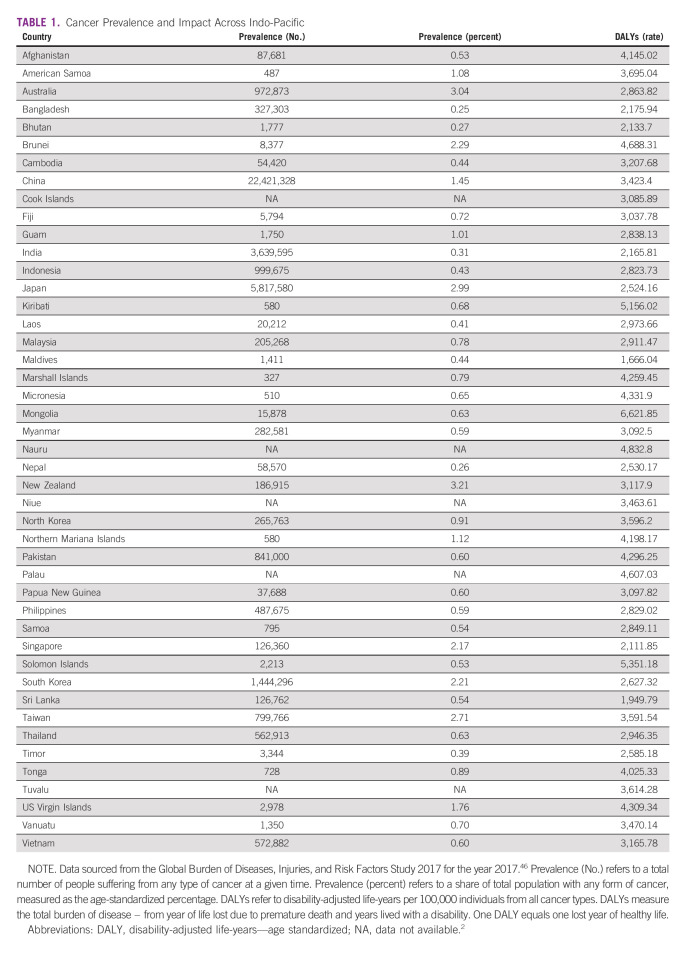
Approximately 100 million people or 1.3% of the world population have a personal history of cancer and are thus considered to be cancer survivors.1 Around 40% of them reside in the area referred to as the Indo-Pacific.2 The term Indo-Pacific describes a geopolitical area extending from India across the interconnected space of the Indian and Pacific Oceans, with strong regional economic and political alliances and some of the world's fastest growing economies (India, Bangladesh, and Vietnam), making it one of the most strategically important regions globally.3 Indo-Pacific corresponds to two WHO regions: the Western Pacific and the South East Asia. It accounts for 60% of the world population, 45% of global cancer incidence, and 53% of mortality, with projections for a 48% increase in numbers of cancers over the next 20 years, attributed to population growth and aging.4 Within the region, comprising some of the most populous countries (China and India) and the least populous (Tuvalu), there is great variation in the prevalence of cancer (ranging from 0.25% in Bangladesh to 3.2% in New Zealand), numbers of cancer survivors, and cancer disability burden (Table 1).2
TABLE 1.
Cancer Prevalence and Impact Across Indo-Pacific
CONTEXT
Key Objective
To examine the challenges and opportunities in cancer survivorship care and research in the Indo-Pacific.
Knowledge Generated
The Indo-Pacific region accounts for approximately 40% of the world population of cancer survivors. Although there are significant variations in prevalence, patterns of unmet needs, and health system capability across the region, there are also growing regional partnerships in care delivery and research development. The United Nations' Global Goals and the WHO strategy for the region align well with global priorities for cancer survivorship and may offer directions for advancement in survivorship care through greater care integration and regional collaboration.
Relevance
Advancement in survivorship care needs to address the unique health, social, and cultural needs of Indo-Pacific populations while leveraging regional and global partnerships in survivorship care and research.
CANCER SURVIVORSHIP–DEFINITIONS AND ELEMENTS OF CARE
The commonly accepted definition states that a cancer survivor is a person diagnosed with cancer, from the time of diagnosis for the balance of their life.5 Recently, four distinct phases of survivorship have been proposed including acute, chronic, long-term, and cured, reflecting more closely the phase of illness and thus potentially differing care needs.6 Chronic survivorship refers to the survivorship experience of individuals living with incurable and thus progressive cancer who, until recently, were not considered as cancer survivors despite facing similar, and often greater, challenges.7 The term survivor, although not always appreciated by people with cancer or easily translated to other languages,8 serves to emphasize the unique aspects of survivorship care as an important part of overall cancer care. The key components of quality survivorship care include surveillance and management of physical and psychosocial effects of cancer and its treatment, prevention and surveillance of recurrence and new cancers, health promotion and overall disease prevention, and surveillance and management of comorbid disease.9,10 The priorities given to each of these elements by survivors and their health care providers may differ according to the phase of survivorship, and individual patient's needs.
This paper reviews current challenges and opportunities in cancer survivorship in the Indo-Pacific from the perspective of patients' needs, health system capabilities, patient advocacy, and research to identify priorities for progress.
SYMPTOM BURDEN AND SUPPORTIVE CARE NEEDS
Several studies have examined unmet needs of cancer survivors in Australia, South Korea, China, India, and Singapore.11-14 Only two studies have provided insights into variations in the symptom burden and unmet supportive care needs of cancer survivors across multiple countries. The STEP study involved 1,748 adult survivors who had completed first-line treatment for cancer in nine countries (Australia, China, Japan, South Korea, Myanmar, Thailand, India, Singapore, and Philippines) and one special administrative region (Hong Kong).15 The most frequently reported symptoms were fatigue (66.6%), loss of strength (61.8%), pain (61.6%), and sleep disturbance (60.1%), with no significant differences in symptom burden among cancer survivors between high-income countries (HICs) and low-and middle-income countries (LMICs). The most commonly reported unmet need was concern about cancer recurrence or progression (40.2% reporting moderate and strong needs). The remaining top unmet needs included access to local health services, access to best medical care, managing health together with their medical team, and knowing that their doctors were talking with each other to coordinate care (all with more than 30%-40% reporting moderate/strong needs). Australia and other HICs in the region were similar in terms of unmet needs (all low), but LMICs had significantly higher unmet needs.
The ACTION study examined quality of life, anxiety, and depression symptoms in 5,249 survivors of diverse cancers at 1 year after diagnosis in eight LMICs (Cambodia, Indonesia, Laos, Malaysia, Myanmar, Philippines, Thailand, and Vietnam) and identified that patients with lung cancer and lymphoma had lower global quality of life and higher prevalence of self-reported anxiety and depression compared with patients with other cancers.16 The factors associated with poorer quality of life and higher anxiety and depression included older age, being male, advanced stage at diagnosis, low-income status, and no paid employment.
Research focusing on psychosocial needs has revealed regional and cultural variations in prevalence of anxiety, depression, and psychologic and informational needs across the region.17,18 Studies of financial toxicity, a subjective burden of the cost of cancer and its treatment, including a systematic review and meta-analysis and an eight-country cohort study showed rates of financial toxicity as high as 83% and a 31% incidence of financial catastrophe.19,20 There were also significant gaps in evidence, with no studies on needs of cancer survivors from the Pacific Islands and Territories.
Collectively, these studies emphasize the significant burden of diverse symptoms and needs of cancer survivors across the Indo-Pacific region, pointing out to two key conclusions. First, new survivorship programs and interventions should be developed on the basis of data on needs and priorities, with input from people affected by cancer themselves. Second, there are rich opportunities for research that compares findings across different settings (countries, systems, and contexts) as this information may assist in understanding predictors and mechanisms of greater unmet needs and inform relevant interventions and strategies. Such research can only be possible through strengthening collaborative research networks within the region and globally.
HEALTH SYSTEM CAPABILITY
There are limited data on existing models of survivorship care within the Indo-Pacific. A review of different cancer survivorship care models, with studies from Australia, Singapore, and Japan, showed no difference between models of care for a range of health care outcomes; however, several outcomes have not been measured, including management of comorbid conditions, relationship difficulties, return to employment, financial toxicity, and transitioning back to daily life.21
A global survey of 27 countries to ascertain the components and structure of follow-up care, delivery of treatment summaries and survivorship care plans, and involvement of primary care in survivorship included eight countries from the Indo-Pacific (Australia, Japan, South Korea, China, Malaysia, India, Philippines, and Vietnam).22 Five of these had a national cancer control plan (NCCP), which included consideration of survivorship care. One HIC did not have an NCCP (Australia) and one LMIC did (the Philippines). HICs were more likely to use guidelines compared with LMICs. There was significant variation between countries, regardless of income level. The challenges in the delivery of survivorship care were common across the globe, which included lack of priority on follow-up care, availability of workforce, distance, and communication and care coordination issues. A special challenge—pediatric and adolescent survivorship care in Pacific Island Countries and Territories (PICTs)—outlined below shows one example of how these considerations intersect.
A Special Challenge–Pediatric and Adolescent Survivorship Care in PICTs
In contrast to HICs, the survival rates for pediatric cancers in LMICs remain unacceptably low, particularly in the small PICTs.25 There is a wide variability in the models of care adopted across the PICTs, ranging from developing in-country childhood cancer treatment programs (Fiji and Papua New Guinea), to relying on twinning relationships where children with cancer receive treatment in partnering institutions in other countries and then return home for maintenance or survivorship care (New Caledonia, Tonga, and Samoa). Major challenges include a lack of oncology-trained physicians in the region (estimates suggest that there are two pediatricians with oncology training across a population of > 9 million children). Other challenges include a lack of acknowledgment of the unique care required by children with cancer and their families, lack of NCCPs that address childhood cancer, and small numbers of child cancer patients in each individual PICT. Parents of children with cancer in the PICTs often need to provide for their entire family with very few resources, which can lead to treatment noncompletion when parents are unable to support both their child with cancer and their other family members. Community attitudes toward childhood cancer vary widely. In some PICTs, childhood cancer can still be viewed as universally fatal and therefore not worthwhile in seeking treatment. There can be a reliance on traditional healers, which results in late presentations.26 Many children suffer from comorbid conditions such as malnutrition or tuberculosis, which can complicate their cancer treatment.
There are multiple efforts toward addressing these challenges. Twinning projects have proven successful in raising survival rates; however, the impact of out-of-country care and restrictions since the COVID-19 pandemic have resulted in a greater focus on supporting more in-country care.27 Globally, the WHO is aiming to improve child cancer outcomes worldwide through the Global Initiative for Childhood Cancer, which focuses on the country needs assessment, development of centers of excellence and care networks, context-appropriate treatment regimens, advocacy, leveraged financing, and linked policies/governance.28
The STEP Study surveyed 1,501 oncology practitioners across nine participating countries.23 Perceived barriers to survivorship care were similar across the HICs and LMICs, with the highly rated items being lack of time, educational resources, and evidence-based practice guidelines. The Economist Intelligence Unit examined the availability of policies for coordinated and integrated cancer care in the region and identified these in Australia, China, Japan, Malaysia, and South Korea.24 Only Japan had guidelines for long-term follow up and preventive care for cancer survivors, as well as programs for rehabilitation and return to work.
There are opportunities for sharing information, and strategies for improvement of survivorship care within the region, especially given the commonly experienced challenges in care delivery. Especially for low-resource economies and for countries with low population, partnership with large centers may be of benefit. Development of a regional network would also enable staff support and development.
PATIENT AND NONGOVERNMENT ORGANIZATION SUPPORT
Given limited health system resources, patient and other nongovernment organizations can play an important role in supporting cancer survivors. In 2016, Rare Cancers Australia conducted a survey of patient organizations in 18 countries in the region.29 They identified several advocacy organizations, most relying heavily on volunteer support. Their main activities were providing information and support to patients and caregivers and raising awareness. Community organizations in HICs tended to have more engagement with policymakers and in research. Patient organization contributed to cancer policy development in Australia, Japan, Malaysia, the Philippines, South Korea, and Singapore.24 One example was the passage of the Universal Health Care Act and the National Integrated Cancer Control Act in the Philippines in 2019 spearheaded by a country-wide coalition of Filipino patient organizations, although these laws are yet to be enacted.
In LMICs, the nongovernment organizations tend to focus on providing funding for treatment and diagnosing cancer, where in some cases such as the Shwe Yaung Hnin Si Cancer Foundation in Myanmar and the Alola Foundation in Timor-Leste, these groups are at times the only form of support/survivorship care. Their work can be siloed and could be strengthened by collaboration between clinical/academic institutions. Building relationships with academic researchers can assist with programs evaluation and build a bridge between research projects and services provision. A successful example of this is a trial of peer-to-peer support for patients with cancer in Vietnam where an evidence-based model of peer-to-peer support has been successfully implemented through partnerships between medical/academic institutions and patient groups.30
Patient and nongovernment organizations should be considered integral in advancing survivorship care and research as partners in cocreating better care and research, informing care and highlighting unmet needs and priorities of the populations they serve.
SURVIVORSHIP RESEARCH
Although there is diverse and growing cancer research capability across the region, unlike cancer treatment clinical trials, most survivorship research is undertaken outside of collaborative groups, in single centers and not responding to explicit research priorities. A recent study developed priorities for cancer survivorship research in Australia, including research on physiologic and psychosocial outcomes, research on quality of care, models of care, self-management, communication and patient navigation, special population research including rare cancers, advanced cancers, rural and remote populations, pediatric cancers, and populations with lower socioeconomic status.31 Similar priorities have been identified in Japan with additional emphasis on economic concerns and employment and cancer stigma.32 The Australian study also highlighted the need for dedicated research infrastructure including data capability, research collaborations, funding, reporting standards, and investment in research.31
The data capability across the region is variable. Thailand, for example, monitors service coverage and financial risk protection through national surveys, administrative data, and disease registries.33 The WHO hosts two regional data collaborations: Asia Pacific Observatory on Health Systems and Policies (APO) and the Alliance for Health Policy and Systems Research.34 Although neither of these are specifically focused on cancer survivorship, their work can contribute to advancement of survivorship care indirectly. For example, APO partners with interested governments, agencies, and researchers to promote evidence-informed health system policy development in the region. Their recent work on integrated care for chronic diseases in the Asia Pacific can inform how cancer survivorship care be best integrated into the overall health care delivery across the region.35 The Alliance for Health Policy and System Research aims to advance knowledge on policy-relevant health system research, disseminate research findings, and build capacity in health service research. Its work on social and commercial determinants of health may be of particular relevance to cancer survivors.36
There are regional opportunities for building research skills with particular focus on supportive and survivorship care. The ACORD (Australia & Asia Pacific Oncology Research Development) workshop ran from Australia and included participants from the region and CReDO (the International Collaboration for Research Methods Development in Oncology) workshop in India.37 Unfortunately, funding for survivorship research remains limited compared with other areas of research.38
OPPORTUNITIES FOR ADVANCEMENT
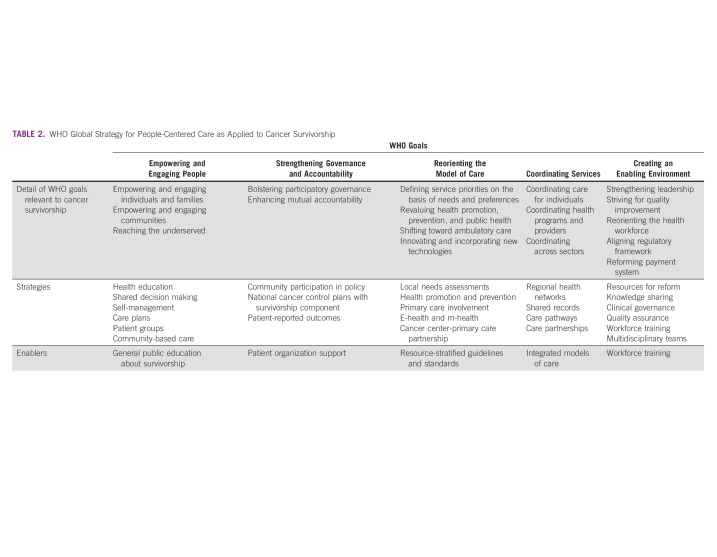
Progress in cancer survivorship care and research requires leveraging of the global interconnectedness of cancer control, while allowing for the variation in needs, preferences, and capacity. There is international recognition that even in well-resourced HICs, the growing number of cancer survivors far exceeds any growth in the health workforce,39,40 requiring reorientation of the model of care to fit with the overall priorities for global health care delivery. The priorities for survivorship care in the United States41,42 and Europe43 align well with the United Nations Sustainable44 Development Goals, which include reduction of premature mortality from noncommunicable disease through prevention and treatment and promotion of mental health and well-being. Similarly, the WHO global strategy on people-centred care 2016-2026 emphasizes empowering patients, reorienting model of care away from short-term (acute) to longer-term health promotion, prevention and ambulatory care, coordinating services, and enabling environment for care.45 Table 2 illustrates how these goals could apply to cancer survivorship. The enabling elements highlighted in the table are the areas that would particularly benefit from regional collaborations and partnerships with relevant professional organizations, patient advocacy groups, and industry partners.
TABLE 2.
WHO Global Strategy for People-Centered Care as Applied to Cancer Survivorship
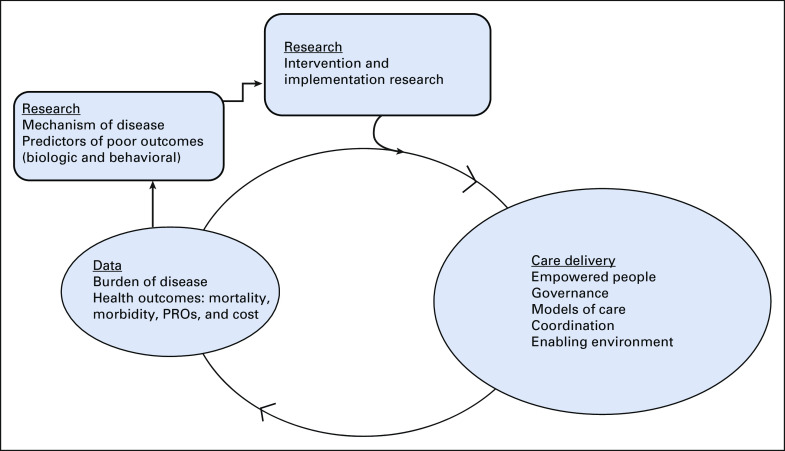
Figure 1 integrates the key variables important in the delivery of survivorship care with a closed feedback loop between real-world data on the burden of disease and health outcomes informing the priorities for care delivery including models, enabling environment, and governance. The performance of the care delivery system can in turn be monitored by monitoring the change in health care outcomes and burden of disease, leading to further refinements. The assessment of burden of disease in cancer survivorship needs to include not just cancer mortality but also competing causes of morbidity and mortality, disability, and cost, including reduced productivity and unemployment. Understanding of the burden of disease and care disparities can guide research efforts that address priority areas and investigate underlying mechanisms that could then inform intervention development. Similar to care delivery, research should leverage partnerships and integration to ensure impact. For example, survivorship outcomes should be integrated into cancer therapy clinical trials.
FIG 1.
The inter-relationship between care delivery, data monitoring, and research in cancer survivorship. PRO, patient reported outcomes.
In conclusion, cancer survivorship in the Indo-Pacific presents many challenges in this large region with diverse needs and health system capabilities. There are many examples of excellence that can be built upon to improve outcomes, and reduce disparities, and emerging collaborations that could be expanded. Advancement in cancer survivorship in the region needs to straddle two seemingly competing priorities. On one hand, it needs to recognize the unique medical, social, and cultural needs of the populations served, and develop clinical services and research priorities that best address these needs. On the other hand, there are great opportunities for integrating these efforts into a large regional undertaking. Only through collaborations in care, research, and policy development can we avoid unnecessary duplication, address the unique needs of survivors affected by rare cancers or small population cohorts, and build capacity to support the limited workforce. Such collaboration should recognize that cancer survivorship is one aspect of chronic disease experience and survivorship care could benefit from closer integration into the broader global health care priorities. It is through reconciling these two goals of unity in diversity, that true progress can be made.
Bogda Koczwara
Employment: Australian Radiology Clinics
Alexandre Chan
Consulting or Advisory Role: Blueprint Medicines, Lilly, Hengrui Medicine
Carolyn Taylor
Travel, Accommodations, Expenses: Novartis, Pfizer
Other Relationship: Pfizer
Nirmala Bhoo‐Pathy
Honoraria: Roche, Novartis
Speakers' Bureau: Roche, Novartis
Research Funding: Pfizer, Novartis, Zuellig Pharma
Bishal Gyawali
This author is a member of the JCO Global Oncology Editorial Board. Journal policy recused the author from having any role in the peer review of this manuscript.
Consulting or Advisory Role: Vivio Health
C.S. Pramesh
This author is a member of the JCO Global Oncology Editorial Board. Journal policy recused the author from having any role in the peer review of this manuscript.
Stock and Other Ownership Interests: Aurobindo
Miyako Takahashi
Honoraria: Takeda, Chugai Pharma, Pfizer, AstraZeneca Japan, Kyowa Kirin International, Shionogi
Yu Ke
Employment: GlaxoSmithKline
No other potential conflicts of interest were reported.
SUPPORT
C.E.W. receives support from the NHMRC of Australia (GNT 2008300); R.J.C. receives salary support from the NHMRC of Australia (GNT1194051).
AUTHOR CONTRIBUTIONS
Conception and design: Bogda Koczwara, Alexandre Chan, Michael Jefford, Wendy W.T. Lam, Claire E. Wakefield, Yan Lou, Raymond J. Chan
Collection and assembly of data: Bogda Koczwara, Alexandre Chan, Michael Jefford, Wendy W.T. Lam, Carolyn Taylor, Bishal Gyawali
Data analysis and interpretation: Alexandre Chan, Michael Jefford, Wendy W.T. Lam, Claire E. Wakefield, Nirmala Bhoo-Pathy, Bishal Gyawali, Gregory Harvet, C.S. Pramesh, Miyako Takahashi, Yu Ke
Manuscript writing: All authors
Final approval of manuscript: All authors
Accountable for all aspects of the work: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated unless otherwise noted. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or ascopubs.org/go/authors/author-center.
Open Payments is a public database containing information reported by companies about payments made to US-licensed physicians (Open Payments).
Bogda Koczwara
Employment: Australian Radiology Clinics
Alexandre Chan
Consulting or Advisory Role: Blueprint Medicines, Lilly, Hengrui Medicine
Carolyn Taylor
Travel, Accommodations, Expenses: Novartis, Pfizer
Other Relationship: Pfizer
Nirmala Bhoo‐Pathy
Honoraria: Roche, Novartis
Speakers' Bureau: Roche, Novartis
Research Funding: Pfizer, Novartis, Zuellig Pharma
Bishal Gyawali
This author is a member of the JCO Global Oncology Editorial Board. Journal policy recused the author from having any role in the peer review of this manuscript.
Consulting or Advisory Role: Vivio Health
C.S. Pramesh
This author is a member of the JCO Global Oncology Editorial Board. Journal policy recused the author from having any role in the peer review of this manuscript.
Stock and Other Ownership Interests: Aurobindo
Miyako Takahashi
Honoraria: Takeda, Chugai Pharma, Pfizer, AstraZeneca Japan, Kyowa Kirin International, Shionogi
Yu Ke
Employment: GlaxoSmithKline
No other potential conflicts of interest were reported.
REFERENCES
- 1.Global Burden of Disease 2019 Cancer Collaboration; Kocarnik JM, Compton K, et al. : Cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life years for 29 cancer groups from 2010 to 2019: A systematic analysis for the Global Burden of Disease Study 2019. JAMA Oncol 8;420-444, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Roser M, Ritchie H: Cancer. 2015. https://ourworldindata.org/cancer [Google Scholar]
- 3.Medcalf R: Reimagining Asia: From Asia-Pacific to Indo-Pacific, in Rozman G, Liow J (eds): International Relations and Asia’s Southern Tier. Asan-Palgrave Macmillan Series. Singapore, Springer, 2018 [Google Scholar]
- 4.Ferlay J, Laversanne M, Ervik M, et al. : Global Cancer Observatory: Cancer Tomorrow. Lyon, France: International Agency for Research on Cancer, 2020. https://gco.iarc.fr/tomorrow [Google Scholar]
- 5.National Coalition for Cancer Survivorship. https://canceradvocacy.org/about/our-mission/
- 6.Surbone A, Tralongo P: Categorization of cancer survivors: Why we need it. J Clin Oncol 34:3372-3374, 2016 [DOI] [PubMed] [Google Scholar]
- 7.Langbaum T, Smith TJ: Time to study metastatic-cancer survivorship. N Engl J Med 380:1300-1302, 2019 [DOI] [PubMed] [Google Scholar]
- 8.O'Callaghan C, Schofield P, Butow P, et al. : I might not have cancer if you didn't mention it": A qualitative study on information needed by culturally diverse cancer survivors. Support Care Cancer 24:409-418, 2016 [DOI] [PubMed] [Google Scholar]
- 9.Institute of Medicine and National Research Council . From Cancer Patient to Cancer Survivor: Lost in Transition. Washington, DC, The National Academies Press, 2006 [Google Scholar]
- 10.Nekhlyudov L, Mollica MA, Jacobsen PB, et al. : Developing a quality of cancer survivorship care framework: Implications for clinical care, research, and policy. J Natl Cancer Inst 111:1120-1130, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lisy K, Langdon L, Piper A, Jefford M: Identifying the most prevalent unmet needs of cancer survivors in Australia: A systematic review. Asia Pac J Clin Oncol 15:e68-e78, 2019 [DOI] [PubMed] [Google Scholar]
- 12.Miroševič Š, Prins JB, Selič P, et al. : Prevalence and factors associated with unmet needs in post-treatment cancer survivors: A systematic review. Eur J Cancer Care (Engl) 28:e13060, 2019 [DOI] [PubMed] [Google Scholar]
- 13.Srivastava S, Kumar A: Breast cancer survivorship among Indian women. An overview. Asian J Nurs Education Res 12:262-266, 2022 [Google Scholar]
- 14.Loh KWJ, Ng T, Choo SP, et al. : Cancer supportive and survivorship care in Singapore: Current challenges and future outlook. JCO Glob Oncol 4:1-8, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Molassiotis A, Yates P, Li Q, et al. : Corrections to “Mapping unmet supportive care needs, quality-of-life perceptions and current symptoms in cancer survivors across the Asia-Pacific region: Results from the International STEP Study”. Ann Oncol 30:493, 2019 [DOI] [PubMed] [Google Scholar]
- 16.The ACTION Study Group; Peters S, Yip C, et al. : Health-related quality of life and psychological distress among cancer survivors in Southeast Asia: Results from a longitudinal study in eight low- and middle-income countries. BMC Med 15:10, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ostovar S, Modarresi Chahardehi A, Mohd Hashim IH, et al. : Prevalence of psychological distress among cancer patients in Southeast Asian countries: A systematic review. Eur J Cancer Care 31:e13669, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fielding R, Lam WWT, Shun SC, et al. : Attributing variance in supportive care needs during cancer: Culture-service, and individual differences, before clinical factors. PLoS One 8:e65099, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Donkor A, Atuwo-Ampoh VD, Yakanu F, et al. : Financial toxicity of cancer care in low- and middle-income countries: A systematic review and meta-analysis. Support Care Cancer 30:7159-7190, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.ACTION Study Group; Jan S, Kimman M, et al. : Financial catastrophe, treatment discontinuation and death associated with surgically operable cancer in South-East Asia: Results from the ACTION Study. Surgery 157:971-982, 2015 [DOI] [PubMed] [Google Scholar]
- 21.Chan RJ, Crawford-Williams F, Crichton M, et al. : Effectiveness and implementation of models of cancer survivorship care: An overview of systematic reviews. J Cancer Surviv 1-25, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Mollica MA, Mayer DK, Oeffinger KC, et al. : Follow-up care for breast and colorectal cancer across the globe: Survey findings from 27 countries. JCO Glob Oncol 6:1394-1411, 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chan RJ, on behalf of t, he STEP study collaborators, Yates P, Li Q, et al. : Oncology practitioners’ perspectives and practice patterns of post-treatment cancer survivorship care in the Asia-Pacific region: Results from the STEP study. BMC Cancer 17:715, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.The Economist : Cancer preparedness in Asia-Pacific: Progress towards universal cancer control. The Economist Intelligence Unit, 2020. https://worldcancerinitiative.economist.com/pdf/Roche-cancer-preparedness-in-asia/Roche_Cancer_White_paper.pdf [Google Scholar]
- 25.Ekeroma A, Dyer R, Palafox N, et al. : Cancer management in the Pacific region: A report on innovation and good practice. Lancet Oncol 20:e493-e502, 2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Anga G, Vince JD: Paediatric cancer in Papua New Guinea: Moving to the next stage. Papua New Guinea Med J 59:23-29, 2016 [Google Scholar]
- 27.Rodriguez-Galindo C, Friedrich P, Alcasabas P, et al. : Toward the cure of all children with cancer through collaborative efforts: Pediatric oncology as a global challenge. J Clin Oncol 33:3065-3073, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.CureAll Framework : WHO Global Initiative for Childhood Cancer: Increasing Access, Advancing Quality, Saving Lives. Geneva, Switzerland, World Health Organization, 2021 [Google Scholar]
- 29.Cancer Patient Organizations in Asia : Report of Findings from a Regional Survey. Rare Cancers Australia, 2016 [Google Scholar]
- 30.Le PD, Taylor C, Cabanes A, Tran HTT: Culture matters: Adapting supportive programs for cancer patients in low- and middle-income countries. Support Care Cancer 30:9-12, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Crawford-Williams F, Koczwara B, Chan RJ, et al. : Defining research and infrastructure priorities for cancer survivorship in Australia: A modified Delphi study. Support Care Cancer 30:3805-3815, 2022 [DOI] [PubMed] [Google Scholar]
- 32.Takahashi M: Cancer survivorship: Current status of research, care, and policy in Japan. Jpn J Clin Oncol 46:599-604, 2016 [DOI] [PubMed] [Google Scholar]
- 33.Witthayapipopsakul W, Kulthanmanusorn A, Vongmongkol V, et al. : Achieving the targets for universal health coverage: How is Thailand monitoring progress? WHO South East Asia. WHO South-East Asia J Public Health 8:10-17, 2019 [DOI] [PubMed] [Google Scholar]
- 34.Singh P, Travis P: Universal health coverage in the World Health Organization South-East Asia region: How can we make it "business unusual"? WHO South East Asia. WHO South-East Asia J Public Health 7:1-4, 2018 [DOI] [PubMed] [Google Scholar]
- 35.Liu C, Tang S: Integrated Care for Chronic Diseases in Asia Pacific Countries. New Delhi, India, World Health Organization Regional Office for South-East Asia, 2021 [Google Scholar]
- 36.2021 Annual Report of the Alliance for Health Policy and Systems Research. Geneva, Switzerland, World Health Organization; 2022 [Google Scholar]
- 37.Ranganathan P, Chinnaswamy G, Sengar M, et al. : The International Collaboration for Research Methods Development in Oncology (CReDO) workshops: Shaping the future of global oncology research. Lancet Oncol 22:e369-e376, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Eckhouse S, Lewison G, Sullivan R: Trends in the global funding and activity of cancer research. Mol Oncol 2:20-32, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alfano CM, Jefford M, Maher J, et al. : Building Personalized cancer follow-up care pathways in the United States: Lessons learned from implementation in England, Northern Ireland, and Australia. Am Soc Clin Oncol Ed Book 39:625-639, 2019 [DOI] [PubMed] [Google Scholar]
- 40.Jefford M, Howell D, Li Q, et al. : Improved models of care for cancer survivors. Lancet 399:1551-1560, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Jacobsen PB, Mollica MA: Understanding and addressing global inequities in cancer survivorship care. J Psychosoc Oncol Res Pract 1:e5, 2019 [Google Scholar]
- 42.Bradley CJ, Kitchen S, Bhatia S, et al. : Policies and practices to address cancer's long-term adverse consequences. J Natl Cancer Inst 114:1065-1071, 2022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Vaz-Luis I, Masiero M, Cavaletti G, et al. : ESMO Expert Consensus Statements on cancer survivorship: Promoting high-quality survivorship care and research in Europe. Ann Oncol 33:111903792-111911339, 2022 [DOI] [PubMed] [Google Scholar]
- 44.United Nations: United Nations Sustainable Development Goals. https://www.un.org/sustainabledevelopment/health/
- 45.WHO Global Strategy on Integrated People-Centred Health Services 2016-2026. Geneva, Switzerland, World Health Organization; 2015 [Google Scholar]
- 46.James SL, Abate D, Abate KH, et al. : Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 392:1789-1858, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]