Abstract
As a member state of the International Health Regulations 2005, Cambodia is continuously strengthening its capacity to respond to health emergencies and prevent the international spread of diseases. Despite this, Cambodia’s capacity to prevent, detect and rapidly respond to public health threats remained limited at the onset of the pandemic, as was the case in most countries. This paper describes epidemiological phases, response phases, strategy and lessons learnt in Cambodia between 27 January 2020 and 30 June 2022. We classified epidemiological phases in Cambodia into three phases, in which Cambodia responded using eight measures: (1) detect, isolate/quarantine; (2) face coverings, hand hygiene and physical distancing measures; (3) risk communication and community engagement; (4) school closures; (5) border closures; (6) public event and gathering cancellation; (7) vaccination; and (8) lockdown. The measures corresponded to six strategies: (1) setting up and managing a new response system, (2) containing the spread with early response, (3) strengthening the identification of cases and contacts, (4) strengthening care for patients with COVID-19, (5) boosting vaccination coverage and (6) supporting disadvantaged groups. Thirteen lessons were learnt for future health emergency responses. Findings suggest that Cambodia successfully contained the spread of SARS-CoV-2 in the first year and quickly attained high vaccine coverage by the second year of the response. The core of this success was the strong political will and high level of cooperation from the public. However, Cambodia needs to further improve its infrastructure for quarantining and isolating cases and close contacts and laboratory capacity for future health emergencies.
Keywords: COVID-19, epidemiology, public health
Summary box.
COVID-19 spread globally, but how the pandemic played out in each country depended on various factors, including government responses and the general public’s adherence to COVID-19 measures.
Early response—Early detection, Early isolation, Early contact tracing, Early treatment and Early engagement—is the core of successful SARS-CoV-2 containment.
Achieving high vaccination coverage correlates with a decline in the number of deaths and leads to eventual full reopening of the country.
Responding to the pandemic requires decisive leadership and good governance, which refers to decisions being made quickly, in a timely manner, and without delay.
High level of cooperation from the public is a fundamental factor for success in containing the spread in the early phase; in the later stage, the massively successful vaccination campaign was also a large contributing factor.
Introduction
Starting in early 2020, COVID-19 spread globally. However, how the epidemic played out in each country depended on various factors, including the government responses and the general public’s adherence to COVID-19 measures.1
Cambodia’s health system has significantly improved in the last three decades contributing to a rise in life expectancy.2 However, its readiness in responding to a health emergency was still limited at the onset of the pandemic. In 2014, WHO estimated that Cambodia had only 0.2 physicians per 1000 population.3 4 The ratio of hospital beds was also low at 0.9 per 1000 population.4 5 There was limited infrastructure for isolation of patients with highly infectious diseases.
As a member state of the International Health Regulation (IHR) 2005, Cambodia committed to implementing the IHR’s framework and continuously strengthening its capacity to respond to health emergencies, including outbreaks. In spite of this, the Joint External Evaluation by the IHR—a process of evaluating a country’s capacity to prevent, detect and rapidly respond to public health threats—indicated that Cambodia had limited capacity in 2016.6
Cambodia became a member state of the IHR in 2007.7 The Cambodian Communicable Disease Control Department (CCDC) serves as the focal institute in Cambodia’s commitment to fully implementing the IHR framework.7 CCDC established a rapid response team (RRT) network with over 2000 members deployed in provincial health departments and operational district offices nationwide.8 9 CCDC has a national surveillance system called ‘Cambodia Early Warning System (CamEWARN)’ which collected and aggregated data of seven epidemic-prone diseases from all public hospitals and health centres in Cambodia.10 In 2016, CamEWARN introduced the hotline 115 system as an extension to provide a platform for health centres to report suspected or notifiable cases under surveillance. A standard operating procedure for health emergencies, the ‘Cambodian Emergency Operations Centre and Incident Management System Standard Operating Procedures’, was prepared and published in August 2019.11 The country has a Biosafety Level 3 (BSL-3) laboratory at the Institut Pasteur du Cambodge (IPC) and a BSL-2+ laboratory at the National Institute of Public Health.
At the onset of the pandemic, an Inter-ministerial COVID-19 Response Committee was formed. At that time, the capacity of the two laboratories was limited to performing a total of 500 PCR tests per day.8 To date, the COVID-19 response in Cambodia has not been well documented in scientific publications.8 While several papers described the early phases of COVID-19 responses including non-pharmaceutical interventions (NPIs), many other important aspects, such as rapid scale-up of laboratory capacity and vaccination, were overlooked.12 13 Our paper describes the epidemiological phases, response phases, strategy and lessons learnt in Cambodia between 27 January 2020 (when the first case was detected) and 30 June 2022, several months after Cambodia’s full reopening.
Epidemiological phases
Data related to COVID-19 such as new cases, numbers of tests, deaths and vaccinations were reported to the Inter-ministerial COVID-19 Response Committee.
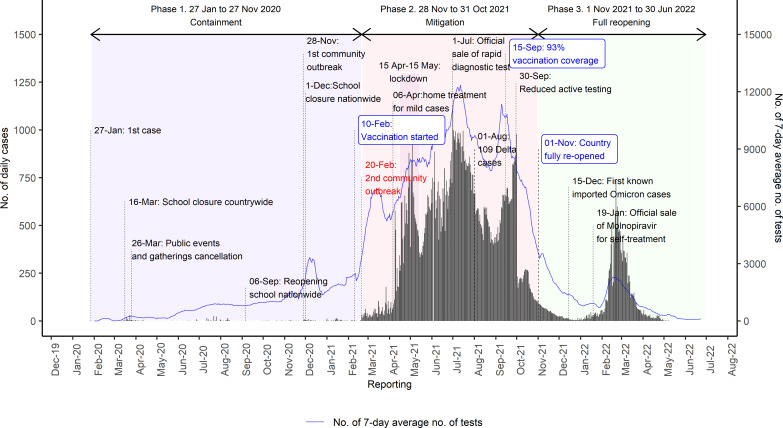
Figure 1 presents the daily number of COVID-19 cases and PCR tests in Cambodia. In Cambodia, we identified three significant phases of the pandemic: containment phase, mitigation phase and full reopening phase.
Figure 1.
COVID-19 daily cases, tests and deaths in Cambodia, 2020–2022. Data are based on the official data from the Ministry of Health (MoH).
Phase 1 (27 January to 19 February 2021): containment phase
In phase 1, COVID-19 was well contained. Cambodia had only 484 cases, mainly imported and no deaths (figure 1 and table 1).
Table 1.
Reported COVID-19 cases and deaths by phase in Cambodia, 27 January 2020 to 30 June 2022
| Phase of COVID-19 outbreak | Theme | All cases | Death |
| Phase 1: 27 January 2020 to 19 February 2021 | Containment with NPIs | 484 | 0 |
| 27 January to 30 April 2020 | Initial response
|
122 | 0 |
| 1 May to 31 October 2020 | Relaxing after long period of low cases | 169 | 0 |
| 1 November 2020 to 19 February 2021 | Intensifying response for larger scale outbreak | 193 | 0 |
| Phase 2: 20 February to 31 October 2021 | Large community outbreak and vaccination
|
118 129 | 2781 |
| Phase 3: 1 November 2021 to 30 June 2022 | Full reopening
|
17 669 | 275 |
NPI, non-pharmaceutical intervention.
Phase 2 (20 February to 31 October 2021): mitigation phase
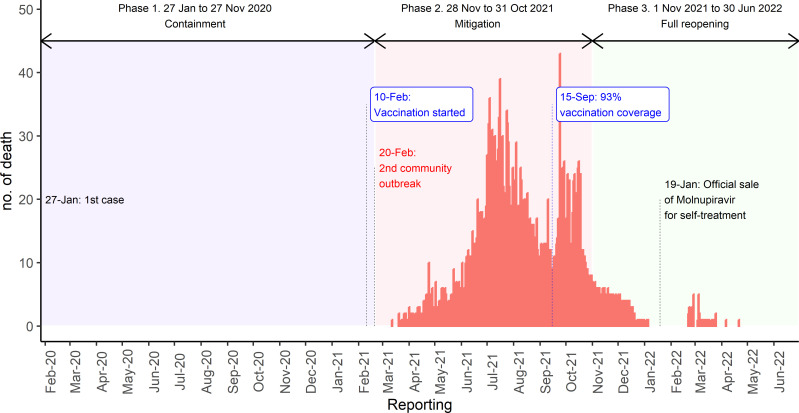
In phase 2, a large community outbreak occurred that lasted for 252 days with 118 129 cases (figure 1 and table 1). A total of 2781 COVID-19 deaths were reported (figure 2 and table 1).
Figure 2.
COVID-19 death trends in Cambodia, 2021–2022. Data are based on the official data from the Ministry of Health (MoH).
Phase 3 (1 November 2021 to 30 June 2022): full reopening
Phase 3 had 17 669 cases (figure 1 and table 1). In this phase, 275 deaths were reported.
Response phases
The government implemented eight significant measures during phases 1 and 2: (1) detect, isolate/quarantine; (2) face coverings, hand hygiene and physical distancing measures; (3) risk communication and community engagement; (4) school closures; (5) border closures; (6) public event and gathering cancellation; (7) vaccination; and (8) lockdown (table 2). Each of these measures was implemented quickly when the need for such intervention was seen to be warranted. The first six measures were implemented in phase 1, and measures 7 and 8 were added in phase 2.
Table 2.
Description of the eight measures used in Cambodia in response to the COVID-19 outbreak
| No | Measure | Description | Time frame |
| 1 | Detect, isolate/quarantine | This measure was used to detect cases for isolation and find contacts for quarantine. Contact tracing was the primary measure to trace the contacts, test them and quarantine them. Contact tracing commenced within 24 hours after a confirmed case was detected. The contacts were classified into high, medium and low risks. High and medium-risk contacts were tested at least two times during the quarantine. Low-risk contacts were tested if they had any signs or symptoms during the quarantine period.39 |
|
| 2 | Face coverings, hand hygiene and physical distancing | This measure was known as ‘3 DOs and 3 DON’Ts’. The ‘3 DOs’ refers to (1) wearing a face mask properly, (2) washing hands frequently with alcohol, gel or soap and (3) maintaining a physical distance of at least 1.5 m from others. The ‘3 DON’Ts’ refers to (1) not going to places that are not well ventilated, (2) not going to crowded places and (3) not touching others, shaking hands or hugging. |
|
| 3 | Risk communication and community engagement | It refers to the regular sharing of official information (eg, intensified press release, press conference, media talks, etc) through various MoH communication channels to timely raise awareness and dispel circulating myths and rumours, especially on social media. |
|
| 4 | School closure | School closure refers to the halt of in-person teaching in schools. The nationwide school closure commenced on 16 March when Cambodia had detected 24 cases. On 6 September 2020, the government reopened the schools country-wide after a low possibility of a community outbreak. On 1 December 2020, the government closed all schools country-wide again after a large cluster was detected. School closures were continued until the country’s full reopening on 1 November 2021. |
|
| 5 | Border restriction/closure | On 16 March 2020, Cambodia closed all border gates with Vietnam. On 16 April 2020, it implemented travel restrictions for passengers from France, Germany, Iran, Italy, Spain and the USA. On 20 May 2020, the government required all passengers to have a COVID-19 negative certificate within 72 hours before flying (effective until 31 October 2021); it also required health insurance with a minimum amount of US$50 000, and another test on arrival and quarantine for 14 days at a government-designated place (effective until 1 November 2021). |
|
| 6 | Public event and gathering cancellation | This measure was used to cancel all public events (eg, Khmer New Year) and gatherings (eg, wedding celebrations, usual funerals, memorial services and all festivals). |
|
| 7 | Vaccination | The goal of COVID-19 vaccination is to reduce transmission, severe cases, hospitalisations and deaths from COVID-19. On 10 February 2021, ten days before Cambodia declared the large community outbreak, Cambodia started vaccine rollout with the Sinopharm vaccine. The vaccination campaign accelerated in April 2021 as cases increased exponentially. By mid-September 2021, 93% of the 15.55 million population had received at least two doses/completed immunisation. |
|
| 8 | Lockdown | Lockdown is a large-scale local travel restriction. Cambodia started a country-wide lockdown between 15 April and 15 May 2021. By ‘lockdown’, we refer to restrictions on movement between villages or communes. Individuals could travel within the village or communes; however, they were advised to stay at home. |
|
MoH, Ministry of Health.
Phase 1 (27 January 2020 to 19 February 2021): containment with non-pharmaceutical interventions
After detecting the first case, on 30 January 2020, mandatory temperature screenings for all travellers entering Cambodia at all points of entry (airports and international borders) were immediately implemented. However, in March and April 2020, Cambodia detected several clusters of imported cases that were not identified through the temperature screening system, but rather through notifications from WHO’s IHR channel and event-based surveillance (screening local and international news). The virus spread locally from these primary cases.
To respond to these clusters, intensive contact tracing was undertaken to trace, test and quarantine the contacts. This strategy was an essential component of ‘Measure 1: detect, isolate/quarantine’. Contact tracing commenced within 24 hours after a case was detected. All contacts were quarantined at quarantine centres or in their homes for 14 days from the last date of exposure and monitored every day for the development of COVID-19 symptoms. Due to the labour-intensive nature of contact tracing, the CamEWARN hotline 115 system that was launched in 2016 and the police forces deployed nationwide were used to support the RRTs.14 The CamEWARN hotline 115 system was updated to take calls from the public during the COVID-19 pandemic to augment the contact tracing team to identify contacts and screen for tests.14 Contact tracing teams first called contacts to review their symptoms, inform them of the automated calls that they will be receiving thereafter and instruct them to press 0 for none symptom and press 1 for any symptoms. An average of 2654 automated calls were sent per day between April 2020 and March 2022.14 Thousands of police officers were trained in contact tracing to support the Ministry of Health (MoH) in this activity.
Cambodia also implemented Measure 2: face covering, hand hygiene and physical distancing since the first case was detected. The government strongly advised people to take such measures for self-protection and compliance by the population was very high. An online and telephone survey by UNICEF in April 2020 found that 75% of survey participants (aged 16 and over) practised at least one item of Measure 2 frequently.15
The government, through MoH, also implemented Measure 3: risk communication and community engagement from the onset. Regular sharing of official information through various MoH communication channels helped dispel circulating myths, false information and rumours, especially on social media.16 The MoH reiterated simple messages to the public, known as ‘3 DOs and 3 DON’Ts’. The ‘3 DOs’ refers to (1) wearing a face mask properly, (2) frequent hand disinfection using alcohol, gel-based formulations or soap and (3) maintaining physical distance of at least 1.5 m from others. The ‘3 DON’Ts’ refers to (1) not going to places that are not well ventilated, (2) not going to crowded places and (3) not touching others, shaking hands or hugging. The nationwide communication campaigns stimulated cooperation from the public. They were launched by the MoH through the ‘Sub-Committee on Education, Training, and Public Communication of the Inter-ministerial Committee to Fight COVID-19’ with the theme ‘Acting together to stop COVID-19 transmission’. A World Bank survey found that 99% of survey respondents received public messages; the UNICEF survey also found that 80% of survey respondents said public messages were the reasons they practised precautions.15 17
On 16 March 2020, when the country’s total number of detected cases reached 24, Measure 4: school closures was imposed nationwide. As 23 of the cases (95.8%) were imported, Cambodia also implemented Measure 5: border closures. Cambodia first closed all border gates with Vietnam before full closure with other countries. On 26 March 2020, when the country reached 90 cases, Measure 6: cancellation of all public events (eg, Khmer New Year) and gatherings (eg, wedding celebrations, usual funerals, memorial services, all festivals) was imposed. Travel restrictions for passengers from France, Germany, Iran, Italy, Spain and the USA were implemented on 16 April 2020.
By 20 May 2020, following the increasing trend of cases, travel restrictions were modified and the government required all passengers to have a COVID-19 negative test certificate within 72 hours before flying, health insurance with a minimum cover of US$50 000, another test on arrival and quarantine for 14 days at a government-designated place.
After a few months with low cases, the government considered Cambodia had a low risk of transmission outbreak and decided to reopen all schools nationwide on 6 September 2020.
On 3 November 2020, the Hungarian foreign minister came on a 2-day visit to Cambodia and met a considerable number of government officials including the prime minister, as well as students and teachers, on different occasions. On 6 November 2020, the foreign minister tested positive for SARS-CoV-2 on his return to Bangkok, Thailand. This became locally known as the ‘3 November Event’. Everyone who attended these gatherings and their contacts (over 2000 people) were tested and quarantined at home for 14 days since the last date of exposure. Four cases were detected as part of this cluster. It was unclear who the source of infection was, as the Hungarian foreign minister tested negative within 72 hours before flying to Cambodia. The ‘3 November Event’ prompted the government to tighten all measures due to its high potential for community transmission. On 23 November 2020, the government announced the closure of the ‘3 November Event’ after no more cases were detected.
On 28 November 2020, Cambodia announced its first community outbreak after a woman hospitalised with respiratory symptoms later tested positive for SARS-CoV-2; this is locally known as the ‘28 November community outbreak’. Six of her family members also tested positive. They had no history of travel abroad. However, she and her family visited several provinces in Cambodia and shopping centres for ‘Black Friday’. As a response, massive testing and quarantine were implemented. All individuals who were at sites where one or more of the confirmed cases had visited were tested. Certain commercial businesses (eg, AEON supermarket) were closed for 14 days. On 1 December 2020, the government reinstated nationwide school closures for in-person classes and ordered online classes to be administered instead. This remained in effect until the country’s full reopening. Within the span of 1 month, over 20 000 people were tested and home quarantined as part of this cluster. Forty-one cases (no deaths) were detected from this event. On 29 December 2020, the government declared the end of the ‘28 November community outbreak’.
Phase 2 (20 February to 31 October 2021): mitigation with vaccination campaign
Ten days before this phase, on 10 February 2021, Cambodia started Measure 7: rolling out COVID-19 vaccination with the Sinopharm vaccine after China donated 1 million doses of the said vaccine.
On 19 February 2021, two foreign women escaped the quarantine hotels to visit a night club while waiting for test results. Their results were positive for SARS-CoV-2. It triggered a large-scale testing of the night club’s visitors. Over 20 cases were identified. On the same date, the laboratory of the National Institute of Public Health also detected several cases among those who had requested pretravel testing.
On 20 February 2021, Cambodia announced a second community outbreak, locally known as the ‘20 February community outbreak’.
Measure 1: trace, isolate/quarantine was intensified. All individuals in the buildings or sites where one or more confirmed cases were known to have visited were tested. Around 8000 tests were performed per day, which was the full capacity of Cambodia’s laboratories at that time. However, as the cases increased exponentially (figure 1), the other five measures were also intensified. Additionally, Measure 8: lockdown was implemented covering the period between 15 April and 15 May 2021. Despite these more stringent measures, cases continued to rise (figure 1).
During the same period, from April 2021, the vaccination campaign was sped up and was continuously implemented without interruption. On average, 50 000 doses were provided daily and a vaccination coverage of 93% of the total population (n=14 485 634 out of 15 552 211) was quickly reached within 5 months by 15 September 2021.
On achieving this high vaccination coverage rate, the government stopped active surveillance but monitored two indicators—severe cases and deaths—to ensure that the COVID-19 situation remained under control.
Phase 3 (1 November 2021 to 30 June 2022): full reopening
Without any unusual increase in severe cases and deaths for 30 days in a row, the government decided to lift all compulsory containment measures from 1 November 2021. However, the government still advised people to continue with the ‘3 DOs and 3 DON’Ts’, provided booster doses routinely and continued to support the disadvantaged groups.
Strategy
We identified six themes from the COVID-19 responses in Cambodia.
Theme 1: setting up and managing a new response system
Cambodia learnt quickly and adapted to the dynamics of the disease. When the number of COVID-19 cases started to increase in March 2020, the prime minister immediately led the national response. He created and chaired the National COVID-19 Response Committee. This committee was composed of high-level committees to give advice on the various aspects of the country’s COVID-19 response. The high-level committees included 25 provincial COVID-19 committees, each chaired by the provincial governors, a high-level MoH task force to mobilise resources and the technical working group led by Cambodia’s CCDC with technical support from governmental and non-governmental stakeholders to provide technical advice on the COVID-19 emergency response.
The new systems were built on the ‘Cambodian Emergency Operations Centre and Incident Management System Standard Operating Procedures’ in 2019 and WHO’s 2020 COVID-19 strategic preparedness and response plan focusing on nine pillars, including (1) coordination and planning, (2) laboratory, (3) surveillance, (4) points of entry, (5) RRTs, (6) infection prevention and control, (7) case management and continuity of essential services, (8) logistics, procurement and supply management and (9) risk communication and community engagement.11 This strategic preparedness and response plan was modified and includes vaccination as a new pillar.
Theme 2: containing the spread with early response
As described previously, six measures were implemented to contain the spread of the virus. These measures had a background strategy, the so-called ‘5 Es’—Early detection, Early isolation, Early contact tracing, Early treatment and Early education.
Theme 3: strengthening the identification of cases and contacts
Cambodia trained new RRTs, increasing from around 2000 to over 5000 by the end of phase 1.8 9 In 2020, at the beginning of the response, IPC was the main laboratory performing PCR test with around 400 tests per 24 hours. The National Reference Laboratory at the National Institute of Public Health could perform around 100 PCR tests per 24 hours. With strong support from developing partners, testing capacity increased from 500 PCR tests per day in April 2020 to around 15 000 PCR tests per day in July 2021.8 To reduce the delay from sample transportation, 18 new laboratories in Phnom Penh and 11 provinces were set up.8
Theme 4: strengthening care for patients with COVID-19
To reduce the case fatality rate, Cambodia had to strengthen the capacity of its healthcare system.18 Cambodia addressed this issue by training many doctors and nurses to manage COVID-19 cases.
During phase 1, Cambodia trained public healthcare providers from over 1300 public healthcare facilities, including health centres, to treat and care for patients with COVID-19.8 In addition, it trained doctors and nurses in training to treat and care for patients with COVID-19.
School buildings, wedding buildings and abandoned hotels were temporarily repurposed as isolation and treatment centres.
Theme 5: boosting vaccination coverage
In April 2021, when the cases seemed unstoppable, Cambodia boosted the vaccination rate to build herd immunity.
After basic vaccination with the Sinovac, Sinopharm, Moderna, AstraZeneca or Janssen vaccines, adult booster doses were given with AstraZeneca and Pfizer vaccines. Children received the Sinovac and/or Pfizer (paediatric) vaccines and booster doses.
A total of 54.06 million doses of COVID-19 vaccine were obtained (table 3). The majority of the vaccines were Sinovac (63.7%), followed by Sinopharm (15.0%), Pfizer (adults and paediatric; 10.0%), AstraZeneca (7.8%) and Covishield (1.2%), and the remainder were Janssen and Moderna (2.3%).
Table 3.
Vaccine doses obtained by the Cambodian government until 5 February 2023
| Type of vaccine | Doses received | % |
| Sinovac | 34 424 800 | 63.7 |
| Sinopharm | 8 100 000 | 15.0 |
| Pfizer | 4 489 290 | 8.3 |
| Pfizer Paediatric | 923 990 | 1.7 |
| AstraZeneca | 4 224 040 | 7.8 |
| Janssen | 1 060 100 | 2.0 |
| Covishield | 649 000 | 1.2 |
| Moderna | 188 160 | 0.3 |
| Total | 54 059 380 | 100.0 |
Theme 6: supporting disadvantaged groups
Lockdown negatively impacts those in disadvantaged groups, particularly daily wage earners (eg, garment workers, Tuk-tuk (motorcycle) and taxi drivers, construction workers and street vendors).19 The government and local and international development partners strive to respond in a timely manner to help the disadvantaged groups.19 Initially, delivering food supplies was too slow and challenging due to the absence of a food distribution infrastructure specifically for the poor.13 19 20 Nevertheless, between May 2020 and May 2021, the government was able to provide social assistance through the COVID-19 Cash Transfer Programme to 700 000 low-income households, equivalent to more than 2.8 million individuals (around 18% of Cambodia’s total population). By June 2021, each of these households had received an average of US$366 in nine instalments.17
Lessons learnt
From Cambodia’s COVID-19 experiences and responses, we highlight 13 lessons learnt.
COVID-19 response requires decisive leadership and good governance
The COVID-19 pandemic is a ‘wicked problem’21 and many decisions were made amidst uncertainties. Leadership is a core part of governance, referring to the government’s ability to provide guidance, plan and make appropriate modifications to the laws or regulations at all levels and sectors to enable an effective response.
We learnt that responding to the pandemic requires decisive leadership, referring to decisions being taken fast, timely and without delay. This decisive leadership must be supported by good governance to effectively implement newly introduced policies or guideline. Literature suggests that decisive leadership led to success in responding to COVID-19 at the early phase in China, New Zealand, Taiwan and South Korea.22–26 With this characteristic, Cambodia was able to respond promptly, despite limited prepandemic capacity.
Laboratory capacity determines the response speed
The country should be able to conduct tests quickly without having to ship samples overseas. Laboratory capacity limits the speed of the response, as there would be delays in conducting the tests and releasing of results, impacting community transmission and deaths due to COVID-19. A rapid scale-up of laboratory capacity was essential. An example of high mortality and excess deaths due to delays in providing COVID-19 results was demonstrated in Ecuador.27 Taiwan and Singapore learnt from the SARS response in the 2000s and understood well the need to extend laboratory capacity; they took early actions that may have significantly contributed to their success in containing the virus spread in the early stage and overall mortality rate over time.28 In Cambodia, the RRT demands an immediate laboratory result (within 24 hours), so that they can decide in the field. Cambodia managed to scale up its laboratory rapidly to response to the need of response team and dynamic of the disease.
Risk communication and community engagement could fight the infodemics but must be consistent
Effective risk communication and community engagement has been critical for people to receive reliable information, to gain trust and to strengthen the cooperation of the public.29 Fighting the infodemic should be intense. It is important to agree that only one person or group shares COVID-19 information to make it consistent and avoid public confusion.
Contact tracing worked well in a small-scale response and stopped working when the community outbreak started
Contact tracing was to find the cases, isolate them and find their contacts; and it provided real-time information, which was necessary for the response teams to decide where to impose additional restrictions. However, it only works in settings where cooperation from the public is high. Moreover, it only works before community outbreak occurs. Contact tracing should be stopped when the evidence of community outbreak is confirmed to save resources for a mitigation plan.
Contact tracing is labour intensive but can be supported by technology and non-health sector
Contact tracing requires strong public collaboration. The hotline is a place where contacts can communicate with the RRT and seek advice. Automated calls to contacts reduce the workload for the RRT and provide timely results.14 Contact tracing can be done by the non-health sector. Police provide support in tackling cases who did not cooperate with health authorities.
School closures caused class disruption but it saved elderly lives
Schools are a perfect environment for transmission and a risk for elderly (aged 50 and over) who usually live with their children and grandchildren. However, school closures were highly controversial due to their effects on children’s learning. Cambodia implemented early school closures and empty schools were used as quarantine centres. This measure may have helped Cambodia successfully contain the virus for more than a year and prevent deaths from COVID-19.
However, long-term school closures have an immediate and long-term impact on the county’s development. According to a UNICEF survey, about 8% of students did not return to school and are less likely to return.30 The online classes or television programme classes could not replace the in-person class to support students’ learning activities at home.30 School closures should be done with careful consideration balancing risks and benefits and an education plan during crises or pandemics should be developed for future response.
Face coverings, hand hygiene, physical distancing, border restriction/closures and public event and gathering cancellation were not controversial in Cambodia
People in Cambodia tended to easily accept face coverings, hand hygiene and physical distancing; border restriction/closure; and public event and gathering cancellation. The cooperation was high. No rigorous evaluation has been conducted to understand the reasons. However, we believe in two combined effects. First, the government has engaged the public effectively, and second, it is a nature of the people of Cambodia to be cooperative.
Lockdown was not fully interrupting chain of transmission, hard to enforce and must accompany support to disadvantaged groups
Lockdown is a controversial measure for many settings as it affects the livelihoods of many individuals.31
In Cambodia, lockdown refers to a restriction imposed on the movement of individuals beyond their villages or communes. However, they were permitted to travel outside their homes within villages or communes. In some places, people could travel within districts or provinces. That means people can still have social interactions within their limited spaces. The efficacy of such strategy in preventing infection may not be high.32
Supporting the needs of low-income families was essential to reduce the social burden of COVID-19. The slow response to this particular issue was due to the limited existing registration system of people who need support.13 However, the government managed to provide food and cash support to around 700 000 households or 2.8 million individuals.17 From this experience, it is important to register and regularly update those who need support or so-called IDPoor in Cambodia.33
Lockdown should be done with careful consideration of risks and benefits. Registration systems to quickly identify people who need the most support can contribute to its faster provision. Individual practices to prevent transmission should always be a top priority.
Vaccination gave Cambodia a ticket to reopen the country, but it could be more effective by prioritising vulnerable groups at the early stage
As a low-income country, Cambodia was unique in achieving high vaccination coverage quickly. On achieving a 93% vaccination coverage in mid-September 2021, a marked decline in the number of deaths was noted by October 2021, approximately 1 month later. Cambodia was then able to fully reopen the country.
However, at the early stage, Cambodia did not prioritise the vaccine for the elderly—obviously more at higher risk of COVID-19 deaths—due to the safety concerns. Also, the government might have had the fear that any reported adverse vaccination events in the elderly—which could occur more frequently in this age group—could pose a risk to the entire vaccination campaign.
Cooperation from the public was the necessary factor
From the measures described above, adherence and compliance from the general public are required.12 The government called it solidarity. This compliance is a fundamental factor for success in containing the spread in the early phase and the very successful vaccination campaign in the later stage.
The background strategy of 5 Es was central for success
The background strategy of the ‘5 Es’ was behind the intensified implementation of each measure. In responding to the pandemic, every action must be timely to avoid running behind the transmission.
Care for patients with COVID-19 was inadequate
Although there are no quantitative data that can be used to describe the adequacy of care for patients with COVID-19, it can be observed and understood that the shortage of healthcare workers presented significant challenges in coping with the situation. In addition, the highly contagious nature of COVID-19 prevented healthcare workers from taking full care for the patients as well as instituting all measures otherwise done in other clinical cases (eg, suctioning of secretions). This may be one of the main contributory factors to COVID-19 deaths.
Healthcare facility structure can be modified (ie, provision of isolation facilities) and pretraining and in-service training on patient care during health emergencies can be included in the curricula and training programmes. A supply chain system for protective equipment can also be put in place.
Cambodia got advantages of strong collaboration between government and development partners
Developing partners such as the United Nations and its agencies, other international agencies, local and international non-governmental organisations and bilateral cooperation have played crucial roles in the COVID-19 response in Cambodia. However, we do not have access to sufficient data on their contributions, hindering our ability to precisely and quantitatively document their impact. Notable support included: partial vaccine donations to scaling up vaccinations, financial and medical equipment and materials, and technical assistance to build laboratory capacity, healthcare strengthening (eg, expending intensive care unit, constructing new COVID-19 treatment sites and renovating of referral hospitals for COVID-19 treatment) and assistance in policy development.8 34 35 The support went beyond the COVID-19 response, but it also addressed emergency food assistance, social assistance to the poor and economic recovery.36–38
The support of development partners and other agencies and organisations is vital, especially for low and middle-income countries. While we cannot fully discern all lessons learnt from this aspect, international cooperation always plays an important role in any response to emergencies and crises.
Concerted efforts rather than parallel programmes would be more favourable, also to ensure greater coverage of the needs of a country and its people.
Conclusion
Despite limited levels of preparedness prior to the pandemic, Cambodia successfully contained the spread of SARS-CoV-2 in the first year and quickly attained high vaccine coverage by the second year of the response. The core of this success was the strong political will, high cooperation from the public and strong support from developing partners such as the United National Family, international agencies, local and international non-governmental organisations and bilateral cooperation. However, Cambodia needs to improve its infrastructure in order to quarantine contacts, isolate cases and increase its laboratory capacity to better prepare for future health emergencies.
This review is among the few that presents the COVID-19 response, and highlights lessons learnt in Cambodia for organising and investing in future responses.
This paper has not explicitly covered a few important aspects such as good governance, resource mobilisation, and multilateral cooperation (eg, role of authorities and other ministries), and important roles of developing partners. Additionally, the COVID-19 data presented in this paper may be highly under-reported and may not reflect the actual trends due to limited testing capacity and changing surveillance strategies.
Acknowledgments
We thank all the Inter-ministerial COVID-19 Response Committee and Cambodia’s Communicable Disease Control Department (CCDC) for providing data.
Footnotes
Handling editor: Seye Abimbola
Twitter: @SreanChhim
Contributors: SC, GK, SM, WVDP, WVD, PI, CC and VO designed the study. SC analysed the data. SC, GK, SM, WVDP, WVD, PI, CC and VO wrote the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: VO (who works at the Ministry of Health), CC and PI work at NIPH and played active roles in COVID-19 response and policy design. SC (the former scholar of the Master of Philosophy in Applied Epidemiology at the Australian National University) was deployed to support the response from the beginning. These authors may have a positive bias towards the success of the COVID-19 response in Cambodia.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available in a public, open access repository. Data are publicly available. It can be accessed via WHO online database (Cambodia: WHO Coronavirus Disease (COVID-19) Dashboard with Vaccination Data | WHO Coronavirus (COVID-19) Dashboard with Vaccination Data).
Ethics statements
Patient consent for publication
Not applicable.
References
- 1. Van Damme W, Dahake R, Delamou A, et al. The COVID-19 pandemic: diverse contexts; different epidemics-how and why? BMJ Glob Health 2020;5:e003098. 10.1136/bmjgh-2020-003098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization . Regional office for the Western P. the Kingdom of Cambodia health system review. Manila. 2015. Available: https://apps.who.int/iris/bitstream/handle/10665/208213/9789290616917_eng.pdf
- 3. The World Bank . Physicians (per 1,000 per people)-Cambodia, Washington DC. 2014. Available: https://data.worldbank.org/indicator/SH.MED.PHYS.ZS?locations=KH
- 4. World Health Organization . The global health observatory. Geneva, Switzerland. 2020. Available: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/hospital-beds-(per-10-000-population)
- 5. The World Bank . Beds (per 1,000 per people)-Cambodia, Washington DC. 2016. Available: https://data.worldbank.org/indicator/SH.MED.BEDS.ZS?locations=KH
- 6. World Health Organization . Joint external evaluation of IHR core capacities. Geneva, Switzerland: WHO. 2017. Available: https://apps.who.int/iris/handle/10665/254705
- 7. World Health Organization (WHO) . Joint external evaluation of IHR core capacities. Geneva, Switzerland: WHO. 2017. Available: https://apps.who.int/iris/handle/10665/254705
- 8. Chhim S, Wuddhika IV, Pa K. A descriptive assessment of the National Institute of public health’s role in supporting the COVID-19 response in Cambodia, 2020–2021: National Institute of public health’s role in COVID-19 response. Western Pacific Surveillance and Response 2023;14:7. 10.5365/wpsar.2023.14.1.974 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. World Health Organization . The first 100 days of the COVID-19 response: past investments in health security system pay off, and learning lessons for the future. 2020. Available: https://www.who.int/cambodia/news/feature-stories/detail/the-first-100-days-of-the-covid-19-response-past-investments-in-health-security-system-pay-off-and-learning-lessons-for-the-future
- 10. Cambodiann communicable diseases control department (CCDC). Phnom Penh : Camewarn: Cambodia early warning system. 2023. Available: http://cdcmoh.gov.kh/surveillance/camewarn
- 11. Ministry of Health (MoH) . Cambodian emergency operations centre and incident management system standard operating procedures, phnom penh, cambodia2019. n.d. Available: https://niph.org.kh/niph/uploads/library/pdf/GL244_5_6102813189454430703_eng.pdf
- 12. Nit B, Samy AL, Tan SL, et al. Understanding the slow COVID-19 trajectory of Cambodia. Public Health Pract (Oxf) 2021;2:100073. 10.1016/j.puhip.2020.100073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tatum M. Cambodia ends controversial COVID-19 restrictions. Lancet 2021;397:S0140-6736(21)01196-X. 10.1016/S0140-6736(21)01196-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Suy Lan C, Sok S, Chheang K, et al. Cambodia National health Hotline-participatory surveillance for early detection and response to disease outbreaks. Lancet Reg Health West Pac 2022;29. 10.1016/j.lanwpc.2022.100584 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. UNICEF . Review of risk communication and community engagement initiative for covid-19: prevention behaviours in Cambodia phnom penh. Cambodia. 2020. Available: https://www.unicef.org/cambodia/media/3856/file/FinalReport.pdf
- 16. World Health . 2019 novel coronavirus (2019-ncov): strategic preparedness and response plan, Geneva, Switzerland. n.d. Available: https://www.who.int/publications/i/item/strategic-preparedness-and-response-plan-for-the-new-coronavirus
- 17. Karamba W, Salcher I, Tong K. Results from the high-frequency phone survey of households round. n.d. Available: https://documents1.worldbank.org/curated/en/833701624563697124/pdf/Main-Report.pdf
- 18. Sheikhbardsiri H, Raeisi AR, Nekoei-Moghadam M, et al. Surge capacity of hospitals in emergencies and disasters with a preparedness approach: a systematic review. Disaster Med Public Health Prep 2017;11:612–20. 10.1017/dmp.2016.178 [DOI] [PubMed] [Google Scholar]
- 19. Macdonald S. Learning from Cambodia’s COVID-19 response: foreign policy in focus (FPIF). 2021. Available: https://fpif.org/learning-from-cambodias-covid-19-response/
- 20. Johnson S, Srey V. Thousands of cambodians go hungry in strict lockdown zones, phnom penh. Cambodia. 2021. Available: https://www.theguardian.com/global-development/2021/may/13/thousands-of-cambodians-go-hungry-in-strict-lockdown-zones
- 21. Schiefloe PM. The corona crisis: a wicked problem. Scand J Public Health 2021;49:5–8. 10.1177/1403494820970767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Nicola M, Sohrabi C, Mathew G, et al. Health policy and leadership models during the COVID-19 pandemic: a review. Int J Surg 2020;81:122–9. 10.1016/j.ijsu.2020.07.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Al Saidi AMO, Nur FA, Al-Mandhari AS, et al. Decisive leadership is a necessity in the COVID-19 response. Lancet 2020;396:295–8. 10.1016/S0140-6736(20)31493-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Stoller JK. Reflections on leadership in the time of COVID-19. Leader 2020;4:77–9. 10.1136/leader-2020-000244 [DOI] [Google Scholar]
- 25. Kaul V, Shah VH, El-Serag H. Leadership during crisis: lessons and applications from the covid-19 pandemic. Gastroenterology 2020;159:809–12. 10.1053/j.gastro.2020.04.076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Phillips G, Kendino M, Brolan CE, et al. Lessons from the frontline: leadership and governance experiences in the COVID-19 pandemic response across the Pacific region. Lancet Reg Health West Pac 2022;25:100518. 10.1016/j.lanwpc.2022.100518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Torres I, Sippy R, Sacoto F. Assessing critical gaps in COVID-19 testing capacity: the case of delayed results in Ecuador. BMC Public Health 2021;21:637. 10.1186/s12889-021-10715-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Cheng H-Y, Li S-Y, Yang C-H. Initial rapid and proactive response for the COVID-19 outbreak-Taiwan's’experience. J Formos Med Assoc 2020;119:771–3. 10.1016/j.jfma.2020.03.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Zhang Y, Tambo E, Djuikoue IC, et al. Early stage risk communication and community engagement (RCCE) strategies and measures against the coronavirus disease 2019 (COVID-19) pandemic crisis. Glob Health J 2021;5:44–50. 10.1016/j.glohj.2021.02.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. UNICEF . COVID-19 socio-economic impact assessment: UNICEF. 2021. Available: https://www.unicef.org/cambodia/media/5471/file/COVID-19%20Socio-Economic%20Impact%20Assessment.pdf
- 31. World Health Organization . Coronavirus disease (COVID-19): herd immunity, lockdowns and COVID-19: who. 2020. Available: https://www.who.int/news-room/questions-and-answers/item/herd-immunity-lockdowns-and-covid-19
- 32. Um S, Vang D, Oy S, et al. The descriptive epidemiology of covid-19 linked to community transmission and lockdown effect in Cambodia. 2021;2:09. [Google Scholar]
- 33. Kaba MW, Baesel K, Poch B, et al. IDPoor: a poverty identification programme that enables collaboration across sectors for maternal and child health in Cambodia. BMJ 2018;363:k4698. 10.1136/bmj.k4698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. US Embassy in Cambodia . U.S. donates two million COVID-19 vaccines to the Cambodian people, phnom penh. Cambodia. 2022. Available: https://kh.usembassy.gov/u-s-donates-two-million-covid-19-vaccines-to-the-cambodian-people/
- 35. US Mission to ASEAN . [ fact sheet ] U.S support for ASEAN in fighting COVID-19: US mission to ASEAN. 2022. Available: https://asean.usmission.gov/fact-sheet-u-s-support-for-asean-in-fighting-covid-19/
- 36. Asian Development Bank (ADB) . Cambodia: COVID-19 active response and expenditure support program: ADB. 2023. Available: https://www.adb.org/projects/54195-001/main
- 37. United Nations (UN) . Information note # 3: social assistance & un Cambodi’'s COVID-19 responce. 2021. Available: https://cambodia.un.org/en/127454-information-note-3-social-assistance-un-cambodias-covid-19-response
- 38. Keo S. Information note: un Cambodia’s COVID-19 response to current community outbreak, phnom penh, Cambodia. 2021. Available: https://cambodia.un.org/en/126617-information-note-un-cambodia%E2%80%99s-covid-19-response-current-community-outbreak
- 39. Chhim S. Applied epidemiology in Cambodia. The Australian National University (Australia), 2021. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data are available in a public, open access repository. Data are publicly available. It can be accessed via WHO online database (Cambodia: WHO Coronavirus Disease (COVID-19) Dashboard with Vaccination Data | WHO Coronavirus (COVID-19) Dashboard with Vaccination Data).