Abstract
Background
Endoscopic retrograde cholangiopancreatography (ERCP) and EUS are challenging procedures requiring a high level of expertise to provide effective and safe patient care. Thus, high‐quality training is needed to achieve competence. We aimed to evaluate the status of European ERCP/EUS training programs, to evaluate adherence to international recommendations, and to propose possible solutions for future improvements.
Methods
A web‐based survey was developed and ERCP/EUS experts and trainees across Europe were invited to participate.
Results
Forty‐one experts (out of 50; 82%) and 30 trainees (out of 70; 42.9%) from 18 countries answered the questionnaire. The training program application process is mainly driven by individual requests (87.8%). All surveyed departments offer combined ERCP/EUS training and the majority have adequate facilities and trainers. Although centers are high‐volume and provide long‐term fellowships, trainee hands‐on exposure is not very high (43% expect to do (or did) 100–150 ERCPs and 69% up to 150 EUSs). A formal curriculum is in place in 53.7% centers, including simulation‐training in 27.3%. Competence is assessed in 65.7% of centers, but validated tools are applied in only 33.3%.
Conclusions
This survey first provides an overview of ERCP/EUS training programs across Europe. It shows that there is adherence to international guidelines to a certain degree, but several gaps in the application process, use of simulators for training, training curriculum and assessment of performance have been recognized. Overcoming these shortcomings could serve as a basis for further improvement in ERCP/EUS training.
Keywords: Curriculum, ERCP, Europe, EUS, training
Key summary.
ERCP and EUS are challenging procedures requiring a high level of expertise to provide effective and safe patient care. Thus, high‐quality training is needed to achieve competence.
We aimed to evaluate the status of European Endoscopic retrograde cholangiopancreatography (ERCP)/endoscopic ultrasound (EUS) training programs and the adherence to international recommendations, and to propose possible solutions for future improvements, through the development of a web‐based survey that was distributed to ERCP/EUS experts and trainees across Europe.
Participants across 18 European countries answered the questionnaire, providing a first overview of ERCP/EUS training programs across Europe.
There is adherence to international guidelines to a certain degree, but several gaps in the application process, use of simulators for training, training curriculum and assessment of performance have been recognized.
Overcoming these shortcomings could serve as a basis for further improvement in ERCP/EUS training.
INTRODUCTION
Digestive endoscopy is becoming more complex and subspecialized, with a growing number of different advanced gastrointestinal endoscopy procedures available, such as Endoscopic retrograde cholangiopancreatography (ERCP) and interventional endoscopic ultrasound (EUS). However, these challenging procedures raise the risk of adverse events and, because they are highly operator‐dependent, require a high level of endoscopic expertise comprised unique technical, cognitive, and integrative skills. 1
Quality in endoscopy is highly dependent on the quality of training. 2 Consequently, there is an increasing need for dedicated ERCP/EUS training to develop these specialized competencies, reflecting the growing number of training programs in the United States and Europe. 3 However, we must also consider the potential additional impact of trainee participation in critical outcomes of already risky procedures such as ERCP and EUS, 4 , 5 , 6 , 7 further raising the requirement for high standards of quality in these programs.
To reduce the variation in the quality of endoscopy procedures, which significantly impacts patient outcomes, 8 international societies, such as the European Society of Gastrointestinal Endoscopy (ESGE), have increasingly embraced the quality improvement paradigm. This initiative involves the development of evidence‐based reviews, issuing fundamental recommendations that should be followed to standardize and optimize quality in ERCP/EUS performance 9 and curriculum training 10 and ensuring patients are optimally managed. Nonetheless, despite the publication of these ERCP/EUS training and credentialing recommendations, the capability of European fellowships to meet these guidelines has not been adequately assessed. 11
The current study aimed to evaluate the status of European ERCP/EUS training programs, analyze adherence to international recommendations, and propose possible solutions for future improvements.
METHODS
Study design and participants
A cross‐sectional web survey examining the status of European ERCP/EUS training programs, current infrastructures and competence assessment, and adherence to ESGE guidelines was conducted from January to March 2022.
Training Program Directors (PD) and Experts from a list of 50 European ERCP and EUS training centers, recognized by ESGE and/or other national organizations, were invited to answer the survey. Experts were also asked to name up to three trainees that would be willing to participate and an invitation was also sent to them.
Development and content of survey instrument
Two online Google form survey instruments were developed, one for PD/Experts and the other for trainees (Supplementary material 1s, 2s). The five‐part survey items consisted of 37 and 27 questions, respectively, organized into the following domains: characterization of the current process for ERCP/EUS training application; characterization of ERCP/EUS training departments; characterization of ERCP/EUS trainers; evaluation of departments' adherence to ESGE Curriculum; evaluation of PD/experts and trainees' overall opinions regarding the current ERCP/EUS training and determination of opportunities for improvement.
The questions were formatted as open‐ended, check all that apply, multiple‐choice, yes or no, 5‐point Likert scales (anchors ranging from “strongly agree” to “strongly disagree”; or from “Extremely important” to “not important”) and boxes for free‐text comments.
The final survey version was distributed after pilot testing among the authors.
Survey distribution and collection of data
The survey was disseminated to experts and trainees via email. The email invitation was introduced by a brief statement describing the purpose of the data and informing respondents that their participation constituted their voluntary consent to the study, and a link to the survey was included. Two mailing reminders were sent to non‐respondents to encourage maximum participation. All information provided per user was automatically recorded in a software database (Microsoft Excel).
Ethics committee approval was not obtained since this study involved no sharing of patient data.
Survey responses were voluntary and individual answers remained confidential and only seen by the researchers. Published data is reported as average or as totals from the group, no individual responses were reported and data is not directly traceable to participants.
Study endpoints
Primary endpoint: assess the organization of current ERCP/EUS training programs.
Secondary endpoints: document endoscopist adherence to current recommendations and determine possible improvement solutions.
Data analysis
Quantitative data are expressed as mean and standard deviation and categorical data as number and percentage. All calculations were performed using Microsoft Excel.
RESULTS
The response rate was 82% from the experts (from 41 departments out of 50) and 42.9% from the trainees (30 out of 70) from 18 European countries (Figure 1).
FIGURE 1.
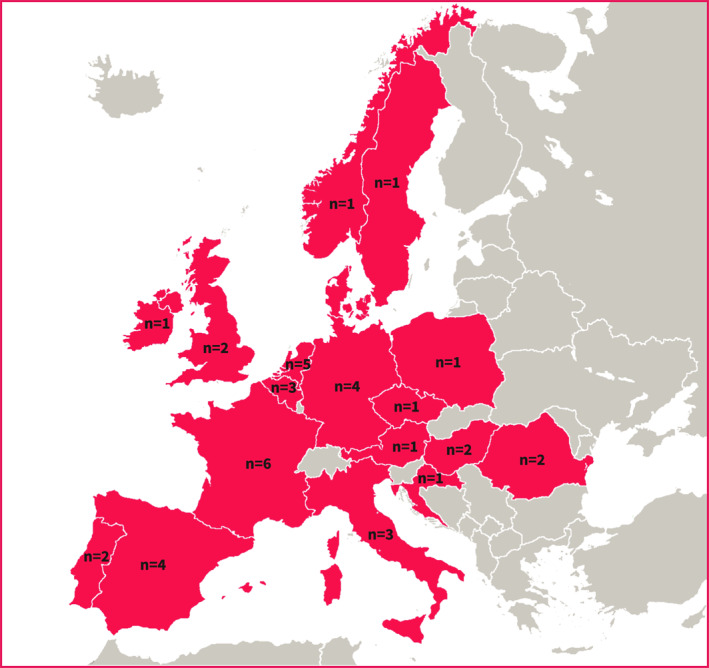
Geographical distribution of respondents to Endoscopic retrograde cholangiopancreatography (ERCP)/endoscopic ultrasound (EUS) training survey: Austria (n = 1), Croatia (n = 1), Czech Republic (n = 1), Denmark (n = 1), Northern Ireland (n = 1), Norway (n = 1), Poland (n = 1), Sweden (n = 1); Hungary (n = 2), Portugal (n = 2), Romania (n = 2), United Kingdom (n = 2); Belgium (n = 3), Italy (n = 3); Germany (n = 4), Spain (n = 4); The Netherlands (n = 5), France (n = 6).
Application process
Twenty‐five centers (out of 37; 67.6%) accept 50% or less than the total number of applications received.
The application process has been conducted through individual request (n = 36; 87.8%), Curriculum Vitae (n = 17; 41.5%), formal interview (n = 16; 39%), recommendation letter (n = 12; 30%), society endoscopy fellowship grant (n = 11; 29.3%), motivation letter (n = 12; 29.3%), payment of an application fee (n = 3; 7.3%), practical evaluation (n = 3; 7.3%), and theoretical evaluation (0%). A request from another Institution (n = 2) was also mentioned as a method for the application process.
Criteria for trainee acceptance in the ERCP/EUS training program were rated according to the PD/experts' opinion (Table 1).
TABLE 1.
PD/Experts opinion on trainees' criteria for acceptance in American Gastrointestinal Endoscopy fellowships.
| Criteria evaluated for trainee acceptance | EI | VI | MI | SI | NI |
|---|---|---|---|---|---|
| Endoscopic skills | 46.3% | 46.3% | 7.4% | 0 | 0 |
| Appreciation in the interview | 22% | 46.3% | 22% | 7.3% | 2.4% |
| Curriculum vitae (CV) | 17.1% | 41.5% | 36.6% | 2.4% | 2.4% |
| Recommendation letter | 12.1% | 22% | 46.3% | 9.8% | 9.8% |
| Motivation letter | 9.8% | 36.5% | 22% | 19.5% | 12.2% |
| Theoretical knowledge | 9.8% | 56.1% | 24.4% | 7.3% | 2.4% |
| EBGH test score | 0 | 4.9% | 22% | 26.8% | 46.3% |
| Membership of endoscopy societies | 4.9% | 12.2% | 17.1% | 36.6% | 29.2% |
| Age | 2.4% | 22% | 34.1% | 26.8% | 14.7% |
| Research experience | 2.4% | 22% | 43.9% | 26.8% | 4.9% |
| Gender | 0 | 0 | 4.9% | 2.4% | 92.7% |
| Honours awarded | 0 | 0 | 34.1% | 34.1% | 31.8% |
| Others (mentioned in free‐text box) |
|
||||
Abbreviations: EI, Extremely important; EBGH, European Board of Gastroenterology and Hepatolog; MI, Moderately important; NI, Not important; SI, Slightly important; VI, Very important.
Among all the criteria considered to be “extremely important” to be evaluated before acceptance in the training, “endoscopic skills” were considered to be the most crucial ones (31 out of 38; 81.6%), followed by “appreciation in the interview” and “CV” (n = 13 each; 34.2%).
Characteristics of ERCP/EUS training departments
Volume of procedures per center
All the departments provide training in ERCP and EUS. Data related to case volume per year across centers can be found in Figure 2.
FIGURE 2.
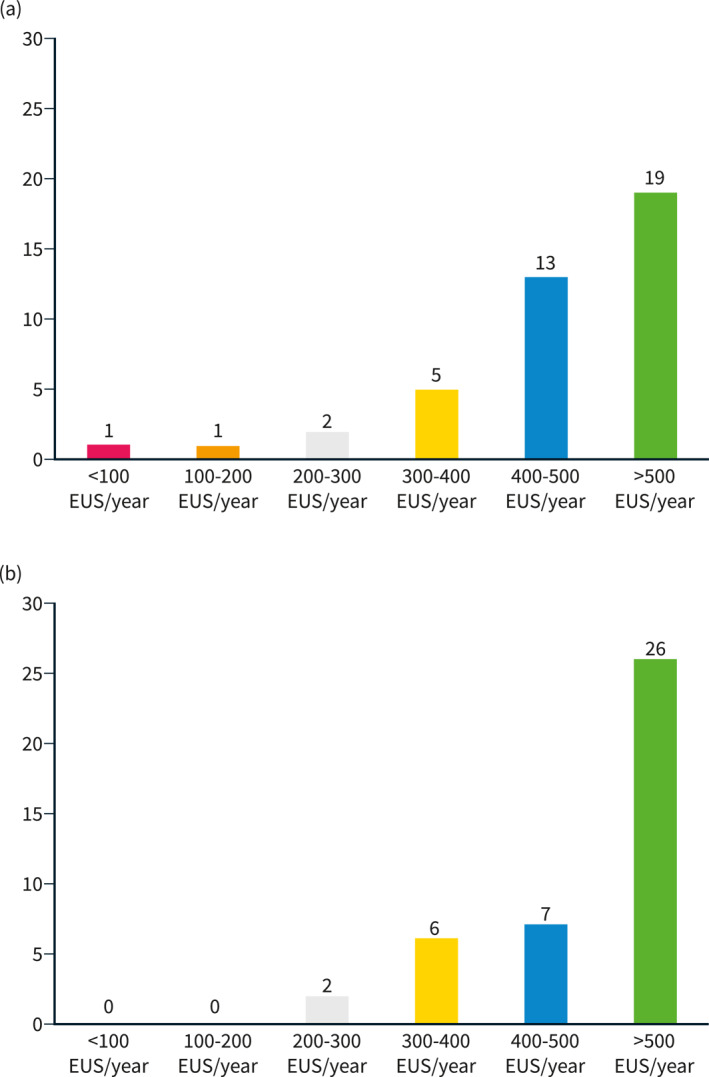
Average number of procedures per year in each center: Endoscopic ultrasound (EUS) (a) and Endoscopic retrograde cholangiopancreatography (ERCP) (b).
Per year, the majority of departments accept 1–2 trainees for EUS (n = 29; 70.7%) and for ERCP (n = 35; 85.4%).
Most of the trainees (n = 25; 83.3%) do combined ERCP/EUS training and expect to do (or did) 100–150 ERCPs/year (43%) and up to 150 EUSs/year (69%); only 3% (n = 1) expect to do more than 300 ERCPs and 250 EUSs (Figure 3).
FIGURE 3.
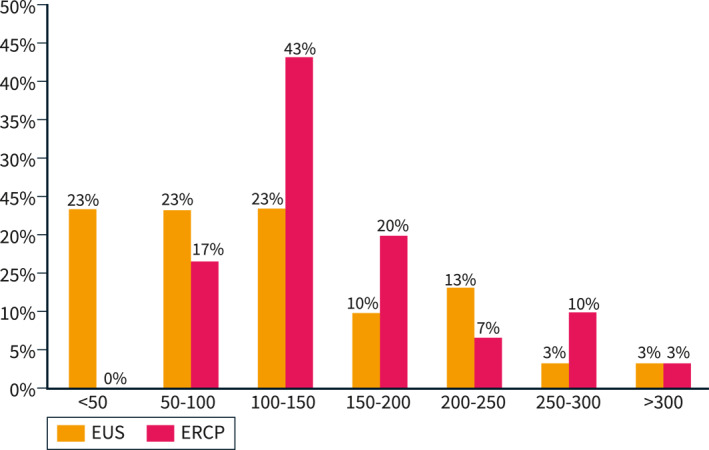
Average number of endoscopic ultrasound (EUS)/ERCP expected to be done by trainees at the end of the training.
Facilities of ERCP/EUS training centers
Training centers provide the following facilities: multidisciplinary hepaticopancreaticobiliary meetings (n = 37; 90.2%), onsite hepaticopancreaticobiliary surgery (n = 37; 90.2%), onsite interventional radiology (n = 39; 95.1%), trainee involvement in research and service improvement initiatives (n = 36; 87.8%), ERCP and EUS simulation training (n = 21; 51.2%).
Characteristics of ERCP/EUS trainers
Twenty‐seven departments (65.9%) designate specific trainers to teach ERCP/EUS. The majority have 2–3 EUS trainers (n = 23; 56.1%) and 1–3 ERCP trainers (n = 25; 60.9%).
There is agreement between trainers and trainees regarding trainer characteristics considered to be “extremely important” to excel in ERCP/EUS (Figure 4).
FIGURE 4.
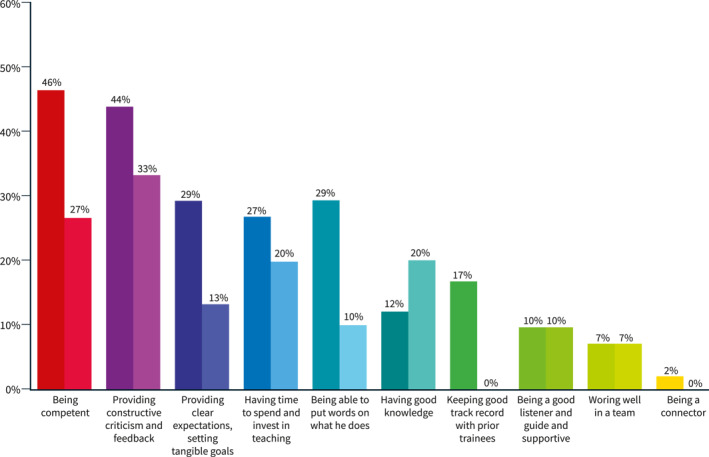
Trainer's characteristics considered to be “extremely important” according to the experts' opinion (left columns) and trainees' opinion (right columns)—exceptions: “keep good track record with prior trainees” and “being a connector” were mentioned only by experts.
Trainers have been performing ERCP/EUS independently for less than three years in 19.5% (n = 8), between 3 and 10 years in 39% (n = 16), and more than 10 years in 41.5% (n = 17). Program Directors/Experts took an average of 18 months (range: 3–60 months) to start performing ERCP/EUS independently and 4 years to perform 1000 ERCPs/EUSs each (range: 2–10 years).
Most of the experts (n = 40; 97.6%) consider training courses on how to teach ERCP/EUS to be beneficial, but the majority (n = 29; 70.7%) do not have access to them.
ERCP/EUS training program structure
Duration of training
Most departments provide at least 12 months of specific ERCP/EUS training (n = 22; 53.7%) and trainees plan to have, on average, an 18‐month fellowship (range: 3–36 months). Twenty‐four months is the longest duration for an ERCP/EUS fellowship (n = 7; 17.1%).
There is wide variation (between 1 and 24 months) between departments regarding the minimum duration for a hands‐on ERCP/EUS fellowship.
Training curriculum
Approximately half of the training programs (n = 22; 53.7%) have a formal ERCP/EUS curriculum, which includes dedicated “hands‐on” training (n = 22; 100%), didactic sessions/courses (n = 14; 63.6%), endoscopy simulator training (n = 6; 27.3%), and participation in clinical research (n = 3; 13.6%).
Simulation‐based training
Although PD/Experts mentioned the availability of endoscopy simulators in 51.2% (n = 22) of departments, only six respondent trainees from 5 departments referred to having access to them during their training.
Different types of simulators are available: mechanical simulators (n = 16; 53.3%); a virtual reality simulator (n = 9; 30%); animal models (ex vivo) (n = 9; 30%); and animal models (in vivo) (n = 3; 10%).
Trainees use simulators at different stages of training: before (n = 10; 33.3%), at the beginning (n = 7; 23.3%), or during the whole hands‐on training period (n = 5; 16.7%).
Competence assessment
Twenty‐seven departments (65.9%) perform a formal assessment during ERCP/EUS training programs, which is done: at set intervals throughout the fellowship (n = 12; 44.4%); randomly throughout the fellowship (n = 7; 25.9%); at the end of the fellowship (n = 8; 38.1%).
The method(s) used to assess whether the trainee achieved endoscopic competence in ERCP/EUS are adequate performance on specific quality metrics, for example, cannulation rate or documentation of EUS landmarks (n = 15; 55.6%); the achievement of certain benchmarks (e.g., procedure volume) (n = 14; 51.9%); verbal attending evaluations (n = 11; 26.8%); adequate performance on a skills assessment tool, for example, The ERCP and EUS Skills Assessment Tool and Direct Observation of Procedural Skills (DOPS) (n = 7; 33.3%), written attending evaluation (n = 3; 14.3%).
Specific parameters of the ERCP/EUS trainee's competence assessment were rated according to PD/expert opinion (Table 2).
TABLE 2.
Criteria evaluated by Program Directors (PD)/Experts for trainee's assessment of Endoscopic retrograde cholangiopancreatography (ERCP)/endoscopic ultrasound (EUS) competence.
| Criteria evaluated for trainee's assessment of competence | EI | VI | MI | SI | NI |
|---|---|---|---|---|---|
| Knowledge of procedure indications and contraindications | 75.6% | 19.5% | 4.9% | 0 | 0 |
| Recognition of pathology | 68.3% | 29.3% | 2.4% | 0 | 0 |
| Appropriate selection of therapeutic manoeuvres/tools | 68.3% | 31.7% | 0 | 0 | 0 |
| Recognition of anatomic landmarks | 61% | 39% | 0 | 0 | 0 |
| Complication rates | 53.7% | 24.3% | 22% | 0 | 0 |
| Correct surveillance/follow‐up recommendations | 43.9% | 43.9% | 12.2% | 0 | 0 |
| Appropriate informed consent discussion | 34.1% | 46.4% | 19.5% | 0 | 0 |
| Independent procedure completion rates | 34.1% | 53.7% | 12.2% | 0 | 0 |
| Procedures volume | 31.7% | 51.3% | 14.6% | 2.4% | 0 |
| Monitoring patient discomfort/experience | 22% | 53.7% | 14.6% | 7.3% | 2.4% |
| Appropriate selection and use of sedation | 17% | 53.7% | 22% | 4.9% | 2.4% |
| Appropriate antibiotic prophylaxis before ERCP/EUS | 19.5% | 46.3% | 29.3% | 4.9% | 0 |
| Reporting | 24.4% | 61% | 14.6% | 0 | 0 |
Abbreviations: EI, Extremely important; MI, Moderately important; NI, Not important; SI, Slightly important; VI, Very important.
Self‐assessment tools
Although only 2 PD/Experts recommend using self‐assessment tools, such as the ERCP Rotterdam Assessment Form (RAF‐E) and Gastrointestinal Endoscopy Self‐Assessment Program Self‐Assessment tool, 11 trainees (36.7%) maintain a dedicated notebook to register completion rates and complications.
Adherence to ESGE recommendations
Based on all gathered data from PD/Experts and trainees, we summarized the department adherence rates to the ESGE Curriculum for ERCP/EUS training (Table 3).
TABLE 3.
Adherence rate to European Society of Gastrointestinal Endoscopy (ESGE) Recommendations on Endoscopic retrograde cholangiopancreatography (ERCP)/endoscopic ultrasound (EUS) Training.
| Number of ESGE recommendation | Number positive answers | Number negative answers | % Adherence to the recommendation |
|---|---|---|---|
| 1. Every endoscopist should have achieved competence in UGI endoscopy before commencing training in ERCP or EUS, that is, having personal experience of at least 300 gastroscopies and meeting the ESGE quality measures for UGI endoscopy | 24 | 6 | 80% |
| 2a. Simulation‐based training represents a positive development to accelerate the trainee's learning curve and should be encouraged. | 21 | 20 | 51.2% |
| 2b. When available, trainees should start training by undertaking structured supervised ERCP/EUS simulator‐based training before commencing hands‐on training in the workplace | 9 | 12 | 42.9% |
| 3. Where it is available, simulation‐based training should evolve in a stepwise approach for training: Virtual reality and mechanical simulators should be used during early training, followed by hands‐on endoscopy training | |||
| 4, 5. Trainees should undertake formal courses to complement ERCP/EUS training. ERCP and EUS trainees should engage with a range of learning resources to supplement formal courses and experiential learning. | 15 | 21 | 41.7% |
| 6. ERCP and EUS training should follow a structured syllabus to guide what is covered in workplace learning, formal training courses, and self‐directed study | 22 | 19 | 53.7% |
| 7. A minimum training period of 12 months of high volume training is likely to be required to obtain minimum proficiency in both ERCP and diagnostic EUS. | 22 | 19 | 53.7% |
| 8. A significant proportion of training should be based in high volume a training centers that are able to offer trainees a sufficient wealth of experience for at least 12 months: | |||
| 8a. ERCP | 39 | 2 | 95.1% |
| 8b. EUS | 37 | 4 | 90.2% |
| 9. An ERCP/EUS training center should ideally be able to provide: | |||
| 9a. Multidisciplinary hepatobiliopancreatic meetings | 37 | 4 | 90.2% |
| 9b. Onsite hepaticopancreaticobiliary surgery | 37 | 4 | 90.2% |
| 9c. Onsite interventional radiology | 39 | 2 | 95.1% |
| 9d. ERCP and EUS simulation | 21 | 20 | 51.2% |
| 9e. Involvement in research, service improvement initiatives | 36 | 5 | 87.8% |
| 10, 11. A trainee's principal trainer should ideally have more than 3 years' experience of independent ERCP and/or EUS practice. | 33 | 8 | 80.5% |
| 13. Formal assessments tools should be used regularly during ERCP and EUS training to track the acquisition of trainees' competence and to support trainee feedback | 12 | 19 | 44.4% |
| 14. Trainees should be encouraged to undertake self‐assessment and keep a contemporaneous logbook of all cases, which includes the degree of trainer support that was needed for each aspect of the procedure | 9 | 12 | 42.9% |
| 15. A trainee should undergo: | |||
| 15a. Formal summative assessment process | 27 | 14 | 65.9% |
| 15b. Prior commencing independent practice in ERCP/EUS | 8 | 33 | 38.1% |
| 20, 28. The number of ERCP/EUS performed may be a surrogate marker of competence, but in isolation is an inexact means to demonstrate competence. Most trainees are likely to need to have performed >300 ERCPs/> 250 diagnostic EUSs to be in a position to demonstrate competency | 1 | 24 | 4% |
Abbreviation: UGI, Upper gastrointestinal.
High‐volume training centers defined as performing >300 EUS/ERCPs per year.
General opinion regarding ERCP/EUS training
The feelings experts and trainees have concerning the current ERCP/EUS training programs provided by their department are shown in Table 4.
TABLE 4.
Experts (Tr) and trainees (Te) opinions regarding Endoscopic retrograde cholangiopancreatography (ERCP)/endoscopic ultrasound (EUS) training programs.
| Opinion about training program | ES | VS | MS | SS | NS | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Tr | Te | Tr | Te | Tr | Te | Tr | Te | Tr | Te | |
| Overall quality of endoscopy training | 7.3% | 40% | 63.4% | 46% | 24.4% | 10% | 4.9% | 4% | 3.3% | 0 |
| Trainee's selection process | 2.4% | 16.7% | 51.2% | 33.3% | 36.6% | 33.3% | 9.8% | 13.4% | 0 | 3.3% |
| Environment/facilities of institutions | 4.9% | 36.7% | 68.3% | 53.3% | 19.5% | 6.7% | 7.3% | 3.3% | 0 | 0 |
| Overall competence assessment | 0 | 26.7% | 70.7% | 43.3% | 22% | 26.7% | 7.3% | 3.3% | 0 | 0 |
Abbreviations: ES, Extremely satisfied; MS, Moderately satisfied; NS, Not satisfied; SS, Slightly satisfied; VS, Very satisfied.
For some trainees, training is hampered by having too many trainees simultaneously, lack of procedure volume, or trainer's inability to let the trainee touch the scope. On the other hand, for some PD/experts, training is hampered by lack of time and a very heavy clinical burden on trainers, with competing clinical and bureaucratic requirements. Additionally, there is a lack of formal support from national societies and no remuneration for training included in the reimbursement systems. There is no actual auditing or performance evaluation.
DISCUSSION
This web‐based survey represents the first international attempt to obtain a comprehensive “portrait” regarding ERCP and EUS training program structures by capturing data from facilities in Europe. This study presents data on a significant part of European countries.
The majority of the centers have an application acceptance rate of 50% or less, which shows a high demand for ERCP/EUS training programs that is currently unmet. In addition, the number of applications per year is increasing in some regions (33.3% of cases). Nonetheless, it should be noted that it is not possible to assess whether applicants rejected at one center were accepted at another one. Thus, the actual rejection rate may be lower than shown here.
As suggested in the literature 12 and confirmed in our results, there is no standardized application process in these training programs, and the application process relies heavily on subjective evaluation of the applicants (e.g., individual application, interview). An application selection method that could be uniformly applied across centers could minimize application selection biases. Endoscopic skills were considered the most important criterion for acceptance into training programs. Thus, it would make sense to include a formal evaluation of these skills in the application process, especially given that there are currently available validated assessment tools for endoscopy performance, such as DOPS. 13 , 14 , 15 It should be noted that good performance in basic endoscopy may not translate to good performance in ERCP/EUS as no relationship between basic handling skills and therapeutic skills has been demonstrated. 16 In addition, it can be questionable to perform this kind of practical evaluation on actual patients due to safety and legal concerns. Endoscopy simulators could play a role in this trainee screening process. 17 The importance of certain non‐technical skills has been recently acknowledged 18 and, while being incorporated in assessment tools such as DOPS, should also be considered during the trainee selection process.
One interesting and somewhat contradictory finding is that, despite theoretical knowledge being considered by a large percentage of experts to be a very important parameter to be evaluated in this process, the EBGH score was only slightly to moderately valued for the majority. Possible explanations could be the lack of knowledge about the EBGH examination or the preference of the PD to conduct their own theoretical evaluations (which may hamper the standardization needed for training).
Another parameter not considered to be important to experts for trainee acceptance was gender, although 70% of the respondent trainees were male. Available data do not allow assumptions regarding trainee gender distribution from the PD responses, but it can be assumed that the large percentage of selected male trainees is not gender related. Although it was not possible to obtain a justification for this result, it is true that women remain underrepresented in Gastroenterology, especially in ERCP/EUS. A recent study 19 confirmed that women represent a minority in this field, corresponding to 14% of current ERCP/EUS fellows and to 13.2% of endoscopy chiefs. Inflexible hours and calls, exposure to fluoroscopy during childbearing age, lack of women endoscopists at conferences/courses, and lack of mentorship for female trainees were perceived barriers to recruitment. To strive toward equity in ERCP/EUS, the number of women being recruited to these fellowships should increase, and structural changes and policies should be implemented to aid the development of women during their career in this field.
Some trainers considered the “perspective of continuing ERCP/EUS after training” as a valuable criteria worth mentioning before acceptance into the fellowship. Given the limited number of training vacancies available, it makes sense to attribute these to those with the highest likelihood of continuing their ERCP/EUS practice. Furthermore, and as already suggested, 16 it would make sense to have national and international institutions determining beforehand the need for additional human resources for centers/countries, which could be better accomplished based on predefined criteria. These criteria could consider several parameters, such as the forecasted number of ERCPs to be performed, 20 case volume per endoscopist, procedure complexity, academic setting, and availability of support from other specialities.
To ensure good training, a good trainer is mandatory. 21 Nonetheless, objectively, clinical and teaching prerequisites for an ideal trainer are not determined. This study determined the best qualities that a trainer should have for interviewing ERCP/EUS PD/experts and trainees. From the PDs’ point of view, the three most important characteristics of a trainer are being competent (46%), providing constructive criticism and feedback (44%), and having clear expectations and tangible goals (32%). Surprisingly, trainees, comparatively, undervalued the trainer's competence and correct setting of expectations, which could be a manifestation of the Dunning‐Kruger effect, 22 a form of cognitive bias where those with low skills overestimate their ability (expecting to attain a good level of performance regardless of the trainer's skills). High variability in teaching methods was mentioned by those having different trainers. Nonetheless, as trainees also agree, having more than one trainer may be beneficial to take advantage of all the possible qualities good mentors have. 21
The threshold for defining a low volume (LV) center in the included centers ranged from 87 to 200 annual ERCPs per center; 23 therefore, we defined a high volume (HV) center as one with more than 200 procedures per year. The majority of the departments surveyed are considered to be very HV. High volume centers are considered to be better fit to handle complex cases as they have better outcomes than LV centers, 23 providing an ideal setting for learning ERCP/EUS, specifically the clinical decision‐making process and the steps to avoid complications. In addition, the HV of procedures available may provide ample opportunities for hands‐on practice of these procedures, parameters considered to be extremely important to both PD/experts and trainees, in line with results from other surveys in other medical specialities. 24 Accordingly, a large percentage of centers will only accept 1–2 trainees per year, which can be assumed to be an effort to provide an adequate case load for the trainees.
Nonetheless, the expected number of procedures performed during training is lower than the recommended minimum for independent practice. This may be due to the complexity of the cases in HV academic centers. For a trainee starting the technique, it may take a couple of months to build up a fair number of relatively simple cases for practice leading to more complex cases. Clinical‐based predictive tools, such as the Trainee Involvement in ERCP Risk Score risk score, could improve ERCP training through an individualized selection of cases for hands‐on training without exposing patients to higher risks (Voiosu et al., unpublished data). In addition, trainees could be exposed to other forms of training, such as simulators, to try to overcome this issue. Another possible takeaway is that formal fellowship programs in HV centers may only be the first step toward independent practice and should probably be complemented with a period of supervised performance of ERCP/EUS in LV centers. Although these centers have lower volumes, cases will typically be less complex, providing a suitable environment for the reinforcement of the theoretical and practical principles acquired during training in HV centers. Of note, PD/experts took an average of 18 months to start performing ERCP/EUS independently. In this regard, Voiosu et al. 25 described the evolution of ERCP practice of an advanced endoscopist at the beginning of this independent practice. It was interesting to confirm that, beyond the training period, it is expected that the learning curve keeps evolving as experience increases.
Although around half of the departments have endoscopy simulators available, they are not part of the regular formal training programs. Possible explanations for this underuse of the simulators might be lack of permanent availability (only during workshops), lack of clinical validation of their role leading to a lower perceived value of this training modality, and the price.
However, around 50% of departments do not have a formal ERCP/EUS curriculum and 65.9% do not perform any kind of formal assessment of trainee performance. Although validated assessment tools are formally used in only 33.3% of those who do, more than half of the training programs measure traditional benchmarks and performance metrics. Such practice is following the shift away from the absolute number of procedures performed as the only measure of competence to a more tailored and milestone‐based training and assessment, 3 since learning curves among individual trainees can be substantially different. 26 , 27 , 28 , 29 , 30 Regarding specific quality metrics, one interesting finding is that to know on “whom” should we perform the procedure (or do not) (“knowledge of procedure indications and contraindications” and “recognition of pathology”) and “how” (“appropriate selection of therapeutic manoeuvres and tools”) are more valued than “independent procedure completion rates” or “complication rates”. Although case volume and opportunities for hands‐on practice are very much appreciated, PD/experts attribute high importance to the correct framework for decision‐making rather than solely technical skills.
Taking into account adherence rates to ESGE guidelines and global PD/expert and trainee opinions regarding ERCP/EUS training programs, some specific aspects can still be improved, such as:
Standardizing the trainee selection process, while considered to be essential, is still performed in a very subjective manner;
Optimizing training structure, assuring that the aims of the fellowship are explicit, and all domains and skills required to achieve competence are communicated to trainees;
Assessing the real impact of simulation training on achieving better clinical performance to optimize its use in regular ERCP/EUS training programs;
Adopting a systematic assessment of competence, using standardized and validated tools, may allow the identification of specific skill deficiencies and individualized strategies to overcome them; and
Granting privileges to trainers, endoscopy departments, and hospitals by institutions or societies, including improving facilities and providing dedicated time and remuneration for those who truly can and are willing to teach.
The main limitation of this study is related to the fact that this is a survey‐based analysis. Although the trainer response rate was relatively high (82%), there is no objective manner to confirm the information provided in the responses. On the other hand, the trainee response rate was rather low, despite the mailing reminders. Reasons for non‐participation can only be speculated (lack of motivation, concern over PD reactions to answers). Nonetheless, trainers and trainees agreed on most of the common questions, which is reassuring regarding the quality of their answers. Self‐reporting bias should also be considered when analysing this kind of survey.
Another limitation is related to the fact that this questionnaire was developed specifically for this study and did not make use of a validated training quality assessment instrument. A pilot evaluation by two experienced GIs was undertaken to minimize issues related to the questionnaire itself. The main issue regarding this point is that adherence to ESGE recommendations was made based on a subjective evaluation of the responses. This was done to avoid duplication of the questions since some were already asked to characterize the training center.
Finally, this study is limited by the number of specific centers included, which may represent a selection bias and underrepresentation of the general European panorama. As there is neither a centralized updated database of training centers for ERCP/EUS in Europe nor a formal list of requisites to recognize a center as a training center, the centers contacted for this study were selected based on recognition by ESGE and/or other national organizations. Future endeavors aimed at the development of centralized registry of ERCP/EUS training centers could serve as a stimulus toward the uniformization of training center recognition criteria and training protocols.
This survey is the first to provide an overview of ERCP/EUS training programs across Europe. Additionally, it showed that there is adherence, to a certain degree, to international guidelines on ERCP/EUS training. However, several gaps, in the standardization of the application process, the number of procedures performed, use of simulators for complementing training, and in the adoption of a formal ERCP/EUS training curriculum and assessment of trainee performance, have also been recognized. Overcoming these shortcomings could serve as a basis for further improvement in ERCP/EUS training.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interest to declare.
Supporting information
Supplementary Information S1
Supplementary Information S2
ACKNOWLEDGMENTS
Aabaken L, Arcidiacono P, Barthet M, Bruno M, Cardenas A, Costamagna G, Deprez P, Dominguez E, Figueiredo P, Garcia J, Giovannini M, Hritz I, Hucl T, Laleman W, László C, Macedo G, Mayerle J, Miranda MP, Neuhaus H, Pereira S, Poley JW, Repici A, Rey JF, Rhami G, Rösch T, Rustemovic N, Saurin JC, Schofl R, Siersema P, Swahn F, Tantau M, Tham T, Vanbiervliet G, Van Hooft J, Vilmann P, Voiosu T, Von Han T, Webster G, Wiechowska A, Wielenga MC, and all the trainees that agreed to participate in the study.
de Campos ST, Arvanitakis M, Devière J. A portrait of Endoscopic retrograde cholangiopancreatography and EUS training programs in Europe: current practices and opportunities for improvement. United European Gastroenterol J. 2023;11(4):350–60. 10.1002/ueg2.12377
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Wani S, Keswani RN, Han S, Aagaard EM, Hall M, Simon V, et al. Competence in endoscopic ultrasound and endoscopic retrograde cholangiopancreatography, from training through independent practice. Gastroenterology. 2018; 155(5): 1483‐94.e7. 10.1053/j.gastro.2018.07.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Bisschops R, Dekker E, East JE, Johnson G, Pimentel‐Nunes P, Sanders DS, et al. European Society of Gastrointestinal Endoscopy (ESGE) curricula development for postgraduate training in advanced endoscopic procedures: rationale and methodology. Endoscopy. 2019;51(10):976–9. 10.1055/a-1000-5603 [DOI] [PubMed] [Google Scholar]
- 3. Wani S, Keswani RN, Petersen B, Edmundowicz SA, Walsh CM, Huang C, et al. Training in EUS and ERCP: standardizing methods to assess competence. Gastrointest Endosc. 2018;87(6):1371–82. 10.1016/j.gie.2018.02.009 [DOI] [PubMed] [Google Scholar]
- 4. Voiosu T, Boskoski I, Voiosu AM, Benguș A, Ladic A, Klarin I, et al. Impact of trainee involvement on the outcome of ERCP procedures: results of a prospective multicenter observational trial. Endoscopy. 2020;52(02):115–22. 10.1055/a-1049-0359 [DOI] [PubMed] [Google Scholar]
- 5. Wani S. Does trainee participation impact critical outcomes in ERCP?: referring to Voiosu T et al. p. 115–122. Endoscopy. 2020;52(02):92–3. 10.1055/a-1084-6525 [DOI] [PubMed] [Google Scholar]
- 6. Gkolfakis P, Arvanitakis M. Trainee involvement in ERCP: safe under close surveillance. Endoscopy. 2020;52(04):318. 10.1055/a-1089-9163 [DOI] [PubMed] [Google Scholar]
- 7. Khan U, Abunassar M, Chatterjee A, James PD. Advanced endoscopy trainee involvement early in EUS training may Be associated with an increased risk of adverse events. J Can Assoc Gastroenterol. 2020;3(2):83–90. 10.1093/jcag/gwy066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rees CJ, Koo S, Anderson J, McAlindon M, Veitch AM, Morris AJ, et al. British society of gastroenterology Endoscopy Quality Improvement Programme (EQIP): overview and progress. Frontline Gastroenterol. 2019;10(2):148–53. 10.1136/flgastro-2018-101073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Domagk D, Oppong K, Aabakken L, Czako L, Gyokeres T, Manes G, et al. Performance measures for ERCP and endoscopic ultrasound: a European society of gastrointestinal endoscopy (ESGE) quality improvement initiative. Endoscopy. 2018;50(11):1116–27. a‐0749‐8767. 10.1055/a-0749-8767 [DOI] [PubMed] [Google Scholar]
- 10. Johnson G, Webster G, Boškoski I, Campos S, Golder SK, Schlag C, et al. Curriculum for ERCP and endoscopic ultrasound training in Europe: European society of gastrointestinal endoscopy (ESGE) position statement. Endoscopy. 2021;53(10):1071–87. 10.1055/a-1537-8999 [DOI] [PubMed] [Google Scholar]
- 11. Cotton PB. Quality endoscopists and quality endoscopy units. J Interv Gastroenterol. 2011;1(2):83–7. 10.4161/jig.1.2.15048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jovanovic I, Mönkemüller K. Quality in endoscopy training—the endoscopic retrograde cholangiopancreatography case. Ann Transl Med. 2018;6(13):264. 10.21037/atm.2018.03.03 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Siau K, Dunckley P, Feeney M, Johnson G. ERCP assessment tool: evidence of validity and competency development during training. Endoscopy. 2019;51(11):1017–26. 10.1055/a-0991-0044 [DOI] [PubMed] [Google Scholar]
- 14. The Joint Advisory Group on Gastrointestinal Endoscopy (JAG) ; Siau K, Crossley J, Johnson G, Feeney M, Hawkes ND, et al. Direct observation of procedural skills (DOPS) assessment in diagnostic gastroscopy: nationwide evidence of validity and competency development during training. Surg Endosc. 2020;34(1):105–14. 10.1007/s00464-019-06737-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Barton JR, Corbett S, van der Vleuten CP. The validity and reliability of a Direct Observation of Procedural Skills assessment tool: assessing colonoscopic skills of senior endoscopists. Gastrointest Endosc. 2012;75(3):591–7. 10.1016/j.gie.2011.09.053 [DOI] [PubMed] [Google Scholar]
- 16. Anderson J, Lockett M. Training in therapeutic endoscopy: meeting present and future challenges. Frontline Gastroenterol. 2019;10(2):135–40. 10.1136/flgastro-2018-101086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Voiosu T, Puscasu C, Orlandini B, Cavlina M, Bekkali N, Eusebi LH, et al. Motion training on a validated mechanical ERCP simulator improves novice endoscopist performance of selective cannulation: a multicenter trial. Endosc Int Open. 2021; 09(02): E145–51. 10.1055/a-1315-1994 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Campos S, Deviere J, Arvanitakis M. Who will excel in advanced endoscopy? A study assessing the criteria and perceptions of experts with regard to the selection of ERCP and EUS trainees. Endoscopy International Open accepted for publication. 10.1055/a-2017-3827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Yu JX, Berzin TM, Enestvedt B, Anderson MA, Popov VB, Thompson CC, et al. Gender disparities in advanced endoscopy fellowship. Endosc Int Open. 2021;09(03):E338–42. 10.1055/a-1311-0899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cotton PB. Are low‐volume ERCPists a problem in the United States? A plea to examine and improve ERCP practice—NOW. Gastrointest Endosc. 2011;74(1):161–6. 10.1016/j.gie.2011.03.1233 [DOI] [PubMed] [Google Scholar]
- 21. Lieberman D. How to select a mentor as a trainee and junior faculty. Gastroenterology. 2016;151(1):17–19. 10.1053/j.gastro.2016.05.014 [DOI] [PubMed] [Google Scholar]
- 22. Dunning D. The Dunning–Kruger effect. In: Advances in experimental social psychology. Elsevier; 2011. p. 247–96. [Google Scholar]
- 23. Keswani RN, Qumseya BJ, O’Dwyer LC, Wani S Association between endoscopist and center endoscopic retrograde cholangiopancreatography volume with procedure success and adverse outcomes: a systematic review and meta‐analysis. Clin Gastroenterol Hepatol. 2017;15(12):1866–75.e3. 10.1016/j.cgh.2017.06.002 [DOI] [PubMed] [Google Scholar]
- 24. Shantha JG, Shulman B, Gonzalez M, Hink EM, Durairaj VD. American society of ophthalmic plastic and reconstructive surgery fellowship survey: fellows selection criteria for training programs. Ophthalmic Plast Reconstr Surg. 2013;29(6):428–30. 10.1097/IOP.0b013e31829a72a1 [DOI] [PubMed] [Google Scholar]
- 25. Voiosu T, Voiosu A, Benguş A, Mateescu B. ERCP practice beyond the training period – bridging the gap between guidelines and real‐life practice: a single operator experience of 679 procedures. Rom J Intern Med. 2019; 57(2): 151–8. 10.2478/rjim-2018-0038 [DOI] [PubMed] [Google Scholar]
- 26. Wani S, Hall M, Wang AY, DiMaio CJ, Muthusamy VR, Keswani RN, et al. Variation in learning curves and competence for ERCP among advanced endoscopy trainees by using cumulative sum analysis. Gastrointest Endosc. 2016;83(4):711–19.e11. 10.1016/j.gie.2015.10.022 [DOI] [PubMed] [Google Scholar]
- 27. Wani S, Hall M, Keswani RN, Aslanian HR, Casey B, Burbridge R, et al. Variation in aptitude of trainees in endoscopic ultrasonography, based on cumulative sum analysis. Clin Gastroenterol Hepatol. 2015;13(7):1318–25.e2. 10.1016/j.cgh.2014.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wani S, Keswani R, Hall M, Han S, Ali MA, Brauer B, et al. A prospective multicenter study evaluating learning curves and competence in endoscopic ultrasound and endoscopic retrograde cholangiopancreatography among advanced endoscopy trainees: the rapid assessment of trainee endoscopy skills study. Clin Gastroenterol Hepatol. 2017;15(11):1758–67.e11. 10.1016/j.cgh.2017.06.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Shahidi N, Ou G, Lam E, Enns R, Telford J. When trainees reach competency in performing endoscopic ultrasound: a systematic review. Endosc Int Open. 2017;05(04):E239–43. 10.1055/s-0043-100507 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wani S, Han S, Simon V, Hall M, Early D, Aagaard E, et al. Setting minimum standards for training in EUS and ERCP: results from a prospective multicenter study evaluating learning curves and competence among advanced endoscopy trainees. Gastrointest Endosc. 2019;89(6):1160–8.e9. 10.1016/j.gie.2019.01.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Information S1
Supplementary Information S2
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


