PURPOSE
Virtual tumor board (VTB) via videoconference facility involving multiple specialists in the decision making for various tumors is well accepted, especially in high-income countries. Information on virtual tumor boards for head and neck cancers especially from low- and middle-income countries is sparse. In this study, we have audited the findings of the National Cancer Grid VTBs performed for head and neck cancers.
METHODS
All patients discussed in the head and neck VTBs at our center between December 2016 and February 2022 were included in the study. Details such as the type of institute sending patients for discussion, its location, subsites within the head and neck region, histopathology, treatment setting or question for the VTB, and availability of guidelines for such patient scenarios were assessed. Also, a survey was sent to assess the usefulness of the VTBs.
RESULTS
A total of 208 patients were discussed in 54 VTB sessions. The most common head and neck sites discussed in the VTBs were the oral cavity (n = 64, 30.7%) followed by skull base/nose and paranasal sinuses/eyelid-orbit tumors (n = 49, 23.5%). Nonsquamous cell carcinoma was the most common histopathology discussed; recurrent cancers/residual diseases were the most common treatment settings (n = 134, 64.4%) for which there were no existing guidelines. Survey results showed that most VTB decisions were implementable, and respondents felt that VTBs were a useful educational tool as well.
CONCLUSION
Our study affirms the feasibility of VTBs in low- and middle-income countries' health care systems for managing uncommon malignancies and clinical situations, which act as an important educational platform.
INTRODUCTION
The complex nature of cancer biology and the need for multimodality treatments mean that multiple professionals are involved in the decision making and management of a single patient. The formation of teams of health care professionals with various speciality skills forms the basis of multidisciplinary treatment (MDT). The UK Department of Health defines MDT as “a group of people of different healthcare disciplines which meets together at a given time (whether physically in one place or by video or teleconferencing) to discuss a given patient, and who are each able to contribute independently to the diagnostic and treatment decisions about the patient.”1 MDT is beneficial for patient outcomes and to improve the delivery of health care.2,3 At present, it is a norm in modern oncology care and is a requirement for cancer care units in many countries.4,5
CONTEXT
Key Objective
The most common head and neck sites discussed in the virtual tumor boards (VTBs) were the oral cavity followed by skull base neoplasms. Nonsquamous cell carcinoma was the most common histopathology discussed, and recurrent cancers/residual diseases were the most common treatment settings. There were no existing guidelines for the majority of patients discussed in the VTBs. The participants felt that the VTB decisions were implementable, and respondents felt that the VTBs were a useful educational tool as well.
Knowledge Generated
Virtual tumor boards can be effectively conducted in low- and middle-income countries health care systems, as demonstrated in our study, for managing uncommon malignancies and clinical situations when there are no guidelines or recommendations available and act as an important educational platform.
Relevance
This model was initiated much before the COVID-19 pandemic and can be emulated in conditions where in-person multidisciplinary tumor boards cannot be conducted. It can also help centers in remote locations have access to expert opinions and guidance and help benefit patients at large.
Although ideal, implementation of regular MDTs depends on various factors like the availability of the local hospital infrastructure and the presence of various specialists on-site. This may not be available in many under-resourced health care centers.6 Virtual tumor boards (VTBs) using videoconferencing facilities offer an elegant solution in these scenarios. Although VTBs for various tumors have been established in many high-income countries (HICs),7-9 literature regarding the feasibility and utility of VTB in low- and middle-income countries (LMICs) like India is scarce.
The National Cancer Grid (NCG) in India was initiated in 2012-2013, funded by the Government of India through the Department of Atomic Energy, with the vision of providing standardized cancer care across the country and creating human resources to tackle the growing burden of cancer and provide a ready platform for collaborative cancer research.10 At present, with more than 270 member institutions (private and public sector) from urban and rural areas across the country, it is the largest cancer care network in the world. VTBs were initiated by the NCG in December 2016 for various cancer subsites for providing a resource of expert opinions and guidance for centers that might not have a dedicated subspeciality service. This study presents our experience in establishing VTBs with participation involving various institutions involved in treating cancer across India. We analyzed the patients presented in the head and neck sessions of the NCG VTBs at our center (as the hub) to understand the nature of the patients discussed and their utility for various participating institutions.
METHODS
In this retrospective study, patients discussed in the head and neck VTB sessions conducted by the NCG from December 2016 to February 2022 were included. The NCG VTBs used the Project ECHO India platform.11 The hub and spoke model was used to conduct the VTBs wherein one center takes the responsibility of the host and the other centers log in and participate. Our center acted as the host for the VTBs, and difficult clinical situations were presented from NCG centers across the country. Experts from NCG centers participated in the discussions and provided their expert opinion on the patients that were discussed. Residents and trainees from these institutes were encouraged to participate in the VTB and ask questions to the expert faculty.
Each cancer site (head and neck, breast, thoracic, gastrointestinal, etc) was allotted prescheduled sessions (calendar shared with centers every quarter), and patients related to these sites were discussed in the respective sessions. The patients to be discussed in the VTB were presented using a standardized template, which included the clinical details, pathology and radiology findings (all deidentified), and specific questions about the patient. The presentation summary thus prepared was sent to the host institute, which was then circulated via e-mail to all the participating members, before the VTB.
Patients were presented in the scheduled slot for discussion of head and neck cancers (once a month) by the concerned institution, and experts from the host institute and other participating centers discussed the plan for further management. On the basis of the discussion, a consensus was arrived at in the VTB, and these were summarized and sent to the respective centers via e-mail as recommendations.
For analyzing the impact of VTB, an electronic questionnaire‐based survey (Google form)12 was sent out to participating centers—the questions related to the reasons for patients being sent for discussion in the VTB, whether they agreed to the VTB recommendations, whether the VTB recommendations could be executed (if not, reasons for the same), whether they would discuss the VTB recommendations with the patients, and whether the VTB was useful as an educational platform.
In this study, patients with head and neck cancer presented at the NCG VTBs were analyzed to study the tumor site, the reason for referral, the nature of the institute referring the patients, usefulness, and barriers to implementing the advised treatment. The study was conducted in accordance with the Declaration of Helsinki as revised in 2013. Statistical analysis was performed using SPSS version 20, and descriptive analysis and qualitative analysis were performed. In addition, the chi-square test was performed to understand the associations between the centers and the probable associations between the types of patients and reasons discussed in the VTB.
RESULTS
A total of 208 patients were discussed in 54 head and neck VTB sessions conducted at our center between December 2016 and February 2022. All the planned sessions could be conducted smoothly without any technical failures, connectivity issues, or malfunctioning of the setup from either end with a good audio-visual experience. In each HN VTB session, a median of four patients (range, 1-9 patients) were discussed and a median of 19 cancer centers (range, 5-41 centers) participated in these sessions.
Both the government-/public-funded (n = 106, 51%) and private/corporate hospitals (n = 93, 44.7%) presented and discussed patients from their institutes (Table 1). All the government-/public-funded hospitals were academic institutes, whereas only 34 (36.5%) of the 93 private/corporate hospitals were academic institutes (P < .001). The majority of private/corporate hospitals, ie, 77 (82.7%) of 93, were located in urban areas, whereas the government-/public-funded hospitals were equally (53 centers each) located in urban and rural areas (P < .001). In the head and neck VTBs, there were 23 centers that have repeatedly participated and presented the patients. Of the 23 centers, there were five centers where there was no in-house tumor board, and hence, they would participate to have an overall opinion for the particular patient.
TABLE 1.
Details of the Institutes That Participated in the VTB and Features of the Patients Discussed in the VTB
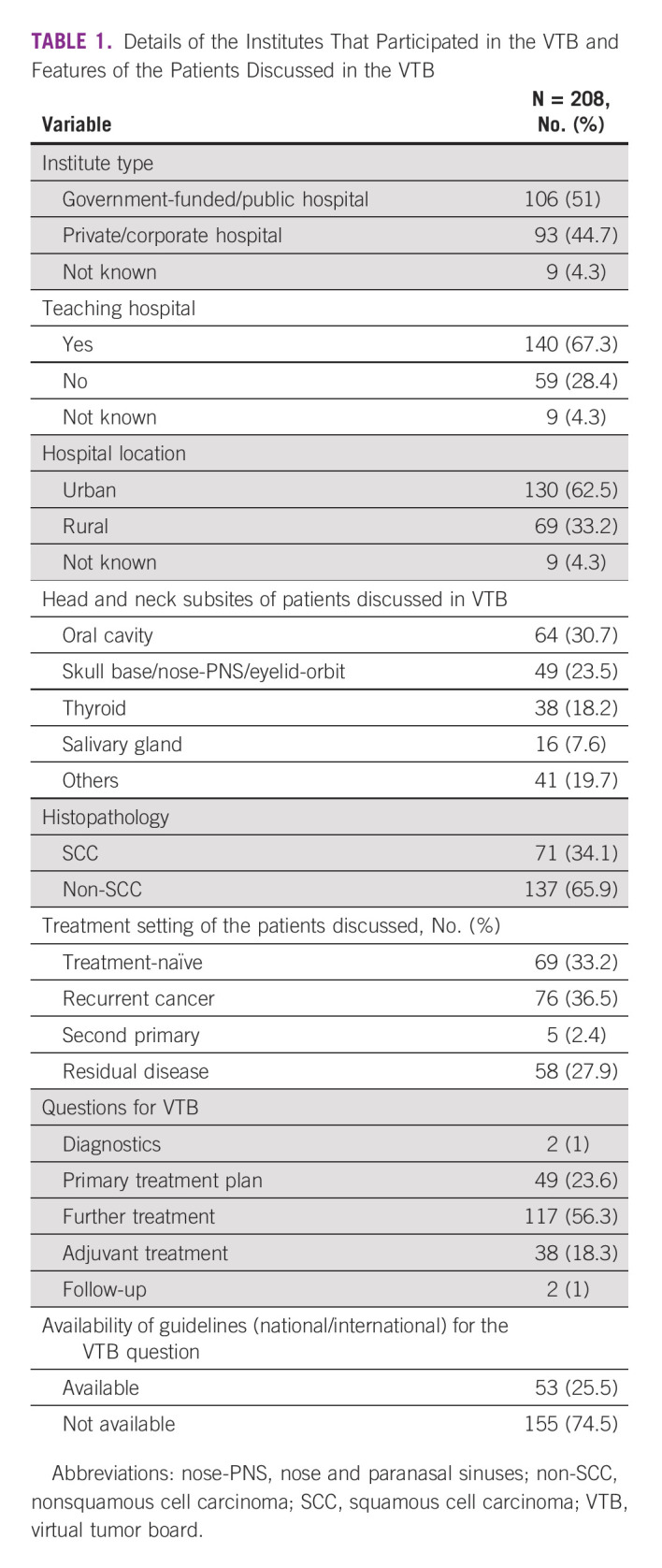
Among the subsites presented in the VTB, oral cavity cancers were most commonly discussed (n = 64, 30.7%), followed by skull base/nose and paranasal sinuses/eyelid-orbit tumors (n = 49, 23.5%), and thyroid (n = 38, 18.2%). The commonest clinical scenario discussed was of patients with recurrent cancers (n = 76, 36.5%) followed by treatment-naive patients (n = 69, 33.2%). Fifty-eight patients (27.9%) had received some incomplete treatment, for which opinion regarding further treatment was sought in the VTBs. The majority of the patients discussed sought further treatment plans in terms of the necessity of adjuvant treatment (n = 117, 56.3%) or treatment completion after having received incomplete treatment prior (n = 38; 18.3%). Most patients discussed were those with recurrences or for residual disease after incomplete treatment received prior (n = 134, 64.4%), for which there were no available treatment guidelines compared with treatment-naive (P = .025).
There were no national or international guidelines available for the questions raised for the majority of the patients discussed (n = 155, 74.5%) in the VTB. Almost two thirds of the patients discussed had nonsquamous cell carcinoma histology (n = 137, 65.9%). The majority of the patients discussed in the recurrent and residual disease setting needed inputs from multiple disciplines to arrive at a consensus regarding further management (n = 110; P = .05).
Survey
Fifty-two NCG centers responded to the survey (Table 2). Most often, the reasons for discussing the patients in the VTB were one or all of the following: no consensus at the local tumor board discussion, second opinion, and/or the patient scenario did not fit into standard evidence-based guidelines.
TABLE 2.
VTB Survey Questions and Responses
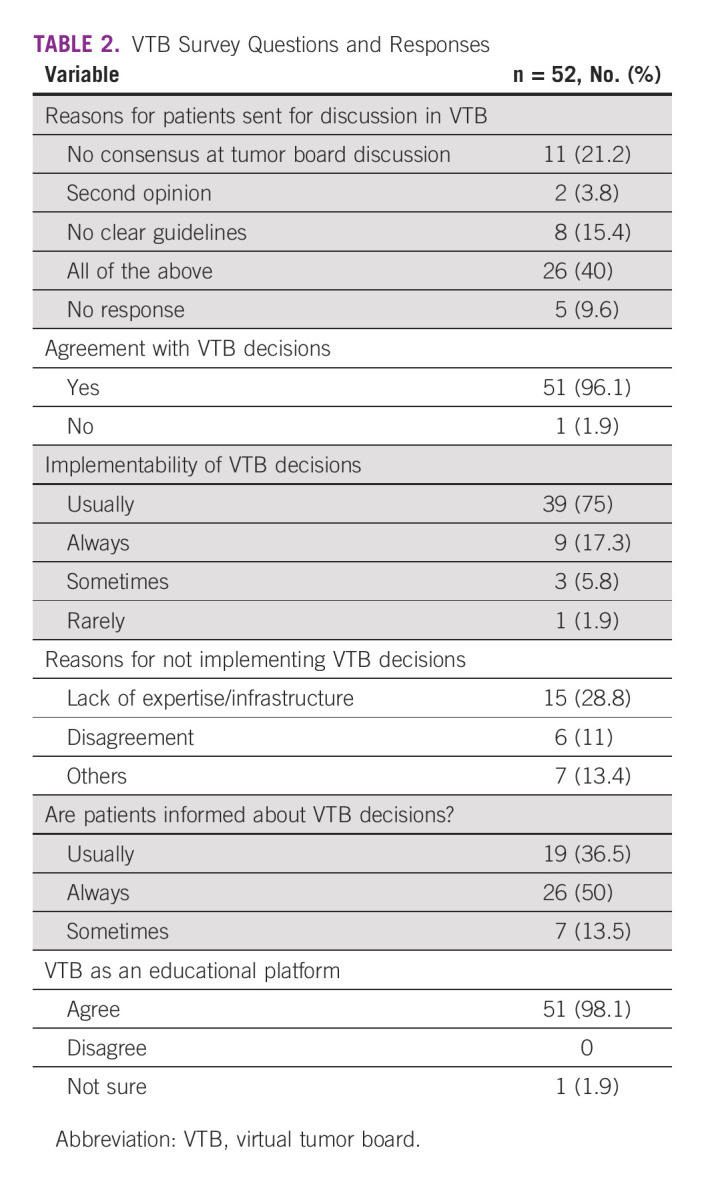
Almost all centers (n = 51, 96.1%) had an agreement with the decisions taken in the VTB regarding their patients. The VTB decisions were mostly implementable in their respective centers (X%). The most common reason for not implementing the VTB recommendation was the nonavailability of expertise (n = 15, 28.8%). Most centers discussed the VTB decisions with their patients (n = 45, 86.5%). Almost all centers (n = 51, 96.1%) agreed that the VTB was also a useful educational platform.
DISCUSSION
Our study demonstrated the feasibility of disease-specific virtual tumor boards for oncology care and case-based learning in India. Public-funded/government and private and corporate cancer care providers, appeared to benefit from participation in VTBs, regardless of whether they were academic or nonacademic centers; similarly, both rural and urban hospitals participated regularly in these sessions. Most clinical scenarios being discussed had no existing standard evidence-based guidelines underlining the fact that VTBs are complementary to guidelines. Complex clinical scenarios like recurrent disease were considered appropriate to get expert multidisciplinary opinions before treatment decisions were finalized. Most participants agreed with the discussion and treatment decisions taken during the VTBs, discussed them with their patients, and implemented them in practice. Most participants also considered that the VTBs fulfilled an important educational function.
Health care delivery systems in LMICs like India face significant challenges because of wide socioeconomic disparity, shortage of trained health care workers, lack of health care facilities in rural areas, and large out-of-pocket expenditures.13-15 The current COVID-19 pandemic has further increased the gaps in health care because of the nonavailability of travel facilities and shortage of expert health care personnel and resources.16 Although our VTBs were started much before the pandemic (in 2016), the establishment of VTBs offers a ready solution to address some of these issues.
In our study, more than 60% of the participating centers in the VTBs were located in urban areas, highlighting the fact that specialized cancer care in India is mainly concentrated in major cities. In addition, both corporate and public sector institutes participated equally in VTBs, indicating that MDT discussions can help in forming a consensus treatment plan irrespective of the type of oncology care. A large majority (65.9%) of the patients discussed in VTB were of uncommon nonsquamous histology, with a lack of clear guidelines in management being the reason for presenting these patients to VTBs. As these clinical situations are uncommon and do not fit into standard evidence-based guidelines, individual cancer centers and oncologists may lack the expertise or resources for the treatment of these conditions; hence, collaborative MDTs like ours can help to pool the experience from various institutes, provide an opportunity to form consensus guidelines, and potentially even lead to collaborative research protocols. This may also benefit in improving the health care delivery and treatment outcomes for such uncommon tumors. The majority (n = 134, 64.4%) of clinical situations discussed in the VTBs had either residual disease after incomplete treatment or recurrent cancers. This also points to the nonavailability of guidelines to treat patients in these settings and the necessity for discussion with experts to attain clarity and deliver better treatment to patients.
Telemedicine (TM) has become an integral part of health care delivery, and its use has been reported for cardiovascular diseases, respiratory conditions, diabetes, and mental health issues17 and also in various oncology settings such as remote palliative care, survivorship care, and remote chemotherapy supervision.18 There has been a rapid acceptance of TM, especially during the COVID-19 pandemic to continue cancer care with institutes switching to virtual patient visits to minimize the risk of exposure in immunocompromised patients.19-21
Virtual tumor boards with MDT can be a very useful avenue in such situations for making expert consultations and management plans available to a far-reaching patient base. Various studies from Western countries have previously reported on the use of teleconferencing for conducting a VTB.22-24 Marshall et al22 in their experience of establishing a regional VTB between the Houston (TX) Veterans Affairs Medical Center (VAMC; referral center) and the New Orleans (LA) VAMC (referring center) for 14 VTB discussions reported that VTB was highly acceptable to both the providers and the participants. A study from Houston, Tx, reported that the establishment of special VTB for hepatocellular carcinoma resulted in an improvement in quality and timelines for conducting MDT and thus positively influenced the care of patients with hepatocellular carcinoma.9 Multidisciplinary management with tele- or videoconferencing for patients with cancer is rapidly becoming an accepted norm and has several benefits to offer.
In a scoping review to study the benefits and drawbacks of videoconferencing in oncology networks,25 it was found that there were several benefits to patients, such as less travel for diagnosis, better coordination of care, better access to scarce facilities and expertise, and treatment in their own community. Benefits for health care professionals included optimized treatment plans through multidisciplinary discussion of complex patients, an ability to inform all health care professionals simultaneously, enhanced care coordination, less travel, and continuous medical education. The role of VTBs as an important educational tool has also been highlighted in our study as the majority of the participating centers were teaching hospitals; trainees and fellows from participating institutes were encouraged to participate and interact with the national faculty during VTBs, promoting case-based learning. Almost all the responders (> 98%) agreed that VTBs served as a valuable educational resource. These benefits are likely to be more pronounced in LMICs compared with HICs where access is less of a problem; however, these are useful even in certain under-resourced areas in HICs.
Teleconferencing has been reported as a largely acceptable way of MTDs;26 however, there are certain limitations in establishing and smooth functioning of VTB. In a systematic review to study barriers to TM, it was reported that issues with technically challenged staff, resistance to change, and cost of the equipment and technology are some of the commonest problems for regular use of TM.
Our study reports the audit of VTBs conducted for patients with head and neck cancers from a large LMIC cancer care provider network and has several strengths. First, our VTBs were initiated much before COVID-19 and therefore reflect the feasibility and uptake in a noncrisis situation; the benefits would likely be even more apparent during a crisis like the COVID-19 pandemic. Second, the feasibility and involvement of cancer centers in the NCG VTBs were agnostic to the type of provider (publicly funded and private), setting (academic or nonacademic), and location (urban or rural). Third, most decisions taken during the VTBs were implemented by the participating centers, demonstrating the value that centers placed in the MDT discussions. Finally, the educational aspects of regular VTBs raise the prospects of upskilling nonspecialist oncologists and trainees. Our study has some limitations—we do not have the follow-up data on patients in whom VTB decisions influenced care. In addition, we were unable to objectively quantify the educational impact of the VTBs beyond the survey results. Nevertheless, our study adds substantially to the literature on virtual approaches to multidisciplinary decision making in cancer.
In conclusion, our study confirms the feasibility and utility of VTBs in our health care model to provide access to multidisciplinary expertise in cancer centers, facilitate discussion among professionals especially for managing uncommon malignancies and clinical situations, and act as an important educational platform in LMICs. With the COVID-19 pandemic forcing the adoption of technology in virtually all areas of health care, this model can be replicated across medical specialities and promote superior care in situations where multidisciplinary decision making is critical.
C.S. Pramesh
This author is a member of the JCO Global Oncology Editorial Board. Journal policy recused the author from having any role in the peer review of this manuscript.
Stock and Other Ownership Interests: Aurobindo
No other potential conflicts of interest were reported.
DATA SHARING STATEMENT
Data sharing can be considered on request.
AUTHOR CONTRIBUTIONS
Conception and design: Shivakumar Thiagarajan, Amit Joshi, Devendra Chaukar, Ravi Kannen, C.S. Pramesh
Administrative support: Vinisha Poojari, Devendra Chaukar, C.S. Pramesh
Provision of study materials or patients: All authors
Collection and assembly of data: Shivakumar Thiagarajan, Vinisha Poojari, Sajith Babu, Prashant Penumadu, Suman Kumar
Data analysis and interpretation: Shivakumar Thiagarajan, Vidisha Tuljapurkar, Sarbani Ghosh-Laskar, Khuzema Fatehi, Prashant Penumadu, Asawari Patil, Ravi Kannan
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/go/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
C.S. Pramesh
This author is a member of the JCO Global Oncology Editorial Board. Journal policy recused the author from having any role in the peer review of this manuscript.
Stock and Other Ownership Interests: Aurobindo
No other potential conflicts of interest were reported.
REFERENCES
- 1.Health in Wales | Document | Calman Hine Report. http://www.wales.nhs.uk/document/112166/info/ [Google Scholar]
- 2.Patil RD, Meinzen-Derr JK, Hendricks BL, et al. : Improving access and timeliness of care for veterans with head and neck squamous cell carcinoma: A multidisciplinary team’s approach. Laryngoscope 126:627-631, 2016 [DOI] [PubMed] [Google Scholar]
- 3.Newman EA, Guest AB, Helvie MA, et al. : Changes in surgical management resulting from case review at a breast cancer multidisciplinary tumor board. Cancer 107:2346-2351, 2006 [DOI] [PubMed] [Google Scholar]
- 4.Licitra L, Keilholz U, Tahara M, et al. : Evaluation of the benefit and use of multidisciplinary teams in the treatment of head and neck cancer. Oral Oncol 59:73-79, 2016 [DOI] [PubMed] [Google Scholar]
- 5.2020 Standards and Resources. https://www.facs.org/quality-programs/cancer/coc/standards/2020 [Google Scholar]
- 6.Bouvier AM, Bauvin E, Danzon A, et al. : Place of multidisciplinary consulting meetings and clinical trials in the management of colorectal cancer in France in 2000. Gastroenterol Clin Biol 31:286-291, 2007 [DOI] [PubMed] [Google Scholar]
- 7.Shea CM, Teal R, Haynes-Maslow L, et al. : Assessing the feasibility of a virtual tumor board program: A case study. J Healthc Manag 59:177-193, 2014 [PMC free article] [PubMed] [Google Scholar]
- 8.Stevenson MM, Irwin T, Lowry T, et al. : Development of a virtual multidisciplinary lung cancer tumor board in a community setting. JCO Oncol Pract 9:e77-e80, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salami AC, Barden GM, Castillo DL, et al. : Establishment of a regional virtual tumor board program to improve the process of care for patients with hepatocellular carcinoma. JCO Oncol Pract 11:e66-e74, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pramesh CS, Badwe RA, Bhoo-Pathy N, et al. : Priorities for cancer research in low- and middle-income countries: A global perspective. Nat Med 28:649-657, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Project ECHO: https://www.echoindia.in/
- 12.Virtual Tumor Board (VTB) Survey: https://docs.google.com/forms/d/e/1FAIpQLSdgozlblf7TW_YUmfUhoq7viuu7BiYqLinSeldQpD6u86t1rQ/viewform?usp=sf_link
- 13.Kasthuri A: Challenges to healthcare in India—The five A’s. Indian J Community Med 43:141-143, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Rao M, Rao KD, Kumar AS, et al. : Human resources for health in India. Lancet 377:587-598, 2011 [DOI] [PubMed] [Google Scholar]
- 15.Pramesh CS, Badwe RA, Borthakur BB, et al. : Cancer burden and health systems in India 3: Delivery of affordable and equitable cancer care in India. Lancet Oncol 15:e223-e233, 2014 [DOI] [PubMed] [Google Scholar]
- 16.Pramesh CS, Chinnaswamy G, Sengar M, et al. : COVID-19 and cancer care in India. Nat Cancer 2:1257-1259, 2021 [DOI] [PubMed] [Google Scholar]
- 17.Flodgren G, Rachas A, Farmer AJ, et al. : Interactive telemedicine: Effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2015:CD002098, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weinkove R, McQuilten ZK, Adler J, et al. : Managing haematology and oncology patients during the COVID-19 pandemic: Interim consensus guidance. Med J Aust 212:481-489, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hollander JE, Carr BG: Virtually perfect? Telemedicine for Covid-19. N Engl J Med 382:1679-1681, 2020 [DOI] [PubMed] [Google Scholar]
- 20.Pramesh CS, Badwe RA: Cancer management in India during Covid-19. N Engl J Med 382:e61, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Curigliano G, Banerjee S, Cervantes A, et al. : Managing cancer patients during the COVID-19 pandemic: An ESMO multidisciplinary expert consensus. Ann Oncol 31:1320-1335, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Marshall CL, Petersen NJ, Naik AD, et al. : Implementation of a regional virtual tumor board: A prospective study evaluating feasibility and provider acceptance. Telemed J E Health 20:705-711, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gagliardi A, Smith A, Goel V, et al. : Feasibility study of multidisciplinary oncology rounds by videoconference for surgeons in remote locales. BMC Med Inform Decis Mak 3:7, 2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Billingsley KG, Schwartz DL, Lentz S, et al. : The development of a telemedical cancer center within the Veterans Affairs Health Care System: A report of preliminary clinical results. Telemed J E Health 8:123-130, 2002 [DOI] [PubMed] [Google Scholar]
- 25.van Huizen LS, Dijkstra PU, van der Werf S, et al. : Benefits and drawbacks of videoconferencing for collaborating multidisciplinary teams in regional oncology networks: A scoping review. BMJ Open 11:e050139, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Stalfors J, Holm-Sjögren L, Schwieler A, et al. : Satisfaction with telemedicine presentation at a multidisciplinary tumour meeting among patients with head and neck cancer. J Telemed Telecare 9:150-155, 2003 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data sharing can be considered on request.


