Abstract
Background:
Perioperative bleeding is a common and potentially life-threatening complication after surgery. We sought to identify the frequency, patient characteristics, causes, and outcomes of perioperative bleeding in patients undergoing noncardiac surgery.
Methods:
In a retrospective cohort study of a large administrative database, adults age ≥45 years hospitalized for noncardiac surgery in 2018 were identified. Perioperative bleeding was defined using ICD-10 diagnosis and procedure codes. Clinical characteristics, in-hospital outcomes, and first hospital readmission within 6 months were assessed by perioperative bleeding status.
Results:
We identified 2,298,757 individuals undergoing non-cardiac surgery, among which 35,429 (1.54%) had perioperative bleeding. Patients with bleeding were older, less likely to be female, and more likely to have renal and cardiovascular disease. All-cause, in-hospital mortality was higher in patients with versus without perioperative bleeding (6.0% vs. 1.3%; adjusted OR [aOR] 2.38, 95% CI 2.26–2.50). Patients with versus without bleeding had a prolonged inpatient length of stay (6 [IQR 3–13] versus 3 [IQR 2–6] days, p<0.001). Among those who were discharged alive, hospital readmission was more common within 6 months among patients with bleeding (36.0% vs. 23.6%; adjusted HR 1.21, 95% CI 1.18–1.24). The risk of in-hospital death or readmission was greater in patients with versus without bleeding (39.8% vs. 24.5%; aOR 1.33, 95% CI 1.29–1.38). When stratified by revised cardiac risk index (RCRI), there was a stepwise increase in surgical bleeding risk with increasing perioperative cardiovascular risks.
Conclusions:
Perioperative bleeding is reported in 1 out of every 65 non-cardiac surgeries, with a higher incidence in patients at elevated cardiovascular risk. Among postsurgical inpatients with perioperative bleeding, ≈1 of every 3 patients died during hospitalization or were readmitted within 6-months. Strategies to reduce perioperative bleeding are warranted to improve outcomes following non-cardiac surgery.
Keywords: bleeding, mortality, outcomes, perioperative, rehospitalization, readmission, survival, surgery
Introduction:
Perioperative bleeding is a major complication of noncardiac surgery.1,2 Although, bleeding and thrombosis are competing risks in the perioperative period, past efforts to improve perioperative outcomes have focused on mitigation of thrombotic risks. However, in the Perioperative Ischemic Evaluation-2 (POISE-2) trial, perioperative aspirin use did not reduce the incidence of perioperative cardiovascular events but did increase the risk of major bleeding.3 More recent efforts to improve perioperative care have focused on reducing the incidence of bleeding. The POISE-3 trial recently demonstrated that tranexamic acid administered immediately before and after non-cardiac surgery significantly reduces post-operative bleeding. There was no evidence of a clinically relevant increase in cardiovascular risk associated with use of tranexamic acid, although despite narrow confidence intervals, statistical noninferiority could not be claimed.4
The impact of perioperative bleeding remains poorly characterized. In a large prospective observational study of adults undergoing non-cardiac surgery, major bleeding was strongly associated with 30-day mortality.2 Other smaller series also report associations between perioperative hemorrhage and post-operative mortality, but these studies restricted analyses to patient subgroups or subtypes of non-cardiac surgery, used transfusion as a surrogate for bleeding, or reported only short-term 30-day surgical outcomes.5–7 Outcomes after hospital discharge among patients with post-surgical bleeding are not well described. Hospital readmission is a frequently cited quality metric after noncardiac surgery, with implications to costs of care, quality of life, morbidity, and major adverse outcomes.8 To provide additional context for the impact of perioperative bleeding on perioperative care, we sought to identify the clinical characteristics and short and intermediate-term outcomes of patients hospitalized for non-cardiac surgery with and without perioperative bleeding.
Methods:
Surgical Hospitalizations
In a retrospective cohort study, adults age ≥45 years who were hospitalized for non-cardiac surgery from January through June 2018 were identified from the United States Agency for Healthcare Research and Quality (AHRQ) Healthcare Cost and Utilization Project’s (HCUP) Nationwide Readmissions Database (NRD), a large national administrative database. Patients were included if they underwent a surgical procedure in the operating room during the index hospital admission, defined by a primary International Classification of Diseases, Tenth Revision Clinical Modification (ICD-10) procedure code and a corresponding HCUP Procedure Class indicating a major therapeutic non-cardiac surgery. Primary non-cardiac surgeries were clustered by ICD-10 Clinical Classifications Software Refined (CCSR) codes into the following major surgical subtypes: endocrine surgery, otolaryngology, general surgery, genitourinary, gynecologic, neurosurgery, obstetrics, orthopedics, skin/breast, thoracic, transplant, and vascular surgery. Patients undergoing primary diagnostic procedures, cardiac surgery or invasive cardiology procedures, radiation therapy, dental surgery, and eye surgery were excluded. Among patients with multiple surgical hospitalizations during the calendar year, the first hospitalization for surgery was considered to be the index procedure in this analysis. Perioperative bleeding was identified by ICD-10 diagnosis and procedure codes for bleeding during the index surgical admission, as defined in Supplemental Table 1.9 Other perioperative complications were identified as defined in Supplemental Table 2.
Outcomes and Hospital Readmission after Perioperative Bleeding
In-hospital, all-cause mortality was recorded for all patients based on the NRD discharge disposition. Six-month hospital readmissions were identified based on methodology outlined by HCUP.10 We restricted this analysis to patients discharged between January and June 2018 to ensure complete 183-day follow-up for all patients within the calendar year. Among patients with multiple readmissions within 6 months after the index surgery, only the first readmission was included in the all-cause readmission analysis. Primary ICD-10 diagnosis codes were used to determine the indication for hospital readmission and clustered into predefined CCSR categories. In-hospital, all-cause mortality was identified from the discharge disposition during these hospital readmissions.
Subgroup and Sensitivity Analyses
We evaluated bleeding in patient subgroups stratified by age, sex, and cardiovascular risk factors based on a modified Revised Cardiac Risk Index (RCRI). To define the RCRI, we assigned 1 point for each of the following: ischemic heart disease (ICD-10 diagnosis codes I20–25, Z9861, Z955, Z951), a history of cerebrovascular disease (ICD-10 diagnosis codes I60-I69), a history of congestive heart failure (ICD-10 diagnosis codes I110, I420, I421, I50), a diagnosis of diabetes mellitus with long-term insulin use (ICD-10 Z794, Z9641), chronic kidney disease or end stage renal disease as defined by CCSR codes (ICD-10 D631, E0822, E0922, E1022, E1122, E1322, I120, I129, I130, I1310, I1311, I132, N181, N182, N183, N1830, N1831, N1832, N184, N185, N186, N189, R880, Z4901, Z4902, Z4931, Z4932), and high risk surgery defined as thoracic, vascular, or transplant surgery.11,12 To confirm that the bleeding events were indeed secondary to a major non-cardiac surgery, we performed a sensitivity analysis excluding patients who underwent a primary non-cardiac surgery intended to control bleeding or hemorrhage during the index hospitalization. We also performed a sensitivity analysis excluding patients undergoing non-cardiac transplant surgery. To evaluate the consistency of our findings across relevant subgroups, we examined the relationship between bleeding and outcomes in analyses stratified by age, sex, RCRI, and anemia and CAD status.
Statistical analysis
Categorical variables are reported as percentages and compared by Pearson’s χ2 tests. Continuous variables are reported as mean ± standard error (SE) and compared using logistic regression. Multivariable logistic regression models were generated to estimate odds ratios (OR) for in-hospital mortality and for the composite endpoint of in-hospital death or hospital readmission at 6 months, overall and in subgroup analyses, adjusted for patient demographics, cardiovascular risk factors, and comorbidities. Covariates for adjustment included: age, sex, tobacco use, hypertension, hyperlipidemia, diabetes mellitus, chronic kidney disease, coronary artery disease, congestive heart failure, valvular heart disease, atrial fibrillation and flutter, pulmonary circulatory disease, peripheral vascular disease, alcohol abuse, chronic anemia, chronic pulmonary disease, coagulopathy, dementia, depression, drug abuse, fluid and electrolyte disorders, hypothyroidism, liver disease, malignancy, obesity, neurological disorders, paralysis, peptic ulcer disease, rheumatoid arthritis / collagen vascular disease, weight loss, primary insurance payer, hospital size, hospital location, and type of non-cardiac surgery. To evaluate associations between bleeding and mortality stratified by RCRI, logistic regression models were adjusted for age, sex, and elective surgical hospitalization status. Cox proportional hazard models were used to estimate the hazard of hospital readmission at 6-months in patients with and without perioperative bleeding, after adjustment for clinical covariates.
Sampling weights were applied to determine national incidence estimates according to HCUP guidance. Statistical analyses were performed using SPSS 27 (IBM SPSS Statistics, Armonk, NY, USA). Statistical tests are two-sided and with significance levels set at <0.05.
The NRD is a publicly available, de-identified dataset, and this analysis did not require approval by an Institutional Review Board. No extramural funding was used to support this work. The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the paper and its final contents.
Results:
We identified a total of 2,298,757 patients undergoing in-hospital non-cardiac surgery between January and June 2018. Perioperative bleeding was reported in 35,429 (1.54%) patients. Patients with perioperative bleeding were older, less likely to be female, more likely to have renal disease, and more likely to have cardiovascular disease, including coronary artery disease, heart failure, valvular heart disease, atrial fibrillation or flutter, and peripheral artery disease (Table 1). Chronic anemias, coagulopathies, and malignancies were also more prevalent in patients with bleeding during surgical hospitalization. When stratified by surgery type, perioperative bleeding was most common among patients undergoing transplant (7.6%), vascular (4.4%), otolaryngology (3.7%), skin or breast (3.7%), and general (2.8%) surgeries (Figure 1).
Table 1.
Baseline characteristics of patients with and without perioperative bleeding during hospitalization for non-cardiac surgery.
| No Perioperative Bleeding (n=2,263,328) | Any Perioperative Bleeding (n=35,429) | p-value | |
|---|---|---|---|
| Age in years; mean (SEM) | 66.65 (0.068) | 67.42 (0.137) | <0.001 |
| Female Sex (%) | 1226171 (54.2%) | 15981 (45.1%) | <0.001 |
| Cardiovascular Risk Factors & Disease | |||
| Tobacco Use | 282955 (12.5%) | 4806 (13.6%) | <0.001 |
| Hypertension | 1488698 (65.8%) | 24974 (70.5%) | <0.001 |
| Hyperlipidemia | 961218 (42.5%) | 14789 (41.7%) | 0.106 |
| Diabetes Mellitus (any) | 604662 (26.7%) | 10413 (29.4%) | <0.001 |
| without chronic complications | 290302 (12.8%) | 4052 (11.4%) | <0.001 |
| with chronic complications | 329025 (14.5%) | 6744 (19%) | <0.001 |
| Chronic Kidney Disease | 300626 (13.3%) | 8048 (22.7%) | <0.001 |
| Coronary Artery Disease | 396686 (17.5%) | 9783 (27.6%) | <0.001 |
| Prior PCI | 114640 (5.1%) | 2790 (7.9%) | <0.001 |
| Prior CABG | 91383 (4%) | 2342 (6.6%) | <0.001 |
| Congestive heart failure | 185829 (8.2%) | 6280 (17.7%) | <0.001 |
| Valvular heart disease | 109042 (4.8%) | 3363 (9.5%) | <0.001 |
| Atrial Fibrillation and Flutter | 259236 (11.5%) | 7864 (22.2%) | <0.001 |
| Pulmonary circulatory disease | 13308 (0.6%) | 835 (2.4%) | <0.001 |
| Peripheral vascular disease | 182508 (8.1%) | 6109 (17.2%) | <0.001 |
| Other Comorbidities | |||
| Acquired immunodeficiency syndrome | 3354 (0.1%) | 50 (0.1%) | 0.794 |
| Alcohol abuse | 62595 (2.8%) | 1782 (5%) | <0.001 |
| Chronic Anemia (any) | 330080 (14.6%) | 7670 (21.6%) | <0.001 |
| Chronic pulmonary disease | 423506 (18.7%) | 7876 (22.2%) | <0.001 |
| Coagulopathy | 90991 (4%) | 6635 (18.7%) | <0.001 |
| Dementia | 94858 (4.2%) | 1465 (4.1%) | 0.733 |
| Depression | 309253 (13.7%) | 4509 (12.7%) | 0.002 |
| Drug abuse | 37907 (1.7%) | 731 (2.1%) | <0.001 |
| Hypothyroidism | 334627 (14.8%) | 5118 (14.4%) | 0.220 |
| Liver Disease | 85804 (3.8%) | 2727 (7.7%) | <0.001 |
| Malignancy (any) | 273406 (12.1%) | 6766 (19.1%) | <0.001 |
| Obesity | 511223 (22.6%) | 6791 (19.2%) | <0.001 |
| Other neurological disorders | 193070 (8.5%) | 3990 (11.3%) | <0.001 |
| Paralysis | 69485 (3.1%) | 2328 (6.6%) | <0.001 |
| Peptic Ulcer Disease | 21558 (1%) | 901 (2.5%) | <0.001 |
| Rheumatoid arthritis / Collagen vascular disease | 88649 (3.9%) | 1266 (3.6%) | 0.021 |
| Primary Insurance Payer | <0.001 | ||
| Medicare | 1329241 (58.8%) | 22334 (63.1%) | |
| Medicaid | 160011 (7.1%) | 2985 (8.4%) | |
| Private Insurance | 653318 (28.9%) | 8386 (23.7%) | |
| Self-Pay | 35908 (1.6%) | 572 (1.6%) | |
| Other / Unknown | 84851 (3.7%) | 1151 (3.2%) | |
| Hospital Size | <0.001 | ||
| Small | 419740 (18.5%) | 4663 (13.2%) | |
| Medium | 593173 (26.2%) | 8465 (23.9%) | |
| Large | 1250416 (55.2%) | 22300 (62.9%) | |
| Hospital Location | <0.001 | ||
| Large metropolitan area (>1 million) | 1243084 (54.9%) | 20489 (57.8%) | |
| Small metropolitan area (<1 million) | 863536 (38.2%) | 12932 (36.5%) | |
| Micropolitan areas | 125926 (5.6%) | 1702 (4.8%) | |
| Rural area | 30783 (1.4%) | 305 (0.9%) |
Figure 1.
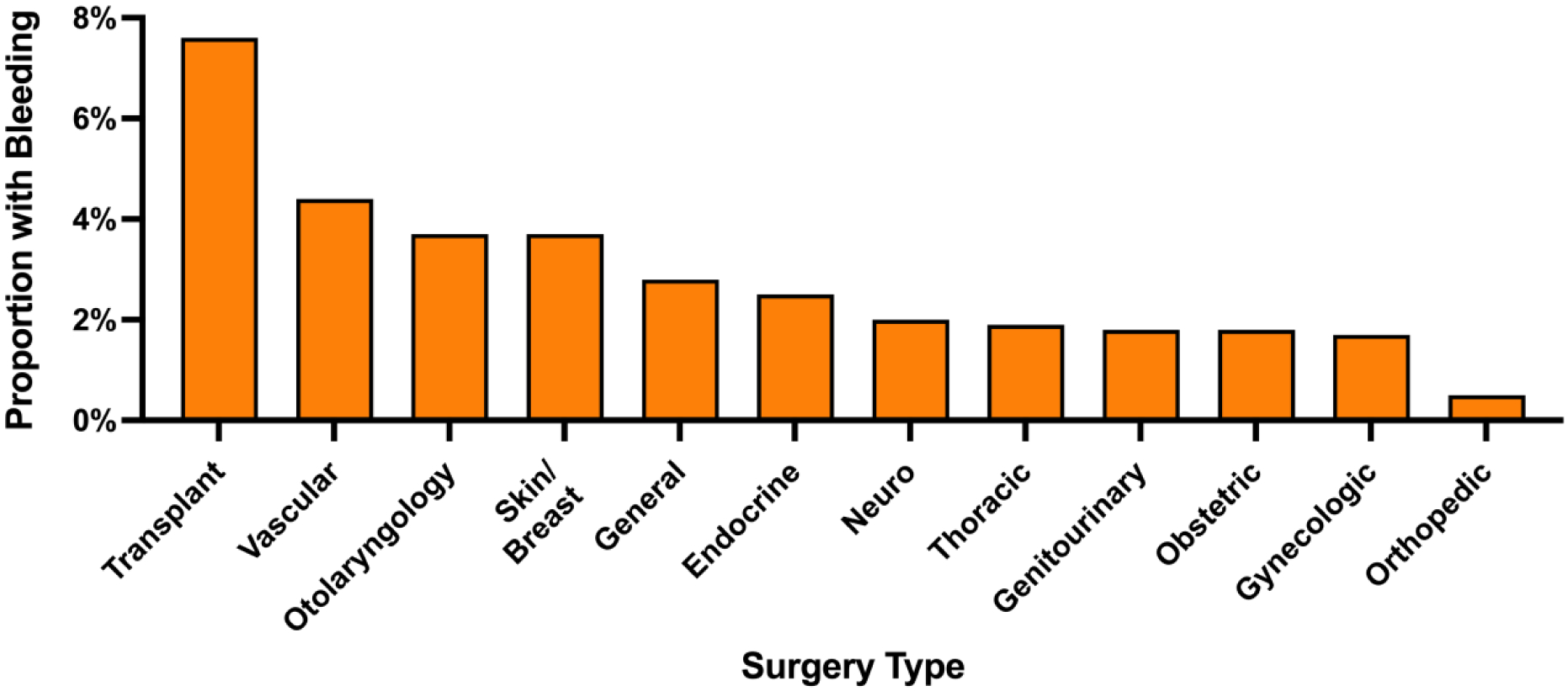
Incidence of perioperative bleeding reported by type of non-cardiac surgery.
Overall, all-cause, in-hospital mortality occurred in 1.3% patients undergoing non-cardiac surgery. Mortality was significantly higher in patients with versus without perioperative bleeding (6.0% vs. 1.3%, p<0.001; adjusted odds ratio [aOR] 2.38, 95% CI 2.26–2.50). The absolute excess mortality risk with versus without a perioperative bleed was 4.7% (95% CI 4.5% − 5.0%). Excess mortality associated with perioperative bleeding was observed in all subtypes of noncardiac surgery (Supplemental Figure 1). Patients with perioperative bleeding were more likely to develop perioperative complications, including acute myocardial infarction, respiratory failure, prolonged mechanical ventilation, septic, cardiogenic and hypovolemic shock, and vasopressor use, than patients without bleeding (Supplemental Table 3). Patients with bleeding had a longer inpatient length of stay than patients without bleeding (6 days [IQR 3–13] versus 3 days [IQR 2–6], p<0.001). Among survivors of the surgical admission, patients with perioperative bleeding were more likely to be discharged to a nursing or intermediate care facility for rehabilitation after surgery (24.0% vs. 20.4%, p<0.001, Supplemental Table 4).
Among patients who were discharged alive from the index surgical hospitalization, all-cause hospital readmission at 6 months was more common among patients with versus without perioperative bleeding (36.0% vs. 23.6%, p<0.001; unadjusted hazard ratio [HR] 1.67, 95% CI 1.63–1.72) with an absolute excess risk of readmission of 12.4% (95% CI 11.9–12.9). The cumulative incidence of hospital readmission and daily proportion of patients admitted after discharge from index surgical admissions with and without perioperative bleeding are shown in Figure 2. After adjusting for demographics, comorbidities, and surgery type, bleeding was associated with an excess hazard for hospital readmission at 6 months (adjusted HR 1.21, 95% CI 1.18–1.24, Supplemental Table 5).
Figure 2.
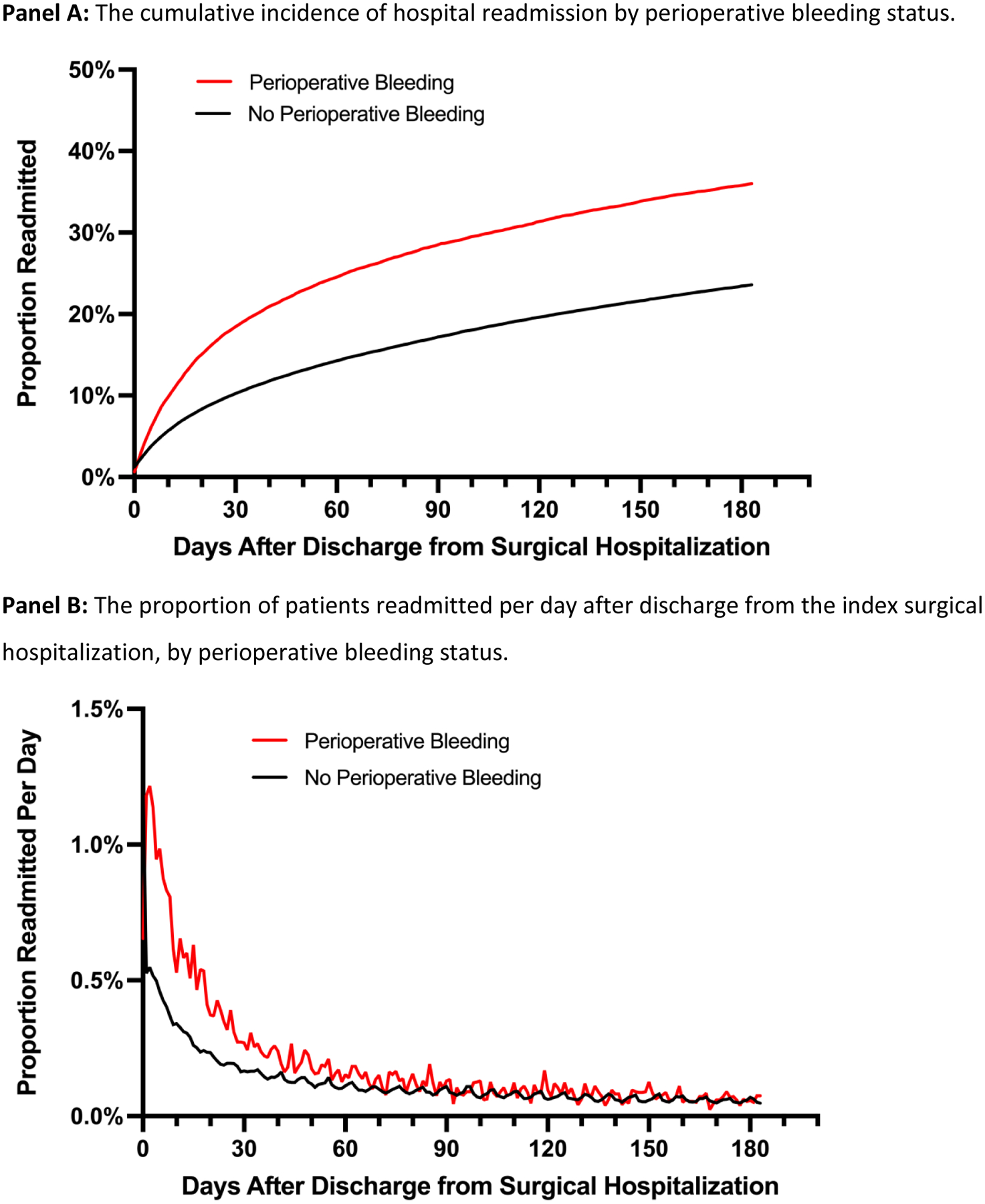
The proportion of patients readmitted to the hospital after discharge from index surgical admissions with and without perioperative bleeding.
Indications for the first hospital readmission within the 6 months following surgery, are shown in Table 2 categorized by CCSR classifications. Perioperative bleeding was associated with the largest absolute increases in the proportion of hospital readmissions for circulatory disorders (16.7% vs. 13.2%; absolute difference 3.5%, 95% CI 2.9–4.2), disease of the digestive system (14.3% vs. 12.4%; absolute difference 1.9%, 95% CI 1.3–2.6)), and genitourinary disorders (8% vs 6.1%, absolute difference 1.9%, 95% CI 1.4–2.3). Indications for hospital readmission over time among patients with and without perioperative bleeding are shown in Supplemental Figure 2. Bleeding during first readmission was more common in patients with versus without bleeding at the time of the index non-cardiac surgery (10.3% vs. 2.2%, p<0.001). During the first hospital readmission, a greater proportion of patients with prior perioperative bleeding died compared to patients without recent history of surgical bleeding (3.6% vs. 2.7%, p<0.001). Overall, the risk of in-hospital death or hospital readmission was greater in patients with versus without perioperative bleeding (39.8% vs. 24.5%, p<0.001; aOR 1.33, 95% CI 1.29–1.38, Figure 3), with an absolute excess risk of 15.3% (95% CI 14.8–15.8).
Table 2.
6-month hospital readmission in patients with and without perioperative bleeding during hospitalization for non-cardiac surgery.
| No Perioperative Bleeding (n=2,235,025) | Any Perioperative Bleeding (n=33,307) | Absolute Risk Difference (95% CI) | p-value | |
|---|---|---|---|---|
| 180-Day Hospital Readmission | 527229 (23.6%) | 11984 (36.0%) | 12.4% (11.9–12.9) | <0.001 |
| Primary Diagnosis During Hospital Readmission: | ||||
| Diseases of the Circulatory System | 69361 (13.2%) | 2003 (16.7%) | 3.6% (2.9–4.2) | |
| Diseases of the Digestive System | 65282 (12.4%) | 1717 (14.3%) | 1.9% (1.3–2.6) | |
| Diseases of the Genitourinary System | 32267 (6.1%) | 955 (8%) | 1.9% (1.4–2.3) | |
| Diseases of the Respiratory System | 29526 (5.6%) | 813 (6.8%) | 1.2% (0.7–1.6) | |
| Diseases of the Blood and Immune Mechanism | 5200 (1%) | 225 (1.9%) | 0.9% (0.6–1.1) | |
| Injury, Poisoning and External Causes* | 99410 (18.9%) | 2349 (19.6%) | 0.7% (0–1.5) | |
| Diseases of the Skin and Subcutaneous Tissue | 13007 (2.5%) | 383 (3.2%) | 0.7% (0.4–1) | |
| Infectious and Parasitic Diseases | 44891 (8.5%) | 1103 (9.2%) | 0.7% (0.2–1.2) | |
| Neoplasms | 22923 (4.3%) | 579 (4.8%) | 0.5% (0.1–0.9) | |
| Other | 25346 (4.8%) | 587 (4.9%) | 0.1% (−0.3–0.5) | |
| Unknown | 603 (0.1%) | 22 (0.2%) | 0.1% (0–0.2) | |
| Diseases of the Nervous System | 14931 (2.8%) | 317 (2.6%) | −0.2% (−0.5 to −0.1) | |
| Mental Health and Behavioral Disorders | 5899 (1.1%) | 88 (0.7%) | −0.4% (−0.5 to −0.2) | |
| Endocrine, Nutritional and Metabolic Diseases | 26435 (5%) | 402 (3.4%) | −1.7% (−2.0 to −1.3) | |
| Musculoskeletal and Connective Tissue Diseases | 72149 (13.7%) | 442 (3.7%) | −10.0% (−10.3 to −9.6) | |
| Bleeding During First Readmission | 11338 (2.2%) | 1230 (10.3%) | 8.1% (7.6 to 8.7) | <0.001 |
| In-Hospital Mortality during First Readmission | 14171 (2.7%) | 426 (3.6%) | 0.9% (0.5–1.2) | <0.001 |
Injury, Poisoning and External Causes includes: fractures, sprains, wounds, amputations, allergic reactions, drug reactions, poisoning/toxicities, and complications of devices, implants or grafts, as defined by the HCUP CCSR category.
Figure 3.
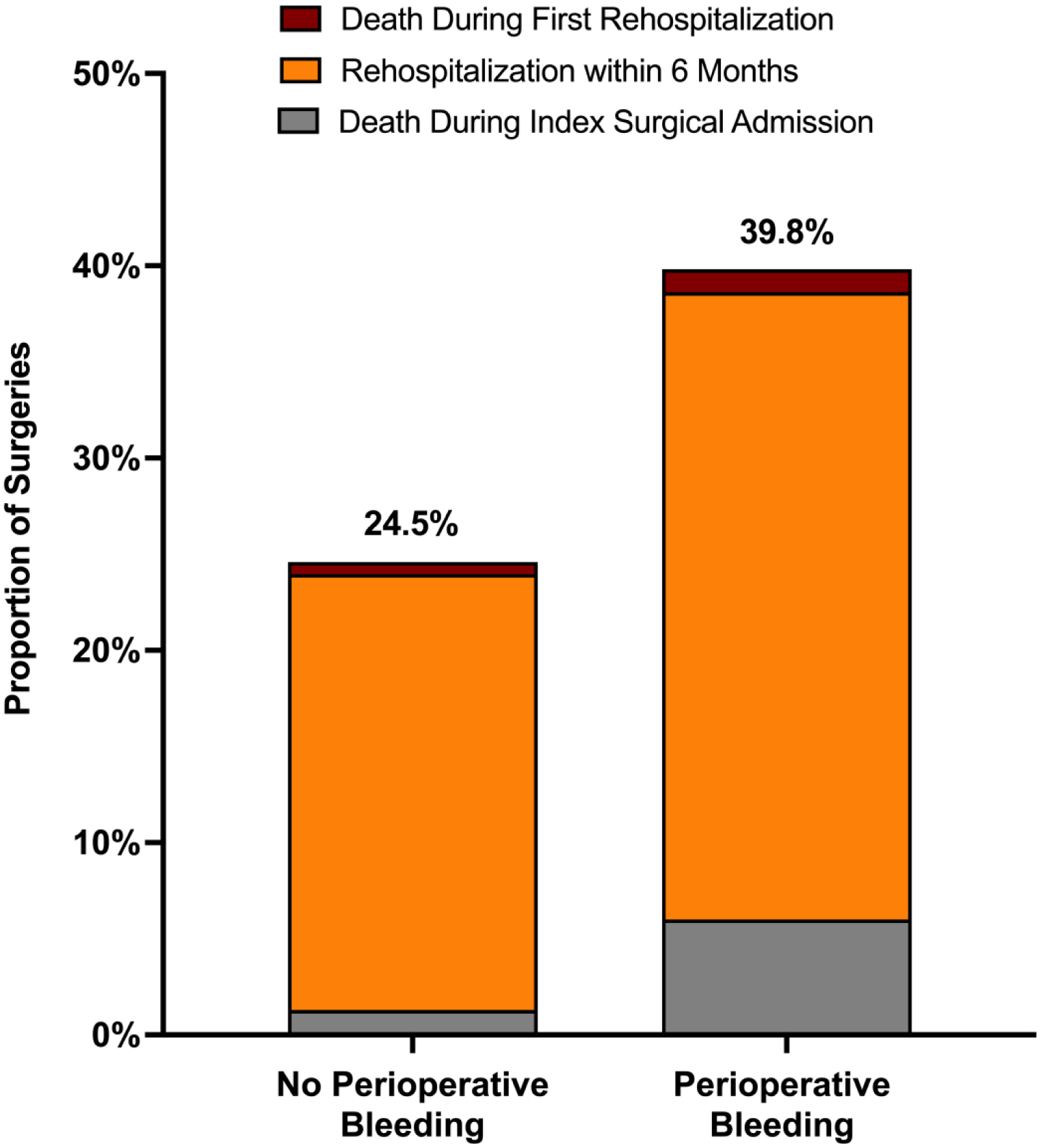
In-hospital mortality during index hospitalization, readmission to 6 months, and death during first readmission.
When stratified by sex, men had significantly higher incidence of bleeding than women (1.8% vs 1.3%, aOR 1.40, 95% CI 1.36–1.45). When stratified by RCRI, there was a stepwise increase in the incidence of bleeding with increasing perioperative cardiovascular risk, with a 1.0% bleeding risk in patients with an RCRI of 0, and a 4.1% risk of bleeding in patients with an RCRI of 4 or more (Figure 4, Panel A). At all levels of perioperative cardiovascular risk, perioperative bleeding was associated with excess in-hospital mortality (Figure 4, Panel B). Outcomes of bleeding, stratified by type of index non-cardiac surgery, are shown in Supplemental Table 6.
Figure 4.
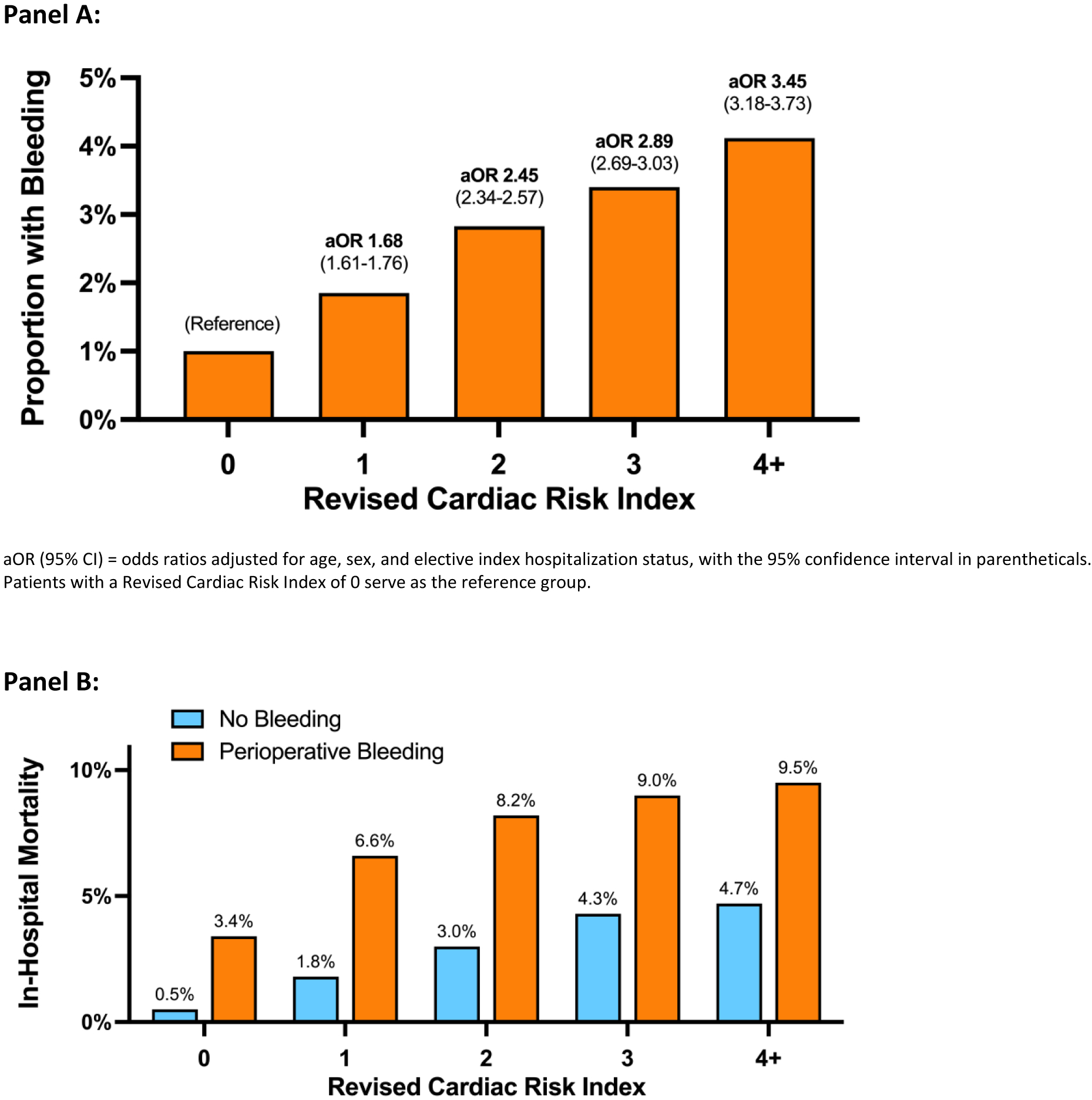
The incidence of perioperative bleeding by Revised Cardiac Risk Index (Panel A), and the risk of in-hospital mortality stratified by Revised Cardiac Risk Index and perioperative bleeding status (Panel B).
In a sensitivity analysis excluding 5,820 patients who underwent a primary non-cardiac surgery intended to control bleeding or hemorrhage, perioperative bleeding remained strongly associated with in-hospital mortality (5.0% vs. 0.9%; aOR 1.82, 95% CI 1.72–1.92), and death or all-cause readmission at 6-months (30.4% vs. 16.7%; aOR 1.31, 95% CI 1.28–1.34). In a sensitivity analysis excluding 10,856 patients who underwent non-cardiac transplant surgery, bleeding remained associated with in-hospital death (6.0% vs. 1.3%, p<0.001; aOR 2.37, 95% CI 2.25–2.50) and death or 6-month readmission (39.3% vs. 24.4%, aOR 1.33, 95% CI 1.28–1.38). In a series of subgroup analyses, bleeding was associated with excess risk of in-hospital death or readmission at 6-months in subgroups stratified by age, sex, coronary artery disease, anemia, and RCRI (Supplemental Figure 3). We identified significant interactions between bleeding and comorbidities, including coronary artery disease, anemia, and RCRI, for the endpoints of in-hospital mortality and death or readmission at 6-months (Supplemental Figure 3).
Discussion:
In this large study of patients undergoing in-hospital major non-cardiac surgery in the United States, perioperative bleeding occurred in at least 1 of every 65 surgeries, with the highest risks in transplant and vascular surgeries. Patients with perioperative bleeding were older and had a higher burden of cardiovascular and non-cardiac comorbidities. Among patients with documented perioperative bleeding, 1 in every 17 died during hospitalization, and 1 in every 3 survivors were readmitted within 6 months. Perioperative bleeding was associated with a 12.4% absolute excess risk of readmission after surgery, with the greatest increase in hospitalizations for cardiovascular indications. If approximately 5 million in-hospital non-cardiac surgeries are performed in the United States each year,11 perioperative bleeding appears to be associated with an excess of ≈3,500 perioperative deaths annually.
The current analyses extend the findings from prior observational cohorts. In an analysis of the VISION study, major bleeding (bleeding defined by a drop in hemoglobin <7.0 g/dL, transfusion of ≥1 unit of packed red blood cells, or death) occurred in 15.6% of patients and was the factor with the largest attributable fraction (17%) associated with 30-day mortality.2 We also observed that bleeding was strongly associated with in-hospital mortality, even in traditionally lower-risk patients without cardiovascular disease or anemia. Despite the sobering outcomes associated with perioperative bleeding in this and prior studies, new approaches exist to reduce the risks of perioperative bleeding, thus offering opportunities to improve short and intermediate-term clinical outcomes. The multi-national POISE-3 trial found that tranexamic acid was associated with a 24% reduction in the composite of life-threatening bleeding, major bleeding, or bleeding into a critical organ when compared to placebo.4 Applying the bleeding risk reduction observed from POISE-3 to the current study, routine use of tranexamic acid in non-cardiac surgery could decrease perioperative bleeding to fewer than 1 in every 85 surgeries, which might lead to fewer perioperative deaths, decreases in morbidity, and rehospitalizations associated with perioperative bleeding.
The complex relationship between bleeding and thrombosis also warrants consideration. Ischemic and thrombotic cardiovascular risks of non-cardiac surgery are well established, and the prevalence of cardiovascular risk factors and disease among surgical patients has increased in recent years.11,13–16 Consequently, prior efforts to improve perioperative outcomes focused on reducing perioperative thrombotic risks. In non-surgical cohorts with atrial fibrillation, many of the same risk factors predict both bleeding and thrombosis, and patients at the highest bleeding risks also have greatest risks for thromboembolism and mortality.17 Our analysis indicates a similar relationship between perioperative cardiovascular risk and the incidence of bleeding; we observed stepwise increases in bleeding risk associated with increasing RCRI. This has important practical implications, since pharmacologic efforts to mitigate perioperative bleeding, whether through cessation of antithrombotic therapy, or administration of an exogenous antifibrinolytic such as tranexamic acid, might lead to an unintended increase in thrombotic events. Conversely, administration of antithrombotic therapies can promote excess perioperative bleeding, with potentially devastating consequences.3 Perioperative bleeding may also lead to interruption (or discontinuation) of antithrombotic drugs, potentially compounding ischemic risks; in the current analysis, we observed an increase in the proportion of readmissions for circulatory disorders among patients who had perioperative bleeding. Thus, balancing the risks of bleeding and thrombosis requires careful consideration and treatment strategies must be individualized. Early re-initiation of clinically indicated antithrombotic therapies held in the setting of surgical bleeding may decrease cardiovascular rehospitalizations. Further studies are necessary to identify novel risk factors associated with excess bleeding risks and low thrombotic risks. Ultimately this would permit application of therapy to reduce bleeding in the subgroup of patients who may derive the greatest benefit.
Limitations:
This is a very large, real-world analysis of the incidence and outcomes of perioperative bleeding across multiple types of non-cardiac surgery and among patients across a spectrum of cardiovascular risk. However, there are a few notable limitations. First, data are derived from diagnosis and procedure codes recorded in the Nationwide Readmissions Database and are subject to errors in coding and reporting bias. Perioperative bleeding based on ICD-10 codes may underestimate the frequency of post-operative bleeding in routine clinical care. To maximize specificity, our definition of surgical bleeding excluded patients who received blood transfusions but did not have an ICD-10 code for bleeding during the surgical hospitalization. Since criteria for perioperative bleeding are not well defined, perioperative bleeding was based on local physician evaluation and hospital documentation. Our definition, selected for higher specificity, comes at a cost of lower sensitivity. As clinical providers may neglect to document surgical bleeding in some cases, definitions based on administrative coding data are likely to underestimate the true incidence of perioperative bleeding complications. This may bias the study findings. Other discrete clinical data, including the results of laboratory testing, are not recorded in the NRD. Consequently, baseline and post-operative nadir hemoglobin could not be used to determine the severity of anemia. Given these limitations in the source data, we were unable to align bleeding in this analysis with prior consensus definitions published by the ISTH and those used in the POISE series of trials.3,4,18,19 In-hospital and discharge medications, including antithrombotic therapy associated with increased risks of bleeding, were not recorded in the NRD and could not be included in risk models. The sequence of major non-cardiac surgery preceding bleeding could not be confirmed based on the data available in this administrative database. However, a sensitivity analysis excluding patients who underwent a primary non-cardiac surgery intended to control bleeding or hemorrhage during the index hospitalization yielded results that were consistent with our primary analyses. Although in-hospital deaths were recorded, out-of-hospital mortality following perioperative bleeding could not be determined in this analysis. Competing risks of out-of-hospital death may bias estimates of the relationship between bleeding and 6-month hospital readmission post-discharge. This may underestimate long-term risks associated with perioperative bleeding. We were unable to evaluate longer term follow-up beyond 6-months due to limitations of calendar-year datasets. Finally, we cannot exclude the possibility that perioperative bleeding is merely a marker of an unrecognized latent risk factor, such as coagulopathy, that mediates the association between surgical bleeding and adverse outcomes in the short and long term.
Conclusions:
Perioperative bleeding is reported in 1 out of every 65 non-cardiac surgeries and is strongly associated with in-hospital mortality, 6-month hospital readmission, and death or readmission at 6 months. Strategies to reduce the incidence of bleeding are needed and should be considered to improve clinical care.
Supplementary Material
Funding:
Dr. Smilowitz is supported, in part, by the National Heart, Lung, And Blood Institute of the National Institutes of Health under Award Number K23HL150315. Dr. Berger is funded, in part, by the National Heart and Lung Blood Institute of the National Institute of Health (R01HL139909 and R35HL144993).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: Dr. Smilowitz serves on an advisory board for Abbott Vascular. The remainder of the authors report no conflicts of interest to disclose.
References
- 1.Roshanov PS, Eikelboom JW, Sessler DI, et al. Bleeding Independently associated with Mortality after noncardiac Surgery (BIMS): an international prospective cohort study establishing diagnostic criteria and prognostic importance. British journal of anaesthesia. 2021;126(1):163–171. [DOI] [PubMed] [Google Scholar]
- 2.Vascular Events in Noncardiac Surgery Patients Cohort Evaluation Study I, Spence J, LeManach Y, et al. Association between complications and death within 30 days after noncardiac surgery. CMAJ. 2019;191(30):E830–E837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Devereaux PJ, Mrkobrada M, Sessler DI, et al. Aspirin in patients undergoing noncardiac surgery. N Engl J Med. 2014;370(16):1494–1503. [DOI] [PubMed] [Google Scholar]
- 4.Devereaux PJ, Marcucci M, Painter TW, et al. Tranexamic Acid in Patients Undergoing Noncardiac Surgery. N Engl J Med. 2022. [DOI] [PubMed] [Google Scholar]
- 5.Smilowitz NR, Oberweis BS, Nukala S, et al. Association Between Anemia, Bleeding, and Transfusion with Long-term Mortality Following Noncardiac Surgery. Am J Med. 2016;129(3):315–323.e312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu WC, Smith TS, Henderson WG, et al. Operative blood loss, blood transfusion, and 30-day mortality in older patients after major noncardiac surgery. Ann Surg. 2010;252(1):11–17. [DOI] [PubMed] [Google Scholar]
- 7.Obi AT, Park YJ, Bove P, et al. The association of perioperative transfusion with 30-day morbidity and mortality in patients undergoing major vascular surgery. J Vasc Surg. 2015;61(4):1000–1009 e1001. [DOI] [PubMed] [Google Scholar]
- 8.Glance LG, Kellermann AL, Osler TM, et al. Hospital readmission after noncardiac surgery: the role of major complications. JAMA surgery. 2014;149(5):439–445. [DOI] [PubMed] [Google Scholar]
- 9.Redfors B, Watson BM, McAndrew T, et al. Mortality, Length of Stay, and Cost Implications of Procedural Bleeding After Percutaneous Interventions Using Large-Bore Catheters. JAMA Cardiol. 2017;2(7):798–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barrett M, Steiner C, Andrews R, Kassed C, Nagamine M. Methodological Issues when Studying Readmissions and Revisits Using Hospital Adminstrative Data. U.S. Agency for Healthcare Research and Quality. HCUP Methods Series Report # 2011–01 Web site. https://www.hcup-us.ahrq.gov/reports/methods/2011_01.pdf. Published 2011. Updated March 9, 2011. Accessed June 1, 2017. [Google Scholar]
- 11.Smilowitz NR, Gupta N, Ramakrishna H, Guo Y, Berger JS, Bangalore S. Perioperative Major Adverse Cardiovascular and Cerebrovascular Events Associated With Noncardiac Surgery. JAMA Cardiol. 2017;2(2):181–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andersson C, Wissenberg M, Jorgensen ME, et al. Age-specific performance of the revised cardiac risk index for predicting cardiovascular risk in elective noncardiac surgery. Circ Cardiovasc Qual Outcomes. 2015;8(1):103–108. [DOI] [PubMed] [Google Scholar]
- 13.Ruetzler K, Smilowitz NR, Berger JS, et al. Diagnosis and Management of Patients With Myocardial Injury After Noncardiac Surgery: A Scientific Statement From the American Heart Association. Circulation. 2021;144(19):e287–e305. [DOI] [PubMed] [Google Scholar]
- 14.Smilowitz NR, Gupta N, Guo Y, Berger JS, Bangalore S. Perioperative acute myocardial infarction associated with non-cardiac surgery. Eur Heart J. 2017;38(31):2409–2417. [DOI] [PubMed] [Google Scholar]
- 15.Smilowitz NR, Beckman JA, Sherman SE, Berger JS. Hospital Readmission After Perioperative Acute Myocardial Infarction Associated With Noncardiac Surgery. Circulation. 2018;137(22):2332–2339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Smilowitz NR, Gupta N, Guo Y, Beckman JA, Bangalore S, Berger JS. Trends in cardiovascular risk factor and disease prevalence in patients undergoing non-cardiac surgery. Heart. 2018;104(14):1180–1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lip GY, Banerjee A, Lagrenade I, Lane DA, Taillandier S, Fauchier L. Assessing the risk of bleeding in patients with atrial fibrillation: the Loire Valley Atrial Fibrillation project. Circ Arrhythm Electrophysiol. 2012;5(5):941–948. [DOI] [PubMed] [Google Scholar]
- 18.Schulman S, Angeras U, Bergqvist D, et al. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in surgical patients. Journal of thrombosis and haemostasis : JTH. 2010;8(1):202–204. [DOI] [PubMed] [Google Scholar]
- 19.Mehran R, Rao SV, Bhatt DL, et al. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation. 2011;123(23):2736–2747. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


