Abstract
The global burden of paediatric and congenital heart disease (PCHD) is substantial. We propose a novel public health framework with recommendations for developing effective and safe PCHD services in low-income and middle-income countries (LMICs). This framework was created by the Global Initiative for Children’s Surgery Cardiac Surgery working group in collaboration with a group of international rexperts in providing paediatric and congenital cardiac care to patients with CHD and rheumatic heart disease (RHD) in LMICs. Effective and safe PCHD care is inaccessible to many, and there is no consensus on the best approaches to provide meaningful access in resource-limited settings, where it is often needed the most. Considering the high inequity in access to care for CHD and RHD, we aimed to create an actionable framework for health practitioners, policy makers and patients that supports treatment and prevention. It was formulated based on rigorous evaluation of available guidelines and standards of care and builds on a consensus process about the competencies needed at each step of the care continuum. We recommend a tier-based framework for PCHD care integrated within existing health systems. Each level of care is expected to meet minimum benchmarks and ensure high-quality and family centred care. We propose that cardiac surgery capabilities should only be developed at the more advanced levels on hospitals that have an established foundation of cardiology and cardiac surgery services, including screening, diagnostics, inpatient and outpatient care, postoperative care and cardiac catheterisation. This approach requires a quality control system and close collaboration between the different levels of care to facilitate the journey and care of every child with heart disease. This effort was designed to guide readers and leaders in taking action, strengthening capacity, evaluating impact, advancing policy and engaging in partnerships to guide facilities providing PCHD care in LMICs.
Keywords: paediatrics, public health, thoracic surgery, cardiovascular disease, review
WHAT IS ALREADY KNOWN ON THIS TOPIC
Paediatric and congenital heart disease (PCHD) care is inaccessible to many people and particularly in low-income and middle-income countries (LMICs).
There are currently no structured, evidence driven recommendations for the development of quality PCHD care in resource-limited settings.
WHAT THIS STUDY ADDS
This framework charts the way forward in addressing critical and long‐standing PCHD health and workforce challenges.
New recommendations aiming to provide a framework to healthcare practitioners and policymakers in designing and delivering quality PCHD care services at each level of the healthcare system.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
We propose a tier-based framework for PCHD care integrated within existing health systems.
Each level of care is expected to meet benchmarks and ensure high-quality and family centred care.
This approach requires a quality control system and close collaboration between the different levels of care to facilitate the journey and care of every child with heart disease.
We recommend careful tracking of the this new framework’s
Background
Congenital heart disease (CHD) is the most common birth defect, with an incidence of ~1 in 100 live births, a significant number of whom cannot survive past their first year without appropriate care and intervention.1–3 This incidence does not include the inherited cardiac rhythm abnormalities which often require medications, intervention and/or follow-up. Neonatal arrhythmias have been reported in 1%–5% of live births.4–6 For children older than 1 year of age, 10% of all mortality can be attributed to sudden death.7 An annual incidence of sudden cardiac death (SCD) is reported to be 1.5 in 100 000 persons 1–20 years of age. Furthermore, 40% of SCDs remained unexplained after autopsy, of which about one-third are found to have cardiac gene mutations.8 The Global Burden of Disease (GBD) study estimated >7 million children live with cardiovascular disease, contributing to an annual mortality of 261 247 from CHD in 2017, with the majority of deaths occurring in low-income and middle-income countries (LMICs).2 The study also reported a high morbidity of 589 479 years lived with disability (YLD) in 2017, comparable to lower respiratory infections. This number increases exponentially when the burden of rheumatic heart disease (RHD) is considered, adding another 1 900 974 YLD.
The options for children with CHD are medical management, interventional/surgical therapies or comfort care. It is estimated that nearly half of these children require surgical management, however a large proportion of people in LMICs lack timely access to safe and affordable cardiac surgical and rehabilitative care.9 Congenital heart surgery is a highly specialised field that has evolved over the last decades allowing most of those who need it to live into adulthood.10 11 However, cardiac surgery requires extensive resources and expertise within a well-functioning, high-quality microsystem12 with the same improvement in mortality not seen in LMICs, where cardiac surgery capability has not adequately developed. Children born with CHD in LMICs continue to disproportionately bear the GBD.11 A 2017 study reported that CHD mortality in low-income countries has declined by only 6% since 1990, compared to a steady decline of over 50% in high-income countries (HICs). Despite this, CHD in LMICs remains a low national priority on the global public health and global surgery agenda.2 In addition to being a ‘neglected’ disease, the disparities seen in CHD care in LMICs are further complicated by co-morbidities such as malnutrition and infection and other barriers to care provision (table 1 and box 1).13 14
Table 1.
Barriers to providing quality congenital heart disease care along the care continuum
| Recognition | Diagnosis | Referral | Stabilisation and transport | Treatment | Follow-up |
| Lack of prenatal and antenatal screening protocols. Lack of availability of screening equipment and trained personnel. Inconsistent well-child visits. Inability to get remote consultation from high-level cardiac care facilities. This may be due to unavailability of telehealth-telemedicine equipment or a well-defined consultation pathway. Demands on the trained paediatric cardiologist of catering to large patient volumes may also make a teleconsultation process ineffective. |
Lack of availability of diagnostic equipment, infrastructure and trained personnel. | Unable to recognise need for referral. Weak referral pathways. Lack of effective communication with referral centres. |
Inconsistent access to centres equipped to recognise and stabilise patients. Inadequate transport and communication system. Untrained paramedics staff with inadequate care provided to patients during transport. |
Inconsistent access to centres equipped to manage patients medically and surgically. Unavailability of required infrastructure and expertise. |
Inadequate emphasis on long-term follow-up and counselling. Unavailability of remote telehealth-telemedicine platforms to streamline care. |
Box 1. Key barriers themes to providing quality congenital heart disease (CHD) care.
Barriers to access: financial, policy and socio-economic constraints.
Patient/Caregiver barriers: lack of caregiver awareness and poor health-seeking behaviour.
Health system barriers: lack of resources, infrastructure, technology, trained personnel, quality and safety measures. Hierarchical cultures disrupting team dynamics and poor multidisciplinary care coordination.
Government-level barriers: lack of advocacy, prioritisation of national and global health agenda, healthcare financing systems, poor governance, accountability and cost-benefit assessment for providing CHD care nationally.
Similarly, a GBD study reported that in 2015 there were 33.4 million cases of RHD, contributing to 319 400 deaths and 10.5 million disability-adjusted life-years. Although RHD mortality has decreased over time, LMICs have lagged significantly, with Oceania, South Asia and central sub-Saharan Africa reporting the highest mortality.15 16
A limited number of children with paediatric and congenital heart disease (PCHD) in LMICs have access to excellent care through the few cardiac surgery centres and sporadic short-term medical missions.17 Surgical centres often do not have adequate infrastructure, human resources or supplies to address the full spectrum of cardiac surgical care for children. Moreover, due to the lack of a robust approach and consensus on how effectively to establish and run a PCHD programme, many centres offer limited scope of services and demonstrate variable and poor outcomes.18 The available guidelines developed in HICs are only partially accountable for the pervasive service and ongoing quality challenges in resource-limited settings,19–22 while limited data are available from LMICs describing a road-map of creating PCHD services.23 The goal of the recommendations is not to create a new vertical system but to incorporate the minimum services needed in the health system. We believe it will allow for a smoother transition and better collaboration between departments focused on newborn and child health and non-communicable diseases (NCDs), which typically do not plan for services for childhood-onset heart diseases. This framework is provide a common and share taxonomy that aims to define the basic recommendations for developing high-quality and reliable PCHD services globally and to propose a new service classification for facilities with increasing capacity and capabilities. Moreover, a growing literature argues that access without quality may cause more harm than benefit, is costlier and can lead to mistrust in the health system. Regular assessment of patient, provider and system outcomes implemented around a continuous quality improvement (CQI) process is central to our recommendations.24
Methods
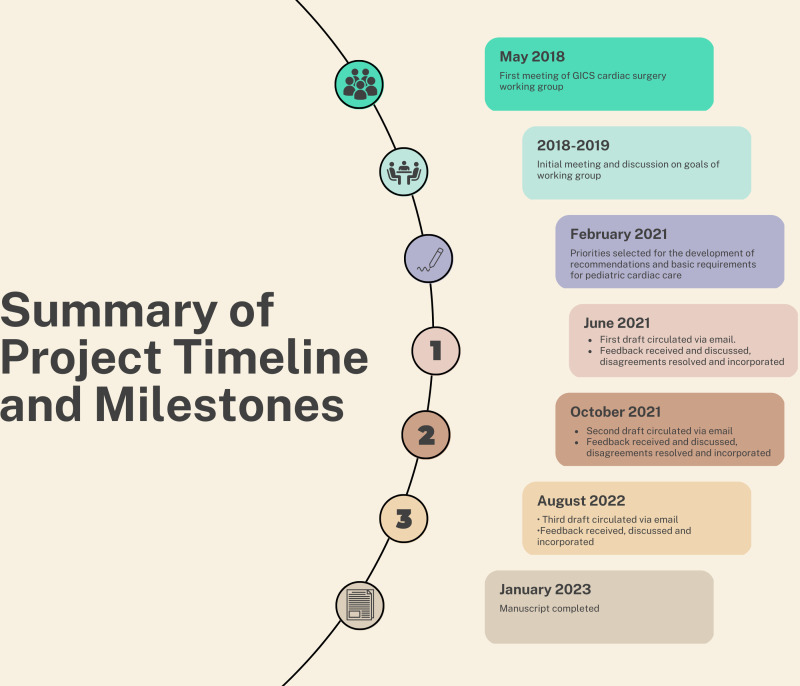
We conducted an exhaustive literature review (see online supplemental text), followed by iterative discussion on resources, existing guidelines and challenges faced in global PCHD care. We generated a basic set of recommendations structured around each step in the journey a child must take in requiring cardiac care. The framework was created by the newly formed cardiac surgery working group of the Global Initiative for Children’s Surgery. Detailed input was sought from physicians and allied health staff in LMICs and those in HICs and non-governmental organisations (NGOs) with extensive experience of working in LMICs as either trainers or humanitarian assistance providers. Feedback from patient and family groups was also provided from the Global Alliance for Rheumatic and Congenital Hearts. We received responses from 17 countries, 12 of which are LMICs (figure 1). The NGOs based their experience on an additional 43 LMICs. The final draft of the recommendations incorporated multiple rounds of this feedback (figure 2).
Figure 1.
Countries represented in authorship.
Figure 2.
Summary of project timeline and milestones. GICS, Global Initiative for Children’s Surgery.
bmjgh-2023-012049supp001.pdf (541.9KB, pdf)
Results
Service mapping
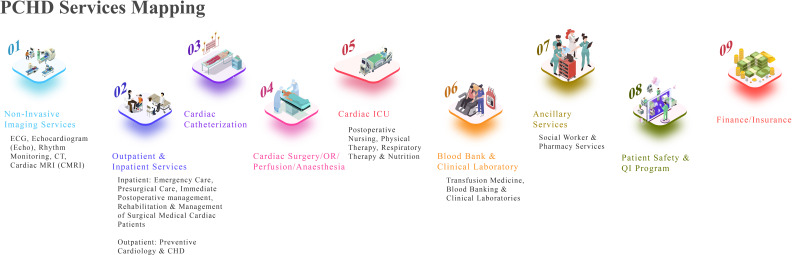
Exceptioanl PCHD services requires a complex continuum of care that entails non-invasive diagnostic cardiology (echocardiogram, CT scan, etc), outpatient and inpatient cardiology including preventative cardiology services, cardiac catheterisation, cardiac surgery including cardiac anaesthesia and perfusion, postoperative cardiac intensive care unit (CICU), nursing and allied health services, including physical therapy, respiratory therapy, transfusion medicine, clinical laboratories, nutrition services, patient safety and QI programmes, postsurgery rehabilitation and ancillary services such as social workers and pharmacy services (figure 3).
Figure 3.
Pediatric and congenital heart disease (PCHD) service(s) mapping. ICU, intensive care unit.
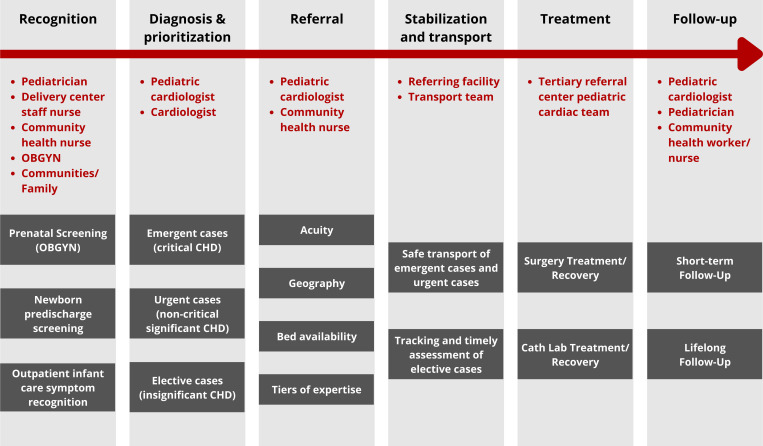
Service delivery assumptions
We considered the following foundational assumptions rather than viewing care as a single surgical event. These assumptions pertain to the complete care continuum in effective management of PCHD (figure 4) as previously described.25
Figure 4.
Care continuum of a child with heart disease. CHD, congenital heart disease; OBGYN, obstetrics and gynaecology. Adapted from Nair SM et al. A population health approach to address the burden of congenital heart disease in Kerala, India. Global Heart 2021; 16(1): 71
Seamless referral systems
The framework relies on close collaboration in a seemless manner between different levels of care providers to facilitate effective patient care. A communication, patient handoff and referral system between hospitals and providers is essential to provide quality, timely care.26 27 Integration with existing public (government and private) health systems and care delivery pathways is essential for sustainable and scalable solutions.
Health financing system and financial support options
Government financing is key to developing sustainable paediatric cardiac programmes, whether through direct budget lines or national social insurance programmes. Unfortunatley, out-of-pocket payment for surgical services is still common in LMICs, which is a major barrier to accessing care and many programmes seek alternative forms of financing to support their patient population.28 29
Increased volume and scope of service to develop competencies and efficiency
Higher volumes in congenital cardiac surgery have been shown to improve efficiency, safety and quality of outcomes.30
Multidisciplinary clinical care
Advanced cardiac care must be provided in a setting that can facilitate a multidisciplinary approach with shared decision-making between surgery, cardiology, anaesthesia, perfusion and intensive care, as well as all other required areas of paediatric care such as infectious diseases, neurology, psychiatry, radiology, nutrition and allied health services such as psychology and physiotherapy.
Primacy of an ongoing CQI programme
As health care moves toward the quadruple aim 31 of improving patient experience, improving the health of populations, lowering costs, and increasing satisfaction among providers, congenital heart surgery programs must evolve to meet the growing scrutiny, demands, and expectations of numerous stakeholders. Improved outcomes and reduced interinstitutional variability are achieved through prioritization of quality assurance and improvement.Data and outcomes must be monitored to allow for continuous QI efforts.18 QI must be emphasised at all levels of the patient’s journey.32 Higher-level centres are expected to participate in QI registries for data collection and benchmarking. Lower-level programmes not yet reporting to patient registries should set internal QI targets with the goal of consistent improvement. CQI audit metrics should cover the complete care continuum of patient with CHD (figure 5).33
Figure 5.
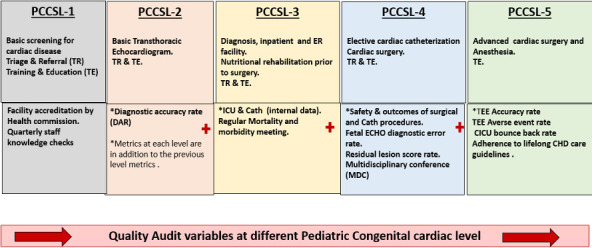
Quality audit variables at different pediatric and congenital cardiac service levels (PCCSL).CHD, congenital heart disease; CICU, cardiac intensive care unit; ICU, intensive care unit; TEE, trans-oesophageal echocardiography.
An environment that integrates sustainability through research, training and teaching
Higher-level facilities must make an active effort to build a culture prioritising research, detailed invidual and integrated team training of the workforce.
A supportive system and environment that prioritises a life-course approach
PCHD surgery is not curative. All CHD and RHD survivors face a high risk of long-term morbidity and reinterventions. Risk of mortality in CHD has been reported between 2 and 23 times higher than age-matched peers.34–36 Patient selection for surgery should therefore consider long-term outcomes and realistic across the life span. A clear plan for ongoing cardiac care must be established for and communicated to all patients and caregivers as well to policy makers.
Ability to advocate and effect public policies pertaining to PCHD care at national and international levels
Advocacy for inclusion in NCDs and maternal and child health policies is central to addressing the disparities in paediatric and congenital cardiac care.37
Paediatric and congenital cardiac service levels
We charted a roadmap of defined levels and benchmarks for PCHD services from a primary health centre to advanced surgical centres. The levels1–5 are based on the World Bank health facilities classification (online supplemental table S1) and are defined by the complexity of care provided (table 2).38
Table 2.
Summary of paediatric and congenital cardiac services by health system complexity levels
| Level of care complexity | Basic paediatric and congenital cardiac services level 1 (PCCSL-1) | Intermediate paediatric and congenital cardiac services level 2 (PCCSL-2) | Complex/Advanced paediatric and congenital cardiac services level 3 (PCCSL-3) | Complex/Advanced paediatric and congenital cardiac services level 4 (PCCSL-4) | Complex/Advanced paediatric and congenital cardiac services level 5 (PCCSL-5) |
| Type of facility (DCP3 classification) | Health centre | First-level hospital | Referral hospital: second level | Referral hospital: third level | Referral hospital: National Children’s Hospital. |
| Responsibilities | Basic screening for cardiac disease Triage and referral Training and education Liaison with referral centres for follow-up care |
Basic diagnostic cardiology Superficial postoperative wound care Treatment of patent ductus arteriosus-dependent disease with intravenous prostaglandin E2 Triage and referral Training and education Liaison with referral centres for follow-up care |
Comprehensive screening and non-invasive diagnostic cardiology Outpatient, inpatient and emergency cardiac care Training and education Triage and referral |
Elective and emergent cardiac catheterisations Cardiac surgeries Training and education |
All elective or emergent cardiac catheterisations and cardiac surgeries including neontal cardiac procedures. Training, education, and research. |
| Age treated | All | All | All | All | All |
| Anaesthesia | No | Expert conscious sedation skills | General anaesthesia skills | Paediatric and congenital heart anaesthesia(s) or adult cardiac anaesthesia(s) with paediatric experience | Paediatric and congenital heart anaesthesia(s) or adult cardiac anaesthesia(s) with paediatric experience and credentials. |
| Human resources | Nurses and staff with basic paediatric training | Cardiac sonographers (anyone with some congenital heart disease imaging experience) Paediatric nurses Paediatric physicians Visiting paediatric cardiologist |
In addition to what is needed in PCCSL1 and 2, paediatric cardiologists with basic interventional cardiology experience Cardiac surgery backup |
Paediatric and congenital heart surgeon(s) or adult cardiac surgeon(s) with paediatric experience.Appropriately trained pediatric interventional cardiologist. | Paediatric and congenital heart surgeon(s) with expertise in neonatal cardiac surgeries. Pediatric interventional cardiologist with experience in neontal cardiac procedures. |
| Required skills | Basic cardiac history, examination and pulse oximetry. Ability to measure blood pressures. |
Diagnostic echocardiography Resuscitation and stabilisation Basic medical management Superficial wound care Basic pain management |
Comprehensive cardiac diagnosis, imaging and medical care Resuscitation and stabilisation Basic intensive care including ICU facilities for neonates on Prostaglandins. Emergent cardiac catheterisation procedures (pericardiocentesis, temporary pacemaker insertion, balloon atrial septostomy) |
Fetal echocardiography Electrophysiology services Cardiac intensive care Cardiac catheterisation (PREDIC3T categories 0–4) Cardiac surgery: RACHS-2 categories 1 and 2 STAT 1 and 2 ABC 1 and 2 PRAIS2 10 - 15 |
Cardiac catheterisation: all procedures. Cardiac surgery: all procedures. Adult CHD services. Cardiac transplant/LVAD/ECMO. |
| Infrastructure | Basic outpatient Infrastructure Transportation and referral system Investing in a low-cost telemedicine platform for timely consultation from higher-level centres |
Basic inpatient and outpatient infrastructure Transportation and referral system |
Infrastructure for basic inpatient cardiology services Transportation and referral system |
Functionally and physically separate paediatric echocardiography lab Infrastructure for CICU, cardiac catheterisation and cardiac surgery (can be functionally separate but physically shared facility with adult services) |
Functionally and physically separate CICU preferably including ECMO. Functionally and preferably physically separate cardiac catheterisation services. Infrastructure for advanced cardiac surgery. |
| Equipment and supplies | Basic medical equipment Pulse oximeters Stethoscopes ECG Chest X-ray (if available) Blood pressure apparatus See online supplemental appendix table 2 |
See online supplemental appendix table 2 | See online supplemental appendix tables 2 and 3 | Equipment and supplies to support the proposed complexity of children’s cardiac care See online supplemental appendix tables 1–3 |
See online supplemental appendix tables 1-3. |
| Quality and safety | CME and CPD of healthcare providers around use of pulse oximetry and cardiac-specific history taking, examination and blood pressure measurement. Quality audits of transport and referral mechanisms. |
QI framework for diagnostic accuracy in echocardiography adapted from ACPC QNET of the ACC51 52 | In addition to what is required in PCCSL 1 and 2, reporting of inpatient complication rate, infection rate, crude mortality rate for emergency interventions and length of stay Regular M&M meetings . |
In addition to what is present in other lower-level centres, a QI and safety representative QI framework for diagnostics, cardiac catheterisation and cardiac surgery by preferably being on international registries like IQIC, ACC QNET, etc Long-term care plan for patients undergoing cardiac surgery, as a way to develop adult CHD service |
In addition to above, multidisciplinary programme review, additional advanced echocardiography metrics from ACPC QNET, adherence to lifelong CHD care guidelines. |
ABC, Aristotle Basic Complexity; ACC, American College of Cardiology; ACPC QNET, Adult Congenital & Paediatric Cardiology Quality Network; CHD, congenital heart disease; CICU, cardiac intensive care unit; CME, continuous medical education; CPD, continuous professional development; ECMO, extracorporeal membrane oxygenation; ICU, intensive care unit; IQIC, International Quality Improvement Collaborative; LVAD, left ventricular assist device; M&M, morbidity and mortality; PRAIS2, partial risk adjustment in surgery; PREDIC3T, Procedural Risk in Congenital Cardiac Catheterisation; QI, quality improvement; RACHS, Risk Adjustment for Congenital Heart Surgery; RHD, rheumatic heart disease; STAT, The Society of Thoracic Surgeons-European Association for Cardio-Thoracic Surgery; TEE, trans-oesophageal echocardiography.
bmjgh-2023-012049supp002.pdf (55KB, pdf)
Each level of the framework defines benchmarks that programmes should meet before moving towards increasingly complex care. In cardiac surgical and interventional services, the scope is based on complexity of diagnosis and procedure as defined by the following established methods of case/procedure risk categorisation:
Cardiac surgery: Risk Adjustment for Congenital Heart Surgery-2, The Society of Thoracic Surgeons-European Association for Cardio-Thoracic Surgery, Aristotle Basic Complexity and Partial Risk Adjustment in Surgery 2 models.39–42
Cardiac catheterisation: Procedural Risk in Congenital Cardiac Catheterisation categories.43
Although we describe five tiers/levels of care, many countries or programmes may align these to their existing national healthcare infrastructure, availability of expertise, function and quality of the services provided within their context. Countries where frontline health workers are better trained and can perform skills like basic echocardiogram, levels 1 and 2 can be merged.
Paediatric and congenital cardiac services level 1: community health centre
Paediatric and congenital cardiac services level 1 (PCCSL-1) facilities are in rural or low-resource settings (ie, primary healthcare centre of a public healthcare system) that can provide only basic screening for congenital cardiac disease via history taking and physical examination including auscultation, blood pressure monitoring and pulse oximetry. Patients identified via screening would be referred/transported to higher levels of care as needed. Use of telemedicine platforms to connect with cardiologists at higher-level centres is an effective way of remote consultation.44 45 Such a platform has been used for supervision of basic echocardiograohy done by non-cardiologist medical practitioners.44 This may also help with initial management and in determining the urgency of transferring the child to a higher facility.44 46 The scope of services and infrastructure requirements of such facilities are described below.
Scope of service: basic cardiac screening, no cardiac surgery. Minimum requirements to provide cardiac care at this level include (online supplemental table S2a):
Screening for cardiac disease
A basic infrastructure for outpatient evaluation of paediatric patients, with nurses and staff trained to use and interpret pulse oximeters, blood pressure apparatus, weighing machines and stethoscopes are needed at this level. Patients presenting to PCCSL-1 facilities should be screened for severe illness including CHD through clinical assessment of basic danger signs and pulse oximetry (online supplemental table S3 and online supplemental figure S1 and S2).47 48 Patients who fail pulse oximetry screen and/or have other identifiable signs of severe disease should immediately be referred to the nearest facility that can establish definitive diagnosis and provide initial management. Since PCCSL-1 facilities cannot manage these patients, it is an absolute requirement to have an efficient referral and transport system in place with pre-identified affiliated higher-level hospitals. At PCCSL-1, paediatric patients presenting without any evidence of cardiac disease must also be seen from the perspective of prevention. Considering the high prevalence, morbidity and mortality (M&M) of RHD in selected LMICs, there is a need for protocols to screen at-risk populations and provide secondary prophylaxis for RHD in the form of timely penicillin administration, preferably through registers of confirmed cases.16 49 The ability to identify households with adults with coronary artery disease, hypertension, diabetes, obesity or stroke will help screen the children at risk for non-communicable heart disease. Healthy diet and lifestyle modifications counselling of high-risk families should be performed routinely.50 Nutritional interventions to counter malnourishment in patients with CHD awaiting interventions can also be done via these facilities.
Training and education
Providers at this level will be trained to screen for and identify cardiac disease using basic skills and equipment mentioned above. This can be done in collaboration with higher-level centres in the area and through continuous medical education (CME) workshops. Additionally, the staff should be basic life support certified according to American Heart Association-defined schedules.
Quality improvement (table 2, figure 5)
Meaningful QI efforts entail assessment of the effectiveness of the CME as mentioned above. The ability to identify neonates with CHD that need intervention within first months of life can be used as a metric at this level, although the accuracy of screening tools used, and skill set of the frontline health workers using these tools may impair the validity of the metric. The frontline health workers can be assessed for their skills and knowledge regarding the effective use of screening tools and timely referral of patients suspected of having CHD.
Paediatric and congenital cardiac services level 2: first-level hospital
Paediatric and congenital cardiac services level 2 (PCCSL-2) facilities should have basic diagnostic capabilities. These facilities would require infrastructure, human resources and skills for diagnostic echocardiography (ECHO), including a sonographer who has experience/training in congenital cardiac imaging as well as a visiting/part-time paediatric cardiologist to supervise ECHO.
Scope of service: basic diagnostic paediatric cardiology, medical management of cardiac emergencies, basic postoperative care. Minimum requirements within each arm of the cardiac service include (online supplemental table S2b):
Cardiology
Non-invasive diagnostic cardiology
At least one person (either a dedicated cardiac sonographer or the visiting cardiologist) trained to perform ECHO with some experience in identifying congenital and acquired structural cardiac defects.
At least one visiting/part-time paediatric cardiologist for supervision of ECHO. This supervision can either be done in person or via a simple low-cost telehealth platform in connection with paediatric cardiology services at a higher-level centre (PCCSL-3 or above). These cardiologists should then be able to refer patients who may require further evaluation, management, intervention or surgery to higher levels of care.
Outpatient cardiology
In addition to what has been described for PCCSL-1:
Resuscitation and stabilisation including treatment of duct-dependent critical CHD with prostaglandin E2 and ability to immediately refer to higher-level centre.
Basic management of postoperative patients including superficial wound care and follow-up, assessments (especially postinterventions).
Regular (at least monthly) paediatric cardiology outpatient clinics.
Basic management of patients with RHD including anticoagulation for metallic prosthetic valves.
Recognition, initial management, follow-up and outpatient management of other acquired paediatric heart diseases like Kawasaki disease, myocarditis, acute presentation of rhythm abnormalities, etc.
Cardiac surgery
No cardiac surgery is performed at this level.
Triage and referral
Patients identified on screening to have life-threatening cardiac lesions should be stabilised and then referred in a timely manner to higher-level centres for further management. Patients who are stable but have been identified to have a potential structural defect on screening can be evaluated via diagnostic ECHO under supervision of the cardiologist affiliated with the centre. If needed, these patients can then be referred to the next level of care or evaluated by the visiting paediatric cardiologist in clinic.
Training and education
Providers at this level will be expected to receive similar training and education as level 1, with a focus on diagnostic cardiology. Continuous professional development (CPD) of the sonographer should be done through regular refresher courses and feedback by the paediatric cardiologist.
Quality improvement
In addition to the above, QI efforts should focus on diagnostic ECHO and medical management. There should be an ECHO archiving system with consistent tracking of diagnostic accuracy and errors as described in table 2 and table 3, figure 5. This effort should ideally be monitored by the supervising cardiologist working with the PCCSL-2 facility.
Table 3.
Detail of quality audit variables at different congenital cardiac levels
| Metric | Definition | Numerator | Denominator | Target | Comments |
| PCCSL-2 | |||||
| Diagnostic accuracy rate* | The proportion of potentially preventable and clinically important inaccurate diagnoses among congenital heart surgical patients Minor: no change in patient plan Moderate: change in plan but no harm Severe: catastrophic event/death |
Number of inaccurate diagnoses | Number of CHD scans done | Minor: <5% Moderate: <2% Severe: 0% |
This will be done as previously described taxonomy of diagnostic error in congenital echocardiography.35 40 |
| PCCSL-3 (in addition to above metrics) | |||||
| ICU and inpatient complications rate | CAUTI, CLABSI, VAP, soft tissue infections | <5/1000 central line days. <5/1000 urinary catheter days. <5 VAP/1000 ventilator-days. 10% soft tissue infections |
Programmes can follow standard defintions and methods to calculate CAUTI, CLABSI, VAP and soft tissue infections. Standard report per 1000 line/catheter/ventilator days can be used for tracking these metrics. |
||
| Crude mortality rate | Number of mortalities | Number of patients admitted | <10% | Since programmes are not expected to be on a registry at this level, targets can be set internally with a focus on consistent improvement. | |
| ICU LOS | Mean/median LOS in ICU | Expected LOS in ICU according to lesion | – | ||
| Emergent cardiac catheterisation procedure outcomes | Crude mortality rate in hospital after emergent cardiac catheterisation | Number of mortalities attirbuted to the emergent procedure. | Number of emergent procedures performed in a year | <10% | – |
| Regular M&M meetings | Number of M&M meetings conducted per year | – | – | >2 | – |
| PCCSL-4 (in addition to above metrics) | |||||
| Safety and outcomes of cardiac catheterisation procedures |
|
– | – | – | At this level and above, centres will be expected to be on a QI registry such as IQIC to ensure regular data collection and benchmarking. Cumulative data (median length of ICU or hospital stay, mortality rates, etc) from IQIC reports can be used to create benchmarks. |
| Safety and outcomes of cardiac surgery procedures |
|
– | – | – | |
| Fetal diagnostic error rate* | This measure provides a mechanism for fetal echocardiography laboratories to record and analyse diagnostic discrepancies between fetal and postnatal findings | Number of fetal patients with a moderate or severe discrepancy between prenatal and postnatal diagnosis | Fetuses born during the quarter with prenatal CHD diagnosis needing intervention within first year of life | <5% | Comparison of prenatal imaging findings and reports with postnatal investigations and reports or repeat fetal echocardiogram. |
| Residual lesion score | To keep a record of residual lesion based on predischarge postoperative echocardiogram | Number of procedures with RLS category 3 or more56 | Total number of surgeries performed | <10% | |
| MDC | Safety of surgical procedures | Cases discussed in MDC | Total number of surgeries | 100% | To ensure that all cases undergo MDC. |
| PCCSL-5 (in addition to above metrics) | |||||
| TEE accuracy rate* | Accuracy of pre-operative diagnosis based on TEE | Total number of pre-operative TEEs with one or more major discrepancies identified within 24 hours of surgery | Total number of pre-operative TEEs performed | 0% | Postcardiac surgery TEE, retrospective medical record review and operative reports. |
| TEE adverse events rate* | Rate of adverse events associated with TEE | Number of TEEs with adverse events identified during a TEE assessment | Total number of TEEs performed | <2% | |
| Bounce back rate | Rate of readmissions to ICU | Number of patients shifted back to ICU within 24 hours | Number of patients shifted from ICU to ward | <2% | To ensure nursing staff in step-down units/wards are well trained. Also to avoid early, inappropriate shifting of patient from ICU. |
| Lifelong follow-up care rate | Adherence to lifelong CHD care guidelines60 | Number of patients in whom lifelong follow-up guidelines are being followed | Total number of patients with CHD in the programme | >80% | |
*Metrics adapted from the non-invasive ACPC QNET network.51 52
ACPC QNET, Adult Congenital and Paediatric Cardiology Quality Network; CAUTI, catheter-associated urinary tract infection; CHD, congenital heart disease; CLABSI, central line-associated bloodstream infection; ICU, intensive care unit; IQIC, International Quality Improvement Collaborative; LOS, length of stay; MDC, multidisciplinary conference; M&M, morbidity and mortality; PCCSL, paediatric and congenital cardiac service levels; PPM, permanent pcemaker; QI, quality improvement; TEE, trans-oesophageal echocardiography; VAP, ventilator-associated pneumonia.
Paediatric and congenital cardiac services level 3: referral hospital—second-level hospital
A paediatric and congenital cardiac services level 3 (PCCSL-3) centre is the first level at which paediatric cardiology care is offered for simple lesions by dedicated paediatric cardiologists and other subspecialists.
Scope of service: outpatient and inpatient cardiology care, emergent cardiac catheterisation. Minimum requirements within each arm of the cardiac service include (online supplemental table S2c):
Cardiology
PCCSL-3 facilities will be expected to offer non-invasive diagnostic cardiology services like ECG, ECHO, fetal ECHO, X-ray, ambulatory blood pressure monitoring and Holter exams.
Outpatient and inpatient cardiology services will be expected, including diagnostic cardiology, outpatient and initial inpatient management of acquired and congenital cardiac diseases, palliative care for patients with end-stage cardiac disease, postoperative and lifelong follow-up, preventive cardiology and emergency cardiac care.
PCCSL-3 facilities should lead prevention and screening (community or school based) efforts for RHD and non-communicable cardiovascular disease in the community in collaboration with PCCSL-1 and PCCSL-2 facilities.
PCCSL-3 centre are expected to have at least one cardiologist with basic interventional cardiology experience. Only emergent, life-saving cardiac catheterisation procedures should be performed at a PCCSL-3 facility. This includes balloon atrial septostomy or pericardiocentesis for cardiac tamponade (bedside ECHO-guided or using fluoroscopy where available) and temporary pacemaker placement. Patients requiring more complex procedures should be referred to a higher level of care for further management after initial stabilisation. Cardiology services in PCCSL-3 facilities should have access to either a shared catheterisation laboratory or a sterile set-up for emergency bedside procedures.
As there is no elective cardiac intervention offered at this level, a dedicated CICU is not necessary. However, it is expected that these facilities will have an intensive care setup like neonatal and/or paediatric intensive care units (ICUs) and can handle cardiac patients that require intensive care but are not stable enough to be transported to PCCSL-4 or PCCSL-5 centres. PCCSL-3 centres would require paediatric intensivists or paediatrician with experience in intensive care management and paediatric intensive care nurses with experience in cardiology.
Cardiac surgery
Cardiac surgeon (adult or paediatric) in the same or affiliated hospital who can be present as surgical back up/support during emergent cardiac catheterisation.
Key support service
PCCSL-3 centres are expected to have access to a formal infection control team which can perform ongoing monitoring, reporting and follow-up of environment and hospital-based infection rates and trends.
Triage and referral
All patients presenting to PCCSL-3 centres can be triaged and appropriately managed medically and/or through emergent intervention. PCCSL-3 centres can stabilise these patients and transport/refer them to PCCSL-4 or PCCSL-5 centres if the need for cardiac surgery is identified. These centres also have the responsibility to receive and manage patients referred from PCCSL-1 and PCCSL-2 facilities in their respective areas and must establish clear protocols for communication and transport with them.
Training and education
PCCSL-3 centres should lead training and education efforts at their own facility as well as affiliated PCCSL-1 and PCCSL-2 facilities for physicians, nurses and other allied health providers focused on screening for heart disease and providing basic cardiac care. These centres will be expected to do outreach clinics and supervise diagnostic cardiology, data tracking and QI efforts at affiliated PCCSL-1 and PCCSL-2 facilities.
Quality improvement (table 2, table 3 and figure 5)
In addition to QI variables tracked at PCCSL-1 and PCCSL-2, QI efforts should be focused on both diagnostic cardiology and inpatient cardiology care. PCCSL-3 centres should establish a patient medical record system at their own level as well as facilitate a similar system at affiliated PCCSL-1 and PCCSL-2 facilities. They should have the ability to transfer information and communicate regarding patient records for all referred patients. PCCSL-3 centres will also be expected to conduct regular inpatient M&M meetings. It is recommended that diagnostic ECHO-related metrics at these centres can and should be tracked and reported to an international registry/collaborative like the American College of Cardiology Quality Network.51–54
Paediatric and congenital cardiac services level 4: referral hospital—third-level hospital
Paediatric and congenital cardiac services level 4 (PCCSL-4) centre will be the first-level facility at which comprehensive elective and emergent paediatric and congenital cardiac surgery and catheterisation are offered.
Minimum requirements within each arm of the cardiac service include (online supplemental table S2d):
Cardiology
In addition to the full spectrum of cardiology care described in PCCSL-3, PCCSL-4 centres will be expected to offer both emergent and elective cardiac catheterisation services with paediatric and congenital cardiac surgery support present in the same centre for all ages, including patients with adult CHD (ACHD). This requires a paediatric cardiologist with comprehensive training in interventional cardiology as well as nurses and staff with experience in cardiac catheterisation. Cardiac catheterisation procedures within PREDIC3T categories 0–4 (online supplemental table S4) can be offered at this level.
Cardiac surgery
PCCSL-4 centres are expected to perform a range of cardiac surgery procedures (described in table 2). This requires access to an operating room, operative equipment, a trained paediatric and congenital cardiac surgeon or adult cardiac surgeon with paediatric experience (at least 50% time dedicated to PCHD surgery), cardiac anaesthetists, perfusionists and an operation room team with experience in cardiac surgery, as well as 24/7 access to pharmacy (drug interactions monitoring/review and clinical consultations), blood products and clinical laboratory (for blood gases and basic chemistries).
Intensive care
PCCSL-4 centres require a dedicated CICU or a dedicated space in a combined unit for cardiac surgery patients or an assigned space in a paediatric ICU. These patients must be cared for by paediatric intensivists. paediatric intensive care nurses and other allied staff trained and experienced in postoperative cardiac care.
Key support services
PCCSL-4 centres will be expected to have access to infection control. These centres should also preferably have access to respiratory, occupational, physical and speech therapists. Access to a nutritionist is also preferred.
Triage and referral
PCCSL-4 centres will offer the full spectrum of cardiology care and some level of cardiac intervention and surgery. However, when patients requiring more complex cardiac surgery or intervention are encountered, they must be referred to a PCCSL-5 centre that is equipped to handle those patients. These centres should also establish systematic referral pathways for patients identified at any lower level centre in their area. A dedicated social worker can be responsible to ensure effective communication and care coordination.
Training and education
PCCSL-4 centres should have internal continuous training and education efforts, as well as lead similar efforts at affiliated lower-level centres. Paediatric cardiology, interventional cardiology and cardiac surgery training fellowships can also be established with appropriate accreditation to fulfil the local requirements. Integrated research programmes addressing contextual needs are crucial for developing new evidence-based practice relevant to low-resource settings.
Quality improvement
In addition to what is required in the previous PCSSL levels, a dedicated quality and safety manager is needed to supervise QI efforts for diagnostics, outpatient and inpatient cardiology as well as cardiac catheterisation and surgery. These centres should be connected to a data registry for diagnostic imaging, cardiac catheterisation and surgery and consistently track and report their outcomes. An example of such a registry which collects data from LMIC CHD programmes is the International Quality Improvement Collaborative (IQIC).55 IQIC provides a platform to document outcomes of cardiac surgery and interventions in patients with CHD and provides this service free of cost to LMIC centres. Mandatory, regular multidisciplinary conference where presurgical cases are discussed with review of data and images and lessons applied from previous cases should be attended by the cardiovascular team and all department members involved in care of these patients. A system of reviewing M&M in cardiac surgery and catheterisation, and quality audits in diagnostic imaging should be established to ensure continuous learning and QI. Additionally, fetal ECHO diagnostic error rates and residual lesion scores based on predischarge postoperative ECHO should also be collected (figure 5 and table 3).56
Additional requirements
A comprehensive cost tracking system with funding sources must be established with quarterly audits of financial status.
Effort should be made to formulate a long-term care plan for all patients undergoing cardiac surgery addressing physical, mental and social needs, as a way to develop specialised ACHD service.
Paediatric and congenital cardiac services level 5: referral hospital—National Children’s Hospital
Pediatric and congenital cardiac services level 5 (PCCSL-5) centres should be highly specialised facilities equipped to handle the full spectrum of paediatric and congenital cardiac care, including all cardiac surgery and catheterisation procedures, especially for neonates with CHD. These capabilities can only be established in the setting of a well-functioning cardiology and cardiac surgery service as described above that consistently tracks and demonstrates acceptable outcomes.
Minimum requirements within each arm of the cardiac service include (online supplemental table S2e):
Cardiology
PCCSL-5 centres are expected to provide the full spectrum of cardiology as described in PCCSL-4 including diagnostic, outpatient, inpatient, emergency cardiac care, electrophysiology, and fetal cardiology.
PCCSL-5 centres are expected to offer both emergent and elective cardiac catheterisation services for patients of any age (especially neonates) and type of cardiac lesion. This requires at least two to four paediatric cardiologists with comprehensive training in interventional cardiology as well as nurses and staff with experience in cardiac catheterisation and resuscitation.
Cardiac surgery
PCCSL-5 centres should be able to perform all cardiac surgery procedures. This requires a dedicated operating room, at least two paediatric and congenital cardiac surgeons (with expertise in neonatal cardiac surgery), a dedicated operative team including an anaesthetist and perfusionist trained in paediatric and congenital heart disease, 24/7 access to pharmacy and blood products and a clinical laboratory.
Intensive care
PCCSL-5 centres are expected to have a dedicated CICU staffed by intensivists, intensive care nurses and other staff trained and experienced in congenital, paediatric and postoperative cardiac care (especially neonatal cardiac patients). Such centres should preferably have ECMO services. It is recommended to have advanced practice nurses for mentoring and continued nursing education.
Key support and allied health services
PCCSL-5 centres will be expected to have access to the following professional services: respiratory occupational, physical and speech therapists, nutritionist, social support services, child psychology.
Triage and referral
PCCSL-5 centres must establish a network of satellite lower-level centres in the area they serve with 24/7 communication, patient record systems and transport systems.
Training and education
PCCSL-5 centres should conduct internal continuous training and education efforts as well as lead similar efforts at affiliated lower-level services as described for PCCSL-3 and PCCSL-4. Continuing education for all paediatric and congenital cardiac staff should be provided regularly including immersive simulation to improve individual and team performance.57 Paediatric cardiology, interventional cardiology and cardiac surgery training fellowships as well as congenital cardiac nurse residency programmes can be established with appropriate accreditation. Similarly, allied health training certification courses (for sonographers, cardiac catheterisation lab technicians, congenital perfusionists, etc) should be established. Integrated research programmes based on local needs are crucial for developing new evidence-based practice. Postgraduate research outputs such as PhDs are encouraged.58
Quality improvement (table 2, table 3 and figure 5)
In addition to the requirements described for previous PCCSLs, additional ECHO metrics such as residual lesion scores based on predischarge postoperative ECHO and ICU bounce back rate should also be tracked. At this level, a heart centre quality council should have a strong oversight of all aspects of quality audits across the programme.59 Efforts should be made to track holistic, lifelong patient-centric outcomes. The International Consortium of Health Outcome Measures CHD standard sets and the American College of Cardiology/American Heart Association guidelines for management of adults with CHD can be used to track lifelong care including physical, mental and social aspects of health of patients with CHD.59 60
Access to other paediatric non-cardiac specialties
PCCSL-5 centres should have ready access for consultation with other paediatric specialists, for example, nephrology, genetics, neurosurgery, neurology, paediatric general surgery, etc.
Additional requirements
In addition to the multidisciplinary and M&M meetings and cost of care assessment, the following should also be addressed:
Specialised ACHD service.
Research for clinical and/or basic science.
Advocacy for financing and inclusion in universal health coverage.
Advocacy with private insurance providers.
Quality audit metrics at each step of the care continuum
Over the recent past, several tools have been recommended to achieve improvement in paediatric and congenital cardiac patient outcomes. These tools include pioneering work by surgeons, advances in anesthesiology, critical care and nursing, improved diagnostic tools and innovations in non-surgical interventional techniques.61 62 The application of QI methods at all five health system levels should improve clinical outcomes in this field (figure 5). CQI strives to support deep reflection all elements of care, understand data, reduce variation and implement changes to PCHD practice so patients can receive the best care at the right time (see table 3 for details across the continuum of care). We recommend that LMIC centres join the IQIC and when participation in cardiac care registries is not possible, they should try to use the validated QI metrics in internal, self-maintained quality reports.
Discussion
CHD is rising as a major contributor to childhood mortality together with NCDs as leading causes of mortality around the world. While HICs have seen a significant reduction in M&M from RHD and CHD, these benefits have not been reflected in LMICs’ outcomes. Since LMICs are often under-resourced and understaffed, care provision must be integrated with existing health systems to avoid duplication of resources or creation of parallel, competing systems.
Complex cardiac care should be provided at higher-level facilities, which must meet established benchmarks to reach each level. Every child’s journey from their first contact with the healthcare system must be facilitated and streamlined. This includes screening, diagnosis, counselling, referral and transport. The goal of every facility providing cardiac care should be to work at its respective level to provide high-quality care tailored to suit community needs.
We define CQI as the daily use of QI methods as a regular part of practice engaging all practice staff, constantly measuring structure, processes, outcomes against effective practices (benchmarking), moving from one QI project to the next, pursuing the goal of “The right care for every child every time”. It is based on clear scientific principles,62 a valid way of measuring change and has theories of reliability and human factors that underpin the interventions to help pediatric cardiologists and other clinical providers to ask the right questions when seeking to drive improvement
The need for centres providing high-complexity cardiac care depends on population density and disease burden. The European Association for Cardio-Thoracic Surgery guidelines recommend one centre for 4–6 million population with a minimum surgical activity of 250 operations per year (125 operations per surgeon).19 Furthermore, centres performing neonatal and infant surgery should perform at least 100 infant operations annually.19 We have proposed a hub and spoke model for interaction between the higher-level centres (PCCSL-4 and PCCSL-5) and the lower-level facilities (PCCSL-1, PCCSL-2, PCCSL-3). The PCCSL-4 and PCCSL-5 centres could serve as central ‘hubs’ guiding congenital cardiac care in all lower-level facilities in their catchment area, including education, training, research, transport/referral, communication, supervision, coaching of faculty and QI efforts.
This framework draws attention to the need to provide public guidance with ongoing input from professional societies. Paediatric and adult cardiac services in LMICs often share resources and personnel. We recommend that while PCCSL-4 centres can function in such an arrangement, PCCSL-5 centres should have dedicated and trained paediatric teams, equipment and infrastructure. We recommend that adult CHD and RHD care be provided together with paediatric care, as in low-resource settings those subspecialists are often lacking. Additionally, close collaboration with adult cardiologists and cardiac surgeons may help provide comprehensive, holistic care to these patients. We note that a robust collaboration between adult and paediatric cardiology services is vital in caring for adults with CHD.
Limitations
Our study has several limitations. First, while we attempted to obtain a diverse global perspective, LMICs vary in their geopolitical, socioeconomic and cultural characteristics and many countries are not represented. Our aim was to chart a general set of recommendations which can be adapted and customized to each country’s unique healthcare system and policies. Second, we acknowledge that the proposed framework for PCHD services development can only thrive in the setting of sustainable and equitable healthcare financing. Lack of appropriate healthcare financing is a major concern in LMICs, as universal healthcare and health coverage is rare, leading most patients to rely either on out-of-pocket payments or charitable organisations. Third, we have not included policy and healthcare financing recommendations for developing sustainable PCHD care. We intend to cover these recommendations in a subsequent effort. Fourth, only limited input from experts in nursing care, allied health and hospital management was incorporated into preparing these recommendations. We acknowledge the importance of these professionals as stakeholders in paediatric care and leaders in the process of change. Fifth, further research to include patient and family perspectives is needed.
Conclusions
We recommend a life-course approach wherein medical centres are expected to establish long-term care plans for their patients, their carers and communities. PCCSLs 1–3 can provide high-quality non-surgical cardiac care, and PCCSLs 4 and 5 can develop cardiac surgical and interventonal care with an increasing level of complexity and ongoing efforts to improve their performance. We believe that healthcare facilities developing cardiac surgery/intervention capabilities should first establish an escalating level of services as described in PCCSLs 1–3. Integration with existing public healthcare delivery pathways is essential to create a sustainable and scalable PCHD care continuum. For example, basic screening can be integrated within community healthcare programmes and basic cardiac surgical services can be provided at district-level tertiary care hospitals. Participation in PCHD registries is essential as a major component of ongoing and realistic quality assessment and ongoing continuous improvement efforts.
Acknowledgments
The authors would like to acknowledge the Pakistan Children’s Heart Foundation (PCHF) for their feedback from a patient advocacy perspective.
Muhammad Fahad Khan, Marketing and Communication Associate, SIUT for helping with the infographics and figures in the manuscript.
Footnotes
Handling editor: Seye Abimbola
Twitter: @DrBabarHasan, @bhatti_areesh, @teamheartrwanda, @distypearson, @DVervoort94, @bzheleva
BSH and AB contributed equally.
Contributors: BSH, AB and BZ contributed to the conceptualisation, design, literature search, manuscript writing and manuscript editing. BSH and AB contributed equally to this paper. All authors participated in discussion, reviewed and edited the manuscript, provided feedback, contributed to analysis of available literature and approved the final manuscript. BSH is the guarantor and accepts full responsibility for the work and/or the conduct of the study, had access to the data, and controlled the decision to publish
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Disclaimer: The views expressed in this article are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute, the National Institutes of Health or the United States Department of Health and Human Services.
Liesl Zühlke is funded by the South African Medical Research Council (SAMRC) through its Division of Research Capacity Development under the Mid-Career Scientist Programme from funding received from the South African National Treasury. The content hereof is the sole responsibility of the authors and do not necessarily represent the official views of the SAMRC. Liesl Zühlke also receives support from the National Research Foundation of South Africa (NRFSA), as well as the UK Medical Research Council (MRC) and the UK Department for International Development (DFID) under the MRC/DFID Concordat agreement, via the African Research Leader Award (MR/S005242/1)
Massimo Caputo's work is supported by British Heart Foundation.
Map disclaimer: The inclusion of any map (including the depiction of any boundaries therein), or of any geographic or locational reference, does not imply the expression of any opinion whatsoever on the part of BMJ concerning the legal status of any country, territory, jurisdiction or area or of its authorities. Any such expression remains solely that of the relevant source and is not endorsed by BMJ. Maps are provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the 'Methods' section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data sharing not applicable as no datasets generated and/or analysed for this study.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
Not applicable.
References
- 1. van der Linde D, Konings EEM, Slager MA, et al. Birth prevalence of congenital heart disease worldwide: a systematic review and meta-analysis. J Am Coll Cardiol 2011;58:2241–7. 10.1016/j.jacc.2011.08.025 [DOI] [PubMed] [Google Scholar]
- 2. GBD 2017 Congenital Heart Disease Collaborators . Global, regional, and national burden of congenital heart disease, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet Child Adolesc Health 2020;4:185–200. 10.1016/S2352-4642(19)30402-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hoffman JIE, Kaplan S, Liberthson RR. Prevalence of congenital heart disease. Am Heart J 2004;147:425–39. 10.1016/j.ahj.2003.05.003 [DOI] [PubMed] [Google Scholar]
- 4. Badrawi N, Hegazy RA, Tokovic E, et al. Arrhythmia in the neonatal intensive care unit. Pediatr Cardiol 2009;30:325–30. 10.1007/s00246-008-9355-4 [DOI] [PubMed] [Google Scholar]
- 5. Kundak AA, Dilli D, Karagöl B, et al. Non benign neonatal arrhythmias observed in a tertiary neonatal intensive care unit. Indian J Pediatr 2013;80:555–9. 10.1007/s12098-012-0852-3 [DOI] [PubMed] [Google Scholar]
- 6. Ban JE. Neonatal arrhythmias: diagnosis, treatment, and clinical outcome. Korean J Pediatr 2017;60:344–52. 10.3345/kjp.2017.60.11.344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Wren C. Sudden death in children and adolescents. Heart 2002;88:426–31. 10.1136/heart.88.4.426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bagnall RD, Weintraub RG, Ingles J, et al. A prospective study of sudden cardiac death among children and young adults. N Engl J Med 2016;374:2441–52. 10.1056/NEJMoa1510687 [DOI] [PubMed] [Google Scholar]
- 9. Higashi H, Barendregt JJ, Kassebaum NJ, et al. The burden of selected congenital anomalies amenable to surgery in low and middle-income regions: cleft lip and palate, congenital heart anomalies and neural tube defects. Arch Dis Child 2015;100:233–8. 10.1136/archdischild-2014-306175 [DOI] [PubMed] [Google Scholar]
- 10. van der Bom T, Zomer AC, Zwinderman AH, et al. The changing epidemiology of congenital heart disease. Nat Rev Cardiol 2011;8:50–60. 10.1038/nrcardio.2010.166 [DOI] [PubMed] [Google Scholar]
- 11. Vervoort D, Swain JD, Pezzella AT, et al. Cardiac surgery in low- and middle-income countries: a state-of-the-art review. Ann Thorac Surg 2021;111:1394–400. [DOI] [PubMed] [Google Scholar]
- 12. Vervoort D, Premkumar A, Ghandour H, et al. Health system needs to establish cardiac surgery centers. Thorac Cardiovasc Surg 2021;69:729–32. 10.1055/s-0040-1721395 [DOI] [PubMed] [Google Scholar]
- 13. Kankeu HT, Saksena P, Xu K, et al. The financial burden from non-communicable diseases in low- and middle-income countries: a literature review. Health Res Policy Syst 2013;11:31. 10.1186/1478-4505-11-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mendis S. The policy agenda for prevention and control of non-communicable diseases. Br Med Bull 2010;96:23–43. 10.1093/bmb/ldq037 [DOI] [PubMed] [Google Scholar]
- 15. Belay W, Aliyu MH. Rheumatic heart disease is missing from the global health agenda. Ann Glob Health 2021;87:110. 10.5334/aogh.3426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Watkins DA, Johnson CO, Colquhoun SM, et al. Global, regional, and national burden of rheumatic heart disease, 1990-2015. N Engl J Med 2017;377:713–22. 10.1056/NEJMoa1603693 [DOI] [PubMed] [Google Scholar]
- 17. Murala JSK, Karl TR, Pezzella AT. Pediatric cardiac surgery in low-and middle-income countries: present status and need for a paradigm shift. Front Pediatr 2019;7:214. 10.3389/fped.2019.00214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Zimmerman M, Sable C. Congenital heart disease in low-and-middle-income countries: focus on sub-Saharan Africa. Am J Med Genet C Semin Med Genet 2020;184:36–46. 10.1002/ajmg.c.31769 [DOI] [PubMed] [Google Scholar]
- 19. Daenen W, Lacour-Gayet F, Aberg T, et al. Optimal structure of a congenital heart surgery department in Europe. Eur J Cardiothorac Surg 2003;24:343–51. 10.1016/s1010-7940(03)00444-5 [DOI] [PubMed] [Google Scholar]
- 20. Section on Cardiology and Cardiac Surgery, American Academy of Pediatrics . Guidelines for pediatric cardiovascular centers. Pediatrics 2002;109:544–9. 10.1542/peds.109.3.544 [DOI] [PubMed] [Google Scholar]
- 21. Sholler G, Selbie L. The Australian National standards of care for childhood-onset heart disease. J Paediatr Child Health 2021;57:2043. 10.1111/jpc.15790 [DOI] [PubMed] [Google Scholar]
- 22. NHS England . Congenital heart disease standards & specifications. NHS England, 2016. [Google Scholar]
- 23. Sen S, Ramakrishnan S. Minimum requirements for pediatric cardiac procedures in the Indian scenario. Ann Pediatr Card 2022;15:439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kruk ME, Gage AD, Arsenault C, et al. High-quality health systems in the sustainable development goals era: time for a revolution. Lancet Glob Health 2018;6:e1196–252. 10.1016/S2214-109X(18)30386-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Nair SM, Zheleva B, Dobrzycka A, et al. A population health approach to address the burden of congenital heart disease in Kerala, India. Global Heart 2021;16:.:71. 10.5334/gh.1034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Hesselink G, Schoonhoven L, Barach P, et al. Improving patient handovers from hospital to primary care: a systematic review. Ann Intern Med 2012;157:417–28. 10.7326/0003-4819-157-6-201209180-00006 [DOI] [PubMed] [Google Scholar]
- 27. Hesselink G, Zegers M, Vernooij-Dassen M, et al. Improving patient discharge and reducing hospital readmissions by using intervention mapping. BMC Health Serv Res 2014;14:389. 10.1186/1472-6963-14-389 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Okoroh JS, Riviello R. Challenges in healthcare financing for surgery in sub-Saharan Africa. Pan Afr Med J 2021;38:198. 10.11604/pamj.2021.38.198.27115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Jaspers L, Colpani V, Chaker L, et al. The global impact of non-communicable diseases on households and impoverishment: a systematic review. Eur J Epidemiol 2015;30:163–88. [DOI] [PubMed] [Google Scholar]
- 30. Burki S, Fraser CD. Larger centers may produce better outcomes: is regionalization in congenital heart surgery a superior model? Semin Thorac Cardiovasc Surg Pediatr Card Surg Annu 2016;19:10–3. 10.1053/j.pcsu.2015.11.001 [DOI] [PubMed] [Google Scholar]
- 31.Wang A; Ahmed, R; Ray J; Hughes P; Eric McCoy E; Marc A. Auerbach, A, Barach P. Supporting the quadruple AIM using simulation and human factors during COVID-19 care. Am J Med Qual 2021:73–83. 10.1097/01.JMQ.0000735432.16289.d2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Varkey P, Reller MK, Resar RK. Basics of quality improvement in health care. Mayo Clin Proc 2007;82:735–9. 10.4065/82.6.735 [DOI] [PubMed] [Google Scholar]
- 33. Barach PR, Jacobs JP, Laussen PC, et al. Outcomes analysis, quality improvement, and patient safety for pediatric and congenital cardiac care: theory, implementation, and applications. Progress in Pediatric Cardiology 2011;32:65–7. [Google Scholar]
- 34. Diller G-P, Kempny A, Alonso-Gonzalez R, et al. Survival prospects and circumstances of death in contemporary adult congenital heart disease patients under follow-up at a large tertiary centre. Circulation 2015;132:2118–25. [DOI] [PubMed] [Google Scholar]
- 35. Wu MH, Lu CW, Chen HC, et al. Adult congenital heart disease in a nationwide population 2000-2014: epidemiological trends, arrhythmia, and standardized mortality ratio. J Am Heart Assoc 2018;7:e007907. 10.1161/JAHA.117.007907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Videbæk J, Laursen HB, Olsen M, et al. Long-term nationwide follow-up study of simple congenital heart disease diagnosed in otherwise healthy children. Circulation 2016;133:474–83. 10.1161/CIRCULATIONAHA.115.017226 [DOI] [PubMed] [Google Scholar]
- 37. Vervoort D, Zheleva B, Jenkins KJ, et al. Children at the heart of global cardiac surgery: an advocacy stakeholder analysis. World J Pediatr Congenit Heart Surg 2021;12:48–54. 10.1177/2150135120955189 [DOI] [PubMed] [Google Scholar]
- 38. Surgery GIfCs . Optimal resources for children’s surgical care. guidelines FOR different levels of CARE. 2019. [Google Scholar]
- 39. Jacobs JP, Jacobs ML, Lacour-Gayet FG, et al. Stratification of complexity improves the utility and accuracy of outcomes analysis in a multi-institutional congenital heart surgery database: application of the risk adjustment in congenital heart surgery (RACHS-1) and aristotle systems in the Society of Thoracic Surgeons (STS) congenital heart surgery database. Pediatr Cardiol 2009;30:1117–30. 10.1007/s00246-009-9496-0 [DOI] [PubMed] [Google Scholar]
- 40. Jenkins KJ, Gauvreau K, Newburger JW, et al. Consensus-based method for risk adjustment for surgery for congenital heart disease. J Thorac Cardiovasc Surg 2002;123:110–8. 10.1067/mtc.2002.119064 [DOI] [PubMed] [Google Scholar]
- 41. Cocomello L, Caputo M, Cornish R, et al. External validation of the improving partial risk adjustment in surgery (prais-2) model for 30-day mortality after paediatric cardiac surgery. BMJ Open 2020;10:e039236. 10.1136/bmjopen-2020-039236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Allen P, Zafar F, Mi J, et al. Risk stratification for congenital heart surgery for icd-10 administrative data (RACHS-2). J Am Coll Cardiol 2022;79:465–78. 10.1016/j.jacc.2021.11.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Quinn BP, Yeh M, Gauvreau K, et al. Procedural risk in congenital cardiac catheterization (PREDIC3t). J Am Heart Assoc 2022;11:e022832. 10.1161/JAHA.121.022832 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Mattos SdaS, Hazin SMV, Regis CT, et al. A telemedicine network for remote paediatric cardiology services in north-east Brazil. Bull World Health Organ 2015;93:881–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Alkmim MB, Figueira RM, Marcolino MS, et al. Improving patient access to specialized health care: the telehealth network of Minas Gerais, Brazil. Bull World Health Organ 2012;90:373–8. 10.2471/BLT.11.099408 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. DeWyer A, Scheel A, Kamarembo J, et al. Establishment of a cardiac telehealth program to support cardiovascular diagnosis and care in a remote, resource-poor setting in Uganda. PLoS One 2021;16:e0255918. 10.1371/journal.pone.0255918 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Mahle WT, Newburger JW, Matherne GP, et al. Role of pulse oximetry in examining newborns for congenital heart disease: a scientific statement from the American Heart Association and American Academy of Pediatrics. Circulation 2009;120:447–58. 10.1161/CIRCULATIONAHA.109.192576 [DOI] [PubMed] [Google Scholar]
- 48. Group YICSS. Clinical signs that predict severe illness in children under age 2 months: a multicentre study. Lancet 2008;371:135–42. 10.1016/S0140-6736(08)60106-3 [DOI] [PubMed] [Google Scholar]
- 49. Watkins DA, Beaton AZ, Carapetis JR, et al. Rheumatic heart disease worldwide: JACC scientific expert panel. J Am Coll Cardiol 2018;72:1397–416. 10.1016/j.jacc.2018.06.063 [DOI] [PubMed] [Google Scholar]
- 50. Rogers VW, Motyka E. 5-2-1-0 goes to school: a pilot project testing the feasibility of schools adopting and delivering healthy messages during the school day. Pediatrics 2009;123 Suppl 5:S272–6. 10.1542/peds.2008-2780E [DOI] [PubMed] [Google Scholar]
- 51. Behera SK, Smith SN, Tacy TA. Impact of accreditation on quality in echocardiograms: a quantitative approach. J Am Soc Echocardiogr 2017;30:913–22. 10.1016/j.echo.2017.06.008 [DOI] [PubMed] [Google Scholar]
- 52. Mohsin S, Hasan B, Ather M, et al. Quality improvement initiative in paediatric echocardiography laboratory in a low- to middle-income country. Eur Heart J Qual Care Clin Outcomes 2022;8:821–9. 10.1093/ehjqcco/qcab084 [DOI] [PubMed] [Google Scholar]
- 53. Benavidez OJ, Gauvreau K, Jenkins KJ, et al. Diagnostic errors in pediatric echocardiography: development of taxonomy and identification of risk factors. Circulation 2008;117:2995–3001. 10.1161/CIRCULATIONAHA.107.758532 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. WHO . Guideline: updates on the management of severe acute malnutrition in infants and children, 2013. [PubMed] [Google Scholar]
- 55. Hickey PA, Connor JA, Cherian KM, et al. International quality improvement initiatives. Cardiol Young 2017;27:S61–8. 10.1017/S1047951117002633 [DOI] [PubMed] [Google Scholar]
- 56. Nathan M, Levine JC, Van Rompay MI, et al. Impact of major residual lesions on outcomes after surgery for congenital heart disease. J Am Coll Cardiol 2021;77:2382–94. 10.1016/j.jacc.2021.03.304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Lara G, Khushali S, Barach P. Simulation based medical education in graduate medical education training and assessment programs. Progress in Pediatric Cardiology 2017;44:33–42. [Google Scholar]
- 58. Vervoort D, Parikh UM, Raj A, et al. Global cardiovascular care: an overview of high-level political commitment. Asian Cardiovasc Thorac Ann 2020;28:258–65. 10.1177/0218492320930844 [DOI] [PubMed] [Google Scholar]
- 59. Hummel K, Whittaker S, Sillett N, et al. Development of an international standard set of clinical and patient-reported outcomes for children and adults with congenital heart disease: a report from the International Consortium for Health Outcomes Measurement Congenital Heart Disease Working Group. Eur Heart J Qual Care Clin Outcomes 2021;7:354–65. 10.1093/ehjqcco/qcab009 [DOI] [PubMed] [Google Scholar]
- 60. Stout KK, Daniels CJ, Aboulhosn JA, et al. 2018 AHA/ACC guideline for the management of adults with congenital heart disease: executive summary: a report of the american college of cardiology/american heart association task force on clinical practice guidelines. Circulation 2019;139:e637–97. 10.1161/CIR.0000000000000602 [DOI] [PubMed] [Google Scholar]
- 61. Johnson J, Barach P. Improving pediatric cardiac care with continuous quality improvement methods and tools. In: Barach P, Jacobs J, Laussen P, et al., eds. Outcomes Analysis, Quality Improvement, and Patient Safety for Pediatric and Congenital Cardiac Disease. New York, NY: Springer Books, 2014. [Google Scholar]
- 62.Barach P. Kleinman, L. Measuring and improving comprehensive pediatric cardiac care: learning from continuous quality improvement methods and tools. Progress in Pediatric Cardiology 2018;48:82–92. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2023-012049supp001.pdf (541.9KB, pdf)
bmjgh-2023-012049supp002.pdf (55KB, pdf)
Data Availability Statement
Data sharing not applicable as no datasets generated and/or analysed for this study.