Abstract
The early months of the COVID-19 pandemic saw a decline in psychotropic medication use; however, little is known about how this trend evolved as the pandemic progressed and how it varied across different payers in the United States. Using a national multi-payer pharmacy claims database and adopting a quasi-experimental research design, this study examines trends in psychotropic medication prescriptions dispensed from July 2018 - June 2022. The study finds that the number of patients with dispensed psychotropic medications and the number of psychotropic medications dispensed declined during the early months of the pandemic but experienced a statistically significant growth in later periods compared to the pre-pandemic rate. Average days supply of psychotropic medications dispensed increased significantly throughout the pandemic. Commercial insurance remained the primary payer for psychotropic medication during the pandemic, but there was a significant increase in the number of prescription fills covered under Medicaid. This implies that public insurance programs played an increasing role in financing psychotropic medication use during the COVID-19 pandemic.
Keywords: Psychotropic medication, Mental health, COVID-19
1. Introduction
Since the start of the COVID-19 pandemic, there have been concerns about its potential adverse impacts on the incidence of mental health conditions, the experiences of people with mental health conditions, and access to treatment (Holmes et al., 2020). Individuals with mental health conditions may be disproportionately affected by COVID-19, both directly and indirectly. For example, individuals with serious mental illness have a higher prevalence of health conditions associated with severe COVID-19 than those without serious mental illness and may be at increased risk for contracting COVID-19 (Novak et al., 2021). Social isolation and economic stress during the pandemic may have led to or exacerbated anxiety and depression, and individuals with mental health conditions likely faced additional barriers to accessing needed treatment services and other supports (Druss 2020; Holmes et al., 2020).
Studies conducted early in the pandemic found significant proportions of patients diagnosed with COVID-19 subsequently reported symptoms of mental illness, including post-traumatic stress disorder (PTSD), depression, and anxiety (Bo et al., 2020; Mazza et al., 2020). Research has also found an increased incidence of psychiatric disorders following COVID-19 diagnosis among individuals with no prior psychiatric history (Taquet et al., 2021). Together, these factors have raised concerns about an increasing burden of mental health conditions since the COVID-19 pandemic.
At the same time as the burden of mental health conditions has been increasing, the treatment delivery and health insurance coverage landscapes have both changed substantially. The COVID-19 pandemic resulted in a significant shift in the delivery of mental health services. The Coronavirus Aid, Relief, and Economic Security (CARES) Act passed in March 2020 included provisions that expanded telehealth coverage for Medicare and Medicaid beneficiaries, including reimbursement at rates equivalent to those for in-person services. The early months of the pandemic saw a significant increase in telehealth services (Demeke et al., 2021), especially for mental health services, where telehealth accounted for approximately 48% of all outpatient services delivered (Zhu et al., 2022). What has remained less clear is how psychotropic medication (such as antidepressants, antipsychotics, mood stabilizers, stimulants, etc.) prescribing may have changed as part of this shift in mental health care delivery .
Research covering the early months of the pandemic found a decline in the number of patients that were prescribed psychotropic medication as well as a decline in the number of psychotropic medications prescribed (Nason et al., 2021; Hirschtritt et al., 2021; Leong et al., 2022), maybe because of initial difficulties in arranging access to telehealth providers. Nason et al. (2021) found a 2.5–7.5 percent decline in psychotropic medications dispensed during the first five months of the pandemic using a national pharmacy claims database. Similarly, Hirschtritt et al. (2021) found a decline in psychotropic prescription fills (<2%) using pharmacy claims data from a Northern California private healthcare system. Leong et al. (2022) found an 8% decline in number of patients prescribed psychotropic medication during April - December 2020 using administrative data from the Manitoba province in Canada. However, it is not known if this declining trend continued in the later period of the pandemic. The literature has documented an increase in mental health conditions both during the early and the latter period of the pandemic (Holmes et al., 2020) – understanding trends in psychotropic medication fills in the later period of the pandemic might indicate whether treatment receipt was able to keep pace with the need for mental health services. It is also not known if the days supply of psychotropic medication changed during the pandemic (e.g. it is possible that days supply increased to counterbalance social distancing challenges) and whether there was a shift in the payer-type (commercial vs Medicaid vs Medicare). This is an important omission from the literature, as the pandemic saw a significant increase in public health insurance coverage and a decline in the uninsured rate, (Bundorf et al., 2021) and Medicaid continues to be the largest payer for mental health services in the US (CMS, 2022).
This study expands on the previous literature by adopting a quasi-experimental research design using a national multi-payer pharmacy claims database to examine trends in psychotropic medication prescriptions from July 2018 to June 2022 after accounting for the beginning of the COVID-19 pandemic in the U.S. in March 2020. Specifically, the current study reports monthly trends in the number of psychotropic prescriptions dispensed, the average days supply of psychotropic prescriptions, and how psychotropic prescriptions dispensed varied by payer-type (private insurance, Medicaid, Medicare and cash). The study also reports the number of patients prescribed psychotropic medication.
2. Methods
2.1. Data
The data for the analysis were drawn from IQVIA's National Prescription Audit (NPA), PayerTrak, and Total Patient Tracker (TPT) databases, covering prescriptions from July 2018 to June 2022. NPA includes over 3 billion prescriptions per year, representing more than 92% of prescriptions dispensed at retail pharmacies (chain, independent, and food store pharmacies and mail-orders) and covers all 50 states and the District of Columbia. We used NPA data to analyze the total number of psychotropic prescriptions dispensed per month and the average days’ supply for dispensed prescriptions per month (see Appendix 1 for the list of psychotropic medication names by class). Similar to NPA, PayerTrak also includes over 3 billion prescriptions per year and covers more than 92% of prescriptions dispensed in retail settings. Additionally, PayerTrak includes information on the source of payer for the prescriptions, enabling us to analyze how the number of psychotropic medications dispensed varied each month by payer type (private insurance, Medicaid, Medicare and cash payment). TPT data capture the total number of unique patients at the national level across all drugs and therapeutic classes in the retail outpatient setting. TPT eliminates duplicate patients and multiple prescription fills, allowing us to produce unique patient counts. We used TPT data to estimate the total number of patients per month who were prescribed psychotropic medications. IQVIA data sets are statistically deidentified and as such are exempt from the U.S. Department of Health and Human Services regulations that require institutional review board approval.
2.2. Analysis
We used interrupted time series (ITS) analysis, a quasi-experimental research design, to estimate changes in each psychotropic medication outcome associated with the declaration of 2020 COVID-19 PHE (March 2020). The following equation was used for the regression:
where Yt is the outcome variable measured at each monthly time point t, Tt is the time since the start of observation (in months), Xt is a dummy (indicator) variable representing the COVID-19 pandemic (pre–March 2020 periods = 0, post-March 2020 periods = 1), XtTt is a timeperiod interaction term, Zt is a set of indicator variables to control for month length (28 or 29 and 30 days vs. 31 days), and εt is the error term. We specified the models to test for both a one-time change immediately when the COVID-19 pandemic began (intercept/level change, β2) and a difference in trends between the pre- and post-COVID-19 pandemic periods (slope change, β3). We estimated the models using ordinary least squares with Newey-West standard errors to account for autocorrelated error terms. All analyses were conducted in Stata/MP 17.
3. Results
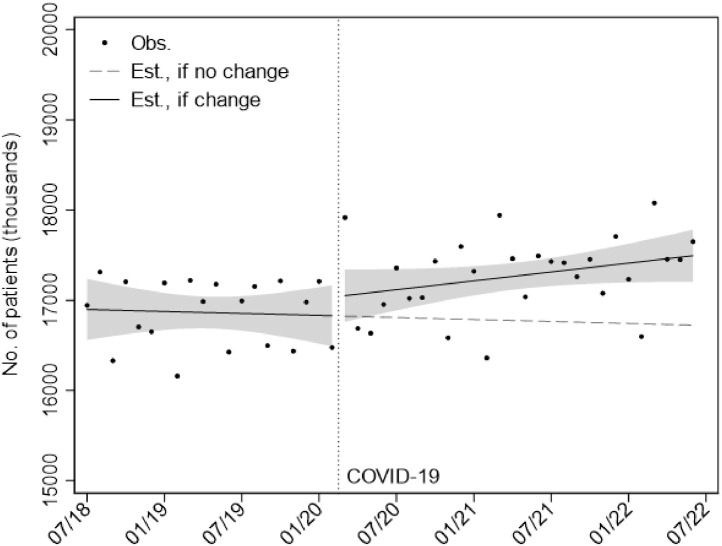
Fig. 1 (observed data points and unadjusted model predictions) and Table 1 (adjusted model estimates) show that the change in the number of patients filling a medication was not significantly different than zero. The unadjusted trend in Fig. 1 appears negative, while the estimate from the adjusted ITS model was +5380 patients/month (p = 0.392). In the adjusted ITS model, we did not detect a significant, immediate shift in the number of patients with psychotropic prescription fills per month at the start of the pandemic in March 2020 (+76,990 patients, p = 0.476). During the pandemic, the number of patients with filled psychotropic medications increased at a statistically significant rate (+20,110 patients/month, p = 0.003), adjusting for month length. This rate, however, was not significantly different than the adjusted pre-COVID rate (+14,730 patients/month, p = 0.165).
Fig. 1.
Monthly number of patients with psychotropic prescription fills, July 2018 to June 2022 Notes: Obs., observed; est., estimated. Estimates were derived from an unadjusted Interrupted Time Series model accounting for changes in level and slope. Shaded areas indicate 95% confidence intervals. Data Source: IQVIA Total Patient Tracker.
Table 1.
Psychotropic Prescription Fills July 2018 – June 2022: Total Fills, and Prescription length.
| Patients | Prescriptions | Rx Days | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Coef. | SE | P | Coef. | SE | P | Coef. | SE | P | |
| Intercept | 17,020.06 | 67.06 | <0.001 | 41,412.48 | 230.81 | <0.001 | 32.50 | 0.14 | <0.001 |
| Slopes | |||||||||
| Pre-COVID | 5.38 | 6.22 | 0.392 | 5.04 | 22.28 | 0.822 | 0.13 | 0.01 | <0.001 |
| Post-COVID | 20.11 | 6.31 | 0.003 | 53.83 | 21.63 | 0.017 | −0.00 | 0.01 | 0.813 |
| Difference | 14.73 | 10.43 | 0.165 | 48.79 | 37.29 | 0.198 | −0.13 | 0.02 | <0.001 |
| Level | |||||||||
| Difference | 76.99 | 107.14 | 0.476 | 501.16 | 361.44 | 0.173 | 0.88 | 0.24 | 0.001 |
| Days per month (ref. = 31) | |||||||||
| 29 | −919.74 | 94.22 | <0.001 | −3376.52 | 314.60 | <0.001 | |||
| 30 | −386.00 | 93.53 | <0.001 | −1365.47 | 339.13 | <0.001 | |||
| N | 48 | 48 | 48 | ||||||
| Lag | 2 | 3 | 1 | ||||||
Notes: N = 48 for all models. Linear regressions with Newey-West standard errors to account for autocorrelation.
Data Source: IQVIA Total Patient Tracker and National Prescription Audit.
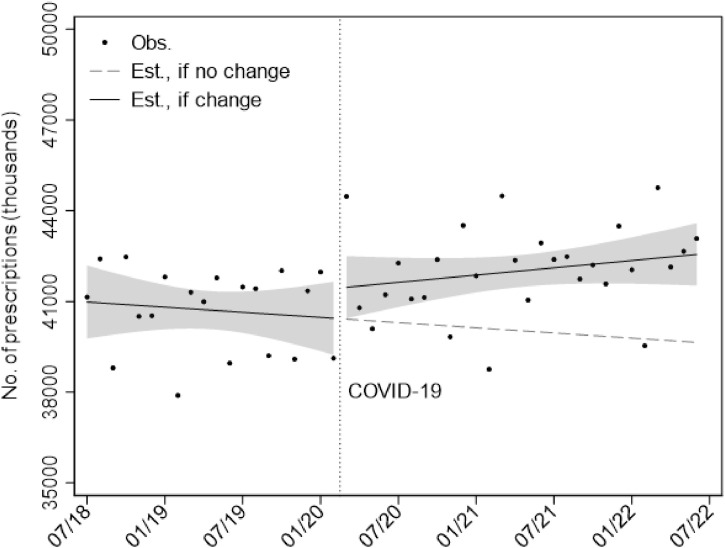
The observed and predicted values of monthly psychotropic prescriptions dispensed are presented in Fig. 2 (predicted values based on unadjusted ITS models). Adjusted ITS results are also shown in Table 1. In general, filled prescriptions followed a similar pattern to our patient level outcome. Fig. 2 appears to show a pre-COVID decrease from about 41.9 million prescriptions to about 38.1 million at the start of the pandemic. After controlling for month length, however, there was not a significant pre-COVID trend in either direction (+5040 fills/month, p = 0.822). During the pandemic, the number of psychotropic medication fills each month did increase at a significant adjusted rate (+53,830 fills/month, p = 0.017), but this was not significantly different than the adjusted pre-period trend. We also did not observe a statistically significant immediate level change at the start of the pandemic.
Fig. 2.
Monthly number of psychotropic prescription fills, July 2018 to June 2022 Notes: Obs., observed; est., estimated. Estimates were derived from an unadjusted Interrupted Time Series model accounting for changes in level and slope. Shaded areas indicate 95% confidence intervals. Data Source: IQVIA National Prescription Audit.
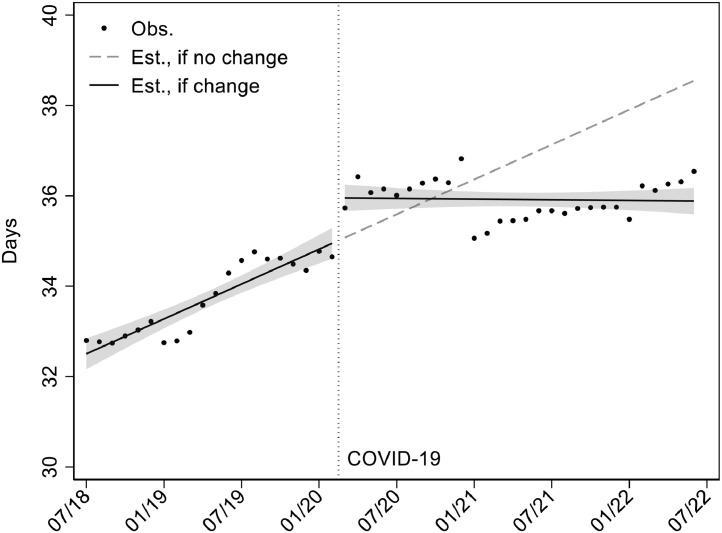
Fig. 3 shows that the average days supply of psychotropic prescriptions dispensed each month was about 33–34 days in the pre-pandemic period and about 36 days during the pandemic. ITS model-based estimates (Table 1) indicate that the average length of a prescription was significantly increasing by about 0.13 days per month (p<0.001) in the pre-period. At the beginning of the pandemic there was a significant, immediate level shift of about 0.88 days (p<0.001), but during the pandemic the increasing trend did not continue (during pandemic: 0.00 days/month, p = 0.813;).
Fig. 3.
Average days supply of psychotropic prescription fills, July 2018 to June 2022 Notes: Obs., observed; est., estimated. Estimates were derived from an unadjusted Interrupted Time Series model accounting for changes in level and slope. Shaded areas indicate 95% confidence intervals. Data Source: IQVIA National Prescription Audit.
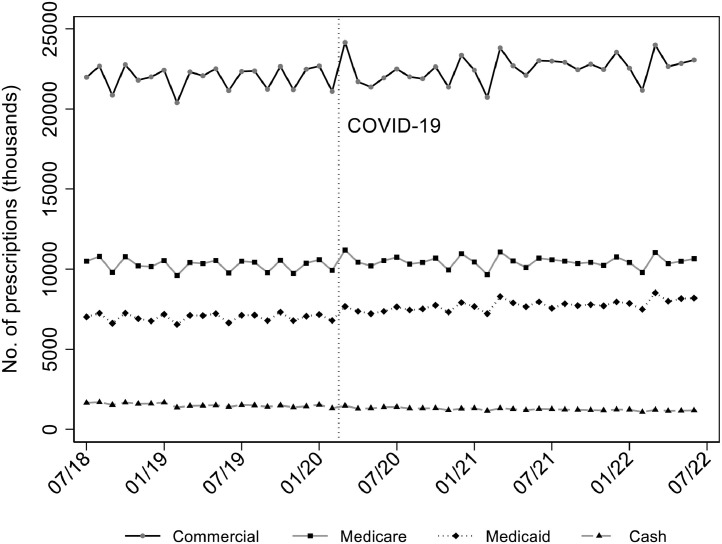
Fig. 4 displays trends in psychotropic prescription fills by payer. Commercial insurance was the primary payer of psychotropic medications during the pre-pandemic period (∼ 50% of all psychotropic prescriptions). This continued after the pandemic with commercial insurance paying for about 20–25 million fills per month, accounting for almost 50% of all psychotropic prescriptions. Medicare was the second-leading payer for psychotropic medications filled in retail pharmacies, paying for about 10–11 million fills a month. Medicaid paid for about 7–8 million fills a month), and last, cash (fully out-of-pocket) payments accounted for about 1–2 million fills per month. Table 2 shows ITS model-based estimates of levels and rates of change before and during the pandemic. For fills paid by commercial insurance, there were no significant changes associated with the pandemic, but there was a significant, increasing trend of about 34,480 additional fills per month during the pandemic period (p = 0.018). For psychotropic medications paid for by Medicaid, there was a statistically significant increase in level in March 2020 of about 320,370 prescriptions per month (p<0.001) and a significant change in slope by about 21,310 prescriptions per month from before to during the pandemic (p<0.001). There was no statistically significant change in the slope for fills paid by Medicare . Prescriptions for psychotropic medications paid for in cash were already declining during the pre-pandemic period (an average of 11,930 fewer per month, p<0.001) and continued to decline at a statistically significant rate of about −7450 fewer fills per month during the pandemic (p<0.001) compared to pre-pandemic.
Fig. 4.
Monthly number of psychotropic prescriptions fills by payer, July 2018 to June 2022 Data Source: IQVIA National Sales Perspective.
Table 2.
Psychotropic Prescription Fills by Payer Type July 2018 – June 2022.
| Commercial | Medicaid | Medicare | Cash | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coef. | SE | P | Coef. | SE | P | Coef. | SE | P | Coef. | SE | P | |
| Intercept | 22,214.32 | 107.72 | <0.001 | 7045.63 | 42.45 | <0.001 | 10,496.24 | 77.87 | <0.001 | 1656.29 | 21.53 | <0.001 |
| Slopes | ||||||||||||
| Pre-COVID | 15.95 | 11.38 | 0.169 | 5.73 | 2.98 | 0.061 | −4.71 | 7.53 | 0.535 | −11.93 | 1.92 | <0.001 |
| Post-COVID | 34.48 | 13.95 | 0.018 | 27.04 | 4.06 | <0.001 | −0.23 | 5.46 | 0.966 | −7.45 | 1.01 | <0.001 |
| Difference | 18.53 | 21.51 | 0.394 | 21.31 | 4.92 | <0.001 | 4.48 | 10.97 | 0.685 | 4.47 | 2.25 | 0.053 |
| Level | ||||||||||||
| Difference | −54.16 | 237.09 | 0.820 | 320.37 | 63.58 | <0.001 | 265.40 | 98.47 | 0.010 | −30.45 | 29.36 | 0.306 |
| Days per month (ref. = 31) | ||||||||||||
| 29 | −1896.34 | 147.01 | <0.001 | −519.03 | 65.30 | <0.001 | −806.98 | 103.04 | <0.001 | −154.17 | 19.42 | <0.001 |
| 30 | −756.60 | 170.44 | <0.001 | −201.63 | 66.25 | 0.004 | −350.07 | 98.36 | 0.001 | −57.17 | 15.92 | 0.001 |
| N | 48 | 48 | 48 | 48 | ||||||||
| Lag | 2 | 4 | 3 | 1 | ||||||||
Notes: N = 48 for all models. Linear regression with Newey-West standard errors to account for autocorrelation.
Data Source: IQVIA National Sales Perspective.
Stratifying our analysis of the number of patients with psychotropic prescription fills across four therapeutic classes (antidepressants, anxiolytics/sedatives, antipsychotics, and stimulants), we observed similar patterns (Appendix Table 2 ). While there was some gradual growth across the entire study period, there were not consistent changes from before to during the pandemic.
Table A2.
. Number of Patients with Psychotropic Prescription Fills by Therapeutic Class July 2018 – June 2022.
| Antidepressants | Anxiolytics/Sedatives | Antipsychotics | Stimulants | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coef. | SE | P | Coef. | SE | P | Coef. | SE | P | Coef. | SE | P | |
| Intercept | 17,461.39 | 64.13 | <0.001 | 11,093.30 | 49.83 | <0.001 | 2585.35 | 10.26 | <0.001 | 2630.53 | 31.73 | <0.001 |
| Slopes | ||||||||||||
| Pre-COVID | 25.18 | 7.65 | 0.002 | −14.07 | 4.01 | 0.001 | 6.82 | 0.95 | <0.001 | 13.01 | 2.43 | <0.001 |
| Post-COVID | 42.21 | 7.50 | <0.001 | −2.56 | 3.71 | 0.493 | 6.45 | 0.80 | <0.001 | 19.92 | 2.23 | <0.001 |
| Difference | 17.03 | 12.19 | 0.170 | 11.50 | 5.85 | 0.056 | −0.37 | 1.27 | 0.770 | 6.91 | 3.33 | 0.044 |
| Level | ||||||||||||
| Difference | −48.17 | 157.07 | 0.761 | 173.73 | 73.70 | 0.023 | 51.33 | 19.57 | 0.012 | −196.56 | 46.22 | <0.001 |
| Days per month (ref. = 31) | ||||||||||||
| 29 | −973.22 | 120.98 | <0.001 | −655.78 | 59.97 | <0.001 | −118.00 | 15.45 | <0.001 | −136.76 | 25.82 | <0.001 |
| 30 | −397.90 | 107.42 | 0.001 | −283.81 | 65.64 | <0.001 | −52.77 | 14.88 | 0.001 | −57.82 | 16.91 | 0.001 |
| N | 48 | 48 | 48 | 48 | ||||||||
| Lag | 4 | 4 | 4 | 4 | ||||||||
Notes: Linear regressions with Newey-West standard errors to account for autocorrelation. Data Source: IQVIA Total Patient Tracker.
4. Discussion
Using a national multi-payer pharmacy claims database, this study found that the trends in the number of patients with psychotropic medication fills, and the number of fills declined during the early period of the pandemic but experienced a significant growth during the later period and exceeded the pre-pandemic trends. Average days supply of psychotropic medications dispensed increased significantly from about 33 days in the pre-pandemic period to about 36 days during the pandemic. Commercial insurance remained the primary payer for psychotropic medication during the pandemic, but there was a significant increase in the number of prescription fills covered under Medicaid of about 21,000 fills per month above and beyond the pre-pandemic trend. Though prior studies documented a small decline in psychotropic medications dispensed in the early months of the pandemic (Nason et al., 2021; Hirschtritt et al., 2021; Leong et al., 2022), our results show that, as the pandemic continued and in the context of a rising prevalence of mental health conditions, psychotropic medication use grew at statistically significant rates between March 2020 and June 2022.
The COVID-19 pandemic prompted numerous policy changes in the mental health treatment delivery system at both the federal and state level. These changes include flexibilities around prescriptions via telehealth, including increased reimbursement and coverage for telehealth services, and home delivery options for patients, expedited licensing and lowering barriers to interstate practice for providers among others (Moreno et al., 2020). An evaluation of the impacts of these specific polices implemented during COVID-19 on the initiation and continuation of psychotropic medication use for mental health conditions will be an important avenue for future research to explore.
Psychotropic medication and psychotherapy are both effective in treating most mental health conditions. There is some evidence that combined treatments may be more effective than each of these treatments alone (NIMH, 2023). The literature also shows that receipt of psychotherapy enhances adherence to medication (NIMH, 2023). However, a significant proportion of patients with mental health conditions receive psychotropic medication without any psychotherapy (Olfson and Marcus, 2010). An important avenue for future research to consider would be to examine how the COVID-19 pandemic has impacted the use of psychotherapy in conjunction with and without psychotropic medication.
The study also found a significant increase in psychotropic medication being paid for by Medicaid during the pandemic, although private insurance still remained the primary payer for psychotropic medications. This finding is consistent with the literature that has documented a higher enrollment in public health insurance programs after the initial shock to employment in March 2020 (Bundorf et al., 2021) Even before the pandemic, Medicaid was a major payer for behavioral health services (CMS, 2021), but the pandemic may have accelerated this growth. To our knowledge, most of the changes in Medicaid policies during our study period are related to the COVID-19 PHE. The unique nature of the pandemic, and the economic downturn it caused, prompted many states to adopt Medicaid emergency authorization to expand eligibility and/or modify eligibility rules, eliminate/waive premiums, and streamline the application and enrollment processes. All of this might help to explain the growing share of psychotropic medication being covered by Medicaid.
4.1. Limitations
Despite the comprehensive nature and timeliness of the data, the findings of this study should be viewed in the context of some limitations. First, the study examined psychotropic medications in general, but it was not coupled with electronic medical records to determine if their use was for a psychiatric condition. It is also important to note that IQVIA does not include federal sources such as Veterans Affairs and Indian Health Services. Second, race/ethnicity of the patients were not available in the IQVIA data sets used in the study. The literature has shown the impact of the COVID-19 pandemic to be more pronounced among people of color (Shim and Starks, 2021), and examining racial/ethnic differences in psychotropic medications during the pandemic will be an important direction for future studies to pursue. Third, our study was not able to distinguish between psychotropic medication initiation vs continuation. Examining treatment initiation and continuation will have important policy implications as the pandemic continues to evolve. Finally, a methodological limitation of our ITS estimation strategy is the lack of a non-treatment or a control group. In quasi-experimental research design, it is a common practice to include a control group; however, finding a suitable control group in our case was difficult because COVID-19 impacted almost every aspect of the US health care system. Thus, it is prudent to view our results as demonstrating strong associations rather than causal relationships.
4.2. Conclusions/Implications
Expanding and maintaining access to mental health treatment has been a key priority in the federal and state response to the COVID-19 pandemic. The results of our study show that the use of psychotropic medication remained stable during the pandemic with public insurance programs playing an important role in helping patients to pay for their treatment. However, it is still not known whether the gap in unmet need for mental health treatment narrowed or increased.
Declaration of Competing Interest
None.
Footnotes
Disclaimer: The views expressed here are those of the authors and do not necessarily reflect the views of the Office of the Assistant Secretary for Planning & Evaluation, Substance Abuse & Mental Health Services Administration, or US Department of Health & Human Services.
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.psychres.2023.115248.
Appendix A
Appendix B. Supplementary materials
References
- Bo H.-X., Li W., Yang Y., et al. Posttraumatic stress symptoms and attitude toward crisis mental health services among clinically stable patients with COVID-19 in China. Psychol Med. Published online. 2020:1–2. doi: 10.1017/S0033291720000999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bundorf M.K., Gupta S., Kim C. Trends in US health insurance coverage during the COVID-19 pandemic. JAMA Health Forum. 2021;2(9) doi: 10.1001/jamahealthforum.2021.2487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Medicare and Medicaid Services. Behavioral Health Services. https://www.medicaid.gov/medicaid/benefits/behavioral-health-services/index.html Accessed October 26, 2022.
- Demeke H.B., Merali S., Marks S., et al. Trends in use of telehealth among health centers during the COVID-19 Pandemic — United States. MMWR Morb. Mortal Wkly. Rep. 2021;70:240–244. doi: 10.15585/mmwr.mm7007a3. June 26–November 6, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Druss B.G. Addressing the COVID-19 pandemic in populations with serious mental illness. JAMA Psychiatry. 2020;77(9):891–892. doi: 10.1001/jamapsychiatry.2020.0894. [DOI] [PubMed] [Google Scholar]
- Hirschtritt M.E., Slama N., Sterling S.A., Olfson M., Iturralde E. Psychotropic medication prescribing during the COVID-19 pandemic. Medicine (Baltimore) 2021;100(43):e27664. doi: 10.1097/MD.0000000000027664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes E.A., O'Connor R.C., Perry V.H., et al. Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry. 2020;7(6):547–560. doi: 10.1016/S2215-0366(20)30168-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leong C., Kowalec K., Eltonsy S., et al. Psychotropic medication use before and during COVID-19: a population-wide study. Front. Pharmacol. 2022;13 doi: 10.3389/fphar.2022.886652. Published 2022 Apr 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mazza M.G., De Lorenzo R., Conte C., et al. Anxiety and depression in COVID-19 survivors: role of inflammatory and clinical predictors. Brain Behav. Immun. 2020;89:594–600. doi: 10.1016/j.bbi.2020.07.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreno C., Wykes T., Galderisi S., et al. How mental health care should change as a consequence of the COVID-19 pandemic. Lancet Psychiatry. 2020;7(9):813–824. doi: 10.1016/S2215-0366(20)30307-2. [published correction appears in Lancet Psychiatry. 2021 Jul;8(7):e16] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nason I., Stein D.T., Frank R.G., Stein M.B. Decline In New Starts Of Psychotropic Medications During The COVID-19 Pandemic. Health Aff. (Millwood). 2021;40(6):904–909. doi: 10.1377/hlthaff.2021.00028. [DOI] [PubMed] [Google Scholar]
- National Institute of Mental Health. Mental Health Medication. https://www.nimh.nih.gov/health/topics/mental-health-medications Accessed May 1, 2023.
- Novak P., Sanmartin M.X., Ali M.M., Chen J. Health conditions associated with severe illness from COVID-19 among individuals with serious mental illness. Psychiatr. Serv. 2021;72(4):468–469. doi: 10.1176/appi.ps.202000300. [DOI] [PubMed] [Google Scholar]
- Olfson M., Marcus S.C. National trends in outpatient psychotherapy. Am. J. Psychiatry. 2010;167(12):1456–1463. doi: 10.1176/appi.ajp.2010.10040570. DecEpub 2010 Aug 4. PMID: 20686187. [DOI] [PubMed] [Google Scholar]
- Shim R.S., Starks S.M. COVID-19, structural racism, and mental health inequities: policy implications for an emerging syndemic. Psychiatr. Serv. 2021;72(10):1193–1198. doi: 10.1176/appi.ps.202000725. [DOI] [PubMed] [Google Scholar]
- Taquet M., Geddes J.R., Husain M., Luciano S., Harrison P.J. 6-month neurological and psychiatric outcomes in 236,379 survivors of COVID-19: a retrospective cohort study using electronic health records. Lancet Psychiatry. 2021;8(5):416–427. doi: 10.1016/S2215-0366(21)00084-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu J.M., Myers R., McConnell K.J., Levander X., Lin S.C. Trends In Outpatient Mental Health Services Use Before And During The COVID-19 Pandemic. Health Aff (Millwood) 2022;41(4):573–580. doi: 10.1377/hlthaff.2021.01297. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.