Abstract
Food allergy prevention involves recommendations to the maternal diet during pregnancy and breast feeding, early life feeding and introduction of solid foods. Pregnant and breastfeeding women are not recommended to exclude any food allergens from their diet, but data are lacking to support active consumption of food allergens for prevention of food allergy. Breastfeeding is recommended for the many health benefits to the mother and child but has not shown any association with reduction in childhood food allergies. There is currently no recommendation regarding the use of any infant formula for allergy prevention, including the use of partially or extensively hydrolyzed formulas. Once the introduction of solid food commences, based on randomized controlled trials, it is advised to actively introduce peanuts and egg early into the infant diet and continue with consumption of these. Although there are limited data with respect to other major food allergens and whether early introduction may prevent allergy development, there is no need to delay the introduction of these allergens into the infant diet. Interpreting food allergen consumption in the context of cultural food practices has not been studied, but it makes sense to introduce the infant to family foods by 1 year of age. Consumption of foods typical of the Western diet and foods high in advanced glycation end products may be associated with an increase in food allergies. Similarly, intake of micronutrients, such as vitamin D and omega-3 fatty acids in both the maternal and infant diet, needs further clarification in the context of food allergy prevention.
Keywords: Food allergy, microbiome, nutrients, nutrition, prevention
1. Introduction
Food allergy prevention guidelines have changed to a great extent in the past 2 decades [1-7] (Table 1).
Table 1.
Summary of the national and international guidance on the prevention of food allergies
| Consensus statement: American Academy of Allergy, Asthma, and Immunology; American College of Allergy, Asthma, and Immunology; Canadian Society of Allergy and Clinical Immunology (2020) [2] | European Academy of Allergy and Clinical Immunology (2020) [3] | Japanese Pediatric Guidelines for Food Allergy (2020) [4] | Canadian Pediatric Society (2019) [5] | Asia Pacific Academy of Pediatric Allergy, Respirology, and Immunology (2018) [6] | Australasian Society of Clinical Immunology and Allergy (2016) [7] | |
|---|---|---|---|---|---|---|
| Foods of relevance | All foods | All foods | All foods | All foods | All foods | All foods |
| BF | EBF recommended for all mothers; no association between EBF and prevention of FA | EBF for around the first 6 months of life and continued BF for the first year | No evidence that BF prevents food allergy | BF for up to 2 years and beyond | Continue BF up to 2 years | BF for at least 6 months and for as long as mother and infant wish to continue |
| Pregnant or BF mothers | Does not recommend maternal exclusion of common allergens Does not support the use of any food supplement |
Recommends against avoiding food allergens | Recommends against avoiding allergens | Recommends a healthy diet Exclusion of any foods (including allergenic) not recommended Recommends up to 3 servings of oily fish per week No recommendation on probiotics |
||
| Introduction of solid foods | All infants: Some families choose to start CF at age 4–6 months | All infants: start at around age 5–6 months | Infants at no or low risk of FA: introduce CF at around age 6 months | Healthy infants: start CF at age 6 months. | All infants: start when infant is ready—around 6 months of age but not before age 4 months. | |
| Introduction of food allergens | Introduce peanut and cooked hen’s egg to all infants starting around age 6 months but not before age 4 months. Do not delay introduction of other allergenic CF (CM, soy, wheat, tree nuts, sesame, fish, shellfish) at around age 6 months but not before age 4 months. |
All infants: introduce peanut and well-cooked hen’s egg as part of CF starting at age 4–6 months. | All infants, including high-risk infants: delayed introduction of food allergens is not recommended. | High-risk infants: introduce allergenic solids at around age 6 months but not before age 4 months. Introduce allergenic foods one at a time, to gauge reaction, without unnecessary delay between each new food. Once tolerated, offer the allergenic food a few times a week to maintain tolerance. |
High-risk infants with family history of FA: do not delay introduction of allergenic foods. High-risk infants with severe eczema: skin prick test or oral food challenge (or both) to peanut and egg may be required. Do not delay introduction of allergenic foods. |
All infants, including high-risk infants: introduce allergenic solid foods, including peanut, cooked hen’s egg, dairy, and wheat, within the first year of life. High-risk infants: there is good evidence that regular peanut intake before age 12 months can reduce peanut allergy; moderate evidence that cooked hen’s egg before age 8 months (in infants with family history of allergy) reduces risk of developing hen’s egg allergy. |
| Continued intake | No frequency, just add as regular part of diet | Unless there is an allergic reaction to the food, continue to give the food to your baby regularly (twice weekly), as part of a varied diet. Trying a food and then not giving it regularly may result in food allergy development. | ||||
| Formula | Recommends against the use of any hydrolyzed formulas for prevention of FA or sensitization | No recommendation for or against the use of hydrolyzed infant formulas Recommends against soy protein formula in the first 6 months of life |
Insufficient evidence on the usefulness of hydrolyzed milk in preventing the onset of food allergies | Does not recommend hydrolyzed (partially or extensively) infant formula for prevention of allergic disease Recommends use of standard CMF when BF is not possible |
||
| Other | Recommends feeding infants a diverse diet, as this may prevent FA No recommendation on prebiotics and probiotics |
No recommendations for or against: -vitamin supplements, fish oil, prebiotics, probiotics, or synbiotics in pregnancy, when BF, or in infancy -altering the duration of EBF -hydrolyzed infant formulas |
No recommendation on probiotics during pregnancy |
AD, atopic dermatitis; BF, breastfeeding; CF, complementary foods; CMF, cow’s milk formula; EBF, exclusive breastfeeding; FA, food allergy; NIAID, National Institute of Allergy and Infectious Diseases.
Adapted with permission from Sampath et al. [1].
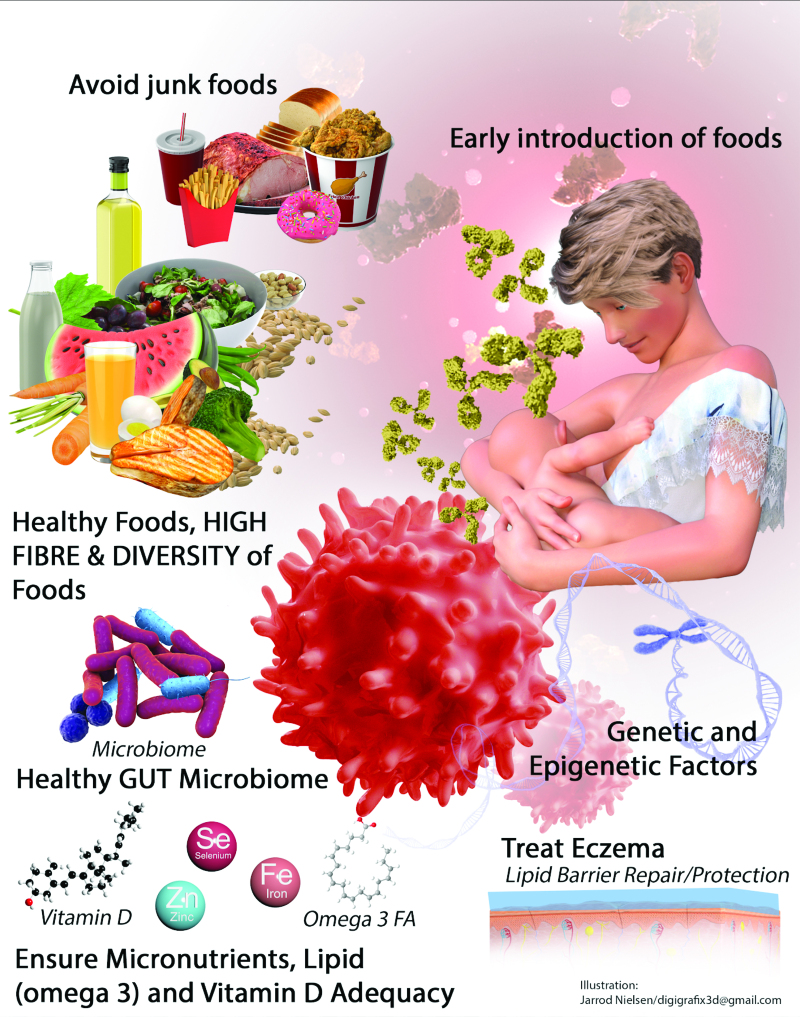
These changes include dietary advice given regarding the maternal diet during pregnancy and breastfeeding (BF) and age of introduction of potentially allergenic foods during infancy. Knowledge regarding the overall maternal and infant diet and the role of micronutrients in food allergy prevention has increased. Understanding about the interconnectivity of nutrition, microbiome, immune system, and epigenetics has also increased, highlighting the advances made in the knowledge base underpinning food allergy prevention.
This review article will provide an overview on the role of the maternal diet during pregnancy and lactation, the infant diet, the role of BF, and formula feeding in food allergy prevention. The characteristics and function of the microbiome in food allergy prevention will also be discussed. The article will summarize information from observational studies, randomized controlled trials (RCTs), systematic reviews, and guidelines/consensus documents.
2. Maternal diet in pregnancy and during BF
2.1. Food allergens
Earlier, allergy prevention guidelines recommended that pregnant and BF women from high-risk families should avoid peanut and other food allergens in the United States and elsewhere [9]. A meta-analysis conducted by the Food Standards Agency in the United Kingdom summarizing 5 RCTs [8, 10-13] concluded that there was no evidence that food allergen avoidance, either single or multiple foods, with or without other interventions, was associated with reduced offspring food allergy outcomes [14]. Food allergen avoidance during pregnancy and BF for prevention of food allergy in offspring is currently not recommended by national [2, 15-17]and international [3-6, 9, 18, 19] guidelines and consensus statements. Guideline documents (Table 1) also highlight that food allergen avoidance during pregnancy and lactation may also lead to nutritional deficiencies [20].
There is some conflicting evidence about consumption of food allergens during BF and infant food allergy outcomes [21, 22]. Regarding food allergen consumption during pregnancy and lactation, one study indicated that maternal peanut consumption during pregnancy, and followed by introduction of peanut into the infant diet while still being breastfed, may prevent peanut sensitization [23]. This finding was supported by another study, which indicated that maternal peanut intake during BF may prevent peanut sensitization [24]. Neither of these studies looked at clinical food allergy as an outcome, and more studies are needed to address the complexity of food allergen consumption by pregnant women, BF mothers, and infants and the overlap between BF and infant food allergen introduction. Studies need to evaluate clinical outcomes.
2.2. Maternal food diversity patterns
The role of diet diversity (DD) in pregnancy and lactation in offspring allergy outcomes has only been reported in one study. Venter et al. [25]. computed DD scores [26] using dietary data obtained from food propensity questionnaires (FPQs) [27] that were completed by mothers at 2 time points during pregnancy. Total DD scores were computed using all 41 questions included in the FPQ. The healthy DD scores included FPQ items identified as healthy according to the US dietary guidelines [28]. The unhealthy DD scores included FPQ items identified as unhealthy per the US dietary guidelines [28]. The adjusted models showed that increases in maternal healthy DD scores were significantly associated with lower odds of children diagnosed with “any allergy excluding wheeze,” atopic dermatitis, asthma, and wheeze up to age 4. The adjusted models showed that increases in maternal unhealthy DD scores were significantly associated with higher odds of children diagnosed with atopic dermatitis by age 4. The adjusted models showed no significant associations between the maternal total DD during pregnancy and any of the offspring allergy outcomes up to age 4. There were no significant associations between any of the 5 measures of maternal diet and child food allergy by age 4 due to lack of power. No study has investigated the association between DD during BF and offspring allergy outcomes.
2.3. Diet indices
Four diet indices have been studied to investigate the association between maternal diet during pregnancy and offspring allergy outcomes: the healthy eating index (HEI) [29-31], the diet inflammatory index (DII) [31, 32], the Mediterranean diet index (MDI) [29, 33-36] and the maternal diet index (MDI) [37]. One study found no association between the HEI and childhood atopy and reported allergy outcomes (including food allergy) at 3 and 10 years [30]. Studies using the DII [31, 32] and the MDI [29, 33-35] in pregnancy did not report on associations with offspring food allergies. Venter et al. [37]. recently developed and replicated a diet index showing that increased maternal intake of vegetables and yogurt, and reduced intake of fried potatoes, red meat, rice and grains, pure fruit juice, and cold cereals were significantly associated with a reduced risk of allergic rhinitis, atopic dermatitis, asthma, and wheeze in offspring up to 4 years of age. A 16% reduction in food allergy was seen but this was not significant. The role of different diet indices during lactation and in allergy prevention in infants has also not been studied. Therefore, no recommendations can be made about the role of dietary patterns or indices in pregnancy and lactation and offspring food allergy outcomes.
2.4. Food types and nutrients
2.4.1. Foods
RCTs using single foods during lactation have not been performed. One observational study showed that citrus and kiwi fruit consumption during lactation may be associated with a reduced risk of cow’s milk allergy in infants [38]. A European Academy of Allergy and Clinical Immunology (EAACI) systematic review noted there was no evidence to suggest that intake of any particular food during pregnancy or lactation reduces food allergy outcomes [26].
2.4.2. Nutrients
The EAACI systematic review found weak evidence from observational studies that increased intake of copper and vitamin C during pregnancy may reduce offspring food allergy outcomes [39].
A systematic review and meta-analysis based on 2 RCTs from EAACI [39] indicated that omega-3 fatty acid intake during pregnancy was not associated with reduced offspring food allergy outcomes. Vadhaninia et al. [40]. reported in their systematic review that omega-3 supplementation in pregnancy significantly reduced sensitization to egg and peanut in offspring. There are no RCTs using omega-3 supplementation in lactation only. One RCT administered omega-3 fatty acids during pregnancy and BF in high-risk mothers and found a decrease in food allergy [41]. In their systematic review, Garcia-Larsen et al. [14] reported reduced sensitization to peanut and egg in the infant and/or child if omega-3 fatty acids were administered during pregnancy and/or lactation.
2.5. Vitamin D
Goldring et al. [42] reported no significant association between vitamin D supplementation in pregnancy, given either as a single, large bolus or as daily intake of vitamin D, and offspring allergy outcomes. Garcia-Larsen et al. [14] indicated in their systematic review that vitamin D supplementation in pregnancy and/or lactation and/or early life feeding was not associated with offspring food allergies [14]. There is currently no evidence to support vitamin D supplementation during pregnancy or lactation for food allergy prevention.
2.6. Prebiotics and probiotics
Several studies have investigated the association between probiotic intake during pregnancy and/or lactation and offspring allergy outcomes. None of them reported on food allergy as an outcome. In addition, there are no reported data from RCTs using prebiotics and synbiotics in pregnancy and/or lactation only and food allergy outcomes. Only 1 RCT used probiotic supplementation in high-risk women during pregnancy in addition to prebiotics and probiotics in early life and reported reduced food allergy outcomes in the supplemented group [43]. Garcia-Larsen et al. [14]. summarized studies throughout pregnancy, lactation, and early life and found a significant reduction in CM sensitization, but not offspring food allergy.
In summary, the only recommendation that can be made to pregnant and lactating women is that there is no need to exclude food allergens from their diets. There is, however, also no evidence to suggest that they must eat these foods during pregnancy if not part of their normal diet. Pregnant and lactating women should follow a healthy, nutritious diet, although evidence linking healthy eating or any other measure of overall food intake with food allergy prevention is lacking. Intake of nutrients, prebiotics, probiotics, and synbiotics during pregnancy and/or lactation and offspring allergy outcomes need further investigation.
3. Infant diet
3.1. BF and formula feeding
Breast milk is considered the optimal source of nutrition for infants. Although breast milk is known for its beneficial effects on the infant’s gut microbiome and immune system, it’s role in food allergy prevention remains unproven (Table 1).
EAACI [3, 14, 44] and the UK Food Standards Agency concluded from their systematic reviews that BF may not reduce the risk of food allergy. This conclusion is further supported by recommendations from the American Academy of Pediatrics [16] and the American Academy of Asthma, Allergy and Immunology/American College of Allergy and Asthma and Immunology/Canadian Society of Allergy and Clinical Immunology (AAAAI/ACAAI/CSACI) 2020 [15] consensus statements indicating that the role of BF in food allergy prevention is uncertain. BF should, however, always be supported due to its benefits for the mother and infant [45].
Current, international food allergy guidelines do not support the use of any infant formula for food allergy prevention (Table 1). This is a change from previous guidelines that recommended the use of partially and/or extensively hydrolyzed formulas in food allergy prevention. This particularly contradicts the US Food and Drug Administration decision that a partially hydrolyzed formula could reduce the risk of eczema and conclusions from a previous Cochrane review, which reported that hydrolyzed formulas could prevent the development of CM allergies [46].
In summary, BF should be supported when mothers choose to breastfeed. For those mothers who choose not to breast feed, a standard cow’s milk formula (CMF) should be recommended due to the lack of alternative recommendations.
4. Early allergen introduction and prevention of food allergy
To date, many allergen-specific RCTs have investigated the effects between early introduction of major allergens and the prevention of the respective food allergy. These RCTs have been performed in both standard-risk and high-risk infants (Table 2).
Table 2.
Summary of randomized controlled trials of early allergenic food introduction for food allergy prevention
| Study | Full title | Study type | Population | Intervention | Primary outcome | Results |
|---|---|---|---|---|---|---|
| LEAP (UK) [47] |
Learning Early About Peanut Allergy | Nonblinded RCT (n = 640) |
High-risk infants • moderate-to-severe eczema and/or egg allergy |
•Thrice weekly consumption of 2 g of peanut protein vs complete avoidance of peanut after randomization at 4–11 months, through 60 months of life | IgE-mediated peanut allergy based on OFC at month 60 | • ITT analysis showed prevalence of peanut allergy 13.7% in the avoidance group vs 1.9% in the consumption group (P < 0.001) |
| STAR (Australia) [48] |
Solid Timing for Allergy Reduction | Blinded RPCT (n = 86) |
High-risk infants with moderate-to-severe eczema | • Daily consumption of egg vs placebo powder from 4 to 8 months • 0.9 g raw whole egg powder daily (0.4 g protein/day) • Cooked egg at 8 months |
IgE-mediated egg allergy at 12 months based on positive SPT and egg OFC | • Study terminated early: 1/3 of patients reacted to egg at entry OFC • At 12 months, 33% had egg allergy in the egg group vs 51% in control (not significant) |
| PETIT (Japan) [49] |
Preventing Egg Allergy in Infants with AD | Blinded RCT (n = 121) |
High-risk infants with atopic dermatitis | • Daily consumption of 50 mg heated egg from 6 to 9 months • Daily consumption of 250 mg heated egg from 9 to 12 months |
IgE-mediated egg allergy at 12 months of age based on OFC | • Prevalence of egg allergy 37.7% in placebo vs 8.3% in the egg group (P = 0.0013) • No SAEs |
| STEP (Australia) [50] |
Starting Time for Egg Protein | Blinded RPCT (n = 820) |
Intermediate risk: • atopic moms (allergic disease + positive envir SPT) • Infants: no allergic dz |
• Daily consumption of egg vs placebo powder from 4 to 6.5 months • 0.9 g raw whole egg powder daily (0.4 g protein/day) |
IgE-mediated egg allergy at 12 months based on positive SPT and egg OFC | • No significant differences in egg allergy between groups • No anaphylactic reactions at initial egg introduction |
| BEAT (Australia) [51] |
Beating Egg Allergy Trial | Blinded RPCT (n = 319) |
Intermediate risk: • Infants with first-degree relative with atopy • Infants: negative egg SPT |
• Daily consumption of egg vs placebo powder at 4 months • 350 mg protein daily raw whole egg powder • Cooked egg at 8 months |
Sensitization to egg by SPT at 12 months of age | • Subjects in egg group vs placebo had significantly less egg sensitization (10.7% vs 20.5%, P = 0.03) • No harm with egg introduction |
| HEAP (Germany) [52] |
Hen’s Egg Allergy Prevention | Blinded RPCT (n = 406) |
Normal-risk general population: • Infants with IgE < 0.35 kU/L at enrollment |
• Thrice weekly 2.5 g egg protein from 4 to 6 months of age until 12 months | Sensitization to egg based on egg IgE ≥ 0.35 kU/L at 12 months of age | • No evidence of preventing egg sensitization or allergy • High rate of anaphylaxis at egg introduction at entry |
| ABC Trial (Japan) [53] |
Atopy Induced by Breastfeeding or Cow’s Milk Formula | Nonblinded RCT (n = 312) |
Intermediate risk: • Infants with first-degree relative with atopy |
• Randomized to 2 interventions: • (1) active: BF and/or CMF in first 3 days of life; (2) placebo: BF and/or amino-acid (EF)-based formula in first 3 days |
Primary: Sensitization to CM Secondary: IgE-mediated milk allergy at 24 months based on OFC |
• Primary outcome: 24 infants (16.8%) sensitized in the BF/EF group vs 46 infants (32.2%) in the BF plus CMF group (relative risk [RR], 0.52; 95% CI, 0.34–0.81). • Secondary outcome: IgE-mediated CM allergy in the BF/EF vs BF plus CMF groups (4 [2.6%] vs 20 [13.2%]; RR, 0.20; 95% CI, 0.07–0.57) |
| SPADE (Japan) [54] |
Strategy for Prevention of Milk Allergy by Daily Ingestion of Infant Formula in Early Infancy | Nonblinded RCT (n = 518) |
Normal-risk general population | • Randomized between 1 and 2 months of age to daily consumption of at least 10 mL of a CMF or avoidance of CM (soy formula) • Ongoing BF recommended until 6 months of age |
IgE-mediated milk allergy at 6 months of age based on OFC | • ITT analysis showed 2 of 242 ingestion-group infants (0.8%) vs 17 of 249 avoidance group (6.8%) had milk allergy (P < 0.001) • Screening OFC at age 1 month to 20 mL of CMF; no SAEs |
| EAT (UK) [55] |
Enquiring About Tolerance | Nonblinded RCT (n = 1,303) |
Normal risk: Exclusively breastfed until allergenic foods introduced |
• EIG introduced 2 g of protein twice weekly at 3 months of peanut, cooked egg, CM, sesame, whitefish, wheat • SIG at 6 months of above 6 foods |
IgE-mediated food allergy to at least 1 of the 6 allergens at 1 or 3 years of age based on OFC | • ITT analysis showed no difference in food allergy between EIG vs SIG • PP analysis showed significantly less prevalence of peanut allergy (P = 0.003) and egg allergy (P = 0.009) in EIG vs SIG |
| PreventADALL (Norway, Sweden) [56] |
Preventing Atopic Dermatitis and ALLergies | Nonblinded RCT (n = 2,397) |
Normal-risk general population | • Randomized to 4 intervention groups: (1) no intervention; (2) skin; (3) food; (4) combined skin and food • Food: introduction of peanut, CM, egg, and wheat from 3 months of age vs no specific advice on food introduction |
IgE-mediated peanut, CM, egg, or wheat allergy at 36 months of age based on OFC | • ITT analysis showed prevalence of food allergy reduced in food intervention group compared to no food intervention group: risk difference –1.6% (95% CI, –2.7 to –0.5); OR, 0.4 (95% CI, 0.2–0.8) • Reduced risk of food allergy seen with peanut but not with other 3 foods |
BF, breastfeeding; CM, cow’s milk; CMF, cow’s milk formula; dz, disease; EF, elemental formula; EIG, early introduction group; envir, environment; IgE, immunoglobulin E; ITT, intention to treat; OFC, oral food challenge; PP, per protocol; RCT, randomized controlled trial; RPCT, randomized placebo controlled trial; SAEs, serious adverse events; SIG, standard introduction group; SPT, skin prick test.
4.1. Peanut
Two RCTs have investigated the timing of peanut introduction and the risk of developing peanut allergy. The intention to treat (ITT) analysis of the Learning Early About Peanut Allergy study demonstrated a statistically significant risk reduction (17% absolute risk reduction [ARR]) associated with early peanut introduction in 4- to 11-month-old high-risk infants (having severe eczema and/or egg allergy) [47]. The per protocol (PP) analysis (not the ITT analysis) of the EAT study [55] noted small, significant ARR differences for introduction of peanut at 3 months compared with introduction after 6 months (ARR, 2.5%) in infants not considered by investigators to be at high risk for the development of food allergy. A meta-analysis inclusive of 1,550 infants from these 2 studies performed by Ierodiakonou et al. noted “moderate certainty” of evidence that introducing peanut between 4 and 11 months reduced the risk of developing peanut allergy (relative risk [RR] 0.29; 95% confidence interval [CI], 0.11–0.74) [57].
4.2. Egg
Five RCTs have investigated the timing of egg introduction and risk of egg allergy. Two studies targeted high-risk infants with eczema: the Solids Timing for Allergy Reduction (STAR) trial [48], which found a trend toward reduced risk of developing egg allergy at 1 year (RR, 0.65, P = 0.11) associated with introduction of raw, pasteurized, powdered egg protein at 4 vs 8 months of life; and the Prevention of Egg Allergy with Tiny Amount Intake (PETIT) study [49], which noted a strong protective effect in the early introduction group (RR, 0.22; 95% CI, 0.08–0.61; P = 0.0012; numbers needed to treat [NNT], 3.4) who consumed 50 mg/day heated egg powder from 6 to 9 months of life, and then 250 mg/day from 9 to 12 months (vs placebo). In 2 studies that defined infants at higher risk because of having an atopic relative, the Starting Time for Egg Protection (STEP) study [50] noted a nonsignificant 3.3% ARR in the development of egg allergy at age 1 in infants who received raw, pasteurized egg protein at 4 to 6 vs 10 months, and in Beating Egg Allergy Trial (BEAT) study [51], there was no significant difference in egg allergy at age 1 in infants who were randomized to raw, pasteurized egg introduction at 4 to 6 vs 8 months, but there was a 9.7% ARR in egg sensitization associated with earlier introduction. In the standard-risk infant study, Hen’s Egg Allergy Prevention (HEAP) [52], there was no significant difference in rates of egg sensitization or oral food challenge (OFC)-proven egg allergy at age 1 in infants introduced to raw, pasteurized egg vs placebo at 4 to 6 months (RR, 3.3; P = 0.35). Lastly, the PP analysis of the EAT study noted small, significant ARR differences for introduction of egg at 3 months compared with introduction after 6 months (ARR 4.1%) in infants not at risk for the development of food allergy [55].Based on a meta-analysis of 5 RCTs (STAR, STEP, BEAT, HEAP, and PETIT), inclusive of 1,915 children, Ierodiakonou et al. also determined there was a “moderate certainty” of evidence that introducing egg between 4 and 6 months reduced the risk of developing egg allergy (RR, 0.56; 95% CI, 0.36–0.87). In terms of safety, collectively, the studies showed that early introduction of well-cooked egg is safer and more effective than raw, pasteurized egg for prevention of egg allergy.
4.3. Milk
Two RCTs have examined the timing of CM introduction and the risk of CM allergy development. The Atopy Induced by Breastfeeding or Cow’s Milk Formula (ABC) trial [53] was performed in infants at intermediate risk due to a first-degree relative with atopy who were randomized to BF with or without an amino-acid-based elemental formula (EF) for at least the first 3 days of life (BF/EF group) or supplemented with CMF from the first day of life (BF/CMF group). Although the study noted higher rates of CM sensitization and CM allergy in the BF/CMF group, it is difficult to interpret the study findings because the duration of CMF intake before discontinuation differed widely among infants, and some did not stop. In the normal-risk Strategy for Prevention of Milk Allergy by Daily Ingestion of Infant Formula in Early Infancy (SPADE) study [54], infants randomized to CM at 1 to 2 months of age were found to have a significantly lower rate of CM allergy compared with those randomized to avoidance of CM (use of soy formula). Although the above 2 RCTs differ in their results, it should be noted that in the normal-risk EAT [55] and prevent atopic dermatitis and allergies (PreventADALL) [56] studies, there was no significant finding with respect to the timing of CM introduction in the EAT study [55], but the PreventADALL study [56] did show an overall reduced prevalence of food allergy in the food intervention group.
4.4. Other major food allergens
There are less data regarding early introduction of other potentially allergenic complementary foods. There have been no RCTs for the remaining other 6 major food allergens, but data from the EAT study on wheat, sesame, and codfish showed no significant association with reduced (or increased) rates of allergy development to these items (respectively) based on the early vs. standard time of introduction, and may serve as the highest quality evidence to evaluate the effect of potential early introduction that is available for these allergens [55]. Data are even more sparse for other major food allergens: no RCTs have investigated challenge-proven prevention outcomes associated with the timing of introduction of soy, tree nuts, or shellfish [57].
In summary, current data from RCTs strongly support the early introduction of peanut and egg in infant diets for the prevention of these food allergies. Although some RCT data on early CM introduction are conflicting, early and ongoing exposure to CMF supplementation may prevent CM allergy. While there are limited or no RCT data for other highly allergenic foods, there are no data showing harm in introducing these allergenic foods within the first year of life, and thus early introduction may be beneficial as well.
5. Infant DD
DD is defined as the number of foods or food groups consumed over a given reference period [58]. Diet variety is synonymous with DD [58]. DD can be defined as the number of foods [59-65], food groups [59, 66-80], foods within a food group [81-85] eaten, and data can be collected over a time period ranging from a day to 1 year [26]. An EAACI [26] task force report concluded that higher DD in infancy may reduce the odds of developing food allergy in later childhood. This article set standards for measuring DD, suggesting that the food items consumed, the time period, and the frequency of consumption should be reported.
5.1. Infant DD and food allergen sensitization
Three studies reported on the association between infant DD and food allergen sensitization (Table 3). All 3 studies reported that increased DD in infancy was associated with reduced sensitization in childhood [86, 87, 90].
Table 3.
Common definitions of diet diversity used
| Study | Definition |
|---|---|
| Protection Against Allergy Study in Rural Environments (PASTURE) [86] Multicenter EU study |
1. Diet diversity: the 15 foods commonly eaten by 80% of the children in the study in the first year of life, which also included all food allergens: any cow’s milk, yogurt, other milk products; eggs; nuts; vegetables or fruits; cereals; bread; meat; fish; soy; margarine or butter; cake; and chocolate 2. A second definition: included the 6 major foods introduced in the first 6 months or first 12 months of life, which did not include all food allergens: vegetables or fruits; cereals; bread; meat; cake; and yogurt |
| Finnish study [87] | The number of foods introduced at 3, 4, and 6 months of age |
| Food Allergy Research and Intolerance study (FAIR) [85] UK |
1. Count of 21 common foods eaten in infancy: overall diet diversity 2. WHO definition of diet diversity (7 food groups: grains/roots/tubers, legumes/nuts, dairy, flesh foods, eggs, vitamin A-rich fruits and vegetables, other fruits and vegetables) 3. Number of fruits and vegetables consumed: fruit and vegetable diversity 4. Count of 8 common food allergens: milk, egg, wheat, fish, soy, peanut, tree nuts, sesame |
| China [88] | The number of food groups consumed (0–11 food groups) |
| Korea [89] | 1. Food group diversity 2. Food allergen diversity 3. WHO definition of diet diversity |
WHO, World Health Organization.
5.2. Infant DD and food allergy
Four observational studies in infancy studied the association between infant DD and childhood food allergy. Roduit et al. [86] reported that infants with a more diverse diet had a lower prevalence of reported doctor’s diagnosed food allergy by 6 years. In this study [91], there was no association between DD in the second year of life and food allergy at 6 years. Consumption of yogurt and CM were, however, inversely associated with food allergy development. Venter et al. [85]. reported that increased DD at 6 and 9 months was significantly associated with reduced food allergy over the first 10 years of life. For each additional food consumed by 6 months, the odds of developing food allergy by 10 years were reduced by 11%. Based on the World Health Organization (WHO) definition of DD and fruits and vegetables diversity by 6 months, a significant reduction in the odds of developing food allergy by 10 years was seen. Food allergen diversity by 12 months was significantly associated with reduced odds of food allergy by 10 years. For each further food allergen introduced, the odds of food allergy were reduced by 33%.
Comparing intake of 1 to 5 food groups vs 8 to 11 food groups, Zhong et al. [88]. reported that reduction in food diversity at 12 months of age was significantly associated with an increased risk of parent-reported food allergy by 2 years of age. A research group from Korea [89] reported higher DD based on food group consumption, number of food allergens consumed, and the WHO definition of diversity at 3 and 4 months were associated with a lower prevalence of hen’s egg allergy in the high-risk group. No associations were seen in the control group. Diversity scores at 6 months of age were not associated with food allergy outcomes.
5.3. Food allergen diversity based on RCTs
Quake et al. [92] performed an RCT, feeding 180 infants between 4 and 6 months of age single foods (milk, egg, or peanut as 300 mg protein/day: 2,100 mg protein/food allergen/week) vs 2 foods (milk/egg, egg/peanut, milk/peanut as 300 mg/mix/day: 1,050 mg protein/food allergen/week) vs a multiple food mix of 10 food allergens (milk/egg/peanut/cashew/almond/shrimp/walnut/wheat/salmon/hazelnut at low [300 mg/day: 21 [3 mg × 7] mg/food allergen/week], medium [63 [9 mg × 7] mg/food allergen/week], or high doses [210 [30 mg × 7] mg/food allergen/week]) vs no early introduction. All infants were breastfed until at least 6 months of age and assessed for food allergy at 2 to 4 years after the end of the study. The study outcomes indicated that the percent of participants able to consume 8 g of total protein from the 10-allergen mixture (800 mg allergen/food) was significantly higher in all mixed protein groups compared with controls (q < 0.01). The EAT study could also be considered a study using food allergen diversity, but data comparing food allergen diversity in the control vs active group were not reported [55]. A recent study indicates that early and regular consumption of food allergens on a population level shows a reduction in food allergies similar to RCTs. See Table 4 for a DD and allergen diversity meal plan. This meal plan contains 7 food allergens and over 30 plant-based foods per week.
Table 4.
Diet diversity meal plan
| Infant: 7–9 months plus | |||||||
|---|---|---|---|---|---|---|---|
| Sunday | Monday | Tuesday | Wednesday | Thursday | Friday | Saturday | |
| Allergens | Peanut butter and yogurt | Cashew butter and walnut butter | Egg and sesame | Peanut butter Soy |
Egg and walnut butter | Yogurt Soy |
Cashew butter and sesame |
| Breakfast | 2 TB white rice 1 TB homemade apple purée/mash/baked apple slices with 1 teaspoon peanut butter |
2 TB boiled brown rice with 1–2 teaspoons cashew butter 1 TB pitted cherry purée |
2 TB oat baby cereal 1 TB pineapple purée |
2 TB multigrain baby cereal with 1 teaspoon peanut butter 1 TB apricot purée |
2 TB brown rice baby cereal 1 TB mango purée |
2 TB quinoa baby cereal 1 TB prune purée |
2 TB brown rice baby cereal teaspoon cashew butter 1 TB peach purée |
| Lunch | 2 TB roasted sweet potato purée/mashed/softly cooked slices 1 TB banana purée/strips 1 TB puréed meat/softly cooked meat |
1 TB spinach purée/mashed 1 TB puréed/boiled/shredded chicken |
1 TB Napa cabbage 1–2 TB tomato egg |
2 TB purée/softly cooked cauliflower mashed/chunky salmon |
2 TB watercress purée 1–2 TB water-steamed egg |
1 TB soybean sprouts 1 TB carrots 2.5 teaspoon yogurt |
1 TB broccoli purée/softly cooked broccoli 1 TB pork purée/pulled pork |
| Dinner | 1 TB mung bean sprout purée 1 TB mango purée/slices 1–2 TB yogurt |
1 TB kabocha squash ¾ to 1½ teaspoons walnut butter |
1 TB mashed zucchini/softly cooked slices ½ to 1 teaspoon sesame in sesame noodles |
1 TB soybean sprouts 1 TB raspberry puréed/mashed/soft fruit |
1 TB mashed or sliced pear ¾ to 1½ teaspoons walnut butter |
Softly cooked noodles (rice or wheat) 1 TB cooked puréed/mashed or chunky tomato sauce |
1 TB green peas ½ to 1 teaspoon sesame paste stir into vegetable purée |
TB, tablespoon.
In summary, once infants are ready to eat, a diverse diet based on cultural food habits, which includes both plant-based foods and food allergens, should be recommended. Once food allergens are introduced, frequent intake is recommended.
6. The bigger picture of prevention
6.1. Microbiome
The gut microbiome is found to be associated with food allergy outcomes in several studies [93-96]. The gut microbiome composition and diversity of children who develop milk and egg allergies differ from that of non-food-allergic children [94, 95]. Gut microbiome differences have also been reported in children who develop tolerance to milk and those who remain allergic [93]. Differences in the gut microbiome profile in children sensitized to food allergens and non-sensitized children have also been reported [97]. Hua et al. [98]. showed that microbial taxa and microbiota richness differed between food-allergic and non-food-allergic adults. However, it is still unclear which particular species or genus may prevent the development of food allergies [96, 99, 100], and the immunomodulatory effect of the gut microbiome may depend on its potential to produce butyrate [101].
Short-chain fatty acids (butyrate, acetate, and propionate) may protect against the development of food allergy [101]. Butyrate, in particular, may play a role in tolerance development through downregulating interleukin (IL)-5 and IL-13 (Th2 cytokine) production [102, 103], and modulating immune regulation in the gut and peripheral tissues [104-108].
Diet, particularly DD, plays an important role in the gut microbiome composition and function 27,110 Claesson et al. [109]. showed in an elderly population that increased diet was associated with increased gut microbial diversity. Similarly, increased DD in the infant diet during the first year of life is also associated with increased microbial diversity [110].
Recently, the EAT study showed that the introduction of 6 major allergenic foods leads to a significant increase in microbial diversity, measured by the Shannon index and increase of Prevotellaceae and Proteobacteria, compared with exclusively breastfed infants [111]. A Korean research group reported data on DD in infancy, gut microbial composition and development of hen’s egg allergy [89]. DD was defined according to the WHO definition of minimum DD, food group diversity, and food allergen diversity. In high-risk infants, increased DD was associated with increased microbial diversity and reduced expression of IL-13. Lower DD was associated with increased expression of IL-4, IL-5, IL-6, and IL-8. Roduit et al. [101]. reported that a diverse diet rich in fruit, vegetables, fish, and yogurt in infancy was associated with increased butyrate production. A diet rich in dietary fibers [112] such as arabinoxylan [113], can also affect microbiome function, and is associated with increased butyrate production. A recent EAACI systematic review concluded that there is significant potential for using fiber intake to manipulate the gut microbiome composition and metabolic functions, thereby promoting immune health [114].
Consumption of plant-based foods and its role in gut microbiome composition have been highlighted by the American Gut Project [115]. This study showed that in adults, consumption of 30 plant-based foods per week leads to optimal gut microbial diversity (Table 4).
Targeted manipulation of the gut microbiome may support food allergy prevention and tolerance induction, but manipulation strategies are currently unclear. There has been a lack of data for the use of overall diet, nutrients, prebiotics, synbiotics, and probiotics during pregnancy, lactation, and early infancy for food allergy prevention. Further research is much needed.
6.2. Ultraprocessed foods and advanced glycation end products
The modern Western pattern diet is associated with increased consumption of ultraprocessed foods. This pattern of eating is linked to increasing rates of food allergy. Ultraprocessed diet is inadequate in terms of nutritional value; it is low in fiber and high in salt and sugars, particularly fructose [116]. Diets high in sugar combined with food processing such as dehydration, microwaving and frying lead to the formation of advanced glycation end products (AGEs) that are epidemiologically and immunologically linked to trends in food allergy [117]. AGEs bind to receptors that are part of the innate threat reception network called the receptor for advanced glycation end products (RAGE). RAGE agonists include alarmins such as amyloid and danger-associated molecular patterns, including high-mobility molecular group box 1 and S100 proteins [118]. The foods being consumed in the Western dietary pattern, which is largely taken up globally, contain the ingredients to form compounds that signal tissue injury. High-fructose corn syrup is an ever-increasing component as sweeteners and as a component of animal feed and in soft drinks. The Western pattern diet contains approximately 2,000% more fructose than a traditional diet [119]. Fructose has a greater capacity than glucose to form AGEs.
RAGE ligands have the capacity to injure the gut epithelium [120], which may facilitate aberrant antigen presentation and food allergy. HMBG1–RAGE interactions are important in antigen uptake and presentation, T-cell, IgE responses [121]and Th2 polarization [122]. HMBG1 has been demonstrated to increase mast cell accumulation, and AGEs are capable of activating mast cells and promoting the release of proallergic mediators [123].
Epidemiological correlates of food allergy and high-sugar consumption in pregnancy are related to higher rates of inhalant and food allergies in offspring [18]. Urban eating patterns involve increased consumption of sugar and processed foods, and there is a corresponding higher rate of food allergies [124]. Although this observational data does not prove causation, it is worthy of consideration when assessing food allergy prevention and management.
Another possible axis for considerations of the effect of dietary AGEs is the microbiome, and high AGE consumption is shown to result in deleterious effects to the microbiome [125].
The Western pattern diet is estimated to result in consumption of 7 to 8 kg of synthetic chemical additives, including preservatives, acidity regulators, colorants, and emulsifiers [126],which have been proposed to contribute to food allergy via modification of the gut microbiome [127].
6.3. Micronutrients: vitamin D and omega-3 fatty acids
Low vitamin D levels are linked to increased risk of food allergy and anaphylaxis, evident from epidemiological data that indicate living in regions farther away from the equator can increase the risk of peanut allergy by up to 6-fold [128]. Birth in winter and spring (associated with lower levels of vitamin D in mother and offspring) is associated with increased risk of food allergy [129].
Long-chain omega-3 fatty acids (LCn3s) are mainly sourced either directly or via supplements from fish oils and include eicosapentaenoic acid and docosahexaenoic acid. Another source of LCn3s is from plants such as walnut, chia seeds, Brussels sprouts, and algae in the form of alpha‐linolenic acid. Fatty acids are a source material for eicosanoids such as prostaglandins and leukotrienes, and LCn3s are reported to result in the production of less inflammatory products than omega-3 fatty acids (LCn6s), which appear as a frequently consumed fat in the Western diet. Antenatal consumption of fish oil during pregnancy and lactation is linked to lower levels of prostaglandin E2, and this has been suggested to alter the Th2 balance and risk for atopy in infants [130].
Another mechanism of response is due to dietary lipids and their interaction on gut microbiota [131]. Bacterial endotoxins cause systemic inflammation via endotoxemia (which is highest after meals), and this can be modified by dietary lipids [132, 133]. High-fat diet influences microbial composition, endotoxemia, and impairment of barrier function [134-136], and this can be modified by omega-3 polyunsaturated fatty acids (PUFAs) [133]. Inflammatory responses are reduced via LCn3s becoming incorporated into membrane signaling platforms called lipid rafts, which influences intracellular and intercellular signaling of immune cells [137-139]. G-protein coupled receptors can bind fatty acids such as GPR120, which influences nuclear factor B signaling and downstream genes [140].
Data on consumption of LCn3s in the antenatal period and early infancy have been reproduced in many studies worldwide for prevention of inhalant allergies, as summarized in recent reviews [141, 142]. The data on food allergy are not as reproducible or as strong. A murine study has shown that a diet comprising 13% salmon oil could partially prevent hen’s egg allergy [143]. Another murine study with tuna oil showed a reduction in experimental CM and peanut allergy associated with in an increase in T regulatory cells with a reduction of both Th1 and Th2 activation [144, 145]. Several human studies have reported supplementation of LCn3s in pregnancy and in infancy can be associated with a reduction in atopic disease and food sensitization, particularly to hens egg [41, 146-149]. A meta-analysis [148] of 3 studies [41, 146, 149] examining hen’s egg sensitization reported an effect with the RR of hen’s egg sensitization in infancy (RR, 0.54; 95% CI, 0.39–0.75; P < 0.0003 and sensitization to any food RR 0.58; 0.45–0.75; <0.0001. This contrasts with other studies that did not find any effect of LCn3 supplementation [150, 151]. It is worth noting that 2 of these studies, which showed benefits came from Australia, where an early life rate of raw egg white sensitization was reported to be 16.5% (95% CI, 15.1–17.9) and challenge-proven raw egg allergy to be 8.9% (95% CI, 7.8–10.0), such that disease incidence may influence the results of an intervention [152]. There is variability across studies in the amount of LCn3 consumed and when considering lipids and their possible benefits, as well as consideration of omega 6 fatty acid intake [26]. Mothers cannot expect to supplement themselves and their offspring from a poor diet. Another possible benefit of LCn3s is that they are estimated to contain 70.6 IU vitamin D3/mL [153], which is found, as outlined in this review, to have a strong association with reduced risk of food allergy, particularly in lipid form. It has been recommended that infants and children who have fish allergy can consume LCn3s in plant forms [154].
7. Summary and conclusion
Food allergy guidelines have changed over the past 2 decades. As clear risk factors for the development of food allergy are lacking, food allergy prevention guidelines are relevant to all families in that all families may be at some inherent risk today. Pregnant and BF women are not recommended to avoid food allergens. BF is not associated with reduced prevalence of food allergies, but it is recommended for all mother–infant dyads due to a range of other health outcomes. Peanut and cooked egg should be introduced as soon as solid food introduction commences, but there is no need to delay the introduction of other allergenic foods, and infants should be fed family foods. Once an allergen is introduced, frequent and continued intake is required to maintain tolerance. Mechanistic studies link maternal and infant diet with the microbiome, epigenetic, and immunological indices, but studies are required to establish clear pathways of interaction.
Conflicts of interest
Dr. Fleischer’s institution has received research support from Aimmune Therapeutics and DBV Technologies; serves as a nonpaid member of the Medical Advisory Board for Food Allergy and Anaphylaxis Connection Team and the Medical Advisory Council National Peanut Board; receives royalties from UpToDate; and serves as a consultant for Aquestive, DBV Technologies, Genentech, and Nasus, all of which are outside of this submitted work. Dr. Smith reports personal fees from the Nestle Nutrition Institute and speaker fee from Danone and Bayer outside of the submitted work. Dr. Venter reports grants from Reckitt Benckiser Food Allergy Research and Education, National Peanut Board; personal fees from Reckitt Benckiser, Nestle Nutrition Institute, Danone, Abbott Nutrition, Else Nutrition, Before Brands and Owen outside the submitted work.
Author contributions
Each author drafted different sections of the article. The article was then circulated, and the authors approved the final version of the article.
Footnotes
Published online 30 March 2023
References
- 1.Sampath V, Abrams EM, Adlou B, Sampath V, Abrams EM, Adlou B, Akdis C, Akdis M, Brough HA, Chan S, Chatchatee P, Chinthrajah RS, Cocco RR, Deschildre A, Eigenmann P, Galvan C, Gupta R, Hossny E, Koplin JJ, Lack G, Levin M, Shek LP, Makela M, Mendoza-Hernandez D, Muraro A, Papadopoulous NG, Pawankar R, Perrett KP, Roberts G, Sackesen C, Sampson H, Tang MLK, Togias A, Venter C, Warren CM, Wheatley LM, Wong GWK, Beyer K, Nadeau KC, Renz H. Food allergy across the globe. J Allergy Clin Immunol 2021;148:1347–64. [DOI] [PubMed] [Google Scholar]
- 2.Fleischer DM, Chan ES, Venter C, Spergel JM, Abrams EM, Stukus D, Groetch M, Shaker M, Greenhawt M. A consensus approach to the primary prevention of food allergy through nutrition: guidance from the American Academy of Allergy, Asthma, and Immunology; American College of Allergy, Asthma, and Immunology; and the Canadian Society for Allergy and Clinical Immunology. J Allergy Clin Immunol Pract 2021;9:22–43.e4. [DOI] [PubMed] [Google Scholar]
- 3.Halken S, Muraro A, de Silva D, Halken S, Muraro A, de Silva D, Khaleva E, Angier E, Arasi S, Arshad H, Bahnson HT, Beyer K, Boyle R, du Toit G, Ebisawa M, Eigenmann P, Grimshaw K, Hoest A, Jones C, Lack G, Nadeau K, O'Mahony L, Szajewska H, Venter C, Verhasselt V, Wong GWK, Roberts G; European Academy of Allergy and Clinical Immunology Food Allergy and Anaphylaxis Guidelines Group. EAACI guideline: preventing the development of food allergy in infants and young children (2020 update). Pediatr Allergy Immunol 2021;32:843–858. [DOI] [PubMed] [Google Scholar]
- 4.Ebisawa M, Ito K, Fujisawa T; Committee for Japanese Pediatric Guideline for Food Allergy, The Japanese Society of Pediatric Allergy and Clinical Immunology; Japanese Society of Allergology. Japanese guidelines for food allergy 2020. Allergol 2020;69:370–86. [DOI] [PubMed] [Google Scholar]
- 5.Abrams EM, Hildebrand K, Blair B, Chan ES. Timing of introduction of allergenic solids for infants at high risk. Paediatr Child Health 2019;24:56–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tham EH, Shek LP, Van Bever HP, Vichyanond P, Ebisawa M, Wong GW, Lee BW; Asia Pacific Association of Pediatric Allergy Respirology & Immunology (APAPARI). Early introduction of allergenic foods for the prevention of food allergy from an Asian perspective-An Asia Pacific Association of Pediatric Allergy, Respirology & Immunology (APAPARI) consensus statement. Pediatr Allergy Immunol 2018;29:18–27. [DOI] [PubMed] [Google Scholar]
- 7.Netting MJ, Campbell DE, Koplin JJ, Beck KM, McWilliam V, Dharmage SC, Tang MLK, Ponsonby A-L, Prescott SL, Vale S, Loh RKS, Makrides M, Allen KJ; Centre for Food and Allergy Research, the Australasian Society of Clinical Immunology and Allergy, the National Allergy Strategy, and the Australian Infant Feeding Summit Consensus Group. An Australian consensus on infant feeding guidelines to prevent food allergy: outcomes from the Australian Infant Feeding Summit. J Allergy Clin Immunol Pract 2017, 5:1617–1624. [DOI] [PubMed] [Google Scholar]
- 8.Arshad SH, Matthews S, Gant C, Hide DW. Effect of allergen avoidance on development of allergic disorders in infancy. Lancet 1992;339:1493–7. [DOI] [PubMed] [Google Scholar]
- 9.Australasian Society of Clinical Immunology and Allergy guidelines for infant feeding and allergy prevention. 2016. Available at: https://www.allergy.org.au/patients/fast-facts/introducing-foods-and-allergy-prevention. Accessed February 2023. [DOI] [PubMed] [Google Scholar]
- 10.Falth-Magnusson K, Kjellman NI. Allergy prevention by maternal elimination diet during late pregnancy–a 5-year follow-up of a randomized study. J Allergy Clin Immunol 1992;89:709–13. [DOI] [PubMed] [Google Scholar]
- 11.Lilja G, Dannaeus A, Foucard T, Graff-Lonnevig V, Johansson SG, Oman H. Effects of maternal diet during late pregnancy and lactation on the development of atopic diseases in infants up to 18 months of age–in-vivo results. Clin Exp Allergy 1989;19:473–9. [DOI] [PubMed] [Google Scholar]
- 12.Zeiger RS, Heller S, Mellon MH, Forsythe AB, O’Connor RD, Hamburger RN, Schatz M. Effect of combined maternal and infant food-allergen avoidance on development of atopy in early infancy: a randomized study.[Erratum appears in J Allergy Clin Immunol 1989 Nov;84(5 Pt 1):677]. J Allergy Clin Immunol 1989;84:72–89. [DOI] [PubMed] [Google Scholar]
- 13.Odelram H, Vanto T, Jacobsen L, Kjellman NI. Whey hydrolysate compared with cow’s milk-based formula for weaning at about 6 months of age in high allergy-risk infants: effects on atopic disease and sensitization. Allergy 1996;51:192–5. [PubMed] [Google Scholar]
- 14.Garcia-Larsen V, Ierodiakonou D, Jarrold K, Cunha S, Chivinge J, Robinson Z, Geoghegan N, Ruparelia A, Devani P, Trivella M, Leonardi-Bee J, Boyle RJ. Diet during pregnancy and infancy and risk of allergic or autoimmune disease: a systematic review and meta-analysis. PLoS Med 2018;15:e1002507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fleischer DM, Sicherer S, Greenhawt M, Campbell D, Chan E, Muraro A, Halken S, Katz Y, Ebisawa M, Eichenfield L, Sampson H, Lack G, Toit GD, Roberts G, Bahnson H, Feeney M, Hourihane J, Spergel J, Young M, As’aad A, Allen K, Prescott S, Kapur S, Saito H, Agache I, Akdis CA, Arshad H, Beyer K, Dubois A, Eigenmann P, Fernandez-Rivas M, Grimshaw K, Hoffman-Sommergruber K, Host A, Lau S, O’Mahony L, Mills C, Papadopoulos N, Venter C, Agmon-Levin N, Kessel A, Antaya R, Drolet B, Rosenwasser L; American Academy of Allergy Asthma & Immunology; American Academy of Pediatrics, American College of Allergy; Asthma & Immunology, Australasian Society of Clinical Immunology and Allergy; Canadian Society of Allergy and Clinical Immunology; European Academy of Allergy and Clinical Immunology; Israel Association of Allergy and Clinical Immunology; Japanese Society for Allergology; Society for Pediatric Dermatology; World Allergy Organization. Consensus communication on early peanut introduction and the prevention of peanut allergy in high-risk infants. J Allergy Clin Immunol 2015;136:258–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Greer FR, Sicherer SH, Burks AW, Committee on Nutrition, Section on Allergy and Immunology. The effects of early nutritional interventions on the development of atopic disease in infants and children: the role of maternal dietary restriction, breastfeeding, hydrolyzed formulas, and timing of introduction of allergenic complementary foods. Pediatrics 2019;143:e20190281. [DOI] [PubMed] [Google Scholar]
- 17.Togias A, Cooper SF, Acebal ML, Togias A, Cooper SF, Acebal ML, Assa’ad A, Baker JR, Jr, Beck LA, Block J, Byrd-Bredbenner C, Chan ES, Eichenfield LF, Fleischer DM, Fuchs GJ, 3rd, Furuta GT, Greenhawt MJ, Gupta RS, Habich M, Jones SM, Keaton K, Muraro A, Plaut M, Rosenwasser LJ, Rotrosen D, Sampson HA, Schneider LC, Sicherer SH, Sidbury R, Spergel J, Stukus DR, Venter C, Boyce JA. Addendum guidelines for the prevention of peanut allergy in the United States: report of the National Institute of Allergy and Infectious Diseases-sponsored expert panel. J Allergy Clin Immunol 2017;139:29–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Turner PJ, Feeney M, Meyer R, Perkin MR, Fox AT. Implementing primary prevention of food allergy in infants: new BSACI guidance published. Clin Exp Allergy 2018;48:912–5. [DOI] [PubMed] [Google Scholar]
- 19.Assessing the health benefits and risks of the introduction of peanut and hen’s egg into the infant diet before six months of age in the UK. A joint statement from the scientific advisory committee on nutrition and the committee on toxicity of chemicals in food, consumer products and the environment. 2018. Available at: https://cot.food.gov.uk/sites/default/files/jointsacncotallergystatement-april2018.pdf. Accessed February 2023.
- 20.Venter C, Brown KR, Maslin K, Palmer D, Maternal dietary intake in pregnancy and lactation and allergic disease outcomes in offspring. Pediatr Allergy Immunol 2017;28: 135–43. [DOI] [PubMed] [Google Scholar]
- 21.Grimshaw KE, Maskell J, Oliver EM, Morris RCG, Foote KD, Mills ENC, Roberts G, Margetts BM. Introduction of complementary foods and the relationship to food allergy. Pediatrics 2013;132:e1529–38. [DOI] [PubMed] [Google Scholar]
- 22.Venter C, Maslin K, Dean T, Arshad SH. Does concurrent breastfeeding alongside the introduction of solid food prevent the development of food allergy?. J Nutr Sci 2016;5:e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Azad MB, Dharma C, Simons E, Tran M, Reyna ME, Dai R, Becker AB, Marshall J, Mandhane PJ, Turvey SE, Moraes TJ, Lefebvre DL, Subbarao P, Sears MR. Reduced peanut sensitization with maternal peanut consumption and early peanut introduction while breastfeeding. J Dev Orig Health Dis 2020:1–8. [DOI] [PubMed] [Google Scholar]
- 24.Pitt TJ, Becker AB, Chan-Yeung M, Chan ES, Watson WTA, Chooniedass R, Azad MB. Reduced risk of peanut sensitization following exposure through breast-feeding and early peanut introduction. J Allergy Clin Immunol 2018;141:620–5 e1. [DOI] [PubMed] [Google Scholar]
- 25.Venter C, Palumbo MP, Glueck DH, Sauder KA, Perng W, O’Mahony L, Pickett K, Greenhawt M, Fleischer DM, Dabelea D. Comparing the diagnostic accuracy of measures of maternal diet during pregnancy for offspring allergy outcomes: the healthy start study. J Allergy Clin Immunol Pract 2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Venter C, Greenhawt M, Meyer RW, Agostoni C, Reese I, du Toit G, Feeney M, Maslin K, Nwaru BI, Roduit C, Untersmayr E, Vlieg-Boerstra B, Iöll P-S, Roberts GC, Smith P, Akdis CA, Agache I, Ben-Adallah M, Bischoff S, Frei R, Garn H, Grimshaw K, Hoffmann-Sommergruber K, Lunjani N, Muraro A, Poulsen LK, Renz H, Sokolowska M, Stanton C, O’Mahony L. EAACI position paper on diet diversity in pregnancy, infancy and childhood: novel concepts and implications for studies in allergy and asthma. Allergy 2020;75:497–523. [DOI] [PubMed] [Google Scholar]
- 27.Subar AF, Dodd KW, Guenther PM, Kipnis V, Midthune D, McDowell M, Tooze JA, Freedman LS, Krebs-Smith SM. The food propensity questionnaire: concept, development, and validation for use as a covariate in a model to estimate usual food intake. J Am Diet Assoc 2006;106:1556–63. [DOI] [PubMed] [Google Scholar]
- 28.Dietary Guidelines for Americans: DGA 2020 - 2025. 2020. Available at: https://www.dietaryguidelines.gov/sites/default/files/2020-12/Dietary_Guidelines_for_Americans_2020-2025.pdf. Accessed January 2031.
- 29.Lange NE, Rifas-Shiman SL, Camargo CA, Jr, Gold DR, Gillman MW, Litonjua AA. Maternal dietary pattern during pregnancy is not associated with recurrent wheeze in children. J Allergy Clin Immunol 2010;126:250–5,5 e1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moonesinghe H, Patil VK, Dean T, Arshad SH, Glasbey G, Grundy J, Venter C. Association between healthy eating in pregnancy and allergic status of the offspring in childhood. Ann Allergy Asthma Immunol 2016;116:163–5. [DOI] [PubMed] [Google Scholar]
- 31.Chen LW, Lyons B, Navarro P, Shivappa N, Mehegan J, Murrin CM, Hébert JR, Kelleher CC, Phillips CM. Maternal dietary inflammatory potential and quality are associated with offspring asthma risk over 10-year follow-up: the Lifeways Cross-Generation Cohort Study. Am J Clin Nutr 2020;111:440–7. [DOI] [PubMed] [Google Scholar]
- 32.Hanson C, Rifas-Shiman SL, Shivappa N, Wirth MD, Hebert JR, Gold D, Camargo CA, Sen S, Sordillo JE, Oken E, Litonjua AA. Associations of prenatal dietary inflammatory potential with childhood respiratory outcomes in project viva. J Allergy Clin Immunol Pract 2020;8:945–952.e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Castro-Rodriguez JA, Ramirez-Hernandez M, Padilla O, Pacheco-Gonzalez RM, Perez-Fernandez V, Garcia-Marcos L. Effect of foods and Mediterranean diet during pregnancy and first years of life on wheezing, rhinitis and dermatitis in preschoolers. Allergol Immunopathol 2016;44:400–9. [DOI] [PubMed] [Google Scholar]
- 34.Chatzi L, Garcia R, Roumeliotaki T, Basterrechea M, Begiristain H, Iñiguez C, Vioque J, Kogevinas M, Sunyer J; INMA study group. Mediterranean diet adherence during pregnancy and risk of wheeze and eczema in the first year of life: INMA (Spain) and RHEA (Greece) mother-child cohort studies. Br J Nutr 2013;110:2058–68. [DOI] [PubMed] [Google Scholar]
- 35.Chatzi L, Torrent M, Romieu I, Garcia-Esteban R, Ferrer C, Vioque J, Kogevinas M, Sunyer J. Mediterranean diet in pregnancy is protective for wheeze and atopy in childhood. Thorax 2008;63:507–13. [DOI] [PubMed] [Google Scholar]
- 36.Bedard A, Northstone K, Henderson AJ, Shaheen SO. Mediterranean diet during pregnancy and childhood respiratory and atopic outcomes: birth cohort study. Eur Respir J 2020;55:1901215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Venter C, Palumbo MP, Glueck DH, Sauder KA, O'Mahony L, Fleischer DM, Ben-Abdallah M, Ringham BM, Dabelea D. The maternal diet index in pregnancy is associated with offspring allergic diseases: the healthy start study. Allergy 2022;77:162–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tuokkola J, Luukkainen P, Tapanainen H, Kaila M, Vaarala O, Kenward MG, Virta LJ, Veijola R, Simell O, Ilonen J, Knip M, Virtanen SM. Maternal diet during pregnancy and lactation and cow’s milk allergy in offspring. Eur J Clin Nutr 2016;70:554–9. [DOI] [PubMed] [Google Scholar]
- 39.Venter C, Agostoni C, Arshad SH, Ben-Abdallah M, Toit GD, Fleischer DM, Greenhawt M, Glueck DH, Groetch M, Lunjani N, Maslin K, Maiorella A, Meyer R, Antonella M, Netting MJ, Nwaru BI, Palmer DJ, Palumbo MP, Roberts G, Roduit C, Smith P, Untersmayr E, Vanderlinden LA, O’Mahony L. Dietary factors during pregnancy and atopic outcomes in childhood: a systematic review from the European Academy of Allergy and Clinical Immunology. Pediatr Allergy Immunol 2020;31:889–912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Vahdaninia M, Mackenzie H, Dean T, Helps S. Omega-3 LCPUFA supplementation during pregnancy and risk of allergic outcomes or sensitization in offspring: a systematic review and meta-analysis. Ann Allergy Asthma Immunol 2019;122:302–13 e2. [DOI] [PubMed] [Google Scholar]
- 41.Furuhjelm C, Warstedt K, Larsson J, Fredriksson M, Böttcher MF, Fälth-Magnusson K, Duchén K. Fish oil supplementation in pregnancy and lactation may decrease the risk of infant allergy. Acta Paediatr 2009;98:1461–7. [DOI] [PubMed] [Google Scholar]
- 42.Goldring ST, Griffiths CJ, Martineau AR, Robinson S, Yu C, Poulton S, Kirkby JC, Stocks J, Hooper R, Shaheen SO, Warner JO, Boyle RJ. Prenatal vitamin d supplementation and child respiratory health: a randomised controlled trial. PLoS One 2013;8:e66627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kukkonen AK, Savilahti EM, Haahtela T, Savilahti E, Kuitunen M. Ovalbumin-specific immunoglobulins A and G levels at age 2 years are associated with the occurrence of atopic disorders. Clin Exp Allergy 2011;41:1414–21. [DOI] [PubMed] [Google Scholar]
- 44.de Silva D, Halken S, Singh C, Muraro A, Angier E, Arasi S, Arshad H, Beyer K, Boyle R, du Toit G, Eigenmann P, Grimshaw K, Hoest A, Jones C, Khaleva E, Lack G, Szajewska H, Venter C, Verhasselt V, Roberts G; European Academy of Allergy Clinical Immunology Food Allergy Anaphylaxis Guidelines Group. Preventing food allergy in infancy and childhood: systematic review of randomised controlled trials. Pediatr Allergy Immunol 2020;31:813–26. [DOI] [PubMed] [Google Scholar]
- 45.James DC, Dobson B; American Dietetic Association. Position of the American Dietetic Association: promoting and supporting breastfeeding. J Am Diet Assoc 2005;105:810–8. [DOI] [PubMed] [Google Scholar]
- 46.Osborn DA, Sinn JK, Jones LJ. Infant formulas containing hydrolysed protein for prevention of allergic disease. Cochrane Database Syst Rev 2018;10:Cd003664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Du Toit G, Roberts G, Sayre PH, Bahnson HT, Radulovic S, Santos AF, Brough HA, Phippard D, Basting M, Feeney M, Turcanu V, Sever ML, Gomez Lorenzo M, Plaut M, Lack G; LEAP Study Team. Randomized trial of peanut consumption in infants at risk for peanut allergy. N Engl J Med 2015;372:803–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Palmer DJ, Metcalfe J, Makrides M, Gold MS, Quinn P, West CE, Loh R, Prescott SL. Early regular egg exposure in infants with eczema: a randomized controlled trial. J Allergy Clin Immunol 2013;132:387–92 e1. [DOI] [PubMed] [Google Scholar]
- 49.Natsume O, Kabashima S, Nakazato J, Yamamoto-Hanada K, Narita M, Kondo M, Saito M, Kishino A, Takimoto T, Inoue E, Tang J, Kido H, Wong GWK, Matsumoto K, Saito H, Ohya Y; PETIT Study Team. Two-step egg introduction for prevention of egg allergy in high-risk infants with eczema (PETIT): a randomised, double-blind, placebo-controlled trial. Lancet 2017;389:276–86. [DOI] [PubMed] [Google Scholar]
- 50.Palmer DJ, Sullivan TR, Gold MS, Prescott SL, Makrides M. Randomized controlled trial of early regular egg intake to prevent egg allergy. J Allergy Clin Immunol 2017;139:1600–7. [DOI] [PubMed] [Google Scholar]
- 51.Wei-Liang Tan J, Valerio C, Barnes EH, Turner PJ, Van Asperen PA, Kakakios AM, Campbell DE; Beating Egg Allergy Trial (BEAT) Study Group. A randomized trial of egg introduction from 4 months of age in infants at risk for egg allergy. J Allergy Clin Immunol 2017;139:1621–8 e8. [DOI] [PubMed] [Google Scholar]
- 52.Bellach J, Schwarz V, Ahrens B, Trendelenburg V, Aksünger O, Kalb B, Niggemann B, Keil T, Beyer K. Randomized placebo-controlled trial of hen’s egg consumption for primary prevention in infants. J Allergy Clin Immunol 2017;139:1591–9 e2. [DOI] [PubMed] [Google Scholar]
- 53.Urashima M, Mezawa H, Okuyama M, Urashima T, Hirano D, Gocho N, Tachimoto H. Primary prevention of cow’s milk sensitization and food allergy by avoiding supplementation with cow’s milk formula at birth: a randomized clinical trial. JAMA Pediatr 2019;173:1137–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Sakihara T, Otsuji K, Arakaki Y, Hamada K, Sugiura S, Ito K. Randomized trial of early infant formula introduction to prevent cow’s milk allergy. J Allergy Clin Immunol 2021;147:224–32.e8. [DOI] [PubMed] [Google Scholar]
- 55.Perkin MR, Logan K, Tseng A, Raji B, Ayis S, Peacock J, Brough H, Marrs T, Radulovic S, Craven J, Flohr C, Lack G; EAT Study Team. Randomized trial of introduction of allergenic foods in breast-fed infants. N Engl J Med 2016;374:1733–43. [DOI] [PubMed] [Google Scholar]
- 56.Skjerven HO, Lie A, Vettukattil R, Rehbinder EM, LeBlanc M, Asarnoj A, Carlsen K-H, Åshild Despriee W, Färdig M, Gerdin SW, Granum B, Gudmundsdóttir HK, Haugen G, Hedlin G, Håland G, Jonassen CM, Landrø L, Olsson Mägi C-A, Olsen IC, Rudi K, Saunders CM, Skram MK, Staff AC, Söderhäll C, Tedner SG, Aadalen S, Aaneland H, Nordlund B, Lødrup Carlsen KC. Early food intervention and skin emollients to prevent food allergy in young children (PreventADALL): a factorial, multicentre, cluster-randomised trial. Lancet 2022;399:2398–411. [DOI] [PubMed] [Google Scholar]
- 57.Ierodiakonou D, Garcia-Larsen V, Logan A, Groome A, Cunha S, Chivinge J, Robinson Z, Geoghegan N, Jarrold K, Reeves T, Tagiyeva-Milne N, Nurmatov U, Trivella M, Leonardi-Bee J, Boyle RJ. Timing of allergenic food introduction to the infant diet and risk of allergic or autoimmune disease: a systematic review and meta-analysis. JAMA 2016;316:1181–92. [DOI] [PubMed] [Google Scholar]
- 58.Ruel MT. Is dietary diversity an indicator of food security or dietary quality? A review of measurement issues and research needs. International Food Policy Research Institute; 2002:1–58. [DOI] [PubMed] [Google Scholar]
- 59.Krebs-Smith SM, Smiciklas-Wright H, Guthrie HA, Krebs-Smith J. The effects of variety in food choices on dietary quality. J Am Diet Assoc 1987;87:897–903. [PubMed] [Google Scholar]
- 60.Roche ML, Creed-Kanashiro HM, Tuesta I, Kuhnlein HV. Traditional food diversity predicts dietary quality for the Awajun in the Peruvian Amazon. Public Health Nutrition 2008;11:457–65. [DOI] [PubMed] [Google Scholar]
- 61.Lachat C, Raneri JE, Smith KW, Kolsteren P, Van Damme P, Verzelen K, Penafiel D, Vanhove W, Kennedy G, Hunter D, Odhiambo FO, Ntandou-Bouzitou G, De Baets B, Ratnasekera D, Ky HT, Remans R, Termote C. Dietary species richness as a measure of food biodiversity and nutritional quality of diets. Proc Natl Acad Sci U S A 2018;115:127–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Remans R, Flynn DF, DeClerck F, Diru W, Fanzo J, Gaynor K, Lambrecht I, Mudiope J, Mutuo PK, Nkhoma P, Siriri D, Sullivan C, Palm CA. Assessing nutritional diversity of cropping systems in African villages. PLoS ONE [Electronic Resource] 2011;6:e21235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Bezerra IN, Sichieri R. Household food diversity and nutritional status among adults in Brazil. Int J Behav Nutr Phys Act 2011;8:22. doi: 10.1186/1479-5868-8-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Onyango A, Koski KG, Tucker KL. Food diversity versus breastfeeding choice in determining anthropometric status in rural Kenyan toddlers. Int J Epidemiol 1998;27:484–9. [DOI] [PubMed] [Google Scholar]
- 65.Ntwenya JE, Kinabo J, Msuya J, Mamiro P, Mamiro D, Njoghomi E, Liwei P, Huang M. Rich food biodiversity amid low consumption of food items in Kilosa District, Tanzania. Food Nutr Bull 2017;38:501–11. [DOI] [PubMed] [Google Scholar]
- 66.Jones AD. On-farm crop species richness is associated with household diet diversity and quality in subsistence- and market-oriented farming households in Malawi. J Nutr 2017;147:86–96. [DOI] [PubMed] [Google Scholar]
- 67.Chomat AM, Solomons NW, Koski KG, Wren HM, Vossenaar M, Scott ME. Quantitative methodologies reveal a diversity of nutrition, infection/illness, and psychosocial stressors during pregnancy and lactation in Rural Mam-Mayan Mother-Infant Dyads from the Western Highlands of Guatemala. Food Nutr Bull 2015;36:415–40. [DOI] [PubMed] [Google Scholar]
- 68.Rukundo PM, Andreassen BA, Kikafunda J, Rukooko B, Oshaug A, Iversen PO. Household food insecurity and diet diversity after the major 2010 landslide disaster in Eastern Uganda: a cross-sectional survey. Br J Nutr 2016;115:718–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Christian AK, Marquis GS, Colecraft EK, Lartey A, Sakyi-Dawson O, Ahunu BK, Butler LM. Caregivers’ nutrition knowledge and attitudes are associated with household food diversity and children’s animal source food intake across different agro-ecological zones in Ghana. Br J Nutr 2016;115:351–60. [DOI] [PubMed] [Google Scholar]
- 70.Ey Chua EY, Zalilah MS, Ys Chin YS, Norhasmah S. Dietary diversity is associated with nutritional status of Orang Asli children in Krau Wildlife Reserve, Pahang. Malays J Nutr 2012;18:1–13. [PubMed] [Google Scholar]
- 71.Wright MJ, Bentley ME, Mendez MA, Adair LS. The interactive association of dietary diversity scores and breast-feeding status with weight and length in Filipino infants aged 6-24 months. Public Health Nutr 2015;18:1762–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Woo JG, Herbers PM, McMahon RJ, Davidson BS, Ruiz-Palacios GM, Peng Y-M, Morrow AL. Longitudinal development of infant complementary diet diversity in 3 international cohorts. J. Pediatr 2015;167:969–74.e1. [DOI] [PubMed] [Google Scholar]
- 73.Chandrasekhar S, Aguayo VM, Krishna V, Nair R. Household food insecurity and children’s dietary diversity and nutrition in India. evidence from the comprehensive nutrition survey in Maharashtra. Matern Child Nutr 2017; Suppl 2:e12447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Agize A, Jara D, Dejenu G. Level of knowledge and practice of mothers on minimum dietary diversity practices and associated factors for 6-23-month-old children in Adea Woreda, Oromia, Ethiopia. Biomed Res Int 2017;2017:7204562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gewa CA, Murphy SP, Weiss RE, Neumann CG. Determining minimum food intake amounts for diet diversity scores to maximize associations with nutrient adequacy: an analysis of schoolchildren’s diets in rural Kenya. Public Health Nutr 2014;17:2667–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Shamim AA, Mashreky SR, Ferdous T, Davidson BS, Ruiz-Palacios GM, Peng Y-M, Morrow AL. Pregnant women diet quality and its sociodemographic determinants in southwestern Bangladesh. Food Nutr Bull 2016;37:14–26. [DOI] [PubMed] [Google Scholar]
- 77.Leroy JL, Razak AA, Habicht JP. Only children of the head of household benefit from increased household food diversity in northern Ghana. J Nutr 2008;138:2258–63. [DOI] [PubMed] [Google Scholar]
- 78.Msaki MM, Hendriks SL. Do food quality and food quantity talk the same? Lesson from household food security study in Embo, South Africa. J Am Coll Nutr 2013;32:165–76. [DOI] [PubMed] [Google Scholar]
- 79.Hatloy A, Torheim LE, Oshaug A. Food variety–a good indicator of nutritional adequacy of the diet? A case study from an urban area in Mali, West Africa. Eur J Clin Nutr 1998;52:891–8. [DOI] [PubMed] [Google Scholar]
- 80.Mok E, Vanstone CA, Gallo S, Li P, Constantin E, Weiler HA. Diet diversity, growth and adiposity in healthy breastfed infants fed homemade complementary foods. Int J Obes 2017;41:776–82. [DOI] [PubMed] [Google Scholar]
- 81.Conklin AI, Monsivais P, Khaw KT, Wareham NJ, Forouhi NG. Dietary diversity, diet cost, and incidence of type 2 diabetes in the united kingdom: a prospective cohort study.[Erratum appears in PLoS Med. 2016 Aug;13(8):e1002123; PMID: 27541996]. PLoS Med 2016;13:e1002085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Isa F, Xie LP, Hu Z, Zhong Z, Hemelt M, Reulen RC, Wong YC, Tam P-C, Yang K, Chai C, Zeng X, Deng Y, Zhong W-D, Zeegers MP. Dietary consumption and diet diversity and risk of developing bladder cancer: results from the South and East China case-control study. Cancer Causes Control 2013;24:885–95. [DOI] [PubMed] [Google Scholar]
- 83.Hatloy A, Hallund J, Diarra MM, Oshaug A. Food variety, socioeconomic status and nutritional status in urban and rural areas in Koutiala (Mali). Public Health Nutr 2000;3:57–65. [DOI] [PubMed] [Google Scholar]
- 84.Motbainor A, Worku A, Kumie A. Stunting is associated with food diversity while wasting with food insecurity among underfive children in East and West Gojjam Zones of Amhara Region, Ethiopia. PLoS ONE [Electronic Resource] 2015;10:e0133542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Venter C, Maslin K, Holloway JW, Silveira LJ, Fleischer DM, Dean T, Arshad SH. Different measures of diet diversity during infancy and the association with childhood food allergy in a UK Birth cohort study. J Allergy Clin Immunol Pract 2020;8:2017–26. [DOI] [PubMed] [Google Scholar]
- 86.Roduit C, Frei R, Depner M, Schaub B, Loss G, Genuneit J, Pfefferle P, Hyvärinen A, Karvonen AM, Riedler J, Dalphin J-C, Pekkanen J, von Mutius E, Braun-Fahrländer C, Lauener R; PASTURE study group. Increased food diversity in the first year of life is inversely associated with allergic diseases. J Allergy Clin Immunol 2014;133:1056–64. [DOI] [PubMed] [Google Scholar]
- 87.Nwaru BI, Takkinen HM, Niemela O, Kaila M, Erkkola M, Ahonen S, Tuomi H, Haapala A-M, Kenward MG, Pekkanen J, Lahesmaa R, Kere J, Simell O, Veijola R, Ilonen J, Hyöty H, Knip M, Virtanen SM. Introduction of complementary foods in infancy and atopic sensitization at the age of 5 years: timing and food diversity in a Finnish birth cohort. Allergy 2013;68:507–16. [DOI] [PubMed] [Google Scholar]
- 88.Zhong C, Guo J, Tan T, Wang H, Lin L, Gao D, Li Q, Sun G, Xiong G, Yang X, Hao L, Yang H, Yang N. Increased food diversity in the first year of life is inversely associated with allergic outcomes in the second year. Pediatr Allergy Immunol 2022;33:e13707. [DOI] [PubMed] [Google Scholar]
- 89.Lee BR, Jung HI, Kim SK, Kwon M, Kim H, Jung M, Kyung Y, Kim BE, Choi S-J, Oh S-Y, Baek S-Y, Kim S, Bae J, Ahn K, Kim J. Dietary Diversity during early infancy increases microbial diversity and prevents egg allergy in high-risk infants. Immune Netw 2022;22:e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Maslin K, Pickett K, Ngo S, Anderson W, Dean T, Venter C. Dietary diversity during infancy and the association with childhood food allergen sensitization. Pediatr Allergy Immunol 2022;33:e13650. [DOI] [PubMed] [Google Scholar]
- 91.Stampfli M, Frei R, Divaret-Chauveau A, Schmausser-Hechfellner E, Karvonen AM, Pekkanen J, Riedler J, Schaub B, von Mutius E, Lauener R, Roduit C; Protection against Allergy–Study in Rural Environments Study Group. Inverse associations between food diversity in the second year of life and allergic diseases. Ann Allergy Asthma Immunol 2022;128:39–45. [DOI] [PubMed] [Google Scholar]
- 92.Quake AZ, Liu TA, D’Souza R, Jackson KG, Woch M, Tetteh A, Sampath V, Nadeau KC, Sindher S, Chinthrajah RS, Cao S. Early introduction of multi-allergen mixture for prevention of food allergy: pilot study. Nutrients 2022;14:737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Bunyavanich S, Shen N, Grishin A, Wood R, Burks W, Dawson P, Jones SM, Leung DYM, Sampson H, Sicherer S, Clemente JC. Early-life gut microbiome composition and milk allergy resolution. J Allergy Clin Immunol 2016;138:1122–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Fazlollahi M, Chun Y, Grishin A, Wood RA, Burks AW, Dawson P, Jones SM, Leung DYM, Sampson HA, Sicherer SH, Bunyavanich S. Early-life gut microbiome and egg allergy. Allergy 2018;73:1515–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Dong P, Feng JJ, Yan DY, Lyu YJ, Xu X. Early-life gut microbiome and cow’s milk allergy- a prospective case - control 6-month follow-up study. Saudi J Biol Sci 2018;25:875–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Feehley T, Plunkett CH, Bao R, Choi Hong SM, Culleen E, Belda-Ferre P, Campbell E, Aitoro R, Nocerino R, Paparo L, Andrade J, Antonopoulos DA, Berni Canani R, Nagler CR. Healthy infants harbor intestinal bacteria that protect against food allergy. Nat Med 2019;25:448–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Azad MB, Konya T, Guttman DS, Field CJ, Sears MR, HayGlass KT, Mandhane PJ, Turvey SE, Subbarao P, Becker AB, Scott JA, Kozyrskyj AL; CHILD Study Investigators. Infant gut microbiota and food sensitization: associations in the first year of life. Clin Exp Allergy 2015;45:632–43. [DOI] [PubMed] [Google Scholar]
- 98.Hua X, Goedert JJ, Pu A, Yu G, Shi J. Allergy associations with the adult fecal microbiota: analysis of the American Gut Project. EBioMedicine 2016;3:172–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Chen CC, Chen KJ, Kong MS, Chang HJ, Huang JL. Alterations in the gut microbiotas of children with food sensitization in early life. Pediatr Allergy Immunol 2016;27:254–62. [DOI] [PubMed] [Google Scholar]
- 100.Stefka AT, Feehley T, Tripathi P, Qiu J, McCoy K, Mazmanian SK, Tjota MY, Seo G-Y, Cao S, Theriault BR, Antonopoulos DA, Zhou L, Chang EB, Fu Y-X, Nagler CR. Commensal bacteria protect against food allergen sensitization. Proc Natl Acad Sci U S A 2014;111:13145–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Roduit C, Frei R, Ferstl R, Loeliger S, Westermann P, Rhyner C, Schiavi E, Barcik W, Rodriguez-Perez N, Wawrzyniak M, Chassard C, Lacroix C, Schmausser-Hechfellner E, Depner M, von Mutius E, Braun-Fahrländer C, Karvonen AM, Kirjavainen PV, Pekkanen J, Dalphin J-C, Riedler J, Akdis C, Lauener R, O’Mahony L; PASTURE/EFRAIM study group. High levels of butyrate and propionate in early life are associated with protection against atopy. Allergy 2019;74:799–809. [DOI] [PubMed] [Google Scholar]
- 102.Tan J, McKenzie C, Vuillermin PJ, Goverse G, Vinuesa CG, Mebius RE, Macia L, Mackay CR. Dietary fiber and bacterial SCFA enhance oral tolerance and protect against food allergy through diverse cellular pathways. Cell Rep 2016;15:2809–24. [DOI] [PubMed] [Google Scholar]
- 103.Thio CL, Chi PY, Lai AC, Chang YJ. Regulation of type 2 innate lymphoid cell-dependent airway hyperreactivity by butyrate. J Allergy Clin Immunol 2018;142:1867–83 e12. [DOI] [PubMed] [Google Scholar]
- 104.Berni Canani R, De Filippis F, Nocerino R, Laiola M, Paparo L, Calignano A, De Caro C, Coretti L, Chiariotti L, Gilbert JA, Ercolini D. Specific signatures of the gut microbiota and increased levels of butyrate in children treated with fermented cow’s milk containing heat-killed lactobacillus paracasei CBA L74. Appl Environ Microbiol 2017;83:e01206–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Arpaia N, Campbell C, Fan X, Dikiy S, van der Veeken J, deRoos P, Liu H, Cross JR, Pfeffer K, Coffer PJ, Rudensky AY. Metabolites produced by commensal bacteria promote peripheral regulatory T-cell generation. Nature 2013;504:451–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Furusawa Y, Obata Y, Hase K. Commensal microbiota regulates T cell fate decision in the gut. Semin Immunopathol 2015;37:17–25. [DOI] [PubMed] [Google Scholar]
- 107.Smith PM, Howitt MR, Panikov N, Michaud M, Gallini CA, Bohlooly-Y M, Glickman JN, Garrett WS. The microbial metabolites, short-chain fatty acids, regulate colonic Treg cell homeostasis. Science 2013;341:569–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Peng L, Li ZR, Green RS, Holzman IR, Lin J. Butyrate enhances the intestinal barrier by facilitating tight junction assembly via activation of AMP-activated protein kinase in Caco-2 cell monolayers. J Nutr 2009;139:1619–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Claesson MJ, Jeffery IB, Conde S, Power SE, O’Connor EM, Cusack S, Harris HMB, Coakley M, Lakshminarayanan B, O’Sullivan O, Fitzgerald GF, Deane J, O’Connor M, Harnedy N, O’Connor K, O’Mahony D, van Sinderen D, Wallace M, Brennan L, Stanton C, Marchesi JR, Fitzgerald AP, Shanahan F, Hill C, Ross RP, O’Toole PW. Gut microbiota composition correlates with diet and health in the elderly. Nature 2012;488:178–84. [DOI] [PubMed] [Google Scholar]
- 110.Laursen MF, Andersen LB, Michaelsen KF, Mølgaard C, Trolle E, Bahl MI, Licht TR. Infant gut microbiota development is driven by transition to family foods independent of maternal obesity. mSphere 2016;1:e00069–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Marrs T, Jo JH, Perkin MR, Rivett DW, Witney AA, Bruce KD, Logan K, Craven J, Radulovic S, Versteeg SA, van Ree R, McLean WHI, Strachan DP, Lack G, Kong HH, Flohr C. Gut microbiota development during infancy: Impact of introducing allergenic foods. J Allergy Clin Immunol 2021;147:613–21.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Zhang Z, Shi L, Pang W, Liu W, Li J, Wang H, Shi G. Dietary fiber intake regulates intestinal microflora and inhibits ovalbumin-induced allergic airway inflammation in a mouse model. PloS one 2016;11:e01477–78-e.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Bach Knudsen KE, Lærke HN, Hedemann MS, Nielsen TS, Ingerslev AK, Gundelund Nielsen DS, Theil PK, Purup S, Hald S, Schioldan AG, Marco ML, Gregersen S, Hermansen K. Impact of diet-modulated butyrate production on intestinal barrier function and inflammation. Nutrients 2018;10:1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Venter C, Meyer RW, Greenhawt M, Pali-Scholl I, Nwaru B, Roduit C, Untersmayr E, Adel-Patient K, Agache I, Agostoni C, Akdis CA, Feeney M, Hoffmann-Sommergruber K, Lunjani N, Grimshaw K, Reese I, Smith PK, Sokolowska M, Vassilopoulou E, Vlieg-Boerstra B, Amara S, Walter J, O’Mahony L. Role of dietary fiber and prebiotics in promoting immune health – an EAACI position paper. Allergy 2022; 77:3185–98. [DOI] [PubMed] [Google Scholar]
- 115.McDonald D, Hyde E, Debelius JW, Morton JT, Gonzalez A, Ackermann G, Aksenov AA, Behsaz B, Brennan C, Chen Y, DeRight Goldasich L, Dorrestein PC, Dunn RR, Fahimipour AK, Gaffney J, Gilbert JA, Gogul G, Green JL, Hugenholtz P, Humphrey G, Huttenhower C, Jackson MA, Janssen S, Jeste DV, Jiang L, Kelley ST, Knights D, Kosciolek T, Ladau J, Leach J, Marotz C, Meleshko D, Melnik AV, Metcalf JL, Mohimani H, Montassier E, Navas-Molina J, Nguyen TT, Peddada S, Pevzner P, Pollard KS, Rahnavard G, Robbins-Pianka A, Sangwan N, Shorenstein J, Smarr L, Song SJ, Spector T, Swafford AD, Thackray VG, Thompson LR, Tripathi A, Vázquez-Baeza Y, Vrbanac A, Wischmeyer P, Wolfe E, Zhu Q; American Gut Consortium; Rob Knight. American Gut: an open platform for citizen science microbiome research. mSystems 2018; 3:e00031–18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Marriott BP, Cole N, Lee E. National estimates of dietary fructose intake increased from 1977 to 2004 in the United States. J Nutr 2009;139:1228s–35s. [DOI] [PubMed] [Google Scholar]
- 117.Smith PK. Do advanced glycation end-products cause food allergy?. Curr Opin Allergy Clin Immunol 2017;17:325–31. [DOI] [PubMed] [Google Scholar]
- 118.Fritz G. RAGE: a single receptor fits multiple ligands. Trends Biochem Sci 2011;36:625–32. [DOI] [PubMed] [Google Scholar]
- 119.Bomback AS, Derebail VK, Shoham DA, Anderson CA, Steffen LM, Rosamond WD, Kshirsagar AV. Sugar-sweetened soda consumption, hyperuricemia, and kidney disease. Kidney Int 2010;77:609–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Sappington PL, Yang R, Yang H, Tracey KJ, Delude RL, Fink MP. HMGB1 B box increases the permeability of Caco-2 enterocytic monolayers and impairs intestinal barrier function in mice. Gastroenterology 2002;123:790–802. [DOI] [PubMed] [Google Scholar]
- 121.Ott C, Jacobs K, Haucke E, Navarrete Santos A, Grune T, Simm A. Role of advanced glycation end products in cellular signaling. Redox Biol 2014;2:411–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Akirav EM, Henegariu O, Preston-Hurlburt P, Schmidt AM, Clynes R, Herold KC. The receptor for advanced glycation end products (RAGE) affects T cell differentiation in OVA induced asthma. PLoS One 2014;9:e95678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Sick E, Brehin S, André P, Coupin G, Landry Y, Takeda K, Gies JP. Advanced glycation end products (AGEs) activate mast cells. Br J Pharmacol 2010;161:442–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Gupta A, Singh A, Fernando RL, Dharmage SC, Lodge CJ, Waidyatillake NT. The association between sugar intake during pregnancy and allergies in offspring: a systematic review and a meta-analysis of cohort studies. Nutr Rev 2022;80:904–18. [DOI] [PubMed] [Google Scholar]
- 125.Chen Y, Guo TL. Dietary advanced glycation end-products elicit toxicological effects by disrupting gut microbiome and immune homeostasis. J Immunotoxicol 2021;18:93–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Mepham B. Food additives: an ethical evaluation. Br Med Bull 2011;99:7–23. [DOI] [PubMed] [Google Scholar]
- 127.Harusato A, Chassaing B, Dauriat CJG, Ushiroda C, Seo W, Itoh Y. Dietary emulsifiers exacerbate food allergy and colonic type 2 immune response through microbiota modulation. Nutrients 2022; 14:4983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Allen KJ, Koplin JJ, Ponsonby AL, Gurrin LC, Wake M, Vuillermin P, Martin P, Matheson M, Lowe A, Robinson M, Tey D, Osborne NJ, Dang T, Tina Tan H-T, Thiele L, Anderson D, Czech H, Sanjeevan J, Zurzolo G, Dwyer T, Tang MLK, Hill D, Dharmage SC. Vitamin D insufficiency is associated with challenge-proven food allergy in infants. J Allergy Clin Immunol 2013;131:1109–16.e6. [DOI] [PubMed] [Google Scholar]
- 129.Mullins RJ, Clark S, Katelaris C, Smith V, Solley G, Camargo CA, Jr. Season of birth and childhood food allergy in Australia. Pediatr Allergy Immunol 2011;22:583–9. [DOI] [PubMed] [Google Scholar]
- 130.Calder PC. Mechanisms of action of (n-3) fatty acids. J Nutr 2012;142:592s–9s. [DOI] [PubMed] [Google Scholar]
- 131.Berg R. Bacterial translocation from the gastrointestinal tract. In: Mechanisms in the pathogenesis of enteric diseases. New York: Springer Science+Business Media; 1999:11–30. [Google Scholar]
- 132.Erridge C. The capacity of foodstuffs to induce innate immune activation of human monocytes in vitro is dependent on food content of stimulants of Toll-like receptors 2 and 4. Br J Nutr 2011;105:15–23. [DOI] [PubMed] [Google Scholar]
- 133.Mani V, Hollis JH, Gabler NK. Dietary oil composition differentially modulates intestinal endotoxin transport and postprandial endotoxemia. Nutr Metab (Lond) 2013; 10:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Pendyala S, Walker JM, Holt PR. A high-fat diet is associated with endotoxemia that originates from the gut. Gastroenterology 2012;142:1100–1.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Hamilton MK, Boudry G, Lemay DG, Raybould HE. Changes in intestinal barrier function and gut microbiota in high-fat diet-fed rats are dynamic and region dependent. Am J Physiol Gastrointest Liver Physiol 2015;308:G840–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Parks BW, Nam E, Org E, Kostem E, Norheim F, Hui ST, Pan C, Civelek M, Rau CD, Bennett BJ, Mehrabian M, Ursell LK, He A, Castellani LW, Zinker B, Kirby M, Drake TA, Drevon CA, Knight R, Gargalovic P, Kirchgessner T, Eskin E, Lusis AJ. Genetic control of obesity and gut microbiota composition in response to high-fat, high-sucrose diet in mice. Cell Metab 2013;17:141–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Turk HF, Chapkin RS. Membrane lipid raft organization is uniquely modified by n-3 polyunsaturated fatty acids. Prostaglandins Leukot Essent Fatty Acids 2013;88:43–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Stulnig TM, Huber J, Leitinger N, Anderson CA, Steffen LM, Rosamond WD, Kshirsagar AV. Polyunsaturated eicosapentaenoic acid displaces proteins from membrane rafts by altering raft lipid composition. J Biol Chem 2001;276:37335–40. [DOI] [PubMed] [Google Scholar]
- 139.Kim W, Fan YY, Barhoumi R, Smith R, McMurray DN, Chapkin RS. n-3 polyunsaturated fatty acids suppress the localization and activation of signaling proteins at the immunological synapse in murine CD4+ T cells by affecting lipid raft formation. J Immunol 2008;181:6236–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Oh DY, Talukdar S, Bae EJ, Imamura T, Morinaga H, Fan WQ, Li P, Lu WJ, Watkins SM, Olefsky JM. GPR120 is an omega-3 fatty acid receptor mediating potent anti-inflammatory and insulin-sensitizing effects. Cell 2010;142:687–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Sartorio MUA, Pendezza E, Coppola S, Paparo L, D'Auria E, Zuccotti GV, Berni Canani R. Potential role of Omega-3 polyunsaturated fatty acids in pediatric food allergy. Nutrients 2021; 14:152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Hogenkamp A, van Vlies N, Fear AL, van Esch BC, Hofman GA, Garssen J, Calder PC. Dietary fatty acids affect the immune system in male mice sensitized to ovalbumin or vaccinated with influenza. J Nutr 2011;141:698–702. [DOI] [PubMed] [Google Scholar]
- 143.van den Elsen LW, Bol-Schoenmakers M, van Esch BC, Hofman GA, van de Heijning BJM, Pieters RH, Smit JJ, Garssen J, Willemsen LEM. DHA-rich tuna oil effectively suppresses allergic symptoms in mice allergic to whey or peanut. J Nutr 2014;144:1970–6. [DOI] [PubMed] [Google Scholar]
- 144.van den Elsen LW, Meulenbroek LA, van Esch BC, Hofman GA, Boon L, Garssen J, Willemsen LEM. CD25+ regulatory T cells transfer n-3 long chain polyunsaturated fatty acids-induced tolerance in mice allergic to cow’s milk protein. Allergy 2013;68:1562–70. [DOI] [PubMed] [Google Scholar]
- 145.Dunstan JA, Mori TA, Barden A, Beilin LJ, Taylor AL, Holt PG, Prescott SL. Fish oil supplementation in pregnancy modifies neonatal allergen-specific immune responses and clinical outcomes in infants at high risk of atopy: a randomized, controlled trial. J Allergy Clin Immunol 2003;112:1178–84. [DOI] [PubMed] [Google Scholar]
- 146.Palmer DJ, Sullivan T, Gold MS, Prescott SL, Heddle R, Gibson RA, Makrides M. Effect of n-3 long chain polyunsaturated fatty acid supplementation in pregnancy on infants’ allergies in first year of life: randomised controlled trial. BMJ 2012;344:e184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Best KP, Gold M, Kennedy D, Martin J, Makrides M. Omega-3 long-chain PUFA intake during pregnancy and allergic disease outcomes in the offspring: a systematic review and meta-analysis of observational studies and randomized controlled trials. Am J Clin Nutr 2016;103:128–43. [DOI] [PubMed] [Google Scholar]
- 148.Manley BJ, Makrides M, Collins CT, McPhee AJ, Gibson RA, Ryan P, Sullivan TR, Davis PG; DINO Steering Committee. High-dose docosahexaenoic acid supplementation of preterm infants: respiratory and allergy outcomes. Pediatrics 2011;128:e71–7. [DOI] [PubMed] [Google Scholar]
- 149.Clausen M, Jonasson K, Keil T, Beyer K, Sigurdardottir ST. Fish oil in infancy protects against food allergy in Iceland-results from a birth cohort study. Allergy 2018;73:1305–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.D’Vaz N, Meldrum SJ, Dunstan JA, Martino D, McCarthy S, Metcalfe J, Tulic MK, Mori TA, Prescott SL. Postnatal fish oil supplementation in high-risk infants to prevent allergy: randomized controlled trial. Pediatrics 2012;130:674–82. [DOI] [PubMed] [Google Scholar]
- 151.Best KP, Sullivan TR, Palmer DJ, Gold M, Martin J, Kennedy D, Makrides M. Prenatal omega-3 LCPUFA and symptoms of allergic disease and sensitization throughout early childhood - a longitudinal analysis of long-term follow-up of a randomized controlled trial. World Allergy Organiza 2018; 11:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Osborne N, Gurrin L, Koplin J, Martin P, Robinson M, Slaa M, Thiele L, Miles L, Dawson D, Tan Hern TT, Dang T, Hill D, Lowe A, Matheson M, Ponsonby A-L, Tang M, Wake M, Dharmage S, Allen K; for_the_HealthNuts_Study_Group. Prevalence of food challenge: confirmed food allergies in a large pediatric population based study in Melbourne, Australia. Allergy 2010;65:375. [Google Scholar]
- 153.Sadeghi M, Mehr SS, Mirlohi M. Dose the only information on Vitamin D3 content of fish oil and fish liver oil in the Iranian scientific resource corroborate the respective international data? J Res Med Sci 2014;19:1205–6. [PMC free article] [PubMed] [Google Scholar]
- 154.Skypala IJ, McKenzie R. Nutritional issues in food allergy. Clin Rev Allergy Immunol 2019;57:166–78. [DOI] [PubMed] [Google Scholar]