Abstract
Introduction:
The National Academy of Medicine recommends the U.S. adopt an interpretative front-of-package food labeling system, but uncertainty remains about how this system should be designed. This study examined reactions to front-of-package food labeling systems that use positive labels to identify healthier foods, negative labels to identify unhealthier foods, or both.
Methods:
In August 2021, U.S. adults (n=3,051) completed an online randomized experiment. Participants were randomly assigned to 1 of 4 labeling conditions: control (calorie), positive, negative, or both positive and negative labels. Labels were adapted from designs for a “healthy” label drafted by the Food and Drug Administration and displayed on the front of products’ packaging. Participants selected products to purchase, identified healthier products, and reported reactions to the labels. Analyses, conducted in 2022, examined the healthfulness of participants’ selections using the Ofcom Nutrient Profiling Model score (0–100, higher scores are healthier).
Results:
Participants exposed to only positive labels, only negative labels, or both positive and negative labels had healthier selections than participants in the control arm (differences vs control=1.13 [2%], 2.34 [4%], and 3.19 [5%], respectively, all ps<0.01). The both-positive-and-negative-labels arm outperformed the only-negative-labels (p=0.03) and only-positive-labels arms (p<0.001). The only-negative-labels arm outperformed the only-positive-labels arm (p=0.005). All 3 interpretative labeling systems also led to improvements in identification of healthier products and beneficial psychological reactions (e.g., attention, thinking about health effects; all ps<0.05).
Conclusions:
Front-of-package food labeling systems that use both positive and negative labels could encourage healthier purchases and improve understanding more than systems using only positive or only negative labels.
INTRODUCTION
Unhealthy diet remains a leading cause of death in the U.S.1 Providing easy-to-understand nutrition information via labels is a core public health strategy for encouraging healthier eating. Currently, the main nutrition label required in the U.S. is the Nutrition Facts Label. This label is usually located on the back or side of product packaging and provides numeric nutrition information (e.g., calories, grams of sugar). By contrast, the National Academy of Medicine recommends adoption of a food labeling system that is displayed on the front of product packaging and that interprets product healthfulness, rather than only providing numeric information.2 Research indicates that such interpretative, front-of-package food labels could better inform consumers and encourage healthier food choices than the numeric, back-of-package Nutrition Facts Label.2-4
What remains unknown is how to design interpretative front-of-package food labeling systems to maximize these benefits. Existing and proposed labeling systems have taken varying approaches. For example, in 2021, the U.S. Food and Drug Administration (FDA) announced plans to develop a label to help consumers identify foods that meet FDA’s definition of “healthy.”5 The FDA’s proposed “healthy” label is an example of a positive (or endorsement) food labeling system in which positive labels are applied to products meeting nutrition standards but no information is provided about unhealthier products.3,4,6 By contrast, several Latin American countries have adopted warning label systems that use negative labels to discourage consumption of unhealthier foods,7 but do not label healthier products. Some voluntary labeling systems (e.g., NutriScore) use spectrum ratings that include both positive and negative labels (although not all of these systems explicitly reference healthfulness). Using both positive and negative labels could have additive effects, as these labels are posited to influence behavior through different pathways: among other differences, negative labels may elicit stronger emotional reactions, while positive labels may generate larger improvements in self-efficacy.8-11
Prior experiments have evaluated different food labeling systems, with most finding benefits from systems that explicitly identify unhealthier foods.12-20 Studies have not, however, directly compared only-positive, only-negative, and both-positive-and-negative labeling systems while also controlling for other influential aspects of label design such as size and shape. To inform regulatory action, this study examined consumer reactions to front-of-package food labeling systems that use only positive labels for healthier foods, only negative labels for unhealthier foods, or both.
METHODS
Study Sample
A national convenience sample of 3,674 U.S. adults (aged ≥18 years) was recruited in August 2021 through Cloud Research Prime Panels, a survey research firm. Online convenience samples can yield generalizable findings for experiments such as those used in this study.21 The Harvard Longwood Campus IRB approved the study. The study was pre-registered prior to data collection (https://aspredicted.org/XVW_HCC, https://aspredicted.org/TKL_JRQ).
Procedures
Participants completed an online survey (median duration=13.1 minutes). After providing informed consent, participants were randomly assigned using simple randomization to 1 of 4 labeling arms: (1) Control (only calorie labels were shown on products’ front of package); (2) Only positive labels (positive labels were added to healthier products with no additional labels on unhealthier products); (3) Only negative labels (negative labels were added to unhealthier products with no additional labels on healthier products); or (4) Both positive and negative labels (positive labels were added to healthier products and negative labels were added to unhealthier products). The control arm displayed calorie labels because these labels appear on the front of most packaged beverages and snack foods in the U.S.22 For the interpretative labeling arms, the interpretative labels were displayed alongside calorie labels to mimic how new labels would likely appear on products. At the time of the study, the FDA had not released its revised definition of “healthy,”23 so products were classified as “healthier” and “unhealthier” using regulatory standards from the United Kingdom (UK)24,25 (detailed below).
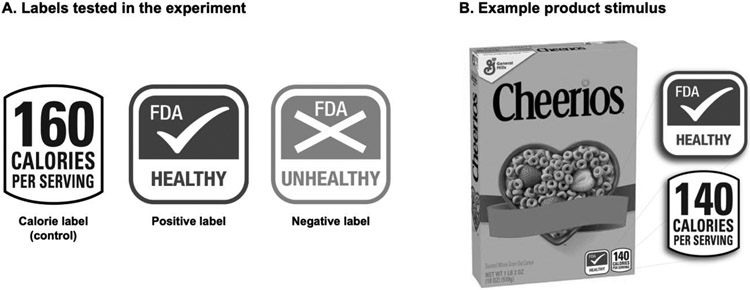
The study labels (Figure 1a) were modeled on labels proposed or adopted in the U.S. Calorie labels displayed calories per serving, similar to “Facts Up Front” labels.22 Positive labels were similar to labels drafted by FDA as part of their research on “healthy” symbols26 and were shown in green because green labels are perceived as healthier than other colors.20 Negative labels matched the positive labels on size, shape, and format, but were shown in red and used an “X” symbol to trigger automatic associations with “stop.”20,27
Figure 1. Front-of-package labels (Panel A) and example product stimulus (Panel B) used in experiment.
Note: Labels and products were shown in full color. Participants viewed 6–10 products in each category. Products displayed participants’ assigned label(s) on the front of products’ packaging alongside enlarged label(s) shown next to the products, as depicted in Panel B. All products displayed calorie labels, regardless of labeling arm.
In the main experiment, participants completed 4 purchase tasks, 1 in each of 4 product categories: beverages, cereals, soups, and snacks, shown in random order. These categories are top contributors to calories, sugar, sodium, and saturated fat consumption in the U.S.28-31 and include a range of healthier and unhealthier options. For each purchase task, participants were instructed to select the 1 item they would most like to purchase from a set of 6–10 products shown in random arrangement. A variety of flavors and product types were offered, including equal numbers of healthier and unhealthier products (Appendix Table 1). The survey displayed products with the participants’ assigned label(s) on the front of package alongside enlarged label(s) shown next to the product (Figure 1b). No prices were shown. To incentivize participants to select items they wanted to receive, the survey indicated that 25 participants would be randomly chosen to have one of their selections delivered to them or receive an electronic gift card of equivalent value. After completing the purchase tasks, participants responded to survey questions (detailed below).
Measures
The primary outcome was healthfulness of participants’ food and beverage selections, measured using the UK Ofcom Nutrient Profiling Model (NPM) system.24,25 Prospective studies demonstrate that healthier diets as identified by this model are associated with lower risk of obesity32 and cardiovascular disease.33 Foods lower in calories, saturated fat, sugar, and sodium and higher in fiber, protein, and fruit, vegetable, and nut content are scored as healthier. Healthfulness scores were calculated on a 1–100 scale, with higher scores indicating healthier selections.25,34-36 Products were categorized as “healthier” (score >62 for foods; >68 for beverages) or “unhealthier” (score ≤62 for foods; ≤68 for beverages) based on UK regulatory cutoffs for determining foods eligible to be marketed to children.24,25 One limitation of the Ofcom NPM is that beverages receive a narrower range of scores than foods because sugar is often the primary nutrient present in beverages. Therefore, analyses also assessed products’ calorie, saturated fat, sodium, total sugar, fiber, and protein densities as secondary outcomes. Appendix Table 1 details products’ nutritional content.
Next, the survey assessed participants’ ability to correctly identify healthier products. Participants viewed 4 pairs of products: 1 pair from each product category, with categories shown in random order. Each pair included 1 healthier and 1 unhealthier item shown in random arrangement. Products were displayed with calorie labels and participants’ randomly assigned label(s) (if any), similar to the purchase task. Participants selected the product they thought was healthier or indicated the products were equally healthy.37 Responses were coded as correct if participants selected the healthier item and incorrect otherwise.
Next, the survey assessed psychological reactions to the labels, outcomes that can shed light on labels’ potential to generate longer-term behavior change.3,8,38-41 Selection of psychological reactions was guided by the Warning Impact Model, which posits that warnings affect behavior by increasing attention, thinking about harms, and emotions,8,39 and by prior research on food and tobacco labels.38,42-44 Participants viewed their randomly assigned label and rated the label on perceived effectiveness, attention, thinking about health effects, negative emotions, message reactance, and label avoidance.8,45-49 Response options ranged from 1 (low) to 5 (high). Finally, the survey assessed whether the label increased perceived control over healthy eating decisions.50 Because reactions to positive and negative labels were expected to differ, participants rated only 1 label; participants assigned to both labels for the purchase tasks were re-allocated using simple randomization to view either the positive or the negative label.
At the end of the survey, participants were debriefed and informed that those randomly chosen in the lottery would receive a gift card of equivalent or greater value to their product selection. Participants could then request their data be deleted. Survey items and response options are shown in Appendix Table 2.
Statistical Analysis
Power analyses indicated that the target enrollment of ~3,100 would provide 80% power to detect a small effect (d=0.10) of each interpretative front-of-package label on healthfulness of selections compared to control, based on a prior study of food labels15 and assuming alpha=0.05 and correlation among repeated measures=0.6.51 Analyses excluded participants who did not complete the survey, completed the survey in <3.88 minutes (one-third of median completion time in a soft launch), or requested their data be excluded in the debrief (Appendix Figure 1). The analytic sample included 3,051 participants.
Analyses used mixed effects linear regression to examine the impact of labeling arm on the primary outcome (healthfulness of food and beverage selections) while accounting for repeated measures within participants. Models regressed healthfulness on indicator variables for labeling arm (excluding the control as the referent) and indicator variables for product category, treating the intercept as random. Analyses calculated average differential effects (ADEs, i.e., treatment effects) for each interpretative labeling arm (i.e., only-positive-labels, only-negative-labels, both-positive-and-negative-labels) compared to the control arm. Analyses then used χ2 tests to assess whether these ADEs differed from one another (indicating differential effectiveness of the interpretative labeling systems; the study was not specifically powered for these comparisons, though they were pre-registered). Moderation analyses added interactions between participant characteristics and labeling arms to primary models, using separate models for each potential moderator (age, gender, education, race/ethnicity, income, trust in the federal government, use of the Nutrition Facts Label, and perceived diet quality, Appendix Methods).
Similar models were used to examine secondary outcomes (i.e., nutrient densities and correct identification of healthier products). Analyses additionally used ordinary least squares (OLS) regressions to conduct similar analyses stratified by product category. Finally, analyses used OLS regression to examine psychological reactions to the labels. Continuous psychological variables were standardized prior to analyses to facilitate comparisons across outcomes assessed with different scales.
Analyses were conducted in Stata MP 17.1 in 2022. Analyses used 2-tailed tests and adjusted for multiple comparisons within families (i.e., dependent variables) by controlling the false discovery rate (FDR) at q=0.05 using the linear step-up method52 (Appendix Methods); adjusted p-values are reported.
RESULTS
Participants had an average age of 45.6 years (SD=18.7). About 59% identified as non-Hispanic White, 17% as non-Hispanic Black, 13% as Latino(a), and 11% as non-Hispanic other race or multi-racial (Table 1). The study sample had similar age, race, and education distributions as the U.S. overall, but included more females and households with lower income than the U.S. overall (Appendix Table 3).
Table 1.
Participant Characteristics, n=3,051 U.S. Adults
| Characteristic | Control (calorie labels) |
Only positive labels |
Only negative labels |
Both positive and negative labels |
|---|---|---|---|---|
| n=766 | n=760 | n=762 | n=763 | |
| N (%) | N (%) | N (%) | N (%) | |
| Age | ||||
| 18–29 years | 184 (24) | 186 (24) | 199 (26) | 206 (27) |
| 30–44 years | 196 (26) | 217 (29) | 177 (23) | 196 (26) |
| 45–59 years | 164 (21) | 147 (19) | 162 (21) | 137 (18) |
| 60 years or older | 222 (29) | 210 (28) | 224 (29) | 224 (29) |
| Gender | ||||
| Female | 461 (61) | 464 (61) | 448 (59) | 455 (60) |
| Male | 289 (38) | 282 (37) | 291 (38) | 292 (39) |
| Non-binary or another gender | 11 (1) | 12 (2) | 19 (3) | 10 (1) |
| Gay, lesbian, or bisexual | 90 (12) | 105 (14) | 99 (13) | 98 (13) |
| Latino(a) or Hispanic | 95 (13) | 92 (12) | 106 (14) | 93 (12) |
| Race | ||||
| White | 515 (68) | 504 (66) | 495 (65) | 491 (65) |
| Black or African American | 146 (19) | 144 (19) | 140 (18) | 144 (19) |
| American Indian or Alaska Native | 8 (1) | 16 (2) | 14 (2) | 21 (3) |
| Asian or Pacific Islander | 43 (6) | 42 (6) | 32 (4) | 49 (6) |
| Other or Multiracial | 48 (6) | 53 (7) | 77 (10) | 52 (7) |
| Education | ||||
| High school diploma or less | 213 (28) | 241 (32) | 226 (30) | 227 (30) |
| Some college | 211 (28) | 192 (25) | 190 (25) | 201 (27) |
| College graduate or associates degree | 264 (35) | 250 (33) | 251 (33) | 249 (33) |
| Graduate degree | 73 (10) | 76 (10) | 91 (12) | 80 (11) |
| Household income, annual | ||||
| $0 to $24,999 | 244 (32) | 240 (32) | 213 (28) | 238 (32) |
| $25,000 to $49,999 | 216 (28) | 204 (27) | 219 (29) | 225 (30) |
| $50,000 to $74,999 | 125 (16) | 136 (18) | 138 (18) | 118 (16) |
| $75,000 or more | 175 (23) | 179 (24) | 183 (24) | 168 (22) |
| Income ≤150% Federal Poverty Level | 262 (35) | 251 (33) | 249 (33) | 241 (32) |
| Use of Nutrition Facts panel | ||||
| Never or rarely | 242 (32) | 250 (33) | 232 (31) | 228 (30) |
| Sometimes | 299 (39) | 287 (38) | 290 (38) | 306 (41) |
| Most of the time or always | 220 (29) | 220 (29) | 233 (31) | 220 (29) |
| Self-rated diet quality | ||||
| Poor or fair | 235 (31) | 229 (30) | 237 (31) | 224 (30) |
| Good | 333 (44) | 322 (42) | 316 (42) | 337 (45) |
| Very good or excellent | 193 (25) | 208 (27) | 204 (27) | 193 (26) |
| Trust in federal government | ||||
| Never | 167 (22) | 159 (21) | 145 (19) | 167 (22) |
| Only sometimes | 370 (49) | 401 (53) | 404 (54) | 392 (52) |
| Most of the time or just about always | 223 (29) | 197 (26) | 205 (27) | 191 (25) |
Note: Proportions may not sum to 100% due to rounding. Missing data ranged from 0.0 to 1.4%.
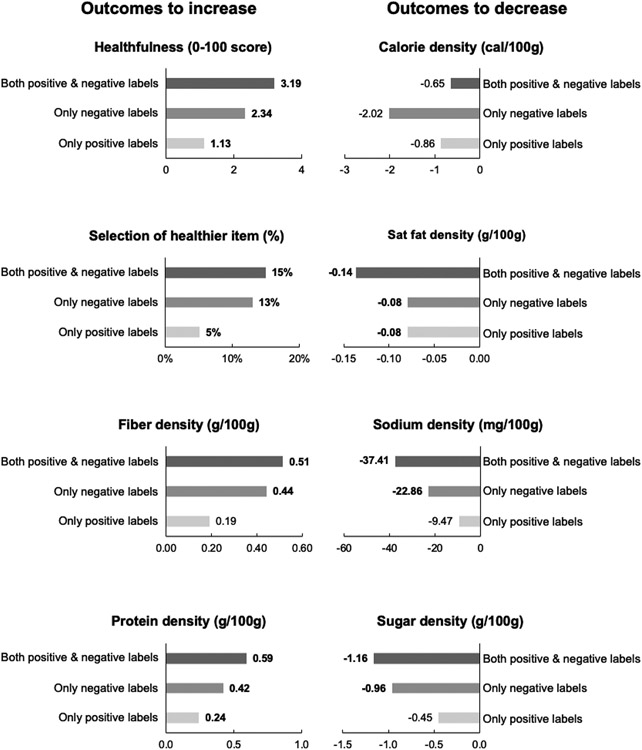
Participants in the only-positive-labels arm selected healthier foods and beverages than participants in the control arm (ADE=1.13 points on the 1–100 scale, 95% CI: 0.38, 1.88, p=0.007, Figure 2, Appendix Tables 4 and 5), an approximate 2% improvement. Likewise, participants in the only-negative-labels arm had healthier selections than participants in the control arm (ADE=2.34, 95% CI: 1.59, 3.09, p<0.001, ~4% improvement), as did participants in the both-positive-and-negative-labels arm (ADE=3.19, 95% CI: 2.44, 3.94, p<0.001, ~5% improvement). The effects of the 3 interpretative labeling systems differed from one another. The both-positive-and-negative-labels system outperformed the only-negative-labels system (p for comparison of ADEs=0.03) and the only-positive-labels system (p<0.001). Additionally, the only-negative-labels system outperformed the only-positive-labels system (p=0.005).
Figure 2. Impact of interpretative front-of-package food and beverage labeling systems relative to the control arm (calorie labels only) on purchase task outcomes.
Note: Healthfulness and classification as a healthier item were assessed using the UK Ofcom Nutrient Profiling Model24,25 on a 1–100 scale, where higher scores indicate foods are healthier.25 Figure shows impact of labeling systems that used only positive labels, only negative labels, and both positive and negative labels, expressed as differences compared to the control arm. Bold values indicate the outcome for participants in the interpretative labeling arm was statistically different from the outcome for participants in the control arm, p<0.05.
The interpretative labels also led to improvements in the nutritional profile of product selections. These included reductions of 0.08–0.14 g/100g in saturated fat density, 9.47–37.41 mg/100g in sodium density, and 0.45–1.16 g/100g in sugar density compared to the control arm, as well as increases of 0.19–0.51 g/100g in fiber density and 0.24–0.59 g/100g in protein density (though improvements in sugar, sodium, and fiber density for the only-positive-labels arm were not statistically significant). Labeling arms did not differ from one another in calorie density. For most nutrient density outcomes, exposure to the both-positive-and-negative-labels system led to significantly larger improvements than exposure to the only-positive-labels system, while there were few significant differences between the both-positive-and-negative-labels system and the only-negative-labels system (Appendix Table 5).
The interpretative front-of-package labels also improved consumers’ ability to correctly identify healthier items (range of ADEs=11–23 percentage points, all ps<0.001). The largest improvements were observed among consumers exposed to the both-positive-and-negative-labels system (Appendix Table 5).
The pattern of results for purchase outcomes and consumer understanding was similar in analyses stratifying by product category (Appendix Tables 6-9). Exceptions included that in the stratified analyses, the only-positive-labels system did not increase overall healthfulness for cereal, soup, or snack selections compared to the control arm. Another exception was that all 3 of the interpretative labeling systems reduced calorie density for beverage selections.
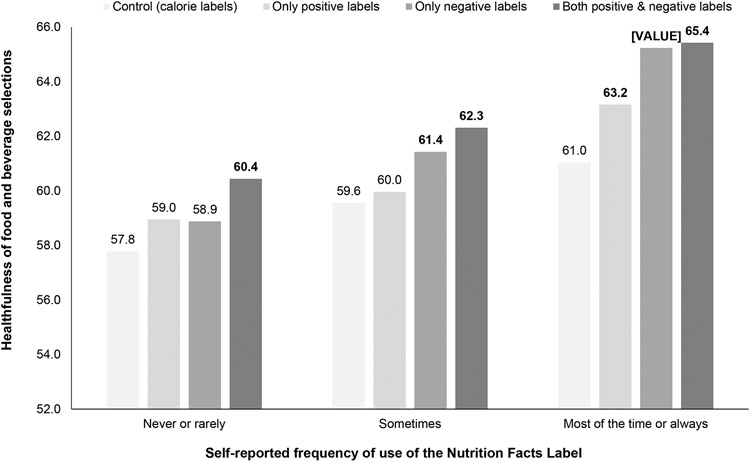
In moderation analyses, the impact of the interpretative labeling systems on purchase healthfulness did not differ by most participant characteristics, including by age, gender, education level, race/ethnicity, income, trust in the government, or perceived diet quality (all ps for joint significance of interaction terms >0.05). The only exception was that the 3 interpretative labeling systems led to larger increases in healthfulness (vs. control) for participants who reported using the Nutrition Facts Label most of the time or always (range of ADEs=2.1–4.4 points) compared to participants who reported using the label sometimes (range of ADEs=0.4–2.8) or rarely or never (range of ADEs=1.1–2.7; p for interaction=0.03; Figure 3).
Figure 3. Healthfulness of food and beverage selections in purchase tasks, by labeling arm and self-reported use of the Nutrition Facts Label.
Note: Product healthfulness was assessed using the UK Ofcom Nutrient Profiling Model24,25 on a 1–100 scale, where higher scores are healthier.25 Figure shows predicted mean healthfulness in the purchase task by labeling arm and self-reported frequency of use of the Nutrition Facts Label. Bold values indicate that the predicted mean in the interpretative labeling arm is statistically different from the predicted mean in the control arm, p<0.05.
In survey questions assessing label reactions, both the positive and the negative labels were rated as more effective at discouraging unhealthy food purchases and more effective at encouraging healthy food purchases than the calorie label (range of ADEs=0.09–0.44, ps<0.05, Appendix Table 10). Likewise, compared to the calorie label control, both interpretative labels led to higher self-reported attention and more thinking about health effects (range of ADEs=0.20–0.42) and increased participants’ likelihood of reporting the label made them feel “more in control of making healthy eating decisions” (ADEs=8–11 percentage points) (all ps≤0.001). The positive label led to lower negative emotions than the calorie label (ADE= −0.15), while the negative label led to higher negative emotions (ADE=0.55) (ps≤0.001). The negative label led to more reactance (ADE=0.42) and avoidance (ADE=0.43) than the calorie label (ps<0.001), while the positive label did not affect reactance or avoidance. The 2 interpretative labels differed on several outcomes: the negative label led to higher attention, negative emotions, perceived discouragement, reactance, and avoidance ratings than the positive label (ps<0.01).
DISCUSSION
In this randomized experiment with a large sample of U.S. adults, exposure to any interpretative front-of-package food label led to improvements in consumer understanding and healthfulness of hypothetical food and beverage selections. The largest benefits were observed among participants exposed to both positive and negative labels. The labeling system that used only negative labels also outperformed the system that used only positive labels, consistent with prior studies.12-14 These findings align with negative dominance theory9 and suggest that interpretative front-of-package labeling systems should explicitly discourage less healthy products, rather than only encouraging healthier options.
The negative labels led to higher self-reported attention and negative emotions than the positive labels, similar to prior research.12 These reactions may explain why the negative labels led to healthier product selections than the positive labels, given that research on cigarette8 and sugary drink38,53 warnings has found that attention and negative emotions are key pathways through which warnings affect consumer behavior. Participants also reported stronger desire to avoid looking at the negative labels than the positive labels, but prior research indicates that avoidance is a sign that consumers are processing messages more deeply.42 These results suggest that food labels should be designed to grab attention and generate emotional responses, even if these designs also lead consumers to want to avoid looking at the labels.
The effects of the interpretative front-of-package labeling systems on healthfulness of selections did not differ by most participant characteristics tested. The one exception was that the interpretative labeling systems led to larger improvements in healthfulness among participants who reported using the Nutrition Facts Label more frequently. This suggests that implementation of new front-of-package labels should be supported by educational campaigns encouraging consumers to use food labels, similar to those that accompanied implementation of Chile’s front-of-package warnings.54
The effects of the interpretative labels on participants’ product selections were relatively small, equivalent to improvements of 2%–5% in overall healthfulness and 3%–14% in sugar, sodium, saturated fat, fiber, and protein densities compared to the control arm. Although new labeling systems could have additional benefits beyond their effects on consumer behavior (e.g., by spurring product reformulation3,55-60), additional policies beyond labels will likely be needed to curb diet-related diseases. Moreover, front-of-package labeling systems generally shift consumers toward healthier versions of ultra-processed foods, and alternate approaches may be needed to encourage consumption of whole foods.3
Although the interpretative labels led to substantial improvements in consumers’ ability to identify healthier items, 20%–46% of participants exposed to these labels still failed to identify healthier items, depending on product category. This may be because products in the interpretative labeling arms showed the interpretative labels alongside calorie labels; the inclusion of multiple labels may confuse consumers, particularly in instances when lower-calorie products are not healthier than higher-calorie options. Additional research on the independent and joint effects of different front-of-package labels is warranted.
Limitations
Strengths of this study include the large sample, randomized design, and use of real products as experimental stimuli. Limitations include that labels’ color, message, and symbol were varied simultaneously, so analyses could not disentangle the individual effects of these characteristics. Additionally, the experimental setting differed in several ways from the real world. One difference was that labels were shown as enlarged callouts next to products, likely making labels more salient61 and potentially drawing attention to the study’s purpose. However, online retailers could choose to—or policymakers could require them to—display front-of-package labels in a similar manner as in this study. Other differences between the experimental design and the real-world included that a single threshold was applied to differentiate healthier/unhealthier products, which may not be realistic; no prices were shown; and participants viewed a small selection of products with an even ratio of healthier/unhealthier foods. Additionally, selections were hypothetical and could be affected by social desirability bias. To reduce this possibility, responses were anonymous62 and participants were incentivized to select items they wanted.
CONCLUSIONS
Interpretative front-of-package labeling systems hold promise for informing consumers and promoting healthier diets. Labeling systems that use both positive and negative labels could encourage healthier purchases and promote consumer understanding more than systems using only positive or only negative labels.
Supplementary Material
ACKNOWLEDGMENTS
AHG was supported by T32 HL 098048 and K01 HL 158608. AAM was supported by T32 CA 057711. MGS was supported by T32 DK 007703.
The funders had no role in the management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; or decision to submit the manuscript for publication.
Footnotes
The authors have no conflicts of interest to declare. The authors have no financial disclosures.
REFERENCES
- 1.Mokdad AH, Ballestros K, Echko M, et al. The state of US health, 1990-2016: Burden of diseases, injuries, and risk factors among US states. JAMA. 2018;319(14):1444–1472. 10.1001/jama.2018.0158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nathan R, Yaktine A, Lichtenstein AH, Wartella EA. Front-of-Package Nutrition Rating Systems and Symbols: Promoting Healthier Choices. National Academies Press; 2012. [PubMed] [Google Scholar]
- 3.Roberto CA, Ng SW, Ganderats-Fuentes M, et al. The influence of front-of-package nutrition labeling on consumer behavior and product reformulation. Annu Rev Nutr. 2021;41:529–550. 10.1146/annurev-nutr-111120-094932. [DOI] [PubMed] [Google Scholar]
- 4.Kelly B, Jewell J. What Is the Evidence on the Policy Specifications, Development Processes and Effectiveness of Existing Front-of-Pack Food Labelling Policies in the WHO European Region? World Health Organization; 2018. https://www.euro.who.int/en/publications/abstracts/what-is-the-evidence-on-the-policy-specifications,-development-processes-and-effectiveness-of-existing-front-of-pack-food-labelling-policies-in-the-who-european-region-2018. Accessed June 12, 2022. [PubMed] [Google Scholar]
- 5.U.S. Food and Drug Administration. FDA In Brief: FDA Issues Procedural Notice on Potential Plans to Conduct Research About Use of 'Healthy' Symbols on Food Products. FDA. https://www.fda.gov/news-events/press-announcements/fda-brief-fda-issues-procedural-notice-potential-plans-conduct-research-about-use-healthy-symbols. Published May 6, 2021. Accessed June 12, 2022. [Google Scholar]
- 6.Jones A, Neal B, Reeve B, Mhurchu CN, Thow AM. Front-of-pack nutrition labelling to promote healthier diets: current practice and opportunities to strengthen regulation worldwide. BMC Glob Health. 2019;4(6):e001882. 10.1136/bmjgh-2019-001882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Global Food Research Program. Countries with mandatory or voluntary interpretative labels on packaged foods and drinks. https://docs.google.com/viewer?url=https%3A%2F%2Fwww.globalfoodresearchprogram.org%2Fwp-content%2Fuploads%2F2021%2F09%2FFOP_Regs_maps_2021_September.pdf. Published September 2021. Accessed June 12, 2022. [Google Scholar]
- 8.Brewer N, Parada H Jr., Hall M, Boynton M, Noar S, Ribisl K. Understanding why pictorial cigarette pack warnings increase quit attempts. Ann Behav Med. 2019;53(3):232–243. 10.1093/abm/kay032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rozin P, Royzman E. Negativity bias, negativity dominance, and contagion. Pers Soc Psychol Rev. 2001;5(4):296–320. 10.1207/S15327957PSPR0504_2. [DOI] [Google Scholar]
- 10.Petty RE, Cacioppo JT. Communication and Persuasion: Central and Peripheral Routes to Attitude Change. Springer; 1986. 10.1016/S0065-2601(08)60214-2. [DOI] [Google Scholar]
- 11.Gallagher KM, Updegraff JA. Health message framing effects on attitudes, intentions, and behavior: A meta-analytic review. Ann Behav Med. 2012;43(1):101–116. 10.1007/s12160-012-9446-6. [DOI] [PubMed] [Google Scholar]
- 12.de Alcantara M, Ares G, de Castro IPL, Deliza R Gain vs. loss-framing for reducing sugar consumption: Insights from a choice experiment with six product categories. Food Res Int. 2020;136:109458. 10.1016/j.foodres.2020.109458. [DOI] [PubMed] [Google Scholar]
- 13.Neal B, Crino M, Dunford E, et al. Effects of Different Types of Front-of-Pack Labelling Information on the Healthiness of Food Purchases-A Randomised Controlled Trial. Nutrients. 2017;9(12):1284. 10.3390/nu9121284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ares G, Varela F, Machin L, et al. Comparative performance of three interpretative front-of-pack nutrition labelling schemes: Insights for policy making. Food Qual Pref. 2018;68:215–225. 10.1016/j.foodqual.2018.03.007. [DOI] [Google Scholar]
- 15.Ducrot P, Julia C, Méjean C, et al. Impact of different front-of-pack nutrition labels on consumer purchasing intentions: A randomized controlled trial. Am J Prev Med. 2016;50(5):627–636. 10.1016/j.amepre.2015.10.020. [DOI] [PubMed] [Google Scholar]
- 16.Talati Z, Egnell M, Hercberg S, Julia C, Pettigrew S. Food choice under five front-of-package nutrition label conditions: an experimental study across 12 countries. Am J Public Health. 2019;109(12):1770–1775. 10.2105/AJPH.2019.305319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Egnell M, Talati Z, Hercberg S, Pettigrew S, Julia C. Objective Understanding of Front-of-Package Nutrition Labels: An International Comparative Experimental Study across 12 Countries. Nutrients. 2018;10(10):1542. 10.3390/nu10101542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hagmann D, Siegrist M. Nutri-Score, multiple traffic light and incomplete nutrition labelling on food packages: Effects on consumers' accuracy in identifying healthier snack options. Food Qual Pref. 2020;83:103894. 10.1016/j.foodqual.2020.103894. [DOI] [Google Scholar]
- 19.Egnell M, Talati Z, Galan P, et al. Objective understanding of the Nutri-score front-of-pack label by European consumers and its effect on food choices: an online experimental study. Int J Behav Nutr Phys Act. 2020;17(1):1–13. 10.1186/s12966-020-01053-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cabrera M, Machín L, Arrúa A, et al. Nutrition warnings as front-of-pack labels: Influence of design features on healthfulness perception and attentional capture. Public Health Nutr. 2017;20(18):3360–3371. 10.1017/S136898001700249X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jeong M, Zhang D, Morgan J, et al. Similarities and differences in tobacco control research findings from convenience and probability samples. Ann Behav Med. 2018;53(5):476–485. 10.1093/abm/kay059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Watson E Facts Up Front labels now on 90% of foods in some categories, says GMA as it launches new educational website. bakeryandsnacks.com. https://www.bakeryandsnacks.com/Article/2013/04/18/Facts-up-Front-labels-now-on-90-of-foods-in-some-categories. Published May 18, 2017. Accessed June 12, 2022. [Google Scholar]
- 23.Food and Drug Administration. Use of the Term Healthy on Food Labeling. FDA. https://www.fda.gov/food/food-labeling-nutrition/use-term-healthy-food-labeling. Published online March 23, 2022. Accessed June 12, 2022. [Google Scholar]
- 24.Department of Health. Nutrient Profiling Technical Guidance. United Kingdom Department of Health; 2011. https://docs.google.com/viewer?url=https%3A%2F%2Fassets.publishing.service.gov.uk%2Fgovernment%2Fuploads%2Fsystem%2Fuploads%2Fattachment_data%2Ffile%2F216094%2Fdh_123492.pdf. Accessed June 12, 2022. [Google Scholar]
- 25.Rayner M, Scarborough P, Lobstein T. The UK Ofcom Nutrient Profiling Model: Defining “healthy” and “Unhealthy” Foods and Drinks for TV Advertising to Children. 2009. https://docs.google.com/viewer?url=https%3A%2F%2Fwww.ndph.ox.ac.uk%2Fcpnp%2Ffiles%2Fabout%2Fuk-ofcom-nutrient-profile-model.pdf. Accessed June 12, 2022. [Google Scholar]
- 26.U.S. Food and Drug Administration. Agency Information Collection Activities; Proposed Collection; Comment Request; Quantitative Research on a Voluntary Symbol Depicting the Nutrient Content Claim "Healthy" on Packaged Foods. https://www.regulations.gov/docket/FDA-2021-N-0336/document. Published May 7, 2021. Accessed June 12, 2022.
- 27.Grummon AH, Hall MG, Taillie LS, Brewer NT. How should sugar-sweetened beverage health warnings be designed? A randomized experiment. Prev Med. 2019;121:158–166. 10.1016/j.ypmed.2019.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Huth PJ, Fulgoni VL, Keast DR, Park K, Auestad N. Major food sources of calories, added sugars, and saturated fat and their contribution to essential nutrient intakes in the US diet: Data from the National Health and Nutrition Examination Survey (2003-2006). Nutr J. 2013;12(1):1–10. 10.1186/1475-2891-12-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Poti JM, Dunford EK, Popkin BM. Sodium reduction in US households' packaged food and beverage purchases, 2000 to 2014. JAMA Intern Med. 2017;177(7):986–994. 10.1001/jamainternmed.2017.1407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bailey RL, Fulgoni VL, Cowan AE, Gaine PC. Sources of added sugars in young children, adolescents, and adults with low and high intakes of added sugars. Nutrients. 2018;10(1):102. 10.3390/nu10010102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Quader ZS, Zhao L, Gillespie C, et al. Sodium intake among persons aged≥ 2 years-United States, 2013-2014. MMWR Morb Mortal Wkly Rep. 2017;66(12):324. 10.15585/mmwr.mm6612a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Egnell M, Seconda L, Neal B, et al. Prospective associations of the original Food Standards Agency nutrient profiling system and three variants with weight gain, overweight and obesity risk: results from the French NutriNet-Santé cohort. Br J Nutr. 2021;125(8):902–914. 10.1017/S0007114520003384. [DOI] [PubMed] [Google Scholar]
- 33.Adriouch S, Julia C, Kesse-Guyot E, et al. Prospective association between a dietary quality index based on a nutrient profiling system and cardiovascular disease risk. Eur J Prev Cardiol. 2016;23(15):1669–1676. 10.1177/2047487316640659. [DOI] [PubMed] [Google Scholar]
- 34.Bragg MA, Liu PJ, Roberto CA, Sarda V, Harris JL, Brownell KD. The use of sports references in marketing of food and beverage products in supermarkets. Public Health Nutr. 2013;16(4):738–742. 10.1017/S1368980012003163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bragg MA, Yanamadala S, Roberto CA, Harris JL, Brownell KD. Athlete endorsements in food marketing. Pediatrics. 2013;132(5):805–810. 10.1542/peds.2013-0093. [DOI] [PubMed] [Google Scholar]
- 36.Findling MTG, Werth PM, Musicus AA, et al. Comparing five front-of-pack nutrition labels' influence on consumers' perceptions and purchase intentions. Prev Med. 2018;106:114–121. 10.1016/j.ypmed.2017.10.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Musicus AA, Moran AJ, Lawman HG, Roberto CA. Online randomized controlled trials of restaurant sodium warning labels. Am J Prev Med. 2019;57(6):e181–e193. 10.1016/j.amepre.2019.06.024. [DOI] [PubMed] [Google Scholar]
- 38.Grummon AH, Brewer NT. Health warnings and beverage purchase behavior: Mediators of impact. Ann Behav Med. 2020;54(9):691–702. 10.1093/abm/kaaa011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Noar S, Hall M, Francis D, Ribisl K, Pepper J, Brewer N. Pictorial cigarette pack warnings: A meta-analysis of experimental studies. Tob Control. 2015;25:341–354. 10.1136/tobaccocontrol-2014-051978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Noar SM, Barker J, Bell T, Yzer M. Does perceived message effectiveness predict the actual effectiveness of tobacco education messages? A systematic review and meta-analysis. Health Commun. 2018;35(2):148–157. 10.1080/10410236.2018.1547675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bigsby E, Cappella JN, Seitz HH. Efficiently and effectively evaluating public service announcements: Additional evidence for the utility of perceived effectiveness. Commun Monogr. 2013;80(1):1–23. 10.1080/03637751.2012.739706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hall MG, Mendel JR, Noar SM, Brewer NT. Why smokers avoid cigarette pack risk messages: Two randomized clinical trials in the United States. Soc Sci Med. 2018;213:165–172. 10.1016/j.socscimed.2018.07.049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hall MG, Sheeran P, Noar SM, et al. Negative affect, message reactance and perceived risk: How do pictorial cigarette pack warnings change quit intentions? Tob Control. 2017;27(e2):e136–e142. 10.1136/tobaccocontrol-2017-053972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Baig SA, Noar SM, Gottfredson NC, Lazard AJ, Ribisl KM, Brewer NT. Message perceptions and effects perceptions as proxies for behavioral impact in the context of anti-smoking messages. Prev Med Rep. 2021;23:101434. 10.1016/j.pmedr.2021.101434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Nonnemaker J, Farrelly M, Kamyab K, Busey A, Mann N. Experimental Study of Graphic Cigarette Warning Labels. RTI International; 2010. https://www.fda.gov/media/136126/download. Accessed June 12, 2022. [Google Scholar]
- 46.Fathelrahman AI, Omar M, Awang R, Cummings KM, Borland R, Samin ASBM. Impact of the new Malaysian cigarette pack warnings on smokers' awareness of health risks and interest in quitting smoking. Int J Envir Res Public Health. 2010;7(11):4089–4099. 10.3390/ijerph7114089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hall MG, Sheeran P, Noar SM, Ribisl KM, Boynton MH, Brewer NT. A brief measure of reactance to health warnings. J Behav Med. 2017;40(3):520–529. 10.1007/s10865-016-9821-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Baig SA, Noar SM, Gottfredson NC, Boynton MH, Ribisl KM, Brewer NT. UNC Perceived Message Effectiveness: Validation of a brief scale. Ann Behav Med. 2019;53(8):732–742. 10.1093/abm/kay080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Hyland A, Ambrose BK, Conway KP, et al. Design and methods of the Population Assessment of Tobacco and Health (PATH) Study. Tob Control. 2017;26(4):371–378. 10.1136/tobaccocontrol-2016-052934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Acton R, Hammond D. Do consumers think front-of-package "high in" warnings are harsh or reduce their control? A test of food industry concerns. Obesity (Silver Spring). 2018;26(11):1687–1691. 10.1002/oby.22311. [DOI] [PubMed] [Google Scholar]
- 51.French SA, Wall M, Mitchell NR, Shimotsu ST, Welsh E. Annotated receipts capture household food purchases from a broad range of sources. Int J Behav Nutr Phys Act. 2009;6(1):37. 10.1186/1479-5868-6-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J R Stat Soc Series B Stat Methodol. 1995;57(1):289–300. 10.1111/j.2517-6161.1995.tb02031.x. [DOI] [Google Scholar]
- 53.Donnelly G, Zatz L, Svirsky D, John L. The effect of graphic warnings on sugary-drink purchasing. Psychol Sci. 2018;29(8):1321–1333. 10.1177/0956797618766361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Taillie LS, Reyes M, Colchero MA, Popkin B, Corvalán C. An evaluation of Chile's Law of Food Labeling and Advertising on sugar-sweetened beverage purchases from 2015 to 2017: A before-and-after study. PLOS Med. 2020;17(2):e1003015. 10.1371/journal.pmed.1003015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Reyes M, Taillie LS, Popkin B, Kanter R, Vandevijvere S, Corvalán C. Changes in the amount of nutrient of packaged foods and beverages after the initial implementation of the Chilean Law of Food Labelling and Advertising: A nonexperimental prospective study. PLOS Med. 2020;17(7):e1003220. 10.1371/journal.pmed.1003220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Vyth EL, Steenhuis IH, Roodenburg AJ, Brug J, Seidell JC. Front-of-pack nutrition label stimulates healthier product development: a quantitative analysis. Int J Behav Nutr Phys Act. 2010;7:65. 10.1186/1479-5868-7-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Grummon AH, Petimar J, Zhang F, et al. Calorie labeling and product reformulation: A longitudinal analysis of supermarket prepared foods. Am J Prev Med. 2021;61(3):377–385. 10.1016/j.amepre.2021.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Grummon AH, Petimar J, Soto M, et al. Changes in calorie content of menu items at large chain restaurants after implementation of calorie labels. JAMA Netw Open. 2021;4(12):e2141353. 10.1001/jamanetworkopen.2021.41353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Eckel Robert H, Borra Susan, Lichtenstein Alice H, Yin-Piazza Shirley Y. Understanding the Complexity of Trans Fatty Acid Reduction in the American Diet. Circulation. 2007;115(16):2231–2246. 10.1161/CIRCULATIONAHA.106.181947. [DOI] [PubMed] [Google Scholar]
- 60.Mhurchu CN, Eyles H, Choi YH. Effects of a voluntary front-of-pack nutrition labelling system on packaged food reformulation: The Health Star Rating System in New Zealand. Nutrients. 2017;9(8). 10.3390/nu9080918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Dubois P, Albuquerque P, Allais O, et al. Effects of front-of-pack labels on the nutritional quality of supermarket food purchases: Evidence from a large-scale randomized controlled trial. J Acad Mark Sci. 2021;49(1):119–138. 10.1007/s11747-020-00723-5. [DOI] [Google Scholar]
- 62.Grimm P Social desirability bias. In: Kamakura W, ed. Wiley International Encyclopedia of Marketing. John Wiley & Sons, Ltd; 2011. 10.1002/9781444316568.wiem02057. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.