Abstract
There is little knowledge about how the COVID-19 pandemic has impacted people who are socially marginalised, including individuals who face barriers when attempting to access services such as social safety nets, the labour market, or housing. There is even less understanding about women living under these circumstances. The aims of this study are therefore to examine the material and mental impacts of COVID-19 among socially marginalised women (compared with socially marginalised men) as well as influencing factors. The study is based on survey data (N = 304) involving people who are clients of social care organisations in thirteen European countries. The sample includes clients: a) living in their homes, b) in facilities, and c) on the street and in temporary accommodations. Results indicate that although material impacts were not significantly different for female and male respondents, socially marginalised women have experienced more severe mental impacts of the COVID-19 pandemic than socially marginalised men. Female respondents have been significantly more worried about COVID-19 infection than men, and they report significantly more PTSD-symptoms related to the pandemic. Quantitative results indicate that these differences are related to the fact that the female respondents worry more about health risks (e.g. falling ill). Female respondents also seem to be harder hit mentally by the material impacts of COVID-19. Among the free text survey answers regarding the biggest problem for the respondents after the outbreak of the pandemic, the most prevalent reply (among both men and women) was related to material impacts of the pandemic (39% of the respondents), particularly the loss of work (65%). While women reported deterioration of social relations more often, men mentioned lacking access to services more frequently.
Keywords: COVID-19, Mental health, Material outcomes, Women, Gender, Marginalisation
1. Introduction
Crises never impact populations within societies equally and often place a disproportionate burden on segments that are the most “socially excluded and economically insecure” [1]; p. 3). Within research on natural disasters, women appear prominently as such a segment of an affected population, with differentiated outcomes compared to men. These differentiated outcomes are a direct result of the gender dynamics which emanate from inequality and prescribed gender roles, which in turn influence levels of exposure and vulnerability that women face in a disaster as well as their ability to cope and recover in a post-disaster context [2]. For example, women are particularly susceptible to facing more severe economic impacts after a disaster due to overrepresentation in sectors often impacted the most by infrastructural disruptions and tend to have fewer assets than men or hold assets in a less tangible form than men, which decreases their resilience in the face of price spikes or damages to assets, for example (Ibid, 2021). In terms of health, women face lowered life expectancies as a result of a natural disaster, which increases with the severity of the disaster itself and their socioeconomic status (Neumayer & Plümper, 2007). Women also face differentiated mental health outcomes, with higher frequencies of post-traumatic stress and depression being found among females in Staten Island, New York, following Hurricane Sandy in 2012 (Gruebner et al., 2015) and higher frequencies of post-disaster psychological stress being associated with older age and lower levels of social support following an earthquake in 1989 in Australia (WHO, 2002).
After the emergence of the COVID-19 pandemic in 2019, the outcomes for and experiences of women have been particularly focused on, as the pandemic has revealed itself to be as much of a disaster as an earthquake or a flood. In this regard, higher levels of worry related to the pandemic have been noted [3,4] as well as increased susceptibility to experiencing unemployment and loss of income due to higher representation in sectors disrupted or shut down by regulations to prevent the spread of the virus [5,6]. Differentiated mental health outcomes, including greater psychological impacts (Ausín et al., 2021) and symptoms of anxiety, depression [7] and PTSD (Brivio et al., 2021) have also been emphasised. Correspondingly, male gender has been found to be a protective factor associated with mental health outcomes in a study conducted in China, Malaysia, Iran, Pakistan, Philippines, Thailand, and Vietnam [8], and a systematic review of mental health symptom changes before and during the COVID-19 pandemic noted that anxiety and general mental health worsened more for females than males [9].
This paper seeks to build on this body of knowledge by focusing on the outcomes of socially marginalised women and will seek to gain a better understanding of the factors which influenced these outcomes by employing an intersectional lens to vulnerability in disasters. Based on the aforementioned factors, this paper will pursue to discuss what can be done in order to reduce the material and mental health impacts of socially marginalised women during pandemics and in disasters in general.
2. Previous research
2.1. Taking an intersectional approach to vulnerability
The theory of intersectionality first emerged at the end of the 1980s in the United States through the work of Kimberlé Crenshaw with the aim of bringing the experiences of Black women to the forefront, as they had previously been excluded both in antidiscrimination law as well as feminist and antiracist theory and politics [10]. By establishing a means of examining how structures of power and inequality interacted with aspects such as race, ethnicity, gender, and class to produce differentiated effects, a theoretical framework was created which allows for researchers to examine and critique a myriad of different situations and contexts. As Carbado, Crenshaw, Mays, and Tomlinson note in their work (Ibid, p. 304) “paying attention to the movement of intersectionality helps to make clear that the theory is never done; it is always an analysis in-progress”.
It is for this reason that the theory of intersectionality can be applied to research on natural disasters and hazards to better understand their effects on certain populations. In other words, adopting such a perspective helps to avoid homogenising the impacts of disasters and the needs of those affected by them and instead allows for a deeper understanding of the ways that certain factors interact with each other to result in differentiated outcomes. For example, rather than viewing women as vulnerable upon the onset of the COVID-19 pandemic simply because they are women, researchers have taken a closer look at the ways that socioeconomic status [11,12], housing circumstances [13,14], ethnicity [15,16], and migration status [17] interact with gender to influence situational vulnerability and susceptibility to negative outcomes. According to Ref. [18]; an intersectional approach can help to move away from the paradigm of all-encompassing vulnerability based on demographic characteristics and can instead allow to move towards an understanding of vulnerability as being merely a “snapshot of a particular situation” that illuminates how multiple social differences are (re)produced in response to hazards and crises [18] (p.6).
The need for such a perspective was highlighted in the work of Orru et. al[19] who analysed how elements of intersectionality have been implemented in practice in eight European disaster management systems. The authors found that in some countries, vulnerability was categorised due to “ascribed characteristics” such as age or chronic illness and, ultimately, neglected some “underlying causes of uneven coping capacities” (ibid, p. 758). In order to address this lack of nuance, the authors developed a framework with four conceptual spectrums in order to disentangle the cumulating factors which interact to influence vulnerability in a crisis. These four spectrums include individual capacities and needs, societal support networks, critical services and means, and public support structures which subsequently can “intersect in unique ways, aggravate each other or balance each other out depending on the crisis situation” [20] (p. 9). These spectrums were pivotal to the development of the survey of which this paper's analysis is based and were invaluable in gaining an understanding of the differences in the individual coping capacities of the survey's respondents.
Therefore, this paper seeks to build on this approach and contribute to the existing body of knowledge on intersectionality and vulnerability in disasters by examining the ways that social exclusion, marginality, and gender intersect in order to influence negative outcomes related to the COVID-19 pandemic, particularly in regard to access to material resources (food, shelter, and income) and the mental health of women who are clients of social care organisations in comparison to men. In so doing, this paper will illustrate that, even among women who are considered to be “socially marginalised”, there are still varying factors which contribute to their outcomes in a crisis.
2.2. Factors influencing outcomes on material resources and mental health
Within literature on socially marginalised women in general, they are more likely to face greater economic ramifications due to the pandemic [21], as well as food insecurity (Scarlett et al., 2021); [22], and higher frequencies of psychosocial distress [11] However, according to Kuran et. al., (2020, p. 6) [18]; an understanding of who is vulnerable in a given situation can only be acquired by adopting a “deep and nuanced identification and analysis of elements of vulnerability that might intersect and result in differentiated degrees of vulnerability”. Therefore, in the case of socially marginalised women, elements to consider when examining outcomes would include gender and social exclusion as a result of race or ethnicity, housing situation, socioeconomic status, and migration status. The following sections will outline previous research which illustrates how these intersections have shaped the experiences of socially marginalised women related to the pandemic, rather than homogenise their outcomes.
The interaction of race and ethnicity with gender, for example, serves to generate unique experiences related to the pandemic due in no small part to the embeddedness of racism and discrimination within institutions [21]. In the United States, the outcomes of the pandemic are disproportionately felt by women of color and ethnic minority women who not only face a prominent lack of linguistically and culturally sensitive information related to COVID-19 but must navigate their lives in the midst of institutions that have historically disregarded their needs (Ibid). For women of color in the U.S, these factors are compounded by their daily realities, as they are disproportionately employed in sectors deemed ‘essential’, face disparities in the quality of healthcare they receive, and have fewer resources to cope with a crisis such as a pandemic in general (Pirtle & Wright, 2021). In Europe, Roma women tend to live in conditions of extreme poverty which, in conjunction with barriers to accessing healthcare, increase their susceptibility to the virus [23]. In Bulgaria, for example, these risks are heightened even further, as over-policing increased in Roma communities and became a more frequent presence than healthcare authorities within the first six months of the pandemic [24].
Homelessness is yet another factor which intersects with gender to influence outcomes. According to Grammatikopoulou et al. (2020) [25] women affected by homelessness may be at an increased risk of contracting COVID-19 due to overcrowded conditions in shelters and difficulties maintaining proper hygiene. Homelessness has also been revealed to shape mental health outcomes as a result of the pandemic, with research by Riley et. al., (2021) [26] noting symptoms of depression (55%) and anxiety (45%) among women living in unstable housing circumstances in San Francisco, California. In a similar vein Scarlett et. al., (2021) [14], noted that risk factors associated with depression among individuals residing in emergency or temporary accommodation in France included being female, in addition to being single, chronically ill, or facing food insecurity.
Other researchers, such as Douglas et. al., (2020) [11] have emphasised the role that socioeconomic status has in exacerbating critical outcomes for women, both in terms of coping and in terms of overall mental wellbeing, noting that it can increase psychosocial stress and financial insecurity as a result of the pandemic due to low or lack of financial reserves. Similarly Fuller-Rowell et. al., (2021) [12], have noted how, when socioeconomic status is accounted for, an increase in sleep problems globally can be observed, with women experiencing higher frequencies of sleep problems than men, in addition to higher rates of symptoms of depression. Furthermore Gebhard et. al., (2020) [27], have also advocated for taking socioeconomic status into account when attempting to uncover the underlying factors behind gender disparities in COVID-19-related outcomes. Socioeconomic status does not standalone, however, and is a multidimensional factor influenced by a myriad of other factors, including holding precarious or vulnerable jobs [15,21], higher concentrations of women in sectors impacted by crisis-related disruptions [5], and having less resources than men overall to help them recover from a loss such as sudden unemployment [28].
Migration status is also revealed as a contributing factor to these outcomes if socioeconomic status is viewed in this manner. A study in Israel noted the difficulties that migrants faced during the COVID-19 pandemic, which included precarious employment related to being female, being older in age, having a lower socioeconomic status, and having resided in the country for less than five years [29]. In a similar vein Paremoer et. al., (2021) [16], noted how the intersections between exploitative working environments, gender, class, and migration status impacted susceptibility to contracting COVID-19, and Scarlett et. al (2021) [14] linked symptoms of depression to recent unemployment and food insecurity, with higher frequencies being found in asylum-seekers or migrants with a residence permit when compared to French respondents. Furthermore, higher frequencies of anxiety and depression among migrant women were also found in research analysing the impact of the pandemic on over 20,000 respondents [17].
Another factor which is currently underexplored in research is the link between exposure to previous hazards and mental health outcomes related to the COVID-19 pandemic and the ways that such exposure interplays with marginalisation, exclusion, and gender. For example, a study by Breslau et al. in Detroit, United States (1999) noted that exposure to a previous hazard increased the risk of PTSD and that this risk increases if an individual is exposed to multiple hazards [30]. Min Ying Wong et al. (2022) have also recently contributed to this area of study by seeking to understand how exposure to social and political unrest in Hong Kong in 2019 influenced mental health outcomes during the COVID-19 pandemic among women. Their findings illustrated that nearly a quarter of their respondents showed potential symptoms of PTSD, which was nearly twice the rate of suspected PTSD prior to the social unrest (Ibid, 2022). Although there is research acknowledging the potential for aspects of the COVID-19 pandemic (food shortages, lockdowns, etc.) to trigger memories of previous hazard exposure among migrants [31,32], to our knowledge no other research currently exists which analyses this link among populations with various degrees of exclusion and marginalisation. There is also no current research to our knowledge which analyses this link in a gender disaggregated manner.
2.3. Hypotheses
Based on trends observed in previous research, we expect to find a higher prevalence of negative material impacts such as loss of income and decreased access to food and shelter among socially marginalised women than among socially marginalised men (Hypothesis 1). Second, we expect worse mental health impacts among socially marginalised women as a result of the pandemic than among socially marginalised men (Hypothesis 2). Lastly, we expect to observe higher frequencies of PTSD among socially marginalised women related to the pandemic than among socially marginalised men, especially if they have been previously exposed to a hazard or a disaster (Hypothesis 3). These hypotheses assume that the intersection of gender and various dimensions of social marginalisation are related to worse material and mental impacts of COVID-19.
3. Methods
3.1. Quantitative survey
3.1.1. Recruitment of respondents
This paper utilised responses to a survey which sought to better understand the experiences of socially marginalised groups related to the COVID-19 pandemic since March 2020.
The survey was conducted among the clients of social care organisations like the Salvation Army or other NGOs in thirteen European countries (Hungary, Estonia, Norway, Portugal, Spain, Germany, the Czech Republic, Finland, Denmark, Italy, Belgium, the Netherlands, and France). The clients who were interviewed were recipients of organisations that provided services ranging from food distribution to shelter for individuals who are homeless to care facilities where individuals live for longer time periods. As a result, respondents ranged from individuals who live in their own homes to individuals who live on the street. The immigration status of the respondents also varied, and included individuals who were national citizens of the country where the survey was conducted, asylum-seekers, migrants with residence permits, and individuals who were undocumented when the survey was conducted.
The study was approved by the Norwegian Centre for Research Data, and similar institutions or research ethics committees in other countries also participated in the study. Respondents were mainly recruited in the second half of 2020, (although interviews continued until August of 2021) and were asked to participate in the survey when they visited the care organisations or received services from them. Most respondents were recruited and interviewed through the Salvation Army, but other social care organisations, such as the Red Cross, were also used. The interviews were conducted face-to-face, in calm and private areas within the institutions. The interviewers were given a training focusing on ethics and practical survey issues by IZEW (International Centre for Ethics in the Sciences and Humanities, at the University of Tübingen in Germany).
The social care organisation staff invited individuals to participate in the survey interview through general announcements and requests. Respondents were informed that no negative consequence would come from rejecting the invitation and participating in the survey was presented similarly to other voluntary activities of the Salvation Army. This information was also conveyed in the information sheet given and/or read to the interviewee in their native language. To mitigate any dependency and implications on future relations, participants were also given the choice to opt for Salvation Army staff from a different service centre to conduct the interview. Additionally, service users were able to express a preference for a male or female interviewer.
We were aware that interviewing participants about sensitive topics such as experiences of hazards and threats may cause participants distress and discomfort, but we also kept in mind that giving participants the space to talk about such experiences may have positive and therapeutic effects from reporting their experiences to third parties. Therefore, during the interviews, reflexivity and special techniques were used to ensure that the participants were not harmed in any way. The interviewers were trained in these techniques prior to conducting the interviews. In addition, all interviewers were trained on how to ethically recruit and interview service users in order to prevent an exploitation of social hierarchies or dependencies.
3.1.2. Survey themes
Background variables. The survey includes questions about sex, age, residence status (national citizen, asylum seeker, residing in the country without documentation etc.), and whether respondents perceive that they represent a minority.
Living arrangements. In the classification of living and sleeping arrangements, we use the Framework for Understanding Homelessness on a Global Scale [33]. The framework allows for the classification of individuals according to the level of protection they enjoy in their living arrangements: people without accommodation, people living in temporary or crisis accommodation and people living in severely inadequate and/or insecure housing. We ask respondents: “Where have you been living and sleeping most of the time over the past year?“, and divide the answers on three alternatives: 1) My own home, 2) Centre/facility, 3) Street or temporarily arrangement. The category “Street or temporary arrangement” is comprised of the alternatives: Street or other open space, Car, With friends or relatives on a temporary basis, Hotel, motel etc., Trailer or tent, Abandoned houses and homeless hostel. Centre/facility is comprised of the following possible answers: Rehabilitation centre (people with drug or alcohol problems, resocialisation after prison) and Facility for migrants. We also ask respondents how many years they have lived without a home and how many years they have been receiving services from the social care organisation or NGO. The level of protection provided by living arrangements is the main source of vulnerability we use in the study.
Exposure to COVID-19. The survey measures exposure to COVID-19 in several ways. We asked respondents whether they have been infected themselves, whether friends have been infected, and whether they have lost someone close to COVID-19. We also measure exposure to COVID-19 as societal exposure, and measured the country with the highest infection rate per inhabitant (i.e. Portugal). Additionally, we ask about material impacts of the pandemic: “The pandemic has had a negative effect on my income, access to shelter, food etc.?”
Psychological and physiological health. We apply Nikoo et. al's (2015) [34] enumeration of the frequent physical and mental illnesses among individuals in precarious material situations. In the survey we asked: “Have you ever been told by a doctor that you have any of the following conditions?” We provided 15 different answer alternatives for the respondents, comprised of different physiological and psychological diagnoses. We made two variables of these. The variable “physiological diagnoses” concerns heart and lung conditions (i.e. risk group), while the variable “psychological diagnoses” include schizophrenia, depression and personality disorders. This study focuses on the impact of the latter on mental health outcomes related to the pandemic.
Experience with previous disasters. The survey includes 16 answer alternatives about experiences with previous man-made and natural disasters, such as “In the last ten years, have you experienced any of the following natural or man-made hazards?” (e.g. extreme heat, earthquake, wildfire, terrorist attack, war). We also ask respondents to rate the physiological and mental strain they experienced as a result of the disasters.
Material impact is measured through the question: “The pandemic has had a negative effect on my income, access to shelter, food etc.?” Answer alternatives ranged from 1 (totally disagree) to 5 (totally agree).
Psychological impact. We measure psychological impact of the pandemic by means of three variables: The first is: “The pandemic has had a negative effect on my mental wellbeing, or my mental health.” In these questions we rely on the United Nations University's “Handbook for assessing loss and damage in vulnerable communities” [35]. The second question is “Since March 2020, I have been afraid of being infected with COVID-19”, which was developed by the research team. The answer alternatives to these two questions ranged from 1 (totally disagree) to 5 (totally agree). Furthermore, the questionnaire delves into the psychological trauma caused by the pandemic using selected items from an adopted version of the post-traumatic stress disorder scale (Bliese et al., 2008). The third variable measuring psychological impact is symptoms of PTSD because of the pandemic: “To what extent have you felt the following during/after the pandemic”, where the possible answers include: “I have recurring thoughts or memories of the pandemic”, “I feel sudden emotional or physical reaction when reminded the pandemic”, “I avoid thoughts or feelings associated with the pandemic”. Numbers were associated with these answers and ranged from 1 (not at all) to 4 (all the time). We combined these three items into a scale (min: 3, max: 12). The internal reliability of the PTSD index was acceptable (Cronbach's Alpha .71).
Free text questions. The survey includes an open free text question, focusing on respondents’ biggest problem (if any) during the pandemic: “Since the outbreak of the pandemic in March 2020, what has caused the biggest problem for you?” Analysing the free text answers, we have divided the answers into five main categories, “material impacts”, “health”, “social relations”, “freedom of movement”, and “impact of measures”, plus two summary categories, “other” and “no answer”. Although these types of impacts are related, we define them as separate categories to grasp the most important aspects of the COVID-19 impacts on the respondents. We will expand further on that in the results section. Four of the five main categories (exception: “freedom of movement” have then been divided into two to four subcategories.
3.1.3. Analysis
When comparing the mean scores of different groups, we use one-way Anova tests, which compare whether the mean scores are equal (the null hypothesis) or (significantly) different. We use Chi square tests to compare groups' scores on particular variables, if we, for instance, cannot compare means due to the variables’ level of measurement. The Chi square test tests whether the actual distribution of groups on a variable is statistically significantly different from a coincidental distribution, or an independent normally distributed sample.
We use hierarchical, linear regression analyses, where independent variables are included in successive steps to assess the conditions explaining variation in the respondents’ answers to the two variables measuring mental impacts: a) Negative impacts on mental wellbeing or mental health, b) PTSD symptoms. The most basic independent variables (i.e. the demographic) are included first, e.g. age, sex, living arrangements. Then the other independent variables are included. The regression analyses enable us to examine the separate effects of the independent variables on the dependent variables, controlled for the other variables. Of course, we cannot conclude about causality, as this is a cross-sectional and correlational study. We nevertheless use the term predict when we describe the regression analyses.
4. Results
4.1. Description of the sample: who are the socially marginalised women in the study?
Altogether, we analysed answers provided by 313 respondents from 13 European countries in our survey (Table 1 ).
Table 1.
Respondents from the 13 different countries, including the share of female respondents.
| Country | Number | Percent | Share of women |
|---|---|---|---|
| Estonia | 61 | 19% | 26% |
| Hungary | 32 | 10% | 48% |
| Norway | 28 | 9% | 43% |
| Portugal | 52 | 17% | 19% |
| Spain | 20 | 6% | 55% |
| Germany | 13 | 4% | 0% |
| Czech Republic | 37 | 12% | 27% |
| Finland | 11 | 4% | 18% |
| Denmark | 4 | 1% | 0% |
| Italy | 7 | 2% | 14% |
| Belgium | 26 | 8% | 23% |
| Netherlands | 17 | 5% | 6% |
| France | 5 | 2% | 40% |
| Total | 313 | 100% | 28% |
Low numbers in some of the countries participating in the study are largely due to COVID-19 restrictions, which have impeded data collection. Table 1 also shows that 28% (n = 88) of the respondents are female. Two of the respondents chose the third alternative “undefined” when reporting their gender. Most of the respondents are recruited through social care organisations run by the Salvation Army (SAL), but in some countries we have also recruited respondents through social care organisations run by other NGOs.
Only 21% of the respondents were 39 years old or younger (Table 2 ). About half of the respondents are between 40 and 60 years old, while 25% are 60 years old or more.
Table 2.
Respondents’ age distribution on six different categories.
| 18–29 | 30–39 | 40–49 | 50–59 | 60–69 | 70 or < | Total | Total | |
|---|---|---|---|---|---|---|---|---|
| Women | 6% | 15% | 20% | 32% | 24% | 2% | 100% | 84 |
| Men | 6% | 16% | 27% | 26% | 19% | 5% | 100% | 219 |
| Total | 6% | 16% | 25% | 28% | 20% | 5% | 100% | 303 |
The differences between the age groups of men and women are not very big, although it should be mentioned that there are higher shares of men in the age group 40–49, while there are somewhat higher shares of women in the age groups 50–59 and 60–69.
The majority of the respondents (72%) report that they are national citizens, while 21% report that they are immigrants with a residence permit, asylum seekers, or are residing in the country without documentation. The remaining share (7%) preferred not to answer this question. Comparing men and women in the sample, 20% of the women were immigrants with a residence permit, asylum seekers, or were residing in the country without documentation, compared to 23% of the men.
We also asked respondents: “Would you consider yourself part of a minority (e.g. cultural, ethnic, health/disability related, sexual orientation)?” A share of 20% answered yes (25% women vs. 18% men). Respondents who answered yes were also encouraged to specify their minority category. Some of the respondents mentioned particular nationalities that may be minorities within countries, other wrote “cultural”, “ethnic”, or “my sexual orientation”.
Regarding the living conditions of respondents, we combine the answer alternatives into three categories (Table 3 ).
Table 3.
Respondents’ answers to the question: “Where have you been living and sleeping most of the time over the past year?“, distributed over four categories. Mean scores for years living without your own home and years as a SCO client.
| Living arrangement | Percent | Number | Women | Men |
|---|---|---|---|---|
| My home | 24% | 75 | 40% | 20% |
| Centre/Facility | 14% | 43 | 16% | 14% |
| Street or temporary arrangement | 55% | 174 | 44% | 66% |
| Total | 100% | 292 | 100% | 100% |
Seven per cent of the respondents answered “other”, and this is not included in Table 3. Of 292 identified living arrangements, 24% reported “Living in their own home”. These include clients of soup kitchens, day centres, or other care organisations. Centre/facility refers to centres for alcohol and drug addiction, resocialisation after prison, facilities for migrants and other care organisations providing long-term accommodation. Living on the street or under temporary arrangement refers to living on the street, open spaces, cars, abandoned houses, homeless shelters, refuges or under other temporary arrangement (e.g. with friends or relatives). We also define homeless shelters as temporary, as they generally offer only over-night stay and are lacking stability.
Comparing men and women in the sample, we see that the sample is biased with respect to the living arrangements of men and women. Women have a higher share of respondents living in their homes (twice the share of men), and there is a higher share of men living on the street, compared with women (P = 0.001).
Respondents were also asked about psychological (schizophrenia, depression, personality disorder) and physiological diseases (heart and lung conditions). Comparing male and female respondents’ answers to psychological diagnoses, 21% male respondents reported such diagnoses, compared to 27% of the women. Concerning physiological diagnoses, 32% male respondents reported such diagnoses, compared to 27% of the women. Thus, we see more psychological diagnoses among female respondents and more physiological diagnoses among the male respondents.
4.2. Exposure to COVID-19 among the respondents
The survey asks the respondents several questions about their experiences with the pandemic. We refer to this as their exposure to the pandemic: direct (whether they were infected themselves) and indirect (e.g. whether their friends were infected). A total of 22 of the 313 respondents (7%) answered that they have been infected (6% women, 7% men). The average number of infected acquaintances is 3.7 (2.8 for women and 4 for men). A total of 23 respondents (7%) reported that they had lost someone close to them due to the COVID-19 pandemic (7% women, 8% men).
Finally, when it comes to direct and indirect exposure to COVID-19, respondents from Spain (20%), Portugal (14%) and the Czech Republic (16%) had the highest shares of respondents who had been infected themselves. Respondents in the two former countries reported that between 10 and 13 acquaintances had been infected with COVID-19.
4.3. Impacts of the COVID-19 pandemic
The following sections will outline the material and mental health impacts of COVID-19 among socially marginalised women.
4.3.1. Material impacts
Negative material and economic impacts are measured with the question: “The pandemic has had a negative effect on my income, access to shelter, food etc.” While 45% of the female respondents agreed with this statement, 42% of the male respondents agreed. Although there was a higher share of women who strongly agreed than men (26% vs. 18%), a Chi-square test indicates that differences are not statistically significant (p = 0.503).
4.3.2. Mental impacts
We focus on three types of mental health impacts in the study. The first measure of psychological impact is the statement “Since March 2020, I have been afraid of being infected with COVID-19.” While 42% of the female respondents agreed with this statement, 38% of the men agreed. The difference is more significant when looking at shares disagreeing with the statement (37% for women vs. 53% for men). A chi-square test indicates that differences are statistically significant at the 1%-level (p=<0.01). Thus, we may conclude that the female respondents have been more afraid of being infected with COVID-19 than the male respondents.
The second measure of psychological impact was a PTSD-scale based on three items. We made a sum scale index of the three questions with minimum value 3 (1*3) and maximum value 12 (4*3). While the female respondents scored 6.6 points on this index, the male respondents scored 5.7 point (p = 0.004). Thus, we see significantly more PTSD symptoms related to the pandemic among female respondents.
The third measure of mental impacts was “The pandemic has had a negative effect on my mental wellbeing, or my mental health”. While 51% of the female respondents agreed with this statement, 38% of men agreed. Although a chi-square test indicates that differences are not statistically significant (p = 0.212), this result is in line with the (statistically significant) results for the two other measures of mental impacts in the study, indicating more negative mental impacts of the pandemic for female respondents.
4.3.3. Free text answers
The survey includes an open free text question, focusing on respondents’ biggest problem (if any) during the pandemic: “Since the outbreak of the pandemic in March 2020, what has caused the biggest problem for you?” A total of 209 of the respondents replied to this question, including 63 women and 144 men (and two who did not tick off any of these gender categories). The reply rate on this question is 72% among women versus 64% among men. It is important to remember that this question invites the respondents to comment on the “biggest problem” caused by both the COVID-19 virus and the related mitigation measures, or a combination of the two.
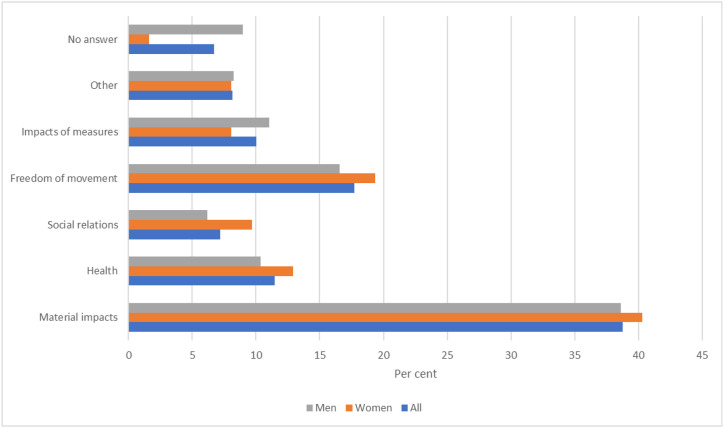
After reading through the free text answers we identified five main themes that we have included as categories: “Material impacts”, “health”, “social relations”, “freedom of movement”, and “impact of measures”. In addition, we have included two general categories, “other” and “no answer”. The main categories have also been divided into subcategories. Fig. 1 shows the main results.
Fig. 1.
“Since the outbreak of the pandemic in March 2020, what has caused the biggest problem for you?” Results of thematic analysis of free text answers, based on 207 answers. (63 women and 144 men). Per cent.
When the respondents were asked about what has caused the biggest problem for them after the outbreak of the pandemic, 39% of the respondents replied some sort of material impact. This was the most prevalent answer to this question, followed by lacking freedom of movement (18%), (physical/mental) health (11%), and impacts of measures (10%). Typical material impact replies included e.g. “unemployment”, “reduced income”, “lost accommodation”. Typical freedom of movement replies included e.g. “I can't leave the house”, “That I cannot go and return”, “Confinement”. Typical health replies were e.g. “Psychological stress”, “Fears of illness and what will happen”, “Fears of hospitalisation”. Typical impact of measure replies were e.g.: “The closure of shops and activities”, “Wearing a mask”. These were other impacts of measures than those included in the other impact categories. Typical social relations replies were e.g. separation from people you love, e.g. parents, children. Examples of “other” replies were e.g. “The hysteria has been a nuisance”, “Navigate the new regulations”. Thus, we see that only the health impact relates to the impact of the virus/pandemic, while the reported impacts mainly relate to different aspects of the impact of the mitigation measures, e.g. material impacts, social relations, freedom of movement. Although these types of impacts are related, we define them as separate categories to grasp the most important aspects of the COVID-19 impacts on the respondents.
Results indicate that women tend to emphasise negative effects related to social relations (2,5% points higher than men) more in their free text answer to the biggest problem for them after the outbreak of the pandemic in addition to restrictions related to freedom of movement (1,7% points higher than men). Men tend to emphasise impacts of measures more (2% points higher than women). Additionally, men were more likely than women to provide no answer to this question (5% points higher than women).
The 81 answers related to material impacts can be divided into four subcategories: “Economy” (21%), “work” (65%), “shelter” (10%), and “food” (4%). Typical replies in the category economy were e.g. “The lack of money and what all this causes”, and “Coping with the family's financial situation”. Typical replies in the category work were e.g. “unemployment”, “no traveling to or from work”, “less or no work; couldn't do so much”. Typical replies in the category shelter were e.g. “Homeless”, “Looking for accommodation and work”, Typical replies in the category food were e.g. “Find food and have access to hygiene”, “Food, house and job”. We did not find notable differences between the answers of men and women concerning material impacts.
The 24 answers related to health impacts can be divided into three subcategories: “Physical health”, “mental health”, and “fear/insecurity”. Most of the answers (79%) fit into the category “fear/insecurity”. Typical answers here were: “unexpected, I don't know what will happen”, “mental influence, fear, because there is a severe virus, can be fatal”.
The 21 answers related to impacts of measures were divided into two subcategories: “access of services” and “masks”. Typical answers related to access of services were: “daily life has been more complicated because of the closure of services”, “Closed services for homeless people, no activities for substance abusers”, “lack of occupational therapy”, “Everything is closed, everything is limited, you have little choice, this also has to do with choosing a place to sleep”.
The 15 answers related to social relations were divided into four subcategories: “General” (e.g “Isolation”, “Solitude”), “individuals” (e.g. “I didn't get together with mom. Mom's 76, and I can't meet her, I'm worried about her”, “separation from my girlfriend”), “death” (e.g “My father died of corona”), and “worse”, (e.g “My former neighbor, because of the stress of this experience followed me with a knife”, “people have become selfish”).
4.4. Multivariate analyses
The second aim of the study is to examine factors influencing the material and mental impacts of COVID-19 among socially marginalised women in comparison to men. We do this through multivariate analyses, examining the effects of several independent variables (e.g self-assessed health, psychological disease, type of income, resilience) and controlling for key variables like living arrangements, age, etc. In this section, we conduct three multivariate analyses: one analysis focusing on factors influencing material impacts, and two analyses to examine factors influencing the mental impacts of the COVID-19 pandemic for socially marginalised women and men: the fear of being infected with COVID-19 as the dependent variable and another with PTSD symptoms related to COVID-19. We do not include the third measure of mental COVID-19 impacts in the multivariate analyses, as we did not see statistically significant differences between men and women on this variable.
4.4.1. Negative material impacts of COVID-19
In Table 4 we present linear regression analyses examining factors influencing the dependent variable: “The pandemic has had a negative effect on my income, access to shelter, food etc.”
Table 4.
Linear regression. Dependent variable: ““The pandemic has had a negative effect on my income, access to Shelter, food, etc.” Standardised beta coefficients.
| Variables | General sample | Women | Men |
|---|---|---|---|
| Gender (male = 2) | .010 | ||
| Age | −.168*** | .141 | −.179*** |
| Own home (No = 1, Yes = 2) | .167*** | −.042 | .165** |
| Resilience scale (3 items) | −.159*** | .032 | −.204*** |
| Portugal/Spain/Czech | −.006 | .080 | −.023 |
| (In)formal paid work as income (=2) | .106* | −.111 | .122* |
| Social benefits as income (=2) | −.151*** | −.128 | −.159** |
| Adjusted R2 | .107 | −.008 | .136 |
*p < 0.1, **p < 0.05, ***p < 0.01.
The adjusted R2 value indicates that the model for the general sample explains 11% in the dependent variable, and 14% for the male respondents but none of the variation in the answers of the female respondents on the dependent variable. This indicates that the included independent variables fail to cover the factors explaining negative material COVID-19 impacts for female respondents. This is a crucial area for future research. For this reason, we only present the significant results in Table 4, related to the general sample and the male sample below.
First, the table indicates that respondents who score higher on the individual resilience scale in the general sample and in the sample of male respondents report of less negative material impacts of COVID-19, controlled for the other variables in the model. Second, age contributes negatively and significantly in the general sample and in the male sample, indicating that this is related to less negative material impacts controlled for the other variables in the model. Third, the variable “Own home” contributes positively and significantly in the general sample and in the male sample, indicating that respondents who live in their homes experience more negative material impacts, controlled for the other variables in the model.
We also see that type of income significantly influences material impacts of COVID-19: (In)formal paid work as income is positively and significantly related to negative material impacts, while social benefits as main income is negatively and significantly related to negative material impacts. This means that the former type of income is more likely to be lost due to COVID-19, involving negative material impacts, while the latter type of income is not lost, and thus not related to negative material impacts due to COVID-19.
We have examined the significance level of the F-changes in the three regression analyses in Table 4, to assess whether some of the variables added in the steps significantly improved the predictions in each step. The following variables contributed to significant changes (p=<0.01) in the R-square for the general sample: age, living in your own home and social benefits as main source of income. Additionally, the resilience scale contributed to significant changes (p=<0.05) in the R square. In the sample including only women, none of the variables contributed to significant changes (p=<0.01) in the R-square. In the sample including only men, the following variables contributed to significant changes (p=<0.01) in the R-square: age, living in your own home and the resilience scale. Additionally, social benefits and (in)formal paid work as main source of income contributed to significant changes (p=<0.05) in the R square.
4.4.2. Fear of being infected with COVID-19
In Table 5 we present linear regression analyses examining factors influencing the dependent variable: “Since March 2020, I have been afraid of being infected with COVID-19”.
Table 5.
Linear regression. Dependent variable: “Since March 2020, I have been afraid of being infected with COVID-19” Standardised beta coefficients.
| Variables | General sample | Women | Men |
|---|---|---|---|
| Age | −.003 | −.024 | −.004 |
| Own home (No = 1, Yes = 2) | −.013 | .047 | −.019 |
| Portugal/Spain/Czech | .038 | −.020 | .051 |
| Trust gov. Info on COVID-19 | .183*** | .226** | .164*** |
| Television as info source (=2) | .096* | .042 | .115** |
| General health worry | .544*** | .483*** | .561*** |
| Self-assessed health | .099* | −.041 | .142** |
| Gender (Male = 2) | −.023 | ||
| Adjusted R2 | .355 | .255 | .369 |
*p < 0.1, **p < 0.05, ***p < 0.01.
First, we see that the variable "General health worry" is positively and significantly related to being afraid of COVID-19 infection. This means that respondents who agree with the statement “I generally worry about risks related to my health (e.g. falling ill)” are more afraid of COVID-19 infection. Female respondents score significantly higher on the "General health worry" variable than male respondents (3.2 vs. 2.7 points) (p = 0.029), indicating that this might be an important explanation to the higher COVID-19 infection worry of women. Second, the table indicates that respondents who agree with the statement “I trust the information that the government of this country provides on the ways of avoiding Covid-19 infection” are significantly more afraid of COVID-19 infection. Third, using television as a source of information about COVID-19 is also related to higher levels of worry about infection. Fourth, we see that higher levels of negative self-assessed health also are positively and significantly related to higher levels of worry about infection. This means that the poorer respondents assess their own physical health to be, the more they worry about COVID-19 infection. The adjusted R2 value indicates that the model for the general sample explains 36% in the dependent variable, 26% for the female respondents and 37% for the male respondents.
We have examined the significance level of the F-changes in the models in the three regression analyses in Table 5, to assess whether some of the variables added in the steps significantly improved the predictions in each step. The following variables contributed to significant changes (p=<0.01) in the R-square for the general sample: living in Portugal/Spain/Czech Republic, trust in authorities' information about COVID-19, general worry about health risks (e.g. falling ill). Additionally, living in your own home and television as a source of information contributed to significant changes (p=<0.05) in the R square. In the sample including only women, only general worry about health risks (e.g. falling ill) contributed to significant changes (p=<0.01) in the R-square. In the sample including only men, the following variables contributed to significant changes (p=<0.01) in the R-square: trust in authorities’ information about COVID-19, television as a source of information, general worry about health risks (e.g. falling ill). Additionally, self-assessed physical health contributed to significant changes (p=<0.05) in the R square.
4.4.3. Factors influencing symptoms of PTSD because of the pandemic
In Table 6 we present linear regression analyses examining factors influencing symptoms of PTSD because of the pandemic.
Table 6.
Linear regression. Dependent variable: «Symptoms of PTSD because of the pandemic » Standardised beta coefficients.
| Variables | General sample | Women | Men |
|---|---|---|---|
| Immigrants, asylum seekers, without documentation (=2) | .140** | −.057 | .205*** |
| Age | .060 | .075 | .058 |
| Own home (No = 1, Yes = 2) | .150** | .316** | .095 |
| Portugal/Spain/Czech (=2) | .232*** | .066 | .286*** |
| Experienced previous disasters (=2) | .152** | .013 | .190** |
| Negative material impacts | .188*** | .279** | .163** |
| Gender (Male = 2) | −.128** | ||
| Adjusted R2 | .192 | .140 | .181 |
*p < 0.1, **p < 0.05, ***p < 0.01.
First, we see that the variable "Immigrant, asylum seeker, without documentation" contributes positively and significantly, which means that these respondents are more likely to experience PTSD symptoms related to the pandemic. This is also the case when we control for the other variables in the model. Second, the variable “Living in your own home” contributes positively and significantly, which means that respondents living in their own homes are more likely to experience PTSD symptoms related to the pandemic. This applies, however, only to female respondents, and not to male respondents. The contribution of this variable is considerable in the female sample, indicating an important issue for future research. Third, the variable "Portugal/Spain/Czech" contributes positively and significantly for the general sample and for male respondents, indicating that respondents who live in these countries report of higher levels of PTSD symptoms. This variable measures exposure to COVID-19 infection, as these are the countries in the sample where respondents had the highest level of exposure to COVID-19 infections. Fourth the variable “Have experienced war, terrorism, extreme cold, violent demonstrations, earthquake” contributes positively and significantly for the general sample and for male respondents, indicating that respondents who have experienced previous traumas like this are more likely to experience PTSD symptoms related to the pandemic, controlled for the other variables in the model. Fifth, the variable "negative COVID-19 impact on income etc." contributes positively and significantly for all groups, indicating that people who have experienced such negative impacts report of higher levels of PTSD symptoms, controlled for the other variables in the model. The contribution of this variable is stronger for the female respondents, indicating that they might be harder hit mentally by the material impacts of COVID-19. Finally, gender contributes significantly and negatively in the general sample indicating that female respondents experience more PTSD symptoms related to the pandemic, when we control for the other variables. The adjusted R2 value indicates that the model for the general sample explains 19% in the dependent variable, 14% for the female respondents and 18% for the male respondents.
We have examined the significance level of the F-changes in the three regression analyses in Table 6, to assess whether some of the variables added in the steps significantly improved the predictions in each step. The following variables contributed to significant changes (p=<0.001) in the R-square for the general sample: living in your own home, living in Portugal/Spain/Czech Republic. Additionally, experience with previous hazards and negative material impacts related to COVID-19 contributed to significant changes (p=<0.01) as well as immigrant status and gender (p=<0.05). In the sample including only women, only living in your home (p=<0.01) and negative material impacts contributed to significant changes in R square. In the sample including only men, the following variables contributed to significant changes in the R-square: living in Portugal/Spain/Czech Republic (p=<0.001), immigrant status, previous experience with hazards (p=<0.01) and living in your own home and negative material impacts (p=<0.05).
5. Concluding discussion
5.1. Factors influencing material and mental impacts and questions for future research
The survey and the free text results provided very interesting insights into the ways that various spectrums of vulnerability intersect with gender and social marginalisation in order to influence material and mental outcomes related to the COVID-19 pandemic. One prominent example emanated from the “social support networks” spectrum, which refers to socioeconomic and social inclusion [20]. In the case of our respondents, living in your own home was associated with more negative material impacts, especially if there was a loss of formal or informal income. Although the survey and free text results were able to uncover other intersectionalities in this regard, such as being homeless and having a hard time finding work or living in your own home and struggling to take care of your family financially, it was impossible to find variables that were correlated with negative material impacts for women specifically. This is a shortcoming of the survey but is certainly an area that should be explored further in future research.
Despite being unable to gain a more nuanced understanding of the material impacts related to the COVID-19 pandemic, the survey did reveal that negative material impacts were related to a higher frequency of PTSD-symptoms among socially marginalised women, which relates both to the “individual needs and capacities” spectrum as well as the “social support networks” spectrum. This connection was especially apparent if they live in their own homes. This could be because mothers were especially vulnerable to losing or quitting their jobs as a result of the pandemic and on average faced an increase in responsibilities related to their household and families [36]. This supposition is also echoed by the World Health Organisation's research on gender disaggregated impacts in post-disaster contexts, stating that increased caregiving responsibilities may result in placing the needs of family and loved ones above their own, and may explain declines in emotional well-being (2002). Higher levels of general health worry found among women within the surveyed sample may also partially explain the frequency of PTSD-symptoms, as women may be particularly fearful of infecting family members and loved ones [3] due to more frequent engagement in caregiving activities [37]. They may also experience reduced external support in order to help them cope with this strain [38]. However, similarly to the difficulties of the study identifying variables correlated with negative material impacts, it was also difficult to gain a better understanding of how particular housing arrangements such as homelessness or living in temporary accommodation, could possibly be linked to other mental health outcomes for women. This is certainly an area that should be explored in future research.
Although it was expected that the survey results would reveal particular outcomes for women due to an intersection of the “individual capacities and needs” spectrum with exposure to previous hazards [20], the expected correlation was only found among male respondents, although the survey revealed that women experience more PTSD-symptoms related to the pandemic overall. This is a very interesting finding and one that deserves further investigation in the future, as overall women experience more stressful life events than men throughout their lives [13] and are at a higher risk of developing PTSD compared to men [39] which is likely to formulate unique mental outcomes when interacting with social exclusion in post-disaster contexts.
5.2. What can be done to reduce the impacts?
This study highlighted, first and foremost, the lack of gender-disaggregated data among populations with varying degrees of vulnerability and marginalisation regarding the material and mental impacts of disasters. This is problematic, not only because it heightens the invisibility of gender-differentiated narratives in a post-disaster context for these populations, but also because it hinders the ability of disaster management personnel to incorporate them into their decision-making and planning [2]. Since the COVID-19 pandemic is a disaster both in regard to material and psychological impacts, incorporating these narratives into crisis management and planning is especially important in order to respond appropriately to the diversity of needs within populations. For example, by considering the “accessibility and functionality of public support structures” spectrum of vulnerability, crisis management professionals and national authorities could identify institutions to be improved upon in order to ameliorate adverse outcomes. This could be done by expanding social safety nets or providing additional social assistance in a disaster in order to minimise stress and negative mental outcomes emanating from crisis-related financial difficulties and disruptions to the labour market. This could also come in the form of aiding organisations such as night shelters, day centres, residential shelters, and soup kitchens who provide material, pyscho-social, and other forms of support to their clients. Research by Orru et. al (2021) [40] noted that these forms of support, as well as reliable crisis and risk information, went a long way to ensure that clients felt safe and taken care of during the pandemic-especially since many of them had nowhere else to go. Maintaining the same level of care during a crisis, however, relies on support from authorities-particularly in regard to the provision of extra financial resources and enhancing coordination of social care efforts between the state and non-governmental care services.
Other strategies that could also be utilised to mitigate disproportionate impacts are related to the “accessibility and functionality of critical services and means” spectrum of vulnerability [20]. For example, the provision of additional mental health services-particularly in a face-to-face setting if possible but also via online medical platforms-are one option. Internet cognitive behaviour therapy (iCBT) is one evidence-based intervention that could be employed, as its virtual nature could help prevent the spread of COVID-19 while combatting anxiety (Ho et al., 2020) and treating psychiatric symptoms such as insomnia [41] in a cost-effective manner [42]. However, it is important to note that the benefit of online services would be limited if access to them cannot be equitably facilitated and barriers, such as language, internet literacy, or even access to digital technology (e.g. phones) cannot be ameliorated. If equitable access is ensured, such services could also help address the higher frequency of PTSD-symptoms related to the pandemic that was exhibited among women in the study's sample.
5.3. Methodological limitations and issues for future research
Table 2 shows that only 28% of the respondents in the sample are women. Although this lower share of women might be portrayed as a methodological weakness, it is due to the fact that 170 (60%) of the respondents live on the street or under temporary arrangements (cf. Table 3). Only 20% of the respondents living on the street or under temporary arrangements are women. This reflects the fact that the majority of people experiencing homelessness are men Milaney et. al (2020) [43] report for instance that women made up 27% of the Canadian homeless population in 2016. The shares of male and female respondents are more even for respondents living in their home (44% women) and in facilities (32% women). Thus, the relatively low share of women in our sample is as one should expect, given the studied population. Additionally, the share of male respondents provides a basis for comparison of material and mental impacts.
It is, however, evident that the higher number of male respondents influences the results for the general sample on the studied outcome variables. This is likely to influence the results on the univariate analyses, e.g. the general shares agreeing with negative material and mental impacts related to the COVID-19 pandemic. This is the reason that we systematically compare results on the studied outcome variables for men and women separately, in the bivariate analyses. This is also the reason that we control for gender in the general multivariate regression analyses and conduct separate regression analyses for men and women. The uneven gender balance in the sample might however have an influence in the separate regression analyses for female respondents. As the number of respondents (focusing only on women) in these analyses is relatively low (84), the numbers of respondents within the compared groups are also low for the female respondents. As a result, the statistical power is probably low in these analyses, indicating the need for future studies to include a larger number of female respondents. Given the relatively low share of women e.g. among some groups of marginalised people (e.g. people experiencing homelessness), this will require larger general samples, or more targeted sampling, focusing especially on female respondents.
One major limitation of this study was its’ use of questionnaires which relied on self-reported answers to measure psychological health. It should be noted that the gold standard for establishing any sort of psychiatric diagnosis involves structured clinical interviews and functional neuroimaging, which should be applied in future face-to-face research [[44], [45], [46]].
Additionally, it can be noted that respondents' answers to questions about material and mental impacts, psychological and physiological diagnoses might be influenced by gender stereotypes. Our results show that more women reported psychological diseases while more men reported physiological diseases. On the one hand, this might be connected to gender stereotypes, or masculinity norms, stating e.g. that “men don't have depression”. Thus, the gender differences we have seen in the study might to some extent be influenced by reporting effects. Examining the importance of gender stereotypes in studies examining mental impacts of disasters indicates an important issue for future research. On the other hand, it is important to note that several studies show worse mental impacts reported by women in the COVID-19 pandemic reflect social and economic gender inequalities exacerbated by the disaster Figueroa et. al (2021) [47] report increased domestic violence against women, soaring unemployment rates among women, and increased unpaid familial care taken up by women—all factors that can worsen women's health, during COVID-19. Previous studies also provide interesting intersectional analyses of factors influencing mental impacts of COVID-19 among men and women. Cabezas-Rodriguez et. al (2021) [48] conclude based on a systematic review that the mental health of men was more influenced by employment conditions, while mental health impacts of women were more influenced by working conditions, the double presence and civil status. Further, depending on the size of the household (women) and unemployment (men), people in lower social classes had poorer mental health outcomes. These nuanced results illustrating intersectional relationships and worse outcomes for lower social classes indicate that reporting effects perhaps not pose a serious threat to data quality on mental impacts, e.g. as men do report negative mental impacts.
Since the sample size of the study was so small and there were less than ten individuals surveyed in some countries, it was difficult to extract more than implications of themes in this paper and impossible to generalise. However, this study highlights the importance of gaining the perspectives of individuals that are affected by various degrees of marginalisation and exclusion in order to gain a more nuanced perspective on vulnerability and its intersections with gender, which should be expanded upon in future research.
When discussing the different mental outcomes of COVID-19 on women and men, it is also important to remember that women appear to be more prone to depression than men in situations without disasters, based on the study of Lim et. al (2018) [49]. This might perhaps shed light on why the women in our sample report more negative mental impacts than men, related to COVID-19. This is an important issue for future research.
Finally, it should be mentioned that research on gender differences is not easy as gender stereotypes and gender images may influence the (socially accepted) answers that are given so that it can be difficult to differentiate the actual differences in the situation of men and women. For example, in many countries it may be expected of men to present themselves as “strong and tough”. At the same time, mental health issues may still be framed as “weakness” in some contexts. Regarding measuring the mental impacts through “being afraid of being infected” it might be more socially accepted for women to admit they are afraid. It is difficult to control for this bias in our study, as we only have the answers provided by the respondents to rely on. These results show a higher prevalence of mental impacts among female respondents, and a higher prevalence of psychological diagnoses among the female respondents. The latter result is in accordance with previous research from other contexts showing a higher prevalence of e.g. depression among women as compared to men [49]. Thus, we should not dismiss our results indicating more severe mental impacts among the female respondents, although it is still important to remember the potential influence of the discussed bias. This is an important issue for future research. We cannot totally rule out a «gendered social acceptability of answers». However, the patterns in the answers of female and male respondents does not indicate that men generally report fewer negative impacts, as a «gendered social acceptability of answers » bias would imply. The material impacts of men and women are comparable in the survey results. Additionally, men and women also have a comparable reporting of material impacts as their “biggest problem” in their free text answers. The most prevalent answer (among both men and women) was related to material impacts of the pandemic (39% of the respondents). The most common material impact that was mentioned (among both men and women) was loss of work (65%). Additionally, they also provide different answers in their other reports on “biggest problem related to COVID-19: Female respondents reported deterioration of social relations more often than men, while men mentioned lacking access to services more often than women.”
Funding
The study was funded by the Horizon 2020 project BuildERS, grant agreement No 833496.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Submission to Special Issue: Falling Through Social Safety Nets? The Disaster Experiences of the Most Marginalised in Europe.
Data availability
The data that has been used is confidential.
References
- 1.World Health Organization Gender and health in disasters. 2002. https://www.who.int/gender/other_health/genderdisasters.pdf Available at:
- 2.Erman A., De Vries Robbé S., Thies S., Kabir K., Maruo M. Gender dimensions of disaster risk and resilience. 2021. https://openknowledge.worldbank.org/bitstream/handle/10986/35202/Gender-Dimensions-of-Disaster-Risk-and-Resilience-Existing-Evidence.pdf?sequence=1 Available at:
- 3.Bronfman N., Repetto P., Cordón P., Castañeda J., Cisternas P. Gender differences on psychosocial factors affecting COVID-19 preventive behaviors. 2021. Vol 13(11) [DOI]
- 4.Barber S.J., Kim H. COVID-19 worries and behavior changes in older and younger men and women. J. Gerontol. B Psychol. Sci. Soc. Sci. 2021;76(2):e17–e23. doi: 10.1093/geronb/gbaa068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.World Bank Group Gender dimensions of the COVID-19 pandemic. 2020. https://openknowledge.worldbank.org/bitstream/handle/10986/33622/Gender- Dimensions-of-the-COVID-19-Pandemic.pdf Available Online:
- 6.Women U.N. From insights to action: gender equality in the wake of COVID-19. 2020. https://reliefweb.int/sites/reliefweb.int/files/resources/From%20insights%20to%20action%20-%20Gender%20equality%20in%20the%20wake%20of%20COVID-19.pdf Available at:
- 7.Wang C., Pan R., Wan X., Tan Y., Xu L., Ho C., Ho R. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Publ. Health. 2020;17(5) doi: 10.2290/ijerph17051729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang C., Tee M., Roy A., Fardin M., Srichokchatchawan W., Habib H., Tran B., Hussain S., Hoang M., Le X., Ma W., Pham H., Shirazi M., Taneepanicskul N., Tan Y., Tee C., Xu L., Xu Z., Vu G., Zhou D., Koh B., McIntyre R., Ho C., Ho R., Kuruchittham V. The impact of COVID-19 pandemic on physical and mental health of Asians: a study of seven middle-income countries in Asia. PLoS One. 2021;16(2) doi: 10.1371/journal.pone.0246824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dal Santo T., Sun Y., Wu Y., He C., Wang Y., Jiang X., Li K., Bonardi O., Krishnan A., Boruff J., Rice D., Markham S., Levis B., Azar M., Neupane D., Tasleem A., Yao A., Thombs-Vite I., Agic B., Fahim C., Martin M., Sockalingam S., Turecki G., Beneditti A., Thombs B. Systematic review of mental health symptom changes by sex or gender in early-COVID-19 compared to pre-pandemic. Nature Portfolio. 2022;12 doi: 10.1038/s41598-022-14746-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carbado D., Crenshaw K., Mays V., Tomlinson B. Intersectionality: mapping the movements of a theory. Du. Bois Rev. 2013;10(2):303. doi: 10.1017/S1742058X13000349. https://doi:10.1017/S1742058X13000349 212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Douglas M., Katikireddi S., Taulbut M., McKee M., McCartney G. Mitigating the wider health effects of the covid-19 pandemic response. BMJ. 2020;369(m1557):1–6. doi: 10.1136/bmj.m1557. https://doi: 10.1136/bmj.m1557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fuller-Rowell R., Nichols O., Doan S., Adler-Baeder F., El-Sheikh M. Changes in depressive symptoms, physical symptoms, and sleep-wake problems from before to during the COVID-19 pandemic among emerging adults: inequalities by gender, socioeconomic position, and race. Society for the Study of Emerging Adulthood. 2021;9(5):1–14. doi: 10.1177/21676968211042111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rodriguez-Moreno S., Vázquez J., Roca P., Panadero S. Differences in stressful life events between men and women experiencing homelessness. J. Community Psychol. 2020;49(2):375–389. doi: 10.1002/jcop.22465. https://doi:10.1002/jcop.22465 [DOI] [PubMed] [Google Scholar]
- 14.Scarlett H., Davisse-Paturet C., Longchamps C., El Aarbaoui T., Allaire C., Colleville A., Convence- Arulthas M., Crouzet L., Ducarroz S., Melchior M. Depression during the COVID- 19 pandemic amongst residence of homeless shelters in France. Journal of Affective Disorders Reports. 2021;6:1–8. doi: 10.1016/j.jadr.2021.100243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ndumbe-Eyoh S., Muzumdar P., Betker C., Oickle D. ‘Back to better’: amplifying health equity, and determinants of health perspectives during the COVID-19 pandemic. Global Health Promotion. 2021;28(2):7–16. doi: 10.1177/17579759211000975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Paremoer L., Nandi S., Serag H., Baum F. COVID-19 pandemic and the social determinants of health. 2021. Vol 372(129), pp. 1–5. [DOI] [PMC free article] [PubMed]
- 17.Spiritus-Beerden E., Verelst A., Devleiger I., Primdahl N., Guedes F., Chiarenza A., De Maesschalck S., Durbeej N., Garrido R., Gaspar de Matos M., Ioannidi E., Murphy R., Oulahal R., Osman F., Padilla B., Paloma V., Shedhadeh A., Sturm G., van den Muijsenbergh M., Vasilikou K., Watters C., Willems S., Skovdal M., Derluyn I. Mental Health of refugees and migrants during the covid-19 pandemic: the role of experienced discrimination and daily stressors. Int. J. Environ. Res. Publ. Health. 2021;18(12):1–14. doi: 10.3390/ijerph18126354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kuran C., Morsut C., Kruke B., Krüger M., Segnestam L., Orru K., Naevestad T., Airola M., Keränen J., Gabel F., Hansson S., Torpan S. Vulnerability and vulnerable groups from an intersectionality perspective. Int. J. Disaster Risk Reduc. 2020;50:1–8. doi: 10.1016/j.ijdrr.2020.101826. [DOI] [Google Scholar]
- 19.Orru K., Hansson S., Gabel F., Tammpuu P., Kruger M., Savadori L., Meyer S.F., Torpan S., Jukarainen P., Schieffelers A., Lovasz G., Rhinard M. Approaches to ‘vulnerability’ in eight European disaster management systems. Disasters. 2021;46(3):742–767. doi: 10.1111/disa.12481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Orru K., Klaos M., Nero K., Gabel F., Hansson S., Naevestad T.-O. Imagining and assessing future risks: a dynamic scenario-based social vulnerability analysis framework for disaster planning and response. J. Contingencies Crisis Manag. 2022 doi: 10.1111/1468-5973.12436. [DOI] [Google Scholar]
- 21.Ryan N., El Ayadi A. A call for a gender-responsive, intersectional approach to address COVID-19. 2020;15(9):104–1412. doi: 10.1080/17441692.2020.1791214. [DOI] [PubMed] [Google Scholar]
- 22.Burki T. The indirect impact of COVID-19 on Women. Lancet. 2020;20:904–905. doi: 10.1016/S1473-3099(20)30568-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.European Public Health Alliance Ethnicity as a fundamental cause of health inequity: the case of Roma in Europe during COVID-19. 2021. https://epha.org/ethnicity-as-a- fundamental-cause-of-health-inequity-the-case-of-roma-in-europe-during-covid-19/ Available at:
- 24.Wenham C., Schonard M., Marcuzzo S. The gendered impact of the COVID-19 crisis and post-crisis period. 2020. https://www.europarl.europa.eu/RegData/etudes/STUD/2020/658227/IPOL_STU(2020)658227_EN.pdf Available at:
- 25.Grammatikopoulou M., Gkiouras K., Pepa A., Persnyaki A., Taousani E., Milapidou M., Smyrnakis E., Goulis D. Health status of women affected by homelessness: a cluster of in concreto human rights violations and a time for action. Maturitas. 2021;154:31–45. doi: 10.1016/j.maturitas.2021.09.007. [DOI] [PubMed] [Google Scholar]
- 26.Riley E., Dilworth S., Satre D., Silverberg M., Neilands T., Mangurian C., Weiser S. Factors associated with symptoms of depression and anxiety among women experiencing homelessness and unstable housing during the covid-19 pandemic. JAMA Netw. Open. 2021;4(7):1–4. doi: 10.1001/jamanetworkopen.2021.17035. https://doi:10.1001/jamanetworkopen.2021.17035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Gebhard C., Regitz-Zagrosek V., Neuhauser H., Morgan R., Klein S. Impact of sex and gender on COVID-19 outcomes in Europe. Biol. Sex Differ. 2020;11(29):1–13. doi: 10.1186/s13293-020-00304-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peck J. The disproportionate impact of COVID-19 on women relative to men: a conservation of resources perspective. Feminist Frontiers. 2020;28(s2):484–497. doi: 10.1111/gwao.12597. [DOI] [Google Scholar]
- 29.Zlotnick C., Dryjanksa L., Suckerman S. Factors linked to accessing COVID-19 recommendations among working migrants. Publ. Health Nurs. 2021;39(1):1–9. doi: 10.1111/phn.12982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Breslau N., Chilcoat H., Kessler R., Davis G. Previous exposure to trauma and PTSD effects of subsequent trauma: results from the Detroit area survey of trauma. Am. J. Psychiatr. 1999;156(6):902–907. doi: 10.1176/ajp.156.6.902. [DOI] [PubMed] [Google Scholar]
- 31.Rees S., Fisher J. Covid-19 and the mental health of people with refugee backgrounds. Int. J. Health Serv. 2020;50:415–417. doi: 10.1177/0020731420942475. [DOI] [PubMed] [Google Scholar]
- 32.Mattar S., Piwowarcyzk L. Covid-19 and U.S-based refugee populations: commentary, psychological trauma. Theory, Research, Practice, and Policy. 2020;12:S228–S229. doi: 10.1037/tra0000602. [DOI] [PubMed] [Google Scholar]
- 33.Busch-Geertsema V., Culhane D., Fitzpatrick S. Developing a global framework for conceptualising and measuring homelessness. Habitat Int. 2016;55:124–132. doi: 10.1016/j.habitatint.2016.03.004. [DOI] [Google Scholar]
- 34.Nikoo N., Motamed M., Nikoo M., Neilson E., Saddicha S., Krausz M. Chronic physical health conditions among homeless. Journal of Health Disparities Research and Practice. 2015;8(1):81–97. [Google Scholar]
- 35.Van der Geest K., Schindler M. United Nations University Institute for Environment and Human Security; 2017. Handbook for Assessing Loss and Damage in Vulnerable Communities. [Google Scholar]
- 36.Andrew A., Cattan S., Costa Dias M., Farquharson C., Kraftman L., Krutikova S., Phimister A., Sevilla A. How are mothers and fathers balancing work and family under lockdown? 2020. https://ifs.org.uk/publications/14860 Available at: [DOI] [PMC free article] [PubMed]
- 37.Xiong J., Lipsitz O., Nasri F., Lui L., Gill H., Phan L., Chen-Li D., Iacobucci M., Ho R., Majeed A., McIntyre R. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 2020;277:55–64. doi: 10.1016/j.jad.2020.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fisher A., Ryan M. Gender inequalities during COVID-19. Group Process. Intergr. Relat. 2021;24(2):237–245. doi: 10.1177/1368430220984248. [DOI] [Google Scholar]
- 39.Olff M. Sex and gender differences in post-traumatic stress disorder: an update. Eur. J. Psychotraumatol. 2017;8(4) doi: 10.1080/20008198.2017.1351204. [DOI] [Google Scholar]
- 40.Orru K., Nero K., Nævestad T.-O., Schieffelers A., Olson A., Airola M., Kazemekaityte A., Lovasz G., Scurci G., Ludvigsen J., de los Rios Pérez D.A. Resilience in care organisations: challenges in maintaining support for vulnerable people in Europe during the Covid-19 pandemic. Disasters. 2021;45(S1) doi: 10.1111/disa.12526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Soh H., Ho R., Ho C., Tam W. Efficacy of digital cognitive behavioural therapy for insomnia: a meta-analysis of randomised controlled trials. Sleep Med. 2020;75:315–325. doi: 10.1016/j.sleep.2020.08.020. [DOI] [PubMed] [Google Scholar]
- 42.Zhang M., Ho R. Moodle: the cost-effective solution for internet cognitive behavioral therapy (I-CBT) interventions. Technol. Health Care. 2017;25(1):163–165. doi: 10.3233/THC-161261. [DOI] [PubMed] [Google Scholar]
- 43.Milaney K., Williams N., Lockerbie S.L., et al. Recognizing and responding to women experiencing homelessness with gendered and trauma-informed care. BMC Publ. Health. 2020;20:397. doi: 10.1186/s12889-020-8353-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Husain S., Tang T.B., Yu R., Tam W., W, Tran B., Quek T., Hwang S., Chang C., Ho C., Ho R. Cortical haemodynamic response measured by functional near infrared spectroscopy during a verbal fluency task in patients with major depression and borderline personality disorder. EBioMedicine. 2021;66 doi: 10.1016/j.ebiom.2019.11.047. Https://doi:10.1016/j.ebiom.2019.11.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Husain S., Yu R., Tang T.B., Tam W., W, Tran B., Quek T., T, Hwang S., Chang C., Ho C., Ho R. Validating a functional near-infrared spectroscopy diagnostic paradigm for Major Depressive Disorder. Sci. Rep. 2020;10(1):9740. doi: 10.1038/s41598-020-66784-2. Https://doi:10.1038/s41598-020-66784-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Ho C., Lim L., Lim A., Chan N., Tan R., Lee S., Ho R. Diagnostic and predictive applications of functional near-infrared spectroscopy for major depressive disorder: a systematic review. Front. Psychiatr. 2020;11:378. doi: 10.3389/fpsyt.2020.00378. https://doi:10.3389/fpsyt.2020.00378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Figueroa C.A., Luo T., Aguilera A., Lyles C.R. The need for feminist intersectionality in digital health. The Lancet Digital Health. 2021;3(8):e526–e533. doi: 10.1016/S2589-7500(21)00118-7. [DOI] [PubMed] [Google Scholar]
- 48.Cabezas-Rodríguez A., Utzet M., Bacigalupe A. Which are the intermediate determinants of gender inequalities in mental health?: a scoping review. Int. J. Soc. Psychiatr. 2021;67(8):1005–1025. doi: 10.1177/00207640211015708. [DOI] [PubMed] [Google Scholar]
- 49.Lim G., Tam W., Lu Y., Ho C., Zhang M., Ho R. Prevalence of depression in the community from 30 countries between 1994 and 2014. Sci. Rep. 2018;8:2861. doi: 10.1038/s41598-018-21243-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that has been used is confidential.