Abstract
Neuroendocrine carcinoma (NEC) of the larynx is the most frequent neuroendocrine neoplasm of the head and neck and the most common nonsquamous carcinoma of the larynx. It usually occurs in the supraglottic area, in smoking men. We report a case of a 58-year-old woman with no history of smoking who presented with an atypical carcinoid, arising in the right piriform sinus of the larynx. During the 5-year follow-up, the patient developed metastases in the lymph nodes, palatine tonsils, parotid glands, breasts and skin. For this reason the patient underwent several surgical procedures, radiotherapy and eventually was qualified for chemotherapy. Our case shows that NEC of the larynx can have an atypical presentation. The diagnosis requires careful pathological evaluation with immunohistochemistry and a wide spectrum of imaging. The serum concentration of chromogranin A seems to be not useful in the diagnosis and follow-up of laryngeal NEC.
Keywords: neuroendocrine neoplasm, neuro-endocrine cancer, atypical carcinoid, metastases, case report, laryngeal tumor
INTRODUCTION
Neuroendocrine neoplasm (NEN) is a rare type of tumor, with increasing incidence in the recent years. Most of the NENs are localised in the gastrointestinal tract and lungs (1). NENs of the head and neck represent a spectrum of well-differentiated (typical carcinoid − TC), moderately differentiated (atypical carcinoid − AC) and poorly differentiated small cell or large cell neuroendocrine carcinoma (NEC) (2). The larynx accounts for less than 1% of NEN localisations, but it is the most common site of head and neck NEN (3). Data from single high-referral centers show that NEC of the larynx constitutes less than 1 percent of all laryngeal neoplasms, but still, it is the most common nonsquamos carcinoma of this organ (4-6).
The AC is the most common type of laryngeal NEN and it usually presents as a tumor in a supraglottic area with a high metastatic rate and predisposition to painful skin and subcutaneous metastases (3). Additionally, a high rate of recurrences and limited disease specific survival was described (7). Patients, typically heavy smoking men in the sixth or seventh decade of life, complain of dysphagia or sore throat. (3,6). Histological differentiation is crucial since it determines the survival and management of the disease. The best treatment option for an atypical carcinoid is surgical resection, with no clear benefit from radiation (8).
Cases of women with AC of the larynx were described in the past. Wang et al. showed a case of the patient with typical subcutaneous and skin metastases that did not react to the used treatment (9). On the other hand Giordiano et al. did not observe any metastatic spread or recurrence of AC in their patient (10).
This report is of a 58-year-old woman with no history of smoking, who presented with an AC, arising in the right piriform sinus of the larynx, who had widespread metastases at 5-year follow-up.
CASE REPORT
The 58-year-old female, without any comorbidities and negative smoking history, was referred to our tertiary referral center in October 2014 after a neck procedure. Because of dysphagia, she had been diagnosed at another hospital, where a diagnosis of laryngeal tumor of the right piriform sinus was established. She was operated for the first time (I) in April 2014. The histopathological examination revealed an AC with a Ki67 index of 14% and positive reaction for Thyroid Transcription Factor-1 (TTF1) which suggested metastatic character of the lesion. Because of pathological uptake in tonsils observed in 18-fluoro-deoxy-glucose positive emission tomography/computed tomography (18FDG-PET/CT), she had a bilateral tonsils excision performed (II). Both single-photon emission computed tomography with 99-Tectrotide and magnetic resonance (MRI) of head and neck performed postoperatively did not reveal any signs of the neoplasm.
At the first visit in our center, neck ultrasonography (USG) did not reveal any abnormal findings and chromogranin A (CgA) level remained within normal ranges. Because of suspicion of medullary thyroid cancer, histopathological samples were once again analyzed. Pathologist experienced in NEN diagnosis consulted histopathological samples from the first procedure and diagnosed AC of the larynx, with Ki67 index of 15%. Then the patient underwent several biopsies from the tumor bed which revealed infiltration of the cells from poorly-differentiated NEC. Despite lack of pathological uptake on Galium 68 DOTATATE PET/CT (68Ga-PET/CT), 18FDG-PET/CT was suggestive of recurrence in the soft tissue on the right side of the larynx/trachea border. In May 2015 patient underwent laryngoscopy with a biopsy taken from the vocal fold. Histopathological examination revealed infiltration of AC (Ki67 15%). CT showed progression of the lesion located in the right vocal fold what suggested recurrence of the neoplasm. In June 2015, for the first time, the patient was presented on multidisciplinary consultation at our center. Because of the monofocal character of disease and histological diagnosis, the patient was referred to another surgery. In June 2015 patient underwent partial laryngectomy with the larynx reconstruction (III). Because of perineural infiltration and non-radical character of the procedure, in July 2015 total laryngectomy (IV) was performed. Histological examination confirmed AC with lymph nodes metastases. Postoperative examinations (including 18FDG-PET/CT MR of head and neck, 68Ga-PET/CT) did not present signs of recurrence.
Eventually, MR of the head and neck from February 2018 raised a suspicion of multifocal recurrence in tumor bed and metastases to the right neck lymph nodes, what was confirmed by 68Ga-PET (low expression of somatostatin receptors). For this reason patient underwent another operation (V) in April 2018 – the bilateral excision of neck lymph nodes. The pathologist diagnosed AC metastases with infiltration of the neck muscles and subcutaneous tissue. Postoperative 68Ga-PET/CT showed pathological uptake in the neck and right breast. This finding led to excision of the submandibular tumor and left submandibular gland (VI), where only the submandibular tumor was infiltrated by NEN cells in histopathology. Mammography (MMG) showed a tumor of the right breast with a diameter a of 12 millimeters, Breast Imaging Reporting and Database System score (BIRADS) of 5. Second multidisciplinary consultation at our center proposed a biopsy of the breast tumor, CT of the neck, chest, abdomen and pelvis. Histological examination of the specimen from breast biopsy raised a suspicion of NEN metastases. Moreover, a biopsy of the left parotid gland suggested AC metastases. Therefore, the patient underwent an excision of a tumor of the left parotid gland and subcutaneous tumor in the area of tracheostomy (VII). Pathological examination confirmed the AC metastases (Ki67% 15%) with margins positive for neoplastic cells, indicating non-radical procedure. Postoperative physical examination revealed for the first time disseminated painful nodules in the area of the right scapula, subclavian area and occiput. These nodules did not show pathological uptake in 68Ga-PET. Third multidisciplinary consultation advised to surgically remove breast tumor and one of the skin lesions. In January 2019 tumor of the right breast and small nodules mentioned above were excised (VIII). Histopathological examination confirmed metastases of AC with Ki67 of 15%, with positive reaction for synaptophysin, CgA, but negative reactions for estrogen and progesteron receptors and GATA3. Postoperative biopsy of a nodule located in the neck revealed infiltration of NEN cells. For this reason fourth multidisciplinary consultation advised radiotherapy of the neck and subclavian area. Before the radiotherapy patient underwent excision of subcutaneous nodules located in the neck, subclavian and submandibular area (IX). Histopathological examination revealed a poorly differentiated large cell NEC with Ki67 of 20%. Additionally, the patient had a germline DNA examination performed, but no mutation in the CHEK2 gene was observed. In October 2019 the patient was irradiated with the fractional doses of 3 Gy to a maximal dosage of 30 Gy. Subsequent MMG suggested the presence of a tumor of the right and left breast with diameter of 32 and 9 millimeters, respectively, BIRADS 5. For this reason the patient was referred to excision of the right breast tumor, which was performed in February 2020 (X). The histopathological examination revealed NEC metastases with focal Ki67 of 30%. During the follow-up US image suggested metastases in the subcutaneous tissue and neck nodes, what led the patient to another surgery (XI) – the excision of the neck lymph nodes in March 2020. The histopathological examination from operating center suggested medullary thyroid carcinoma (MTC) metastases, but consultation of the experienced pathologist confirmed metastases of NEC with Ki67 of 30%. Postoperative CT was suggestive of neck lymph nodes and left parotid gland metastases what was confirmed with the biopsy. Therefore, by the decision of multidisciplinary consultation, the patient was referred to chemotherapy with capecitabine and temozolomide. During the whole period of observation, the serum CgA levels remained stable. At the moment of manuscript submission, the patient started her chemotherapy.
Histopathological diagnosis
The first histopathological diagnosis was based on WHO Classification of Head and Neck Tumours, 2005. The biopsy revealed a tumor growing in nests, cords and sheets. It was composed of a round and oval cells with medium size and vesicular nuclei, with little “crush artefact”. There was a moderate cellular pleomorphism. The mitotic count was 3 mitoses per 10 high power fields. Moderate nuclear atypia and prominent nucleoli were seen, but no necrosis was observed. The tumour had an infiltrative pattern of growth, with perineural invasion and vascular invasion.
Immunohistochemistry revealed a positive reactions for: Chromogranin, Synaptophysin, Cytokeratin AE1/AE3 (CK AE1/AE3), Cytokeratin 7 (CK 7). Reactions for thyroglobulin (Tg), TTF1, HMB-45, Melan-A, S-100 Protein, and CK 5/6 remained negative. Moreover, examination suggested that the procedure was not radical.
During the disease course, we observed dedifferentiation of the tumor with increasing Ki67 (up to 30%) what was the base for the diagnosis of NEC of the larynx. In the differential diagnosis we considered metastases from other organs and MTC, but negative reactions for calcitonin, TTF-1, Melan-A and clinical data (no primary tumor in other organs in imaging) allowed us to confirm the diagnosis of AC, and later NEC.
Figure 1 represents the flowchart of the performed procedures. Figures 2-7 represent pathological images of laryngeal tumor from the first and third procedure.
Figure 1.
The flowchart of the performed procedures. Abbreviations: CAPTEM – Capecitabine + Temozolomide (chemotherapy protocol). HP – histopathology; IHC – Immunohistochemistry; CK – Cytokeratin; TG – Thyroglobulin; TTF-1 – Thyroid Transcription Factor 1; NEN – Neuroendocrine Neoplasia; ER – Estrogen receptor; PR – progesterone receptor.
Figure 2.

Photomicrograph of the histology of the laryngeal tumor. Note the mitotic figures, cytological atypia and nucleoli. Haematoxylin-eosin stain. Magnification 40x.
Figure 7.
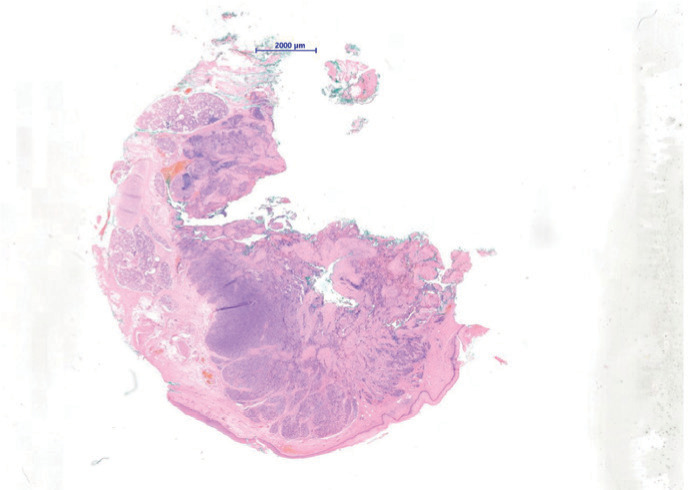
Photomicrograph of the histology of the laryngeal tumor in small magnification. Magnification 40x.
Figure 3.

Photomicrograph of the immunohistochemistry of the laryngeal biopsy. The histology shows brown neoplastic cells with positive reaction for synaptophisin. Immunohistochemistry for Synaptophysin Magnification 20x.
Figure 4.

Photomicrograph of the immunohistochemistry of the laryngeal biopsy. The histology shows brown neoplastic cells with positive reaction for chromogranin A. Immunohistochemistry for Chromogranin. Magnification 20x.
Figure 5.

Photomicrograph of the histology of the laryngeal tumor. The histology shows angioinvasion. Haematoxylin-eosin stain. Magnification 20x.
Figure 6.

Photomicrograph of the histology of the laryngeal tumor. The histology shows perineural invasion. Haematoxylin-eosin stain. Magnification 40x.
DISCUSSION
The presented case report has shown that AC of the larynx can present unusually, in non-smoking woman, with a significant metastatic spread and multiple recurrences. Moreover, it emphasizes the importance of thorough pathological examination performed by experienced pathologist and the use of a wide spectrum of imaging techniques to assess the patient. Additionally, the importance of individualized therapeutic management and poor performance of standard NEN markers were pointed out.
NENs, with their rising incidence, are becoming a growing problem in the oncology. Latest published data from the SEER database suggests that NENs incidence raised from 1.09 per 100 000 in 1973 to 6.98 per 100,000 in 2012(11). Therefore, one should always consider NENs in differential diagnosis, especially in slowly growing disseminated tumors. As shown in our case report, it requires a pathologist experienced in the field of NENs with the available wide spectrum of immunohistochemistry markers. It is especially important considering significant changes regarding terminology of these tumors (2).
As for the markers, our paper emphasizes the poor performance of CgA blood levels as a marker of NENs. During the whole period of observation CgA levels remained stable (below or slightly above the cutoff), despite the progression of the disease, what made it useless in the determination of recurrence and decision-making process. It is consistent with other papers describing its poor performance in NENs of the other primary site (12,13). Unfortunately, we have only scarce data about its performance in laryngeal NEN(14). Nevertheless, because of low availability of better methods and present recommendations from Neuroendocrine Societies we still base on CgA levels in NENs (15).
In our case, MTC was suspected at the beginning to be the primary site of the neoplasm. There are a few described cases of laryngeal NEN with positive calcitonin staining, but it is rarely related to elevated serum calcitonin levels (14). Our patient not only had a negative staining for the calcitonin, but also did not present lesions in the thyroid, which could be a primary site of the neoplasm. Nevertheless, MTC should always be taken into differential diagnosis in such cases.
Presented patient was a 58-year-old, non-smoking female what did not match the most frequent phenotype of patient with AC of the larynx, described previously (3,7). Previously described cases of woman with AC of the larynx differ in comparison to our experiences. Wang et al. presented a patient with an AC of similar Ki67 index and painful, disseminated subcutaneous and skin metastases. In this case chemotherapy was introduced significantly earlier, but 3 lines of that treatment were not effective in treatment of skin metastases. Only after intrathecal administration of ropivacaine the pain was relieved (9). On the other hand Giordiano et al. showed a case of woman with AC and no metastases or recurrence after surgery. It is probably related to a very short time of the follow-up (10). Also a case report of successful usage of novel therapeutic methods in female patient with AC of the larynx was described, but again a short time of the follow-up limits the value of the conclusions (16).
Our patient survived more than 68 months from the diagnosis. Unfortunately, it is difficult to relate it to described mortality data of AC, since some of the tumors included in the analysis would be reclassified according to newest classification, what could influence the outcomes (6).
Skin metastases were reported as a typical feature of this type of laryngeal NEC and were seen even in the first described case of laryngeal NEC (3,17). These metastases are of big importance since they are painful, grow rapidly and are resistant to treatment, so that they became the main complaint of our patient (9).
Treatment of laryngeal NEC depends on the stage and histological type. AC of the larynx should be referred for surgical excision as it was done for eleven times in our case (8). For the long time disease was controlled with surgical excisions of tumors. It is difficult to say whether the earlier decision about chemotherapy would be beneficial for this patient. As described in the literature, radiotherapy was also not successful in our experience (8). Our case report demonstrates that in terms of AC treatment, an individual management of the patient should be preferred.
In conclusion, this case report has shown that AC of the larynx can have an atypical presentation. The diagnosis requires careful pathological evaluation with immunohistochemistry to exclude the main differential diagnoses of medullary thyroid carcinoma, and paraganglioma. A wide spectrum of imaging is needed to exclude metastases or local invasion. Serum concentration of Chromogranin A seems not to be useful in the diagnosis and follow-up.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- 1.Hofland J, Kaltsas G, de Herder WW. Advances in the Diagnosis and Management of Well-Differentiated Neuroendocrine Neoplasms. Endocr Rev. 2020;41(2):371–403. doi: 10.1210/endrev/bnz004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rindi G, Klimstra DS, Abedi-Ardekani B, Asa SL, Bosman FT, Brambilla E, Busam KJ, de Krijger RR, Dietel M, El-Naggar AK, Fernandez-Cuesta L, Klöppel G, McCluggage WG, Moch H, Ohgaki H, Rakha EA, Reed NS, Rous BA, Sasano H, Scarpa A, Scoazec JY, Travis WD, Tallini G, Trouillas J, van Krieken JH, Cree IA. A common classification framework for neuroendocrine neoplasms: an International Agency for Research on Cancer (IARC) and World Health Organization (WHO) expert consensus proposal. Mod Pathol. 2018;31(12):1770–1786. doi: 10.1038/s41379-018-0110-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.López F, Hunt JL, Nixon IJ, Rinaldo A, Williams MD, Cardesa A, Ferlito A. How phenotype guides management of the neuroendocrine carcinomas of the larynx. J Laryngol Otol. 2018;132(7):568–574. doi: 10.1017/S0022215118000968. [DOI] [PubMed] [Google Scholar]
- 4.Stoyanov GS, Kitanova M, Dzhenkov DL, Ghenev P, Sapundzhiev N. Demographics of Head and Neck Cancer Patients: A Single Institution Experience. Cureus. 2017;2;9(7):e1418. doi: 10.7759/cureus.1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nallathambi C, Yumkhaibam SD, Singh LJ, Singh TT, Singh IY, Daniel N. Clinico-Epidemiologic Patterns of Laryngeal Cancer: 5-year Results from a Regional Cancer Centre in Northeastern India. Asian Pac J Cancer Prev. 016;17(5):2439–2443. [PubMed] [Google Scholar]
- 6.Ordonez-Perez B. Neuroendocrine Carcinomas of the Larynx and Head and Neck: Challenges in Classification and Grading. Head and Neck Pathology. 2018;12:1–8. doi: 10.1007/s12105-018-0894-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gillenwater A, Lewin J, Roberts D, El-Naggar A. Moderately Differentiated Neuroendocrine Carcinoma (Atypical Carcinoid) of the Larynx: A Clinically Aggressive Tumor. Laryngoscope. 2005;115(7):1191–1195. doi: 10.1097/01.MLG.0000166179.40750.1B. [DOI] [PubMed] [Google Scholar]
- 8.van der Laan TP, Plaat BE, van der Laan BF, Halmos GB. Clinical recommendations on the treatment of neuroendocrine carcinoma of the larynx: A meta-analysis of 436 reported cases. Head Neck. 2015;37(5):707–715. doi: 10.1002/hed.23666. [DOI] [PubMed] [Google Scholar]
- 9.Wang KR, Jia YJ, Zhou SH, Wang QY, Bao YY, Feng ZY, Yao HT, Fan J. Cutaneous and Subcutaneous Metastases From Atypical Laryngeal Carcinoids. Medicine (Baltimore) 2016;95(7):e2796. doi: 10.1097/MD.0000000000002796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Giordano G, Corcione L, Giordano D, D’Adda T, Gnetti L, Ferri T. Primary moderately differentiated neuroendocrine carcinoma (atypical carcinoid) of the larynx: A case report with immunohistochemical and molecular study. Auris Nasus Larynx. 2009;36(2):228–231. doi: 10.1016/j.anl.2008.05.002. [DOI] [PubMed] [Google Scholar]
- 11.Dasari A, Shen C, Halperin D, Zhao B, Zhou S, Xu Y, Shih T, Yao JC. Trends in the Incidence, Prevalence, and Survival Outcomes in Patients With Neuroendocrine Tumors in the United States. JAMA Oncol. 2017;3(10):1335–1342. doi: 10.1001/jamaoncol.2017.0589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dam G, Grønbæk H, Sorbye H, Thiis Evensen E, Paulsson B, Sundin A, Jensen C, Ebbesen D, Knigge U, Tiensuu Janson E. Prospective Study of Chromogranin A as a Predictor of Progression in Patients with Pancreatic, Small-Intestinal, and Unknown Primary Neuroendocrine Tumors. Neuroendocrinology. 2020;110(3-4):217–224. doi: 10.1159/000503833. [DOI] [PubMed] [Google Scholar]
- 13.Malczewska A, Kidd M, Matar S, Kos-Kudła B, Bodei L, Oberg K, Modlin IM. An Assessment of Circulating Chromogranin A as a Biomarker of Bronchopulmonary Neuroendocrine Neoplasia: A Systematic Review and Meta-Analysis. Neuroendocrinology. 2020;110(3-4):198–216. doi: 10.1159/000500525. [DOI] [PubMed] [Google Scholar]
- 14.Feola T, Puliani G, Sesti F, Modica R, Biffoni M, Di Gioia C, Carletti R, Anastasi E, Di Vito V, Centello R, Lenzi A, Isidori AM, Faggiano A, Giannetta E. Laryngeal Neuroendocrine Tumor With Elevated Serum Calcitonin: A Diagnostic and Therapeutic Challenge. Case Report and Review of Literature. Front Endocrinol (Lausanne) 2020;11:397. doi: 10.3389/fendo.2020.00397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kunz PL, Reidy-Lagunes D, Anthony LB, Bertino EM, Brendtro K, Chan JA, Chen H, Jensen RT, Kim MK, Klimstra DS, Kulke MH, Liu EH, Metz DC, Phan AT, Sippel RS, Strosberg JR, Yao JC, North American Neuroendocrine Tumor Society Consensus Guidelines for the Management and Treatment of Neuroendocrine Tumors. Pancreas. 2013;42(4):557–577. doi: 10.1097/MPA.0b013e31828e34a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Muderris T, Bercin S, Sevil E, Acar B, Kiris M. Transoral Robotic Surgery for Atypical Carcinoid Tumor of the Larynx. J Craniofac Surg. 2013;24:1996–1999. doi: 10.1097/SCS.0b013e3182a28c2c. [DOI] [PubMed] [Google Scholar]
- 17.Goldman NC, Hood CI, Singleton GT. Carcinoid of the larynx. Arch Otolaryngol. 1969;90(1):64–67. doi: 10.1001/archotol.1969.00770030066013. [DOI] [PubMed] [Google Scholar]



