Key Points
-
•
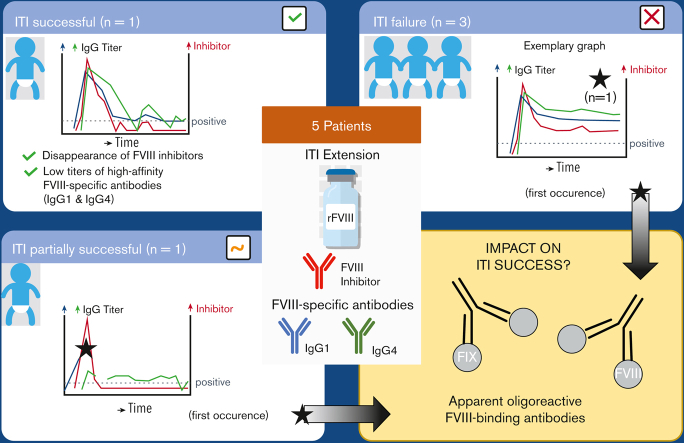
ITI success in the HIPS-ITI extension study was associated with sustained titer minimization of high-affinity FVIII-specific antibodies.
-
•
One patient with partial ITI success and 1 patient with ITI failure developed apparent oligoreactive FVIII-binding antibodies during ITI.
Visual Abstract
Abstract
Factor VIII (FVIII) inhibitor formation is a major clinical concern during replacement therapy in patients with hemophilia A. Immune tolerance induction (ITI) is the only therapeutic approach to attempt inhibitor eradication and establishment of long-term immune tolerance to FVIII. Hemophilia Inhibitor Previously Untreated Patient (PUP) Study (HIPS) was a prospective clinical trial to investigate changes in the immune system of PUPs with severe hemophilia A. Five patients who developed persistent FVIII inhibitors during HIPS entered an ITI extension arm (HIPS-ITI). During HIPS-ITI, inhibitor patients received ITI with the same FVIII product (a single source of recombinant, human full-length FVIII) used in HIPS until successful tolerance, declared failure, or a maximum of 2 years after HIPS-ITI enrollment, whichever came first. Blood samples and clinical data were collected monthly. Longitudinal FVIII-binding antibody signatures, associated binding specificities, and apparent affinities were determined for each patient at each sampling time point. ITI was successful or partially successful in 2 patients and failed in 3. Both groups presented with distinct FVIII-specific antibody signatures. ITI success required the disappearance of FVIII inhibitors, which was associated with the eradication or sustained titer minimization of high-affinity FVIII-specific antibodies, particularly of the immunoglobulin G1 (IgG1) and IgG4 subclasses. In contrast, ITI failure, as reflected by FVIII inhibitor persistence, was associated with persistent high-affinity FVIII-specific antibodies. Interestingly, 1 patient with partial ITI success and 1 patient with ITI failure developed apparent oligoreactive FVIII-binding antibodies during ITI. The explanation of the true nature of these antibodies requires more comprehensive follow-ups in future studies. This trial was registered at www.clinicaltrials.gov as #NCT01652027.
Introduction
Congenital hemophilia A is a rare X-linked recessive bleeding disorder caused by a deficiency in functionally active coagulation factor VIII (FVIII). Most patients with hemophilia A receive exogenous FVIII replacement. The major clinical concern throughout replacement therapy is the development of neutralizing anti-FVIII antibodies (FVIII inhibitors). Up to 30% of previously untreated patients (PUPs) with severe hemophilia A develop FVIII inhibitors within their first 20 exposure days (EDs) to FVIII concentrates.1, 2, 3, 4, 5 Although bypassing agents (eg, recombinant FVIIa, FVIII Inhibitor Bypassing Activity) and nonreplacement therapies (eg, emicizumab) ensure efficient bleed control, the use of FVIII replacement products still has unparalleled advantages.6, 7, 8 Therefore, the formation of FVIII inhibitors should be prevented or inhibitor eradication should be attempted upon clinically significant inhibitor titer detection.9
Immune tolerance induction (ITI) therapy is the only established approach to eradicate FVIII inhibitors and to achieve long-term immune tolerance to FVIII in patients with hemophilia A with inhibitors.10 During ITI, inhibitor patients are exposed to frequent exogenous FVIII infusions, given in regular intervals over a prolonged period. A universal ITI treatment regimen has not been defined. The choice of the appropriate ITI protocol depends on a variety of variables, such as FVIII inhibitor titer at the time of ITI initiation, peak historical FVIII inhibitor titer, or peak FVIII inhibitor titer while on ITI. Some of these parameters serve as predictors of ITI success based on results collected in registries, treatment guidelines, or experience reports.11, 12, 13, 14, 15 Overall success rates for different ITI protocols vary between 60% and 80%.16,17
The underlying immune mechanisms responsible for the disappearance of FVIII inhibitors and the prevention of new inhibitor formation have not been fully elucidated.18, 19, 20 Three mechanisms have been hypothesized to play a pivotal role in this process: (1) The prevention of memory B-cell differentiation into antibody-secreting plasma cells by the administration of high FVIII doses, as demonstrated in preclinical in vivo models of hemophilia A.21,22 This process might result in the deletion of FVIII-specific memory B cells.23 (2) Anergy of FVIII-specific effector T cells caused by exhaustion or overstimulation and an induction of regulatory T cells upon chronic FVIII exposure under noninflammatory conditions.24, 25, 26 (3) The formation of anti-idiotypic antibodies targeting autoreactive B cells and anti-FVIII antibodies.27, 28, 29 Genetic, environmental, and treatment-related risk factors, such as the administration of FVIII replacement at times of concomitant stimulation of the innate immune system (“high immunologic danger”), were not only reported as potential drivers for FVIII inhibitor formation but also hypothesized to negatively affect ITI success.1,3,26,30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42
The inhibitory effect of neutralizing anti-FVIII antibodies is quantified with the Bethesda or the Nijmegen-modified Bethesda coagulation-based assays.43, 44, 45 Apart from neutralizing anti-FVIII antibodies in patients with hemophilia A with inhibitors, nonneutralizing anti-FVIII antibodies have been detected in patients without inhibitors and in healthy donors. These findings indicate that FVIII inhibitors represent only a fraction of the overall antibody response elicited by FVIII.46, 47, 48, 49, 50, 51 Recently, we reported the results of the Hemophilia Inhibitor PUP Study (HIPS; www.clinicaltrials.gov, #NCT01652027), which combined coagulation-based inhibitor assays and enzyme-linked immunosorbent assays (ELISAs) for immunoglobulin (Ig) isotype–/IgG subclass–specific profiling of FVIII-specific antibodies associated with the assessment of apparent affinities of these antibodies. Our data revealed 4 subgroups of patients with distinct anti-FVIII antibody signatures. Subgroup 1 (7 patients) did not form any detectable FVIII-binding antibodies. Subgroup 2 (7 patients) solely developed nonneutralizing, FVIII-binding IgG1. Subgroup 3 (2 patients) developed FVIII-binding IgG1 antibodies only, which were associated with transient FVIII inhibitors. Subgroup 4 (7 patients) formed persistent FVIII inhibitors. These inhibitors were associated with the development of high-affinity FVIII-specific IgG1, followed by IgG3 and IgG4.52 ITI was initiated in patients of subgroup 4 after the inhibitor was detected. Five of the 7 patients in subgroup 4 were enrolled in an ITI extension arm (HIPS-ITI) for further follow-up after completing their first 50 EDs during HIPS. ITI treatment continued for a maximum of 2 years after enrollment or until successful tolerance or declared failure, whichever came first. The ITI protocol included monthly blood sampling, which enabled continued antibody and additional immune system analyses to facilitate a better understanding of the underlying mechanisms contributing to the success or failure of ITI.
This article presents the results of our comprehensive antibody analytics program, which included patients who developed persistent FVIII inhibitors during HIPS and were subsequently enrolled in the HIPS-ITI extension. Our results indicate that ITI success in the HIPS-ITI extension study required the disappearance of FVIII inhibitors, which was associated with the removal or sustained titer minimization of high-affinity FVIII-specific antibodies, particularly of the IgG1 and IgG4 subclasses.
Materials and methods
Study design
HIPS was a prospective, multicentered, longitudinal cohort study of PUPs with severe hemophilia A (www.clinicaltrials.gov, #NCT01652027). HIPS design details and results on longitudinal FVIII-specific antibody formation were recently published.52 ITI was already initiated during HIPS in 5 patients, who developed persistent FVIII inhibitors. Subsequently, these patients were enrolled in the HIPS-ITI extension arm for further follow-up after the 50th FVIII ED was reached. They were followed until tolerance was achieved, failure was declared, or for 2 years after enrollment, whichever came first. Each center obtained approval from their independent ethics committee and respective institutional review board. Moreover, all participating hemophilia treatment centers passed study-specific qualification testing to ensure the quality of the biological specimens collected.52
Enrollment criteria, treatment, and clinical procedures
Patients who developed persistent FVIII inhibitors during HIPS were eligible for the ITI-extension study. HIPS-specific enrollment criteria were previously published.52 Written informed consent, approved by the respective independent ethics committee and institutional review board, was obtained from a parent or a legally authorized representative of each study participant before HIPS and HIPS-ITI enrollment.
Patients were treated with a single source of recombinant, human, full-length FVIII (FVIII; antihemophilic factor [recombinant], Advate; Baxalta US, a Takeda company, Lexington, MA). The type of regimen, dosing, and frequency of infusions throughout HIPS and HIPS-ITI were at the discretion of each investigator. The use of bypass agents, but not immunosuppressive medication, was permitted during ITI.
HIPS-ITI patients had blood samples collected once a month (+7 days). Blood was tested for inhibitors and for FVIII antibody signatures at each time point.
Once inhibitor testing became negative during ITI, successful tolerance was confirmed in a 2-step approach: (1) a 48-hour postinfusion sample had to be negative for FVIII inhibitors and (2) a FVIII activity measurement obtained 48 hours after an infusion of 50 international units (IU) FVIII/kg had to be ≥0.01 IU/mL (1%). This approach followed the guidelines published by the United Kingdom Hemophilia Center Doctors Organization in 2013.9
Parents and treatment centers were required to maintain a diary to record information about FVIII infusions including date of infusion, number of units infused, number of vials used, lot number(s), reason for infusion, and adverse events. In addition, the diary included information about infections, immunizations, additional medications and dietary supplements, hospitalizations, surgeries, and trauma.
Detection of neutralizing antibodies
FVIII inhibitor coagulation testing was performed at a central laboratory located at the Medical University of Vienna, Austria, by following the Nijmegen-modified Bethesda assay methodology. The lower limit of inhibitor detection was 0.4 Bethesda units (BU)/mL. A patient was considered FVIII inhibitor positive if inhibitors were detected at a level ≥0.6 BU/mL on at least 2 consecutive EDs. If a positive inhibitor peaked at ≤5 BU/mL after rechallenge with FVIII, it was considered a low-titer inhibitor. A positive inhibitor >5 BU/mL was considered as a high-titer inhibitor.
Detection of FVIII- or FIX-binding antibodies
FVIII-binding antibodies of IgG subclasses 1 to 4 and of isotypes IgA and IgM were analyzed using an ELISA platform, which was fully validated according to guidelines by the European Medicines Agency and the US Food and Drug Administration, as described.46 FIX-binding total Ig was detected by using a similarly validated ELISA with FIX as coating antigen. More specific assay outlines are provided in the online supplement (supplemental Section 1.1).
Assessment of specificity and apparent affinity constants of FVIII- and FIX-binding antibodies
FVIII specificity and associated apparent affinity constants (KAs) of FVIII-binding IgA and IgG subclasses 1 to 4 were determined using a competition-based modification of the ELISA platform mentioned above. Test principle, nonlinear regression modeling for data evaluation, as well as technical and validation details of the apparent affinity ELISA approach were described by Hofbauer et al47 and are summarized in the online supplement (supplemental Section 1.2).
If nonlinear regression modeling for apparent KA determination was not possible, a classical competition approach with an elevated antigen concentration of 351 nmol FVIII was performed for confirmation of FVIII specificity.46
FIX specificity of FIX-binding total Ig was investigated by following a similar competition approach.
Definition of the term “apparent oligoreactive antibodies”
FVIII-binding antibodies were described as apparent oligoreactive antibodies if the following observations were made during the analysis of a plasma sample obtained from a HIPS-ITI patient:
-
1.
The plasma sample contained antibodies that bound to FVIII immobilized to the ELISA plate. The titer for these FVIII-binding antibodies could be assessed.
-
2.
The same plasma samples also contained antibodies that bound to FIX immobilized to the ELISA plate. The titer for these FIX-binding antibodies could be assessed.
-
3.
Binding of antibodies to FVIII or FIX, respectively, could not be prevented by preincubation of the respective plasma sample with soluble FVIII or FIX, respectively.
-
4.
The same plasma samples did not contain antibodies that bound to an uncoated ELISA plate blocked with bovine serum albumin, which was used for blocking unspecific binding sites in all ELISAs.
Statistical analyses
Calculations regarding FVIII inhibitors, FVIII- and FIX-binding antibody titers as well as associated apparent KAs with 95% confidence intervals and affinity cluster analyses were performed as described.46,47,52 Correlations of antibody titers were reported using the nonparametric Spearman correlation coefficient. GraphPad Prism (version 8.4.3; GraphPad Software) was used to generate graphical visualizations and perform statistical calculations.
Results
HIPS-ITI patient characteristics and treatment details
All HIPS-ITI patients had high- or moderate-risk F8 mutations (intron 22 inversion [n = 4], duplication [n = 1]) and developed high-titer FVIII inhibitors. HIPS-ITI–specific patient characteristics and treatment details, such as age at first FVIII infusion, FVIII inhibitor titer before ITI initiation, the ED at which ITI was initiated, peak FVIII inhibitor titer during ITI, ITI treatment regimen, overall ITI duration, time from FVIII inhibitor detection to ITI termination, total number of EDs during HIPS and HIPS-ITI, and the ITI outcome, are summarized in Table 1. Additional information, such as family history of hemophilia A and FVIII inhibitors, F8 gene mutation, ethnic background, and number of EDs before first FVIII inhibitor detection, were provided by Reipert et al52 and are summarized in supplemental Table 1.
Table 1.
HIPS-ITI patient characteristics and treatment details
| HIPS-ITI patient identification no. | HIPS patient identification no.52 | Age at first FVIII infusion (mo) | FVIII inhibitor titer before ITI initiation (BU/mL) | ITI initiation | Peak FVIII inhibitor titer during ITI (BU/mL) | ITI treatment regimen | Overall ITI duration (mo) | Time from FVIII inhibitor detection to ITI termination (mo) | Total FVIII EDs | ITI outcome |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 21 | 10.3 | 7.7∗ | ED11 | 323.0 | ITI mo 1-5 (ED11-ED146): 190 U/kg qd ITI mo 6-7 (ED147-ED214): 177 U/kg qd ITI mo 8-14 (ED215-ED407): 79-88 U/kg qd |
14 | 20.5 | 407 | ITI success |
| 2 | 20 | 12.0 | 10.6† | ED16 | 9.5 | ITI mo 1-8 (ED16-ED162): 178 U/kg qd ITI mo 9-11 (ED163-ED260): 100 U/kg qd ITI mo 12-16 (ED261-ED389): 90-105 U/kg qd |
16 | 16.7 | 389 | ITI partial success |
| 3 | 22 | 6.3 | 85.3‡ | ED12 | 3049.0 | ITI mo 1-8 (ED12-ED228): 210 U/kg qd ITI mo 9-10 (ED229-ED260): 200 U/kg qd |
10 | 23.6 | 260 | ITI failure |
| 4 | 19 | 12.6 | 30.6 | ED13 | 796.0 | ITI mo 1-10 (ED13-ED305): 105 U/kg qd ITI mo 11-14 (ED306-ED426): 94 U/kg qd ITI mo 15-22 (ED427-ED524): 85 U/kg (3 times/wk) |
22 | 43.3 | 524 | ITI failure |
| 5 | 23 | 9.2 | 6.3 | ED13 | 124.0 | ITI mo 1-5 (ED13-ED130): 155 U/kg qd ITI mo 6-9 (ED131-ED267): 143 U/kg qd ITI mo 10 (ED268-ED293): 69 U/kg qd ITI mo 11-12 (ED294-ED344): 138 U/kg qd ITI mo 13 (ED345-ED360): 69 U/kg qd |
13 | 20.7 | 360 | ITI failure |
No, number; qd, daily.
One month before ED11.
One day before ED16.
Three months before ED12.
None of the 5 HIPS-ITI patients had favorable features for ITI success, such as a low-risk F8 genotype or a peak FVIII inhibitor titer ≤5 BU/mL at ITI initiation. Only 1 patient (HIPS-ITI patient 2) had a peak FVIII inhibitor titer ≤100 BU/mL, which has been identified as prediction factor for successful ITI outcome.15
FVIII-specific antibody signatures in inhibitor patients with successful or partially successful ITI treatment
ITI was successful in HIPS-ITI patient 1 (Figure 1) and partially successful in HIPS-ITI patient 2 (Figure 2). None of the 2 patients had preexisting FVIII-binding antibodies at HIPS baseline. At ITI termination, both patients were FVIII inhibitor negative 48 hours after the last ITI infusion. Therefore, both fulfilled the first criterion for ITI success per study protocol. Patient 1 also passed the second ITI success criterion and presented with a residual FVIII activity of 6% determined in the patient’s plasma 48 hours after a 50.0 IU/kg bolus. Patient 2 did not meet the second criterion because the residual FVIII activity dropped below 1% at ∼26 hours after a 53.4 IU/kg infusion. However, as the patient was able to resume prophylaxis and responded well to replacement therapy, ITI was evaluated as partially successful.
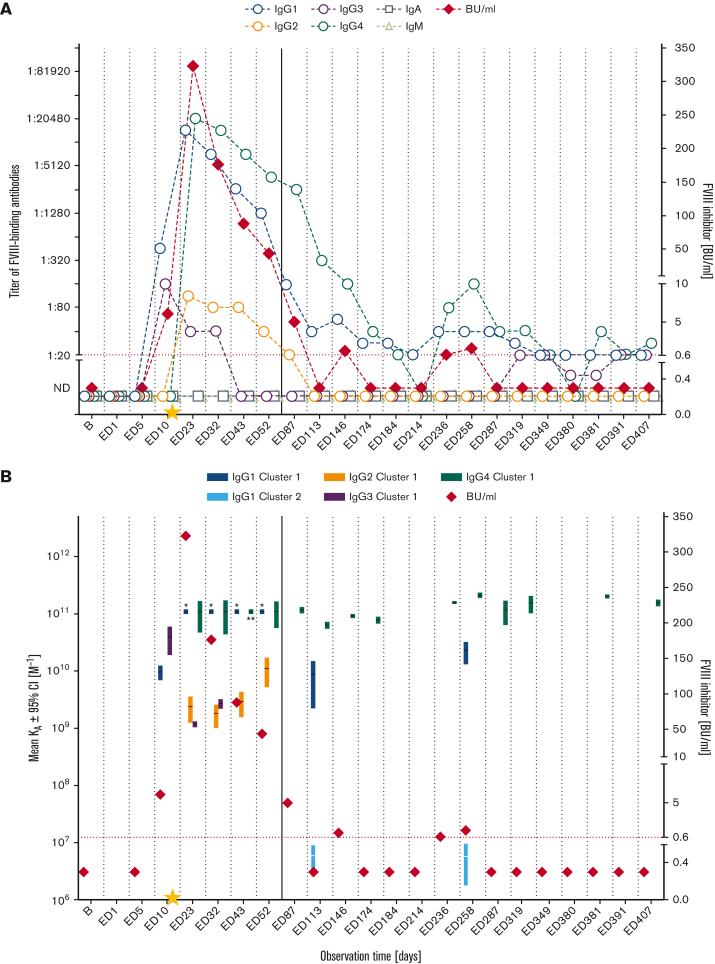
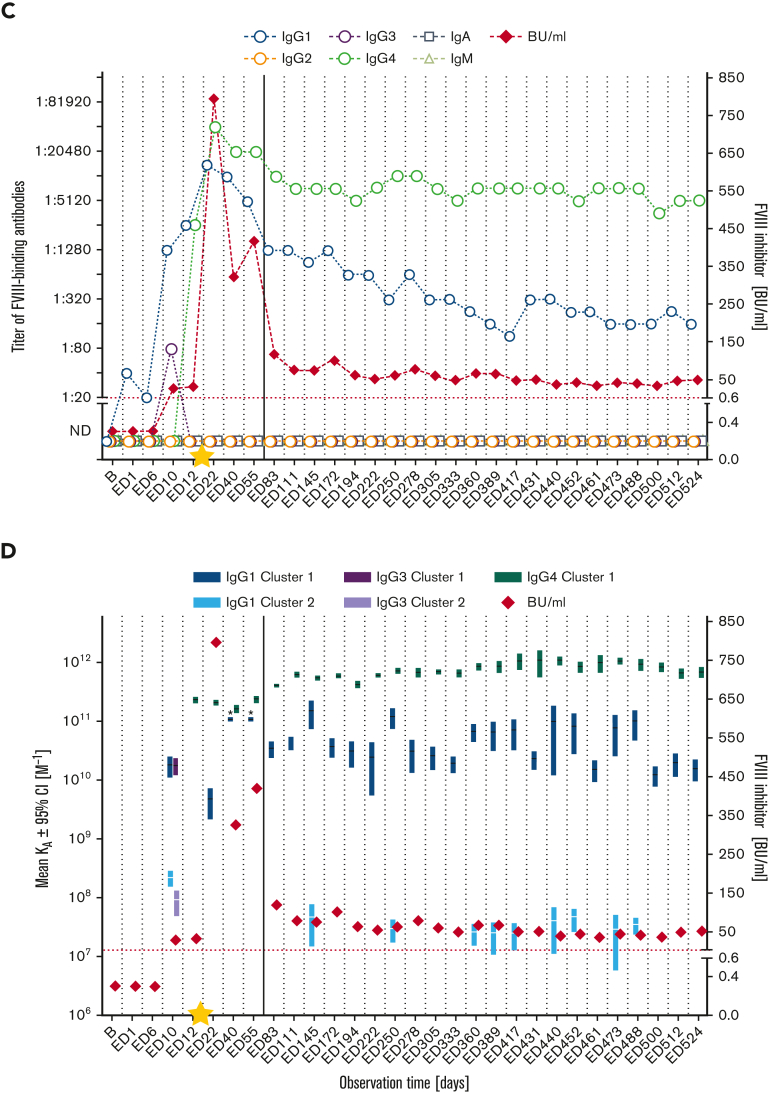
Figure 1.
Longitudinal monitoring of FVIII-specific antibodies and FVIII inhibitors in HIPS-ITI patient 1 during HIPS and HIPS-ITI. (A) FVIII-specific antibody titers (IgG1, IgG2, IgG3, IgG4, IgA, IgM as indicated) and FVIII inhibitors (BU/mL) for HIPS-ITI patient 1. The red dotted line represents the limit for positive evaluation of FVIII inhibitors (0.6 BU/mL). The yellow star marks the initiation of ITI treatment at ED11. The continuous vertical line indicates the end of HIPS and the start of HIPS-ITI. (B) Mean KA for FVIII-specific antibodies differentiated for individual IgG subclasses and FVIII inhibitors (BU/mL) for HIPS-ITI patient 1. Data for apparent KAs include the 95% confidence intervals (CIs) for up to 2 affinity clusters for each IgG subclass (dark colors: cluster 1; light colors: cluster 2). The red dotted line represents the limit for positive evaluation of FVIII inhibitors (0.6 BU/mL). The asterisks mark antibodies with apparent affinities that were too high (KAs > 1011 M−1) to be assessed. Therefore, their apparent KAs were reported as 1011 M−1. The yellow star marks the initiation of ITI treatment at ED11. The continuous vertical line indicates the end of HIPS and the start of HIPS-ITI. ∗IgG1 cluster 1, ∗∗IgG4 cluster 1. B, baseline; ND, not detectable (below the detection limit of 1:20 for FVIII-binding antibodies).
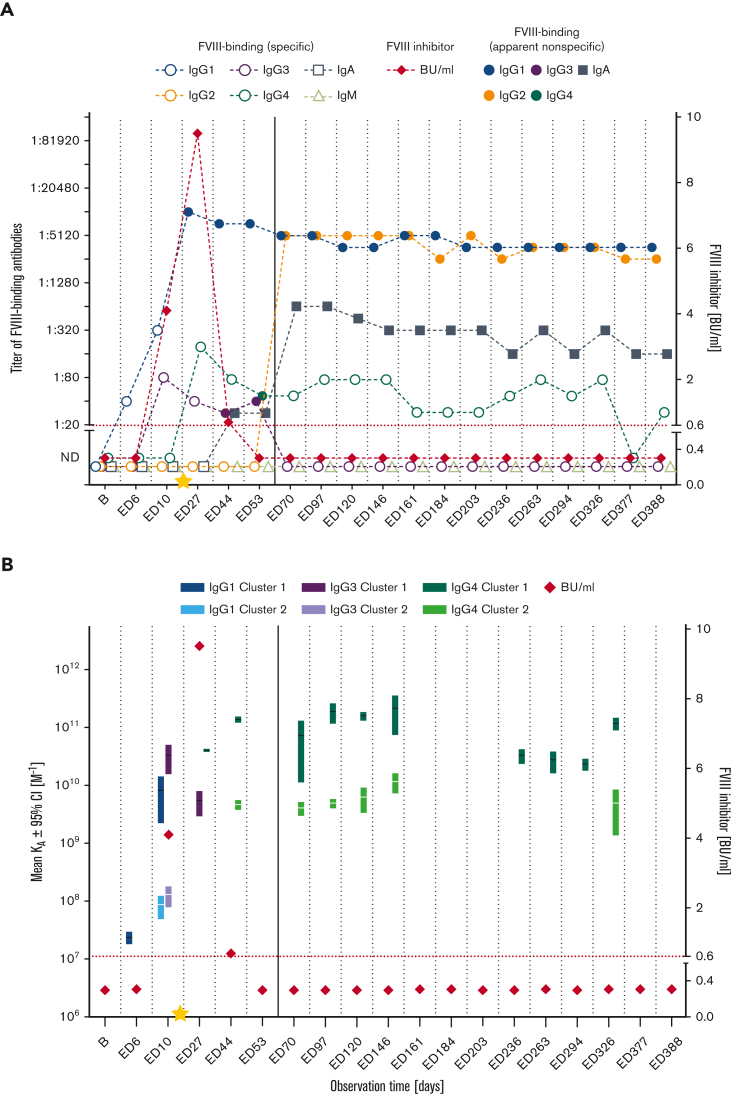
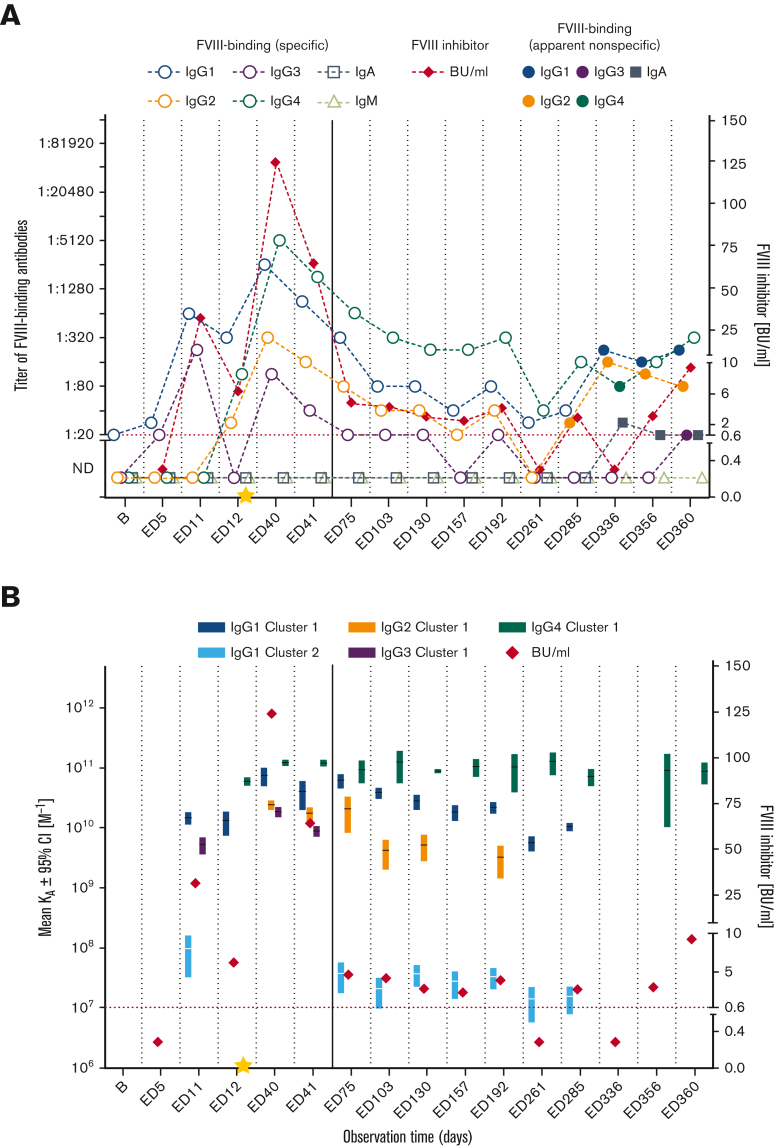
Figure 2.
Longitudinal monitoring of specific and apparent nonspecific FVIII-binding antibodies and FVIII inhibitors in HIPS-ITI patient 2 during HIPS and HIPS-ITI. (A) FVIII-binding (specific) antibody titers (IgG1, IgG2, IgG3, IgG4, IgA, IgM; open circles, open squares, open triangles as indicated), FVIII-binding (apparent nonspecific) antibody titers (IgG1, IgG2, IgG3, IgG4, IgA; filled circles, filled squares as indicated), and FVIII inhibitors (BU/mL) for HIPS-ITI patient 2. The red dotted line represents the limit for positive evaluation of FVIII inhibitors (0.6 BU/mL). The yellow star marks the initiation of ITI treatment at ED16. The continuous vertical line indicates the end of HIPS and the start of HIPS-ITI. (B) Mean KA for FVIII-binding (specific) antibodies differentiated for individual IgG subclasses and FVIII inhibitors (BU/mL) for HIPS-ITI patient 2. Data for apparent KAs include the 95% CIs for up to 2 affinity clusters for each IgG subclass (dark colors: cluster 1; light colors: cluster 2). The red dotted line represents the limit for positive evaluation of FVIII inhibitors (0.6 BU/mL). The yellow star marks the initiation of ITI treatment at ED16. The continuous vertical line indicates the end of HIPS and the start of HIPS-ITI.
HIPS-ITI patient 1 developed FVIII-specific high-affinity IgG1 (KA ∼1010 M−1) and IgG3 (KA > 1010 M−1) as well as FVIII inhibitors, which were first diagnosed at ED10. ITI was initiated on ED11. FVIII-specific high-affinity IgG4 (KA ∼1011 M−1) and FVIII-specific IgG2 were first detected at ED23 and declined afterward. FVIII inhibitor titers peaked on ED23 at 323.0 BU/mL, declined afterward, and transiently disappeared on ED113. Subsequently, FVIII inhibitors fluctuated around the detection limit until ED258 before they persistently disappeared. ITI success was confirmed at ED407. The kinetics of FVIII-specific high-affinity IgG1 (KA ≥ 1010 M−1) and IgG4 (KA ∼1011 M−1) were similar to the kinetics of FVIII inhibitors. IgG1 titers decreased and fluctuated around the detection limit until the end of the study. IgG4 titers dropped completely until ED214 and subsequently fluctuated around the detection limit. FVIII-specific IgG2 disappeared completely, whereas FVIII-specific IgG3 disappeared early during ITI and subsequently fluctuated around the detection limit. A timeline with HIPS-ITI patient 1–specific clinical records is provided in supplemental Figure 1.
HIPS-ITI patient 2 had developed low-affinity FVIII-specific IgG1 (KA < 108 M−1) on ED6. FVIII inhibitors were first detected on ED10, which was accompanied by FVIII-specific IgG1 with increased titers and affinities and by the appearance of high-affinity FVIII-specific IgG3 (KA ∼1010 M−1). ITI was started on ED16. Afterward, FVIII inhibitor titers peaked at 9.5 BU/mL on ED27. At the same time, high-affinity FVIII-specific IgG4 (KA > 1010 M−1) appeared for the first time. Subsequently, FVIII inhibitor titers decreased and disappeared at ED53. High-affinity FVIII-specific IgG4 (KA ∼1010 M−1) fluctuated around the detection limit until the end of the study. ITI was terminated after ED388.
FVIII-specific antibody signatures in inhibitor patients with ITI failure
ITI failed in HIPS-ITI patient 3 (Figure 3A-B), 4 (Figure 3C-D), and 5 (Figure 4). Two of the 3 patients had preexisting FVIII-binding antibodies at HIPS baseline. All 3 patients failed the first criterion for ITI success because they presented with high-titer FVIII inhibitors at ITI termination: 376.0 BU/mL in HIPS-ITI patient 3, 48.6 BU/mL in patient 4, and 9.3 BU/mL in patient 5.
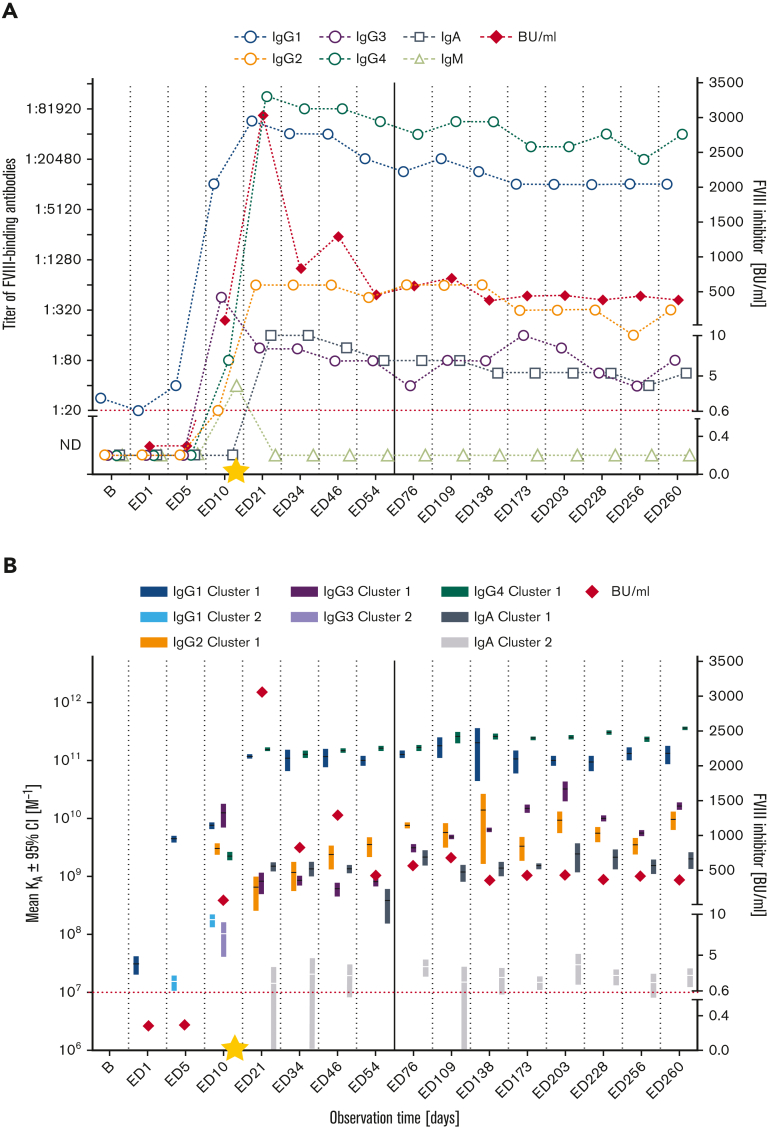
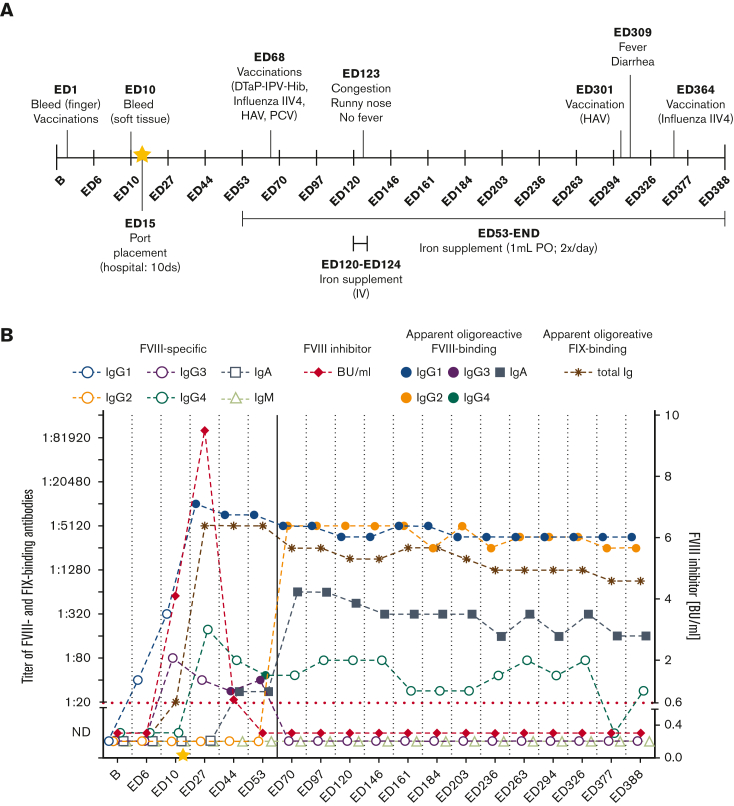
Figure 3.
Longitudinal monitoring of FVIII-specific antibodies and FVIII inhibitors in HIPS-ITI patients 3 and 4 during HIPS and HIPS-ITI. (A,C) FVIII-specific antibody titers (IgG1, IgG2, IgG3, IgG4, IgA, IgM as indicated) and FVIII inhibitors (BU/mL) for HIPS-ITI patients 3 (A) and 4 (C). The red dotted line represents the limit for positive evaluation of FVIII inhibitors (0.6 BU/mL). The yellow star marks the initiation of ITI treatment at ED12 (HIPS-ITI patient 3) and ED13 (HIPS-ITI patient 4). The continuous vertical line indicates the end of HIPS and the start of HIPS-ITI. (B,D) Mean KA for FVIII-specific antibodies differentiated for individual IgG subclasses/Ig isotypes and FVIII inhibitors (BU/mL) for HIPS-ITI patients 3 (B) and 4 (D). Data for apparent KAs include the 95% CIs for up to 2 affinity clusters for each IgG subclass and for IgA (dark colors: cluster 1; light colors: cluster 2). The red dotted line represents the limit for positive evaluation of FVIII inhibitors (0.6 BU/mL). The asterisks mark antibodies with apparent affinities that were too high (KAs > 1011 M−1) to be assessed. Therefore, their apparent KAs were reported as 1011 M−1. The yellow star marks the initiation of ITI treatment at ED12 (HIPS-ITI patient 3) and ED13 (HIPS-ITI patient 4). The continuous vertical line indicates the end of HIPS and the start of HIPS-ITI. ∗IgG1 cluster 1.
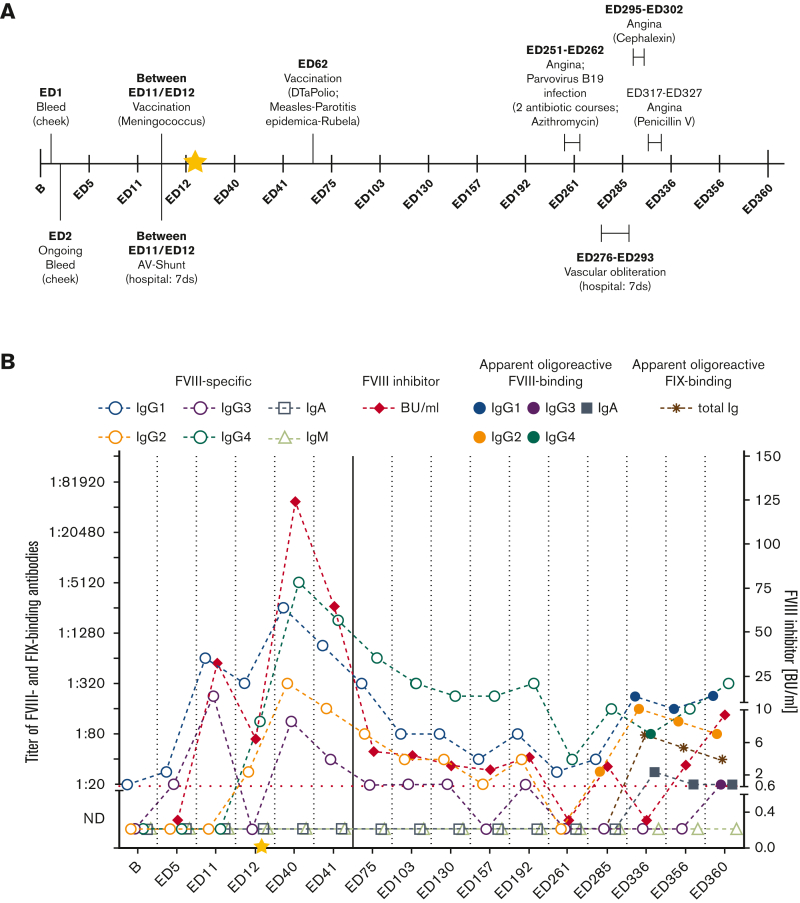
Figure 4.
Longitudinal monitoring of specific and apparent nonspecific FVIII-binding antibodies and FVIII inhibitors in HIPS-ITI patient 5 during HIPS and HIPS-ITI. (A) FVIII-binding (specific) antibody titers (IgG1, IgG2, IgG3, IgG4, IgA, IgM; open circles, open squares, open triangles as indicated), FVIII-binding (apparent nonspecific) antibody titers (IgG1, IgG2, IgG3, IgG4, IgA; filled circles, filled squares as indicated), and FVIII inhibitors (BU/mL) for HIPS-ITI patient 5. The red dotted line represents the limit for positive evaluation of FVIII inhibitors (0.6 BU/mL). The yellow star marks the initiation of ITI treatment at ED13. The continuous vertical line indicates the end of HIPS and the start of HIPS-ITI. (B) Mean KA for FVIII-binding (specific) antibodies differentiated for individual IgG subclasses and FVIII inhibitors (BU/mL) for HIPS-ITI patient 5. Data for apparent KAs include the 95% CIs for up to 2 affinity clusters for each IgG subclass (dark colors: cluster 1; light colors: cluster 2). The red dotted line represents the limit for positive evaluation of FVIII inhibitors (0.6 BU/mL). The yellow star marks the initiation of ITI treatment at ED13. The continuous vertical line indicates the end of HIPS and the start of HIPS-ITI.
HIPS-ITI patient 3 initially entered HIPS with preexisting FVIII-binding IgG1 at baseline. FVIII-specific IgG1 titers and associated apparent KAs increased until ED10, when FVIII inhibitors were first detected. Concurrently, FVIII-specific IgG2, IgG3, and IgG4 appeared. ITI was initiated on ED12. FVIII inhibitors and both titers and affinities of FVIII-specific IgG1, IgG2, and IgG4 increased and peaked at ED21 with peak inhibitor titers of 3049.0 BU/mL. Subsequently, FVIII inhibitors decreased but stayed at high-titer levels until the end of the study. Titers and affinities of FVIII-specific IgG1 and IgG4 persisted with peak levels (≥1:10 240; KA ≥ 1010 M−1). Titers of FVIII-specific IgG2 also persisted, and apparent KAs of IgG2 further increased and remained constant until study termination. Titers of FVIII-specific IgG3 did not increase after ITI initiation and persisted until the end of the study. FVIII-specific IgA appeared first at ED21 and also persisted. ITI in patient 3 was terminated after ED260. A timeline with patient-specific clinical records for HIPS-ITI patient 3 is provided in supplemental Figure 2.
HIPS-ITI patient 4 developed FVIII-binding IgG1, which was first detectable at ED1. On ED10, the patient presented with high-titer FVIII inhibitors accompanied by high-affinity FVIII-specific IgG1 and IgG3 (KA ∼1010 M−1). Although IgG3 disappeared again, FVIII-specific IgG1 increased in titer and affinity. High-affinity FVIII-specific IgG4 (KA > 1011 M−1) appeared at ED12. ITI was initiated on ED13. Subsequently, FVIII inhibitors and high-affinity FVIII-specific IgG1 (KA ≥ 1010 M−1) and IgG4 titers peaked at ED22 with peak inhibitor titers of 796.0 BU/mL. Although a titer reduction of FVIII inhibitors and high-affinity FVIII-specific antibodies (KA ≥ 1010 M−1) was observed, FVIII inhibitors and high-affinity FVIII-specific antibodies persisted until the end of the study. ITI was terminated after ED524. A timeline with patient-specific clinical records for HIPS-ITI patient 4 is provided in supplemental Figure 3.
HIPS-ITI patient 5 presented with preexisting FVIII-binding IgG1 at HIPS baseline, and associated titers subsequently increased after study initiation. At ED11, FVIII inhibitors were first detected, which was accompanied by the appearance of FVIII-specific IgG3 and increased titers of high-affinity FVIII-specific IgG1 (KA ≥ 1010 M−1). FVIII-binding IgG2 and high-affinity FVIII-specific IgG4 (KA ∼1011 M−1) were first detectable at ED12. ITI was initiated on ED13. FVIII inhibitors and FVIII-specific IgG1, IgG2, and IgG4 reached their peak titers at ED40 with peak inhibitor titers of 124.0 BU/mL. The affinity of FVIII-specific IgG1 and IgG4 remained high (KA ≥ 1010 M−1). FVIII inhibitors and FVIII-specific IgG2 had disappeared at ED261, whereas IgG1 and IgG4 titers had dropped to 1:40 or below. Subsequently, FVIII-specific IgG4 titers and FVIII inhibitors increased again and persisted until the end of the study. ITI was terminated after ED360.
Appearance of apparent oligoreactive FVIII-binding antibodies during ITI
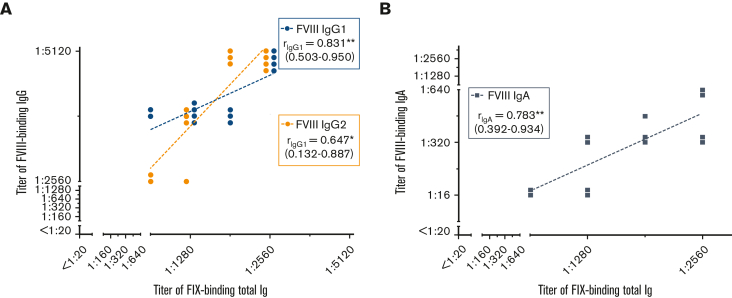
Two ITI patients, HIPS-ITI patient 2 (Figure 5B) and HIPS-ITI patient 5 (Figure 6B), developed apparent oligoreactive antibodies during ITI. Plasma samples of these patients contained antibodies that bound to FVIII and antibodies that bound to FIX, although these patients never received any FIX product. There were significant correlations between FVIII-binding IgG1, IgG2, respectively, IgA titers and FIX-binding total Ig titers (Figure 7). Importantly, the respective plasma samples did not contain any antibodies that bound to the uncoated ELISA plates, which were blocked with bovine serum albumin (supplemental Tables 2 and 3 [HIPS-ITI patient 2 and HIPS-ITI patient 5, respectively]).
Figure 5.
Apparent oligoreactive FVIII- and FIX-binding antibodies in HIPS-ITI patient 2 during HIPS and HIPS-ITI and timeline of clinical events. (A) Timeline of clinical events documented for HIPS-ITI patient 2 throughout HIPS and HIPS-ITI including (i) adverse events with short descriptions, (ii) infections and administered treatment, (iii) hospitalizations, duration of hospitalizations and administered treatment, (iv) immunizations and administered vaccinations, and (v) additionally administered medications and supplements. The yellow star marks the initiation of ITI treatment at ED16. (B) Apparent oligoreactive FVIII- (points, filled squares) and FIX-binding (asterisks) antibody titers as well as FVIII-specific (circles, open squares, open triangles) antibody titers (total Ig, IgG1, IgG2, IgG3, IgG4, IgA, IgM as indicated) and FVIII inhibitors (BU/mL) for HIPS-ITI patient 2. The red dotted line represents the limit for positive evaluation of FVIII inhibitors (0.6 BU/mL). The yellow star marks the initiation of ITI treatment at ED16. The continuous vertical line indicates the end of HIPS and the start of HIPS-ITI. DTaP-IPV-Hib, diphtheria, tetanus, pertussis, inactivated polio vaccine, Haemophilus influenzae type b; IIV4, quadrivalent-inactivated influenza vaccine; HAV, hepatitis A virus; PCV, pneumococcal-conjugated vaccine; PO, by mouth.
Figure 6.
Apparent oligoreactive FVIII- and FIX-binding antibodies in HIPS-ITI patient 5 during HIPS and HIPS-ITI and timeline of clinical events. (A) Timeline of clinical events documented for HIPS-ITI patient 5 throughout HIPS and HIPS-ITI including (i) adverse events with short descriptions, (ii) infections and administered treatment, (iii) hospitalizations, duration of hospitalizations and administered treatment, (iv) immunizations and administered vaccinations, and (v) additionally administered medications and supplements. The yellow star marks the initiation of ITI treatment at ED13. (B) Apparent oligoreactive FVIII- (points, filled squares) and FIX-binding (asterisks) antibody titers as well as FVIII-specific (circles, open squares, open triangles) antibody titers (total Ig, IgG1, IgG2, IgG3, IgG4, IgA, IgM as indicated) and FVIII inhibitors (BU/mL) for HIPS-ITI patient 5. The red dotted line represents the limit for positive evaluation of FVIII inhibitors (0.6 BU/mL). The yellow star marks the initiation of ITI treatment at ED13. The continuous vertical line indicates the end of HIPS and the start of HIPS-ITI. AV, arteriovenous; DTaPolio, diphtheria, tetanus, polio.
Figure 7.
Correlation between titers of apparent oligoreactive FVIII- and FIX-binding antibodies in HIPS-ITI patient 2 during HIPS-ITI. (A-B) Correlation analyses between apparent oligoreactive FVIII-binding IgG1 respectively IgG2 titers and FIX-binding total Ig (A) as well as apparent oligoreactive FVIII-binding IgA and FIX-binding total Ig (B) during HIPS-ITI (ED70 to ED388) of HIPS-ITI patient 2. Spearman correlation coefficients (r) with 95% CIs (given in brackets) are presented in the figure legends. Statistically significant correlations are highlighted, ∗P ≤ .05 and ∗∗P ≤ .01.
HIPS-ITI patient 2 developed apparent oligoreactive FVIII-binding IgG1 immediately after ITI initiation at ED16 and apparent oligoreactive FVIII-binding IgG2 and IgA around ED70 (Figure 5B). All 3 classes of apparent oligoreactive antibodies persisted until the end of the study. Apparent oligoreactive FVIII-binding IgG3 was transiently detected at ED44 and ED53, before FVIII-binding IgG3 disappeared (Figure 5B). Apparent oligoreactive FVIII-binding IgG4 was only observed at ED53. Subsequently, specific monoreactive FVIII-binding IgG4 was detected again and persisted until ED388 (Figure 5B). As indicated in Figure 5A, HIPS-ITI patient 2 had a soft tissue bleed (around ED10) and prolonged bleeding complications during port placement (around ED15). The latter required a 10-day hospitalization and patient monitoring period. These events coincided with the first appearance of apparent oligoreactive FVIII-binding IgG1.
HIPS-ITI patient 5 developed apparent oligoreactive FVIII-binding antibodies at a late stage during ITI at ED285, before the reappearance of FVIII inhibitors at ED356 (Figure 6B). Although apparent oligoreactive FVIII-binding IgG1, IgG2, and IgA persisted until the end of the study, apparent oligoreactive FVIII-binding IgG4 was only transiently observed at ED336 (Figure 6B). Between ED251 and ED327, HIPS-ITI patient 5 had a parvovirus infection, 3 tonsillitis events requiring antibiotic treatment, and a vascular access malfunction, which had to be treated surgically. These events preceded respectively coincided with the appearance of apparent oligoreactive FVIII-binding antibodies (Figure 6A).
Discussion
This article presents data that indicate profound changes in antibody signatures of FVIII-binding antibodies associated with successful ITI or ITI failure in patients who developed high-titer FVIII inhibitors during the HIPS study. Interestingly, 1 patient with partial ITI success and 1 patient with ITI failure developed apparent oligoreactive FVIII-binding antibodies during ITI. The biological significance of these antibodies requires further evaluation in future studies.
ITI success in HIPS-ITI patient 1 required not only the disappearance of FVIII inhibitors but also the disappearance or substantial titer minimization of high-affinity FVIII-specific antibodies, particularly of the IgG1 and IgG4 subclasses. Therefore, we hypothesize that an eradication or considerable clonal reduction of plasma cells secreting high-affinity FVIII-specific antibodies is essential to achieve ITI success. In addition, the formation of novel plasma cells producing high-affinity IgG1 and IgG4 antibodies would need to be prevented. Remaining low titers of FVIII-specific antibodies, which were close to the detection limit, could be produced either by persistent low levels of long-lived plasma cells or by other antibody-secreting cells such as marginal zone B cells or short-lived plasma cells. Marginal zone B cells can undergo both limited Ig class switch recombination and limited somatic hypermutations, resulting in the switch to IgG and IgA antibodies, and in antibody affinity maturation.53, 54, 55, 56, 57, 58 Persistent low levels of FVIII-specific antibodies might even be involved in the induction or maintenance of immune tolerance. IgG1 immune complexes, for example, have been speculated to be important for plasma cell homeostasis. They bind with high affinity to Fc γ receptor IIb (FcγRIIB), expressed on plasma cells, which can result in the induction of plasma cell apoptosis.59,60 Moreover, low-circulating levels of FVIII-specific antibodies might be produced by regulatory plasma cells, which have been described to be involved in immune regulation.61, 62, 63, 64, 65
Partial ITI success in HIPS-ITI patient 2 was associated with the disappearance of FVIII inhibitors and the disappearance of FVIII-specific IgG1 antibodies. However, this patient developed apparent oligoreactive FVIII-binding IgG1, IgG2, and IgA, as well as FIX-binding Ig, which persisted until the end of the study. Apparent oligoreactive IgG3 and IgG4 were only temporarily detected. Although FVIII inhibitors in this patient had disappeared, the residual FVIII activity dropped below 1% at ∼26 hours after a FVIII infusion at the end of the study. At this time, the patient had low-titer FVIII-specific IgG4, which was close to the detection limit and, therefore, similar in titer to the low-titer FVIII-specific IgG4 observed in patient 1, who successfully completed ITI. The clinical difference between patients 1 and 2 could be either due to the epitope recognized by the low-titer FVIII-specific IgG4 or due to the persistence of apparent oligoreactive FVIII-binding antibodies, which were only observed in patient 2. If these antibodies bind FVIII in vivo, they could contribute to the drop in residual FVIII activity after FVIII infusion. At present, we can only speculate about the true nature of these antibodies.
ITI failure in HIPS-ITI patients 3 and 4 was associated with persistent FVIII inhibitors and with the persistence of high-affinity FVIII-specific antibodies of the IgG1 and IgG4 subclasses. This antibody signature likely indicates the persistence of long-lived plasma cells producing high-affinity FVIII-specific antibodies. Long-term survival of plasma cells requires the intimate interaction with a specific microenvironment, for example, in survival niches of the bone marrow.66 It is not fully understood what determines the longevity of long-lived plasma cells. The upregulation of antiapoptotic factors seems to be an important determinant of plasma cell longevity.67 It has been speculated that different transcriptional programs are already imprinted in germinal center B cells during the germinal center reaction preceding plasma cell differentiation.68 Therefore, the local microenvironment during the germinal center reactions could determine the longevity of resulting antibody-producing plasma cells.
ITI failure in HIPS-ITI patient 5 was associated with a different antibody signature. FVIII inhibitors in this patient had already disappeared, and the titers of high-affinity FVIII-specific IgG1 and IgG4 had decreased to levels close to the detection limit (ED261) before the inhibitor reappeared and increased until study termination. At the same time, high-affinity FVIII-specific IgG4 reappeared and increased in titer. This antibody signature could reflect an initial eradication of FVIII inhibitors and a subsequent restimulation of FVIII-specific memory B cells and/or the generation of novel plasma cells producing FVIII inhibitors associated with high-affinity FVIII-specific IgG4. Interestingly, HIPS-ITI patient 5 developed apparent oligoreactive FVIII-binding antibodies that appeared before the reappearance of FVIII inhibitors. We can only speculate that the appearance of these antibodies might have negatively affected ITI success in this patient.
Following regulatory guidelines69,70 on how to analyze and report antidrug antibodies in clinical studies, we would report the apparent oligoreactive FVIII-binding antibodies observed in HIPS-ITI patients 2 and 5 as negative antibody results because we could not show specificity using our standard competition-based specificity assays. However, we decided to report these data as apparent oligoreactive antibodies to stimulate discussion and future studies of such antibodies, which might appear during ITI in some patients with FVIII inhibitors. Currently, it is well accepted that the natural antibody repertoire contains antibodies that can bind to a variety of totally unrelated self and foreign antigens (ie, oligoreactive or polyreactive antibodies).71 More recent studies have demonstrated that circulating antibodies can acquire polyreactivity upon exposure to protein-destabilizing agents,72,73 low-pH environments,74,75 and redox-active substances and cofactors, such as reactive oxygen species,76,77 ferrous ions,78,79 and heme, respectively.80 Prolonged periods of innate immune stimulation (“high immunologic danger”) induced by infections, inflammations, vaccinations, or prolonged bleeding episodes can result in the release of these proinflammatory mediators, which have been demonstrated to foster polyreactivity of antibodies.81, 82, 83, 84, 85 HIPS-ITI patient 5 had a parvovirus infection and tonsillitis, which required 2 courses of antibiotics. Shortly afterward, the patient required surgery because of vascular access malfunction and experienced 2 more tonsillitis events. These events were observed at the same time as the first appearance of his apparent oligoreactive antibodies. HIPS-ITI patient 2 had a soft tissue bleed and prolonged bleeding complications during port placement. From ED53 onward, the patient received an oral iron supplement. For a short period, iron was administered parenterally via the same port as FVIII. Recently, Peyron et al demonstrated that iron supplements administered together with FVIII can cause FVIII oxidation.86 We can only speculate that these clinical events might have facilitated the appearance of circulating apparent oligoreactive antibodies.
A major limitation of this study is the small number of patients who could be included in the HIPS-ITI extension study. The study results must be interpreted with caution. Our conclusions should be considered as hypotheses that require further evaluation in future studies. In particular, the development of apparent oligoreactive FVIII-binding antibodies during ITI requires more follow-ups, especially a comprehensive assessment of the true nature of these antibodies. We were not able to extend the scope of the HIPS-ITI extension study and to initiate follow-up studies with these antibodies because of the limited amount of plasma that was available from the infant patients.
In summary, we conclude that the disappearance of FVIII inhibitors during the HIPS-ITI extension was associated with a removal or titer minimization of circulating high-affinity FVIII-specific antibodies. One patient with partial ITI success and 1 patient with ITI failure developed apparent oligoreactive FVIII-binding antibodies during ITI. Follow-up studies are important to confirm the development of such antibodies during ITI and assess the true nature of such antibodies.
Conflict-of-interest disclosure: H.P., V.B., and D.L.B. received research funding for institution from Baxalta Innovations GmbH, a Takeda company. B.G. is an employee of Baxalta Innovations GmbH, a Takeda company, and holds stock options of Takeda. J. Bowen received research funding from the study sponsor, University of Texas Health Science Center. P.L. received research funding from the study sponsor, University of Texas Health Science Center, and was an employee of Rho Inc. at the time of the study. J. Blatný received consultation/speakers fee from Takeda, Novo Nordisk, Sobi, LFB, Roche, Pfizer, CSL Behring, and Octapharma. C.M. received fees to institution for study participation from Bayer, Baxalta/Shire/Takeda, Biotest, CSL Behring, Novo Nordisk, and Sobi; unrestricted grant to institution from Biotest and CSL Behring; and personal honoraria (consultancy, speaker, chair) from Bayer, Biotest, CSL Behring, Novo Nordisk, Roche, and Pfizer. V.C.R. received research funding to institution and fees to institution for study participation from Takeda, Pfizer, and Grifols. R.D. was an employee of Baylor College of Medicine at the time of the study. M.E.M. received consultation, advisory, and speaker fees from Bayer, BioMarin, Catalyst Bioscience, CSL Behring, Grifols, Kedrion, LFB, Novo Nordisk, Octapharma, Pfizer, Roche, Sanofi, Sobi, Spark Therapeutics, Takeda, and uniQure. B.M.R. was an employee of Baxalta Innovations GmbH, a Takeda company, at the time of the study.
Acknowledgments
The authors thank Keith Hoots and Donna DiMichele for their insights into the study design and analyses. The authors also thank Fritz Scheiflinger (an employee of Baxalta Innovations GmbH, a Takeda company, Vienna, Austria, at the time of the study), who supported the analytical part of the study, and Elizabeth Donnachie, who performed the center qualification of the US clinical centers that participated in the study. HIPS-ITI, as an extension arm to the original HIPS study, is a collaborative clinical research study funded by Baxalta Innovations GmbH, a Takeda company.
Authorship
Contribution: H.P. established the assays, managed the immunological analysis, and wrote the manuscript; H.P. and V.B. ran the antibody analysis and created antibody figures; H.P., V.B., and B.G. reviewed and interpreted the immunological data; V.B., B.G., J. Bowen, P.L., J. Blatný, C.M., V.C.R., R.D., M.E.M., and D.L.B. reviewed and edited the manuscript; J. Bowen assisted with management and completion of the study and collected clinical data; J. Bowen and P.L. reviewed data displays; P.L. extracted relevant clinical data and created analysis data sets; J. Blatný, C.M., V.C.R., R.D., and M.E.M. cared for study subjects; M.E.M. and D.L.B. were coprincipal investigators; M.E.M., D.L.B., and B.M.R. reviewed and interpreted data; D.L.B. designed the study plan; and B.M.R. designed the immunological program of the study and wrote and edited the manuscript.
Footnotes
Data are available on request from the corresponding author, Birgit M. Reipert (birgit.reipert@fh-krems.ac.at).
The full-text version of this article contains a data supplement.
Supplementary Material
References
- 1.Gouw SC, van der Bom JG, Ljung R, et al. Factor VIII products and inhibitor development in severe hemophilia A. N Engl J Med. 2013;368(3):231–239. doi: 10.1056/NEJMoa1208024. [DOI] [PubMed] [Google Scholar]
- 2.Peyvandi F, Mannucci PM, Garagiola I, et al. A randomized trial of factor VIII and neutralizing antibodies in hemophilia A. N Engl J Med. 2016;374(21):2054–2064. doi: 10.1056/NEJMoa1516437. [DOI] [PubMed] [Google Scholar]
- 3.Wight J, Paisley S. The epidemiology of inhibitors in haemophilia A: a systematic review. Haemophilia. 2003;9(4):418–435. doi: 10.1046/j.1365-2516.2003.00780.x. [DOI] [PubMed] [Google Scholar]
- 4.Lusher JM, Arkin S, Abildgaard CF, Schwartz RS. Recombinant factor VIII for the treatment of previously untreated patients with hemophilia A. Safety, efficacy, and development of inhibitors. Kogenate Previously Untreated Patient Study Group. N Engl J Med. 1993;328(7):453–459. doi: 10.1056/NEJM199302183280701. [DOI] [PubMed] [Google Scholar]
- 5.Auerswald G, Thompson AA, Recht M, et al. Experience of Advate rAHF-PFM in previously untreated patients and minimally treated patients with haemophilia A. Thromb Haemost. 2012;107(6):1072–1082. doi: 10.1160/TH11-09-0642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Oldenburg J, Mahlangu JN, Bujan W, et al. The effect of emicizumab prophylaxis on health-related outcomes in persons with haemophilia A with inhibitors: HAVEN 1 study. Haemophilia. 2019;25(1):33–44. doi: 10.1111/hae.13618. [DOI] [PubMed] [Google Scholar]
- 7.Oldenburg J, Mahlangu JN, Kim B, et al. Emicizumab prophylaxis in hemophilia A with inhibitors. N Engl J Med. 2017;377(9):809–818. doi: 10.1056/NEJMoa1703068. [DOI] [PubMed] [Google Scholar]
- 8.Carpenter SL, Khair K, Gringeri A, Valentino LA. Prophylactic bypassing agent use before and during immune tolerance induction in patients with haemophilia A and inhibitors to FVIII. Haemophilia. 2018;24(4):570–577. doi: 10.1111/hae.13534. [DOI] [PubMed] [Google Scholar]
- 9.Collins PW, Chalmers E, Hart DP, et al. Diagnosis and treatment of factor VIII and IX inhibitors in congenital haemophilia: (4th edition). UK Haemophilia Centre Doctors Organization. Br J Haematol. 2013;160(2):153–170. doi: 10.1111/bjh.12091. [DOI] [PubMed] [Google Scholar]
- 10.Nakar C, Shapiro A. Hemophilia A with inhibitor: immune tolerance induction (ITI) in the mirror of time. Transfus Apher Sci. 2019;58(5):578–589. doi: 10.1016/j.transci.2019.08.008. [DOI] [PubMed] [Google Scholar]
- 11.Osooli M, Berntorp E. Inhibitors in haemophilia: what have we learned from registries? A systematic review. J Intern Med. 2015;277(1):1–15. doi: 10.1111/joim.12301. [DOI] [PubMed] [Google Scholar]
- 12.Hay CR, DiMichele DM. The principal results of the International Immune Tolerance Study: a randomized dose comparison. Blood. 2012;119(6):1335–1344. doi: 10.1182/blood-2011-08-369132. [DOI] [PubMed] [Google Scholar]
- 13.Valentino LA, Kempton CL, Kruse-Jarres R, Mathew P, Meeks SL, Reiss UM. US guidelines for immune tolerance induction in patients with haemophilia A and inhibitors Haemophilia. 2015;21(5):559–567. doi: 10.1111/hae.12730. [DOI] [PubMed] [Google Scholar]
- 14.Ljung RCR. How I manage patients with inherited haemophilia A and B and factor inhibitors. Br J Haematol. 2018;180(4):501–510. doi: 10.1111/bjh.15053. [DOI] [PubMed] [Google Scholar]
- 15.Di Minno G, Coppola A, Margaglione M, et al. Predictors of inhibitor eradication by primary immune tolerance induction in severe haemophilia A with high responding inhibitors. Haemophilia. 2022;28(1):55–64. doi: 10.1111/hae.14431. [DOI] [PubMed] [Google Scholar]
- 16.Benson G, Auerswald G, Elezović I, et al. Immune tolerance induction in patients with severe hemophilia with inhibitors: expert panel views and recommendations for clinical practice. Eur J Haematol. 2012;88(5):371–379. doi: 10.1111/j.1600-0609.2012.01754.x. [DOI] [PubMed] [Google Scholar]
- 17.Dimichele D. Inhibitors: resolving diagnostic and therapeutic dilemmas. Haemophilia. 2002;8(3):280–287. doi: 10.1046/j.1365-2516.2002.00626.x. [DOI] [PubMed] [Google Scholar]
- 18.Brackmann HH, White GC, 2nd, Berntorp E, Andersen T, Escuriola-Ettingshausen C. Immune tolerance induction: what have we learned over time? Haemophilia. 2018;24(Suppl 3):3–14. doi: 10.1111/hae.13445. [DOI] [PubMed] [Google Scholar]
- 19.DiMichele DM. Inhibitors in haemophilia: a primer. Haemophilia. 2000;6(suppl 1):38–40. doi: 10.1046/j.1365-2516.2000.00045.x. [DOI] [PubMed] [Google Scholar]
- 20.Reipert BM, van Helden PM, Schwarz HP, Hausl C. Mechanisms of action of immune tolerance induction against factor VIII in patients with congenital haemophilia A and factor VIII inhibitors. Br J Haematol. 2007;136(1):12–25. doi: 10.1111/j.1365-2141.2006.06359.x. [DOI] [PubMed] [Google Scholar]
- 21.Hausl C, Ahmad RU, Sasgary M, et al. High-dose factor VIII inhibits factor VIII-specific memory B cells in hemophilia A with factor VIII inhibitors. Blood. 2005;106(10):3415–3422. doi: 10.1182/blood-2005-03-1182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reipert BM, Allacher P, Hausl C, et al. Modulation of factor VIII-specific memory B cells. Haemophilia. 2010;16(102):25–34. doi: 10.1111/j.1365-2516.2008.01962.x. [DOI] [PubMed] [Google Scholar]
- 23.van Helden PM, Kaijen PH, Fijnvandraat K, van den Berg HM, Voorberg J. Factor VIII-specific memory B cells in patients with hemophilia A. J Thromb Haemost. 2007;5(11):2306–2308. doi: 10.1111/j.1538-7836.2007.02736.x. [DOI] [PubMed] [Google Scholar]
- 24.Chen TC, Cobbold SP, Fairchild PJ, Waldmann H. Generation of anergic and regulatory T cells following prolonged exposure to a harmless antigen. J Immunol. 2004;172(10):5900–5907. doi: 10.4049/jimmunol.172.10.5900. [DOI] [PubMed] [Google Scholar]
- 25.Apostolou I, von Boehmer H. In vivo instruction of suppressor commitment in naive T cells. J Exp Med. 2004;199(10):1401–1408. doi: 10.1084/jem.20040249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schep SJ, Schutgens REG, Fischer K, Boes ML. Review of immune tolerance induction in hemophilia A. Blood Rev. 2018;32(4):326–338. doi: 10.1016/j.blre.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 27.Coutinho A. Will the idiotypic network help to solve natural tolerance? Trends Immunol. 2003;24(2):53–54. doi: 10.1016/s1471-4906(02)00035-2. [DOI] [PubMed] [Google Scholar]
- 28.Gilles JG, Saint-Remy JM. Healthy subjects produce both anti-factor VIII and specific anti-idiotypic antibodies. J Clin Invest. 1994;94(4):1496–1505. doi: 10.1172/JCI117489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gilles JG, Desqueper B, Lenk H, Vermylen J, Saint-Remy JM. Neutralizing antiidiotypic antibodies to factor VIII inhibitors after desensitization in patients with hemophilia A. J Clin Invest. 1996;97(6):1382–1388. doi: 10.1172/JCI118558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Oldenburg J, Schröder J, Brackmann HH, Müller-Reible C, Schwaab R, Tuddenham E. Environmental and genetic factors influencing inhibitor development. Semin Hematol. 2004;41(1 suppl 1):82–88. doi: 10.1053/j.seminhematol.2003.11.016. [DOI] [PubMed] [Google Scholar]
- 31.Pavlova A, Delev D, Lacroix-Desmazes S, et al. Impact of polymorphisms of the major histocompatibility complex class II, interleukin-10, tumor necrosis factor-alpha and cytotoxic T-lymphocyte antigen-4 genes on inhibitor development in severe hemophilia A. J Thromb Haemost. 2009;7(12):2006–2015. doi: 10.1111/j.1538-7836.2009.03636.x. [DOI] [PubMed] [Google Scholar]
- 32.Gouw SC, van den Berg HM, Oldenburg J, et al. F8 gene mutation type and inhibitor development in patients with severe hemophilia A: systematic review and meta-analysis. Blood. 2012;119(12):2922–2934. doi: 10.1182/blood-2011-09-379453. [DOI] [PubMed] [Google Scholar]
- 33.Carpenter SL, Michael Soucie J, Sterner S, Presley R, Hemophilia Treatment Center Network I. Increased prevalence of inhibitors in Hispanic patients with severe haemophilia A enrolled in the Universal Data Collection database. Haemophilia. 2012;18(3):e260–e265. doi: 10.1111/j.1365-2516.2011.02739.x. [DOI] [PubMed] [Google Scholar]
- 34.Aledort LM, Dimichele DM. Inhibitors occur more frequently in African-American and Latino haemophiliacs. Haemophilia. 1998;4(1):68. doi: 10.1046/j.1365-2516.1998.0146c.x. [DOI] [PubMed] [Google Scholar]
- 35.Viel KR, Ameri A, Abshire TC, et al. Inhibitors of factor VIII in black patients with hemophilia. N Engl J Med. 2009;360(16):1618–1627. doi: 10.1056/NEJMoa075760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Astermark J. Inhibitor development: patient-determined risk factors. Haemophilia. 2010;16(102):66–70. doi: 10.1111/j.1365-2516.2008.01923.x. [DOI] [PubMed] [Google Scholar]
- 37.Maclean PS, Richards M, Williams M, et al. Treatment related factors and inhibitor development in children with severe haemophilia A. Haemophilia. 2011;17(2):282–287. doi: 10.1111/j.1365-2516.2010.02422.x. [DOI] [PubMed] [Google Scholar]
- 38.Eckhardt CL, van der Bom JG, van der Naald M, Peters M, Kamphuisen PW, Fijnvandraat K. Surgery and inhibitor development in hemophilia A: a systematic review. J Thromb Haemost. 2011;9(10):1948–1958. doi: 10.1111/j.1538-7836.2011.04467.x. [DOI] [PubMed] [Google Scholar]
- 39.Auerswald G, Bidlingmaier C, Kurnik K. Early prophylaxis/FVIII tolerization regimen that avoids immunological danger signals is still effective in minimizing FVIII inhibitor developments in previously untreated patients--long-term follow-up and continuing experience. Haemophilia. 2012;18(1):e18–e20. doi: 10.1111/j.1365-2516.2011.02659.x. [DOI] [PubMed] [Google Scholar]
- 40.Lövgren KM, Søndergaard H, Skov S, Wiinberg B. Non-genetic risk factors in haemophilia A inhibitor management - the danger theory and the use of animal models. Haemophilia. 2016;22(5):657–666. doi: 10.1111/hae.13075. [DOI] [PubMed] [Google Scholar]
- 41.Lacroix-Desmazes S, Voorberg J, Lillicrap D, Scott DW, Pratt KP. Tolerating factor VIII: recent progress. Front Immunol. 2020;10:2991. doi: 10.3389/fimmu.2019.02991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schep SJ, Boes M, Schutgens REG, van Vulpen LFD. An update on the ‘danger theory’ in inhibitor development in hemophilia A. Expert Rev Hematol. 2019;12(5):335–344. doi: 10.1080/17474086.2019.1604213. [DOI] [PubMed] [Google Scholar]
- 43.Kasper CK, Aledort L, Aronson D, et al. Proceedings: A more uniform measurement of factor VIII inhibitors. Thromb Diath Haemorrh. 1975;34(2):612. [PubMed] [Google Scholar]
- 44.Verbruggen B, Novakova I, Wessels H, Boezeman J, van den Berg M, Mauser-Bunschoten E. The Nijmegen modification of the Bethesda assay for factor VIII:C inhibitors: improved specificity and reliability. Thromb Haemost. 1995;73(2):247–251. [PubMed] [Google Scholar]
- 45.Miller CH. Laboratory testing for factor VIII and IX inhibitors in haemophilia: a review. Haemophilia. 2018;24(2):186–197. doi: 10.1111/hae.13424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Whelan SF, Hofbauer CJ, Horling FM, et al. Distinct characteristics of antibody responses against factor VIII in healthy individuals and in different cohorts of hemophilia A patients. Blood. 2013;121(6):1039–1048. doi: 10.1182/blood-2012-07-444877. [DOI] [PubMed] [Google Scholar]
- 47.Hofbauer CJ, Whelan SF, Hirschler M, et al. Affinity of FVIII-specific antibodies reveals major differences between neutralizing and nonneutralizing antibodies in humans. Blood. 2015;125(7):1180–1188. doi: 10.1182/blood-2014-09-598268. [DOI] [PubMed] [Google Scholar]
- 48.Cannavo A, Valsecchi C, Garagiola I, et al. Nonneutralizing antibodies against factor VIII and risk of inhibitor development in severe hemophilia A. Blood. 2017;129(10):1245–1250. doi: 10.1182/blood-2016-06-720086. [DOI] [PubMed] [Google Scholar]
- 49.Krudysz-Amblo J, Parhami-Seren B, Butenas S, et al. Quantitation of anti-factor VIII antibodies in human plasma. Blood. 2009;113(11):2587–2594. doi: 10.1182/blood-2008-08-174987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pratt KP, Gunasekera D, Vir P, et al. Neutralizing and non-neutralizing anti-FVIII antibodies in black and white hemophilia A subjects: a natural history profile. Blood. 2019;134(suppl 1):1131. [Google Scholar]
- 51.Schweiger H, Rejtő J, Hofbauer CJ, et al. Nonneutralizing FVIII-specific antibody signatures in patients with hemophilia A and in healthy donors. Blood Adv. 2022;6(3):946–958. doi: 10.1182/bloodadvances.2021005745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Reipert BM, Gangadharan B, Hofbauer CJ, et al. The prospective Hemophilia Inhibitor PUP Study reveals distinct antibody signatures prior to FVIII inhibitor development. Blood Adv. 2020;4(22):5785–5796. doi: 10.1182/bloodadvances.2020002731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Puga I, Cols M, Barra CM, et al. B cell-helper neutrophils stimulate the diversification and production of immunoglobulin in the marginal zone of the spleen. Nat Immunol. 2011;13(2):170–180. doi: 10.1038/ni.2194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Guinamard R, Okigaki M, Schlessinger J, Ravetch JV. Absence of marginal zone B cells in Pyk-2-deficient mice defines their role in the humoral response. Nat Immunol. 2000;1(1):31–36. doi: 10.1038/76882. [DOI] [PubMed] [Google Scholar]
- 55.MacLennan IC, Toellner KM, Cunningham AF, et al. Extrafollicular antibody responses. Immunol Rev. 2003;194:8–18. doi: 10.1034/j.1600-065x.2003.00058.x. [DOI] [PubMed] [Google Scholar]
- 56.Hendricks J, Bos NA, Kroese FGM. Heterogeneity of memory marginal zone B cells. Crit Rev Immunol. 2018;38(2):145–158. doi: 10.1615/CritRevImmunol.2018024985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Allman D, Wilmore JR, Gaudette BT. The continuing story of T-cell independent antibodies. Immunol Rev. 2019;288(1):128–135. doi: 10.1111/imr.12754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Zuccarino-Catania GV, Sadanand S, Weisel FJ, et al. CD80 and PD-L2 define functionally distinct memory B cell subsets that are independent of antibody isotype. Nat Immunol. 2014;15(7):631–637. doi: 10.1038/ni.2914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Xiang Z, Cutler AJ, Brownlie RJ, et al. FcgammaRIIb controls bone marrow plasma cell persistence and apoptosis. Nat Immunol. 2007;8(4):419–429. doi: 10.1038/ni1440. [DOI] [PubMed] [Google Scholar]
- 60.Nutt SL, Hodgkin PD, Tarlinton DM, Corcoran LM. The generation of antibody-secreting plasma cells. Nat Rev Immunol. 2015;15(3):160–171. doi: 10.1038/nri3795. [DOI] [PubMed] [Google Scholar]
- 61.Lino AC, Dang VD, Lampropoulou V, et al. LAG-3 inhibitory receptor expression identifies immunosuppressive natural regulatory plasma cells. Immunity. 2018;49(1):120–133.e9. doi: 10.1016/j.immuni.2018.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Matsumoto M, Baba A, Yokota T, et al. Interleukin-10-producing plasmablasts exert regulatory function in autoimmune inflammation. Immunity. 2014;41(6):1040–1051. doi: 10.1016/j.immuni.2014.10.016. [DOI] [PubMed] [Google Scholar]
- 63.Suan D, Kräutler NJ, Maag JLV, et al. CCR6 defines memory B cell precursors in mouse and human germinal centers, revealing light-zone location and predominant low antigen affinity. Immunity. 2017;47(6):1142–1153.e4. doi: 10.1016/j.immuni.2017.11.022. [DOI] [PubMed] [Google Scholar]
- 64.Higgins BW, McHeyzer-Williams LJ, McHeyzer-Williams MG. Programming isotype-specific plasma cell function. Trends Immunol. 2019;40(4):345–357. doi: 10.1016/j.it.2019.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fillatreau S. Regulatory functions of B cells and regulatory plasma cells. Biomed J. 2019;42(4):233–242. doi: 10.1016/j.bj.2019.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Slamanig SA, Nolte MA. The bone marrow as sanctuary for plasma cells and memory T-cells: implications for adaptive immunity and vaccinology. Cells. 2021;10(6):1–25. doi: 10.3390/cells10061508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Nguyen DC, Duan M, Ali M, Ley A, Sanz I, Lee FE. Plasma cell survival: the intrinsic drivers, migratory signals, and extrinsic regulators. Immunol Rev. 2021;303(1):138–153. doi: 10.1111/imr.13013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Schuh W, Mielenz D, Jäck HM. Unraveling the mysteries of plasma cells. Adv Immunol. 2020;146:57–107. doi: 10.1016/bs.ai.2020.01.002. [DOI] [PubMed] [Google Scholar]
- 69.Committee for Medicinal Products for Human Use . European Medicines Agency; 2017. Guideline on Immunogenicity assessment of therapeutic proteins. [Google Scholar]
- 70.Center for Drug Evaluation and Research, Center for Biologics Evaluation and Research. Guidance Document . Food and Drug Administration; United States: 2019. Immunogenicity Testing of Therapeutic Protein Products −Developing and Validating Assays for Anti-Drug Antibody Detection. [Google Scholar]
- 71.Notkins AL. Polyreactivity of antibody molecules. Trends Immunol. 2004;25(4):174–179. doi: 10.1016/j.it.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 72.Cabiedes J, Cabral AR, Alarcón-Segovia D. Hidden anti-phospholipid antibodies in normal human sera circulate as immune complexes whose antigen can be removed by heat, acid, hypermolar buffers or phospholipase treatments. Eur J Immunol. 1998;28(7):2108–2114. doi: 10.1002/(SICI)1521-4141(199807)28:07<2108::AID-IMMU2108>3.0.CO;2-R. [DOI] [PubMed] [Google Scholar]
- 73.Bouvet JP, Stahl D, Rose S, Quan CP, Kazatchkine MD, Kaveri SV. Induction of natural autoantibody activity following treatment of human immunoglobulin with dissociating agents. J Autoimmun. 2001;16(2):163–172. doi: 10.1006/jaut.2000.0472. [DOI] [PubMed] [Google Scholar]
- 74.McMahon MJ, O'Kennedy R. Polyreactivity as an acquired artefact, rather than a physiologic property, of antibodies: evidence that monoreactive antibodies may gain the ability to bind to multiple antigens after exposure to low pH. J Immunol Methods. 2000;241(1-2):1–10. doi: 10.1016/s0022-1759(00)00196-4. [DOI] [PubMed] [Google Scholar]
- 75.Djoumerska-Alexieva IK, Dimitrov JD, Voynova EN, Lacroix-Desmazes S, Kaveri SV, Vassilev TL. Exposure of IgG to an acidic environment results in molecular modifications and in enhanced protective activity in sepsis. FEBS J. 2010;277(14):3039–3050. doi: 10.1111/j.1742-4658.2010.07714.x. [DOI] [PubMed] [Google Scholar]
- 76.Alom-Ruiz SP, Anilkumar N, Shah AM. Reactive oxygen species and endothelial activation. Antioxid Redox Signal. 2008;10(6):1089–1100. doi: 10.1089/ars.2007.2007. [DOI] [PubMed] [Google Scholar]
- 77.Dimitrov JD, Ivanovska ND, Lacroix-Desmazes S, Doltchinkova VR, Kaveri SV, Vassilev TL. Ferrous ions and reactive oxygen species increase antigen-binding and anti-inflammatory activities of immunoglobulin G. J Biol Chem. 2006;281(1):439–446. doi: 10.1074/jbc.M509190200. [DOI] [PubMed] [Google Scholar]
- 78.Biemond P, Swaak AJ, van Eijk HG, Koster JF. Superoxide dependent iron release from ferritin in inflammatory diseases. Free Radic Biol Med. 1988;4(3):185–198. doi: 10.1016/0891-5849(88)90026-3. [DOI] [PubMed] [Google Scholar]
- 79.Brieland JK, Fantone JC. Ferrous iron release from transferrin by human neutrophil-derived superoxide anion: effect of pH and iron saturation. Arch Biochem Biophys. 1991;284(1):78–83. doi: 10.1016/0003-9861(91)90266-l. [DOI] [PubMed] [Google Scholar]
- 80.Dimitrov JD, Roumenina LT, Doltchinkova VR, et al. Antibodies use heme as a cofactor to extend their pathogen elimination activity and to acquire new effector functions. J Biol Chem. 2007;282(37):26696–26706. doi: 10.1074/jbc.M702751200. [DOI] [PubMed] [Google Scholar]
- 81.Dimitrov JD, Planchais C, Roumenina LT, Vassilev TL, Kaveri SV, Lacroix-Desmazes S. Antibody polyreactivity in health and disease: Statu variabilis. J Immunol. 2013;191(3):993–999. doi: 10.4049/jimmunol.1300880. [DOI] [PubMed] [Google Scholar]
- 82.Kazatchkine MD, Kaveri SV. Immunomodulation of autoimmune and inflammatory diseases with intravenous immune globulin. N Engl J Med. 2001;345(10):747–755. doi: 10.1056/NEJMra993360. [DOI] [PubMed] [Google Scholar]
- 83.Dimitrov JD, Planchais C, Scheel T, et al. A cryptic polyreactive antibody recognizes distinct clades of HIV-1 glycoprotein 120 by an identical binding mechanism. J Biol Chem. 2014;289(25):17767–17779. doi: 10.1074/jbc.M114.556266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Roumenina LT, Rayes J, Lacroix-Desmazes S, Dimitrov JD. Heme: modulator of plasma systems in hemolytic diseases. Trends Mol Med. 2016;22(3):200–213. doi: 10.1016/j.molmed.2016.01.004. [DOI] [PubMed] [Google Scholar]
- 85.Guthmiller JJ, Lan LY, Fernández-Quintero ML, et al. Polyreactive broadly neutralizing B cells are selected to provide defense against pandemic threat influenza viruses. Immunity. 2020;53(6):1230–1244.e5. doi: 10.1016/j.immuni.2020.10.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Peyron I, Dimitrov JD, Delignat S, et al. Oxidation of factor VIII increases its immunogenicity in mice with severe hemophilia A. Cell Immunol. 2018;325:64–68. doi: 10.1016/j.cellimm.2018.01.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.