Abstract
Objective
To evaluate the prevalence of post-traumatic stress disorder (PTSD) and other psychological disturbances in the Vietnamese healthcare workers (HCWs) at COVID-19 field hospitals.
Methods
A cross-sectional study was conducted using the Impact of Event Scale–Revised (IES-R) to measure PTSD and the Depression Anxiety Stress scale (DASS) to measure other psychological disturbances. The anxiety about COVID-19 was evaluated by the fear of COVID-19 (FOC) scale. A self-developed questionnaire was used to assess work conditions and HCW’s major concerns and preparedness. Ordinal logistic regression was used to identify factors associated with the severity of PTSD. A structural modeling equation (SEM) model was fitted to examine the correlation between PTSD and other psychological disturbances.
Results
A total of 542 HCWs participated in this study. The prevalence of PTSD was 21.2%, most cases were mild. In the ordinal logistic regression analysis, a history of mental illness, poor preparedness, working in a condition with poor resources, a greater number of concerns, and greater fear of COVID-19 were independently associated with higher severity of PTSD. The prevalence of depression, anxiety, and stress was 46.8%, 38.3%, and 60.2, respectively. In the SEM model, PTSD and psychological disturbances had a strong correlation (standardized covariance 0.86).
Conclusion
The prevalence of PTSD and other psychological disturbances was alarmingly high among HCWs who worked at COVID-19 field hospitals. The reported associated factors can be useful for policymakers and health authorities in the preparation for future pandemics.
Keywords: PTSD, COVID-19, healthcare workers, DASS, fear of COVID, psychological disturbances
Introduction
In the early period of the COVID-19 pandemic, Vietnam managed to effectively control transmission and maintain zero deaths for months.1 However, the fourth wave of the COVID-19 pandemic, which started on April 27, 2021, has drastically altered the situation, primarily due to the invasion of the Delta variant. As of September 12, 2021, Vietnam had reported 601,349 cases and 15,018 deaths, making this wave the most complicated and lethal COVID-19 period in Vietnam.2 The remarkable increase in the number of confirmed and hospitalized cases had imposed a massive burden on the entire healthcare system.3 In July and August 2021, nearly 15,000 healthcare workers (HCWs) nationwide travelled to the pandemic hotspots in Ho Chi Minh City and other Southern provinces to support local HCWs in screening, triage, and patient care.4
Emergency responses to the pandemic rendered HCWs extremely vulnerable due to the high-risk working environment as well as severe mental toll from high work pressures, witnessing deaths, fear of SARS-CoV-2 infection, homesickness, financial problems, and stigmatization. In a systematic review that included 498 HCWs, the main burdens of healthcare providers during the COVID-19 pandemic were inadequate preparedness, emotional challenges, insufficient equipment and information, and work burnout.5 Despite the mental burden that they had to bear, HCWs did not receive adequate mental health support and were thus more susceptible to anxiety, depression, and post-traumatic stress disorder (PTSD).6 A systematic review reported that the prevalence of anxiety, distress and PTSD of HCWs during the pandemic were 40%, 37%, and 49%, respectively.7
Understanding the picture of mental health in HCWs who participate in responding to pandemics is critical in developing appropriate and cost-effective preventative and therapeutic measures for this understaffed but overworked labor force. Therefore, in this study, we aimed to estimate the psychological disturbances of Vietnamese HCWs who worked at COVID-19 field hospitals.
Materials and Methods
Study Design
We conducted a cross-sectional study on the HCWs who worked at eight COVID-19 field hospitals in Ho Chi Minh City from 15th July to 25th September 2021.
Participant’s Eligibility
All HCWs who were available during the data collection period were included in the study. Those who were not willing to participate and not actively on duty at the time of the survey due to any leave of absence were excluded.
Sample Size
Sample size was calculated based on the prevalence of PTSD in HCWs at COVID-19 field hospitals in a previous study.8 Assuming a prevalence of PTSD in HCWs of 30%, a margin of error of 5%, and a confidence level of 95%, the minimum sample size was 288 participants. Accounting for the non-response rate of 20%, we planned to recruit 346 participants.
Data Collection
We developed an online structured questionnaire using Google Forms, which was then sent to the participants via Zalo and Viber groups of HCWs who were taking care of patients at the field hospitals. After reading the first page that explained the study objectives, participants were asked to provide their informed consent. Only those who chose Yes in the question about informed consent would be taken to the data collection pages; otherwise, the form finished. Collected data included demographic data, medical history, COVID-related information, the preparedness of HCWs before participating in COVID-19 field hospitals, self-assessed work conditions in COVID-19 field hospitals, major concerns, and questionnaires on psychological disturbances.
We evaluated the anxiety about COVID-19 by the fear of COVID-19 (FOC) scale. This scale contains seven items stating the mental and bodily changes when thinking about COVID-19. Participants were asked to rate their agreement to the items using a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree). The overall scores ranged from 7 to 35, with higher scores indicating greater COVID-19 fear. The validated scale of COVID-19 fear was reported with good reliability in various medical settings in Vietnam.9,10
Regarding their preparedness, participants were asked to rate their mental and knowledge preparedness as poor/average/good. We created a composite variable of preparedness, where good preparedness was defined as moderated to good preparation in both aspects, while poor preparedness was defined as poor preparation in either aspect.
To assess the work conditions, we asked participants about 13 items, which could be grouped into conditions of facilities and human resources. For most items, the participants rated their assessment of the condition using a 3-point scale (1 = not at all / poor / never, and 3 = very / good / always). The number of deaths witnessed, nurse-to-patient ratio, doctor-to-patient ratio, and degree of respect from colleagues and patients were assessed in a more detailed scale (4 or 5 points).
We assessed five major concerns including worry about getting COVID-19, spreading COVID-19, impacts on economic status, losing connection with people, and being overloaded using a 4-point Likert scale (1 = never to 4 = always). The responses of often or always were considered “having the major concern”, and we counted the number of major concerns that each participant had.
Study Outcomes
PTSD was our primary endpoint and was measured by the Impact of Event Scale–Revised (IES-R), a psychometric tool developed by Horowitz in 1979 and revised in 1997 to assess catastrophic psychological damage produced by unexpected events.11 The instrument has twenty-two items, belonging to three dimensions (intrusion, avoidance, and hyperarousal). Participants were asked about the degree of distress caused by difficulties for the past seven days and rated the degree using a 5-point Likert-type scale with a range of 0 = not at all to 4 = extremely. The “intrusion” subscale has eight items, “avoidance” eight items, and “hyperarousal” six items. The subscale score is the average score of the items (range 0–4). Item scores are then summed to the overall score (range 0–88). Based on the overall IES-R score, the participant can be classified as normal (0–23), mild (24–32), moderate (33–36) and severe psychological distress (37–88). In our study, a participant with an overall score of 24 or higher was considered “possible PTSD”.12–14 The IES-R has been tested for reliability and validity, confirming its strong internal consistency, test-retest reliability, and moderate criterion validity.15–17
Secondary outcomes included other psychological disturbances measured by Depression Anxiety Stress scale (DASS). The DASS is a set of three self-report scales designed to measure the negative emotional states of depression, anxiety, and stress. We used DASS-21, which has twenty-one items, divided into three subscales of depression, anxiety, and stress, each containing seven items. Participants were asked about the psychological disturbances occurred for the past seven days and response using a 4-point Likert-type scale with a range of 0 = not at all to 3 = most of the time. Depression, anxiety, and stress scores are measured by summing the scores of their items. Because the DASS-21 is a shorter version of the 42-item original DASS, the score for each subscale must be multiplied by 2 to calculate the final score. The cut-off points for each subscale were similar to those in previous studies, and based on these thresholds, the final score were classified as: normal, mild, moderate, severe, or extremely severe.18–20 The DASS has been tested for reliability and validity, confirming its excellent internal consistency, discriminative, concurrent and convergent validities.21–24
Statistical Analysis
Variables were presented as frequency and percentage for categorical variables, and mean (standard deviation) or median (interquartile range, Q1-Q3) for continuous variables. Stacked bar charts were used to illustrate the distribution of responses regarding outcomes, fear of COVID, and major concerns.
All psychometric scales were evaluated for their psychometric properties using confirmatory factor analysis (CFA) and Cronbach alpha. We did not provide a detailed report of these analyses since they were not our primary objective; results could be provided upon request. All psychometric scales had borderline validity (all reported goodness of fit statistics were very close to their criterion cutoffs) and good internal consistency (S1 Table).
To summarize the work conditions, we first dichotomized the item responses (detailed cutoffs can be provided upon request). Then, latent class analysis (LCA) models were fitted to explore the different types (classes) of work conditions. We later included these types of work conditions in multivariable regression models to evaluate the outcome regarding the differences in work conditions.
The ordinal logistic regression model was used to identify factors associated with the severity of PTSD. The candidates for the regression models were selected on the theoretical basis through literature review and clinical experience; factors that were not selected based on theory but associated with the outcomes of interest in the univariate analysis might also be included in the models.
We also fitted a structural modeling equation (SEM) model to examine the structure of PTSD and other psychological disturbances constructs. The psychological disturbances construct included three observed variables: depression, anxiety, and stress, which were the total subscale score of the DASS-21. The PTSD construct included the three IES-R subscales (intrusion, avoidance, and hyperarousal). The SEM model aimed to show the correlation between PTSD and other psychological disturbances.
All analyses were performed using Stata/BE 17 (StataCorp LLC, College Station, TX, US). An analysis with P-values of less than 0.05 was considered statistically significant.
Ethical Consideration
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of Bach Mai Hospital under decision No. 2727/QĐ-BVBM dated June 8th, 2021. Online informed consent was obtained before data collection. The participants were informed about the study objectives and their right to withdraw at any moment without giving a reason. Their responses were anonymous and kept confidential.
Results
Participants Characteristics
Five hundreds and forty-three HCWs agreed to participate in this study, of which, 276 (50.8%) were males, 258 (47.5%) married, 252 (46.4%) physicians, 209 (38.5%) nurses, and the median age was 30 years (Q1-Q3 27–36). Nearly half of the participants had more than 5 years of working experience. Sixty-seven (12.3%) of the participants had a history of mental illness (eg, anxiety, insomnia, bipolar disorder), of which, 11 (16.4%) were receiving treatment. All participants, except one, had been vaccinated with 2 doses of COVID-19 vaccine, with the most recent dose being administered for more than 4 weeks before the survey. Forty-nine (9%) participants previously worked at a COVID-19 field hospital, and one-fourth were working for more than 8 weeks at the current COVID-19 field hospital. Half of the participants were working at an emergency department or intensive care unit, while most of them were frequently exposed to COVID-19 patients/samples (Table 1).
Table 1.
Participant Characteristics (n = 543)
| Variables | Results |
|---|---|
| DEMOGRAPHIC | |
| Gender, n (%) | |
| Male | 276 (50.8) |
| Female | 267 (49.2) |
| Age, median (Q1-Q3) | 30.0 (27.0; 36.0) |
| Married and living with spouse, n (%) | 258 (47.5) |
| Religion, n (%) | |
| Buddhism | 78 (14.4) |
| Christian | 15 (2.8) |
| Traditional Vietnamese religion | 43 (7.9) |
| Atheism | 407 (75.0) |
| Postgraduate education, n (%) | 145 (26.7) |
| Specialty, n (%) | |
| Physician | 252 (46.4) |
| Nurse | 209 (38.5) |
| Other* | 82 (15.1) |
| Working experience >5 years, n (%) | 258 (47.5) |
| MEDICAL HISTORY | |
| Having a history of mental illness, n (%) | 67 (12.3) |
| Received treatment, n (%) | 11 (16.4) |
| Having a history of physical illness, n (%) | 101 (18.6) |
| Received treatment, n (%) | 38 (37.6) |
| COVID-RELATED | |
| Vaccination, n (%) | |
| 1st dose received | 6 (1.1) |
| 2nd dose received | 537 (98.9) |
| Time of most recent dose, n (%) | |
| <4 weeks | 52 (9.6) |
| ≥4 weeks | 491 (90.4) |
| Previously worked at a COVID-19 field hospital, n (%) | 49 (9.0) |
| Duration of working at the current COVID-19 field hospital, n (%) | |
| Less than 1 week | 26 (4.8) |
| 1 < 2 weeks | 57 (10.5) |
| 2 < 4 weeks | 110 (20.3) |
| 4 < 8 weeks | 214 (39.4) |
| ≥ 8 weeks | 136 (25.0) |
| Working at ED/ICU at COVID-19 hospital, n (%) | 299 (55.1) |
| Frequently exposure to COVID-19 patients/samples, n (%) | 491 (90.4) |
Notes: *Other specialties included caregivers, technicians, social workers, and volunteers.
Abbreviations: Q, quartile; ICU, Intensive care unit; ED, Emergency department COVID, Corona virus disease.
Preparedness and Work Conditions
Among the participants, 36.3% and 32.2% claimed that they were well prepared before working at the field hospital in terms of knowledge and mental preparation, respectively. Most participants (80.7%) were classified as “having good preparedness”.
More than half of the participants responded that their hospital had easy access to PPE (59.7%), good infection prevention and control (IPC) protocols (66.3%), and good treatment guidelines (53%). Three-fourth of the participants claimed that they had to perform unfamiliar clinical tasks with insufficient preparation; however, most of them acknowledged that they received sufficient support for their routine clinical tasks (95.1%), for knowledge updates (97.6%), good teamwork (98.9%), and respect from patients and their families (97.8%). Only 17.1% and 16.6% of the participants found that the working schedule and the place for mid-time break were appropriate. Work overload was described by the majority of the participants, with around one-third claimed that at their unit, a nurse was in charge of more than ten patients and a doctor was in charge of more than fifteen patients. Majority of the participants (89%) had witnessed at least one death in their shift (Table 2).
Table 2.
Work Conditions Assessed by HCWs at the Field Hospitals (n = 543)
| Variables | Results |
|---|---|
| How was the access to personal protective equipment? n (%) | |
| Poor | 11 (2.0) |
| Average | 208 (38.3) |
| Excellent | 324 (59.7) |
| How was the infection prevention and control protocol? n (%) | |
| Poor | 11 (2.0) |
| Average | 172 (31.7) |
| Excellent | 360 (66.3) |
| How was the treatment guideline? n (%) | |
| Poor | 37 (6.8) |
| Average | 218 (40.1) |
| Excellent | 288 (53.0) |
| Have to conduct unfamiliar clinical task with inadequate preparation, n (%) | |
| Not true | 134 (24.7) |
| Relatively true | 309 (56.9) |
| True | 100 (18.4) |
| Was your teamwork good? n (%) | |
| Poor | 6 (1.1) |
| Average | 309 (56.9) |
| Excellent | 228 (42.0) |
| Was the current working schedule reasonable? n (%) | |
| Not reasonable | 97 (17.9) |
| Relatively reasonable | 353 (65.0) |
| Reasonable | 93 (17.1) |
| Was the mid-time break location reasonable? n (%) | |
| Not reasonable | 96 (17.7) |
| Relatively reasonable | 357 (65.7) |
| Reasonable | 90 (16.6) |
| Did you receive adequate support in daily clinical task? n (%) | |
| Poor | 27 (5.0) |
| Average | 362 (66.7) |
| Excellent | 154 (28.4) |
| How often have you been provided with updated knowledge on the epidemiology, diagnosis, treatment, and prevention of COVID-19? n (%) | |
| Not at all | 13 (2.4) |
| Sometimes | 191 (35.2) |
| Always | 339 (62.4) |
| What number is the most fatalities have you witness during your shift? n (%) | |
| None | 125 (23.0) |
| 1 patient | 101 (18.6) |
| 2–5 patients | 204 (37.6) |
| 6–10 patients | 53 (9.8) |
| More than 10 patients | 60 (11.0) |
| In your unit, what is the ratio of nurse/patient? n (%) | |
| 1 nurse/<3 patients | 41 (7.6) |
| 1 nurse/3–5 patients | 189 (34.8) |
| 1 nurse/6–10 patients | 152 (28.0) |
| 1 nurse/>10 patients | 161 (29.7) |
| In your unit, what is the ratio of doctor/patient? n (%) | |
| 1 doctor/<5 patients | 76 (14.0) |
| 1 doctor/5–9 patients | 150 (27.6) |
| 1 doctor/10–15 patients | 147 (27.1) |
| 1 doctor/>15 patients | 170 (31.3) |
| Did you get the respect from the patients and their family members? n (%) | |
| Not at all | 12 (2.2) |
| Sometimes | 130 (23.9) |
| Often | 309 (56.9) |
| Always | 92 (16.9) |
Abbreviation: COVID, Corona virus disease.
Using an LCA model with seven items, we were able to classify patients into three groups: poor resources, good facilities but poor human resources, and good resources. The marginal plot of class characteristics (S1 Figure) shows the probability of having good work conditions in each item, with good separation between classes. In this LCA model, nearly half of the participants (49.4%) worked at a place with good facilities but poor human resources, and one-fourth each worked at a place with poor resources and good resources.
Major Concerns and Fear of COVID
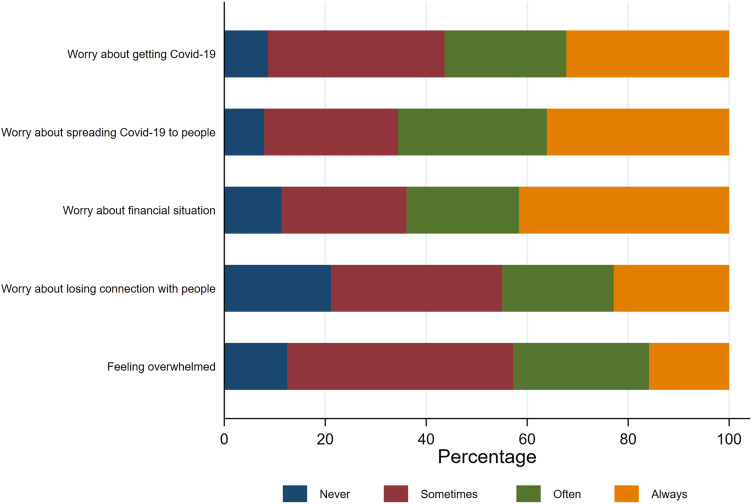
A majority of the participants reported that they often/always worried about getting infected with COVID-19 (56.3%), spreading COVID-19 to the people they live with (65.6%), financial problems (63.9%), losing connection with their family and loved ones (44.9%). The feeling of overwhelmed at work was reported by 42.7% of the participants (Figure 1). Only 80 participants (14.7%) had no apparent concerns, more than half of the participants had 3–5 concerns.
Figure 1.
Major concerns of participants (n = 543).
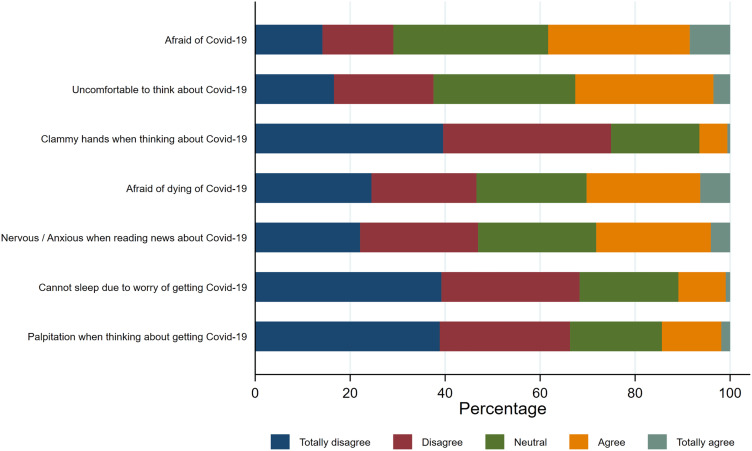
Despite having concerns about their situation during COVID-19, a large proportion of participants (between 30% and 70%) disagreed with statements about the fear of COVID (Figure 2). The most commonly encountered feelings were being most afraid of COVID-19 (38.3%), uncomfortable to think about COVID-19 (32.6%), afraid of dying of COVID-19 (30.2%), and nervous or anxious when reading news about COVID-19 (28.2%).
Figure 2.
Distribution of the fear of COVID score among study participants (n = 543).
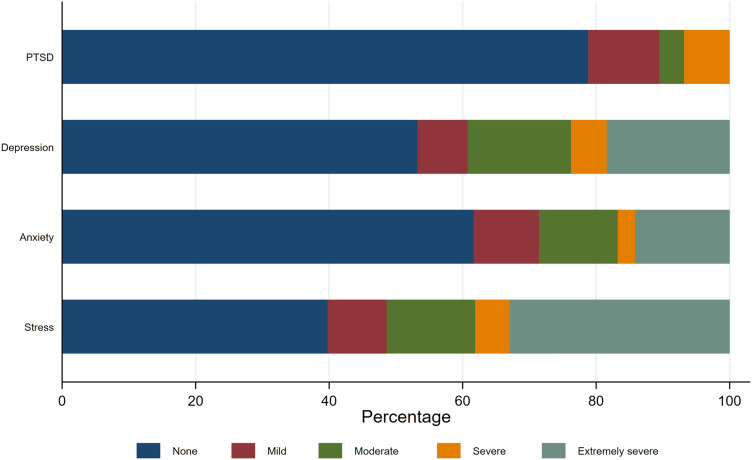
Psychological Outcomes
The prevalence of PTSD among participants in this study was 21.2%. Most of the participants with PTSD were at a mild level. The prevalence of depression, anxiety and stress was 46.8%, 38.3% and 60.2; respectively. Most participants with depression, anxiety and stress were at moderate to extremely severe level (Figure 3 and S1 Table). In the SEM model, all components of PTSD and psychological disturbances contributed to the latent constructs. The standardized covariance between PTSD and other psychological disturbances was 0.86, suggesting that PTSD and other psychological disturbances coexisted in many participants (S2 Figure).
Figure 3.
Psychological outcomes among study participants (n = 543). The classification of severity for PTSD using IES-R does not have the “extremely severe” category.
Factors Associated with PTSD Among Participants
In univariate analysis, younger (<40 years) participants, males, and physicians had higher prevalence of moderate/severe PTSD; the differences were not statistically significant. Higher prevalence of severe PTSD was also observed among those who had a history of mental illness, worked at COVID-19 hospital for >8 weeks, had poor preparedness, worked in a condition with poor resources, and had more concerns. Higher fear of COVID-19 scores were observed in participants with moderate/severe PTSD (Table 3).
Table 3.
Univariate Analysis of Factors Associated with PTSD Among the Study Participants (n = 543)
| Variables | Normal | Mild distress | Moderate distress | Severe distress | Total | p-value |
|---|---|---|---|---|---|---|
| Age ≥ 40, n (%) | 61 (81.3) | 9 (12.0) | 3 (4.0) | 2 (2.7) | 75 (100.0) | 0.49 |
| Gender female, n (%) | 215 (80.5) | 29 (10.9) | 8 (3.0) | 15 (5.6) | 267 (100.0) | 0.58 |
| Specialty, n (%) | ||||||
| Physician | 199 (79.0) | 21 (8.3) | 9 (3.6) | 23 (9.1) | 252 (100.0) | 0.27 |
| Nurse | 161 (77.0) | 29 (13.9) | 8 (3.8) | 11 (5.3) | 209 (100.0) | |
| Other | 68 (82.9) | 8 (9.8) | 3 (3.7) | 3 (3.7) | 82 (100.0) | |
| Having a history of mental illness, n (%) | 34 (50.7) | 9 (13.4) | 8 (11.9) | 16 (23.9) | 67 (100.0) | 0.00 |
| Working at ED/ICU at Covid-19 hospital, n (%) | 236 (78.9) | 26 (8.7) | 14 (4.7) | 23 (7.7) | 299 (100.0) | 0.17 |
| Working at Covid-19 hospital for >8 weeks, n (%) | 95 (69.9) | 18 (13.2) | 8 (5.9) | 15 (11.0) | 136 (100.0) | 0.02 |
| Preparedness, n (%) | ||||||
| Bad | 64 (61.0) | 17 (16.2) | 7 (6.7) | 17 (16.2) | 105 (100.0) | 0.00 |
| Good | 364 (83.1) | 41 (9.4) | 13 (3.0) | 20 (4.6) | 438 (100.0) | |
| Working condition, class, n (%) | ||||||
| Poor resources | 93 (65.5) | 20 (14.1) | 7 (4.9) | 22 (15.5) | 142 (100.0) | 0.00 |
| Good facility, Poor human resources | 213 (79.5) | 32 (11.9) | 9 (3.4) | 14 (5.2) | 268 (100.0) | |
| Good resources | 122 (91.7) | 6 (4.5) | 4 (3.0) | 1 (0.8) | 133 (100.0) | |
| Number of concerns, n (%) | ||||||
| 0 | 75 (93.8) | 3 (3.8) | 2 (2.5) | 0 (0.0) | 80 (100.0) | 0.00 |
| 1 | 66 (91.7) | 6 (8.3) | 0 (0.0) | 0 (0.0) | 72 (100.0) | |
| 2 | 70 (86.4) | 4 (4.9) | 2 (2.5) | 5 (6.2) | 81 (100.0) | |
| 3 | 76 (78.4) | 9 (9.3) | 7 (7.2) | 5 (5.2) | 97 (100.0) | |
| 4 | 77 (73.3) | 14 (13.3) | 4 (3.8) | 10 (9.5) | 105 (100.0) | |
| 5 | 64 (59.3) | 22 (20.4) | 5 (4.6) | 17 (15.7) | 108 (100.0) | |
| Total FOC score, median (Q1-Q3) | 9.0 (5.0; 14.0) | 13.5 (9.0; 15.3) | 15.5 (10.0; 20.8) | 16.0 (9.0; 21.0) | 10.0 (5.0; 15.0) | 0.00 |
Abbreviations: Q, quartile; ICU, Intensive care unit; ED, Emergency department; COVID, Corona virus disease; FOC, fear of COVID.
Variables in bold are statistically significant.
In the ordinal logistic regression analysis, history of mental illness, poor preparedness, working in a condition with poor resources, more concerns, and greater fear of COVID-19 were independent factors associated with higher severity of PTSD (Table 4).
Table 4.
Univariate and Multivariable Analysis of Factors Associated with PTSD Among the Study Participants. (n = 543)
| Variables | Odds ratio | 95% CI | p-value |
|---|---|---|---|
| Age ≥40 years | 0.750 | (0.376, 1.496) | 0.413 |
| Female | 0.732 | (0.457, 1.173) | 0.195 |
| Specialty (reference: Physician) | |||
| Nurse | 1.068 | (0.643, 1.775) | 0.799 |
| Other | 0.653 | (0.319, 1.338) | 0.244 |
| Having a history of mental illness | 4.063 | (2.325, 7.102) | 0.000 |
| Working at COVID-19 hospital for >8 weeks | 1.293 | (0.779, 2.147) | 0.321 |
| Poor preparedness | 1.927 | (1.154, 3.216) | 0.012 |
| Work condition (reference: Good resources) | |||
| Poor resources | 3.042 | (1.420, 6.519) | 0.004 |
| Good facility, Poor human resources | 1.785 | (0.860, 3.707) | 0.120 |
| Number of concerns | 1.281 | (1.086, 1.512) | 0.003 |
| Total FOC score | 1.084 | (1.037, 1.132) | 0.000 |
Note: Variables in bold are statistically significant.
Abbreviations: COVID, Corona virus disease; FOC, fear of COVID; CI, confidence interval.
Discussion
In this study, we examined the prevalence of PTSD symptoms and its associated factors among HCWs working at the field hospitals during the fourth wave of the COVID-19 pandemic in Vietnam. The observed prevalence of PTSD (21.2%) was lower than previously reported (29–76.4%),25–30 probably because our study was conducted during the fourth wave, which was nearly two years since the first outbreak in Vietnam, while other studies were carried out during the early phase of the pandemic. Over these two years, there have been long-term adaptive reactions of the Vietnamese health system in general, and frontline HCWs in particular, to the fight against COVID-19. Particularly, part of the healthcare workforce had participated in the fight since the first wave; therefore, by the fourth wave, they had had much experience in working at field hospitals. Also, some western nations may have a higher risk of PTSD due to high aspirations for a risk-free existence and strong attention to negative mental health impacts resulting from significant life events.31
In our study, poor preparedness was associated with more severe PTSD. Insufficient preparation has been associated with negative psychological consequences among HCWs during previous epidemics of Ebola.32 According to a national cross-sectional study of general public in China during the COVID-19 outbreak, factors regarding preparation (eg, having good preventative and control measures and a highly efficient health system) were reported to be protective factors against psychological disturbances.33 A cross-sectional study among 823 healthcare professionals in Ghana found that those who were “somewhat prepared” and “prepared” experienced less stress and burnout.34 Inadequate preparedness could contribute to HCW stress and burnout—two psychological indicators that reached crisis levels among HCWs globally even before the COVID-19 pandemic.35,36 Without appropriate interventions, stress and burn out could result in lower productivity and effectiveness, decreased job satisfaction and commitment, and poor quality care, which consequently risk the patient’s safety.37,38
HCWs in this study reported a number of concerns about COVID-19 and a high degree of COVID-19 fear. They were worried about getting infected with COVID-19, spreading COVID-19 to the people they live with, financial problems, losing connection with their family and loved ones, and the feeling of overwhelmed at work. These negative feelings were similar to the findings in previous reports39,40 and have been also widely reported in past epidemics such as HIV and SARS.41,42 We also found that having more concerns and having higher degree of fear were independently associated with more severe PTSD. Of notes, fear of COVID-19 is not only a factor associated with PTSD but also other psychological disturbances.34,43 Understanding the psychological impact of having to deal with COVID-19, policymakers and health authorities need to develop targeted interventions such as developing explicit and up-to-date infection control standards and protocols, providing adequate supplies and training on personal protective equipment, and developing innovative solutions to mental care for HCWs.
Our findings suggest the relationships between past mental history, current PTSD, and other psychological disturbances. HCWs with preexisting mental illnesses have been reported to have higher risks of mental health outcomes such as anxiety, depression and burnout.26,44–47 A variety of risk factors make people with mental illnesses susceptible to negative health impacts, including poor physical health, low levels of physical activity, and higher degrees of smoking, drinking, drug abuse, social, and economic hardship.48,49 In the setting of isolated COVID hospitals, the situation worsen as they faced many other pressures such as work overload, isolation, being unable to connect with friends and loved ones, and having to witness death. This suggests that a comprehensive strategy is required to deal with the mental health problems in frontline HCWs, including careful screening before recruiting to the field hospitals, regular monitoring for multiple psychiatric conditions, and in-place plans for switching HCWs between units to provide those with mental issues with proper management and adequate recovery.
This is one of the few studies that had examined the presence of PTSD among Vietnamese HCWs who worked at the field COVID-19 hospitals. The survey was conducted at multiple field hospitals during the heightening period of the COVID-19 wave, enabling us to provide an accurate picture of the prevalent mental health problems among these frontline HCWs. There are some limitations in this study. First, since the participants were not randomly sampled, there might be threats to generalizability, especially when those with severe psychological disturbances might refuse to answer the survey. However, the findings in this study were already very alarming, and our messages are not likely to change. Second, because the study was cross-sectional, we did not make any causal inferences about the relationship between PTSD and other risk factors. Nonetheless, our findings can be used to plan for future pandemics. Third, data were collected via an online form without direct support of a study member. This may result in heterogeneity in the understanding of questions among responders. However, since the study was done at COVID-19 field hospitals, it was impossible for the study teams to enter or travel across the hospitals to interview the HCWs. Also, the psychometric scales used in this study can be used for self-reporting,11,50 thus improving the validity of the responses.
In summary, a study on Vietnamese HCWs who worked at the field COVID-19 hospitals revealed alarmingly high prevalence of PTSD and other psychological disturbances among these HCWs. The factors associated with PTSD reported in this study can be useful for policymakers and health authorities in the preparation for future pandemics.
Disclosure
The authors have declared that no competing interests exist.
References
- 1.Tran TPT, Le TH, Nguyen TNP, Hoang VM. Rapid response to the COVID-19 pandemic: Vietnam government’s experience and preliminary success. J Glob Health. 2020;10(2):020502. doi: 10.7189/jogh.10.020502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Minh LHN, Khoi Quan N, Le TN, Khanh PNQ, Huy NT. COVID-19 timeline of Vietnam: important milestones through four waves of the pandemic and lesson learned. Front Public Health. 2021;9:709067. doi: 10.3389/fpubh.2021.709067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Coronavirus disease (COVID-19) dashboard with vaccination data. Vietnam: World Health Organization. [Google Scholar]
- 4.Vietnam Ministry of Health. Summary of Reports on Healthcare Workers Deployed to Support in the South’s Fight Against Epidemics. Leaders of the ministry’s activities Ministry of Health website; 2021. [Google Scholar]
- 5.Koontalay A, Suksatan W, Prabsangob K, Sadang JM. Healthcare workers’ burdens during the COVID-19 pandemic: a qualitative systematic review. J Multidiscip Healthc. 2021;14:3015–3025. doi: 10.2147/JMDH.S330041 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu KK, Chan SK, Ma TM. Posttraumatic stress after SARS. Emerg Infect Dis. 2005;11(8):1297–1300. doi: 10.3201/eid1108.041083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Saragih ID, Tonapa SI, Saragih IS, et al. Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: a systematic review and meta-analysis. Int J Nurs Stud. 2021;121:104002. doi: 10.1016/j.ijnurstu.2021.104002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nguyen TT, Le XTT, Nguyen NTT, et al. Psychosocial impacts of COVID-19 on healthcare workers during the nationwide partial lockdown in Vietnam in April 2020. Front Psychiatry. 2021;12:562337. doi: 10.3389/fpsyt.2021.562337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nguyen HT, Do BN, Pham KM, et al. Fear of COVID-19 scale-associations of its scores with health literacy and health-related behaviors among medical students. Int J Environ Res Public Health. 2020;17(11):4164. doi: 10.3390/ijerph17114164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nguyen MH, Pham TTM, Nguyen KT, et al. Negative impact of fear of COVID-19 on health-related quality of life was modified by health literacy, eHealth literacy, and digital healthy diet literacy: a multi-hospital survey. Int J Environ Res Public Health. 2021;18(9):4929. doi: 10.3390/ijerph18094929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med. 1979;41(3):209–218. doi: 10.1097/00006842-197905000-00004 [DOI] [PubMed] [Google Scholar]
- 12.Asukai N, Kato H, Kawamura N, et al. Reliability and validity of the Japanese-language version of the impact of event scale-revised (IES-R-J): four studies of different traumatic events. J Nerv Ment Dis. 2002;190(3):175–182. doi: 10.1097/00005053-200203000-00006 [DOI] [PubMed] [Google Scholar]
- 13.Creamer M, Bell R, Failla S. Psychometric properties of the impact of event scale - revised. Behav Res Ther. 2003;41(12):1489–1496. doi: 10.1016/j.brat.2003.07.010 [DOI] [PubMed] [Google Scholar]
- 14.Kawamura N, Kim Y, Asukai N. Suppression of cellular immunity in men with a past history of posttraumatic stress disorder. Am J Psychiatry. 2001;158(3):484–486. doi: 10.1176/appi.ajp.158.3.484 [DOI] [PubMed] [Google Scholar]
- 15.Hyer K, Brown LM. The impact of event scale--revised: a quick measure of a patient’s response to trauma. Am J Nurs. 2008;108(11):60–68. doi: 10.1097/01.NAJ.0000339101.39986.85 [DOI] [PubMed] [Google Scholar]
- 16.Sharif Nia H, Kaur H, Fomani FK, et al. Psychometric properties of the impact of Events Scale-Revised (IES-R) among general Iranian population during the COVID-19 pandemic. Front Psychiatry. 2021;12:692498. doi: 10.3389/fpsyt.2021.692498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chen CS, Cheng CP, Yen CF, et al. Validation of the impact of event scale-revised for adolescents experiencing the floods and mudslides. Kaohsiung J Med Sci. 2011;27(12):560–565. doi: 10.1016/j.kjms.2011.06.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Silva-Costa A, Griep RH, Rotenberg L. [Perceived risk from COVID-19 and depression, anxiety, and stress among workers in healthcare units]. Cad Saude Publica. 2022;38(3):e00198321. Portuguese. doi: 10.1590/0102-311x00198321 [DOI] [PubMed] [Google Scholar]
- 19.Marijanović I, Kraljević M, Buhovac T, et al. Use of the Depression, Anxiety and Stress Scale (DASS-21) questionnaire to assess levels of depression, anxiety, and stress in healthcare and administrative staff in 5 oncology institutions in Bosnia and Herzegovina during the 2020 COVID-19 pandemic. Med Sci Monit. 2021;27:e930812. doi: 10.12659/MSM.930812 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lovibond PF, Lovibond SH. The structure of negative emotional states: comparison of the Depression Anxiety Stress Scales (DASS) with the beck depression and anxiety inventories. Behav Res Ther. 1995;33(3):335–343. doi: 10.1016/0005-7967(94)00075-U [DOI] [PubMed] [Google Scholar]
- 21.Moya E, Larson LM, Stewart RC, Fisher J, Mwangi MN, Phiri KS. Reliability and validity of depression anxiety stress scale (DASS)-21 in screening for common mental disorders among postpartum women in Malawi. BMC Psychiatry. 2022;22(1):352. doi: 10.1186/s12888-022-03994-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Le MTH, Tran TD, Holton S, Nguyen HT, Wolfe R, Fisher J. Reliability, convergent validity and factor structure of the DASS-21 in a sample of Vietnamese adolescents. PLoS One. 2017;12(7):e0180557. doi: 10.1371/journal.pone.0180557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Thiyagarajan A, James TG, Marzo RR. Replication data for: psychometric properties of the 21-item Depression, Anxiety, and Stress Scale (DASS-21) among Malaysians during COVID-19: a methodological study. Humanit Soc Sci Commun. 2022;9(1):1–8. doi: 10.1057/s41599-022-01229-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Lan HTQ, Long NT, Hanh NV. Validation of depression, anxiety and stress scales (DASS-21): immediate psychological responses of students in the e-learning environment. IJHE. 2020;9(5):125. doi: 10.5430/ijhe.v9n5p125 [DOI] [Google Scholar]
- 25.Şahin MK, Aker S, Şahin G, Karabekiroğlu A. Prevalence of depression, anxiety, distress and insomnia and related factors in healthcare workers during COVID-19 pandemic in Turkey. J Community Health. 2020;45(6):1168–1177. doi: 10.1007/s10900-020-00921-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dobson H, Malpas CB, Burrell AJ, et al. Burnout and psychological distress amongst Australian healthcare workers during the COVID-19 pandemic. Australas Psychiatry. 2021;29(1):26–30. doi: 10.1177/1039856220965045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Di Tella M, Romeo A, Benfante A, Castelli L. Mental health of healthcare workers during the COVID-19 pandemic in Italy. J Eval Clin Pract. 2020;26(6):1583–1587. doi: 10.1111/jep.13444 [DOI] [PubMed] [Google Scholar]
- 28.Johnson SU, Ebrahimi OV, Hoffart A. PTSD symptoms among health workers and public service providers during the COVID-19 outbreak. PLoS One. 2020;15(10):e0241032. doi: 10.1371/journal.pone.0241032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Riello M, Purgato M, Bove C, MacTaggart D, Rusconi E. Prevalence of post-traumatic symptomatology and anxiety among residential nursing and care home workers following the first COVID-19 outbreak in Northern Italy. R Soc Open Sci. 2020;7(9):200880. doi: 10.1098/rsos.200880 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rossi R, Socci V, Pacitti F, et al. Mental health outcomes among frontline and second-line health care workers during the coronavirus disease 2019 (COVID-19) pandemic in Italy. JAMA Netw Open. 2020;3(5):e2010185. doi: 10.1001/jamanetworkopen.2020.10185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Heir T, Bonsaksen T, Grimholt T, et al. Serious life events and post-traumatic stress disorder in the Norwegian population. BJ Psych Open. 2019;5(5):e82. doi: 10.1192/bjo.2019.62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Belfroid E, van Steenbergen J, Timen A, Ellerbroek P, Huis A, Hulscher M. Preparedness and the importance of meeting the needs of healthcare workers: a qualitative study on Ebola. J Hosp Infect. 2018;98(2):212–218. doi: 10.1016/j.jhin.2017.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatr. 2020;33(2):e100213. doi: 10.1136/gpsych-2020-100213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Afulani PA, Gyamerah AO, Nutor JJ, et al. Inadequate preparedness for response to COVID-19 is associated with stress and burnout among healthcare workers in Ghana. PLoS One. 2021;16(4):e0250294. doi: 10.1371/journal.pone.0250294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.The Lancet null. Physician burnout: a global crisis. Lancet. 2019;394(10193):93. doi: 10.1016/S0140-6736(19)31573-9 [DOI] [PubMed] [Google Scholar]
- 36.Kopacz MS, Ames D, Koenig HG. It’s time to talk about physician burnout and moral injury. Lancet Psychiatry. 2019;6(11):e28. doi: 10.1016/S2215-0366(19)30385-2 [DOI] [PubMed] [Google Scholar]
- 37.Klein J, Grosse Frie K, Blum K, von Dem Knesebeck O. Burnout and perceived quality of care among German clinicians in surgery. Int J Qual Health Care. 2010;22(6):525–530. doi: 10.1093/intqhc/mzq056 [DOI] [PubMed] [Google Scholar]
- 38.Maslach C, Leiter MP. Understanding the burnout experience: recent research and its implications for psychiatry. World Psychiatry. 2016;15(2):103–111. doi: 10.1002/wps.20311 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sahashi Y, Endo H, Sugimoto T, et al. Worries and concerns among healthcare workers during the coronavirus 2019 pandemic: a web-based cross-sectional survey. Humanit Soc Sci Commun. 2021;8(1):41. doi: 10.1057/s41599-021-00716-x [DOI] [Google Scholar]
- 40.Bayazit H, Ozel M, Arac S, Dulgeroglu-Bayazit D, Joshi A. Posttraumatic stress disorder among health care workers during the COVID-19 pandemic. J Psychiatr Pract. 2022;28(5):354–361. doi: 10.1097/PRA.0000000000000661 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ho SMY, Kwong-Lo RSY, Mak CWY, Wong JS. Fear of severe acute respiratory syndrome (SARS) among health care workers. J Consult Clin Psychol. 2005;73(2):344–349. doi: 10.1037/0022-006X.73.2.344 [DOI] [PubMed] [Google Scholar]
- 42.Meisenhelder JB, LaCharite C. Fear of contagion: the public response to AIDS. Image J Nurs Sch. 1989;21(1):7–9. doi: 10.1111/j.1547-5069.1989.tb00089.x [DOI] [PubMed] [Google Scholar]
- 43.De Pasquale C, Conti D, Dinaro C, D’Antoni RA, La Delfa E, Di Nuovo S. The COVID-19 pandemic and posttraumatic stress disorder: emotional impact on healthcare professions. Front Psychiatry. 2022;13:832843. doi: 10.3389/fpsyt.2022.832843 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.D’Ettorre G, Pellicani V, Ceccarelli G. Post-traumatic stress disorder symptoms in healthcare workers: a ten-year systematic review: post-traumatic stress disorder symptoms in healthcare workers. Acta Bio Med. 2020;91(12–S):e2020009. doi: 10.23750/abm.v91i12-S.9459 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wanigasooriya K, Palimar P, Naumann DN, et al. Mental health symptoms in a cohort of hospital healthcare workers following the first peak of the COVID-19 pandemic in the UK. BJ Psych Open. 2021;7(1):e24. doi: 10.1192/bjo.2020.150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lopes Cardozo B, Gotway Crawford C, Eriksson C, et al. Psychological distress, depression, anxiety, and burnout among international humanitarian aid workers: a longitudinal study. PLoS One. 2012;7(9):e44948. doi: 10.1371/journal.pone.0044948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Chinvararak C, Kerdcharoen N, Pruttithavorn W, et al. Mental health among healthcare workers during COVID-19 pandemic in Thailand. PLoS One. 2022;17(5):e0268704. doi: 10.1371/journal.pone.0268704 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rodgers M, Dalton J, Harden M, Street A, Parker G, Eastwood A. Integrated care to address the physical health needs of people with severe mental illness: a mapping review of the recent evidence on barriers, facilitators and evaluations. Int J Integr Care. 2018;18(1):9. doi: 10.5334/ijic.2605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hert DE, Correll CU, Bobes J, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry. 2011;10(1):52–77. doi: 10.1002/j.2051-5545.2011.tb00014.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gloster AT, Rhoades HM, Novy D, et al. Psychometric properties of the Depression Anxiety and Stress Scale-21 in older primary care patients. J Affect Disord. 2008;110(3):248–259. doi: 10.1016/j.jad.2008.01.023 [DOI] [PMC free article] [PubMed] [Google Scholar]