of block sizes of either 2 or 4 study arm assignments in order to insure balance of intervention participants within each strata. Stratified block randomization was developed by our statistician and carried out via a computerised program by the depression care specialist (DCS) responsible for screening in 3‐4 public health centres. For each eligible patient, the DCS first entered the stratification variables into her laptop computer program and then received immediate notification of the patient's group assignment" No significant differences reported between groups: "The study groups were well‐balanced on socio‐demographic and clinical variables at baseline, except that MOMCare participants were more likely to be unemployed, a difference for which we controlled in the analyses" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions – add any additional sentences No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | Some concerns | Dropout range from 0‐19% (based on unpublished subgroup data provided by authors), with more dropout in TAU (MTT+) group (19%) vs MOMCare (0%) No evidence that the results was not biased by the missing data Reasons for dropout not reported | Low risk of bias | Validated outcome measure used Same measurement and assessment timepoints used for all participants. Although this is a self‐report measure, independent blinded assessment was conducted: "All assessments were conducted via phone by an interviewer blinded to intervention status" | Low risk of bias | Published protocol (Grote 2014), trial registered NCT01045655. All reported results correspond to intended outcome measurements. All reported results correspond to intended analyses. | Some concerns | Overall some concerns due to missing outcome data (unbalanced dropout) |
| Silverstein 2011 | Low risk of bias | Method used to generate random sequence and conceal allocation is adequate: "Eligible mothers were allocated to PSE or control according to a computer generated randomization list. We randomized in block of randomly varying sizes of two and four to ensure balance between study arms. Randomization occurred independently within each individual study and at each study site The allocation sequence was concealed from all study personnel in sequentially numbered, opaque, sealed envelopes" No significant differences reported between groups: "The PSE group had a higher proportion of women experiencing moderately severe depressive symptoms at baseline than the control group (41 vs. 28%)" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding ITT analysis used | Some concerns | 15‐19% dropout (from total sample) No evidence that the results was not biased by the missing data Reasons for dropout not reported | Low risk of bias | Validated outcome measure used Same measurement and assessment timepoints used for all participants Outcome assessors were blinded to treatment condition: "Outcome assessors, investigators, and hospital staff were blinded to study allocation." | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | Some concerns | Overall some concerns due to missing outcome data (moderate dropout) |
Risk of bias for analysis 2.6 Psychological interventions vs inactive control, Outcome 2: Psychological wellbeing (postpartum depression symptom severity), at post‐intervention.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Grote 2012 | Some concerns | Method used to generate random sequence is adequate: "Using a permuted block design stratified by race, we randomly assigned participants to receive either enhanced IPT‐B or UC" Methods used to conceal allocation not described No significant differences reported between groups: "Analyses show that participants in the IPT‐B and UC groups did not differ significantly on any of the baseline demographic or clinical characteristics" Note group size in total sample across IPT‐B and UC is equal, however group size is unequal when looking only at 'more exposure' (i.e., n = 6 in IPT‐B, n = 18 in UC). However, it would be more problematic if larger sample size was in IPT‐B group, as could indicate that preference was given to putting pts in the intervention group | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding single participant with missing outcome data | Low risk of bias | Data available for almost all participants (data seems to be missing from one participant only) | Some concerns | Validated outcome measure used Same measurement and assessment timepoints used for all participants Measurement tool is self‐report so participants are assessors and cannot be blinded. Also states in limitation section: "raters may have been able to determine intervention due to differences in ease on contact to conduct follow up assessment" The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | Some concerns | Overall some concerns due to no information about allocation concealment and potential bias in the measurement of outcome (self‐report) |
| Upshur 2016 | Some concerns | Method used to generate random sequence is not fully adequate (i.e., unclear how the statistician selected the intervention site), while method used to conceal allocation is adequate: "One center was chosen randomly to implement the intervention integrated with usual prenatal care, the other site continued usual prenatal care only, which included prenatal advocate visits and services, routine prenatal care visits, and referral to on‐site mental health services if a woman screened positive for depression or PTSD...by a statistician unfamiliar with the project" Significant differences reported between groups: "Intervention women tended to be younger, and were significantly more likely to speak English, more likely to be born in the USA, more likely to have had an abortion, more likely to report negative coping strategies, and more likely to report current tobacco use and drug use in the previous year" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to design of cluster RCT: "Women were not blinded to condition" No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | Some concerns | 8‐15% dropout from each cluster but outcome data available for both clusters No evidence that the result was not biased by missing outcome data. Reasons for dropout not reported. | Some concerns | Validated outcome measure used Same measurement and assessment timepoints used for all participants Measurement tool is self‐report so participants are assessors and cannot be blinded The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | High risk of bias | Overall high risk of bias due to bias in the timing of identification/recruitment of participants in the cluster RCT (individuals not identified/recruited before cluster randomization, participant selection may have been affected by knowledge of the intervention assigned to each cluster, some baseline imbalances), and additional concerns due to missing outcome data (moderate dropout) and potential bias in the measurement of outcome (self‐report) |
Risk of bias for analysis 2.7 Psychological interventions vs inactive control, Outcome 2: Psychological wellbeing (anxiety symptom severity), at post‐intervention.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Berry 2021 | Some concerns | Method used to generate random sequence is adequate, however allocation is unclear as it appears to have been conducted by the psychologist who delivered the intervention.: "...the clinical psychologist who informed them of their treatment group assignment as dictated by a computer‐generated random assignment schedule". No significant differences reported between groups: "Of the overall dataset (N = 109), those randomized to PREPP did not differ from those to ETAU on CM status, baseline demographic factors, or mood measures" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | Low risk of bias | Data available for all participants, although 55% dropout in total sample, only < 5% dropout based on unpublished subgroup data provided by authors | Low risk of bias | Validated outcome measure used Same measurement and assessment time points used for all participants Outcome assessors were blinded to treatment condition: "Maternal depressive symptoms were measured by a trained interviewer blind to the participants’ group assignment" | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results While two depression measures were used (one self‐report, one clinician rated) authors have provided clinician‐rated data, unlikely this was selected based on results but more likely as it is a less biased measure as assessors were blinded to group allocation All reported results correspond to intended analyses | Some concerns | Overall some concerns due to no information about allocation concealment |
| Grote 2012 | Some concerns | Method used to generate random sequence is adequate: "Using a permuted block design stratified by race, we randomly assigned participants to receive either enhanced IPT‐B or UC" Methods used to conceal allocation not described No significant differences reported between groups: "Analyses show that participants in the IPT‐B and UC groups did not differ significantly on any of the baseline demographic or clinical characteristics" Note group size in total sample across IPT‐B and UC is equal, however group size is unequal when looking only at 'more exposure' (i.e., n = 6 in IPT‐B, n = 18 in UC). However, it would be more problematic if larger sample size was in IPT‐B group, as could indicate that preference was given to putting pts in the intervention group | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding single participant with missing outcome data | Low risk of bias | Data available for almost all participants (data seems to be missing from one participant only) | Some concerns | Validated outcome measure used Same measurement and assessment timepoints used for all participants Measurement tool is self‐report so participants are assessors and cannot be blinded. Also states in limitation section: "raters may have been able to determine intervention due to differences in ease on contact to conduct follow up assessment" The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | Some concerns | Overall some concerns due to no information about allocation concealment and potential bias in the measurement of outcome (self‐report) |
Risk of bias for analysis 2.12 Psychological interventions vs inactive control, Outcome 4: Parent relationship quality, at post‐intervention.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Ammerman 2016 | Some concerns | Method used to generate random sequence is adequate, authors do not specify how the list was created (i.e., computer generated by independent statistician): "Randomization schedule was stratified by race and home visiting model...the randomization schedule was prepared prior to the start of the study and assignments were placed in separate envelopes that were opened sequentially."
Methods used to conceal allocation not fully described. Although envelopes were opened sequentially, no indication that the envelopes were sealed or opaque, so assignment of envelopes without appropriate safegaurds. No significant differences reported between groups |
Low risk of bias | Psychological intervention, likely both participants and intervention providers would be aware of intevention assignment "because some 'home visitors' had mothers in both IH‐CBT and HV conditions, there is a risk of contamination...unlikely that this was a significant concern given the robustness of the superiority of IH‐CBT...none of the home visitors were taught CBT strategies and it is improbable that they would acquire such skills simply by having mothers in treatment" pg 370 Ammerman 2013 No evidence of depatures from usual care, as part of usual care participants were permitted to access treatment outside of the trial, aligning with standard practice. Modified ITT in which participants with missing outcome data were excluded | Low risk of bias | Unpublished data from authors for the trauma exposed subsample shows moderate dropout for intervention group. IH‐CBT: 14% dropout, Home visiting: 5% dropout Low attrition. Comparing effects in ITT data and subgroup data based on modified ITT exluding those with missing data, analysis shows very little difference in M and SD. "dropout was unrelated to initial MDD severity, recurrent vs. single episode MDD, or psychiatric comorbidity (p < .05)." | Some concerns | Validated measure used Each group had same assessments. The ISEL is a self‐report outcome, the participant is the assessor so cannot be blinded The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment recieved | Low risk of bias | No published protocol. Analysis plan provided in report. Reported results correspond to intended outcome measures Reported results crrespond to intended analyses | Some concerns | Overall some concerns due to no information about allocation concealment and the potential bias in the measurement of outcome (self‐report) |
Risk of bias for analysis 2.13 Psychological interventions vs inactive control, Outcome 6: Parent–child relationship, at post‐intervention.
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Madigan 2015 | Some concerns | Method used to generate random sequence and to conceal allocation not described No significant differences reported between groups: "There were no significant differences between the intervention and control group, or the participating and dropped out subjects in terms of socio‐demographic variables, the main study criteria or other mental health variables." | Low risk of bias | Unclear if participants were aware of intervention assignment as the intervention consisted of trauma focused CBT and parenting program while the control group received the parenting program. All participants informed the study was piloting two interventions. No details provided on participant blinding. Carers and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | High risk of bias | 40% dropout (from total sample) No evidence that the results was not biased by the missing data Although reasons for dropout not reported, likely that missing mechanism is related to the true value of the outcome: "Difficulty with treatment adherence is frequently reported in adolescents, and pregnant adolescents in particular, as their desire to engage in research is generally poor" | Low risk of bias | Validated outcome measure used Same measurement and assessment timepoints used for all participants Outcome assessors were blinded to treatment condition: "A trained and highly experienced coder who was blind to intervention groups and study hypotheses coded all SSPs" | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | High risk of bias | Overall high risk of bias due to no information on the randomization process and missing outcome data (large dropout) |
Risk of bias for analysis 2.18 Psychological interventions vs inactive control, Outcome 1: Trauma‐related symptoms, at post‐intervention, subgroup (multiple component interventions).
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Subgroup 2.18.1 Single component ‐ psychological interventions | ||||||||||||
| Madigan 2015 | Some concerns | Method used to generate random sequence and to conceal allocation not described No significant differences reported between groups: "There were no significant differences between the intervention and control group, or the participating and dropped out subjects in terms of socio‐demographic variables, the main study criteria or other mental health variables." | Low risk of bias | Unclear if participants were aware of intervention assignment as the intervention consisted of trauma focused CBT and parenting program while the control group received the parenting program. All participants informed the study was piloting two interventions. No details provided on participant blinding. Carers and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | High risk of bias | 40% dropout (from total sample) No evidence that the results was not biased by the missing data Although reasons for dropout not reported, likely that missing mechanism is related to the true value of the outcome: "Difficulty with treatment adherence is frequently reported in adolescents, and pregnant adolescents in particular, as their desire to engage in research is generally poor" | Some concerns | Validated outcome measure used Same measurement and assessment time points used for all participants Measurement tool is self‐report, so participants are assessors and cannot be blinded The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | High risk of bias | Overall high risk of bias due to no information on the randomization process, missing outcome data (large dropout) and potential bias in the measurement of outcome (self‐report) |
| Upshur 2016 | Some concerns | Method used to generate random sequence is not fully adequate (i.e., unclear how the statistician selected the intervention site), while method used to conceal allocation is adequate: "One center was chosen randomly to implement the intervention integrated with usual prenatal care, the other site continued usual prenatal care only, which included prenatal advocate visits and services, routine prenatal care visits, and referral to on‐site mental health services if a woman screened positive for depression or PTSD...by a statistician unfamiliar with the project" Significant differences reported between groups: "Intervention women tended to be younger, and were significantly more likely to speak English, more likely to be born in the USA, more likely to have had an abortion, more likely to report negative coping strategies, and more likely to report current tobacco use and drug use in the previous year" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to design of cluster RCT: "Women were not blinded to condition" No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | Some concerns | 14% dropout (from total sample) No evidence that the result was not biased by missing outcome data. Reasons for dropout not reported | Some concerns | Validated outcome measure used Same measurement and assessment time points used for all participants Measurement tool is self‐report, so participants are assessors and cannot be blinded The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | Some concerns | Overall some concerns due to missing outcome data (moderate dropout) and potential bias in the measurement of outcome (self‐report) |
| Subgroup 2.18.2 Multiple component interventions | ||||||||||||
| Grote 2012 | Some concerns | Method used to generate random sequence is adequate: "Using a permuted block design stratified by race, we randomly assigned participants to receive either enhanced IPT‐B or UC" Methods used to conceal allocation not described No significant differences reported between groups: "Analyses show that participants in the IPT‐B and UC groups did not differ significantly on any of the baseline demographic or clinical characteristics" Note group size in total sample across IPT‐B and UC is equal, however group size is unequal when looking only at 'more exposure' (i.e., n = 6 in IPT‐B, n = 18 in UC). However, it would be more problematic if larger sample size was in IPT‐B group, as could indicate that preference was given to putting pts in the intervention group | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding single participant with missing outcome data | Low risk of bias | Data available for almost all participants (data seems to be missing from one participant only) | Some concerns | Validated outcome measure used Same measurement and assessment time points used for all participants Measurement tool is self‐report, so participants are assessors and cannot be blinded. Also states in limitation section: "raters may have been able to determine intervention due to differences in ease on contact to conduct follow‐up assessment" The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | Some concerns | Overall some concerns due to no information about allocation concealment and potential bias in the measurement of outcome (self‐report) |
| Grote 2015 | Low risk of bias | Method used to generate random sequence and conceal allocation is adequate: "Randomization to the MOMCare collaborative care intervention or to MSS public health services proceeded by means of an adaptive block randomization scheme to ensure that intervention and MSS groups maintained equal sizes. Randomization was stratified on initial depression severity (SCL‐20 ≤ 40 or > 40) and gestational age (< 22 weeks or ≥ 22 weeks). Within each of the 4 strata we created random orders of block sizes of either 2 or 4 study arm assignments in order to insure balance of intervention participants within each strata. Stratified block randomization was developed by our statistician and carried out via a computerised program by the depression care specialist (DCS) responsible for screening in 3‐4 public health centres. For each eligible patient, the DCS first entered the stratification variables into her laptop computer program and then received immediate notification of the patient's group assignment" No significant differences reported between groups: "The study groups were well‐balanced on socio‐demographic and clinical variables at baseline, except that MOMCare participants were more likely to be unemployed, a difference for which we controlled in the analyses" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | Some concerns | Dropout range from 0‐19% (based on unpublished subgroup data provided by authors), with more dropout in TAU (MTT+) group (19%) vs MOMCare (0%) No evidence that the results was not biased by the missing data Reasons for dropout not reported | Low risk of bias | Validated outcome measure used Same measurement and assessment time points used for all participants Outcome assessors were blinded to treatment condition, even though conventionally the outcome is self‐report: "All assessments were conducted via phone by an interviewer blinded to intervention status" | High risk of bias | Published protocol, trial registered (NCT01045655) Reported results do not correspond to intended outcome measurements, suggesting missing outcome data for non‐significant effect: "Treatment group differences refer to a comparison of the mean of the 3‐, 6‐, 12‐, and 18‐month follow‐up assessments, controlling for baseline values. In the event of a significant main effect for group, we report the pattern of means at each time point". Results section states: "In Tables 2 and 3, we show the significant main effects for group for each variable, with the relevant P‐values at each time point". All reported results correspond to intended analyses | High risk of bias | Overall some concerns due to missing outcome data (unbalanced dropout) and risk that outcomes were selected after the analysis were completed |
Risk of bias for analysis 2.19 Psychological interventions vs inactive control, Outcome 2: Psychological wellbeing (continuous data), at post‐intervention, subgroup (multiple component interventions).
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Subgroup 2.19.1 Single component ‐ psychological interventions | ||||||||||||
| Ammerman 2016 | Some concerns | Method used to generate random sequence is adequate, authors do not specify how the list was created (i.e., computer generated by independent statistician): "Randomization schedule was stratified by race and home visiting model...the randomization schedule was prepared prior to the start of the study and assignments were placed in separate envelopes that were opened sequentially."
Methods used to conceal allocation not fully described. Although envelopes were opened sequentially, no indication that the envelopes were sealed or opaque, so assignment of envelopes without appropriate safegaurds. No significant differences reported between groups |
Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding: "because some 'home visitors' had mothers in both IH‐CBT and HV conditions, there is a risk of contamination...unlikely that this was a significant concern given the robustness of the superiority of IH‐CBT...none of the home visitors were taught CBT strategies and it is improbable that they would acquire such skills simply by having mothers in treatment" Modified ITT excluding participants with missing outcome data | Low risk of bias | 5‐16% dropout (based on unpublished subgroup data provided by authors) Data available for almost all participants | Some concerns | Validated outcome measure used Same measurement and assessment timepoints used for all participants Measurement tool is self‐report so participants are assessors and cannot be blinded The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | Some concerns | Overall some concerns due to no information about allocation concealment and the potential bias in the measurement of outcome (self‐report) |
| Blalock 2013 | Some concerns | Method used to generate random sequence and to conceal allocation is not described. No significant differences reported between groups: "There were no significant differences in any of the demographics between treatment groups or across levels of trauma" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions, but they may not have been aware that one intervention was expected to be superior over another as both interventions were time/attention matched, and both consisted of the same smoking cessation strategy. Control group was still pregnancy relevant and instructional in nature. No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding. ITT analysis |
Some concerns | 32‐41% dropout (from total sample) No evidence that the results was not biased by the missing data Reasons for dropout not reported. | Some concerns | Validated outcome measure used Same measurement and assessment time points used for all participants Measurement tool is self‐ report, so participants are assessors and cannot be blinded. The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received. | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results Potentially not all reported results correspond to intended outcome measurements, as data is not reported for all time points (CES‐D is 6 months post‐ partum). Unclear why they have not reported on all 6 time points (2, 4 and 6 weeks post end of treatment, 2 weeks, 3 months and 6 months postpartum). While depression was measured using two tools and data only reported for one, the authors state "Because all results are identical for the CES‐D and Edinburgh, only the CES‐D results are reported" All reported results correspond to intended analyses. |
Some concerns | Overall some concerns due to no information on the randomization process, missing outcome data (large dropout) and potential bias in the measurement of outcome (self‐report). |
| Madigan 2015 | Some concerns | Method used to generate random sequence and to conceal allocation not described No significant differences reported between groups: "There were no significant differences between the intervention and control group, or the participating and dropped out subjects in terms of socio‐demographic variables, the main study criteria or other mental health variables." | Low risk of bias | Unclear if participants were aware of intervention assignment as the intervention consisted of trauma focused CBT and parenting program while the control group received the parenting program. All participants informed the study was piloting two interventions. No details provided on participant blinding. Carers and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | High risk of bias | 40% dropout (from total sample) No evidence that the results was not biased by the missing data Although reasons for dropout not reported, likely that missing mechanism is related to the true value of the outcome: "Difficulty with treatment adherence is frequently reported in adolescents, and pregnant adolescents in particular, as their desire to engage in research is generally poor" | Some concerns | Validated outcome measure used Same measurement and assessment time points used for all participants Measurement tool is self‐report, so participants are assessors and cannot be blinded The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | High risk of bias | Overall high risk of bias due to no information on the randomization process, missing outcome data (large dropout) and potential bias in the measurement of outcome (self‐report) |
| Silverstein 2011 | Low risk of bias | Method used to generate random sequence and conceal allocation is adequate: "Eligible mothers were allocated to PSE or control according to a computer generated randomization list. We randomized in block of randomly varying sizes of two and four to ensure balance between study arms. Randomization occurred independently within each individual study and at each study site The allocation sequence was concealed from all study personnel in sequentially numbered, opaque, sealed envelopes" No significant differences reported between groups: "The PSE group had a higher proportion of women experiencing moderately severe depressive symptoms at baseline than the control group (41 vs. 28%)" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding ITT analysis used | Some concerns | 15‐19% dropout (from total sample) No evidence that the results was not biased by the missing data Reasons for dropout not reported | Low risk of bias | Validated outcome measure used Same measurement and assessment timepoints used for all participants Outcome assessors were blinded to treatment condition: "Outcome assessors, investigators, and hospital staff were blinded to study allocation." | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | Some concerns | Overall some concerns due to missing outcome data (moderate dropout) |
| Upshur 2016 | Some concerns | Method used to generate random sequence is not fully adequate (i.e., unclear how the statistician selected the intervention site), while method used to conceal allocation is adequate: "One center was chosen randomly to implement the intervention integrated with usual prenatal care, the other site continued usual prenatal care only, which included prenatal advocate visits and services, routine prenatal care visits, and referral to on‐site mental health services if a woman screened positive for depression or PTSD...by a statistician unfamiliar with the project" Significant differences reported between groups: "Intervention women tended to be younger, and were significantly more likely to speak English, more likely to be born in the USA, more likely to have had an abortion, more likely to report negative coping strategies, and more likely to report current tobacco use and drug use in the previous year" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to design of cluster RCT: "Women were not blinded to condition" No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | Some concerns | 14% dropout (from total sample) No evidence that the result was not biased by missing outcome data. Reasons for dropout not reported | Some concerns | Validated outcome measure used Same measurement and assessment time points used for all participants Measurement tool is self‐report, so participants are assessors and cannot be blinded The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | Some concerns | Overall some concerns due to missing outcome data (moderate dropout) and potential bias in the measurement of outcome (self‐report) |
| Subgroup 2.19.2 Multiple‐component interventions | ||||||||||||
| Berry 2021 | Some concerns | Method used to generate random sequence is adequate, however allocation is unclear as it appears to have been conducted by the psychologist who delivered the intervention.: "...the clinical psychologist who informed them of their treatment group assignment as dictated by a computer‐generated random assignment schedule". No significant differences reported between groups: "Of the overall dataset (N = 109), those randomized to PREPP did not differ from those to ETAU on CM status, baseline demographic factors, or mood measures" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | Low risk of bias | Data available for all almost participants, although 55% dropout in total sample, only < 5% dropout based on unpublished subgroup data provided by authors | Low risk of bias | Validated outcome measure used Same measurement and assessment time points used for all participants Outcome assessors were blinded to treatment condition: "Maternal depressive symptoms were measured by a trained interviewer blind to the participants’ group assignment" | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results While two depression measures were used (one self‐report, one clinician rated) authors have provided clinician‐rated data, unlikely this was selected based on results but more likely as it is a less biased measure as assessors were blinded to group allocation All reported results correspond to intended analyses | Some concerns | Overall some concerns due to no information about the allocation concealment |
| Grote 2012 | Some concerns | Method used to generate random sequence is adequate: "Using a permuted block design stratified by race, we randomly assigned participants to receive either enhanced IPT‐B or UC" Methods used to conceal allocation not described No significant differences reported between groups: "Analyses show that participants in the IPT‐B and UC groups did not differ significantly on any of the baseline demographic or clinical characteristics" Note group size in total sample across IPT‐B and UC is equal, however group size is unequal when looking only at 'more exposure' (i.e., n = 6 in IPT‐B, n = 18 in UC). However, it would be more problematic if larger sample size was in IPT‐B group, as could indicate that preference was given to putting pts in the intervention group | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding single participant with missing outcome data | Low risk of bias | Data available for almost all participants (data seems to be missing from one participant only) | Some concerns | Validated outcome measure used Same measurement and assessment time points used for all participants Measurement tool is self‐report, so participants are assessors and cannot be blinded. Also states in limitation section: "raters may have been able to determine intervention due to differences in ease on contact to conduct follow‐up assessment" The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | Some concerns | Overall some concerns due to no information about allocation concealment and potential bias in the measurement of outcome (self‐report) |
| Grote 2015 | Low risk of bias | Method used to generate random sequence and conceal allocation is adequate: "Randomization to the MOMCare collaborative care intervention or to MSS public health services proceeded by means of an adaptive block randomization scheme to ensure that intervention and MSS groups maintained equal sizes. Randomization was stratified on initial depression severity (SCL‐20 ≤ 40 or > 40) and gestational age (< 22 weeks or ≥ 22 weeks). Within each of the 4 strata we created random orders of block sizes of either 2 or 4 study arm assignments in order to insure balance of intervention participants within each strata. Stratified block randomization was developed by our statistician and carried out via a computerised program by the depression care specialist (DCS) responsible for screening in 3‐4 public health centres. For each eligible patient, the DCS first entered the stratification variables into her laptop computer program and then received immediate notification of the patient's group assignment" No significant differences reported between groups: "The study groups were well‐balanced on socio‐demographic and clinical variables at baseline, except that MOMCare participants were more likely to be unemployed, a difference for which we controlled in the analyses" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions – add any additional sentences No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | Some concerns | Dropout range from 0‐19% (based on unpublished subgroup data provided by authors), with more dropout in TAU (MTT+) group (19%) vs MOMCare (0%) No evidence that the results was not biased by the missing data Reasons for dropout not reported | Low risk of bias | Validated outcome measure used Same measurement and assessment time points used for all participants Outcome assessors were blinded to treatment condition, even though conventionally the outcome is self‐report: "All assessments were conducted via phone by an interviewer blinded to intervention status" | Low risk of bias | Published protocol (Grote 2014), trial registered NCT01045655. All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | Some concerns | Overall some concerns due to missing outcome data (unbalanced dropout) |
Risk of bias for analysis 2.20 Psychological interventions vs inactive control, Outcome 2: Psychological wellbeing (dichotomous data), at post‐intervention, subgroup (multiple component interventions).
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Subgroup 2.20.1 Single component ‐ psychological interventions | ||||||||||||
| Silverstein 2011 | Low risk of bias | Method used to generate random sequence and conceal allocation is adequate: "Eligible mothers were allocated to PSE or control according to a computer generated randomization list. We randomized in block of randomly varying sizes of two and four to ensure balance between study arms. Randomization occurred independently within each individual study and at each study site The allocation sequence was concealed from all study personnel in sequentially numbered, opaque, sealed envelopes" No significant differences reported between groups: "The PSE group had a higher proportion of women experiencing moderately severe depressive symptoms at baseline than the control group (41 vs. 28%)" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding ITT analysis used | Some concerns | 15‐19% dropout (from total sample) No evidence that the results was not biased by the missing data Reasons for dropout not reported | Low risk of bias | Validated outcome measure used Same measurement and assessment timepoints used for all participants Outcome assessors were blinded to treatment condition: "Outcome assessors, investigators, and hospital staff were blinded to study allocation." | Low risk of bias | No published protocol, however outcomes in methods section align with those in the results All reported results correspond to intended outcome measurements All reported results correspond to intended analyses | Some concerns | Overall some concerns due to missing outcome data (moderate dropout) |
| Subgroup 2.20.2 Multiple component interventions | ||||||||||||
| Grote 2015 | Low risk of bias | Method used to generate random sequence and conceal allocation is adequate: "Randomization to the MOMCare collaborative care intervention or to MSS public health services proceeded by means of an adaptive block randomization scheme to ensure that intervention and MSS groups maintained equal sizes. Randomization was stratified on initial depression severity (SCL‐20 ≤ 40 or > 40) and gestational age (< 22 weeks or ≥ 22 weeks). Within each of the 4 strata we created random orders of block sizes of either 2 or 4 study arm assignments in order to insure balance of intervention participants within each strata. Stratified block randomization was developed by our statistician and carried out via a computerised program by the depression care specialist (DCS) responsible for screening in 3‐4 public health centres. For each eligible patient, the DCS first entered the stratification variables into her laptop computer program and then received immediate notification of the patient's group assignment" No significant differences reported between groups: "The study groups were well‐balanced on socio‐demographic and clinical variables at baseline, except that MOMCare participants were more likely to be unemployed, a difference for which we controlled in the analyses" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions – add any additional sentences No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | Some concerns | Dropout range from 0‐19% (based on unpublished subgroup data provided by authors), with more dropout in TAU (MTT+) group (19%) vs MOMCare (0%) No evidence that the results was not biased by the missing data Reasons for dropout not reported | Low risk of bias | Validated outcome measure used Same measurement and assessment timepoints used for all participants. Although this is a self‐report measure, independent blinded assessment was conducted: "All assessments were conducted via phone by an interviewer blinded to intervention status" | Low risk of bias | Published protocol (Grote 2014), trial registered NCT01045655. All reported results correspond to intended outcome measurements. All reported results correspond to intended analyses. | Some concerns | Overall some concerns due to missing outcome data (unbalanced dropout) |
Risk of bias for analysis 3.8 Socioecological outcomes (hardship) ‐ post‐intervention (3‐month follow‐up).
| Study | Bias | |||||||||||
| Randomisation process | Deviations from intended interventions | Missing outcome data | Measurement of the outcome | Selection of the reported results | Overall | |||||||
| Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | Authors' judgement | Support for judgement | |
| Booshehri 2018 | Some concerns | Method used to generate random sequence not fully described: "recruitment staff assigned a study ID to participants. Study IDs were 150 random numbers ranging from 1 to 10,000 which were previously assigned to the three study groups, so that each participant was randomly assigned to a particular study group" Methods used to conceal allocation not described No significant differences reported between groups: "Recruitment and randomization processes were successful, as there were no statistically significant differences in all characteristics and baseline outcomes by group" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions – add any additional sentences No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | High risk of bias | 50‐57% dropout (high) No evidence that the results was not biased by the missing data Reasons for dropout not reported | Some concerns | Validated outcome measure used Same measurement and assessment timepoints used for all participants Measurement tool is self‐report so participants are assessors and cannot be blinded (Audio‐Computer Assisted Self‐ Interview) The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | High risk of bias | Published protocol and trial registered (NCT02577705) All reported results correspond to intended outcome measurements Insufficient detail on analysis intentions, there is likely more than one way in which the outcome measurement could have been analyzed | High risk of bias | Overall high risk of bias due no information on allocation concealment, and missing outcome data (large dropout) and insufficient information on the analysis intentions |
| Booshehri 2018 | Some concerns | Method used to generate random sequence not fully described: "recruitment staff assigned a study ID to participants. Study IDs were 150 random numbers ranging from 1 to 10,000 which were previously assigned to the three study groups, so that each participant was randomly assigned to a particular study group" Methods used to conceal allocation not described No significant differences reported between groups: "Recruitment and randomization processes were successful, as there were no statistically significant differences in all characteristics and baseline outcomes by group" | Low risk of bias | Participants and people delivering the interventions would have likely been aware of their group allocation due to differences in the interventions – add any additional sentences No deviation from intended intervention specified, unlikely that the outcome would be impacted by lack of blinding Modified ITT excluding participants with missing outcome data | High risk of bias | 50‐57% dropout (high) No evidence that the results was not biased by the missing data Reasons for dropout not reported | Some concerns | Validated outcome measure used Same measurement and assessment timepoints used for all participants Measurement tool is self‐report so participants are assessors and cannot be blinded (Audio‐Computer Assisted Self‐ Interview) The outcome assessment could be potentially influenced by the knowledge of the intervention received. It is unlikely that the reporting was influenced by the treatment received | High risk of bias | Published protocol and trial registered (NCT02577705) All reported results correspond to intended outcome measurements Insufficient detail on analysis intentions, there is likely more than one way in which the outcome measurement could have been analyzed | High risk of bias | Overall high risk of bias due no information on allocation concealment, and missing outcome data (large dropout) and insufficient information on the analysis intentions |
Acknowledgements
We acknowledge the Healing the Past by Nurturing the Future (HPNF) investigator team members not listed as authors, including Judy Atkinson, Deirdre Gartland, Karen Glover, Tanya Hirvoven, Caroline Atkinson, Helen McLachlan, Stephanie Brown, Jan Nicholson, Karen Glover, Yvonne Clark, Sandra Campbell, Fiona Mensah and Danielle Dyall.
We gratefully acknowledge all contributions of key stakeholders in the participatory action research involved in the co‐design of the HPNF project used to inform and fund work on this review.
We thank Cochrane Development, Psychological and Learning Problems for their advice and support during the development of the review. We thank Margaret Anderson for conducting the study searches for the review, and Claire Stansfield for developing a search strategy for a previous review on which this review is based.
The CRG Editorial Team are grateful to the following reviewers for their time and comments: Gemma L Clayton, Population Health Sciences, University of Bristol, UK; Patricia Correia‐Santos, Centro de Investigação em Psicologia (CiPsi), University of Minho, Portugal; Dr Sophie Isobel, University of Sydney, Australia; and one reviewer who chose not to be publicly acknowledged.
Appendices
Appendix 1. Search strategies
Cochrane Central Register of Controlled Trials (CENTRAL)
#1 [mh parents] or [mh ^"single‐parent family"] #2 [mh "Child Rearing"] or [mh "father‐child relations"] or [mh "intergenerational relations"] or [mh "maternal behavior"] or [mh "maternal deprivation"] or [mh "mother‐child relations"] or [mh "maternal‐fetal relations"] or [mh "parent‐child relations"] or [mh parenting] or [mh "paternal behavior"] or [mh "paternal deprivation"] #3 [mh pregnancy] or [mh "pregnancy, unplanned"] or [mh "pregnancy, unwanted"] or [mh "Pregnant Women"] #4 [mh "perinatal care"] or [mh "peripartum period"] or [mh "postnatal care"] or [mh "postpartum period"] or [mh "Preconception Care"] or [mh "prenatal care"] #5 [mh "Labor, Obstetric"] or [mh "Delivery, obstetric"] or [mh midwifery] or [mh "Obstetric nursing"] #6 (parenthood or motherhood or fatherhood or parentificat*) #7 ((parental or maternal or paternal) NEXT(care* or relations* or behavio* or interact* or bonding)) #8 ((parent* or mother* or father*) NEAR/5 (Adaptation or adjustment or becoming or become or expect* or Transform* or transition*)) #9 ((Parents or mothers or fathers) NEAR/5 (breastfeed* or breast NEXT feed* or young NEXT children or small NEXT children or toddlers or infants or preschool* or pre NEXT school* or baby or babies or newborn* or new NEXT born* or caregiving or early NEXT years or nursery)) #10 ((new or young or "first time") NEXT(Parents or Mothers or Fathers)) #11 ((child* or infant* or babies or toddler* or famil*) NEAR/3 (raise or raising or rear* or "bringing up" or "bring up")) #12 ((antenatal or antepartum or ante NEXT natal or ante NEXT partum or birth* or childbirth* or childbearing or conception or parturition or perinatal or peri NEXT natal or postpartum or post NEXT partum or postnatal or post NEXT natal or prenatal or pre NEXT natal or postnatal or pregnancy or primipara* or primigravid* or trimester*) NEAR/3 (care or healthcare or health or service*)) #13 (wom*n NEAR/2 (birth* or labour* or labor*)) #14 (Pregnan* NEAR/3 wom*n) or (Pregnan* NEAR/3 (adolescen* or teen*)) #15 {or #1‐#14} #16 [mh "Adult survivors of child abuse"] #17 [mh "Adult Survivors of Child Adverse Events"] #18 [mh "child abuse"] #19 [mh "Battered Child Syndrome"] #20 [mh "adverse childhood experiences"] #21 [mh "Exposure to violence"] #22 ((Childhood or children or "as a child" or "as an infant" or "early life") NEAR/3 (abuse or abused or abusive or neglect* or maltreat* or incest* or assault* or trauma* or victimi*ed or violen*)) #23 ((witness* or expos*) NEAR/3 (abuse* or abusive or trauma* or violen*)) #24 ((intergeneration* or inter NEXT generation* or transgeneration* or trans NEXT generation* or famil*) NEAR/3 (abus* or assault* or incest* or maltreat* or neglect* or trauma* or victimi*ed or violence)) #25 (generation* NEAR/3 (abus* or assault* or incest* or maltreat* or neglect* or trauma* or victimi*ed or violence)) #26 (cycle NEAR/2 (abus* or trauma* or neglect* or maltreat* or violen* or posttrauma* or post NEXT trauma* or toxic NEXT stress)) #27 ((Transmission or transmit*) NEAR/2 (generation* or family NEXT pattern*)) and (abus* or trauma* or neglect* or maltreat* or violen* or posttrauma* or post NEXT trauma* or toxic NEXT stress) #28 ((Transmission or transmit*) NEAR/2 (abus* or trauma* or neglect* or maltreat* or violen* or posttrauma* or post NEXT trauma* or toxic NEXT stress)) #29 ((break or breaking or breaks or broke) NEAR/3 (cycle* or pattern*)) and (abus* or trauma* or neglect* or maltreat* or violen* or posttrauma* or post NEXT trauma* or toxic NEXT stress) #30 (Adverse NEXT child* NEXT experience* or adverse NEXT child* NEXT event* or aversive NEXT child* NEXT experience* or child* NEXT adversity or early NEXT life NEXT trauma or traumatic NEXT child* NEXT experience) #31 {or #16‐#30} #32 #15 and #30 #33 ( [mh survivors] or [mh disclosure] or [mh "medical history taking"]) and [mh "child abuse"] #34 ((History or histories or historic* or survivor* or continuity or cycle* or discontinuity or disclosure or legacy or disclose* or recovery or unresolved or past) NEAR/3 (abus* or adversity or maltreat* or neglect* or posttrauma* or post NEXT trauma* or stress or trauma* or violen*)) #35 {or #33‐#34} #36 #15 AND #35 #37 MeSH descriptor: [Stress, Psychological] this term only #38 MeSH descriptor: [Stress Disorders, Post‐Traumatic] explode all trees #39 (Post NEXT traumatic NEXT stress* or Posttraumatic NEXT stress* or PTSD) #40 (relational NEXT trauma or developmental NEXT trauma or toxic NEXT stress or trauma NEXT informed or complex NEXT trauma*) #41 {or #37‐#40} #42 #15 AND #41 #43 #32 OR #36 OR #42 in Trials #44 (CHICTR* OR CHI NEXT CTR OR IRCT* OR RBR* OR JPRN* OR TCTR* OR SLCTR* OR CTRI* OR EUCT* OR NCT* OR NTR* OR ISRCTN* OR ACTRN* OR DRKS* OR PACT*):AU #45 #43 NOT #44
MEDLINE Ovid
1 exp parents/ or single‐parent family/ 2 Child Rearing/ or father‐child relations/ or intergenerational relations/ or maternal behavior/ or maternal deprivation/ or mother‐child relations/ or maternal‐fetal relations/ or parent‐child relations/ or parenting/ or paternal behavior/ or paternal deprivation/ 3 pregnancy/ or pregnancy, unplanned/ or pregnancy, unwanted/ or Pregnant Women/ 4 perinatal care/ or peripartum period/ or postnatal care/ or postpartum period/ or Preconception Care/ or prenatal care/ 5 Labor, Obstetric/ or Delivery, obstetric/ or midwifery/ or Obstetric nursing/ 6 (parenthood or motherhood or fatherhood or parentificat$).tw,kf. 7 ((parental or maternal or paternal) adj (care$ or relations$ or behavio$ or interact$ or bonding)).tw,kf. 8 ((parent$ or mother$ or father$) adj5 (Adaptation or Adjustment or becoming or become or expect$ or Transform$ or transition$)).tw,kf. 9 ((Parents or Mothers or Fathers) and (breastfeed$ or "young children" or "small children" or toddlers or infants or preschool$ or baby or babies or newborn$ or new born$ or new‐born$ or caregiving or early years or nursery)).tw,kf. 10 ((new or young or "first time") adj (Parents or Mothers or Fathers)).tw,kf. 11 ((child$ or infant$ or babies or toddler$ or famil$) adj3 (raise or raising or rear$ or "bringing up" or "bring up")).tw,kf. 12 ((antenatal or antepartum or ante‐natal or ante‐partum or birth$ or childbirth$ or childbearing or conception or parturition or perinatal or peri‐natal or postpartum or post‐partum or postnatal or post‐natal or prenatal or pre‐natal or postnatal or pregnancy or primipara$ or primigravid$ or trimester$) adj3 (care or healthcare or health or service$)).tw,kf. 13 (wom#n adj2 (birth$ or labour$ or labo?r$)).tw,kf. 14 ((Pregnan$ adj3 wom#n) or (Pregnan$ adj3 (adolescen$ or teen$))).tw,kf. 15 or/1‐14 16 Adult survivors of child abuse/ 17 "Adult Survivors of Child Adverse Events"/ 18 exp child abuse/ 19 Battered Child Syndrome/ 20 adverse childhood experiences/ 21 Exposure to violence/ 22 ((Childhood or children or "as a child" or "as an infant" or "early life") adj3 (abuse or abused or abusive or neglect$ or maltreat$ or incest$ or assault$ or trauma$ or victimi#ed or violen$)).tw,kf. 23 ((witness$ or expos$) adj3 (abuse$1 or abusive or trauma$ or violen$)).tw,kf. 24 ((intergeneration$ or inter‐generation$ or transgeneration$ or trans‐generation$ or famil$) adj3 (abus$ or assault$ or incest$ or maltreat$ or neglect$ or trauma$ or victimi#ed or violence)).tw,kf. 25 (generation$ adj3 (abus$ or assault$ or incest$ or maltreat$ or neglect$ or trauma$ or victimi#ed or violence)).tw,kf. 26 (cycle adj2 (abus$ or trauma$ or neglect$ or maltreat$ or violen$ or posttrauma$ or post‐trauma$ or "toxic stress")).tw,kf. 27 (((Transmission or transmit$) adj2 (generation$ or family pattern$)) and (abus$ or trauma$ or neglect$ or maltreat$ or violen$ or posttrauma$ or post‐trauma$ or "toxic stress")).tw,kf. 28 ((Transmission or transmit$) adj2 (abus$ or trauma$ or neglect$ or maltreat$ or violen$ or posttrauma$ or post‐trauma$ or "toxic stress")).tw,kf. 29 (((break or breaking or breaks or broke) adj3 (cycle$ or pattern$)) and (abus$ or trauma$ or neglect$ or maltreat$ or violen$ or posttrauma$ or post‐trauma$ or "toxic stress")).tw,kf. 30 (Adverse child$ experience$ or adverse child$ event$ or aversive child$ experience$ or child$ adversity or "early life trauma" or traumatic child$ experience).tw,kf. 31 or/16‐30 32 15 and 31 33 (survivors/ or disclosure/ or medical history taking/) and exp child abuse/ 34 ((History or histories or historic$ or survivor$ or continuity or cycle$ or discontinuity or disclosure or legacy or disclose$ or recovery or unresolved or past) adj3 (abus$ or adversity or maltreat$ or neglect$ or posttrauma$ or post‐trauma$ or stress or trauma$ or violen$)).tw,kf. 35 or/33‐34 36 15 and 35 37 Stress Disorders, Post‐Traumatic/ or Stress, Psychological/ ) 38 (Post‐traumatic stress$ or Post traumatic stress$ or PTSD).tw,kf. 39 (relational trauma or developmental trauma or toxic stress or trauma‐informed or complex trauma$).tw,kf. 40 or/37‐39 41 15 and 40 42 32 or 36 or 41 43 randomized controlled trial.pt. 44 controlled clinical trial.pt. 45 randomi#ed.ab. 46 placebo$.ab. 47 drug therapy.fs. 48 randomly.ab. 49 trial.ab. 50 groups.ab. 51 or/43‐50 52 exp animals/ not humans.sh. 53 51 not 52 54 42 and 53
MEDLINE(R) In‐Process & Other Non‐Indexed Citations Ovid
1 (parenthood or motherhood or fatherhood or parentificat$).tw,kf. 2 ((parental or maternal or paternal) adj (care$ or relations$ or behavio$ or interact$ or bonding)).tw,kf. 3 ((parent$ or mother$ or father$) adj5 (Adaptation or Adjustment or becoming or become or expect$ or Transform$ or transition$)).tw,kf. 4 ((Parents or Mothers or Fathers) and (breastfeed$ or "young children" or "small children" or toddlers or infants or preschool$ or baby or babies or newborn$ or new born$ or new‐born$ or caregiving or early years or nursery)).tw,kf. 5 ((new or young or "first time") adj (Parents or Mothers or Fathers)).tw,kf. 6 ((child$ or infant$ or babies or toddler$ or famil$) adj3 (raise or raising or rear$ or "bringing up" or "bring up")).tw,kf. 7 ((antenatal or antepartum or ante‐natal or ante‐partum or birth$ or childbirth$ or childbearing or conception or parturition or perinatal or peri‐natal or peripartum or peri‐partum or postpartum or post‐partum or postnatal or post‐natal or prenatal or pre‐natal or postnatal or pregnancy or primipara$ or primigravid$ or trimester$) adj3 (care or healthcare or health or service$)).tw,kf. 8 (wom#n adj2 (birth$ or labour$ or labo?r$)).tw,kf. 9 ((Pregnan$ adj3 wom#n) or (Pregnan$ adj3 (adolescen$ or teen$))).tw,kf. 10 (((midwi#e$ or obstetric or labour) adj3 (care or healthcare)) or (midwi#e$ service$ or obstetric$ service$)).ti,kf. 11 or/1‐10 12 "Adult survivor$".tw,kf. 13 ((Childhood or children or "as a child" or "as an infant" or "early life") adj3 (abuse or abused or abusive or adverse or adversity or neglect$ or maltreat$ or incest$ or assault$ or trauma$ or victimi#ed or violen$)).tw,kf. 14 ((witness$ or expos$) adj3 (abuse$1 or abusive or trauma$ or violen$)).tw,kf. 15 ((intergeneration$ or inter‐generation$ or transgeneration$ or trans‐generation$ or famil$) adj3 (abus$ or assault$ or incest$ or maltreat$ or neglect$ or trauma$ or victimi#ed or violence)).tw,kf. 16 (generation$ adj3 (abus$ or assault$ or incest$ or maltreat$ or neglect$ or trauma$ or victimi#ed or violence)).tw,kf. 17 (cycle adj2 (abus$ or trauma$ or neglect$ or maltreat$ or violen$ or posttrauma$ or post‐trauma$ or "toxic stress")).tw,kf. 18 (((Transmission or transmit$) adj2 (generation$ or family pattern$)) and (abus$ or trauma$ or neglect$ or maltreat$ or violen$ or posttrauma$ or post‐trauma$ or "toxic stress")).tw,kf. 19 ((Transmission or transmit$) adj2 (abus$ or trauma$ or neglect$ or maltreat$ or violen$ or posttrauma$ or post‐trauma$ or "toxic stress")).tw,kf. 20 (((break or breaking or breaks or broke) adj3 (cycle$ or pattern$)) and (abus$ or trauma$ or neglect$ or maltreat$ or violen$ or posttrauma$ or post‐trauma$ or "toxic stress")).tw,kf. 21 (Adverse child$ experience$ or adverse child$ event$ or aversive child$ experience$ or child$ adversity or "early life trauma" or traumatic child$ experience).tw,kf. 22 ((History or histories or historic$ or survivor$ or continuity or cycle$ or discontinuity or disclosure or legacy or disclose$ or recovery or unresolved or past) adj3 (abus$ or adversity or maltreat$ or neglect$ or posttrauma$ or post‐trauma$ or stress or trauma$ or violen$)).tw,kf. 23 (Post‐traumatic stress$ or Post traumatic stress$ or PTSD).tw,kf. 24 (relational trauma or developmental trauma or toxic stress or trauma‐informed or complex trauma$).tw,kf. 25 or/12‐24 26 11 and 25 27 (random$ or control$ or group$ or cluster$ or placebo$ or trial$ or assign$ or allocat$ or prospectiv$ or meta‐analysis or systematic review or longitudinal$).tw,kf. 28 26 and 27
MEDLINE Epub Ahead of Print Ovid
1 (parenthood or motherhood or fatherhood or parentificat$).tw,kf. 2 ((parental or maternal or paternal) adj (care$ or relations$ or behavio$ or interact$ or bonding)).tw,kf. 3 ((parent$ or mother$ or father$) adj5 (Adaptation or Adjustment or becoming or become or expect$ or Transform$ or transition$)).tw,kf. 4 ((Parents or Mothers or Fathers) and (breastfeed$ or "young children" or "small children" or toddlers or infants or preschool$ or baby or babies or newborn$ or new born$ or new‐born$ or caregiving or early years or nursery)).tw,kf. 5 ((new or young or "first time") adj (Parents or Mothers or Fathers)).tw,kf. 6 ((child$ or infant$ or babies or toddler$ or famil$) adj3 (raise or raising or rear$ or "bringing up" or "bring up")).tw,kf. 7 ((antenatal or antepartum or ante‐natal or ante‐partum or birth$ or childbirth$ or childbearing or conception or parturition or perinatal or peri‐natal or peripartum or peri‐partum or postpartum or post‐partum or postnatal or post‐natal or prenatal or pre‐natal or postnatal or pregnancy or primipara$ or primigravid$ or trimester$) adj3 (care or healthcare or health or service$)).tw,kf. 8 (wom#n adj2 (birth$ or labour$ or labo?r$)).tw,kf. 9 ((Pregnan$ adj3 wom#n) or (Pregnan$ adj3 (adolescen$ or teen$))).tw,kf. 10 (((midwi#e$ or obstetric or labour) adj3 (care or healthcare)) or (midwi#e$ service$ or obstetric$ service$)).ti,kf. 11 or/1‐10 12 "Adult survivor$".tw,kf. 13 ((Childhood or children or "as a child" or "as an infant" or "early life") adj3 (abuse or abused or abusive or adverse or adversity or neglect$ or maltreat$ or incest$ or assault$ or trauma$ or victimi#ed or violen$)).tw,kf. 14 ((witness$ or expos$) adj3 (abuse$1 or abusive or trauma$ or violen$)).tw,kf. 15 ((intergeneration$ or inter‐generation$ or transgeneration$ or trans‐generation$ or famil$) adj3 (abus$ or assault$ or incest$ or maltreat$ or neglect$ or trauma$ or victimi#ed or violence)).tw,kf. 16 (generation$ adj3 (abus$ or assault$ or incest$ or maltreat$ or neglect$ or trauma$ or victimi#ed or violence)).tw,kf. 17 (cycle adj2 (abus$ or trauma$ or neglect$ or maltreat$ or violen$ or posttrauma$ or post‐trauma$ or "toxic stress")).tw,kf. 18 (((Transmission or transmit$) adj2 (generation$ or family pattern$)) and (abus$ or trauma$ or neglect$ or maltreat$ or violen$ or posttrauma$ or post‐trauma$ or "toxic stress")).tw,kf. 19 ((Transmission or transmit$) adj2 (abus$ or trauma$ or neglect$ or maltreat$ or violen$ or posttrauma$ or post‐trauma$ or "toxic stress")).tw,kf. 20 (((break or breaking or breaks or broke) adj3 (cycle$ or pattern$)) and (abus$ or trauma$ or neglect$ or maltreat$ or violen$ or posttrauma$ or post‐trauma$ or "toxic stress")).tw,kf. 21 (Adverse child$ experience$ or adverse child$ event$ or aversive child$ experience$ or child$ adversity or "early life trauma" or traumatic child$ experience).tw,kf. 22 ((History or histories or historic$ or survivor$ or continuity or cycle$ or discontinuity or disclosure or legacy or disclose$ or recovery or unresolved or past) adj3 (abus$ or adversity or maltreat$ or neglect$ or posttrauma$ or post‐trauma$ or stress or trauma$ or violen$)).tw,kf. 23 (Post‐traumatic stress$ or Post traumatic stress$ or PTSD).tw,kf. 24 (relational trauma or developmental trauma or toxic stress or trauma‐informed or complex trauma$).tw,kf. 25 or/12‐24 26 11 and 25 27 (random$ or control$ or group$ or cluster$ or placebo$ or trial$ or assign$ or allocat$ or prospectiv$ or meta‐analysis or systematic review or longitudinal$).tw,kf. 28 26 and 27
Embase Ovid
1 exp parent/ 2 child rearing/ 3 exp child parent relation/ 4 human relation/ 5 maternal deprivation/ 6 parental deprivation/ 7 mother fetus relationship/ 8 pregnancy/ or adolescent pregnancy/ or unplanned pregnancy/ or unwanted pregnancy/ 9 pregnant woman/ 10 perinatal care/ or perinatal period/ 11 puerperium/ or postnatal care/ 12 prenatal care/ 13 prepregnancy care/ 14 labor/ or childbirth/ or labor management/ 15 perinatology/ 16 obstetrical nursing/ 17 (parenthood or motherhood or fatherhood or parentificat$).tw,kf. 18 ((parent$ or mother$ or father$) adj5 (Adaptation or Adjustment or becoming or become or expect$ or Transform$ or transition$)).tw,kf. 19 ((Parents or mothers or fathers) and (breastfeed$ or "young children" or "small children" or toddlers or infants or preschool$ or baby or babies or newborn$ or new born$ or new‐born$ or caregiving or early years or nursery)).tw,kf. 20 ((new or young or "first time") adj (Parents or Mothers or Fathers)).tw,kf. 21 ((Parents or mothers or fathers) adj10 (breastfeed$ or "young children" or "small children" or toddlers or infants or preschool$ or baby or babies or newborn$ or new born$ or new‐born$ or caregiving or early years or nursery)).tw,kf. 22 ((new or young or "first time") adj (Parents or Mothers or Fathers)).tw,kf. 23 ((child$ or infant$ or babies or toddler$ or famil$) adj3 (raise or raising or rear$ or "bringing up" or "bring up")).tw,kf. 24 or/1‐23 25 child abuse survivor/ or childhood trauma survivor/ or childhood sexual abuse survivor/ 26 child abuse/ or child neglect/ or child sexual abuse/ 27 battered child syndrome/ 28 childhood adversity/ 29 childhood trauma/ 30 exposure to violence/ 31 ((Childhood or children or "as a child" or "as an infant" or "early life") adj3 (abuse or abused or abusive or neglect$ or maltreat$ or incest$ or assault$ or trauma$ or victimi#ed or violen$)).tw,kf. 32 ((witness$ or expos$) adj3 (abuse$1 or abusive or trauma$ or violen$)).tw,kf. 33 ((intergeneration$ or inter‐generation$ or transgeneration$ or trans‐generation$ or famil$) adj3 (abus$ or assault$ or incest$ or maltreat$ or neglect$ or trauma$ or victimi#ed or violence)).tw,kf. 34 (generation$ adj3 (abus$ or assault$ or incest$ or maltreat$ or neglect$ or trauma$ or victimi#ed or violence)).tw,kf. 35 (cycle adj2 (abus$ or trauma$ or neglect$ or maltreat$ or violen$ or posttrauma$ or post‐trauma$ or "toxic stress")).tw,kf. 36 (((Transmission or transmit$) adj2 (generation$ or family pattern$)) and (abus$ or trauma$ or neglect$ or maltreat$ or violen$ or posttrauma$ or post‐trauma$ or "toxic stress")).tw,kf. 37 ((Transmission or transmit$) adj2 (abus$ or trauma$ or neglect$ or maltreat$ or violen$ or posttrauma$ or post‐trauma$ or "toxic stress")).tw,kf. 38 (((break or breaking or breaks or broke) adj3 (cycle$ or pattern$)) and (abus$ or trauma$ or neglect$ or maltreat$ or violen$ or posttrauma$ or post‐trauma$ or "toxic stress")).tw,kf. 39 (Adverse child$ experience$ or adverse child$ event$ or aversive child$ experience$ or child$ adversity or "early life trauma" or traumatic child$ experience).tw,kf. 40 or/25‐39 41 24 and 40 42 (survivor/ or exp anamnesis/) and exp child abuse/ 43 ((History or histories or historic$ or survivor$ or continuity or cycle$ or discontinuity or disclosure or legacy or disclose$ or recovery or unresolved or past) adj3 (abus$ or adversity or maltreat$ or neglect$ or posttrauma$ or post‐trauma$ or stress or trauma$ or violen$)).tw,kf. 44 or/42‐43 45 24 and 44 46 posttraumatic stress disorder/ or sexual trauma/ or mental stress/ 47 psychotrauma/ 48 posttraumatic stress disorder/ or sexual trauma/ or mental stress/ or psychotrauma/ 49 (relational trauma or developmental trauma or toxic stress or trauma‐informed or complex trauma$).tw,kf. 50 or/46‐49 51 24 and 50 52 41 or 45 or 51 53 Randomized controlled trial/ 54 Controlled clinical study/ 55 random$.ti,ab. 56 randomization/ 57 intermethod comparison/ 58 placebo.ti,ab. 59 (compare or compared or comparison).ti. 60 ((evaluated or evaluate or evaluating or assessed or assess) and (compare or compared or comparing or comparison)).ab. 61 (open adj label).ti,ab. 62 ((double or single or doubly or singly) adj (blind or blinded or blindly)).ti,ab. 63 double blind procedure/ 64 parallel group$1.ti,ab. 65 (crossover or cross over).ti,ab. 66 ((assign$ or match or matched or allocation) adj5 (alternate or group$1 or intervention$1 or patient$1 or subject$1 or participant$1)).ti,ab. 67 (assigned or allocated).ti,ab. 68 (controlled adj7 (study or design or trial)).ti,ab. 69 (volunteer or volunteers).ti,ab. 70 human experiment/ 71 trial.ti. 72 or/53‐71 73 (random$ adj sampl$ adj7 ("cross section$" or questionnaire$1 or survey$ or database$1)).ti,ab. not (comparative study/ or controlled study/ or randomi?ed controlled.ti,ab. or randomly assigned.ti,ab.) 74 Cross‐sectional study/ not (randomized controlled trial/ or controlled clinical study/ or controlled study/ or randomi?ed controlled.ti,ab. or control group$1.ti,ab.) 75 (((case adj control$) and random$) not randomi?ed controlled).ti,ab. 76 (Systematic review not (trial or study)).ti. 77 (nonrandom$ not random$).ti,ab. 78 "Random field$".ti,ab. 79 (random cluster adj3 sampl$).ti,ab. 80 (review.ab. and review.pt.) not trial.ti. 81 "we searched".ab. and (review.ti. or review.pt.) 82 "update review".ab. 83 (databases adj4 searched).ab. 84 (rat or rats or mouse or mice or swine or porcine or murine or sheep or lambs or pigs or piglets or rabbit or rabbits or cat or cats or dog or dogs or cattle or bovine or monkey or monkeys or trout or marmoset$1).ti. and animal experiment/ 85 Animal experiment/ not (human experiment/ or human/) 86 or/73‐85 87 72 not 86 88 52 and 87
CINAHL Plus EBSCOhost
S1 (MH "Parents+") S2 (MH "Child Rearing") OR (MH "Parenting Education") OR (MH "Parenting") OR (MH "Intergenerational Relations") OR (MH "Parent‐Child Relations+") OR (MH "Maternal Role") OR (MH "Paternal Behavior") OR (MH "Paternal Attitudes") OR (MH "Maternal Attitudes") OR (MH "Attachment Behavior") S3 (MH "Pregnancy") OR (MH "Attitude to Pregnancy") OR (MH "Pregnancy, Unwanted") OR (MH "Pregnancy, Unplanned") OR (MH "Expectant Mothers") S4 (MH "Obstetric Care") OR (MH "Midwifery") OR (MH "Midwifery Service") OR (MH "Obstetric Nursing") OR (MH "Perinatal Nursing") OR (MH "Labor") S5 TI(parenthood or motherhood or fatherhood or parentificat*) OR AB(parenthood or motherhood or fatherhood or parentificat*) S6 TI((parental or maternal or paternal) N1 (care* or relations* or behavio* or interact* or bonding)) OR AB((parental or maternal or paternal) N1 (care* or relations* or behavio* or interact* or bonding)) S7 TI((parent* or mother* or father*) N5 (Adaptation or adjustment or becoming or become or expect* or Transform* or transition*)) OR AB((parent* or mother* or father*) N5 (Adaptation or adjustment or becoming or become or expect* or Transform* or transition*)) S8 TI((Parents or mothers or fathers) N3 (breastfeed* or "young children" or "small children" or toddlers or infants or preschool* or baby or babies or newborn* or "new born*" or "new‐born*" or caregiving or "early years" or nursery) ) OR AB((Parents or mothers or fathers) N3 (breastfeed* or "young children" or "small children" or toddlers or infants or preschool* or baby or babies or newborn* or "new born*" or "new‐born*" or caregiving or "early years" or nursery) ) S9 TI((new or young or "first time") N1 (parents or mothers or fathers)) OR AB((new or young or "first time") N1 (parents or mothers or fathers)) S10 TI((child* or infant* or babies or toddler* or famil*) N3 (raise or raising or rear* or "bringing up" or "bring up")) OR AB((child* or infant* or babies or toddler* or famil*) N3 (raise or raising or rear* or "bringing up" or "bring up")) S11 TI((antenatal or antepartum or ante‐natal or ante‐partum or birth* or childbirth* or childbearing or conception or parturition or perinatal or peri‐natal or peripartum or peri‐partum or postpartum or post‐partum or postnatal or post‐natal or prenatal or pre‐natal or postnatal or pregnancy or primipara* or primigravid* or trimester*) N3 (care or healthcare or health or service*)) OR AB((antenatal or antepartum or ante‐natal or ante‐partum or birth* or childbirth* or childbearing or conception or parturition or perinatal or peri‐natal or peripartum or peri‐partum or postpartum or post‐partum or postnatal or post‐natal or prenatal or pre‐natal or postnatal or pregnancy or primipara* or primigravid* or trimester*) N3 (care or healthcare or health or service*)) S12 TI(wom?n N2 (birth* or labo#r*)) OR AB(wom?n N2 (birth* or labo#r*)) S13 TI((Pregnan* N1 wom?n) or (Pregnan* N1 (adolescen* or teen*))) OR AB((Pregnan* N1 wom?n) or (Pregnan* N1 (adolescen* or teen*))) S14 S1 OR S2 OR S3 OR S4 OR S5 OR S6 OR S7 OR S8 OR S9 OR S10 OR S11 OR S12 OR S13 S15 (MH "Child Abuse Survivors") S16 (MH "Child Abuse, Sexual") S17 (MH "Adverse Childhood Experiences") S18 (MH "Exposure to Violence") S19 TI((Childhood or children or "as a child" or "as an infant" or "early life") N3 (abuse or abused or abusive or neglect* or maltreat* or incest* or assault* or trauma* or victimi?ed or violen*)) OR AB((Childhood or children or "as a child" or "as an infant" or "early life") N3 (abuse or abused or abusive or neglect* or maltreat* or incest* or assault* or trauma* or victimi?ed or violen*)) S20 TI((witness* or expos*) N3 (abuse* or abusive or trauma* or violen*)) OR AB((witness* or expos*) N3 (abuse* or abusive or trauma* or violen*)) S21 TI((intergeneration* or inter‐generation* or transgeneration* or trans‐generation* or famil*) N3 (abus* or assault* or incest* or maltreat* or neglect* or trauma* or victimi?ed or violence)) OR AB((intergeneration* or inter‐generation* or transgeneration* or trans‐generation* or famil*) N3 (abus* or assault* or incest* or maltreat* or neglect* or trauma* or victimi?ed or violence)) S22 TI(generation* N3 (abus* or assault* or incest* or maltreat* or neglect* or trauma* or victimi?ed or violence)) OR AB(generation* N3 (abus* or assault* or incest* or maltreat* or neglect* or trauma* or victimi?ed or violence)) S23 TI(cycle N2 (abus* or trauma* or neglect* or maltreat* or violen* or posttrauma* or post‐trauma* or "toxic stress")) OR AB(cycle N2 (abus* or trauma* or neglect* or maltreat* or violen* or posttrauma* or post‐trauma* or "toxic stress")) S24 TI(((Transmission or transmit*) N2 (generation* or family pattern*)) and (abus* or trauma* or neglect* or maltreat* or violen* or posttrauma* or post‐trauma* or "toxic stress")) OR AB(((Transmission or transmit*) N2 (generation* or family pattern*)) and (abus* or trauma* or neglect* or maltreat* or violen* or posttrauma* or post‐trauma* or "toxic stress")) S25 TI((Transmission or transmit*) N2 (abus* or trauma* or neglect* or maltreat* or violen* or posttrauma* or post‐trauma* or "toxic stress")) OR AB((Transmission or transmit*) N2 (abus* or trauma* or neglect* or maltreat* or violen* or posttrauma* or post‐trauma* or "toxic stress")) S26 TI (((break or breaking or breaks or broke) N3 (cycle* or pattern*)) and (abus* or trauma* or neglect* or maltreat* or violen* or posttrauma* or post‐trauma* or "toxic stress")) OR AB(((break or breaking or breaks or broke) N3 (cycle* or pattern*)) and (abus* or trauma* or neglect* or maltreat* or violen* or posttrauma* or post‐trauma* or "toxic stress")) S27 TI("Adverse child* experience*" or "adverse child* event*" or "aversive child* experience*" or "child* adversity" or "early life trauma" or "traumatic child* experience") OR AB("Adverse child* experience*" or "adverse child* event*" or "aversive child* experience*" or "child* adversity" or "early life trauma" or "traumatic child* experience") S28 S15 OR S16 OR S17 OR S18 OR S19 OR S20 OR S21 OR S22 OR S23 OR S24 OR S25 OR S26 OR S27 S29 ((MH "Survivors") OR (MH "Self Disclosure") OR (MH "Patient History Taking+") AND (MH "Child Abuse+") S30 TI((History or histories or historic* or survivor* or continuity or cycle* or discontinuity or disclosure or legacy or disclose* or recovery or unresolved or past) N3 (abus* or adversity or maltreat* or neglect* or posttrauma* or post‐trauma* or stress or trauma* or violen*)) OR AB((History or histories or historic* or survivor* or continuity or cycle* or discontinuity or disclosure or legacy or disclose* or recovery or unresolved or past) N3 (abus* or adversity or maltreat* or neglect* or posttrauma* or post‐trauma* or stress or trauma* or violen*)) S31 S29 OR S30 S32 (MH "Stress Disorders, Post‐Traumatic") OR (MH "Stress, Psychological") S33 TI(("Post‐traumatic stress*" or "Post traumatic stress*" or PTSD) N5 (abus* or adversity or maltreat* or neglect* or posttrauma* or post‐trauma* or stress or trauma* or violen*)) OR AB(("Post‐traumatic stress*" or "Post traumatic stress*" or PTSD) N5 (abus* or adversity or maltreat* or neglect* or posttrauma* or post‐trauma* or stress or trauma* or violen*)) S34 TI("relational trauma" or "developmental trauma" or "toxic stress" or "trauma‐informed" or "complex trauma*") OR AB("relational trauma" or "developmental trauma" or "toxic stress" or "trauma‐informed" or "complex trauma*") S35 S32 OR S33 OR S34 S36 S14 AND (S28 OR S31 OR S35) S37 MH ("Randomized controlled trials") or MH(" double‐blind studies") OR MH ("single‐blind studies") OR MH(" random assignment") OR MH( "pretest‐posttest design") OR MH ("cluster sample") or MH (placebos) or MH ("crossover design") OR MH ("comparative studies") or PT("randomized controlled trial") S38 TI (randomised OR randomized) OR AB (random*) OR AB(control W5 group) or AB (cluster W3 RCT) OR TI (trial) OR (MH (sample size) AND AB (assigned OR allocated OR control)) S39 S37 OR S38 S40 (MH (animals+) or MH (animal studies) or TI (animal model*) ) NOT MH (human) S41 S39 NOT S40 S42 S36 AND S41
APA PsycInfo Ovid
1 parents/ or exp adoptive parents/ or expectant parents/ or exp fathers/ or exp mothers/ or exp single parents/ 2 exp Childrearing Attitudes/ or exp Childrearing Practices/ or exp Parenting/ or exp Parenting Style/ 3 exp parent child relations/ 4 intergenerational relations/ 5 attachment behavior/ 6 exp pregnancy/ or *birth/ or childbirth training/ or perinatal period/ or postnatal period/ or exp prenatal care/ 7 exp "labor (childbirth)"/ or exp intrapartum period/ 8 midwifery/ 9 Obstetrics/ and Nursing/ 10 (parenthood or motherhood or fatherhood or parentificat$).tw. 11 ((parental or maternal or paternal) adj (care$ or relations$ or behavio$ or interact$ or bonding)).tw. 12 ((parent$ or mother$ or father$) adj5 (Adaptation or Adjustment or becoming or become or expect$ or Transform$ or transition$)).tw. 13 ((Parents or Mothers or Fathers) and (breastfeed$ or "young children" or "small children" or toddlers or infants or preschool$ or baby or babies or newborn$ or new born$ or new‐born$ or caregiving or early years or nursery)).tw. 14 ((Parents or Mothers or Fathers) and (breastfeed$ or breast feed$ or "young children" or "small children" or toddlers or infants or preschool$ or baby or babies or newborn$ or new born$ or new‐born$ or caregiving or early years or nursery)).tw. 15 ((new or young or "first time") adj (Parents or Mothers or Fathers)).tw. 16 ((child$ or infant$ or babies or toddler$ or famil$) adj3 (raise or raising or rear$ or "bringing up" or "bring up")).tw. 17 ((antenatal or antepartum or ante‐natal or ante‐partum or birth$ or childbirth$ or childbearing or conception or parturition or perinatal or peri‐natal or peripartum or peri‐partum or postpartum or post‐partum or postnatal or post‐natal or prenatal or pre‐natal or postnatal or pregnancy or primipara$ or primigravid$ or trimester$) adj3 (care or healthcare or health or service$)).tw. 18 (wom#n adj2 (birth$ or labour$ or labo?r$)).tw. 19 ((Pregnan$ adj3 wom#n) or (Pregnan$ adj3 (adolescen$ or teen$))).tw. 20 or/1‐19 21 exp Child Abuse/ 22 Battered Child Syndrome/ 23 exposure to violence/ 24 childhood adversity/ 25 survivors/ and Sexual Abuse/ ) 26 ((Childhood or children or "as a child" or "as an infant" or "early life") adj3 (abuse or abused or abusive or neglect$ or maltreat$ or incest$ or assault$ or trauma$ or victimi#ed or violen$)).tw. 27 ((witness$ or expos$) adj3 (abuse$1 or abusive or trauma$ or violen$)).tw. 28 ((intergeneration$ or inter‐generation$ or transgeneration$ or trans‐generation$ or famil$) adj3 (abus$ or assault$ or incest$ or maltreat$ or neglect$ or trauma$ or victimi#ed or violence)).tw. 29 (generation$ adj3 (abus$ or assault$ or incest$ or maltreat$ or neglect$ or trauma$ or victimi#ed or violence)).tw. 30 (cycle adj2 (abus$ or trauma$ or neglect$ or maltreat$ or violen$ or posttrauma$ or post‐trauma$ or "toxic stress")).tw. 31 (((Transmission or transmit$) adj2 (generation$ or family pattern$)) and (abus$ or trauma$ or neglect$ or maltreat$ or violen$ or posttrauma$ or post‐trauma$ or "toxic stress")).tw. 32 ((Transmission or transmit$) adj2 (abus$ or trauma$ or neglect$ or maltreat$ or violen$ or posttrauma$ or post‐trauma$ or "toxic stress")).tw. 33 (((break or breaking or breaks or broke) adj3 (cycle$ or pattern$)) and (abus$ or trauma$ or neglect$ or maltreat$ or violen$ or posttrauma$ or post‐trauma$ or "toxic stress")).tw. 34 (Adverse child$ experience$ or adverse child$ event$ or aversive child$ experience$ or child$ adversity or "early life trauma" or traumatic child$ experience).tw. 35 or/21‐34 36 20 and 35 37 (Survivors/ or Self‐Disclosure/ or Patient History/) and exp child abuse/ 38 ((History or histories or historic$ or survivor$ or continuity or cycle$ or discontinuity or disclosure or legacy or disclose$ or recovery or unresolved or past) adj3 (abus$ or adversity or maltreat$ or neglect$ or posttrauma$ or post‐trauma$ or stress or trauma$ or violen$)).tw. 39 37 or 38 40 20 and 39 41 posttraumatic stress disorder/ or complex ptsd/ or posttraumatic stress/ or trauma‐informed care/ or trauma/ or "stress and trauma related disorders"/ 42 (relational trauma or developmental trauma or toxic stress or trauma‐informed or complex trauma$).tw. 43 (Post‐traumatic stress$ or Post traumatic stress$ or PTSD).tw. 44 or/41‐43 45 20 and 44 46 36 or 40 or 45 47 randomized controlled trials/ 48 clinical trials/ 49 treatment effectiveness evaluation/ 50 exp treatment outcomes/ 51 followup studies/ 52 longitudinal studies/ 53 Placebo/ 54 Experiment Controls/ 55 exp program evaluation/ 56 (randomis$ or randomiz$).tw. 57 placebo.ab. 58 (control$ adj (experiment$ or trial$)).tw. 59 (TAU or "treatment as usual" or "usual care" or "wait$ list").ab. 60 (random$ adj3 (allocat$ or assign$)).ab. 61 or/47‐60 62 46 and 61
Web of Science Core Collection databases (Science Citation Index, Social Science Citation Index, Conference Proceedings Citation Index ‐ Science, Conference Proceedings Citation Index ‐ Social Sciences & Humanities)
# 28 #27 AND #26 # 27 TS=(random* OR control* OR RCT* OR placebo* OR blind* OR longitudinal or prospective or TAU or "usual care" or "treatment as usual") # 26 #25 OR #21 OR #19 # 25 #24 AND #9 # 24 #23 OR #22 # 23 TI=("relational trauma" or "developmental trauma" or "toxic stress" or" trauma informed "or "complex trauma*") OR AB=("relational trauma" or "developmental trauma" or "toxic stress" or" trauma informed "or "complex trauma*") # 22 (TI=("Post traumatic stress*" or "Posttraumatic stress*" or PTSD) OR AB=("Post traumatic stress*" or "Posttraumatic stress*" or PTSD)) AND (TI=(abus* or assault* or incest* or maltreat* or neglect* or trauma* or victimi*ed or violence) or AB=(abus* or assault* or incest* or maltreat* or neglect* or trauma* or victimi*ed or violence) ) # 21 #20 AND #9 # 20 TI=((History or histories or historic* or survivor* or continuity or cycle* or discontinuity or disclosure or legacy or disclose* or recovery or unresolved or past) NEAR/3 (abus* or adversity or maltreat* or neglect* or posttrauma* or "post trauma*" or stress or trauma* or violen*) ) OR AB=((History or histories or historic* or survivor* or continuity or cycle* or discontinuity or disclosure or legacy or disclose* or recovery or unresolved or past) NEAR/3 (abus* or adversity or maltreat* or neglect* or posttrauma* or "post trauma*" or stress or trauma* or violen*) ) # 19 #18 AND #9 # 18 #17 OR #16 OR #15 OR #14 OR #13 OR #12 OR #11 OR #10 # 17 TI=("Adverse child* experience*" or "adverse child* event*" or "aversive child* experience*" or "child* adversity" or "early life trauma" or "traumatic child* experience") OR AB=("Adverse child* experience*" or "adverse child* event*" or "aversive child* experience*" or "child* adversity" or "early life trauma" or "traumatic child* experience") # 16 TI=(((break or breaking or breaks or broke) NEAR/3 (cycle* or pattern*) ) and (abus* or trauma* or neglect* or maltreat* or violen* or posttrauma* or "post trauma*" or "toxic stress") ) # 15 TI=(((Transmission or transmit*) NEAR/2 (generation* or "family pattern*") ) and (abus* or trauma* or neglect* or maltreat* or violen* or posttrauma* or "post trauma*" or "toxic stress") ) OR AB=(((Transmission or transmit*) NEAR/2 (generation* or "family pattern*") ) and (abus* or trauma* or neglect* or maltreat* or violen* or posttrauma* or "post trauma*" or "toxic stress") ) # 14 TI=(cycle NEAR/2 (abus* or trauma* or neglect* or maltreat* or violen* or posttrauma* or "post trauma*" or "toxic stress") ) OR AB=(cycle NEAR/2 (abus* or trauma* or neglect* or maltreat* or violen* or posttrauma* or "post trauma*" or "toxic stress") ) # 13 TI=(generation* NEAR/3 (abus* or assault* or incest* or maltreat* or neglect* or trauma* or victim*ed or violence) ) OR AB=(generation* NEAR/3 (abus* or assault* or incest* or maltreat* or neglect* or trauma* or victim*ed or violence) ) # 12 TI=((intergeneration* or "inter generation*" or transgeneration* or "trans generation*" or famil*) NEAR/3 (abus* or assault* or incest* or maltreat* or neglect* or trauma* or victimi*ed or violence) ) OR AB=((intergeneration* or "inter generation*" or transgeneration* or "trans generation*" or famil*) NEAR/3 (abus* or assault* or incest* or maltreat* or neglect* or trauma* or victimi*ed or violence) ) # 11 TI= ((witness* or expos*) NEAR/3 (abuse* or abusive or trauma* or violen*) ) OR AB=((witness* or expos*) NEAR/3 (abuse* or abusive or trauma* or violen*) ) # 10 TI=((Childhood or children or "as a child" or "as an infant" or "early life") NEAR/3 (abuse or abused or abusive or neglect* or maltreat* or incest* or assault* or trauma* or victimi*ed or violen*) ) OR AB=((Childhood or children or "as a child" or "as an infant" or "early life") NEAR/3 (abuse or abused or abusive or neglect* or maltreat* or incest* or assault* or trauma* or victimi*ed or violen*) ) # 9 #8 OR #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1 # 8 TI=((Pregnan* NEAR/3 wom*n) or (Pregnan* NEAR/3 (adolescen* or teen*) )) # 7 TI=(wom*n NEAR/2 (birth* or labour* or labor*) ) # 6 TI=((antenatal or antepartum or "ante natal" or "ante partum" or birth* or childbirth* or childbearing or conception or parturition or perinatal or "peri natal" or postpartum or "post partum" or postnatal or "post natal" or prenatal or "pre natal" or postnatal or pregnancy or primipara* or primigravid* or trimester*) NEAR/3 (care or healthcare or health or service*) ) OR AB=((antenatal or antepartum or "ante natal" or "ante partum" or birth* or childbirth* or childbearing or conception or parturition or perinatal or "peri natal" or postpartum or "post partum" or postnatal or "post natal" or prenatal or "pre natal" or postnatal or pregnancy or primipara* or primigravid* or trimester*) NEAR/3 (care or healthcare or health or service*) ) # 5 TI=((new or young or "first time") AND (Parents or Mothers or Fathers) ) # 4 TI=((Parents or mothers or fathers) NEAR/3 (breastfeed* or "breast feed*" or "young children" or "small children" or toddlers or infants or preschool* or "pre school*" or baby or babies or newborn* or "new born*" or caregiving or "early years" or nursery) ) OR AB=((Parents or mothers or fathers) NEAR/3 (breastfeed* or "breast feed*" or "young children" or "small children" or toddlers or infants or preschool* or "pre school*" or baby or babies or newborn* or "new born*" or caregiving or "early years" or nursery) ) # 3 TI=((parent* or mother* or father*) NEAR/3 (Adaptation or adjustment or becoming or become or expect* or Transform* or transition*) ) OR AB=((parent* or mother* or father*) NEAR/3 (Adaptation or adjustment or becoming or become or expect* or Transform* or transition*) ) # 2 TI=((parental or maternal or paternal) NEAR/1 (care* or relations* or behavio* or interact* or bonding) ) OR AB=((parental or maternal or paternal) NEAR/1 (care* or relations* or behavio* or interact* or bonding) ) OR AK=((parental or maternal or paternal) NEAR/1 (care* or relations* or behavio* or interact* or bonding) ) # 1 TI= (parenthood or motherhood or fatherhood or parentificat*)
Cochrane Database of Systematic Reviews (CDSR)
#1 [mh parents] or [mh ^"single‐parent family"] #2 [mh "Child Rearing"] or [mh "father‐child relations"] or [mh "intergenerational relations"] or [mh "maternal behavior"] or [mh "maternal deprivation"] or [mh "mother‐child relations"] or [mh "maternal‐fetal relations"] or [mh "parent‐child relations"] or [mh parenting] or [mh "paternal behavior"] or [mh "paternal deprivation"] #3 [mh pregnancy] or [mh "pregnancy, unplanned"] or [mh "pregnancy, unwanted"] or [mh "Pregnant Women"] #4 [mh "perinatal care"] or [mh "peripartum period"] or [mh "postnatal care"] or [mh "postpartum period"] or [mh "Preconception Care"] or [mh "prenatal care"] #5 [mh "Labor, Obstetric"] or [mh "Delivery, obstetric"] or [mh midwifery] or [mh "Obstetric nursing"] #6 (parenthood or motherhood or fatherhood or parentificat*) #7 ((parental or maternal or paternal) NEXT(care* or relations* or behavio* or interact* or bonding)):TI,AB #8 ((parent* or mother* or father*) NEAR/5 (Adaptation or adjustment or becoming or become or expect* or Transform* or transition*)):TI,AB #9 ((Parents or mothers or fathers) NEAR/5 (breastfeed* or breast NEXT feed* or young NEXT children or small NEXT children or toddlers or infants or preschool* or pre NEXT school* or baby or babies or newborn* or new NEXT born* or caregiving or early NEXT years or nursery)):TI,AB #10 ((new or young or "first time") NEXT(Parents or Mothers or Fathers)):TI,AB #11 ((child* or infant* or babies or toddler* or famil*) NEAR/3 (raise or raising or rear* or "bringing up" or "bring up")):TI,AB #12 ((antenatal or antepartum or ante NEXT natal or ante NEXTpartum or birth* or childbirth* or childbearing or conception or parturition or perinatal or peri NEXT natal or postpartum or post NEXT partum or postnatal or post NEXT natal or prenatal or pre NEXT natal or postnatal or pregnancy or primipara* or primigravid* or trimester*) NEAR/3 (care or healthcare or health or service*)):TI,AB #13 (wom*n NEAR/2 (birth* or labour* or labor*)):TI,AB #14 (Pregnan* NEAR/3 wom*n) or (Pregnan* NEAR/3 (adolescen* or teen*)):TI,AB #15 {or #1‐#14} #16 [mh "Adult survivors of child abuse"] #17 [mh "Adult Survivors of Child Adverse Events"] #18 [mh "child abuse"] #19 [mh "Battered Child Syndrome"] #20 [mh "adverse childhood experiences"] #21 [mh "Exposure to violence"] #22 ((Childhood or children or "as a child" or "as an infant" or "early life") NEAR/3 (abuse or abused or abusive or neglect* or maltreat* or incest* or assault* or trauma* or victimi*ed or violen*)):TI #23 ((witness* or expos*) NEAR/3 (abuse* or abusive or trauma* or violen*)):TI #24 ((intergeneration* or inter NEXT generation* or transgeneration* or trans NEXT generation* or famil*) NEAR/3 (abus* or assault* or incest* or maltreat* or neglect* or trauma* or victimi*ed or violence)):TI #25 (generation* NEAR/3 (abus* or assault* or incest* or maltreat* or neglect* or trauma* or victim*ed or violence)):TI #26 (cycle NEAR/2 (abus* or trauma* or neglect* or maltreat* or violen* or posttrauma* or post NEXT trauma* or toxic NEXT stress)):TI #27 ((Transmission or transmit*) NEAR/2 (generation* or family NEXT pattern*)) and (abus* or trauma* or neglect* or maltreat* or violen* or posttrauma* or post NEXT trauma* or toxic NEXT stress):TI #28 ((Transmission or transmit*) NEAR/2 (abus* or trauma* or neglect* or maltreat* or violen* or posttrauma* or post NEXT trauma* or toxic NEXT stress)):TI #29 ((break or breaking or breaks or broke) NEAR/3 (cycle* or pattern*)) and (abus* or trauma* or neglect* or maltreat* or violen* or posttrauma* or post NEXT trauma* or toxic NEXT stress):TI #30 (Adverse NEXT child* NEXT experience* or adverse NEXT child* NEXT event* or aversive NEXT child* NEXT experience* or child* NEXT adversity or early NEXT life NEXT trauma or traumatic NEXT child* NEXT experience):TI #31 {or #16‐#30} #32 #15 and #31 #33 ( [mh survivors] or [mh disclosure] or [mh "medical history taking"]) and [mh "child abuse"] #34 ((History or histories or historic* or survivor* or continuity or cycle* or discontinuity or disclosure or legacy or disclose* or recovery or unresolved or past) NEAR/3 (abus* or adversity or maltreat* or neglect* or posttrauma* or post NEXT trauma* or stress or trauma* or violen*)):TI #35 {or #33‐#34} #36 #15 AND #35 #37 MeSH descriptor: [Stress, Psychological] this term only #38 MeSH descriptor: [Stress Disorders, Post‐Traumatic] explode all trees #39 (Post NEXT traumatic NEXT stress* or Posttraumatic NEXT stress* or PTSD):TI #40 (relational NEXT trauma or developmental NEXT trauma or toxic NEXT stress or trauma NEXT informed or complex NEXT trauma*):TI #41 {or #37‐#40} #42 #15 AND #41 #43 #32 OR #36 OR #42 in Cochrane Reviews, Cochrane Protocols
PTSDPubs ProQuest
(MAINSUBJECT.EXACT("Pregnancy") OR MAINSUBJECT.EXACT("Childbirth") OR MAINSUBJECT.EXACT("Single Parents") OR MAINSUBJECT.EXACT("Parents") OR MAINSUBJECT.EXACT("Intergenerational Effects") OR MAINSUBJECT.EXACT("Midwifery") OR TI(parenthood or motherhood or fatherhood or parentificat*) OR AB(parenthood or motherhood or fatherhood or parentificat*) OR TI((parental or maternal or paternal) NEAR/1 (care* or relations* or behavio* or interact* or bonding)) OR AB((parental or maternal or paternal) NEAR/1 (care* or relations* or behavio* or interact* or bonding)) OR TI((parent* or mother* or father*) NEAR/5 (Adaptation or adustment or becoming or become or expect* or Transform* or transition*)) OR AB((parent* or mother* or father*) NEAR/5 (Adaptation or adustment or becoming or become or expect* or Transform* or transition*)) OR TI((Parents or mothers or fathers) NEAR/3 (breastfeed* or "young children" or "small children" or toddlers or infants or preschool* or baby or babies or newborn* or "new born*" or "new‐born*" or caregiving or "early years" or nursery) ) OR AB((Parents or mothers or fathers) NEAR/3 (breastfeed* or "young children" or "small children" or toddlers or infants or preschool* or baby or babies or newborn* or "new born*" or "new‐born*" or caregiving or "early years" or nursery) ) OR TI((new or young or "first time") NEAR/1 (parents or mothers or fathers)) OR AB((new or young or "first time") NEAR/1 (parents or mothers or fathers)) OR TI((child* or infant* or babies or toddler* or famil*) NEAR/3 (raise or raising or rear* or "bringing up" or "bring up")) OR AB((child* or infant* or babies or toddler* or famil*) NEAR/3 (raise or raising or rear* or "bringing up" or "bring up")) OR TI((antenatal or antepartum or ante‐natal or ante‐partum or birth* or childbirth* or childbearing or conception or parturition or perinatal or peri‐natal or peripartum or peri‐partum or postpartum or post‐partum or postnatal or post‐natal or prenatal or pre‐natal or postnatal or pregnancy or primipara* or primigravid* or trimester*) NEAR/3 (care or healthcare or health or service*)) OR AB((antenatal or antepartum or ante‐natal or ante‐partum or birth* or childbirth* or childbearing or conception or parturition or perinatal or peri‐natal or peripartum or peri‐partum or postpartum or post‐partum or postnatal or post‐natal or prenatal or pre‐natal or postnatal or pregnancy or primipara* or primigravid* or trimester*) NEAR/3 (care or healthcare or health or service*)) OR TI(wom*n NEAR/2 (birth* or labor or labour)) OR AB(wom*n Near/2 (birth* or labor* or labour)) OR TI((Pregnan* NEAR/1 wom*n) or (Pregnan* NEAR/1 (adolescen* or teen*))) OR AB((Pregnan* NEAR/1 wom*n) or (Pregnan* NEAR/1 (adolescen* or teen*)))) AND (MAINSUBJECT.EXACT.EXPLODE("Clinical Trial") OR TI(TRIAL OR RANDOMLY OR RAND0MI*ED OR RCT) OR AB (trial or random* or control* or group* or cluster* or placebo* or trial* or assign* or allocat* or RCT))
EPISTEMONIKOS
title:(abus* OR trauma* OR neglect* OR maltreat* OR violen* OR posttrauma* OR "post traumatic" OR PTSD OR "toxic stress") AND title:(pregnan* OR pre‐pregnan* OR birth OR labour OR labor OR prenatal* OR pre‐natal* OR peri‐natal OR perinatal OR antenatal OR ante‐natal OR postnatal* OR post‐natal* OR childbirth OR parent* OR mother* OR father*)
Publication type: Systematic review
ClinicalTrials.gov
Interventional Studies | abuse OR survivor | birth OR pregnancy OR perinatal OR prenatal OR postnatal OR parent OR mother OR father
WHO ICTRP
(child AND maltreat OR child AND abuse OR abuse AND survivor OR adult AND survivor OR child AND trauma) AND (birth OR pregnancy OR perinatal OR prenatal OR postnatal OR parent OR mother OR father)
Appendix 2. Example data extraction form
| 1. Study identifiers and characteristics of the study design |
|
| 2. Participant characteristics |
|
| 3. Characteristics of intervention and control (comparator) intervention for parents |
|
| 4. Outcomes |
|
| 5. Other information |
|
| ID: identifier; PROGRESS+: place of residence, race/ethnicity/culture/language, occupation, gender/sex, religion, education, socioeconomic status, social capital; and personal characteristics associated with discrimination (e.g. age), features of relationships (e.g. parents who smoke), and time‐dependent relationships (e.g. leaving hospital). | |
Appendix 3. Glossary of terms
| Term | Acronym | Definition |
| Adverse childhood experiences | ACEs | ACE refers to some of the most intensive and frequently occurring sources of stress that children may experience early in life. Such experiences include multiple types of abuse; neglect; violence between parents or carers; other types of serious household dysfunction such as alcohol and substance abuse; and peer, community and collective violence (WHO 2018a). |
| Child–parent psychotherapy | CPP | CPP is an intervention model for children aged 0 to 5 years who:
The treatment is based in attachment theory but also integrates psychodynamic, developmental, trauma, social learning and cognitive behavioural theories. Therapeutic sessions include the child and parent or primary carer. The primary goal of CPP is to support and strengthen the relationship between a child and his or her carer as a vehicle for restoring the child's cognitive, behavioural and social functioning. Treatment also focuses on contextual factors that may affect the carer–child relationship (Lieberman 2004; NCTSN 2012). |
| Cognitive behavioural therapy | CBT | CBT is a form of psychological treatment that has been demonstrated to be effective for a range of problems, including depression, anxiety disorders, alcohol and drug use problems, marital problems, eating disorders and severe mental illness. Numerous research studies suggest that CBT leads to significant improvement in functioning and quality of life. In many studies, CBT has been as effective as, or more effective than, other forms of psychological therapy or psychiatric medications. CBT is based on several core principles, including:
CBT treatment usually involves efforts to change thinking patterns; strategies might include:
CBT treatment usually involves efforts to change behavioural patterns; strategies might include:
|
| Hyperarousal | — | Hyperarousal is the abnormally heightened state of anxiety, which occurs whenever you think about a traumatic event. It is 1 of 3 sets of criteria used to diagnose post‐traumatic stress disorder and acute stress disorder. Symptoms of hyperarousal include exaggerated startle response, disturbed sleep, difficulty in concentrating or remembering, and excessive vigilance (APA 2020). |
| Hypervigilance | — | Hypervigilance is 1 hyperarousal symptom of post‐traumatic stress disorder, which manifests as a need to always scan the surroundings for potential threats. The result of constantly being on alert can be inappropriate (or even aggressive) reactions in everyday situations. Those displaying hypervigilance can be so involved in their scrutiny of what is around them, that they tend to ignore their family and friends. They may overreact to loud sounds and bangs, unexpected noises, smells, etc. Even familiar surroundings and people can be an issue as hypervigilance can make people acutely aware of subtle details normally ignored, e.g. body language, a person's voice and tone, their mood, their expressions – all things that are continually assessed. Some common behaviours of hypervigilance are:
|
| Parenting capacity | — | Parenting capacity is defined as the ability of parents or carers to ensure that the child's developmental needs are being appropriately and adequately responded to, and to be able to adapt to their child/ren's changing needs over time (Budd 1996). |
| Parent–infant attachment | — | Parent–infant attachment is 1 unique aspect of the emotional relationship between a child and a parent (carer), with its purpose being to make a child safe, secure and protected. Attachment is distinguished from other aspects of parenting, such as disciplining, entertaining and teaching. It is a key factor in the way an infant's brain organises itself and how the child develops socially, emotionally, intellectually and physically. Observations of parent–infant attachment include the attitudes and behaviours of parents towards their children, in addition to the reciprocity (exchange of positive emotions and mutually satisfying behaviour) that occurs in the interactional process and the situational factors that may influence the relationship (Bell 1998; Belsky 1980; Benoit 2004; Bowlby 1988). |
| Parenting self‐efficacy | PSE | Parenting self‐efficacy is a cognitive construct, which refers to the parent's (carer's) confidence about their ability to successfully raise children. Jones and Prinz (2005) define PSE as the expectation carers hold about their ability to parent successfully. PSE is important as it relates to family functioning (Jones 2005; Wittkowski 2017). |
| Power Threat Meaning Framework | PTMF | The PTMF is a new perspective on why people sometimes experience a whole range of forms of distress, confusion, fear, despair and troubled or troubling behaviour. It is an alternative to the more traditional models based on psychiatric diagnosis. The main aspects of the PTMF are summarised in the following questions, which can apply to individuals, families or social groups.
An additional 2 questions help to think about the skills and resources people might have, and how these ideas and responses can be pulled together into a personal narrative or story.
|
| PROGRESS–Plus | PROGRESS+ | PROGRESS refers to the following.
Plus refers to:
|
| Psycho‐educational programme | — | Psycho‐educational parenting programmes can be utilised as a universal approach to teach problem‐solving and communication skills and provide education and resources. Brief psycho‐educational interventions providing information can be effective in reducing symptoms of psychological distress and support parents with stress (Missler 2020). |
| Trauma‐informed care | TIC | TIC is an approach based on knowledge of the impact of trauma, aimed at ensuring environments and services are welcoming and engaging for service recipients and staff. TIC is a strengths‐based framework grounded in an understanding of and responsiveness to the impact of trauma, which emphasises physical, psychological and emotional safety for everyone, and which creates opportunities for survivors to rebuild a sense of control and empowerment. A programme, organisation or system that is trauma informed:
|
| Trauma‐focused cognitive behavioural therapy | TF‐CBT | TF‐CBT was developed by Cohen, Mannarino and Deblinger. It is a parent–child treatment, which uses cognitive behavioural principles and exposure techniques to prevent and treat post‐traumatic stress, depression and behavioural problems. The goal of TF‐CBT is to reduce post‐traumatic stress disorder symptoms (De Arellano 2014; Deblinger 2003). |
Data and analyses
Comparison 1. Parenting interventions vs inactive control.
Comparison 2. Psychological interventions vs inactive control.
Comparison 3. Service system approaches vs inactive control.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Ammerman 2016.
| Study characteristics | |
| Methods |
|
| Participants |
|
| Interventions |
Intervention ‐ In‐Home Cognitive Behavioural Therapy (IH‐CBT)
Comparator ‐ standard home visiting
|
| Outcomes |
Assessment time point(s)
Primary outcome(s) Parental psychological wellbeing
Parents' relationship quality
Parenting skills
Secondary outcome(s) Parent engagement
Parental social functioning
Cost or cost‐effectiveness
Adverse outcome(s): none specified |
| Notes |
Comment(s)
Funding source: The National Institute of Mental Health Conflicts of interest: the authors declared that there were no conflicts of interest |
Berry 2021.
| Study characteristics | |
| Methods |
|
| Participants |
|
| Interventions |
Intervention ‐ Practical Resources for Effective Postpartum Parenting (PREPP)
Comparator ‐ enhanced treatment as usual
|
| Outcomes |
Assessment time point(s)
Note: Assessments were also conducted at 10 weeks postpartum and 16 weeks postpartum; however, results from these time points are not reported Primary outcome(s) Parental psychological wellbeing
Secondary outcome(s) Parent engagement
Child emotional and behavioural outcomes
Adverse outcome(s): none specified |
| Notes |
Comment(s)
Funding source: National Institute of Mental Health; the Eunice Kennedy Shriver National Institute of Child Health and Human Development; the Robinhood Foundation Conflicts of interest: the authors declared that there were no conflicts of interest |
Blalock 2013.
| Study characteristics | |
| Methods |
|
| Participants |
|
| Interventions |
Intervention ‐ Cognitive Behavioural Analysis System of Psychotherapy (CBASP)
Comparator ‐ Health and Wellness control (HW)
|
| Outcomes |
Assessment time point(s)
Note: Assessments were also conducted at 2, 4 and 6 weeks post‐intervention, 2 weeks postpartum and 3 months postpartum; however, results from these time points are not reported Primary outcome(s) Parental psychological wellbeing
Substance use
Secondary outcome(s): Parent engagement
Adverse outcome(s): none specified |
| Notes |
Comment(s)
Funding source: National Institute on Drug Abuse Conflicts of interest: the authors did not report if there were any conflicts of interest |
Booshehri 2018.
| Study characteristics | |
| Methods |
|
| Participants |
|
| Interventions |
Intervention 1 ‐ Building Wealth and Health Network (partial)
Intervention 2 ‐ Building Wealth and Health Network (full)
Comparator ‐ treatment as usual
|
| Outcomes |
Assessment time point(s)
Primary outcome(s) Parental psychological wellbeing
Secondary outcome(s) Parent engagement
Changes in social capital
Child developmental outcomes
Adverse outcome(s): none specified |
| Notes |
Comment(s)
Funding source: Claneil Foundation, Inc, Annie E Casey Foundation, First Hospital, and TD Bank. Annie E. Casey Foundation provided partial guidance in the study design Conflicts of interest: The authors declared that there were no conflicts of interest. |
Cicchetti 2006.
| Study characteristics | |
| Methods |
|
| Participants |
|
| Interventions |
Intervention 1 ‐ Infant‐parent psychotherapy (IPP), called child‐parent psychotherapy (CPP) in Stronach 2013
Intervention 2 ‐ psycho‐educational parenting intervention (PPI)
Comparator 1 ‐ community standard (CS)
Comparator 2 ‐ Non‐maltreatment comparison group
|
| Outcomes |
Assessment time point(s)
Primary outcome(s) Parent‐child relationship
Secondary outcome(s) Parent engagement
Child emotional and behavioural outcomes
Adverse outcome(s): none specified |
| Notes |
Comment(s)
Funding source: Administration of Children, Youth, and Families; the National Institute of Mental Health; the Spunk Fund, Inc Conflicts of interest: The authors did not report if there were any conflicts of interest. |
Grote 2012.
| Study characteristics | |
| Methods |
|
| Participants |
|
| Interventions |
Intervention ‐ brief interpersonal psychotherapy (IPT‐B)
Comparator ‐ enhanced treatment as usual (ETAU)
|
| Outcomes |
Assessment time point(s)
Primary outcome(s) Parental complex trauma symptoms
Parental psychological wellbeing
Secondary outcome(s) Parent engagement
Parental social functioning
Adverse outcome(s): none specified |
| Notes |
Comment(s)
Funding source: National Institute of Mental Health; the Staunton Farm Foundation; the General Clinical Research Centres (National Centre for Research Resources) Conflict of interest: the trial authors made the following declarations in the conflicts of interest statement: "Dr. Grote, Dr. Spieker, Ms. Lohr, and Ms. Geibel report no competing interests. Dr. Swartz has received CME honoraria from Servier, Astra Zeneca, and Sanofi. She receives royalties from UpToDate. Dr. Frank serves on an advisory board and has received honoraria from Servier, International and receives royalties from Guilford Press and the American Psychological Association Press. Dr. Katon serves on an advisory board at Lilly and has received honoraria from Lilly, Forest, and Pfizer." (Grote 2012, page 564) |
Grote 2015.
| Study characteristics | |
| Methods |
|
| Participants |
|
| Interventions |
Intervention ‐ MOMCare + Maternity Support Services‐PLUS (MSS‐PLUS)
Comparator ‐ Maternity Support Services‐PLUS (MSS‐PLUS)
|
| Outcomes |
Assessment time point(s)
Note: at 3‐month follow‐up, 88% of mothers still pregnant; 6‐month follow‐up, 3 months postpartum; 12‐month follow‐up, mean 9 months postpartum; 18‐month follow‐up, mean 15 months postpartum Primary outcome(s) Parental complex trauma symptoms
Parental psychological wellbeing
Secondary outcome(s) Parent engagement
Cost or cost‐effectiveness
Adverse outcome(s): none specified |
| Notes |
Comment(s)
Funding source: National Institute of Mental Health Conflicts of interest: the authors declared that there were no conflicts of interest |
Haight 2005.
| Study characteristics | |
| Methods |
|
| Participants |
|
| Interventions |
Intervention ‐ emotional support/coaching
Comparator ‐ wait‐list
|
| Outcomes |
Assessment time point(s)
Primary outcome(s) Parenting skills
Secondary outcome(s): Parent engagement
Adverse outcome(s): none specified |
| Notes |
Comment(s): no unpublished data requested or reported in meta‐analyses Funding source: Children and Family Research Centre Conflicts of interest: the authors did not report if there were any conflicts of interest |
Liu 2021.
| Study characteristics | |
| Methods |
|
| Participants |
|
| Interventions |
Intervention ‐ Filming Interactions to Nurture Development (FIND) + standard EHS services
Comparator ‐ Early Head Start (EHS) programme
|
| Outcomes |
Assessment time point(s)
Primary outcome(s) Parenting skills
Secondary outcome(s) Parent engagement
Child emotional and behavioural outcomes
Adverse outcome(s): none specified |
| Notes |
Comment(s)
Funding source: Administration for Children and Families Conflicts of interest: the authors declared that there were no conflicts of interests |
Madigan 2015.
| Study characteristics | |
| Methods |
|
| Participants |
|
| Interventions |
Intervention ‐ trauma‐focused (TF‐CBT) + TAU (parenting course)
Comparator ‐ parenting course
|
| Outcomes |
Assessment time point(s)
Note: behavioural problems only assessed at baseline and 12‐month follow‐up, and disorganised infant attachment only assessed at 12‐month follow‐up Primary outcome(s) Parental complex trauma symptoms
Parental psychological wellbeing
Parent‐child relationship
Secondary outcome(s): Parent engagement
Adverse outcome(s): none specified |
| Notes |
Comment(s):
Funding source: Ontario Mental Health Foundation; the Provincial Centre for Excellence for Child and Youth Mental Health (Children's Hospital of Eastern Ontario); the Hospital for Sick Children's Psychiatry Endowment Fund Conflicts of interest: the authors did not report if there were any conflicts of interest |
Pasalich 2019.
| Study characteristics | |
| Methods |
|
| Participants |
|
| Interventions |
Intervention ‐ Promoting First Relationships (PFR)
Comparator ‐ three‐call resource and referral (R&R)
|
| Outcomes |
Assessment time point(s)
Note: secure base behaviour only assessed at baseline and 6‐month follow‐up Primary outcome(s) Parent‐child relationship
Secondary outcome(s): Parent engagement
Adverse outcome(s): none specified |
| Notes |
Comment(s)
Funding source: Eunice Kennedy Shriver National Institute of Child Health and Human Development; Australian Research Council Discovery Early Career Researcher Award Conflicts of interest: the authors declared that there were no conflicts of interest |
Rosenblum 2017.
| Study characteristics | |
| Methods |
|
| Participants |
|
| Interventions |
Intervention ‐ Mom Power
Comparator ‐ attention control
|
| Outcomes |
Assessment time point(s)
Primary outcome(s) Parental complex trauma symptoms
Parental psychological wellbeing
Parenting skills
Secondary outcome(s) Parent engagement
Changes in parental social capital
Adverse outcome(s): none specified |
| Notes |
Comment(s)
Funding source: Department of Community Health (State of Michigan); Michigan Institute for Clinical & Health Research; the Robert Wood Johnson Health & Society Scholars Program Conflicts of interest: the authors declared that there were no conflicts of interest |
Silverstein 2011.
| Study characteristics | |
| Methods |
|
| Participants |
|
| Interventions |
Intervention ‐ Problem‐Solving Education (PSE)
Comparator ‐ treatment as usual
|
| Outcomes |
Assessment time point(s)
Note: Assessments were also conducted as baseline, 1‐month follow‐up and 2‐month follow‐up (outcome data not reported for the subsample) Primary outcome(s) Parental psychological wellbeing
Secondary outcome(s) Parent engagement
Parental social functioning
Adverse outcome(s): none specified |
| Notes |
Comment(s)
Funding source: National Institute of Child Health and Human Development; the Robinhood Foundation; the Robert Wood Johnson Foundation under its Physician Faculty Scholars Program Conflict of interest: the trial authors made the following declarations in the conflicts of interest statement: "Dr. Silverstein also receives support from the National Institute of Mental Health (K23MH074079). Dr. Feinberg receives support from the National Institute of Nursing Research (K23NR010588)" (Silverstein 2011, page 483) |
Steele 2019.
| Study characteristics | |
| Methods |
|
| Participants |
|
| Interventions |
Intervention ‐ Group Attachment‐Based Intervention (GABI)
Comparator ‐ Systematic Training for Effective Parenting (STEP)
|
| Outcomes |
Assessment time point(s)
Note: Assessments were also conducted at baseline; however, the results from this time point are not reported Primary outcome(s) Parent‐child relationship
Parenting skills
Secondary outcome(s): Parent engagement
Adverse outcome(s): none specified |
| Notes |
Comment(s): unpublished data requested for subsample with high exposure (for or more adverse childhood events), but authors did not have capacity to send the data. No unpublished data reported in meta‐analyses. As 77% of parents experienced 4 or more adverse childhood experiences (high exposure), the mean adverse childhood events was high (5.7 events) and other traumas and adversity were extremely high, data from the whole sample was included Funding source: Health Resources and Services Administration Grant Conflicts of interest: the authors declared that there were no conflicts of interest |
Upshur 2016.
| Study characteristics | |
| Methods |
|
| Participants |
|
| Interventions |
Intervention ‐ Seeking Safety (SS) + TAU
Comparator ‐ treatment as usual
|
| Outcomes |
Assessment time point(s)
Primary outcome(s) Parental complex trauma symptoms
Parental psychological wellbeing
Secondary outcome(s) Parent engagement
Parental social functioning
Adverse outcome(s): none specified |
| Notes |
Comment(s)
Funding source: Health Resources and Services Administration Grant Conflicts of interest: the authors declared that there were no conflicts of interest |
ACEs: Adverse Childhood Experiences; CBASP: Cognitive Behavioural Analysis System of Psychotherapy; CBT: Cognitive Behavioural Therapy; Cluster‐RCT: cluster‐randomised controlled trial; CM‐: Low Exposure to Child Maltreatment; CM+: Exposure to Child Maltreatment; CPP: Child‐Parent Psychotherapy; CS: Community Standard; DHS: Department of Human Services; DSHS: Department of Social and Health Services; EHS: Early Head Start; E‐TAU: Enhanced Treatment as Usual; FIND: Filming Interactions to Nurture Development; GABI: Group Attachment‐Based Intervention; GYN: gynaecologist; HFA: Healthy Families America; HW: Health and Wellness Control; IH‐CBT: In Home Cognitive Behavioural Therapy; IPP: Infant‐Parent Psychotherapy; IPT: Interpersonal Psychotherapy; IPT‐B: Brief Interpersonal Psychotherapy; MINI: Mini International Neuropsychiatric Interview; MSS: Maternity Support Services; MSS‐Plus: Maternity Support Services‐PLUS; N: number of participants in the sample; NFP: Nurse‐family Partnership; NICU: Neonatal Intensive Care Unit; OB: obstetrician; PFR: Promoting First Relationships; PHQ‐9: Patient Health Questionnaire 9; PPI: Psychoeducational Parenting Intervention; PREPP: Practice Resources for Effective Postpartum Parenting; PRIME‐MD: Primary Care Evaluation of Mental Disorders; PSE: Problem‐Solving Education; PTSD: post‐traumatic stress disorder; QALYs: quality adjusted life year; R&R: Three‐call Resources and Referral; RCT: randomised controlled trial; SCL: Hopkins Symptom Checklist; SD: standard deviation; SES: socio‐economic status; SORT‐45: Toddler Attachment Sort‐45; SS: Seeking Safety; SS+TAU: Seeking Safety + Treatment as Usual; STEP: Systematic Training for Effective Parenting; TANF: Temporary Assistance for Needy Families; TAU: treatment as usual; TF‐CBT: Trauma Focused Cognitive Behavioural Therapy; TLFB: Timeline Follow‐Back; WIC: Women, Infants and Children
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Ammerman 2022 | Parents not experiencing CPTSD symptoms and/or childhood maltreatment |
| Cohen 2020 | Ineligible study design: symposia highlights detailing ineligible studies |
| Demeusy 2020 | Parents not experiencing CPTSD symptoms and/or childhood maltreatment |
| Fergusson 2005 | Parents not experiencing CPTSD symptoms and/or childhood maltreatment |
| Hildebrandt 2020 | Not an RCT |
| Hubmann 2015 | Parents not experiencing CPTSD symptoms and/or childhood maltreatment |
| Lytle 2018 | Not an RCT |
| Macfie 2020 | Not an RCT |
| McGinnis 2018 | Ineligible intervention |
| Perrone 2021 | Parents not experiencing CPTSD symptoms and/or childhood maltreatment |
| Portwood 2011 | Parents not experiencing CPTSD symptoms and/or childhood maltreatment |
| Riem 2021 | Parents not experiencing CPTSD symptoms and/or childhood maltreatment |
| Stevens‐Simon 2001 | Parents not experiencing CPTSD symptoms and/or childhood maltreatment |
| Taylor 1997 | Parents not experiencing CPTSD symptoms and/or childhood maltreatment |
| Taylor 1998 | Parents not experiencing CPTSD symptoms and/or childhood maltreatment |
| Tiwari 2005 | Parents not experiencing CPTSD symptoms and/or childhood maltreatment |
| Tomfohr‐Madsen 2020 | Parents not experiencing CPTSD symptoms and/or childhood maltreatment |
| Tran 2019 | Not an RCT |
| Wisner 2017 | Parents not experiencing CPTSD symptoms and/or childhood maltreatment |
CPTSD: complex post‐traumatic stress disorder RCT: randomised controlled trial
Characteristics of ongoing studies [ordered by study ID]
Kaltenbach 2021.
| Study name | Life Beyond Trauma: 1‐on‐1 e‐Health Program for Parents of Neurodiverse Children |
| Methods | Individual RCT (parallel groups; 2 arms) |
| Participants |
Target sample size: 500 to 800 participants Age: 18 years and over Sex: female and male participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention: immediate e‐NET Group; a version of narrative exposure therapy adapted to the needs of parents of neurodiverse children delivered via videoconferencing Comparator: wait‐list control group; parents will receive e‐NET 3 months after the baseline survey |
| Outcomes |
Assessment time point(s)
Primary outcome
Secondary outcomes
|
| Starting date | 29 June 2020 |
| Contact information |
|
| Notes |
Status: completed (study results not published). Authors were contacted to request the unpublished data, but no response has been received Location: USA Funding source: Canadian Institutes for Health Research, the Strategy for Patient Oriented Research (CHILD‐BRIGHT Network) and the IWK Health Centre Conflicts of interest: the authors declared that there were no conflicts of interest |
NCT03175796.
| Study name | Infant mental health home visiting mitigates impact of maternal adverse childhood experiences on toddler language competence: a randomized controlled trial |
| Methods | RCT (parallel groups; 2 arms) |
| Participants |
Sample size: 62 participants Age: 18 years and over Sex: female participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention: IMH‐HV. Weekly home visits for up to one year by a trained IMH‐HV treatment provider. Treatment delivery consistent with the IMH‐HV manual Comparator: treatment as usual control group. No intervention provided as part of participation in this study; families are free to access community resources including any available treatment(s) in the community |
| Outcomes |
Assessment time point(s)
Primary outcomes
|
| Starting date | 12 October 2017 |
| Contact information | Katherine Rosenblum (katier@med.umich.edu) |
| Notes | The report was published after we had completed data extraction and analysis for this review Location: USA Funding source: not reported Conflicts of interest: the authors declared that there were no conflicts of interest |
NCT03938350.
| Study name |
Public title: Dialectical behavior therapy for pregnant women Scientific title: Dialectical behavior therapy skills training for high‐risk African American pregnant women: feasibility and acceptability of implementation in prenatal clinics |
| Methods | Individual RCT (parallel groups; 2 arms) |
| Participants |
Target sample size: 60 participants Age: 18 years and over Sex: female participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention: DBT skills training. Participants in this group will receive 8 weeks of DBT skills training Comparison: treatment as usual. Participants in this study arm will receive treatment as usual consisting of routine prenatal care with any mental health assessment, social work involvement or mental health service provision based on clinician referral or self‐referral |
| Outcomes |
Assessment time point(s)
Primary outcomes
Secondary outcomes
|
| Starting date | 16 October 2019 |
| Contact information |
|
| Notes |
Status: completed, no results published Location: USA Funding source: not reported Conflicts of interest: the authors did not report if there were any conflicts of interest |
NCT04818112.
| Study name |
Public title: A randomized controlled trial to improve mother‐infant synchrony among women with childhood adversity Scientific title: same as public title |
| Methods | Individual RCT (parallel groups; 2 arms) |
| Participants |
Target sample size: 250 participants Age: 18 years and over Sex: female participants Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention: behavioural auditory, tactile, visual and vestibular intervention. A 15‐minute behavioural intervention, which is a multisensory infant massage contingent on infant cues Comparator: attention control. An attention control group that receives education on safe infant care and the same amount of attention as the intervention group |
| Outcomes |
Assessment time point(s)
Primary outcome
Secondary outcomes
|
| Starting date | 12 July 2021 |
| Contact information |
|
| Notes |
Status: recruiting participants Location: USA Funding source: not reported Conflicts of interest: the authors did not report if there were any conflicts of interest |
NL9179.
| Study name |
Public title: Samen stap voor stap vooruit Scientific title: Effectively intervening in traumatized parents and children after structural domestic violence |
| Methods | Individual RCT (parallel groups; 2 arms) |
| Participants |
Target sample size: 150 mother/child dyads Age: not specified (child aged between 6 months and 6 years old) Sex: female mothers Inclusion criteria
Exclusion criteria
|
| Interventions |
Intervention: NIKA. A short‐term, attachment‐based, video‐feedback intervention for parents and their children aged between 0 and 6 years old Comparator: eye movement desensitisation and reprocessing (EMDR, head‐to‐head trial). A brief trauma therapy aimed at reducing the negative load of the memories of traumatic events. The parent is asked to bring the traumatic event to mind while the therapist provides a distracting task |
| Outcomes |
Assessment time point(s): not reported The trial registration did not specify the scales they will use to assess the primary and secondary outcomes Primary outcomes
Secondary outcomes
|
| Starting date | 7 January 2021 |
| Contact information | Sabine van der Asdonk (s.van.der.asdonk@fsw.leidenuniv.nl) |
| Notes |
Status: recruiting participants Location: The Netherlands Funding source: not reported Conflicts of interest: the authors did not report if there were any conflicts of interest |
ACE: adverse childhood experience; BCAP: Brief Child Abuse Potential Inventory; DBT: Dialectical Behavioural Therapy; DNA: deoxyribonucleic acid; DSM‐5: Diagnostic and Statistical Manual 5; EMDR: Eye Movement Desensitisation and Reprocessing; e‐NET: Electronic Narrative Exposure Therapy; GAD‐7: Generalised Anxiety Disorder‐7; IGR: intrauterine growth retardation; IMH‐HV: infant mental health home visiting; ITSEA: Infant‐Toddler Social and Emotional Assessment; LEC‐5: Life Events Checklist for DSM‐5; NIKA: Nederlandse Interventie Kortdurend op Atypisch opvoedgedrag; PCL‐5: PTSD Checklist for DSM‐5; PC‐PTSD‐5: Primary Care PTSD Screen for DSM‐5; PHQ‐9: Patient Health Questionnaire‐9; PROMIS: Patient‐Reported Outcomes Measurement Information System; PTSD: post‐traumatic stress disorder; PTSI: post‐traumatic stress injury; RCT: randomised controlled trial; SGA: small for gestational age; WMCI: Working Model of the Child Interview
Differences between protocol and review
-
We planned to include a comparison of all interventions versus control. We did not include this comparison as we considered that there was too high a level of heterogeneity across the intervention categories for this comparison to add any value. For example, psychological interventions assessed psychological wellbeing outcomes, while parenting interventions assessed parenting capacity and parenting skills outcomes. We felt that combining these diverse outcomes in a single comparison would not be useful to readers. Subsequently, the planned subgroup analyses detailed below could not be conducted.
-
For the comparison of all interventions versus control:
Type of intervention (psychological therapies, parenting programmes, mind–body approaches, pharmacological and biomedical therapies, and service system approaches).
Participant characteristics using PROGRESS+ plus framework (O'Neill 2014): age (under 18 years, 18 to 29 years, 30 or over years); ethnicity (dominant or 'minority' ethnic population at risk of disadvantage); country of birth (low‐ to middle‐income or high‐income); indigenous status (all indigenous); socioeconomic status (SES; low or not low SES); parent gender (majority male versus majority female); majority current complex trauma symptoms or childhood maltreatment history (sexual abuse versus other type of abuse history); education (majority less than high school versus majority completed high school); mental health comorbidity (yes or no); recruitment through mental health service, prison, or government mandated parenting programme, as there is substantial evidence that complex trauma does not impact parents uniformly, and some population groups experience greater impacts of complex trauma, as well as potentially differential experiences of 'parenting interventions'.
Intervention characteristics (delivery modality, face‐to‐face or online); in home or group‐based, single practitioner or multidisciplinary team delivery, or both; number of contacts (one, two to five, more than five); total length of contact time (less than one hour, two to 10 hours, more than 10 hours), as knowledge of intervention characteristics that may enhance the effectiveness of an intervention is important for decision‐makers and programme developers.
-
In terms of participant characteristics, we planned to report any factors that may account for increased heterogeneity, and if this was not feasible to report all the above factors individually. We planned to use the data to generate the following variables to conduct subgroup analyses to examine their effects:
'any indicator of disadvantage', generated from a combination of the following: aged less than 18 years, 'minority' ethnic population at risk of disadvantage, low‐ to middle‐income country, majority indigenous parents, low SES, majority education less than high school, or recruited through prison;
'mental health comorbidity', generated from current complex trauma symptoms, mental health comorbidity or recruited through mental health service or government mandated parenting programme; and
maltreatment involving sexual abuse (no studies found).
-
In the protocol we said we would code studies as meeting the PROGRESS+ criteria for 'indigenous' population when all participants were indigenous. This was amended to code studies as meeting the criteria when the majority of participants identified as indigenous in line with other criteria used in the review (e.g. majority ethnic minority population).
We planned to group outcomes for synthesis, considering the following two periods: pregnancy, up to six weeks' postpartum; and more than seven weeks' postpartum (up to five years, to account for longer‐term follow‐up after intervention completion) and to select the outcome measured at the longest follow‐up where an outcome was measured at multiple time points within a period. We selected broad time periods in anticipation of having sparse data for synthesis. Given the importance of understanding effects across the postpartum period, we planned to extract data for outcomes at three, six, 12, 18 and 24 months' postpartum, and for birth to six months, seven to 12 months and greater than one year after intervention, for synthesis at a more granular level, if sufficient data were available (including in future updates, as the evidence base in this emerging area grows). Due to a limited range of time points available, we extracted and reported data for all available time points.
Contributions of authors
| Initials of author | Contribution of author |
| KAJ | Responsible for managing and co‐ordinating the review; responsible for conceptualisation and write up of the overall review; responsible for selection and screening of studies, data extraction form development, data extraction and entry to RevMan Web; responsible for the assessment of risk of bias; substantial responsibility for planned data analysis, interpretation of results, and development of summary of findings tables; responsible for GRADE certainty assessments; all with contributions from other review authors, as described |
| IF | Provided substantial support to conceptualisation and write up overall review; contributed to selection (screening) of studies; data extraction; data analysis; responsible for the assessment of risk of bias; responsible for GRADE certainty assessments and editing of review |
| SEB | Topic expertise; contributed substantially to conceptualisation, planning of methods and provided statistical advice for development of the analysis plan; critically reviewed the review; responsible for GRADE certainty assessments; contributed to data analysis, interpretation of results and editing of review |
| JEM | Topic expertise; contributed substantially to conceptualisation, planning of methods and provided advice for development of the analysis plan; critically reviewed the review; contributed to data analysis, interpretation of results and editing of review |
| TMB | Critically reviewed the review; contributed to data extraction form development; selection of studies (screening); data extraction; assessment of risk of bias and editing of review |
| CR | Contributed to conceptualisation of the overall review, critically reviewed the review; contributed to the selection of studies (screening) |
| RF | Critically reviewed the review; contributed to the selection of studies (screening); data extraction; assessment of risk of bias and editing of review |
| ED | Critically reviewed the review; contributed to the selection of studies (screening); data extraction; assessment of risk of bias and editing of review |
| IK | Critically reviewed the review; contributed to the selection of studies (screening); data extraction; assessment of risk of bias and editing of review |
| SA | Topic expertise; critically reviewed the review; contributed to data extraction and appraisal of studies |
| MM | Topic expertise; critically reviewed the review |
| LS | Contributed to conceptualisation of the review, topic expertise; critically reviewed the review |
| HH | Contributed substantial support to conceptualisation of the review, topic expertise; critically reviewed the review |
| CC | Senior and corresponding author; guarantor for the review; topic expertise; conceptualisation of this review and critical input into the review design and methods; contributed to data extraction, data analysis and editing of review; and Principal Investigator for the Healing the Past by Nurturing the Future project, from which this review has been conducted. |
Sources of support
Internal sources
-
University of Melbourne, Australia
Provided salary support for RF and CC
-
Monash University, Australia
Provided salary support for SEB, JEM
External sources
-
National Health and Medical Research Council (NHMRC), Australia
This review is being undertaken as part of the Healing the Past by Nurturing the Future project, which is funded by the Australian National Health and Medical Research Council (NHMRC) (project grant 1141593) and which provided salary funding for the following review authors; Kimberley Jones, Isabella Freijah, Tess Bright, Elise Davis and Ilias Kamitsis. Catherine Chamberlain, Elise Davis and Helen Herman are CIs on this grant. Carol Reid receives a PhD stipend funded from The Healing the Past by Nurturing the Future project.
Several authors have received additional NHMRC support, which contributes to their salary: Catherine Chamberlain and Joanne McKenzie are supported by Career Development Fellowships (1088813; 1143429).
Declarations of interest
This review is being undertaken as part of the Healing the Past by Nurturing the Future project. The Healing the Past by Nurturing the Future work is supported by a National Health and Medical Research Council (NHMRC) project grant (1141593).
All authors declare they have no financial, personal or professional interests that could be construed to have influenced the conduct or results of this systematic review.
KAJ: reports a grant from the Medical Research Future Fund (MRFF), which aims to improve the health and wellbeing of Aboriginal and Torres Strait Islander mothers and babies, paid to the Indigenous Health Equity Unit, Melbourne School of Population and Global Health, University of Melbourne, Carlton, Australia.
SEB: has declared that she has no conflicts of interest.
JEM: has declared that she has no conflicts of interest.
IF: has declared that she has no conflicts of interest.
TMB: reports a grant from the MRFF, which aims to improve the health and wellbeing of Aboriginal and Torres Strait Islander mothers and babies; paid to the Indigenous Health Equity Unit, Melbourne School of Population and Global Health, University of Melbourne, Carlton, Australia.
RF is a qualified nurse and reports a grant from the MRFF, which aims to improve the health and wellbeing of Aboriginal and Torres Strait Islander mothers and babies; paid to the Indigenous Health Equity Unit, Melbourne School of Population and Global Health, University of Melbourne, Carlton, Australia.
ED: reports two grants from the MRFF, which (1) aim to improve health outcomes for Indigenous parents and their infants in a rural setting and (2) aim to improve the health and wellbeing of Aboriginal and Torres Strait Islander mothers and babies; both paid to the Indigenous Health Equity Unit, Melbourne School of Population and Global Health, University of Melbourne, Carlton, Australia.
IK: reports a grant from the MRFF, which aims to improve the health and wellbeing of Aboriginal and Torres Strait Islander mothers and babies; paid to the Indigenous Health Equity Unit, Melbourne School of Population and Global Health, University of Melbourne, Carlton, Australia.
SA: has declared that she has no conflicts of interest.
MM: reports being the PI of three studies that are eligible for inclusion in the work: Rosenblum KL, Muzik M, Morelen DM, Alfafara EA, Miller NM, Waddell RM, et al. A community‐based randomized controlled trial of Mom Power parenting intervention for mothers with interpersonal trauma histories and their young children. Archives of Women's Mental Health 2017;20(5):673‐86. [DOI: 10.1007/s00737‐017‐0734‐9; PMCID: PMC5709180; PubMed: 28647759]; Rosenblum KL, Lawler J, Alfafara EA, Miller N, Schuster M, Muzik M. Improving maternal representations in high‐risk mothers: a randomized, controlled trial of the Mom Power parenting intervention. Child Psychiatry & Human Development 2018;49(3):372‐84. [DOI: 10.1007/s10578‐017‐0757‐5; PMCID: PMC5862741; PubMed: 28936602]; Muzik M, Rosenblum K L, Schuster M, Ribaudo J, Alfafara E, Miller N. Mom Power: a multi‐family intervention for mothers with childhood trauma histories and their young children, aimed to support mental health and parenting. Archives of women's mental health 2019;22(5):672. These studies were funded by: Department of Community Health, State of Michigan (grants F023865‐2009 and F029321‐2010); Michigan Institute for Clinical & Health Research (grant UL1RR024986‐2010); and the Robert Wood Johnson Health & Society Scholars Program (grant N012918‐2010). The funders had no role in the design, methods, data analysis or reporting.
LS: has declared that she has no conflicts of interest.
HH: has declared that she has no conflicts of interest.
CR: has declared that she has no conflicts of interest.
CC: reports being the Principal Investigator for two MRFF grants, which aim to implement and evaluate trauma‐integrated perinatal care for Aboriginal and Torres Strait Islander families from the Australian Medical Research Future Fund, and the recipient of a Career Development Fellowship and Project Grant to improve health equity for Aboriginal and Torres Strait Islander families from the National Health and Medical Research Council; all paid to the Indigenous Health Equity Unit, Melbourne School of Population and Global Health, University of Melbourne, Carlton, Australia. CC is a Women in Science and Principal Indigenous Committee member with National Health and Medical Research Council, and a board member with the Australian Health Practitioner Regulation Agency; personal payments.
New
References
References to studies included in this review
Ammerman 2016 {unpublished data only}
- Ammerman RT, Altaye M, Putnam FW, Teeters AR, Zou Y, Van Ginkel JB. Depression improvement and parenting in low-income mothers in home visiting. Archives of Women's Mental Health 2015;18(3):555-63. [DOI: 10.1007/s00737-014-0479-7] [PMCID: PMC4420724] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammerman RT, Mallow PJ, Rizzo JA, Putnam FW, Van Ginkel JB. Cost-effectiveness of in-home cognitive behavioral therapy for low-income depressed mothers participating in early childhood prevention programs. Journal of Affective Disorders 2017;208:475-82. [DOI: 10.1016/j.jad.2016.10.041] [PMCID: PMC5154809] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammerman RT, Peugh JL, Teeters AR, Putnam FW, Van Ginkel JB. Child maltreatment history and response to CBT treatment in depressed mothers participating in home visiting. Journal of Interpersonal Violence 2016;31(5):774-91. [DOI: 10.1177/0886260514556769] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Ammerman RT, Putnam FW, Altaye M, Stevens J, Teeters AR, Van Ginkel JB. A clinical trial of in-home CBT for depressed mothers in home visitation. Behavior Therapy 2013;44(3):359-72. [DOI: 10.1016/j.beth.2013.01.002] [PMCID: PMC3693767] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ammerman RT, Putnam FW, Altaye M, Teeters AR, Stevens J, Van Ginkel JB. Treatment of depressed mothers in home visiting: impact on psychological distress and social functioning. Child Abuse & Neglect 2013;37(8):544-54. [DOI: 10.1016/j.chiabu.2013.03.003] [PMCID: PMC3742640] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Berry 2021 {unpublished data only}
- Berry OJ. Postpartum depression prevention through the mother-infant dyad: the role of childhood trauma. Journal of the American Academy of Child and Adolescent Psychiatry 2019;58(Suppl 10):S299. [DOI: 10.1016/j.jaac.2019.09.017] [DOI] [Google Scholar]
- Berry OO, Babineau V, Lee S, Feng T, Scorza P, Werner EA, et al. Perinatal depression prevention through the mother-infant dyad: the role of maternal childhood maltreatment. Journal of Affective Disorders 2021;290:188-96. [DOI: 10.1016/j.jad.2021.04.068] [PMCID: PMC8217280 (available on 2022-07-01)] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scorza P, Monk C, Lee S, Feng T, Berry OO, Werner E. Preventing maternal mental health disorders in the context of poverty: pilot efficacy of a dyadic intervention. American Journal of Obstetrics & Gynecology MFM 2020;2(4):100230. [DOI: 10.1016/j.ajogmf.2020.100230] [PMCID: PMC7893538] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner EA, Gustafsson HC, Lee S, Feng T, Jiang N, Desai P, et al. PREPP: postpartum depression prevention throughthe mother–infant dyad. Archives of Women's Mental Health 2016;19(2):229-42. [DOI: 10.1007/s00737-015-0549-5] [PMCID: PMC4738166] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Blalock 2013 {unpublished data only}
- Blalock JA, Minnix JA, Mathew AR, Wetter DW, McCullough JP, Cinciripini PM. Relationship of childhood trauma to depression and smoking outcomes in pregnant smokers. Journal of Consulting and Clinical Psychology 2013;81(5):821-30. [DOI: 10.1037/a0033381] [PMCID: PMC2881321] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cinciripini PM, Blalock JA, Minnix JA, Robinson JD, Brown VL, Lam C, . Effects of an intensive depression-focused intervention for smoking cessation in pregnancy. Journal of Consulting and Clinical Psychology 2010;78(1):44-54. [DOI: ] [PMCID: PMC2881321] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Booshehri 2018 {published data only}
- Booshehri LG, Dugan J, Patel F, Bloom S, Chilton M. Trauma-informed Temporary Assistance for Needy Families (TANF): a randomized controlled trial with a two-generation impact. Journal of Child and Family Studies 2018;27(5):1594-604. [DOI: 10.1007/s10826-017-0987-y] [PMCID: PMC5886995] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun J, Patel F, Kirzner R, Newton-Famous N, Owens C, Welles SL, et al. The Building Wealth and Health Network: methods and baseline characteristics from a randomized controlled trial for families with young children participating in temporary assistance for needy families (TANF). BMC Public Health 2016;16:583. [DOI: 10.1186/s12889-016-3233-4] [PMCID: PMC4947340] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cicchetti 2006 {published and unpublished data}
- Cicchetti D, Rogosch FA, Toth SL, Sturge-Apple ML. Normalizing the development of cortisol regulation in maltreated infants through preventive interventions. Development and Psychopathology 2011;23(3):789-800. [DOI: 10.1017/S0954579411000307] [PMCID: PMC4191893] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cicchetti D, Rogosch FA, Toth SL. Fostering secure attachment in infants in maltreating families through preventive interventions. Development and Psychopathology 2006;18(3):623-49. [DOI: ] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Stronach EP, Toth SL, Rogosch F, Cicchetti D. Preventive interventions and sustained attachment security in maltreated children. Development and Psychopathology 2013;25(4 Pt 1):919-30. [DOI: 10.1017/S0954579413000278] [PMCID: PMC3857699] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stronach EP. Preventive interventions and sustained attachment security in maltreated children: a 12-month follow-up of a randomized controlled trial [Doctoral thesis]. Rochester (NY): University of Rochester, 2011. [Google Scholar]
- Toth SL, Sturge-Apple ML, Rogosch FA, Cicchetti D. Mechanisms of change: testing how preventative interventions impact psychological and physiological stress functioning in mothers in neglectful families. Development and Psychopathology 2015;27(4 Pt 2):1661-74. [DOI: 10.1017/S0954579415001017] [PMCID: PMC4633703] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Grote 2012 {published data only}
- Grote NK, Spieker SJ, Lohr MJ, Geibel SL, Swartz HA, Frank E, et al. Impact of childhood trauma on the outcomes of a perinatal depression trial. Depression & Anxiety 2012;29(7):563-73. [DOI: 10.1002/da.21929] [PMCID: PMC3554235] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grote NK, Swartz HA, Geibel SL, Zuckoff A, Houck PR, Frank E. A randomized controlled trial of culturally relevant, brief interpersonal psychotherapy for perinatal depression. Psychiatric Services 2009;60(3):313-21. [DOI: 10.1176/appi.ps.60.3.313] [PMCID: PMC3032494] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Grote 2015 {unpublished data only}
- Grote NK, Katon WJ, Lohr MJ, Carson K, Curran M, Galvin E, et al. Culturally relevant treatment services for perinatal depression in socio-economically disadvantaged women: the design of the MOMCare study. Contemporary Clinical Trials 2014;39(1):34-49. [DOI: 10.1016/j.cct.2014.07.001] [PMCID: PMC4226398] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grote NK, Katon WJ, Russo JE, Lohr MJ, Curran M, Galvin E, et al. A randomized trial of collaborative care for perinatal depression in socioeconomically disadvantaged women: the impact of comorbid posttraumatic stress disorder. Journal of Clinical Psychiatry 2016;77(11):1527-37. [DOI: 10.4088/JCP.15m10477] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Grote NK, Katon WJ, Russo JE, Lohr MJ, Curran M, Galvin E, et al. Collaborative care for perinatal depression in socioeconomically disadvantaged women: a randomized trial. Depression & Anxiety 2015;32(11):821-34. [DOI: 10.1002/da.22405] [PMCID: PMC4630126] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grote NK, Simon GE, Russo J, Lohr MJ, Carson K, Katon W. Incremental benefit-cost of MOMCare: collaborative care for perinatal depression among economically disadvantaged women. Psychiatric Services 2017;68(11):1164-71. [DOI: 10.1176/appi.ps.201600411] [PMID: ] [DOI] [PubMed] [Google Scholar]
Haight 2005 {published data only}
- Haight WL, Black JE, Mangelsdorf S, Giorgio G, Tata L, Schoppe SJ, et al. Making visits better: the perspectives of parents, foster parents, and child welfare workers. Child Welfare 2002;81(2):173-202. [PMID: ] [PubMed] [Google Scholar]
- Haight WL, Mangelsdorf S, Black J, Szewczyk M, Schoppe S, Giorgio G, et al. Enhancing parent-child interaction during foster care visits: experimental assessment of an intervention. Child Welfare 2005;84(4):459-81. [PMID: ] [PubMed] [Google Scholar]
Liu 2021 {unpublished data only}
- Liu S, Phu T, Dominguez A, Hurwich-Reiss E, McGee D, Watamura S, et al. Improving caregiver self-efficacy and children's behavioral outcomes via a brief strength-based video coaching intervention: results from a randomized controlled trial. Prevention Science 2021 May 7 [Epub ahead of print]. [DOI: 10.1007/s11121-021-01251-6] [PMID: ] [DOI] [PubMed]
Madigan 2015 {published data only}
- Madigan S, Vaillancourt K, McKibbon A, Benoit D. The reporting of maltreatment experiences during the Adult Attachment Interview in a sample of pregnant adolescents. Attachment & Human Development 2012;14(2):119-43. [DOI: 10.1080/14616734.2012.661230] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Madigan S, Vaillancourt K, McKibbon A, Benoit D. Trauma and traumatic loss in pregnant adolescents: the impact of trauma-focused cognitive behavior therapy on maternal unresolved states of mind and posttraumatic stress disorder. Attachment & Human Development 2015;17(2):175-98. [DOI: 10.1080/14616734.2015.1006386] [PMID: ] [DOI] [PubMed] [Google Scholar]
Pasalich 2019 {unpublished data only}
- Hastings PD, Kahle S, Fleming C, Lohr MJ, Fainsilber Katz L, Oxford ML. An intervention that increases parental sensitivity in families referred to child protective services also changes toddlers' parasympathetic regulation. Developmental Science 2019;22(1):e12725. [DOI: 10.1111/desc.12725] [PMCID: PMC6294712] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oxford ML, Spieker SJ, Lohr MJ, Fleming CB, Dillon C, Rees J. Ensuring implementation fidelity of a 10-week home visiting program in two randomized clinical trials. Maternal and Child Health Journal 2018;22(3):376-83. [DOI: 10.1007/s10995-017-2387-8] [PMCID: PMC5845475] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oxford ML, Spieker SJ, Lohr MJ, Fleming CB. Promoting First Relationships®: randomized trial of a 10-week home visiting program with families referred to child protective services. Child Maltreatment 2016;21(4):267-77. [DOI: 10.1177/1077559516668274] [PMCID: PMC5357588] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasalich DS, Fleming CB, Spieker SJ, Lohr MJ, Oxford ML. Does parents' own history of child abuse moderate the effectiveness of the Promoting First Relationships® intervention in child welfare? Child Maltreatment 2019;24(1):56-65. [DOI: 10.1177/1077559518809217] [PMID: ] [DOI] [PubMed] [Google Scholar]
Rosenblum 2017 {unpublished data only}
- Muzik M, Rosenblum KL, Schuster M, Ribaudo J, Alfafara E, Miller N. Mom Power: a multi-family intervention for mothers with childhood trauma histories and their young children, aimed to support mental health and parenting. Archives of Women's Mental Health 2019;22(5):672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenblum KL, Lawler J, Alfafara EA, Miller N, Schuster M, Muzik M. Improving maternal representations in high-risk mothers: a randomized, controlled trial of the Mom Power parenting intervention. Child Psychiatry & Human Development 2018;49(3):372-84. [DOI: 10.1007/s10578-017-0757-5] [PMCID: PMC5862741] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenblum KL, Muzik M, Morelen DM, Alfafara EA, Miller NM, Waddell RM, et al. A community-based randomized controlled trial of Mom Power parenting intervention for mothers with interpersonal trauma histories and their young children. Archives of Women's Mental Health 2017;20(5):673-86. [DOI: 10.1007/s00737-017-0734-9] [PMCID: PMC5709180] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Silverstein 2011 {published data only}
- Silverstein M, Feinberg E, Cabral H, Linhart YD, Sandler J, Hegel M, et al. Potential impact of trauma on the ability to prevent depression among low-income mothers. Depression & Anxiety 2011;28(6):478-84. [DOI: 10.1002/da.20817] [PMCID: PMC3110557] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silverstein M, Kistin C, Bair-Merritt M, Wiltsey-Stirman S, Feinberg E, Diaz-Linhart Y, et al. Avoidance as an obstacle to preventing depression among urban women at high risk for violent trauma. Archives of Women's Mental Health 2016;19(1):63-70. [DOI: 10.1007/s00737-015-0521-4] [PMCID: PMC6013058] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Steele 2019 {published data only}
- Murphy A, Steele H, Bate J, Nikitiades A, Allman B, Bonuck K, et al. Group attachment-based intervention: trauma-informed care for families with adverse childhood experiences. Family and Community Health 2015;38(3):268-79. [DOI: 10.1097/FCH.0000000000000074] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Steele H, Murphy A, Bonuck K, Meissner P, Steele M. Randomized control trial report on the effectiveness of Group Attachment-Based Intervention (GABI©): improvements in the parent-child relationship not seen in the control group. Development and Psychopathology 2019;31(1):203-17. [DOI: 10.1017/S0954579418001621] [PMID: ] [DOI] [PubMed] [Google Scholar]
Upshur 2016 {unpublished data only}
- Upshur CC, Wenz-Gross M, Weinreb L, Moffitt JJ. Using prenatal advocates to implement a psychosocial education intervention for posttraumatic stress disorder during pregnancy: feasibility, care engagement, and predelivery behavioral outcomes. Women's Health Issues 2016;26(5):537-45. [DOI: 10.1016/j.whi.2016.06.003] [PMID: ] [DOI] [PubMed] [Google Scholar]
- Weinreb L, Wenz-Gross M, Upshur C. Postpartum outcomes of a pilot prenatal care-based psychosocial intervention for PTSD during pregnancy. Archives of Women's Mental Health 2018;21(3):299-312. [DOI: 10.1007/s00737-017-0794-x] [PMID: ] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Ammerman 2022 {published data only}
- Ammerman RT, Peugh JL, Teeters AR, Sakuma K-L, Jones DE, Hostetler ML, et al. Promoting parenting in home visiting: a CACE analysis of Family Foundations. Journal of Family Psychology 2022;36(2):225-35. [DOI: 10.1037/fam0000888] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cohen 2020 {published data only}
- Cohen JA, Amaya-Jackson L. New developments in evidence-based trauma treatments and relevance for child and adolescent psychiatrists. Journal of the American Academy of Child & Adolescent Psychiatry 2020;59(10S):S322.
Demeusy 2020 {published data only}
- Demeusy EM. A multi-component intervention to prevent child maltreatment: long-term effects on parenting and child functioning [PhD thesis]. Rochester (NY): University of Rochester, 2020. [PROQUEST NO.: 28028845] [Google Scholar]
Fergusson 2005 {published data only}
- Fergusson DM, Grant H, Horwood LJ, Ridder EM. Randomized trial of the Early Start program of home visitation. Pediatrics 2005;116(6):e803-9. [DOI: 10.1542/peds.2005-0948] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hildebrandt 2020 {published data only}
- Hildebrandt UC, Graham JC, Grant TM. Predictors and moderators of improved social-emotional functioning in mothers with substance use disorders and their young children enrolled in a relationship-based case management program. Infant Mental Health Journal 2020;41(5):677-96. [DOI] [PubMed] [Google Scholar]
Hubmann 2015 {published data only}
- Hubmann P, Burkhardt SCA, Neuhauser A, Schaub S, Lanfranchi A, Ehlert U. Effects of an early intervention program on chronic biological stress – a longitudinal RCT with psychosocially disadvantaged children. In: Psychoneuroendocrinology. Vol. 61. 2015:35.
Lytle 2018 {published data only}
- Lytle S, Nagle-Yang S, Wolfish E, Gabriel M, Amin J, Huth-Bocks A. Mom Power: promoting parenting and maternal mental heath among families with young children. Journal of the American Academy of Child & Adolescent Psychiatry 2021;57(10S):S248.
Macfie 2020 {published data only}
- Macfie J, Towers CV, Fortner KB, Stuart GL, Zvara BJ, Kurdziel-Adams G, et al. Medication-assisted treatment vs detoxification for women who misuse opioids in pregnancy: associations with dropout, relapse, neonatal opioid withdrawal syndrome (NOWS), and childhood sexual abuse. Addictive Behaviors Reports 2020;12:100315. [DOI: 10.1016/j.abrep.2020.100315] [PMCID: PMC7752716] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
McGinnis 2018 {published data only}
- McGinnis EW, Guth S, Hudziak T, Marsh J, Meyer M, Hall A, et al. A randomized controlled trial with over-selection of peripartum wellness: program engagement in women across a range of risk. Journal of the American Academy of Child & Adolescent Psychiatry 2018;57(10S):S146. [Google Scholar]
Perrone 2021 {published data only}
- Perrone L, Imrisek SD, Dash A, Rodriguez M, Monticciolo E, Bernard K. Changing parental depression and sensitivity: randomized clinical trial of abc's effectiveness in the community. Development and Psychopathology 2021;33(3):1026-40. [DOI: 10.1017/S0954579420000310] [PMID: ] [DOI] [PubMed] [Google Scholar]
Portwood 2011 {published data only}
- Portwood SG, Lambert RG, Abrams LP, Brooks Nelson E. An evaluation of the Adults and Children Together (ACT) Against Violence Parents Raising Safe Kids Program. Journal of Primary Prevention 2011;32:147-60. [DOI] [PubMed] [Google Scholar]
Riem 2021 {published data only}
- Riem MM, Lotz AM, Horstman LI, Cima M, Verhees MW, Alyousefi-van Dijk K, et al. A soft baby carrier intervention enhances amygdala responses to infant crying in fathers: a randomized controlled trial. Psychoneuroendocrinology 2021;132:105380. [DOI: 10.1016/j.psyneuen.2021.105380] [PMID: ] [DOI] [PubMed] [Google Scholar]
Stevens‐Simon 2001 {published data only}
- Stevens-Simon C, Nelligan D, Kelly L. Adolescents at risk for mistreating their children. Part II: a home- and clinic-based prevention program. Child Abuse & Neglect 2001;25(6):753-69. [DOI: 10.1016/s0145-2134(01)00237-x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Taylor 1997 {published data only}
- Taylor JA, Davis RL, Kemper KJ. A randomized controlled trial of group versus individual well child care for high-risk children: maternal-child interaction and developmental outcomes. Pediatrics 1997;99(6):e9. [DOI: 10.1542/peds.99.6.e9] [PMID: ] [DOI] [PubMed] [Google Scholar]
Taylor 1998 {published data only}
- Taylor JA, Kemper KJ. Group well-child care for high-risk families: maternal outcomes. Archives of Pediatrics & Adolescent Medicine 1998;152(6):579-84. [DOI: 10.1001/archpedi.152.6.579] [PMID: ] [DOI] [PubMed] [Google Scholar]
Tiwari 2005 {published data only}
- Tiwari A, Leung WC, Leung TW, Humphreys J, Parker B, Ho PC. A randomised controlled trial of empowerment training for Chinese abused pregnant women in Hong Kong. BJOG 2005;112(9):1249-56. [DOI: 10.1111/j.1471-0528.2005.00709.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Tomfohr‐Madsen 2020 {published data only}
- Tomfohr-Madsen LM, Sedov I, MacKinnon A, Giesbrecht G. Mindfulness-based cognitive therapy in pregnancy on sleep quality: secondary analysis from a randomized controlled trial. Psychosomatic Medicine 2020;86(6):A201. [Google Scholar]
Tran 2019 {published data only}
- Tran T, Fisher J, Tuan T, Tran H, Nguyen T, Biggs B-A, et al. Learning clubs to improve women’s health and infant’s health and development in rural Vietnam: Acceptability, feasibility and indicators of impact of a multicomponent intervention. Archives of Women's Mental Health 2019;22(5):660. [Google Scholar]
Wisner 2017 {published data only}
- Wisner KL, Sit DKY, McShea M, Luther JF, Eng HF, Dills JL, et al. Telephone-based depression care management for postpartum women: a randomized controlled trial. Journal of Clinical Psychiatry 2017;78(9):1369-75. [DOI: 10.4088/JCP.15m10563] [PMCID: PMC7295181] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to ongoing studies
Kaltenbach 2021 {published data only}
- Kaltenbach E, Chisholm M, Xiong T, Thomson D, Crombach A, McGrath PJ. Online narrative exposure therapy for parents of children with neurodevelopmental disabilities suffering from posttraumatic stress symptoms - study protocol of a randomized controlled trial. European Journal of Psychotraumatology 2021;21(1):1991650. [DOI: 10.1080/20008198.2021.1991650] [DOI] [PMC free article] [PubMed] [Google Scholar]
- NCT04385927. Life Beyond Trauma: 1-on-1 e-health program for parents of neurodiverse children. www.clinicaltrials.gov/ct2/show/NCT04385927 (first received 13 May 2020).
NCT03175796 {published data only}
- NCT03175796. Infant Mental Health-Home Visiting Randomized Controlled Trial (IMH-HV RCT). https://clinicaltrials.gov/ct2/show/NCT03175796.
- Riggs JL, Rosenblum KL, Muzik M, Jester J, Freeman S, Huth-Bocks A, et al. Infant mental health home visiting mitigates impact of maternal adverse childhood experiences on toddler language competence: a randomized controlled trial. Journal of Developmental & Behavioral Pediatrics 2022;43(4):e227-36. [NCT03175796] [DOI] [PubMed] [Google Scholar]
- Rosenblum K, Muzik M, Riggs J. 20.4 Infant mental health home visiting buffers the adverse impact of maternal adverse childhood experiences on toddler and parent outcomes. Journal of the American Academy of Child and Adolescent Psychiatry 2020;59 (10 Suppl):S297. [Google Scholar]
NCT03938350 {published data only}
- NCT03938350. Dialectical behavior therapy for pregnant women [Dialectical behavior therapy skills training for high-risk African American pregnant women: feasibility and acceptability of implementation in prenatal clinics]. www.clinicaltrials.gov/ct2/show/NCT03938350 (first received 6 May 2019).
NCT04818112 {published data only}
- NCT04818112. A randomized controlled trial to improve mother-infant synchrony among women with childhood adversity. www.clinicaltrials.gov/ct2/show/NCT04818112 (first received 26 March 2021).
NL9179 {published data only}NL9179
- NL9179. Samen stap voor stap vooruit [Effectively intervening in traumatized parents and children after structural domestic violence]. trialsearch.who.int/?TrialID=NL9179 (first received 7 January 2021).
Additional references
Abidin 1995
- Abidin R. Parenting Stress Index. Lutz (FL): Psychological Assessment Resources Inc, 1995. [Google Scholar]
Abidin 1990
- Abidin RR. Parenting Stress Index (PSI), Short Form: Test Manual. Charlottesville (VA): Pediatric Psychology Press, 1990. [Google Scholar]
Agazzi 2019
- Agazzi H, Adams C, Ferron E, Ferron J, Shaffer-Hudkins E, Salloum A. Trauma-informed behavioral parenting for early intervention. Journal of Child and Family Studies 2019;28(8):2172-86. [DOI: 10.1007/s10826-019-01435-3] [DOI] [Google Scholar]
Ainsworth 1978
- Ainsworth MD, Blehar MC, Waters E, Wall SN. Patterns of Attachment: a Psychological Study of the Strange Situation. Hillsdale (NJ): Lawrence Erlbaum Associates, 1978. [Google Scholar]
Ainsworth 1997
- Ainsworth MS. The personal origins of attachment theory. An interview with Mary Salter Ainsworth. Interview by Peter L Rudnytsky. Psychoanalytic Study of the Child 1997;52:386-405. [PMID: ] [PubMed] [Google Scholar]
Alexander 2014
- Alexander PC. Intergenerational Cycles of Trauma and Violence: An Attachment and Family Systems Perspective. New York (NY): WW Norton & Company, 2014. [Google Scholar]
Alink 2019
- Alink LR, Cyr C, Madigan S. The effect of maltreatment experiences on maltreating and dysfunctional parenting: a search for mechanisms. Development and Psychopathology 2019;31(1):1-7. [DOI: 10.1017/S0954579418001517] [DOI] [Google Scholar]
Ammerman 2009
- Ammerman RT, Putnam FW, Altaye M, Chen L, Holleb LJ, Stevens J, et al. Changes in depressive symptoms in first time mothers in home visitation. Child Abuse & Neglect 2009;33(3):127-38. [DOI: 10.1016/j.chiabu.2008.09.005] [PMCID: PMC2710301] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Anda 2006
- Anda RF, Felitti VJ, Bremner JD, Walker JD, Whitfield C, Perry BD, et al. The enduring effects of abuse and related adverse experiences in childhood. A convergence of evidence from neurobiology and epidemiology. European Archives of Psychiatry and Clinical Neuroscience 2006;256(3):174-86. [DOI: 10.1007/s00406-005-0624-4] [PMCID: PMC3232061] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Anderson 2011
- Anderson LM, Petticrew M, Rehfuess E, Armstrong R, Ueffing E, Baker P, et al. Using logic models to capture complexity in systematic reviews. Research Synthesis Methods 2011;2(1):33-42. [DOI: 10.1002/jrsm.32] [PMID: ] [DOI] [PubMed] [Google Scholar]
Anghel 2019
- Anghel LA, Farcas AM, Oprean RN. An overview of the common methods used to measure treatment adherence. Medicine and Pharmacy Reports 2019;92(2):117-22. [DOI: 10.15386/mpr-1201] [DOI] [PMC free article] [PubMed] [Google Scholar]
APA 2017
- American Psychological Association. Clinical practice guideline for the treatment of post-traumatic stress disorder. What is cognitive behavioural therapy? 2017. www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral (accessed 5 March 2021).
APA 2020
- American Psychological Association. APA dictionary of psychology. dictionary.apa.org/hyperarousal (accessed 6 March 2021).
Arabena 2016
- Arabena K, Ritte R, Panozzo S, Agerholm J, Rolwey K, Johnston L, et al. First 1000 days Australia: an evidence-based model conceived of and led by Indigenous people to foster resilience, leadership and innovation in Aboriginal and Torres Strait Islander families through focusing on the period from (pre)conception to the age of two; 2016. static1.squarespace.com/static/5d1563ccaaafe00001ca3d2c/t/5d1841a20489990001d8a955/1561870778994/First1000DaysAustralia_Overview2016.pdf (accessed 20 March 2019).
Arch 2012
- Arch JJ, Dimidjian S, Chessick C. Are exposure-based cognitive behavioral therapies safe during pregnancy? Archives of Women's Mental Health 2012;15(6):445-57. [DOI: 10.1007/s00737-012-0308-9] [PMID: ] [DOI] [PubMed] [Google Scholar]
Arons 2005
- Arons J. "In a black hole": the (negative) space between longing and dread: home-based psychotherapy with a traumatized mother and her infant son. Psychoanalytic Study of the Child 2005;60(1):101-27. [DOI: 10.1080/00797308.2005.11800748] [PMID: ] [DOI] [PubMed] [Google Scholar]
Attkisson 1996
- Attkisson C, Greenfield TK. The Client Satisfaction Questionnaire (CSQ) scales and the Service Satisfaction Scale-30 (SSS-30). In: Sederer LL, Dickey B, editors(s). Outcomes Assessment in Clinical Practice. Baltimore (MD): Williams & Wilkins, 1996:120-7. [Google Scholar]
Austin 2017
- Austin MP, Highet N, Expert Working Group. Mental health care in the perinatal period: Australian clinical practice guideline; October 2017. cope.org.au/wp-content/uploads/2017/10/Final-COPE-Perinatal-Mental-Health-Guideline.pdf (accessed prior to 25 June 2021).
Ayers 2018
- Ayers S, Crawley R, Button S, Thornton A, Field AP, Flood C, et al. Evaluation of expressive writing for postpartum health: a randomised controlled trial. Journal of Behavioral Medicine 2018;41(5):614-26. [DOI: 10.1007/s10865-018-9970-3] [PMCID: PMC6209049] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Baas 2020
- Baas MA, Van Pampus MG, Braama L, Stramrood CA, De Jongh A. The effects of PTSD treatment during pregnancy: systematic review and case study. European Journal of Psychotraumatology 2020;11(1):1762310. [DOI: 10.1080/20008198.2020.1762310] [PMCID: PMC7473051] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Baker 2016
- Baker CN, Brown SM, Wilcox PD, Overstreet S, Arora P. Development and psychometric evaluation of the Attitudes Related to Trauma-Informed Care (ARTIC) Scale. School Mental Health 2016;8:61-76. [DOI: 10.1007/s12310-015-9161-0] [DOI] [Google Scholar]
Bant 2018
- Bant SE, Begic V, Komiti A, Newman L, Tonge B, Judd F, et al. Building Early Attachment and Resilience (BEAR Study): preliminary findings of maternal sensitivity and infant attachment security in an at risk sample. Nature >< Nurture. New Challenges for a 3rd Millennium Infant Mental Health: 16th Congress of the World Association for Infant Mental Health (WAIMH); 2018 May 26-30; Rome, Italy. [DOI: 10.13140/RG.2.2.31364.63361] [DOI]
Barlow 2007
- Barlow J, Davis H, McIntosh E, Jarrett, P, Mockford C, Stewart-Brown S. Role of home visiting in improving parenting and health in families at risk of abuse and neglect: results of a multicentre randomised controlled trial and economic evaluation. Archives of Disease in Childhood 2007;92(3):229-33. [DOI: 10.1136/adc.2006.095117] [PMCID: PMC2083433] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Barlow 2011
- Barlow J, Smailagic N, Bennett C, Huband N, Jones H, Coren E. Individual and group based parenting programmes for improving psychosocial outcomes for teenage parents and their children. Cochrane Database of Systematic Reviews 2011, Issue 3. Art. No: CD002964. [DOI: 10.1002/14651858.CD002964.pub2] [PMCID: PMC4164375] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bartholomew 1991
- Bartholomew K, Horowitz LM. Attachment styles among young adults: a test of a four-category model. Journal of Personality and Social Psychology 1991;61(2):226-44. [DOI: 10.1037/0022-3514.61.2.226] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bayley 2006
- Bayley N. Bayley Scales of Infant and Toddler Development. 3rd edition. Bloomington (MN): PsychCorp, Pearson, 2006. [Google Scholar]
Beck 1988a
- Beck AT, Steer RA, Carbin MG. Psychometric properties of the Beck Depression Inventory: twenty-five years of evaluation. Clinical Psychology Review 1988;8(1):77-100. [DOI: 10.1016/0272-7358(88)90050-5] [DOI] [Google Scholar]
Beck 1988b
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. Journal of Consulting and Clinical Psychology 1988;56(6):893-7. [DOI: 10.1037//0022-006x.56.6.893] [PMID: ] [DOI] [PubMed] [Google Scholar]
Beck 2000
- Beck CT, Gable RK. Postpartum Depression Screening Scale: development and psychometric testing. Nursing Research 2000;49(5):272-82. [DOI: 10.1097/00006199-200009000-00006] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bell 1998
- Bell L, St-Cyr Tribble D, Paul D, Lang A. A concept analysis of parent–infant attachment. Journal of Advanced Nursing 1998;28(5):1071-81. [DOI: 10.1046/j.1365-2648.1998.00815.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bell 2013
- Bell ML, McKenzie JE. Designing psycho-oncology randomised trials and cluster randomised trials: variance components and intra-cluster correlation of commonly used psychosocial measures. Psycho-oncology 2013;22(8):1738-47. [DOI: 10.1002/pon.3205] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bellhouse 2021
- Bellhouse C, Newman L, Bilardi JE, Temple-Smith M. A systematic narrative review of psychological interventions available in the antenatal period to prepare parents for parenting. Current Psychology 2021;9:1-14. [Google Scholar]
Bellis 2014
- Bellis MA, Lowey H, Leckenby N, Hughes K, Harrison D. Adverse childhood experiences: retrospective study to determine their impact on adult health behaviours and health outcomes in a UK population. Journal of Public Health 2014;36(1):81-91. [DOI: 10.1093/pubmed/fdt038] [PMID: ] [DOI] [PubMed] [Google Scholar]
Bellis 2019
- Bellis MA, Hughes K, Ford K, Ramos Rodriguez G, Sethi D, Passmore J. Life course health consequences and associated annual costs of adverse childhood experiences across Europe and North America: a systematic review and meta-analysis. Lancet. Public Health 2019;4(10):e517-28. [DOI: 10.1016/S2468-2667(19)30145-8] [PMCID: PMC7098477] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Belsky 1980
- Belsky J. Child maltreatment: an ecological integration. American Psychologist 1980;35(4):320-35. [DOI: 10.1037//0003-066x.35.4.320] [PMID: ] [DOI] [PubMed] [Google Scholar]
Benoit 2004
- Benoit D. Infant–parent attachment: definition, types, antecedents, measurement and outcome. Paediatrics & Child Health 2004;9(8):541-5. [DOI: 10.1093/pch/9.8.541] [PMCID: PMC2724160] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Berthelot 2018
- Berthelot N, Lemieux R, Lacharité C. Development of a prenatal program for adults with personal histories of childhood abuse or neglect: a Delphi consensus consultation study. Health Promotion and Chronic Disease Prevention in Canada: Research, Policy and Practice 2018;38(11):393-403. [DOI: 10.24095/hpcdp.38.11.01] [PMCID: PMC6262983] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bimler 2002
- Bimler D, Kirkland J. Unifying versions and criterion sorts of the AQS with a spatial model. Canadian Journal of Early Childhood Education 2002;9(1):2-18. [ERIC #: EJ671920] [Google Scholar]
Bisson 2020
- Bisson JI, Gelderen M, Roberts NP, Lewis C. Non-pharmacological and non-psychological approaches to the treatment of PTSD: results of a systematic review and meta-analyses. European Journal of Psychotraumatology 2020;11(1):1795361. [DOI: 10.1080/20008198.2020.1795361] [PMID: ] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bisson 2021
- Bisson J, Olff M. Prevention and treatment of PTSD: the current evidence base. European Journal of Psychotraumatology 2021;12(1):1824381. [DOI: 10.1080/20008198.2020.1824381] [DOI] [PMC free article] [PubMed] [Google Scholar]
Black 2017
- Black MM, Walker SP, Fernald LC, Andersen CT, DiGirolamo AM, Lu C, et al. Early childhood development coming of age: science through the life course. Lancet 2017;389(10064):77-90. [DOI: 10.1016/S0140-6736(16)31389-7] [PMCID: PMC5884058] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bohus 2020
- Bohus M, Kleindienst N, Hahn C, Müller-Engelmann M, Ludäscher P, Steil R, et al. Dialectical behavior therapy for posttraumatic stress disorder (DBT-PTSD) compared with cognitive processing therapy (CPT) in complex presentations of PTSD in women survivors of childhood abuse: a randomized clinical trial. JAMA Psychiatry 2020;77(12):1235-45. [DOI: 10.1001/jamapsychiatry.2020.2148] [PMCID: PMC7376475] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bottoms 2007
- Bottoms BL, Rudnicki AG, Epstein MA. A retrospective study of factors affecting the disclosure of childhood sexual and physical abuse. In: Pipe M-E, Lamb ME, Orbach Y, Cederborg A-C, editors(s). Child Sexual Abuse: Disclosure, Delay, and Denial. Mahwah (NJ): Lawrence Erlbaum Associates Publishers, 2007:175-94. [Google Scholar]
Bowen 2016
- Bowen EA, Murshid NS. Trauma-informed social policy: a conceptual framework for policy analysis and advocacy. American Journal of Public Health 2016;106(2):223-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bowlby 1969
- Bowlby J. Attachment and Loss: Volume I: Attachment. Michigan (MI): Hogarth Press and The Institute of Psycho-Analysis, 1969. [Google Scholar]
Bowlby 1988
- Bowlby J. The origins of attachment. In: A Secure Base: Clinical Applications of Attachment Theory. London (UK): Routledge, 1988:20-38. [Google Scholar]
BPS 2021
- British Psychological Society. Introduction to the PTMF. www.bps.org.uk/power-threat-meaning-framework/introduction-ptmf (accessed 5 March 2021).
Brave Heart 1998
- Brave Heart Maria Yellow Horse, DeBruyn Lemyra M. The American Indian holocaust: healing historical unresolved grief. American Indian and Alaska Native Mental Health Research 1998;8:60-82. [PubMed] [Google Scholar]
Bretherton 1992
- Bretherton I. The origins of attachment theory: John Bowlby and Mary Ainsworth. Developmental Psychology 1992;28(5):759-75. [DOI: 10.1037/0012-1649.28.5.759] [DOI] [Google Scholar]
Briggs‐Gowan 2004
- Briggs-Gowan MJ, Carter AS, Irwin JR, Wachtel K, Cicchetti DV. The Brief Infant-Toddler Social and Emotional Assessment: screening for social-emotional problems and delays in competence. Journal of Pediatric Psychology 2004;29(2):143-55. [DOI: 10.1093/jpepsy/jsh017] [PMID: ] [DOI] [PubMed] [Google Scholar]
Britto 2017
- Britto PR, Lye SJ, Proulx K, Yousafzai AK, Matthews SG, Vaivada T, et al. Nurturing care: promoting early childhood development. Lancet 2017;389(10064):91-102. [DOI] [PubMed] [Google Scholar]
Budd 1996
- Budd KS, Holdsworth MJ. Issues in clinical assessment of minimal parenting competence. Journal of Clinical Child Psychology 1996;25(1):2-14. [DOI: 10.1207/s15374424jccp2501_1] [DOI] [Google Scholar]
Bunting 2019
- Bunting L, Montgomery L, Mooney S, MacDonald M, Coulter S, Hayes D, et al. Trauma informed child welfare systems—a rapid evidence review. International Journal of Environmental Research and Public Health 2019;16(13):2365. [DOI: ] [PMCID: PMC6651663] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Campbell 2020
- Campbell M, McKenzie JE, Sowden A, Katikireddi SV, Brennan SE, Ellis S, et al. Synthesis without meta-analysis (SWiM) in systematic reviews: reporting guideline. BMJ 2020;368:16890. [DOI: 10.1136/bmj.l6890] [PMCID: PMC7190266] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Caro 2019
- Caro P, Turner W, Macdonald G. Comparative effectiveness of interventions for treating the psychological consequences of sexual abuse in children and adolescents. Cochrane Database of Systematic Reviews 2019, Issue 6. Art. No: CD013361. [DOI: 10.1002/14651858.CD013361] [DOI] [PMC free article] [PubMed] [Google Scholar]
Carver 1989
- Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. Journal of Personality and Social Psychology 1989;56(2):267-83. [DOI: 10.1037/0022-3514.56.2.267] [PMID: ] [DOI] [PubMed] [Google Scholar]
Chaffin 2011
- Chaffin M, Funderburk B, Bard D, Valle LA, Gurwitch R. A combined motivation and parent–child interaction therapy package reduces child welfare recidivism in a randomized dismantling field trial. Journal of Consulting and Clinical Psychology 2011;79(1):84-95. [DOI: 10.1037/a0021227] [PMID: ] [DOI] [PubMed] [Google Scholar]
Chamberlain 2019a
- Chamberlain C, Gee G, Brown SJ, Atkinson J, Herrman H, Gartland D, et al. Healing the Past by Nurturing the Future—co-designing perinatal strategies for Aboriginal and Torres Strait Islander parents experiencing complex trauma: framework and protocol for a community-based participatory action research study. BMJ Open 2019;9(6):e028397. [DOI: 10.1136/bmjopen-2018-028397] [PMCID: PMC6575864] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chamberlain 2019b
- Chamberlain C, Gee G, Harfield S, Campbell S, Brennan S, Clark Y, et al. Parenting after a history of childhood maltreatment: a scoping review and map of evidence in the perinatal period. PLOS One 2019;14(3):e0213460. [DOI: 10.1371/journal.pone.0213460] [PMCID: PMC6415835] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chamberlain 2019c
- Chamberlain C, Ralph N, Hokke S, Clark Y, Gee G, Stansfield C, et al. Healing The Past By Nurturing The Future: a qualitative systematic review and meta-synthesis of pregnancy, birth and early postpartum experiences and views of parents with a history of childhood maltreatment. PLOS One 2019;14(12):e0225441. [DOI: 10.1371/journal.pone.0225441] [PMCID: PMC6910698] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Chapman 2004
- Chapman DP, Whitfield CL, Felitti VJ, Dube SR, Edwards VJ, Anda RF. Adverse childhood experiences and the risk of depressive disorders in adulthood. Journal of Affective Disorders 2004;82(2):217-25. [DOI: 10.1016/j.jad.2003.12.013] [PMID: ] [DOI] [PubMed] [Google Scholar]
Cloitre 2013
- Cloitre M, Garvert DW, Brewin CR, Bryant RA, Maercker A. Evidence for proposed ICD-11 PTSD and complex PTSD: a latent profile analysis. European Journal of Psychotraumatology 2013;4:20706. [DOI: 10.3402/ejpt.v4i0.20706] [PMCID: PMC3656217] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Cloitre 2018
- Cloitre M, Shevlin M, Brewin CR, Bisson JI, Roberts NP, Maercker A, et al. The International Trauma Questionnaire: development of a self-report measure of ICD-11 PTSD and complex PTSD. Acta Psychiatrica Scandinavica 2018;138(6):536-46. [DOI: 10.111/acps.12956] [PMID: ] [DOI] [PubMed] [Google Scholar]
Cloitre 2019
- Cloitre M, Hyland P, Bisson JI, Brewin CR, Roberts NP, Karatzias T, et al. ICD-11 posttraumatic stress disorder and complex posttraumatic stress disorder in the United States: a population-based study. Journal of Traumatic Stress 2019;32(6):833-42. [DOI: 10.1002/jts.22454] [PMID: ] [DOI] [PubMed] [Google Scholar]
Cochrane Methods Equity 2021
- Cochrane Methods Equity. PROGRESS-Plus. methods.cochrane.org/equity/projects/evidence-equity/progress-plus (accessed 6 March 2021).
Cohen 1983
- Cohen S, Hoberman HM. Positive events and social supports as buffers of life change stress. Journal of Applied Social Psychology 1983;13(2):99-125. [DOI: 10.1111/j.1559-1816.1983.tb02325.x] [DOI] [Google Scholar]
Cohen 1997
- Cohen S, Doyle WJ, Skoner DP, Rabin BS, Gwaltney JM Jr. Social ties and susceptibility to the common cold. JAMA 1997;277(24):1940-4. [DOI: 10.1001/jama.1997.03540480040036] [PMID: ] [DOI] [PubMed] [Google Scholar]
Coles 2009
- Coles J, Jones K. "Universal precautions": perinatal touch and examination after childhood sexual abuse. Birth 2009;36(3):230-6. [DOI: 10.1111/j.1523-536X.2009.00327.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
Conching 2019
- Conching AKS, Thayer Z. Biological pathways for historical trauma to affect health: a conceptual model focusing on epigenetic modifications. Social Science & Medicine 2019;230:74-82. [DOI] [PubMed] [Google Scholar]
COPE 2017
- Centre of Perinatal Excellence (COPE). Mental Health in the Perinatal Period. Australian Clinical Practice Guideline; October 2017. cope.org.au/wp-content/uploads/2018/05/COPE-Perinatal-MH-Guideline_Final-2018.pdf (accessed 14 April 2021).
Counts 2017
- Counts JM, Gillam RJ, Perico S, Eggers KL. Lemonade for life—a pilot study on a hope-infused, trauma-informed approach to help families understand their past and focus on the future. Children and Youth Services Review 2017;79:228-34. [DOI: 10.1016/j.childyouth.2017.05.036] [DOI] [Google Scholar]
Covidence [Computer program]
- Covidence systematic review software. Version accessed 17 August 2022. Melbourne, Australia: Veritas Health Innovation, 2022. Available at covidence.org.
Cox 1987
- Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry 1987;150:782-6. [DOI: 10.1192/bjp.150.6.782] [PMID: ] [DOI] [PubMed] [Google Scholar]
Crittenden 2017
- Crittenden PM. Raising Parents: Attachment, Representation, and Treatment. New York (NY): Routledge, 2017. [Google Scholar]
Cusick 2019
- Cusick S, Georgieff MK. The first 1000 days of life: the brain's window of opportunity. www.unicef-irc.org/article/958 (accessed 27 March 2019).
Dahlberg 2002
- Dahlberg LL, Krug EG. Chapter 1. Violence – a global public health problem. In: Krug EG, Dahlberg LL, Mercy JA, Zwi AB, Lozano R, editors(s). World Report on Violence and Health. Geneva: World Health Organization, 2002:1-19. [WEB PAGE: www.who.int/violence_injury_prevention/violence/world_report/chapters/en/] [Google Scholar]
Day 2009
- Day T, Baker F, Darlington Y. Experiences of song writing in a group programme for mothers who had experienced childhood abuse. Nordic Journal of Music Therapy 2009;18(2):133-49. [DOI: 10.1080/08098130903062405] [DOI] [Google Scholar]
De Arellano 2014
- De Arellano MA, Lyman DR, Jobe-Shields L, George P, Dougherty RH, Daniels AS, et al. Trauma-focused cognitive-behavioral therapy for children and adolescents: assessing the evidence. Psychiatric Services 2014;65(5):591-602. [DOI: 10.1176/appi.ps.201300255] [PMCID: PMC4396183] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Deblinger 2003
- Deblinger E, Cohen J, Mannarino A. Child and Parent Trauma-Focused Cognitive Behavioral Therapy Treatment Manual. Pittsburgh (PA): Allegheny General Hospital Center for Traumatic Stress in Children and Adolescents, 2003. [Google Scholar]
Dechartres 2013
- Dechartres A, Trinquart L, Boutron I, Ravaud P. Influence of trial sample size on treatment effect estimates: meta-epidemiological study. BMJ 2013;346:f2304. [DOI: 10.1136/bmj.f2304] [PMCID: PMC3634626] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Deeks 2002
- Deeks JJ. Issues in the selection of a summary statistic for meta-analysis of clinical trials with binary outcomes. Statistics in Medicine 2002;21(11):1575-600. [DOI: 10.1002/sim.1188] [PMID: ] [DOI] [PubMed] [Google Scholar]
Deeks 2019
- Deeks JJ, Higgins JP, Altman DG, editor(s). Chapter 10: Analysing data and undertaking meta-analyses. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editors(s). Cochrane Handbook for Systematic Reviews of Interventions. 2nd edition. Chichester (UK): John Wiley & Sons, 2019:241-84. [Google Scholar]
DerSimonian 1986
- DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled Clinical Trials 1986;7(3):177-88. [DOI: 10.1016/0197-2456(86)90046-2] [PMID: ] [DOI] [PubMed] [Google Scholar]
DOH 2020
- Australian Government Department of Health (DoH). Clinical practice guidelines: pregnancy care 2020 edition, 2020. www.health.gov.au/resources/pregnancy-care-guidelines.
Dong 2003
- Dong M, Anda RF, Dube SR, Giles WH, Felitti VJ. The relationship of exposure to childhood sexual abuse to other forms of abuse, neglect, and household dysfunction during childhood. Child Abuse & Neglect 2003;27(6):625-39. [DOI: 10.1016/s0145-2134(03)00105-4] [PMID: ] [DOI] [PubMed] [Google Scholar]
Dretzke 2009
- Dretzke J, Davenport C, Frew E, Barlow J, Stewart-Brown S, Bayliss S, et al. The clinical effectiveness of different parenting programmes for children with conduct problems: a systematic review of randomised controlled trials. Child and Adolescent Psychiatry and Mental Health 2009;3(1):7. [DOI: 10.1186/1753-2000-3-7] [PMCID: PMC2660289] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ehring 2014
- Ehring T, Welboren R, Morina N, Wicherts JM, Freitag J, Emmelkamp PM. Meta-analysis of psychological treatments for posttraumatic stress disorder in adult survivors of childhood abuse. Clinical Psychology Review 2014;34(8):645-57. [DOI: 10.1016/j.cpr.2014.10.004] [PMID: ] [DOI] [PubMed] [Google Scholar]
Eilers 2021
- Eilers R, Rimane E, Vogel A, Renneberg B, Steil R, Rosner R. Response of young patients with probable ICD-11 complex PTSD to treatment with developmentally adapted cognitive processing therapy. European Journal of Psychotraumatology 2021;12(1):1929024. [DOI: 10.1080/20008198.2021.1929024] [PMCID: PMC8253183] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Elbanna 2021
- Elbanna A, Petrou S, Yiu HH, Daher S, Forrester D, Scourfield J, et al. Systematic review of economic evaluations of children's social care interventions. Children and Youth Services Review 2021;121:1-15. [DOI: 10.1016/j.childyouth.2020.105864] [DOI] [Google Scholar]
Elbourne 2002
- Elbourne DR, Altman DG, Higgins JP, Curtin F, Worthington HV, Vail A. Meta-analyses involving cross-over trials: methodological issues. International Journal of Epidemiology 2002;31(1):140-9. [DOI: ] [DOI] [PubMed] [Google Scholar]
Erickson 2019
- Erickson N, Julian M, Muzik M. Perinatal depression, PTSD, and trauma: impact on mother–infant attachment and interventions to mitigate the transmission of risk. International Review of Psychiatry 2019;31(3):245-63. [DOI: 10.1080/09540261.2018.1563529] [PMID: ] [DOI] [PubMed] [Google Scholar]
Fava 2016
- Fava NM, Simon VA, Smith E, Khan M, Kovacevic M, Rosenblum KL, et al. Perceptions of general and parenting-specific posttraumatic change among postpartum mothers with histories of childhood maltreatment. Child Abuse & Neglect 2016;56:20-9. [DOI: 10.1016/j.chiabu.2016.04.007] [PMCID: PMC4884472] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Feldman 2010
- Feldman R. The relational basis of adolescent adjustment: trajectories of mother–child interactive behaviors from infancy to adolescence shape adolescents' adaptation. Attachment & Human Development 2010;12(1-2):173-92. [DOI: 10.1080/14616730903282472] [PMID: ] [DOI] [PubMed] [Google Scholar]
Felitti 1998
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine 1998;14(4):245-58. [DOI: 10.1016/s0749-3797(98)00017-8] [PMID: ] [DOI] [PubMed] [Google Scholar]
Finkelhor 2014
- Finkelhor D, Shattuck A, Turner HA, Hamby SL. The lifetime prevalence of child sexual abuse and sexual assault assessed in late adolescence. Journal of Adolescent Health 2014;55(3):329-33. [DOI: 10.1016/j.jadohealth.2013.12.026] [PMID: ] [DOI] [PubMed] [Google Scholar]
Fisher 2018
- Fisher J, Acton C, Rowe H. Mental health problems among childbearing women: historical perspectives and social determinants. In: Muzik M, Rosenblum KL, editors(s). Motherhood in the Face of Trauma: Pathways Towards Healing and Growth. Cham (Switzerland): Springer International Publishing, 2018:3-20. [DOI: 10.1007/978-3-319-65724-] [DOI] [Google Scholar]
Foa 1999
- Foa EB, Ehlers A, Clark DM, Toli D, Orsillo SM. The Posttraumatc Cognitions Inventory (PTCI): development and validation. Psychological Assessment 1999;11(3):303-14. [DOI: 10.1037/1040-3590.11.3.303] [DOI] [Google Scholar]
Font 2016
- Font SA, Maguire-Jack K. Pathways from childhood abuse and other adversities to adult health risks: the role of adult socioeconomic conditions. Child Abuse & Neglect 2016;51:390-9. [DOI: 10.1016/j.chiabu.2015.05.013] [PMCID: PMC4670808] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Ford 2006
- Ford JD, Russo E. Trauma-focused, present-centered, emotional self-regulation approach to integrated treatment for posttraumatic stress and addiction: trauma adaptive recovery group education and therapy (TARGET). American Journal of Psychotherapy 2006;60(4):335-55. [DOI: 10.1176/appi.psychotherapy.2006.60.4.335] [PMID: ] [DOI] [PubMed] [Google Scholar]
Frechtling 2007
- Frechtling JA. Logic Modeling Methods in Program Evaluation. San Francisco (CA): Jossey-Bass, 2007. [Google Scholar]
Frost 2020
- Frost R, Hyland P, Shevlin M, Murphy J. Distinguishing complex PTSD from borderline personality disorder among individuals with a history of sexual trauma: a latent class analysis. European Journal of Trauma & Dissociation 2020;4(1):100080. [DOI: 10.1016/j.ejtd.2018.08.004] [DOI] [Google Scholar]
Funnell 2011
- Funnell SC, Rogers PJ. Purposeful Program Theory: Effective Use of Theories of Change and Logic Models. San Francisco (CA): Josey-Bass, 2011. [Google Scholar]
Gannon 2017
- Gannon M, Mackenzie M, Kaltenbach K, Abatemarco D. Impact of mindfulness-based parenting on women in treatment for opioid use disorder. Journal of Addiction Medicine 2017;11(5):368-76. [DOI: 10.1097/ADM.0000000000000336] [PMID: ] [DOI] [PubMed] [Google Scholar]
Giladi 2013
- Giladi Lotem, Bell Terece S. Protective factors for intergenerational transmission of trauma among second and third generation Holocaust survivors.. Psychological Trauma: Theory, Research, Practice, and Policy 2013;5(4):384. [Google Scholar]
Gouveia 2019
- Gouveia FV, Gidyk DC, Giacobbe P, Ng E, Meng Y, Davidson B, et al. Neuromodulation strategies in post-traumatic stress disorder: from preclinical models to clinical applications. Brain Sciences 2019;9(2):45. [DOI: 10.3390/brainsci9020045] [PMCID: PMC6406551] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- GRADEpro GDT: GRADEpro Guideline Development Tool [Software]. Version accessed 17 August 2022. Hamilton (ON): McMaster University and Evidence Prime, 2022. Available from gradepro.org.
Gratz 2004
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment 2004;26(1):41-54. [DOI: 10.1023/B:JOBA.0000007455.08539.94] [DOI] [Google Scholar]
Graybeal 2007
- Graybeal CT. Evidence for the art of social work. Families in Society 2007;88(4):513-23. [DOI: 10.1606/1044-3894.3673] [DOI] [Google Scholar]
Green 2007
- Green BL, Furrer C, McAllister C. How do relationships support parenting? Effects of attachment style and social support on parenting behavior in an at-risk population. American Journal of Community Psychology 2007;40(1):96-108. [DOI] [PubMed] [Google Scholar]
Griffin 1994
- Griffin DW, Bartholomew K. Models of the self and other: fundamental dimensions underlying measures of adult attachment. Journal of Personality and Social Psychology 1994;67(3):430-45. [DOI: 10.1037/0022-3514.67.3.430] [DOI] [Google Scholar]
Gross 1993
- Gross D, Conrad B, Fogg L, Willis L, Garvey C. What does the NCATS (Nursing Child Assessment Teaching Scale) measure? Nursing Research 1993;42(5):260-5. [PMID: ] [PubMed] [Google Scholar]
Grote 2017
- Grote NK, Simon GE, Russo J, Lohr MJ, Carson K, Katon W. Incremental benefit-cost of MOMCare: collaborative care for perinatal depression among economically disadvantaged women. Psychiatric Services 2017;68(11):1164-71. [DOI: 10.1176/appi.ps.201600411] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hagan 2017
- Hagan MJ, Browne DT, Sulik M, Ippen CG, Bush N, Lieberman AF. Parent and child trauma symptoms during child–parent psychotherapy: a prospective cohort study of dyadic change. Journal of Traumatic Stress 2017;30(6):690-7. [DOI: 10.1002/jts.22240] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hardcastle 2018
- Hardcastle K, Bellis MA, Ford K, Hughes K, Garner J, Rodriguez GR. Measuring the relationships between adverse childhood experiences and educational and employment success in England and Wales: findings from a retrospective study. Public Health 2018;165:106-16. [DOI: 10.1016/j.puhe.2018.09.014] [PMID: ] [DOI] [PubMed] [Google Scholar]
Harris 2020
- Harris M, Andrews K, Gonzalez A, Prime H, Atkinson L. Technology-assisted parenting interventions for families experiencing social disadvantage: a meta-analysis. Prevention Science 2020;21(5):714-27. [DOI: 10.1007/s11121-020-01128-0] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hartung 2001
- Hartung J, Knapp G. A refined method for the meta-analysis of controlled clinical trials with binary outcome. Statistics in Medicine 2001;20(24):3875-89. [DOI: 10.1002/sim.1009] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hendriksen 2014
- Hendriksen H, Olivier B, Oosting RS. From non-pharmacological treatments for post-traumatic stress disorder to novel therapeutic targets. European Journal of Pharmacology 2014;732:139-58. [DOI: 10.1016/j.ejphar.2014.03.031] [PMID: ] [DOI] [PubMed] [Google Scholar]
Herman 1992
- Herman J. Trauma and Recovery. The Aftermath of Violence—From Domestic Abuse to Political Terror. New York (NY): Basic Books, 1992. [Google Scholar]
Hiebert‐Murphy 2000
- Hiebert-Murphy D, Richert M. A parenting group for women dealing with child sexual abuse and substance abuse. International Journal of Group Psychotherapy 2000;50(3):397-405. [DOI: 10.1080/00207284.2000.11491016] [PMID: ] [DOI] [PubMed] [Google Scholar]
Higgins 2003
- Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327(7414):557-60. [DOI: 10.1136/bmj.327.7414.557] [PMCID: PMC192859] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2022
- Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (updated February 2022). Cochrane, 2022. Available from training.cochrane.org/handbook.
Higgins 2022a
- Higgins JP, Eldridge S, Li T (editors). Chapter 23: Including variants on randomized trials. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane, 2022. Available from training.cochrane.org/handbook.
Higgins 2022b
- Higgins JP, Savović J, Page MJ, Elbers RG, Sterne JA. Chapter 8: Assessing risk of bias in a randomized trial. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane, 2022. Available from www.training.cochrane.org/handbook.
Hoeboer 2021
- Hoeboer CM, De Kleine RA, Oprel DA, Schoorl M, Van der Does W, Van Minnen A. Does complex PTSD predict or moderate treatment outcomes of three variants of exposure therapy? Journal of Anxiety Disorders 2021;80:102388. [DOI: 10.1016/j.janxdis.2021.102388] [PMID: ] [DOI] [PubMed] [Google Scholar]
Hohlfeld 2018
- Hohlfeld AS, Harty M, Engel ME. Parents of children with disabilities: a systematic review of parenting interventions and self-efficacy. African Journal of disability 2018;7:437. [DOI: 10.4102/ajod.v7i0.437] [PMCID: PMC6244143] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hopper 2010
- Hopper EK, Bassuk EL, Olivet J. Shelter from the storm: trauma-informed care in homelessness services settings. Open Health Services and Policy Journal 2010;3(2):80-100. [DOI: 10.2174/1874924001003020080] [DOI] [Google Scholar]
Hosenbocus 2011
- Hosenbocus S, Chahal R. SSRIs and SNRIs: a review of the discontinuation syndrome in children and adolescents. Journal of the Canadian Academy of Child and Adolescent Psychiatry 2011;20(1):60-7. [PMCID: PMC3024727] [PMID: ] [PMC free article] [PubMed] [Google Scholar]
Hoskins 2021
- Hoskins MD, Sinnerton R, Nakamura A, Underwood JF, Slater A, Lewis C, et al. Pharmacological-assisted psychotherapy for post-traumatic stress disorder: a systematic review and meta-analysis. European Journal of Psychotraumatology 2021;12(1):1853379. [DOI: 10.1080/20008198.2020.1853379] [PMCID: PMC7874936] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Howe 2006
- Howe D. Developmental attachment psychotherapy with fostered and adopted children. Child and Adolescent Mental Health 2006;11(3):128-34. [DOI] [PubMed] [Google Scholar]
Hulshof 2020
- Hulshof TA, Zuidema SU, Gispen-de Wied CC, Luijendijk HJ. Run-in periods and clinical outcomes of antipsychotics in dementia: a meta-epidemiological study of placebo-controlled trials. Pharmacoepidemiology and Drug Safety 2020;29(2):125-33. [DOI: 10.1002/pds.4903] [PMCID: PMC7027584] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hyland 2017
- Hyland P, Shevlin M, Brewin CR, Cloitre M, Downes A, Jumbe S, et al. Validation of post-traumatic stress disorder (PTSD) and complex PTSD using the International Trauma Questionnaire. Acta Psychiatrica Scandinavica 2017;136(3):313-22. [DOI: 10.1111/acps.12771] [PMID: ] [DOI] [PubMed] [Google Scholar]
Isobel 2018
- Isobel S, Goodyear M, Furness T, Foster K. Preventing intergenerational trauma transmission: a critical interpretive synthesis. Journal of Clinical Nursing 2018;28(7-8):1100-13. [DOI] [PubMed] [Google Scholar]
Izzo 2000
- Izzo C, Weiss L, Shanahan T, Rodriguez-Brown F. Parental self-efficacy and social support as predictors of parenting practices and children's socioemotional adjustment in Mexican immigrant families. Journal of Prevention & Intervention in the Community 2000;20(1-2):197-213. [Google Scholar]
Jeong 2021
- Jeong J, Franchett EE, Ramos de Oliveira CV, Rehmani K, Yousafzai AK. Parenting interventions to promote early child development in the first three years of life: a global systematic review and meta-analysis. PLOS Medicine 2021;18(5):e1003602. [DOI: 10.1371/journal.pmed.1003602] [PMCID: PMC8109838] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Johnstone 2018
- Johnstone L, Boyle M. The power threat meaning framework: an alternative nondiagnostic conceptual system. Journal of Humanistic Psychology 2018;N/A:1-18. [Google Scholar]
Jones 2005
- Jones TL, Prinz RJ. Potential roles of parental self-efficacy in parent and child adjustment: a review. Clinical Psychology Review 2005;25(3):341-63. [DOI: 10.1016/j.cpr.2004.12.004] [PMID: ] [DOI] [PubMed] [Google Scholar]
Jonzon 2004
- Jonzon E, Lindblad F. Disclosure, reactions, and social support: findings from a sample of adult victims of child sexual abuse. Child Maltreatment 2004;9(2):190-200. [DOI: 10.1177/1077559504264263] [PMID: ] [DOI] [PubMed] [Google Scholar]
Karatzias 2017
- Karatzias T, Shevlin M, Fyvie C, Hyland P, Efthymiadou E, Wilson D, et al. Evidence of distinct profiles of posttraumatic stress disorder (PTSD) and complex posttraumatic stress disorder (CPTSD) based on the new ICD-11 Trauma Questionnaire (ICD-TQ). Journal of Affective Disorders 2017;207:181-7. [DOI] [PubMed] [Google Scholar]
Karatzias 2019
- Karatzias T, Murphy P, Cloitre M, Bisson J, Roberts N, Shevlin M, et al. Psychological interventions for ICD-11 complex PTSD symptoms: systematic review and meta-analysis. Psychological Medicine 2019;49(11):1761-75. [DOI: 10.1017/S0033291719000436] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kezelman 2012
- Kezelman C, Stavropoulos P. Practice Guidelines for Treatment of Complex Trauma and Trauma Informed Care and Service Delivery. Sydney (Australia): Blue Knot Foundation, 2012. [Google Scholar]
Kezelman 2019
- Kezelman C, Stavropoulos P. Practice Guidelines for Clinical Treatment of Complex Trauma. Sydney (Australia): Blue Knot Foundation, 2019. [Google Scholar]
King 2019
- King S, Chen KD, Chokshi B. Becoming trauma informed: validating a tool to assess health professional's knowledge, attitude, and practice. Pediatric Quality & Safety 2019;4(5):e215. [DOI: 10.1097/pq9.0000000000000215] [PMCID: PMC6831052] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kirkland 2004
- Kirkland J, Bimler D, Drawneek A, McKim M, Schölmerich A. An alternative approach for the analyses and interpretation of attachment sort items. Early Child Development and Care 2004;174(7-8):701-19. [PMID: 10.1080/0300443042000187185] [DOI] [Google Scholar]
Ko 2008
- Ko SJ, Ford JD, Kassam-Adams N, Berkowitz SJ, Wilson C, Wong M, et al. Creating trauma-informed systems: child welfare, education, first responders, health care, juvenile justice. Professional Psychology: Research and Practice 2008;39(4):396-404. [DOI: ] [Google Scholar]
Kogan 2004
- Kogan SM. Disclosing unwanted sexual experiences: results from a national sample of adolescent women. Child Abuse & Neglect 2004;28(2):147-65. [DOI: 10.1016/j.chiabu.2003.09.014] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kotchick 2005
- Kotchick BA, Dorsey S, Heller L. Predictors of parenting among African American single mothers: personal and contextual factors. Journal of Marriage and Family 2005;67(2):448-60. [Google Scholar]
Krug 2002
- Krug EG, Mercy JA, Dahlberg LL, Zwi AB. The world report on violence and health. Lancet 2002;360(9339):1083-8. [DOI: 10.1016/S0140-6736(02)11133-0] [PMID: ] [DOI] [PubMed] [Google Scholar]
Kubany 1996
- Kubany ES, Haynes SN, Abueg FR, Manke FP, Brennan JM, Stahura C. Development and validation of the Trauma-Related Guilt Inventory (TRGI). Psychological Assessment 1996;8(4):428-44. [DOI: 10.1037/1040-3590.8.4.428] [DOI] [Google Scholar]
Lange 2020
- Lange BC, Condon EM, Gardner F. Parenting among mothers who experienced child sexual abuse: a qualitative systematic review. Qualitative Health Research 2020;30(1):146-61. [DOI: 10.1177/1049732319882914] [PMID: ] [DOI] [PubMed] [Google Scholar]
Larrieu 2004
- Larrieu JA, Zeanah CH. Treating parent-infant relationships in the context of maltreatment: an integrated systems approach. In: Sameroff AJ, McDonough SC, Rosenblum KL, editors(s). Treating Parent-Infant Relationship Problems: Strategies for Intervention. London, UK: Guilford Press, 2004:243-64. [Google Scholar]
Latimer 2013
- Latimer S, Meade T, Tennant A. Measuring engagement in deliberate self-harm behaviours: psychometric evaluation of six scales. BMC Psychiatry 2013;13(4):1-11. [DOI: 10.1186/1471-244X-13-4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Law 2019
- Law E, Fisher E, Eccleston C, Palermo TM. Psychological interventions for parents of children and adolescents with chronic illness. Cochrane Database of Systematic Reviews 2019, Issue 3. Art. No: CD009660. [DOI: 10.1002/14651858.CD009660.pub4] [PMCID: PMC6450193] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
LeCroy 2011
- LeCroy CW, Krysik J. Randomized trial of the healthy families Arizona home visiting program. Children and Youth Services Review 2011;33(10):1761-6. [DOI: 10.1016/j.childyouth.2011.04.036] [DOI] [Google Scholar]
Lefebvre 2021
- Lefebvre C, Glanville J, Briscoe S, Littlewood A, Marshall C, Metzendorf M-I, et al. Technical Supplement to Chapter 4: Searching for and selecting studies. In: Higgins JP, Thomas J, Chandler J, Cumpston MS, Li T, Page MJ, et al, editor(s). Cochrane Handbook for Systematic Reviews of Interventions Version 6.2 (updated February 2021). Cochrane, 2021. Available from: www.training.cochrane.org/handbook.
Levenson 2017
- Levenson J. Trauma-informed social work practice. Social Work 2017;62(2):105-13. [DOI] [PubMed] [Google Scholar]
Lewis 2020
- Lewis C, Roberts NP, Andrew M, Starling E, Bisson JI. Psychological therapies for post-traumatic stress disorder in adults: systematic review and meta-analysis. European Journal of Psychotraumatology 2020;11(1):1729633. [DOI: 10.1080/20008198.2020.1729633] [PMCID: PMC7144187] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Lieberman 2004
- Lieberman A, Horn P. Assessment and treatment of young children exposed to traumatic events. In: Osofsky JD, editors(s). Young Children and Trauma: Intervention and Treatment. London (UK): Guilford Press, 2004:111-38. [Google Scholar]
London 2005
- London K, Bruck M, Ceci SJ, Shuman DW. Disclosure of child sexual abuse: what does the research tell us about the ways that children tell? Psychology, Public Policy, and Law 2005;11(1):194-226. [DOI: 10.1037/1076-8971.11.1.194] [DOI] [Google Scholar]
London 2008
- London K, Bruck M, Wright DB, Ceci SJ. Review of the contemporary literature on how children report sexual abuse to others: findings, methodological issues, and implications for forensic interviewers. Memory 2008;16(1):29-47. [DOI: 10.1080/09658210701725732] [PMID: ] [DOI] [PubMed] [Google Scholar]
Marks 1986
- Marks IM. Behavioural Psychotherapy: Maudsley Pocket Book of Clinical Management. Bristol (UK): John Wright, 1986. [Google Scholar]
Marshall 2018
- Marshall IJ, Noel-Storr A, Kuiper J, Thomas J, Wallace BC. Machine learning for identifying randomized controlled trials: an evaluation and practitioner's guide. Research Synthesis Methods 2018;9(4):602-14. [DOI: 10.1002/jrsm.1287] [PMCID: PMC6030513] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
McKenna 2022
- McKenna BG, Choi J, Brennan PA, K Knight A, Smith AK, R Pilkay S, et al. Maternal adversity and epigenetic age acceleration predict heightened emotional reactivity in offspring: implications for intergenerational transmission of risk. Research on Child and Adolescent Psychopathology 2022 Oct 13 [Online ahead of print]. [DOI: 10.1007/s10802-022-00981-7] [DOI] [PubMed]
McKenzie 2019a
- McKenzie JE, Brennan SE, Ryan RE, Thompson HJ, Johnston RV. Chapter 9. Summarising study characteristics and preparing for synthesis. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editors(s). Cochrane Handbook of Systematic Reviews of Interventions. 2nd edition. Chichester (UK): Wiley & Sons, 2019:229-40. [Google Scholar]
McKenzie 2019b
- McKenzie JE, Brennan SE. Chapter 12: Synthesizing and presenting findings using other methods. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editors(s). Cochrane Handbook for Systematic Reviews of Interventions. 2nd edition. Chichester (UK): Wiley & Sons, 2019:321-47. [Google Scholar]
McTavish 2020
- McTavish JR, Gonzalez A, Santesso N, MacGregor JC, McKee C, MacMillan HL. Identifying children exposed to maltreatment: a systematic review update. BMC Pediatrics 2020;20:1-14. [DOI: 10.1186/s12887-020-2015-4] [DOI] [PMC free article] [PubMed] [Google Scholar]
Melton 2020
- Melton H, Meader N, Dale H, Wright K, Jones-Diette J, Temple M, et al. Interventions for adults with a history of complex traumatic events: the INCiTE mixed-methods systematic review. Health Technology Assessment (Winchester, England) 2020;24(43):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mihelic 2017
- Mihelic M, Morawska A, Filus A. Effects of early parenting interventions on parents and infants: a meta-analytic review. Journal of Child and Family Studies 2017;26:1507-26. [DOI: 10.1007/s10826-017-0675-y] [DOI] [Google Scholar]
Miklósi 2017
- Miklósi M, Szabó M, Simon L. The role of mindfulness in the relationship between perceived parenting, early maladaptive schemata and parental sense of competence. Mindfulness 2017;8(2):471-80. [DOI: 10.1007/s12671-016-0619-4] [DOI] [Google Scholar]
Missler 2020
- Missler M, Straten A, Denissen J, Donker T, Beijers R. Effectiveness of a psycho-educational intervention for expecting parents to prevent postpartum parenting stress, depression and anxiety: a randomized controlled trial. BMC Pregnancy and Childbirth 2020;20(1):658. [DOI: 10.1186/s12884-020-03341-9] [PMCID: PMC7603696] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mitchell 2020
- Mitchell AE, Morawska A, Mihelic M. A systematic review of parenting interventions for child chronic health conditions. Journal of Child Health Care 2020;24(4):603-28. [DOI: 10.1177/1367493519882850] [PMID: ] [DOI] [PubMed] [Google Scholar]
Moog 2018
- Moog NK, Entringer S, Rasmussen JM, Styner M, Gilmore JH, Kathmann N, et al. Intergenerational effect of maternal exposure to childhood maltreatment on newborn brain anatomy. Biological Psychiatry 2018;83(2):120-7. [DOI: 10.1016/j.biopsych.2017.07.009] [PMCID: PMC5723537] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Morelen 2018
- Morelen D, Rosenblum KL, Muzik M. Childhood maltreatment and motherhood: implications for maternal well-being and mothering. In: Muzik M, Rosenblum KL, editors(s). Motherhood in the Face of Trauma: Pathways Towards Healing and Growth. Cham (Switzerland): Springer International Publishing, 2018:23-37. [DOI: 10.1007/978-3-319-65724-0] [DOI] [Google Scholar]
Morrill 2016
- Morrill MI, Hawrilenko M, Córdova JV. A longitudinal examination of positive parenting following an acceptance-based couple intervention. Journal of Family Psychology 2016;30(1):104. [DOI] [PMC free article] [PubMed] [Google Scholar]
Morrison 2014
- Morrison J, Pikhart H, Ruiz M, Goldblatt P. Systematic review of parenting interventions in European countries aiming to reduce social inequalities in children’s health and development. BMC Public Health 2014;14:1040. [DOI: 10.1186/1471-2458-14-1040] [PMCID: PMC4203958] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mundt 2002
- Mundt JC, Marks IM, Shear MK, Greist JM. The Work and Social Adjustment Scale: a simple measure of impairment in functioning. British Journal of Psychiatry 2002;180(5):461-4. [DOI: 10.1192/bjp.180.5.461] [PMID: ] [DOI] [PubMed] [Google Scholar]
Muzik 2015
- Muzik M, Rosenblum KL, Alfafar EA, Schuster MM, Miller NM, Waddell RM, et al. Mom Power: preliminary outcomes of a group intervention to improve mental health and parenting among high-risk mothers. Archives of Women's Mental Health 2015;18(3):507-21. [DOI: 10.1007/s00737-014-0490-z] [PMCID: PMC4439267] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Nanni 2012
- Nanni V, Uher R, Danese A. Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: a meta-analysis. American Journal of Psychiatry 2012;169(2):141-51. [DOI: 10.1176/appi.ajp.2011.11020335] [PMID: ] [DOI] [PubMed] [Google Scholar]
Narayan 2019
- Narayan AJ, Ippen CG, Harris WW, Lieberman AF. Protective factors that buffer against the intergenerational transmission of trauma from mothers to young children: a replication study of angels in the nursery. Development and Psychopathology 2019;31(1):173-87. [DOI: 10.1017/S0954579418001530] [PMID: ] [DOI] [PubMed] [Google Scholar]
NCTSN 2012
- National Child Traumatic Stress Network. Child–Parent Psychotherapy; 2012. www.nctsn.org/interventions/child-parent-psychotherapy (accessed 5 March 2021).
Nillni 2018
- Nillni YI, Mehralizadec A, Mayerb L, Milanovicb S. Treatment of depression, anxiety, and trauma-related disorders during the perinatal period: a systematic review. Clinical Psychology Review 2018;66:136-48. [DOI: 10.1016/j.cpr.2018.06.004] [PMCID: PMC6637409] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Noel‐Storr 2021
- Noel-Storr A, Dooley G, Affengruber L, Gartlehner G. Citation screening using crowdsourcing and machine learning produced accurate results: evaluation of Cochrane's modified Screen4Me service. Journal of Clinical Epidemiology 2021;130:23-31. [DOI: 10.1016/j.jclinepi.2020.09.024] [PMID: ] [DOI] [PubMed] [Google Scholar]
O'Neill 2014
- O'Neill J, Tabish H, Welch V, Petticrew M, Pottie K, Clarke M, et al. Applying an equity lens to interventions: using PROGRESS ensures consideration of socially stratifying factors to illuminate inequities in health. Journal of Clinical Epidemiology 2014;67(1):56-64. [DOI: 10.1016/j.jclinepi.2013.08.005] [PMID: ] [DOI] [PubMed] [Google Scholar]
Oprel 2021
- Oprel DA, Hoeboer CM, Schoorl M, De Kleine RA, Cloitre M, Wigard IG, et al. Effect of prolonged exposure, intensified prolonged exposure and STAIR+prolonged exposure in patients with PTSD related to childhood abuse: a randomized controlled trial. European Journal of Psychotraumatology 2021;12(1):1851511. [DOI: 10.1080/20008198.2020.1851511] [PMCID: PMC8500700] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Oral 2016
- Oral R, Ramirez M, Coohey C, Nakada S, Walz A, Kuntz A, et al. Adverse childhood experiences and trauma informed care: the future of health care. Paediatric Research 2016;79(1-2):227-33. [DOI: 10.1038/pr.2015.197] [PMID: ] [DOI] [PubMed] [Google Scholar]
Oxford 2016
- Oxford ML, Spieker SJ, Lohr MJ, Fleming CB. Promoting First Relationships(®): randomized trial of a 10-week home visiting program with families referred to child protective services. Child Maltreatment 2016;21(4):267-77. [DOI: 10.1177/1077559516668274] [PMCID: PMC5357588] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Oxford 2018
- Oxford ML, Spieker SJ, Lohr MJ, Fleming CB, Dillon C, Rees J. Ensuring implementation fidelity of a 10-week home visiting program in two randomized clinical trials. Maternal and Child Health Journal 2018;22(3):376-83. [DOI: 10.1007/s10995-017-2387-8] [PMCID: PMC5845475] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
O’Neill 2018
- O’Neill L, Fraser T, Kitchenham A, McDonald V. Hidden burdens: a review of intergenerational, historical and complex trauma, implications for indigenous families. Journal of Child & Adolescent Trauma 2018;11(2):173-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
Page 2019
- Page MJ, Higgins JP, Sterne JA. Chapter 13: Assessing risk of bias due to missing results in a synthesis. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editors(s). Cochrane Handbook for Systematic Reviews of Interventions. 2nd edition. Chichester (UK): John Wiley & Sons, 2019:349-74. [Google Scholar]
Page 2021
- Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. [DOI: 10.1136/bmj.n71] [PMCID: PMC8005924] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Paris 2013
- Paris E. Interrupting trauma and advancing development: considering parent education in contemporary psychoanalytic treatment. Clinical Social Work Journal 2013;41(1):84-92. [DOI: 10.1007/s10615-012-0412-3] [DOI] [Google Scholar]
Perlman 2011
- Perlman F, Brandell J. Psychoanalytical theory. In: Brandell JR, editors(s). Theory & Practice in Clinical Social Work. 2nd edition. London (UK): Sage Publications, 2011:38-80. [Google Scholar]
Peters 2008
- Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L. Contour-enhanced meta-analysis funnel plots help distinguish publication bias from other causes of asymmetry. Journal of Clinical Epidemiology 2008;61(10):991-6. [DOI: 10.1016/j.jclinepi.2007.11.010] [PMID: ] [DOI] [PubMed] [Google Scholar]
Petruccelli 2019
- Petruccelli K, Davis J, Berman T. Adverse childhood experiences and associated health outcomes: a systematic review and meta-analysis. Child Abuse & Neglect 2019;97:104127. [DOI: 10.1016/j.chiabu.2019.104127] [PMID: ] [DOI] [PubMed] [Google Scholar]
Phoenix Australia 2020
- Phoenix Australia. Australian Guidelines for the Prevention and Treatment of Acute Stress Disorder, Posttraumatic Stress Disorder and Complex PTSD; July 2020. www.phoenixaustralia.org/australian-guidelines-for-ptsd/ (accessed 3 December 2019).
Piccini 2021
- Piccini O. The mother’s body, the role of pleasure in the mother–infant relationship, and the traumatic risk. International Forum of Psychoanalysis 2021;30(3):129-38. [PMID: ] [Google Scholar]
Pickering 2015
- Pickering JA, Sanders MR. The Triple P-Positive Parenting Program: an example of a public health approach to evidence-based parenting support. Family Matters 2015;96:53-63. [WEB PAGE: aifs.gov.au/sites/default/files/fm96-jp.pdf] [Google Scholar]
Plant 2017
- Plant DT, Pawlby S, Pariante CM, Jones FW. When one childhood meets another – maternal childhood trauma and offspring child psychopathology: a systematic review. Clinical Child Psychology and Psychiatry 2017;23(3):483-500. [DOI] [PubMed] [Google Scholar]
Pontoppidan 2016
- Pontoppidan M, Klest SK, Patras J, Rayce SB. Effects of universally offered parenting interventions for parents with infants: a systematic review. BMJ Open 2016;6(9):e011706. [DOI: 10.1136/bmjopen-2016-011706] [PMCID: PMC5051433] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Popp 2015
- Popp L, Schneider S. Attention placebo control in randomized controlled trials of psychosocial interventions: theory and practice. Trials 2015;16:150. [DOI: 10.1186/s13063-015-0679-0] [PMCID: PMC4404062] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
PTSD UK 2021
- PTSD UK. What is PTSD hypervigilance? www.ptsduk.org/what-is-ptsd-hypervigilance/ (accessed 6 March 2021).
Raistrick 1994
- Raistrick D, Bradshaw J, Tober G, Weiner J, Allison J, Healey C. Development of the Leeds Dependence Questionnaire (LDQ): a questionnaire to measure alcohol and opiate dependence in the context of a treatment evaluation package. Addiction 1994;89(5):563-72. [DOI: 10.1111/j.1360-0443.1994.tb03332] [PMID: ] [DOI] [PubMed] [Google Scholar]
Rajecki 1978
- Rajecki DW, Lamb ME, Obmascher P. Toward a general theory of infantile attachment: a comparative review of aspects of the social bond. Behavioral and Brain Sciences 1978;1(3):417-36. [DOI: 10.1017/S0140525X00075816] [DOI] [Google Scholar]
Rayce 2020
- Rayce SB, Rasmussen IS, Væver MS, Pontoppidan M. Effects of parenting interventions for mothers with depressive symptoms and an infant: systematic review and meta-analysis. British Journal of Psychiatry Open 2020;6(1):E9, 1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rehfuess 2018
- Rehfuess EA, Booth A, Brereton L, Burns J, Gerhardus A, Mozygemba K, et al. Towards a taxonomy of logic models in systematic reviews and health technology assessments: a priori, staged, and iterative approaches. Research Synthesis Methods 2018;9(1):13-24. [DOI: 10.1002/jrsm.1254] [PMID: ] [DOI] [PubMed] [Google Scholar]
Reid 2021
- Reid C, Gee G, Bennetts SK, Clark Y, Atkinson C, Dyall D, et al. Using participatory action research to co-design perinatal support strategies for Aboriginal and Torres Strait Islander parents experiencing complex trauma. Women and Birth 2021 Dec 24 [Epub ahead of print]. [DOI: 10.1016/j.wombi.2021.12.005] [PMID: ] [DOI] [PubMed]
Reuveni 2021
- Reuveni I, Lauria M, Monk C, Werner E. The impact of childhood trauma on psychological interventions for depression during pregnancy and postpartum: a systematic review. Archives of Women's Mental Health 2021;24(3):367-80. [DOI: 10.1007/s00737-020-01066-4] [PMCID: PMC8176623] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
RevMan Web 2020 [Computer program]
- Review Manager Web (RevMan Web). Version 1.22.0. The Cochrane Collaboration, 2020. Available at revman.cochrane.org.
RoB 2 tool 2020
- RoB 2 tool. A revised Cochrane risk of bias tool for randomized trials. www.riskofbias.info/welcome/rob-2-0-tool (accessed 20 March 2020).
Rosenblum 2017
- Rosenblum KL, Muzik M, Morelen DM, Alfafara EA, Miller NM, Waddell RM, et al. A community-based randomized controlled trial of Mom Power parenting intervention for mothers with interpersonal trauma histories and their young children. Archives of Women's Mental Health 2017;20(5):673-86. [DOI: 10.1007/s00737-017-0734-9] [PMCID: PMC5709180] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rosenblum 2018
- Rosenblum K, Lawler J, Alfafara E, Miller N, Schuster M, Muzik M. Improving maternal representations in high-risk mothers: a randomized, controlled trial of the Mom Power parenting intervention. Child Psychiatry & Human Development 2018;49(3):372-84. [DOI: 10.1007/s10578-017-0757-5] [PMCID: PMC5862741] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Rouhe 2015
- Rouhe H, Salmela-Aro K, Toivanen R, Tokola M, Halmesmäki E, Ryding E-L, et al. Group psychoeducation with relaxation for severe fear of childbirth improves maternal adjustment and childbirth experience – a randomised controlled trial. Journal of Psychosomatic Obstetrics & Gynaecology 2015;36(1):1-9. [DOI: 10.3109/0167482X.2014.980722] [PMID: ] [DOI] [PubMed] [Google Scholar]
Sahle 2021
- Sahle BW, Reavley NJ, Li W, Morgan AJ, Yap MB, Reupert A, et al. The association between adverse childhood experiences and common mental disorders and suicidality: an umbrella review of systematic reviews and meta-analyses. European Child & Adolescent Psychiatry 2021 Feb 27 [Epub ahead of print]. [DOI: 10.1007/s00787-021-01745-2] [PMID: ] [DOI] [PubMed]
SAMHSA 2014
- Substance Abuse and Mental Health Services Administration (SAMHSA). SAMHSA's concept of trauma and guidance for a trauma-informed approach, July 2014. store.samhsa.gov/system/files/sma14-4884.pdf (accessed 13 September 2019).
Santesso 2020
- Santesso N, Glenton C, Dahm P, Garner P, Akl EA, Alper B, et al. GRADE guidelines 26: informative statements to communicate the findings of systematic reviews of interventions. Journal of Clinical Epidemiology 2020;119:126-35. [DOI] [PubMed] [Google Scholar]
Savage 2019
- Savage L-É, Tarabulsy GM, Pearson J, Collin-Vézina D, Gagné L-M. Maternal history of childhood maltreatment and later parenting behaviour: a meta-analysis. Development and Psychopathology 2019;31(1):9-21. [DOI: 10.1017/S0954579418001542] [PMID: ] [DOI] [PubMed] [Google Scholar]
Schandelmaier 2020
- Schandelmaier S, Briel M, Varadhan R, Schmid CH, Devasenapathy N, Hayward RA, et al. Development of the Instrument to assess the Credibility of Effect Modification Analyses (ICEMAN) in randomized controlled trials and meta-analyses. Canadian Medical Association Journal 2020;192(32):E901-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schofield 2013
- Schofield TJ, Lee RD, Merrick MT. Safe, stable, nurturing relationships as a moderator of intergenerational continuity of child maltreatment: a meta-analysis. Journal of Adolescent Health 2013;53(4 Suppl):S32-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schünemann 2019a
- Schünemann HJ, Higgins JP, Vist GE, Glasziou P, Akl E, Skoetz N, et al. Chapter 14: Completing 'Summary of findings' tables and grading the certainty of the evidence. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editors(s). Cochrane Handbook for Systematic Reviews of Interventions. 2nd edition. Chichester (UK): John Wiley & Sons, 2019:375-402. [Google Scholar]
Schünemann 2019b
- Schünemann HJ, Vist GE, Higgins JP, Santesso N, Deeks JJ, Glasziou P, et al. Chapter 15: Interpreting results and drawing conclusions. In: Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al, editors(s). Cochrane Handbook for Systematic Reviews of Interventions. 2nd edition. Chichester (UK): John Wiley & Sons, 2019:403-32. [Google Scholar]
Schünemann 2022
- Schünemann HJ, Vist GE, Higgins JPT, Santesso N, Deeks JJ, Glasziou P, et al. Chapter 15: Interpreting results and drawing conclusions. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022). Cochrane, 2022. Available from www.training.cochrane.org/handbook.
Scorza 2020
- Scorza P, Monk C, Lee S, Feng T, Berry OO, Werner E. Preventing maternal mental health disorders in the context of poverty: pilot efficacy of a dyadic intervention. American Journal of Obstetrics & Gynecology MFM 2020;2(4):100230. [DOI: 10.1016/j.ajogmf.2020.100230] [PMCID: PMC7893538] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Seng 2013
- Seng JS, Sperlich M, Low LK, Ronis DL, Muzik M, Liberzon I. Childhood abuse history, posttraumatic stress disorder, postpartum mental health, and bonding: a prospective cohort study. Journal of Midwifery & Women's Health 2013;58(1):57-68. [DOI: 10.1111/j.1542.2011.2012.00237.x] [PMCID: PMC3564506] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sethi 2013
- Sethi D, Bellis M, Hughes K, Gilbert R, Mitis F, Galea G. European report on preventing child maltreatment; 2013. www.euro.who.int/__data/assets/pdf_file/0019/217018/European-Report-on-Preventing-Child-Maltreatment.pdf?ua=1 (accessed 19 November 2019).
Shevlin 2018
- Shevlin M, Hyland P, Roberts NP, Bisson JI, Brewin CR, Cloitre M. A psychometric assessment of disturbances in self-organization symptom indicators for ICD-11 complex PTSD using the International Trauma Questionnaire. European Journal of Psychotraumatology 2018;9(1):1419749. [DOI: 10.1080/20008198.2017.1419749] [PMCID: PMC5774393] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sidik 2002
- Sidik K, Jonkman JN. A simple confidence interval for meta-analysis. Statistics in Medicine 2002;21(21):3153-9. [DOI: 10.1002/sim.1262] [PMID: ] [DOI] [PubMed] [Google Scholar]
Sirey 2005
- Sirey JA, Meyers BS, Teresi JA, Bruce ML, Ramirez M, Raue PJ, et al. The Cornell Service Index as a measure of health service use. Psychiatric Services 2005;56(12):1564-9. [DOI: 10.1176/appi.ps.56.12.1564] [PMID: ] [DOI] [PubMed] [Google Scholar]
Slee 2019
- Slee A, Nazareth I, Bondaronek P, Liu Y, Cheng Z, Freemantle N. Pharmacological treatments for generalised anxiety disorder: a systematic review and network meta-analysis. Lancet 2019;393(10173):768-77. [DOI: 10.1016/s0140-6736(18)31793-8] [PMID: ] [DOI] [PubMed] [Google Scholar]
Smith 2000
- Smith DW, Letourneau EJ, Saunders BE, Kilpatrick DG, Resnick HS, Best CL. Delay in disclosure of childhood rape: results from a national survey. Child Abuse & Neglect 2000;24(2):273-87. [DOI: 10.1016/s0145-2134(99)00130-1] [PMID: ] [DOI] [PubMed] [Google Scholar]
SmithBattle 2017
- SmithBattle L, Chantamit-O-Pas C, Freed P, McLaughlin D, Schneider JK. Moms growing together: piloting action methods and expressive arts in a therapeutic group for teen mothers. Journal of Child and Adolescent Psychiatric Nursing 2017;30(2):72-9. [DOI: 10.1111/jcap.12172] [PMID: ] [DOI] [PubMed] [Google Scholar]
Somer 2001
- Somer E, Szwarcberg S. Variables in delayed disclosure of childhood sexual abuse. American Journal of Orthopsychiatry 2001;71(3):332-41. [DOI: 10.1037/0002-9432.71.3.332] [PMID: ] [DOI] [PubMed] [Google Scholar]
Sperlich 2017
- Sperlich M, Seng JS, Li Y, Taylor J, Bradbury-Jones C. Integrating trauma-informed care into maternity care practice: conceptual and practical issues. Journal of Midwifery & Women's Health 2017;62(6):661-72. [DOI: 10.1111/jmwh.12674] [PMID: ] [DOI] [PubMed] [Google Scholar]
Steele 2019
- Steele H, Murphy A, Bonuck K, Meissner P, Steele M. Randomized control trial report on the effectiveness of Group Attachment-Based Intervention (GABI©): improvements in the parent–child relationship not seen in the control group. Development and Psychopathology 2019;31(1):203-17. [DOI: 10.1017/S0954579418001621] [PMID: ] [DOI] [PubMed] [Google Scholar]
Sterne 2019
- Sterne JA, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019;366:14898. [DOI: 10.1136/bmj.l4898] [PMID: ] [DOI] [PubMed] [Google Scholar]
Stevens 2020
- Stevens NR, Miller ML, Soibatian C, Otwell C, Rufa AK, Meyer DJ, et al. Exposure therapy for PTSD during pregnancy: a feasibility, acceptability, and case series study of Narrative Exposure Therapy (NET). BMC Psychology 2020;8(1):130. [DOI: 10.1186/s40359-020-00503-4] [PMCID: PMC7727253] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Stevens 2021
- Stevens NR, Miller ML, Puetz A-K, Padin AC, Adams N, Meyer DJ. Psychological intervention and treatment for posttraumatic stress disorder during pregnancy: a systematic review and call to action. Journal of Traumatic Stress 2021;34(3):575-85. [DOI: 10.1002/jts.22641] [PMID: ] [DOI] [PubMed] [Google Scholar]
Stoltenborgh 2015
- Stoltenborgh M, Bakermans-Kranenburg MJ, Alink LR, Van Ijzendoorn MH. The prevalence of child maltreatment across the globe: review of a series of meta‐analyses. Child Abuse Review 2015;24(1):37-50. [DOI: 10.1002/car.2353] [DOI] [Google Scholar]
Stronach 2013
- Stronach EP, Toth SL, Rogosch F, Cicchetti D. Preventive interventions and sustained attachment security in maltreated children. Development and Psychopathology 2013;25(4 Pt 1):919-30. [DOI: 10.1017/S0954579413000278] [PMCID: PMC3857699] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Sánchez‐Meca 2011
- Sánchez-Meca J, Rosa-Alcázar AI, López-Soler C. The psychological treatment of sexual abuse in children and adolescents: a meta-analysis. International Journal of Clinical and Health Psychology 2011;11(1):67-93. [WEB PAGE: www.um.es/metaanalysis/pdf/5034.pdf] [Google Scholar]
Thomas 2020
- Thomas J, McDonald S, Noel-Storr A, Shemilt I, Elliott J, Mavergames C, et al. Machine learning reduced workload with minimal risk of missing studies: development and evaluation of a randomized controlled trial classifier for Cochrane Reviews. Journal of Clinical Epidemiology 2020;133:140-51. [DOI: 10.1016/j.jclinepi.2020.11.003] [PMID: ] [DOI] [PMC free article] [PubMed]
Thompson 2002
- Thompson SG, Higgins JPT. How should meta‐regression analyses be undertaken and interpreted? Statistics in medicine 2002;21(11):1559-73. [DOI] [PubMed] [Google Scholar]
Trauma Informed Oregon 2016
- Trauma Informed Oregon. What is trauma informed care? 2016. traumainformedoregon.org/wp-content/uploads/2016/01/What-is-Trauma-Informed-Care.pdf (accessed 5 March 2021).
Upshur 2016
- Upshur CC, Wenz-Gross M, Weinreb L, Moffitt JJ. Using prenatal advocates to implement a psychosocial education intervention for posttraumatic stress disorder during pregnancy: feasibility, care engagement, and predelivery behavioral outcomes. Women's Health Issues 2016;26(5):537-45. [DOI: 10.1016/j.whi.2016.06.003] [PMID: ] [DOI] [PubMed] [Google Scholar]
Van der Kolk 2014
- Van der Kolk B. Learning to inhabit your body: yoga. In: Van Der Kolk B, editors(s). The Body Keeps the Score: Mind, Brain and Body in the Transformation of Trauma. London (UK): Penguin Books, 2014:265-78. [Google Scholar]
Varese 2012
- Varese F, Smeets F, Drukker M, Lieverse R, Lataster T, Viechtbauer W, et al. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophrenia Bulletin 2012;38(4):661-71. [DOI: 10.1093/schbul/sbs050] [PMCID: PMC3406538] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Waleed 2019
- Waleed M, Kazmi I, Farooq M, Hamid A, Fara K, Allgar V, et al. Clustering by health professionals in individually randomised controlled trials. European Medical Journal 2019;4(4):53-61. [WEB PAGE: tinyurl.com/56unxsdz] [Google Scholar]
Walton 2017
- Walton H, Spector A, Tombor I, Michie S. Measures of fidelity of delivery of, and engagement with, complex, face-to-face health behaviour change interventions: a systematic review of measure quality. British Journal of Health Psychology 2017;22:872-903. [DOI: 10.1111/bjhp.12260] [DOI] [PMC free article] [PubMed] [Google Scholar]
Werner 2016
- Werner EA, Gustafsson HC, Lee S, Feng T, Jiang N, Desai P, et al. PREPP: postpartum depression prevention through the mother–infant dyad. Archives of Women's Mental Health 2016;19(2):229-42. [DOI: 10.1007/s00737-015-0549-5] [PMCID: PMC4738166] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
Whittingham 2011
- Whittingham K, Wee D, Boyd R. Systematic review of the efficacy of parenting interventions for children with cerebral palsy. Child: Care, Health and Development 2011;37(4):475-83. [DOI: 10.1111/j.1365-2214.2011.01212.x] [PMID: ] [DOI] [PubMed] [Google Scholar]
WHO 2018a
- World Health Organization. Adverse Childhood Experiences International Questionnaire (ACE-IQ), 2018. www.who.int/publications/m/item/adverse-childhood-experiences-international-questionnaire-(ace-iq) (accessed 6 March 2021).
WHO 2018b
- World Health Organization. International Standards for Clinical Trial Registries – Version 3.0. World Health Organization 2018.
WHO 2019
- World Health Organization. ICD-11: International Classification of Diseases, 11th Revision. icd.who.int/ (accessed 6 March 2021).
WHO 2020
- World Health Organization. Fact sheet: child maltreatment; June 2020. www.who.int/en/news-room/fact-sheets/detail/child-maltreatment (accessed 17 November 2019).
Wittkowski 2017
- Wittkowski A, Garrett C, Calam R, Weisberg D. Self-report measures of parental self-efficacy: a systematic review of the current literature. Journal of Child and Family Studies 2017;26(11):2960-78. [DOI: 10.1007/s10826-017-0830-5] [PMCID: PMC5646137] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
WMA 2017
- World Medical Association. WMA Statement On Child Abuse and Neglect; October 2017. www.wma.net/policies-post/wma-statement-on-child-abuse-and-neglect/ (accessed 27 November 2019).
Yehuda 2008
- Yehuda R, Bell A, Bierer LM, Schmeidler J. Maternal, not paternal, PTSD is related to increased risk for PTSD in offspring of Holocaust survivors. Journal of Psychiatric Research 2008;42(13):1104-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yehuda 2018
- Yehuda R, Lehrner A. Intergenerational transmission of trauma effects: putative role of epigenetic mechanisms. World Psychiatry 2018;17(3):243-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zaccagnino 2013
- Zaccagnino M, Cussino M. EMDR and parenting: a clinical case. Journal of EMDR Practice and Research 2013;7(3):154-66. [DOI: 10.1891/1933-3196.7.3.154] [DOI] [Google Scholar]
Zajac 2019
- Zajac L, Raby KL, Dozier M. Attachment state of mind and childhood experiences of maltreatment as predictors of sensitive care from infancy through middle childhood: results from a longitudinal study of parents involved with child protective services. Development and Psychopathology 2019;31(1):113-25. [DOI: 10.1017/S0954579418001554] [PMID: ] [DOI] [PubMed] [Google Scholar]
Zlotnick 2011
- Zlotnick C, Capezza NM, Parker D. An interpersonally based intervention for low-income pregnant women with intimate partner violence: a pilot study. Archives of Women's Mental Health 2011;14(1):55-65. [DOI: 10.1007/s00737-010-0195-x] [PMCID: PMC3042850] [PMID: ] [DOI] [PMC free article] [PubMed] [Google Scholar]
References to other published versions of this review
Protocol
- Reid C, McKenzie JE, Brennan SE, Bennetts SK, Clark Y, Mensah F, et al. Interventions during pregnancy or up to two years after birth for parents who are experiencing complex trauma or have experienced maltreatment in their childhood (or both) to improve parenting capacity or socio-emotional well-being. Cochrane Database of Systematic Reviews 2021, Issue 7. Art. No: CD014874. [DOI: 10.1002/14651858.CD014874] [DOI] [Google Scholar]


