Abstract
Rural, American Indian/Alaska Native (AI/AN) people, a population at elevated risk for complex pregnancies, have limited access to risk-appropriate obstetric care. Obstetrical bypassing, seeking care at a non-local obstetric unit, is an important feature of perinatal regionalization that can alleviate some challenges faced by this rural population, at the cost of increased travel to give birth. Data from five years (2014–2018) of birth certificates from Montana, along with the 2018 annual survey of the American Hospital Association (AHA) were used in logistic regression models to identify predictors of bypassing, with ordinary least square regression models used to predict factors associated with the distance (in miles) birthing people drove beyond their local obstetric unit to give birth. Logit analyses focused on hospital-based births to Montana residents delivered during this time period (n=54,146 births). Distance analyses focused on births to individuals who bypassed their local obstetric unit to deliver (n = 5,991 births). Individual-level predictors included maternal sociodemographic characteristics, location, perinatal health characteristics, and health care utilization. Facility-related measures included level of obstetric care of the closest and delivery hospitals, and distance to the closest hospital-based obstetric unit. Findings suggest that birthing people living in rural areas and on American Indian reservations were more likely to bypass to give birth, with bypassing likelihood depending on health risk, insurance, and rurality. AI/AN and reservation-dwelling birthing people traveled significantly farther when bypassing. Findings highlight that distance traveled was even farther for AI/AN people facing pregnancy health risks (23.8 miles farther than White people with pregnancy risks) or when delivering at facilities offering complex care (14–44 miles farther than White people). While bypassing may connect rural birthing people to more risk-appropriate care, rural and racial inequities in access persist, with rural, reservation-dwelling AI/AN birthing people experiencing greater likelihood of bypassing and travelling greater distances when bypassing.
Keywords: obstetrics/gynecology, health care disparities, rural health, racial/ethnic differences in health and health care, access/demand/utilization of services, birthing people, American Indians, Montana
INTRODUCTION
Jean Bear, a resident of Hays, Montana (located on the Fort Belknap Reservation) was referred 168.8 miles away to Billings, Montana for being high risk, pregnant with twins, because the closest Indian Health Service (IHS) clinic on her reservation lacked obstetrical services.1 Seven million rural childbearing-aged birthing people, like Jean Bear, reside in a county that lacks a birth center, obstetric [OB] provider, or hospital offering obstetric care.2 Rural American Indian/Alaska Native (AI/AN) birthing people have consistently poor access to obstetric services,3–7 especially complex obstetric care.8,9 Compared to people living in urban areas, rural birthing people are at greater risk for severe maternal morbidity and mortality.10,11 AI/AN birthing people have almost twice the odds of infant mortality and severe maternal morbidity, and four to seven times higher odds of maternal mortality, compared to non-Hispanic White individuals.12–14
IHS is an important source of health care for tribally-enrolled AI/AN people. About 60% of eligible AI/AN people use some form of IHS healthcare, which is delivered through federally run, tribally run, Urban Indian Organizations or Purchased/Referred Care (PRC) programs, largely on or near reservations;21 thereby restricting service delivery access.22 IHS is the first pre-paid health plan in the US designed to fulfill treaty obligations on behalf of the US government in exchange for tribes ceding their lands. It is not an insurance, rather it is a health service delivery system that also distributes funding to tribally led health service units.23 Today, both IHS and tribally run facilities provide care for 2.56 million AI/AN people from 574 federally recognized tribes in 37 states through a combined 46 hospitals (24 run directly by IHS), and 492 clinic units (of which 75 are IHS clinics). IHS-funded clinics provide a range of health care services, including prenatal care, to AI/AN birthing people. However, limited budgets, staffing issues, and geographic remoteness may limit access to prenatal care and contribute to inadequate prenatal care.24–26 Many smaller IHS hospital-based obstetric units have closed,28 and over 90% of AI/AN births occur outside IHS facilities.27 In the state of Montana, the focus of the current study, only one IHS-funded hospital currently provides OB services.
Rural hospital-based OB units are closing and further straining the fragile rural health care infrastructure,15 particularly in counties where more Black, Indigenous, and people of color reside.16 After losing obstetric services, rural areas experience increases in out-of-hospital, preterm births, and births at hospitals lacking obstetric services.17 As hospitals close and obstetric services are lost, infant mortality rises.18,19 Proximity to specialized services impacts service use. Rural AI/AN birthing individuals live farthest away from OB units, driving the most by distance8,20 and time.3
The Andersen-Aday behavioral model of health service use articulates that both structural characteristics of the health care delivery system and patient characteristics influence the likelihood that individuals are potentially able to access services within a system, as well as how they realize that access through utilization.30,31 Individual characteristics that shape health-seeking behavior (e.g., health risks, travel time to care, preference) operate within the constraints of the existing health care system (e.g., available space, proximity, available resources). For some birthing people, this access to health care manifests as OB bypassing.
While many birthing people seek obstetric care at the most proximal obstetric unit, others use services at a non-local obstetric unit – obstetrical bypassing – as people who do not utilize their local obstetric unit bypass to an obstetric unit farther away. Bypassing might enable people to receive more risk-appropriate care for their health needs,32,33 or may indicate lower quality of care at the bypassed hospital, or better care at the chosen hospital.34 Cost of care, distance to care, and patient characteristics are also associated with bypassing.20,34–39 Patient characteristics associated with higher bypassing rates include: complex medical diagnosis,32,34,40–44 higher income,44–47 younger age,43,46,48 private insurance,41,43 expanded insurance type,32,42 personal dissatisfaction and social-cultural reasons such as commonality with community or seeking culturally safe or concordant care.46 AI/AN people5 and patients on Medicaid or those who self-pay,41,48 are more likely to seek care at their local hospital. Low-volume hospitals are more likely to be bypassed,35 with greater bypassing towards hospitals providing complex medical procedures.37,43,47
Several factors are associated with patterns of obstetrical bypassing. Hospitals that lack a NICU are more likely to be bypassed.32 Individuals with resources tend to travel longer distances to access birth facilities with higher volume and level of care.45 Those on Medicare, Medicaid, and self-payers have lower obstetric bypass rates than those with commercial insurance, whereas birthing people with complicated births, older individuals, and non-Hispanic White birthing people all have higher bypassing rates.5,20,42,49–51 Birthing people with inadequate prenatal care are more likely to deliver locally.5 Rural birthing people, preterm births, complicated pregnancies, and individuals without access to higher levels of care bypass at higher rates, while rural birthing people on Medicaid are less likely to bypass.32,49 Higher rates of exposure to and perceptions of racial discrimination within health care settings and mistrust of providers or facilities may contribute to bypassing behavior as people seek more culturally safe care.52–55
To meet the needs of rural populations and improve perinatal outcomes, we must understand how birthing people in rural areas access health services. Montana is a good case study for understanding rural obstetric care access, as it has the lowest percentage of reproductive-aged women living within an hour’s drive of a hospital-based obstetric unit (68%) among all states in the contiguous US.56 A geographically large and remote area, recent data indicates that birthing people in Montana travel on average 42 minutes to deliver at a hospital, with 20% traveling over one hour and 5% driving over two hours.8 Some individuals traveled upwards of 10 hours to give birth. These data from Montana point to wide disparities between rural AI/AN and White birthing people in their access to OB facilities and services. Less is known about whether inequities exist among rural and AI/AN populations when giving birth at non-local facilities.
Our study makes several important contributions to the field. First, this study is the first to identify both predictors of bypassing and factors associated with the distance (in miles) birthing people drove beyond their local hospital to give birth. Second, our study generates knowledge on AI/AN birthing peoples’ bypassing behavior32 and is the first to examine racial differences in distances traveled when bypassing. Third, we examine the association between reservation-dwelling status and obstetrical bypassing, which has not been considered before. Findings suggest that multiple social determinants of health and structural barriers play a role in bypassing behavior and reveal that rural reservation-dwelling AI/AN birthing people are disproportionately burdened with more travel distance than their White counterparts.
METHODS
Data came from Montana birth certificates from 2014–2018 (n=60,461). Montana is a rural US state with the fifth-highest proportion of AI/AN population and limited access to OB services.3 Montana’s most traveled roadways are in rural areas, with only 4% of the state’s travel located within urban areas.57 Therefore, accessing OB services in this context involves greater travel distances, compared to urban areas, and is a useful context for considering rural obstetrical bypassing. Non-residents of Montana (n=961, 1.6%), records missing information on the birth facility (n=41; 0.00%) or driving distance (n = 3; 0.00%), and records for individuals who gave birth at home (n=1,440; 2.4%), at a birthing center (n=871; 1.5%) or at a hospital that did not have an obstetric unit (n = 1,027; 1.8%), were excluded for a final analytic sample of 56,117 births. Records missing values for the independent variables from the final multivariate logistic regression models were excluded from those analyses (n=1,523; 2.3%) as were records where the birthing person reported paying for childbirth using other forms of insurance (n=300; 0.01%) for a final sample of 54,146 in logistic regression models. Analyses examining driving distance were restricted to the sub-sample of bypassed births, defined as births where the birthing person traveled farther than 15 miles past their closest hospital facility with an obstetric unit to give birth (n= 6,291). The final sample in Ordinary-Least-Squares (OLS) regression models was limited to bypassing births with non-missing values on independent variables (n=5,991).
Measurements of level of OB care came from the 2018 annual survey of the AHA and includes level 1 (basic care, offering services for uncomplicated cases), level 2 (specialty care, services for all uncomplicated and most complicated cases), and level 3 (sub-specialty care, services for all complicated cases).
Measures
Dependent Variables. Our primary dependent variable was whether or not a birthing person bypassed the local hospital-based obstetric unit(s) (hereafter denoted OB unit) to give birth at a non-local OB unit (0 = no, 1 = yes). We also examined the additional distance (in miles) that individuals who bypassed drove to give birth beyond their local OB unit, following a similar approach as Kozhimannil et al.32, and defining “local” as any OB unit(s) within 15 miles of the birthing person’s closest OB unit. Driving distances were calculated from the centroid of the ZIP Code of residence to each OB unit, using a Python script to access the Google Distance Matrix API.
Independent Variables. Sociodemographic characteristics included the birthing individual’s race (AI/AN, Non-Hispanic White, Non-Hispanic Black, Non-Hispanic Asian, and Hispanic), age (in years), and education (less than high school, high school, some college, college graduate or more). Measures of location included an indicator of whether the birthing person lived on an American Indian reservation (0 = no, 1 = yes). Rurality of residence was measured at the county level, using the United States Department of Agriculture Economic Research Service Rural-Urban Continuum Code (RUCC), which classifies the rurality of a county based on both the size of the population and the adjacency to metropolitan areas.58 There are nine different RUCC categories, but all 56 counties in Montana (MT) fell into one of the following six categories:
3 “metro, population < 250,000” (5 MT counties)
5 “nonmetro, urban population > 20,000, nonadjacent to metro area” (4 MT counties)
6 “nonmetro, urban population between 2,500 and 19,999, adjacent to metro area” (4 MT counties)
7 “nonmetro, urban population between 2,500 and 19,999, nonadjacent to metro area” (14 MT counties)
8 “nonmetro, completely rural or less than 2,500 urban population, adjacent to metro area” (9 MT counties)
9 “nonmetro, completely rural or less than 2,500 urban population, nonadjacent to metro area” (20 MT counties).
Pregnancy and birth measures included binary indicators of whether the birthing individual had any previous live births, if the birth was by cesarean, and if the birth was preterm, low birth weight, or to multiples (e.g., twins; 0 = no, 1= yes). Information on the provider who attended the birth was captured with a categorical variable (1 = doctor [including MDs and DOs], 2 = midwife [including CNMs and other midwives], and 3 = other providers). A binary indicator was included if the birthing person had any of the following pregnancy risk factors: gestational diabetes, pre-gestational diabetes, gestational hypertension, pre-gestational hypertension, eclampsia, pervious preterm birth, previous poor birth outcome (including perinatal death, small for gestational age, intrauterine growth restricted), use of fertility drugs or Assisted Reproductive Technology, or previous cesarean delivery. The Kotelchuck prenatal care index was used to measure adequacy of prenatal health care utilization (ranging from 0 “no prenatal care” to 4 “adequate plus prenatal care”).59 Payment source was measured with binary indicators (self-pay, private insurance, Medicaid, military insurance, and Indian Health Services [IHS]).
Models predicting the driving distance (in miles) traveled by birthing people who bypassed also included OB unit-level measures: the OB levels of the closest hospital (i.e., the facility that was bypassed) and the birth hospital (i.e., the hospital to which they bypassed and gave birth), and the distance to the closest OB unit.
Analytic Strategy
For obstetrical bypassing analyses, we first conducted a series of logistic regression models predicting the likelihood that a birthing person bypassed their local OB unit to give birth, focusing on individual-level sociodemographic and health characteristics as predictors. Second, we conducted OLS regression models predicting the driving distance for birthing people who bypassed their closest OB unit. An Institutional Review Board determined this study was exempt from review, as data was anonymized and publicly available.
RESULTS
Descriptive data
Only 11% of birthing people in our sample bypassed their local OB unit (Table 1). Rates of bypassing were higher for individuals with: AI/AN identity, less education, at least one pregnancy risk factor, preterm births, low birth weight births, cesarean delivery, attended by a doctor, previous live birth, births to multiples, less adequate prenatal care, no health insurance, residence on a reservation, and especially among those living in rural areas (Table 1). See online appendix for descriptive information about births to AI/AN people in the sample (Table A1).
Table 1:
Descriptive Information on Births to Birthing People in Montana
| Full sample of hospital births (n=56,117) | Sub-sample of bypassed births (n=6,291) | |||
|---|---|---|---|---|
| Overall Average/Percentage | Average distance traveled to give birth (miles) | % who Bypassed | Average bypass distance traveled beyond local hospital (miles) | |
| Bypassed local hospital | 11.14% | 105.3 | 76.8 | |
| Delivered at local hospital | 88.86% | 20.3 | ||
| Lives on a reservation | 9.15% | 52.9 | 18.34% | 91.3 |
| Lives off reservation | 90.85% | 27.5 | 10.38% | 74.5 |
| Race | ||||
| White | 82.56% | 27.7 | 11.01% | 72.8 |
| Black | 0.69% | 24.5 | 7.75% | 86.0 |
| AI/AN | 10.89% | 48.7 | 14.34% | 101.4 |
| Asian | 1.28% | 20.4 | 8.10% | 62.4 |
| Hispanic | 4.58% | 25.0 | 7.13% | 72.7 |
| Age (in years) | 28.10 (min 12, max 55) | |||
| Education | ||||
| Less than high school | 10.37% | 37.5 | 13.56% | 80.0 |
| High school | 28.70% | 30.5 | 11.26% | 78.6 |
| Some college | 31.32% | 30.9 | 11.64% | 77.2 |
| College plus | 29.61% | 25.2 | 9.66% | 72.4 |
| Had pregnancy risk factor(s) | 27.88% | 33.3 | 13.10% | 87.8 |
| Had no pregnancy risk factors | 72.12% | 28.4 | 10.38% | 71.4 |
| Birth was preterm | 8.49% | 40.7 | 18.08% | 107.0 |
| Birth was not preterm | 91.51% | 28.8 | 10.48% | 71.9 |
| Birth was low birth weight | 7.14% | 40.0 | 17.83% | 106.8 |
| Birth was not low birth weight | 92.86% | 29.0 | 10.62% | 72.9 |
| Cesarean section | 30.46% | 32.1 | 13.06% | 84.7 |
| Vaginal delivery | 69.54% | 28.8 | 10.30% | 72.4 |
| Attending provider type | ||||
| Doctor (MD, DO) | 89.59% | 30.17 | 11.66% | 82.37 |
| Midwife (including CNM) | 9.77% | 26.22 | 6.82% | 79.35 |
| Other | 0.65% | 28.99 | 14.56% | 62.15 |
| Had a previous live birth | 62.30% | 31.0 | 11.60% | 78.3 |
| No previous live births | 37.70% | 27.7 | 10.36% | 73.8 |
| Birth was to multiples | 3.19% | 43.8 | 20.11% | 115.3 |
| Singleton birth | 96.81% | 29.3 | 10.84% | 74.4 |
| Kotelchuck Prenatal Care index | ||||
| No prenatal care | 0.91% | 41.4 | 11.51% | 118.6 |
| Inadequate care | 15.38% | 39.6 | 14.18% | 90.7 |
| Intermediate care | 7.71% | 35.4 | 14.44% | 74.9 |
| Adequate care | 40.94% | 27.7 | 10.59% | 66.6 |
| Adequate plus care | 35.06% | 26.1 | 9.56% | 78.6 |
| Insurance | ||||
| Self-pay | 3.17% | 37.8 | 16.10% | 87.1 |
| Private insurance | 52.11% | 27.6 | 11.17% | 73.0 |
| Medicaid | 41.14% | 31.7 | 11.12% | 80.2 |
| Military insurance | 2.13% | 22.2 | 4.22% | 65.6 |
| Indian Health Services | 1.66% | 38.6 | 8.56% | 86.7 |
| Rurality Urban Continuum Codes | ||||
| 3 | 36.82% | 15.5 | 0.59% | 159.8 |
| 5 | 29.15% | 20.1 | 6.20% | 70.1 |
| 6 | 8.22% | 37.3 | 18.30% | 45.8 |
| 7 | 15.93% | 47.0 | 28.20% | 95.5 |
| 8 | 3.58% | 61.1 | 21.85% | 64.8 |
| 9 | 6.29% | 86.9 | 37.06% | 61.8 |
Note: RUCC codes described in measurement section
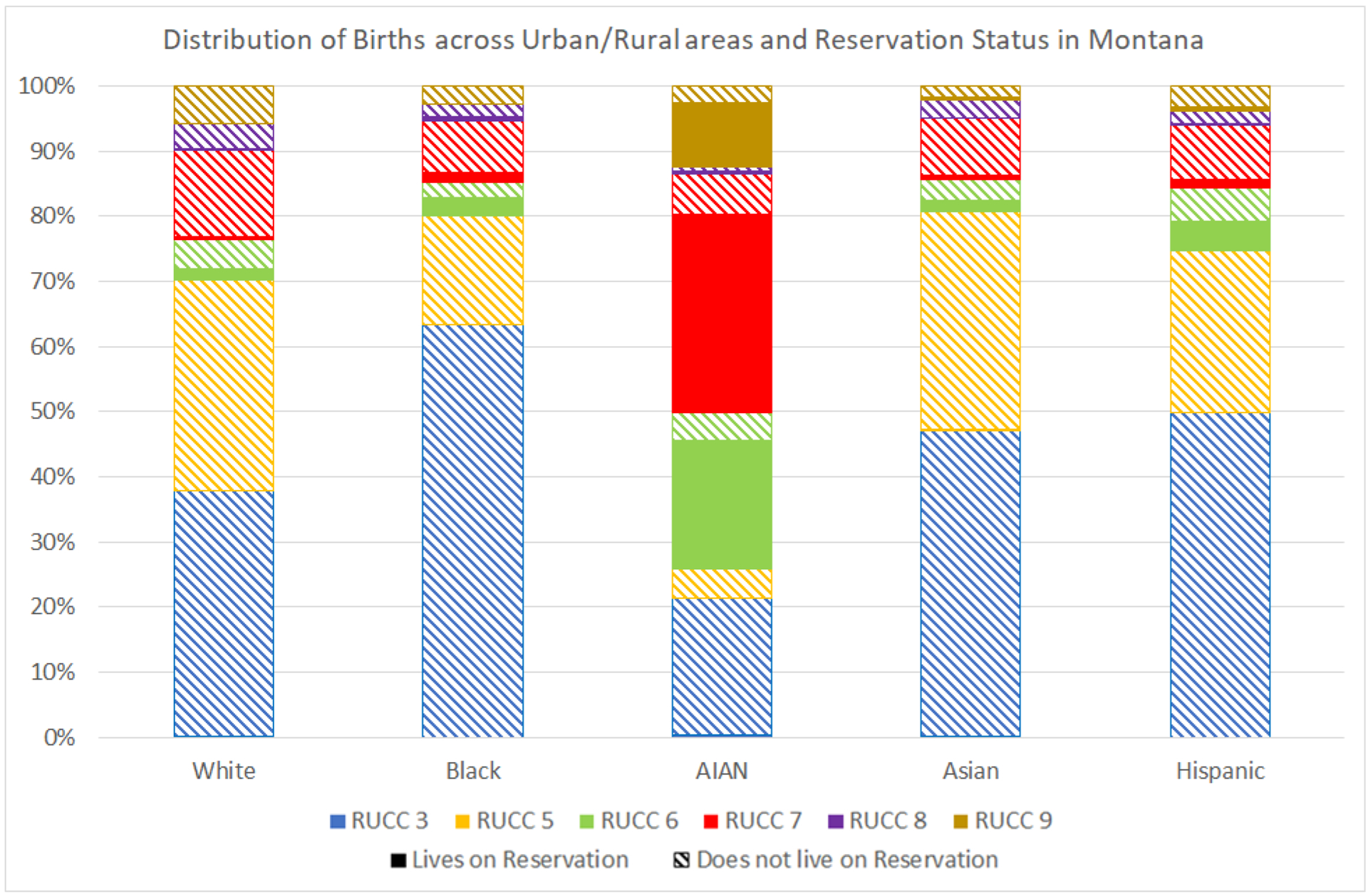
Figure 1 helps to illustrate the residential location of birthing individuals in our sample of births, by race and ethnicity and reservation-status. This figure highlights that the majority of White (70%), Black (80%), Asian (81%), and Hispanic (75%) birthing people live in metro (RUCC 3) or urban areas with populations of more than 20,000 (RUCC 5). However, only 26% of AI/AN birthing people lived in these metro or urban areas. Figure 1 further depicts that the majority of birthing people who live on reservations are AI/AN (73% of the reservation-dwelling population), with 61% of all AI/AN birthing people living on reservation. White individuals make up the second largest percentage (23%) of birthing people living on reservations. Reservation-dwelling birthing people predominantly resided in RUCC 6 (42%) or RUCC 7 (41%), representing non-metro, urban areas with populations between 2,500–19,999 either adjacent or non-adjacent to metro areas, respectively.
Figure 1:
Location of births to birthing people by location, race, and reservation status
Predicting bypassing behavior
Table 2 presents the results of multivariate logistic regression models predicting the odds of obstetric bypassing. Birthing people who lived on a reservation had 132% higher odds of bypassing compared to people who lived off-reservation (model 1). Additional nested models (not shown) indicated that the higher likelihood of bypassing among AI/AN birthing people observed in the descriptive statistics (see Table 1) was mediated by reservation status; after controlling for reservation-status, White birthing people had a significantly higher odds of bypassing compared to birthing people from other racial groups. Lower education levels and older maternal age were associated with a higher likelihood of bypassing.
Table 2:
Factors Associated with Odds of Bypassing the Nearest Hospital to give birth at a farther hospital-based obstetric unit
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
|---|---|---|---|---|---|
| Lives on Reservation | 2.322* (2.084,2.586) | 2.139** (1.885,2.427) | 2.562* (2.269,2.892) | 0.904 (0.802,1.019) | 10.63* (3.268,34.57) |
| Race (White ref) | |||||
| Black | 0.674* (0.459,0.992) | 0.670* (0.456,0.985) | 0.672* (0.457,0.989) | 1.072 (0.698,1.645) | 1.030 (0.667,1.590) |
| AI/AN | 0.763* (0.680,0.856) | 0.784* (0.698,0.881) | 0.765* (0.682,0.858) | 0.670* (0.590,0.760) | 0.591* (0.515,0.678) |
| Asian | 0.641* (0.481,0.854) | 0.641* (0.481,0855) | 0.639* (0.480,0.852) | 0.918 (0.672,1.254) | 0.934 (0.682,1.278) |
| Hispanic | 0.573* (0.489,0.671) | 0.573* (0.489,0.672) | 0.574* (0.489,0.672) | 0.764* (0.644,0.907) | 0.766* (0.644,0.910) |
| Age (in years) | 1.010* (1.004,1.016) | 1.010* (1.004,1.016) | 1.010* (1.004,1.016) | 1.015* (1.008,1.021) | 1.015* (1.008,1.021) |
| Education (college plus ref) | |||||
| Less than High School education | 1.545* (1.378,1.732) | 1.550* (1.383,1.738) | 1.545* (1.378,1.733) | 1.192* (1.054,1.347) | 1.179* (1.042,1.334) |
| High school | 1.329* (1.219,1.449) | 1.323* (1.214,1.443) | 1.331* (1.221,1.451) | 1.173* (1.068,1.289) | 1.182* (1.075,1.299) |
| Some college | 1.306* (1.210,1.410) | 1.302* (1.206,1.406) | 1.308* (1.212,1.412) | 1.121* (1.031,1.219) | 1.134* (1.042,1.233) |
| Had pregnancy risk factor(s) | 1.140* (1.066,1.218) | 1.138* (1.065,1.216) | 1.186* (1.106,1.272) | 1.181* (1.099,1.269) | 1.189* (1.106,1.279) |
| Birth was preterm | 1.543* (1.388,1.717) | 1.538* (1.382,1.711) | 1.543* (1.387,1.716) | 1.746* (1.552,1.963) | 1.764* (1.567,1.987) |
| Birth was low birth weight | 1.282* (1.144,1.438) | 1.282* (1.143,1.438) | 1.284* (1.145,1.439) | 1.505* (1.326,1.709) | 1.512* (1.330,1.719) |
| Cesarean section | 1.086* (1.018,1.158) | 1.085* (1.018,1.157) | 1.089* (1.021,1.161) | 1.060 (0.988,1.136) | 1.040 (0.969,1.116) |
| Attending provider type (Doctor ref) | |||||
| Midwife | 0.612* (0.546,0.687) | 0.613* (0.547,0.688) | 0.613* (0.547,0.687) | 0.789* (0.698,0.892) | 0.690* (0.609,0.782) |
| Other provider | 1.333 (0.984,1.807) | 1.351 (0.997,1.832) | 1.334 (0.984,1.808) | 0.497* (0.364,0.679) | 0.521* (0.381,0.713) |
| Had a previous live birth | 1.032 (0.970,1.099) | 1.031 (0.968,1.097) | 1.032 (0.970,1.099) | 0.950 (0.887,1.017) | 0.956 (0.893,1.024) |
| Birth was to multiples | 1.499* (1.305,1.722) | 1.510* (1.315,1.735) | 1.491* (1.298,1.713) | 1.596* (1.363,1.868) | 1.545* (1.318,1.811) |
| Kotelchuck Prenatal Care index (adequate plus ref) | |||||
| No prenatal care | 0.929 (0.685,1.259) | 0.960 (0.708,1.302) | 0.926 (0.683,1.255) | 0.811 (0.588,1.119) | 0.661* (0.476,0.917) |
| Inadequate care | 1.610* (1.479,1.753) | 1.611* (1.479,1.755) | 1.612* (1.480,1.755) | 1.415* (1.289,1.554) | 1.398* (1.273,1.537) |
| Intermediate care | 1.760* (1.588,1.950) | 1.758* (1.586,1.948) | 1.762* (1.590,1.953) | 1.594* (1.423,1.786) | 1.569* (1.399,1.761) |
| Adequate care | 1.286* (1.201,1.376) | 1.285* (1.200,1.376) | 1.289* (1.204,1.380) | 1.166* (1.082,1.256) | 1.148* (1.065,1.238) |
| Insurance (self-pay ref) | |||||
| Private insurance | 0.759* (0.661,0.871) | 0.737* (0.642,0.846) | 0.759* (0.661,0.872) | 0.784* (0.672,0.916) | 0.779* (0.666,0.911) |
| Medicaid | 0.597* (0.520,0.685) | 0.597* (0.520,0.685) | 0.598* (0.520,0.685) | 0.625* (0.535,0.730) | 0.627* (0.536,0.733) |
| Military insurance | 0.270* (0.196,0.371) | 0.267* (0.195,0.368) | 0.271* (0.197,0.373) | 1.132 (0.785,1.632) | 1.099 (0.760,1.588) |
| Indian Health Services (IHS) | 0.260* (0.196,0.346) | 1.709* (1.095,2.699) | 0.262* (0.197,0.348) | 0.224* (0.167,0.300) | 0.146* (0.108,0.197) |
| Reservation X Insurance | |||||
| Lives on reservation X Private Insurance | 1.543* (1.267,1.878) | ||||
| Lives on reservation X IHS | 0.100* (0.059,0.170) | ||||
| Lives on Reservation X Pregnancy risk | 0.752* (0.636,0.889) | ||||
| Rurality Urban Continuum Codes (RUCC; RUCC 3 ref) | |||||
| 5 | 12.10* (9.938,14.72) | 12.38* (10.15,15.10) | |||
| 6 | 46.25* (37.71,56.74) | 65.75* (53.32,81.09) | |||
| 7 | 84.19* (69.46,102.0) | 72.93* (59.97,88.70) | |||
| 8 | 47.76* (38.50,59.25) | 46.56** (37.39,57.98) | |||
| 9 | 118.60** (97.16,144.7) | 142.90* (116.7,175.0) | |||
| Reservation X RUCC | |||||
| Lives on reservation X RUCC 5 | 0.177* (0.043,0.738) | ||||
| Lives on reservation X RUCC 6 | 0.035* (0.011,0.114) | ||||
| Lives on reservation X RUCC 7 | 0.230* (0.070,0.755) | ||||
| Lives on reservation X RUCC 8 | 0.238* (0.067,0.853) | ||||
| Lives on reservation X RUCC 9 | 0.025* (0.007,0.084) | ||||
| Constant | 0.076* (0.060,0.096) | 0.077* (0.061,0.097) | 0.074* (0.058,0.093) | 0.004* (0.002,0.005) | 0.004* (0.003,0.005) |
| Pseudo R2 | 0.031 | 0.033 | 0.031 | 0.238 | 0.250 |
| BIC | 36797.7 | 36734.7 | 36797.4 | 29056.3 | 28634.1 |
Notes: coefficients are odds ratios; 95% confidence intervals are in parentheses; n = 54,146 births to individuals who were residents of Montana at the time of birth, who gave birth at a hospital facility
p < .05
RUCC codes described in measurement section
Several pregnancy-related characteristics were associated with bypassing. Birthing individuals who had at least one pregnancy risk factor had 14% higher odds of bypassing compared to those without any pregnancy risk factors. People with preterm births had 54% higher odds of bypassing and those with low birth-weight births had 28% higher odds of bypassing compared to those with at-term births and heavier births, respectively. People who delivered via cesarean section had 9% higher odds of bypassing compared to those delivering vaginally, while people who were attended by a doctor had 39% higher odds of bypassing compared to those attended by a midwife. People who birthed multiples had 50% higher odds of bypassing compared to those with singleton births. Birthing people receiving less adequate care were more likely to bypass compared to those with adequate plus prenatal care. No significant differences were noted among birthing people reporting no prenatal care. Birthing people who self-paid were significantly more likely to bypass, compared to those paying with private insurance (24% higher odds), Medicaid (40% higher odds), military insurance (73% higher odds), and IHS (74% higher odds). Results rotating the reference category (not shown), indicate that the odds of bypassing were highest for self-payers followed by those with private insurance, then Medicaid, with similarly low odds of bypassing for those with military and IHS coverage.
Nested regression models (not shown) indicated that the inclusion of reservation status in models with insurance variables significantly increased the magnitude of IHS and private-insurance coefficients, suggesting moderation; the association between bypassing and insurance depends on whether the individuals giving birth were reservation-dwelling. As indicated by the interaction terms (Table 2, model 2), birthing people who lived on reservation and had private insurance were more likely to bypass than those who lived on reservation and did not have private insurance, while birthing people who lived on reservation and had IHS coverage were significantly less likely to bypass than those who lived on reservation and did not have IHS coverage. Supplementary post-estimation analyses were conducted to estimate the predicted probability of bypassing by reservation and insurance status (see Appendix Table A2). According to these results, birthing people who lived off-reservation and did not have IHS coverage had a 10% probability of bypassing while people who lived off-reservation and did have IHS had a 16% probability of bypassing. For reservation-dwelling birthing people, having no IHS coverage was associated with a 24% probability of bypassing but having IHS coverage was associated with only a 5% probability of bypassing. Among birthing people living off-reservation, having no private insurance was associated with a 12% probability of bypassing while those with private insurance had a 9% probability of bypassing. While birthing people living on-reservation generally had higher probabilities of bypassing, reservation-dwelling birthing people who did not have private insurance had a slightly lower probability of bypassing (22%) compared to those who did have private insurance (24%).
To account for whether the experience of bypassing differed for individuals experiencing heightened health risk during pregnancy, supplementary analyses were conducted stratifying the regression model by pregnancy risk (results not shown). These analyses suggested that, once again, the odds of bypassing were different for birthing people living on reservation. As indicated by the interaction term in model 3, the association between pregnancy risk and bypassing was significantly lower for birthing people living on reservation compared to those living off reservation. Supplementary poste-stimation analyses were conducted to estimate the predicted probably of bypassing by reservation and pregnancy risk (see Appendix Table A1). According to these results, birthing people who lived off-reservation and had a pregnancy risk had a slightly higher predicted probability of bypassing (11%) compared to those who did not have a pregnancy risk (10% probability). However, among reservation-dwelling birthing people, the probability of bypassing was lower among birthing people whose pregnancies involved some risk factor (20%) compared to reservation-dwelling individuals who did not have any risk factors (21% probability).
As described in Figure 1, the distribution of births for birthing people of different racial groups and reservation-dwelling status varied significantly across place, such that AI/AN and reservation-dwelling individuals who gave birth are more often living in rural areas, with reservations predominantly located in RUCC 6 and 7. Results in model 4 indicate that rurality is significantly and substantially associated with the odds of bypassing. Compared to birthing people living in metro areas (RUCC 3), people living in more rural areas had between 11 to 117 times higher odds of bypassing, with birthing people living in the most rural and remote areas having the highest odds of bypassing. Also note that birthing people living in more remote regions (metro non-adjacent; RUCC 7 and RUCC 9) had significantly higher odds of bypassing, compared to their counterparts living in areas with similarly sized populations but located adjacent to metro areas (respectively, metro adjacent; RUCC 6 and RUCC 8). Comparing the results of model 1 to model 4, note that the coefficient for reservation is substantially reduced and changes direction, suggesting that part of the reason that reservation-status is associated with a higher likelihood of bypassing is because reservation-dwelling birthing people live in more rural areas.
To explore the intersection of rurality and reservation, model 5 includes interaction terms between rurality (RUCC) and reservation status. The nature of these interactions is quite nuanced. Supplementary post-estimation analyses were conducted to estimate the predicted probability of bypassing by reservation and rurality (see Appendix Table A1). According to these results, in most areas reservation-dwelling birthing people had a significantly higher predicted probability of bypassing compared to birthing people who lived off-reservation, including in metro areas (RUCC 3; 5% probability versus 0.05 % probability), urban non-metro areas with populations over 20,000 (RUCC 5; 11% versus 6% probability), and completely rural areas located adjacent to metro regions (RUCC 8; 37% versus 19% probability). Focusing on the rural regions where most reservation-dwelling birthing people live (RUCC 6 and RUCC 7), we see that adjacency to a metro region is particularly relevant for bypassing behavior. Reservation-dwelling birthing people living in urban areas with populations between 2,500 and 19,999 but adjacent to a metro region (RUCC 6) had a lower probability of bypassing (11%) than people living in similarly rural areas but off-reservation (25% probability). This perhaps reflects that OB units serving reservation-populations, that accept IHS PRC payments, are likely located in the metro regions of these areas. On the other hand, reservation-dwelling birthing people living in similarly rural but more remote areas (RUCC 7) had a significantly higher probability of bypassing (46%) compared to birthing people living in these areas but off-reservation (27%). In fact, reservation-dwelling birthing people located in these areas had the highest predicted probability of bypassing of any reservation status-by-rurality group. Finally, while reservation-dwelling birthing people living in completely rural areas but adjacent to metro regions (RUCC 8) were more likely to bypass than their counterparts living off reservation, reservation-dwelling birthing people living in completely rural and remote areas (RUCC 9) were less likely to bypass (16%) than non-reservation-dwelling individuals in similarly rural areas (41% probability). This might reflect a differential distribution of nearby facilities serving reservation-dwelling birthing individuals.
Predicting distance bypassed
Birthing people who bypassed drove on average 76.6 miles past their closest OB unit to give birth (Table 1; median = 55.8 miles, maximum = 554.7 miles). Birthing people who bypassed were more likely to bypass to facilities offering complex care (22% bypass to level 1, 32% bypass to level 2, 46% bypass to level 3), and traveled farther distances when bypassing to complex care (on average 45 miles to level 1, 84.4 miles to level 2, 86.3 miles to level 3).
Table 3 presents the results of multivariate OLS regression models predicting the distance that birthing people bypassed past their local hospital to give birth, among the sample of people who bypassed (n=5,991). Birthing people who lived on reservation traveled 9 miles farther than individuals who lived off-reservation when they bypassed, controlling for rurality, sociodemographic and perinatal health characteristics, health care utilization, and OB unit-level factors (model 1). AI/AN birthing people who bypassed traveled almost 15 miles farther than White birthing people who bypassed to give birth, all else equal. Birthing people with a college education traveled 9.5 miles farther to give birth when they bypassed compared to those without a high school education. Level of rurality was also related to the distance traveled past the closest OB unit to give birth, such that birthing people living in metro areas who bypassed traveled the greatest distance. Recall from results in Table 2 that birthing people living in urban areas were the least likely to bypass; results in Table 3 suggest that if birthing people from urban areas did bypass they would then travel quite far past their closest OB unit to give birth, often in other urban areas, demonstrating the expansive space those in Montana must travel between urban areas.
Table 3:
Factors associated with distance bypassed among birthing people who bypass their local hospital (in miles; OLS regression)
| Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |
|---|---|---|---|---|---|
| Lives on Reservation | 9.14* (3.45,14.83) | 9.19* (3.50,14.87) | 10.81* (5.03,16.59) | 8.04* (2.37,13.70) | 9.76* (4.00,15.51) |
| Race (White ref) | |||||
| Black | −1.37 (−21.87,19.13) | −1.37 (−21.87,19.13) | −1.37 (−21.87,19.13) | −1.37 (−21.87,19.13) | −1.37 (−21.87,19.13) |
| AI/AN | 14.93* (8.87,20.99) | 9.834* (3.01,16.66) | 14.00* (7.91,20.08) | −4.26 (−13.09,4.56) | −8.06 (−17.31,1.19) |
| Asian | 0.71 (−14.61,16.04) | 0.67 (−14.64,15.98) | 0.70 (−14.62,16.01) | 0.34 (−14.90,15.58) | 0.31 (−14.92,15.54) |
| Hispanic | −1.53 (−9.96,6.90) | −1.43 (−9.85,7.00) | −1.82 (−10.25,6.60) | −1.31 (−9.70,7.07) | −1.56 (−9.93,6.82) |
| Age (in years) | −0.20 (−0.50,0.10) | −0.23 (−0.53,0.08) | −0.20 (−0.50,0.10) | −0.22 (−0.52,0.08) | −0.24 (−0.54,0.06) |
| Education (college plus ref) | |||||
| Less than High School education | −9.56* (−15.23,−3.89) | −9.74* (−15.41,−4.08) | −9.33* (−14.99,−3.66) | −10.10* (−15.74,−4.46) | −9.94* (−15.58,−4.30) |
| High school | 0.57 (−3.83,4.97) | 0.49 (−3.91,4.89) | 0.68 (−3.72,5.08) | 0.72 (−3.66,5.10) | 0.77 (−3.60,5.15) |
| Some college | 2.17 (−1.79,6.12) | 2.05 (−1.91,6.02) | 2.19 (−1.77,6.14) | 1.67 (−2.26,5.61) | 1.64 (−2.30,5.57) |
| Rurality Urban Continuum Codes (RUCC; RUCC 3 ref) | |||||
| 5 | −51.03* (−67.3,−34.8) | −50.58* (−66.8,−34.4) | −51.65* (−67.9,−35.4) | −53.55* (−69.7,−37.4) | −53.90* (−70.1,−37.7) |
| 6 | −100.10* (−116.5,−86.7) | −99.55* (−116.0,−83.1) | −101.00* (−117.4,−84.6) | −100.40* (−116.8,−84.1) | −101.00* (−117.4,−84.7) |
| 7 | −45.26* (−61.4,−29.1) | −44.66* (−60.8,−28.5) | −46.13* (−62.3,−30.0) | −44.92* (−61.0,−28.9) | −45.49* (−61.6,−29.4) |
| 8 | −73.41* (−89.9,−56.9) | −72.89* (−89.4,−56.4) | −74.11* (−90.6,−57.6) | −73.91* (−90.3,−57.5) | −74.30* (−90.7,−57.9) |
| 9 | −67.36* (−83.8,−50.9) | −66.81* (−83.3,−50.4) | −68.21* (−84.7,−51.8) | −67.90* (−84.3,−51.5) | −68.44* (−84.8,−52.1) |
| Had pregnancy risk factor(s) | 10.57* (7.15,14.00) | 8.67* (5.05,12.29) | 10.56* (7.14,13.98) | 10.42* (7.01,13.83) | 9.31* (5.71,12.91) |
| Birth was preterm | 9.77* (4.10,15.44) | 9.64* (3.98,15.31) | 9.89* (4.22,15.55) | 9.21* (3.57,14.85) | 9.28* (3.64,14.91) |
| Birth was low birth weight | 10.71* (4.74,16.68) | 10.75* (4.78,16.72) | 10.56* (4.59,16.53) | 10.82* (4.88,16.76) | 10.69* (4.75,16.62) |
| Cesarean section | 1.25 (−2.07,4.57) | 1.14 (−2.18,4.46) | 1.11 (−2.20,4.43) | 1.42 (−1.89,4.71) | 1.21 (−2.09,4.51) |
| Attending provider type (Doctor ref) | |||||
| Midwife | 0.52 (−5.60,6.64) | 0.32 (−5.80,6.43) | 0.44 (−5.68,6.55) | 0.17 (−5.92,6.26) | −0.03 (−6.11,6.05) |
| Other provider | −7.79 (−23.52,7.95) | −7.71 (−23.43,8.02) | −7.64 (−23.37,8.08) | −10.55 (−26.22,5.13) | −10.34 (−26.01,5.32) |
| Had a previous live birth | 0.78 (−2.48,4.05) | 0.64 (−2.62,3.90) | 0.70 (−2.56,3.96) | 0.53 (−2.72,3.77) | 0.36 (−2.88,3.61) |
| Birth was to multiples | 15.82* (9.04,22.61) | 16.26* (9.48,23.04) | 15.75* (8.97,22.53) | 15.90* (9.16,22.65) | 16.11* (9.36,22.85) |
| Kotelchuck Prenatal Care index (No prenatal care ref) | |||||
| Inadequate care | −21.82* (−37.5,−6.2) | −22.69* (−38.3,−7.0) | −22.11* (−37.8,−6.5) | −22.13* (−37.7,−6.5) | −22.80* (−38.4,−7.19) |
| Intermediate care | −29.79* (−45.8,−13.8) | −30.81* (−46.9,−14.8) | −30.01* (−46.0,−14.0) | −29.66* (−45.6,−13.7) | −30.35* (−46.4,−14.4) |
| Adequate care | −34.40* (−50.1,−18.7) | −35.45* (−51.1,−19.8) | −34.65* (−50.3,−19.0) | −33.86* (−49.5,−18.2) | −34.62* (−50.2,−19.0) |
| Adequate plus care | −31.85* (−47.5,−16.6) | −32.79* (−48.5,−17.1) | −32.06* (−47.7,−16.4) | −31.31* (−47.0,−15.7) | −31.98* (−47.6,−16.3) |
| Payer (private insurance ref) | |||||
| Self-pay | 9.06* (2.02,16.09) | 8.96* (1.93,15.99) | 9.00* (1.97,16.03) | 9.16* (2.17,16.16) | 9.07* (2.08,16.05) |
| Medicaid | 1.52 (−1.98,5.02) | 1.51 (−1.99,5.01) | 1.34 (−2.16,4.84) | 1.38 (−2.10,4.86) | 1.21 (−2.27,4.69) |
| Military insurance | 0.60 (−15.4,16.6) | 0.20 (−15.8,16.2) | 0.59 (−15.4,16.6) | 0.36 (−15.6,16.3) | 0.13 (−15.8,16.0) |
| Indian Health Services (IHS) | −0.86 (−14.3,12.5) | −0.76 (−14.2,12.6) | 24.4* (3.53,45.2) | −0.58 (−13.9,12.7) | 24.4* (3.72,45.2) |
| OB Level of closest hospital (Level 1 ref) | |||||
| Level 2 | −0.55 (−5.97,4.87) | −0.46 (−5.87,4.96) | −0.72 (−6.14,4.69) | −0.59 (−5.98,4.80) | −0.70 (−6.09,4.68) |
| Level 3 | 34.80* (19.33,50.28) | 35.27* (19.80,50.74) | 34.09* (18.62,49.57) | 34.41* (19.02,49.80) | 33.99* (18.60,49.38) |
| Distance to closest hospital (miles) | −0.12* (−0.22,−0.03) | −0.12* (−0.22,−0.03) | −0.13* (−0.22,−0.03) | −0.14* (−0.23,−0.05) | −0.14* (−0.23,−0.05) |
| OB Level of birth hospital (Level 1 ref) | |||||
| Level 2 | 41.47* (37.1,45.8) | 41.38* (37.1,45.7) | 41.64* (37.3,46.0) | 33.95* (29.2,38.7) | 34.24* (29.5,39.0) |
| Level 3 | 48.46* (44.4,52.5) | 48.58* (44.5,52.7) | 48.58* (44.5,52.7) | 44.33* (39.9,48.8) | 44.49* (40.0,49.0) |
| Interactions | |||||
| AI/AN X Pregnancy Risk | 13.97* (5.4,22.6) | 8.27^ (−0.41,16.95) | |||
| Lives on Reservation X IHS | −42.19* (−68.9,−15.5) | −41.82* (−68.4,−15.2) | |||
| AI/AN X OB Level of birth hospital | |||||
| AI/AN X OB Level 2 | 47.82* (36.4,59.2) | 46.45* (34.9,58.0) | |||
| AI/AN X OB Level 3 | 17.19* (7.4,27.0) | 17.56* (7.7,27.4) | |||
| Constant | 126.70* (102.3,151.2) | 128.60* (104.2,153.0) | 127.90* (103.5,152.3) | 132.80* (108.5,157.1) | 134.90* (110.5,159.2) |
| R2 | 0.257 | 0.258 | 0.258 | 0.265 | 0.267 |
| BIC | 65459.6 | 65458.1 | 65458.6 | 65408.2 | 65412.1 |
Notes: confidence intervals are in parentheses; n = 5,991 births to individuals who were residents of Montana at the time of birth, who bypassed their closest hospital to give birth
p < .05
RUCC codes described in measurement section
Perinatal health characteristics were also related to distance traveled when bypassing, such that birthing people facing greater health risk traveled significantly farther when bypassing (Table 3, model 1). People experiencing at least one pregnancy risk factor traveled 10.6 miles farther when bypassing compared to those without risk factors. People whose births were preterm and low birth weight traveled 9.8 and 10.7 miles farther when bypassing, respectively, compared to people who gave birth at term and to babies of normal weight. People who gave birth to multiples traveled 15.8 miles farther when bypassing, compared to people with singleton births.
Health care utilization and characteristics of hospital facilities were also related to distance traveled. Birthing people who did not receive any prenatal care during pregnancy traveled the farthest distance when bypassing, with greater differences in distance traveled compared to birthing people who experienced inadequate (21.8 miles farther), intermediate (29.8 miles farther), adequate (34.4 miles farther), and adequate plus prenatal care (31.9 miles farther) during pregnancy. Uninsured birthing people traveled 9 miles farther to bypass compared to birthing people with private insurance. Birthing people whose closest hospital was a level 3 obstetric unit traveled 34.8 miles farther when bypassing compared to people whose closest hospital was level 1. The farther away birthing people lived from their closest OB unit, the less distance they would travel when bypassing. Finally, people who bypassed to give birth at a level 2 hospital traveled 41.5 miles and those delivering at a level 3 hospital traveled 48.5 miles farther past their local OB unit compared to those who bypassed to a level 1 hospital.
A series of nested regression models indicated a moderating role of race and reservation status for other characteristics (results available upon request); the association between bypass distance and both pregnancy risk and obstetric level of the birth hospital varied significantly for AI/AN birthing people and the association between bypass distance and IHS coverage varied by reservation-status. The inclusion of an interaction term in model 2 suggests that AI/AN birthing people with a pregnancy risk factor traveled almost 14 miles farther when bypassing compared to non-Hispanic White individuals with pregnancy risk. Results in model 3 indicate that the association between IHS payments and bypass distance traveled significantly differed by birthing person’s reservation status. Birthing people who lived off reservation paying with IHS traveled 42 miles farther when bypassing compared to people who lived on-reservation paying with IHS. Finally, results in model 4 suggest that AI/AN birthing people traveled significantly farther when bypassing to level 2 and level 3 facilities, compared to non-Hispanic White people bypassing to level 2 and level 3 facilities. Supplementary post-estimation analyses were conducted to estimate the linear prediction of bypass distance across these intersections (see Appendix Table A2). Non-Hispanic White and AI/AN people bypassing to give birth at a level 1 hospital traveled similar distances to give birth (43 miles versus 39 miles). However, AI/AN people who bypassed to give birth at a level 2 or level 3 obstetric unit traveled significantly farther to give birth (121 miles and 101 miles respectively) compared to White individuals bypassing to the same obstetric level type (77 miles and 88 miles respectively). This suggests that the burden of bypassing to seek more complex obstetric care is significantly greater for AI/AN birthing people compared to non-Hispanic Whites, even controlling for factors such as rurality, health risk, and characteristics of their local hospital.
DISCUSSION
Regionalization of health care is a strategy used to increase access to health services, especially for rural residents.60 Perinatal regionalization involves formal agreements and partnerships between service delivery sites, designed to ensure that individuals give birth at or are transferred to an obstetric unit that can provide the appropriate level of care that is needed.61 Similarly, IHS facilities have criteria when to transfer birthing people during prenatal care or for delivery through their local PRC agreement.29 Ideally, birthing people whose closest birth facility is not suited to provide an appropriate level of care would bypass to a higher-level facility that can provide those services.
Our results suggest that this is not occurring in Montana for birthing people living on a reservation and/or with an AI/AN identity. On average, individuals who bypassed to give birth drove 76.7 miles past their local OB unit. When AI/AN people bypassed they traveled significantly farther than their White counterparts. Bypassing was more common among any reservation-dwelling birthing person and involved more inconvenience in terms of distance traveled. Supplementary analyses suggest that AI/AN birthing people were more likely to bypass to lower-level facilities (31% bypass to level 1) compared to White people (20% bypass to level 1). As most AI/AN people live rurally (RUCC 6 and 7), when bypassing to higher levels of obstetric care they traveled significantly farther than their White peers who bypassed to the same obstetric level and lived in other rural areas of the state. This finding reflects the remote nature of reservations in Montana, where many AI/AN people live, as well as the poorer access to complex obstetric care among AI/AN birthing people.8 Furthermore, AI/AN individuals with pregnancy health risks were more likely to bypass to a level 1 obstetric unit (27%) and traveled significantly farther (24 miles; see Table A2) compared to bypassing White individuals with similar health risks (14%). While pregnancy risks generally increased the likelihood of bypassing, surprisingly, among reservation-dwelling birthing people, experiencing a pregnancy risk was associated with a lower likelihood of bypassing, compared to people living on reservation without any risks. Results highlight that payer source was associated with bypassing behavior in different ways for people living on- or off-reservation. Reservation-dwelling birthing people with private insurance may have actively chosen to bypass local hospitals as they had more options for care and sought perceived higher-quality facilities to receive care. Those living on reservations with IHS coverage may have been referred to deliver at non-IHS facilities by PRC. It is difficult to determine to what degree of free choice versus limitations and constraints affected delivery site choice. Future research is needed to uncover the dynamics of high bypassing rates among AI/AN and reservation-dwelling people, including how patient experiences and decision-making relate to delivery site choice (e.g., seeking culturally safe care, concerns for discrimination, perceptions or experience of “better” care at one facility over another etc.). Given the long travel distances facing rural, AI/AN, and reservation-dwelling individuals who bypass to give birth, policymakers should consider the challenges this brings for individuals and families (i.e., need for housing accommodations in non-local area, childcare coverage, etc.), and what resources are needed to support them.
Rural obstetric units are closing2 and access to obstetric care appears particularly bleak for birthing people who rely on IHS coverage. Among the twelve IHS service delivery sites in the state of Montana, only one has an obstetric unit. Despite IHS availability for some AI/AN women, those relying on IHS faced challenges accessing services, particularly among those residing off-reservation. Jean Bear’s story resonates with identified issues concerning IHS coverage. Even though Jean met tribal enrollment criteria for accessing IHS service and lived near her local IHS hospital, the facility had stopped delivering babies in the 1970s, so she was referred to another prenatal clinic (>100 miles away), and found she was high risk and referred again to a specialty clinic making her commute over 6 hours for prenatal care. Findings also highlight the challenges facing reservation-dwelling birthing people who do not have coverage under IHS, who are more likely to bypass (24%) relative to reservation-dwellers who do have IHS coverage (5%) and travel significantly farther when doing so (42 miles). This may reflect, in part, the limited options for non-tribally enrolled AI/AN people living on reservations in accessing health care. Policy makers should consider how eligibility criteria for IHS services may be further reducing access for this population of AI/AN people.
Even with longstanding legal obligations from the federal government to provide health care to Native people, IHS is chronically underfunded, likely contributing to poor AI/AN health outcomes.65–69 For example, the 2017 IHS per capita expenditures for patient health services were $3,332, compared to $9,207 per capita spending nationally.66 An inadequately funded IHS-system may be impacting the ability of AI/AN birthing people to access services in a regionalized system through bypassing, including for high-risk birthing people who might benefit from bypassing to more specialized services. Considering the lack of IHS-funded OB units and the long travel distances for AI/AN people to seek care both locally and non-locally, it is critical to ensure that there is adequate budget for PRC programs to connect birthing people with risk-appropriate care. On the other hand, investment in tribal- and IHS-sponsored facilities should be prioritized to improve consistent, long-term access to services for birthing people. In 2014, almost a decade ago, recommendations were made by the Committee on American Indian/Alaska Native Women’s Health for ensuring safety in low birth-volume IHS facilities.28 It is unclear if the recommended actions have been implemented, however the results of the current paper suggest there is work to be done.
Social determinants of health related to race and place, rooted in historical policies, contribute to structural barriers affecting health care access and use. Indian reservations were created to isolate AI/AN people. As a result of traumatic policies that devastated tribal communities (e.g. General Allotment Act that greatly diminished tribal land holdings, forced boarding school assimilation policies, termination and relocation of tribal families away from reservations into urban areas, bans on cultural practices and religious ceremonies, etc.),63 it is by design that tribes were geographically isolated from White settler resources. The repercussions of this continue today, manifesting in differential access to resources (e.g., infrastructure and economic stability), and services (e.g., healthcare). Perceived risk of racism at hospitals is another factor that may affect AI/AN birthing people’s bypassing behavior, though this is not well investigated. Addressing discrimination and building capacity for culturally-competent care may come from expanding workforce diversity, as highlighted in recent recommendations to the US Department of Health and Human Resources to fund workforce diversity initiatives (both in racial background and occupational types) to improve AI/AN maternal/infant outcomes.64
Limitations to our study include data entry bias from transcription error of self-reported data presented on birth certificates to the data system. Data gleaned from birth certificates give rough approximations of individual sociodemographic factors, and while zip codes allow us to infer approximate driving distances, we did not calculate distances from home addresses which may have resulted in longer or shorter distances traveled. While information on health insurance coverage is available from the perspective of individuals (i.e., birth certificates) we do not have information about whether providers and facilities accept particular forms of insurance.
Racial inequity in access to the available obstetric system reflects broader processes that contribute to structural racism. When racial inequities become embedded within systems, including health care systems, structural racism is manifested.70,71 Findings from this study highlight that AI/AN birthing people in Montana face an increased likelihood of bypassing local facilities and greater inconvenience in distance traveled to seek care, especially complex care. AI/AN birthing people already have documented obstacles in accessing health care including: transportation, inconsistent continuity of care, dissimilar patterns of communication, and documented concerns engaging with perinatal providers including: long wait times, lack of trust in providers, cultural insensitivity, discrimination, and providers cultivating short-term to non-existent relationships with tribal communities.54,72,73 These barriers to seeking care for AI/AN birthing people reflect individual-level inequities in access, which is a manifestation of system-level inequities in resource distribution (i.e., structural racism).22
Supplementary Material
Highlights.
Rural, American Indian (AI) people have limited access to obstetric (OB) services
Delivering at a non−local hospital, OB bypassing, may connect rural people to care
AI and reservation−dwelling people are more likely to bypass and travel farther
AI people with health risk travel farther to deliver than White people with risk
AIs travel farther to bypass to OB units with complex care, and less likely to
Funding Acknowledgement
Research reported in this manuscript was supported by the National Institute of General Medical Sciences of the National Institutes of Health under Award Number P20GM104417. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declarations of interest: none
Credit Author Statement
Maggie L. Thorsen: Conceptualization, Methodology, Software, Formal Analysis, Data Curation, Writing Original Draft, Writing – Review & Editing, Project Administration; Funding Acquisition
Sean Harris: Methodology, Software, Formal Analysis, Data Curation, Writing – Review & Editing
Janelle Palacios: Writing – Original Draft; Writing – Review & Editing
Ronald McGarvey: Software, Formal Analysis, Writing – Review & Editing, Visualization
Andreas Thorsen: Conceptualization; Methodology, Software, Data Curation, Writing – Review & Editing, Funding Acquisition
REFERENCES
- 1.Tomkins L Thrown a lifeline. How Medicaid is rebuilding healthcare on Fort Belknap. Native News. The University of Montana School of Journalism; 2017(26):4–9. https://nativenews.jour.umt.edu/2017/thrown-lifeline-fort-belknap/ [Google Scholar]
- 2.March of Dimes. Nowhere To Go: Maternity Care Deserts Across the U.S 2020. https://www.marchofdimes.org/materials/2020-Maternity-Care-Report.pdf
- 3.Rayburn WF, Richards ME, Elwell EC. Drive times to hospitals with perinatal care in the United States. Obstetrics & Gynecology. 2012;119(3):611–616. [DOI] [PubMed] [Google Scholar]
- 4.Probst JC, Moore CG, Glover SH, Samuels ME. Person and place: the compounding effects of race/ethnicity and rurality on health. American journal of public health. 2004;94(10):1695–1703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Von Reichert C, McBroom WH, Reed FW, Wilson PB. Access to health care and travel for birthing: Native American-White differentials in Montana. Geoforum. 1995;26(3):297–308. [Google Scholar]
- 6.Caldwell JT, Ford CL, Wallace SP, Wange MC, Takahashi LM . Intersection of living in a rural versus urban area and race/ethnicity in explaining access to health care in the United States. American journal of public health. 2016;106(8):1463–1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Johnson PJ, Call KT, Blewett LA The importance of geographic data aggregation in assessing disparities in American Indian prenatal care. American journal of public health. 2010;100(1):122–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thorsen ML, Harris S, McGarvey R, Palacios J, Thorsen A. Evaluating disparities in access to obstetric services for American Indian women across Montana. The Journal of Rural Health. 2022;38(1):151–160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kozhimannil K, Hung P, Casey M, Lorch S. Factors associated with high-risk rural women giving birth in non-NICU hospital settings. Journal of Perinatology. 2016;36(7):510–515. [DOI] [PubMed] [Google Scholar]
- 10.Anderson B, Gingery A, McClellan M, Rose R, Schmitz D, Schou P. NRHA policy paper: Access to rural maternity care. National Rural Health Association Policy Brief. 2019; [Google Scholar]
- 11.Kozhimannil KB, Interrante JD, Henning-Smith C, Admon LK. Rural-urban differences in severe maternal morbidity and mortality in the US, 2007–15. Health affairs. 2019;38(12):2077–2085. [DOI] [PubMed] [Google Scholar]
- 12.Kozhimannil KB, Interrante JD, Tofte AN, Admon LK. Severe maternal morbidity and mortality among indigenous women in the United States. Obstetrics and gynecology. 2020;135(2):294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bryant AS, Worjoloh A, Caughey AB, Washington AE. Racial/ethnic disparities in obstetric outcomes and care: prevalence and determinants. American journal of obstetrics and gynecology. 2010;202(4):335–343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.McKnight BK, Frankenstein S, Kingman AG, Antoine P, Levsen MJ, Letellier TL, Pilcher A, Abourezk CT, Simmons TE, Islam T, Means NS Maternal Mortality and Health Disparities of American Indian Women in South Dakota: A report by the South Dakota Advisory Committee to the U.S. Commission on Civil Rights. 2021. https://www.usccr.gov/files/2021/07-14-Maternal-Mortality-and-Health-Disparities-of-American-Indian-Women-in-South-Dakota.pdf
- 15.Hung P, Kozhimannil KB, Casey MM, Moscovice IS. Why are obstetric units in rural hospitals closing their doors? Health services research. 2016;51(4):1546–1560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hung P, Henning-Smith CE, Casey MM, Kozhimannil KB Access to obstetric services in rural counties still declining, with 9 percent losing services, 2004–14. Health affairs. 2017;36(9):1663–1671. [DOI] [PubMed] [Google Scholar]
- 17.Kozhimannil KB, Hung P, Henning-Smith C, Casey MM, Prasad S. Association between loss of hospital-based obstetric services and birth outcomes in rural counties in the United States. Jama. 2018;319(12):1239–1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Powell J, Skinner C, Lavender D, Avery D, Leeper J. Obstetric care by family physicians and infant mortality in rural Alabama. The Journal of the American Board of Family Medicine. 2018;31(4):542–549. [DOI] [PubMed] [Google Scholar]
- 19.Lorch SA, Srinivas SK, Ahlberg C, Small DS. The impact of obstetric unit closures on maternal and infant pregnancy outcomes. Health services research. 2013;48(2pt1):455–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Samuelson JL, Buehler JW, Norris D, Sadek R. Maternal characteristics associated with place of delivery and neonatal mortality rates among very‐low‐birthweight infants, Georgia. Paediatric and perinatal epidemiology. 2002;16(4):305–313. [DOI] [PubMed] [Google Scholar]
- 21.Office of the Assistant Secretary for Planning and Evaluation. Health Insurance Coverage and Access to Care for American Indians and Alaska Natives: Current Trends and Key Challenges. 2021. https://aspe.hhs.gov/sites/default/files/2021-07/aspe-aian-health-insurance-coverage-ib.pdf [Google Scholar]
- 22.Eberth JM, Hung P, Benavidez GA, et al. The Problem Of The Color Line: Spatial Access To Hospital Services For Minoritized Racial And Ethnic Groups: Study examines spatial access to hospital services for minoritized racial and ethnic groups. Health Affairs. 2022;41(2):237–246. [DOI] [PubMed] [Google Scholar]
- 23.Indian Health Service. About IHS. Accessed January 18, 2023. https://www.ihs.gov/aboutihs/
- 24.Raglan GB, Lannon SM, Jones KM, Schulkin J. Racial and ethnic disparities in preterm birth among American Indian and Alaska Native women. Maternal and child health journal. 2016;20(1):16–24. [DOI] [PubMed] [Google Scholar]
- 25.Sequist TD, Cullen T, Acton KJ. Indian Health Service innovations have helped reduce health disparities affecting American Indian and Alaska Native people. Health Affairs. 2011;30(10):1965–1973. [DOI] [PubMed] [Google Scholar]
- 26.Cromer KJ, Wofford L, Wyant DK. Barriers to healthcare access facing American Indian and Alaska Natives in rural America. Journal of community health nursing. 2019;36(4):165–187. [DOI] [PubMed] [Google Scholar]
- 27.Indian Health Service. Maternal Mortality and Morbidity in Indian Country. 2017. https://www.ihs.gov/sites/dccs/themes/responsive2017/display_objects/documents/IHSmaternalmortalityfsfinal.pdf
- 28.Waxman AG, Haffner WH, Howe J, et al. A 50-year commitment to American Indian and Alaska native women. Obstetrics & Gynecology. 2020;136(4):739–744. [DOI] [PubMed] [Google Scholar]
- 29.Indian Health Service. Indian Health Manual. Chapter 13 Maternal and Child Health: Part 3- Professional Service. Accessed January 18, 2023. [Google Scholar]
- 30.Aday LA, Andersen R. A framework for the study of access to medical care. Health services research. 1974;9(3):208. [PMC free article] [PubMed] [Google Scholar]
- 31.Andersen RM, McCutcheon A, Aday LA, Chiu GY, Bell R. Exploring dimensions of access to medical care. Health services research. 1983;18(1):49. [PMC free article] [PubMed] [Google Scholar]
- 32.Kozhimannil KB, Casey MM, Hung P, Prasad S, Moscovice IS. Location of childbirth for rural women: implications for maternal levels of care. American journal of obstetrics and gynecology. 2016;214(5):661. e1–661. e10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lorch SA, Rogowski J, Profit J, Phibbs CS Access to risk-appropriate hospital care and disparities in neonatal outcomes in racial/ethnic groups and rural–urban populations. Seminars in Perinatology. 2021;45(4):151409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Adams EK, Wright GE. Hospital choice of Medicare beneficiaries in a rural market: why not the closest? The Journal of rural health. 1991;7(2):134–152. [DOI] [PubMed] [Google Scholar]
- 35.Buczko W Bypassing of local hospitals by rural Medicare beneficiaries. The Journal of Rural Health. 1994;10(4):237–246. [DOI] [PubMed] [Google Scholar]
- 36.Roh C-Y, Lee K-H, Fottler MD. Determinants of hospital choice of rural hospital patients: the impact of networks, service scopes, and market competition. Journal of Medical Systems. 2008;32(4):343–353. [DOI] [PubMed] [Google Scholar]
- 37.Williamson HA Jr, Gary Hart L, Pirani MJ, Rosenblatt RA. Market shares for rural inpatient surgical services: where does the buck stop? The Journal of Rural Health. 1994;10(2):70–79. [DOI] [PubMed] [Google Scholar]
- 38.Gauthier B, Wane W. Bypassing health providers: the quest for better price and quality of health care in Chad. Social Science & Medicine. 2011;73(4):540–549. [DOI] [PubMed] [Google Scholar]
- 39.Bezu S, Binyaruka P, Mæstad O, Somville V. Pay-for-performance reduces bypassing of health facilities: Evidence from Tanzania. Social Science & Medicine. 2021;268:113551. [DOI] [PubMed] [Google Scholar]
- 40.Basu J, Mobley LR. Illness severity and propensity to travel along the urban–rural continuum. Health & place. 2007;13(2):381–399. [DOI] [PubMed] [Google Scholar]
- 41.Radcliff TA, Brasure M, Moscovice IS, Stensland JT. Understanding rural hospital bypass behavior. The Journal of rural health. 2003;19(3):252–259. [DOI] [PubMed] [Google Scholar]
- 42.Roh CY, Moon MJ. Nearby, but not wanted? The bypassing of rural hospitals and policy implications for rural health care systems. Policy Studies Journal. 2005;33(3):377–394. [Google Scholar]
- 43.Weigel PA, Ullrich F, Finegan CN, Ward MM. Rural bypass for elective surgeries. The Journal of Rural Health. 2017;33(2):135–145. [DOI] [PubMed] [Google Scholar]
- 44.Tai WTC, Porell FW, Adams EK Hospital choice of rural Medicare beneficiaries: patient, hospital attributes, and the patient–physician relationship. Health Services Research. 2004;39(6p1):1903–1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bronstein JM, Morrisey MA. Bypassing rural hospitals for obstetrics care. Journal of Health Politics, Policy and Law. 1991;16(1):87–118. [DOI] [PubMed] [Google Scholar]
- 46.Sanders SR, Erickson LD, Call VR, McKnight ML, Hedges DW. Rural health care bypass behavior: how community and spatial characteristics affect primary health care selection. The Journal of Rural Health. 2015;31(2):146–156. [DOI] [PubMed] [Google Scholar]
- 47.Rao KD, Sheffel A. Quality of clinical care and bypassing of primary health centers in India. Social science & medicine. 2018;207:80–88. [DOI] [PubMed] [Google Scholar]
- 48.Goldsteen RL, Falcone DJ, Broyles RW, Goldsteen K, Reilly BJ. Local factors affecting the tendency to bypass local hospitals for inpatient mental health care: an exploratory analysis. The Journal of Rural Health. 1994;10(2):89–96. [DOI] [PubMed] [Google Scholar]
- 49.Kozhimannil K, Casey M, Hung P, Prasad S, Moscovice I Women Delivering Babies in Non-Local Hospitals: Differences by Rurality and Insurance Status. June 2015. University of Minnesota Rural Health Research Center Policy Brief http://rhrc.umn.edu/wp-content/files_mf/nonlocalobpolicybrief.pdf [Google Scholar]
- 50.Phibbs CS, Mark DH, Luft HS, et al. Choice of hospital for delivery: a comparison of high-risk and low-risk women. Health Services Research. 1993;28(2):201. [PMC free article] [PubMed] [Google Scholar]
- 51.Regan M, McElroy K. Women’s perceptions of childbirth risk and place of birth. J Clin Ethics. 2013;24(3):239–52. [PubMed] [Google Scholar]
- 52.Call KT, McAlpine DD, Johnson PJ, Beebe TJ, McRae JA, Song Y. Barriers to care among American Indians in public health care programs. Medical care. 2006:595–600. [DOI] [PubMed] [Google Scholar]
- 53.Brooks-Cleator L, Phillipps B, Giles A. Culturally safe health initiatives for Indigenous Peoples in Canada: a scoping review. Canadian Journal of Nursing Research. 2018;50(4):202–213. [DOI] [PubMed] [Google Scholar]
- 54.Johnson MB. Prenatal Care for American Indian Women. MCN: The American Journal of Maternal/Child Nursing. 2020;45(4):221–227. [DOI] [PubMed] [Google Scholar]
- 55.Trivedi AN, Ayanian JZ. Perceived discrimination and use of preventive health services. Journal of general internal medicine. 2006;21(6):553–558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Rayburn WF, Richards ME, Elwell EC. Drive Times to Hospitals With Perinatal Care in the United States. Obstetrics and Gynecology. Mar 2012;119(3):611–616. doi: 10.1097/AOG.0b013e318242b4cb [DOI] [PubMed] [Google Scholar]
- 57.Montana Department of Transportation. Montana’s 2020 Traffic Statistics. 2020. https://mdt.maps.arcgis.com/apps/MapSeries/index.html?appid=71c3f510d09540688b437f38290532ff
- 58.Economic Research Service USDoA. Rural-Urban Continuum Codes Documentation. . https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/documentation/
- 59.Kotelchuck M The adequacy of prenatal care utilization index: its US distribution and association with low birthweigth. American journal of public health. 1994;84(9):1486–1489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Elrod JK, Fortenberry JL. The hub-and-spoke organization design: an avenue for serving patients well. BMC health services research. 2017;17(1):25–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Kunz SN, Phibbs CS, Profit J. The changing landscape of perinatal regionalization. Elsevier; 2020:151241. [DOI] [PubMed] [Google Scholar]
- 62.Artiga S, Ubri P, Foutz J. Medicaid and American Indians and Alaska Natives. Henry J. Kaiser Family Foundation; 2017. https://www.kff.org/medicaid/issue-brief/medicaid-and-american-indians-andalaska-natives/ [Google Scholar]
- 63.Palacios JF, Portillo CJ. Understanding Native women’s health: Historical legacies. Journal of Transcultural Nursing. 2009;20(1):15–27. [DOI] [PubMed] [Google Scholar]
- 64.US Department of Health and Human Services. Making Amends: Recommended Strategies and Actions to Improve the Health and Safety of American Indian and Alaska Native Mothers and Infants. ACIMM Report to Secretary Becerra on Birth Outcomes of AI/AN Women and Infants. 2023. [Google Scholar]
- 65.Warne D, Frizzell LB. American Indian health policy: historical trends and contemporary issues. American journal of public health. 2014;104(S3):S263–S267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.National Congress of American Indians. Health Care: Reducing Disparities in the Federal Health Care Budget. Fiscal Year Indian Budget Request. . 2019. https://www.ncai.org/07_NCAI-FY20-Healthcare.pdf
- 67.Baldwin L-M, Grossman DC, Murowchick E, et al. Trends in perinatal and infant health disparities between rural American Indians and Alaska natives and rural Whites. American Journal of Public Health. 2009;99(4):638–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Cunningham PJ, Cornelius LJ. Access to ambulatory care for American Indians and Alaska Natives; the relative importance of personal and community resources. Social Science & Medicine. 1995;40(3):393–407. [DOI] [PubMed] [Google Scholar]
- 69.Jaramillo ET, Willging CE. Producing insecurity: healthcare access, health insurance, and wellbeing among American Indian elders. Social Science & Medicine. 2021;268:113384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Gee GC, Ford CL. Structural racism and health inequities: Old issues, New Directions1. Du Bois review: social science research on race. 2011;8(1):115–132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Feagin J, Bennefield Z. Systemic racism and US health care. Social science & medicine. 2014;103:7–14. [DOI] [PubMed] [Google Scholar]
- 72.Hanson JD. Understanding prenatal health care for American Indian women in a Northern Plains tribe. Journal of Transcultural Nursing. 2012;23(1):29–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Akinade T, Kheyfets A, Piverger N, Layne TM, Howell EA, Janevic T. The influence of racial-ethnic discrimination on Women’s health care outcomes: A mixed-methods systematic review. Social Science & Medicine. 2022:114983. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


