Introduction
To date, many cases of bullous pemphigoid (BP) under treatment with dipeptidyl peptidase-4 inhibitors (DPP-4i) have been reported; however, there are a few reports of pemphigoid nodularis induced by DPP-4i. We herein report a case which developed pruritic nodules one and a half years after starting DPP-4i, in which anti-BP180 NC16A antibody was negative while full-length BP180 ELISA was positive.
Case Report
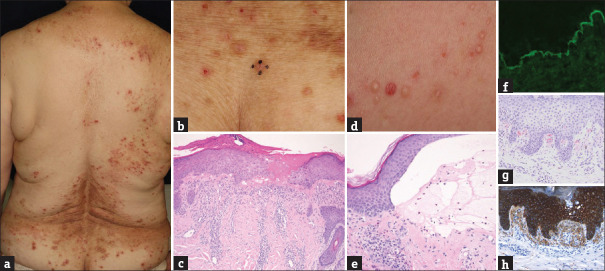
A 74-year-old woman was referred to our department, complaining of pruritic eruptions on the body that had appeared 3 years earlier. She had been treated with topical corticosteroid ointment and oral antihistamines in another hospital but had no improvement. She had type 2 diabetes and had been taking DPP-4i for four and a half years. Physical examination showed a number of erythematous papules with erosions and nodules on the trunk and extremities [Figure 1a and b]. Histopathological examination showed dermal fibrosis with lymphocyte and eosinophil infiltration [Figure 1c]. Laboratory tests showed an increase in the number of eosinophils (13%), as well as an increase in serum creatinine (0.98 mg/dl), and blood urea nitrogen (23 mg/dl). The serum titer of the anti-BP180 NC16A IgG antibody and the anti-BP230 antibody was 6.3 U/ml (cut-off, <9) and <5 U/ml, respectively. Under the diagnosis of prurigo nodularis, narrow band-ultraviolet B (NB-UVB) irradiation was started for nodular lesions. After irradiation was performed 12 times in total, tense blisters appeared on both thighs [Figure 1d]. Histopathology showed subepidermal blisters with lymphocyte and eosinophil infiltration [Figure 1e]. Direct immunofluorescence showed linear deposition of IgG and C3 in the basement membrane zone [Figure 1f]. As cryopreservation of the initial biopsy was not available, we performed indirect immunofluorescence with the serum obtained when the patient first visited us and when blisters appeared after irradiation therapy. Both results showed linear deposition of IgG in the basement membrane zone. DPP-4i was discontinued and oral prednisolone (40 mg/day) was administered, which results in an improvement in blisters and nodules. Retrospectively, the full-length BP180 ELISA was measured using serum at the initial visit, which showed 61.36 U/ml (cut-off: <4.64 U/ml). Both nodular and bullous lesions were successfully treated with oral prednisolone. Approximately, one year later, pruritic papules appeared on the back. Histopathology using Dylon staining showed amyloid deposition, as well as positive AE1/AE3, in the dermal papilla [Figure 1g and h].
Figure 1.
(a) Erythematous papules with erosions and some nodules on the trunk and extremities. (b) Some nodules on the hips. (c) Histological examination showed infiltration of lymphocytes and eosinophils in the upper dermis (haematoxylin and eosin stain, original magnification x100). (d) Tense blisters appeared on both thighs. (e) Histopathology showed subepidermal blisters and infiltration of lymphocytes and eosinophils in the upper dermis and in the blisters (haematoxylin and eosin stain, original magnification x200). (f) Direct immunofluorescence showed linear deposition of IgG at the basement membrane zone. (g) Histopathology using Dylon staining showed amyloid deposition in the dermal papilla
Discussion
The characteristics of the present case are i) the patient had been diagnosed as having refractory nodular prurigo and treated as refractory nodular prurigo, for which had been treated for at least 3 years; ii) bullous lesions appeared following NB-UVB irradiation for nodule lesions; iii) DPP-4i had been administered for diabetes for four and half years prior to the appearance of blisters and iv) anti-BP180 NC16A antibody was negative while full-length BP180 ELISA was positive. We diagnosed the patient as having BP with nodular lesions (pemphigoid nodularis). To date, only a few cases of nodular pemphigoid with administration of DPP-4i have been reported. The period of taking DPP-4i until the diagnosis of nodular pemphigoid was between half a year and 2 years. In the present case, nodular lesions appeared one and a half years after starting DPP-4i, which persisted without bullous lesions for 3 years but developed blisters following phototherapy.
According to a previous analysis of 181 cases of nonbullous lesions appearing as initial symptoms of BP, erythema was the most common (31.8%), followed by nodules or papules (13.8%).[1] The precipitating factors of BP include UV radiation, thermal burn, surgical wounds, surgical grafts, ostomy, and several traumatic triggers.[2,3] Some cases of pemphigoid nodularis after phototherapy were reported,[4] two of whom were taking DPP-4i. Both of them were negative for anti-BP180 NC16A antibody but positive for full-length BP180 antibody.[5] A recent study detected autoantibodies against the midportion of BP180 without detection of anti-BP180 NC16A autoantibodies in 14 of 121 BP patients, among whom 7 (50%) were taking DPP-4i for diabetes.[6] Patients who are positive for full-length BP180 ELISA show noninflammatory clinical features.[6] To our knowledge, there are only a few cases of pemphigoid nodularis under taking DPP-4i showing full-length BP-180.[5,7] Therefore, the associations between autoantibodies targeting only full-length BP180 ELISA with pemphigoid nodularis remain still unknown.
Finally, the present case developed itchy papules with amyloid deposition after the improvement of pemphigoid nodularis. Some reports have suggested that lichen amyloidosis is caused by chronic friction due to scratching. Amyloid deposition was in parallel with keratin staining in the present case, suggesting that amyloid fibril was derived from degenerated keratinocytes due to damage in pemphigoid nodularis. However, similar cases to our case have not been reported, and thus further studies are necessary.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
We reported a rare case of nodular pemphigoid. There are few cases of patients with nodular pemphigoid taking DPP-4i; thus, further study is necessary to investigate the associations between autoantibodies targeting only full-length BP180 ELISA with nodular lesions.
References
- 1.Yung CW, Soltani K, Lorincz AL. Pemphigoid nodularis. J Am Acad Dermatol. 1981;5:54–60. doi: 10.1016/s0190-9622(81)70077-x. [DOI] [PubMed] [Google Scholar]
- 2.Zhang Y, Luo Y, Han Y, Tian R, Li W, Yao X. Non-bullous lesions as the first manifestation of bullous pemphigoid: A retrospective analysis of 181 cases. J Dermatol. 2017;44:742–6. doi: 10.1111/1346-8138.13782. [DOI] [PubMed] [Google Scholar]
- 3.Asbrink E, Hovmark A. Clinical variations in bullous pemphigoid with respect to early symptoms. Acta Derma Venereol. 1981;61:417–21. [PubMed] [Google Scholar]
- 4.Amber KT, Korta DZ, Feraudy S, Grando SA. Vesiculobullous eruption in a patient receiving psoralen ultraviolet A (PUVA) treatment for prurigo nodules: A case of PUVA-aggravated pemphigoid nodularis. Clin Exp Dermatol. 2017;42:833–5. doi: 10.1111/ced.13172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Izumi K, Nishie W, Mai Y, Wada M, Natsuga K, Ujiie H, et al. Autoantibody profile differentiates between inflammatory and noninflammatory bullous pemphigoid. J Invest Dermatol. 2016;136:2201–2210. doi: 10.1016/j.jid.2016.06.622. [DOI] [PubMed] [Google Scholar]
- 6.Tani S, Tsujioka H. Bullous pemphigoid developing during narrowband UVB therapy for prurigo nodularis. Practical Dermatol. 2016;38:883–886. in Japanese. [Google Scholar]
- 7.Okuhira A, Matsuoka M, Matsuura T, Kadono T, Kawakami T, Soma Y, et al. Nodular Pemphigoid Caused by Dipeptidyl Peptidase-4 Inhibitor. Rinsho Derma. 2018;60:607–10. in Japanese. [Google Scholar]