Abstract
Background
Cardiovascular diseases contribute to considerable morbidity and mortality in the USA. We sought to establish regional disparities across the nation contributing to cardiovascular disease (CVD) among non-elective young adult hospitalizations.
Methods
The National Inpatient Sample (2019) was utilized to identify the incidence of non-elective hospitalizations among young adults (18–44 yrs) and analyze the burden of CVD risk factors and outcomes (MACCE; all-cause mortality, AMI, cardiac arrest and stroke) in different US regions.
Results
A total of 5,833,930 (median age 32 [26–37] years) non-elective admissions were recorded; plurality from the south (39.6%). Most admissions were white (51.4%) and female (65.5%) amid all regions. The burden of CVD risk factors was significantly higher in the South followed by the Mid-west regions. The South had the highest and the Northeast had the lowest rates of MACE (2.9% vs 2.3%) and stroke (1.0% vs 0.8%). The risk of AMI was high for the south and Midwest regions (1.1%). All-cause mortality was highest in South and West regions (0.7%). Multivariate adjusted odds for these cardiovascular events were higher in the West (aOR 1.22; 95%CI 1.12–1.33) followed by South (aOR 1.16; 95%CI 1.07–1.26) regions.
Conclusions
This population-based study assessing non-elective admissions in the young revealed a higher burden of CVD risk factors and rate of MACCE in the South compared to other areas of the USA. Regional policies should be tailored to the local CVD risk burden.
Keywords: Regional disparities, Young adults, Non-elective/emergency, Cardiovascular disease, Major adverse cardiac and cerebrovascular events
1. Introduction
Despite improving cardiovascular disease (CVD) burden and mortality in all the geographical regions of the United States, there is a growing concern regarding the widening geographical disparity over time. Certain regions, particularly those in the South, are lagging in mortality reduction. The geographical disparity in CVD mortality is thought to be related to inequalities in behavioral risk factors and socioeconomic conditions. In addition, the health disparities extend beyond geography and include ethnicity, race, and socioeconomic status. The overall cost of these combined disparities in the US has been estimated at 1.24 trillion U.S. Dollars annually. Consequently, the reduction of health inequalities including those between geographical areas has been a major health policy goal in the United States for at least the past four decades.1,2
Cardiovascular diseases continue to be the leading cause of death in the US.3 However, analyses regarding the geographical disparities of CVD events and mortality have been few.1 The documentation of the regional disparities, with the highest and lowest CVD rates, can provide information regarding the extent to which cardiovascular event and mortality reduction can be achieved.4 Additionally, a spatial–temporal analysis of cardiovascular mortality would help to identify geographical areas with high rates of CVD mortality and lower rates of mortality reduction.5 This identifies the regions with an urgent need for action. Herein, we aim to establish regional disparities across the USA contributing to CVD (Cardiovascular events) among young adults during non-elective hospitalizations.
2. Methods
We retrospectively identified all non-elective admissions among young patients (aged 18–44 years) using the National Inpatient Sample dataset from 2019. The NIS database provides a nationwide assessment of over 35 million hospitalizations annually covering 97% of the US population. We assessed the burden of CVD risk factors and in-hospital outcomes in different geographical locations in the USA. We used previously validated and relevant ICD-10 diagnostic codes for MACCE (major adverse cardiovascular and cerebrovascular events). Demographics such as sex, race/ethnicity, the full list of comorbidities as well as patient location and teaching-hospital status were collected. This study was exempt from the Institutional Review Board approval in light of the de-identified database.
The primary outcomes/endpoints were rates of MACCE (all-cause mortality, acute myocardial infarction, cardiac arrest, and stroke). The secondary end-points were the adjusted odds ratio for cardiovascular events by region using multivariable regression models controlled for relevant demographics, hospital-level characteristics, comorbidities, and prior history of cardiovascular events or procedures. We utilized weighted data and complex survey modules with IBM SPSS Statistics version 25.0 (IBM Corp., Armonk, NY, USA) for all analyses. We used Pearson chi-square test for categorical measures and the Mann–Whitney U test for continuous variables. A p-value of <0.05 was considered the threshold for statistical significance.
3. Results
A total of 5,833,930 non-elective admissions are recorded with a median age of 32 (26–37 years). There was a plurality from the South with 39.6%, followed by the West and Midwest with 22.5% % and 20.6% of admissions respectively, and the smallest proportion from the Northeast at 17.2%. Most admissions were among whites (65.5%), and females (65.5%) amid all regions [Table 1]. Smaller percentages were black, Hispanic and Native American. The Midwest appeared to be the least racially diverse. The most racially diverse region was the South, 48.9% being white (28.4%) black and (16.6%) Hispanic. The West was the other region where the whites occupied a plurality of 42.9%, however, less diverse than the South, as the only other significant ethnic group was Hispanics at 34.1%. In the Midwest and the Northeast, there were a majority of whites.
Table 1.
Baseline characteristics, comorbidities and outcomes in non-elective admissions among young adults from different regions.
| REGION OF HOSPITALS | NORTHEAST | MIDWEST | SOUTH | WEST | TOTAL |
|---|---|---|---|---|---|
| No. of admissions (%) | 1005757(17.2%) | 1201864(20.6%) | 2312009(39.6%) | 1314300(22.5%) | 5833930(100%) |
|
| |||||
| Age (years) at admission, median [IQR] | 32[26–37] | 31[26–37] | 32[26–37] | 31[26–37] | 32[26–37] |
|
| |||||
| Sex | |||||
|
| |||||
| Male | 36.5% | 35.7% | 34.3% | 32.4% | 34.5% |
| Female | 63.5% | 64.3% | 65.7% | 67.6% | 65.5% |
|
| |||||
| Race | |||||
|
| |||||
| White | 52.4% | 65.7% | 48.9% | 42.5% | 65.5% |
| Black | 19.5% | 21.9% | 28.4% | 9.0% | 51.4% |
| Hispanic | 17.0% | 7.0% | 16.6% | 34.1% | 21.2% |
| Asian or Pacific Islander | 4.0% | 2.1% | 1.9% | 8.2% | 18.7% |
| Native American | 0.2% | 1.1% | 0.5% | 2.3% | 3.7% |
| Others | 6.8% | 2.1% | 3.7% | 4.0% | 1.0% |
|
| |||||
| Primary expected payer | |||||
|
| |||||
| Medicare | 7.7% | 8.7% | 8.0% | 5.1% | 7.4% |
| Medicaid | 43.2% | 39.3% | 34.5% | 48.5% | 40.2% |
| Private including HMO | 41.0% | 40.3% | 35.5% | 38.1% | 38.0% |
| Self Pay | 4.8% | 7.8% | 16.2% | 4.4% | 9.8% |
| No charges | 0.1% | 0.5% | 1.6% | 0.2% | 0.8% |
| Others | 3.2% | 3.5% | 4.1% | 3.7% | 3.7% |
|
| |||||
| Location/teaching hospital status | |||||
|
| |||||
| Rural | 3.8% | 10.0% | 7.6% | 3.8% | 6.6% |
| Urban non-teaching | 8.4% | 13.0% | 18.6% | 20.5% | 16.1% |
| Urban teaching | 87.8% | 77.0% | 73.8% | 75.7% | 77.3% |
|
| |||||
| Comorbidities | |||||
|
| |||||
| Hypertension, complicated | 4.1% | 5.6% | 6.6% | 4.8% | 5.6% |
| Hypertension, uncomplicated | 10.5% | 13.0% | 13.7% | 9.3% | 12.0% |
| Diabetes, complicated | 4.8% | 6.4% | 7.0% | 5.5% | 6.1% |
| Diabetes, uncomplicated | 4.8% | 4.8% | 5.0% | 5.1% | 4.9% |
| Hyperlipidemia | 5.5% | 6.8% | 6.4% | 5.0% | 6.0% |
| Tobacco use disorder | 22.9% | 29.8% | 23.8% | 17.2% | 23.4% |
| Peripheral Vascular Disease | 0.9% | 1.1% | 1.0% | 0.9% | 1.0% |
| Drug Abuse | 13.8% | 13.5% | 11.8% | 12.4% | 12.6% |
| Prior MI | 0.6% | 1.0% | 0.9% | 0.6% | 0.8% |
| Prior TIA/Stroke | 0.9% | 1.3% | 1.3% | 0.9% | 1.1% |
|
| |||||
| Outcomes | |||||
|
| |||||
| All cause mortality | 0.6% | 0.6% | 0.7% | 0.7% | 0.6% |
| Acute myocardial infarction | 0.9% | 1.1% | 1.1% | 0.8% | 1.0% |
| Cardiac arrest/VF | 0.4% | 0.5% | 0.5% | 0.4% | 0.5% |
| Stroke | 0.8% | 0.9% | 1.0% | 0.9% | 0.9% |
| MACCE | 2.3% | 2.6% | 2.9% | 2.4% | 2.6% |
|
| |||||
| Disposition | |||||
|
| |||||
| Routine | 82.8% | 86.5% | 87.4% | 87.4% | 86.4% |
| Transfer to short term hospitals | 1.6% | 1.6% | 1.3% | 1.5% | 1.5% |
| Transfer to others, SNF, ICF | 4.5% | 4.7% | 3.5% | 3.8% | 4.0% |
| Home health care (HHC) | 5.9% | 3.4% | 3.6% | 3.2% | 3.9% |
| AMA | 4.6% | 3.1% | 3.4% | 3.4% | 3.6% |
|
| |||||
| Adjusted Odds Ratio for MACCE | P values | aOR * | 95%CI | ||
|
| |||||
| South vs Northeast | <0.001 | 1.16 | 1.07–1.26 | ||
| West vs Northeast | <0.001 | 1.22 | 1.12–1.33 | ||
| Midwest vs Northeast | <0.001 | 1.08 | 0.99–1.18 | ||
P<0.005 indicates statistical significance, MACCE= Major Adverse Cardiac and Cerebrovascular EventsIQR=interquartile range, SNF=Skilled nursing facility, ICF=intermediate care facility, CI=confidence interval.
Multivariable analysis were adjusted for patient/sociodemographic characteristics and preexisting cardiovascular and extracardiac comorbidities. Adjusted P <0.001.
Overall, the most common primary expected payer was Medicaid with 40.2% of the admissions being enrollees, followed by private Health maintenance organizations (HMO) at 38% of admissions. This pattern was consistent in each region of the USA where the majority of hospitalized individuals utilized Medicaid or private HMO in near equal distributions. However, overall utilization was reduced in the South where a combined 70% of hospital admissions were enrolled with either Medicaid or private HMO. 86.6% of admissions in the West were enrolled with Medicaid or private HMOs, the highest such percentage in this regional analysis.
The burden of CVD risk factors was significantly higher in the South followed by the Midwest region [Table 1]. The South had the highest percentage of smokers (29.8%) and hypertension (13.7% with uncomplicated hypertension and 6.6% with complicated hypertension). While the South had the highest prevalence of complicated diabetes, the Northeast had the lowest prevalence (7.0% vs 4.8%). The highest prevalence of uncomplicated diabetes was noted in the West (5.1%) followed closely by the South (5.0%). The Midwest demonstrated the highest prevalence of hyperlipidemia (6.8%) whilst the West had the lowest prevalence (5.0%). The Northeast followed by the Midwest had the highest prevalence of drug abuse (13.8% and 13.5% respectively), albeit, the prevalence of drug use among different regions appeared to be a bit more uniform as the South and the West have a prevalence of 11.8% and 12.4% respectively. The Midwest had the highest prevalence of previous MI (1.0%) and previous TIA/Stroke (1.3%), followed by the South (prior MI at 0.9%, prior TIA/Stroke at 1.3%).
The Northeast had the highest percentage of young adult patients presenting to urban-teaching hospitals (87.8%) whereas the South had the lowest (73.8%). Both the Northeast and the West had the lowest percentage of patients presenting to rural hospitals (3.8%), vs the Midwest (10%) which had the highest percentage.
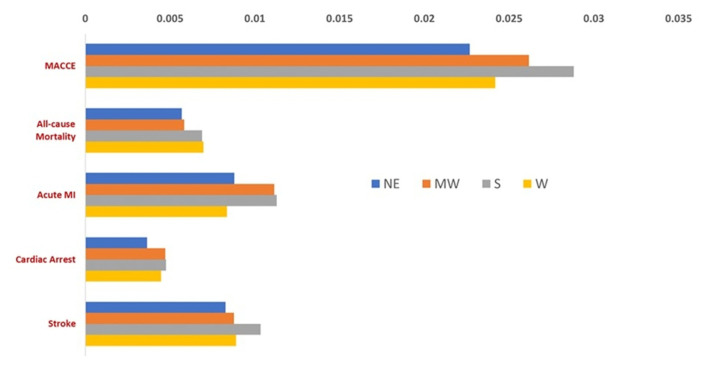
The South had the highest and the Northeast had the lowest rates of MACE (2.9% vs 2.3%) and stroke (1.0% vs 0.8%). The incidence of acute myocardial infarction was high for the South and Midwest regions at 1.1%. All-cause mortality was highest among South and West regions (0.7%) [See Fig. 1]. When non-elective young adult admissions were adjusted for confounders, both the South and the West had higher odds of MACCE compared to the Northeast; South vs Northeast (aOR1.16, 95%CI 1.07–1.26, p < 0.001), West vs. Northeast (aOR 1.22, 95%CI 1.12–1.33, p < 0.001) regardless of primary cause of hospitalizations [Table 1].
Figure 1.
Nationwide frequency of adverse cardiovascular events in young non-elective hospitalizations, 2019.
4. Discussion
This study demonstrates the South as the most racially diverse region with the highest prevalence of cardiovascular risk factors and the highest incidence of MACCE in non-electively hospitalized young adults. The Midwest had the highest prevalence of tobacco consumption and prior histories of MI, TIA and stroke. After adjusting for covariates, young adult non-elective admissions in the West followed by the South had the highest odds of MACCE when compared to the Northeast.
Between 1969 and 2011, CVD mortality rates have declined at a faster pace in the Northeast as compared to the Southern regions. Nonetheless, regional disparities were evident even in 1969, as the mortality rate was 9% higher in the Southeast than in New England, but notably, this difference increased such that the difference in the mortality rate between these two areas was 22% in 1990 and 48% in 2011. Over that period, there was an increase in the relative risk of cardiovascular mortality for the Southern regions in comparison to New England and mountainous regions, even after adjusting for covariates. In 2011, the Southeastern states such as Alabama or Mississippi had the highest cardiovascular mortality rates. Thus, the absolute disparities in the State level CVD mortality as measured by the interquartile range and absolute mean deviation decreased over time, but the relative disparities in State level CVD mortality have widened.1
Whilst the present study did not demonstrate trends in Cardiovascular mortality or Cardiovascular risk factors and outcomes, the results from the National inpatient sample in 2019 are concordant with the above trends where non-elective young adult admissions from the South have maintained the highest incidence of adverse outcomes and all-cause mortality on the background of the highest prevalence of Cardiovascular risk factors.
The causes for regional disparities could be related to relative area deprivation, established cardiovascular risk factors such as smoking, high Body mass index, sedentary lifestyle, glucose intolerance/diabetes prevalence, urban lifestyle, racial/ethnic composition and lack of access to primary medical care and health insurance, and can account for more than 50% of variance by county as shown previously. Singh et al., illustrated that CVD mortality rates were 18% higher in counties with high smoking rates (>36%) when compared to areas with less smoking (<12%). Counties with obesity rates of more than 40% had 54% higher CVD mortality and counties with a diabetes prevalence >14% had a 19% higher CVD mortality. Furthermore, persons in the most deprived counties had 15% higher CVD mortality than those in the most affluent counties.1 From the foregoing, it is evident that behavioral risk factors account for the vast majority of cardiovascular events and deaths.6 The geographical disparities of cardiovascular deaths may be understood in the context of the geographical distribution of these cardiovascular risk factors. This present study highlights the significance of the geographical distribution of cardiovascular risk factors such as smoking, obesity, hypertension, and diabetes that helps explain the regional disparities of CVD events and mortality.
Our study demonstrated that the South, the region with the highest incidence of major adverse cardiovascular and cerebrovascular events had the lowest rates of Medicaid enrollment and utilization of private HMOs. This region also had the highest rates of self-pay of all regions. Interestingly, our study also revealed that the South had the lowest percentage of Urban teaching hospitals listed as designated sites of healthcare delivery. Thus, both the factors including primary expected payer and teaching-hospital status could explain the high incidence of MACCE in the South.
The relative increase in cardiovascular risk factors in the South7 leads to an examination of the relative racial diversity that could be found in this region. From our study, the South had the highest percentage of African Americans. Graham et al., in an examination of the disparities of CVD risk in the United States, examined the CVD risk in African American communities.2 There was a disproportionate rate of cardiovascular disease in the US African-American population; with the subgroup having a higher burden of myocardial infarction, heart failure, stroke and other cardiovascular events.8 Further, on a population level, there was a higher overall prevalence of risk factors that go unrecognized and untreated with a higher likelihood of adverse outcomes and potentially higher morbidity and mortality.9 For instance, African-Americans have the highest rates of hypertension in the world.10 Among various minority population groups; African-American men have the highest overall death rate from cardiovascular disease and African-American women have higher overall deaths related to cardiovascular disease than white women.11,12 Deaths occur much earlier in African-American individuals than their white counterparts and even after consideration of modifiable health behaviors, racial and ethnic differences stood as the underlying reason for these disparities.13,14 Moreover, this group is less likely to receive treatment and less likely to achieve control of Cardiovascular risk factors.15 This helps us to understand that the geographical distribution of certain racial and ethnic groups with possible underlying genetic predisposition and cardiovascular risk factors may itself be an explanation for geographical variation or regional disparities in cardiovascular events in young adult (18–44 yrs) non-elective admissions in the United States.
This study derives its data from the national inpatient sample database therefore, it is anticipated it would be truly reflective of current epidemiological patterns. This database is also sponsored by the Healthcare Cost and Utilization project and maintained by the Agency for Healthcare Research and Quality making it a well-trusted and reliable source. Despite establishing current regional healthcare disparities, this study did not establish the yearly trend over the last 10 years. Therefore, we are not able to determine whether there have been any changes to the yearly trends as determined by Singh et al. This information would be informative in the establishment of public health strategies to address the current disparities that exist. This study also didn’t include data regarding cardiovascular mortality which excludes the possibility of comparisons with other studies which take into account the trends in Cardiovascular mortality. The primary discharge diagnosis was not considered and there was no long-term follow-up. There were no lab parameters or medication data included. The causative role in non-elective admissions and MACCE could not be established and the variation in triage and hospital transfer policies on outcomes could not be evaluated. More prospective studies are warranted to track and follow outcomes in emergent young adult admissions.
5. Conclusions
The regional disparity in the distribution of cardiovascular risk factors and adverse cardiovascular outcomes have a complete etiological basis which is still actively investigated. This study demonstrates that the South has the highest rates of cardiovascular risk factors and adverse cardiovascular events in non-elective young adult admissions aged 18–44 yrs as compared to the Northeast. The results of this investigation may yield vital information in the reduction of underlying health inequality and complex behavior which may put individuals in certain regions at risk over others, and the possibility of eliminating the relative risk that may be conferred by race/ethnicity.
Acknowledgment
None.
Footnotes
Conflict of interest
None.
Disclosure
None.
Funding source
None
References
- 1. Singh G. Widening geographical disparities in cardiovascular disease mortality in the United States, 1969–2011. Int J MCH AIDS. 2014;3(2) [PMC free article] [PubMed] [Google Scholar]
- 2. Graham G. Disparities in cardiovascular disease risk in the United States. Curr Cardiol Rev. 2015;11(3):238–245. doi: 10.2174/1573403X11666141122220003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hoyert DL. 75 years of mortality in the United States, 1935–2010. NCHS Data Brief. 2012;(88):1–8. [PubMed] [Google Scholar]
- 4. Singh GK, Kogan MD, van Dyck PC. A multilevel analysis of state and regional disparities in childhood and adolescent obesity in the United States. J Community Health. 2008;33(2):90–102. doi: 10.1007/s10900-007-9071-7. [DOI] [PubMed] [Google Scholar]
- 5. Gillum RF, Mehari A, Curry B, Obisesan TO. Racial and geographic variation in coronary heart disease mortality trends. BMC Publ Health. 2012;12:410. doi: 10.1186/1471-2458-12-410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Mendis S, Puska P, Norrving B. World Health Organization. World heart federation, world stroke organization. Global atlas on cardiovascular disease prevention and control. World health organization in collaboration with the world heart federation and the world stroke organization. 2011 [Google Scholar]
- 7. Blackwell DL, Lucas JW, Clarke TC. Summary health statistics for U.S. adults: national health interview survey, 2012. Vital Health Stat. 2014;10(260):1–161. [PubMed] [Google Scholar]
- 8. Bonow RO, Grant AO, Jacobs AK. The cardiovascular state of the union: confronting healthcare disparities. Circulation. 2005;111(10):1205–1207. doi: 10.1161/01.CIR.0000160705.97642.92. [DOI] [PubMed] [Google Scholar]
- 9. Kurian AK, Cardarelli KM. Racial and ethnic differences in cardiovascular disease risk factors: a systematic review. Ethn Dis. 2007;17(1):143–152. [PubMed] [Google Scholar]
- 10. Ong KL, Cheung BMY, Man YB, Lau CP, Lam KSL. Prevalence, awareness, treatment, and control of hypertension among United States adults 1999–2004. Hypertension. 2007;49(1):69–75. doi: 10.1161/01.HYP.0000252676.46043.18. [DOI] [PubMed] [Google Scholar]
- 11. Mensah GA, Mokdad AH, Ford ES, Greenlund KJ, Croft JB. State of disparities in cardiovascular health in the United States. Circulation. 2005;111(10):1233–1241. doi: 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- 12. Roger VL, Go AS, Lloyd-Jones DM, et al. Heart disease and stroke statistics–2011 update: a report from the American Heart Association. Circulation. 2011;123(4):e18–e209. doi: 10.1161/CIR.0b013e3182009701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Wyatt SB, Williams DR, Calvin R, Henderson FC, Walker ER, Winters K. Racism and cardiovascular disease in African Americans. Am J Med Sci. 2003;325(6):315–331. doi: 10.1097/00000441-200306000-00003. [DOI] [PubMed] [Google Scholar]
- 14. Redmond N, Baer HJ, Hicks LS. Health behaviors and racial disparity in blood pressure control in the national health and nutrition examination survey. Hypertension. 2011;57(3):383–389. doi: 10.1161/HYPERTENSIONAHA.110.161950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Watkins LO. Epidemiology and burden of cardiovascular disease. Clin Cardiol. 2004;27(S3):2–6. doi: 10.1002/clc.4960271503. [DOI] [PMC free article] [PubMed] [Google Scholar]