Abstract
Background:
Ambulatory surgery presents unique challenges regarding adequate pain management and education. Studies have documented issues with transfer of information and patient comfort. Our objective was to explore perioperative nurses’ perspectives of current practices and challenges with pain management and education.
Materials and methods:
We used a qualitative descriptive design and conducted four focus group interviews, with 24 total participants from two perioperative areas of an academic medical center, using a standardized script. Using qualitative analysis software, two investigators reviewed the data and coded major themes and subthemes. The consolidated criteria for reporting qualitative studies guidelines were followed for reporting the data.
Results:
We identified four major themes impacting current perioperative pain management and education practices: communication among the perioperative care team, sources of nurses’ frustrations in the perioperative setting, patient expectations for pain, and nurse-driven pain management and education. Nurses highlighted their work became easier with adequate information transfer and trust from physicians. Frustrations stemmed from surgeon, system, and patient factors. Nurses often use their clinical experience and judgment in managing patients throughout the perioperative period. Furthermore, nurses felt patients have limited pain education and stressed education throughout the surgical care pathway could improve overall care.
Conclusions:
Perioperative pain management, assessment, and education practices are inconsistent, incomplete, and sources of frustrations according to participants. Participant experiences highlight the need for improved and standardized models. Patient pain education should use a multidisciplinary approach, beginning at the point of surgery scheduling and continuing through postoperative follow-up.
Keywords: Qualitative research, Nursing, Perioperative, Pain management, Pain education, Ambulatory surgery
Introduction
Ambulatory (i.e., outpatient or same-day) surgery is increasing in frequency because of increased surgical efficiency, innovative technologies, and numbers of ambulatory surgical centers.1,2 Ambulatory surgery currently comprises >50% of all hospital-based surgical procedures.3 Despite its frequency, outpatient surgery comes with challenges in discharge planning, adequate patient education, pain management, and perioperative communication. Patients may be unprepared for discharge home, especially considering less time with clinicians during recovery and lingering effects of anesthesia, limiting their ability to comprehend discharge information.1,4–7
Managing perioperative pain requires a multidisciplinary approach involving surgeons, anesthesiologists, and nurses. Perioperative nurses play a vital role in assisting with a safe transition from preoperative preparation to surgery to discharge home. They also assist in pain education, use of multimodal pain regimens, and safe discharge teaching.8 Postoperative care, pain assessment, and pain management are topics frequently discussed with patients and their families. Given limited time in an ambulatory surgical setting to adequately counsel patients, communication between surgeons, anesthesiologists, and perioperative nurses is essential. Studies have demonstrated that patient satisfaction and confidence after same-day surgery is tied to communication between providers and adequacy of education delivery.7,9–11 Patients have also expressed being overwhelmed with discharge instructions and noted inadequacies in perioperative education.5,12 Failures in perioperative communication have also been documented in multiple qualitative studies with care providers.10,13,14
Recent clinical practice guidelines addressing post-operative pain management, authored by panels of pain organizations, aim to provide optimal pain management and standardize postoperative instructions.15,16 However, clinicians often have different responsibilities and priorities, which may affect communication and patient care. Differences in training, clinical experience, subspecialization, misunderstanding between providers, or other unknown variables may further contribute to these difficulties in communication.10,17 Furthermore, limited knowledge of nurses’ roles in pain management hinders adequate multidisciplinary collaboration. The Heath and Reid-Finlay conceptual framework for nursing pain management integrates three existing frameworks to denote the importance of nursing knowledge, skill, supportive attitude, and accountability for successful pain management.18 This framework demonstrates “how these four elements are essential to the nursing process…and enable the nurse to provide confident effective care and successfully manage the pain needs of the patient.”18 Nurses also face unique and significant challenges in adequately assessing and managing pain as the first line caregivers for patients recovering from surgery.8 Improved awareness and understanding of the specific problems identified by perioperative nurses may lead to strategies to improve patient pain management and quality of care. Few studies have explored the perspectives of nurses in ambulatory surgical settings concerning perioperative pain management and education practices. To explore this knowledge gap, we conducted focus group (FG) sessions with perioperative nurses.
Materials and methods
Study design and setting
We conducted a qualitative descriptive study to broadly explore nurses’ perspectives surrounding perioperative pain practices specific for patients undergoing same-day surgery. We used an exploratory approach with an iterative content analysis to understand, from the perspective of perioperative nurses, the complexities related to pain management and education in an ambulatory surgical setting. Furthermore, we wanted to better understand factors that may affect current practice and pose barriers for effective management. We received full-review institutional review board approval for this study. The reporting of the data is in alignment with consolidated criteria for reporting qualitative studies guidelines.19 The study occurred at a tertiary, academic medical center located in the Midwest United States. We conducted FGs with nurses from perioperative areas of two operating room (OR) settings: Cambridge Tower (CT) and Bell Tower (BT). The CT ORs are used by otolaryngology-head and neck surgery, neurosurgery, surgical oncology, colorectal surgery, and plastic surgery subspecialists. The BT ORs are the sites for general surgery, vascular surgery, urology, obstetrics and gynecology, orthopedics, and ophthalmology. For both locations, patients routinely have a preanesthesia clinic (PAC) visit before their surgery. For patients being discharged directly from the postanesthesia care unit (PACU), postoperative pain management orders are placed by the surgical teams in both settings. The nursing and anesthesia teams provide additional pain orders in the perioperative period, often after initial discussion with surgeons.
Instruments and data collection
FGs occurred between July 2019 and September 2019. Inclusion criteria included perioperative nurses currently working in the perioperative area of CT or BT. There were no specific exclusion criteria. Recruitment occurred with investigators personally introducing the study to perioperative nurse managers followed by an invitational email. The managers then invited all perioperative nurses to participate. All participants provided written informed consent to participate in an FG. No informants withdrew after informed consent. Participants were assigned a number, and their anonymity in the FG transcripts was maintained during data analysis. Four FGs were conducted (n = 10, 5, 6, and 4). Fifteen perioperative providers were sampled from CT (nurses #1–15), and 10 from BT (nurses #16–25) for a total sample size of 25 participants. However, one participant’s responses and demographics are not reported, as they were identified as a Medical Assistant after completion of the interviews, bringing the total sample to 24 nurses. All participants had preoperative and PACU experience and could provide essential information regarding pain practices for patients being directly discharged from PACU. FGs were conducted in a conference room of the respective hospital tower where the participants worked. Each FG session had at least two to three moderators (authors J.K.S., C.E.F., and A.D.R.), all of whom had clinical research and nursing experience. The moderators also had extensive background experience in pain management practices at the hospital and in facilitating interviews.
Following consent, participants completed a brief demographic survey. Moderators then facilitated semi-structured discussions and maintained the focus on understanding pain management and education practices in the perioperative period. Moderators used a standard script to guide the discussion and asked four broad questions followed by probes if participants did not understand or respond to the initial question. The interview guide was developed using input from investigators and other pain management nurse specialists. The preliminary questions and probing questions were discussed among these specialists and investigators. They were further revised to ensure consistency, validity, and ability to glean the necessary information from interviews and identify areas of improvement of surgical-related pain management and education. The four interview questions were as follows:
In general, what are the best practices currently in place regarding pain medications or management in the perioperative period?
What are the current protocols in place in the perioperative period regarding pain management?
What information do patients currently receive from providers regarding perioperative pain?
What other tools or resources are desired by perioperative care providers?
We audio recorded and visually recorded each session with a digital recorder and a video conference software. Field notes were taken by the same individual (R.N.) at each FG on major themes and nonverbal communication. Following each FG, researchers reviewed each audio recording and transcript to prepare for the next FG session, allowing the research team to pose specific questions to clarify previous topics and identify concepts that could be evaluated further with a new group of participants. FGs were conducted until thematic saturation was obtained or until no new relevant knowledge was being gathered, which was determined following the fourth FG. The mean time of the FGs was 43 min (range 38–46 min).
Data management and analysis
All FGs were initially transcribed verbatim by the second author (C.C.F.) and checked for accuracy against the audio/video, with field notes (R.N.) of nonverbal communication incorporated. These notes helped to gain insight into participants’ emotions and body language, as specific concepts were discussed. Transcripts were not returned to participants for comment or correction, but pain management specialists reviewed them for accuracy and consistency with interviews. The four transcripts were uploaded into Dedoose qualitative analysis software for data management and thematic analysis. A six-step coding system (Figure) similar to that of Braun and Clarke was used to analyze the data.20 All codes and themes were derived inductively from the transcripts. Field notes were also reviewed and considered in developing additional codes during data analysis. Two investigators (R.N. and J.A.V.) reviewed and coded transcripts independently. These codes were compared using overlay capabilities in Dedoose and subsequently discussed to reach consensus or consolidated. Overarching themes were then identified using root codes and child codes and reviewed. Themes were also considered in light of the broader context of the Heath and Reid-Finlay conceptual framework for nursing management of pain (Table).18 Finally, two other investigators (K.J.S. and B.J.P.) further assisted with code checking and consistency, simplification, and subsequent descriptive analysis.
Fig –
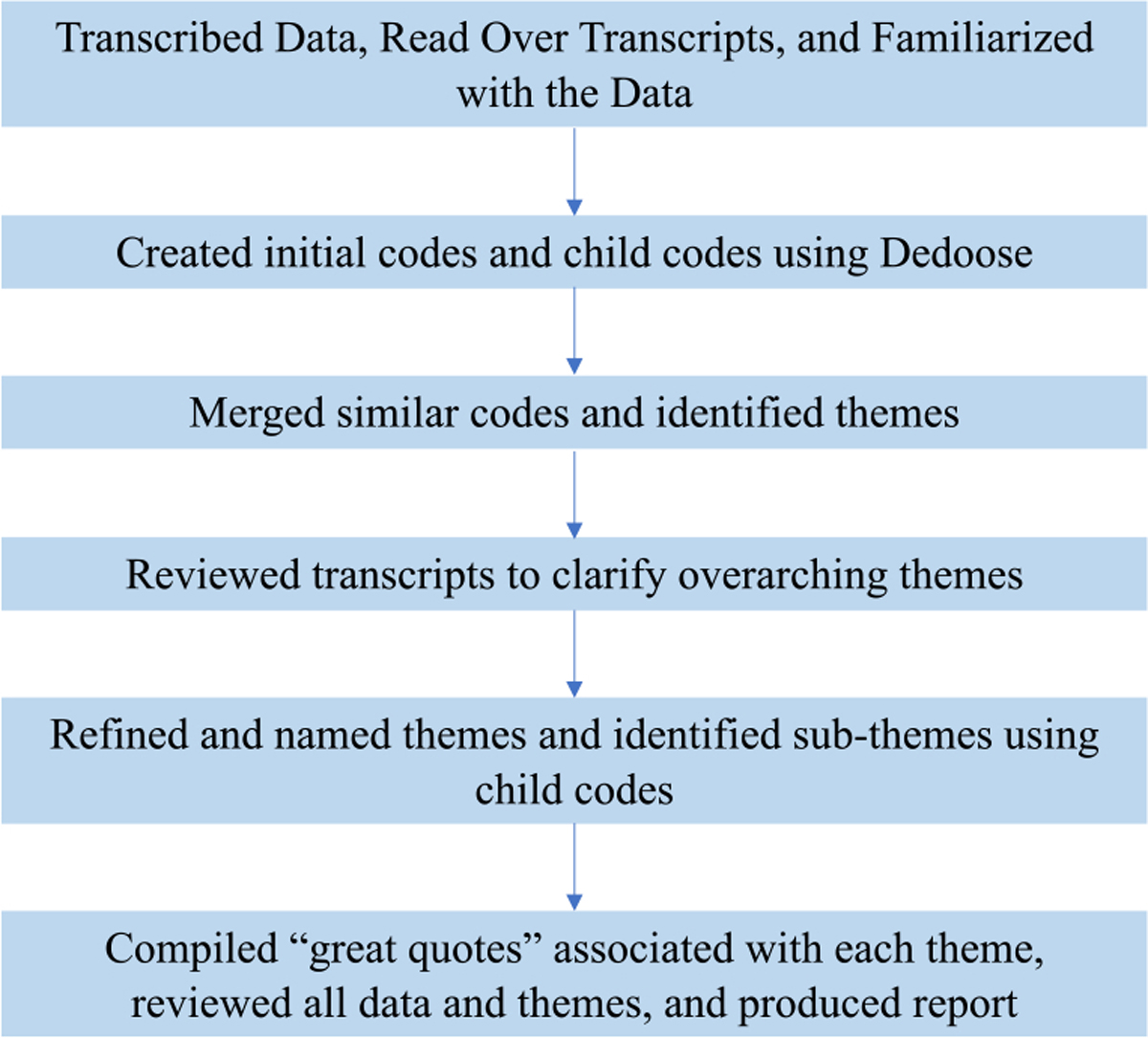
Six-step thematic analysis.
Table.
Themes and subthemes emerging from data analysis that impact current perioperative care practices and pose potential barriers for effective pain management and education.
| Theme | Subtheme | Heath and Reid-Finlay conceptual framework for nursing management of pain concepts |
|---|---|---|
|
| ||
| Communication among the perioperative care team | Helpful communication practices | Knowledge |
| Trust between nursing and anesthesia team | Skill | |
| Sources of nurses’ frustration in the perioperative setting | Surgeons | Attitude/accountability |
| System | Skill/knowledge | |
| Patients | Attitude | |
| Patient expectations for pain | Limited patient education | Attitude |
| Opportunities for improvement | Accountability | |
| Nurse-driven pain management and education | Preoperative experience | Knowledge/skill/attitude |
| Postoperative experience | Knowledge/skill | |
Results
Participants’ ages ranged from 24 to 64 y, with a mean of 34.4 y (SD 13.3), and most were female (n = 23). Most participants were White-non-Hispanic (n = 17), with three African American, two Asian, one White Hispanic, and one other race. Most participants were baccalaureate prepared (n = 23), with one having a diploma in nursing. Total years of nursing experience ranged from 6 mo to 40 y with a mean of 8.7 y (SD 10.0). Experience in the perioperative setting ranged from 6 mo to 16 y, with a mean of 4.8 y (SD 4.6). Analysis of the qualitative data revealed four major themes and various subthemes, highlighted in Table.
Communication among the perioperative care team
In managing pain perioperatively, clear communication and a thorough PAC evaluation, personalized PACU orders, and collaboration between providers helps perioperative nursing personnel better perform their job. One participant stated, “I go with the anesthesia notes. Anesthesia notes will tell you everything about the patient. You don’t even have to hunt from one page to another. Anesthesia does a thorough investigation” (nurse #17). Nurses routinely use the patient medical and medication history tabs in the electronic medical record (EMR) that the anesthesiologist updates at the PAC visit to increase their knowledge about the patient. These become especially useful in assessing and preparing for patients on chronic pain therapy or with complex medical problems. Furthermore, nurses appreciate anesthesiologists and Certified Registered Nurse Anesthetists who provide updates on intraoperative care and what to expect postoperatively. Another participant highlighted, “our PACU orders have gotten more individualized for each patient. People putting in the orders…kind of pick what they think benefits the patient most” (nurse #19). Finally, participants repeatedly stated that while anesthesiologists “rule” the perioperative setting and surgeons “rule” the OR, collaboration among providers remains essential. Anesthesia staff often discuss preoperative blocks and epidurals with surgeons and consult the surgical team if pain is uncontrolled or a different pain management course is needed.
In addition to effective communication between anesthesia and the surgical team, trust between nursing and the anesthesia team was deemed important for patient care. However, this trust must be developed. One participant shared, “We have the best anesthesiologists. They support us, and I do believe they trust us. It’s a matter of getting their trust. If you’re a newbie in recovery (PACU), they will still have to gauge as to how far you can go with your critical thinking in pushing IV pain medications. But once you get their trust, it’s easy to talk to them” (nurse #17).
Once that trust is gained, nurses feel comfortable openly talking about effective pain management practices and using their own nursing judgments in assessing patient pain. A participant specifically stated, “There’s a lot of collaborating between the nurse and the anesthesia person. I feel like they’re always receptive to our suggestions and working together to find the best option for the patient” (nurse #25). Participants in all FGs often noted they work collaboratively with the anesthesia team to determine pain management and discharge time, especially if their skilled assessment indicated a patient was not ready to be discharged home.
Sources of nurses’ frustrations in the perioperative setting
Participants expressed multiple frustrations regarding perioperative pain management, stemming from various surgeon, system, and patient factors (Table). Differences between surgeons’ pain management approaches and the lack of consistency across and within subspecialties were common sources of frustration. Across all FGs, participants agreed that, even among surgeons in the same subspecialty performing similar procedures, “every single surgeon is different” and has their own preferences in perioperative pain management, education, and expectations. Multiple participants agreed with one nurse’s statement:
It’s too hard to keep up, we work with some 1 wk and then we don’t see them for a month and then they come back…and then there’s change…so it’s just kind of very different for specific surgeons (nurse #5).
Differences in surgeon’s preferences make establishing a routine for pain management difficult. Furthermore, nearly all participants indicated that more streamlined communication and surgeon consistency in pain medication usage and discharge instructions would be helpful.
Frustration about surgeons’ pain management education for patients exists as well. Participants in both CT and BT noted preoperative pain education was “very sub-par, very inconsistent,” and unstructured. Several participants stated they became frustrated when surgeons were inaccessible during an operative day, and patients reported pain or had specific questions about their postoperative care the nurse could not answer. Some participants commented they would frequently have to recheck postoperative discharge information listed on the after-visit summary (AVS) with what patients were told by their attending surgeon. In addition, the information often differed from the instructions relayed by resident surgeons. One nurse stated, “there’s multiple times where I’ve been reading [the AVS] and the surgeon comes in, ‘oh don’t do that, do this!’” (nurse #8). The nurse then must re-explain post-operative pain management, leading to patient confusion.
Participants’ frustrations in the perioperative period also stemmed from inconsistencies and inadequacy in system-wide pain assessment tools for patients. Current practice includes the use of the traditional 0–10 numerical pain scale, with pain medication administration determined by a patient’s self-reported pain rating on this scale. However, multiple participants consistently stated this scale was often inadequate in gauging a patient’s true pain. Nurses often rely on their own nursing judgment, knowledge, skill, and experience when determining a patient’s actual pain and often administer pain medication based on their judgment. For example, one patient may claim “their pain’s a 10 out of 10, but then they go right back to sleep” (nurse #25), whereas another may be “screaming for a three or four” pain level (nurse #18). Participants indicated it was challenging to properly assess their patients’ pain postoperative because of these types of problems with the 0–10 scale. They also use other pain scales, such as the Wong-Baker FACES, FLACC (for children), or verbal representations of pain because many patients have difficulty quantifying their pain appropriately using the 0–10 scale.
Another system challenge that frustrated nurses and limited adequate pain education were having sufficient time for education. One participant stated, “I don’t really talk particularly about pain. We’re so busy [reviewing] the anesthesia orders, consent, the pre-op history. Especially if it’s [the first surgery of the day]” (nurse #18). Others echoed this sentiment across the FGs, claiming time was a major factor in providing adequate preoperative pain education, whereas sedative medication that increased the chance of patients forgetting what was discussed prevented effective postoperative education. Interestingly, a few nurses who had experience working in both CT and BT stated they had more time in the former setting, possibly because of its larger space, less congestion, and lower operative volume.
Patient factors and behaviors can also lead to frustration. Although much of this frustration is because of the difficulty of assessing pain as previously described, other factors were also noted that made pain management a challenge. For example, one participant explained how anxiety and pain often coexist and build on each other postoperatively and how that may affect attitude and appropriate management:
I feel like people who are just really anxious, they’ll be like, ‘Oh, I’m 10 out of 10 pain.’ But then they’re sleeping, and their vital signs are baseline. And then if they hear someone, then they start waking up and they’re screaming again. So, I don’t want to, like, not believe them, but then their vitals suggest that they are managed. You know like, they’re not really in pain but they just kind of want that attention because they’re kind of scared, they’re anxious (nurse #16).
Participants from both CT and BT also stated they need to identify patients who are recurrent surgical patients and treat their pain differently than they would a first-time surgical patient or an older patient. However, one participant also claimed:
Sometimes [patients] influence the way you give medication, so I don’t know how to overcome that because he/she’s screaming at you, and you can’t do anything. So, we probably push more than what you want to push. It’s really hard (nurse #18).
Others stated that patients hear about specific drugs outside the hospital, such as fentanyl or morphine, and expect to have control over specific medications they are provided. This makes it challenging for nurses to follow various surgeons’ PACU orders and frustrating for them in caring for these patients.
Participants also frequently commented that patients do not feel that acetaminophen or other over-the-counter medications will adequately manage their postoperative pain and automatically expect additional prescribed pain medication. For opioid pain medications, numerous participants commented that patients are not appropriately educated on the risks and benefits, use of these medications only as needed, or proper disposal of unneeded pills. Participants frustratingly noted that nurses are often having to provide that information or redirecting patients to contact their surgical team. However, discussions of addiction were of concern to some participants. They were hesitant to broach this topic, and very few openly addressed it if raised by patients.
Patient expectations for pain
Participants consistently commented on how patients have limited education about postoperative pain and noted multiple opportunities for improvement. Participants in all FGs repeatedly stated patients commonly expect to have “zero pain” or “no discomfort” after surgery. When patients proclaim they didn’t “expect the surgery to be so painful,” nurses have to explain how “it’s still an incision” (nurse #20); or “your entire stomach has been opened, yes, you’re going to have pain” (nurse #22); and it is simply not realistic to expect no pain. Participants indicated that they feel surgeons rarely provide adequate education for the surgery-specific pain or how pain medication can help. One participant stated, with agreement from others, “the only addressing of pain control from a physician standpoint in my experience is anesthesia” (nurse #3). Without adequate information before surgery and inconsistent information after surgery, patients are left without clear direction on how to manage pain.
Participants in all FGs offered multiple suggestions to improve patient preparation for postsurgical pain. Specifically, participants indicated a need for patients to receive more overall education, beginning in the preoperative clinic visit. One colorectal surgeon who previously provided comprehensive preoperative education on patient expectations for pain was notable for this beneficial practice. One nurse stated this surgeon’s patients “get a blue apron type packet…and it talks about every situation they’re going to go through the day of [surgery], talking about the potential ostomy, the potential pain management, and straight instructions clarifying…all different kinds of instructions” (nurse #2). Others remarked how the PAC visit, “where they have less tension, less time constraints,” could include patient education, especially considering that it also often occurs closer to the surgical date. Participants from CT indicated they appreciate resident and attending surgeons who follow up on patients postoperatively and answer questions about their pain. Improved postoperative pain education and awareness of pain management for family members are other opportunities to improve overall expectations and education of patients.
Nurse-driven pain management and education
Both preoperative and postoperative experiences were discussed as areas where nurses affect pain management and education. Nurses in both settings stated they constantly use their skills and knowledge to reassure patients preoperatively about expected pain and pain management. To improve patient education and expectations for pain, nurses often explain to patients their process for assessing pain and addressing pain control in the preoperative setting when patients are more awake and aware. By explaining the 0–10 scale, “why we are giving the medication and what the medication is” (nurse #14), and their own experiences with different patients before surgery, participants indicated it was easier to prepare patients for their postoperative experience. All participants agreed that perioperative pain education is “very nurse-driven,” especially given the variability, inconsistencies, and frustrations mentioned previously, and they have modified their practices to educate patients during various steps of the process.
In preparing for discharge, similar to preoperative education, most participants from both settings stated they commonly educate and take the initiative postoperatively by explaining to patients the medications prescribed, how to take the medication, what to expect for pain, and when to contact the care team. All participants stated they constantly document medication timing and highlight and note important information on the AVS to better prepare patients for discharge. In addition, participants indicated they commonly rely on their own clinical judgments and experiences in helping patients. One nurse asserted:
I use a lot of nursing adjustments still too. Which, I feel like that comes with time and, especially with new orientees, it takes a while to get comfortable with being confident in what you’re giving and how much you’re giving. Because sometimes an order will say to give 50 and I’m like, I don’t think [the patient] can handle 50.A lot of judgment calls (nurse #25).
Although these situations can cause angst and frustration, participants noted their judgment and experience empower them to check with surgeons and possibly have orders modified. Finally, all participants indicated they used various nonpharmacologic interventions in managing their patient’s pain, including “distraction,” “warm blankets and pillows,” “music therapy,” “ice packs,” “positioning changes,” and social support. However, surgeon preferences can also affect which nonpharmacologic therapies can be implemented, resulting in nurses having to constantly adapt their recommendations.
Discussion
The results of this study highlight four central themes that impact current perioperative care practices and pose barriers to effective perioperative pain management and education during ambulatory surgery. These themes are reflected in the four concepts of Heath and Reid-Finlay’s conceptual framework…knowledge, skill, attitude, and accountability—of nursing management of pain but also offer new areas of study and opportunities for improvement. Nurses appreciate clear and cohesive communication in caring for patients after surgery. However, there are many causes of frustration for nurses that may hinder effective care, such as variations in surgeon practice, system barriers, and patient behaviors. Nurses play a vital role in ensuring a smooth transition to discharge and feel the ability to use their own judgment and practices to improve patient education and management is important. Furthermore, there was consensus that preoperative pain management education is a desired area of improvement to align patient expectations for pain with their actual experience as many patients are unaware they will experience postoperative pain.
Communication among perioperative care providers is vital to providing safe and effective care for patients. The results presented here reinforce this, further suggesting that nurses in this study believed current communication practices are effective between surgeons and perioperative anesthesia and nursing teams. Successful transition of care has been shown to be most effective when there is structured preparation and information transfer.7 Participants in this study appreciated that anesthesiologists conduct a thorough evaluation before the surgical day and provide clear details about medications given during surgery, patient vital signs, and any complications after surgery that help in caring for the patient in PACU. However, other studies present contradictory findings in the perioperative setting, claiming failures in communication often stem from these same handovers, unclear protocols, incomplete or disorganized details, or lack of verbal relay of information.10,13,14,17 These communication breakdowns may affect patient safety and healing.13,14,21 Although participants in this study indicated the EMR, clear physician–surgeon notes, and trust between perioperative nurses and anesthesia allows for safe and effective care, poor transfer of information through the EMR has been documented.22–24 However, nurses in our study work primarily in the ambulatory surgery setting, where the more episodic and less nuanced aspects may make it easier to rely more on the EMR compared with inpatient surgery.
Although participants claimed current communication practices were helpful, much of their frustrations originate from surgeon inconsistencies in perioperative care. This has been a finding in previous studies.10,17 Participants in our study stressed a need to improve standardization and consistent communication along the care continuum, and a more systemic approach across the surgical pathway may be needed to do this and improve quality of care.14 However, variability in patient conditions, surgeon availability, team composition, and environment can pose a significant challenge for creating standardized models for handovers and postoperative care.7 Increased awareness of the nursing role in perioperative care by surgeons through discussion with nurses at surgery didactic sessions and input from perioperative nursing staff in creation of pain protocols may help to overcome these barriers and develop more appropriate clinical practice guidelines for perioperative care.
Participant views regarding patient education was a salient topic of our study. Perspectives were twofold: frustration with inconsistency among surgical instructions and opinions of inadequate preoperative preparation regarding pain. With respect to the former, we discovered attending surgeons and their residents may provide conflicting instructions, and nurses often need to clarify these messages. This is significant as variability in education and management can theoretically pose risks for patient care if patients have unclear guidance on wound care or pain management. Information inconsistency and disconnect between verbal and written information have been shown to contribute to patient insecurity and discomfort with discharge after their operations.25,26 Conversely, clarity and consistency of information can empower patients to have a more active role in their recovery.25
With respect to preoperative pain preparation, participants in our study found preoperative counseling to be inadequate. Patients were poorly educated about postoperative pain and often had unrealistic expectations. For example, nurses stated that patients frequently expected no postoperative pain or believed that medications would completely remove all pain. Participants in this study strongly believed that providing more education preoperatively would be ideal, and this information should be repeated and reinforced after surgery.26 Nurses appreciated surgeons who provided pain-related educational handouts to patients before surgery that covered expectations and felt those patients were better prepared. These initiatives reflect enhanced recovery after surgery principles. Enhanced recovery after surgery focuses on improving the patient experience, beginning with helpful patient education provided 1 wk before the surgery date.26 However, policies to ensure standardized messaging and approval of handouts hindered the use of surgeon-specific developed handouts at our institution and may limit similar initiatives elsewhere. Creation of these handouts and recommendations for patient guidance using nursing input may help counter those institutional barriers.
Participants in our study further stressed providing pain education postoperatively was not appropriate for several reasons, including patient sedation, limited time before discharge, inconsistencies between attending and resident surgeon instructions, and patient preoccupation with surgery success. These sentiments are supported by the existing literature on perioperative education. For example, patients find it challenging to recall information given to them after surgery.22,26 Similarly, limited perioperative time, quick turnover and discharge, and sedative effects of anesthesia have been shown to hinder adequate postoperative patient education and transfer of vital information regarding post-procedural care and pain.1,5,7 A previous recommendation stresses verbal information, supplemented with written details be provided at least 40 min after the surgical procedure.4 In addition to this, participants in our FGs suggested strategies such as earlier postoperative follow-up of patients by surgeons and utilization of the PAC and surgical scheduling visits to improve patient education.
Frustrations with assessment practices and patient behaviors—a major theme voiced by participants—are well supported in the literature. Although the 0–10 pain scale is a common tool in nursing practice, nurses rely on more than this arbitrary number in assessing patients’ pain. This is important as patients may misunderstand the 0–10 scale, and patient and clinician interpretation of the meaning of a numeric rating on the scale can also substantially differ.27 Nurses in our study stated they rely on prior experiences to create their own methods of assessing and subsequently treating pain. Participants believed the 0–10 scale was unreliable and limited in assessing patient pain and was often not compatible with patient behavior, something voiced in other studies.28,29 Jang et al. has explored how nurses use various ways of reasoning in assessing and managing pain, concluding nurses use various experiences, intuition, and clinical knowledge in caring for patients postoperatively.28 However, nurses’ subjectivity in pain assessment may introduce a bias in appropriately gauging and treating patients’ pain. A better understanding of the multifaceted application of nursing experience and judgments in assessing pain would be more useful than continued reliance on the numerical scale alone.28,30
Discussion of addiction appears to be limited in the perioperative setting, according to our FG participants, and may be better suited for incorporation into preoperative education. Many participants shared patients’ preconceived notions about opioid-based medications led to hesitancy in asking for pain medication. Brown et al. explored this in elderly patients who indicated opioid medications should be reserved for severe pain only with concerns of addiction, preventing them from asking for opioids.31 Furthermore, participants were often hesitant themselves to discuss possible addictive effects of opioids, indicating that ideally, this should be discussed with patients before the day of surgery. Patients need to be educated about all topics surrounding pain, and they have a curiosity and desire for knowledge that would help them prepare for discharge and recovery.5,32 This information helps alleviate their concerns regarding pain, postoperative care, and ability to resume daily functions.5
Participants also identified various actions nurses take to manage patients’ pain and provide education. Discharge planning has been shown to be effective when patients receive information about pain and symptom management, recovery and acclimation to daily life, and how to obtain more information.1 Nurses in our study do their best in easing the transition for patients by documenting timing of medications given, providing nonpharmacologic therapy, and using their experiences with other patients to explain what to expect for pain following surgery. In addition, nurses sometimes involve family members and caregivers in postoperative pain management and education, which has been shown to facilitate a safe discharge.33
This study is not without limitations. Participants were all from a single large academic medical center; hence, external validity is limited. However, the patient population is diverse and undergo various types of surgery. In addition, participants were diverse in age, race, and years of experience in a practice setting that is variable in terms of environment, space, and operations. We believe this mitigated this limitation. There was also variability in FG size (ranging from 4 to 10 participants) but not an equal variability in length of time to complete the FGs. We may have missed important comments in larger FGs, and certain participants may be overrepresented from the smaller FGs. In addition, participants did not review transcripts after the FGs; although this may limit the credibility of our study, review was not feasible because of the number of participants and logistical barriers, and we ensured checks for accuracy and consistency by having pain management specialists review the transcripts and using multiple coders. Participants in this study were a convenience sample, so the perspectives shared were only from those already willing to discuss their experience. As we did not include all employed perioperative nurses, we may have missed important opinions and experiences.
Further recommendations
As noted in this study, optimal perioperative care and pain management is dependent on a high-functioning multidisciplinary team. Surgeons, anesthesiologists, and nurses all play a crucial role in perioperative recovery. As numerous FG participants stated, patient education and preparation for discharge should begin preoperatively with the surgical team. In hospital settings similar to the one sampled in this study, continued education can occur when the patient visits the anesthesia team preoperatively for assessment, followed with complementary education by nurses in the perioperative setting that builds on prior discussions and allows nurses to contribute their knowledge and skills. Pain management, expectations, and assessment should be discussed and individualized to each patient at each of these time points. Improved awareness of nursing’s role in perioperative pain management and education by surgeons can improve patient care and allow for this streamlining. It is also important to gauge patient anxiety and experience surrounding pain to improve management. Furthermore, standardized subspecialty-specific pain protocols are desired by perioperative nurses to limit frustration and confusion among patients and care providers. Further research should focus on developing and examining these interventions to improve perioperative pain management education and care.
Conclusions
Current perioperative pain management and education practices are felt to be inconsistent and incomplete by perioperative nurses in this study. Although participants indicated communication between them and anesthesia providers is currently beneficial, variability in surgeon practices spurs frustration and may affect current care quality. Because of limitations in existing pain assessment methodologies, nurses rely on their experience and judgment in pain assessment and management. Many patients are undereducated and unprepared for pain after surgery, revealing an important gap and target for future improvements such as multidisciplinary standardization of pain assessment, education, and management to improve patient expectations and safety following surgery.
Acknowledgment
The authors would like to thank Sally Barhydt and Amanda Themmesch for reviewing and proofreading this article and for their helpful comments.
Footnotes
Disclosure
The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
REFERENCES
- 1.Gilmartin J Contemporary day surgery: patients’ experience of discharge and recovery. J Clin Nurs. 2007;16:1109–1117. [DOI] [PubMed] [Google Scholar]
- 2.Badlani N Ambulatory surgery center ownership models. J Spine Surg. 2019;5:S195–S203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Steiner CA, Karaca Z, Moore BJ, Imshaug MC, Pickens G. Surgeries in hospital-based ambulatory surgery and hospital inpatient settings. 2014. Available at: www.Hcup-Us.Ahrq.gov/reports/statbriefs/sb223-Ambulatory-Inpatient-Surgeries-2014.Pdf. Accessed July 11, 2020. [PubMed]
- 4.Blandford CM, Gupta BC, Montgomery J, Stocker ME. Ability of patients to retain and recall new information in the post-anaesthetic recovery period: a prospective clinical study in day surgery. Anaesthesia. 2011;66:1088–1092. [DOI] [PubMed] [Google Scholar]
- 5.Berg K, Arestedt K, Kjellgren K. Postoperative recovery from the perspective of day surgery patients: a phenomenographic study. Int J Nurs Stud. 2013;50:1630–1638. [DOI] [PubMed] [Google Scholar]
- 6.Joshi GP, Kehlet H, PROSPECT Working Group. Guidelines for perioperative pain management: need for re-evaluation. Br J Anaesth. 2017;119:703–706. [DOI] [PubMed] [Google Scholar]
- 7.Reine E, Rustøen T, Ræder J, Aase K. Postoperative patient handovers—variability in perceptions of quality: a qualitative focus group study. J Clin Nurs. 2019;28:663–676. [DOI] [PubMed] [Google Scholar]
- 8.Hayes K, Gordon DB. Delivering quality pain management: the challenge for nurses. AORN J. 2015;101:328–334. [DOI] [PubMed] [Google Scholar]
- 9.Trinh LN, Fortier MA, Kain ZN. Primer on adult patient satisfaction in perioperative settings. Perioper Med (Lond). 2019;8:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Braaf S, Riley R, Manias E. Failures in communication through documents and documentation across the perioperative pathway. J Clin Nurs. 2015;24:1874–1884. [DOI] [PubMed] [Google Scholar]
- 11.Gunningberg L, Idvall E. The quality of postoperative pain management from the perspectives of patients, nurses and patient records. J Nurs Manag. 2007;15:756–766. [DOI] [PubMed] [Google Scholar]
- 12.Dowzicky PM, Shah AA, Barg FK, Eriksen WT, McHugh MD, Kelz RR. An assessment of patient, caregiver, and clinician perspectives on the post-discharge phase of care. Ann Surg. 2019. [DOI] [PubMed] [Google Scholar]
- 13.Milby A, Böhmer A, Gerbershagen MU, Joppich R, Wappler F. Quality of postoperative patient handover in the post-anaesthesia care unit: a prospective analysis. Acta Anaesthesiol Scand. 2014;58:192–197. [DOI] [PubMed] [Google Scholar]
- 14.Nagpal K, Arora S, Vats A, et al. Failures in communication and information transfer across the surgical care pathway: interview study. BMJ Qual Saf. 2012;21:843–849. [DOI] [PubMed] [Google Scholar]
- 15.Joshi GP, Van de Velde M, Kehlet H, et al. Development of evidence-based recommendations for procedure specific pain management: PROSPECT methodology. Anaesthesia. 2019;74:1298–1304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the American pain society, the American society of regional Anesthesia and Pain Medicine, and the American society of Anesthesiologists’ committee on regional Anesthesia, executive committee, and Administrative council. J Pain. 2016;17:131–157. [DOI] [PubMed] [Google Scholar]
- 17.Nagpal K, Vats A, Ahmed K, Vincent C, Moorthy K. An evaluation of information transfer through the continuum of surgical care: a feasibility study. Ann Surg. 2010;252:402–407. [DOI] [PubMed] [Google Scholar]
- 18.Heath DL, Reid-Finlay MM. A conceptual framework for nursing management of pain. Contemp Nurse. 1998;7:68–71. [DOI] [PubMed] [Google Scholar]
- 19.Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19:349–357. [DOI] [PubMed] [Google Scholar]
- 20.Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101. [Google Scholar]
- 21.Lyon A, Solomon MJ, Harrison JD. A qualitative study assessing the barriers to implementation of enhanced recovery after surgery. World J Surg. 2014;38:1374–1380. [DOI] [PubMed] [Google Scholar]
- 22.Kaptain K, Ulsøe M, Dreyer P. Surgical perioperative pathways—patient experiences of unmet needs show that a person-centred approach is needed. J Clin Nurs. 2019;28:2214–2224. [DOI] [PubMed] [Google Scholar]
- 23.Sockolow PS, Bowles KH, Adelsberger MC, Chittams JL, Liao C. Challenges and facilitators to adoption of a point-of-care electronic health record in home care. Home Health Care Serv Q. 2014;33:14–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Staggers N, Clark L, Blaz JW, Kapsandoy S. Why patient summaries in electronic health records do not provide the cognitive support necessary for nurses’ handoffs on medical and surgical units: insights from interviews and observations. Health Inform J. 2011;17:209–223. [DOI] [PubMed] [Google Scholar]
- 25.Sibbern T, Bull Sellevold V, Steindal SA, Dale C, Watt-Watson J, Dihle A. Patients’ experiences of enhanced recovery after surgery: a systematic review of qualitative studies. J Clin Nurs. 2017;26:1172–1188. [DOI] [PubMed] [Google Scholar]
- 26.Aasa A, Hovbäck M, Berterö CM. The importance of preoperative information for patient participation in colorectal surgery care. J Clin Nurs. 2013;22:1604–1612. [DOI] [PubMed] [Google Scholar]
- 27.van Dijk JFM, van Wijck AJM, Kappen TH, Peelen LM, Kalkman CJ, Schuurmans MJ. Postoperative pain assessment based on numeric ratings is not the same for patients and professionals: a cross-sectional study. Int J Nurs Stud. 2012;49:65–71. [DOI] [PubMed] [Google Scholar]
- 28.Jang JH, Park WH, Kim H-I, Chang SO. Ways of reasoning used by nurses in postoperative pain assessment. Pain Manag Nurs. 2019. [DOI] [PubMed] [Google Scholar]
- 29.Chatchumni M, Namvongprom A, Eriksson H, Mazaheri M. Thai nurses’ experiences of post-operative pain assessment and its’ influence on pain management decisions. BMC Nurs. 2016;15:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Zisk-Rony RY, Lev J, Haviv H. Nurses’ report of in-hospital pediatric pain assessment: examining challenges and perspectives. Pain Manag Nurs. 2015;16:112–120. [DOI] [PubMed] [Google Scholar]
- 31.Brown C, Constance K, Bédard D, Purden M. Colorectal surgery patients’ pain status, activities, satisfaction, and beliefs about pain and pain management. Pain Manag Nurs. 2013;14:184–192. [DOI] [PubMed] [Google Scholar]
- 32.Andersson V, Otterstrom-Rydberg E, Karlsson A-K. The importance of written and verbal information on pain treatment for patients undergoing surgical interventions. Pain Manag Nurs. 2015;16:634–641. [DOI] [PubMed] [Google Scholar]
- 33.Shoqirat N, Mahasneh D, Singh C, Al Hadid L. Do surgical patients’ characteristics and behaviours affect nurses’ pain management decisions? A qualitative inquiry. Int J Nurs Pract. 2019;25:e12779. [DOI] [PubMed] [Google Scholar]


