Abstract
Purpose:
Home health agencies delivering care in rural counties face unique challenges when providing care to older adults; long travel times between each visit can limit the number of patients seen each day. In 2010, Medicare began paying home health (HH) providers 3% more to serve rural beneficiaries without evaluating the policy’s impact on patient outcomes.
Methods:
Using 100% Medicare data on postacute HH episodes from 2007 to 2014, we estimated the impact of higher payments on beneficiaries outcomes using difference-in-differences analysis, comparing rehospitalizations between rural and urban postacute HH episodes before and after 2010.
Findings:
Our sample included 5.6 million postacute HH episodes (18% rural). In the preperiod, the 30- and 60-day rehospitalization rates for urban HH episodes were 11.30% and 18.23% compared to 11.38% and 18.39% for rural HH episodes. After 2010, 30- and 60-day rehospitalization rates declined, 10.08% and 16.49% for urban HH episodes and 9.87% and 16.08% for rural HH episodes, respectively. The difference-in-difference estimate was 0.29 percentage points (P = .005) and 0.57 percentage points (P < .001) for 30- and 60-day rehospitalization, respectively.
Conclusions:
Increasing payments resulted in a statistically significant reduction in rehospitalizations for rural postacute HH episodes. The add-on payment is set to sunset in 2022 and its impact on access and quality to HH for rural older adults should be reconsidered.
Keywords: home care services, Medicare, postacute care, rehospitalization, rural health
INTRODUCTION
Home health (HH) care has grown substantially in the last 2 decades, increasing from 3.9 to 6.6 million episodes.1 Under Traditional Medicare, beneficiaries who are certified homebound and need intermittent skilled care are eligible to receive HH. About 30% of Medicare beneficiaries who are hospitalized are referred to HH2 and among postacute care settings, HH has the largest geographic variation.3 For low-acuity patients, it is seen as a lower-cost alternative to skilled nursing facilities, but it may have higher rehospitalization rates.4
Home health agencies (HHAs) delivering care in rural counties face unique challenges. Travel times between each visit can be long which limits the number of patients seen each day and increases the marginal cost of visits.5,6 Research on urban-rural differences in postacute care finds that rural patients use less HH care.7–10 Although HHAs in rural counties are more likely to have timely initiation of services,11 they are more likely to have emergency department visits compared to urban ones.12 Two previous studies on rehospitalization among HH patients with heart failure had mixed findings; rural areas had lower 30-day rehospitalizations compared to urban areas,13 and conversely that geography had relatively little influence on rehospitalizations.14 Research focused on Medicare beneficiaries with rehabilitation-sensitive conditions found that agencies in rural counties were more likely to have beneficiaries be hospitalized during the episode.15
From October 2000 through December 2019, Medicare has used a prospective payment system that pays HHAs a predetermined average rate for each 60-day episode. In January 2020, the system changed to a 30-day episode, known as the Patient-Driven Groupings Model. These payment rates are based on patients’ conditions, service use, and adjusted based on geographic factors to reflect differences in area wages. In addition to these factors, Medicare has used temporary payment adjusters to increase payments for HH episodes that occur in rural counties, known as the rural add-on payment. The rural add-on payment adjuster was first introduced in April 2001, paying rural episodes 10% higher rates for 2 years. Since then, it has been reintroduced through several laws on a temporary basis at lower rates: Medicare Prescription Drug, Improvement, and Modernization Act, 5% from April 2004 to March 2005; Deficit Reduction Act, 5% from January 2006 to December 2006; Affordable Care Act, 3% from April 2010 to December 2016; Medicare Access and CHIP Reauthorization Act of 2015, 3% from January to December 2017; Bipartisan Budget Act of 2018, 3% from January to December 2018; and Bipartisan Budget Act of 2018, 0%-4% based on population density and HH utilization that is phased out over 2–4 years.
Few studies have examined the rural add-on payment impact on access to HH and so far, none have examined its impact on outcomes. Using data from 2002 to 2017, researchers found that the supply of HH in rural areas was similar to those in adjacent urban counties, and only the higher add-on payments (5%+) yielded changes in rural HH supply commensurate with urban counties not adjacent to rural counties.16 Other research examining the 3% increase following the Affordable Care Act indicates that HH care utilization relative to nursing home care increased minimally in rural counties compared to urban counties following the HH payment add-on but also experienced a decrease in visits once using HH.17
This study fills those gaps by comparing 30- and 60-day hospitalization rates for rural versus urban patients using postacute HH, before and after the April 2010 reinstitution of the 3% add-on payment. Centers for Medicare and Medicaid Services (CMS) has prioritized reducing rehospitalizations through various initiatives, such as the Hospital Readmission Reduction Program, which incentivized hospitals to reduce their readmission rates. These findings should have implications for the 2022 sunset of the rural add-on payments.
METHODS
Data sources
We used data from 2007 to 2015. Medicare administrative data included 100% Medicare inpatient claims, HH claims, Provider of Service file, Medicare Beneficiary Summary File and Chronic Condition Data Warehouse, the residential history file,18 and Area-Health Resource File. We obtained enrollment in Fee-for-service (FFS) Medicare from the Medicare Beneficiary Summary File.
Sample
The study population included Medicare FFS beneficiaries with a postacute HH episode after an inpatient hospitalization from 2007 to 2014. We excluded Medicare Advantage beneficiaries because the payment policy did not apply to those beneficiaries and their claims are not available in the Medicare FFS data files. To be consistent with the CMS measure for rehospitalizations, we also excluded the following HH episodes: (1) if there was no index hospitalization within 5 days prior to HHA admission; (2) if the patient received treatment in another setting in between (eg, skilled nursing facility); (3) if the episode was a low-utilization stay (less than 4 visits over the episode); and (4) if the patient was transferred to another HHA. To enter the analytic file for the study, patients needed to have an index hospital stay, defined as a hospital discharge within 5 days of entering HH care. The hospital discharge date was derived from the inpatient claims and matched within 5 days of the “from” date on the HH claim.
Variables
Our primary outcome was rehospitalizations measured as a dichotomous variable in the 30 and 60 days after HH admission (through February 2015 for HH episodes starting in 2014).
The main interaction of interest is between rural residence and an indicator that the policy was in effect when the HH episode began (starting in April 2010). Rural residence was determined using the county code on the Medicare Beneficiary Summary File. We followed the definition CMS used for determining qualification for the add-on payment at the time, if the county was in a core-based statistical area defined by the Office of Management and Budget it was determined to be urban, if it was not in a core-based statistical area, the county was considered rural (as defined in section 1886(d)(2)(D) of the Social Security Act).
We used the Area-Health Resource File for county-level characteristics related to the demand for HH (population 85 years or older per 100,000 and nursing facilities per 100,000). We used provider of Service files and HH claims to identify the profit status of the HHA (nonprofit, for-profit, and governmental), how long they were certified under Medicare (less than 5 years, 5–9 years, 10–19 years, 20 or more years), and HHA size measured by the number of visits provided in a calendar year (less than 5,000 visits, 5,000–9,999, 10,000–29,999, and 30,000 and more). We included the following patient characteristics from the Medicare Beneficiary Summary File: age, sex, race/ethnicity, and Medicare/Medicaid dual eligibility status. Clinical characteristics included chronic conditions which were taken from the Chronic Conditions Segment: asthma, arthritis, chronic heart failure, chronic kidney disease, a chronic obstructive pulmonary disorder, depression, diabetes, hypertension, ischemic heart disease, and Alzheimer’s disease. We did not include the diagnosis-related grouper of the inpatient hospitalization due to different coding incentives between critical access hospitals and prospective payment hospitals.19 We also did not include any variables regarding HH resource intensity (eg, number of visits) as that could be directly impacted by early rehospitalization.
Statistical analysis
We examine the impact of the rural add-on payment using a difference-in-differences framework. An assumption of the difference-in-differences methodology is that there are parallel trends between the 2 groups being compared, rural and urban. We assess these assumptions by plotting the outcomes quarterly by rurality visually in a line plot. We additionally conduct a placebo test, restricting our data to only the preperiod and run the same regressions using fake treatment dates. If there are no pretrends, we expect the coefficients on our fake interaction terms to not be statistically significant. We use a linear probability model to compare rehospitalizations between rural and urban beneficiaries admitted to an HHA before (January 2007-March 2010) and after (April 2010-December 2014) the policy was implemented. We computed the marginal effects that can be interpreted as percentage point differences in the probability of being rehospitalized within 30 and 60 days. We used state-fixed effects to account for differences in state Medicaid programs that may impact the long-term care landscape and use standard errors clustered at the state level. We considered P-values less than .05 to be statistically significant.
Sensitivity analysis
We conducted several sensitivity analyses to test the robustness of our results. First, we conducted a sensitivity analysis regarding the use of state-fixed effects. Since rural counties within a state can vary widely, we conducted an additional analysis using county-fixed effects and omitting the rural indicator variable. Second, we conducted a sensitivity analysis using HHA fixed effects, omitting the agency characteristics. Last, we conducted a sensitivity analysis around the postperiod due to overlap with the Hospital Readmissions Reduction Policy that began in October 2012. We shortened the postperiod to HH episodes admitted between April 1, 2010 through September 1, 2012 for 30-day rehospitalizations and April 1, 2010 through August 1, 2012 for 60-day hospitalizations.
RESULTS
There were 5,447,428 postacute HH episodes between January 2007 and December 2014; 2,225,918 in the preperiod and 3,221,510 in the postperiod (Table 1). Around 18% of the sample was rural (n = 988,921). Compared to rural patients, urban patients were slightly older (79.4 vs 78.5 years old), less white (81.7% vs 89.9%), less likely to be dually eligible for Medicaid (19.0% vs 22.9%), and less likely to be cared for by a government HHA (2.6% vs 13.0%). Over the study period, the proportion of both rural and urban beneficiaries who are dually eligible for Medicaid decreased (24% in 2007, 21% in 2014 for rural beneficiaries; 19% in 2007, 17% in 2014 for urban beneficiaries).
TABLE 1.
Descriptive characteristics by rurality
| Urban | Rural | ||
|---|---|---|---|
| Number of home health episodes | 4,458,507 | 988,921 | |
| Patient characteristics | P-value | ||
| Age, Mean (SD) | 79.4 (8.1) | 78.5 (7.9) | <.001 |
| Female (%) | 61.6 | 61.1 | <.001 |
| Race/ethnicity (%) | <.001 | ||
| Non-Hispanic White | 81.7 | 89.9 | |
| Black | 9.5 | 6.4 | |
| Hispanic | 5.8 | 2.2 | |
| Other | 3.0 | 1.5 | |
| Medicaid dual-eligible (%) | 19.0 | 22.9 | <.001 |
| Chronic conditions (%) | |||
| Arthritis | 58.2 | 59.4 | <.001 |
| Asthma | 12.7 | 10.7 | <.001 |
| CHF | 43.4 | 43.0 | <.001 |
| Kidney | 38.4 | 34.6 | <.001 |
| COPD | 31.8 | 35.0 | <.001 |
| Depression | 25.7 | 25.4 | <.001 |
| Diabetes | 41.3 | 39.2 | <.001 |
| Hypertension | 89.9 | 88.7 | <.001 |
| Ischemic heart disease | 60.1 | 57.2 | <.001 |
| Alzheimer’s disease | 9.6 | 7.6 | <.001 |
| Agency characteristics | |||
| Profit status (%) | <.001 | ||
| Nonprofit | 48.6 | 43.3 | |
| Proprietary | 48.8 | 43.7 | |
| Government | 2.6 | 13.0 | |
| Medicare tenure (%) | <.001 | ||
| Less than 5 years | 7.2 | 3.3 | |
| 5–10 years | 9.4 | 5.3 | |
| 10–20 years | 21.5 | 23.0 | |
| 20+ years | 61.8 | 68.4 | |
| Agency size (%) | <.001 | ||
| Less than 5,000 visits | 5.6 | 15.4 | |
| 5,000–9,999 visits | 11.1 | 21.0 | |
| 10,000–29,000 visits | 36.5 | 36.2 | |
| 30,000 visits | 46.8 | 27.4 | |
Note: P-value from t-test for continuous variables and chi-squared values for categorical variables.
Abbreviations: CHF: congestive heart failure; COPD: chronic obstructive pulmonary disease; SD: standard deviation.
The unadjusted trends in 30- and 60-day rehospitalization rates by quarter are shown in Figure 1, Panels A and B respectively, with a reference line where the add-on payment was instituted. Visually, the urban and rural hospitalization rates are similar, with seasonal upticks at the end of the year. Additionally, we conducted a placebo test using the restricted sample of data from before the policy (2007–2009; n = 2,047,908) and estimated the regression using a fake policy date of January 2008 (fake prepolicy year of 2007) and January 2009 (fake prepolicy years of 2007 and 2008). These placebo test regressions yielded P-values of .093 and .082, respectively, more evidence to support the parallel trends assumption.
FIGURE 1.
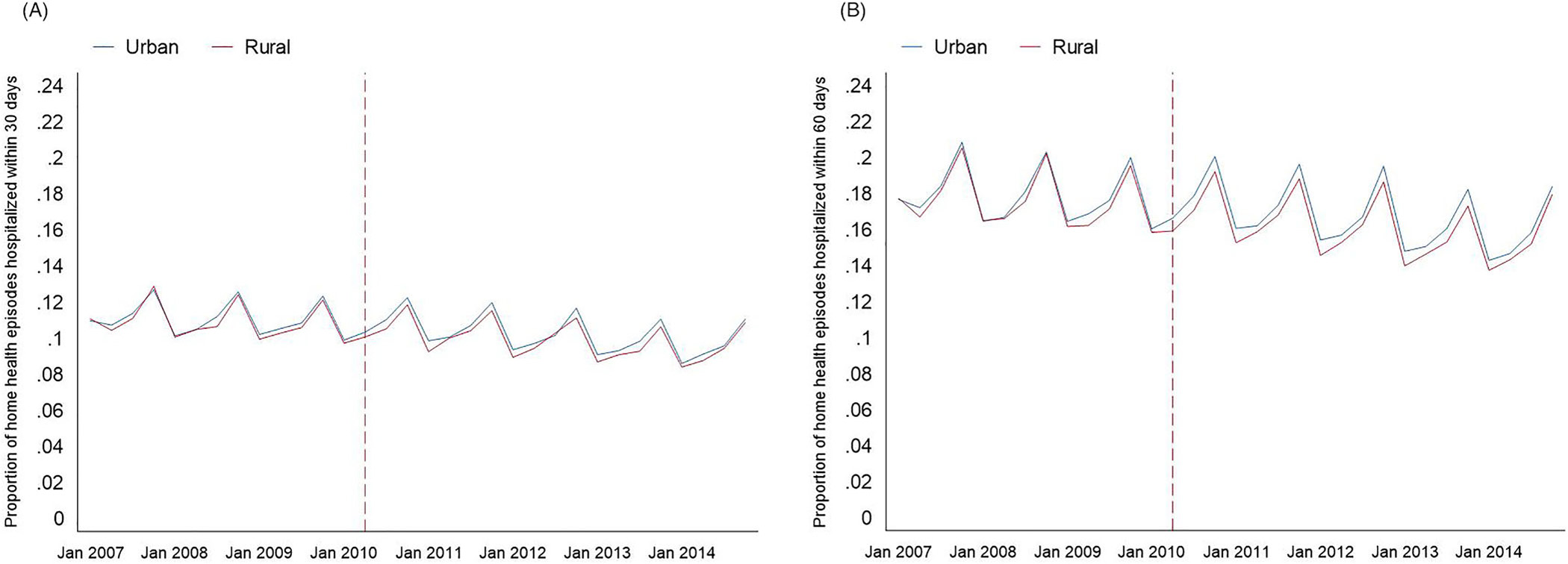
Unadjusted trends in outcomes by rurality.
Notes: The reference line is at April 2010, where the 3% rural add-on payment was implemented. Data are plotted quarterly.
The pooled 30-day unadjusted rehospitalization rate was 10.57% (n = 575,675). In multivariate adjusted results, 11.30% of urban beneficiaries were rehospitalized within 30 days in the preperiod compared to 11.41% of rural beneficiaries. After the policy was implemented, there was a decline for both rural and urban beneficiaries, 30-day rehospitalization rates decreased to 10.08% for urban beneficiaries (1.22 percentage point decline) and 9.88% for rural beneficiaries (1.52 percentage point decline), yielding a difference-in-difference estimate of 0.30 percentage point reduction in 30-day rehospitalization (P = .004), or a relative reduction of 2.9%, associated with the rural add-on payment policy (Table 2). The pooled 60-day rehospitalization rate was 17.17% (n = 935,586). In multivariate adjusted results, 18.24% of urban beneficiaries were rehospitalized within 60 days in the preperiod compared to 18.41% of rural beneficiaries. In the postperiod, there was a decline for both, 16.49% for urban beneficiaries (1.74 percentage point decline) and 16.08% for rural beneficiaries (2.32 percentage point decline). This yielded a difference-in-difference estimate of 0.58 percentage point reduction in 60-day rehospitalization (P < .001), or a relative reduction of 3.4%.
TABLE 2.
Multivariate regression results
| 30-day rehospitalization |
60-day rehospitalization |
|||
|---|---|---|---|---|
| N= | 5,447,346 |
5,447,346 |
||
| Outcome | Percentage point | [95% CI] | Percentage point | [95% CI] |
| Rural | 0.10 | [−0.09, 0.29] | 0.17 | [−0.11, 0.45] |
| Post-Policy | −1.22*** | [−1.35, −1.09] | −1.74*** | [−1.95, −1.53] |
| Rural*Post-Policy | −0.30** | [−0.50, −0.10] | −0.58*** | [−0.88, −0.28] |
| Patient characteristics | ||||
| Age | −0.05*** | [−0.05, −0.04] | −0.04*** | [−0.05, −0.03] |
| Male | Ref. | Ref. | ||
| Female | −0.21*** | [−0.28, −0.15] | −0.36*** | [−0.44, −0.29] |
| Race/ethnicity | ||||
| Non-Hispanic White | Ref. | Ref. | ||
| Black | 0.22 | [−0.00, 0.43] | 0.78*** | [0.44, 1.11] |
| Hispanic | 0.11 | [−0.32, 0.53] | 0.02 | [−0.69, 0.74] |
| Other | −0.23 | [−0.52, 0.06] | −0.54 | [−1.12, 0.04] |
| Nondual eligible | Ref. | Ref. | ||
| Medicaid dual eligible | 0.90*** | [0.73, 1.07] | 1.84*** | [1.57, 2.12] |
| Chronic conditions | ||||
| Arthritis | −0.33*** | [−0.45, −0.21] | −0.23* | [−0.42, −0.03] |
| Asthma | 1.15*** | [1.01, 1.29] | 1.87*** | [1.67, 2.06] |
| CHF | 4.56*** | [4.39, 4.72] | 7.32*** | [7.10, 7.53] |
| Kidney | 5.75*** | [5.59, 5.91] | 8.68*** | [8.42, 8.93] |
| COPD | 3.39*** | [3.29, 3.50] | 5.68*** | [5.52, 5.83] |
| Depression | 3.10*** | [2.98, 3.23] | 5.04*** | [4.83, 5.24] |
| Diabetes | 0.68*** | [0.58, 0.77] | 1.27*** | [1.15, 1.39] |
| Hypertension | 0.76*** | [0.66, 0.86] | 1.02*** | [0.83, 1.20] |
| Ischemic heart disease | 1.83*** | [1.70, 1.96] | 2.95*** | [2.79, 3.11] |
| Stroke | 3.12*** | [3.01, 3.23] | 5.37*** | [5.23, 5.50] |
| Alzheimer’s disease | 1.04*** | [0.94, 1.14] | 2.23*** | [2.09, 2.37] |
| Agency profit-status | ||||
| Nonprofit | Ref. | Ref. | ||
| Proprietary | −0.24*** | [−0.37, −0.11] | −0.25** | [−0.43, −0.07] |
| Government | 0.13 | [−0.05, 0.32] | 0.27* | [0.01, 0.53] |
| Medicare tenure | ||||
| Less than 5 years | Ref. | Ref. | ||
| 5–10 years | −0.08 | [−0.23, 0.07] | −0.20 | [−0.42, 0.03] |
| 10–20 years | −0.09 | [−0.22, 0.05] | −0.14 | [−0.40, 0.12] |
| 20+ years | 0.09 | [−0.09, 0.27] | 0.05 | [−0.25, 0.36] |
| Agency size | ||||
| Less than 5,000 visits | Ref. | Ref. | ||
| 5,000–9,999 visits | 0.00 | [−0.13, 0.13] | −0.01 | [−0.18, 0.16] |
| 10,000–29,000 visits | 0.05 | [−0.07, 0.17] | −0.03 | [−0.19, 0.12] |
| 30,000 visits | 0.11 | [−0.05, 0.26] | 0.03 | [−0.14, 0.21] |
Notes: Regressions also controlled for county characteristics and state-fixed effects. Standard errors are clustered at the county level.
Abbreviations: CHF, chronic heart failure; COPD, chronic obstructive disease.
p < 0.05
p < 0.01
p < 0.001.
Sensitivity analysis results
The main results using county-fixed effects instead of stated-fixed effects were robust: the difference-in-difference estimate is a 0.36 percentage point reduction in 30-day rehospitalization (P < .001) and 0.66 percentage point reduction in 60-day rehospitalization (P < .001) (online Table A1). The main results using agency fixed effects were also robust: the difference-in-difference estimate is a 0.31 percentage point reduction in 30-day rehospitalization (P = .001) and 0.62 percentage point reduction in 60-day rehospitalization (P < .001) (online Table A2).
In the sensitivity analysis with a shortened postperiod to disentangle the effect of the rural add-on payment for HH and the Hospital Readmission Reduction Program, the sample size examining 30-day rehospitalizations was reduced to 3,868,285 HH episodes and 3,813,074 HH episodes for 60-day rehospitalizations (online Table A3). When examining 30-day rehospitalization rates in the multivariate-adjusted analysis, we found a smaller difference-in-difference estimate, 0.20 percentage point, that was no longer statistically significant at conventional levels (P = .051). In the multivariate-adjusted analysis examining 60-day rehospitalization rates, we found a smaller difference-in-difference estimate, 0.45 percentage point, that remained statistically significant (P = .004).
DISCUSSION
This paper provides the first formal examination of the rural add-on payment on beneficiary outcomes for those receiving postacute HH. In this difference-in-difference analysis, we examined the impact of higher payments for HH episodes in rural counties on rehospitalization rates. After the policy was implemented, we found a 3% relative reduction in rehospitalizations for HH patients residing in rural areas compared to urban areas. Our findings were robust to alternative specifications.
The magnitude of the reductions in rehospitalization rates attributable to the payment change was small, roughly a 3% decline. The 3% payment increase is across all rural HH services and the cost savings of less rehospitalizations may not fully compensate for the additional costs. However, there are other benefits beyond avoiding rehospitalizations that are not captured in this study. Those benefits are more difficult to measure, such as better function and a lower burden on family members.20 Finally, the 3% higher payments may help some rural HH providers stay financially viable and not have to close and leave those communities without HH.
The most recent iteration of the rural add-on payment expires at the end of 2022. However, the add-on payment has been decreased by 0.5 percentage points each year since 2019 and adjusted the starting percent (2% vs 4%) of the add-on payment depending on the high/low utilization and high/low population density of the county. The targeted lower add-on payments likely yield differential and more tempered responses from HHAs than the 3% payments examined in this study.
Extending the findings from this study to the current or future iterations of the rural add-on payment should be done cautiously in consideration of many ongoing payment changes to the HH industry (eg, Home Health Value-Based Purchasing Model and Patient-Driven Groupings Model) and the impact of the COVID-19 pandemic. Future research on the targeted rural add-on payments will need to take into account the major overhaul of the HH prospective payment system, Patient Driving Groupings Model, implemented in 2020, which changed the payments to 30-day from 60-day increments and differential payments based on entry (community or institution). Additionally, the Home Health Value-Based Purchasing Model is going to be nationally rolled out with the calendar year 2022 as the preimplementation year and 2023 as the performance year. HHAs will face a 5% payment adjustment, upward or downward, based on their quality performance. Finally, the entire health care industry, including HH, has been impacted by the COVID-19 pandemic. HHAs face many challenges including but not limited to staffing issues, decreased referrals, and personal protection equipment costs.21
This study has several limitations. First, we only focused on postacute HH episodes, but a growing number of HH episodes are not preceded by a hospital stay. The rural add-on payment was not restricted to postacute episodes, and the 60-day rehospitalization measure being reported as part of the HH quality reporting program will include all HH episodes. Second, although rehospitalizations are a national priority, there could be other benefits to these higher payments that are not easily measurable through administrative claims data. Third, we specified rurality at the county level using the same methods that CMS uses to attribute rurality for the rural add-on payments, but this simplifies urban-rural status and does not account for intracounty variation, adjacency to urban counties, or level of rurality. Finally, we excluded Medicare beneficiaries that were enrolled in Medicare Advantage as the payment policy did not apply to them. However, over this time period, the rates of enrollment in Medicare Advantage grew tremendously, from 19% in 2007 to 31% in 2014.22 Since Medicare Advantage enrollees are noted to be favorably selected compared to Traditional Medicare enrollment, the sample of those using postacute HH may have become less healthy over time. However, the favorable risk has decreased over time,23 and we control for health chronic health conditions in our regression analysis.
Despite these limitations, this is one of the first studies to examine how higher payments for HH episodes in rural counties can reduce rehospitalizations. We found a 3% higher payment was associated with a relative reduction in rehospitalizations among rural HH recipients by 3%. As the HH rural add-on payments sunset in the context of major changes to the HH prospective payment system, rural HH outcomes should be continually monitored.
Supplementary Material
Funding information
Funding for this work was supported by the Agency for Healthcare Research and Quality, Grant/Award Number: 1R36HS027054–01
Footnotes
DISCLOSURES
VM is independently compensated as Chair of the Scientific Advisory Committee for naviHealth, a postacute care convener serving Medicare Advantage plans and health systems managing postacute care, including in home health agencies. There are no other potential competing interests.
SUPPORTING INFORMATION
Additional supporting information can be found online in the Supporting Information section at the end of this article.
REFERENCES
- 1.Medicare Payment Advisory Commission. Report to Congress: Medicare Payment Policy. 2018. Accessed January 10, 2022. https://www.medpac.gov/wp-content/uploads/import_data/scrape_files/docs/default-source/reports/mar18_medpac_ch9_sec_rev_0518.pdf
- 2.Jones CD, Wald HL, Boxer RS, et al. Characteristics associated with home health care referrals at hospital discharge: results from the 2012 National Inpatient Sample. Health Serv Res. 2017;52(2):879–894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Li Q, Rahman M, Gozalo P, Keohane LM, Gold MR, Trivedi AN. Regional variations: the use of hospitals, home health, and skilled nursing in traditional Medicare and Medicare advantage. Health Aff. 2018;37(8):1274–1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Werner RM, Coe NB, Qi M, Konetzka RT. Patient outcomes after hospital discharge to home with home health care vs to a skilled nursing facility. JAMA Intern Med. 2019;179(5):617–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Probst J, Eberth JM, Crouch E. Structural urbanism contributes to poorer health outcomes for rural America. Health Aff. 2019;38(12):1976–1984. [DOI] [PubMed] [Google Scholar]
- 6.Skillman S, Patterson D, Coulthard C, Mroz TM. Access to Rural Home Health Services: Views from the Field. 2016. Accessed January 10, 2022. https://depts.washington.edu/fammed/rhrc/wp-content/uploads/sites/4/2016/02/RHRC_FR152_Skillman.pdf
- 7.Burke RE, Jones CD, Coleman EA, Falvey JR, Stevens-Lapsley JE, Ginde AA. Use of post-acute care after hospital discharge in urban and rural hospitals. Am J Accountable Care. 2017;5(1):16–22. [PMC free article] [PubMed] [Google Scholar]
- 8.Hartman L, Jarosek SL, Virnig BA, Durham S. Medicare-certified home health care: urban-rural differences in utilization. J Rural Health. 2007;23(3):254–257. [DOI] [PubMed] [Google Scholar]
- 9.Kenney GM. Is access to home health care a problem in rural areas? Am J Public Health. 1993;83(3):412–414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kosar CM, Loomer L, Ferdows NB, Trivedi AN, Panagiotou OA, Rahman M. Assessment of rural-urban differences in postacute care utilization and outcomes among older US adults. JAMA Netw Open. 2020;3(1):e1918738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ma C, Devoti A, O’Connor M. Rural and urban disparities in quality of home health care: a longitudinal cohort study (2014–2018). J Rural Health. 2022;38:705–712. [DOI] [PubMed] [Google Scholar]
- 12.Chen HF, Landes RD, Schuldt RF, Tilford JM. Quality performance of rural and urban home health agencies: implications for rural add-on payment policies. J Rural Health. 2020;36(3):423–432. [DOI] [PubMed] [Google Scholar]
- 13.Chen HF, Carlson E, Popoola T, Suzuki S. The impact of rurality on 30-day preventable readmission, illness severity, and risk of mortality for heart failure Medicare home health beneficiaries. J Rural Health. 2016;32(2):176–187. [DOI] [PubMed] [Google Scholar]
- 14.Madigan EA, Gordon NH, Fortinsky RH, Koroukian SM, Piña I, Riggs JS. Rehospitalization in a national population of home health care patients with heart failure. Health Serv Res. 2012;47(6):2316–2338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Mroz TM, Meadow A, Colantuoni E, Leff B, Wolff JL. Home health agency characteristics and quality outcomes for Medicare beneficiaries with rehabilitation-sensitive conditions. Arch Phys Med Rehabil. 2018;99(6):1090–1098.e4. [DOI] [PubMed] [Google Scholar]
- 16.Mroz TM, Patterson DG, Frogner BK. The impact of Medicare’s rural add-on payments on supply of home health agencies serving rural counties. Health Aff. 2020;39(6):949–957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Loomer L, Rahman M, Mroz TM, Gozalo PL, Mor V. Do higher payments increase access to post-acute home health care for rural Medicare beneficiaries? J Am Geriatr Soc. 2020;68(3):663–664. [DOI] [PubMed] [Google Scholar]
- 18.Intrator O, Hiris J, Berg K, Miller SC, Mor V. The residential history file: studying nursing home residents’ long-term care histories(*). Health Serv Res. 2011;46(1 Pt 1):120–137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kosar CM, Loomer L, Thomas KS, White EM, Panagiotou OA, Rahman M. Association of diagnosis coding with differences in risk-adjusted short-term mortality between critical access and non-critical access hospitals. JAMA. 2020;324(5):481–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Golberstein E, Grabowski DC, Langa KM, Chernew ME. Effect of Medicare home health care payment on informal care. Inquiry. 2009;46(1):58–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jones CD, Bowles KH. Emerging challenges and opportunities for home health care in the time of COVID-19. J Am Med Dir Assoc. 2020;21(11):1517–1518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Freed M, Damico A. Medicare Advantage in 2022: Enrollment Update and Key Trends. KFF; 2022. Accessed September 21, 2022. https://www.kff.org/medicare/issue-brief/medicare-advantage-in-2022-enrollment-update-and-key-trends/ [Google Scholar]
- 23.McWilliams JM, Hsu J, Newhouse JP. New risk-adjustment system was associated with reduced favorable selection in Medicare advantage. Health Aff. 2012;31(12):2630–2640. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


