Abstract
Background.
Cognitive development after schizophrenia onset can be shaped by interventions such as cognitive remediation, yet no study to date has investigated whether patterns of early behavioral development may predict later cognitive changes following intervention. We therefore investigated the extent to which premorbid adjustment trajectories predict cognitive remediation gains in schizophrenia.
Methods.
In a total sample of 215 participants (170 first-episode schizophrenia participants and 45 controls), we classified premorbid functioning trajectories from childhood through late adolescence using the Cannon-Spoor Premorbid Adjustment Scale. For the 62 schizophrenia participants who underwent 6 months of computer-assisted, bottom-up cognitive remediation interventions, we identified MATRICS Consensus Cognitive Battery scores for which participants demonstrated mean changes after intervention, then evaluated whether developmental trajectories predicted these changes.
Results.
Growth mixture models supported three premorbid functioning trajectories: stable-good, deteriorating, and stable-poor adjustment. Schizophrenia participants demonstrated significant cognitive remediation gains in processing speed, verbal learning, and overall cognition. Notably, participants with stable-poor trajectories demonstrated significantly greater improvements in processing speed compared to participants with deteriorating trajectories.
Conclusions.
This is the first study to our knowledge to characterize the associations between premorbid functioning trajectories and cognitive remediation gains after schizophrenia onset, indicating that 6 months of bottom-up cognitive remediation appears to be sufficient to yield a full standard deviation gain in processing speed for individuals with early, enduring functioning difficulties. Our findings highlight the connection between trajectories of premorbid and postmorbid functioning in schizophrenia and emphasize the utility of considering the lifespan developmental course in personalizing therapeutic interventions.
Keywords: Adolescent development, behavioral intervention, child development, clinical prediction, cognition, cognitive training, developmental course, developmental psychopathology, processing speed, psychosis, social functioning, treatment outcome
Introduction
Neurodevelopmental models of schizophrenia suggest that individuals who ultimately develop schizophrenia undergo early changes in brain development and cognition which are reflected in diverse trajectories of premorbid functioning (Murray & Lewis, 1987; Weinberger, 1987). Although brain development after psychosis onset may be shaped by interventions such as cognitive remediation (Eack et al., 2010; Mothersill & Donohoe, 2019; Ramsay & MacDonald, 2015; Vinogradov, Fisher, & de Villers-Sidani, 2012), it remains unclear whether early developmental trajectories predict cognitive gains following intervention in schizophrenia. To address this gap in the literature, we investigated the extent to which premorbid adjustment trajectories predict individual treatment response to cognitive remediation in first-episode schizophrenia.
Cognitive deficits are widely observed in schizophrenia and are one of the most useful predictors of functioning (Cohen’s d = 0.25) (Fett et al., 2011; Green, Kern, & Heaton, 2004; Kuo et al., 2018). Despite the necessity of pharmacological interventions for treating psychotic symptoms, most antipsychotic medications cause little to no change in cognition (Clissold & Crowe, 2019; Miyamoto, Miyake, Jarskog, Fleischhacker, & Lieberman, 2012; Nielsen et al., 2015), although their consistent use may allow cognitive remediation to be more effective (Nuechterlein et al., 2020). In contrast to limited antipsychotic effects, cognitive remediation in schizophrenia improves both cognition (Cohen’s d = 0.29–0.45) and everyday functioning (Cohen’s d = 0.22–0.41) (Vita et al., 2021; Wykes, Huddy, Cellard, McGurk, & Czobor, 2011). Cognitive remediation interventions systematically improve cognition by helping individuals with schizophrenia practice cognitive exercises, refine problem-solving strategies, and generalize cognitive practices to real-world functioning (Bowie et al., 2020).
Meta-analytic predictions of treatment response suggest that larger cognitive remediation gains are associated with lower educational attainment, lower premorbid IQ, lower global functioning, and higher symptom severity (Vita et al., 2021). These demographic and clinical characteristics overlap with premorbid risk factors associated with transition to psychosis in individuals at clinical high risk (Oliver et al., 2020) and with correlates of premorbid adjustment trajectories in schizophrenia (Chan, Shanahan, Ospina, Larsen, & Burdick, 2019; Cole, Apud, Weinberger, & Dickinson, 2012; Horton, Tarbox, Olino, & Haas, 2015), thereby hinting at the possibility that premorbid courses of development can predict not only clinical course but also the effectiveness of cognitive remediation in modifying clinical course.
In considering premorbid courses of development, individuals with schizophrenia on average demonstrate increasing impairments in social activity and consistently poorer academic and occupational functioning up to 15 years before first hospitalization (Velthorst et al., 2016). In literature dating back to at least 1969, individuals with schizophrenia with higher levels of premorbid functioning generally demonstrate better treatment response to pharmacological interventions compared to individuals with lower levels of premorbid functioning (Goldstein, Judd, Rodnick, & LaPolla, 1969; Hatzimanolis et al., 2020; Klein & Rosen, 1973; Rabinowitz et al., 2011; Strous et al., 2004). Similarly, overall premorbid functioning has been shown to positively predict overall cognitive remediation outcomes (Buonocore et al., 2019). These studies have generally used overall levels of premorbid functioning as predictors of treatment response, thereby masking changes in premorbid functioning across development and making it difficult to infer whether individual courses of premorbid functioning are associated with treatment response. The most informative work to date showed that individuals with schizophrenia can be classified into three trajectories based on changes between premorbid and current IQ (general cognitive ability): compromised, deteriorated, and preserved trajectories (Seccomandi et al., 2021). Notably, the preserved cognitive trajectory showed more gains in executive functioning and working memory than the other two trajectories. Acknowledging that the results of this study contrast with prior meta-analytic findings suggesting greater cognitive remediation gains in individuals with lower premorbid IQ (Vita et al., 2021), behavioral development before schizophrenia onset may influence cognitive remediation outcomes after schizophrenia onset.
Taken together, demographic and clinical factors associated with poor overall premorbid functioning predict larger cognitive remediation gains in the most recent meta-analysis (Vita et al., 2021), whereas initial work investigating differences between premorbid and current IQ indicates that stable-good premorbid cognitive trajectories predict better cognitive remediation treatment response than deteriorating or stable-poor cognitive trajectories (Seccomandi et al., 2021). The most relevant study to date defined premorbid trajectories as the change between premorbid and current IQ (Seccomandi et al., 2021), rather than evaluating multiple periods of premorbid development. As far as we are aware, no studies yet have investigated whether trajectories of premorbid functioning over successive developmental periods are associated with cognitive remediation outcomes. Thus, there is little evidence to date regarding whether good or poor trajectories of premorbid functioning predict increased cognitive remediation gains. Our aim was therefore to establish the extent to which premorbid developmental trajectories predict individual treatment response to cognitive remediation in first-episode schizophrenia. Specifically, we hypothesized that individuals with stable-good trajectories would demonstrate better treatment response to cognitive remediation compared to individuals with deteriorating or stable-poor trajectories.
Methods
Sample
The overall sample consisted of 215 participants, including 62 participants with first-episode schizophrenia who underwent cognitive remediation, 108 participants with first-episode schizophrenia who did not undergo cognitive remediation, and 45 healthy participants who did not undergo cognitive remediation (see online Supplementary Fig. S1 for study flowchart). The participants were drawn from studies at the UCLA Aftercare Research Program (Nuechterlein et al., 2020, 2021; Ventura et al., 2015, 2019). We used a large sample of participants with and without schizophrenia to maximally inform developmental trajectories. Schizophrenia participants were recruited from Los Angeles psychiatric hospitals and clinics and were included if they: (1) had experienced a first psychotic episode within the last 2 years; (2) had a DSM-IV diagnosis of schizophrenia, schizoaffective disorder, depressed type, or schizophreniform disorder using the Structured Clinical Interview for DSM-IV (First, Spitzer, Gibbon, & Williams, 1995); (3) were aged 18–45 years; (4) did not have any known neurological disorder; (5) had no current or recent significant and habitual substance abuse in 6 months prior to study entry and the psychotic disorder was not substance-induced; (6) had a premorbid IQ of at least 70 assessed using the Wechsler Test of Adult Reading (WTAR; Wechsler, 2001); and (7) were sufficiently fluent in English to complete clinical measures. Healthy participants were included if they met the following criteria: (1) did not have any significant DSM-IV psychiatric diagnosis; (2) were aged 18–45 years; (3) did not have any known neurological disorder; (4) did not show significant and habitual drug or alcohol abuse in the 6 months prior to study entry; (5) had a premorbid IQ of at least 70 assessed using the WTAR; and (6) were sufficiently fluent in English to complete clinical measures. The study was approved by the UCLA Institutional Review Boards and all participants provided written informed consent.
Measures
Premorbid adjustment
All participants underwent functioning assessment using the Cannon-Spoor Premorbid Adjustment Scale (PAS; Cannon-Spoor, Potkin, & Wyatt, 1982), a well-established, retrospective clinical rating scale with substantial predictive and concurrent validity and test-retest reliability (Brill, Reichenberg, Weiser, & Rabinowitz, 2008; Morice, Urbanc, & McNicol, 1985). Raters were trained by author J.V., who has decades of experience in training research raters in premorbid adjustment measures. Based on patient interview, the PAS assesses functioning prior to the onset of psychotic symptoms during childhood (ages 5–11), early adolescence (ages 12–15), late adolescence (ages 16–18), and adulthood (ages 19 and older). For each developmental period, functioning was assessed across multiple social and academic domains: (1) sociability and withdrawal; (2) peer relationships; (3) social-sexual relationships (after childhood); (4) scholastic performance (before adulthood); and (5) adaptation to school (before adulthood). The PAS social and academic domains are equivalent across sexes and developmental periods (Allen et al., 2013). Items were rated on a 0–6 Likert scale, with 0 representing good adjustment and 6 representing poor adjustment. In line with prior literature (Horton et al., 2015), scores for adult development were excluded to reduce the possible influence of active psychotic symptoms. Adjustment scores were averaged across domains for each developmental period to summarize overall adjustment at each period, consistent with prior studies (Bechi et al., 2020; Chan et al., 2019; Cole et al., 2012; Horton et al., 2015).
Cognitive remediation treatment response
Schizophrenia participants who underwent cognitive remediation completed the MATRICS Consensus Cognitive Battery (MCCB; Nuechterlein et al., 2008). As a widely-adopted, gold-standard battery for evaluating cognitive changes responsive to intervention in schizophrenia, the MCCB comprises 10 tests in seven cognitive domains: (1) Speed of Processing: Trail Making Test, Part A; the Brief Assessment of Cognition in Schizophrenia (BACS) Symbol Coding subtest; Category Fluency, Animal Naming; (2) Attention/Vigilance: Continuous Performance Test, Identical Pairs; (3) Working Memory: Wechsler Memory Scale, 3rd Edition, Spatial Span subtest; Letter-Number Span test; (4) Verbal Learning: Hopkins Verbal Learning Test – Revised, Immediate Recall; (5) Visual Learning: Brief Visuospatial Memory Test – Revised, Immediate Recall; (6) Reasoning & Problem Solving: Neuropsychological Assessment Battery (NAB), Mazes subtest; and (7) Social Cognition: Mayer-Salovey-Caruso Emotional Intelligence Test (MSCEIT), Managing Emotions branch. An overall composite T score is derived from the T scores for the seven cognitive domain scores. Cognitive remediation gain scores for each participant were computed by subtracting the T score at baseline from the T score at 6 months for each cognitive domain, such that positive gain scores indicated cognitive improvements whereas negative gain scores indicated cognitive declines.
Intervention
Sixty-two schizophrenia participants completed computer-assisted cognitive remediation intervention over 6 months concurrent with antipsychotic medication treatment. Thirty-four participants completed 2 h weekly of cognitive remediation integrating approaches from Neurocognitive Enhancement Therapy (NET; Bell, Bryson, Greig, Corcoran, & Wexler, 2001) and Neuropsychological Educational Approach to Remediation (NEAR; Medalia, Herlands, & Revheim, 2009) as part of the Nuechterlein et al. (2020) study. The other 28 participants completed 4 h weekly of cognitive remediation using Posit Science BrainHQ exercises (Fisher et al., 2015; Mahncke et al., 2006) as part of the Nuechterlein et al. (2021) study.
Although the intervention protocols were part of independent randomized clinical trials, they shared essential overlap in treatment approaches. Consistent with bottom-up training approaches to cognitive remediation (Best & Bowie, 2017), participants across both protocols initially trained in lower-level cognitive skills including processing speed and attention exercises, and then progressed to verbal and visual memory exercises of increasing complexity. Cognitive remediation group sessions included 4–5 participants supervised by a masters- or doctoral-level cognitive trainer. The cognitive trainer provided personalized feedback including positive reinforcement for reaching program goals and suggested task strategies, as described by Medalia et al. (2009). Participants in both protocols also completed 1 h weekly of trainer-facilitated Bridging group sessions focused on discussing strategies for applying the learned cognitive skills in real-world contexts. These Bridging sessions included active engagement from participants, structured feedback from trainers, and peer-to-peer support about improving functioning in academic, occupational, and social domains.
Data preparation
PAS scores were complete and cognitive remediation gain scores were complete except for 3 scores in attention/vigilance (and thus also in overall composite cognitive performance). Cognitive remediation gain scores were examined for outliers. For a minimum score that was at least 5 T score points (0.5 s.d.) lower than the next lowest score, the score was Winsorized to the next lowest score. Maximum scores were similarly Winsorized. A total of 4 cognitive performance gain scores were adjusted. After adjustment, cognitive remediation gain scores for each cognitive domain showed skew of <0.5 and kurtosis of <±0.7.
Analyses
To classify developmental trajectories in the overall sample, we conducted a series of growth mixture models based on mean adjustment scores for each developmental period. Using Mplus, version 8 (Muthén & Muthén, 2010), we compared the fit statistics of models with 1–5 classes. We compared the best-fitting models with prior model classifications reported in the literature to ensure interpretability. We also evaluated fit statistics including entropy (ranging from 0 to 1, with higher values indicating good classification separation), minimum cluster size (with the smallest cluster size being at least 5% of the sample size), and the Bayesian Information Criterion (BIC). We also conducted parametric bootstrapped likelihood ratio tests to evaluate whether a given model fit better than a model with one fewer class. We then used classifications from the selected model to predict cognitive remediation gains.
Within schizophrenia participants who underwent cognitive remediation, we conducted one-sample t tests to determine whether gain scores for each cognitive domain differed significantly from 0. We used χ2 tests and t tests to confirm that developmental trajectory memberships or cognitive remediation gain scores did not differ significantly between intervention protocols. For the cognitive domains in which participants demonstrated significant mean changes after cognitive remediation, we conducted one-way ANOVAs to test whether membership in a developmental trajectory class predicted cognitive gain scores. We then used a multiple regression model to evaluate the extent to which developmental trajectories predict cognitive remediation gain scores beyond key demographic and clinical variables. Analyses evaluating multiple cognitive domains were Bonferroni-corrected (Dunn, 1961).
Results
Sample characteristics
In the overall sample, participants were on average males aged 22 years old with approximately 13 years of parental education (Table 1). Schizophrenia participants had experienced psychosis onset around 21 years of age on average and had been ill for approximately 1 year. Compared to schizophrenia participants and healthy participants who did not undergo cognitive remediation, schizophrenia participants who underwent cognitive remediation did not differ significantly in demographic or clinical variables except for race; participants who underwent cognitive remediation were more likely than those who did not undergo cognitive remediation to identify as African-American, Hispanic/Latinx, or Native American, and less likely to identify as Caucasian. Furthermore, participants in the two intervention protocols did not differ significantly for any demographic or clinical variable except for race, with participants in the BrainHQ protocol being more likely than participants in the NET/NEAR protocol to identify as Hispanic/Latinx or Multiracial/Other (online Supplementary Table S1).
Table 1.
Sample characteristics
| Characteristic | Overall Sample (N = 215) |
Schizophrenia Participants With Cognitive Remediation (N = 62) |
Schizophrenia Participants Without Cognitive Remediation (N = 108) |
Healthy Participants Cognitive Without Remediation (N = 45) |
Statistic | df | p | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean/N | s.d./% | Mean/N | s.d./% | Mean/N | s.d./% | Mean/N | s.d./% | ||||
| Age (years) | 22.39 | 3.94 | 22.29 | 3.61 | 22.43 | 4.32 | 22.42 | 3.47 | 0.025 | 2, 212 | 0.975 |
| Sex (male) | 152 | 70.7% | 48 | 77.4% | 77 | 71.3% | 27 | 60.0% | 3.857 | 2 | 0.145 |
| Parental education (years) | 13.74 | 3.77 | 13.87 | 3.88 | 13.78 | 3.59 | 13.48 | 4.09 | 0.149 | 2, 206 | 0.861 |
| Race | |||||||||||
| African-American | 40 | 18.6% | 19 | 30.7% | 16 | 14.8% | 5 | 11.1% | 8.629 | 2 | 0.013 |
| Asian-American/Pacific Islander | 29 | 13.5% | 5 | 8.1% | 19 | 17.6% | 5 | 11.1% | 3.340 | 2 | 0.188 |
| Caucasian | 109 | 50.7% | 22 | 35.5% | 58 | 53.7% | 29 | 64.4% | 9.534 | 2 | 0.009 |
| Hispanic/Latinx | 11 | 5.1% | 7 | 11.3% | 4 | 3.7% | 0 | 0.0% | 7.739 | 2 | 0.021 |
| Native American | 5 | 2.3% | 4 | 6.5% | 1 | 0.9% | 0 | 0.0% | 6.650 | 2 | 0.036 |
| Multiracial/Other | 21 | 9.8% | 5 | 8.1% | 10 | 9.3% | 6 | 13.3% | 0.885 | 2 | 0.642 |
| Age at psychosis onset (years) | – | – | 21.06 | 3.78 | 21.13 | 4.36 | – | – | 0.011 | 1, 165 | 0.918 |
| Illness duration (years) | – | – | 1.26 | 1.0 | 1.28 | 1.58 | – | – | 0.046 | 1, 165 | 0.831 |
Note. Results of one-way ANOVAs are presented for age, parental education, age at psychosis onset, and illness duration, whereas χ2 tests are reported for sex and race. Parental education was computed from the mean of maternal education and paternal education.
Classifying developmental trajectories
Although the four-trajectory model showed slightly better fit statistics than the three-trajectory model (Table 2), the three-trajectory model showed good fit statistics. Importantly, each of the trajectories in the three-trajectory model matched the trajectories reported in previous studies of premorbid adjustment trajectories (Bechi et al., 2020; Chan et al., 2019; Cole et al., 2012; Horton et al., 2015). We therefore selected the three-trajectory model for further analysis. Overall, 21 participants showed a stable-good trajectory, 28 showed a deteriorating trajectory, and 13 showed a stable-poor trajectory.
Table 2.
Fit statistics of growth mixture models classifying developmental trajectories
| Model | BIC | LRT ( p value) | Entropy | Minimum class size | Minimum class probability |
|---|---|---|---|---|---|
| 1 Class | 1831.886 | – | – | 215 | 1.000 |
| 2 Class | 1629.934 | 223.435 (<0.001) | 0.830 | 79 | 0.924 |
| 3 Class | 1594.504 | 56.912 (<0.001) | 0.793 | 31 | 0.862 |
| 4 Class | 1578.765 | 37.222 (<0.001) | 0.819 | 20 | 0.861 |
| 5 Class | 1580.569 | 19.678 (<0.001) | 0.815 | 8 | 0.792 |
BIC, Bayes Information Criterion; LRT, Likelihood Ratio Test.
Note. Bolded items indicate the model that best matched the prior literature.
Mean adjustment scores differed significantly by trajectory classification [F(2, 212) = 439.687, p < 0.001] and by developmental period [F(1.6, 339.06) = 35.125, p < 0.001], and the interaction between trajectory classification and developmental period was not significant [F(3.2, 339.06) = 1.898, p = 0.125] (Fig. 1, online Supplementary Table S2). For all three trajectories, adjustment did not differ significantly from childhood to early adolescence but worsened from early adolescence to late adolescence. The deteriorating trajectory showed generally intermediate premorbid adjustment compared to the stable-good and stable-poor trajectories.
Fig. 1.
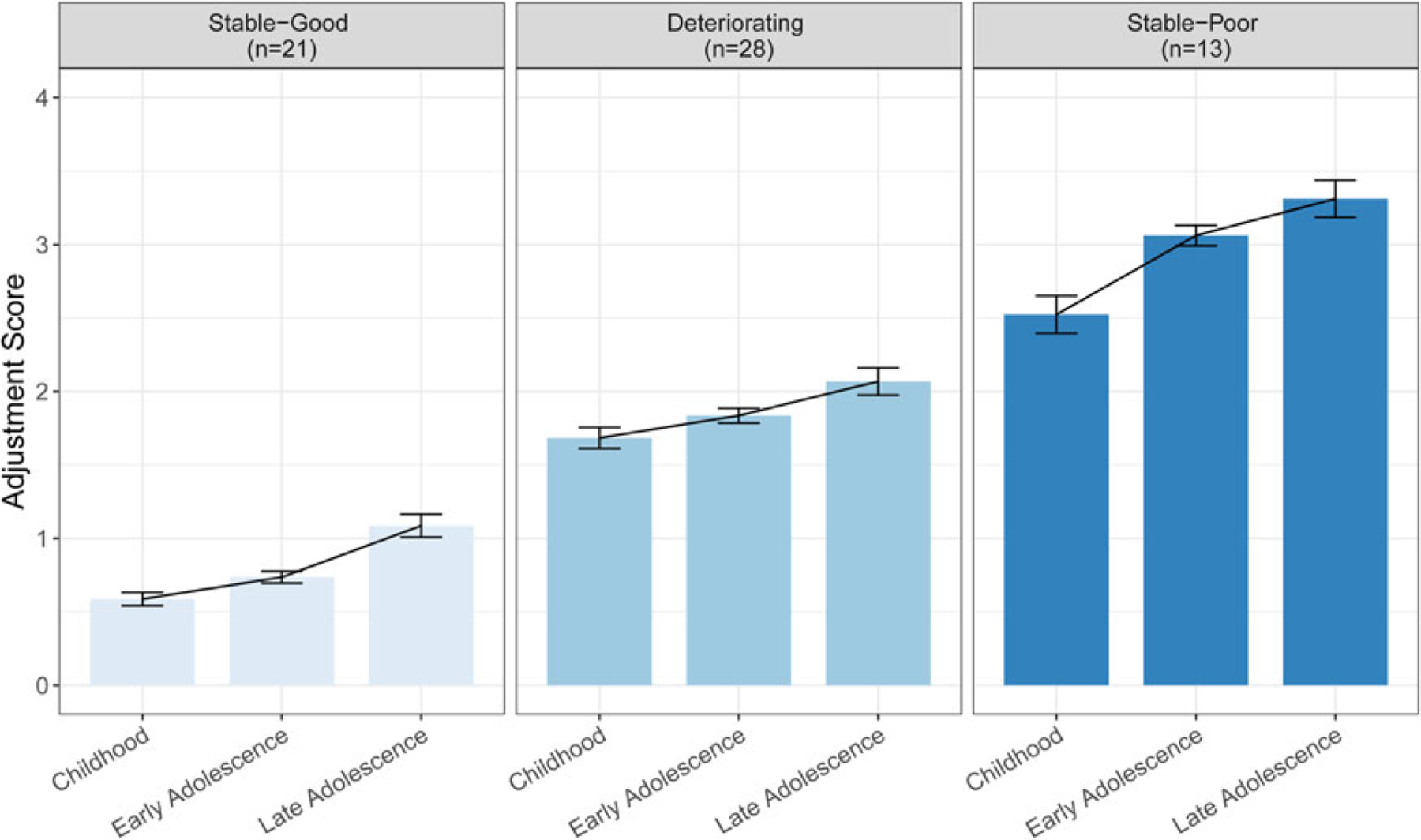
Adjustment scores by developmental trajectory classification.
Note. Adjustment scores based on Cannon-Spoor Premorbid Adjustment Scale (PAS; Cannon-Spoor et al., 1982), with higher scores representing worse adjustment (possible range: 0–6). Across trajectories, average childhood adjustment scores ranged from 0.59 (0.44) to 2.52 (0.71), average early adolescence adjustment scores ranged from 0.74 (0.40) to 3.06 (0.39), and average late adolescence adjustment scores ranged from 1.09 (0.77) to 3.31 (0.70). Standard errors are presented as error bars.
Developmental trajectories differed significantly by sex and by race, with a greater proportion of males being assigned to deteriorating and stable-poor trajectories compared to the stable-good trajectory and a greater proportion of African-American participants being assigned to the stable-poor trajectory compared to the stable-good trajectory (online Supplementary Table S3). Furthermore, compared to healthy participants who were largely classified in the stable-good trajectory, schizophrenia participants were overrepresented in the deteriorating and stable-poor trajectories compared to the stable-good trajectory (online Supplementary Fig. S2).
Predicting cognitive remediation treatment response
After undergoing 6 months of cognitive remediation, schizophrenia participants on average demonstrated significant improvements in overall composite, speed of processing, and verbal learning (Fig. 2, Supplementary Table S4). Participants showed substantial variability in treatment response, with average cognitive change ranging from 0.69 to 5.18 points. Participants did not differ between intervention protocols in cognitive remediation gain scores or developmental trajectory classifications (online Supplementary Tables S5–S6). Within the cognitive remediation sample, membership in the stable-good trajectory comprised 21 participants (33.9%), membership in the deteriorating trajectory comprised 28 participants (45.2%), and membership in the stable-poor trajectory comprised 13 participants (21.0%).
Fig. 2.
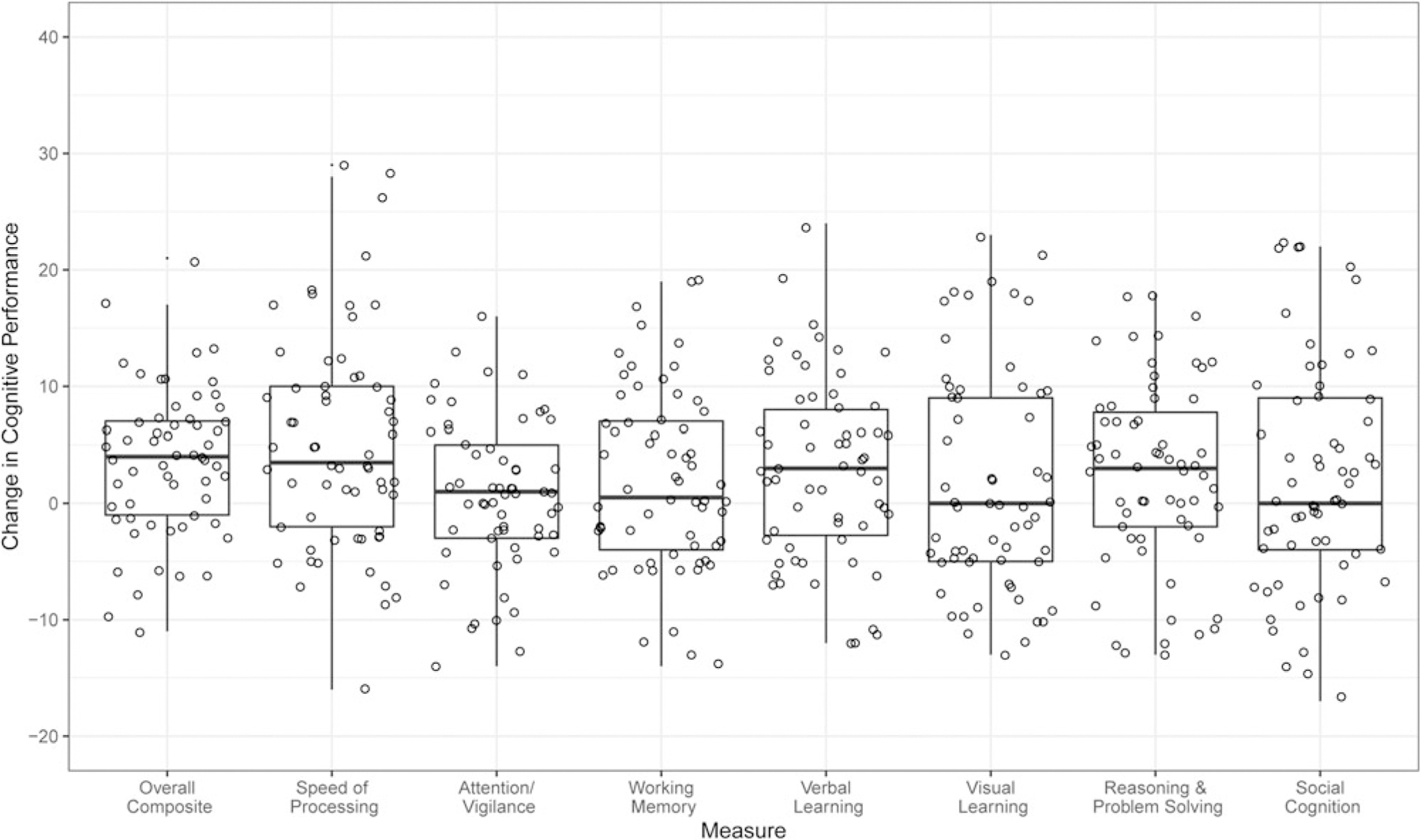
Overall cognitive remediation gains.
Note. Cognitive remediation T scores (mean = 50, s.d. = 10) change between baseline and 6 months of cognitive remediation, with positive values indicating cognitive improvements. p values are Bonferroni-corrected for multiple comparisons. Significant gains: *p < 0.05; ***p < 0.001.
Next, we tested whether developmental trajectories predict changes in overall composite, speed of processing, and verbal learning. Across developmental trajectories, participants demonstrated similar gains in overall composite [F(2, 56) = 1.54, p = 0.670] and in verbal learning [F(2, 59) = 0.015, p = 1.000] (Fig. 3). In contrast, participants demonstrated differential gains in speed of processing based on developmental trajectory membership [F(2, 59) = 4.771, p = 0.036]. On average, participants with a stable-poor trajectory demonstrated speed of processing T score gains of 11.00 points (s.d. = 11.37) in speed of processing, whereas participants with a deteriorating trajectory demonstrated gains of 2.00 points (s.d. = 6.45) and participants with a stable-good trajectory demonstrated of 5.81 points (s.d. = 9.62). Post-hoc pairwise t tests indicated that participants with a stable-poor trajectory showed larger improvements in speed of processing than participants with a deteriorating trajectory [t(15.69) = −2.66, p = 0.018] but did not differ significantly from participants with a stable-good trajectory [t(22.36) = −1.37, p = 0.184]. In addition, participants with a stable-good trajectory did not differ significantly in speed of processing compared to participants with a deteriorating trajectory [t(32.97) = 1.57, p = 0.126]. Compared to deteriorating trajectories, stable-poor trajectories predicted cognitive remediation gains in speed of processing even after accounting for age, sex, parental education, race, age at psychosis onset, and intervention protocol (online Supplementary Table S7). Sensitivity analyses controlling for baseline cognitive scores produced the same overall pattern of results, suggesting that these findings are unlikely to result from regression to the mean.
Fig. 3.
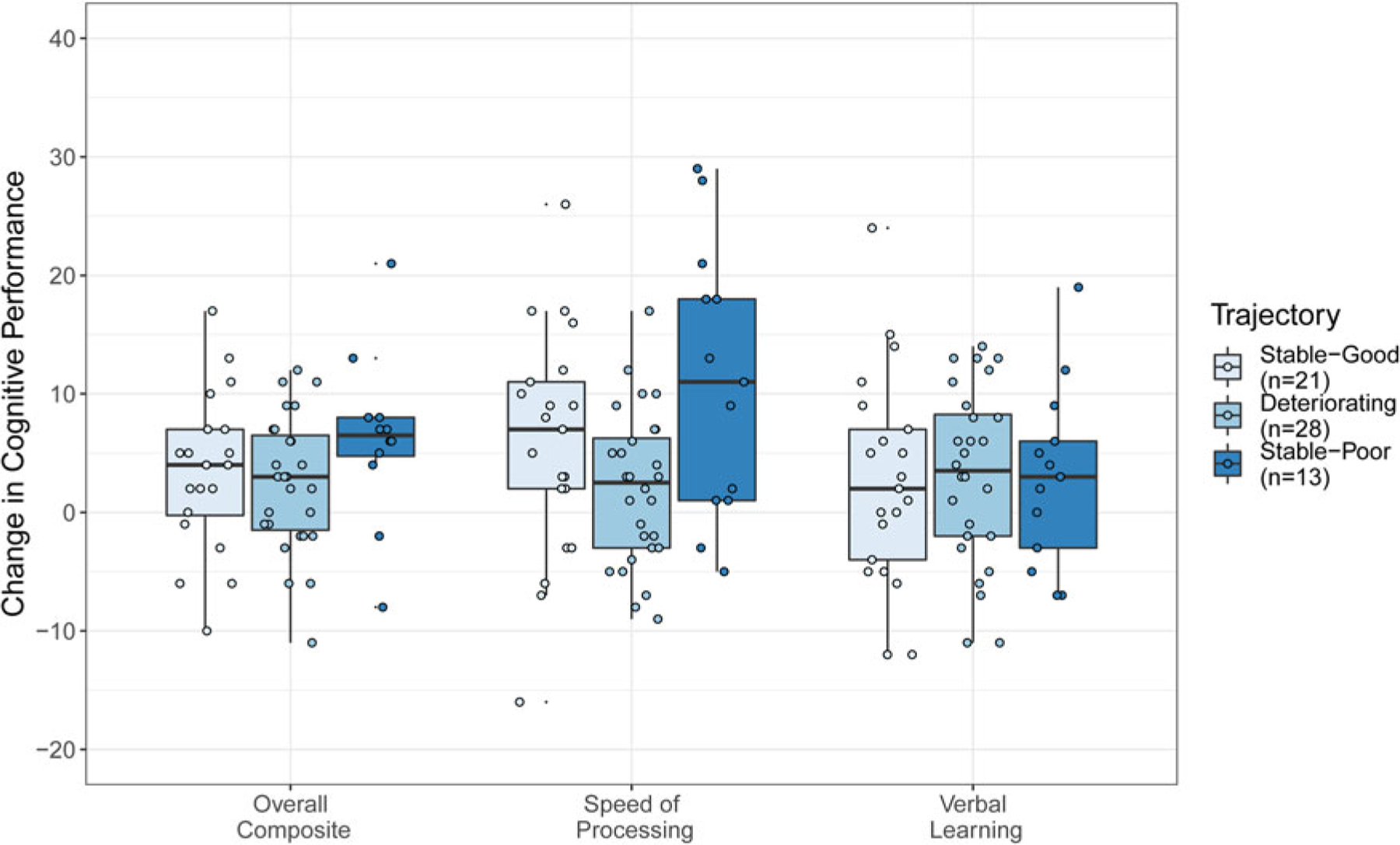
Cognitive remediation gains by developmental trajectory classification.
Note. Cognitive remediation gains are differences in T scores (mean = 50, s.d. = 10) between baseline and after 6 months of cognitive remediation, with positive values indicating cognitive improvements. Significant gains: *p < 0.05 (posthoc comparisons between trajectories in speed of processing were not additionally corrected for multiple comparisons).
Discussion
This is the first study to our knowledge to use developmental trajectories based on adjustment or functioning to predict cognitive remediation treatment response after schizophrenia onset. We replicated prior literature reporting that individuals with schizophrenia can be classified into stable-good, deteriorating, and stable-poor developmental trajectories of premorbid functioning (Bechi et al., 2020; Chan et al., 2019; Cole et al., 2012; Horton et al., 2015). After undergoing 6 months of bottom-up cognitive remediation, individuals with stable-poor developmental trajectories show markedly greater processing speed gains than individuals with deteriorating developmental trajectories. Taking into consideration that the average processing speed gain across the intervention sample was approximately 5.18 T score points (s.d. = 9.28) and that T score distributions have a mean of 50 and a s.d. of 10, an 11 T score point improvement constitutes a full standard deviation improvement in cognitive remediation outcomes for individuals with early, enduring functioning difficulties.
Developmental trajectories did not predict overall cognitive improvements nor verbal learning improvements but predicted processing speed improvements, suggesting that trajectories may not predict generalized cognitive improvements but may instead predict improvements in specific cognitive domains. Our findings build upon the most relevant prior work to date, which used cognitive trajectory classifications to predict cognitive remediation treatment response for executive functioning and working memory, and did not evaluate processing speed or verbal learning (Seccomandi et al., 2021). This earlier study indicated that a preserved cognitive trajectory (most similar to the stable-good trajectory in our study) was associated with increased gains in executive functioning and working memory as compared to the compromised trajectory (similar to the stable-poor trajectory in our study) and the deteriorated trajectory (similar to the deteriorating trajectory in our study) (Seccomandi et al., 2021). IQ reflects general cognitive ability and is more heavily based on higher-level cognitive domains compared to processing speed, and processing speed is impaired in schizophrenia even after accounting for IQ (Knowles, David, & Reichenberg, 2010). Notably, the premorbid developmental trajectories in our study are based on social functioning and academic functioning (which is a rough index of cognitive functioning), which differ from the purely cognitive trajectories reported in the earlier study (Seccomandi et al., 2021). Thus, cognitive trajectories may better predict cognitive remediation gains for higher-order cognitive abilities such as working memory and executive functioning whereas the premorbid developmental trajectories in our study better predict cognitive remediation gains for processing speed rather than verbal learning or overall cognitive performance.
This work underscores continuity between premorbid development and postmorbid development in schizophrenia treated with cognitive remediation (MacBeth & Gumley, 2008). Our results are broadly consistent with recent findings in individuals who show premorbid functioning difficulties that are sufficiently impairing to imply clinical high risk for psychosis (Catalan et al., 2021). Poor premorbid functioning across development predicts psychosis conversion in this at-risk population (Nieman et al., 2014; Tarbox et al., 2013). Furthermore, for individuals at clinical high risk for psychosis, processing speed shows the largest impairment of all cognitive domains (Randers et al., 2021), may account for deficits in other cognitive domains (Hauser et al., 2017), and can improve with bottom-up cognitive remediation (Friedman-Yakoobian, Parrish, Eack, & Keshavan, 2020; Glenthøj, Hjorthøj, Kristensen, Davidson, & Nordentoft, 2017). Given that all three trajectories showed improvements in overall cognitive performance and in two subdomains in our study, cognitive remediation provides an additional boost in processing speed for the stable-poor trajectory. Taken together, individuals who show substantial functioning difficulties before schizophrenia onset, especially from early on in their developmental course, show benefits in processing speed following bottom-up cognitive remediation.
We were able to demonstrate a connection between premorbid development and postmorbid outcome due to the consistent developmental timing of cognitive remediation in the intervention sample, with schizophrenia participants having undergone assessment and intervention within 2 years of experiencing a first psychotic episode. Our developmental trajectory classifications were further informed by including healthy participants, who were largely classified as having stable-good trajectories, in contrast to schizophrenia participants. Our study’s three-trajectory classification has been previously identified in first-episode schizophrenia and in chronic schizophrenia (Bechi et al., 2020; Chan et al., 2019; Cole et al., 2012; Horton et al., 2015), suggesting that this developmental trajectory model does not depend on illness chronicity. Compared to individuals in the chronic stages of illness, individuals in the early stages of illness show larger cognitive remediation gains for processing speed, working memory, and executive functioning (Bowie, Grossman, Gupta, Oyewumi, & Harvey, 2014; Corbera, Wexler, Poltorak, Thime, & Kurtz, 2017; Deste et al., 2019). Thus, although individuals show smaller cognitive remediation gains in chronic illness stages compared to early illness stages, premorbid developmental trajectories may show similar relationships with cognitive remediation gains during later, chronic developmental periods of schizophrenia as in earlier, recent-onset developmental periods of schizophrenia.
This study presents an innovative framework for linking trajectories of premorbid functioning to cognitive changes following intervention. Classifying premorbid developmental trajectories in the large overall sample enabled us to characterize developmental trajectories in schizophrenia relative to developmental trajectories in healthy participants. The recency of psychosis onset in the intervention sample minimized confounding from illness iatrogenic effects such as long-term antipsychotic use. Moreover, the intervention sample completed assessments of premorbid functioning across several domains and key developmental periods and demonstrated a wide range of cognitive performance gains across multiple cognitive domains in a gold-standard assessment battery. Overall, participants showed diverse developmental trajectories and diverse treatment responses to cognitive remediation.
Acknowledging these strengths, our findings should be considered in light of certain limitations. Our measure of premorbid functioning was retrospective and would be bolstered by converging evidence from prospective measures of premorbid functioning. However, this limitation is not unique to our study design and is a challenge for any study of premorbid functioning in individuals who have a schizophrenia diagnosis. Intervention changes could be influenced by factors that affect cognitive test performance, such as motivation, effort, or defeatist beliefs. Given that these factors could also have been improved through the course of cognitive remediation, future studies may evaluate whether these factors meaningfully contribute to the relationship between developmental trajectories and cognitive remediation performance. The size of the intervention sample was also moderate and the smallest classified group in this sample was the developmental trajectory showing the largest intervention gains. Despite the limited sample size, the cognitive remediation gains in the stable-poor trajectory group are striking and warrant larger-scale replication efforts. Furthermore, the two intervention protocols involved different treatment doses, with half of the intervention sample undergoing 2 h weekly of cognitive remediation and the other half of the intervention sample undergoing 4 h weekly of cognitive remediation. Despite the differences in intervention doses between the protocols, the two intervention protocols did not differ in developmental trajectory memberships or cognitive gain scores across cognitive domains, and the overall pattern of findings remained the same after accounting for intervention protocol. Thus, our findings support the overarching commonalities between the two protocols in key aspects including sample recruitment and bottom-up cognitive remediation approaches.
In sum, this study offers a new outlook for predicting cognitive remediation treatment response not only from postmorbid demographic and clinical factors or premorbid general cognition but from premorbid developmental trajectories. For individuals with stable-poor premorbid functioning trajectories, 6 months of bottom-up cognitive remediation appears to be sufficient to yield a full standard deviation gain in processing speed. Our findings thus inform efforts to strategically personalize cognitive remediation interventions based on premorbid developmental patterns of functioning and integrate developmental trajectories as potential moderators of treatment response in future intervention studies. More broadly, this work supports a link between premorbid development and postmorbid outcome following targeted behavioral intervention, emphasizing the utility of considering the lifespan developmental course in treating adult-onset psychiatric disorders such as schizophrenia.
Supplementary Material
Financial support.
This work was supported by the National Institutes of Health (K.H.N.: R01 MH-037705, R34 MH-102529, R01 MH-110544, and P50 MH-066286; J.K.F.: K08 MH-118577).
Footnotes
Supplementary material. The supplementary material for this article can be found at https://doi.org/10.1017/S0033291722003312
Conflict of interest. None.
Ethical standards. The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
References
- Allen DN, Strauss GP, Barchard KA, Vertinski M, Carpenter WT, & Buchanan RW (2013). Differences in developmental changes in academic and social premorbid adjustment between males and females with schizophrenia. Schizophrenia Research, 146(1–3), 132–137. doi: 10.1016/j.schres.2013.01.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bechi M, Agostoni G, Buonocore M, Bosinelli F, Spangaro M, Bianchi L, … Bosia M (2020). The influence of premorbid adjustment and autistic traits on social cognitive dysfunction in schizophrenia. Journal of the International Neuropsychological Society, 26(3), 276–285. doi: 10.1017/s1355617719000961 [DOI] [PubMed] [Google Scholar]
- Bell M, Bryson G, Greig T, Corcoran C, & Wexler BE (2001). Neurocognitive enhancement therapy with work therapy: Effects on neuropsychological test performance. Archives of General Psychiatry, 58(8), 763–768. doi: 10.1001/archpsyc.58.8.763 [DOI] [PubMed] [Google Scholar]
- Best MW, & Bowie CR (2017). A review of cognitive remediation approaches for schizophrenia: From top-down to bottom-up, brain training to psychotherapy. Expert Review of Neurotherapeutics, 17(7), 713–723. doi: 10.1080/14737175.2017.1331128 [DOI] [PubMed] [Google Scholar]
- Bowie CR, Bell MD, Fiszdon JM, Johannesen JK, Lindenmayer JP, McGurk SR, … Wykes T (2020). Cognitive remediation for schizophrenia: An expert working group white paper on core techniques. Schizophrenia Research, 215, 49–53. doi: 10.1016/j.schres.2019.10.047 [DOI] [PubMed] [Google Scholar]
- Bowie CR, Grossman M, Gupta M, Oyewumi LK, & Harvey PD (2014). Cognitive remediation in schizophrenia: Efficacy and effectiveness in patients with early versus long-term course of illness. Early Intervention in Psychiatry, 8(1), 32–38. doi: 10.1111/eip.12029 [DOI] [PubMed] [Google Scholar]
- Brill N, Reichenberg A, Weiser M, & Rabinowitz J (2008). Validity of the premorbid adjustment scale. Schizophrenia Bulletin, 34(5), 981–983. doi: 10.1093/schbul/sbm128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buonocore M, Bosinelli F, Bechi M, Spangaro M, Piantanida M, Cocchi F, … Bosia M (2019). The role of premorbid adjustment in schizophrenia Focus on cognitive remediation outcome. Neuropsychological Rehabilitation, 29(10), 1611–1624. doi: 10.1080/09602011.2018.1433048 [DOI] [PubMed] [Google Scholar]
- Cannon-Spoor HE, Potkin SG, & Wyatt RJ (1982). Measurement of premorbid adjustment in chronic schizophrenia. Schizophrenia Bulletin, 8 (3), 470–484. doi: 10.1093/schbul/8.3.470 [DOI] [PubMed] [Google Scholar]
- Catalan A, Salazar de Pablo G, Vaquerizo Serrano J, Mosillo P, Baldwin H, Fernández-Rivas A, … Fusar-Poli P (2021). Annual research review: Prevention of psychosis in adolescents - systematic review and meta-analysis of advances in detection, prognosis and intervention. Journal of Child Psychology and Psychiatry, 62(5), 657–673. doi: 10.1111/jcpp.13322 [DOI] [PubMed] [Google Scholar]
- Chan CC, Shanahan M, Ospina LH, Larsen EM, & Burdick KE (2019). Premorbid adjustment trajectories in schizophrenia and bipolar disorder: A transdiagnostic cluster analysis. Psychiatry Research, 272, 655–662. doi: 10.1016/j.psychres.2018.12.169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clissold M, & Crowe SF (2019). Comparing the effect of the subcategories of atypical antipsychotic medications on cognition in schizophrenia using a meta-analytic approach. Journal of Clinical and Experimental Neuropsychology, 41(1), 26–42. doi: 10.1080/13803395.2018.1488952 [DOI] [PubMed] [Google Scholar]
- Cole VT, Apud JA, Weinberger DR, & Dickinson D (2012). Using latent class growth analysis to form trajectories of premorbid adjustment in schizophrenia. Journal of Abnormal Psychology, 121(2), 388–395. doi: 10.1037/a0026922 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbera S, Wexler BE, Poltorak A, Thime WR, & Kurtz MM (2017). Cognitive remediation for adults with schizophrenia: Does age matter? Psychiatry Research, 247, 21–27. doi: 10.1016/j.psychres.2016.10.084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deste G, Barlati S, Galluzzo A, Corsini P, Valsecchi P, Turrina C, & Vita A (2019). Effectiveness of cognitive remediation in early versus chronic schizophrenia: A preliminary report. Frontiers in Psychiatry, 10, 236. doi: 10.3389/fpsyt.2019.00236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn OJ (1961). Multiple comparisons among means. Journal of the American Statistical Association, 56(293), 52–64. doi: 10.2307/2282330 [DOI] [Google Scholar]
- Eack SM, Hogarty GE, Cho RY, Prasad KM, Greenwald DP, Hogarty SS, & Keshavan MS (2010). Neuroprotective effects of cognitive enhancement therapy against gray matter loss in early schizophrenia: Results from a 2-year randomized controlled trial. Archives of General Psychiatry, 67(7), 674–682. doi: 10.1001/archgenpsychiatry.2010.63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fett AK, Viechtbauer W, Dominguez MD, Penn DL, van Os J, & Krabbendam L (2011). The relationship between neurocognition and social cognition with functional outcomes in schizophrenia: A meta-analysis. Neuroscience and Biobehavioral Reviews, 35(3), 573–588. doi: 10.1016/j.neubiorev.2010.07.001 [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JB (1995). Structured clinical interview for DSM-IV axis I disorders New York: New York: State Psychiatric Institute. [Google Scholar]
- Fisher M, Loewy R, Carter C, Lee A, Ragland JD, Niendam T, … Vinogradov S (2015). Neuroplasticity-based auditory training via laptop computer improves cognition in young individuals with recent onset schizophrenia. Schizophrenia Bulletin, 41(1), 250–258. doi: 10.1093/schbul/sbt232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman-Yakoobian MS, Parrish EM, Eack SM, & Keshavan MS (2020). Neurocognitive and social cognitive training for youth at clinical high risk (CHR) for psychosis: A randomized controlled feasibility trial. Schizophrenia Research, 243, 302–306. doi: 10.1016/j.schres.2020.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glenthøj LB, Hjorthøj C, Kristensen TD, Davidson CA, & Nordentoft M (2017). The effect of cognitive remediation in individuals at ultra-high risk for psychosis: A systematic review. npj Schizophrenia, 3(1), 20. doi: 10.1038/s41537-017-0021-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldstein MJ, Judd LL, Rodnick EH, & LaPolla A (1969). Psychophysiological and behavioral effects of phenothiazine administration in acute schizophrenics as a function of premorbid status. Journal of Psychiatric Research, 6(4), 271–287. doi: 10.1016/0022-3956(69)90021-1 [DOI] [PubMed] [Google Scholar]
- Green MF, Kern RS, & Heaton RK (2004). Longitudinal studies of cognition and functional outcome in schizophrenia: Implications for MATRICS. Schizophrenia Research, 72(1), 41–51. doi: 10.1016/j.schres.2004.09.009 [DOI] [PubMed] [Google Scholar]
- Hatzimanolis A, Stefanatou P, Kattoulas E, Ralli I, Dimitrakopoulos S, Foteli S, … Stefanis NC (2020). Familial and socioeconomic contributions to premorbid functioning in psychosis: Impact on age at onset and treatment response. European Psychiatry, 63(1), e44. doi: 10.1192/j.eurpsy.2020.41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hauser M, Zhang JP, Sheridan EM, Burdick KE, Mogil R, Kane JM, … Correll CU (2017). Neuropsychological test performance to enhance identification of subjects at clinical high risk for psychosis and to be most promising for predictive algorithms for conversion to psychosis: A meta-analysis. Journal of Clinical Psychiatry, 78(1), e28–e40. doi: 10.4088/JCP.15r10197 [DOI] [PubMed] [Google Scholar]
- Horton LE, Tarbox SI, Olino TM, & Haas GL (2015). Trajectories of premorbid childhood and adolescent functioning in schizophrenia-spectrum psychoses: A first-episode study. Psychiatry Research, 227(2–3), 339–346. doi: 10.1016/j.psychres.2015.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein DF, & Rosen B (1973). Premorbid asocial adjustment and response to phenothiazine treatment among schizophrenic inpatients. Archives of General Psychiatry, 29(4), 480–485. doi: 10.1001/archpsyc.1973.04200040034006 [DOI] [PubMed] [Google Scholar]
- Knowles EE, David AS, & Reichenberg A (2010). Processing speed deficits in schizophrenia: Reexamining the evidence. American Journal of Psychiatry, 167(7), 828–835. doi: 10.1176/appi.ajp.2010.09070937 [DOI] [PubMed] [Google Scholar]
- Kuo SS, Almasy L, Gur RC, Prasad K, Roalf DR, Gur RE, … Pogue-Geile MF (2018). Cognition and community functioning in schizophrenia: The nature of the relationship. Journal of Abnormal Psychology, 127(2), 216–227. doi: 10.1037/abn0000326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacBeth A, & Gumley A (2008). Premorbid adjustment, symptom development and quality of life in first episode psychosis: A systematic review and critical reappraisal. Acta Psychiatrica Scandinavica, 117(2), 85–99. doi: 10.1111/j.1600-0447.2007.01134.x [DOI] [PubMed] [Google Scholar]
- Mahncke HW, Connor BB, Appelman J, Ahsanuddin ON, Hardy JL, Wood RA, … Merzenich MM (2006). Memory enhancement in healthy older adults using a brain plasticity-based training program: A randomized, controlled study. Proceedings of the National Academy of Sciences of the USA, 103(33), 12523–12528. doi: 10.1073/pnas.0605194103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Medalia A, Herlands T, & Revheim N (2009). Cognitive remediation for psychological disorders: Therapist guide (1st ed.). New York, NY: Oxford University Press. [Google Scholar]
- Miyamoto S, Miyake N, Jarskog LF, Fleischhacker WW, & Lieberman JA (2012). Pharmacological treatment of schizophrenia: A critical review of the pharmacology and clinical effects of current and future therapeutic agents. Molecular Psychiatry, 17(12), 1206–1227. doi: 10.1038/mp.2012.47 [DOI] [PubMed] [Google Scholar]
- Morice R, Urbanc S, & McNicol D (1985). The Premorbid Adjustment Scale (PAS): Its use in an Australian study. Australian and New Zealand Journal of Psychiatry, 19(4), 390–395. doi: 10.3109/00048678509158847 [DOI] [PubMed] [Google Scholar]
- Mothersill D, & Donohoe G (2019). Neural effects of cognitive training in schizophrenia: A systematic review and activation likelihood estimation meta-analysis. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, 4(8), 688–696. doi: 10.1016/j.bpsc.2019.03.005 [DOI] [PubMed] [Google Scholar]
- Murray RM, & Lewis SW (1987). Is schizophrenia a neurodevelopmental disorder? British Medical Journal (Clinical Research Edition), 295(6600), 681–682. doi: 10.1136/bmj.295.6600.681 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2010). Mplus: Statistical analysis with latent variables: User’s guide Los Angeles: Muthén & Muthén. [Google Scholar]
- Nielsen RE, Levander S, Kjaersdam Telléus G, Jensen SO, Østergaard Christensen T, & Leucht S (2015). Second-generation antipsychotic effect on cognition in patients with schizophrenia – a meta-analysis of randomized clinical trials. Acta Psychiatrica Scandinavica, 131(3), 185–196. doi: 10.1111/acps.12374 [DOI] [PubMed] [Google Scholar]
- Nieman DH, Ruhrmann S, Dragt S, Soen F, van Tricht MJ, Koelman JH, … de Haan L (2014). Psychosis prediction: Stratification of risk estimation with information-processing and premorbid functioning variables. Schizophrenia Bulletin, 40(6), 1482–1490. doi: 10.1093/schbul/sbt145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuechterlein KH, Green MF, Kern RS, Baade LE, Barch DM, Cohen JD, … Marder SR (2008). The MATRICS Consensus Cognitive Battery, part 1: Test selection, reliability, and validity. American Journal of Psychiatry, 165(2), 203–213. doi: 10.1176/appi.ajp.2007.07010042 [DOI] [PubMed] [Google Scholar]
- Nuechterlein KH, McEwen SC, Ventura J, Subotnik KL, Turner LR, Boucher M, … Hayata JN (2021). Aerobic exercise enhances cognitive training effects in first episode schizophrenia: Randomized clinical trial demonstrates cognitive and functional gains [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nuechterlein KH, Ventura J, Subotnik KL, Gretchen-Doorly D, Turner LR, Casaus LR, … Medalia A (2020). A randomized controlled trial of cognitive remediation and long-acting injectable risperidone after a first episode of schizophrenia: Improving cognition and work/school functioning. Psychological Medicine, 52(8), 1517–1526. doi: 10.1017/S0033291720003335. [DOI] [PubMed] [Google Scholar]
- Oliver D, Reilly TJ, Baccaredda Boy O, Petros N, Davies C, Borgwardt S, … Fusar-Poli P (2020). What causes the onset of psychosis in individuals at clinical high risk? A meta-analysis of risk and protective factors. Schizophrenia Bulletin, 46(1), 110–120. doi: 10.1093/schbul/sbz039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rabinowitz J, Napryeyenko O, Burba B, Martinez G, Neznanov NG, Fischel T, … Schreiner A (2011). Premorbid functioning and treatment response in recent-onset schizophrenia: Prospective study with risperidone long-acting injectable. Journal of Clinical Psychopharmacology, 31(1), 75–81. doi: 10.1097/JCP.0b013e31820568c6 [DOI] [PubMed] [Google Scholar]
- Ramsay IS, & MacDonald III. A. W. (2015). Brain correlates of cognitive remediation in schizophrenia: Activation likelihood analysis shows preliminary evidence of neural target engagement. Schizophrenia Bulletin, 41(6), 1276–1284. doi: 10.1093/schbul/sbv025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Randers L, Jepsen JRM, Fagerlund B, Nordholm D, Krakauer K, Hjorthøj C, … Nordentoft M (2021). Generalized neurocognitive impairment in individuals at ultra-high risk for psychosis: The possible key role of slowed processing speed. Brain and Behavior, 11(3), e01962. doi: 10.1002/brb3.1962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seccomandi B, Agbedjro D, Bell M, Keefe RSE, Keshavan M, Galderisi S, … Cella M (2021). Can IQ moderate the response to cognitive remediation in people with schizophrenia? Journal of Psychiatric Research, 133, 38–45. doi: 10.1016/j.jpsychires.2020.12.013 [DOI] [PubMed] [Google Scholar]
- Strous RD, Alvir JM, Robinson D, Gal G, Sheitman B, Chakos M, & Lieberman JA (2004). Premorbid functioning in schizophrenia: Relation to baseline symptoms, treatment response, and medication side effects. Schizophrenia Bulletin, 30(2), 265–278. doi: 10.1093/oxfordjournals.schbul.a007077 [DOI] [PubMed] [Google Scholar]
- Tarbox SI, Addington J, Cadenhead KS, Cannon TD, Cornblatt BA, Perkins DO, … Woods SW (2013). Premorbid functional development and conversion to psychosis in clinical high-risk youths. Development and Psychopathology, 25(4 Pt 1), 1171–1186. doi: 10.1017/s0954579413000448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Velthorst E, Reichenberg A, Kapra O, Goldberg S, Fromer M, Fruchter E, … Weiser M (2016). Developmental trajectories of impaired community functioning in schizophrenia. JAMA Psychiatry, 73(1), 48–55. doi: 10.1001/jamapsychiatry.2015.2253 [DOI] [PubMed] [Google Scholar]
- Ventura J, Subotnik KL, Gitlin MJ, Gretchen-Doorly D, Ered A, Villa KF, … Nuechterlein KH (2015). Negative symptoms and functioning during the first year after a recent onset of schizophrenia and 8 years later. Schizophrenia Research, 161(2–3), 407–413. doi: 10.1016/j.schres.2014.10.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ventura J, Subotnik KL, Gretchen-Doorly D, Casaus L, Boucher M, Medalia A, … Nuechterlein KH (2019). Cognitive remediation can improve negative symptoms and social functioning in first-episode schizophrenia: A randomized controlled trial. Schizophrenia Research, 203, 24–31. doi: 10.1016/j.schres.2017.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vinogradov S, Fisher M, & de Villers-Sidani E (2012). Cognitive training for impaired neural systems in neuropsychiatric illness. Neuropsychopharmacology, 37(1), 43–76. doi: 10.1038/npp.2011.251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vita A, Barlati S, Ceraso A, Nibbio G, Ariu C, Deste G, … Wykes T (2021). Effectiveness, core elements, and moderators of response of cognitive remediation for schizophrenia: A systematic review and meta-analysis of randomized clinical trials. JAMA Psychiatry, 78(8), 848–858. doi: 10.1001/jamapsychiatry.2021.0620. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D (2001). Wechsler Test of Adult Reading: WTAR: Psychological corporation [Google Scholar]
- Weinberger DR (1987). Implications of normal brain development for the pathogenesis of schizophrenia. Archives of General Psychiatry, 44(7), 660–669. doi: 10.1001/archpsyc.1987.01800190080012 [DOI] [PubMed] [Google Scholar]
- Wykes T, Huddy V, Cellard C, McGurk SR, & Czobor P (2011). A meta-analysis of cognitive remediation for schizophrenia: Methodology and effect sizes. American Journal of Psychiatry, 168(5), 472–485. doi: 10.1176/appi.ajp.2010.10060855 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


