Summary
Background
Stroke has been the leading cause of death in China for decades. The extremely low intravenous thrombolysis rate is largely due to the prehospital delays that make patients ineligible for the time-sensitive therapy. Limited studies evaluated prehospital delays across China. We investigated prehospital delays in the stroke population across China and the associated age, rurality, and geographic disparities.
Methods
A cross-sectional study design was employed using the Bigdata Observatory platform for Stroke of China in 2020, the nationwide, prospective, multicentre registry of patients with acute ischaemic stroke (AIS). Mixed-effect regression models were used to account for the clustered data.
Findings
The sample contained 78,389 AIS patients. The median onset-to-door (OTD) time was 24 h, with only 11.79% (95% confidence interval [CI]: 11.56–12.02%) patients arriving at hospitals within 3 h. About 12.43% (95% CI: 12.11–12.74%) of patients 65 years or older arrived at hospitals within 3 h, which was significantly higher than the young and middle-aged patients (11.03%; 95% CI: 10.71–11.36%). After controlling for potential confounders, young and middle-aged patients were less likely to present to hospitals within 3 h (adjusted odds ratio: 0.95; 95% CI: 0.90–0.99) compared to patients 65 years or older. The 3-h hospital arrival rate was the highest in Beijing (18.40%, 95% CI: 16.01–20.79%), which was almost 5 times higher than that in Gansu (3.45%, 95% CI: 2.69–4.20%). The arrival rate in urban areas was almost 2 times higher than that in rural areas (13.35% versus. 7.66%).
Interpretation
We found that the low rates of timely arrival at hospitals after a stroke is more salient in the younger population, rural settings, or those residing in less developed geographic regions. This study calls for more tailored interventions focusing on younger people, rural areas, and less developed geographic regions.
Funding
The National Natural Science Foundation of China; CIHR, Grant/Award Number: 81973157, PI: JZ. Natural Science Foundation of Shanghai; CIHR, Grant/Award Number: 17dz2308400, PI: JZ. Funding from the University of Pennsylvania; Grant/Award Number: CREF-030, PI: RL.
Keywords: Prehospital delay, Onset-to-door, Acute ischaemic stroke, Rural, Geographic, Age, Bigdata observatory platform for stroke of China
Research in context.
Evidence before this study
Using MeSH terms, we performed a scoping review by searching the literature as of Dec 1, 2022 in Medline, for studies published in English related to the hospital arrival time and prehospital delay rate for acute ischemic stroke. The search terms included “onset to door time” or “onset to hospital time” “hospital arrival time” “time to arrival” or “time to hospital” “time to presenting to hospital” and “ischemic stroke”, “ischemic stroke”, “China”, “Chinese”. A total of 129 articles were found, and after the screening, we identified 8 studies that reported the hospital arrival time and prehospital delay rate in the Chinese stroke population. Six studies also assessed the factors associated with prehospital delay. However, most of these studies were at a hospital or city level, and there is little evidence on a national level. No previous study included patients from every province across mainland China or investigated variations in prehospital delay according to both geographical factors and individual age.
Added value of this study
Our study provides the most recent nationwide data on prehospital delay across China and identified significant age, rural-urban, and geographical disparities in prehospital delay among AIS patients. We reported that the proportion of patients with hospital arrival within 3 h of onset continued to be low across China. People at a younger age were more likely to be delayed in arriving at hospitals than their old counterparts after a stroke, the timely hospital presentation rate in developed geographic regions was 5 times higher than that in less developed geographic regions, and the arrival rate in urban areas was almost 2 times higher than that in rural areas.
Implications of all the available evidence
Our study warrants tailored interventions, such as Stroke 1-2-0 interventional campaigns, to shorten prehospital delays for patients with stroke in China; our study also calls for a shift of interventional campaigns to younger people, rural areas, and less developed geographic regions.
Introduction
Stroke is the leading cause of death in China.1 Rapid restoration of blood supply to brain tissue is critical to preserving or regaining neurological function following an acute ischaemic stroke (AIS). Patients with AIS are generally eligible for intravenous alteplase (IVT) within a 4.5-h time window or endovascular thrombectomy (EVT) within a 6-h time window from stroke symptom onset.1 According to the U.S. Centers for Disease Control and Prevention, patients should arrive at hospitals within 3 h of symptom onset to receive timely treatments that are effective in improving functional outcomes and reducing mortality.2 Approximately 1%–10% of AIS patients receive IVT in China, which is much lower than those reported in high-income countries (HICs).1 The main reason for such low rates of IVT is that patients typically arrive at the hospitals too late to be eligible for time-sensitive therapies. As a result, the prehospital delays have posed enormous clinical and economic burdens to patients, families, and society.
Although older people are more likely to have a stroke, a stroke could occur at any age. Stroke in young adults has been emerging as a global health crisis.3 In the past decade, the prevalence of stroke in young people has been continuously increasing. Unfortunately, a very limited number of studies have examined hospital arrival times by different age groups. As a result, it remains unclear if the times from symptom onset to hospital arrivals differ between younger and older adults.
Medline search with appropriate MeSH terms was performed to identify the current gaps in the literature. Data on prehospital delays have been reported in a small number of regional studies in China,4, 5, 6, 7, 8, 9 but little is known at a national level. Many studies were from a single hospital in China. Using data from two different hospitals, Fang et al. and Yuan et al., in 2011 and 2022 reported the prehospital delay in Shanghai, China.5,6 Based on a hospital in Suzhou, a city geographically close to Shanghai, Zhu et al. reported the prehospital delay rate.7 There are also three studies that reported the prehospital delay in multiple cities, but were limited to small sample sizes.4,8,9 However, little is known at a national level. In addition, some of the studies also assessed the factors associated with prehospital delay, which mainly focused on individual and treatment characteristics.4, 5, 6 However, information on rural-urban and geographical variations is urgently needed for tailored interventions due to the diversified culture and economic imbalance in China. Using the national, multicentre data from the Bigdata Observatory Platform for Stroke of China (BOSC), this study is the first to report disparities in pre-hospital delays by age, rurality, and province among the stroke population across China.
Methods
Ethics approval
This study was approved by the ethics committees of the Institutional Review Boards of Minhang Hospital at Fudan University (Number: 2020-039-01K). The approval date is July 29, 2020.
Study design
This study employs a cross-sectional design using the Bigdata Observatory Platform for Stroke of China (BOSC) in 2020. This study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guideline (eTable S1 in the Supplement).10
Data source
The Bigdata Observatory Platform for Stroke of China (BOSC) was established and has been administered by the Ministry of Health China Stroke Prevention Project Committee (CSPPC) since 2011, aiming to monitor and improve the quality of stroke care in mainland China.11 With the Chinese government's financial support of 838.4 million CNY, BOSC collects data on incident stroke patients in 31 provinces across mainland China. All stroke centres in the CSPPC are required to collect data on established quality-of-care indicators (e.g., time from hospital arrival to initial treatment) with the concurrence of care. Upon admission to the hospital (or during the first 24 h), trained medical staff conduct face-to-face interviews with the patients or their proxies to collect data on socio-demographics, medical history, lifestyle factors, time from stroke onset to hospital admission, and mode of transportation to the hospital. The National Institutes of Health Stroke Scale (NIHSS) was also administered to evaluate the severity of stroke upon admission.12 To ensure high quality of data, medical staff received training on data entry into the interactive, web-based database of BOSC. A structured validation was performed periodically to check the completeness and plausibility of the data. Additional details of the data sources are described elsewhere.13
Study sample
We identified adults aged 18 years or older with a primary diagnosis of ischaemic stroke in the BOSC between Jan 1, 2020, and Dec 31, 2020. A total of 232 hospitals across 31 provinces in mainland China were included. We included patients with an AIS diagnosis and were admitted to hospitals within 7 days of symptom onset, based on the clinical practices and existing literatures.9 Patients were excluded if they1: had missing data on age, sex, or date/time of symptom onset2; had onset of ischaemic stroke within the hospital, or3 transferred from other hospitals. Because the sample size in Xizang was too small (N = 7), these cases were not included in the analysis for confidentiality reasons.13 In the sensitivity analysis, we further limited the study subjects to those who arrived at the hospital within 2 days of symptom onset.5
Outcome measures
The primary outcomes were onset-to-door (OTD) time and 3-h hospital arrival rate. The onset-to-door (OTD) time was calculated as the time duration from the time of stroke symptom onset to the time of hospital arrival as recorded in the BOSC. The time of stroke symptom onset was defined as the time when symptoms first occurred, and were collected from patients or their proxies who reported stroke-related symptoms.13 If the stroke onset occurred during the night or sleep, the time of awakening was used as the time of stroke onset.14,15 The time of hospital arrival was defined as the time when the patients presented to the participating hospital. The 3-h hospital arrival rate was defined as the number of patients with an OTD time <3.0 h divided by the total number of AIS cases.5 The 3-h cutoff threshold is clinically relevant to acute stroke treatment and commonly used in the current literature. More recent published studies shown that EVT was also effective for certain AIS patients arriving 6–24 h16 or even over 24 h after stroke onset, therefore, patients were also categorized into 6 clinically relevant groups according to OTD time as follows: <3.0 h, 3.0–5.9 h, 6.0–11.9 h, 12.0–23.9 h, 24.0–47.9 h, and 2–7days.5,9,17,18
Covariates
Demographic characteristics included age and sex. Age was categorized into young/middle-aged people (18–64 years) and old people (65+ years). Patient or proxy-reported characteristics included prior medical history (e.g., stroke, hypertension) and lifestyle factors (e.g., cigarette smoking, alcohol drinking). We also extracted data on the characteristics of stroke onset (e.g., onset time) and use of emergency medical services (e.g., ambulance, emergency department [ED]). Stroke severity at hospital admission was categorized into 3 groups according to the NIHSS score: minor1, 2, 3, 4; moderate,5, 6, 7, 8, 9, 10, 11, 12, 13, 14 and severe stroke (15+). According to the ‘Provisions on the Statistical Division of Urban and Rural Areas’ released by the National Bureau of Statistics, rural areas were defined as if the residence was in the township or village level.
Statistical analysis
For descriptive statistics, frequencies with percentages were reported for categorical variables; means with standard deviations (SD) were reported for continuous variables. Due to the large sample size, some statistically significant differences may not be clinically meaningful. Hence, the absolute standardized difference, which is independent on sample size, was used to compare the differences in baseline characteristics between AIS patients aged <65 and over 65 years old. Absolute standardized difference >10 was considered significant differences between two groups.19 Because the distribution of OTD time was not normally distributed based on the normality test, the medians and interquartile range [IQR] were reported. The 3-h hospital arrival rate was estimated for each province and by different residence settings and the choropleth map was used to characterize rural-urban and geographic variations across China.
Given that patients might be clustered within hospitals, we used multivariable mixed-effect regression models with generalized estimating equations to account for clustering by hospitals.20 To assess individual characteristics associated with prehospital delay, a mixed-effects linear regression analysis was performed with OTD time as a dependent variable among patients with NIHSS score.20 We also carried out a logistic regression analysis with 3-h hospital arrival (whether or not <3.0 h) as a dependent variable and estimated adjusted odds ratios (AORs) with a 95% confidence interval (CIs). The selection of covariates was based on the clinical importance according to the consultation with clinical experts and existing guidelines.
To systematically examine how prehospital delay varied by subpopulation, we did a comprehensive analysis of population subgroups with defined a priori by age (18–44, 45–64, 65–74, 75–84, and 85+years) and other factors (sex, geographical region, residence setting, stroke severity, onset time, mode of transportation, and patient source). To evaluate the association between age and the likelihood of 3-h hospital arrival, we repeated the mixed-effect regression analysis in the subgroup with >1000 patients.
All analyses were conducted using SAS Version 9.4 (SAS Institute, Inc). Two-sided P < 0.05 was considered statistically significant.
Sensitivity analysis
We conducted the following sensitivity analyses1: Given the retrospective nature of the study, we limited the study sample to AIS patients who arrived at the hospital within 7 days.21 Because some studies also used a 2-day timeframe,5 we also repeated the analyses for patients who presented to the hospital within 2 days of symptom onset for comparisons and contrasts.2 Since our analysis has a large sample size, we also used multivariate linear regression models to measure effect sizes, which can measure the extent of the association between variables.3 In the regression analysis, age was treated as a continuous variable.
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
A total of 209,493 patients were identified from the BOSC. The study excluded 91,570 patients who had missing data on date/time of stroke onset or hospital arrival, 29,330 patients who had stroke onset in other calendar years, 435 patients who had no primary diagnosis of IS, 910 patients who were transferred from other hospitals, 1158 patients who had missing data on age, and 7701 who were admitted to hospital after 7 days of onset. Therefore, total of 78,389 AIS patients were included in the analysis after applying the predefined inclusion/exclusion criteria (eFig. S1 in the Supplement).
The mean (±SD) age was 65.63 (±11.92) years (Table 1). 35,773 (45.64%) were aged 18–64 years old. The majority of the study sample were men (49,999 [63.78%]) and were from Eastern China (22,640 [28.88%]). As for stroke severity by NIHSS, 38,383 (48.96%) patients had a minor stroke, 17,164 (21.90%) had a moderate stroke, and 3510 (4.48%) had a severe stroke. More than half of the patients had hypertension (46,839 [59.75%]). 11,828 (14.04%) arrived at the hospital via ambulances. Young/middle-aged patients of 18–64 years had a higher proportion of men (25,640 [71.67%]) and living in Northeast China (6583 [18.40%]). People aged 65 years and older were more likely to use an ambulance or visit an ED than other age groups.
Table 1.
Demographic and clinical characteristics of the patients with AIS in BOSC, 2020.
| Characteristics | All (n = 78.389) | Age groups |
||
|---|---|---|---|---|
| 18–64 years (n = 35.773) |
65+ years (n = 42.616) |
Absolute standardized differencea | ||
| Age, mean ± SD | 65.63 ± 11.92 | 55.15 ± 7.53 | 74.42 ± 6.65 | −271.25 |
| Sex | ||||
| Male | 49,999 (63.78%) | 25,640 (71.67%) | 24,359 (57.16%) | −30.67 |
| Female | 28,390 (36.22%) | 10,133 (28.33%) | 18,257 (42.84%) | 30.67 |
| Regionsb | ||||
| Northern China | 11,876 (15.15%) | 6106 (17.07%) | 5770 (13.54%) | 9.81 |
| Northeast China | 12,426 (15.85%) | 6583 (18.40%) | 5843 (13.71%) | 12.81 |
| Eastern China | 22,640 (28.88%) | 9513 (26.59%) | 13,127 (30.8%) | −9.32 |
| Central China | 13,780 (17.58%) | 6371 (17.81%) | 7409 (17.39%) | 1.11 |
| Southern China | 5788 (7.38%) | 2602 (7.27%) | 3186 (7.48%) | −0.78 |
| Southwest China | 5513 (7.03%) | 1977 (5.53%) | 3536 (8.30%) | −10.94 |
| Northwest China | 6366 (8.12%) | 2621 (7.33%) | 3745 (8.79%) | −5.37 |
| Setting | ||||
| Rural | 21,507 (27.44%) | 10,767 (30.10%) | 10,740 (25.20%) | 10.96 |
| Urban | 56,882 (72.56%) | 25,006 (69.90%) | 31,876 (74.80%) | −10.96 |
| Stroke severity by NIHSS | ||||
| Minor stroke (<5) | 38,383 (48.96%) | 18,055 (50.47%) | 20,328 (47.70%) | 5.54 |
| Moderate stroke (5–14) | 17,164 (21.9%) | 7394 (20.67%) | 9770 (22.93%) | −5.47 |
| Severe stroke (15+) | 3510 (4.48%) | 1066 (2.98%) | 2444 (5.73%) | −13.53 |
| Unknown | 19,332 (24.66%) | 9258 (25.88%) | 10,074 (23.64%) | −13.53 |
| Cigarette smoking | ||||
| Non-smoker | 52,005 (66.34%) | 20,679 (57.81%) | 31,326 (73.51%) | −33.53 |
| Current smoker | 21,093 (26.91%) | 13,189 (36.87%) | 7904 (18.55%) | 41.82 |
| Past smoker | 5291 (6.75%) | 1905 (5.33%) | 3386 (7.95%) | −10.54 |
| Alcohol drinking | ||||
| Non-drinker | 58,720 (74.91%) | 24,113 (67.41%) | 34,607 (81.21%) | −31.99 |
| Light drinker | 12,640 (16.12%) | 7240 (20.24%) | 5400 (12.67%) | 20.52 |
| Heavy drinker | 7029 (8.97%) | 4420 (12.36%) | 2609 (6.12%) | 21.65 |
| Medical history | ||||
| Stroke | 16,757 (21.38%) | 6306 (17.63%) | 10,451 (24.52%) | −16.97 |
| Transient ischemic attack | 163 (0.21%) | 81 (0.23%) | 82 (0.19%) | 0.96 |
| Cerebral haemorrhage | 1521 (1.94%) | 694 (1.94%) | 827 (1.94%) | −0.004 |
| Hypertension | 46,839 (59.75%) | 20,007 (55.93%) | 26,832 (62.96%) | −14.36 |
| Diabetes | 18,132 (23.13%) | 8039 (22.47%) | 10,093 (23.68%) | −0.01 |
| Hyperlipidemia | 12,824 (16.36%) | 5928 (13.91%) | 6896 (19.28%) | −10.76 |
| Atrial fibrillation | 3049 (3.89%) | 536 (1.50%) | 2513 (5.90%) | −23.47 |
| Myocardial infarction | 612 (0.78%) | 203 (0.57%) | 409 (0.96%) | −4.51 |
| Peripheral vascular disease | 450 (0.57%) | 116 (0.32%) | 334 (0.78%) | −6.19 |
| Onset during night | 19,750 (25.19%) | 9082 (25.39%) | 10,668 (25.03%) | −0.82 |
| Weekend onset | 21,856 (27.88%) | 9945 (27.80%) | 11,911 (27.95%) | −0.33 |
| Admitted through ED | 45,039 (57.46%) | 20,510 (57.33%) | 24,529 (57.56%) | −0.45 |
| Arrival via ambulance | 11,524 (14.70%) | 4911 (13.73%) | 6613 (15.52%) | −5.07 |
SD, standard deviation; NIHSS, National Institutes of Health Stroke Scale; ED: emergency department. Night time was defined as 6 PM to 6 AM.
The absolute standardized difference >10 indicates a significant difference between the two groups.
Northern China includes Beijing, Tianjin, Hebei, Shanxi, and Inner Mongolia; Northeast China includes Liaoning, Jilin, and Heilongjiang; Eastern China includes Shanghai, Jiangsu, Zhejiang, Anhui, Fujian, Jiangxi, and Shandong; Central China includes Henan, Hubei, and Hunan; Southern China includes Guangdong, Guangxi, and Hainan; Southwest China includes Chongqing, Sichuan, Guizhou, Yunnan, and Xizang; Northwest China includes Shaanxi, Gansu, Qinghai, Ningxia and Xinjiang.
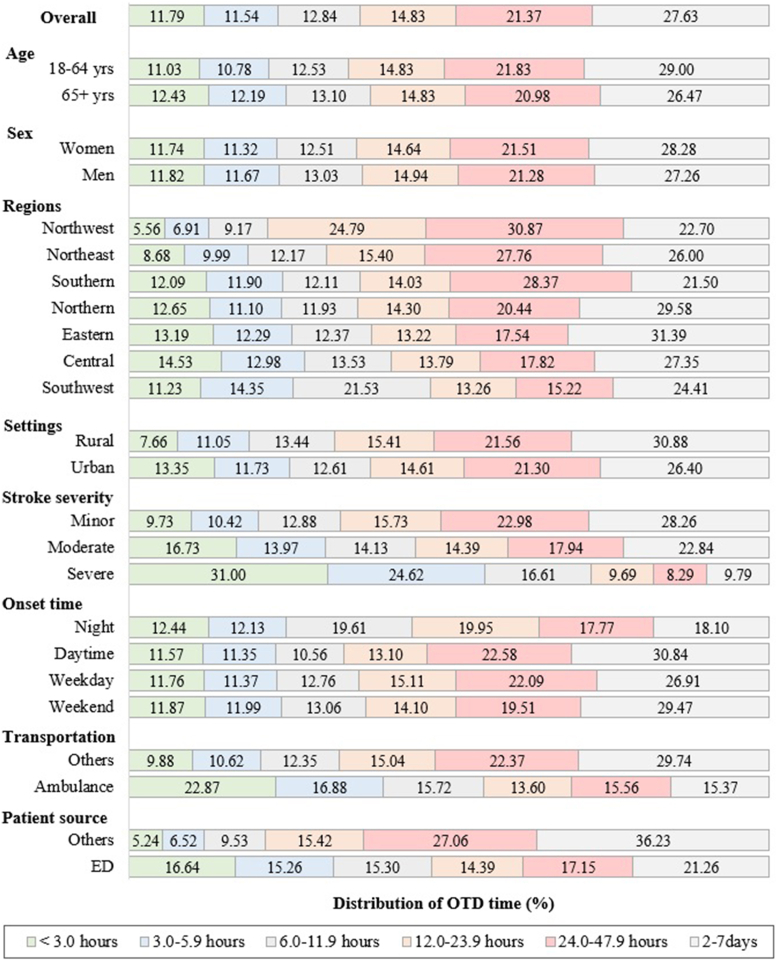
Among all the AIS patients, the median OTD time was 23.83 h (IQR: 6.38–48.70 h). 9242 (Fig. 1; 11.79%; 95% CI: 11.56–12.02%) patients with AIS presented to hospitals within 3 h, 9049 (11.54%; 95% CI: 11.32–11.77%) presented at 3.0–5.9 h; 10,066 (12.84%; 95% CI: 12.61–13.08%) presented at 6.0–11.9 h, 11,624 (14.83%; 95% CI: 14.58–15.08%) presented at 12.0–23.9 h, 16,750 (21.37%; 95% CI: 21.08–21.65%) presented at 24.0–47.9 h; and 21,658 (27.63%; 95% CI: 27.32%–27.94%) presented in 2–7days. There was no difference in the 3-h hospital arrival rate between women and men (11.74% versus 11.82%), and the OTD distribution between the groups was similar. Compared with daytime onset, stroke onset between 6 PM and 6 AM had a higher 3-h hospital arrival rate (12.44% versus 11.57%). Using an ambulance had a higher 3-h hospital arrival rate than no ambulance used (22.87% versus 9.88%).
Fig. 1.
Distribution of OTD time (%) in AIS patients stratified by patient characteristics. The proportion of patients with OTD time <3.0 h, 3.0–5.9 h, 6.0–11.9 h, 12.0–23.9 h, 24.0–47.9 h, and 2–7 days, by patient characteristics.
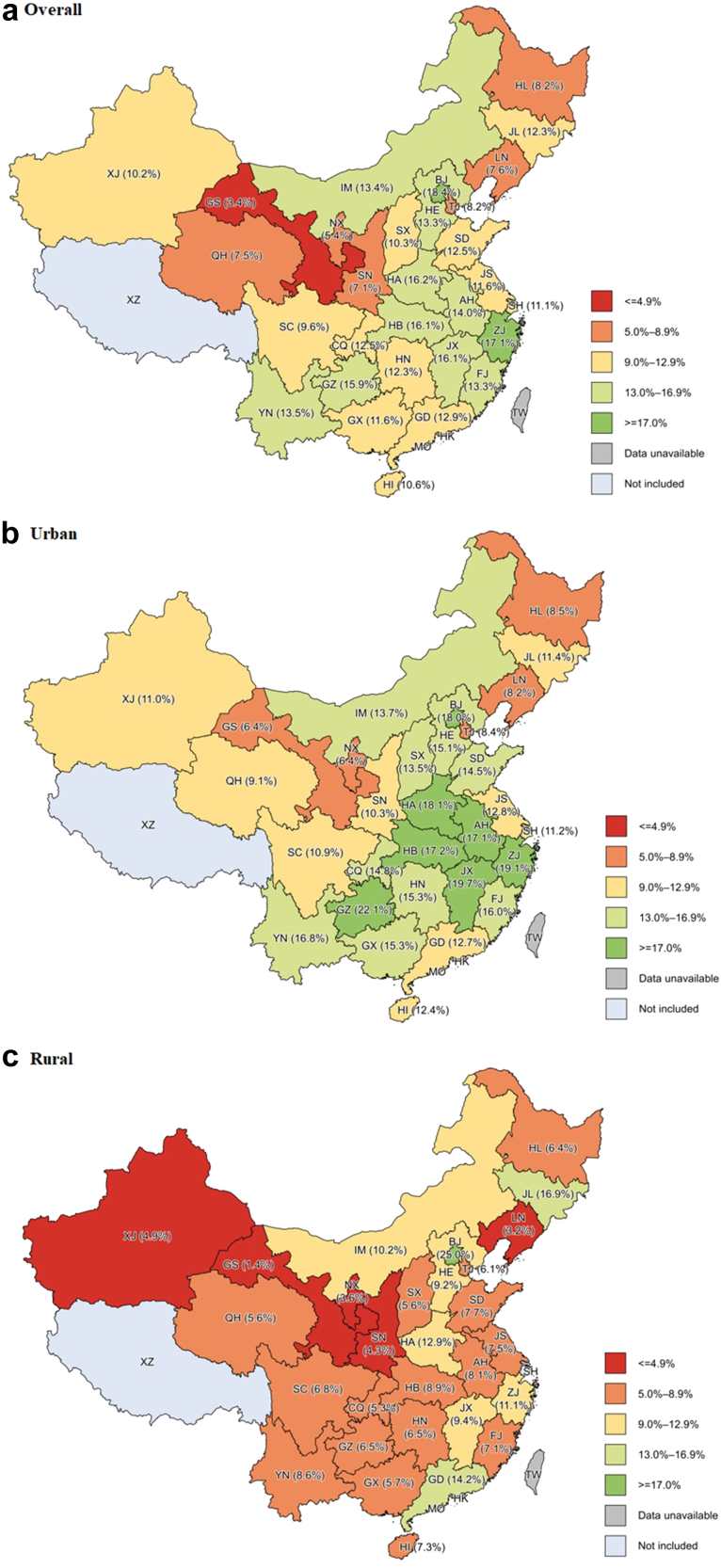
Geographically, the Northwest region (e.g., Gansu) of China had the lowest 3-h hospital arrival rates (Fig. 1; 5.56%; 95% CI: 5.00–6.12%). Central regions had the highest 3-h hospital arrival rate (14.53%; 95% CI: 13.94–15.12%), which was nearly 3 times that in the Northwest. There were substantial variations in hospital arrival time across provinces. Visually, there were more provinces with 3-h hospital arrival rates of <10% in the Northwest and Northeast of China (Fig. 2). The 3-h hospital arrival rate was highest in Beijing (18.40%; 95% CI: 16.01–20.79%), the capital city of China, which was almost 5 times higher than that in Gansu (3.44%; 95% CI: 2.69–4.20%), the province with the lowest per capita disposable income. Generally, AIS patients living in urban areas had a two times higher 3-h hospital arrival rate than those living in rural areas (13.35%; 95% CI: 13.07–13.63% versus 7.66%; 95% CI: 7.30–8.01%).
Fig. 2.
Maps showing regional differences in the 3-h hospital arrival rates of AIS patients by provinces. The proportion of patients with OTD time <3.0 h in (a) overall, (b) urban, and (c) rural settings. BJ: Beijing; TJ: Tianjin; HE: Hebei; SX: Shanxi; IM: Inner Mongolia; LN: Liaoning; JL: Jilin; HL: Heilongjiang; SH: Shanghai; JS: Jiangsu; ZJ: Zhejiang; AH: Anhui; FJ: Fujian; JX: Jiangxi; SD: Shandong; HA: Henan; HB: Hubei; HN: Hunan; GD: Guangdong; GX: Guangxi; HI: Hainan; CQ: Chongqing; SC: Sichuan; GZ: Guizhou; YN: Yunnan; XZ: Xizang; SN: Shaanxi; GS: Gansu; QH: Qinghai; NX: Ningxia; XJ: Xinjiang; HK: Hongkong; TW: Taiwan; MO: Macao.
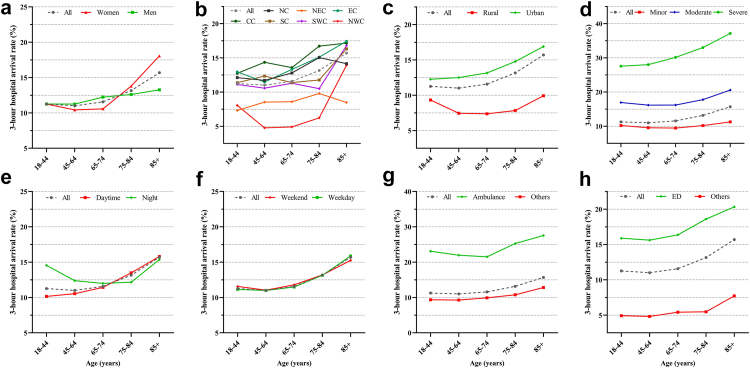
Our study found that the young and middle-aged group (18–64 years old) had longer OTD time and lower hospital arrival rate than those aged 65 or older. About 12.43% (Fig. 1; 95% CI: 12.11–12.74%) of patients 65 years or older presented to hospitals within 3 h, which was nearly 15% higher than the young and middle-aged patients (11.03%; 95% CI: 10.71–11.36%). Across all subgroups, patients at younger ages generally had a lower 3-h hospital arrival rate than their older counterparts (Fig. 3).
Fig. 3.
Three-hour hospital arrival rates by age and by other individual characteristics among patients with AIS. NC: Northern China; NEC: Northeast China; EC: Eastern China; CC: Central China; SC: Southern China; SWC: Southwest China; NWC: Northwest China. Three-hour hospital arrival rate by age groups and by (a) sex, (b) regions, (c) settings (rural versus. urban), (d) stroke severity (minor, moderate, and severe), (e) time of stroke onset (daytime versus. nighttime), (f) day of stroke onset, (g) mode of transportation (ambulance versus. others), (h) patient source (emergency department versus. others).
After adjusting for potential confounding factors, young/middle-aged patients were associated with longer OTD time (Table 2; Coefficient ± SD: 1.27 ± 0.30 h) and were less likely to present at a hospital within 3 h (AOR: 0.95; 95% CI: 0.90–0.99), compared to patients 65 years or older. Women had longer OTD time than men (Coefficient ± SD: 1.57 ± 0.35) but had a similar likelihood of 3-h hospital arrival (AOR: 0.97; 95% CI: 0.92–1.04). Patients living in rural areas had a lower likelihood of arriving at hospitals within 3 h than those living in urban areas (AOR: 0.48; 95% CI: 0.45–0.51). In the subgroup analyses, young/middle-aged patients living in urban areas had a lower likelihood to present to hospital within 3 h, but those living in rural areas had a similar likelihood to their older counterparts (eTable S2). Young/middle-aged patients generally had non-statistically significant odds of arriving at hospital within 3 h, the only exceptions were patients with severe stroke, those with stroke onset during the night, and those not transported by ambulance (eFig. S2).
Table 2.
Individual characteristics associated with OTD time and 3-h hospital arrival for patients with AIS in BOSC, 2020.
| Characteristics | OTD Time (hours)a |
3-h hospital arrivala |
||
|---|---|---|---|---|
| Coefficient | SD | AOR | 95% CI | |
| Age | ||||
| 18–64 years | 1.27 | 0.30 | 0.95 | 0.90–0.99 |
| 65+ years | reference | – | reference | – |
| Sex | ||||
| Male | reference | – | reference | – |
| Female | 1.57 | 0.35 | 0.97 | 0.92–1.04 |
| Provinces | ||||
| Beijing | reference | – | reference | – |
| Anhui | −10.47 | 5.70 | 1.35 | 1.09–1.67 |
| Chongqing | −1.13 | 7.70 | 0.83 | 0.60–1.14 |
| Fujian | −8.08 | 6.17 | 0.78 | 0.61–0.99 |
| Gansu | −22.74 | 7.93 | 0.28 | 0.20–0.38 |
| Guangdong | −15.10 | 5.80 | 1.05 | 0.84–1.31 |
| Guangxi | −14.02 | 6.14 | 0.84 | 0.66–1.08 |
| Guizhou | −4.08 | 7.66 | 1.33 | 0.98–1.82 |
| Hainan | −15.63 | 8.79 | 1.17 | 0.84–1.62 |
| Hebei | −12.32 | 5.75 | 1.09 | 0.89–1.35 |
| Heilongjiang | −9.80 | 6.46 | 0.52 | 0.42–0.65 |
| Henan | −15.30 | 5.31 | 1.57 | 1.28–1.92 |
| Hubei | −13.59 | 6.83 | 1.69 | 1.33–2.15 |
| Hunan | −7.14 | 5.49 | 1.06 | 0.86–1.31 |
| Inner Mongolia | −12.02 | 6.08 | 1.26 | 1.00–1.58 |
| Jiangsu | −7.49 | 5.68 | 0.84 | 0.68–1.03 |
| Jiangxi | −12.23 | 6.49 | 1.62 | 1.28–2.06 |
| Jilin | −4.52 | 6.94 | 0.97 | 0.76–1.22 |
| Liaoning | −10.75 | 5.79 | 0.67 | 0.54–0.84 |
| Ningxia | −7.17 | 8.84 | 0.73 | 0.47–1.12 |
| Qinghai | −7.64 | 8.79 | 0.60 | 0.38–0.96 |
| Shaanxi | −10.24 | 6.58 | 0.88 | 0.67–1.17 |
| Shandong | −8.17 | 5.58 | 1.14 | 0.92–1.40 |
| Shanghai | 0.08 | 10.96 | 0.670 | 0.51–0.95 |
| Shanxi | −13.01 | 6.64 | 0.90 | 0.70–1.17 |
| Sichuan | −9.84 | 5.89 | 0.64 | 0.51–0.80 |
| Tianjin | 2.45 | 6.95 | 0.44 | 0.34–0.58 |
| Xinjiang | −15.83 | 11.44 | 0.62 | 0.40–0.95 |
| Yunnan | −9.69 | 7.05 | 0.98 | 0.72–1.32 |
| Zhejiang | −6.61 | 6.28 | 1.15 | 0.92–1.45 |
| Setting | ||||
| Urban | reference | – | reference | – |
| Rural | 4.94 | 0.35 | 0.48 | 0.45–0.51 |
| Cigarette smoking | ||||
| Non-smoker | reference | – | reference | – |
| Current smoker | −0.35 | 0.42 | 1.01 | 0.94–1.08 |
| Past smoker | 1.28 | 0.62 | 0.93 | 0.84–1.04 |
| Alcohol drinking | ||||
| Non-drinker | reference | – | reference | – |
| Light drinker | −1.49 | 0.47 | 0.97 | 0.88–1.07 |
| Heavy drinker | 0.66 | 0.57 | 1.05 | 0.97–1.14 |
| Stroke severity | ||||
| Minor stroke (LT5) | reference | – | reference | – |
| Moderate stroke5, 6, 7, 8, 9, 10, 11, 12, 13, 14 | −4.94 | 0.33 | 1.66 | 1.57–1.76 |
| Severe stroke (GT15) | −15.24 | 0.65 | 2.94 | 2.70–3.20 |
| Prior stroke | 1.40 | 0.37 | 0.85 | 0.80–0.91 |
| Onset during night | −7.81 | 0.34 | 0.96 | 0.90–1.01 |
| Weekend onset | 0.84 | 0.32 | 1.00 | 0.94–1.05 |
| Admitted through ED | −17.68 | 0.38 | 2.98 | 2.78–3.19 |
| Arrival via ambulance | −3.11 | 0.46 | 1.62 | 1.52–1.72 |
SD, standard deviation; NIHSS, National Institutes of Health Stroke Scale; ED: emergency department.
For the relationship between OTD time and age categories, mixed-effects linear regression models were used with the adjustment of confounding factors. For the relationship between the 3-h hospital arrival rate and age categories, mixed-effects logistic regression models were used with the adjustment of confounding factors. Covariates included sex, regions, cigarette smoking, alcohol drinking, medical history, stroke severity, onset time, transportation and patient source.
In the sensitivity analyses, when the sample selection criteria were defined using the 2-day timeframe, the median OTD time was 12.30 h (IQR: 4.42–24.00). The proportion of AIS patient arriving hospital within 3 h was 15.91% (95% CI: 15.61–16.21%). Young/middle-aged patients were again associated with longer OTD time (13.33 h versus. 11.98 h) and lower 3-h hospital arrival rate (15.16% versus. 16.52%), compared with people over the age of 65 (eTable S3 in the Supplement). The covariates with relatively large effect sizes included age, provinces, settings, onset during night, stroke severity, admitted through ED, and arrival via ambulance, which were consistent with logistic regressions and can be meaningful for clinical practice (eTable S4 in the Supplement). When age was treated as a continuous variable, each additional year of age was associated with a 0.06 ± 0.01 h decrease in OTD hours holding other covariates constant (eTable S5 in the Supplement).
Discussion
Access to timely stroke care has been shown to reduce morbidity and mortality.22 The mortality rate of stroke in mainland China is still four times higher than that of Europe and the United States, and a growing number of studies showed that the main reason for this high mortality rate in China may be due to the extremely long prehospital delays. It is reported that in HICs, the 3-h arrival rate are ranged from 40 to 60%.17,18,23 Our study reported a much lower proportion of timely arrival at hospitals, which should be a much more accurate estimate of current prehospital delays in China because our findings are based on the national registry data, as compared with previous published studies that only focused on economically-developed regions. By contrast, our study sample included rural regions compared to previous reports that focused on urban China or cities only, and we used the most recent data (2020) compared with those previous studies a decade ago. Our study's finding of a substantially low proportion of patients' timely access to treatment is alarming compared with those in HICs.17,18,23 Our study partly explains the reason why the use of life-saving therapies is much lower in China than in western countries.
Significantly, this study found that young/middle-aged patients have longer pre-hospital delays of 24 h compared with older adults of 23 h. In addition, young/middle-aged patients consistently reported lower rates of presenting at a hospital within 3 h across almost all subgroups, especially those living in urban China or those having severe stroke. In the sensitivity analysis of using a 2-day timeframe as an alternative, young/middle-aged patients continued to have longer OTD times.
Numerous factors may have contributed to this growing pre-hospital delay in the younger population in China. First, most educational efforts have been traditionally focused on the older population, which may have led to significantly less awareness of stroke symptoms among young/middle-aged adults. Second, young and middle-aged adults may be less likely to use emergency services (e.g., ambulance). For instance, our study found that the majority of stroke onset occurs during daytime for young/middle-aged patients, while this group of people arrived at hospitals more quickly if the onset occurred after 6 PM (non-office hours). Third, older adults generally have more comorbidities, which is reported to be associated with increased use of emergency services and awareness of self-well-being. For instance, the literature documents that patients with a history of coronary artery disease, atrial fibrillation, or a history of stroke are reported to have shorter prehospital delay times.4 Fourth, our study found that a substantially higher proportion of younger adults are heavy drinkers and smokers than older adults, which are strong indicators of non-health-seeking behaviors. Going forward, educational efforts should be focused on developing tailored educational efforts targeting young people. The educational programs should also incorporate multiple new social channels, such as WeChat, DouYin, Sina Weibo, and Tencent Video, which have become popular among the younger generation.
China is a country with diversified culture and economic imbalance with the poorest regions in the Northwest and richest regions in the Central South and Southeast. Our study found significant geographic disparities in pre-hospital delays, which could be particularly explained by the socioeconomic variations. Provinces (e.g., Gansu) with lower annual disposable income tends to have the longer median OTD time and the lower 3-h hospital arrival rates, and vice versa (eTable S6 in the Supplement). In addition to the socioeconomic status such as income, educational attainment, and employment rates, social support are risk factors for stroke and may negatively affect the effectiveness of stroke treatment24 and adversely impact the intention to seek emergency medical service [EMS] due to affordability concerns.25 North and West China have been reported to have a higher incidence and higher prevalence of vascular risk factors.26,27 Despite the higher stroke prevalence and incidence in these geographic regions, lower levels of stroke awareness and stroke knowledge largely overlaps with the regions that have a high risk of strokes and reported low socioeconomic status. In addition, there are many fewer tertiary hospitals having the ability to employ rapid response of EMS in these undeveloped regions with low socioeconomic status. This is also supported by our findings that patients living in rural areas are less likely to arrive at hospitals promptly than those living in urban areas. Lastly, a disproportionate majority of the ethnic groups of the Chinese people reside in the Northwest, such as Gansu, Xinjiang, Ningxia, and Inner Mongolia, with their diversified cultures possibly contributing to their use and ability to afford expensive EMS services.
In the “Stroke Chain of Survival” developed by the American Heart Association and the American Stroke Association, there were three specifying action areas, including symptom recognition, calling emergency medical services, and rapid response by EMS. All three aspects should be addressed together to reduce hospital arrival time to maximize post-stroke functional recovery. With the recent improvement in the EMS system, stroke-related death and disability could be attributable to these two barriers: failure to identify and failure to rescue.28 Therefore, more effort should be made to improve awareness of stroke symptoms and the ability to respond quickly to stroke onset, particularly in young and middle-aged people and those residing in geographic regions with low social-economic status. In English-speaking countries, the FAST (Facial drooping, Arm weakness, Speech problems, and Time) strategy is an easy way to inform the public about how to recognize and respond to stroke symptoms. The choice to seek medical attention was typically prompted by the most frequent stroke warning sign, which was abrupt confusion and difficulty speaking or understanding speech, followed by acute numbness or weakness on one side of the body.17 Stroke 120, a China localized tool adapted from FAST, demonstrated a promising impact in shortening prehospital delay.5,29,30 Given the huge variations in social-economic development more locally-adapted interventions like stroke 120 should be employed to improve public awareness and early detection of stroke.
There are some limitations of our study. First, despite the efforts made by BOSC to improve data quality, some data on patient characteristics (e.g., age) and NIHSS scores were not documented. Some patients and caregivers may not report the stroke onset time accurately. Second, the time of awakening was used as the time of stroke onset for patients with waking-up stroke,13,14 the OTD time might be underestimated. Third, social-economic factors that are closely associated with rurality status were not readily available in the databases. Fourth, even though the sample covers more than 200 stroke centers across 31 provinces in mainland China, our sample may not be representative, particularly for AIS patients living in rural areas or with fewer tertiary hospitals. Lastly, our research is a cross-sectional study, which does not help to establish a causal relationship among stroke patients.
Conclusions
In this study, we found that the median OTD time was 24 h, and only 11.8% of stroke patients arrived at the hospital within 3 h in China; the young/middle-aged population has higher rates of pre-hospital delays and longer OTD time, and significant rural-urban and geographic disparities exist in pre-hospital delay rates and times. Tailored intervention strategies such as Stroke 120 should be focused on the younger generations, rural residents, and geographically disadvantaged populations with low social-economic status or diversified cultures among ethnic groups across China.
Contributors
JY: conceptualization, methodology, formal analysis, writing original draft, and review & editing manuscript; ZKL: conceptualization, methodology, writing original draft, and review & editing manuscript; XX: methodology, writing original draft, and review & editing manuscript; ML: methodology, review & editing manuscript; YL: data curation, review & editing manuscript; LW: conceptualization, methodology, supervision, funding acquisition, project administration, and review & editing manuscript; RL: conceptualization, methodology, supervision, funding acquisition, project administration, and review & editing manuscript; JZ: conceptualization, methodology, supervision, funding acquisition, project administration, and review & editing manuscript.
Data sharing statement
All relevant data from the present study are included in the article. Other deidentified data are available from the corresponding author upon reasonable request following the publication of this article.
Editor note
The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
There are no financial conflicts of interest to disclose.
Acknowledgements
We acknowledge the doctors and nurses for BOSC data collection.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.lanwpc.2023.100693.
Contributor Information
Long-De Wang, Email: longde_wang@yeah.net.
Renyu Liu, Email: RenYu.Liu@pennmedicine.upenn.edu.
Jing Zhao, Email: zhao_jing@fudan.edu.cn.
Appendix A. Supplementary data
References
- 1.Wu S., Wu B., Liu M., et al. Stroke in China: advances and challenges in epidemiology, prevention, and management. Lancet Neurol. 2019;18(4):394–405. doi: 10.1016/S1474-4422(18)30500-3. [DOI] [PubMed] [Google Scholar]
- 2.National Center for Chronic Disease Prevention and Health Promotion Treat and Recover from Stroke. https://www.cdc.gov/stroke/treatments.htm#print Last Updated: April 5, 2022; Available from:
- 3.Vrudhula A., Zhao J., Liu R. Too young to have a stroke?-a global health crisis. Stroke Vasc Neurol. 2019;4(4):173–175. doi: 10.1136/svn-2019-000295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jin H., Zhu S., Wei J.W., et al. Factors associated with prehospital delays in the presentation of acute stroke in urban China. Stroke. 2012;43(2):362–370. doi: 10.1161/STROKEAHA.111.623512. [DOI] [PubMed] [Google Scholar]
- 5.Yuan J., Li M., Liu Y., et al. Analysis of time to the hospital and ambulance use following a stroke community education intervention in China. JAMA Netw Open. 2022;5(5) doi: 10.1001/jamanetworkopen.2022.12674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fang J., Yan W., Jiang G.X., Li W., Cheng Q. Time interval between stroke onset and hospital arrival in acute ischemic stroke patients in Shanghai, China. Clin Neurol Neurosurg. 2011;113(2):85–88. doi: 10.1016/j.clineuro.2010.09.004. [DOI] [PubMed] [Google Scholar]
- 7.Zhu Y., Zhang X., You S., et al. Factors associated with pre-hospital delay and intravenous thrombolysis in China. J Stroke Cerebrovasc Dis. 2020;29(8) doi: 10.1016/j.jstrokecerebrovasdis.2020.104897. [DOI] [PubMed] [Google Scholar]
- 8.Bi Q., Zhang Z., Zhang W.W., Li Q. [Study on prehospital time and influencing factors of stroke patients in 15 Chinese cities] Zhonghua Liu Xing Bing Xue Za Zhi. 2006;27(11):996–999. [PubMed] [Google Scholar]
- 9.Jiang B., Ru X., Sun H., et al. Pre-hospital delay and its associated factors in first-ever stroke registered in communities from three cities in China. Sci Rep. 2016;6 doi: 10.1038/srep29795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.von Elm E., Altman D.G., Egger M., Pocock S.J., Gøtzsche P.C., Vandenbroucke J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–1457. doi: 10.1016/S0140-6736(07)61602-X. [DOI] [PubMed] [Google Scholar]
- 11.Chao B.H., Tu W.J., Wang L.D. Initial establishment of a stroke management model in China: 10 years (2011-2020) of stroke prevention project committee, national health commission. Chin Med J (Engl) 2021;134(20):2418–2420. doi: 10.1097/CM9.0000000000001856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lyden P., Raman R., Liu L., Emr M., Warren M., Marler J. National Institutes of Health Stroke Scale certification is reliable across multiple venues. Stroke. 2009;40(7):2507–2511. doi: 10.1161/STROKEAHA.108.532069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tu W.J., Chao B.H., Ma L., et al. Case-fatality, disability and recurrence rates after first-ever stroke: a study from bigdata observatory platform for stroke of China. Brain Res Bull. 2021;175:130–135. doi: 10.1016/j.brainresbull.2021.07.020. [DOI] [PubMed] [Google Scholar]
- 14.Addo J., Ayis S., Leon J., Rudd A.G., McKevitt C., Wolfe C.D. Delay in presentation after an acute stroke in a multiethnic population in South london: the South london stroke register. J Am Heart Assoc. 2012;1(3) doi: 10.1161/JAHA.112.001685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anderson N.E., Broad J.B., Bonita R. Delays in hospital admission and investigation in acute stroke. BMJ. 1995;311(6998):162. doi: 10.1136/bmj.311.6998.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Boulanger J.M., Lindsay M.P., Gubitz G., et al. Canadian stroke best practice recommendations for acute stroke management: prehospital, emergency department, and acute inpatient stroke care, 6th edition, update 2018. Int J Stroke. 2018;13(9):949–984. doi: 10.1177/1747493018786616. [DOI] [PubMed] [Google Scholar]
- 17.Wolters F.J., Li L., Gutnikov S.A., Mehta Z., Rothwell P.M. Medical attention seeking after transient ischemic attack and minor stroke before and after the UK Face, Arm, Speech, Time (FAST) public education campaign: results from the oxford vascular study. JAMA Neurol. 2018;75(10):1225–1233. doi: 10.1001/jamaneurol.2018.1603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nishijima H., Kon T., Ueno T., et al. Effect of educational television commercial on pre-hospital delay in patients with ischemic stroke. Neurol Sci. 2016;37(1):105–109. doi: 10.1007/s10072-015-2372-1. [DOI] [PubMed] [Google Scholar]
- 19.Austin P.C. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083–3107. doi: 10.1002/sim.3697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rose K.M., Rosamond W.D., Huston S.L., Murphy C.V., Tegeler C.H. Predictors of time from hospital arrival to initial brain-imaging among suspected stroke patients: the North Carolina Collaborative Stroke Registry. Stroke. 2008;39(12):3262–3267. doi: 10.1161/STROKEAHA.108.524686. [DOI] [PubMed] [Google Scholar]
- 21.Ryu W.S., Hong K.S., Jeong S.W., et al. Association of ischemic stroke onset time with presenting severity, acute progression, and long-term outcome: a cohort study. PLoS Med. 2022;19(2) doi: 10.1371/journal.pmed.1003910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Langhorne P., Ramachandra S. Organized inpatient (stroke unit) care for stroke: network meta-analysis. Stroke. 2020;51(12):e349–e350. doi: 10.1161/STROKEAHA.120.030825. [DOI] [PubMed] [Google Scholar]
- 23.Lacy C.R., Suh D.C., Bueno M., Kostis J.B. Delay in presentation and evaluation for acute stroke: Stroke Time Registry for Outcomes Knowledge and Epidemiology (S.T.R.O.K.E.) Stroke. 2001;32(1):63–69. doi: 10.1161/01.str.32.1.63. [DOI] [PubMed] [Google Scholar]
- 24.Marshall I.J., Wang Y., Crichton S., McKevitt C., Rudd A.G., Wolfe C.D. The effects of socioeconomic status on stroke risk and outcomes. Lancet Neurol. 2015;14(12):1206–1218. doi: 10.1016/S1474-4422(15)00200-8. [DOI] [PubMed] [Google Scholar]
- 25.Yuan J., Shan G.L., Li S.D., Gao C.P., Cui L.Y., Peng B. Impact of regional differences in stroke symptom awareness and low-income status on seeking emergency medical service in China. Chin Med J (Engl) 2021;134(15):1812–1818. doi: 10.1097/CM9.0000000000001604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Xu G., Ma M., Liu X., Hankey G.J. Is there a stroke belt in China and why? Stroke. 2013;44(7):1775–1783. doi: 10.1161/STROKEAHA.113.001238. [DOI] [PubMed] [Google Scholar]
- 27.Liu M., Wu B., Wang W.Z., Lee L.M., Zhang S.H., Kong L.Z. Stroke in China: epidemiology, prevention, and management strategies. Lancet Neurol. 2007;6(5):456–464. doi: 10.1016/S1474-4422(07)70004-2. [DOI] [PubMed] [Google Scholar]
- 28.Wang D., Wang Y. Tissue window, not the time window, will guide acute stroke treatment. Stroke Vasc Neurol. 2019;4(1):1–2. doi: 10.1136/svn-2018-000211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Yong Wang Y.L., Dou Li, Zheng Kunwen, Chi Feng, Zhao Jing. Recent developments in ischemic stroke prehospital care from stroke 120 special task forces. Transl Perioper Pain Med. 2021;8(2):342–345. [Google Scholar]
- 30.Zhao J., Liu R. Stroke 1-2-0: a rapid response programme for stroke in China. Lancet Neurol. 2017;16(1):27–28. doi: 10.1016/S1474-4422(16)30283-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.