Abstract
Introduction
Breast cancer (BC) is the primary cancer among women. The World Health Organization recommends a bilateral screening mammogram every 2 years for women aged 50 to 74 years. However, it has been shown that there is an absence of information about the benefits and risks of screening. Shared medical decision-making is important to ensure patients are involved in the decision process. Decision aids can facilitative this decision-making process. This article presents a protocol to evaluate the effect of a decision aid on participation rates in the French organized BC screening program.
Methods and analysis
Design and setting. The design is a 2 arm randomized controlled study, performed in the Pays de la Loire region (French West Coast). Randomization will be based on general medicine practices (Primary Care).
Participants
Women aged between 50 and 74 years, eligible for BC screening. In this region, there are 75000 women, and 2800 general practitioners eligible for recruitment.
Intervention
In the « Decision aid for organized cancer screening » arm, the intervention will distribute invitation letters to eligible women combined with the provision of decision aid to these women and their general practitioners and an incentive to implement shared medical decision-making. In the « Standard organized cancer screening » arm, only the screening invitation will be sent to eligible women.
Primary endpoint
BC screening participation rates will be assessed after an 18-month follow-up period.
Statistical analysis
In this non-inferiority trial, the percentage of women who are up-to-date with their screening at 18 months after the intervention will be compared across arms using a generalized mixed linear model.
Discussion
The research team expect to demonstrate that providing a better explanation of the benefits and risks of BC screening is not at odds with screening participation. The study results should help policy makers thinking about implementing shared medical decision-making within the framework of organized BC screening programs in the future.
Ethics and dissemination
On 6 December 2021, the protocol received a favorable opinion from the French Committee for the Protection of Persons (2021-A01583-38). This study is registered with ClinicalTrials.gov, number NCT05607849. (Version 1, November 7, 2022; https://www.clinicaltrials.gov/ct2/show/NCT05607849). The study findings will be used for publication in peer-reviewed scientific journals and presentations in scientific meetings.
Keywords: breast cancer screening, organized screening, general practitioner, randomized controlled trial, shared medical decision making, decision aid
1. Background
In 2020, breast cancer (BC) was the most commonly diagnosed cancer in women worldwide and was responsible for 1 in 6 cancer deaths (1). It was also the leading cancer in terms of incidence and mortality in French women (2).
International randomized trials have shown the effectiveness of BC screening using mammography, reporting a 15% to 20% decrease in specific mortality after 10 years of follow-up (3–8). To improve screening, the French authorities set up a national organized screening (OS) program in 2004 (9). The program targets women aged 50 to 74 years and follows World Health Organization (WHO) recommendations by inviting women at average risk for BC to have a bilateral mammogram every 2 years (10). It also provides reminders for women who have not spontaneously participated in screening within the recommended time intervals. All these invitations are sent by post. Current participation was 45.6% over the 2019-2020 period with a target of 65% (11).
Even within a framework for promoting screening, participation in screening remains an act of voluntary care and results from a health choice. In France, a citizen consultation highlighted dysfunctions in the current organization of screening and the subsequent consequences. These included a misunderstanding of the issues, and the absence of information about the benefits and risks of screening in the invitation letter sent every 2 years (12). The literature points out that the benefit/risk ratio of screening is difficult for a woman to predict from an individual perspective (3, 4, 13–16). Although participation in OS decreases mortality directly related to BC, it has significant disadvantages including false positive results, overdiagnosis and overtreatment which impact the patient’s quality of life (17). Health authorities recommend that these disadvantages are discussed in the invitation sent to these women, so that they have balanced and complete information, and can make an informed choice whether or not to participate in screening (12, 18).
Many authors have worked to improve information given to women and their involvement in the decision-making process. Shared decision-making is considered one of the fundamental approaches to improve health care quality (19, 20) Decision aids (DAs) can facilitate Shared Medical Decision-Making (SMDM). DAs should simply set out the best available evidence and the implications in terms of risks and benefits (21–23). Several DAs dealing with BC screening have been developed internationally (21, 23, 24). In 2018, the National Cancer Institute (INCa) funded the development of a DA specific to the French context as part of a call for research projects. The resulting DA was the “Discutons-mammo.fr” website, built in a collaborative and multi-professional way, and in accordance with international standards (25). The literature highlights that SMDM is best achieved if (i) women are informed about the existence of DAs and encouraged to discuss the OS with a healthcare professional (“coaching”) (26), (ii) health professionals are informed of the existence of DA, the different stages of the SMDM and the importance of their implementation (27). Finally, the use and dissemination of DAs requires evidence of their benefit, or at least evidence that DAs do not interfere with recommended care practices.
The primary objective of this study is to evaluate the impact sending a letter informing women of the existence of the DA “Discutons-mammo.fr” has on the BC screening participation rate in an organized setting, in routine practice and in the general population.
The secondary objectives are (i) to evaluate the predictive factors of using OS, and (ii) to measure the effectiveness of the intervention on SMDM implementation.
2. Methods and analysis
2.1. Design
The design is a non-inferiority, cluster, randomized controlled clinical trial with 2 parallel groups, performed in the Pays de la Loire region (West Coast of France) composed of 5 departments.
2.2. Setting
In France, all patients over the age of 16 must follow a coordinated care pathway. General practitioners (GP) are at the center of this system. They coordinate access to care and specialists, are involved in screening and must be consulted as a priority. The GP system is based on a reciprocal choice: that of the patient and that of the GP.
The study is based on the regular GP/patient pair to measure the effect of the intervention. A cluster is defined as a group of GPs within the same primary practice address.
2.3. Structure in charge of the organization of screening
OS management is entrusted to regional organizations in charge of cancer screening called CRCDC (“Centre Régional de Coordination de Dépistage des Cancers”). These organizations are in charge of collecting screening data for all women eligible for BC screening and follow-up cases with a positive or abnormal result. They collect information from health care providers (health insurance, pathology and cytology laboratories, hospital information systems, GPs, and cancer registries) involved in screening.
2.4. Participants
Women aged between 50 and 74 years at the start of the study, who are eligible for BC screening, live in the Pays de la Loire region, and are registered with a participating GP will be eligible for inclusion in the study. Any women who are being followed-up for BC or an anomaly, have a medical or family history of BC, have refused or whose GP has refused to participate in the study, have participated in other studies on BC screening, or are under guardianship or curatorship will not be eligible for inclusion. Participating GPs will be the registered GPs for the included women practicing in the Pays de la Loire region. The inclusion and exclusion criteria for women and GPs are shown in Table 1 . The list of eligible women will be extracted from the CRCDC. The association regular GP-eligible women will be realized by the health insurance system.
Table 1.
Inclusion and exclusion criteria for GPs and women.
| General practitioner | Women | |
|---|---|---|
| Inclusion criteria | Specializing in General Medicine (excluding Special Practice Mode) | 50 to 74 years old |
| Working in Pays de la Loire | Residing in Pays de la Loire | |
| Having seen more than 100 different patients in the year prior to enrolment | Eligible for organized screening for the month in question | |
| Present on the patient list of a participating GP | ||
| Affiliated to the health insurance system | ||
| Non-inclusion criteria | Refusing to participate in the study | Having a regular GP refusing to participate in the study |
| Working in a Health Center | Affiliated with a health center | |
| Participating in other breast cancer screening studies | Participating in other breast cancer screening studies | |
| Under curatorship-tutorship | ||
| Excluded from organized screening because they have a history of breast cancer | ||
| Having ongoing follow-up (breast cancer or abnormality or medical surveillance or high-risk woman) |
GP, General Practitioner.
2.5. Randomization
GPs will be clustered within practices to avoid contamination bias stemming from shared tracking mechanisms and communication among GPs within a practice. As a result, two GPs working in a given practice will be assigned to the same study arm. The women will then be allocated to the same arm as their GP.
2.6. Intervention and control procedures
One intervention arm and one control arm are planned.
In the “Decision aid for organized cancer screening” group (intervention arm), the intervention will combine sending letters to women and their GP. Women will receive their invitation to have a mammogram accompanied by a flyer mentioning the existence of the DA and encouraging them to consult their GP to make a shared decision. Physicians will receive a letter informing them of the correspondence their patients have received, the existence of the DA, a presentation of the different stages of SMDM and an incentive for their implementation.
In the “Standard organized cancer screening” group (control arm), the intervention will be limited to sending invitation letters, corresponding to the national standard (9).
2.7. Participant blinding and informed consent
The GPs and women in the intervention and control arms will receive a regulatory letter by post informing them that they are participating in a study on screening ( Figure 1 ). Opposition to participation in the study is possible in both arms for women and GPs.
Figure 1.
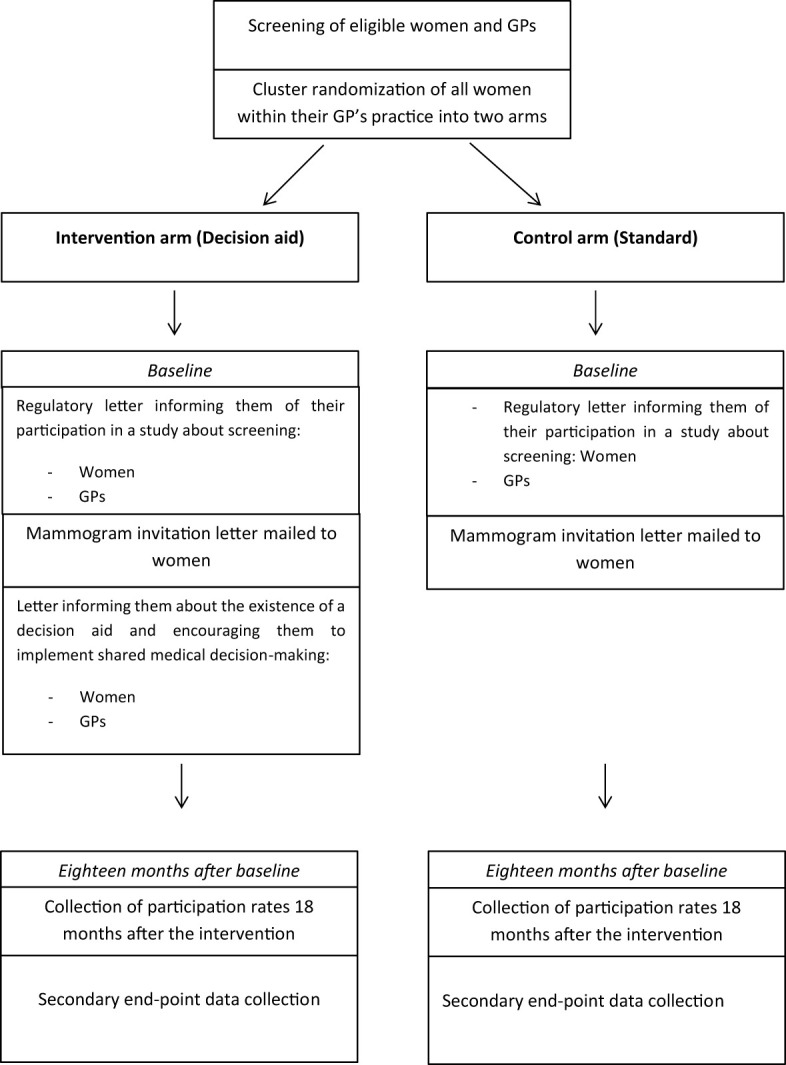
Study design.
2.8. Objectives, primary endpoint, and judgement criterion
2.8.1. Primary objective and primary endpoint
The main part of this study is to assess whether sending information to women and GPs mentioning the existence of DAs and encouraging SMDM implementation along with the screening information letter (intervention arm) affects participation rate in BC OS, compared to only sending the invitation letter to eligible women (control arm) (see Supplementary Material 1 ).
The primary outcome is the participation rate in BC OS, in each arm during the 18 months following the invitation being sent. This duration takes into account the waiting times observed to benefit from screening mammography (see Supplementary Material 1 ).
2.8.2. Secondary objectives and evaluation criteria
2.8.2.1. Assessing the predictive factors of the use of organized screening
The first secondary objective is to assess the predictive factors of OS use. Several studies have reported social inequalities in screening (28, 29). Suggested factors include increased age (30) and lower socio-economic status (31). Proxies of economic status are complementary health insurance status and French DEPrivation index of the place of residence. Therefore, as an associated secondary outcome, the study plans to collect the participation rate according to age and socio-economic level (beneficiaries of the Complementary Solidarity Health and municipality of residence according to the deprivation index).
In addition, the irregularity of women’s medical follow-up (32), the presence of a chronic pathology (33, 34) or psychiatric disorders (35, 36), and previous non-participation in screening (32) have also been reported as explanatory factors for non-participation in screening. Data will therefore also be collected over the 18-month period before and after the intervention to assess the health of participating women based on the Charlson Comorbidity Index (37) using the French health data collection system. Data will include: (i) the number of consultations and home visits to/by different healthcare professionals (GPs, midwives, gynecologists), and the number of journeys by taxi or medical transport, (ii) the prescription of certain reimbursed treatments and examinations performed (see Supplementary Material 2 ), (iii) participation in other cancer screenings.
2.8.2.2. Measure SMDM implementation and assess the level of decision-making conflict
The second secondary objective is to measure the effect of the intervention on SMDM implementation and quality, as part of an ancillary study. While the use of DAs is still marginal in occupational practices, the study should provide a better understanding of how such a tool is used and perceived when it is made available to healthcare professionals.
To assess the SMDM quality, a composite criterion will be used. The validated Shared Decision Making Questionnaire (SDM-Q-9) (38) will be used to evaluate SMDM implementation. The validated Decisional Conflict Scale (DCS) will be used to assess decision-making conflict (39). Intent to participate will be measured using a multiple-choice question. Knowledge about OS and women’s doubts, questions and concerns will be assessed and collected using a questionnaire created for the study. Secondary outcomes will be SDM-Q9 and DCS scores, intention to participate and level of knowledge. This will be measured 2 months after the intervention, in a sample of women from each study arm (see Supplementary Material 1 ).
2.9. Collected data source
The CRCDC and the French Health Insurance System will collect the data needed to conduct the research in their databases. These data will be transferred to an open project space within the National Health Data System (NSDS) allowing their analysis. This data transfer will be carried out in accordance with the data protection regulations that govern personal data protection in the European Union. The Health Insurance data managers will pair the data collected from these databases at the patient level and proceed to data pseudonymization before analyses by the statistician.
2.10. Statistical analysis
All data will be described globally and by randomization arm. The research is a non-inferiority clinical trial. The statistical unit is the woman eligible for screening. The materiality threshold will be set at 5% in a bilateral situation. Statistical analyses will be performed using R 3.6.0 software (R Foundation for Statistical Computing, Vienna, Austria. URL https://www.R-project.org/).
2.10.1. Main criterion
The percentage of women having undergone BC screening, 18 months after the intervention, will be compared between the arms using a generalized linear mixed model, to adjust the analysis for the random effect of the practice.
A two-sided 95% confidence interval of the difference in participation rates between the two arms will be calculated. The lower bound of this confidence interval will be compared to the non-inferiority margin. Non-inferiority will be demonstrated if the lower bound of the confidence interval is greater than the margin of non-inferiority defined at 2%, on the Intention to Treat (ITT) population and Per-Protocol population. If non-inferiority is demonstrated and if the participation rate in the intervention arm is higher than the participation rate in the control arm, the hypothesis will be verified with a superiority test (bilateral at 5%, according to the same model as that of the non-inferiority analysis) (40). If the test is significant, it will be concluded that the participation rate in the intervention arm is significantly higher than the participation rate in the control arm.
2.10.2. Exploratory secondary analyses
Participation rates in exploratory subgroup analyses will be studied in the same manner as the primary endpoint. The same margin of non-inferiority will be used. There is no provision for alpha risk adjustment for these analyses. The different subgroups are: (i) women aged 50 to 59/60 to 69/70 to 74 years at baseline, (ii) beneficiaries/not beneficiaries of the Complementary Solidarity Health at baseline, (iii) women who consulted/did not consult at least one GP, gynecologist or midwife (during the follow-up period for women who did not have a bilateral mammogram during the 18 months, or from baseline until the date of the bilateral mammogram for women who had the screening) (iv) women residing in a municipality with a low deprivation index (per quintile of the deprivation index) (41).
Predictors of OS use will be assessed using a multivariate generalized mixed model fitted to the physician as a random effect, and as fixed effects: (i) the number of visits to the treating physician, GP, gynecologist, or midwife in the 18 months prior to enrolment, and from baseline to bilateral mammography or to the end of the follow-up period for women who did not have bilateral mammography, (ii) the woman’s age at baseline, (iii) the presence of a chronic condition measured via chronic drug use and testing, (iv) previous participation in OS.
A stepwise algorithm based on the Akaike information criterion (AIC) will be implemented to select variables that provide meaningful information independent of the main factors.
SMDM quality will be measured using the DCS and SDM-Q9 scales, responses to participation intent and knowledge of women about the OS. It will be compared between groups using a Student superiority test.
The care pathway of the women responding to the questionnaires will be studied and in particular the concordance between patients’ intention and effective participation in BC screening.
2.10.3. Analysis population
Statistical analyses will be performed on all randomized physicians and patients included in the study. As data are collected on medico-administrative databases, very little missing data is expected (only the very rare case of women changing reimbursement schemes). If these women did not have a mammogram as part of the OS at the time of their change of plan affiliation, they will be considered non-participants for the assessment of the primary endpoint in the ITT analysis. Women who died during the study period and had not had a mammogram at the time of death, will also be considered non-participants for the assessment of the primary endpoint. The same applies to women who underwent individual screening during the study period.
A sensitivity analysis on a Per-Protocol population will be performed by removing from the analysis patients for whom a return mail has been received (for example “No longer living at the address indicated”)), patients who have moved outside the Pays de la Loire region, patients who have changed regular GP, patients whose regular GP has ceased to practice during the study period or has died, patients who have been individually screened, who do not enter OS for known medical reasons after the start of the study, or who died during the follow-up period.
2.11. Statistical justification for sample size
2.11.1. Main study sample
Based on a participation rate in 2020 of 49% for the five participating departments (11) assuming a margin of non-inferiority of 2 points to demonstrate that participation is non-inferior in the intervention arm, and considering a power of 80% and a bilateral alpha risk of 5%, the number of women to be included is equal to 9,808 in each arm, being a total of 19,616 women.
There are 2,847 GPs in the five departments (42). Considering that GPs operate from 1,570 different practices (42) the number of women targeted per practice will be 48. With an average cluster size of 48 women and an intraclass coefficient of 5%, the number of subjects to be included to account for this cluster randomization must be multiplied by 3.35, or 65,647 women (32,824 per group).
The number of GPs included will be approximately 2,847 in the five departments. The recruitment potential is approximately 25,000 women per month (personal communication from the CRCDC). The inclusion will therefore be done over 3 consecutive months.
2.11.2. Ancillary study sample
In her article, Pérez-Lacasta observed a difference in the decision-making conflict scale score between women who received information and those who did not of 18.53 vs. 13.77 (standard deviation at 20.25) (43). On these assumptions, 762 responses would be required to arrive at a significant difference.
The ancillary survey conducted by questionnaire to assess SMDM quality will be carried out on an independent sample of 5,000 women, equally divided between the 2 arms. Based on a response rate of 20%, the number of questionnaires collected will be 1,000.
2.12. Justification of the non-inferiority margin
In a non-inferiority trial, the margin chosen must meet two criteria: (i) be less than the differences observed in the superiority trials already conducted, and (ii) be less than the Minimal Clinically Important Difference.
International evidence on whether the use of DAs changes participation in the OS is scarce, without clear direction. It may therefore result in an increase (44) or a decrease in participation rates (45). Recent studies do not show a change in participation rates when women are invited to participate in decision-making (43, 46, 47).
The non-inferiority margin was set at 2% in agreement with the BC OS medical experts at the CRCDC. This is the largest difference in clinically acceptable OS participation. The Cochrane literature review reports an average of 1 death averted per 2,000 women screened over 10 years (44), the observation of 10 healthy women who would not have been diagnosed if they had not participated in screening and who will be treated unnecessarily (44). Thus, of the 75,000 women who will be included in the study, and according to our participation hypotheses, a 2% decrease in participation in the intervention group would imply the non-screening of 750 women. No additional deaths from BC are expected following the procedure, but between 3 and 4 women will not be treated unnecessarily.
The trial will therefore be conclusive if the lower bound of the two-sided 95% confidence interval of the difference in participation between the randomization arms is greater than 2.
2.13. Status and study schedule
The beginning of the intervention will correspond to letters being sent to the included women and their GPs (T0).
The ancillary study will begin 2 months after T0, with a follow-up at 2 months.
Patients will be followed for 18 months. The freezing of the OS participation database within 18 months will be carried out 30 months after the intervention (M30). This schedule takes into account the time required for data entry. All statistical analyses and valuations of results will be conducted from M30.
Table 2 presents the time schedule for enrolment, intervention, and assessments.
Table 2.
Time schedule for enrolment, intervention and assessments.
| Study period | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Enrollment | allocation | Postallocation | Closeout | |||||||
| TimePoint | _t1 | 0 | t1 | t2 | t3 | t4 | t5 | … T18 | T30 | |
| Enrollment: | ||||||||||
| Eligibility screen | X | |||||||||
| Inform consent (main study) Inform consent (ancillary study) |
X | X | X | |||||||
| Allocation | X | |||||||||
| Interventions: | ||||||||||
| Decision aid for organized cancer screening | X | X | X | …. X | ||||||
| Standard organized cancer screening | X | X | X | …. X | ||||||
| Evaluations: | ||||||||||
| Proportion of women aged 50 to 74 who had a screening mammogram 18 months after the procedure. | X | |||||||||
| Participation rate 18 months after the intervention according to age, socio-economic level, medical follow-up, presence of a chronic pathology, psychiatric pathology, previous participation in screening. | X | |||||||||
| SDM-Q9 and DCS scores 2 months after the start of the intervention. | X | |||||||||
| Answers to the intention to participate questionnaire, answers to the knowledge questionnaire 2 months after the start of the intervention. | X | |||||||||
SDM-Q9, Shared Decision Making Questionnaire; DCS, Decisional Conflict Scale. X = realization of the stage.
2.14. Patient involvement
Women were involved in designing and developing the DA.
2.15. Data storage and retention
Directly identifying and pseudonymized data relating to women and professionals willing to participate in the research will be kept in active database, in the CRCDC and French health insurance system information systems, up to two years after the last publication of the research results or, in the absence of publication, until the final research report has been signed. Pseudonymized data will also be kept in additional archives by archiving on paper and computer media for a period of fifteen years. These durations are based on the regulations applicable to research compliant with MR003 Reference Methodology, according to deliberation 2018-154 of May 3, 2018.
This study protocol has been prepared according to the 2013 SPIRIT guideline for clinical trial protocols (48). It was recorded in ClinicalTrials.gov (number NCT05607849, November 7, 2022; Version 1).
3. Discussion
3.1. Results and expected benefits of the DEDICACES study
The DEDICACES (“DEcision partagée dans le cadre du DépIstage du CAnCEr du Sein en soins premiers”) study should make it possible to evaluate whether the provision of a French DA (in accordance with international standards, built with patients and professionals) modifies participation in BC OS. At the end of the study, the research team expects to demonstrate that providing a better explanation of the benefits and risks of BC screening is not at odds with screening participation. Some women may choose not to participate, while others may choose to participate. In total, the average participation could therefore remain equivalent to the current participation rates. In addition, providing a DA without modifying participation would be significant progress in informing women and reducing decision-making conflict (and therefore better adherence). In this scenario, DA and SMDM on cancer screening for women would also meet societal demands for greater ethical practice in medical care for individuals.
While formalized SMDM practices in France are still rare, the study should make GPs aware of SMDM in BC screening. It will thus increase GP expertise on this topic and enable them to better answer their patients’ questions potentially leading to an increase in the number of women participating in screening.
Finally, the main perspective of the study is the generalization of DAs, which will be made available to women and healthcare professionals involved in BC screening.
Foreign literature has fed into the reflection of this study. International evidence on whether DA use modifies screening participation is scarce and results are contradictory (24, 44, 45, 49). A Cochrane literature review (44) reported that better informing women about their cancer risk and screening may increase participation, reporting a low level of evidence based on 3 studies (44, 50). On the other hand, the DECIDEO study born conducted in France reported a (limited) decrease in participation, estimated at 2% (45). Controlled trials have been performed evaluating tools to measure the effectiveness of shared decision interventions. These improve women’s knowledge about participation options and promote clear choices for BC screening (43, 51–53). On the other hand, the results for decision regret and decision conflict are more variable (43, 49, 52, 54, 55). There is uncertainty about whether interventions targeting both patients and healthcare professionals increase SMDM, compared to an intervention targeting either member of the pair (27). Furthermore, while factors associated with low participation have been widely described (28, 29, 56–58) literature does not report a relationship between DA availability and improved use of screening mammography for women meeting the criteria associated with lower participation.
Overall, these studies reveal the need for a robust and large-scale evaluation as we propose in this protocol. The central role of the regular GP in the care pathway, makes France an ideal location to conduct this study.
3.2. Strengths and limitations
The proposed research is characterized by the robustness of the design. Randomization is performed on GP medical practices with the aim of limiting confounding bias between arms. Research is also distinguished by its power; it is conducted in a region of western France, with differences in ease of access to healthcare professionals and screening participation. The trial will include several thousand women, about 4 to 30 times more than other studies evaluating DAs for screening mammography (24). Finally, the study is characterized by its reproducibility. The design is built with the intention of screening, and the intervention is easily reproducible.
There are some limitations. The content of the consultation with the GP cannot be studied. The ancillary study, which will be conducted on a small sample of women, will provide initial answers about SMDM quality using a questionnaire. Low response rates to postal questionnaires may limit the available data for this analysis. However, the use of prepaid return envelopes and a reminder should increase the response rate to questionnaires.
Ethics statement
On 6 December 2021, the protocol received a favorable opinion from the French Committee for the Protection of Persons (2021-A01583-38). The CRCDC will distribute information on the study protocol to healthcare professionals (GPs, gynecologists, midwives) in the region by post 3 months before the intervention. A separate letter informing physicians randomized to the intervention arm of their right not to participate in the research will be sent out during the same period. A letter will be sent informing patients in each arm about their participation in the main study and their opportunity to object. A letter will also be sent inviting patients to answer the ancillary study questionnaires for the and advising them about their freedom of choice to participate. The CRCDC will collect all objections to participation via the Data Protection Officer (DPO). Women and GPs will be able to apply to the DPO to be informed of the overall research results.
Author contributions
Study concept and design: SH, A-SB, EF, and CR. Acquisition, analysis, or interpretation of the data: SH, AG, DT, A-SB, KB, AL, EB, FN, and CR. Drafting of the manuscript: SH, DT, EF, AG, and CR. Critical revision of the manuscript for important intellectual content: SH, EF, and CR. Statistical analysis: AG. Administrative, technical, or material support: A-SB, KB, AL, EB, FN, and CR. Study supervision: SH and CR. The corresponding author attests that all listed authors meet the authorship criteria and that no others meeting this criterion have been omitted. All authors read and approved the final manuscript. The lead author affirms that this manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as planned (and, if relevant, registered) have been explained. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors would like to thank Mr Mark Bowyer for the translation of the manuscript. This article is supported by the French network of University Hospitals HUGO (“Hôpitaux Universitaires du Grand Ouest”).
Funding Statement
This work was carried out in the context of a French research project, called DEDICACES (grant number: 2021-A01583-38), which is coordinated by the University Hospital of Nantes and funded by the French national cancer Institute (Inca) over the period 2019–2022. Inca did not participate in the design of the study, in the collection, interpretation, or analysis of the data, nor in the drafting of the manuscript.
Abbreviations
BC, Breast cancer; DA, Decision aids; DPO, Data Protection Officer; DCS, Decisional Conflict Scale; GP, General Practitioner; OS, Organized Screening; ITT, Intention to Treat; NSDS, National Health Data System; SDM-Q, Shared Decision Making Questionnaire; SMDM, Shared Medical Decision Making.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fonc.2023.1128467/full#supplementary-material
Objectives, judgement criteria, data collection and source of the data collected
Characteristics of treatments and examinations carried out collected to assess the woman’s state of health
References
- 1. Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin (2021) 71(3):209−49. [DOI] [PubMed] [Google Scholar]
- 2. International Agency for Research on Cancer. World Health Organization. Global Cancer Observatory . Estimated cancer incidence, mortality and prevalence worldwide in 2020: breast cancer. (Lyon France: World Health Organization; ). (2020). [Google Scholar]
- 3. Gøtzsche PC, Jørgensen KJ. Screening for breast cancer with mammography. Cochrane Database Syst Rev (2013) 2013(6):CD001877. doi: 10.1002/14651858.CD001877.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Myers ER, Moorman P, Gierisch JM, Havrilesky LJ, Grimm LJ, Ghate S, et al. Benefits and harms of breast cancer screening: a systematic review. JAMA. 20 oct (2015) 314(15):1615. doi: 10.1001/jama.2015.13183 [DOI] [PubMed] [Google Scholar]
- 5. Tabár L, Gad A, Holmberg LH, Ljungquist U, Fagerberg CJG, Baldetorp L, et al. Reduction in mortality from breast cancer after mass screening with mammography. Lancet (1985) 325(8433):829−32. doi: 10.1016/S0140-6736(85)92204-4 [DOI] [PubMed] [Google Scholar]
- 6. Perry N, Europäische Kommission . European Guidelines for quality assurance in breast cancer screening and diagnosis. 4th ed. Luxembourg: Office for Official Publ. of the Europ. Communities; (2006). 416 p. [Google Scholar]
- 7. Duffy SW, Tabár L, Yen AM, Dean PB, Smith RA, Jonsson H, et al. Mammography screening reduces rates of advanced and fatal breast cancers: results in 549,091 women. Cancer (2020) 126(13):2971−9. doi: 10.1002/cncr.32859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Shapiro S, Strax P, Venet L. Periodic breast cancer screening in reducing mortality from breast cancer. JAMA (1971) 215(11):1777−85. doi: 10.1001/jama.1971.03180240027005 [DOI] [PubMed] [Google Scholar]
- 9. Institut National du Cancer . Le programme de dépistage organisé [the organised screening programme] (2022). Available at: https://www.e-cancer.fr/Professionnels-de-sante/Depistage-et-detection-precoce/Depistage-du-cancer-du-sein/Le-programme-de-depistage-organise.
- 10. World Health Organization WHO position paper on mammography screening. Geneva: World Health Organization; (2014). 78 p. Available at: https://apps.who.int/iris/handle/10665/137339. [PubMed] [Google Scholar]
- 11. Santé Publique France . Taux de participation au programme de dépistage organisé du cancer du sein 2019-2020 et évolution depuis 2005 [Participation rates in the 2019-2020 organized breast cancer screening program and changes since 2005] (2021). Available at: https://www.santepubliquefrance.fr/maladies-et-traumatismes/cancers/cancer-du-sein/articles/taux-de-participation-au-programme-de-depistage-organise-du-cancer-du-sein-2019-2020-et-evolution-depuis-2005.
- 12. Cases C, Di Palma M, Drahi E, Fainzang S, Landais P, de Montgolfier S, et al. Rapport du comité d’orientation. ensemble améliorons le dépistage du cancer du sein. concertation citoyenne et scientifique [Report of the steering committee. In: Together let’s improve breast cancer screening. citizen and scientific consultation] (Paris France: French national Cancer; ) (2016). p. 166. Available at: http://www.concertation-depistage.fr/wp-content/uploads/2016/10/depistage-cancer-sein-rapport-concertation-sept-2016.pdf. [Google Scholar]
- 13. Jørgensen KJ, Kalager M, Barratt A, Baines C, Zahl PH, Brodersen J, et al. Overview of guidelines on breast screening: why recommendations differ and what to do about it. Breast (2017) 31:261−9. doi: 10.1016/j.breast.2016.08.002 [DOI] [PubMed] [Google Scholar]
- 14. Pace LE, Keating NL. A systematic assessment of benefits and risks to guide breast cancer screening decisions. JAMA. (2014) 311(13):1327. doi: 10.1001/jama.2014.1398 [DOI] [PubMed] [Google Scholar]
- 15. Mandelblatt JS. Effects of mammography screening under different screening schedules: model estimates of potential benefits and harms. Ann Intern Med 17 nov (2009) 151(10):738. doi: 10.7326/0003-4819-151-10-200911170-00010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Independent UK Panel on Breast Cancer Screening . The benefits and harms of breast cancer screening: an independent review. Lancet (2012) 380(9855):1778−86. doi: 10.1016/S0140-6736(12)61611-0 [DOI] [PubMed] [Google Scholar]
- 17. Klarenbach S, Sims-Jones N, Lewin G, Singh H, Thériault G, Tonelli M, et al. Recommendations on screening for breast cancer in women aged 40–74 years who are not at increased risk for breast cancer. CMAJ (2018) 190(49):E1441−51. doi: 10.1503/cmaj.180463 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. French Authority for Health . Dépistage et prévention du cancer du sein. actualisation du référentiel de pratiques de l’examen périodique de santé [Breast cancer screening and prevention. updating of the guidelines for the periodic health examination] (2015). Available at: https://www.has-sante.fr/upload/docs/application/pdf/2015-04/refces_k_du_sein_vf.pdf.
- 19. Barry MJ, Edgman-Levitan S. Shared decision making — the pinnacle of patient-centered care. N Engl J Med (2012) 366(9):780−1. doi: 10.1056/NEJMp1109283 [DOI] [PubMed] [Google Scholar]
- 20. Schrager S, Phillips G, Burnside E. A simple approach to shared decision making in cancer screening. Fam Pract Manage (2017) 24(3):5−10. [PMC free article] [PubMed] [Google Scholar]
- 21. The Ottawa Hospital Research Institute Répertoire des outils d’aide à la décision. [Listing of decision aid tools] (2021). Available at: https://decisionaid.ohri.ca/francais/repertoire.html.
- 22. Blanc B. Comment pratiquer la prise de décision partagée en médecine générale? [How to practice shared decision making in general practice?]. Rennes (2015) 1:69. [Google Scholar]
- 23. Hild S, Johanet M, Valenza A, Thabaud M, Laforest F, Ferrat E, et al. Quality of decision aids developed for women at average risk of breast cancer eligible for mammographic screening: systematic review and assessment according to the international patient decision aid standards instrument. Cancer (2020) 126(12):2765−74. doi: 10.1002/cncr.32858 [DOI] [PubMed] [Google Scholar]
- 24. Esmaeili M, Ayyoubzadeh SM, Javanmard Z, R. Niakan Kalhori S. A systematic review of decision aids for mammography screening: focus on outcomes and characteristics. Int J Med Inf mai (2021) 149:104406. doi: 10.1016/j.ijmedinf.2021.104406 [DOI] [PubMed] [Google Scholar]
- 25. Hild S, Teigné D, Cerisey C, Gocko X, Aubin-Auger I, et al. Décider ensemble de participer, ou non, au dépistage organisé du cancer du sein [Decide together whether or not to participate in organized breast cancer screening] [Internet]. décider ensemble de participer, ou non, au dépistage organisé du cancer du sein(2021). Available at: https://discutons-mammo.fr/.
- 26. Stacey D, Kryworuchko J, Belkora J, Davison BJ, Durand MA, Eden KB, et al. Coaching and guidance with patient decision aids: a review of theoretical and empirical evidence. BMC Med Inform Decis Mak. (2013) 13 Suppl 2:S11. doi: 10.1186/1472-6947-13-S2-S11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Légaré F, Adekpedjou R, Stacey D, Turcotte S, Kryworuchko J, Graham ID, et al. Interventions for increasing the use of shared decision making by healthcare professionals. Cochrane Database Syst Rev (2018) 7. doi: 10.1002/14651858.CD006732.pub4/full [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Martín-López R, Jiménez-García R, Lopez-de-Andres A, Hernández-Barrera V, Jiménez-Trujillo I, Gil-de-Miguel A, et al. Inequalities in uptake of breast cancer screening in Spain: analysis of a cross-sectional national survey. Public Health (2013) 127(9):822−7. doi: 10.1016/j.puhe.2013.03.006 [DOI] [PubMed] [Google Scholar]
- 29. Szczepura A, Price C, Gumber A. Breast and bowel cancer screening uptake patterns over 15 years for UK south Asian ethnic minority populations, corrected for differences in socio-demographic characteristics. BMC Public Health déc (2008) 8(1):346. doi: 10.1186/1471-2458-8-346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Bouvard V, Wentzensen N, Mackie A, Berkhof J, Brotherton J, Giorgi-Rossi P, et al. The IARC perspective on cervical cancer screening. N Engl J Med (2021) 11385(20):1908−18. doi: 10.1056/NEJMsr2030640 [DOI] [PubMed] [Google Scholar]
- 31. Duport DN, Beltzer N. Dépistage organisé du cancer du col de l’utérus. evaluation du dépistage organisé du cancer du col de l’utérus dans les quatre départements pérennes et les neuf départements expérimentaux. expérimentation 2010-2014 [Organised cervical cancer screening. evaluation of organised cervical cancer screening in the four permanent departments and the nine experimental departments]. St Maurice Santé Publique Fr (2016) 42:46. [Google Scholar]
- 32. Plourde N, Brown HK, Vigod S, Cobigo V. Contextual factors associated with uptake of breast and cervical cancer screening: a systematic review of the literature. Women Health (2016) 56(8):906−25. doi: 10.1080/03630242.2016.1145169 [DOI] [PubMed] [Google Scholar]
- 33. Diaz A, Kang J, Moore SP, Baade P, Langbecker D, Condon JR, et al. Association between comorbidity and participation in breast and cervical cancer screening: a systematic review and meta-analysis. Cancer Epidemiol (2017) 47:7−19. doi: 10.1016/j.canep.2016.12.010 [DOI] [PubMed] [Google Scholar]
- 34. Hsieh HM, Shen CT, Chen LS, Chen FM, Yeh SC. Moderation effect of mammography screening among women with multiple chronic conditions. Sci Rep 10 févr (2022) 12:2303. doi: 10.1038/s41598-022-06187-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Mitchell AJ, Pereira IES, Yadegarfar M, Pepereke S, Mugadza V, Stubbs B. Breast cancer screening in women with mental illness: comparative meta-analysis of mammography uptake. Br J Psychiatry J Ment Sci (2014) 205(6):428−35. doi: 10.1192/bjp.bp.114.147629 [DOI] [PubMed] [Google Scholar]
- 36. Woodhead C, Cunningham R, Ashworth M, Barley E, Stewart RJ, Henderson MJ. Cervical and breast cancer screening uptake among women with serious mental illness: a data linkage study. BMC Cancer. 21 oct (2016) 16(1):819. doi: 10.1186/s12885-016-2842-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, et al. Updating and validating the charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol (2011) 173(6):676−82. doi: 10.1093/aje/kwq433 [DOI] [PubMed] [Google Scholar]
- 38. Kriston L, Scholl I, Hölzel L, Simon D, Loh A, Härter M. The 9-item shared decision making questionnaire (SDM-Q-9). development and psychometric properties in a primary care sample. Patient Educ Couns. (2010) 80(1):94−9. doi: 10.1016/j.pec.2009.09.034 [DOI] [PubMed] [Google Scholar]
- 39. O’Connor AM. User manual - decisional conflict scale (1993). Available at: https://decisionaid.ohri.ca/docs/develop/User_Manuals/UM_decisional_conflict.pdf.
- 40. European Medicines Agency . ICH E9 statistical principles for clinical trials . Available at: https://www.ema.europa.eu/en/ich-e9-statistical-principles-clinical-trials.
- 41. Rey G, Jougla E, Fouillet A, Hémon D. Ecological association between a deprivation index and mortality in France over the period 1997 – 2001: variations with spatial scale, degree of urbanicity, age, gender and cause of death. BMC Public Health déc (2009) 9(1):46. doi: 10.1186/1471-2458-9-33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Data Hub . Ods annuaire Santé : liste, localisation et tarifs des professionnels de santé [Health Directory : list, location and prices of health professionals]. opendatasoft; (2023). Available at: https://data.opendatasoft.com/explore/dataset/medecins%40public/export/?flg=fr. [Google Scholar]
- 43. Pérez-Lacasta MJ, Martínez-Alonso M, Garcia M, Sala M, Perestelo-Pérez L, Vidal C, et al. Effect of information about the benefits and harms of mammography on women’s decision making: the InforMa randomised controlled trial. Housten A éditeur. PloS One (2019) 14(3):e0214057. doi: 10.1371/journal.pone.0214057 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Edwards A. Effects of communicating individual risks in screening programmes: cochrane systematic review. BMJ (2003) 327(7417):703−9. doi: 10.1136/bmj.327.7417.703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Bourmaud A, Soler-Michel P, Oriol M, Regnier V, Tinquaut F, Nourissat A, et al. Decision aid on breast cancer screening reduces attendance rate: results of a large-scale, randomized, controlled study by the DECIDEO group. Oncotarget (2016) 7(11):12885−92. doi: 10.18632/oncotarget.7332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Montero-Moraga JM, Posso M, Román M, Burón A, Sala M, Castells X, et al. Effect of an information leaflet on breast cancer screening participation: a cluster randomized controlled trial. BMC Public Health (2021) 21(1):1301. doi: 10.1186/s12889-021-11360-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Roberto A, Colombo C, Candiani G, Satolli R, Giordano L, Jaramillo L, et al. A dynamic web-based decision aid to improve informed choice in organised breast cancer screening. a pragmatic randomised trial in Italy. Br J Cancer (2020) 123(5):714−21. doi: 10.1038/s41416-020-0935-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Chan AW, Tetzlaff JM, Altman DG, Laupacis A, Gøtzsche PC, Krleža-Jerić K, et al. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann Intern Med (2013) 158(3):200. doi: 10.7326/0003-4819-158-3-201302050-00583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Ross RL, Rubio K, Rodriguez HP. Mammography and decision aid use for breast cancer screening in older women. Am J Prev Med (2022) 63(4):630−5. doi: 10.1016/j.amepre.2022.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Rat C, Pogu C, Le Donne D, Latour C, Bianco G, Nanin F, et al. Effect of physician notification regarding non-adherence to colorectal cancer screening on patient participation in fecal immunochemical test cancer screening : a randomized clinical tria. Rev DÉpidémiologie Santé Publique (2018) 66:S142−3. doi: 10.1016/j.respe.2018.03.357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Martínez-Alonso M, Carles-Lavila M, Pérez-Lacasta MJ, Pons-Rodríguez A, Garcia M, Rué M, et al. Assessment of the effects of decision aids about breast cancer screening: a systematic review and meta-analysis. BMJ Open (2017) 7(10):e016894. doi: 10.1136/bmjopen-2017-016894 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Schapira MM, Hubbard RA, Seitz HH, Conant EF, Schnall M, Cappella JN, et al. The impact of a risk-based breast cancer screening decision aid on initiation of mammography among younger women: report of a randomized trial. MDM Policy Pract (2019) 4(1):238146831881288. doi: 10.1177/2381468318812889 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Stacey D, Légaré F, Lewis K, Barry MJ, Bennett CL, Eden KB, et al. Decision aids for people facing health treatment or screening decisions. Cochrane Database Syst Rev (2017) 4). doi: 10.1002/14651858.CD001431.pub5/full/fr [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Hersch J, Barratt A, Jansen J, Irwig L, McGeechan K, Jacklyn G, et al. Use of a decision aid including information on overdetection to support informed choice about breast cancer screening: a randomised controlled trial. Lancet Lond Engl (2015) 385(9978):1642−52. doi: 10.1016/S0140-6736(15)60123-4 [DOI] [PubMed] [Google Scholar]
- 55. Shay LA, Lafata JE. Where is the evidence? a systematic review of shared decision making and patient outcomes. Med Decis Making (2015) 35(1):114−31. doi: 10.1177/0272989X14551638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Shirzadi S, Nadrian H, Asghari Jafarabadi M, Allahverdipour H, Hassankhani H. Determinants of mammography adoption among iranian women: what are the differences in the cognitive factors by the stages of test adoption? Health Care Women Int (2017) 38(9):956−70. doi: 10.1080/07399332.2017.1338705 [DOI] [PubMed] [Google Scholar]
- 57. Ponce-Chazarri L, Ponce-Blandón JA, Immordino P, Giordano A, Morales F. Barriers to breast cancer-screening adherence in vulnerable populations. Cancers. (2023) 15(3):604. doi: 10.3390/cancers15030604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Lau J, Shrestha P, Shaina Ng J, Jianlin Wong G, Legido-Quigley H, Tan KK. Qualitative factors influencing breast and cervical cancer screening in women: a scoping review. Prev Med Rep (2022) 27:101816. doi: 10.1016/j.pmedr.2022.101816 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Objectives, judgement criteria, data collection and source of the data collected
Characteristics of treatments and examinations carried out collected to assess the woman’s state of health


